Beruflich Dokumente
Kultur Dokumente
Nursing Care Plan Acarpenter 1
Hochgeladen von
api-383586399Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Care Plan Acarpenter 1
Hochgeladen von
api-383586399Copyright:
Verfügbare Formate
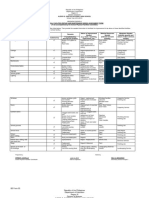
Nursing Care Plan – Amanda Carpenter
Initials: M.J.
Significant Medical Diagnoses: Cerebrovascular accident (mini stroke) 2010 Jan 15, Hypertension,
Hyperthyroidism, Macular degeneration (blind) rt. eye, Chronic Leukemia, Basal cell Carcinoma of skin
Safety Considerations: Resident independence, OTC medication use, self-reported heart condition with fluid
Activities of Daily Living/Activity level and restrictions: Independent. PRN 1x assist
Assessment of issue (NANDA Nursing Diagnosis): Risk for Respiratory Distress
Assessment Outcomes Interventions or Plan Rationale for Interventions Evaluation or result
Issue of Short term:
Short term: 1.Head of bed 45 when 1.GAEB (Good Air
exploration: Decrease 1.Position resident in supine increases thoracic Entry Bilaterally)
Risk for resident’s semi-Fowler’s position capacity, full ROM of and reduction in
Respiratory respiratory with bed mechanics diaphragm, and increased dyspnea and RR
Distress rate below and pillows lung expansion by 2.Resident self-report
30 breaths2.Situating in personal decreased abdominal improved mood,
Subjective data:
per minute context to decrease crowding. nurse-client
Sore throat,
by the end anxiety by increasing 2.Anxiety can increase relationship, and
Sore tongue,
of shift nursing companionship dyspnea and respiratory reduction in
Pain radiates to
time and building rate. Companionship to dyspnea and RR
the left ear,
therapeutic relationship situate in personal context 3.Resident’s
Weakness,
3.Monitor respiratory promotes relaxation, respiratory rate
Poor sleep
status (Sp02, GAEB, healing, and further below 30 breaths
quality,
RR), by auscultation of reduction in respiratory per minute by last
LTC Staff
chest and use of pulse rate. assessment of shift
provides less
oximeter, each hour on 3.Pulse oximeter and
care due to
shift. Report all auscultation are effective
resident’s level
findings immediately methods to identify changes
of independence,
Taking OTC in oxygenation. Monitoring
lozenges oxygenation and reporting
provided by is a safety measure to
granddaughter minimize resident risk.
Long term: Long term: Long term: Long term:
Objective data: Resident to 4.Facilitate 4.Promotes effective patient 4.Completion of
Sp02 95% resolve interdisciplinary care, and physician required physician
RR 32 episodic collaboration with to rule out or treat dyspnea assessment and
(Dyspnea) risk of physician to assess secondary to infection admin. of treatment
HR 72 respiratory respiratory risk 5.Nursing assistance with as per order to
Tympanic distress by etiology and treatment ADLs helps conserve decrease dyspnea
Temp. 37.3C absence of options within 7 days resident energy and and pain
BP 92/59 dyspnea and 5.Increase food and fluid assisting meals encourages 5.Resident
SOBOE pain in one intake by assisting 3 greater intake for improved maintaining bedrest
Increased month meals per day nutrition to promote health with ADL
abdominal in 6.Resident and staff 6.Informing the circle of care assistance to
drawings teaching/education. to protect resident safety. decrease dyspnea
Absence of Resident education for Increasing assistance will and increase pain
edema in lower use of call bell for any prevent overexertion and resolution
extremities physical changes. Staff promoting call bell use will 6.Education/teaching
Non-productive education of resident help to inform care and creates a reduction
cough status and new readily address any changes in pain severity and
Restlessness limitations. in physical status dyspnea
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- 5V To 48V DC Converter For Phantom Power Supplies - Full DIY Project PDFDokument3 Seiten5V To 48V DC Converter For Phantom Power Supplies - Full DIY Project PDFAbdul NoorNoch keine Bewertungen
- Enhanced Hybrid English 10 Q1 M2Dokument13 SeitenEnhanced Hybrid English 10 Q1 M2VNoch keine Bewertungen
- Bexley Selection Tests Specimen Questions - Verbal ReasoningDokument8 SeitenBexley Selection Tests Specimen Questions - Verbal Reasoningpflora41Noch keine Bewertungen
- Transport System Question and AnswersDokument12 SeitenTransport System Question and Answerskumara guruparanNoch keine Bewertungen
- Nielsen Shopper Insights - Retailers Segment - Client 051115 PDFDokument63 SeitenNielsen Shopper Insights - Retailers Segment - Client 051115 PDFn0isyb0yNoch keine Bewertungen
- Diagnostic CentreDokument66 SeitenDiagnostic CentreMoolam RaoNoch keine Bewertungen
- Determination of Fat (Food Analysis)Dokument7 SeitenDetermination of Fat (Food Analysis)Nabila Husna100% (2)
- Biological Molecules Notes o LevelDokument10 SeitenBiological Molecules Notes o LevelFangsNoch keine Bewertungen
- Lesson 2 Professionals and Practitioners in CounselingDokument93 SeitenLesson 2 Professionals and Practitioners in CounselingDaneNoch keine Bewertungen
- Exercise 1. QuantifiersDokument1 SeiteExercise 1. QuantifiersIrynaNoch keine Bewertungen
- Ngo PrimaDokument11 SeitenNgo PrimaAleksandar BačlijaNoch keine Bewertungen
- Behavioral Economics - Problem Set 1Dokument4 SeitenBehavioral Economics - Problem Set 1Evans LoveNoch keine Bewertungen
- H2S Scrubber SpecificationDokument1 SeiteH2S Scrubber SpecificationKapwell LimitedNoch keine Bewertungen
- Relationship between cytokines and hazards in waste workersDokument8 SeitenRelationship between cytokines and hazards in waste workersSalsa BilaNoch keine Bewertungen
- Brigada Eskwela Forms 1 and 3Dokument4 SeitenBrigada Eskwela Forms 1 and 3Mar Sebastian100% (1)
- QUES3Dokument10 SeitenQUES3Múrtåzâ LãxmīdhârNoch keine Bewertungen
- SVM-7600 Series Bedside Monitor Advanced Monitoring and ReviewDokument4 SeitenSVM-7600 Series Bedside Monitor Advanced Monitoring and ReviewCathy Palongpong TumaraoNoch keine Bewertungen
- Chapter 03 The Eye and RetinaDokument10 SeitenChapter 03 The Eye and RetinaSimrat WNoch keine Bewertungen
- Dog Training Book Rex in The CityDokument56 SeitenDog Training Book Rex in The CitybebekbuluhNoch keine Bewertungen
- Key Areas of Risk For Woolworths Ltd.Dokument19 SeitenKey Areas of Risk For Woolworths Ltd.Allison BestNoch keine Bewertungen
- G8 en La Evaluación GeriátricaDokument12 SeitenG8 en La Evaluación GeriátricaMIGUEL MORENONoch keine Bewertungen
- IGA Report FINAL 10 07 2016Dokument171 SeitenIGA Report FINAL 10 07 2016Timothy SchwartzNoch keine Bewertungen
- Promotion of Tax Culture in Pakistan: Perspective, Prospects and ChallengesDokument5 SeitenPromotion of Tax Culture in Pakistan: Perspective, Prospects and ChallengesRaheel JoyiaNoch keine Bewertungen
- Chemical and Enzymatic Synthesis of LanthioninesDokument15 SeitenChemical and Enzymatic Synthesis of LanthioninesSam SonNoch keine Bewertungen
- People V Veneracion Case DigestDokument3 SeitenPeople V Veneracion Case DigestraykarloBNoch keine Bewertungen
- Chemistry ProjectDokument11 SeitenChemistry ProjectEktaMallikNoch keine Bewertungen
- Cell Cycle DisordersDokument22 SeitenCell Cycle DisordersFatima IffatNoch keine Bewertungen
- 02 - Motor PDFDokument80 Seiten02 - Motor PDFRenato Assis da SilvaNoch keine Bewertungen
- Definition, Limits and Agents of MetamorphismDokument13 SeitenDefinition, Limits and Agents of MetamorphismSajid IqrarNoch keine Bewertungen
- Chemical Engineering Science: Ishara Dedunu Kamalanathan, Peter James MartinDokument11 SeitenChemical Engineering Science: Ishara Dedunu Kamalanathan, Peter James MartinarulrajasiNoch keine Bewertungen