Beruflich Dokumente
Kultur Dokumente
Wechalekar2015 PDF
Hochgeladen von
Franccesca Guidotti CortesiOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Wechalekar2015 PDF
Hochgeladen von
Franccesca Guidotti CortesiCopyright:
Verfügbare Formate
Seminar
Systemic amyloidosis
Ashutosh D Wechalekar, Julian D Gillmore, Philip N Hawkins
Tissue deposition of protein fibrils causes a group of rare diseases called systemic amyloidoses. This Seminar focuses Published Online
on changes in their epidemiology, the current approach to diagnosis, and advances in treatment. Systemic light chain December 21, 2015
http://dx.doi.org/10.1016/
(AL) amyloidosis is the most common of these conditions, but wild-type transthyretin cardiac amyloidosis (ATTRwt) S0140-6736(15)01274-X
is increasingly being diagnosed. Typing of amyloid fibrils, a critical determinant of therapy, has improved with the
National Amyloidosis Centre,
wide availability of laser capture and mass spectrometry from fixed histological tissue sections. Specific and accurate University College London
evaluation of cardiac amyloidosis is now possible using cardiac magnetic resonance imaging and cardiac repurposing (Royal Free Campus), London,
of bone scintigraphy tracers. Survival in AL amyloidosis has improved markedly as novel chemotherapy agents have UK (A D Wechalekar FRCPath;
J D Gillmore FRCP;
become available, but challenges remain in advanced disease. Early diagnosis, a key to better outcomes, still remains P N Hawkins FMedSci)
elusive. Broadening the amyloid-specific therapeutic landscape to include RNA inhibitors, fibril formation stabilisers
Correspondence to:
and inhibitors, and immunotherapeutic targeting of amyloid deposits holds promise to transform outcomes in Dr Ashutosh D Wechalekar,
systemic amyloidoses. National Amyloidosis Centre,
University College London l
(Royal Free Campus), Rowland
Introduction AL amyloidosis as three to five cases per million
Hill Street, London NW3 2PF, UK
The amyloidoses are a rare group of diseases that result population.5 Death certificates from the UK indicate a.wechalekar@ucl.ac.uk
from extracellular deposition of amyloid, a fibrillar that amyloidosis has an incidence of about one per
material derived from various precursor proteins that 100 000 population and is the cause of death in 0·58 per
self-assemble with highly ordered abnormal cross 1000 individuals.6 Analysis of Swedish hospital discharge
β-sheet conformation.1,2 Deposition of amyloid can and outpatient registers found an incidence of 8·29 per
occur in the presence of an abnormal protein (eg, million person-years for non-hereditary amyloidosis and
hereditary amyloidosis and acquired systemic 3·2 per million person-years for AL amyloidosis.7 Table 1
immunoglobulin light chain [AL] amyloidosis), in shows the frequency of different amyloid types among
association with prolonged excess abundance of a 5100 individuals with amyloidosis or amyloidogenic
normal protein (eg, reactive systemic [AA] amyloidosis mutations assessed at the National Amyloidosis Centre
and β2-microglobulin [β2M] dialysis-related amyloidosis), (NAC) in the UK from 1987 to 2012.9
and, for reasons unknown, accompanying the ageing Patterns of referral to the NAC have changed
process (eg, wild-type transthyretin amyloidosis substantially over the past two decades.9 The frequency of
[ATTRwt; or senile systemic amyloidosis] and atrial AL amyloidosis, as a proportion of total referrals every
natriuretic peptide amyloidosis). year, has essentially remained stable over the decades
More than 30 proteins have been identified to form (67% of all cases). Conversely, a remarkable progressive
amyloid in man,3 but recent use of mass spectrometry to decrease has been seen in the proportion of patients
identify amyloid suggests that many more proteins referred with AA amyloidosis—from 32% of all cases
might be amyloidogenic.4 The most frequent type of during 1987–95 to 6·8% during 2009–12—which probably
amyloidosis in high-income countries is AL amyloidosis. reflects improvement of treatment of inflammatory
The availability of new technologies has improved arthropathies with biological drugs. Referral of patients
diagnosis and enabled accurate fibril typing and better with wild-type TTR amyloidosis (ATTRwt)-related
risk stratification. Outcomes have improved, at least in cardiomyopathy has increased greatly—from fewer than
AL amyloidosis, and several novel therapies are on the ten (0·2%) cases during 1988–99 to more than 100 (6·4%)
horizon for various types of amyloidosis, including cases in 2009–12, which probably reflects the increasing
antibody-based therapy and RNA inhibition strategies.
However, management of patients with advanced organ
involvement at diagnosis remains a major challenge, Search strategy and selection criteria
with nearly a third of all patients with AL amyloidosis A literature search was performed between 1990 and 2014
still dying within a few months of diagnosis. Early using PubMed and Web of Science with the search terms
diagnosis of amyloidosis remains an elusive goal that “amyloidosis” or “amyloid*” and each of “systemic
requires education of both physicians and patients. amyloidosis“, “AL“, “AA“, “ATTR“, “AFib“, “AApoA1”, ”ALys”,
This Seminar reviews progress in the field over the ”Aβ2M”, ”ALect2”, ”epidemiology”, ”imaging”, ”diagnosis”,
past decade. “treatment“, “chemotherapy”, ”stem cell transplantation”, and
“outcome”. We also reviewed conference abstracts of the
Epidemiology of amyloidosis international amyloidosis workshops in Rome 2010 and
Few epidemiological data have been published for Groningen 2012, the Annual Meeting of the American Society
amyloidosis. The first population-based study of AL of Hematology, 2010–2012, and the International Myeloma
amyloidosis was done in Olmsted County, MN, USA, Workshops 2011 and 2013.
and was published in 1992. It reported the incidence of
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 1
Seminar
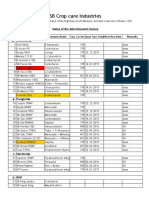
Acquired or Patients seen Underlying Precursor protein Organ involvement Treatment Treatment
hereditary at UK-NAC disorder target
(%; n=5100)
Heart Kidneys Liver PN Other
(AN)
AL Acquired 4067 (68%) Plasma cell Monoclonal +++ +++ ++ +(+) Soft tissue Chemotherapy or dFLC <40 mg/L
dyscrasia immunoglobulin gastrointestinal ASCT
light chain
AA Acquired 633 (12%) Inflammatory SAA –/+ (late) +++ +(late) – Gastrointestinal Suppression of SAA <4 mg/L
disorders (RA, JIA, (late) inflammation
IVDU, FPS)
ATTR Acquired 168 (3·2%) ·· Wild-type TTR +++ – – – Carpal tunnel Supportive Optimum control
syndrome of heart failure
Hereditary 339 (6·6%) Mutations in TTR Abnormal TTR ++ – – +++ (+++) – Liver transplant Optimum control
gene (younger patients of congestive
with heart failure and
V30M-related symptoms of
ATTR), diflunisal, PN/AN
(doxycycline/
TUDCA)
Supportive
AFib Hereditary 87 (1·7%) Mutations in Abnormal – +++ –/+ – – Supportive, organ Preserve renal
fibrinogen fibrinogen transplant function
α-chain gene
ALect2 Acquired 16 (0·3%) Uncertain Lect2 – +++ ++ – – Supportive Preserve renal
function
AApoA1 Hereditary 40 (0·8%) Mutations in Abnormal ApoA1 + ++ ++ +/−(–) Testis Supportive, organ Preserve renal
apolipoprotein A1 transplant function
gene
ALys Hereditary 17 (0·3%) Mutations in Abnormal – + ++ – Gastrointestinal Supportive ··
lysozyme gene lysozyme or skin
AGel Hereditary 4 (0·1%) Mutations in Abnormal gelsolin – -/+ – ++(–) – Supportive ··
gelsolin gene cranial
Aβ2M Acquired or 93 (1·8%) Long-term dialysis Aβ2M – – – – (+*) Carpal tunnel Supportive, renal ··
hereditary syndrome, transplant
arthropathy
Aβ2M=β2-microglobulin-related. AFib=fibrinogen A α-chain. AGel=gelsolin amyloid. AL=amyloid light chain. ALect2=leucocyte cell–derived chemotaxin 2. ALys=lysozyme amyloid. AN=autonomic neuropathy.
ASCT=autologous stem cell transplant. ATTR=amyloid transthyretin. dFLC=difference between involved and uninvolved free light chain. FPS=familial periodic fever syndromes. IVDU=intravenous drug abuse.
JIA=juvenile inflammatory arthritis. PN=peripheral neuropathy. RA=rheumatoid arthritis. SAA=serum amyloid A. TTR=transthyretin. TUDCA=tauro-ursodeoxycholic acid. UK-NAC=UK National Amyloidosis
Centre. *AN only in familial Aβ2M amyloidosis.8 + indicates relative frequency: +++ very common, ++ common; + less common; –/+ rare; – not applicable or does not occur in this condition. (drug)=undergoing
clinical trials. AA=amyloid A. AApoA1= apolipoprotein A1 amyloid.
Table 1: Characteristics of the common types of amyloidosis
contribution of cardiac MRI to diagnosis. The true between the two countries—80% in Portugal compared
incidence of ATTRwt amyloidosis in elderly people with 11% in Sweden17—for reasons that are as yet
remains unknown, but cardiac amyloid deposits of this unclear. In County Donegal in northwest Ireland, the
type have been reported at autopsy in a quarter of Thr60Ala variant of TTR has a population prevalence of
individuals older than 80 years.10 Amyloidosis of the 1·1%.18 The Val122Ile variant, which is carried by 3–4%
recently described leucocyte chemotactic factor-2 (ALect2) of the African American population, is associated with
type11 now seems to be the third most common cause of late-onset amyloid cardiomyopathy,19 but the disease
acquired renal amyloidosis, occurring predominantly in penetrance seems to be very low. The population
patients from South Asia, North Africa, the Middle East, frequency of other familial amyloidoses remains
and Mexico.12–14 unknown. Apolipoprotein A1 (ApoA1) amyloidosis
The epidemiology of hereditary amyloidosis is poorly accounted for 0·8% of all cases of amyloidosis seen at
studied, other than familial amyloid polyneuropathy the NAC, but the population incidence is unknown.
(ATTR-FAP), which results from mutations in TTR and
occurs with a frequency of less than 1:100 000 in Europe. Amyloid fibrils
The frequency of TTR mutations is high in some All amyloid deposits are composed of protein fibrils
populations. For example, the Val30Met variant of TTR that have a remarkably similar structure, with a
has a prevalence of 1:538 in northern Portugal15 and 4% diameter of 7–13 nm and a common core structure
in northern Sweden,16 but penetrance differs markedly consisting of anti-parallel β-strands (less commonly,
2 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Seminar
parallel β-strands) that form sheets.20–23 All amyloid exceptionally rare.31 The hallmark of hereditary AApoA1
deposits also contain several minor non-fibrillary and lysozyme (ALys) amyloidosis is involvement of the
constituents, including glycosaminoglycans (GAGs) kidneys and liver, which is very slowly progressive,
and serum amyloid P component (SAP).24,25 The specific, sometimes over decades.35
highly ordered ultrastructure of amyloid fibrils accounts Neuropathy is a feature of AL amyloidosis and some
for their characteristic property of binding Congo hereditary types of ATTR and AApoA1 amyloidosis.
red dye in a spatial manner that produces green Amyloid peripheral neuropathy is predominantly
birefringence when viewed under cross-polarised light. axonal and involves both the small and large fibres. It
This birefringence remains the histological gold begins with loss of the small fibre-mediated sensations
standard for confirming the presence of amyloid in of heat or cold, can be painful,36 and can be difficult
tissue samples. The universal presence of common to differentiate from the more common chronic
non-fibrillary constituents within amyloid deposits is inflammatory demyelinating polyneuropathy. Auto-
the basis for specific imaging (SAP scintigraphy) and nomic neuropathy causes impotence as an early
novel therapeutic approaches (targeting GAGs26 or symptom in men, which is followed by postural
amyloid-associated SAP27). hypotension, early satiety, and diarrhoea or constipation
(or both). Other than amyloidosis and severe diabetic
Clinical features of amyloidosis neuropathy, diseases that cause a combination of
The potential for amyloid deposits to affect almost any progressive sensory motor peripheral neuropathy and
organ system means that the clinical features of systemic autonomic neuropathy are rare. Cranial neuropathy
amyloidosis are diverse, and they are rarely specific to occurs in hereditary gelsolin (AGel) amyloidosis in
one type of amyloidosis, which leads to difficulties and association with corneal lattice dystrophy and cutis
delays in diagnosis. Table 1 details features of the laxa. About a fifth of all patients with systemic AL
common types of amyloidosis. Clinical features that are amyloidosis have peripheral neuropathy at presentation,
virtually pathognomonic of AL amyloidosis include a but isolated neuropathy in the absence of other organ
combination of macroglossia and periorbital purpura involvement is uncommon in AL amyloidosis.
(figure 1), but these occur in less than a third of all cases. Involvement of soft tissues, apart from carpal tunnel
Isolated periorbital purpura is occasionally seen in other syndrome, is almost unique to AL amyloidosis.
types of amyloidosis. Macroglossia, muscular pseudohypertrophy, enlargement
Cardiac involvement is the leading cause of morbidity of the salivary glands, and submandibular soft-tissue
and mortality in amyloidosis.28 It occurs in about 50% of infiltration are common. Carpal tunnel syndrome is a
patients with AL amyloidosis,29 is a dominant feature in common early symptom in wild-type and hereditary
patients with wild-type and variant ATTR amyloidosis ATTR amyloidosis, and deposition of wild-type TTR
(although it is rare in patients with Val30Met-associated amyloid is found in about a third of elderly people
disease30), and can be a prominent feature in hereditary undergoing carpal tunnel decompression.37 A history of
AApoA1 amyloidosis, but it is very rare in AA carpal tunnel syndrome predating unexplained symptoms
amyloidosis.31 Amyloid deposition in the heart typically of heart failure in elderly patients should prompt
presents as restrictive cardiomyopathy, often with suspicion of cardiac ATTR amyloidosis.
disproportionate signs of right ventricular failure Localised AL amyloidosis is associated with in-situ
(oedema, raised jugular venous pressure, and production of amyloidogenic light chains by clonal
congestive hepatomegaly), while low cardiac output and B cells in the affected tissue. Common sites include the
hypotension are features of advanced disease. Patients respiratory tract, bladder, eyelids, and skin. This form of
with AL amyloidosis are often more symptomatic than amyloidosis is an indolent disease that almost never
patients with other types of amyloidosis given an evolves systemically, but it can nevertheless have serious
apparently similar degree of amyloid deposition in the consequences (ie, the mass lesion can occupy space in a
heart, which supports in-vitro evidence of myocardial critical area of the body). Local surgical measures to
cell toxicity of amyloidogenic light chains in this control symptoms are usually appropriate, and radio-
subtype.32,33 therapy can have a role in selected cases.38
The kidneys are the organs most commonly involved in
AL, AA, fibrinogen A α-chain (AFib), ALect2, and AApoA1 Diagnosis
amyloidoses. Albuminuria, which often progresses to A stepwise approach to diagnosis and staging of
nephrotic syndrome, is typical, but renal dysfunction amyloidosis is critical and involves confirmation of
might remain asymptomatic until it is very advanced. amyloid deposition, identification of fibril type,
AFib amyloidosis, which results from mutations in the assessment of the underlying amyloidogenic disorder,
fibrinogen A α chain gene, is the most common hereditary and evaluation of the extent and severity of amyloidotic
renal amyloidosis in the UK.34 Proteinuria or renal organ involvement. Serum cardiac biomarkers are an
dysfunction is a characteristic feature of AA amyloidosis, important validated method for risk stratification and
and clinical presentation without renal involvement is staging in AL amyloidosis.39
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 3
Seminar
Clinical features raising suspicion of amyloidosis
• Peri-orbital purpura
• Macroglossia (A)
• Nail dystrophy (B)
• Monoclonal protein and diastolic heart failure with preserved apical systolic
function and “bulls-eye” on 2D strain imaging (C), thick-walled heart with
low-voltage ECG, monoclonal protein and albuminuria, peripheral and
autonomic neuropathy, and family history
A B C
Baseline tests of organ function Confirmation of diagnosis
• Serum creatinine • Tissue biopsy or abdominal fat
• eGFR aspiration for Congo red stain
• 24 h proteinuria • Fibril typing with IHC, IEM,
• FBC or LCMS
• Liver function tests
• Clotting
• ECG
• NT-proBNP
• Troponin T/I
Suspected AL amyloidosis Cardiac investigations Suspected hereditary amyloidosis Where available (to determine and
• Serum and urine SPE/IFE • Echocardiogram • Appropriate genetic sequencing track whole body amyloid load):
123
• Serum FLC For selected cases: I-SAP scintigraphy
• Bone marrow • Cardiac MRI
aspiration/biopsy • 99mTcDPD/pyrophosphate scan
• Skeletal imaging
Figure 1: Clinical features raising suspicion of amyloidosis and diagnostic approach for a patient with suspected systemic amyloidosis
¹²³I-SAP=123-iodine-labelled serum amyloid P component. 2D=two dimensional. ⁹⁹mTc-DPD=99m-technetium-labelled 3,3-diphosphono-1,2-propanodicarboxylic
acid. AL=amyloid light-chain. ECG=electrocardiography. eGFR=estimated glomerular filtration rate. FBC=full blood count. FLC=free light-chain.
IEM=immunoelectronmicroscopy. IFE=immunofixation electrophoresis. IHC=immunohistochemistry. LCMS=laser capture microscopy followed by mass spectrometry.
MRI=magnetic resonance imaging. NT-proBNP=N-terminal pro-brain natriuretic peptide. SPE=serum protein electrophoresis.
Advanced and irreversible organ dysfunction has often significance (MGUS) with abnormal free light chain ratio
ensued by the time a clinical diagnosis of amyloidosis is of lambda:kappa free light chains should be part of
made, so keeping a high index of suspicion is important standard practice, as an abnormality of either may herald
for early diagnosis. Specific combinations of symptoms development of amyloidosis.
should trigger suspicion for a diagnosis of amyloidosis,
such as nephrotic syndrome and heart failure; peripheral Histological demonstration of amyloid deposits and
and autonomic neuropathy; thick-walled heart failure confirmation of fibril type
with normal or low-voltage electrocardiogram; recurrent Demonstration of characteristic green birefringence
carpal tunnel syndrome; a combination of carpal tunnel under cross-polarised light following Congo red staining
syndrome and heart failure in elderly people; and of biopsied tissue remains the gold standard for
appropriate family history (figure 1). Regular testing for confirming deposition of amyloid (figure 2). Novel
the N-terminal of the prohormone brain natriuretic fluorescent dyes, such as conjugated polymer
peptide (NT-proBNP) and urine sampling for albuminuria pentameric formic thiophene acetic acid (pFTAA), show
in patients with monoclonal gammopathy of uncertain promise for identifying (figure 2) and typing amyloid
4 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Seminar
deposits.40,41 Biopsy of an organ in which amyloid is Congo red stain (bright field) Immunohistochemistry (anti-SAA antibody)
suspected is the most common approach, but there is a
risk of bleeding, so biopsy should be considered only if
other methods do not reveal amyloid deposits.
Microscopic amyloid deposits are very widespread in
systemic forms of the disease, and abdominal fat
aspiration is a simple and innocuous high-yield
alternative to target organ biopsy. A negative fat aspirate
does not exclude amyloidosis, and biopsy of rectal or
labial salivary glands are alternatives with reasonable
diagnostic sensitivity.42
Confirmation of the type of amyloid fibril is crucial,
since this will guide therapy. Immunohistochemistry
remains the most widely available method for fibril
typing.43 Its diagnostic value is very high in AA
amyloidosis (figure 2) and in most cases of ATTR
amyloidosis, but the results are not definitive in many
patients with AL amyloidosis (appendix). Immuno-
electron microscopy with gold-labelled anti-fibril protein
antibodies is very sensitive but of limited availability.44
Congo red stain (cross polarised light) pTFAA stain (fluorescent microscopy)
The proteomic method of mass spectrometric analysis
of amyloidotic material (appendix) is the new gold
standard for fibril typing.18,19 This method involves laser
microdissection and capture of Congo red-stained
deposits from a fixed tissue section using a laser capture
microscope or the direct use of fat aspirate samples
followed by tryptic digestion and tandem mass
spectrometry. Computer algorithms then match the
peptides to a protein reference database. This is
technically challenging and requires validation in each
laboratory before ‘routine’ clinical use. Gene sequencing
must be performed when there is any suspicion of
hereditary amyloidosis. An online database provides an
updated list of amyloidogenic mutations and an outline
of associated phenotypes in hereditary amyloidosis.
Assessment of the underlying disorder
Assessment or identification of the underlying disorder
is the next step in patients with AL and AA amyloidosis.
A combination of serum and urine testing with Figure 2: Congo red staining of tissue biopsy, the gold standard for confirming amyloid deposition
immunofixation electrophoresis (IFE) and measurement Top and bottom left panels show Congo red staining (top, bright field) and typical apple green birefringence
of free light chain (FLC) in serum is required to detect (bottom) under cross-polarised light in a patient with AA amyloidosis. Diagnosis was confirmed by
immunohistochemical staining by antibodies to serum amyloid A (SAA; top right panel). Bottom right panel
the often very subtle monoclonal protein underlying AL shows bright green fluorescence exhibited by renal amyloid deposits using the novel luminescent conjugated
amyloidosis45 and will be informative in more than polymer pentameric formic thiophene acetic acid (pFTAA) in a patient with AL amyloidosis (pFTAA image
95% of cases.46 By contrast with the light chain isotype reproduced courtesy of Professor Gunella Westermark, Sweden).
in MGUS and myeloma, AL fibrils are four times more
often lambda than kappa light chains. The amount of Assessing the extent of disease—role of imaging See Online for appendix
plasma cell infiltrate in the bone marrow is usually very Assessment of amyloid-related end-organ damage
modest (median 10%).47,48 Genetic studies of bone informs prognosis, the need for supportive care, and For the database of
marrow plasma cells and investigations to rule out formulation of a risk-adapted treatment plan. SAP amyloidogenic mutations see
http:/www.
myeloma, including bone imaging, should be done scintigraphy, the only specific imaging method available, amyloidosismutations.com
at baseline.49 In patients with AA amyloidosis, enables the amyloid load in the liver, kidneys, spleen,
investigations are needed to identify the underlying adrenal glands, bones, and various other sites to be
inflammatory disorder, including sequencing of the ascertained and monitored serially (figure 3).50
genes that cause familial periodic fever syndromes Scintigraphy with SAP shows that the quantity of amyloid
in the 10–20% in whom the cause of AA amyloidosis present in a given organ correlates poorly with the level
is obscure. of organ dysfunction and that regression of amyloid
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 5
Seminar
deposits occurs at different rates in different organs cardiac ATTR do not have reduced QRS voltages on
(figure 3). Dual modality ¹²³I-labelled SAP single-photon electrocardiography but rather have an inappropriately
emission computerised tomography (SPECT) facilitates “normal” voltage on ECG for the degree of left
accurate localisation of deposits of amyloid in soft tissue. ventricular wall thickening. Two-dimensional (2D)
This technique is unable to image amyloid in the moving strain mapping shows relative preservation of apical
heart and is only available at the NAC in London and the function, which can be an early clue to amyloidosis,
University of Groningen in the Netherlands. since it gives rise to a “bulls-eye” pattern when the
Echocardiography, including tissue Doppler and segmental strain is plotted (figure 1D), which is rare in
strain imaging, is important to document baseline other cardiomyopathies.
cardiac structure and function.28,51 Echocardiography Cardiac MRI has been an important imaging
shows “pan-cardiac” thickening (increased thickness of development, since it is easily available and has high
left and right ventricular free walls, septum, valves, and specificity for diagnosis of cardiac amyloidosis.53,54
intra-atrial septum, with dilatation of the atria), which Amyloid cardiomyopathy demonstrates a typical pattern
is rare in other infiltrative cardiomyopathies. A of late subendocardial or diffuse enhancement after
thick-walled heart on an echocardiogram but with a gadolinium contrast injection (figure 4).39,40 Cardiac MRI
normal or low voltage electrocardiogram remains a can give accurate anatomical information, including the
diagnostic hallmark of amyloidosis, with high sensitivity wall thickness and left ventricular mass. Equilibrium
(72–79%) and specificity (91–100%).52 It is noteworthy, contrast MRI (Eq-CMR) uses a low-dose gadolinium
however, that a substantial proportion of patients with infusion for contrast and allows accurate quantification
of the myocardial interstitial volume fraction, which is
Pre-treatment 3 years after treatment greatly expanded in amyloidosis,55 therefore providing a
novel tool to monitor amyloid load in the heart.
The bone-seeking radionuclide tracers ⁹⁹m-technetium-
3,3-diphosphono-1,2-propanodicarboxylic acid (⁹⁹mTc-DPD)
and ⁹⁹mTc-pyrophosphate (⁹⁹mTc-PYP) also seem to localise
with remarkable sensitivity in cardiac ATTR deposits.56–61
Scans with ⁹⁹mTc-DPD seem to show asymptomatic ATTR
cardiac deposits before any other imaging modality.62
Uptake into other types of cardiac amyloid may occur,
but this is usually minor (figure 4).60 Scintigraphy with
⁹⁹mTc-DPD/PYP may have a role in screening for cardiac
ATTR amyloidosis in elderly patients with cardiac failure
of unclear aetiology and in differentiating cardiac ATTR
from other types of cardiac amyloidosis.
Scintigraphy with ¹²³I-labelled meta-iodobenzyl-
guanidine (¹²³I-mIBG) can provide information on cardiac
autonomic neuropathy, but its place in clinical practice
remains to be established.63,64 PET tracers developed to
image amyloid in the brain of patients with Alzheimer’s
disease have potential value for systemic amyloidosis, and
¹¹C-labelled Pittsburgh Compound-B (¹¹C-PiB)65 and
florbetapir66 have shown promise in imaging cardiac
amyloidosis, particularly the latter (an imaging agent
licensed for Alzheimer’s disease), which might show
different patterns in AL and ATTR amyloidoses.
Risk stratification and staging
The prognosis of patients with amyloidosis is influenced
by the extent of organ damage, especially by cardiac
involvement in those with AL amyloidosis. Risk
stratification in patients with AL amyloidosis is critical for
optimum selection of therapy. Various variables are
Figure 3: ¹²³Iodine-labelled serum amyloid P component scintigraphy powerful clinical indicators of poor outcome, including
Whole body image (A) shows marked uptake in the liver, with attenuation of the normal blood pool signal in a poor performance status, severe postural hypotension,
patient with systemic AL amyloidosis with liver and renal involvement. The patient was treated with combination
New York Heart Association functional class 3 or higher,
chemotherapy and achieved complete clonal response. A scan after 3 years (B) shows near complete regression of
amyloid deposits from the liver, with return of the normal blood pool signal. Uptake is seen in the kidneys (arrows), and low systolic blood pressure (SBP; <100 mm Hg).67
which were previously obscured by uptake in the enlarged amyloidotic liver. AL=amyloid light-chain. Increased concentrations in serum of the cardiac
6 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Seminar
A B C
Figure 4: ⁹⁹mTc-3,3-diphosphono-1,2-propanodicarboxylic acid (⁹⁹mTc-DPD) scintigraphy (A, B and C) and cardiac MRI (D)
(A) Scan of a patient with systemic AL amyloidosis with cardiac involvement, showing low-grade cardiac uptake of ⁹⁹mTc DPD in the heart. (B) Scan of a patient with
senile cardiac amyloidosis due to deposition of wild-type variant transthretin amyloid (ATTRwt), showing striking uptake of ⁹⁹mTc-DPD in the heart, with marked
reduction in the bone signal—a pattern characteristic of cardiac TTR amyloidosis. (C) ⁹⁹mTc DPD-gated SPECT image of the patient shown in (B), demonstrating
greater involvement of the septum and base of the heart, with relative sparing of the apex of the left ventricle, which is in keeping with sparing of apical cardiac
function on echocardiography. (D) Cardiac MRI scan of a patient with AL amyloidosis, showing typical subendocardial ring of enhancement after gadolinium contrast
injection. AL=amyloid light-chain. ATTRwt=wild-type variant transthretin amyloid. SPECT=single-photon emission computed tomography. TTR=transthyretin.
biomarkers NT-proBNP (>332 ng/l), cardiac troponin-T are often poorly tolerated because of impaired organ
(cTNT) and cardiac troponin-I (cTNI) (cTNT function. Orthotropic liver transplantation to remove or
>0·035 ng/mL, cTnI >0·1 ng/mL, or high-sensitivity diminish the hepatic source of genetically variant
troponin >0·077 ng/mL)68 provide the basis of the amyloidogenic proteins has a role in selected patients with
well-validated Mayo Clinic staging system.39 Those in hereditary ATTR, AApoAI, and AFib amyloidoses.
whom both biomarkers are abnormal (stage III) have Assessment of response in patients with amyloidosis
median survival of 7–8 months.39,68,69 Patients with comprises dual evaluation of a treatment’s suppression
NT-proBNP >8500 ng/L (especially in the presence of SBP of supply of amyloid precursor protein and its effects on
<100 mm Hg) had median survival of 3 months in a the function of the affected amyloidotic organs, which is
historical series70 and can be called stage IIIb. Patients with substantially dependent on the former. Concentrations
higher concentrations of FLC at diagnosis also have of SAA lower than 4 mg/L are associated with best
poorer outcomes,71,72 as do patients with bone marrow outcomes in AA amyloidosis. Consensus criteria to
plasmacytosis greater than 10% at presentation.73 A staging define haematological and organ responses (which are
system for renal involvement in AL has been published.74 strong predictors of survival) in AL amyloidosis have
been published.75,76 Patients who achieve a complete
Management response (no detectable monoclonal immunoglobulin
Principles of treatment [M] band in serum or urine by immunofixation and
A reduction in the supply of precursor proteins for amyloid normal serum free light chains) or very good partial
fibril underpins all current treatment for amyloidosis, response (dFLC <40 mg/:) have the best outcomes.76 A
although this is not yet possible for some types. Various partial response—that is, a reduction of 50% or more in
drugs can be very effective in AL and AA amyloidoses but concentrations of aberrant FLC—is no longer considered
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 7
Seminar
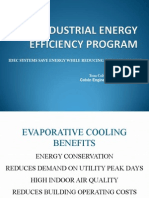
patients with AL amyloidosis.77 The reduced functional
100 2008–12 median not reached; estimated 4 year OS 50%
2004–07 median 2·2 years; estimated 4 year OS 38% reserve of amyloidotic organs and poor performance
2001–03 median 1·7 years; estimated 4 year OS 34% status results in much greater treatment toxicity in AL
1996–2000 median 1·4 years; estimated 4 year OS 28%
≤1995 median 1·5 years; estimated 4 year OS 28% amyloidosis, so a risk-adapted approach to treatment is
80
critical. Frequent assessments of haematological
response are needed, with a view to changing treatment
rapidly (as early as three cycles). Median survival in
60
patients with AL amyloidosis has nearly doubled over
Survival (%)
the past decade, but nearly one-quarter of all patients
still die of disease-related complications within a few
40
months of diagnosis (figure 5). With successful
treatment, such as autologous stem cell transplant
(ASCT),78 outcomes in AL amyloidosis are superior to
20
those in myeloma,78 presumably because of the smaller
clonal burden79 and the lack of high-risk cytogenetics in
AL amyloidosis.80 Table 2 details treatment regimens and
0
0 5 10 15 outcomes for AL amyloidosis.
Time (years) Patients with AL amyloidosis can be classified as at low,
intermediate, or high risk. Low-risk patients are those
Figure 5: Kaplan–Meier survival curve showing improvement over time in overall survival of patients with
systemic AL amyloidosis seen at the National Amyloidosis Centre in the UK (n=3486)
with excellent performance status; NT-proBNP lower
Estimated 4-year survival has improved from 28% for patients diagnosed in the early part of the past decade to than 5000 ng/mL; cTNT lower than 0·06 ng/mL, no
nearly 50% for patients diagnosed in the past four years (log rank p values: p=0·008 for 2008–12 vs 2004–07; significant pleural effusions, autonomic neuropathy, or
p=0·03 for 2004–07 vs 2001–03; p=0·29 for 2001–03 vs 1996–2000; p=0·64 for 1996–2000 vs up to 1995). This amyloid-related gastrointestinal bleeding; and good renal
improvement in survival coincides with the availability of novel agents such as thalidomide and bortezomib for the
treatment of AL amyloidosis. However, over the past two decades, no improvement has been seen in early
function. Such patients, who represent about 15–20%
mortality in the first few months after diagnosis of AL amyloidosis. AL=amyloid light chain. OS=overall survival. of all cases, are potential candidates for high-dose
melphalan followed by ASCT.94–96 Although a small
satisfactory in many patients.76 A decrease in serum randomised trial failed to prove superiority of ASCT over
levels of NT-proBNP of 30% or 300 ng/L is a robust chemotherapy,86 data from various non-randomised
measure of cardiac response and a powerful guide to studies show excellent clonal response rates—that is,
adequacy of treatment in AL amyloidosis.68 very good partial light chain responses (VGPR) in 56% of
Supportive care, with multidisciplinary involvement, is patients,97 44% of whom achieved a complete clonal
crucial to control symptoms, maintain organ function, response98 that translated to improvement in organ
and manage treatment toxic effects. Supportive measures function in three-quarters of such patients, progression
include meticulous control of blood pressure in patients free survival (PFS) longer than 8 years (an endpoint
with renal amyloidosis, strict fluid management in those not yet reported with a non-transplant approach), and
with cardiac amyloidosis (including judicious use of median overall survival longer than 10 years.87 Autologous
diuretics and avoidance of angiotensin-converting stem cell transplantation can be undertaken safely given
enzyme inhibitors in patients with low blood pressure), strict selection of patients, particularly using cardiac
use of α-agonists such as midodrine in patients with biomarkers with recent treatment-related mortality lower
autonomic neuropathy that is causing severe postural than 10%.94,95 A strategy in which bortezomib is used for
hypotension, and adequate nutritional support. induction or consolidation seems to achieve the desired
VGPR target in >90% of treated patients.99,100 Although
Treatment of AL amyloidosis early response rates of this order are now possible using
Treatment of AL amyloidosis comprises chemotherapy combinations of novel drugs, long-term outcomes
that targets the underlying clonal plasma cell dyscrasia, remain to be proven.87 Autologous stem cell trans-
with the aim of rapidly reducing production of plantation is best undertaken in centres with experience
amyloidogenic light chains to limit progressive damage in amyloidosis.
to amyloidotic organs.75 The plasma cell dyscrasias that Most patients with AL amyloidosis are at intermediate
underlie AL amyloidosis can range from benign MGUS risk and are treated with combination chemotherapy
(which does not otherwise need treatment) to frankly regimens. The wide choice of treatment regimens
malignant plasma cell proliferation (eg multiple without randomised data comparing their efficacy
myeloma). Most patients with AL amyloidosis have makes selection of the best treatment for these patients
plasma cell dyscrasia at the MGUS end of the spectrum, difficult; with different paths followed in different
but 10–15% have truly comorbid multiple myeloma. countries it is crucial to enrol patients with this rare
Over the past decade, the remarkable progress in drugs disease into clinical trials. Regimens such as oral
for multiple myeloma, which have been adapted for AL melphalan with dexamethasone (MDex) and a
amyloidosis, has translated into improved treatments for risk-adapted strategy involving a combination of
8 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Seminar
Number of Response (%) Median progression- Median overall
patients free survival (years*) survival (years)
Clonal, % of Organ
responders (%
with complete
response)
Standard chemotherapy
Oral melphalan–dexamethasone81,82 46 67% (33%) 48% 3·8 5·1
Cyclophosphamide–thalidomide–dexamethasone83 75 74% (21%) 27% 1·7 3·4
Bortezomib84 70 69% (38%) 29% At 12 months: 75% 84%
Lenalidomide–dexamethasone85 22 41% (–) 23% 1·6 ··
ASCT
ASCT86 37 67% (41%) 45% 2·7 1·8
ASCT87 421 ·· (43%) 53% 3·4 8·4
Risk-adapted ASCT (followed by bortezomib consolidation)88 40 79% (58%) 70% At 2 years: 69% At 2 years: 82%
Novel chemotherapy combinations
Cyclophosphamide–bortezomib–dexamethasone89 43 81% (65%) 46% At 2 years: 53% At 2 years: 98%
Cyclophosphamide–lenalidomide–dexamethasone90 35 60% (11%) 31% 2·4 3·1
Melphalan–lenalidomide–dexamethasone91 26 58% (23%) 50% At 2 years: 54% At 2 years: 81%
Pomalidomide–dexamethasone92 33 48% (3%) 15% 1·2 2·3
Ixazomib93 16 42% (8%) ·· ·· ··
*Unless otherwise specified. ··=data not available. ASCT=autologous stem cell transplant.
Table 2: Treatment regimens for patients with AL amyloidosis
cyclophosphamide, thalidomide, and dexamethasone pomalidomide are useful for patients with relapsed or
(CTDa) were accepted as the standard of care for AL refractory disease after previous proteasome inhibitors and
amyloidosis81 and are associated with haematological for those presenting with neuropathic disease.
responses in 65–75% patients within 3–4 months of No particular regimen has yet been shown to be
treatment.81,83 Proteasome inhibitors are a new class of superior or to reduce early cardiac deaths in very
drugs for myeloma,101 and the plasma cells of patients high-risk (stage IIIb) patients.70 The need for a rapid
with AL amyloidosis seem to show exquisite sensitivity response often leads to selection of a bortezomib-based
to them.102 The use of bortezomib—the first such agent regimen, but improvements in outcomes with
in clinical practice—as a single agent or augmented by bortezomib in this patient population remain to be
dexamethasone produces high clonal response proven.110 Chemotherapy should be started at low
rates in patients with AL as initial treatment and after doses, and the patient should be kept under very close
relapse.103–105 A combination of bortezomib with monitoring (especially cardiac monitoring) because of
cyclophosphamide and dexamethasone (CyBorD) gives the high risk of destabilising organ function with drug
very high response rates >90% for patients treated toxic effects. Improved outcomes in this subset are a
upfront, with 60% achieving complete response or major unmet medical need.
VGPR.89,106 This treatment therefore offers the hope of
very rapid and deep clonal responses and improvements Treatment of AA amyloidosis
in function of organs, including the heart, and it is the Reduction of the SAA production with treatment of
front-line treatment of choice in most intermediate-risk the underlying inflammatory disorder is the key to
patients. An international randomised phase 3 trial is management of AA amyloidosis.31 Choice of therapy
comparing the addition of bortezomib to standard depends on the nature of the underlying problem.
MDex, and results of studies with newer proteasome Antimicrobial therapy is needed for patients with AA
inhibitors such as ixazomib (which is administered amyloidosis in whom infection is the main problem—
orally) and carfilzomib (which has reduced neurotoxic for example, bronchiectasis or tuberculosis. Colchicine
effects) are awaited with interest. is a highly effective treatment for familial Mediterranean
Lenalidomide and pomalidomide are newer immuno- fever.111,112 Biological therapies, predominantly tumour
modulatory agents with better toxicity profiles than necrosis factor (TNF) inhibitors such as etanercept,
thalidomide. Good responses are reported with both infliximab and adalumimab, have improved outcomes
agents,85,92,107 especially when combined with alkylators,91,108,109 in patients with rheumatological disorders.113,114
but complete responses are lower than those reported Interleukin-1 blockade with anakinra or canakinumab
with bortezomib-based therapies. Lenalidomide and is highly effective in auto-inflammatory disorders,
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 9
Seminar
including TNF-related periodic fever syndrome amyloidosis, and highly selected younger patients have
(TRAPS)115,116 and cryopyrin-associated periodic fever been reported to do very well after cardiac
syndromes (CAPS).117,118 Patients with AA amyloidosis in transplantation.128,129
whom the underlying inflammatory disorder cannot be Hereditary AFib is predominantly a renal disease34 and
characterised might also respond to specific inhibition outcomes after renal transplantation are reasonably
of interleukin (IL) 1 or IL-6. good, with median graft survival of about 6 years, limited
Glycosaminoglycans are a universal constituent of all by recurrent renal deposition of amyloid.34 Liver
amyloid deposits, and inhibition of the interaction transplantation at the same time as kidney transplantation
between GAGs and amyloid fibrils is a promising has been shown to eliminate the amyloidogenic variant
approach to treatment of AA amyloidosis. Eprodisate—a and prevent further deposition of amyloid,130 but the
negatively charged, sulphonated molecule of low procedure-related mortality is high and long-term
molecular weight (with structural similarities to heparan benefits are yet to be shown.131
sulphate)119—is hypothesised to inhibit formation of AA Patients with AApoAI amyloidosis have a variable
amyloid fibrils by interfering with their interaction with disease phenotype depending on the specific mutation.132,133
GAGs.120 In a phase 3, placebo-controlled trial in patients Reported long-term outcomes of liver, kidney, and heart
with AA amyloidosis,25 eprodisate was associated with transplantation have been remarkably good134 despite
half the risk of reduced creatinine clearance; another trial recurrent deposition of amyloid.
is underway to confirm these findings.
Novel therapies for transthyretin amyloidosis
Treatment of hereditary amyloidosis Several very promising therapies are in development for
Treatment of patients with hereditary amyloidosis ATTR amyloidosis. In-vitro studies indicate that the
remains unsatisfactory. The main approach is organ amyloidogenic misfolding of TTR can be inhibited by
transplantation to replace a failing amyloidotic organ. compounds that bind TTR in the plasma to maintain its
When the liver is the major source of the precursor normal soluble native tetrameric structure. Tafamidis, a
protein, this also may be transplanted in order to replace novel TTR stabiliser, has been developed specifically to
the mutant amyloidogenic protein with the normal treat ATTR amyloidosis.135 In a small phase 3 trial,
non-amyloidogenic protein.121 neuropathic disease in patients with Val30Met-related
ATTR amyloidosis progressed at a slower rate over
Organ transplantation for hereditary amyloidosis 18 months with tafamidis than with placebo,136 leading to
Fibrinogen, TTR, and ApoA-I are synthesised mainly marketing approval of the drug by the European Medicines
in the liver. Hence, liver transplantation has a role in Agency. Other stabiliser drugs are also in development.137
patients with amyloidosis resulting from mutations in Diflunisal, a non-steroidal anti-inflammatory drug,
the respective genes. Although organ transplantation can stabilised transthyretin in vitro,138,139 reduced the rate of
be a lifesaving procedure in patients with hereditary neurological progression, and preserved quality of life at
amyloidosis, careful selection and counselling of patients 2 years compared with placebo.140 Diflunisal is a cheaper
are important. Procedure-related morbidity can be high and, on the basis of limited data, an apparently equally
due to amyloidotic organ damage; additional risks efficacious alternative to tafamidis for the treatment of
are associated with long-term immunosuppression, neuropathic ATTR amyloidosis. In-vitro data suggest that
including secondary malignancies and renal impairment. doxycycline and tauro-ursodeoxycholic acid (TUDCA)
Liver transplantation is the treatment of choice in may interfere with the process of TTR fibrillogenesis,
younger patients with hereditary ATTR amyloidosis with a phase 2 trial in Italy reporting stable disease over
associated with the Val30Met variant and early in the 18 months among patients with ATTR-FAP amyloidosis
disease course.122 Liver transplantation can be beneficial treated with a combination of these drugs. In a slowly
in some patients with other TTR mutations, but the near progressive disease with limited recovery of function,
universal presence of cardiac amyloid deposits in such assessment of the real value of any of these agents remains
patients has proved very problematic, as wild-type TTR challenging, and no study has yet compared either of
can still be deposited as amyloid on the pre-existing these strategies.
template of amyloid already present in the heart.123 Transthyretin is almost exclusively synthesised by the
Curiously, although the liver is the site of production of liver, which is the anatomical site most efficiently
TTR, amyloid deposition in patients with ATTR targeted by novel RNA-inhibiting therapies. Two such
amyloidosis does not occur in the liver itself. The liver is approaches are now in clinical development: small
healthy, and healthy livers from patients with hereditary interfering RNA therapy and anti-sense oligonucleotide
ATTR amyloidosis thus have been used as domino grafts therapy.141 Both approaches seem to be highly effective,
for patients with other types of liver disease,124 although reducing levels of ATTR by >80% in healthy volunteers
recipients can develop acquired ATTR amyloidosis.125–127 and patients with ATTR amyloidosis, without major toxic
Cardiac disease is the dominant clinical feature in effects,142 and thus hold great promise for patients with
patients with ATTRwt and V122I-related ATTR ATTR amyloidosis.
10 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Seminar
Enhancing regression by immunotherapeutic 6 Pinney JH, Smith CJ, Taube JB, et al. Systemic amyloidosis in
targeting England: an epidemiological study. Br J Haematol 2013;
161: 525–32.
Interest is growing in developing therapeutic antibodies 7 Hemminki K, Li X, Försti A, Sundquist J, Sundquist K. Incidence
to target amyloid deposits directly. A chimeric antibody, and survival in non-hereditary amyloidosis in Sweden.
Mu11–1F4, reacts with many AL fibrils;143,144 its localisation BMC Public Health 2012; 12: 974.
8 Valleix S, Gillmore JD, Bridoux F, et al. Hereditary systemic
has been studied in patients with PET imaging145 and it amyloidosis due to Asp76Asn variant β2-microglobulin.
is now in phase 1 clinical trials. Another monoclonal N Engl J Med 2012; 366: 2276–83.
antibody, mAb2A4, binds AL/AA fibrils and human AL 9 Wechalekar AD, Gillmore JD, Foard D, et al. 25 years of systemic
amyloidosis. In: Hazenberg PB, ed. International amyloidosis
amyloid extracts,146 leading to regression of amyloid in symposium. Groningen: Netherlands, 2012.
mouse models of AA and AL amyloidosis. This antibody 10 Tanskanen M, Peuralinna T, Polvikoski T, et al. Senile systemic
has been further developed as NEOD001 and has amyloidosis affects 25% of the very aged and associates with genetic
variation in alpha2-macroglobulin and tau: a population-based
recently completed phase 1 trials in systemic amyloidosis autopsy study. Ann Med 2008; 40: 232–39.
in the USA, showing promising improvement in cardiac 11 Benson MD, James S, Scott K, Liepnieks JJ, Kluve-Beckerman B.
biomarkers and proteinuira. Leukocyte chemotactic factor 2: A novel renal amyloid protein.
Serum amyloid P component binds to all amyloid fibrils Kidney Int 2008; 74: 218–22.
12 Murphy C, Wang S, Kestler D, et al. Leukocyte chemotactic factor 2
in vitro and protects them from degradation by phagocytic (LECT2)-associated renal amyloidosis. Amyloid 2011;
cells and proteolytic enzymes.147 We have developed 18 (suppl 1): 223–25.
R-1-[6-[R-2-carboxy-pyrrolidin-1-yl]-6-oxo-hexanoyl] 13 Murphy CL, Wang S, Kestler D, et al. Leukocyte chemotactic factor 2
(LECT2)-associated renal amyloidosis: a case series. Am J Kidney Dis
pyrrolidine-2-carboxylic acid (CPHPC, or GSK2315698), a 2010; 56: 1100–7.
drug that cross-links pairs of SAP molecules in vivo148 and 14 Larsen CP, Walker PD, Weiss DT, Solomon A. Prevalence and
triggers their prompt and virtually complete clearance morphology of leukocyte chemotactic factor 2-associated amyloid in
renal biopsies. Kidney Int 2010; 77: 816–19.
from the blood. Clinical studies indicate that GSK2315698
15 Sousa A, Coelho T, Barros J, Sequeiros J. Genetic epidemiology of
is well tolerated and safe and causes rapid and sustained familial amyloidotic polyneuropathy (FAP)-type I in Póvoa do
depletion of circulating SAP,149 but it leads only to gradual Varzim and Vila do Conde (north of Portugal). Am J Med Genet 1995;
depletion of SAP from amyloid deposits. However, 60: 512–21.
16 Holmgren G, Costa PM, Andersson C, et al. Geographical
antibodies to SAP can then target the SAP remaining on distribution of TTR met30 carriers in northern Sweden:
amyloid deposits, and as SAP is a universal component of discrepancy between carrier frequency and prevalence rate.
amyloid deposits, these antibodies will target all types J Med Genet 1994; 31: 351–54.
17 Hellman U, Alarcon F, Lundgren HE, Suhr OB, Bonaiti-Pellie C,
of amyloid fibril proteins. In a mouse model of AA Plante-Bordeneuve V. Heterogeneity of penetrance in familial
amyloidosis, they produced rapid clearance of amyloid amyloid polyneuropathy, ATTR Val30Met, in the Swedish
deposits by macrophage- and complement-mediated population. Amyloid 2008; 15: 181–6.
18 Reilly MM, Staunton H, Harding AE. Familial amyloid
mechanisms.27 Early results of a phase 1 trial using the polyneuropathy (TTR ala 60) in North West Ireland: a clinical,
combined approach of GSK2315698 and GSK2398852, a genetic, and epidemiological study. J Neurol Neurosurg Psychiatry
monoclonal antibody to SAP, appear to show promising 1995; 59: 45–49.
19 Jacobson DR, Pastore RD, Yaghoubian R, et al. Variant-sequence
results with marked and rapid reduction in liver amyloid transthyretin (isoleucine 122) in late-onset cardiac amyloidosis in
deposits, but data on efficacy in cardiac and renal disease black Americans. N Engl J Med 1997; 336: 466–73.
are awaited.150 20 Sawaya MR, Sambashivan S, Nelson R, et al. Atomic structures of
In summary, amyloidosis is not as rare as perceived, amyloid cross-beta spines reveal varied steric zippers. Nature 2007;
447: 453–57.
should be suspected early by clinicians of all specialties, 21 Bonar L, Cohen AS, Skinner MM. Characterization of the amyloid
and is very treatable, with newer therapies holding fibril as a cross-beta protein. Proc Soc Exp Biol Med 1969;
promise of rapid organ recovery and better survival. 131: 1373–75.
22 Glenner GG, Terry WD. Characterization of amyloid. Annu Rev Med
Contributors 1974; 25: 131–35.
ADW designed the paper, performed the literature search, and wrote the 23 Sunde M, Serpell LC, Bartlam M, Fraser PE, Pepys MB, Blake CC.
paper. JDG and PNH designed and wrote the paper. Common core structure of amyloid fibrils by synchrotron X-ray
diffraction. J Mol Biol 1997; 273: 729–39.
Declaration of interests
ADW has received honoraria from Janssen-Cilag and Celgene. JDG and 24 Pepys MB, Rademacher TW, Amatayakul-Chantler S, et al. Human
serum amyloid P component is an invariant constituent of amyloid
PNH declare no competing interests.
deposits and has a uniquely homogeneous glycostructure.
References Proc Natl Acad Sci USA 1994; 91: 5602–06.
1 Lachmann HJ, Hawkins PN. Systemic amyloidosis. 25 Tan SY, Pepys MB. Amyloidosis. Histopathology 1994; 25: 403–14.
Curr Opin Pharmacol 2006; 6: 214–20. 26 Dember LM, Hawkins PN, Hazenberg BP, et al, and the
2 Merlini G. Systemic amyloidosis: are we moving ahead? Eprodisate for AA Amyloidosis Trial Group. Eprodisate for the
Neth J Med 2004; 62: 104–05. treatment of renal disease in AA amyloidosis. N Engl J Med 2007;
3 Sipe JD, Benson MD, Buxbaum JN, et al. Nomenclature 2014: 356: 2349–60.
Amyloid fibril proteins and clinical classification of the amyloidosis. 27 Bodin K, Ellmerich S, Kahan MC, et al. Antibodies to human serum
Amyloid 2014; 21: 221–24. amyloid P component eliminate visceral amyloid deposits. Nature
4 Esplin BL, Gertz MA. Current trends in diagnosis and management 2010; 468: 93–97.
of cardiac amyloidosis. Curr Probl Cardiol 2013; 38: 53–96. 28 Falk RH. Diagnosis and management of the cardiac amyloidoses.
5 Kyle RA, Linos A, Beard CM, et al. Incidence and natural history of Circulation 2005; 112: 2047–60.
primary systemic amyloidosis in Olmsted County, Minnesota, 1950 29 Merlini G. CyBorD: stellar response rates in AL amyloidosis.
through 1989. Blood 1992; 79: 1817–22. Blood 2012; 119: 4343–45.
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 11
Seminar
30 Pinney JH, Whelan CJ, Petrie A, et al. Senile systemic amyloidosis: 50 Hawkins PN, Lavender JP, Pepys MB. Evaluation of systemic
clinical features at presentation and outcome. amyloidosis by scintigraphy with 123I-labeled serum amyloid P
J Am Heart Assoc 2013; 2: e000098. component. N Engl J Med 1990; 323: 508–13.
31 Lachmann HJ, Goodman HJ, Gilbertson JA, et al. Natural history 51 Buss SJ, Emami M, Mereles D, et al. Longitudinal left ventricular
and outcome in systemic AA amyloidosis. N Engl J Med 2007; function for prediction of survival in systemic light-chain
356: 2361–71. amyloidosis: incremental value compared with clinical and
32 Liao R, Jain M, Teller P, et al. Infusion of light chains from patients biochemical markers. J Am Coll Cardiol 2012; 60: 1067–76.
with cardiac amyloidosis causes diastolic dysfunction in isolated 52 Selvanayagam JB, Hawkins PN, Paul B, Myerson SG, Neubauer S.
mouse hearts. Circulation 2001; 104: 1594–97. Evaluation and management of the cardiac amyloidosis.
33 Shi J, Guan J, Jiang B, et al. Amyloidogenic light chains induce J Am Coll Cardiol 2007; 50: 2101–10.
cardiomyocyte contractile dysfunction and apoptosis via a 53 Maceira AM, Joshi J, Prasad SK, et al. Cardiovascular magnetic
non-canonical p38alpha MAPK pathway. Proc Natl Acad Sci USA resonance in cardiac amyloidosis. Circulation 2005; 111: 186–93.
2010; 107: 4188–93. 54 Mekinian A, Lions C, Leleu X, et al, and the Lille Amyloidosis Study
34 Gillmore JD, Lachmann HJ, Rowczenio D, et al. Diagnosis, Group. Prognosis assessment of cardiac involvement in systemic
pathogenesis, treatment, and prognosis of hereditary fibrinogen A AL amyloidosis by magnetic resonance imaging. Am J Med 2010;
alpha-chain amyloidosis. J Am Soc Nephrol 2009; 20: 444–51. 123: 864–68.
35 Sattianayagam PT, Gibbs SD, Rowczenio D, et al. Hereditary 55 Banypersad SM, Sado DM, Flett AS, et al. Quantification of
lysozyme amyloidosis—phenotypic heterogeneity and the role of myocardial extracellular volume fraction in systemic AL
solid organ transplantation. J Intern Med 2012; 272: 36–44. amyloidosis: an equilibrium contrast cardiovascular magnetic
36 Reilly MM, Staunton H. Peripheral nerve amyloidosis. resonance study. Circ Cardiovasc Imaging 2013; 6: 34–39.
Brain Pathol 1996; 6: 163–77. 56 Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS.
37 Sekijima Y, Uchiyama S, Tojo K, et al. High prevalence of wild-type (99m)Tc-pyrophosphate scintigraphy for differentiating light-chain
transthyretin deposition in patients with idiopathic carpal tunnel cardiac amyloidosis from the transthyretin-related familial and
syndrome: a common cause of carpal tunnel syndrome in the senile cardiac amyloidoses. Circ Cardiovasc Imaging 2013;
elderly. Hum Pathol 2011; 42: 1785–91. 6: 195–201.
38 Gertz MA, Comenzo R, Falk RH, et al. Definition of organ 57 Chen W, Dilsizian V. Molecular imaging of amyloidosis: will the
involvement and treatment response in immunoglobulin light heart be the next target after the brain? Curr Cardiol Rep 2012;
chain amyloidosis (AL): a consensus opinion from the 14: 226–33.
10th International Symposium on Amyloid and Amyloidosis, Tours, 58 Castano A, Bokhari S, Brannagan TH, 3rd, Wynn J, Maurer MS.
France, 18–22 April 2004. Am J Hematol 2005; 79: 319–28. Technetium pyrophosphate myocardial uptake and peripheral
39 Dispenzieri A, Gertz MA, Kyle RA, et al. Serum cardiac troponins neuropathy in a rare variant of familial transthyretin (TTR)
and N-terminal pro-brain natriuretic peptide: a staging system for amyloidosis (Ser23Asn): a case report and literature review.
primary systemic amyloidosis. J Clin Oncol 2004; 22: 3751–57. Amyloid 2012; 19: 41–46.
40 Sipe JD, Benson MD, Buxbaum JN, et al, and the Nomenclature 59 Rapezzi C, Quarta CC, Guidalotti PL, et al. Usefulness and
Committee of the International Society of Amyloidosis. Amyloid limitations of 99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid
fibril protein nomenclature: 2012 recommendations from the scintigraphy in the aetiological diagnosis of amyloidotic
Nomenclature Committee of the International Society of cardiomyopathy. Eur J Nucl Med Mol Imaging 2011; 38: 470–78.
Amyloidosis. Amyloid 2012; 19: 167–70. 60 Rapezzi C, Guidalotti P, Salvi F, Riva L, Perugini E. Usefulness of
41 Nilsson KP, Ikenberg K, Aslund A, et al. Structural typing of 99mTc-DPD scintigraphy in cardiac amyloidosis.
systemic amyloidoses by luminescent-conjugated polymer J Am Coll Cardiol 2008; 51: 1509–10.
spectroscopy. Am J Pathol 2010; 176: 563–74. 61 Perugini E, Guidalotti PL, Salvi F, et al. Noninvasive etiologic
42 Foli A, Palladini G, Caporali R, et al. The role of minor salivary diagnosis of cardiac amyloidosis using 99mTc-3,3-diphosphono-1,2-
gland biopsy in the diagnosis of systemic amyloidosis: results of a propanodicarboxylic acid scintigraphy. J Am Coll Cardiol 2005;
prospective study in 62 patients. Amyloid 2011; 18 (suppl 1): 80–82. 46: 1076–84.
43 Schönland SO, Hegenbart U, Bochtler T, et al. 62 Hutt DF, Quigley AM, Page J, et al. Utility and limitations of
Immunohistochemistry in the classification of systemic forms of 3,3-diphosphono-1,2-propanodicarboxylic acid scintigraphy in
amyloidosis: a systematic investigation of 117 patients. Blood 2012; systemic amyloidosis. Eur Heart J Cardiovasc Imaging 2014;
119: 488–93. 15: 1289–98.
44 Arbustini E, Morbini P, Verga L, et al. Light and electron 63 Hongo M, Urushibata K, Kai R, et al. Iodine-123
microscopy immunohistochemical characterization of amyloid metaiodobenzylguanidine scintigraphic analysis of myocardial
deposits. Amyloid 1997; 4: 157–70. sympathetic innervation in patients with AL (primary) amyloidosis.
45 Palladini G, Russo P, Bosoni T, et al. Identification of amyloidogenic Am Heart J 2002; 144: 122–29.
light chains requires the combination of serum-free light chain 64 Lekakis J, Dimopoulos MA, Prassopoulos V, et al. Myocardial
assay with immunofixation of serum and urine. Clin Chem 2009; adrenergic denervation in patients with primary (AL) amyloidosis.
55: 499–504. Amyloid 2003; 10: 117–20.
46 Lachmann HJ, Gallimore R, Gillmore JD, et al. Outcome in 65 Antoni G, Lubberink M, Estrada S, et al. In vivo visualization of
systemic AL amyloidosis in relation to changes in concentration of amyloid deposits in the heart with 11C-PIB and PET.
circulating free immunoglobulin light chains following J Nucl Med 2013; 54: 213–20.
chemotherapy. Br J Haematol 2003; 122: 78–84. 66 Dorbala S, Vangala D, Semer J, et al. Imaging cardiac amyloidosis:
47 Deshmukh M, Elderfield K, Rahemtulla A, Naresh KN. a pilot study using ¹⁸F-florbetapir positron emission tomography.
Immunophenotype of neoplastic plasma cells in AL amyloidosis. Eur J Nucl Med Mol Imaging 2014; 41: 1652–62.
J Clin Pathol 2009; 62: 724–30. 67 Wechalekar A, Schonland SO, Kastritis E, et al. European
48 Paiva B, Vidriales MB, Pérez JJ, et al, the GEM (Grupo Español de collaborative study of treatment outcomes in 347 patients with
MM) Cooperative Study Ggroup, and the PETHEMA (Programa systemic AL amyloidosis with Mayo stage III disease. Blood 2011;
para el Estudio de la Terapéutica en Hemopatías Malignas) 118: 995.
Cooperative Study Group. Multiparameter flow cytometry 68 Palladini G, Barassi A, Klersy C, et al. The combination of
quantification of bone marrow plasma cells at diagnosis provides high-sensitivity cardiac troponin T (hs-cTnT) at presentation and
more prognostic information than morphological assessment in changes in N-terminal natriuretic peptide type B (NT-proBNP) after
myeloma patients. Haematologica 2009; 94: 1599–602. chemotherapy best predicts survival in AL amyloidosis. Blood 2010;
49 Kyle RA, Durie BG, Rajkumar SV, et al. Monoclonal gammopathy of 116: 3426–30.
undetermined significance (MGUS) and smoldering 69 Kristen AV, Giannitsis E, Lehrke S, et al. Assessment of disease
(asymptomatic) multiple myeloma: IMWG consensus perspectives severity and outcome in patients with systemic light-chain
risk factors for progression and guidelines for monitoring and amyloidosis by the high-sensitivity troponin T assay. Blood 2010;
management. Leukemia 2010; 24: 1121–27. 116: 2455–61.
12 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Seminar
70 Wechalekar AD, Schonland SO, Kastritis E, et al. A European 90 Kumar SK, Hayman SR, Buadi FK, et al. Lenalidomide,
collaborative study of treatment outcomes in 346 patients with cyclophosphamide, and dexamethasone (CRd) for light-chain
cardiac stage III AL amyloidosis. Blood 2013; 121: 3420–27. amyloidosis: long-term results from a phase 2 trial. Blood 2012;
71 Dispenzieri A, Lacy MQ, Katzmann JA, et al. Absolute values of 119: 4860–67.
immunoglobulin free light chains are prognostic in patients with 91 Moreau P, Jaccard A, Benboubker L, et al. Lenalidomide in
primary systemic amyloidosis undergoing peripheral blood stem combination with melphalan and dexamethasone in patients with
cell transplantation. Blood 2006; 107: 3378–83. newly diagnosed AL amyloidosis: a multicenter phase 1/2
72 Wechalekar A, Wassef N, Lachmann H, et al. High early mortality dose-escalation study. Blood 2010; 116: 4777–82.
and poor outcomes for patients with AL amyloidosis presenting 92 Dispenzieri A, Buadi F, Laumann K, et al. Activity of pomalidomide
with high serum free light chains - a new risk stratification model. in patients with immunoglobulin light-chain amyloidosis.
Haematologica 2009; 94: 222. Blood 2012; 119: 5397–404.
73 Kourelis TV, Kumar SK, Gertz MA, et al. Coexistent multiple 93 Merlini G, Sanchorawala V, Zonder JA, et al. MLN9708, a novel,
myeloma or increased bone marrow plasma cells define equally investigational oral proteasome inhibitor, in patients with relapsed
high-risk populations in patients with immunoglobulin light chain or refractory light-chain amyloidosis (AL): results of a phase 1 study.
amyloidosis. J Clin Oncol 2013; 31: 4319–24. Blood 2012; 120: 731 (abstr).
74 Palladini G, Hegenbart U, Milani P, et al. A staging system for renal 94 Gertz MA, Lacy MQ, Dispenzieri A, et al. Trends in day 100 and
outcome and early markers of renal response to chemotherapy in 2-year survival after auto-SCT for AL amyloidosis: outcomes before
AL amyloidosis. Blood 2014; 124: 2325–32. and after 2006. Bone Marrow Transplant 2011; 46: 970–75.
75 Comenzo RL, Reece D, Palladini G, et al. Consensus guidelines for 95 Gertz MA, Lacy MQ, Dispenzieri A, et al. Refinement in patient
the conduct and reporting of clinical trials in systemic light-chain selection to reduce treatment-related mortality from SCT in
amyloidosis. Leukemia 2012; 26: 2317–25. amyloidosis. Bone Marrow Transplant 2013; 48: 557–61.
76 Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for 96 Comenzo RL, Gertz MA. Autologous stem cell transplantation for
response to treatment in immunoglobulin light chain amyloidosis primary systemic amyloidosis. Blood 2002; 99: 4276–82.
based on free light chain measurement and cardiac biomarkers: 97 Sanchorawala V, Seldin DC, Magnani B, Skinner M, Wright DG.
impact on survival outcomes. J Clin Oncol 2012; 30: 4541–49. Serum free light-chain responses after high-dose intravenous
77 Gertz MA, Dispenzieri A. Immunoglobulin light-chain amyloidosis: melphalan and autologous stem cell transplantation for AL
growing recognition, new approaches to therapy, active clinical (primary) amyloidosis. Bone Marrow Transplant 2005; 36: 597–600.
trials. Oncology 2012; 26: 152–61. 98 Skinner M, Sanchorawala V, Seldin DC, et al. High-dose melphalan
78 Dispenzieri A, Seenithamby K, Lacy MQ, et al. Patients with and autologous stem-cell transplantation in patients with AL
immunoglobulin light chain amyloidosis undergoing autologous amyloidosis: an 8-year study. Ann Intern Med 2004; 140: 85–93.
stem cell transplantation have superior outcomes compared with 99 Landau H, Hassoun H, Rosenzweig MA, et al. Bortezomib and
patients with multiple myeloma: a retrospective review from a dexamethasone consolidation following risk-adapted melphalan and
tertiary referral center. Bone Marrow Transplant 2013; 48: 1302–07. stem cell transplantation for patients with newly diagnosed
79 Bochtler T, Hegenbart U, Heiss C, et al. Hyperdiploidy is less light-chain amyloidosis. Leukemia 2013; 27: 823–28.
frequent in AL amyloidosis compared with monoclonal 100 Sanchorawala V, Brauneis D, Shelton AC, et al. Induction therapy
gammopathy of undetermined significance and inversely associated with bortezomib followed by bortezomib-high dose melphalan and
with translocation t(11;14). Blood 2011; 117: 3809–15. stem cell transplantation for AL amyloidosis: results of a
80 Gertz MA, Greipp PR, Kyle RA. Classification of amyloidosis by the prospective clinical trial. Biol Blood Marrow Transplant 2015;
detection of clonal excess of plasma cells in the bone marrow. published online April 6. DOI:10.1016/j.bbmt.2015.04.001.
J Lab Clin Med 1991; 118: 33–39. 101 Richardson PG, Barlogie B, Berenson J, et al. A phase 2 study of
81 Palladini G, Perfetti V, Obici L, et al. Association of melphalan bortezomib in relapsed, refractory myeloma. N Engl J Med 2003;
and high-dose dexamethasone is effective and well tolerated in 348: 2609–17.
patients with AL (primary) amyloidosis who are ineligible for 102 Dimopoulos MA, Kastritis E. Bortezomib for AL amyloidosis:
stem cell transplantation. Blood 2004; 103: 2936–38. moving forward. Blood 2011; 118: 827–28.
82 Palladini G, Russo P, Nuvolone M, et al. Treatment with oral 103 Reece DE, Sanchorawala V, Hegenbart U, et al, and the VELCADE
melphalan plus dexamethasone produces long-term remissions in CAN2007 Study Group. Weekly and twice-weekly bortezomib in
AL amyloidosis. Blood 2007; 110: 787–88. patients with systemic AL amyloidosis: results of a phase 1
83 Wechalekar AD, Goodman HJB, Lachmann HJ, Offer M, dose-escalation study. Blood 2009; 114: 1489–97.
Hawkins PN, Gillmore JD. Safety and efficacy of risk-adapted 104 Wechalekar AD, Lachmann HJ, Offer M, Hawkins PN,
cyclophosphamide, thalidomide, and dexamethasone in systemic Gillmore JD. Efficacy of bortezomib in systemic AL amyloidosis
AL amyloidosis. Blood 2007; 109: 457–64. with relapsed/refractory clonal disease. Haematologica 2008;
84 Reece DE, Hegenbart U, Sanchorawala V, et al. Efficacy and safety 93: 295–98.
of once-weekly and twice-weekly bortezomib in patients with 105 Kastritis E, Wechalekar AD, Dimopoulos MA, et al. Bortezomib
relapsed systemic AL amyloidosis: results of a phase 1/2 study. with or without dexamethasone in primary systemic (light chain)
Blood 2011; 118: 865–73. amyloidosis. J Clin Oncol 2010; 28: 1031–37.
85 Dispenzieri A, Lacy MQ, Zeldenrust SR, et al. The activity of 106 Mikhael JR, Schuster SR, Jimenez-Zepeda VH, et al.
lenalidomide with or without dexamethasone in patients with Cyclophosphamide-bortezomib-dexamethasone (CyBorD) produces
primary systemic amyloidosis. Blood 2007; 109: 465–70. rapid and complete hematologic response in patients with
86 Jaccard A, Moreau P, Leblond V, et al, and the Myélome Autogreffe AL amyloidosis. Blood 2012; 119: 4391–94.
(MAG) and Intergroupe Francophone du Myélome (IFM) Intergroup. 107 Sanchorawala V, Finn KT, Fennessey S, et al. Durable hematologic
High-dose melphalan versus melphalan plus dexamethasone for AL complete responses can be achieved with lenalidomide in
amyloidosis. N Engl J Med 2007; 357: 1083–93. AL amyloidosis. Blood 2010; 116: 1990–91.
87 Cibeira MT, Sanchorawala V, Seldin DC, et al. Outcome of AL 108 Kastritis E, Terpos E, Roussou M, et al. A phase 1/2 study of
amyloidosis after high-dose melphalan and autologous stem cell lenalidomide with low-dose oral cyclophosphamide and low-dose
transplantation: long-term results in a series of 421 patients. dexamethasone (RdC) in AL amyloidosis. Blood 2012; 119: 5384–90.
Blood 2011; 118: 4346–52. 109 Palladini G, Russo P, Milani P, et al. A phase II trial of
88 Landau H, Hassoun H, Rosenzweig MA, et al. Bortezomib and cyclophosphamide, lenalidomide and dexamethasone in previously
dexamethasone consolidation following risk-adapted melphalan and treated patients with AL amyloidosis. Haematologica 2013;
stem cell transplantation for patients with newly diagnosed light 98: 433–36.
chain amyloidosis. Leukemia 2013; 27: 823–28. 110 Venner CP, Gillmore JD, Sachchithanantham S, et al. A matched
89 Venner CP, Lane T, Foard D, et al. Cyclophosphamide, bortezomib, comparison of cyclophosphamide, bortezomib and dexamethasone
and dexamethasone therapy in AL amyloidosis is associated with (CVD) versus risk-adapted cyclophosphamide, thalidomide and
high clonal response rates and prolonged progression-free survival. dexamethasone (CTD) in AL amyloidosis. Leukemia 2014;
Blood 2012; 119: 4387–90. 8: 2304–10.
www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X 13
Seminar
111 Lane T, Loeffler JM, Rowczenio DM, et al. AA amyloidosis 131 Gillmore JD, Lachmann HJ, Wechalekar A, Hawkins PN.
complicating the hereditary periodic fever syndromes. Hereditary fibrinogen A alpha-chain amyloidosis: clinical
Arthritis Rheum 2013; 65: 1116–21. phenotype and role of liver transplantation. Blood 2010; 115: 4313.
112 Pinney JH, Lachmann HJ. Systemic AA. Systemic AA amyloidosis. 132 Dubrey SW, Comenzo RL. Amyloid diseases of the heart: current
Subcell Biochem 2012; 65: 541–64. and future therapies. Q JM 2012; 105: 617–31.
113 Obici L, Merlini G. AA amyloidosis: basic knowledge, unmet 133 Rowczenio D, Dogan A, Theis JD, et al. Amyloidogenicity and
needs and future treatments. Swiss Med Wkly 2012; 142: w13580. clinical phenotype associated with five novel mutations in
114 Nakamura T, Higashi S, Tomoda K, Tsukano M, Shono M. apolipoprotein A-I. Am J Pathol 2011; 179: 1978–87.
Etanercept can induce resolution of renal deterioration in patients 134 Gillmore JD, Stangou AJ, Lachmann HJ, et al. Organ
with amyloid A amyloidosis secondary to rheumatoid arthritis. transplantation in hereditary apolipoprotein AI amyloidosis.
Clin Rheumatol 2010; 29: 1395–401. Am J Transplant 2006; 6: 2342–7.
115 Pettersson T, Kantonen J, Matikainen S, Repo H. Setting up TRAPS. 135 Johnson SM, Connelly S, Fearns C, Powers ET, Kelly JW. The
Ann Med 2012; 44: 109–18. transthyretin amyloidoses: from delineating the molecular
116 Obici L, Meini A, Cattalini M, et al. Favourable and sustained mechanism of aggregation linked to pathology to a regulatory-
response to anakinra in tumour necrosis factor receptor-associated agency-approved drug. J Mol Biol 2012; 421: 185–203.
periodic syndrome (TRAPS) with or without AA amyloidosis. 136 Coelho T, Maia LF, Martins da Silva A, et al. Tafamidis for
Ann Rheum Dis 2011; 70: 1511–12. transthyretin familial amyloid polyneuropathy: a randomized,
117 Kuemmerle-Deschner JB, Hachulla E, Cartwright R, et al. Two-year controlled trial. Neurology 2012; 79: 785–92.
results from an open-label, multicentre, phase III study evaluating 137 Kolstoe SE, Mangione PP, Bellotti V, et al. Trapping of palindromic
the safety and efficacy of canakinumab in patients with cryopyrin- ligands within native transthyretin prevents amyloid formation.
associated periodic syndrome across different severity phenotypes. Proc Natl Acad Sci USA 2010; 107: 20483–88.
Ann Rheum Dis 2011; 70: 2095–102. 138 Sekijima Y, Dendle MA, Kelly JW. Orally administered diflunisal
118 Lachmann HJ, Kone-Paut I, Kuemmerle-Deschner JB, et al, and the stabilizes transthyretin against dissociation required for
Canakinumab in CAPS Study Group. Use of canakinumab in the amyloidogenesis. Amyloid 2006; 13: 236–49.
cryopyrin-associated periodic syndrome. N Engl J Med 2009; 139 Miller SR, Sekijima Y, Kelly JW. Native state stabilization by
360: 2416–25. NSAIDs inhibits transthyretin amyloidogenesis from the most
119 Kisilevsky R, Szarek WA. Novel glycosaminoglycan precursors as common familial disease variants. Lab Invest 2004; 84: 545–52.
anti-amyloid agents part II. J Mol Neuroscience 2002; 19: 45–50. 140 Berk JL, Suhr OB, Obici L, et al, and the Diflunisal Trial Consortium.
120 Kisilevsky R, Ancsin JB, Szarek WA, Petanceska S. Heparan sulfate Repurposing diflunisal for familial amyloid polyneuropathy:
as a therapeutic target in amyloidogenesis: prospects and possible a randomized clinical trial. JAMA 2013; 310: 2658–67.
complications. Amyloid 2007; 14: 21–32. 141 Adams D. Recent advances in the treatment of familial amyloid
121 Sattianayagam P, Gibbs SD, Pinney JH, et al. The role of liver polyneuropathy. Ther Adv Neurol Disord 2013; 6: 129–39.
transplantation in hereditary non-neuropathic systemic 142 Coelho T, Adams D, Silva A, et al. Safety and efficacy of RNAi
amyloidosis. Gastroenterology 2011; 140: S-963 (abstr). therapy for transthyretin amyloidosis. N Engl J Med 2013;
122 de Carvalho M, Conceicao I, Bentes C, Luis ML. Long-term 369: 819–29.
quantitative evaluation of liver transplantation in familial amyloid 143 Solomon A, Weiss DT, Wall JS. Therapeutic potential of chimeric
polyneuropathy (Portuguese V30M). Amyloid 2002; 9: 126–33. amyloid-reactive monoclonal antibody 11-1F4. Clin Cancer Res 2003;
123 Stangou AJ, Hawkins PN, Heaton ND, et al. Progressive cardiac 9: 3831S–8S.
amyloidosis following liver transplantation for familial amyloid 144 Hrncic R, Wall J, Wolfenbarger DA, et al. Antibody-mediated
polyneuropathy: implications for amyloid fibrillogenesis. resolution of light chain-associated amyloid deposits.
Transplantation 1998; 66: 229–33. Am J Pathol 2000; 157: 1239–46.
124 Ericzon BG, Larsson M, Wilczek HE. Domino liver transplantation: 145 Wall JS, Kennel SJ, Stuckey AC, et al. Radioimmunodetection of
risks and benefits. Transplant Proc 2008; 40: 1130–31. amyloid deposits in patients with AL amyloidosis. Blood 2010;
125 Pradotto L, Franchello A, Milesi A, et al. Amyloid polyneuropathy 116: 2241–44.
following domino liver transplantation. Muscle Nerve 2012; 45: 918–19. 146 Wall JS, Kennel SJ, Williams A, et al. AL amyloid imaging and
126 Antonini TM, Lozeron P, Lacroix C, et al. Reversibility of acquired therapy with a monoclonal antibody to a cryptic epitope on amyloid
amyloid polyneuropathy after liver retransplantation. fibrils. PLoS One 2012; 7: e52686.
Am J Transplant 2013; 13: 2734–8. 147 Tennent GA, Lovat LB, Pepys MB. Serum amyloid P component
127 Abdelfatah MM, Hayman SR, Gertz MA. Domino liver prevents proteolysis of the amyloid fibrils of Alzheimer disease and
transplantation as a cause of acquired familial amyloid systemic amyloidosis. Proc Natl Acad Sci USA 1995; 92: 4299–303.
polyneuropathy. Amyloid 2014; 21: 136–7. 148 Pepys MB, Herbert J, Hutchinson WL, et al. Targeted
128 Hamour IM, Lachmann HJ, Goodman HJ, et al. Heart pharmacological depletion of serum amyloid P component for
transplantation for homozygous familial transthyretin (TTR) V122I treatment of human amyloidosis. Nature 2002; 417: 254–59.
cardiac amyloidosis. Am J Transplant 2008; 8: 1056–9. 149 Gillmore JD, Tennent GA, Hutchinson WL, et al. Sustained
129 Fuchs U, Zittermann A, Suhr O, et al. Heart transplantation in a pharmacological depletion of serum amyloid P component in
68-year-old patient with senile systemic amyloidosis. patients with systemic amyloidosis. Br J Haematol 2010;
Am J Transplant 2005; 5: 1159–62. 148: 760–67.
130 Stangou AJ, Banner NR, Hendry BM, et al. Hereditary fibrinogen A 150 Richards DM, Cookson LM, Berges AC, et al. Therapeutic clearance
alpha-chain amyloidosis: phenotypic characterization of a systemic of amyloid by antibodies to serum amyloid p component.
disease and the role of liver transplantation. Blood 2010; N Engl J Med 2015; 373: 1106–14.
115: 2998–3007.
14 www.thelancet.com Published online December 21, 2015 http://dx.doi.org/10.1016/S0140-6736(15)01274-X
Das könnte Ihnen auch gefallen
- Systemic AL Amyloidosis Current Approaches To DiagDokument12 SeitenSystemic AL Amyloidosis Current Approaches To DiagAnia WagnerNoch keine Bewertungen
- 1 s2.0 S135730391300073X MainDokument3 Seiten1 s2.0 S135730391300073X MainMiguel Angel Santacruz VasquezNoch keine Bewertungen
- Amyloidosis-The Diagnosis and Treatment of An Underdiagnosed DiseaseDokument17 SeitenAmyloidosis-The Diagnosis and Treatment of An Underdiagnosed DiseaseAnia WagnerNoch keine Bewertungen
- Amiloidosis 2Dokument12 SeitenAmiloidosis 2david1086Noch keine Bewertungen
- Updates in Cardiac Amyloidosis. A ReviewDokument14 SeitenUpdates in Cardiac Amyloidosis. A ReviewPuig CozarNoch keine Bewertungen
- Multiple Myeloma-Associated AL Amyloidosis Is A Distinctive Therapeutic Bone Marrow Transplantation 2006Dokument9 SeitenMultiple Myeloma-Associated AL Amyloidosis Is A Distinctive Therapeutic Bone Marrow Transplantation 2006Gustavo MartinezNoch keine Bewertungen
- Amyloidosis PDFDokument8 SeitenAmyloidosis PDFKarthik KoneruNoch keine Bewertungen
- No Laughing Matter: Subacute Degeneration of The Spinal Cord Due To Nitrous Oxide InhalationDokument7 SeitenNo Laughing Matter: Subacute Degeneration of The Spinal Cord Due To Nitrous Oxide InhalationgshjfkNoch keine Bewertungen
- ArticuloDokument21 SeitenArticuloGiovanni EscobarNoch keine Bewertungen
- Amiloidosis. Evaluacion Multimodal JACC 2020Dokument16 SeitenAmiloidosis. Evaluacion Multimodal JACC 2020Guillermo CenturionNoch keine Bewertungen
- Amlreview PDFDokument12 SeitenAmlreview PDFMitaNoch keine Bewertungen
- Imaging Cardiac AmyloidosisDokument16 SeitenImaging Cardiac Amyloidosiskromatin9462Noch keine Bewertungen
- Ditorials Erspectives: David C. Seldin, Vaishali SanchorawalaDokument5 SeitenDitorials Erspectives: David C. Seldin, Vaishali Sanchorawalasalmamaged7619Noch keine Bewertungen
- Clinico - Hematological Analysis of Pancytopenia: A Bone Marrow StudyDokument6 SeitenClinico - Hematological Analysis of Pancytopenia: A Bone Marrow StudySrinath M VNoch keine Bewertungen
- AL Amyloidosis Advances in Diagnosis and ManagemenDokument4 SeitenAL Amyloidosis Advances in Diagnosis and Managemenfitra khoNoch keine Bewertungen
- Cardiac AmyloidosisDokument20 SeitenCardiac Amyloidosisrizqina ajraNoch keine Bewertungen
- Acute Erythroid Leukemia: Review ArticleDokument10 SeitenAcute Erythroid Leukemia: Review Articlemita potabugaNoch keine Bewertungen
- Doppler-Atlas Sickle Cell AnemiaDokument5 SeitenDoppler-Atlas Sickle Cell AnemiadanielNoch keine Bewertungen
- Seminar: Lionel Adès, Raphael Itzykson, Pierre FenauxDokument14 SeitenSeminar: Lionel Adès, Raphael Itzykson, Pierre FenauxAchmad Teguh Fikri PratamaNoch keine Bewertungen
- European J of Heart Fail - 2021 - Castiglione - Use of Biomarkers To Diagnose and Manage Cardiac AmyloidosisDokument14 SeitenEuropean J of Heart Fail - 2021 - Castiglione - Use of Biomarkers To Diagnose and Manage Cardiac AmyloidosisRui FonteNoch keine Bewertungen
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseVon EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseNoch keine Bewertungen
- Review Articles: Medical ProgressDokument12 SeitenReview Articles: Medical ProgressmoiNoch keine Bewertungen
- Fast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsVon EverandFast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsNoch keine Bewertungen
- Acute Myeloid Leukemia With Myelodysplasia RelatedDokument6 SeitenAcute Myeloid Leukemia With Myelodysplasia RelatedAgus WiniNoch keine Bewertungen
- General Principles: Harrison's Online Chapter 112. AmyloidosisDokument12 SeitenGeneral Principles: Harrison's Online Chapter 112. AmyloidosisBeerappaJanpetNoch keine Bewertungen
- Bone Marrow Failure and Severe Aplastic Anemia Revision 1.1Dokument3 SeitenBone Marrow Failure and Severe Aplastic Anemia Revision 1.1Rasha Al MousaNoch keine Bewertungen
- Infiltrative Cardiomyopathies Cil Med 2015Dokument10 SeitenInfiltrative Cardiomyopathies Cil Med 2015Luis Miguel Ruiz VelasquezNoch keine Bewertungen
- Biomarkers in AmyloidosisDokument11 SeitenBiomarkers in AmyloidosisMathew McCarthyNoch keine Bewertungen
- CRISPRDokument10 SeitenCRISPRJoel LuceroNoch keine Bewertungen
- Oncologic Emergencies-The Old 2020Dokument11 SeitenOncologic Emergencies-The Old 2020Carlos Alfredo Vargas QuinteroNoch keine Bewertungen
- Laryngeal Amyloidosis: ReviewDokument8 SeitenLaryngeal Amyloidosis: ReviewLuis De jesus SolanoNoch keine Bewertungen
- Oxidative Dna Damage in Patients With Type 2 Diabetes MellitusDokument7 SeitenOxidative Dna Damage in Patients With Type 2 Diabetes MellitusmuniraliiNoch keine Bewertungen
- Hom 3Dokument7 SeitenHom 3Mira SrikandiNoch keine Bewertungen
- Cardiac Amyloidosis: Updates in Diagnosis and ManagementDokument13 SeitenCardiac Amyloidosis: Updates in Diagnosis and ManagementDhino Armand Quispe SánchezNoch keine Bewertungen
- Age-Related Macular Degeneration: Current Treatment ConceptsVon EverandAge-Related Macular Degeneration: Current Treatment ConceptsW.E. AlbertiNoch keine Bewertungen
- JCM 13 02046Dokument24 SeitenJCM 13 02046Etienne UiSNoch keine Bewertungen
- Avances en Leucemias AgudasDokument20 SeitenAvances en Leucemias AgudasMayra Alejandra Prada SerranoNoch keine Bewertungen
- Amyloidosis: Pathogenesis and New Therapeutic Options: Ournal of Linical NcologyDokument10 SeitenAmyloidosis: Pathogenesis and New Therapeutic Options: Ournal of Linical NcologyJeyachandran MariappanNoch keine Bewertungen
- Catheter Ablation For Atrial Arrhythmias in Patients With Cardiac AmyloidosisDokument7 SeitenCatheter Ablation For Atrial Arrhythmias in Patients With Cardiac AmyloidosisjjsanchezmunozNoch keine Bewertungen
- Update On Treatment of Light Chain AmyloidosisDokument13 SeitenUpdate On Treatment of Light Chain AmyloidosisAnia WagnerNoch keine Bewertungen
- Acute Myeloid Leukemia ThesisDokument5 SeitenAcute Myeloid Leukemia ThesisBuyCheapEssayOmaha100% (2)
- LAL Case Report2Dokument3 SeitenLAL Case Report2hematocosas123Noch keine Bewertungen
- The Qualitative Estimation of BCR-ABL Transcript: An In-Lab Procedural Study on Leukemia PatientsVon EverandThe Qualitative Estimation of BCR-ABL Transcript: An In-Lab Procedural Study on Leukemia PatientsNoch keine Bewertungen
- Acuteleukemia: Hayley Rose-Inman,, Damon KuehlDokument18 SeitenAcuteleukemia: Hayley Rose-Inman,, Damon KuehlJorge Tovar AvilaNoch keine Bewertungen
- Chronic Myeloid Leukemia Dissertation ThesisDokument8 SeitenChronic Myeloid Leukemia Dissertation ThesisHelpWithFilingDivorcePapersCanada100% (2)
- Aplastic Anemia: Review of Etiology and TreatmentDokument7 SeitenAplastic Anemia: Review of Etiology and TreatmentCleber MaiaNoch keine Bewertungen
- The Permanganate Method: PotassiumDokument16 SeitenThe Permanganate Method: PotassiumNathan McCorkleNoch keine Bewertungen
- 10 1038@nrdp20156Dokument17 Seiten10 1038@nrdp20156Desi DwiNoch keine Bewertungen
- Heart Failure in The Last Year Progress and PerspeDokument26 SeitenHeart Failure in The Last Year Progress and Perspekavij50040Noch keine Bewertungen
- Amiloidosis Cardiaca 2021Dokument10 SeitenAmiloidosis Cardiaca 2021gragerinNoch keine Bewertungen
- 1 s2.0 S0268960X08000787 Main PDFDokument7 Seiten1 s2.0 S0268960X08000787 Main PDFmohamedhazemelfollNoch keine Bewertungen
- Levels of Markers of Myocardial Infarction and Atherogenicity in Individuals With Sickle Cell TraitDokument6 SeitenLevels of Markers of Myocardial Infarction and Atherogenicity in Individuals With Sickle Cell TraitKIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- Low Laser TherapyDokument2 SeitenLow Laser TherapySuzana PoloncaNoch keine Bewertungen
- Angiosacroma PDFDokument9 SeitenAngiosacroma PDFeltouffuNoch keine Bewertungen
- 2023 What A Neurologist Must Know of TTR AmyloidosisDokument11 Seiten2023 What A Neurologist Must Know of TTR AmyloidosisAlejandra Gonzalez DuarteNoch keine Bewertungen
- Review: Ocular and Orbital Involvement in LeukemiaDokument22 SeitenReview: Ocular and Orbital Involvement in LeukemiadechastraNoch keine Bewertungen
- DC zh800310000453Dokument22 SeitenDC zh800310000453JennyNoch keine Bewertungen
- Frequently Asked Questions: Lecture 7 To 9 Hydraulic PumpsDokument5 SeitenFrequently Asked Questions: Lecture 7 To 9 Hydraulic PumpsJatadhara GSNoch keine Bewertungen
- Small Data, Big Decisions: Model Selection in The Small-Data RegimeDokument10 SeitenSmall Data, Big Decisions: Model Selection in The Small-Data Regimejuan carlos monasterio saezNoch keine Bewertungen
- 5000-5020 en PDFDokument10 Seiten5000-5020 en PDFRodrigo SandovalNoch keine Bewertungen
- Mini Project A-9-1Dokument12 SeitenMini Project A-9-1santhoshrao19Noch keine Bewertungen
- Ict's - 2022 - Mentorship - Summarized - Thread - by - Trader - Theory - Sep 22, 22 - From - RattibhaDokument11 SeitenIct's - 2022 - Mentorship - Summarized - Thread - by - Trader - Theory - Sep 22, 22 - From - RattibhaChristiana OnyinyeNoch keine Bewertungen
- Ocr A Level History Russia CourseworkDokument7 SeitenOcr A Level History Russia Courseworkbcrqhr1n100% (1)
- Products ListDokument11 SeitenProducts ListPorag AhmedNoch keine Bewertungen
- NCPDokument6 SeitenNCPJoni Lyn Ba-as BayengNoch keine Bewertungen
- Evaporative CoolingDokument68 SeitenEvaporative Coolingshivas34regal100% (1)
- 353 Version 7thDokument1 Seite353 Version 7thDuc NguyenNoch keine Bewertungen
- IFSSO Newsletter Jul-Sep 2010Dokument2 SeitenIFSSO Newsletter Jul-Sep 2010rjotaduranNoch keine Bewertungen
- Preliminary Examination The Contemporary WorldDokument2 SeitenPreliminary Examination The Contemporary WorldJane M100% (1)
- Aavi 3Dokument4 SeitenAavi 3Arnie IldefonsoNoch keine Bewertungen
- Windows Insider ProgramDokument10 SeitenWindows Insider ProgramVasileBurcuNoch keine Bewertungen
- Different Principles Tools and Techniques in Creating A BusinessDokument5 SeitenDifferent Principles Tools and Techniques in Creating A BusinessLuna LedezmaNoch keine Bewertungen
- Distance SortDokument6 SeitenDistance SortAI Coordinator - CSC JournalsNoch keine Bewertungen
- Training Course For 2 Class Boiler Proficiency Certificate (Gujarat Ibr)Dokument3 SeitenTraining Course For 2 Class Boiler Proficiency Certificate (Gujarat Ibr)JAY PARIKHNoch keine Bewertungen
- PP Checklist (From IB)Dokument2 SeitenPP Checklist (From IB)Pete GoodmanNoch keine Bewertungen
- Studies - Number and Algebra P1Dokument45 SeitenStudies - Number and Algebra P1nathan.kimNoch keine Bewertungen
- 0409 Book About Minoru Yamasaki, ReviewDokument4 Seiten0409 Book About Minoru Yamasaki, RevieweviannNoch keine Bewertungen
- Altos Easystore Users ManualDokument169 SeitenAltos Easystore Users ManualSebNoch keine Bewertungen
- 04 Membrane Structure NotesDokument22 Seiten04 Membrane Structure NotesWesley ChinNoch keine Bewertungen
- ACTIX Basic (Sample CDMA)Dokument73 SeitenACTIX Basic (Sample CDMA)radhiwibowoNoch keine Bewertungen
- Operator'S Manual PM20X-X-X-BXX: 2" Diaphragm PumpDokument12 SeitenOperator'S Manual PM20X-X-X-BXX: 2" Diaphragm PumpOmar TadeoNoch keine Bewertungen
- CIGRE Operational Evaluation of RTV Coating Performance Over 17 Years On The Coastal Area at Jubail-SADokument9 SeitenCIGRE Operational Evaluation of RTV Coating Performance Over 17 Years On The Coastal Area at Jubail-SAMalik Shoaib khalidNoch keine Bewertungen
- HG32High-Frequency Welded Pipe Mill Line - Pakistan 210224Dokument14 SeitenHG32High-Frequency Welded Pipe Mill Line - Pakistan 210224Arslan AbbasNoch keine Bewertungen
- Credit CardDokument6 SeitenCredit CardJ Boy LipayonNoch keine Bewertungen
- How To Make An Effective PowerPoint PresentationDokument12 SeitenHow To Make An Effective PowerPoint PresentationZach Hansen100% (1)
- ITCNASIA23 - Visitor GuideDokument24 SeitenITCNASIA23 - Visitor Guideibrahim shabbirNoch keine Bewertungen
- BS 215-2-1970-Aluminium Conductors and Aluminium Conductors Steel-Reinforced For Overhead Power TransmissionDokument16 SeitenBS 215-2-1970-Aluminium Conductors and Aluminium Conductors Steel-Reinforced For Overhead Power TransmissionDayan Yasaranga100% (2)