Beruflich Dokumente
Kultur Dokumente
CKD PDF
Hochgeladen von
mkafabillahOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CKD PDF
Hochgeladen von
mkafabillahCopyright:
Verfügbare Formate
Clinical Review Article
Series Editor: Mark A. Perazella, MD, FACP
Chronic Kidney Disease:
A New Classification and Staging System
Mark A. Perazella, MD, FACP
Robert F. Reilly, MD
hronic kidney disease (CKD) is a growing gram in 1996 increased 12.5% over the previous year,
C health problem in the United States. Several
recently published studies emphasize that CKD
is underdiagnosed and undertreated.1 – 4 It
therefore cannot be overstated that recognition of this
chronic condition is crucial to facilitate the employ-
computing to an estimated $10.96 billion.10 A larger im-
pact can be predicted from the estimated growth of
both the CKD and ESRD populations.
The growth of the ESRD population will also exac-
erbate the predicted shortfall in nephrology clinicians.
ment of measures that can slow progression to end- The increase in both CKD and ESRD populations may
stage renal disease (ESRD). Also, appropriate and time- overwhelm the ability of nephrologists and other
ly interventions in patients with CKD would enhance health care providers to fully provide interventions that
therapy of comorbid conditions, reduce associated will improve both the length and quality of patients’
complications, and improve patient outcomes. These lives if an organized approach to this problem is not in
are certainly achievable goals, as many effective thera- place. Hence, it became imperative that the CKD epi-
pies for slowing the progression of CKD and correcting demic be addressed in a comprehensive fashion. The
or reducing associated comorbidities have become NKF took the challenge and created the CKD Work
available in the past few decades.5 – 7 To this end, a sys- Group to achieve this goal.
tem to classify stages of CKD is justified to permit a logi-
cal approach to diagnosis and therapy in these patients. DEFINING CKD AND DEVELOPING A STAGING SYSTEM
A working group of the National Kidney Foundation Several terms have been used to describe the period
(NKF) recently published clinical practice guidelines to between the initial diagnosis of kidney disease and the
aid physicians in diagnosing and managing CKD.8 institution of renal replacement therapy (ie, dialysis or
Based on the NKF guidelines, this article will examine transplantation). Such terms have included pre-ESRD,
the implications of CKD growth, establish a definition chronic renal insufficiency, chronic renal failure, and chronic
for CKD, describe a system to classify stages of CKD, renal disease. Unfortunately, none of these terms is par-
and briefly review the prevalence of and treatment ticularly accurate and, in fact, may be confusing to non-
options for CKD. nephrology physicians. The term pre-ESRD gives the
impression that dialysis is an inevitable outcome of all
SCOPE OF THE PROBLEM kidney diseases and implies that no effective therapies
The implications of rapid growth in both the inci- exist to halt or slow the progression of CKD. The terms
dence and prevalence of CKD are enormous. The most renal insufficiency, chronic renal failure, chronic renal disease
worrisome is that this growth will result in a huge influx and pre-ESRD have negative connotations; also, these
of patients into the ESRD system. Based on data from terms include the word renal, which is not easily under-
the US Renal Data System, the incidence of ESRD stood by patients or their families. For these reasons,
has increased steadily for the past 15 years, rising from
142 cases per million population in 1987 to 308 cases
per million population in the year 2000.9 Expansion of
Dr. Perazella and Dr. Reilly are Associate Professors of Medicine in the
the ESRD population will have a significant economic Section of Nephrology, Department of Medicine, Yale University School of
impact on the already overextended Medicare system. Medicine, New Haven, CT. Dr. Perazella also is a member of the
For example, Medicare expenditures for the ESRD pro- Hospital Physician Editorial Board.
18 Hospital Physician March 2003 www.turner-white.com
Perazella & Reilly : Classification of CKD : pp. 18 – 22, 45
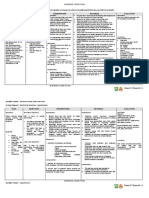
Table 1. Staging System and Action Plan for Chronic Kidney Disease
Stage Description GFR (mL/min per 1.73 m2) Action*
— At increased risk for CKD ≥ 90 with risk factors† Screening
CKD risk reduction
1 Kidney damage‡ with ≥ 90 Diagnosis and treatment
normal or increased GFR Slow progression of CKD
Treat comorbidities
Cardiovascular disease risk
reduction
2 Mild decrease in GFR 60–89 Estimate progression
3 Moderate decrease in GFR 30–59 Evaluate and treat complications
4 Severe decrease in GFR 15–29 Prepare for renal replacement
therapy
5 Kidney failure < 15 or dialysis Replacement if uremic
Adapted from National Kidney Foundation (NKF) Kidney Disease Outcome Quality Initiative (K/DOQI) Advisory Board. K/DOQI clinical practice
guidelines for chronic kidney disease: evaluation, classification, and stratification. Kidney Disease Outcome Quality Initiative. Am J Kidney Dis
2002;39(2 Suppl 2):S65. With permission from Elsevier Science.
CKD = chronic kidney disease; GFR = glomerular filtration rate.
*Includes actions from preceding stages.
†Risk factors: hypertension, dyslipidemia, diabetes mellitus, anemia, systemic lupus erythematosus, chronic analgesic ingestion.
‡Kidney damage as manifested by abnormalities noted on renal pathology, blood, urine, or imaging tests.
the term chronic kidney disease was chosen by the CKD GFR was subsequently developed by the CKD Work
Work Group. Group (Table 1).
The first order of business for the work group was to Defining CKD using this staging system provides a
define and classify CKD. The glomerular filtration rate common language for communication between the
(GFR) is the best overall measure of kidney function. various health care providers. The system will allow
Factors that influence GFR include both structural (or more reliable estimates of the prevalence of earlier
functional) kidney disease as well as patient age. In gen- stages and of populations at increased risk for CKD. In
eral, the annual decline of GFR with age is approxi- addition, evaluation of factors associated with a high
mately 1 mL/min per 1.73 m2 of body surface area, risk of progression can be recognized. Treatments can
beginning after the patient reaches approximately be more effectively examined and the development of
20 to 30 years of age.11 Although a chronic decline in adverse outcomes in this population can be more easily
GFR (a level of less than 60 mL/min per 1.73 m2 for determined. Finally, a classification and staging system
≥ 3 months) is evidence of CKD, substantial kidney also facilitates the application of clinical practice guide-
damage can exist without a decrease in GFR. In this lines, clinical performance measures and quality im-
circumstance, kidney damage is defined as a structural provement programs.
or functional abnormality of the kidney that can lead
to impaired kidney function that persists for 3 months ESTIMATION OF GFR AS AN INDEX OF KIDNEY
or more with or without a decreased GFR. Manifest- FUNCTION
ations of kidney damage can include pathologic abnor- Serum creatinine is the most commonly used bio-
malities noted on renal biopsy specimens or abnormali- chemical parameter for estimating GFR and as such has
ties revealed by blood, imaging, or urine tests. Utilizing been employed as an index of renal function. However,
this definition, CKD is present if the GFR is less than it is not an accurate measure of GFR, and it is especially
60 mL/min per 1.73 m2. In addition, CKD is present if inaccurate as an estimate of GFR when the serum creati-
the GFR is greater than or equal to 60 mL/min per nine level is between 1 and 2 mg/dL. This is because
1.73 m2 if other evidence of kidney damage also exists. creatinine, unlike inulin, is secreted by the renal tubules.
A classification and staging system based on the level of As renal function declines, the amount of creatinine
www.turner-white.com Hospital Physician March 2003 19
Perazella & Reilly : Classification of CKD : pp. 18 – 22, 45
secreted by the tubules increases and raises the amount The Cockcroft-Gault equation ([140 – age in years] ×
of creatinine in the urine (not filtered by the glomeru- weight in kg/[72 × serum creatinine], with the result for
lus). The ability of the renal tubule to secrete creatinine females multiplied by 0.85) was originally developed to
is maximal at a serum creatinine concentration of ap- estimate creatinine clearance.12 Although it provides an
proximately 2 mg/dL. This effect acts to falsely increase adequate estimate of GFR, the MDRD equations are
the creatinine clearance, resulting in an overestimation more accurate.13 MDRD equation 7 is the preferred for-
of GFR. The serum creatinine concentration is also mula, but it requires measurement of blood urea nitro-
affected by body mass, muscle mass, diet, drugs, and lab- gen (BUN) and serum albumin. The formula is (170 ×
oratory analytical methods. “Normal” ranges of serum [serum creatinine (mg/dL)]– 0.999 × [age (years)]– 0.176 ×
creatinine quoted by laboratories are particularly mis- [0.762 if female] × [1.18 if African American] × [BUN
leading because they do not take into account the age, (mg/dL)]–0.170 × [albumin (g/dL)]+0.318). An abbreviated
race, sex, or body size of the individual. As an example, form of the MDRD equation that does not require
consider the following patients, both of whom have BUN or albumin measurement was also developed and
a serum creatinine level of 1.3 mg/dL. “Patient A” is a is: (186 × [serum creatinine (mg/dL)]– 1.154 × [age
20-year-old, 80-kg man. “Patient B” is an 80-year-old, (years)]– 0.203 × [0.742 if female] × [1.21 if African
60-kg woman. Using the Cockcroft-Gault equation, pa- American]) and maintains reasonably good accuracy.
tient A’s GFR is estimated at 102 mL/min per 1.73 m2, Links to calculators for these equations can be found at
which is within the normal range, whereas patient B’s http://www.kidney.org/professionals/doqi/index.cfm.
GFR is estimated at 32 mL/min per 1.73 m2. Patient B’s The MDRD equation was tested in a large sample of
GFR is clearly reduced and suggests the presence of sig- patients (N = 558) with a range of kidney diseases
nificant CKD. Unfortunately, patients such as patient B and ethnicities (European Americans and African
are often thought of as having relatively normal kidney Americans).13 GFR values were validated in the sample
function and will receive medications that are not prop- group using urinary clearance of 125I-iothalamate as the
erly dosed for their levels of kidney function. In addi- gold standard. It is important to recognize that certain
tion, prophylaxis for exposure to nephrotoxins such as patient groups were not well represented in the MDRD
radiocontrast media may be overlooked because the study sample. Groups not evaluated include patients at
renal function is assumed to be normal. extremes of age and body size; the severely malnour-
Nephrologists have known for decades that inulin ished or obese; patients with skeletal muscle diseases,
clearance is the gold standard test for measuring GFR. paraplegia, or quadriplegia; vegetarians; those with
Unfortunately, this test is cumbersome and relatively rapidly changing kidney function; and patients prior to
expensive, and it is not widely available for clinical use. dosing drugs with significant toxicity that are excreted
Iothalamate (125I-iothalamate) clearance is used at some by the kidneys. Therefore, clearance measurements are
centers to estimate GFR and is a reasonably accurate still required in groups who were underrepresented in
substitute for the inulin clearance method. This method the MDRD sample to fully validate the formula for all
is also expensive and somewhat cumbersome to per- patients.
form as a routine clinical test. A 24-hour urine collec-
tion for creatinine clearance is the accepted alternative PREVALENCE OF CKD STAGES
measure of GFR because it is widely available and is a The next goal of the CKD Work Group was to obtain
test that is familiar to most clinicians. However, this test is prevalence estimates for each stage of CKD. Prevalence
often difficult for patients to carry out and perform cor- estimates were obtained by utilizing a reference group
rectly, and it is less accurate than either inulin or iothala- comprised of patients evaluated in the Third National
mate clearance. Health and Nutrition Examination Survey (NHANES
To simplify estimation of renal function in patients, III).8 Between 1988 and 1994, NHANES III enrolled
GFR estimates from prediction equations are utilized. 33,994 Americans aged 2 months and older. In this sam-
These formulas take into account serum creatinine level, ple of patients, the MDRD equation was used to estimate
age, gender, race, and body size, and they are better esti- GFR. In addition to abnormal GFR levels, the presence
mates of GFR than serum creatinine concentration of micro- or macroalbuminuria on spot urine specimens
alone. The formulas used are sufficiently accurate and, as was considered sufficient evidence of kidney damage.
a result, are recommended by most nephrologists. The The prevalence of each GFR category was subsequently
two most widely used are the Cockcroft-Gault and the determined (Table 2). The level of albuminuria was
Modification of Diet in Renal Disease Study (MDRD) used to estimate the prevalence of the first 2 stages. (The
equations. ratio of albumin [and protein] to creatinine in spot
20 Hospital Physician March 2003 www.turner-white.com
Perazella & Reilly : Classification of CKD : pp. 18 – 22, 45
urine samples has been documented to reliably corre- Table 2. US Prevalence of Chronic Kidney Disease by
late with 24-hour urine measurements for albumin and Stage
protein.14)
Stage 1 and 2 estimates are based on a single mea- Prevalence*
GFR (mL/min
surement of albuminuria. As one might suspect, over- Stage Description per 1.73 m2) N (1000s) %
estimation of prevalence for these stages may result
1 Kidney damage† ≥ 90 5900 3.3
from this approach—microalbuminuria was persistent
with normal
in only 61% of a subset of 1241 patients that were re- or increased
tested.8 However, this overestimation may be balanced GFR
by the exclusion of other patients with kidney disease
2 Mild decrease 60–89 5300 3.0
not manifested by albuminuria. For example, kidney in GFR
damage may also manifest as hematuria, pyuria, or ab-
3 Moderate 30–59 7600 4.3
normal imaging tests. These important kidney param-
decrease in
eters were not evaluated in the NHANES III popula- GFR
tion.
4 Severe decrease 15–29 400 0.2
A staging system based on severity of disease is justi-
in GFR
fied from several perspectives. Adverse outcomes of
CKD are directly related to the prevailing level of kid- 5 Kidney failure < 15 or dialysis 300 0.1
ney function. Furthermore, CKD tends to worsen over Adapted from National Kidney Foundation (NKF) Kidney Disease
time, and the risk for adverse outcomes increases over Outcome Quality Initiative (K/DOQI) Advisory Board. K/DOQI clin-
time with disease severity. In addition, it is well docu- ical practice guidelines for chronic kidney disease: evaluation, classifi-
mented that as GFR declines, the prevalence of hyper- cation, and stratification. Kidney Disease Outcome Quality Initiative.
Am J Kidney Dis 2002;39(2 Suppl 2):S50. With permission from
tension, anemia, elevated parathyroid hormone level,
Elsevier Science.
hyperphosphatemia, hypocalcemia, and hypoalbumine-
mia increases.15,16 GFR = glomerular filtration rate.
*Prevalence based on population of 177 million adults age ≥ 20 years.
APPROACH TO PATIENTS WITH CKD
† Kidney damage as manifested by abnormalities noted on renal
The approach to the patient involves establishing the pathology, blood, urine, or imaging tests.
presence of CKD, determining the stage of disease, and
enacting an action plan based on the stage. The man-
agement of CKD patients requires a multidisciplinary albumin-to-creatinine ratios in spot urine samples to
approach involving primary care physicians, nephrolo- assess for kidney damage, and urinalysis. Finally, imag-
gists, endocrinologists, cardiologists, vascular surgeons, ing of the kidney by ultrasonography is warranted in
physician assistants, nurse practitioners, dietitians, and most CKD patients.
social workers. The goals of this interdisciplinary ap- The approach is implemented in a step-wise fashion
proach are to identify patients either with or at in- and will vary for the individual patient based on the
creased risk for CKD, to slow the progression of CKD to severity of the impairment of the GFR. In a patient with a
ESRD, to identify and treat comorbid conditions, to normal GFR (≥ 90 mL/min per 1.73 m2) or a mildly
identify and prevent complications of CKD, and to pre- impaired GFR (> 60 mL/min per 1.73 m2) the focus will
pare patients mentally and physically for renal replace- be on delaying progression and treating comorbid condi-
ment therapy. As seen in Table 1, the action taken in- tions. Progression is best predicted by plotting the recip-
creases from simple screening maneuvers and risk rocal of the serum creatinine level over time. The Walter
reduction to more complex disease management. Reed Army Medical Center Section of Nephrology Web
The initial evaluation of patients with established site is an excellent resource for this purpose (http://
CKD should include an assessment of comorbid condi- www.wramc.amedd.army.mil/departments/medicine/
tions and a thorough review of medications. Med- nephrology/tools/index.html). This plot will predict a
ications should be adjusted for the level of renal func- date when the GFR will reach target levels that are
tion. Blood pressure monitoring is essential to diagnose approved by the Center for Medicare and Medicaid
hypertension and facilitate optimal blood pressure con- Services for the initiation of renal replacement therapy.
trol to reduce ongoing kidney damage. Laboratory tests In general, the cut-off values are 15 mL/min per 1.73 m2
that should be performed include serum creatinine for diabetic patients and 10 mL/min per 1.73 m2 for
concentration to allow estimation of GFR, protein- or nondiabetic patients.
www.turner-white.com Hospital Physician March 2003 21
Perazella & Reilly : Classification of CKD : pp. 18 – 22, 45
In the past decade, several treatments have been into stages according to estimated GFR and the pres-
shown to slow the progression of CKD. In diabetic ence or absence of kidney damage and proposes a stage-
patients these include tight glucose control and nor- based clinical action plan. The complete K/DOQI
malization of blood pressure.5,6 Strict blood pressure Clinical Practice Guidelines for Chronic Kidney Disease:
control (< 125/75 mm Hg) in diabetic patients and in Evaluation, Classification, and Stratification can be
nondiabetic patients with proteinuria is associated with found at the Web site address http://www.kidney.org/
a slower rate of decline of GFR.16 – 18 ACE inhibitors and professionals/doqi/kdoqi/toc.htm. In addition, a CKD
angiotensin-receptor blockers may slow progression by Web site for primary care practitioners was developed by
mechanisms other than blood pressure lowering.19,20 the Yale University Nephrology Section and can be
Other potentially important therapies include dietary found at http://kidney.med.yale.edu.ckd.
protein restriction, lipid control with statins, smoking The next article in this series will review available
cessation, and correction of anemia. These aspects will interventions for slowing the progression of CKD. Future
be discussed more fully in a future article addressing articles will address anemia and mineral metabolism dis-
the therapies employed to reduce progression of CKD. turbances associated with CKD, cardiovascular disease in
In patients with moderate impairment (GFR of patients with CKD, and the preparation of patients for
30–60 mL/min per 1.73 m2), a search for uremic com- renal replacement therapy. HP
plications (eg, anemia, abnormalities in mineral met-
abolism) should be undertaken. In addition, treatment REFERENCES
of these processes should be initiated. In contrast, the 1. Obrador GT, Ruthazer R, Arora P, et al. Prevalence of
focus of care for patients with severe impairment (GFR and factors associated with suboptimal care before initia-
of 15–30 mL/min per 1.73 m2) should be on appropri- tion of dialysis in the United States. J Am Soc Nephrol
ate preparation for renal replacement therapy. Elec- 1999;10:1793–800.
2. Kausz AT, Khan SS, Abichandani R, et al. Management of
trolyte and acid-base disturbances such as hyperkalemia
patients with chronic renal insufficiency in the North-
and metabolic acidosis need to be monitored and treat- eastern United States. J Am Soc Nephrol 2001;12:1501–7.
ed aggressively. Nutritional state should be assessed and 3. Duncan L, Heathcote J, Djurdjev O, Levin A. Screening
dietary counseling undertaken to optimize protein for renal disease using serum creatinine: who are we
intake without inducing hyperphosphatemia, hyper- missing? Nephrol Dial Transplant 2001;16:1042–6.
kalemia, or metabolic acidosis. Also, correction of ane- 4. Nissenson AR, Collins AJ, Hurley J, et al. Opportunities
mia and mineral metabolism disturbances should con- for improving the care of patients with chronic renal in-
tinue during this late stage. sufficiency: current practice patterns. J Am Soc Nephrol
In addition to those patients who already have CKD, 2001;12:1713–20.
there is an even larger group of patients who are at risk 5. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect
for the development of CKD. This group includes pa- of angiotensin-converting-enzyme inhibition on diabet-
ic nephropathy. The Collaborative Study Group [pub-
tients with diabetes mellitus, hypertension, and systemic
lished erratum appears in N Engl J Med 1993;330:152].
lupus erythematosus, as well as chronic analgesic drug N Engl J Med 1993;329:1456–62.
users. In addition, African Americans appear to be at 6. The effect of intensive treatment of diabetes on the devel-
higher risk for kidney damage than other racial groups. opment and progression of long-term complications in
As part of the initial evaluation of high-risk patients, the insulin-dependent diabetes mellitus. The Diabetes
CKD Work Group advised measurement of blood pres- Control and Complications Trial Research Group. N Engl
sure, serum creatinine level (to estimate GFR), and J Med 1993;329:977–86.
protein- or albumin-to-creatinine ratio in a spot urine 7. Giatras I, Lau J, Levey AS. Effect of angiotensin-converting
specimen to assess for kidney damage. Other selected enzyme inhibitors on the progression of nondiabetic renal
tests, such as renal ultrasonography, computed tomog- disease: a meta-analysis of randomized trials. Angiotensin-
raphy or magnetic resonance imaging of the kidneys, Converting-Enzyme Inhibition and Progressive Renal
Disease Study Group. Ann Intern Med 1997;127:337–45.
serum electrolyte levels, and urinalysis may be indicated
8. National Kidney Foundation (NKF) Kidney Disease
in specific clinical situations. Outcome Quality Initiative (K/DOQI) Advisory Board.
K/DOQI clinical practice guidelines for chronic kidney
CONCLUSION
disease: evaluation, classification, and stratification.
The rising incidence and prevalence of CKD in the Kidney Disease Outcome Quality Initiative. Am J Kidney
United States has mandated a unified approach to its Dis 2002;39(2 Suppl 2):S1–246.
evaluation and classification. The approach put forth by 9. US Renal Data System. USRDS 2001 annual data report.
the NKF’s CKD Work Group stratifies patients with CKD Bethesda (MD): National Institutes of Health, National
(continued on page 45)
22 Hospital Physician March 2003 www.turner-white.com
Perazella & Reilly : Classification of CKD : pp. 18 – 22, 45
(from page 22)
Institute of Diabetes and Digestive and Kidney Diseases; 16. Buckalew VM Jr, Berg RL, Wang SR, et al. Prevalence of
2001. Also available at http://www.usrds.org/adr_2001. hypertension in 1,795 subjects with chronic renal dis-
htm. Accessed 4 Feb 2003. ease: the modification of diet in renal disease study base-
10. Healthy people 2010: chronic kidney disease. Bethesda line cohort. Modification of Diet in Renal Disease Study
(MD): National Institutes of Health, National Institute Group. Am J Kidney Dis 1996;28:811–21.
of Diabetes and Digestive and Kidney Diseases; 2000. 17. Lazarus JM, Bourgoignie JJ, Buckalew VM, et al.
11. Davies DF, Shock NW. Age changes in glomerular filtra- Achievement and safety of a low blood pressure goal in
tion rate, effective renal plasma flow, and tubular excretory chronic renal disease. The Modification of Diet in Renal
capacity in adult males. J Clin Invest 1950;29:496–507. Disease Study Group. Hypertension 1997;29:641–50.
12. Cockcroft DW, Gault MH. Prediction of creatinine clear- 18. Brenner BM, Cooper ME, de Zeeuw D, et al. RENAAL
ance from serum creatinine. Nephron 1976;16:31–41. Study Investigators. Effects of losartan on renal and car-
13. Levey AS, Bosch JP, Lewis JB, et al. A more accurate diovascular outcomes in patients with type 2 diabetes
method to estimate glomerular filtration rate from and nephropathy. N Engl J Med 2001;345:861–9.
serum creatinine: a new prediction equation. Modifica- 19. Lewis EJ, Hunsicker LG, Clarke WR, et al. Collaborative
tion of Diet in Renal Disease Study Group. Ann Intern Study Group. Renoprotective effect of the angiotensin-
Med 1999;130:461–70. receptor antagonist irbesartan in patients with nephropa-
14. Ginsberg JM, Chang BS, Matarese RA, Garella S. Use of thy due to type 2 diabetes. N Engl J Med 2001;345:851–60.
single voided urine samples to estimate quantitative pro- 20. Ravid M, Savin H, Jutrin I, et al. Long-term stabilizing
teinuria. N Engl J Med 1983;309:1543–6. effect of angiotensin-converting enzyme inhibition on
15. Hsu CY, Bates DW, Kuperman GJ, Curhan GC. Re- plasma creatinine and on proteinuria in normotensive
lationship between hematocrit and renal function in type II diabetic patients. Ann Intern Med 1993;118:
men and women. Kidney Int 2001;59:725–31. 577–81.
Copyright 2003 by Turner White Communications Inc., Wayne, PA. All rights reserved.
www.turner-white.com Hospital Physician March 2003 45
Das könnte Ihnen auch gefallen
- Acute Kidney Injury W/ Hyperkalemia NCPDokument5 SeitenAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNoch keine Bewertungen
- Understanding Chronic Kidney Disease: A guide for the non-specialistVon EverandUnderstanding Chronic Kidney Disease: A guide for the non-specialistBewertung: 4 von 5 Sternen4/5 (3)
- Hangnails and HomoeopathyDokument7 SeitenHangnails and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNoch keine Bewertungen
- Detailed Lesson Plan Respiratory SystemDokument7 SeitenDetailed Lesson Plan Respiratory Systemjane89% (9)
- Chronic Kidney DiseaseDokument11 SeitenChronic Kidney Diseasenaly23Noch keine Bewertungen
- Chronic Kidney Disease Progression Modifying TherapiesDokument29 SeitenChronic Kidney Disease Progression Modifying Therapiesdfsdsfsd100% (1)
- Castle Connolly Graduate Board Review SeriesDokument31 SeitenCastle Connolly Graduate Board Review SeriesCCGMPNoch keine Bewertungen
- Early Chronic Kidney DiseaseDokument12 SeitenEarly Chronic Kidney DiseaseDirga Rasyidin L100% (1)
- Fish & Shellfish PoisoningDokument29 SeitenFish & Shellfish Poisoningkolita kamal100% (4)
- Alzheimer's DiseaseDokument469 SeitenAlzheimer's DiseaseGastón G. Fernández100% (3)
- Drug Overdose: Dr. Diah Ari Safitri, SPPDDokument9 SeitenDrug Overdose: Dr. Diah Ari Safitri, SPPDmkafabillahNoch keine Bewertungen
- Chronickidneydisease: Cornelia Charles,, Allison H. FerrisDokument11 SeitenChronickidneydisease: Cornelia Charles,, Allison H. FerrisDiahNoch keine Bewertungen
- HP Mar03 ChronicDokument6 SeitenHP Mar03 ChronicAnonymous MJkYnuNoch keine Bewertungen
- Reviews: Early Detection of CKD: The Benefits, Limitations and Effects On PrognosisDokument12 SeitenReviews: Early Detection of CKD: The Benefits, Limitations and Effects On Prognosisanderson roberto oliveira de sousaNoch keine Bewertungen
- Executive Summaries of 2000 Updates Anemia Hemodialysis Peritoneal Dialysis Vascular Access Nutrition Chronic Kidney Disease History of DOQIDokument11 SeitenExecutive Summaries of 2000 Updates Anemia Hemodialysis Peritoneal Dialysis Vascular Access Nutrition Chronic Kidney Disease History of DOQIAndrie WigunaNoch keine Bewertungen
- Anemia: Chronic Kidney DiseaseDokument12 SeitenAnemia: Chronic Kidney DiseasetyasNoch keine Bewertungen
- Medifocus Dec 2012Dokument67 SeitenMedifocus Dec 2012Pushpanjali Crosslay HospitalNoch keine Bewertungen
- Chronic Kidney Disease20190605 98952 Kssgx8 With Cover Page v2Dokument16 SeitenChronic Kidney Disease20190605 98952 Kssgx8 With Cover Page v2Melly SyafridaNoch keine Bewertungen
- Epidemiology and Causes of Chronic Kidney Disease: What's New?Dokument4 SeitenEpidemiology and Causes of Chronic Kidney Disease: What's New?Ika auliaNoch keine Bewertungen
- Epidemiology of Chronic Kidney Disease Among Older Adults: A Focus On The Oldest OldDokument8 SeitenEpidemiology of Chronic Kidney Disease Among Older Adults: A Focus On The Oldest Oldkhangha.ptNoch keine Bewertungen
- 2017 Chronic Kidney DiseaseDokument9 Seiten2017 Chronic Kidney DiseaseGenoMacaraanNoch keine Bewertungen
- PCP in A Box - Module 1Dokument43 SeitenPCP in A Box - Module 1Fate ChanNoch keine Bewertungen
- Introduction The Case For Updating and Co - 2013 - Kidney International SupplemDokument4 SeitenIntroduction The Case For Updating and Co - 2013 - Kidney International SupplemwardaninurindahNoch keine Bewertungen
- Conservative Management of Chronic Renal Failure: Contemporary IssueDokument6 SeitenConservative Management of Chronic Renal Failure: Contemporary IssueInes TerraheNoch keine Bewertungen
- Chronic Kidney Disease:: The Canary in The Coal MineDokument13 SeitenChronic Kidney Disease:: The Canary in The Coal MinedhearawrsNoch keine Bewertungen
- Non-Steroidal Mra DKD PotassiumDokument10 SeitenNon-Steroidal Mra DKD Potassiumlakshminivas PingaliNoch keine Bewertungen
- Chronic Kidney Disease in Adults - Assessment and ManagementDokument5 SeitenChronic Kidney Disease in Adults - Assessment and ManagementAnahí Cortés HerreraNoch keine Bewertungen
- Chronic Kidney Disease: SeminarDokument16 SeitenChronic Kidney Disease: SeminarMichael Meng100% (1)
- Epidemiology of Chronic Kidney Disease An U - 2022 - Kidney International SupplDokument5 SeitenEpidemiology of Chronic Kidney Disease An U - 2022 - Kidney International SupplSol anonimoNoch keine Bewertungen
- A Role For SGLT 2 Inhibitors in Treating Non Diabetic Chronic Kidney DiseaseDokument21 SeitenA Role For SGLT 2 Inhibitors in Treating Non Diabetic Chronic Kidney DiseaseCarlos Martinez SalgadoNoch keine Bewertungen
- Approach To The Detection and Management of Chronic Kidney DiseaseDokument8 SeitenApproach To The Detection and Management of Chronic Kidney Diseaseapi-301730880Noch keine Bewertungen
- Kulit 5Dokument1 SeiteKulit 5Anonymous 12QYPATm3Noch keine Bewertungen
- Pharmacotherapy in Chronic Kidney Disease Patients Presenting With Acute Coronary SyndromeDokument27 SeitenPharmacotherapy in Chronic Kidney Disease Patients Presenting With Acute Coronary SyndromeaudiNoch keine Bewertungen
- Clinical Practice Guidelines On Hypertension and Antihypertensive Agents in Chronic Kidney Disease (CKD)Dokument9 SeitenClinical Practice Guidelines On Hypertension and Antihypertensive Agents in Chronic Kidney Disease (CKD)Dewi Sekar AyuNoch keine Bewertungen
- Seminar: Angela C Webster, Evi V Nagler, Rachael L Morton, Philip MassonDokument15 SeitenSeminar: Angela C Webster, Evi V Nagler, Rachael L Morton, Philip MassonMaría José GalvisNoch keine Bewertungen
- FDA Approval of Dapagliflozin For Chronic Kidney Disease A Rem - 2021 - The LanDokument2 SeitenFDA Approval of Dapagliflozin For Chronic Kidney Disease A Rem - 2021 - The LanAvril JatariuNoch keine Bewertungen
- Pathophysiology and Classification of Kidney DiseasesDokument10 SeitenPathophysiology and Classification of Kidney DiseasesmedicalNoch keine Bewertungen
- GFR and Albuminuria Level in Acute and Chronic Kidney DiseaseDokument9 SeitenGFR and Albuminuria Level in Acute and Chronic Kidney DiseaseLoreto FernandezNoch keine Bewertungen
- Therapeutic Insights in Chronic Kidney Disease Progression: Amir Shabaka, Clara Cases-Corona and Gema Fernandez-JuarezDokument12 SeitenTherapeutic Insights in Chronic Kidney Disease Progression: Amir Shabaka, Clara Cases-Corona and Gema Fernandez-Juarezkomputer12Noch keine Bewertungen
- Review Article: Inflammatory Factors and Exercise in Chronic Kidney DiseaseDokument13 SeitenReview Article: Inflammatory Factors and Exercise in Chronic Kidney Diseaseadri20121989Noch keine Bewertungen
- Att CKD Oct04Dokument24 SeitenAtt CKD Oct04A9 El-EbidiNoch keine Bewertungen
- 2022 NEJM Uses of GFR and Albuminuria LevelDokument9 Seiten2022 NEJM Uses of GFR and Albuminuria LevelPeter Albeiro Falla CortesNoch keine Bewertungen
- CKD in Adults - UpToDateDokument54 SeitenCKD in Adults - UpToDateNada AhmedNoch keine Bewertungen
- Chronic Kidney Disease: Identification and Management in Primary CareDokument12 SeitenChronic Kidney Disease: Identification and Management in Primary CareLiri AndiyaniNoch keine Bewertungen
- Diabetic Kidney Disease ManagementDokument16 SeitenDiabetic Kidney Disease Managementcecilia zavalaNoch keine Bewertungen
- ERC E HTADokument10 SeitenERC E HTAmiguelalmenarezNoch keine Bewertungen
- Gfad 118Dokument10 SeitenGfad 118pepegiovannyNoch keine Bewertungen
- Insuficiencia Renal CronicaDokument13 SeitenInsuficiencia Renal CronicaCarlos DNoch keine Bewertungen
- BMJ 2022 074216.fullDokument20 SeitenBMJ 2022 074216.fullArmando OrtegaNoch keine Bewertungen
- Definition and Classification of Kidney Diseases: EditorialDokument3 SeitenDefinition and Classification of Kidney Diseases: EditorialdianaNoch keine Bewertungen
- CKD PresentationDokument83 SeitenCKD PresentationMoh'md NuohNoch keine Bewertungen
- Drugs To Use in CKDDokument8 SeitenDrugs To Use in CKDMANOJTHUTHIJANoch keine Bewertungen
- Chronic Kidney Disease: Rizki Aliana AgustinaDokument85 SeitenChronic Kidney Disease: Rizki Aliana AgustinaRofi IrmanNoch keine Bewertungen
- Gfi 163Dokument5 SeitenGfi 163trinda ireneNoch keine Bewertungen
- Renin-Angiotensin System Inhibition in Advanced CKDDokument35 SeitenRenin-Angiotensin System Inhibition in Advanced CKDbokobokobokanNoch keine Bewertungen
- CCR 15 55 (Recovered 1)Dokument9 SeitenCCR 15 55 (Recovered 1)Raka Petra PrazastaNoch keine Bewertungen
- ChenDokument32 SeitenChenMonikaNoch keine Bewertungen
- p4 Class g1.htmDokument14 Seitenp4 Class g1.htmIrara RaNoch keine Bewertungen
- s41581-024-00827-zDokument14 Seitens41581-024-00827-zBruno MañonNoch keine Bewertungen
- Biomarkers of Diabetic Kidney DiseaseDokument16 SeitenBiomarkers of Diabetic Kidney DiseaseAmelia Fitria DewiNoch keine Bewertungen
- Nej MR A 2201153Dokument9 SeitenNej MR A 2201153LETICIA CRISTINO FRANCISCONoch keine Bewertungen
- Pages From June04 Ch2Dokument12 SeitenPages From June04 Ch2junebabeNoch keine Bewertungen
- Practical Approach to CKD in Primary CareDokument10 SeitenPractical Approach to CKD in Primary CareJovieth Trejos MedranoNoch keine Bewertungen
- Mayoclinproc 84 2 012 PDFDokument7 SeitenMayoclinproc 84 2 012 PDFVinceErwinTanNoch keine Bewertungen
- Effects of Statins On Renal FunctionDokument10 SeitenEffects of Statins On Renal Functionangela gagariNoch keine Bewertungen
- Harrisons Principles of Internal Medicine Vol.1 Vol.2 20th Edition2018 Original PDF 3 157 167Dokument11 SeitenHarrisons Principles of Internal Medicine Vol.1 Vol.2 20th Edition2018 Original PDF 3 157 167William MilesNoch keine Bewertungen
- Pathophysiology and Classification of Kidney DiseasesDokument10 SeitenPathophysiology and Classification of Kidney DiseasesmedicalNoch keine Bewertungen
- Food PoisoningDokument12 SeitenFood PoisoningmkafabillahNoch keine Bewertungen
- Medscape Acute Appendicitis PDFDokument5 SeitenMedscape Acute Appendicitis PDFraffellaNoch keine Bewertungen
- G.I. Bleeding: Dr. Diah Ari Safitri, SPPDDokument15 SeitenG.I. Bleeding: Dr. Diah Ari Safitri, SPPDmkafabillahNoch keine Bewertungen
- Alvarado PDFDokument4 SeitenAlvarado PDFGabriel MartinezNoch keine Bewertungen
- G.I. Bleeding: Dr. Diah Ari Safitri, SPPDDokument15 SeitenG.I. Bleeding: Dr. Diah Ari Safitri, SPPDmkafabillahNoch keine Bewertungen
- Mo Uzaki 2015Dokument6 SeitenMo Uzaki 2015mkafabillahNoch keine Bewertungen
- KolestasisDokument8 SeitenKolestasisNur Ainatun NadrahNoch keine Bewertungen
- NIH Public Access: Neonatal CholestasisDokument21 SeitenNIH Public Access: Neonatal CholestasismkafabillahNoch keine Bewertungen
- CHT WFLH Girls Z 0 5 PDFDokument1 SeiteCHT WFLH Girls Z 0 5 PDFmkafabillahNoch keine Bewertungen
- Abu Dhabi DRGDokument62 SeitenAbu Dhabi DRGDolly creationsNoch keine Bewertungen
- NCM101 Health Assessment ExaminationDokument11 SeitenNCM101 Health Assessment ExaminationJonah R. Merano100% (1)
- 020 - Metabolism of Proteins 3Dokument12 Seiten020 - Metabolism of Proteins 3Sargonan RaviNoch keine Bewertungen
- Ligibel JA Et Al. 2022 Exercise, Diet and Weight Management During Cancer Treatment - ASCO GuidelineDokument20 SeitenLigibel JA Et Al. 2022 Exercise, Diet and Weight Management During Cancer Treatment - ASCO GuidelineJasmyn KimNoch keine Bewertungen
- PrimaquineDokument3 SeitenPrimaquineVijayakumar NsNoch keine Bewertungen
- 13 - Adverse Drug Reactions CausesDokument4 Seiten13 - Adverse Drug Reactions CausesRojas Evert AlonsoNoch keine Bewertungen
- Transverse Dimension Diagnosis and Relevance to Functional OcclusionDokument6 SeitenTransverse Dimension Diagnosis and Relevance to Functional OcclusionDino MainoNoch keine Bewertungen
- Necrotizing Soft Tissue Infections GuideDokument21 SeitenNecrotizing Soft Tissue Infections GuideHen RyNoch keine Bewertungen
- Anterior Segment OctDokument53 SeitenAnterior Segment OctA.c. RaghuNoch keine Bewertungen
- MGM Muthoot Medical Centre Patient Transfer CriteriaDokument2 SeitenMGM Muthoot Medical Centre Patient Transfer CriteriaDr Jisha TuNoch keine Bewertungen
- HEPATITIS B VACCINE NURSING RESPONSIBILITIESDokument14 SeitenHEPATITIS B VACCINE NURSING RESPONSIBILITIESJannine BensiNoch keine Bewertungen
- Community Health and Program Services (CHAPS) : Health Disparities Among Racial/Ethnic PopulationsDokument4 SeitenCommunity Health and Program Services (CHAPS) : Health Disparities Among Racial/Ethnic PopulationsMuhammad Bachiar SafrudinNoch keine Bewertungen
- Cervical Lymphoepithelial CystDokument6 SeitenCervical Lymphoepithelial CystAhmed Al-jumailiNoch keine Bewertungen
- Complications of 3rd TrimesterDokument49 SeitenComplications of 3rd TrimesterMA. JYRELL BONITONoch keine Bewertungen
- Femur and Pelvis Fracture (Trauma)Dokument20 SeitenFemur and Pelvis Fracture (Trauma)Ree YahNoch keine Bewertungen
- Askep CKD Bhs InggrisDokument15 SeitenAskep CKD Bhs InggrisFitri MulyaNoch keine Bewertungen
- Int Obs PDFDokument37 SeitenInt Obs PDFsurgeon77Noch keine Bewertungen
- Bronchopulmonary Dysplasia (BPD)Dokument13 SeitenBronchopulmonary Dysplasia (BPD)Joan BuiNoch keine Bewertungen
- Diet PlanDokument6 SeitenDiet Plantrical27 tricalNoch keine Bewertungen
- 5a.ESOPHAGEAL DISORDERSDokument16 Seiten5a.ESOPHAGEAL DISORDERSHayat AL AKOUMNoch keine Bewertungen
- National Institute of Occupational Safety and Health Course CurriculumDokument9 SeitenNational Institute of Occupational Safety and Health Course Curriculummohan dassNoch keine Bewertungen
- Past PapaersDokument515 SeitenPast PapaersShariq ShaNoch keine Bewertungen
- OSCE Chart Cough (KK)Dokument4 SeitenOSCE Chart Cough (KK)api-26938624Noch keine Bewertungen
- GetPdf Cgi PDFDokument9 SeitenGetPdf Cgi PDFAKNTAI002Noch keine Bewertungen
- Dental CatalogueDokument28 SeitenDental CataloguePaulus LagadanNoch keine Bewertungen