Beruflich Dokumente
Kultur Dokumente
Study Hard, Be Smart & Confident and Win. Good Luck!!!!!!!!!!!!!!!!!!!
Hochgeladen von
BasmanMarkus0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
66 Ansichten1 SeiteThis document summarizes 4 medical cases: 1) A 12-year-old boy presented with ankle swelling was assessed for rheumatic fever. 2) A 19-year-old male presented with unilateral red eye and was examined for keratitis. 3) A 4-year-old boy presented with vomiting and diarrhea and was assessed for 5% dehydration and fluid management. 4) A 33-year-old female presented with relationship problems and was evaluated for depression, anxiety, substance use disorder, and referred to a psychologist. The panel discussed hematuria differential diagnosis and hemolytic uremic syndrome. Study hard to be smart, confident and succeed.
Originalbeschreibung:
PESCI
Originaltitel
6th April Acrrm
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenThis document summarizes 4 medical cases: 1) A 12-year-old boy presented with ankle swelling was assessed for rheumatic fever. 2) A 19-year-old male presented with unilateral red eye and was examined for keratitis. 3) A 4-year-old boy presented with vomiting and diarrhea and was assessed for 5% dehydration and fluid management. 4) A 33-year-old female presented with relationship problems and was evaluated for depression, anxiety, substance use disorder, and referred to a psychologist. The panel discussed hematuria differential diagnosis and hemolytic uremic syndrome. Study hard to be smart, confident and succeed.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
66 Ansichten1 SeiteStudy Hard, Be Smart & Confident and Win. Good Luck!!!!!!!!!!!!!!!!!!!
Hochgeladen von
BasmanMarkusThis document summarizes 4 medical cases: 1) A 12-year-old boy presented with ankle swelling was assessed for rheumatic fever. 2) A 19-year-old male presented with unilateral red eye and was examined for keratitis. 3) A 4-year-old boy presented with vomiting and diarrhea and was assessed for 5% dehydration and fluid management. 4) A 33-year-old female presented with relationship problems and was evaluated for depression, anxiety, substance use disorder, and referred to a psychologist. The panel discussed hematuria differential diagnosis and hemolytic uremic syndrome. Study hard to be smart, confident and succeed.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
6 th April, Acrrm Brisbane/ Dr Sumona
CASE 1: 12 yr old aboriginal boy came with painful ankle swelling
Rheumatic fever, asked d/d, physical exam,
How will you manage?
CASE 2: 19 yr old male with unilateral red eye?
Asked d/d, they gave me a picture (keratitis)
Asked how would you exam eye/ mx
CASE 3: 4 yr old boy with vomiting and diarrhoea
Acute gastro enteritis
Mild 5% dehydration
Asked abt fluid mx, s/s of dehydration
Office test: BSL,urine dipstick
Panel asked if you get dark and concentrated urine, What are the d/d then?
I said HUS & refer patient in hospital
CASE 4: 33 yr old female with relationship problem?
Took detail hx
Ruled out depression, anxiety,substance use disorder, mania
Refered to Psychologist for CBT
Study hard, be smart & confident and win.
Good luck!!!!!!!!!!!!!!!!!!!
Das könnte Ihnen auch gefallen
- GPDokument3 SeitenGPYwagar YwagarNoch keine Bewertungen
- Acrrm Recalls Latest PDFDokument16 SeitenAcrrm Recalls Latest PDFRumana Ali100% (2)
- Acrrm Recalls Retouched-2Dokument13 SeitenAcrrm Recalls Retouched-2Rumana AliNoch keine Bewertungen
- Recall 152, 15.6.13 AMC CLINICALDokument23 SeitenRecall 152, 15.6.13 AMC CLINICALAMMARANoch keine Bewertungen
- AMC Clinical 2009 RecallsDokument34 SeitenAMC Clinical 2009 Recallsbreezingthru100% (6)
- PESCI Recalls PDFDokument9 SeitenPESCI Recalls PDFDanishNoch keine Bewertungen
- Amc Question Bank ClinicalsDokument36 SeitenAmc Question Bank ClinicalsSoumen Dutt100% (1)
- April 21st Recalls With Approaches and AMC Feedback Recollected From Several Posted MaterialsDokument6 SeitenApril 21st Recalls With Approaches and AMC Feedback Recollected From Several Posted MaterialsqurbanNoch keine Bewertungen
- AMC OSCE Answers MelbGroup2005Dokument135 SeitenAMC OSCE Answers MelbGroup2005Manish AryanNoch keine Bewertungen
- Pesci 12Dokument5 SeitenPesci 12Rumana Ali100% (3)
- Med and Surg RecallDokument15 SeitenMed and Surg RecallSherif ElbadrawyNoch keine Bewertungen
- Sydney 2008 MarchDokument8 SeitenSydney 2008 MarchYwagar YwagarNoch keine Bewertungen
- Examination: (Look, Listen, Feel !!!!)Dokument13 SeitenExamination: (Look, Listen, Feel !!!!)Sherif Elbadrawy100% (1)
- OSCE Melb11Nov06Dokument7 SeitenOSCE Melb11Nov06janaka1022Noch keine Bewertungen
- AMC Clinical Sample QuestionsDokument20 SeitenAMC Clinical Sample Questionslaroya_31Noch keine Bewertungen
- 4 - Acrrm Pesci - WaDokument1 Seite4 - Acrrm Pesci - WaBasmanMarkusNoch keine Bewertungen
- 16 - Imp QuestionsDokument9 Seiten16 - Imp QuestionsBasmanMarkus100% (1)
- Pesci-U: Pesci (5 December 2011) - Via Video ConferenceDokument2 SeitenPesci-U: Pesci (5 December 2011) - Via Video ConferenceBrianNoch keine Bewertungen
- 2021 Pe ListsDokument40 Seiten2021 Pe ListsPragashRajendirenNoch keine Bewertungen
- Marwan PEDokument12 SeitenMarwan PEHalfidaNoch keine Bewertungen
- ACRRM PESCI Application FormDokument6 SeitenACRRM PESCI Application FormChenthanKrishNoch keine Bewertungen
- Pepsci RecallDokument3 SeitenPepsci RecallRumana AliNoch keine Bewertungen
- AMC-2007 Clinical Examination RecallsDokument156 SeitenAMC-2007 Clinical Examination Recallsbreezingthru100% (1)
- DR Tasrifa Jahan-7th April 2021-Passed Feedback - Online ExamDokument19 SeitenDR Tasrifa Jahan-7th April 2021-Passed Feedback - Online ExamOmesh Prathiraja100% (1)
- 10 April Recalls MelbourneDokument3 Seiten10 April Recalls MelbournequrbanNoch keine Bewertungen
- Marwan PsychiatryDokument201 SeitenMarwan Psychiatrykasuni1senavirathnaNoch keine Bewertungen
- Amc Clinical Recalls - 2004Dokument19 SeitenAmc Clinical Recalls - 2004breezingthruNoch keine Bewertungen
- Psych RecallDokument10 SeitenPsych RecallSherif ElbadrawyNoch keine Bewertungen
- 68 Important Scenarios For ST 5 PracticeDokument20 Seiten68 Important Scenarios For ST 5 PracticeSalem ELsayed Abdel AzizNoch keine Bewertungen
- BrisDokument9 SeitenBrisYwagar YwagarNoch keine Bewertungen
- Marwan File, P.E CasesDokument2 SeitenMarwan File, P.E Caseskasuni1senavirathna0% (1)
- Recall 139, Sum 2.3.13 AMC CLINICALDokument34 SeitenRecall 139, Sum 2.3.13 AMC CLINICALAMMARA100% (3)
- AMC-2008 Clinical Examination RecallsDokument50 SeitenAMC-2008 Clinical Examination Recallsbreezingthru100% (3)
- Clinical Tutorial 2008.11.05Dokument31 SeitenClinical Tutorial 2008.11.05Ywagar Ywagar100% (1)
- AMC Clinical Orthopaedics - RecallsDokument7 SeitenAMC Clinical Orthopaedics - Recallsbreezingthru100% (1)
- May 31Dokument6 SeitenMay 31Sherif ElbadrawyNoch keine Bewertungen
- PE Recall AMC ExamDokument9 SeitenPE Recall AMC ExamSherif Elbadrawy100% (1)
- Marwan PDDokument251 SeitenMarwan PDkasuni1senavirathnaNoch keine Bewertungen
- AMC Clinical Recalls - PAEDIATRICSDokument28 SeitenAMC Clinical Recalls - PAEDIATRICSbreezingthru100% (4)
- AMC Clinical Recall 138, Sum 16.2.13Dokument15 SeitenAMC Clinical Recall 138, Sum 16.2.13AMMARANoch keine Bewertungen
- Dec 11 2018 AMC Clinical RecallsDokument18 SeitenDec 11 2018 AMC Clinical Recallsqurban100% (1)
- Assessing General Practice Knowledge Base: The Applied Knowledge TestDokument3 SeitenAssessing General Practice Knowledge Base: The Applied Knowledge TestMadiha Mujahid0% (1)
- AMC CLINICAL Material and TipsDokument4 SeitenAMC CLINICAL Material and TipsRumana Ali50% (6)
- AMC Clinical Psychiatry NoteDokument59 SeitenAMC Clinical Psychiatry NoteShahriar Ahmed Sujoy100% (3)
- Marwan OGDokument338 SeitenMarwan OGkasuni1senavirathnaNoch keine Bewertungen
- Recall 137, Sum 6.4.13 AMC CLINICALDokument36 SeitenRecall 137, Sum 6.4.13 AMC CLINICALAMMARANoch keine Bewertungen
- ACln2007!09!08MEL Retest Wd97Dokument6 SeitenACln2007!09!08MEL Retest Wd97Ywagar YwagarNoch keine Bewertungen
- Respiratory Recalls Printable Version SMADokument26 SeitenRespiratory Recalls Printable Version SMAAleksandr ShnyrovNoch keine Bewertungen
- Recall 67, 25.2.12Dokument23 SeitenRecall 67, 25.2.12fdsadfNoch keine Bewertungen
- AMC Online - Recalls - V3Dokument167 SeitenAMC Online - Recalls - V3Halfida100% (3)
- AMC Obstetrics TopicsDokument29 SeitenAMC Obstetrics TopicsMoe Zaw Lin100% (1)
- Post-Corona Recalls V4Dokument262 SeitenPost-Corona Recalls V4Halfida100% (1)
- Pancreas QuestionDokument7 SeitenPancreas QuestionRumana Ali100% (1)
- Brisbane July 2008 RecallDokument11 SeitenBrisbane July 2008 RecallYwagar YwagarNoch keine Bewertungen
- Recall 145, Sum 6.4.13AMC CLINICALDokument19 SeitenRecall 145, Sum 6.4.13AMC CLINICALAMMARANoch keine Bewertungen
- Friends Ccs CasesDokument23 SeitenFriends Ccs Casesvivekmo100% (2)
- Thread Session Questions Group 6Dokument2 SeitenThread Session Questions Group 6Mengda ZhangNoch keine Bewertungen
- May 2017 RecallDokument11 SeitenMay 2017 RecallSherif ElbadrawyNoch keine Bewertungen
- Formative Test Family Medicine: Ikatlah Ilmu Dengan Menuliskannya. (Ali Bin Abi Thalib)Dokument23 SeitenFormative Test Family Medicine: Ikatlah Ilmu Dengan Menuliskannya. (Ali Bin Abi Thalib)Raissa Metasari TantoNoch keine Bewertungen
- 4 Tips For Passing PACES: PreparationDokument10 Seiten4 Tips For Passing PACES: PreparationAhmed AbdelgelilNoch keine Bewertungen
- 16 - Imp QuestionsDokument9 Seiten16 - Imp QuestionsBasmanMarkus100% (1)
- Terms and Conditions Swedish State Insurance For Fee-Paying Students - Plus (FAS Plus) 2015-01-01Dokument21 SeitenTerms and Conditions Swedish State Insurance For Fee-Paying Students - Plus (FAS Plus) 2015-01-01BasmanMarkusNoch keine Bewertungen
- Duo LingoDokument41 SeitenDuo LingoBasmanMarkus100% (1)
- 4 - Acrrm Pesci - WaDokument1 Seite4 - Acrrm Pesci - WaBasmanMarkusNoch keine Bewertungen
- Ponstan Suspension 50mgDokument1 SeitePonstan Suspension 50mgBasmanMarkusNoch keine Bewertungen
- IELTS Listening TestDokument10 SeitenIELTS Listening TestBasmanMarkus100% (1)
- IELTS Listening TestDokument10 SeitenIELTS Listening TestBasmanMarkus100% (1)
- Family Medicine OSCEDokument195 SeitenFamily Medicine OSCEBasmanMarkus93% (14)
- نتائجDokument3 SeitenنتائجBasmanMarkusNoch keine Bewertungen
- Practice Osce Scenarios PDFDokument20 SeitenPractice Osce Scenarios PDFa1docNoch keine Bewertungen
- Childhood Autism Rating Scale™ - Second Edition (CARS-2) : August 2015Dokument5 SeitenChildhood Autism Rating Scale™ - Second Edition (CARS-2) : August 2015Alejandro Espinoza67% (3)
- List of Different Phobias2Dokument3 SeitenList of Different Phobias2Deborah ChristineNoch keine Bewertungen
- Dissociative Processes, Multiple Personality, and Dream FunctionsDokument12 SeitenDissociative Processes, Multiple Personality, and Dream FunctionslordgalaxyNoch keine Bewertungen
- Abnormal Psychology, Thirteenth Edition, DSM-5 UpdateDokument43 SeitenAbnormal Psychology, Thirteenth Edition, DSM-5 UpdateJasmin ValloNoch keine Bewertungen
- CIDI 3.0 Bipolar Screening Scales FinalDokument14 SeitenCIDI 3.0 Bipolar Screening Scales FinalAnonymous zxTFUoqzklNoch keine Bewertungen
- Ocd Resource PacketDokument47 SeitenOcd Resource Packetapi-231586322Noch keine Bewertungen
- Depression PsychoticDokument10 SeitenDepression Psychoticharumimiaomiao_198930% (1)
- Poems by Betty Fox Frazer - Psychiatric NurseDokument4 SeitenPoems by Betty Fox Frazer - Psychiatric NurseBetty FoxNoch keine Bewertungen
- DSM-5: Assessment and Treatment of PTSDDokument63 SeitenDSM-5: Assessment and Treatment of PTSDŁukasz Ostrowski100% (1)
- 1collins Donnelly Starving The Anxiety GremlinDokument5 Seiten1collins Donnelly Starving The Anxiety GremlinCarolina Alves0% (1)
- DR S Khoza Department of Clinical Pharmacology University of ZimbabweDokument43 SeitenDR S Khoza Department of Clinical Pharmacology University of ZimbabweCuthbert Tinotenda MusarurwaNoch keine Bewertungen
- Histrionic Personality Disorder: Effects of HPDDokument2 SeitenHistrionic Personality Disorder: Effects of HPDJrBong Semanero100% (1)
- Herman-1992-Journal of Traumatic StressDokument15 SeitenHerman-1992-Journal of Traumatic StressAbdulWakhidNoch keine Bewertungen
- PichosisDokument3 SeitenPichosisalexandraNoch keine Bewertungen
- Suicide ReportDokument4 SeitenSuicide ReportAlikman HadjiamerNoch keine Bewertungen
- Psychiatric Assessment ToolDokument53 SeitenPsychiatric Assessment ToolLori100% (5)
- Tugas UNtar 3Dokument28 SeitenTugas UNtar 3Daniel Filemon PosoNoch keine Bewertungen
- Psychotherapy For Personality Disorders - Gunderson GabbardDokument187 SeitenPsychotherapy For Personality Disorders - Gunderson GabbardMichelle Schultz94% (17)
- Panic DisorderDokument2 SeitenPanic DisorderSalnangNoch keine Bewertungen
- The Kirkbride Plan': A Divergent Way To Treat The Mental IllnessDokument3 SeitenThe Kirkbride Plan': A Divergent Way To Treat The Mental IllnessCasas Mantilla Camilo JuanNoch keine Bewertungen
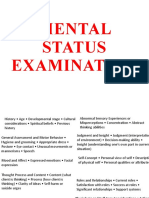
- Mental Status ExaminationDokument16 SeitenMental Status ExaminationConrad C. CatimbangNoch keine Bewertungen
- Somatoform Disorders and Factitious Disorders: DSM-1V-TRDokument33 SeitenSomatoform Disorders and Factitious Disorders: DSM-1V-TRNoelle Grace Ulep Baroman100% (1)
- Borderline Personality Disorder Diagnosis Symptoms TreatmentDokument57 SeitenBorderline Personality Disorder Diagnosis Symptoms TreatmentAnand KirtiNoch keine Bewertungen
- Negative Effects of Gambling Addiction: Elizabeth Kurtz Block 1 1 June 2012Dokument11 SeitenNegative Effects of Gambling Addiction: Elizabeth Kurtz Block 1 1 June 2012EK200620Noch keine Bewertungen
- Anxiety Disorders in Children and Adolescents 1Dokument16 SeitenAnxiety Disorders in Children and Adolescents 1api-253782185Noch keine Bewertungen
- NCP For Obsessions in NCM 117 (Anxiety)Dokument2 SeitenNCP For Obsessions in NCM 117 (Anxiety)unkown userNoch keine Bewertungen
- Abilify Dosing GuideDokument2 SeitenAbilify Dosing GuidemtassyNoch keine Bewertungen
- Nightmare Disorder and Isolated Sleep ParalysisDokument7 SeitenNightmare Disorder and Isolated Sleep ParalysissavitageraNoch keine Bewertungen
- M Chat Tamil 2020Dokument8 SeitenM Chat Tamil 2020Profe CatalinaNoch keine Bewertungen
- SchizophreniaDokument27 SeitenSchizophreniacadpsy100% (3)