Beruflich Dokumente
Kultur Dokumente
GLM0017 Birth After Previous Caesarean Section
Hochgeladen von
Anonymous 5mSMeP2jCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
GLM0017 Birth After Previous Caesarean Section
Hochgeladen von
Anonymous 5mSMeP2jCopyright:
Verfügbare Formate
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
BIRTH AFTER PREVIOUS CAESAREAN SECTION
DEFINITION
A woman with a uterine scar has the option of planned vaginal birth (VBAC) or an elective
repeat caesarean section (ERCS).
Factors to consider include: the material risks in the current pregnancy associated with
each, plans for further childbearing, the likelihood of achieving a vaginal birth and other
aspects of individual importance.
The decision is one for the woman to make in consultation with her carers who have an
obligation to provide her with the relevant information.
This area of practice suffers from misleading terminology. The following terms are
recommended and adapted from the National Institutes of Health Consensus Statement
(2010)1:
Trial of labour (TOL): A plan to birth vaginally in a woman who has had a previous
caesarean section.
Vaginal birth after caesarean section (VBAC): Vaginal birth following a TOL.
Elective repeat caesarean section (ERCS): Planned caesarean section in a
woman who has had one or more prior caesarean sections, whether or not the
caesarean section occurred at a scheduled time.
BACKGROUND
There is widespread public and professional concern regarding the increasing proportion of
births by caesarean section, with increasing rates of primary caesarean sections
leading to a larger proportion of women presenting with a history of prior caesarean. A
pregnant woman with a uterine scar has the option of choosing a planned trial of labour
(TOL) or an elective repeat caesarean section (ERCS).2
It is essential that women make an informed choice regarding whether to plan for a
vaginal birth (VBAC) or elective caesarean (ERCS). It is recommended that the woman,
obstetrician and Lead Maternity Carer (LMC) discuss the benefits and risks of both options
for the woman and her baby, supported by the provision of appropriate literature.
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 1 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
It is further recommend that all women who have experienced a prior caesarean birth are
referred to the newly established ‘Planned Birth after Caesarean Section‟ clinic held at
Christchurch Women’s Hospital to discuss plans for this birth with the obstetric and
midwifery team. LMC’s are encouraged to attend these appointments with the woman in
order to take part in this decision making process.
Previous caesarean birth is a ‘consultation condition’ as per Section 88 Referral Guidelines,
which states ‘The LMC must recommend to the woman that a consultation with a specialist is warranted
given that her pregnancy, labour or birth is or may be affected by the condition. Where a consultation occurs,
the decision regarding on-going care, advice to the LMC on management, and any recommendation to
subsequently transfer care must involve a three-way conversation between the specialist, the LMC and the
3
woman.’
Referrals should be made on BAC Referral form C210043 (Ref.6711) – Appendix 1
MANAGEMENT - ANTENATAL
How should women be counselled in the antenatal period?
Women with a prior history of one uncomplicated lower segment caesarean section, in an
otherwise uncomplicated pregnancy at term, with no contraindications to vaginal birth,
should be encouraged to aim for planned VBAC. This antenatal counselling should be
clearly documented in the woman’s notes, following discussion with the woman and her
LMC. Ideally this should occur in the first half of pregnancy.
Women should receive an information leaflet “Birth after Caesarean Section” Ref 6708
with this consultation.
A documented plan for mode of birth should be agreed between the woman, the
obstetrician and her LMC before the expected/planned birth date (ideally by 36 weeks).
This should include a plan for the event of labour starting prior to a scheduled date for
ERCS.
Women considering their options for birth following a single previous lower segment
caesarean section, should be informed that, overall according to the international literature,
their chances of VBAC are >70%4, 5, 6.
A number of factors are associated with VBAC, including; previous vaginal birth,
particularly previous VBAC, being the single best predictor for VBAC and is associated
with an approximately 87–90% planned VBAC rate.7, 8, 9
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 2 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
Risk factors for requiring caesarean section during TOL are:
(i) induced labour
(ii) no previous vaginal birth
(iii) body mass index (BMI) >3010-12
When all three of these factors are present OR
(iv) the woman has had a previous caesarean section for labour dystocia 9, VBAC
is achieved in only 40% of cases.9
Women with a prior history of two uncomplicated low transverse caesarean sections, in an
otherwise uncomplicated pregnancy at term, with no contraindication for vaginal birth, who
have been fully informed by a consultant obstetrician, may be considered suitable for
planned TOL. Observational studies have of shown VBAC rates of 62-75%13-16 in this
situation.
What are the contraindications to TOL?
Women with a prior history of classical caesarean section are recommended to give
birth by ERCS, as there is uncertainty to the safety and efficacy of planned TOL in this
situation.
Women with a previous uterine incision other than low transverse caesarean section
incision who wish to consider a vaginal birth should be assessed by a consultant
obstetrician with full access to the details of the previous surgery.
There is limited evidence on whether maternal or neonatal outcomes are significantly
influenced
by the number of prior caesarean births or type of prior uterine scar. Nonetheless, due to
higher absolute risks of uterine rupture or unknown risks, planned TOL is contraindicated in
women with:-
previous uterine rupture- risk of recurrent rupture is unknown17, 18
previous high vertical classical caesarean section (2-9% risk of uterine rupture) where
the uterine incision has involved the whole length of the uterine corpus. 17, 18
three or more previous caesarean deliveries (reliable estimate of risks of rupture
unknown).
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 3 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
What are the specific benefits and risks of TOL?
Women considering the options for birth after a previous caesarean should be informed that
ERCS does increase the risk of serious complications in future pregnancies which
includes placenta praevia, placenta accreta and hysterectomy. 21-26
Women considering the options for birth after caesarean section should be informed that
planned TOL carries a risk of uterine rupture of ≤0.5% after 1 caesarean19 (99.5% no
rupture) and <1% following 2 caesareans24. VBAC decreases the caesarean related risks
for future pregnancies.
Planned TOL in special circumstances
How should a woman be counselled in the context other obstetric risk factors?
Women who are preterm and considering the options for birth after a previous caesarean
should be informed that planned preterm TOL has similar VBAC rates to planned term
VBAC but with a lower risk of uterine rupture.27
A cautious approach is advised when considering planned VBAC in women with twin
gestation28, 29, fetal macrosomia7, 17 and short interdelivery interval of less than 2
years30-32, as there is uncertainty in the safety and efficacy of planned TOL in such
situations.
INTRAPARTUM
Intrapartum support and intervention during planned TOL
Where and how should TOL be managed?
Women should be advised that planned TOL should be conducted in a secondary/tertiary
facility. Women should be advised to have close electronic fetal monitoring (EFM)
following the onset of uterine contractions for the duration of labour. An abnormal
cardiotocograph (CTG) is the most consistent finding in uterine rupture and is present in
55–87% of these events.33
There is no requirement for a birthing woman to have an IV line placed for the indication of
previous CS alone, as this can be inserted rapidly if and when required.
In the event that a woman declines close EFM during TOL and following appropriate
counselling, a three-way conversation should ensue to negotiate what form of monitoring
the woman will accept. Counselling is to include the risk of „silent‟ uterine rupture,
resulting in an increased risk of cerebral palsy and fetal demise secondary to a delay in
diagnosis of uterine rupture. As a minimum, intermittent auscultation (I-A) is suggested at
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 4 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
15 minute intervals during the first stage and I-A following every contraction in the second
stage of her TOL.
Also refer to the Electronic Fetal Monitoring guideline GL/M0010
In the unlikely event that a woman presents in advanced labour at a rural or primary unit
and the assessment is that it is unsafe to transfer to the secondary/tertiary facility,
intermittent auscultation (I-A, as above) is the monitoring of choice. The use of
continuous CTG in these settings is not recommended.
Continuous intrapartum (one-to-one) midwifery care is beneficial to enable prompt
identification and management of uterine scar rupture.
Induction and augmentation
How should women with a previous caesarean birth be advised in relation to induction of
labour or augmentation?
Women should be informed of the 2-3-fold increased risk (overall risk of 1.5%) of uterine
rupture and around a1.5-fold increased risk ( 0.75%) of caesarean section in induced
and/or augmented TOL compared with spontaneous labours.34
Women should be informed that there is potentially a higher risk of uterine rupture with
induction of labour with prostaglandins versus non-prostaglandin methods. The current
evidence is inconclusive, with the National Institute of Child Health and Development
(NICHD)16 study prostaglandin induction compared with non-prostaglandin induction
incurred a non-significantly higher risk of uterine rupture of 1.4% versus 0.9%, whereas in
an analysis of nationally collected data from Scotland35, prostaglandin induction compared
with non-prostaglandin induction was associated with a statistically significantly higher
uterine rupture risk of 0.9% versus 0.3%
There should be detailed serial cervical assessments, preferably by the same person, for
both augmented and spontaneous TOL, to ensure that there is adequate cervical progress,
thereby allowing the TOL to continue.
Discussion is recommended regarding the:
decision to induce
method chosen
decision to augment with oxytocin
time intervals for serial vaginal examination
selected parameters of progress that would necessitate and advise on discontinuing
TOL.
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 5 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
The above should be discussed and agreed with the woman and her LMC and a
consultant obstetrician , either directly, or via the obstetric registrar who has discussed
the specific situation with the consultant .
How should augmentation of labour be conducted?
The additional risks in augmented TOL mean that:
although augmentation is not contraindicated it should only be preceded by detailed
obstetric assessment, maternal counselling and by a consultant-led decision
oxytocin augmentation should be titrated such that it should not exceed the
maximum rate of contractions of four in 10 minutes; the ideal contraction frequency
would be three to four in 10 minutes35
Detailed serial cervical assessments, preferably by the same person, are
necessary to show adequate cervical progress, thereby allowing augmentation to
continue.
Management of Suspected scar rupture
Early diagnosis of uterine scar rupture followed by expeditious laparotomy and resuscitation
is essential to reduce associated morbidity and mortality in mother and infant. There is no
single pathognomic clinical feature that is indicative of uterine rupture but the presence of
any of the following peripartum should raise the concern of the possibility of this event and
necessitate full clinical evaluation:36
● abnormal CTG
● severe abdominal pain, especially if persisting between contractions
● chest pain or shoulder tip pain, sudden onset of shortness of breath
● acute onset scar tenderness
● abnormal vaginal bleeding or haematuria
● cessation of previously efficient uterine activity
● maternal tachycardia, hypotension or shock
● loss of station of the presenting part.
The diagnosis is ultimately confirmed at emergency caesarean section or postpartum
laparotomy.
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 6 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
DOCUMENTATION
Electronic Fetal Monitoring Guideline GL/M0010
Electronic Fetal Monitoring M0010.pdf
BAC Referral Form C210043 (Ref.6711) – Appendix 1
REFERENCES
1. National Institutes of Health Consensus Development Conference Statement: Vaginal Birth
After Cesarean: New Insights. March 8–10, 2010.
2. Planned vaginal birth after caesarean section (trial of labour) (C-Obs 38)
http://www.ranzcog.edu.au/component/docman/doc_view/971-c-obs-38-planned-vaginal-birth-after-
caesarean-section-trial-of-labour-.html
3. Ministry of Health. 2012. Guidelines for Consultation with Obstetric and Related Medical
Services (Referral Guidelines). Wellington: Ministry of Health.
4. Guise JM, Berlin M, McDonagh M, Osterweil P, Chan B, Helfand M. Safety of vaginal birth
after cesarean: a systematic review. Obstet Gynecol 2004;103:420–9.
5. Chauhan SP, Martin JN, Jr., Henrichs CE, Morrison JC, Magann EF. Maternal and perinatal
complications with uterine rupture in 142,075 patients who attempted vaginal birth after
caesarean delivery: a review of the literature. Am J Obstet Gynecol 2003; 189:408–17.
6. Mozurkewich EL, Hutton EK. Elective repeat cesarean delivery versus trial of labor: a meta–
analysis of the literature from 1989 to 1999. Am J Obstet Gynecol 2000;183:1187–97.
7. Landon MB, Leindecker S, Spong CY, Hauth JC, Bloom S, Varner MW, et al. The MFMU
Cesarean Registry: factors affecting the success of trial of labor after previous cesarean
delivery. Am J Obstet Gynecol 2005;193:1016–23.
8. Smith GC, White IR, Pell JP, Dobbie R. Predicting caesarean section and uterine rupture
among women attempting vaginal birth after prior cesarean section. PLoS Med 2005;2:871–8.
9. Gyamfi C, Juhasz G, Gyamfi P, Stone JL. Increased success of trial of labor after previous
vaginal birth after cesarean. Obstet Gynecol 2004;104:715–19.
10. Hibbard JU, Gilbert S, Landon MB, Hauth JC, Leveno KJ, Spong CY, et al. Trial of labor or
repeat cesarean delivery in women with morbid obesity and previous cesarean delivery. Obstet
Gynecol 2006;108:125–33.
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 7 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
11. Goodall PT, Ahn JT, Chapa JB, Hibbard JU. Obesity as a risk factor for failed trial of labor in
patients with previous caesarean delivery. Am J Obstet Gynecol 2005;192:1423–6.
12. Juhasz G, Gyamfi C, Gyamfi P, Tocce K, Stone JL. Effect of body mass index and excessive
weight gain on success of vaginal birth after cesarean delivery.
Obstet Gynecol 2005;106:741–6.
13. Macones GA, Cahill A, Pare E, Stamilio DM, Ratcliffe S, Stevens E, et al. Obstetric outcomes
in women with two prior caesarean deliveries: is vaginal birth after cesarean delivery a viable
option? Am J Obstet Gynecol 2005;192:1223–8.
14. Spaans WA, van der Vliet LM, Roell-Schorer EA, Bleker OP, van Roosmalen J. Trial of
labour after two or three previous caesarean sections. Eur J Obstet Gynecol Reprod Biol 2003;
110:16–19.
15. Caughey AB, Shipp TD, Repke JT, Zelop CM, Cohen A, Lieberman E. Rate of uterine
rupture during a trial of labor in women with one or two prior cesarean deliveries. Am J Obstet
Gynecol 1999;181:872–6.
16. Miller DA, Diaz FG, Paul RH. Vaginal birth after cesarean: a 10-year experience. Obstet
Gynecol 1994; 84:255–8.
17. Guise JM, Hashima J, Osterweil P. Evidence–based vaginal birth after Caesarean section.
Best Prac Res Clin Obstet Gynaecol 2005;19:117–30.
18. Turner MJ. Uterine rupture. Best Prac Res Clin Obstet Gynaecol 2002;16:69–79.
16. Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. Maternal and
perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med
2004;351:2581–9.
20. Landon MB, Spong CY, Thom E, Hauth JC, Bloom SL, Varner MW, et al. Risk of uterine
rupture with a trial of labor in women with multiple and single prior cesarean delivery. Obstet
Gynecol 2006;108:12–20.
21. Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of
caesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol 1997;177:1071–8.
22. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa–placenta accreta.
Am J Obstet Gynecol 1997;177:210–214.
23. Makoha FW, Felimban HM, Fathuddien MA, Roomi F, Ghabra T. Multiple cesarean section
morbidity. Int J Gynaecol Obstet 2004;87:227–32.
24. Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J
Obstet Gynecol 2005;192:1458–61.
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 8 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
25. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity
associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006;107:1226–32.
26. Impact of multiple cesarean deliveries on maternal morbidity: a systematic review. Marshall NE,
Fu R, Guise JM. Am J Obstet Gynecol. 2011 Sep;205(3):262.e1-8. Epub 2011 Jun 15
27. Durnwald CP, Rouse DJ, Leveno KJ, Spong CY, MacPherson C, Varner MW, et al. The
Maternal–Fetal Medicine Units Cesarean Registry: safety and efficacy of a trial of labor in
preterm pregnancy after a prior cesarean delivery. Am J Obstet Gynecol 2006;195:1119–26.
28. Varner MW, Leindecker S, Spong CY, Moawad AH, Hauth JC, Landon MB, et al. The
Maternal–Fetal Medicine Unit caesarean registry: trial of labor with a twin gestation. Am J
Obstet Gynecol 2005;193:135–40.
29. Cahill A, Stamilio DM, Pare E, Peipert JP, Stevens EJ, Nelson DB, et al. Vaginal birth after
caesarean (VBAC) attempt in twin pregnancies: is it safe? Am J Obstet Gynecol
2005;193:1050–5.
30. Bujold E, Mehta SH, Bujold C, Gauthier RJ. Interdelivery interval and uterine rupture. Am J
Obstet Gynecol 2002;187:1199–202.
31. Esposito MA, Menihan CA, Malee MP. Association of interpregnancy interval with uterine
scar failure in labor: a case–control study. Am J Obstet Gynecol 2000;183:1180–3.
32. Shipp TD, Zelop CM, Repke JT, Cohen A, Lieberman E. Interdelivery interval and risk of
symptomatic uterine rupture. Obstet Gynecol 2001;97:175–7.
33. Guise JM, McDonagh MS, Osterweil P, Nygren P, Chan BK, Helfand M. Systematic review of
the incidence and consequences of uterine rupture in women with previous caesarean section.
BMJ 2004;329:19–25.
34. Ofir K, Sheiner E, Levy A, Katz M, Mazor M. Uterine rupture: risk factors and pregnancy
outcome. Am J Obstet Gynecol 2003; 189:1042–6.
35. Smith GC, Pell JP, Pasupathy D, Dobbie R. Factors predisposing to perinatal death related to
uterine rupture during attempted vaginal birth after caesarean section: retrospective cohort
study. BMJ 2004;329:375.
35. Royal College of Obstetricians and Gynaecologists. Induction of labour. Evidence-based
Clinical Guideline Number 9. London: RCOG Press; 2001.
36. Turner MJ. Uterine rupture. Best Prac Res Clin Obstet Gynaecol 2002;16:69–79.
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 9 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
WOMEN‟S HEALTH SERVICE
Christchurch Women‟s Hospital
Maternity Guideline
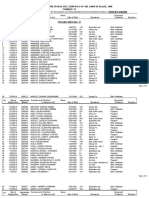
APPENDIX 1
Date Issued: April 2008 Birth after previous caesarean section
Date Revised: October 2013 Maternity Guidelines
Review Date: October 2016 Christchurch Women‟s Hospital
Written/Authorised by: Maternity Guidelines Group Christchurch New Zealand
Review Team: Maternity Guidelines Group
W&CH/GL/M0017 This document is to be viewed via the CDHB Intranet only. Page 10 of 10
All users must refer to the latest version from the CDHB
intranet at all times. Any printed versions, including photocopies,
may not reflect the latest version.
Das könnte Ihnen auch gefallen
- India's institutional flows dominated by domestic investors outpacing foreign investorsDokument14 SeitenIndia's institutional flows dominated by domestic investors outpacing foreign investorsAnonymous 5mSMeP2jNoch keine Bewertungen
- India's institutional flows dominated by domestic investors outpacing foreign investorsDokument14 SeitenIndia's institutional flows dominated by domestic investors outpacing foreign investorsAnonymous 5mSMeP2jNoch keine Bewertungen
- Instrument Symbol Expiry - DT Open High LOWDokument4 SeitenInstrument Symbol Expiry - DT Open High LOWAnonymous 5mSMeP2jNoch keine Bewertungen
- Trade Date Category Buy Value in Rs - CroresDokument2 SeitenTrade Date Category Buy Value in Rs - CroresAnonymous 5mSMeP2jNoch keine Bewertungen
- MWPL Cli 30102019Dokument1 SeiteMWPL Cli 30102019Anonymous 5mSMeP2jNoch keine Bewertungen
- Options Open Interest Analysis SimplifiedDokument17 SeitenOptions Open Interest Analysis SimplifiedAnonymous 5mSMeP2jNoch keine Bewertungen
- Options Open Interest Analysis SimplifiedDokument20 SeitenOptions Open Interest Analysis SimplifiedAnonymous 5mSMeP2jNoch keine Bewertungen
- The Implied Volatility of Forward Starting Options: ATM Short-Time Level, Skew and CurvatureDokument21 SeitenThe Implied Volatility of Forward Starting Options: ATM Short-Time Level, Skew and CurvatureAnonymous 5mSMeP2jNoch keine Bewertungen
- Equity Value: Date Observation Equity Value K-Ratio 1996 3.560552754 K-Ratio 2003 0.356055275 K-Ratio 2013 5.65220227Dokument4 SeitenEquity Value: Date Observation Equity Value K-Ratio 1996 3.560552754 K-Ratio 2003 0.356055275 K-Ratio 2013 5.65220227Anonymous 5mSMeP2jNoch keine Bewertungen
- Fovolt 03042020Dokument9 SeitenFovolt 03042020Anonymous 5mSMeP2jNoch keine Bewertungen
- 7 Intraday Principle 02 NovDokument12 Seiten7 Intraday Principle 02 NovAnonymous 5mSMeP2jNoch keine Bewertungen
- Position As Percentage (%) of MWPL SR No. Underlying Stock Client 1 Client 2 Client 3 Client 4 Client 5 Client 6 Client 7 Client 8Dokument2 SeitenPosition As Percentage (%) of MWPL SR No. Underlying Stock Client 1 Client 2 Client 3 Client 4 Client 5 Client 6 Client 7 Client 8Anonymous 5mSMeP2jNoch keine Bewertungen
- Options Open Interest Analysis SimplifiedDokument17 SeitenOptions Open Interest Analysis SimplifiedAnonymous 5mSMeP2jNoch keine Bewertungen
- 7 Intraday TricksDokument15 Seiten7 Intraday TricksAnonymous 5mSMeP2jNoch keine Bewertungen
- Remedial Mantras for Health, Wealth and ProblemsDokument5 SeitenRemedial Mantras for Health, Wealth and Problemsnarasimhamurthy k v100% (1)
- Position As Percentage (%) of MWPL SR No. Underlying Stock Client 1 Client 2 Client 3 Client 4 Client 5 Client 6 Client 7 Client 8Dokument2 SeitenPosition As Percentage (%) of MWPL SR No. Underlying Stock Client 1 Client 2 Client 3 Client 4 Client 5 Client 6 Client 7 Client 8Anonymous 5mSMeP2jNoch keine Bewertungen
- FfeDokument38 SeitenFfeAnonymous 5mSMeP2jNoch keine Bewertungen
- Position As Percentage (%) of MWPL SR No. Underlying Stock Client 1 Client 2 Client 3 Client 4 Client 5 Client 6 Client 7 Client 8Dokument2 SeitenPosition As Percentage (%) of MWPL SR No. Underlying Stock Client 1 Client 2 Client 3 Client 4 Client 5 Client 6 Client 7 Client 8Anonymous 5mSMeP2jNoch keine Bewertungen
- Moneypati Options OI Sheet Link Password PDFDokument10 SeitenMoneypati Options OI Sheet Link Password PDFSHOEBNoch keine Bewertungen
- Chilakamarthi Prabhakar Chakravarthy Sharma Panchangam PDFDokument205 SeitenChilakamarthi Prabhakar Chakravarthy Sharma Panchangam PDFAnonymous 5mSMeP2jNoch keine Bewertungen
- 33 Matching-M4 HindiDokument94 Seiten33 Matching-M4 HindiAnonymous 5mSMeP2jNoch keine Bewertungen
- Easy Credit Card MITC PDFDokument6 SeitenEasy Credit Card MITC PDFAnonymous 5mSMeP2jNoch keine Bewertungen
- 82 LongevityLifeSpan Part1Dokument14 Seiten82 LongevityLifeSpan Part1Anonymous 5mSMeP2jNoch keine Bewertungen
- DR - Sandya LakshmiDokument1 SeiteDR - Sandya LakshmiAnonymous 5mSMeP2jNoch keine Bewertungen
- Siddha Mahayoga: An Easy Method for Merging the Human Soul with the DivineDokument387 SeitenSiddha Mahayoga: An Easy Method for Merging the Human Soul with the Divinemohanp716515Noch keine Bewertungen
- Savings Charges PDFDokument2 SeitenSavings Charges PDFAnonymous 5mSMeP2jNoch keine Bewertungen
- The Enigma of Arudhas – Part 1Dokument14 SeitenThe Enigma of Arudhas – Part 1Guilherme Alves PereiraNoch keine Bewertungen
- The Enigma of Arudhas – Part 1Dokument14 SeitenThe Enigma of Arudhas – Part 1Guilherme Alves PereiraNoch keine Bewertungen
- 33 Matching-M4 HindiDokument94 Seiten33 Matching-M4 HindiAnonymous 5mSMeP2jNoch keine Bewertungen
- 074 - Rohinaa - Com Curse of ShukraDokument26 Seiten074 - Rohinaa - Com Curse of ShukraAnonymous 5mSMeP2j50% (2)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5782)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- CYPOP14 Support Children and Young People To Have Positive RelationshipsDokument17 SeitenCYPOP14 Support Children and Young People To Have Positive RelationshipsFariha TasnimNoch keine Bewertungen
- Pdev Examm Pogi Si JanriizxxccDokument34 SeitenPdev Examm Pogi Si JanriizxxccBernabeth PanangananNoch keine Bewertungen
- Exercises To Facilitate Change of Baby's Position From Breech To CephalicDokument3 SeitenExercises To Facilitate Change of Baby's Position From Breech To CephalicaziskarnNoch keine Bewertungen
- Prof. Ed. 102 ReviewerDokument11 SeitenProf. Ed. 102 ReviewerKyla CabullosNoch keine Bewertungen
- Full Download Test Bank For Educating Exceptional Children 13th Edition Kirk PDF Full ChapterDokument6 SeitenFull Download Test Bank For Educating Exceptional Children 13th Edition Kirk PDF Full Chaptermosesfortread7gks6k100% (12)
- THE PHYSICAL SELF (Reviewer)Dokument4 SeitenTHE PHYSICAL SELF (Reviewer)Dalde DinaNoch keine Bewertungen
- Human Development and Faith Reaction PaperDokument4 SeitenHuman Development and Faith Reaction PaperLauren StamperNoch keine Bewertungen
- Toddler development milestones by ageDokument1 SeiteToddler development milestones by ageFranciane CorreaNoch keine Bewertungen
- Diary FormatDokument1 SeiteDiary FormatNerlyne Mae PonaseNoch keine Bewertungen
- Rough DraftDokument12 SeitenRough Draftapi-251290100Noch keine Bewertungen
- FS 12 Parents Consent 2023Dokument3 SeitenFS 12 Parents Consent 2023Mae MejaresNoch keine Bewertungen
- Dokumen - Tips - Afg Athena Nadia 3 in 1 Crib Manual Athena Nadia 3 in 1 Crib Manual Afg InternationalDokument4 SeitenDokumen - Tips - Afg Athena Nadia 3 in 1 Crib Manual Athena Nadia 3 in 1 Crib Manual Afg InternationalGeny AnthonyNoch keine Bewertungen
- MAPEH L3 - Physical Changes During Puberty MAPEH 5Dokument13 SeitenMAPEH L3 - Physical Changes During Puberty MAPEH 5Chester ManalangNoch keine Bewertungen
- To The Parents:: Interpretation of Standard Score or Development IndexDokument1 SeiteTo The Parents:: Interpretation of Standard Score or Development IndexAquinas ThomasNoch keine Bewertungen
- Queen's SquareDokument45 SeitenQueen's SquareGarifuna NationNoch keine Bewertungen
- Chapter 4 - Middle ChildhoodDokument3 SeitenChapter 4 - Middle ChildhoodSilvia RodriguezNoch keine Bewertungen
- MAPPING TOOL FOR 11-18 YEAR OLDSDokument7 SeitenMAPPING TOOL FOR 11-18 YEAR OLDSMichelle CabaseNoch keine Bewertungen
- Adolescent PregnancyDokument8 SeitenAdolescent Pregnancyapi-281250888Noch keine Bewertungen
- Nguyen Community ResourceDokument12 SeitenNguyen Community Resourceapi-534423110Noch keine Bewertungen
- Family Interview Paper FinalDokument9 SeitenFamily Interview Paper Finalapi-253494455Noch keine Bewertungen
- The Emotion Regulation Questionnaire For Children and Adolescents (ERQ-CA) : A Psychometric EvaluationDokument11 SeitenThe Emotion Regulation Questionnaire For Children and Adolescents (ERQ-CA) : A Psychometric EvaluationYelitza ValeroNoch keine Bewertungen
- Offer Letter For Support To LucyDokument1 SeiteOffer Letter For Support To LucyjosefNoch keine Bewertungen
- CHCPRT001 Child Protection Work PracticesDokument52 SeitenCHCPRT001 Child Protection Work PracticespoojaNoch keine Bewertungen
- Developmental StageDokument1 SeiteDevelopmental Stagebfly1235100% (1)
- Navigating Biological, Psychological & Social Challenges of AdolescenceDokument19 SeitenNavigating Biological, Psychological & Social Challenges of AdolescenceOlivera John ReyNoch keine Bewertungen
- Teen Pregnancy: By: Sandra GomezDokument16 SeitenTeen Pregnancy: By: Sandra Gomezstarndmoon_889100% (1)
- ChildbirthDokument201 SeitenChildbirthapi-26829072Noch keine Bewertungen
- Antenatal Care IsDokument19 SeitenAntenatal Care IsShivani Shah100% (1)
- Child Abuse and NeglectDokument11 SeitenChild Abuse and NeglectAmit RawlaniNoch keine Bewertungen
- Name: Date: Strand/Section:: I. MULTIPLE CHOICE: Encircle The Letter of The Correct AnswerDokument3 SeitenName: Date: Strand/Section:: I. MULTIPLE CHOICE: Encircle The Letter of The Correct AnswerJessuel Larn-epsNoch keine Bewertungen