Beruflich Dokumente
Kultur Dokumente
Diarrhea Care Plan
Hochgeladen von
zepoli_zepoly6232Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diarrhea Care Plan
Hochgeladen von
zepoli_zepoly6232Copyright:
Verfügbare Formate
Iris Lopez
Dates of care:9/1-9/2/2010
Medical diagnosis: Ulcerative colitis
Ulcerative colitis (UC): A chronic condition of unknown cause usually starting in the rectum and
distal portions of the colon and possibly spreading upward to involve the sigmoid and descending colon
or the entire colon. It is usually intermittent (acute exacerbation with long remissions), but some
individuals (30%–40%) have continuous symptoms. Cure is effected only by total removal of colon
and rectum/rectal mucosa.
Diagnostic studies:
Stool specimens (examinations are used in initial diagnosis and in following disease progression): Mainly
composed of mucus, blood, pus, and intestinal organisms, especially Entamoeba histolytica (active stage). Fecal
leukocytes and RBCs indicate inflammation of GI tract. Stool positive for bacterial pathogens, ova and parasites or
clostridium indicates infections. Stool positive for fat indicates malabsorption.
Proctosigmoidoscopy: Visualizes ulcerations, edema, hyperemia, and inflammation (result of secondary infection of
the mucosa and submucosa). Friability and hemorrhagic areas caused by necrosis and ulceration occur in 85% of these
patients.
Cytology and rectal biopsy: Differentiates between infectious process and carcinoma (occurs 10–20 times more
often than in general population). Neoplastic changes can be detected, as well as characteristic inflammatory
infiltrates called crypt abscesses.
Barium enema: May be performed after visual examination has been done, although rarely done during acute,
relapsing stage, because it can exacerbate condition.
Endoscopic examinations, e.g., sigmoidoscopy, esophagogastroduodenoscopy, or colonoscopy: Identifies
adhesions, changes in luminal wall (narrowing/irregularity); rules out bowel obstruction and allowed biopsy for
features of Crohn’s disease or ulcerative colitis.
Abdominal magnetic resonance imaging (MRI)/computed tomography (CT) scan, ultrasound: Detects
abscesses, masses, strictures, or fistulas.
CBC: May show hyperchromic anemia (active disease generally present because of blood loss and iron deficiency);
leukocytosis may occur, especially in fulminating or complicated cases and in patients on steroid therapy.
Erythrocyte sedimentation rate (ESR): Elevated in acute inflammation according to severity of disease.
Serum iron levels: Lowered because of blood loss or poor dietary intake.
PT: Prolonged in severe cases from altered factors VII and X caused by vitamin K deficiency.
Thrombocytosis: May occur as a result of inflammatory disease process.
Electrolytes: Decreased potassium, magnesium, and zinc are common in severe disease.
Prealbumin/albumin level: Decreased because of loss of plasma proteins/disturbed liver function, decreased dietary
intake.
Alkaline phosphatase: Increased, along with serum cholesterol and hypoproteinemia, indicating disturbed liver
function (e.g., cholangitis, cirrhosis).
Disease-specific antibodies, ANCA (antineutrophil cyctoplasmic antibodies): Positive result increases suspicion of
UC, but negative result does not rule out diagnosis.
Bone marrow: A generalized depression is common in fulminating types/after a long inflammatory process.
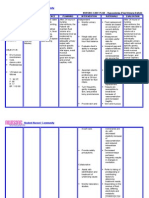
NURSING DIAGNOSIS: Diarrhea
Related to: Inflammation, irritation, or malabsorption of the bowel
Evidenced by: Increased bowel sounds/peristalsis, frequent, and often severe, watery stools (acute phase), changes
in stool color, abdominal pain; urgency (sudden painful need to defecate), cramping
ACTIONS/INTERVENTIONS RATIONALE
Observe and record stool frequency, characteristics, amount, Helps differentiate individual disease and assesses severity
and precipitating factors. of episode.
Remove stool promptly. Provide room deodorizers. Reduces noxious odors to avoid undue patient
embarrassment.
Identify foods and fluids that precipitate diarrhea, e.g., raw Avoiding intestinal irritants promotes intestinal rest
vegetables and fruits, whole-grain cereals, condiments,
carbonated drinks, milk products.
Observe for fever, tachycardia, lethargy, leukocytosis, May signify that toxic megacolon or perforation and
decreased serum protein, anxiety, and prostration peritonitis are imminent/have occurred, necessitating
immediate medical intervention.
Administer medications as indicated: Decreases GI motility/propulsion (peristalsis) and
Antidiarrheals, e.g., diphenoxylate (Lomotil), loperamide diminishes digestive secretions to relieve cramping and
(Imodium), anodyne suppositories; diarrhea. Note: Use with caution in UC because they may
precipitate toxic megacolon.
Administer medications as indicated: Useful in treating mild/moderate exacerbations because of
Anti-inflammatories, e.g.; 5-aminosalicylic acid (5-ASA), both anti-inflammatory and antimicrobial properties. Long-
sulfasalazine (Azulfidine), mesalamine (Pentasa, Asacol, term use may prolong remission. Note: Available in
Rowasa), olsalazine (Dipentum); oral/time-release and pH-dependent forms. Rowasa may be
given as an enema in lieu of sulfasalazine (Azulfidine) for
patients who are sensitive to oral sulfa drugs.
Promote bedrest, provide bedside commode. Rest decreases intestinal motility and reduces the metabolic
rate when infection or hemorrhage is a complication. Urge
to defecate may occur without warning and be
uncontrollable, increasing risk of incontinence/falls if
facilities are not close at hand.
DESIRED OUTCOMES—PATIENT WILL: EVALUATION CRITERIA
Report reduction in frequency of stools, return to more Ineffective: Client was not able to report a reduction in
normal stool consistency. frequency of watery stools
Effective: Client was able to verbalize the consistency of
Identify/avoid contributing factors and observe stool
the stools and foods that might cause/exacerbate abdominal
frequency, characteristics, amount
cramping, flatulence (e.g. alcohol, caffeinated beverages,
chocolate, peppermint, tomatoes, orange juice).
Reference: Nursing Diagnosis Reference Manual, 5th edition, An indispensable guide to better patient
care, Sheila M. Sparks, RN, DNSc, CS and Cynthia M. Taylor, RN, MS, CNAA
Das könnte Ihnen auch gefallen
- NCPsDokument13 SeitenNCPsRocel DevillesNoch keine Bewertungen
- NCP Making (Ulcerative Colitis & Crohn's Disease)Dokument2 SeitenNCP Making (Ulcerative Colitis & Crohn's Disease)R Hornilla ArcegaNoch keine Bewertungen
- Deficit)Dokument2 SeitenDeficit)Lee DeeNoch keine Bewertungen
- Assessment Healt H Patte RN Nursing Diagnosis Desired Outcome (Edit) Intervention (Edit) Evaluation (EDIT) Rema RKSDokument3 SeitenAssessment Healt H Patte RN Nursing Diagnosis Desired Outcome (Edit) Intervention (Edit) Evaluation (EDIT) Rema RKStflorenzNoch keine Bewertungen
- Compartment Syndrome NCP (PAIN)Dokument2 SeitenCompartment Syndrome NCP (PAIN)eunica16Noch keine Bewertungen
- Aiza NCPDokument6 SeitenAiza NCPponponolmedoNoch keine Bewertungen
- COLCHICINE pptx1800128929Dokument15 SeitenCOLCHICINE pptx1800128929April Mergelle LapuzNoch keine Bewertungen
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDokument4 SeitenCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- NCP 3Dokument2 SeitenNCP 3Richson Bacay100% (1)
- Cues Nursing DX Objectives Nursing Interventions RationaleDokument5 SeitenCues Nursing DX Objectives Nursing Interventions RationaleJamie IcabandiNoch keine Bewertungen
- Acc Phu Case NCP HyperthermiaDokument1 SeiteAcc Phu Case NCP Hyperthermiamacy_bautistaNoch keine Bewertungen
- NCP UreteroDokument1 SeiteNCP UreteroCerie Anne OlayNoch keine Bewertungen
- NCP Gastric CancerDokument6 SeitenNCP Gastric Cancerhayascent hilarioNoch keine Bewertungen
- Acute Pain NCPDokument1 SeiteAcute Pain NCPJed AvesNoch keine Bewertungen
- Child - Major Burn PDFDokument3 SeitenChild - Major Burn PDFAldith GrahamNoch keine Bewertungen
- NCP-fluid Volume DeficitDokument4 SeitenNCP-fluid Volume DeficitChrissa Mae Aranilla MayoNoch keine Bewertungen
- Postpartal Thrombophlebitis: Client Assessment Data Base Activity/RestDokument8 SeitenPostpartal Thrombophlebitis: Client Assessment Data Base Activity/RestLei OrtegaNoch keine Bewertungen
- Assessment Explanation of The Problem Planning Nursing Intervention Rationale EvaluationDokument2 SeitenAssessment Explanation of The Problem Planning Nursing Intervention Rationale EvaluationRodolfo Bong SemaneroNoch keine Bewertungen
- NCP HemothoraxDokument3 SeitenNCP HemothoraxMichael John F. NatividadNoch keine Bewertungen
- Altered Renal Perfusion CRFDokument4 SeitenAltered Renal Perfusion CRFKristel Anne Nillo ZepolNoch keine Bewertungen
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDokument8 SeitenNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiNoch keine Bewertungen
- Nursing Care Plan: Histolytica, ADokument4 SeitenNursing Care Plan: Histolytica, AkristennemarieNoch keine Bewertungen
- ALL PathophysiologyDokument2 SeitenALL PathophysiologyDeo Michael Rivera LlamasNoch keine Bewertungen
- NCP UtiDokument1 SeiteNCP UtiElaisa Mae Delos SantosNoch keine Bewertungen
- NCP - Acute PainDokument2 SeitenNCP - Acute PainsAm_300% (1)
- NCP Risk For InfectionDokument6 SeitenNCP Risk For InfectionCazze SunioNoch keine Bewertungen
- NCPDokument4 SeitenNCPMichelleNoch keine Bewertungen
- Nursing Care Plan For LYING inDokument4 SeitenNursing Care Plan For LYING inKarissa CiprianoNoch keine Bewertungen
- Infectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedDokument1 SeiteInfectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedJoshua MendozaNoch keine Bewertungen
- Fluid Volume Loss NCP - PediaDokument2 SeitenFluid Volume Loss NCP - PediaAdrian MallarNoch keine Bewertungen
- As Needed.: Environmental Stimuli 6Dokument4 SeitenAs Needed.: Environmental Stimuli 6Nicole GumolonNoch keine Bewertungen
- Adolescent NCPDokument1 SeiteAdolescent NCPClaire DobleNoch keine Bewertungen
- Burns - Skin Integrity, ImpairedDokument2 SeitenBurns - Skin Integrity, Impairedmakyofrancis20Noch keine Bewertungen
- NCP - Drug Study - Peptic UlcerDokument18 SeitenNCP - Drug Study - Peptic UlcerEmi EspinoNoch keine Bewertungen
- Case Study Ugib Lower MBDokument65 SeitenCase Study Ugib Lower MBQuolette Constante100% (1)
- NCP PpwardDokument15 SeitenNCP PpwardKarl Vincent Soso100% (1)
- Glaucoma NCPDokument4 SeitenGlaucoma NCPChantal CaraganNoch keine Bewertungen
- Assessment Objectives: "Masakit Lagi Yung Lalamunan NyaDokument3 SeitenAssessment Objectives: "Masakit Lagi Yung Lalamunan Nyaangel_pearl413100% (2)
- Nursing Care Plan Risk For InjuryDokument1 SeiteNursing Care Plan Risk For InjuryAce Dioso TubascoNoch keine Bewertungen
- Nursing Care PlanDokument5 SeitenNursing Care Planruggero07100% (2)
- College of Nursing and Allied Medical Sciences: WesleyanDokument3 SeitenCollege of Nursing and Allied Medical Sciences: WesleyanPrince Juzzel Banag100% (1)
- NCP LeukemiaDokument5 SeitenNCP LeukemiaTriciaNoch keine Bewertungen
- NCP Skin IntegityDokument3 SeitenNCP Skin Integityclydell joyce masiarNoch keine Bewertungen
- Nursing Care Plans For AppendicitisDokument2 SeitenNursing Care Plans For AppendicitisRodnie Insauriga GonzalesNoch keine Bewertungen
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Dokument20 SeitenSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizNoch keine Bewertungen
- Hypertonic SolutionsDokument4 SeitenHypertonic SolutionsVanessa PaguiriganNoch keine Bewertungen
- Impaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsDokument3 SeitenImpaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsKat AlaNoch keine Bewertungen
- B NCP On and Off Fever 2b ImproveddocxDokument6 SeitenB NCP On and Off Fever 2b ImproveddocxKylie CatralNoch keine Bewertungen
- Carpenito-Moyet, L. J. (2009) : IndependentDokument3 SeitenCarpenito-Moyet, L. J. (2009) : IndependentClint DelacruzNoch keine Bewertungen
- Nursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentDokument1 SeiteNursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentThomas FarrishNoch keine Bewertungen
- Fluid Volume Deficit BatuDokument2 SeitenFluid Volume Deficit Batumecz26Noch keine Bewertungen
- Cell Ab ActivitiesDokument7 SeitenCell Ab ActivitiesJanelle Cabida Supnad100% (1)
- NCP DiarrheaDokument2 SeitenNCP DiarrheaBracel GarciaNoch keine Bewertungen
- NCP Impaired SkinDokument2 SeitenNCP Impaired Skinarjay2306_obcq100% (1)
- Physical Assessment Appendix FinalDokument6 SeitenPhysical Assessment Appendix FinalLucelle ArellanoNoch keine Bewertungen
- NCP For Bladder CaDokument4 SeitenNCP For Bladder CaChris Tine CaccamNoch keine Bewertungen
- Gastroenteritis: Diseases and Conditions: GastroenteritisDokument6 SeitenGastroenteritis: Diseases and Conditions: GastroenteritisWen RodsaNoch keine Bewertungen
- Bahasa Inggris Kel 6Dokument7 SeitenBahasa Inggris Kel 6Akun NyampahNoch keine Bewertungen
- Nursing Care Plan For "Hepatitis"Dokument12 SeitenNursing Care Plan For "Hepatitis"jhonroks86% (14)
- HEPATITISDokument12 SeitenHEPATITISapi-3764215100% (1)
- The Temple of Athena Nike 2Dokument5 SeitenThe Temple of Athena Nike 2zepoli_zepoly6232Noch keine Bewertungen
- Steps To Perform A Blood TransfusionDokument1 SeiteSteps To Perform A Blood Transfusionzepoli_zepoly6232Noch keine Bewertungen
- On Dan Set RonDokument1 SeiteOn Dan Set Ronzepoli_zepoly6232Noch keine Bewertungen
- Hydrocortisone Inj. (IV)Dokument2 SeitenHydrocortisone Inj. (IV)zepoli_zepoly6232Noch keine Bewertungen
- Parasympathetic Divisions Which Are Anatomically and FunctionallyDokument35 SeitenParasympathetic Divisions Which Are Anatomically and Functionallyzepoli_zepoly6232Noch keine Bewertungen
- Enema Administration: Size of Rectal TubeDokument3 SeitenEnema Administration: Size of Rectal TubeMabesNoch keine Bewertungen
- Bowel EliminationDokument41 SeitenBowel EliminationekhafagyNoch keine Bewertungen
- Osmosis in The Digestive SystemDokument1 SeiteOsmosis in The Digestive SystemNadhiraAzhar_Noch keine Bewertungen
- The Tamil Nadu Dr. M.G.R. Medical University, Chennai Regulations of The UniversityDokument88 SeitenThe Tamil Nadu Dr. M.G.R. Medical University, Chennai Regulations of The UniversityAjay IyerNoch keine Bewertungen
- Case Study - AGE With Some DHNDokument19 SeitenCase Study - AGE With Some DHNJessica Mae Abaquita-javierNoch keine Bewertungen
- Coeliac Trunk, Superior and Inferior Mesenteric ArteriesDokument24 SeitenCoeliac Trunk, Superior and Inferior Mesenteric ArteriesKosisochukwu sixtus Ugwunnaji100% (1)
- Colon CancerDokument7 SeitenColon CancerAdrian Paulo CastivaNoch keine Bewertungen
- PROCTOSIGMOIDOSDokument5 SeitenPROCTOSIGMOIDOSJopet Llanita0% (1)
- Colon Cleansing Kit Users GuideDokument74 SeitenColon Cleansing Kit Users GuideYoungBody0% (1)
- Gastrointestinal Tract Function and DisordersDokument59 SeitenGastrointestinal Tract Function and DisordersTaylorNoch keine Bewertungen
- Digestion&Absorption CheeseburgerDokument3 SeitenDigestion&Absorption CheeseburgerKevin EdwardsNoch keine Bewertungen
- Calvo Fetal GITractDokument154 SeitenCalvo Fetal GITractRaluca HabaNoch keine Bewertungen
- BiofarDokument14 SeitenBiofarAl Pharux Ox-CygenNoch keine Bewertungen
- Factors Affecting Drug Absorption From Rectal SuppositoriesDokument2 SeitenFactors Affecting Drug Absorption From Rectal SuppositoriesRicardo VegaNoch keine Bewertungen
- Water Cures - F. Batmanghelidj, M.DDokument22 SeitenWater Cures - F. Batmanghelidj, M.DEric Callahan100% (1)
- Colostomycare 190521143735Dokument17 SeitenColostomycare 190521143735Abdul Gafoor CPNoch keine Bewertungen
- Large Blood Vessels of The GutDokument61 SeitenLarge Blood Vessels of The GutpoojaNoch keine Bewertungen
- Pathogenesis of Acute Diarrhea in Children - UpToDateDokument13 SeitenPathogenesis of Acute Diarrhea in Children - UpToDateNedelcu MirunaNoch keine Bewertungen
- English For Nurses (Autosaved)Dokument90 SeitenEnglish For Nurses (Autosaved)hieu100% (2)
- Clinical Signs of Retroperitoneal Abscess From.74Dokument6 SeitenClinical Signs of Retroperitoneal Abscess From.74Ali Sibra MulluziNoch keine Bewertungen
- The Peroral Pneumocolon Examination:, PoorDokument3 SeitenThe Peroral Pneumocolon Examination:, PoormanishbabuNoch keine Bewertungen
- SOP Performing A Rat dissection-FINAL - DBDokument12 SeitenSOP Performing A Rat dissection-FINAL - DBGhaniyyatul KhudriNoch keine Bewertungen
- The Digestive System: Cont'd (From Swallowing)Dokument56 SeitenThe Digestive System: Cont'd (From Swallowing)Jerilee SoCute WattsNoch keine Bewertungen
- Digestive SystemDokument17 SeitenDigestive SystemTricia GorozaNoch keine Bewertungen
- KJFP003 01 06Dokument17 SeitenKJFP003 01 06Mai Thiện NhânNoch keine Bewertungen
- ENEMADokument37 SeitenENEMAmftaganas100% (3)
- (Aligned To COT-RPMS Sample) : I. ObjectivesDokument6 Seiten(Aligned To COT-RPMS Sample) : I. ObjectivesAlice C. RiveraNoch keine Bewertungen
- Hap-2 Unit-02 Part 1Dokument9 SeitenHap-2 Unit-02 Part 1Nitesh YadavNoch keine Bewertungen
- Original Article: A Guide To Histomorphological Evaluation of Intestinal Inflammation in Mouse ModelsDokument21 SeitenOriginal Article: A Guide To Histomorphological Evaluation of Intestinal Inflammation in Mouse ModelsOUR STORYNoch keine Bewertungen
- Anatomi Dan Histologi Saluran Cerna BawahDokument20 SeitenAnatomi Dan Histologi Saluran Cerna BawahIlhamDevirxaNoch keine Bewertungen