Beruflich Dokumente
Kultur Dokumente
Postoperative Neck Ultrasonography Surveillance After Thyroidectomy in Patients With Medullary Thyroid Carcinoma: A Multicenter Study
Hochgeladen von
César EscalanteOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Postoperative Neck Ultrasonography Surveillance After Thyroidectomy in Patients With Medullary Thyroid Carcinoma: A Multicenter Study
Hochgeladen von
César EscalanteCopyright:
Verfügbare Formate
Original Research
published: 15 March 2018
doi: 10.3389/fendo.2018.00102
Postoperative neck Ultrasonography
surveillance after Thyroidectomy
in Patients With Medullary Thyroid
carcinoma: a Multicenter study
Hye Shin Ahn1, Dong Wook Kim2*, Yoo Jin Lee2, Chang Yoon Lee3, Ji-hoon Kim4,
Yoon Jung Choi 5, Song Lee 6, Inseon Ryoo7, Jung Yin Huh8, Jin Yong Sung9,
Jin Young Kwak10 and Hye Jin Baek11
1
Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, South Korea,
2
Department of Radiology, Busan Paik Hospital, Inje University College of Medicine, Busan, South Korea, 3 Department of
Radiology, Research Institute and Hospital, National Cancer Center, Gyeonggi, South Korea, 4 Department of Radiology,
Seoul National University Hospital, Seoul National University College of Medicine, Seoul, South Korea, 5 Department of
Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, South Korea, 6 Department of
Radiology, Chak Han Madi Hospital, Incheon, South Korea, 7 Department of Radiology, Korea University Guro Hospital,
Korea University College of Medicine, Seoul, South Korea, 8 Department of Radiology and Research Institute of Radiology,
University of Ulsan College of Medicine, Asan Medical Center, Seoul, South Korea, 9 Department of Radiology, Thyroid
Center, Daerim St. Mary’s Hospital, Seoul, South Korea, 10 Department of Radiology, Severance Hospital, Research Institute
Edited by: of Radiological Science, Yonsei University College of Medicine, Seoul, South Korea, 11 Department of Radiology, Gyeongsang
Antongiulio Faggiano, National University School of Medicine, Gyeongsang National University Changwon Hospital, Changwon, South Korea
University of Naples Federico II, Italy
Reviewed by:
Background: For detecting tumor recurrence of medullary thyroid carcinoma (MTC)
Caterina Mian,
Università degli Studi di Padova, Italy in the neck, an appropriate frequency and interval of postoperative ultrasonography
Pasqualino Malandrino, (US) surveillance remains unclear. This study aimed to assess an appropriate interval
Department of Clinical and
Experimental Medicine, Italy and frequency of postoperative neck US surveillance for detecting tumor recurrence in
*Correspondence: patients who had undergone thyroid surgery due to MTC.
Dong Wook Kim
dwultra@nate.com
Methods: A total of 86 patients who had undergone thyroid surgery for the treatment of
MTC and had at least one postoperative US follow-up examination at any of nine affili-
Specialty section: ated hospitals were included. Postoperative follow-up US, clinical, and histopathological
This article was submitted to
results of patients were reviewed. The tumor recurrence/persistence rate of MTC was
Cancer Endocrinology,
a section of the journal investigated, and the interval and session number of postoperative follow-up US and
Frontiers in Endocrinology clinicopathologic factors were compared between tumor recurrence/persistence and
Received: 28 December 2017 non-recurrence groups.
Accepted: 01 March 2018
Published: 15 March 2018 results: Of the 86 patients, 22 (25.6%) showed tumor recurrence/persistence. Of the
Citation: 22 patients with tumor recurrence/persistence, 11 (50%) showed structural recurrence/
Ahn HS, Kim DW, Lee YJ, Lee CY,
Kim J-h, Choi YJ, Lee S, Ryoo I,
persistence in the neck on follow-up US. In these 11 patients, the mean interval and
Huh JY, Sung JY, Kwak JY and session number of postoperative follow-up US between initial surgery and the first US
Baek HJ (2018) Postoperative Neck
detection of recurrence/persistence was 41.3 ± 39.3 months (range, 6–128 months) and
Ultrasonography Surveillance After
Thyroidectomy in Patients With 2.6 ± 2.3 (range, 1–8), respectively. On follow-up US, 6 (54.5%, 6/11) were diagnosed
Medullary Thyroid Carcinoma: A with tumor recurrence/persistence within 3 years of the initial surgery. Tumor recurrence/
Multicenter Study.
Front. Endocrinol. 9:102.
persistence was significantly correlated with TNM stage (p < 0.001) and multiplicity/
doi: 10.3389/fendo.2018.00102 bilaterality (p = 0.013).
Frontiers in Endocrinology | www.frontiersin.org 1 March 2018 | Volume 9 | Article 102
Ahn et al. Postoperative Neck US in MTC Patients
Keywords: thyroid, malignancy, medullary thyroid carcinoma, ultrasonography, recurrence, surveillance
INTRODUCTION nature of the study. From January 2005 to April 2011, only
patients who met the following criteria were consecutively
Medullary thyroid carcinoma (MTC) is an uncommon thyroid included, although the start time for patient selection differed
cancer which accounts for 3–10% of all thyroid cancers (1, 2). among the institutions due to the scarcity and variations in the
MTCs are derived from the parafollicular C-cells that produce number of MTC cases at each institution: (1) patients who had
calcitonin, and serum calcitonin level is known to be a sensitive undergone thyroid surgery for the treatment of MTC, (2) patients
and specific marker for MTC (3). However, several reports sug- who had at least one postoperative US follow-up examination
gest that advanced MTC may dedifferentiate with a subsequent during the follow-up period, (3) patients who had been clinical
decrease in calcitonin production (4, 5). followed-up for more than 5 years after the initial thyroid surgery,
The prognosis of MTC is intermediate between differentiated and (4) patients in which the presence or absence of tumor recur-
and anaplastic thyroid carcinomas (1). The natural course of rence/persistence could be determined. Ultimately, a total of 86
MTC varies from very slow progression or stable disease extend- patients (53 women and 33 men, age range 7–76 years, mean age
ing over decades to rapid progression and survival of just a few 53.1 ± 11.8 years) were included in the study.
years (1). The reported 5-year survival of MTC is 78–91%, and
the reported 10-year survival is 61–88% (1, 6). Distant metastasis, Neck US Examinations and Follow-ups
which is reportedly observed at initial presentation in 7–23% of All US examinations were performed using one of the following
patients, is known to be the main cause of MTC-related mortality high-resolution US systems: (1) iU 22 (Philips Medical Systems,
(7). Distant metastasis, older age at diagnosis, and more advanced Bothell, WA, USA), (2) HDI 5000 (Philips Medical Systems,
primary tumor or nodal stage have been proposed as prognostic Bothell, WA, USA), (3) LOGIQ9 (GE Healthcare, Milwaukee,
factors for adverse outcomes (8, 9). Also, serum kinetics of MTC WI, USA), (4) Aplio SSA-770A (Toshiba Medical Systems,
markers, such as calcitonin and carcinoembryonic antigen, may Tokyo, Japan), and (5) EUB-7500 (Hitachi Medical Corporation,
be alternative predictors of survival (10). Tokyo, Japan). A 5–12-MHz or an 8–15-MHz linear-array
Thyroid ultrasonography (US) has been used to differenti- transducer was used. Faculty radiologists specializing in head-
ate between malignant and benign thyroid nodules, to guide and-neck imaging or supervised board-certified radiologist
fine-needle aspiration of suspicious thyroid nodules, and to who were participating in head-and-neck radiology fellowship
detect tumor recurrence after thyroid surgery (11, 12). Due to training performed all US examinations. Postoperative US
an increase in thyroid US screening, the detection rate of small follow-up in MTC patients was commonly performed at 0.5-,
thyroid cancers has increased substantially, and earlier detection 1-, or 2-year intervals at each institution. The following features
of smaller MTCs is possible (13–15). In particular, Elisei et al. were investigated via US examination: suspicious thyroid nod-
reported US follow-up results including the neck in patients who ules in the remnant thyroid gland, masses in the postoperative
had undergone thyroid surgery due to MTC (16). They recom- thyroid bed and perithyroidal neck area, and suspicious lymph
mended that postoperative neck US be undertaken at interval of nodes or masses in the neck. In all patients, the interval (i.e.,
6–12 months. However, this may be too short interval, and can period between the initial surgery and postoperative follow-up
result in unnecessary medical costs. To the best of our knowl- US examination) and session number of postoperative follow-
edge, an appropriate interval for postoperative US surveillance up US were investigated. In the tumor recurrence/persistence
remains unclear. This study aimed to determine the detection group, the interval and session number of postoperative neck
rate of tumor recurrence/persistence and characteristics of post- US where tumor recurrence/persistence was first detected were
operative follow-up US in MTC patients by analyzing follow-up recorded.
US results in patients who had undergone thyroid surgery due
to MTC.
Thyroid Surgery and Histopathology
Thyroid surgery was performed by board-certified surgeons of the
MATERIALS AND METHODS affiliated hospitals. The extent of thyroid surgery was determined
by multiple factors, including patient age, family history, tumor
Patients size, extrathyroidal tumor extension, multifocality, bilaterality,
This retrospective analysis was based on patient data collected nodal metastasis, and distant metastasis. In the histopathological
from nine university-affiliated hospitals. The institutional review analysis, the intraglandular location of the MTC, perithyroidal
boards of all participating institutions approved the study, and the tumor invasion within or beyond surgical margins, nodal metas-
need for informed consent was waived due to the retrospective tasis, and the presence of satellite MTC were recorded.
Frontiers in Endocrinology | www.frontiersin.org 2 March 2018 | Volume 9 | Article 102
Ahn et al. Postoperative Neck US in MTC Patients
Classification of Tumor Recurrence/ were compared using Student’s t-test. A p <0.05 was considered
Persistence and Non-Recurrence to indicate statistical significance. The prevalence of MTC recur-
Nine board-certified radiologists from each of the affiliated rence/persistence was calculated, and the interval and session
hospitals retrospectively reviewed the postoperative follow- number of postoperative follow-up US were compared between
up US, clinical, and histopathological results of the patients the recurrence/persistence and non-recurrence groups. Also, we
included in the study. The size, location, multiplicity, and TNM assessed correlations between tumor recurrence/persistence and
stage of tumors were investigated on the basis of US images and variable clinicopathological factors, to predict prognosis.
histopathological results. TNM stage was based on the guidelines
of the American Joint Committee on Cancer (17). The sites of RESULTS
recurrence/persistence were classified as nodal, non-nodal, or
unknown. Non-nodal recurrence/persistence was defined as the Of the 86 patients, the mean size of the primary MTC was
presence of an MTC in the remnant thyroid gland, postopera- 16.9 ± 13.7 mm (range 3.0–88.6 mm). The locations of the pri-
tive thyroid bed, or perithyroidal neck area during the follow- mary MTC included the right lobe (n = 59), the left lobe (n = 26),
up period after surgery as determined via histopathological and the isthmus (n = 1). Thyroid surgery was performed in all
examinations. Nodal recurrence/persistence was defined as the 86 patients, and the TNM stages based on histopathology of
presence of a metastatic lymph node from MTC in the neck the surgical specimens are shown in Table 1. More than 50% of
area during the follow-up period after surgery. US features of patients were diagnosed with intraglandular MTC. There were no
metastatic lymph nodes and local recurrent masses in the opera- cases of tumor invasion into the adjacent tracheal or esophageal
tive bed were characterized in accordance with previous reports wall. Nodal metastases in the lateral neck were demonstrated in
(18, 19). In patients with tumor recurrence/persistence, the loca-
tion, diagnostic method, and management of tumor recurrence/ Table 1 | Demographics and characteristics in the 86 patients.
persistence were reviewed. An interval and session number of
postoperative follow-up US were also recorded. Items
Serum calcitonin levels at the time of initial preoperative labo- Age (mean ± SD, years) 53.1 ± 11.8 (range, 7–76)
ratory investigations and final serologic tests were investigated. Sex Female: male = 53 (61.6):
In the patients with tumor recurrence/persistence, the serum 33 (38.4)
calcitonin level at the time of diagnosis of recurrence/persistence Type of thyroid surgery
was defined as the final serum calcitonin value. Serum calcitonin Total thyroidectomy 78 (90.7)
levels were measured using immunoradiometric assays in eight Hemithyroidectomy 7 (8.1)
Subtotal thyroidectomy 1 (1.2)
affiliated hospitals, and chemiluminescence immunoassays in
Size of primary MTC (mean ± SD, mm) 16.9 ± 13.7 (range, 3–88.6)
one hospital. The cutoffs for calcitonin levels were 0–10 pg/mL
Location of primary MTC
in seven of the hospitals using immunoradiometric assays, 0–14
Right 59 (68.6)
pg/mL in the remaining one hospital using immunoradiometric Left 26 (30.2)
assays, and 0–8.4 pg/mL (male) or 0–5.0 pg/mL (female) in the Isthmus 1 (1.2)
one hospital using chemiluminescent immunoassays. In previ- T stage
ous reports, a normal basal calcitonin level of <10 pg/mL has T1a 22 (25.6)
been used to exclude remnant MTC, and ≥10 pg/mL of serum T1b 29 (33.7)
calcitonin has been deemed indicative of recurrence/persistence T2 10 (11.6)
T3 25 (29.1)
(20, 21).
T4a 0
Based on the literature, postoperative disease status within
N stage
6 months of surgery and at the last follow-up were classified as
Nx (unknown) 3 (3.5)
follows: (1) no tumor recurrence/persistence (biochemical remis- N0 38 (44.2)
sion as defined by a serum calcitonin level of <10 pg/mL and no N1a 20 (23.3)
structural disease evident via neck US or other available imaging N1b 25 (29.1)
modalities during postoperative follow-up), (2) only biochemical M stage
recurrence/persistence (serum calcitonin level of ≥10 pg/mL with Mx (unknown) 15 (17.4)
no evidence of structural disease during postoperative follow-up), M0 70 (81.4)
M1 1 (1.2)
and (3) structural recurrence/persistence (with identification of
structural recurrence/persistence on neck US or other available Multiplicity/bilaterality
Solitary 70 (81.4)
imaging modalities during postoperative follow-up) (20–22). Satellite MTC in the ipsilateral lobe 6 (7.0)
Satellite MTC in the contralateral lobe 1 (1.2)
Satellite MTC in both lobes 9 (10.5)
Statistical Analysis Interval of the last follow-up US (mean ± SD, 78.6 ± 24.9 (range, 23–141)
All statistical analyses were performed using SPSS for Windows months)
(version 21.0, SPSS, Chicago, IL, USA). Categorical variables Session number of the last follow-up US 7.0 ± 3.3 (range, 1–18)
were compared using the chi-square test or Fisher’s exact test, and Data presented in parentheses are percentage of each item.
continuous variables (age, tumor size, and serum calcitonin level) MTC, medullary thyroid carcinoma.
Frontiers in Endocrinology | www.frontiersin.org 3 March 2018 | Volume 9 | Article 102
Ahn et al. Postoperative Neck US in MTC Patients
25 patients (29.1%). Distant metastasis was only noted in one 98 (seventeenth session), and 128 (eighth session) months after
patient (1.2%). The interval between thyroid surgery and the last the initial surgery. The structural recurrence/persistence group
follow-up US was 60 or more months in 74 patients (86.0%) and showed a mean serum calcitonin level of 662.5 ± 1634.7 pg/mL
90 or more months in 22 patients (25.6%). (range 19.2–5545.0 pg/mL).
Of the 86 patients, 64 (74.4%) exhibited no tumor recurrence/ Among the patient demographics variables and general char-
persistence during the follow-up period. Of the 22 (25.6%) acteristics of the primary tumor, tumor recurrence/persistence
remaining patients, 11 (50%) showed biochemical recurrence/ was significantly correlated with TNM stage and multiplicity/
persistence with no structural recurrence/persistence and 11 bilaterality of the tumor (Table 2). The primary MTCs in the
(50%) showed structurally identified recurrence/persistence recurrent/persistent group exhibited higher T and N stages than
(Figures 1 and 2). those of the non-recurrent group (both p < 0.001). Preoperative
Of the 11 patients with structural recurrence/persistence, distant metastasis was only reported in 1 patient who showed
tumor recurrence/persistence was initially detected by follow- tumor recurrence/persistence during the follow-up period.
up US in eight, serum calcitonin analysis in two, and positron In the non-recurrence group, 56 patients (87.5%) exhibited
emission tomography-computed tomography (18F-labeled flude solitary MTC in surgical specimen. However, there was a high
oxyglucose) in one. All patients with structural recurrence/ prevalence of multiple and/or bilateral MTCs in the recurrence/
persistence showed suspicious US features on follow-up US. persistence group compared with the non-recurrence group
Final diagnosis of tumor recurrence/persistence was performed (p = 0.013). Factors such as age, sex of the patient, and the location
by US-guided fine-needle aspiration in six patients, and second- and method of surgical excision of the tumor did not differ signifi-
look surgery in five. Nine of the 11 patients with structural recur- cantly between the recurrence/persistence and non-recurrence
rence/persistence exhibited nodal recurrence/persistence, and groups. There were statistically significant differences in mean
two exhibited non-nodal recurrence/persistence. In this group, interval and session number of postoperative follow-up US
the mean period and session number of the follow-up US in between the non-recurrence group (74.7 months and 6.4, respec-
which tumor recurrence/persistence was initially detected were tively) and the tumor recurrence/persistence group (89.9 months
41.3 ± 39.3 months (range 6–128 months) and 2.6 ± 2.3 (range and 8.7, respectively) (p = 0.013 and 0.005, respectively).
1–8), respectively. Six of the 11 patients were diagnosed with In preoperative serologic tests, the serum calcitonin level was
tumor recurrence/persistence within 3 years of the initial surgery significantly higher in the tumor recurrence/persistence group
(6, 12, 21, 22, 25, and 33 months), and the remaining 4 were (mean 4202.9 ± 15380.3 pg/mL, range 52.3–67633.0 pg/mL) than
diagnosed at 50 (fifth), 62 (fourth session), 92 (seventh session), in the non-recurrence group (mean 277.4 ± 775.9 pg/mL, range
1.5–5790.0 pg/mL) (p = 0.042). In the last serologic test, there
was a significant difference in the serum calcitonin levels of the
Figure 1 | A 51-year-old man with non-nodal recurrence/persistence of
medullary thyroid carcinoma (MTC). Preoperative longitudinal gray-scale
sonograms show a primary MTC (arrows, 25.0 mm at its largest diameter) in Figure 2 | A 54-year-old man with nodal recurrence/persistence of
the right thyroid lobe (A), and a metastatic lymph node (arrows) in the right medullary thyroid carcinoma (MTC). Preoperative longitudinal gray-scale
lateral neck (B). On histopathological examination after total thyroidectomy sonogram shows an MTC (arrows, 9.3 mm at its largest diameter) in the left
with lateral neck dissection, there was perithyroidal tumor invasion (T3) and thyroid lobe (A) and multiple metastatic lymph nodes (arrows) in the left lateral
nodal metastasis in the right neck (N1b). The patient exhibited biochemical neck (B). On histopathological examination after total thyroidectomy with
remission after thyroid surgery, and there was no focal lesion in the lateral neck dissection, there was perithyroidal tumor invasion (T3) and nodal
postoperative thyroid beds and necks on 6, 12, 18, or 24-month follow-up metastasis in the left neck (N1b). The patient showed biochemical remission
ultrasonography (US) after thyroid surgery. In the fifth follow-up US at after thyroid surgery, and the first follow-up ultrasonography (US) at 12 months
30 months after thyroid surgery, transverse (C) and longitudinal (D) after thyroid surgery showed normal lymph nodes (arrows) in the left level-III
gray-scale sonograms showed an oval hypoechoic nodule (arrows, 8.0 mm neck (C). On the second follow-up US at 25 months after thyroid surgery, a
at its largest diameter) in the right postoperative thyroid bed. After US-guided transverse gray-scale sonogram (D) shows a suspicious LN (arrows, 19.9 mm
fine-needle aspiration for this lesion, cytology revealed suspicious MTC, and at its largest diameter) in the left level-III neck. After US-guided fine-needle
this lesion was confirmed as non-nodal recurrence/persistence of MTC after aspiration for this node, cytology revealed nodal metastasis of MTC, and this
the second-look surgery. lesion was confirmed after the second-look surgery.
Frontiers in Endocrinology | www.frontiersin.org 4 March 2018 | Volume 9 | Article 102
Ahn et al. Postoperative Neck US in MTC Patients
Table 2 | Comparison of the factors related to tumor recurrence/persistence. However, the small sample size of MTC patients and tumor recur-
Items Non- Recurrence/ P-value rence/persistence cases may be associated with discrepancy.
recurrence persistence In the present study, the serum calcitonin levels detected in
(n = 64) (n = 22) the preoperative and final serologic tests were compared between
0.708
tumor recurrence/persistence and non-recurrence groups. Higher
Age (mean ± SD, years) 52.3 ± 12.6 53.5 ± 12.0
Sex 0.999 serum calcitonin levels are widely known to be predictive of MTC.
Female 39 (60.9) 14 (63.6) Cohen et al. demonstrated that tumor size was significantly cor-
Male 25 (39.1) 8 (36.4) related with preoperative serum calcitonin level (24). Also, they
Type of thyroid surgery 0.755 reported that a preoperative serum calcitonin level <50 pg/mL
Total thyroidectomy 57 (89.1) 21 (95.5)
Hemithyroidectomy 6 (9.4) 1 (4.5)
was predictive of postoperative calcitonin normalization. Several
Subtotal thyroidectomy 1 (1.6) 0 (0) studies have reported that postoperative calcitonin level is of
Size of primary MTC (mm) 15.9 ± 14.4 19.7 ± 11.1 0.263 predictive value with regard to disease progression and persis-
Location of primary MTC 0.999 tence (21, 25, 26). In our study, serum calcitonin levels in both
Right 44 (68.8) 15 (68.2)
preoperative and postoperative serologic tests were significantly
Left 19 (29.7) 7 (31.8)
Isthmus 1 (1.6) 0 (0)
correlated with tumor recurrence/persistence, as has been
T stage <0.001 reported in previous studies (21, 25, 26).
T1a 20 (31.3) 2 (9.1) In MTC patients, rates of structural recurrence ranging from <1
T1b 25 (39.1) 4 (18.2) to 10.6% have been reported (21, 22). The rate of structural recur-
T2 8 (12.5) 2 (9.1)
rence/persistence was 12.8% (11/86) in our study. Most of these
T3 11 (17.2) 14 (63.6)
T4a 0 (0) 0 (0) (54.5%, 6/11) were detected within 3 years after the initial thyroid
N stage <0.001 surgery. However, the remaining tumor recurrence/persistence
Nx (unknown) 3 (4.7) 0 (0) cases were detected on follow-up US during 4–11 years after
N0 36 (56.3) 2 (9.1) thyroid surgery. Of the 11 patients with structural recurrence/
N1a 16 (25) 4 (18.2)
persistence, 8 had the initial detection of recurrence/persistence
N1b 9 (14.1) 16 (72.7)
M stage <0.001 by follow-up US. Based on our study results, we recommend the
Mx (unknown) 6 (9.4) 9 (40.9) following method of follow-up US for detecting tumor recur-
M0 58 (90.6) 12 (54.5) rence/persistence in MTC patients: (1) the follow-up US with
M1 0 (0) 1 (4.5) annual interval is performed within 3 years after thyroid surgery
Multiplicity/bilaterality 0.013
Solitary 56 (87.5) 14 (63.6)
and (2) the follow-up US with biennial interval is performed dur-
Satellite MTC in the ipsilateral lobe 2 (3.1) 4 (18.2) ing 4–10 years after thyroid surgery. However, this method may
Satellite MTC in the contralateral lobe 0 (0) 1 (4.5) be changeable depending on risk factors of tumor recurrence/
Satellite MTC in both lobes 6 (9.4) 3 (13.6) persistence. For clarity, a large-scale study may be required.
Interval of the last follow-up US 74.7 ± 24.2 89.9 ± 23.8 0.013
In the present study, there were significant differences in mean
(mean ± SD, months)
Session number of the last follow- 6.4 ± 2.8 8.7 ± 4.0 0.005
interval and mean session number of follow-up US between the
up US non-recurrence group and the tumor recurrence/persistence group.
Namely, tumor recurrence/persistence group had longer periods of
Data presented in parentheses are percentage of each item.
MTC, medullary thyroid carcinoma; US, ultrasonography. follow-up US, and more frequent sessions than the non-recurrence
group. The reason for this may be associated with that recurrent/
persistent patients had been diagnosed at a point in time during their
follow-up, consequently they underwent more frequent follow-up
two groups (p = 0.002). The tumor recurrence/persistence group
US over a longer period of time than non-recurrence patients.
showed significantly higher levels of serum calcitonin (mean
This study had several limitations. First, the sample size of the
563.2 ± 1362.4 pg/mL, range 6.1–5545.0 pg/mL) than the non-
study was small. This can compromise the statistical interpretation
recurrence group (mean 3.2 ± 2.2 pg/mL, range 1–9.3 pg/mL).
of results. Second, retrospective analyses of medical records and
US images were performed. This may have resulted in unavoid-
DISCUSSION able selection bias. Third, we did not distinguish tumor recur-
rence from persistence. Finally, there were differences between
Many studies have investigated various prognostic factors in MTC the affiliated hospitals with regard to postoperative follow-up US
patients (7–9, 23). Distant metastasis (known to be the main cause protocols and serum calcitonin measurement. To overcome these
of mortality), advanced age, primary tumor stage, and nodal stage limitations, a prospective study with a large patient population
have been proposed as prognostic factors (7–9). As in these prior must be considered in the near future.
studies, TNM stage and multiplicity/bilaterality of the primary In conclusion, the tumor recurrence/persistence rate of MTC
tumor were significantly correlated with tumor recurrence/ in the neck was 25.6% (22/86), the proportion of structural
persistence in our study. However, age and sex of the patient were recurrence/persistence was 50% (11/22), and tumor recurrence/
not correlated with tumor recurrence/persistence in the present persistence was associated with advanced TNM stage and mul-
study, although they have been reported as prognostic factors in tiplicity/bilaterality. In the majority of patients with structural
previous studies (8, 9, 23). The reason for this difference is unclear. recurrence/persistence in the neck, tumor recurrence/persistence
Frontiers in Endocrinology | www.frontiersin.org 5 March 2018 | Volume 9 | Article 102
Ahn et al. Postoperative Neck US in MTC Patients
was detected during early follow-up US, within 3 years from the by the appropriate ethics review boards (IRB 2016-0068). The
initial thyroid surgery. Thus, for detecting MTC recurrence/ data and materials in this manuscript have not been published
persistence in the neck, annual US surveillance may be sufficient or presented elsewhere in part or in entirety, and are not under
within the first 3 years after thyroid surgery, but depending on the consideration by another journal.
presence of relevant risk factors, annual or biannual US surveil-
lance may be recommendable for 4–10 years after thyroid surgery. AUTHOR CONTRIBUTIONS
ETHICS STATEMENT Concept and design: DK. Acquisition of data: all authors.
Literature review: HA and DK. Analysis and interpretation of
Informed consent was waived for all study participants due to data: HB and DK. Manuscript writing: HA. Refinement of manu-
the retrospective analysis, and the study design was approved script: all authors. Review of final manuscript: DK and YL.
REFERENCES 15. Lee S, Shin JH, Han BK, Ko EY. Medullary thyroid carcinoma: comparison
with papillary thyroid carcinoma and application of current sonographic
1. Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Clark OH. Medullary thy- criteria. AJR Am J Roentgenol (2010) 194:1090–4. doi:10.2214/AJR.09.3276
roid carcinoma: clinical characteristics, treatment, prognostic factors, and 16. Elisei R, Pinchera A. Advances in the follow-up of differentiated or med-
a comparison of staging systems. Cancer (2000) 88:1139–48. doi:10.1002/ ullary thyroid cancer. Nat Rev Endocrinol (2012) 8:466–75. doi:10.1038/
(SICI)1097-0142(20000301)88:5<1139::AID-CNCR26>3.0.CO;2-Z nrendo.2012.38
2. Pelizzo MR, Boschin IM, Bernante P, Toniato A, Piotto A, Pagetta C, et al. 17. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th
Natural history, diagnosis, treatment and outcome of medullary thyroid edition of the AJCC cancer staging manual and the future of TNM. Ann Surg
cancer: 37 years experience on 157 patients. Eur J Surg Oncol (2007) 33:493–7. Oncol (2010) 17:1471–4. doi:10.1245/s10434-010-0985-4
doi:10.1016/j.ejso.2006.10.021 18. Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, et al.
3. Melvin KE, Tashjian AH Jr. The syndrome of excessive thyrocalcitonin pro- Ultrasound criteria of malignancy for cervical lymph nodes in patients
duced by medullary carcinoma of the thyroid. Proc Natl Acad Sci U S A (1968) followed up for differentiated thyroid cancer. J Clin Endocrinol Metab (2007)
59:1216–22. doi:10.1073/pnas.59.4.1216 92:3590–4. doi:10.1210/jc.2007-0444
4. Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E. Nonparallel 19. Kamaya A, Gross M, Akatsu H, Jeffrey RB. Recurrence in the thyroidec-
patterns of calcitonin and carcinoembryonic antigen levels in the follow-up tomy bed: sonographic findings. AJR Am J Roentgenol (2011) 196:66–70.
of medullary thyroid carcinoma. Cancer (1984) 53:278–85. doi:10.1002/1097- doi:10.2214/AJR.10.4474
0142(19840115)53:2<278::AID-CNCR2820530216>3.0.CO;2-Z 20. Roman S, Mehta P, Sosa JA. Medullary thyroid cancer: early detection
5. Kim SH, Kim BS, Jung SL, Lee JW, Yang PS, Kang BJ, et al. Ultrasonographic and novel treatments. Curr Opin Oncol (2009) 21:5–10. doi:10.1097/
findings of medullary thyroid carcinoma: a comparison with papillary CCO.0b013e32831ba0b3
thyroid carcinoma. Korean J Radiol (2009) 10:101–5. doi:10.3348/kjr.2009. 21. Jung KY, Kim SM, Yoo WS, Kim BW, Lee YS, Kim KW, et al. Postoperative
10.2.101 biochemical remission of serum calcitonin is the best predictive factor for
6. Modigliani E, Cohen R, Campos JM, Conte-Devolx B, Maes B, Boneu A, recurrence-free survival of medullary thyroid cancer: a large-scale retrospective
et al. Prognostic factors for survival and for biochemical cure in medullary analysis over 30 years. Clin Endocrinol (2016) 84:587–97. doi:10.1111/cen.12852
thyroid carcinoma: results in 899 patients. The GETC study group. Groupe 22. Lindsey SC, Ganly I, Palmer F, Tuttle RM. Response to initial therapy predicts
d’etude des tumeurs a calcitonine. Clin Endocrinol (Oxf) (1998) 48:265–73. clinical outcomes in medullary thyroid cancer. Thyroid (2015) 25:242–9.
doi:10.1046/j.1365-2265.1998.00392.x doi:10.1089/thy.2014.0277
7. Schlumberger M, Bastholt L, Dralle H, Jarzab B, Pacini F, Smit JW, et al. 2012 23. Pazaitou-Panayiotou K, Chrisoulidou A, Mandanas S, Tziomalos K, Doumala E,
European thyroid association guidelines for metastatic medullary thyroid Patakiouta F. Predictive factors that influence the course of medullary thyroid
cancer. Eur Thyroid J (2012) 1:5–14. doi:10.1159/000336977 carcinoma. Int J Clin Oncol (2014) 19:445–51. doi:10.1007/s10147-013-0588-8
8. Miccoli P, Minuto MN, Ugolini C, Molinaro E, Basolo F, Berti P, et al. Clinically 24. Cohen R, Campos JM, Salaun C, Heshmati HM, Kraimps JL, Proye C, et al.
unpredictable prognostic factors in the outcome of medullary thyroid cancer. Preoperative calcitonin levels are predictive of tumor size and postoperative
Endocr Relat Cancer (2007) 14:1099–105. doi:10.1677/ERC-07-0128 calcitonin normalization in medullary thyroid carcinoma. J Clin Endocrinol
9. Cupisti K, Wolf A, Raffel A, Schott M, Miersch D, Yang Q, et al. Long-term Metab (2000) 85:919–22. doi:10.1210/jcem.85.2.6556
clinical and biochemical follow-up in medullary thyroid carcinoma: a 25. Saltiki K, Rentziou G, Stamatelopoulos K, Georgiopoulos G, Stavrianos C,
single institution’s experience over 20 years. Ann Surg (2007) 246:815–21. Lambrinoudaki E, et al. Small medullary thyroid carcinoma: post-operative
doi:10.1097/SLA.0b013e31813e66b9 calcitonin rather than tumour size predicts disease persistence and progres-
10. Stepanas AV, Samaan NA, Hill CS Jr, Hickey RC. Medullary thyroid sion. Eur J Endocrinol (2014) 171:117–26. doi:10.1530/EJE-14-0076
carcinoma: importance of serial serum calcitonin measurement. Cancer 26. Bumming P, Ahlman H, Nilsson B, Nilsson O, Wangberg B, Jansson S. Can
(1979) 43:825–37. doi:10.1002/1097-0142(197903)43:3<825::AID-CN- the early reduction of tumour markers predict outcome in surgically treated
CR2820430308>3.0.CO;2-Q sporadic medullary thyroid carcinoma? Langenbecks Arch Surg (2008)
11. Virmani V, Hammond I. Sonographic patterns of benign thyroid nodules: 393:699–703. doi:10.1007/s00423-008-0375-6
verification at our institution. AJR Am J Roentgenol (2011) 196:891–5.
doi:10.2214/AJR.10.5363 Conflict of Interest Statement: The authors declare that the research was con-
12. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography ducted in the absence of any commercial or financial relationships that could be
and the ultrasound-based management of thyroid nodules: consensus state- construed as a potential conflict of interest.
ment and recommendations. Korean J Radiol (2011) 12:1–14. doi:10.3348/
kjr.2011.12.1.1 Copyright © 2018 Ahn, Kim, Lee, Lee, Kim, Choi, Lee, Ryoo, Huh, Sung, Kwak
13. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United and Baek. This is an open-access article distributed under the terms of the Creative
States, 1973–2002. JAMA (2006) 295:2164–7. doi:10.1001/jama.295. Commons Attribution License (CC BY). The use, distribution or reproduction in
18.2164 other forums is permitted, provided the original author(s) and the copyright owner
14. Watters DA, Ahuja AT, Evans RM, Chick W, King WW, Metreweli C, et al. are credited and that the original publication in this journal is cited, in accordance
Role of ultrasound in the management of thyroid nodules. Am J Surg (1992) with accepted academic practice. No use, distribution or reproduction is permitted
164:654–7. doi:10.1016/S0002-9610(05)80728-7 which does not comply with these terms.
Frontiers in Endocrinology | www.frontiersin.org 6 March 2018 | Volume 9 | Article 102
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Five Elements Tai Chi Chuan Theory In-DepthDokument10 SeitenFive Elements Tai Chi Chuan Theory In-DepthCésar EscalanteNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Guidelines For The Management of Glucocorticoids During The Peri OperativeDokument10 SeitenGuidelines For The Management of Glucocorticoids During The Peri OperativeCésar EscalanteNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Model Systems in SDHx-related Pheochromocytoma/paragangliomaDokument25 SeitenModel Systems in SDHx-related Pheochromocytoma/paragangliomaCésar EscalanteNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Liraglutide and Cardiovascular Outcomes in Type 2 DiabetesDokument17 SeitenLiraglutide and Cardiovascular Outcomes in Type 2 DiabetesCésar EscalanteNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Steps: Liraglutide (Saxenda) For Weight LossDokument2 SeitenSteps: Liraglutide (Saxenda) For Weight LossCésar EscalanteNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Latent Adrenal Insufficiency: From Concept To DiagnosisDokument12 SeitenLatent Adrenal Insufficiency: From Concept To DiagnosisCésar EscalanteNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Ni Hms 853187Dokument12 SeitenNi Hms 853187César EscalanteNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- 2020 Article 1793Dokument13 Seiten2020 Article 1793César EscalanteNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Diagnosis and Management of Adrenal InsufficiencyDokument29 SeitenDiagnosis and Management of Adrenal InsufficiencyCésar EscalanteNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
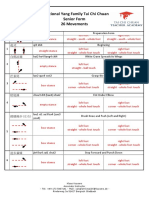
- Traditional Yang Family Tai Chi Chuan Tai Chi Kung 10 MovementsDokument3 SeitenTraditional Yang Family Tai Chi Chuan Tai Chi Kung 10 MovementsCésar EscalanteNoch keine Bewertungen
- Traditional Yang Family Tai Chi Chuan Senior Form 26 MovementsDokument5 SeitenTraditional Yang Family Tai Chi Chuan Senior Form 26 MovementsCésar EscalanteNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Traditional Yang Family Tai Chi Chuan Essential Form 22 MovementDokument5 SeitenTraditional Yang Family Tai Chi Chuan Essential Form 22 MovementCésar EscalanteNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- HHS Public AccessDokument35 SeitenHHS Public AccessBudi PutraNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- iPSC Technology-Based Regenerative Therapy For DiabetesDokument10 SeiteniPSC Technology-Based Regenerative Therapy For DiabetesCésar EscalanteNoch keine Bewertungen
- Hypothalamic Amenorrhea and The Long-Term Health ConsequencesDokument12 SeitenHypothalamic Amenorrhea and The Long-Term Health ConsequencesCésar EscalanteNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Polycystic Ovary SyndromeDokument17 SeitenPolycystic Ovary SyndromeCésar EscalanteNoch keine Bewertungen
- The Effects Induced by Spinal Manipulative Therapy On The Immune and Endocrine SystemDokument12 SeitenThe Effects Induced by Spinal Manipulative Therapy On The Immune and Endocrine SystemCésar EscalanteNoch keine Bewertungen
- The Physiology of Endocrine Systems With AgeingDokument24 SeitenThe Physiology of Endocrine Systems With AgeingCésar EscalanteNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- COVID-19 and The Endocrine System Exploring The Unexplored PDFDokument5 SeitenCOVID-19 and The Endocrine System Exploring The Unexplored PDFDiego CoronelNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- AmenorrheaDokument11 SeitenAmenorrheaisaNoch keine Bewertungen
- Drugs That May Worsen Myasthenia GravisDokument1 SeiteDrugs That May Worsen Myasthenia GravisyulianitadewiNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hypertension and AcromegalyDokument26 SeitenHypertension and AcromegalyCésar EscalanteNoch keine Bewertungen
- A Consensus Statement On Acromegaly Therapeutic OutcomesDokument10 SeitenA Consensus Statement On Acromegaly Therapeutic OutcomesCésar EscalanteNoch keine Bewertungen
- Traditional Chinese Medicine Combined With Conventional Therapy For Female Kidney Stone: A Protocol For Systematic Review.Dokument5 SeitenTraditional Chinese Medicine Combined With Conventional Therapy For Female Kidney Stone: A Protocol For Systematic Review.César EscalanteNoch keine Bewertungen
- 1 PDFDokument2 Seiten1 PDFCésar EscalanteNoch keine Bewertungen
- The Tailgate Study: Differing Metabolic Effects of A Bout of Excessive Eating and DrinkingDokument36 SeitenThe Tailgate Study: Differing Metabolic Effects of A Bout of Excessive Eating and DrinkingCésar EscalanteNoch keine Bewertungen
- 2 PDFDokument6 Seiten2 PDFCésar EscalanteNoch keine Bewertungen
- 2 PDFDokument6 Seiten2 PDFCésar EscalanteNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- 1 PDFDokument2 Seiten1 PDFCésar EscalanteNoch keine Bewertungen
- The Effect of High-Dose Vitamin C On Biochemical Markers of Myocardial Injury in Coronary Artery Bypass SurgeryDokument8 SeitenThe Effect of High-Dose Vitamin C On Biochemical Markers of Myocardial Injury in Coronary Artery Bypass SurgeryCésar EscalanteNoch keine Bewertungen
- 2019 Article 2503Dokument8 Seiten2019 Article 2503Frida RasyidNoch keine Bewertungen
- 701 MD Calls Monitor c1w1Dokument14 Seiten701 MD Calls Monitor c1w1Adrian Lindsy MadriagaNoch keine Bewertungen
- ChangingaDressing ChecklistDokument3 SeitenChangingaDressing ChecklistScribdNoch keine Bewertungen
- Dr. Praveen PresentationDokument63 SeitenDr. Praveen PresentationPraveen KumarNoch keine Bewertungen
- Menstrual CycleDokument15 SeitenMenstrual CycleNazkie Alganion100% (2)
- Daftar PustakaDokument2 SeitenDaftar PustakaputriNoch keine Bewertungen
- Or and DR Instruments PDFDokument59 SeitenOr and DR Instruments PDFMayolianne Dumay100% (1)
- DocumentchnDokument3 SeitenDocumentchnmagickero5Noch keine Bewertungen
- Courtney Harmon Leadership ResumeDokument2 SeitenCourtney Harmon Leadership Resumeapi-482580060Noch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Breast DR BanezDokument46 SeitenBreast DR BanezLian BaylosisNoch keine Bewertungen
- Curs de Ortodontie - Orthodontic Seminars of California - Dr. Larry BrownDokument6 SeitenCurs de Ortodontie - Orthodontic Seminars of California - Dr. Larry BrownAlin AniculaesaNoch keine Bewertungen
- Alternative MedicineDokument12 SeitenAlternative MedicineBashu PoudelNoch keine Bewertungen
- Abdominal Examination: M.Thamrin TanjungDokument13 SeitenAbdominal Examination: M.Thamrin TanjungAurora SalsabillaNoch keine Bewertungen
- HPLC Studies in HemoglobinopathiesDokument6 SeitenHPLC Studies in HemoglobinopathiesDevi SusantiNoch keine Bewertungen
- Midwifery April 2014 PSDokument10 SeitenMidwifery April 2014 PSTheSummitExpressNoch keine Bewertungen
- Tuna Vs TurpDokument5 SeitenTuna Vs TurpDimas Aditya Wahyu PamujiNoch keine Bewertungen
- A Tooth-Stabilized Surgical Template For AlveolectomyDokument3 SeitenA Tooth-Stabilized Surgical Template For Alveolectomyheri asriyadiNoch keine Bewertungen
- Rec Letter From ZhylkybaevaDokument2 SeitenRec Letter From ZhylkybaevaГулнара УмурзаковаNoch keine Bewertungen
- Prenatal Development 1Dokument10 SeitenPrenatal Development 1nate1425Noch keine Bewertungen
- Research PaperDokument9 SeitenResearch Paperapi-319757396Noch keine Bewertungen
- Breast Self Exam BrochureDokument2 SeitenBreast Self Exam Brochureapi-252329688100% (1)
- Warehouse Consolidation ProjectDokument15 SeitenWarehouse Consolidation ProjectGian Eugenio100% (1)
- Resume TemplateDokument3 SeitenResume TemplateLou Dy SolisNoch keine Bewertungen
- List of Abbreviations Used in Medical PrescriptionsDokument10 SeitenList of Abbreviations Used in Medical PrescriptionsFemi AlfarishiNoch keine Bewertungen
- Paediatric Percutaneous Nephrolithotomy (P-PCNL) Reporting ChecklistDokument6 SeitenPaediatric Percutaneous Nephrolithotomy (P-PCNL) Reporting ChecklistJad DegheiliNoch keine Bewertungen
- K44 - Nutrition During LactationDokument26 SeitenK44 - Nutrition During Lactationbilli lisanuddinNoch keine Bewertungen
- Incomplete AbortionDokument2 SeitenIncomplete AbortionKEn PilapilNoch keine Bewertungen
- Recommended Dosages: 1st Trimester 2nd Trimester 3rd Trimester PostpartumDokument1 SeiteRecommended Dosages: 1st Trimester 2nd Trimester 3rd Trimester PostpartumPutri Octavia SariNoch keine Bewertungen
- Maternal Child Nursing Care Perry Hockenberry Lowdermilk 5th Edition Test BankDokument14 SeitenMaternal Child Nursing Care Perry Hockenberry Lowdermilk 5th Edition Test BankPeterThomasizbjf100% (80)
- BooksDokument2 SeitenBooksRox SmithNoch keine Bewertungen
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)