Beruflich Dokumente
Kultur Dokumente
Management of Ventricular Arrhythmias and Sudden Cardiac Death Risk Related To Ischemic and Nonischemic Cardiomyopathy
Hochgeladen von
Yeimer Ortiz MartínezOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Management of Ventricular Arrhythmias and Sudden Cardiac Death Risk Related To Ischemic and Nonischemic Cardiomyopathy
Hochgeladen von
Yeimer Ortiz MartínezCopyright:
Verfügbare Formate
Clinical Review & Education
JAMA Cardiology Clinical Guidelines Synopsis
Management of Ventricular Arrhythmias
and Sudden Cardiac Death Risk Related to Ischemic
and Nonischemic Cardiomyopathy
Sana M. Al-Khatib, MD, MHS; William G. Stevenson, MD
GUIDELINE TITLE 2017 AHA/ACC/HRS Guideline for sonable (moderate-quality evidence); however, even if medi-
Management of Patients With Ventricular Arrhythmias cal therapy appears to be effective and well tolerated, adding
and the Prevention of Sudden Cardiac Death an ICD may be reasonable (moderate-quality evidence).
• In patients with a left-ventricular ejection fraction of 35% or
DEVELOPERS American Heart Association (AHA), American less due to ischemic cardiomyopathy who are at least 40
College of Cardiology (ACC), and Heart Rhythm Society (HRS) days post-myocardial infarction (MI) and at least 90 days
post-revascularization and in patients with NICM, and with
RELEASE DATE October 30, 2017 (online)
New York Heart Association (NYHA) class II or III heart failure
despite guideline-directed medical therapy, an ICD is recom-
mended (high-quality evidence).
PRIOR VERSIONS September 5, 2006
• In patients with a left-ventricular ejection fraction of 30% or
less due to ischemic cardiomyopathy who are at least 40 days
FUNDING SOURCE AHA/ACC/HRS post-MI and at least 90 days postrevascularization, and with
NYHA class I heart failure despite guideline-directed medical
TARGET POPULATION Adults with ventricular arrhythmias therapy, an ICD is recommended (high-quality evidence).
(VAs) and/or at risk for sudden cardiac death (SCD) • In nonhospitalized patients with NYHA class IV symptoms who
are candidates for cardiac transplantation or a left-ventricular
MAJOR RECOMMENDATIONS: assist device, an ICD is reasonable (moderate-quality evidence).
• In patients with heart failure and a left-ventricular ejection frac- • An ICD is not indicated in patients with medication-refrac-
tion or 40% or less, treatment with a β-blocker, a mineralocor- tory NYHA class IV heart failure symptoms who are not also
ticoid receptor antagonist, and either an angiotensin- candidates for advanced heart failure therapies (low-quality
converting enzyme inhibitor, an angiotensin-receptor blocker, evidence).
or an angiotensin receptor-neprilysin inhibitor is recommended • In patients with ischemic cardiomyopathy or NICM and
to reduce SCD and all-cause mortality (high-quality evidence). recurrent VA causing ICD shocks, despite optimal ICD
• In patients with ischemic cardiomyopathy or nonischemic car- programming and ongoing therapy with a β-blocker, amioda-
diomyopathy (NICM) who either survive a cardiac arrest due to rone, or sotalol is useful (moderate-quality evidence).
a VA or experience hemodynamically unstable ventricular • In patients with prior MI and recurrent symptomatic sus-
tachycardia (VT) or stable VT not due to a reversible cause, an tained VT, or who present with VT storm and have failed or
implantable cardioverter defibrillator (ICD) is recommended are intolerant of antiarrhythmic medications, catheter abla-
(moderate-quality evidence). tion is recommended (moderate-quality evidence); if such
• In patients with ischemic cardiomyopathy and unexplained patients have NICM, catheter ablation for VA can be useful
syncope who have inducible, sustained monomorphic VT on (moderate-quality evidence).
an electrophysiology study, an ICD is recommended (moder- • In patients with ischemic cardiomyopathy and sustained
ate-quality evidence). monomorphic VT, coronary revascularization alone is inef-
• In patients with VA resulting from coronary artery spasm, fective to prevent recurrent VT (low-quality evidence).
maximally tolerated doses of a calcium channel blocker and • In patients with NICM who experience unexplained syncope
smoking cessation are recommended (moderate-quality evi- and who do not meet indications for a primary prevention
dence). In such patients, if cardiac arrest occurs despite medi- ICD, an ICD or an electrophysiology study can be beneficial
cal therapy or if medical therapy is not tolerated, an ICD is rea- (moderate-quality evidence).
Summary of the Clinical Problem ing VAs and SCD and to intervene promptly to reduce that risk. Pa-
Ventricular arrhythmias are a major cause of morbidity and mortal- tients with ischemic cardiomyopathy or NICM can be at a high risk
ity and they account for a substantial number of SCDs.1 Therefore, of VAs and SCD.1,2 Therefore, when such patients present with syn-
it is imperative for clinicians to identify patients at risk of develop- cope for which VA is documented or suspected, they should be hos-
jamacardiology.com (Reprinted) JAMA Cardiology Published online April 11, 2018 E1
© 2018 American Medical Association. All rights reserved.
Downloaded From: by a Universidad Libre de Colombia User on 04/14/2018
Clinical Review & Education JAMA Cardiology Clinical Guidelines Synopsis
pitalized for evaluation, monitoring, and management. The workup a subcutaneous ICD in some patients), and catheter ablation. An ex-
of patients presenting with symptoms suggestive of VAs should in- tensive review of the literature was conducted through March 2017.
clude a 12-lead electrocardiogram; ambulatory electrocardio- To be reviewed, studies had to involve human participants, be pub-
graphic monitoring, and if needed, an implantable loop recorder; and lished in English, and be indexed in MEDLINE (through PubMed),
noninvasive and/or invasive EMBASE, the Cochrane Library, or the Agency for Healthcare Re-
imaging studies to assess heart search and Quality. Studies resulting from the literature search were
Supplemental content function and rule out ischemic systematically reviewed.2
heart disease when indicated.2 Of 29 recommendations involving the ongoing management of
In some patients, an electrophysiology study may be needed.2 Even therapy for patients with ischemic cardiomyopathy or NICM who
in the absence of symptoms, some patients with ischemic cardio- have VAs or are at risk of SCD, 12 were class I recommendations, 8
myopathy or NICM warrant implantation of an ICD to reduce the risk were class IIa recommendations, 4 were class IIb recommenda-
of SCD.2 tions, and 5 were class III recommendations. Of the 12 class I rec-
ommendations, 4 had a level of evidence A, 2 had a level of evi-
Characteristics of the Guideline Source dence B-R, 3 had a combination of level of evidence B-R and B-NR,
This guideline was developed by the AHA, the ACC, and the HRS.2 and 3 had a level of evidence B-NR. Of the 29 recommendations, 4
The guideline writing committee comprised 19 members: 12 adult were supported by high-quality evidence and 19 were supported by
electrophysiologists, 1 pediatric electrophysiologist, 1 pediatric car- moderate-quality evidence.2
diologist, 3 general cardiologists (1 with expertise in heart failure), 1
geriatrician with expertise in shared decision making, and 1 patient/ Benefits and Harms
consumer representative. The benefits and risks of each therapy were carefully considered. The
All recommendations in the guideline document were main recommendations on the ongoing management of therapy for
assigned a class of recommendation and a level of evidence.2 The patients with ischemic cardiomyopathy or NICM who have VAs or
class of recommendation is a measure of the strength of the rec- are at risk of SCD are presented in the Supplement.2
ommendation that is determined by an assessment of the esti-
mated benefit vis-à-vis the risk; a class I recommendation indi- Discussion
cates that the benefit of an intervention far exceeds its risk, class The majority of recommendations for the ongoing management of
IIa indicates that the benefit of the intervention moderately therapy for patients with ischemic cardiomyopathy or NICM were
exceeds the risk, class IIb indicates that the benefit may not based on high- and moderate-quality evidence that should inform
exceed the risk, and class III signifies that the benefit is equivalent clinical practice for many years.2
to or is exceeded by the risk. The level of evidence appraises the
quality of the scientific evidence that supports the intervention. Areas in Need of Future Study or Ongoing Research
The level of evidence can be A (evidence from high-quality ran- Areas in need of future research include the identification of pa-
domized clinical trials), B-R (evidence from moderate-quality ran- tients who are most likely to benefit from an ICD among ICD-
domized clinical trials), B-NR (evidence from well-designed, non- eligible patients, characterizing the role of the ICD in patient sub-
randomized studies), C-LD (evidence from randomized or groups not included in the pivotal ICD randomized clinical trials,
nonrandomized studies with limitations of design or execution), or finding methods to identify and treat patients at high individual risk
C-EO (expert opinion based on clinical practice).2 The chair and a for SCD who are not identified by current ICD eligibility criteria; de-
majority of the guideline-writing committee members had no rel- termining the best approach to patients who need elective ICD gen-
evant relations with industry. erator replacement due to battery depletion, but who may no lon-
ger be at low risk for SCA due to a significant improvement in left
Evidence Base ventricular ejection fraction; and obtaining more data on the effi-
For the ongoing management of therapy for patients with ischemic cacy and effectiveness of the subcutaneous ICD, compared with
cardiomyopathy or NICM who have VAs or are at risk of SCD, the rec- transvenous ICDs. In addition, randomized clinical trials on cath-
ommendations covered the importance of excluding reversible eter ablation of VT are needed to evaluate procedural end points,
causes for VAs (eg, ischemia), pharmacologic treatment, an ICD (or mortality, quality of life, and cost.
ARTICLE INFORMATION Conflict of Interest Disclosures: Both authors 2. Al-Khatib SM, Stevenson WG, Ackerman MJ,
Author Affiliations: Division of Cardiology and have completed and submitted the ICMJE Form for et al. AHA/ACC/HRS guideline for management of
Duke Clinical Research Institute, Duke University Disclosure of Potential Conflicts of Interest. Dr patients with ventricular arrhythmias and the
Hospital, Durham, North Carolina (Al-Khatib); Stevenson reports having received consultation prevention of sudden cardiac death [published
Cardiovascular Division, Vanderbilt University fees from St Jude Medical and speaking fees from online October 30, 2017]. Circulation.
Medical Center, Nashville, Tennessee (Stevenson). Boston Scientific. He is a coholder of a patent for
needle ablation consigned to Brigham Hospital. No
Corresponding Author: Sana M. Al-Khatib, MD, other disclosures are reported.
MHS, Duke Clinical Research Institute, 2400 Pratt
Street, Durham, NC 27705 (sana.alkhatib@duke REFERENCES
.edu).
1. Myerburg RJ, Goldberger JJ. Sudden cardiac
Published Online: April 11, 2018. arrest risk assessment: population science and the
doi:10.1001/jamacardio.2018.0016 individual risk mandate. JAMA Cardiol. 2017;2(6):
689-694.
E2 JAMA Cardiology Published online April 11, 2018 (Reprinted) jamacardiology.com
© 2018 American Medical Association. All rights reserved.
Downloaded From: by a Universidad Libre de Colombia User on 04/14/2018
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Pathology+101 Complete)Dokument147 SeitenPathology+101 Complete)Goh Kah Yong100% (2)
- Renal QuizDokument2 SeitenRenal QuizJune Dumdumaya75% (4)
- Stoelting Anasthesia and Co Existing Disease PDFDokument28 SeitenStoelting Anasthesia and Co Existing Disease PDFEgidia SetyaNoch keine Bewertungen
- Osmosis Acute Coronary SyndromesDokument5 SeitenOsmosis Acute Coronary Syndromesvalentinabil3Noch keine Bewertungen
- Establishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratoryDokument15 SeitenEstablishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratorySamuelNoch keine Bewertungen
- p56 - p110Dokument6 Seitenp56 - p110Bhushan D ThombareNoch keine Bewertungen
- Inflamatory Heart DiseaseDokument42 SeitenInflamatory Heart DiseaseChalie MequanentNoch keine Bewertungen
- Queensland RMO Application GuideDokument18 SeitenQueensland RMO Application GuideSOMANATHAN UMAHSUTHANNoch keine Bewertungen
- 1 s2.0 S2772930322004367 MainDokument15 Seiten1 s2.0 S2772930322004367 MainVimal NishadNoch keine Bewertungen
- What Is Tetralogy of FallotDokument3 SeitenWhat Is Tetralogy of FallotJyedenn PonceNoch keine Bewertungen
- Systematic ReviewDokument10 SeitenSystematic ReviewLeeyaa CullenNoch keine Bewertungen
- Critical Care Intravenous Infusion Drug Handbook 3rd EditionDokument61 SeitenCritical Care Intravenous Infusion Drug Handbook 3rd Editionsharon.correia689100% (40)
- Facts About Sudden Cardiac ArrestDokument2 SeitenFacts About Sudden Cardiac ArrestZeljko LekovicNoch keine Bewertungen
- Left Anterior Fascicular Block (LAFB) ECG Review - Criteria and ExamplesDokument1 SeiteLeft Anterior Fascicular Block (LAFB) ECG Review - Criteria and ExamplesWiwik Puji LestariNoch keine Bewertungen
- Electrocardiogram: Dr. PacnaDokument13 SeitenElectrocardiogram: Dr. PacnaEcel AggasidNoch keine Bewertungen
- Renal FailureDokument23 SeitenRenal FailurerjfeeleyNoch keine Bewertungen
- Neacsu Aurelia EssayDokument3 SeitenNeacsu Aurelia EssaySimona NeacsuNoch keine Bewertungen
- 30947630Dokument12 Seiten30947630carolinapolotorresNoch keine Bewertungen
- Mindmap CVS Liana Naamnih Group3Dokument1 SeiteMindmap CVS Liana Naamnih Group3Liana NaamnehNoch keine Bewertungen
- Cardiopulmunary ResucitationDokument13 SeitenCardiopulmunary ResucitationRussel OlivoNoch keine Bewertungen
- VT Origin PDFDokument60 SeitenVT Origin PDFNikita PratamaNoch keine Bewertungen
- Module 1Dokument13 SeitenModule 1MaseaNoch keine Bewertungen
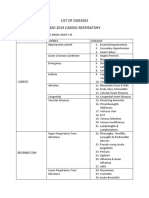
- List of Diseases Imo 2019 Cardio-RespiratoryDokument2 SeitenList of Diseases Imo 2019 Cardio-RespiratoryDimas Adjie Yuda MahendraNoch keine Bewertungen
- Tatalaksana Hiperosmolar Hiperglicemic State (SHH)Dokument16 SeitenTatalaksana Hiperosmolar Hiperglicemic State (SHH)Vidya VidyutNoch keine Bewertungen
- End-Stage Renal DiseaseDokument7 SeitenEnd-Stage Renal Diseasemarvin de castroNoch keine Bewertungen
- Preoperative Cardiac Risk AssessmentDokument16 SeitenPreoperative Cardiac Risk Assessmentkrysmelis MateoNoch keine Bewertungen
- ACS-STEMI Management (Dr. Bambang Herwanto, SPJP)Dokument40 SeitenACS-STEMI Management (Dr. Bambang Herwanto, SPJP)Syafrinaldi JafrilNoch keine Bewertungen
- Nephrotic Syndrome: Akynbay MoldirDokument8 SeitenNephrotic Syndrome: Akynbay MoldirMoldir AkynbayNoch keine Bewertungen
- Beyond Wedge: Clinical Physiology and The Swan-Ganz CatheterDokument12 SeitenBeyond Wedge: Clinical Physiology and The Swan-Ganz Catheterkromatin9462Noch keine Bewertungen
- BCU 2022 First Announcement RevDokument14 SeitenBCU 2022 First Announcement RevAnggar KingStyle100% (1)