Beruflich Dokumente
Kultur Dokumente
Ijahs 2 8 02 Ra
Hochgeladen von
DrMohamed AssadawyOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Ijahs 2 8 02 Ra
Hochgeladen von
DrMohamed AssadawyCopyright:
Verfügbare Formate
Review Article
Lasers in Dentistry: A Review
Chaya M David1, Pankaj Gupta2
Professor and Head, Department of Oral Medicine and Radiology, Dayananda Sagar College of Dental Sciences, Shavige Malleshwara Hills,
1
Kumaraswamy Layout, Bengaluru, Karnataka, India, 2Post-graduate Student, Department of Oral Medicine and Radiology, Dayananda Sagar
College of Dental Sciences, Shavige Malleshwara Hills, Kumaraswamy Layout, Bengaluru, Karnataka, India
ABSTRACT
Lasers were introduced into the field of dentistry as they are a precise and effective way to perform many dental procedures.
Treatment with lasers provides a hope of overcoming the disadvantages of conventional dental procedures. As the applications
for dental lasers expand, greater numbers of dentists will use the technology to provide patients with precision treatment that
may minimize pain and recovery time. Every discipline of dentistry has been positively affected with the use of laser technology
including oral medicine, oral surgery, pediatric and operative dentistry, periodontics and implantology, prosthetic dentistry. The
ability of the lasers to perform less invasive procedures without any discomfort to the patients had made a tremendous impact
on the delivery of dental care. This will continue as this technology will continue to improve and evolve.
Keywords: Argon, Dentistry, Fluorescence, Light amplification by stimulated emission of radiations, Wavelength neodymium-
doped:yttrium aluminum garnet
Corresponding Author: Dr. Pankaj Gupta, Dayananda Sagar College of Dental Sciences, Shavige Malleshwara Hills, Kumaraswamy Layout,
Bengaluru - 560 078, Karnataka, India. Phone: +91-8892307844. E-mail: Pankajtherock3@gmail.com
INTRODUCTION of aluminum oxide, that emitted a deep red-colored
beam. After this invention, dental researchers started
The word LASER is an acronym for light amplification investigating the various potentials of lasers. In 1965,
by stimulated emission of radiation. The principle of Stern and Sognnaes reported that a ruby laser could
the laser was the first known in 1917 when physicist vaporize enamel and had thermal effects on the dental
Albert Einstein described the theory of stimulated pulp. In 1970’s, researchers began to find the clinical
emission.1 Lasers in dentistry are considered to be a oral soft tissue uses of medical CO2 and neodymium-
new technology which is being used in clinical dentistry doped:yttrium aluminum garnet (Nd:YAG) lasers.
to overcome some of the drawbacks posed by the The first laser that had truly both hard and soft tissue
conventional dental procedures. This technology was application was the CO2 laser, invented by Patel in
the first used for dental application in the 1960s but its 1964,2 The Nd:YAG laser was also developed in 1964 by
use has increased rapidly in the last few decades. Today, Geusic, a year after the invention of ruby laser, but it was
the lasers technology is used in the compact disc players, largely overshadowed for a long time by the ruby and
as a pointer for lecturer and above all in the medical other lasers of the era until 1990, when the first pulsed
and dental field. The use of laser technology and its Nd:YAG laser was released which is thought to have a
advancements in the field of medicine and dentistry better interaction with dental hard tissues.
is playing a major role in patient care and well-being.
This article intends a few topics such as laser history, In 1971, The first use of lasers in endodontics was
laser-tissue interaction, lasers wavelength, types and reported by Weichman and Johnson, as they utilize
applications of the use of lasers in various hard and soft high power infrared CO2 laser to seal the apical foramen
tissue procedures in dentistry. in vitro. 2 Research continues for future indications
with an all-tissue laser, including crown and veneer
HISTORY OF LASERS preparations, orthodontic applications, advanced new
implant therapies including sinus augmentation and
In 1960, Theodore Maiman was the first scientist who bone grafting, a gingival tissue resurfacing and even
demonstrates the laser function and also developed low-level laser therapy applications using the yttrium-
a working laser device “known as ruby laser,” made scandium-gallium-garnet (YSGG) laser. Since then, the
7 International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015
David and Gupta Lasers in Dentistry
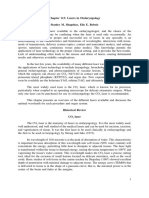
clinical applications of the lasers continue to increase Table 1: Wavelength of laser light used and target
rapidly. At present, lasers are indicated for a variety of tissue
dental procedures which are discussed later. Type of Wavelength (nm) Chromophores Target tissue
lasers pulse mode used
Diode 850-1064 Pigments Gingiva, mucosa
LASER - TISSUE INTERACTION Hemoglobin
Melanin
Laser light has four types of interactions with the Nd:YAG 1064 Pigments Gingiva, mucosa
target tissue which depends on the optical properties Hemoglobin
of that tissue: Absorption, transmission of laser energy, Melanin
reflection, scattering of the laser light. Er:YAG 2940 Water Gingiva, mucosa,
Hydroxyapatite enamel, dentin, bone
Absorption Er, Cr:YSGG 2860 Water Gingiva, mucosa,
Hydroxyapatite enamel, dentin, bone
When the laser is applied to the tissue, there is the
CO2 10640 Water Gingiva, mucosa,
absorption of laser energy in the target tissue. Different
enamel, dentin, bone
laser wavelengths have different absorption coefficients
Nd:YAG: Neodymium-doped:yttrium aluminum garnet, Er:YAG: Erbium:yttrium
with the dental tissue components such as water, aluminum garnet, Cr:YSGG: Chromium:yttrium-scandium-gallium-garnet
pigment, blood contents and mineral. Laser energy can
be absorbed or transmitted based on the composition
surface so there is little energy transmitted to adjacent
of target tissue. Those primary components are termed
tissues.3
chromophores, which can absorb the laser light of
specific wavelength. In general, the longer wavelengths,
Reflection
such as erbium laser has a greater affinity with water
and hydroxyapatite. CO2 laser having wavelength of This property of laser causes laser light to redirects itself
10,600 nm is well absorbed by water and penetrates off the surface, having no effect on the target tissue. This
only to a few microns of the target tissue’s surface.3 The reflected light could be dangerous when redirected to
shorter wavelengths ranging from 500 to 1000 nm are an unintended target such as eyes. However, a caries-
readily absorbed by the pigmented tissue and blood detecting laser device uses the reflected light to measure
elements. For e.g., The pigment hemoglobin has greater the degree of sound tooth structure.
affinity for argon laser while melanin absorbs diode and
Nd:YAG laser. Scattering of the Laser Light
The primary determinant, which decides the depth of There is also scattering of the laser light with
penetration and absorption of laser light in the target correspondence decrease of that energy and possibly
tissue, is the wavelength of the laser used. Depending producing no useful biologic effect. This property can
on the wavelength used, some lasers able to penetrate cause unwanted damage as there is heat transfer to the
the tissue deeper than others. In contrast, other laser has tissue adjacent to the surgical site. However, a beam
a limited penetration and has effect only on the tissue deflected in different directions facilitates the curing of
surface. For example, the Nd:YAG which is indicated for the composite resin or when treating an aphthous ulcer.3
bone and hard tissue applications, penetrates 2-5 mm
into tissue3 while CO2 laser has a limited penetration The clinician must be aware of certain factors before
up to 0.03 to 0.1 mm in the tissue, thus indicated for soft applications of lasers such as appropriate laser
tissue applications. This wavelength provides enough wavelength, beam diameter, focused or defocused mode,
depth to seal the damaged blood, lymphatic vessels and pulse energy or power output, spot size, and tissue
nerve endings resulting in good hemostasis and minimal cooling. The result of using the smaller spot greatly
post-operative morbidity.3 The Table 1 showing the increases the heat transfer from the laser to the tissue
wavelength of laser light used chromophores and their and a corresponding increased heat absorption in that
target tissue. smaller area. If the laser beam is allowed to diverged
from the target tissue, this would results in the increase
Transmission of the beam diameter and thus lessen the energy density
This property depends on the wavelength of laser light of the laser beam.
used. There is the transmission of the laser energy
directly through the tissue without producing any effect If a laser beam is allowed to strike the target tissue for a
on the target tissue. Nd:YAG, Argon and diode laser light longer time, it will cause the tissue temperature to rise.
gets transmitted through water, whereas tissue fluids This time can be regulated by the repetition rate of the
readily absorb the erbium family and CO2 at the outer pulsed laser emission mode as well.
International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015 8
David and Gupta Lasers in Dentistry
CLASSIFICATION OF LASERS3 so surgery can be performed safely as these wavelengths
are poorly absorbed by the dental hard tissue. This laser
Gas lasers: is indicated for gingivoplasty, sulcular debridement and
• Argon deeper coagulation process on gingival and mucosa. The
• Carbon-dioxide chief advantage of the diode lasers is one of a smaller
Liquid: size, portable instrument. These lasers can also stimulate
• Dyes fibroblastic proliferation at low energy levels.6,7
Solid:
• Nd:YAG Nd-YAG Lasers
• Erbium: yttrium aluminum garnet (Er: YAG) Nd:YAG has a solid active medium, which is a garnet
• Diode crystal combined with rare earth elements yttrium and
Semiconductor: aluminum, doped with neodymium ions. The available
• Hybrid silicon laser dental wavelength of 1064 nm is indicated for various
Excimers: soft-tissue procedures such as cutting and coagulating of
• Argon-fluoride gingival and sulcular debridement. This laser provides
• Krypton-fluoride good hemostasis provides a clear operating field during
• Xenon-fluoride soft-tissue procedures. The laser is also indicated for
the removal of incipient caries, although the working
LASERS WAVELENGTH USED IN efficiency is less in comparison with the Er: YAG, or Er,
DENTISTRY chromium (Cr):YSGG lasers. When used in a noncontact,
defocused mode, this wavelength can penetrate several
Argon Lasers millimeters which can be used for procedures such
as treatment of aphthous ulcers or pulpal analgesia.
This laser has an active medium of ionized argon gas, However, due to a decrease in pulpal function,
energized by a high current electrical discharge, and sometimes damage to the dental pulp can results.8
the laser light is delivered fiber-optically in continuous
wave and gated pulsed modes. There are two emission THE ERBIUM FAMILY
argon laser wavelengths used in dentistry: 488 nm
(blue) and 514 nm (blue green). Both wavelengths are The wavelengths that are used are:
poorly absorbed in the enamel and dentin which is
advantageous during cutting and sculpting gingival Erbium, Cr:YSGG (2780 nm)
tissues as there is minimal interaction with the dental
hard tissue without causing any damage to the tooth Erbium, Cr: YSGG (2780 nm) which has an active
surface. Both wavelength is used as an aid for caries medium of a solid crystal of yttrium scandium gallium
detection. When the argon laser light illuminates the garnet doped with erbium and chromium.
tooth, the carious area appears as a dark orange-red color
and is easily discernible from the surrounding healthy Erbium:YAG (2940 nm)
structures.3 Erbium: YAG (2940 nm) which has an active medium
of a solid crystal of yttrium aluminum garnet doped
Argon lasers are indicated in periodontics, as they with erbium. Both lasers aid in caries removal. The laser
possess bactericidal properties against Prevotella produces clean, sharp margins during cavity preparation.
intermedia and Porphyromonas gingivalis and also used Since, depth of penetration of laser wavelength is less, so
to treat vascular malformations such as a hemangioma. pulpal damage is minimal. During caries removal, since
Potential complications of this laser treatment include the laser has an anesthetic effect, the analgesia is not
granuloma formation, bleeding or non-resolution of routinely indicated in the majority of patients. The laser
the lesion.4,5 also assists in removal of endotoxins from root surfaces
so providing an anti-microbial effect. These lasers are
Diode Lasers comfortable to the patients as vibration produces from
The diode laser is manufactured from solid semiconductor the laser are less severe in comparison to the conventional
high-speed drill. Thus, they are less likely to provoke
crystals made from a combination of aluminum (with
intraoperative discomfort or pain.9,10
wavelength of 800 nm) or indium (900 nm), gallium
and arsenic. These wavelengths penetrate deep into the
The Er-Cr:YSGG Laser
mucosa and highly attenuated by the pigmented tissue,
although hemostasis is slow as compared with the argon This laser is widely indicated in restorative and etching
laser. These lasers are excellent soft tissue surgical lasers, procedures. During cavity preparation, the laser
9 International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015
David and Gupta Lasers in Dentistry
provides rough surfaces for bonding without causing concentration of acetylcholine, a pain mediator, through
any significant cracking in the dental hard tissue. The increased acetylcholine esterase activity.12
advantage of this laser for restorative dentistry is that
a carious lesion in close proximity to the gingiva can USES OF LASERS ON HARD TISSUES
be treated and the soft tissue recontoured with the
same instrumentation. Furthermore, tissue retraction Lasers for Caries Detection
for uncovering implants is safe with this wavelength,
because there is minimal heat transferred during the This diagnostic technology in which a Diagnodent, a
procedure. However, the rough surface produced during 655 nm diode laser, aids in the detection of incipient
etching procedures will have a wide range of strengths caries is called laser-induced fluorescence. When the
of enamel bonds which is unreliable. Therefore, the laser irradiates the tooth, the light is absorbed by organic
procedure still requires acid etching to obtain equivalent and inorganic substances present in the dental tissues,
bond strength.10 as well as by metabolites such as bacterial porphyrins.
These porphyrins showed some fluorescence after
CO2 Laser excitation by red light. Since bacteria are present in the
carious lesions, carious tissue exhibits more fluorescence
The CO2 laser is water or air cooled gas discharge, as compared to the healthy tissue which distinguish
containing a gaseous mixture with CO2 molecules, that between the carious and sound tooth structure. It can
helps in producing a beam of infrared light. The light detect occlusal, interproximal carious lesion or identify
energy, whose wavelength is 10,600 nm, well absorbed occult lesions beneath fissure sealants. Although, the
by water and is delivered through a hollow tube-like procedure is considered to be safe, further studies are
waveguide in continuous or gated pulsed mode. The laser required for explorations the beneficial effects of this
wavelength can easily assists in cutting and coagulation innovative technology.13-15
of soft tissue, thus providing a clear operating field. The
laser is indicated for the treatment of mucosal lesion, Lasers for Caries Removal and Cavity Preparation
since it has a limited penetration depth. Post-operative
pain usually is minimal to none as it reduced pain by The Er:YAG lasers are proven to be safe and effective
in caries removal and cavity preparation in pediatric
inducing local neural anesthesia as a function of neuron
and adults patients without significant damage to tooth
sealing and decreased pain mediator release. CO2 laser
structure or patient discomfort. This device also aid in
also has some disadvantages. However, there is delayed
removal of defective composite restoration and ablate
wound healing for a few days, as a result of delayed
the distal carious lesion while a tunneling technique
re-epithelization and a different pattern of wound
(in which the laser’s sapphire tip was angled directly
contraction. Furthermore, the loss of tactile sensation
toward the distal carious lesion), thus preserving the
could pose a disadvantage for the surgeon, but the tissue
tooth’s distal marginal ridge.16,17 The principle used is
ablation can be precise with careful technique.11
fluorescence. As the laser is targeted to the tissue, bacteria
present in the infected dentin provides signal to the
USE OF LASERS IN DENTINAL clinician and could also control the action of a pulsed
HYPERSENSITIVITY (DH) AND PAIN laser to achieve automated caries removal.
MANAGEMENT
Lasers Used for Calculus Removal
DH is one of the most common causes of dental pain.
The Er:YAG laser is used for calculus removal as the
A low level laser therapy (LLLT) has also been used
bacterial porphyrins in dental calculus give a strong
for the treatment of DH. This relies upon laser-induced
fluorescence signal, which can be used to control lasers
changes to neural transmission networks within the
used for scaling. These lasers are effective in removing
dental pulp, rather than alterations to the exposed
lipopolysaccharides and other root surface endotoxins
dentine surface, as is the case with other treatment
and are highly bactericidal against certain periodontal
modalities.
pathogens including P. gingivalis and Actinobacillus
actinomycetemcomitans.
It has been suggested that LLLT may elicit descending
inhibition in the central nervous system, in addition to
Laser Assisted Bleaching
local effects on nerve conduction, although this has yet
to be proven.12 Low-power lasers inhibit the release of The objective of laser bleaching is to achieve the ultimate
mediators from injured tissues. In other words, they power bleaching process using the most efficient energy
decrease concentration of chemical agents such as source while avoiding any adverse effects. Using the
histamine, acetylcholine, serotonin, H+ and K+, all of 488-nm argon laser as an energy source to excite the
which are pain mediators. Low-power lasers inhibit hydrogen peroxide molecule offers more advantages
International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015 10
David and Gupta Lasers in Dentistry
than other heating instruments. The argon laser rapidly USES OF LASERS ON SOFT TISSUES
excites the already unstable and reactive hydrogen
peroxide molecule; the energy then is absorbed into Laser Curettage
all intermolecular and reaches eigenstate vibrations.
Lasers can enhance bleaching by photo-oxidation of Both the Nd:YAG and diode lasers are indicated
colored molecules in the teeth or by interaction with the for curettage. Laser assisted curettage significantly
components of the bleaching gel through photochemical improves outcomes in mild to moderate periodontitis.
reactions. The result is a visually whitened tooth surface.18 The treatment is not invasive and comfortable to
the patients. The beneficial effects of these lasers are
Surgical Procedures due to the bacterial properties particularly against
periodontal pathogens such as A. actinomycetemcomitans
Many different laser wavelengths have been used in and P. gingivalis. However, recent studies have shown
Oral and maxillofacial surgery. Since there is excellent that there are no added advantages of these lasers as
absorption of CO2 laser at wavelength of 10,600 nm in the compared with the conventional debridement.
water-based tissues, it is widely indicated in oral surgical
procedures performed intraorally and extraorally. CO2 Laser Assisted Incisional and Excisional Biopsy
lasers make relatively deep and precise incisions and
thus excellent hemostasis. There is less traumatic bone These procedures are accomplished at 100°C. The lasers
cutting with the use of Erbium lasers resulting in post- are placed in cutting or focused mode, held perpendicular
operative discomfort to the patients. The management to the tissue and follow the surgical outline. When laser
of patients with sleep apnea, TMJ derangements, dental light interact with the soft tissue, there is vaporization
implants, premalignant lesions, and post-traumatic facial of intra and extracellular water content resulting in
scarring has improved significantly with the advent of ablation or removal of biological tissue. However, when
laser surgery. the temperature exceeds 200°C, there is heat generated
within the tissues during the results in carbonization and
In a Clinical trial, 250 patients were treated with CO2 irreversible tissue necrosis.
lasers for conditions like gingival hyperplasia, benign
and malignant lesions, red and white lesions and In addition, there are specific soft tissue indications for the
bleeding, and coagulation disorders. The results showed clinical use of lasers, including gingival depigmentation,
concluded that CO2 laser provides a bloodless field, less gingivectomy/gingivoplasty, operculectomy, sulcus
post-operative discomfort, tissue coagulation and better debridement, pre-impression sulcular retraction,
accessibility in some areas of oral cavity compared to laser assisted new attachment procedures, removal
conventional scalpel surgery. The advantages compared of granulation tissue. Pulp capping, pulpotomy and
to scalpel wounds also included site-specific wound pulpectomy, incisions and draining of abscesses, removal
sterilization; minimal intraoperative trauma and of hyperplastic tissues, frenectomy, vestibuloplasty,
subsequent less post-operative swelling, suturing is and treatment of herpetic and recurrent aphthous
not required in most of the cases, minimal use of local ulcers. Other excisional procedures that can be easily
anesthesia and less post-operative pain, discomfort, and performed using lasers are the removal of benign
better patient acceptance.19 growths such as fibromas or papillomas. In addition,
LLLT is indicated for oral soft tissue lesions such as
Bone Surgery and Osseous Crown Lengthening frictional keratosis, nicotinic stomatitis, leukoplakia,
erythroplakia, verrucous carcinoma.20
The YSGG laser was also the first cleared for bone,
including cutting, shaving, contouring and resecting
It has been shown that Er-Cr:YSGG (Waterlase C-100)
oral osseous tissues. The laser was later cleared for
system is used to release the fibrotic bands of oral
osteoplasty, ostectomy, and osseous recontouring to
submucous fibrosis. It works on “hydro-photonic
correct defects and create physiologic osseous contours
process” in which the energy from the Er-Cr: YSGG laser
necessary for ideal clinical results. In 2003, the YSGG
interacts with water droplets on the tissue to create water
laser was the first laser device cleared for osseous
molecule excitation, micro expansion and propulsion
crown lengthening to achieve biologic width which
giving a clean and precise hard-tissue cutting.
can be completed without laying a flap, suturing, or
damage to the bone (Wang, 2002). The ease of use of the
Photodynamic Therapy
YSGG system provides the dentist with a strong ROI
by performing the most of their own osseous crown A more powerful laser-initiated photochemical reaction is
lengthening procedures, which is important in an era photodynamic therapy (PDT), which has been employed
fueled by prime time “extreme” dental makeovers, and in the treatment of malignancies of the oral mucosa,
growing demand for aesthetic dentistry. particularly multifocal squamous cell carcinoma. As in
11 International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015
David and Gupta Lasers in Dentistry
photo - activated dye, laser-activation of a sensitizing dye Table 2: Laser applications in dentistry
in PDT generates reactive oxygen species. These in turn Application Possible laser types
directly damage cells and the associated blood vascular Basic research All types
network, triggering both necrosis, and apoptosiss.21 Laser tissue interaction
Oral medicine He Ne, diodes
PDT destroy the bulk of tumor cells, there is accumulating Laser doppler flow metry He Ne, diodes
evidence that PDT activates the host immune response, Laser induced fluorescence (caries diagnosis) Diode
and promotes anti-tumor immunity through the Photodynamic therapy (for treatment of oral cancer)
activation of macrophages and T lymphocytes. Clinical To release fibrotic bands in OSMF ErCr:YSGG
Oral soft tissue lesions frictional keratosis, Diode
studies have reported positive results for PDT treatment
leukoplakia, verrucous carcinoma)
of carcinoma in-situ and squamous cell carcinoma in
Oral and maxillofacial surgery
the oral cavity, with response rates approximating 90%.
To achieve hemostasis CO2
The treated sites characteristically show erythema and Tuberosity reduction, alveoloplasty, Erbium
edema, followed by necrosis and frank ulceration. The bone and flap removal
ulcerated lesions typically take up to 8 weeks to heal Conservative dentistry CO2, Nd:YAG, Er:YAG,
fully, and supportive analgesia is required in the first DH
few weeks. Other than short-term photosensitivity, the Cavity preparation Diode
treatment is tolerated well.22 Composite resin light curing CO2, Nd:YAG, Er:YAG
Tooth surface conditioning, removal of Argon, Er:YAG
Lasers in Pediatric Dentistry defective composite restoration
Endodontics Nd:YAG, CO2
Treatment with lasers is beneficial when used in children Root canal treatment, apicoectomy CO2, Nd:YAG
as there is precise and selective interaction of lasers with Periodontics
the soft tissue. All procedures previously discussed Laser-assisted curettage Nd:YAG, diode
are treated in the same manner in the p Pediatric Gingivectomy and gingivoplasty CO2
population as well. Lasers can provide treatment Analgesic effect and bio-stimulation
without the need for needles and high-speed hand pieces Stimulation of wound healing He Ne, diodes, Nd:YAG
causing less intra and post-operative discomfort to the DH: Dentinal hypersensitivity, Nd:YAG: Neodymium-doped:yttrium
children. Furthermore, there is less need for behavioral aluminum garnet, Er:YAG: Erbium:yttrium aluminum garnet,
Cr:YSGG: Chromium:yttrium-scandium-gallium-garnet
management therapies in case of lasers assisted therapy.
During laser treatment, hemostasis can be achieved
without the need of sutures in many patients. planning of patients. Lasers can also prove to be blessing
in disguise if not used safely and properly. As Aaron
The Table 2 summarizes the type of lasers used in Rose Says, “In right light at right time everything is
different specialties of dentistry. extraordinary.”
LIMITATIONS OF LASERS REFERENCES
1. Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical
• It requires additional training and education for periodontal therapy. Periodontol 2000 2004;36:59-97.
various clinical applications and types of lasers. 2. Yamamoto H, Sato K. Prevention of dental caries by acousto-
• High cost required to purchase equipment, optically Q-switched Nd: YAG laser irradiation. J Dent Res
implement technology and invest in required 1980;59:137.
education. 3. Coluzzi DJ. Fundamentals of dental lasers: Science and
instruments. Dent Clin North Am 2004;48:751-70, v.
• More than one laser may be needed since different
4. Kutsch VK. Dental caries illumination with the argon laser. J Clin
wavelengths are required for various procedures. Laser Med Surg 1993;11:323-7.
5. Finkbeiner RL. The results of 1328 periodontal pockets treated
CONCLUSION with the argon laser: Selective pocket thermolysis. J Clin Laser
Med Surg 1995;13:273-81.
6. Moritz A, Gutknecht N, Doertbudak O, Goharkhay K, Schoop U,
The use of laser technology has been widely used in Schauer P, et al. Bacterial reduction in periodontal pockets through
dentistry. When used efficaciously and ethically, lasers irradiation with a diode laser: A pilot study. J Clin Laser Med Surg
have been an essential tool in many dental treatments. 1997;15:33-7.
However, lasers have got its own limitations. It has never 7. Coluzzi DJ. Lasers and soft tissue curettage: An update. Compend
Contin Educ Dent 2002;23:1104-11.
been the “magic wand” in medicine and dentistry. The
8. White JM, Goodis HE, Rose CL. Use of the pulsed Nd: YAG laser
futures of laser dentistry are bright as further researches for intraoral soft tissue surgery. Lasers Surg Med 1991;11:455-61.
are going on. The emergence of lasers for various 9. Hossain M, Nakamura Y, Yamada Y, Kimura Y, Matsumoto N,
applications in dentistry may influence the treatment Matsumoto K. Effects of Er,Cr: YSGG laser irradiation in human
International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015 12
David and Gupta Lasers in Dentistry
enamel and dentin: Ablation and morphological studies. J Clin 17. Louw NP, Pameijer CH, Ackermann WD, Ertl T, Cappius HJ,
Laser Med Surg 1999;17:155-9. Norval G. Pulp histology after Er: YAG laser cavity preparation in
10. Frentzen M, Hoort HJ. The effect of Er: YAG irradiation on enamel subhuman primates – A pilot study. SADJ 2002;57:313-7.
and dentin. J Dent Res 1992;71:571. 18. Laser-assisted bleaching: An update. ADA Council on Scientific
11. Pogrel MA, Muff DF, Marshall GW. Structural changes in dental Affairs. J Am Dent Assoc 1998;129:1484-7.
enamel induced by high energy continuous wave carbon dioxide 19. Pick RM, Pecaro BC. Use of the CO2 laser in soft tissue dental
laser. Lasers Surg Med 1993;13:89-96. surgery. Lasers Surg Med 1987;7:207-13.
12. Khalighi HR, Anbari F, Beygom Taheri J, Bakhtiari S, Namazi Z, 20. Abraham RJ, Arathy S. Laser management of intraoral soft tissue
Pouralibaba F. Effect of low-power laser on treatment of orofacial lesions – A review of literature. IOSR J Dent Med Sci (IOSR-JDMS)
pain. J Dent Res Dent Clin Dent Prospects 2010;4:75-8. 2014;13:59-64.
13. El-Housseiny AA, Jamjoum H. Evaluation of visual, explorer, and 21. Dougherty TJ. An update on photodynamic therapy applications.
a laser device for detection of early occlusal caries. J Clin Pediatr J Clin Laser Med Surg 2002;20:3-7.
Dent 2001;26:41-8. 22. Vowels BR, Cassin M, Boufal MH, Walsh LJ, Rook AH.
14. Tam LE, McComb D. Diagnosis of occlusal caries: Part II. Recent Extracorporeal photochemotherapy induces the production of
diagnostic technologies. J Can Dent Assoc 2001;67:459-63. tumor necrosis factor-alpha by monocytes: Implications for the
15. Lussi A, Megert B, Longbottom C, Reich E, Francescut P. Clinical treatment of cutaneous T-cell lymphoma and systemic sclerosis.
performance of a laser fluorescence device for detection of J Invest Dermatol 1992;98:686-92.
occlusal caries lesions. Eur J Oral Sci 2001;109:14-9.
16. Glockner K, Rumpler J, Ebeleseder K, Städtler P. Intrapulpal How to cite this article: David CM, Gupta P. Lasers in Dentistry: A Review.
temperature during preparation with the Er: YAG laser compared Int J Adv Health Sci 2015;2(8):7-13.
to the conventional burr: An in vitro study. J Clin Laser Med Surg
Source of Support: Nil, Conflict of Interest: None declared.
1998;16:153-7.
13 International Journal of Advanced Health Sciences • Vol 2 Issue 8 • December 2015
Das könnte Ihnen auch gefallen
- Asds 03 0707Dokument5 SeitenAsds 03 0707AL-ABATCHI -10Noch keine Bewertungen
- Role of Lasers in Periodontology: A Review: Aashima B Dang, Neelakshi S RallanDokument5 SeitenRole of Lasers in Periodontology: A Review: Aashima B Dang, Neelakshi S RallanJayaprakash KuppusamyNoch keine Bewertungen
- Laser Innovation Dental PracticeDokument9 SeitenLaser Innovation Dental PracticeIana RusuNoch keine Bewertungen
- G PeriodicityDokument5 SeitenG Periodicitydr parveen bathlaNoch keine Bewertungen
- Laser and It's Application in Prosthetic DentistryDokument6 SeitenLaser and It's Application in Prosthetic DentistrySUKRASENANoch keine Bewertungen
- Research ArticleDokument5 SeitenResearch ArticleAtul ScNoch keine Bewertungen
- Application of Lasers in Dentistry 22 25Dokument4 SeitenApplication of Lasers in Dentistry 22 25SkAliHassanNoch keine Bewertungen
- Class III Malocclusion... مينا عمارDokument9 SeitenClass III Malocclusion... مينا عمارمينا عمار شكري محمودNoch keine Bewertungen
- Application of Laser in Periodontics PDFDokument3 SeitenApplication of Laser in Periodontics PDFRamona MateiNoch keine Bewertungen
- J Lasers Med Sci 2012 3 1 26 32Dokument7 SeitenJ Lasers Med Sci 2012 3 1 26 32Bagis Emre GulNoch keine Bewertungen
- Idjsr Se 0168Dokument4 SeitenIdjsr Se 0168Alfan MaulanaNoch keine Bewertungen
- Laser in Dentistry: An Innovative Tool in Modern Dental PracticeDokument9 SeitenLaser in Dentistry: An Innovative Tool in Modern Dental PracticeLeonardoNoch keine Bewertungen
- Laser in Dentistry: An Innovative Tool in Modern Dental PracticeDokument9 SeitenLaser in Dentistry: An Innovative Tool in Modern Dental PracticeSandhya GuptaNoch keine Bewertungen
- Laser in Dentistry An Innovative Tool in Modern deDokument9 SeitenLaser in Dentistry An Innovative Tool in Modern deRuxandra FitaNoch keine Bewertungen
- J Lasers Med Sci 2012 3 1 26 32Dokument7 SeitenJ Lasers Med Sci 2012 3 1 26 32Muhammad AbazaNoch keine Bewertungen
- Lecture 5 Laser in Operative DentistryDokument7 SeitenLecture 5 Laser in Operative DentistryDt omarNoch keine Bewertungen
- Lasers in PeriodonticsDokument61 SeitenLasers in PeriodonticsDrRanjeet Kumar ChaudharyNoch keine Bewertungen
- Operative Lec 7 2 20210606100733Dokument8 SeitenOperative Lec 7 2 20210606100733احمد علي سبع حمودNoch keine Bewertungen
- Laser in Endodontics-A Review ArticleDokument7 SeitenLaser in Endodontics-A Review ArticleKalpanaNoch keine Bewertungen
- Lasers in Fixed Prosthetic and Cosmetic ReconstructionDokument18 SeitenLasers in Fixed Prosthetic and Cosmetic ReconstructionElena DimitriuNoch keine Bewertungen
- Lasers in Endodontics: ReviewDokument7 SeitenLasers in Endodontics: ReviewShreya BagweNoch keine Bewertungen
- Uses of Laser, Ultrasonics, CBCT - DeD Written ReportDokument13 SeitenUses of Laser, Ultrasonics, CBCT - DeD Written ReportJanelle TamayoNoch keine Bewertungen
- Laser in Conservative DentistryDokument39 SeitenLaser in Conservative DentistryAiluul AlmaaNoch keine Bewertungen
- Lasers Used in Operative Dentistry and EndodonticsDokument28 SeitenLasers Used in Operative Dentistry and EndodonticsNingombam Robinson Singh0% (1)
- Frenectomy1 PDFDokument5 SeitenFrenectomy1 PDFEdi NugrohoNoch keine Bewertungen
- LasersDokument63 SeitenLasersSamridhi SrivastavaNoch keine Bewertungen
- Laser ApplicationsDokument11 SeitenLaser ApplicationsBruno MañonNoch keine Bewertungen
- Evolution of Lasers: A Delight in Dentistry: Articles GeneralDokument7 SeitenEvolution of Lasers: A Delight in Dentistry: Articles Generalshamshuddin patelNoch keine Bewertungen
- Use of Laser Systems in OrthodonticsDokument8 SeitenUse of Laser Systems in OrthodonticsCatherine NocuaNoch keine Bewertungen
- Chapter 113: Lasers in Otolaryngology Stanley M. Shapshay, Elie E. RebeizDokument24 SeitenChapter 113: Lasers in Otolaryngology Stanley M. Shapshay, Elie E. RebeizJonNoch keine Bewertungen
- Laser and Cryosurgery MADE EASYDokument6 SeitenLaser and Cryosurgery MADE EASYMohammedNoch keine Bewertungen
- Lasers in Prosthodontics: Presented By: Dr. Jehan Dordi 2 Yr. MdsDokument142 SeitenLasers in Prosthodontics: Presented By: Dr. Jehan Dordi 2 Yr. MdsAkanksha MahajanNoch keine Bewertungen
- Medical Applications of Laser: - Presented by R.S. Jaiya Dharshini S. ElakkiaDokument28 SeitenMedical Applications of Laser: - Presented by R.S. Jaiya Dharshini S. Elakkiaaaa19Noch keine Bewertungen
- Application of Laser in ProsthodonticsDokument42 SeitenApplication of Laser in Prosthodonticsvarsha ammuNoch keine Bewertungen
- PDFDokument1 SeitePDFAna-Patricia Gumeniuc - TașcăNoch keine Bewertungen
- Laser and Its Application in Medicine: Dr. Mohammed FathiDokument13 SeitenLaser and Its Application in Medicine: Dr. Mohammed FathiAhmed AdelNoch keine Bewertungen
- Laser in ProsthodonticsDokument84 SeitenLaser in ProsthodonticsmarwaNoch keine Bewertungen
- Lasers and Its Role in Endodontics / Orthodontic Courses by Indian Dental AcademyDokument73 SeitenLasers and Its Role in Endodontics / Orthodontic Courses by Indian Dental Academyindian dental academyNoch keine Bewertungen
- Advances in Laser Technology and Cold Lasers in Periodontal Therapy A Review PDFDokument4 SeitenAdvances in Laser Technology and Cold Lasers in Periodontal Therapy A Review PDFInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Prevention 29Dokument4 SeitenPrevention 29Sura Abdel JabbarNoch keine Bewertungen
- Versatility of An 810 NM Diode Laser in DentistryDokument10 SeitenVersatility of An 810 NM Diode Laser in DentistryGloria SequeiraNoch keine Bewertungen
- Soft-Tissue Lasers in OrthodonticsDokument5 SeitenSoft-Tissue Lasers in OrthodonticsEsmeralda SoriaNoch keine Bewertungen
- (Balkan Journal of Dental Medicine) Application of High-Power Diode Laser and Photodynamic Therapy in Endodontic Treatment - Review of The LiteratureDokument4 Seiten(Balkan Journal of Dental Medicine) Application of High-Power Diode Laser and Photodynamic Therapy in Endodontic Treatment - Review of The LiteraturejuanaNoch keine Bewertungen
- Laser Application in Constractive DentistryDokument23 SeitenLaser Application in Constractive Dentistryhanan78632Noch keine Bewertungen
- Lasers General Principles: A Review: January 2013Dokument15 SeitenLasers General Principles: A Review: January 2013Nanda GaibNoch keine Bewertungen
- Laser and Its Use in Pediatric Dentistry: A Review of Literature and A Recent UpdateDokument5 SeitenLaser and Its Use in Pediatric Dentistry: A Review of Literature and A Recent UpdateTiaraNoch keine Bewertungen
- Journal Laser and Its Use in Pediatric Dentistry A ReviewDokument5 SeitenJournal Laser and Its Use in Pediatric Dentistry A ReviewTiaraNoch keine Bewertungen
- Dr. Hossam Eldin Sayed Ali: Lecturer of Medical Biophysics The Research Institute of OphthalmologyDokument32 SeitenDr. Hossam Eldin Sayed Ali: Lecturer of Medical Biophysics The Research Institute of OphthalmologyRiya MathurNoch keine Bewertungen
- Laser-An Emerging Tool in Surgical Periodontal Therapy: An OverviewDokument3 SeitenLaser-An Emerging Tool in Surgical Periodontal Therapy: An OverviewBOHR International Journal of Current research in Dentistry (BIJCRID)Noch keine Bewertungen
- Group 11 - Laser DentistryDokument21 SeitenGroup 11 - Laser DentistryEsper SorianoNoch keine Bewertungen
- Policy On The Use of Lasers For Pediatric DentalDokument4 SeitenPolicy On The Use of Lasers For Pediatric DentalمعتزباللهNoch keine Bewertungen
- The Use of Lasers For Direct Pulp Capping: Takashi Komabayashi, Arata Ebihara, and Akira AokiDokument10 SeitenThe Use of Lasers For Direct Pulp Capping: Takashi Komabayashi, Arata Ebihara, and Akira AokiCamila DAmicoNoch keine Bewertungen
- Lasers in EndodonticsDokument46 SeitenLasers in EndodonticsShazeena QaiserNoch keine Bewertungen
- Lasers in Pediatric Dentistry PedoDokument47 SeitenLasers in Pediatric Dentistry PedoFourthMolar.com50% (2)
- Un Peu Secu LaserDokument15 SeitenUn Peu Secu Laser00000000Noch keine Bewertungen
- Lasers in Conservative DentistryDokument5 SeitenLasers in Conservative DentistryArgjend Ajvazi100% (1)
- Lasers in ProsthodonticsDokument15 SeitenLasers in ProsthodonticsIJAR JOURNALNoch keine Bewertungen
- Femtosecond Laser - Principles and Application in OphthalmologyVon EverandFemtosecond Laser - Principles and Application in OphthalmologyNoch keine Bewertungen
- Cbcthand BookDokument30 SeitenCbcthand BookDrMohamed AssadawyNoch keine Bewertungen
- Vaccines 06 00044 PDFDokument11 SeitenVaccines 06 00044 PDFDrMohamed AssadawyNoch keine Bewertungen
- Chapter Overview: Point Operations!: Relating Gray Values To Brightness!Dokument36 SeitenChapter Overview: Point Operations!: Relating Gray Values To Brightness!DrMohamed AssadawyNoch keine Bewertungen
- 10.1007/978 3 642 28994 1 PDFDokument198 Seiten10.1007/978 3 642 28994 1 PDFDrMohamed AssadawyNoch keine Bewertungen
- CariesDokument4 SeitenCariesDrMohamed AssadawyNoch keine Bewertungen
- 053 Handbook of Medical Imaging Processing and Analysis - Isaac BankmanDokument5 Seiten053 Handbook of Medical Imaging Processing and Analysis - Isaac BankmanDrMohamed AssadawyNoch keine Bewertungen
- Hanbook of DrugsDokument45 SeitenHanbook of DrugsDrMohamed AssadawyNoch keine Bewertungen
- 1.oral Infectious DiseasesDokument68 Seiten1.oral Infectious DiseasesDrMohamed AssadawyNoch keine Bewertungen
- Dr.-Tamara-Part 3Dokument14 SeitenDr.-Tamara-Part 3DrMohamed AssadawyNoch keine Bewertungen
- Clinical and Radiographic of Marginal Periimplant Tissue Stability After Buccal Defect Regeneration Using Porous Titanium GranuDokument12 SeitenClinical and Radiographic of Marginal Periimplant Tissue Stability After Buccal Defect Regeneration Using Porous Titanium GranuDrMohamed AssadawyNoch keine Bewertungen
- Peri Implant Tissue EvaluationDokument129 SeitenPeri Implant Tissue EvaluationDrMohamed Assadawy100% (1)
- Bone Remodling RateDokument111 SeitenBone Remodling RateDrMohamed AssadawyNoch keine Bewertungen
- ThyroidectomyDokument51 SeitenThyroidectomyPopey Moore100% (1)
- PancytopeniaDokument9 SeitenPancytopeniadrhammadtufailNoch keine Bewertungen
- The OncologistDokument7 SeitenThe OncologistManunart FeungpeanNoch keine Bewertungen
- Wood Flour MsdsDokument2 SeitenWood Flour MsdscliffrajjoelNoch keine Bewertungen
- Gasteroenterology 201 247Dokument28 SeitenGasteroenterology 201 247Ahmed Kh. Abu WardaNoch keine Bewertungen
- Multiple MyelomaDokument2 SeitenMultiple MyelomaKolin JandocNoch keine Bewertungen
- DsDokument9 SeitenDsVavaxxxRemusaNoch keine Bewertungen
- Edema de ReinkeDokument9 SeitenEdema de ReinkeDaniel SuárezNoch keine Bewertungen
- NCP Karl Jacon M. FerolinoDokument4 SeitenNCP Karl Jacon M. FerolinoWhyng CabugayanNoch keine Bewertungen
- Pathologic Calcification: Dr. Deepak K. GuptaDokument25 SeitenPathologic Calcification: Dr. Deepak K. Guptaاحمد زيد سعيد100% (1)
- Tumors of SpineDokument13 SeitenTumors of Spinebosnia agusNoch keine Bewertungen
- Nasha Winters First 5 Steps To Take After A Cancer Diagnosis EGuideDokument11 SeitenNasha Winters First 5 Steps To Take After A Cancer Diagnosis EGuideK Mehmet ŞensoyNoch keine Bewertungen
- Dse Eng PP 3Dokument19 SeitenDse Eng PP 3SCYeungNoch keine Bewertungen
- Leukemia 2018 For GNM 2ndDokument36 SeitenLeukemia 2018 For GNM 2ndshapan biswaNoch keine Bewertungen
- Marino 2016Dokument9 SeitenMarino 2016DejanNoch keine Bewertungen
- May 2019 Issue of Active LivingDokument20 SeitenMay 2019 Issue of Active Livingmgruender1100% (2)
- Cancer Statistics, 2011: The Impact of Eliminating Socioeconomic and Racial Disparities On Premature Cancer DeathsDokument25 SeitenCancer Statistics, 2011: The Impact of Eliminating Socioeconomic and Racial Disparities On Premature Cancer DeathshamzaloNoch keine Bewertungen
- Stress and HormonesDokument5 SeitenStress and HormonesDiana Espinoza SegoviaNoch keine Bewertungen
- Atenolol Vs Propranolol ComparisonDokument7 SeitenAtenolol Vs Propranolol Comparisonpooja lokhandeNoch keine Bewertungen
- Role of Classical Conditioning in Learning Gastrointestinal SymptomsDokument8 SeitenRole of Classical Conditioning in Learning Gastrointestinal SymptomsjoaomartinelliNoch keine Bewertungen
- Сhronic pancreatitis: Lykhatska G.VDokument42 SeitenСhronic pancreatitis: Lykhatska G.VOlga CîrsteaNoch keine Bewertungen
- HIV A Virus Like No OtherDokument83 SeitenHIV A Virus Like No Otherbadboy6.868510Noch keine Bewertungen
- Nasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyDokument4 SeitenNasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyEditor IJTSRDNoch keine Bewertungen
- Gastric Surgery MCQDokument6 SeitenGastric Surgery MCQSajag GuptaNoch keine Bewertungen
- Review Health-Seeking BehaviorDokument11 SeitenReview Health-Seeking BehaviorDadanMKNoch keine Bewertungen
- FAQ MaV MaYojanaDokument3 SeitenFAQ MaV MaYojanaDhruv GhevariyaNoch keine Bewertungen
- EAT-Lancet Is A FraudDokument4 SeitenEAT-Lancet Is A FraudAnonymous BWVVQpxNoch keine Bewertungen
- Health - November 2015Dokument116 SeitenHealth - November 2015alejandronealNoch keine Bewertungen
- GNM KidneyDokument4 SeitenGNM KidneyaskoreNoch keine Bewertungen
- AmputationDokument160 SeitenAmputationChamalla Deepak100% (4)