Beruflich Dokumente
Kultur Dokumente
Adam Victors GBR
Hochgeladen von
Fandie PratamaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Adam Victors GBR
Hochgeladen von
Fandie PratamaCopyright:
Verfügbare Formate
1124 PART 5 DISEASES OF SPINAL CORD, PERIPHERAL NERVE, AND MUSCLE
tral and dorsal roots, and dorsal root ganglia and
along the entire length of the peripheral nerves.
Sparse focal infiltrates of inflammatory cells (lym-
phocytes and other mononuclear cells) may also be
found in lymph nodes, liver, spleen, heart, and other
organs. Swelling of nerve roots at the site of their
A dural exit has been emphasized by some authors and
theorized to cause root damage.
Variations of this pattern of peripheral nerve
damage have been observed, each perhaps repre-
senting a different immunopathology. Rarely, in a
clinically typical case, there may be widespread de-
myelinative changes and only a paucity of perivas-
cular lymphocytes. In patients whose electrophysi-
ologic tests display severe axonal damage early in
the illness as discussed later, the pathologic findings
B corroborate the predominantly axonal nature of the
disease with secondary myelin damage and little in-
flammatory response. An occasional case has shown
an inflammatory process with primary axonal dam-
age rather than demyelination (Honovar et al).
Pathogenesis and Etiology Most of the evidence
supports a cell-mediated immunologic reaction di-
rected at peripheral nerve. Waksman and Adams
demonstrated that experimentally induced periph-
eral nerve disease (experimental allergic neuritis, or
C
EAN), clinically and pathologically indistinguish-
able from GBS, develops in animals 2 weeks after
immunization with peripheral nerve homogenates.
Brostoff and colleagues suggested that the antigen
in this reaction is a basic protein, designated P2,
found only in peripheral nerve myelin. Subsequent
investigations by these authors indicated that the
neuritogenic factor might be a specific peptide in the
P2 protein. However, it has become evident that
there is no dominant antigen-antibody reaction in
D GBS and that any number of myelin and axonal el-
ements may be involved in inciting the immune re-
action. The pathologic steps in this proposed reac-
tion are diagrammatically illustrated in Fig. 46-3.
Figure 46-3. Diagram of probable cellular events in acute inflammatory polyneuropathy Hartung and colleagues have found high levels of
(Guillain-Barré syndrome). A. Lymphocytes attach to the walls of endoneurial vessels and soluble interleukin (IL)-2 receptors, that is shed
migrate through the vessel wall, enlarging and transforming as they do so. At this stage no
from activated T cells, and IL-2 itself in the serum
nerve damage has occurred. B. More lymphocytes have migrated into the surrounding tissue.
of patients with acute GBS, reflecting activation of
The first effect on the nerve is breakdown of myelin, the axon being spared (segmental
demyelination). This change appears to be mediated by the mononuclear exudate, but the these cells. As noted below, complement also seems
mechanism is uncertain. C. The lesion is more intense, polymorphonuclear leukocytes being to be a necessary factor in the initial attack on my-
present as well as lymphocytes. There is interruption of the axon in addition to myelin sheath elin.
damage; as a result, the muscle undergoes denervation atrophy and the nerve cell body shows Although the transmission of EAN by T cells
central chromatolysis. If the axonal damage is distal, the nerve cell body will survive, and sensitized to myelin is strong evidence of their role
regeneration and clinical recovery is likely. If, as in D, axonal interruption has occurred in GBS, antimyelin antibodies are probably involved
proximally because of a particularly intense root or proximal nerve lesion, the nerve cell body in the initial part in the disease. The serum from
may die and undergo dissolution. In this situation, there is no regeneration, only the possibility patients with GBS causes damage to myelin in tissue
of collateral reinnervation of muscle from surviving motor fibers. (From Asbury et al, 1969,
cultures and induces a characteristic (“vesicular”)
by permission.)
form of myelin destruction. Subepineural injection
of serum from GBS patients into the sciatic nerve of
virtually all cases show perivascular (mainly perivenous) lympho- rats leads to local demyelination and electrical conduction block.
cytic infiltrates. Later, the characteristic inflammatory cell infil- The studies by Koski and associates of complement-dependent my-
trates and perivenous demyelination are combined with segmental elin damage by IgM antimyelin antibodies in GBS provided evi-
demyelination and a variable degree of wallerian degeneration. The dence that antimyelin antibodies are able to initiate myelin destruc-
cellular infiltrates are scattered throughout the cranial nerves, ven- tion even though T cells and that macrophages are the ultimate
1150 PART 5 DISEASES OF SPINAL CORD, PERIPHERAL NERVE, AND MUSCLE
locities, but there is no conduction block as occurs in other acquired perature-dependent pattern is the most characteristic feature of the
demyelinating polyneuropathies. The pathologic changes are most disease as pointed out by our colleague T. Sabin. The sensory maps
intense in the distal segments of the nerves, with the expected chro- he has drawn (Fig. 46-4) are typical of established cases. The nose,
matolysis of their cell bodies. earlobes, and elbows may be affected early as a result of the cool-
The cause of uremic polyneuropathy is unknown. What has ness of the skin in those areas. The process evolves over years.
been called the “middle molecule” theory is plausible. The end Eventually the anesthesia spreads to involve most of the cutaneous
stage of renal failure is associated with the accumulation of toxic surface. Extensive sensory loss is followed by impaired motor func-
substances in the range of 300 to 2000 molecular weight. Further- tion owing to invasion of muscular nerves where they lie closest
more, the concentration of these substances, which include meth- to the skin (the ulnar nerve is the most vulnerable). There is a loss
ylguanidine and myoinositol, has been shown to correlate with the
degree of neurotoxicity (Funck-Brentano et al). These toxins (and
the clinical signs of neuropathy) are not greatly reduced by chronic
hemodialysis. In contrast, the transplanted kidney effectively elim-
inates substances of wide-ranging molecular weights, which would
account for the almost invariable improvement of neuropathy after
transplantation. As is the case with uremic encephalopathy, urea
alone given to experimental animals and in controlled studies
of humans, does not seem capable of inducing a metabolic neu-
ropathy.
Alcoholic-Nutritional Polyneuropathy (See page 989 and Chap.
41) In all patients with alcoholic-nutritional polyneuropathy who
for some reason remain untreated with vitamin and protein resto-
ration, the weakness and atrophy of the legs, and to a lesser extent
the arms, may reach an extreme degree. Thus this disease, though
subacute in its evolution as described earlier in the chapter, be-
comes a frequent cause of chronic polyneuropathy. There are usu-
ally prominent sensory features and considerable acral pain and
allodynia. Certain cases of diabetic neuropathy behave similarly.
Leprous Polyneuritis This is the classic example of an infectious
neuritis, due to the direct invasion of nerves by the acid-fast My-
cobacterium leprae. The disease is still frequent in India and Cen-
tral Africa, but there are many lesser endemic foci including parts
of South America and of Florida, Texas, and Louisiana that border
on the Gulf of Mexico.
The initial lesion in leprosy is an innocuous-appearing skin
macule or papule, which is often hypopigmented and lacking in
sensation and is caused by the invasion of cutaneous nerves by M.
leprae. In patients with a degree of immunologic resistance to in-
fection the disease may progress no further than this stage, which
is spoken of as indeterminate leprosy, or it may evolve in several
ways, depending mainly upon the resistance of the host. The bacilli
may be locally invasive, producing a circumscribed epithelioid
granuloma that involves cutaneous and subcutaneous nerves and
results in a characteristic hypopigmented patch of superficial numb-
ness and sensory loss (tuberculoid leprosy). The underlying sub-
cutaneous sensory nerves may be palpably enlarged. If a large nerve
in the vicinity of the granuloma is invaded (the ulnar, median,
peroneal, posterior auricular, and facial nerves are most frequently
affected), a sensorimotor deficit in the distribution of that nerve is
added to the patch of cutaneous anesthesia.
In contrast to the limited tuberculoid variety of leprosy, lack
of resistance to the organism permits the proliferation and hema-
togenous spread of bacilli and the diffuse infiltration of skin, ciliary
bodies, testes, lymph nodes, and nerves (lepromatous leprosy).
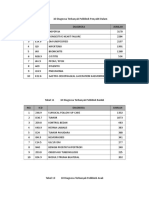
Figure 46-4. Patterns of sensory loss in leprosy. The localization of these
Widespread invasion of the cutaneous nerves produces a symmet- areas to cooler portions of the body is unique to this disorder. Shown in
rical pattern of pain and temperature loss involving the pinnae of the upper figure is the sparing of the palmar and antecubital surfaces and
the ears as well as the dorsal surfaces of hands, forearms, and feet variation in the sensation within the distribution of a single sensory nerve.
and anterolateral aspects of the legs— a distribution that is deter- In the lower figure, almost universal analgesia is found but there is still
mined by the relative coolness of these parts of the skin. This tem- sparing of warmer regions of skin. (From Sabin with permission.)
Das könnte Ihnen auch gefallen
- Drugs For Diabetes MellitusDokument3 SeitenDrugs For Diabetes MellitusGerardLum100% (1)
- Aarushi Crime Scene AnalysisDokument13 SeitenAarushi Crime Scene AnalysisToronto Star90% (10)
- Autoimmune EncephalitisDokument9 SeitenAutoimmune Encephalitispiero reyesNoch keine Bewertungen
- Peroneal Nerve Palsy PDFDokument10 SeitenPeroneal Nerve Palsy PDFChristian Reza WibowoNoch keine Bewertungen
- Neurology Multiple Choice Questions With Explanations: Volume IVon EverandNeurology Multiple Choice Questions With Explanations: Volume IBewertung: 4 von 5 Sternen4/5 (7)
- Essentials of Microbiology 1st Edition PDFDokument648 SeitenEssentials of Microbiology 1st Edition PDFJohn Khna100% (1)
- How A Breath Is Delivered: OutlineDokument16 SeitenHow A Breath Is Delivered: OutlineLesly Peinado TorresNoch keine Bewertungen
- Orogastric Tube InsertionDokument5 SeitenOrogastric Tube InsertionUday KumarNoch keine Bewertungen
- 34 - Polyneuropathy Classification by NCS and EMGDokument16 Seiten34 - Polyneuropathy Classification by NCS and EMGMutiara Kristiani PutriNoch keine Bewertungen
- Autoimmune Axonal Neuropathies. 2023Dokument15 SeitenAutoimmune Axonal Neuropathies. 2023Arbey Aponte PuertoNoch keine Bewertungen
- Diabetic Foot Care Center:: One Stop Service For The Management of Diabetic Foot ProblemsDokument29 SeitenDiabetic Foot Care Center:: One Stop Service For The Management of Diabetic Foot ProblemsscribdNoch keine Bewertungen
- PACES 21 - Communication Skills and EthicsDokument10 SeitenPACES 21 - Communication Skills and EthicsDrShamshad Khan100% (1)
- Combat Boot Palsy: Case Reports: F. GafensDokument3 SeitenCombat Boot Palsy: Case Reports: F. GafensAbdelghani MILIANINoch keine Bewertungen
- Peripheral Nerve Repair and RegenerationDokument15 SeitenPeripheral Nerve Repair and RegenerationjaimeaquilesrinconNoch keine Bewertungen
- Steroid For AINDokument3 SeitenSteroid For AINGadisa DejeneNoch keine Bewertungen
- Peripheral - Nerve - Disorders - (PG - 24 25)Dokument2 SeitenPeripheral - Nerve - Disorders - (PG - 24 25)Fayeann Vedor LoriegaNoch keine Bewertungen
- Ann MS Id 000849Dokument8 SeitenAnn MS Id 000849azucenadeoNoch keine Bewertungen
- Neurplast en El Estres y ATDduman1999 PDFDokument11 SeitenNeurplast en El Estres y ATDduman1999 PDFmarielaNoch keine Bewertungen
- Axelrod 2004Dokument12 SeitenAxelrod 2004Nesa An YahdiyaniNoch keine Bewertungen
- Letters To The Editor: Takuya Konno, MD, PHD Zbigniew K. Wszolek, MDDokument3 SeitenLetters To The Editor: Takuya Konno, MD, PHD Zbigniew K. Wszolek, MDIkaNoch keine Bewertungen
- Rsob 180138Dokument19 SeitenRsob 180138ilmiah neurologiNoch keine Bewertungen
- ChunDokument3 SeitenChungassemNoch keine Bewertungen
- 25 Patofisiologi EpilepsiDokument13 Seiten25 Patofisiologi EpilepsiWisnuBaskoroNoch keine Bewertungen
- References: Alopecia Areata After Biologic Therapy: Report of A Case Related To AdalimumabDokument2 SeitenReferences: Alopecia Areata After Biologic Therapy: Report of A Case Related To AdalimumabMasithaNoch keine Bewertungen
- Vestibular Neuritis, or Driving Dizzily Through Donegal: PerspectiveDokument2 SeitenVestibular Neuritis, or Driving Dizzily Through Donegal: PerspectiveBono GatouzouNoch keine Bewertungen
- Nervous System Lupus: Pathogenesis and Rationale For TherapyDokument11 SeitenNervous System Lupus: Pathogenesis and Rationale For TherapymortazaqNoch keine Bewertungen
- Autoimmune EncephalitisDokument14 SeitenAutoimmune EncephalitisMarco Antonio KoffNoch keine Bewertungen
- Mech HBO BurasDokument5 SeitenMech HBO BurasmedicinahiperbaricaNoch keine Bewertungen
- Breakthroughs in Antemortem Diagnosis of Neurodegenerative DiseasesDokument3 SeitenBreakthroughs in Antemortem Diagnosis of Neurodegenerative DiseasesVijay PrajapatiNoch keine Bewertungen
- Small Fiber Neuropathy: A Burning Problem: ReviewDokument9 SeitenSmall Fiber Neuropathy: A Burning Problem: Reviewdvm22029719Noch keine Bewertungen
- Pathology of Neurodegenerative DiseasesDokument23 SeitenPathology of Neurodegenerative DiseasesMauro GasparofNoch keine Bewertungen
- Special Feature: Definition of The Clinical Spectrum of Kernicterus and Bilirubin-Induced Neurologic Dysfunction (BIND)Dokument6 SeitenSpecial Feature: Definition of The Clinical Spectrum of Kernicterus and Bilirubin-Induced Neurologic Dysfunction (BIND)Abd. Rahim MubarakNoch keine Bewertungen
- Terapias para Doenças NeurodegenerativasDokument41 SeitenTerapias para Doenças Neurodegenerativasaurora cavalcantiNoch keine Bewertungen
- 412 FullDokument14 Seiten412 FullDennyNoch keine Bewertungen
- Envoi Par E-Mail 412.fullDokument14 SeitenEnvoi Par E-Mail 412.fullalmarazneurologiaNoch keine Bewertungen
- Distal Axonopathy: One Neurotoxic: Common Type of LesionDokument9 SeitenDistal Axonopathy: One Neurotoxic: Common Type of LesionshreyasNoch keine Bewertungen
- Nerve Conduction Studies: Australian Family Physician September 2011Dokument6 SeitenNerve Conduction Studies: Australian Family Physician September 2011anjelikaNoch keine Bewertungen
- Bianda Axanditya 22010110130181 Bab2ktiDokument10 SeitenBianda Axanditya 22010110130181 Bab2ktimeiutaNoch keine Bewertungen
- Acute Manifestations of Neuromuscular DiseaseDokument10 SeitenAcute Manifestations of Neuromuscular DiseasetsyrahmaniNoch keine Bewertungen
- Autoimmune Vestibulocerebellar SyndromesDokument19 SeitenAutoimmune Vestibulocerebellar Syndromesrafael rocha novaesNoch keine Bewertungen
- Subjective Cues:: Study of Illness Condition (Sic) Assessment Anatomy Physiology Pathophysiology AnalysisDokument5 SeitenSubjective Cues:: Study of Illness Condition (Sic) Assessment Anatomy Physiology Pathophysiology AnalysisSyed FlyntNoch keine Bewertungen
- Gene-Environment Interactions in Psychiatry: Joining Forces With NeuroscienceDokument8 SeitenGene-Environment Interactions in Psychiatry: Joining Forces With Neurosciencefakeusername01Noch keine Bewertungen
- Scwarthz InflamationDokument14 SeitenScwarthz InflamationHidayati MaulidaNoch keine Bewertungen
- Physiology and Pathophysiology of Chronic Pain: Nicole Bentley, Ahmed J. Awad, Parag G. PatilDokument9 SeitenPhysiology and Pathophysiology of Chronic Pain: Nicole Bentley, Ahmed J. Awad, Parag G. Patilmuzammilia nadrainiNoch keine Bewertungen
- Definition of The Clinical Spectrum of KernicterusDokument7 SeitenDefinition of The Clinical Spectrum of KernicterusFidelis OgonnaNoch keine Bewertungen
- Mcanism B NeurodegenerativeDokument13 SeitenMcanism B NeurodegenerativeAlin CiubotaruNoch keine Bewertungen
- The Role of Nuclear Macromolecules in Innate Immunity: David S. PisetskyDokument5 SeitenThe Role of Nuclear Macromolecules in Innate Immunity: David S. PisetskygermanNoch keine Bewertungen
- Autoimmune Encephalitis: Pathophysiology and Imaging Review of An Overlooked DiagnosisDokument9 SeitenAutoimmune Encephalitis: Pathophysiology and Imaging Review of An Overlooked DiagnosisAulya ArchuletaNoch keine Bewertungen
- Chapter-165Dokument9 SeitenChapter-165Tizazu BayihNoch keine Bewertungen
- Multiple System Atrophy: Cellular and Molecular Pathology: D J Burn, E JarosDokument8 SeitenMultiple System Atrophy: Cellular and Molecular Pathology: D J Burn, E Jarosuzair khanNoch keine Bewertungen
- LanzkowskyPhili 2011 DecreasedPolymorphonu ManualOfPediatricHemaDokument11 SeitenLanzkowskyPhili 2011 DecreasedPolymorphonu ManualOfPediatricHemaPaola DiazNoch keine Bewertungen
- Arch Dis Child 2003 Stonehouse 122 4Dokument4 SeitenArch Dis Child 2003 Stonehouse 122 4carlaNoch keine Bewertungen
- Prion BrainDokument2 SeitenPrion BrainD SNoch keine Bewertungen
- Chronic Traumatic Encephalopathy The Cellular Sequ - 2017 - Journal of ClinicalDokument6 SeitenChronic Traumatic Encephalopathy The Cellular Sequ - 2017 - Journal of ClinicalBruno MañonNoch keine Bewertungen
- Multifocal Motor Neuropathy.Dokument4 SeitenMultifocal Motor Neuropathy.zaquvubeNoch keine Bewertungen
- Gruen 2007Dokument2 SeitenGruen 2007cristianNoch keine Bewertungen
- Postictal Todd's Paralysis Associated With Focal Cerebral Hypoperfusion On Magnetic Resonance Perfusion StudiesDokument3 SeitenPostictal Todd's Paralysis Associated With Focal Cerebral Hypoperfusion On Magnetic Resonance Perfusion StudiesNisa UcilNoch keine Bewertungen
- Fibromyalgiainprimarycare: Jay B. HiggsDokument17 SeitenFibromyalgiainprimarycare: Jay B. HiggsAndres PoloNoch keine Bewertungen
- Out PDFDokument12 SeitenOut PDFMaria RenjaanNoch keine Bewertungen
- Role of Neuroinflammation in Neurodegeneration DevelopmentDokument32 SeitenRole of Neuroinflammation in Neurodegeneration Developmentelibb346Noch keine Bewertungen
- Lumbar Spinal Stenosis Causing Intermittent PriapismDokument8 SeitenLumbar Spinal Stenosis Causing Intermittent PriapismLuis PNoch keine Bewertungen
- Uhthoff's Phenomena in MS-clinical Features and PathophysiologyDokument6 SeitenUhthoff's Phenomena in MS-clinical Features and PathophysiologyEduardo MarinhoNoch keine Bewertungen
- Mechanisms of Neuropathic PainDokument14 SeitenMechanisms of Neuropathic Painfahri azwarNoch keine Bewertungen
- General Anesthesia NEJM 2010 DR Emeri BrownDokument16 SeitenGeneral Anesthesia NEJM 2010 DR Emeri BrownJuli OrtixNoch keine Bewertungen
- 2022 Beaudin Revue Ataxie Cereb RecessiveDokument16 Seiten2022 Beaudin Revue Ataxie Cereb RecessiveLéo VidoniNoch keine Bewertungen
- Sepsis-Associated Encephalopathy and Its Differential DiagnosisDokument6 SeitenSepsis-Associated Encephalopathy and Its Differential DiagnosisMUHAMMAD ARIQ FAKHRIDITOMO TAUFIQNoch keine Bewertungen
- 04 Tetanus BDokument12 Seiten04 Tetanus BRahmatul YasiroNoch keine Bewertungen
- Ob2 Sas 40Dokument7 SeitenOb2 Sas 40????Noch keine Bewertungen
- Eastern Bacoor National High School: Queen's Aisle ST., Queen's Row Central, Bacoor City, Cavite Tel. No. (046) 484-3202Dokument2 SeitenEastern Bacoor National High School: Queen's Aisle ST., Queen's Row Central, Bacoor City, Cavite Tel. No. (046) 484-3202Editha BonaobraNoch keine Bewertungen
- BTG 402 - Biotechnology - 2022Dokument37 SeitenBTG 402 - Biotechnology - 2022Emmanuella OffiongNoch keine Bewertungen
- WT OetDokument13 SeitenWT OetRomana PereiraNoch keine Bewertungen
- Part Abs SamplesDokument12 SeitenPart Abs SamplesgenalinangNoch keine Bewertungen
- MicromedextwoDokument60 SeitenMicromedextwoDaniel Martínez SilvaNoch keine Bewertungen
- Kawasaki Disease: A Comprehensive Review: Kamleshun Ramphul, Stephanie Gonzalez MejiasDokument5 SeitenKawasaki Disease: A Comprehensive Review: Kamleshun Ramphul, Stephanie Gonzalez MejiasAmarantoNoch keine Bewertungen
- Antimicrobial FinalDokument227 SeitenAntimicrobial FinalAbdulrhman MekawyNoch keine Bewertungen
- Tonsillectomy and Adenoidectomy - Pediatric Clinics of North AmericaDokument13 SeitenTonsillectomy and Adenoidectomy - Pediatric Clinics of North AmericayosefNoch keine Bewertungen
- Daftar Pasien RSUP H. Adam Malik Medan - Senin, 24 Juli 2023Dokument3 SeitenDaftar Pasien RSUP H. Adam Malik Medan - Senin, 24 Juli 2023Admin neuro-usu.idNoch keine Bewertungen
- Finecare PlusDokument2 SeitenFinecare PlusMon John GascoNoch keine Bewertungen
- 8326L - MAGPALI VAN HALEN - Activity 3Dokument3 Seiten8326L - MAGPALI VAN HALEN - Activity 3Van HalenNoch keine Bewertungen
- Cronicon: Integrative Case Study Supraspinatus Tendinitis and Physical Therapy ManagementDokument4 SeitenCronicon: Integrative Case Study Supraspinatus Tendinitis and Physical Therapy ManagementAnandhu GNoch keine Bewertungen
- Assessment Nursing Diagnosis Scientific Explanation Planning Implementation Rationale EvaluationDokument3 SeitenAssessment Nursing Diagnosis Scientific Explanation Planning Implementation Rationale EvaluationNurse NotesNoch keine Bewertungen
- Virtual Notebook 1.1.3 Part 2 - Notebook - Day 2Dokument6 SeitenVirtual Notebook 1.1.3 Part 2 - Notebook - Day 2Justice JensenNoch keine Bewertungen
- Pi Care of Third and Fourth Degree Tears OasiDokument6 SeitenPi Care of Third and Fourth Degree Tears OasiPetros Akin-NibosunNoch keine Bewertungen
- Shoulder Pain in Hemiplegia: Statistical Relationship With Five VariablesDokument3 SeitenShoulder Pain in Hemiplegia: Statistical Relationship With Five VariablesSahithya MNoch keine Bewertungen
- Post-Cardiac Arrest Management in Adults - UpToDateDokument34 SeitenPost-Cardiac Arrest Management in Adults - UpToDatehatsune100% (1)
- Studi Kasus: Kehamilan Dengan: Dengan Katub Jantung Prostetik Mekanik Dan Penggunaan AntikoagulanDokument10 SeitenStudi Kasus: Kehamilan Dengan: Dengan Katub Jantung Prostetik Mekanik Dan Penggunaan AntikoagulanMonyet...Noch keine Bewertungen
- Acne Basics: Pathophysiology, Assessment, and Standard Treatment OptionsDokument9 SeitenAcne Basics: Pathophysiology, Assessment, and Standard Treatment OptionsSyahdi Nugraha KadafiNoch keine Bewertungen
- 10 Diagnosa PenyakitDokument3 Seiten10 Diagnosa PenyakitDiny Rachma Putri HNoch keine Bewertungen
- Pharmaceutical Biotechnology-QBDokument8 SeitenPharmaceutical Biotechnology-QBprateekshaNoch keine Bewertungen