Beruflich Dokumente
Kultur Dokumente
GLAUCOMA American Academy of Ophthalmolo
Hochgeladen von
Anonymous 7rQI2K9deCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
GLAUCOMA American Academy of Ophthalmolo
Hochgeladen von
Anonymous 7rQI2K9deCopyright:
Verfügbare Formate
GLAUCOMA
American Academy of Ophthalmology
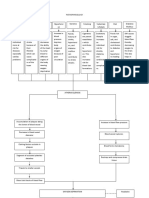
_____________________GLAUCOMA_____________________ CLASSIFICATION OF GLAUCOMA________________________________
A. OPEN-ANGLE GLAUCOMA
DEFINITION: A group of disease that have in common 1. Primary open-angle glaucoma (POAG)
• a characteristic optic neuropathy • not associated with known ocular or systemic disorders that cause
• associated visual field loss increased resistance to aqueous outflow or damage to optic nerve
• elevated IOP is one of the primary risk factors • usually associated with elevated IOP
NORMAL IOP: commonly range in general population is 10-22 mmHg. 2. Normal-tension glaucoma
THREE FACTORS DETERMINE THE IOP • considered in continuum of POAG; often used when IOP is not elevated
1. The rate of aqueous humor production by the ciliary body 3. Juvenile open-angle glaucoma
2. Resistance of aqueous outflow across the trabecular meshwork – • used when open-angle glaucoma diagnosed at young age (typically 10-30
Schlemm’s canal system (in most cases) years of age)
3. The level of episcleral venous pressure. 4. Glaucoma suspect
FACTORS ASSOCIATED WITH THE DEVELOPMENT OF GLAUCOMA • normal optic disc and visual field associated with elevated IOP
1. Increased IOP • suspicious optic disc and/or visual field with normal IOP
2. Advanced age 5. Secondary open-angle glaucoma
3. Racial background • increased resistance to trabecular meshwork outflow associated with
4. Positive family history other conditions (e.g. pigmentary-, phacolytic-, steroid-induced-)
Optic nerve and visual field changes seen in glaucoma are determined by: • increased posttrabecular resistance to outflow secondary to elevated
1. the level of IOP episcleral venous pressure (e.g. carotid cavernous sinus fistula)
2. the resistance of the optic nerve axons to pressure damage B. ANGLE-CLOSURE GLAUCOMA
PRIMARY GLAUCOMA 1. Primary ACG with relative pupillary block
• not associated with known ocular or systemic disorders that cause the • movement of aqueous humor from posterior chamber to anterior chamber
increased resistance to aqueous outflow restricted
• usually affects both eyes • peripheral iris in contact with trabecular meshwork
• may be inherited 2. Acute angle closure
SECONDARY GLAUCOMA • occurs when IOP rises rapidly as a result of relatively sudden blockage of
• associated with ocular or systemic disorders responsible for decreased the trabecular meshwork
aqueous outflow 3. Subacute angle closure (intermittent angle closure)
• the causal diseases are often unilateral • repeated, brief episodes of angle closure with mild symptoms and
• family occurrence is less common elevated IOP, often a prelude to acute angle closure
4. Chronic angle closure
1 Sengdy Chandra Chauhari
• IOP elevation caused by variable portions of anterior chamber angle 2. Trabecular
being permanently closed by PAS • idiopathic (chronic open-angle glaucoma, juvenile open-angle glaucoma)
5. Secondary ACG with pupillary block • “clogging” of trabecular meshwork
• e.g. swollen lens, secluded pupil 1. red blood cells (hemorrhagic-, ghost cell-, sickled red blood cells)
6. Secondary ACG without pupillary block 2. macrophages (hemolytic-, phacolytic-, melanomalytic-)
• posterior pushing mechanism: lens-iris diaphragm pushed forward (e.g. 3. neoplastic cells (primary ocular tumors, neoplastic tumors, juvenile
posterior segment tumor, scleral buckling procedure, uveal effusion) xanthogranuloma)
• anterior pulling mechanism: anterior segment process pulling iris forward 4. pigment particles (pigmentary-, exfoliation syndrome / glaucoma
to form PAS (e.g. iridocorneal endothelial syndrome, neovascular capsulare, malignant melanoma)
glaucoma, inflammation) 5. protein (uveitis, lens-induced glaucoma)
7. Plateau iris syndrome 6. viscoelastic agents
• primary angle closure with or without component of pupillary block, but 7. α-chymotrypsin-induced glaucoma
pupillary block is not predominant mechanism of angle closure 8. vitreous
C. CHILDHOOD GLAUCOMA • alterations of the trabecular meshwork
1. Primary congenital/infantile glaucoma 1. steroid-induced glaucoma
• primary glaucoma present from birth to first few years of life 2. edema (uveitis, scleritis, episcleritis, alkali burns)
2. Glaucoma associated with congenital anomalies 3. trauma (angle recession)
• associated with ocular disorders (e.g. anterior segment dysgenesis, 4. intraocular foreign bodies (hemosiderin, chalcosis)
aniridia) 3. Posttrabecular
• associated with systemic disorders (e.g. rubella, Lowe syndrome) • obstruction of Schlemm’s canal (e.g. collapse at canal)
3. Secondary glaucoma in infants and children • elevated episcleral venous pressure
• e.g. glaucoma secondary to retinoblastoma or trauma 1. carotid cavernous fistula
2. cavernous sinus thrombosis
CLASSIFICATION OF THE GLAUCOMAS 3. retrobulbar tumors
________based on MECHANISM of OUTFLOW OBSTRUCTION________ 4. thyroid ophthalmopathy
OPEN-ANGLE GLAUCOMA MECHANISMS 5. superior vena cava obstruction
1. Pretrabecular (membrane overgrowth) 6. mediastinal tumors
• fibrovascular membrane (neovascular glaucoma) 7. Sturge-Weber syndrome
• endothelial layer, often with Descemet-like membrane (iridocorneal 8. familial episcleral venous pressure elevation
endothelial syndrome, posterior polymorphous dystrophy, penetrating ANGLE-CLOSURE GLAUCOMA MECHANISMS
and non-penetrating trauma) 1. Anterior (“pulling”)
• epithelial downgrowth • contracture of membranes
1. neovascular glaucoma
• fibrous ingrowth
2. iridocorneal endothelial syndrome
• inflammatory membrane (Fuchs heterochromic iridocyclitis, luetic
3. posterior polymorphous dystrophy
interstitial keratitis)
2 Sengdy Chandra Chauhari
4. penetrating and non-penetrating trauma • Treatment is modified based on the proportion of open angle to closed angle
consolidation of inflammatory products and the etiology of the angle-closure component
2. Posterior (“pushing”)
• with pupillary block RISK FACTORS for POAG
1. pupillary block glaucoma • IOP, age, race and positive family history
2. lens-induced mechanisms (phacomorphic lens, ectopia lentis) • Myopia, sex, various systemic factors (diabetes, systemic hypertension,
3. posterior synechiae (iris-vitreous block, pseudophakia, uveitis) arteriosclerotic and ischemic vascular disease)
• without pupillary block RISK FACTORS for PACG
1. ciliary block (malignant) glaucoma • Race: acute PACG is relatively uncommon in blacks
2. lens-induced mechanisms (phacomorphic lens, ectopia lentis) • Sex: women develop acute PACG 3-4 times more often than do men
3. following lens extraction (forward vitreous shift) • Age: acute PACG is most common between the ages of 55 and 65 years
4. anterior rotation of ciliary body (following scleral buckling or • Refraction: PACG is typically associated with hyperopia
panretinal photocoagulation, central retinal vein occlusion) • Inheritance: some of the anatomic features of the eye that predispose to
5. intraocular tumors (retinoblastoma, malignant melanoma) pupillary block (such as forward position of the lens and greater than
6. cysts of the iris and ciliary body average lens thickness) are inherited.
7. retrolenticular tissue contracture (retinopathy of prematurity,
persistent hyperplastic primary vitreous) GENES known to be associated with GLAUCOMA
DEVELOPMENTAL ANOMALIES OF ANGLE TIGR/Myocilin 1q23 (GLC1A) juvenile and adult open-angle glaucoma
• incomplete development of trabecular meshwork / Schlemm’s canal CYP1B1 2p21 (GLC3A) congenital glaucoma
1. congenital (infantile) glaucoma PITX2 4q25 (RIEG1) Rieger syndrome
2. Axenfeld-Rieger syndrome FKGL7 6p25 (IDYS1) iridodysgenesis
3. Peter’s anomaly LMX1B 9q34 (NPS1) glaucoma, with nail-patella syndrome
4. glaucomas associated with other developmental anomalies PAX6 11p13 (AN1) aniridia
• iridocorneal adhesions
1. broad strands (Axenfeld-Rieger syndrome)
2. fine strands that contract to close angle (aniridia)
COMBINED-MECHANISM GLAUCOMA
• Combination of two or more forms of glaucoma present either sequentially or
simultaneously
• IOP elevation can occur as a result of either or both of the following:
1. the intrinsic resistance of the trabecular meshwork to aqueous outflow in
open-angle glaucoma
2. the direct anatomic obstruction of the filtering meshwork by synechiae in
ACG
3 Sengdy Chandra Chauhari
INTRAOCULAR PRESSURE and AQUEOUS HUMOR DYNAMICS______ • Alpha2-agonists
Rate of aqueous formation
Aqueous outflow: posterior chamber → pupil → anterior chamber → trabecular • Normal flow is approximately 2-3 uL/min or a 1% turnover in aqueous
meshwork → Schlemm’s canal → collector channels → volume per minute.
venous system • Varies diurnally and drops during sleep. Decreases with age.
Goldmann equation: Po = (F/C) + Pv • Affected by a variety of factors:
Po = the IOP (mmHg) 1. the integrity of the blood-aqueous barrier
F = the rate of aqueous formation (uL/min) 2. blood flow to the ciliary body
C = the facility of outflow (uL/min/mmHg) 3. neurohumoral regulation of vascular tissue and the ciliary epithelium
Pv = the episcleral venous pressure (mmHg) • Decreases when the eye is injured or inflamed and following the
administration of certain drugs. Decreases with carotid occlusive disease.
Aqueous humor is formed by the ciliary processes
• Each of which is composed of a double layer of epithelium over a core of Facility of outflow (C in the Goldmann equation)
stroma and a rich supply of fenestrated capillaries. • The mean value reported ranges from 0.22-0.28 uL/min/mmHg.
• The apical surfaces of both the outer pigmented and the inner non-pigmented • Decreases with age and is affected by surgery, trauma, medications and
layers of epithelium face each other and are joined by tight junctions, which endocrine factors.
are probably an important part of the blood-aqueous barrier.
• The inner non-pigmented epithelial cells contain numerous mitochondria and TRABECULAR OUTFLOW
microvilli. These cells are thought to be the site of aqueous production. • Trabecular meshwork (uveal, corneoscleral, juxtacanalicular) – Schlemm’s
Aqueous humor formation involves the combination of several processes: canal – venous system
1. Active transport (secretion) • Trabecular meshwork functions as a one-way valve that permits aqueous to
• Consumes energy to move substances against an electrochemical gradient leave the eye by bulk flow but limits flow in the other direction independently
and is independent of pressure. of energy. Aqueous moves both across and between the endothelial cells
• Accounts for the majority of aqueous production and involves activity of lining the inner wall of Schlemm’s canal. Once in Schlemm’s canal, aqueous
the enzyme carbonic anhydrase. enters the episcleral venous plexus by way of scleral collector channels.
2. Ultrafiltration
• Pressure-dependent movement along a pressure gradient (hydrostatic UVEOSCLERAL OUTFLOW
pressure and oncotic pressure, between capillary pressure and IOP) • Anterior chamber → ciliary muscle → supraciliary and suprachoroidal spaces
3. Simple diffusion → exits the eye through the intact sclera or along the nerves and the vessels
• The passive movement of ions across a membrane related to charge. that penetrate it.
Suppression of aqueous formation • Pressure-independent.
• Carbonic anhydrase inhibitors (CAIs) → inhibits the active secretion of • Influenced by age. Increased by cycloplegic, adrenergic, and prostaglandin
bicarbonate or hydrogen ions agents and certain forms of surgery (e.g. cyclodialysis). Decreased by miotics
• Beta-blockers → may affect active transport by causing a decrease in either
the efficiency of the Na+/K+ pump or in the number of pump sites.
4 Sengdy Chandra Chauhari
Tonography • Measures the force necessary to flatten an area of the cornea of 3.06 mm
• This measurement can be taken using a Schiotz tonometer of known weight, diameter. At this diameter, the resistance of the cornea to flattening is
which is placed on the cornea, suddenly elevating IOP. counterbalanced by the capillary attraction of the tear film meniscus for
• The rate at which the pressure declines with time is related to the ease with the tonometer head.
which the aqueous leaves the eye. The decline in IOP over time can be used • Relatively unaffected by ocular rigidity.
to determine outflow facility. • Excessive fluorescein leads to high reading, whereas inadequate
fluorescein leads to low reading.
Episcleral venous pressure • Measurements are affected by corneal edema or scar, alteration in scleral
• Relatively stable, except when alterations in body position and certain rigidity and central corneal thickness.
diseases of the orbit, head and neck obstruct venous return to the heart or 2. Perkins tonometer
shunt blood from the arterial to the venous system. • Using a split-image device and fluorescein staining of the tears.
• The usual range of values is 8-12 mmHg. 3. Non-contact (air-puff) tonometer
• In acute conditions IOP rises approximately 1 mmHg for every 1 mmHg • Measuring the time necessary for a given force of air to flatten a given
increase in episcleral venous pressure. area of the cornea.
4. Portable electronic applanation devices
Factors influencing IOP 5. Pneumatic tonometer
• Time of day, heartbeat, respiration, exercise, fluid intake, systemic • Has a pressure-sensing device that consists of a gas-filled chamber
medications, topical drugs. covered by a Silastic diaphragm.
• Alcohol ↓. Caffeine ↑. Cannabis ↓. 6. Schiotz tonometer
• IOP is higher when the patient is recumbent rather than upright. • Measuring the indentation of the cornea produced by a known weight.
• IOP usually increases with age and is genetically influenced.
Diurnal variation of IOP
• In normal individuals IOP varies 2-6 mmHg over a 24-hour period, as
aqueous humor production changes.
• The higher the pressure, the greater the fluctuation.
• A diurnal fluctuation of greater than 10 mmHg is suggestive of glaucoma.
Imbert-Fick principle
The pressure inside an ideal dry, thin-walled sphere equals the force necessary to
flatten its surface divided by the area of the flattening.
P = F/A (P=pressure, F=force, A=area)
Tonometer
1. Goldmann applanation tonometer
5 Sengdy Chandra Chauhari
CLINICAL EVALUATION_____________________________________ • massive episcleral venous dilation → chronic elevated IOP
The goal of glaucoma management is the preservation of patient’s visual function • black adrenochrome deposits → chronic use of epinephrine derivative drops
and quality of life. • use of topical antiglaucoma medication → decreased tear production, allergic
reactions, foreshortening of the conjunctival fornices, scarring.
--------------------HISTORY and GENERAL EXAMINATION-------------------- • filtering bleb: size, height, degree of vascularization, integrity
History Episclera and sclera
1. The patient’s current complaint • dilation of the episcleral vessels → elevated episcleral venous pressure
2. Symptoms, onset, duration, severity, location • sentinel vessels → intraocular tumor
3. Ocular history • thinning or staphylomatous areas
4. History of present illness Cornea
5. Past ocular medical and surgical history • enlargement of the cornea, breaks in Descemet’s membrane (Haab’s striae)
6. General medical history → developmental glaucoma
7. Past systemic medical history (including medications and allergies) • punctate epithelial defects (especially in the inferonasal interpalpebral region)
8. Review of systems → medication toxicity
9. Social history • microcystic epithelial edema → acute elevated IOP
10. History of ethanol and tobacco
• endothelial abnormalities → underlying associated secondary glaucoma
11. Occupation, avocation, interests
1. Krukenberg spindle in pigmentary glaucoma
12. Family history
2. deposition of exfoliation material in exfoliation syndrome
Refraction
3. keratic precipitates in uveitic glaucoma
• neutralizing any refractive error is crucial for accurate perimetry 4. guttae in Fuchs endothelial dystrophy
• hyperopic eyes → increased risk of ACG 5. irregular and vesicular lesions in posterior polymorphous dystrophy
• myopic eyes → increased risk for pigment dispersion, associated with disc 6. ‘beaten bronze’ appearance in the iridocorneal endothelial syndrome
morphologies that can be clinically confused with glaucoma. • anteriorly displaced Schwalbe’s line → Axenfeld-Rieger syndrome
External adnexae • traumatic or surgical corneal scars, corneal thickness
Its examination and assessment is useful in determining the presence of a variety
Anterior chamber
of conditions associated with secondary glaucomas as well as external ocular
• width of the chamber angle → van Herick method (A narrow slit beam is
manifestations of glaucoma therapy.
directed at an angle of 60˚ onto the cornea just anterior to the limbus. If the
Pupils
distance from the anterior iris surface to the posterior surface of the cornea is
Pupillary responses are one measure of compliance in patients who are on miotic
less than one fourth the thickness of the cornea, the angle may be narrow)
therapy. Corectopia, ectropion uveae and pupillary abnormalities may be observed
• uniformity of depth of the anterior chamber (iris bombe, iris masses)
in some forms of glaucoma. Testing for a RAPD may detect asymmetric optic
nerve damage in glaucoma. • inflammatory cells, red cells, ghost cells, fibrin, vitreous
Conjunctiva Iris
• conjunctival injection → acute elevated IOP, chronic use of sympatho- • heterochromia, iris atrophy, transillumination defects, ectropion uveae,
mimetic drops corectopia, nevi, nodules, exfoliative material
6 Sengdy Chandra Chauhari
• early stages of neovascularization of the anterior segment → fine tufts around • Grade II 20˚ Angle closure possible
the pupillary margin, fine network of vessels on the surface of the iris. • Grade I 10˚ Angle closure probable in time
• evidence of trauma (sphincter tear, iridodonesis), iris pigmentation • Slit <10˚ Angle closure very likely
Lens • O (the iris is against the trabecular meshwork; angle closure is present)
• exfoliative material, phacodonesis, subluxation, dislocation 2. Spaeth system → describes the peripheral iris contour, the insertion of the
• lens size, shape and clarity iris root, and the effects of indentation gonioscopy on the
• posterior subcapsular cataract → chronic corticosteroid use angle configuration.
• presence, type and position of an IOL • Ordinarily, Schlemm’s canal is invisible by gonioscopy. Occasionally during
Fundus gonioscopy in normal eyes, blood refluxes into Schlemm’s canal where it is
• careful assessment of the optic disc seen as a faint red line in the posterior portion of the trabecular meshwork.
• hemorrhage, effusion, masses, inflammatory lesion, retinovascular occlusion, Blood enters Schlemm’s canal when episcleral venous pressure exceeds IOP,
diabetic retinopathy, retinal detachment most commonly because of compression of the episcleral veins by the lip of
the goniolens. Pathological causes include hypotony and elevated episcleral
---------------------------------------GONIOSCOPY--------------------------------------- venous pressure (e.g. carotid-cavernous fistula, Sturge-Weber syndrome)
• Under normal conditions the anterior chamber angle cannot be viewed • Normal blood vessels in the angle include:
directly through the cornea, because light coming from the angle undergoes 1. radial iris vessels, portions of the arterial circle of the ciliary body
total internal reflection at the tear film-air interface. 2. vertical branches of the anterior ciliary arteries
• Because the index of refraction of glass or plastic is similar to that of the → oriented either radially along the iris or circumferentially (in a serpentine
cornea and tears, gonioscopy eliminates this interface and replaces it with a manner) in the ciliary body face
new lens-air interface set at a different angle to the emerging rays. Fuchs heterochromic iridocyclitis → fine, branching, unsheathed, meandering
• Indirect goniolens: Goldmann-type, Zeiss-type Neovascular glaucoma → trunklike vessels crossing the ciliary body and
• Direct goniolens: Koeppe, Barkan, Wurst, Richardson. scleral spur and arborizing over the trabecular meshwork.
• Angle landmarks: Schwalbe’s line and scleral spur → inferior portion • Gonioscopic examination
Posterior cornea pigmentation, guttata
• The width of the angle is determined by :
Schwalbe’s line thickening, anterior displacement
1. the site of insertion of the iris on the ciliary face
2. the convexity of the iris Trabecular meshwork pigmentation, PAS, inflammatory or neovascular
membranes, keratic precipitates
3. the prominence of the peripheral iris roll
Scleral spur iris processes
• The best method for describing the angle is a description or drawing of the
Ciliary body band width, regularity, cyclodialysis cleft
iris contour, the location of the iris insertion, and the angle between the iris
Iris contour, rubeosis, atrophy, cysts, iridodonesis
and the trabecular meshwork.
Pupil, lens exfoliation syndrome, posterior synechiae, position
• Gonioscopic grading systems and regularity, sphincter rupture, ectropion uveae
1. Shaffer system→ describes the angle between the iris and the surface of the
Zonular fibers pigmentation, rupture
trabecular meshwork
• Iris processes → follow the normal curve of the angle; the angle structures
• Grade IV 45˚
are visible in the open spaces between the processes
• Grade III 20-45˚
7 Sengdy Chandra Chauhari
PAS → more solid or sheetlike; composed of iris stroma and obliterate the • Have smaller-diameter axons, smaller receptive fields and slower conduction
angle recess velocity. Synapse in the parvocellular layer of the lateral geniculate body.
• Pigmentation of the trabecular meshwork • Subserve color vision; are most active under higher luminance conditions;
• increases with age; more marked in individuals with darkly pigmented iris discriminate fine detail.
• can be segmental; most marked in the inferior angle; dynamic over time Anatomy of retinal nerve fiber distribution
• Conditions that cause increased anterior chamber angle pigmentation are • Peripheral fibers run closer to choroid and exit in periphery of optic nerve,
pigment dispersion, exfoliation syndrome, malignant melanoma, trauma, while fibers originating closer to the nerve head are situated closer to the
surgery, inflammation, hyphema. vitreous and occupy a more central portion of the nerve.
• Posttraumatic angle recession may be associated with monocular open- The optic nerve branches of the short posterior ciliary artery (differ from its
angle glaucoma. branches in the choriocapillaries)
• Gonioscopic criteria for diagnosing angle recession • They are surrounded by pericytes; lack fenestrations; have tight junction;
1. an abnormality wide ciliary body band have the ability to autoregulate.
2. increased prominence of the sclera spur
3. torn iris processes ------------------------------THE OPTIC NERVE HEAD--------------------------------
4. sclera visible through disrupted ciliary body tissue • Composed of neural tissue, glial tissue, extracellular matrix and blood vessels
5. marked variation of ciliary face width and angle depth in different 1. Nerve fiber layer
quadrants of the same eye • Supported by astrocytes. Can be viewed with the ophthalmoscope using the
• Others findings that may be visible gonioscopically are microhyphema or red-free (green) filter.
hypopyon, retained anterior chamber foreign body, iridodialysis, angle • Blood supply: the central retinal artery; the short posterior ciliary arteries
precipitates suggestive of glaucomatocyclitic crisis, pigmentation of the lens 2. Prelaminar layer
equator, other peripheral lens abnormalities, ciliary body tumors • The depression in the center of the optic disc.
• Blood supply: the short posterior ciliary arteries
The optic nerve 3. Laminar layer
• Consists of approximately 1.2 million axons that are separated into fascicles, • A fenestrated area of connective tissue (lamina cribrosa), through which
with the intervening spaces occupied by astrocytes. The cell bodies of these nerve fibers exit from the eye.
axons lie in the ganglion cell layer of the retina • Blood supply: the short posterior ciliary arteries.
Retinal ganglion cells • Lamina cribrosa appears as a series of approximately 10 stacked plates of
1. Magnocellular neurons (M cells) fenestrated connective tissue whose septae contain small blood vessels. The
• Approximately 10% of all ganglion cells. gray dots that can sometimes be seen ophthalmoscopically in the depths of
• Have larger-diameter axons. Synapse in the magnocellular layer of the lateral the optic cup are the superficial openings of the lamina.
geniculate body. 4. Retrolaminar layer
• Are sensitive to luminance changes in dim illumination (scotopic conditions) • The addition of the myelin sheath produced by oligodendrocytes doubles the
2. Parvocellular neurons (P cells) diameter of the nerve at this point.
• Approximately 90% of all ganglion cells • Blood supply: branches of the meningeal arteries and centrifugal branches
of the central retinal artery.
8 Sengdy Chandra Chauhari
• Best method of examination for the diagnosis of glaucoma
Early glaucomatous cupping • Provides high magnification, excellent illumination, and a stereoscopic view
• Consists of loss of axons, blood vessels, and glial cells → seems to start at the of the disc. Require patient cooperation and moderate pupil size.
level of the lamina cribrosa (associated with compaction and fusion of the
laminar plates), most pronounced at the superior and inferior poles of the disc Early changes of glaucomatous optic neuropathy
More advanced glaucoma 1. Generalized enlargement of the cup
• Tissue destruction extends behind the cribriform plate. Lamina bows • By progressive posterior collapse and compaction of the remaining viable
backward. The optic nerve head takes on an excavated and undermined nerve fibers
appearance. 2. Focal enlargement of the cup
Glaucomatous cupping in infants and children • Notching or narrowing of the rim
• accompanied by an expansion of the entire scleral ring • Acquired optic disc pit formation (deep localized notching where the lamina
→ may explain why cupping seems to occur earlier in children cribrosa is visible at the disc margin)
→ may explain why reversibility of cupping is more prominent with 3. Superficial splinter hemorrhages
successful treatment in these cases • Usually appears as a linear red streak on or near the disc surface
• Clears over several weeks to months. Repeated episodes.
Theories of glaucomatous damage • Individuals with NTG are particularly likely to have disc hemorrhages
1. Mechanical theory → direct compression of the optic nerve fibers against the • An important prognostic sign for the development or progression of visual
lamina cribrosa with interruption of axoplasmic flow field loss
2. Ischemic theory → effects of IOP on the blood supply to the nerve 4. Loss of nerve fiber layer
3. Disturbance of autoregulation (the optic nerve vessels normally increase or
• Appears as a pattern of striations that radiate toward the optic disc
decrease their tone to maintain a constant blood flow independent of IOP)
• May be diffuse or localized to specific bundles
• With the development of glaucoma, the nerve fiber layer thins and becomes
Examination of the optic nerve head
less visible. Can be seen most clearly in high-contrast black-and-white
1. Direct ophthalmoscope
photographs
• Simple to learn. Inexpensive. Can provide a view of the optic disc through a
5. Translucency of the neuroretinal rim
small pupil. Can provide a view of the nerve fiber layer on the posterior pole
• Can be observed in the early stages of nerve fiber loss
(with red-free filter). Does not provide sufficient stereoscopic detail.
6. Development of vessel overpass
2. Indirect ophthalmoscope
• Can be observed in circumstances where the neuroretinal tissue, but not the
• Is used for examining the optic disc in young children, uncooperative
overlying nerve head vasculature, has collapsed. The blood vessels overlying
patients, highly myopic individuals, and individuals with substantial opacities
the collapsed neural rim tissue appear like a highway overpass suspended
of the media.
over, but not in contact with, the underlying tissue.
• The magnification is often inadequate for detecting subtle or localized details
7. Asymmetry of cupping between the patient’s two eyes
important in the evaluation of glaucoma.
3. Slit-lamp biomicroscope combined with a Hruby lens; a posterior pole contact
Other less specific signs of glaucomatous damage include:
lens; or a 60-, 78-, or 90- diopter lens.
• Nasal displacement of the vessels
9 Sengdy Chandra Chauhari
• Narrowing of peripherally retinal vessels 7. Visually evoked cortical potentials (VECP) and electroretinography (ERG)
• Baring of the circumlinear vessels
With advanced damage the cup becomes pale and markedly excavated. Brief definitions of some of the major perimetric terms
Retinal nerve fiber layer defects • Threshold → the differential light sensitivity at which a stimulus of given size
1. Focal abnormalities: slitlike grooves or wedge defects and duration of presentation is seen 50% of the time (in practice, the dimmest
2. Diffuse nerve fiber loss → more common in glaucoma spot detected during testing)
• Suprathreshold → above the threshold (brighter than the threshold stimulus). A
---------------------------------THE VISUAL FIELD--------------------------------- stimulus may also be made suprathreshold by increasing the size or duration of
Visual field is “an island hill of vision in a sea of darkness” presentation.
The island of vision is usually described as a three-dimensional graphic • Kinetic testing → perimetry in which a target is moved from an area where it is
representation of differential light sensitivity at different positions in space. not seen toward an area where it is just seen.
Perimetry refers to the clinical assessment of the visual field. It has two major • Static testing → a stationary stimulus is presented at various locations (the
purposes in the management of glaucoma: brightness, size and duration of the stimulus can be varied at each location to
1. Identification of abnormal fields determine the threshold)
2. Quantitative assessment of normal or abnormal fields to guide follow-up care. • Isopter → a line on a visual field representation connecting points with the
Variety of methods to test visual functions same threshold
1. Differential light perimetry with white light • Depression → a decrease in retinal sensitivity
2. Blue/yellow perimetry • Scotoma → an area of decreased retinal sensitivity within the visual field
• Projects a blue stimulus onto a yellow background. surrounded by an area of greater sensitivity
• Sensitive in the early identification of glaucomatous damage.
3. High-pass resolution perimetry Typical glaucomatous defects
• The stimulus is a ring-shaped target that varies in size. It is made up of a dark 1. Paracentral scotoma
annulus with bright center and dark borders. The average luminance of this 2. Arcuate or Bjerrum scotoma
target is the same as the background. 3. Nasal step
• To determine spatial resolution thresholds. 4. Altitudinal defect
4. Frequency doubling perimetry 5. Temporal wedge
• Uses a low spatial frequency sinusoidal grating undergoing rapid phase-
reversal flicker. Variables in perimetry
• More sensitive in the detection of early glaucomatous loss. 1. Patient
5. Contrast sensitivity 2. Perimetrist
• Measures a subject’s ability to detect a pattern of alternating light and dark 3. Fixation
bands presented at varying frequencies and degrees of contrast. 4. Background luminance (4.0-31.5 apostilbs) → the luminance of the surface
6. Flicker sensitivity onto which the perimetric stimulus is projected affects retinal sensitivity and
• Measures the ability of the subject to recognize the difference between a thus the hill of vision.
flickering light from one that is constantly on. The contrast can be varied.
10 Sengdy Chandra Chauhari
5. Stimulus luminance → The brighter the stimulus, the more visible a given This type of test is the current standard for automated perimetry in glaucoma
stimulus management.
6. Size of stimulus (0 = 1/16 mm2; I = ¼ mm2; II = 1 mm2; III = 4 mm2; IV = 4. SITA
16 mm2; V = 64 mm2) → The larger the stimulus, the more likely it is to be
perceived. Interpretation of a single field
7. Presentation time → The longer the presentation time, the more visible a 1. Quality → The percentage of fixation losses, the false positives and false
given stimulus negatives, and the fluctuations of doubly determined points (less than 2 dB in a
8. Patient refraction → Proper neutralization of refractive error is essential for normal field, less than 3 dB in a field with early damage, less than 4 dB in a
accurate perimetry field with moderate damage). Patient reliability can be evaluated by looking at
9. Pupil size → Testing with pupils smaller than 3 mm in diameter may induce the least damaged areas in badly damaged visual field.
artifacts. 2. Normality or abnormality. When tested under photopic conditions, the normal
10. Wavelength of background and stimulus field demonstrates the greatest sensitivity centrally, with sensitivity falling
11. Speed of stimulus movement → Temporal summation occurs over a time steadily toward the periphery. A cluster of two or more points depressed ≥5 dB
period as long as 0.5 second compared with surrounding points is suspicious. Corresponding points above
and below the horizontal midline should not vary markedly; normally the
Automated static perimetry superior field is depressed 1-2 dB compared with the inferior field.
• Computerized perimeter must be able: 3. Artifacts
1. To determine threshold sensitivity at multiple points in the visual field • Lens rim
2. To perform an adequate test in a reasonable amount of time • Incorrect corrective lens
3. To present results in a comprehensive form. • Cloverleaf field. The Humphrey visual field perimeter test is designed so that
• The best instruments currently available are bowl perimeters that project stimuli four circled points are checked initially and the testing in each quadrant
in programmed locations proceeds outward from these points. If the patient ceases to respond after only
• Four general categories of testing strategy are currently in common use: a few points have been tested, the result is some variation of the cloverleaf
1. Suprathreshold testing. A stimulus, usually one expected to be a little field.
brighter than threshold, is presented at various locations and recorded as seen • High false-positive rate. When a patient responds at a time when no test
or not seen. Sometimes, if it is not seen, it is presented again, and if not seen a stimulus is being presented, a false-positive response is recorded. False-
second time, is recorded as not seen. Then the stimulus may be presented at positive rates greater than 33% suggest unreliability of the test.
maximum brightness to determine if a defect is relative or absolute. This type • High false-negative rate. When a patient fails to respond to a stimulus
of test is designed to screen for moderate to severe defects. presented in a location where a dimmer stimulus was previously seen, a false-
2. Threshold-related screening strategy records tested points as seen or not negative response is recorded. False-negative rates greater than 33% suggest
seen. Screening is done at an intensity 6 dB brighter than the expected unreliability of the test.
threshold, and points missed twice at that level are recorded as defects. This
type of test will detect moderate to severe defects. Interpretation of a series of fields
3. Full-threshold strategy determines retinal sensitivity at each tested point by 1. Separating real change from ordinary variation
altering the stimulus intensity in 4-dB steps until the threshold is crossed.
11 Sengdy Chandra Chauhari
2. Using the information from the field testing to determine the likelihood that a
change is related to glaucomatous progression.
Visual field progression
1. Deepening of an existing scotoma is suggested by the reproducible depression
of a point in an existing scotoma by ≥7 dB.
2. Enlargement of an existing scotoma is suggested by the reproducible depression
of a point adjacent to an existing scotoma by ≥9 dB.
3. Development of a new scotoma is suggested by the reproducible depression of a
previously normal point in the visual field by ≥11 dB, or of two adjacent
previously normal points by ≥5 dB.
Correlation of changes in the visual field with the optic disc is important if:
1. The patient’s optic disc seems less cupped than would be expected for the
degree of field loss
2. The pallor of the disc is more impressive than the cupping.
3. The progression of the visual field loss seems excessive
4. The pattern of visual field loss is uncharacteristic for glaucoma.
Manual perimetry
Goldmann perimetry using the Armaly-Drance screening technique
• Combines a kinetic examination of the peripheral isopters with a
suprathreshold static examination of the central field
Other tests
1. Fluorescein angiography
2. Corneal pachymetry
3. Measurement of episcleral venous pressure
4. Ophthalmodynamometry
5. Carotid noninvasive vascular studies
6. Ocular blood-flow measurements
7. Ultrasonography
12 Sengdy Chandra Chauhari
OPEN-ANGLE GLAUCOMA_____________________________ • Local vascular factors! Higher prevalence of vasospastic disorders such as
migraine headache and Raynaud phenomenon, ischemic vascular diseases,
----------------PRIMARY OPEN-ANGLE GLAUCOMA (POAG) ----------------- autoimmune diseases and coagulopathies.
• Chronic, slowly progressive optic neuropathy characterized by atrophy and • Vascular autoregulatory defects!
cupping of the optic nerve head and associated with characteristic patterns of • Reducing IOP by greater than 30% reduced the rate of visual field progression.
visual field loss. However, since progression was not affected in all patients, other factors may
• Clinical features: usually insidious in onset, slowly progressive and painless; be operative as well. Progression of the visual field loss tended to be slow.
usually bilateral, quite asymmetric; visual loss generally progresses without • The temporal and inferotemporal neuroretinal rim are most affected early in
symptoms. NTG, although other patterns of disc damage may also be observed.
• Risk factors: elevated IOP, race (black), advanced age (>50), family history, • Classification of NTG based on disc appearance:
associated disorders (myopia, diabetes mellitus, cardiovascular disease, CRVO) • A senile sclerotic group with shallow, pale sloping of the neuroretinal rim
• Periodic evaluation of the optic disc and visual field is vital. (primarily in older patients with vascular disease)
• Repeated gonioscopy is indicated to detect possible progressive angle closure • A focal ischemic group with deep, focal, polar notching in the neuroretinal
caused by miotic therapy or age-related lens changes (especially in hyperopic rim
patients), when the chamber becomes shallow, when strong miotics are • The visual field defects in NTG tend to be more focal, deeper and closer to
prescribed, after laser trabeculoplasty or iridectomy, and when IOP rises. fixation, especially early in the course of the disease.
• Differential diagnosis
----------------------------THE GLAUCOMA SUSPECT------------------------------- • Undetected high-tension glaucoma: POAG with diurnal IOP variation,
• Definition: an adult who has normal open angle on gonioscopy and one of the intermittent IOP elevation (ACG, glaucomatocyclitic crisis), previously
following findings in at least one eye: elevated IOP (old secondary glaucoma, normalized IOP in an eye with
• An optic nerve or nerve fiber layer suggestive of glaucoma (enlarged cup/disc previously elevated IOP), use of medication that may cause IOP lowering
ratio, asymmetric cup/disc ratio, notching or narrowing of the neural rim, disc (systemic beta blocker), tonometric error (reduced corneal thickness, low
hemorrhage, or diffuse or local abnormality in the nerve fiber layer) scleral rigidity)
• A suspicious visual field abnormality • Nonglaucomatous optic nerve disease: vascular occlusion, optic nerve head
• An elevated IOP consistently greater than 22 mmHg. drusen, optic nerve head pits and colobomas, chorioretinitis, retinal
• Usually, if two or more of these findings are present, the diagnosis of POAG is detachment, retinoschisis, chiasmal tumors, anterior ischemic optic
supported, especially in the presence of other risk factors. neuropathy.
• Ocular hypertension: elevated IOP in the absence of identifiable optic nerve • Diagnostic evaluation: medical history, measurement of IOP by applanation
damage or visual field loss. tonometry at various times during the day, gonioscopy, careful stereoscopic disc
evaluation. Medical and neurological evaluation.
--------------------NORMAL TENSION GLAUCOMA (NTG) ---------------------- • Criteria for initiating therapy: visual field loss threatening fixation, disc
• Elevated IOP is not the only risk factors in the development of glaucoma, but hemorrhage, and documented visual field or optic nerve progression.
other risk factors, most of which are currently unknown, may play a more • Therapy: medications. If medications is inadequate in controlling the disease →
important role. laser trabeculoplasty, glaucoma filtering surgery with or without antifibrotic
agent (5-fluorouracil or mitomycin-C)
13 Sengdy Chandra Chauhari
• Role of ‘neuroprotective’ agents such as calcium channel blockers, alpha2- • Exfoliation syndrome with glaucoma differs from POAG in often being
agonists, and NMDA (N-methyl-D-aspartate receptor) antagonist?? monocular and showing greater pigmentation of the trabecular meshwork and
higher IOP. The overall prognosis is worse.
--------------------SECONDARY OPEN-ANGLE GLAUCOMA-------------------- • Laser trabeculoplasty → effective, but the response may not be long lasting.
• Exfoliation syndrome (pseudoexfoliation) • Lens extraction → does not alleviate the condition.
• Pigmentary glaucoma • Trabeculectomy → an increase in postoperative inflammation.
• Lens-induced glaucoma (phacolytic glaucoma, lens particle glaucoma, • Increased ocular inflammation can be seen following all ocular surgery in
phacoanaphylaxis) patients with this condition.
• Intraocular tumors
• Ocular inflammation (glaucomatocyclitic crisis, Fuchs heterochromic -----------------------------PIGMENTARY GLAUCOMA------------------------------
iridocyclitis) • Occurs in approximately 25-50% of patients with pigment dispersion syndrome
• Raised episcleral venous pressure • Occurs most commonly in myopic males between the ages of 20 and 50 years.
• Accidental and surgical trauma (hyphema, angle recession glaucoma, • Affected females tend to be older than affected males.
cyclodialysis cleft, hemolytic and ghost cell glaucoma) • Characterized by wide fluctuations in IOP.
• Drugs • High IOP often occurs when pigment is released into the aqueous humor, such
as following exercise or pupillary dilation.
-----------EXFOLIATION SYNDROME (PSEUDOEXFOLIATION) ----------- • Symptoms: haloes, intermittent visual blurring, ocular pain.
• Characterized by the deposition of a distinctive fibrillar material in the anterior • Treatment: medication, laser trabeculoplasty, filtering surgery
segment of the eye (in and on the lens epithelium and capsule, pupillary margin, • Laser iridectomy can minimize posterior bowing of the iris; most often applied
ciliary epithelium, iris pigment epithelium, iris stroma and blood vessels, in eyes with pigment dispersion and ocular hypertension or early glaucomatous
inferior anterior chamber angle or Sampoelesi’s line, corneal endothelium and optic neuropathy.
subconjunctival tissue) Pigment dispersion syndrome________________________________________
• This material probably arises from multiple sources as part of a generalized • Pigment deposition on the corneal endothelium in a vertical spindle pattern
basement membrane disorder. Histochemically, the material resembles amyloid. (Krukenberg spindle), in the trabecular meshwork, and on the lens periphery.
• Other findings: targetlike pattern of deposits on the anterior lens capsule, • Classic spokelike iris transillumination defects
heavily pigmented trabecular meshwork, shallow chamber angle, peripupillary • The spindle pattern on the posterior cornea is caused by the aqueous convection
atrophy, diffuse depigmentation of iris, phacodonesis, iridodonesis, zonular currents and subsequent phagocytosis of pigment by the corneal endothelium.
weakness, abnormalities of the iris vessels. • Krukenberg spindle may occur in other diseases such as exfoliation syndrome.
• Monocular (the unvolved fellow eye may develop the syndrome at a later time) • With age, the signs and symptoms of pigmentary dispersion may decrease in
or binocular with varying degrees of asymmetry. Age related (>70) some individual. Possible causes are normal growth the lens, increase in
• The open-angle glaucoma associated with exfoliation syndrome is thought to be physiologic pupillary block, and loss of accommodation.
caused by the fibrillar material obstructing flow through and causing damage to Gonioscopy
the trabecular meshwork. 1. Homogenous, densely pigmented trabecular meshwork with a speckled ring
of pigment at or anterior to Schwalbe’s line
14 Sengdy Chandra Chauhari
2. Posterior bowing of the midperipheral iris with ‘reverse pupillary block’ • Therapy: medications while the residual lens material resorbs (aqueous
(→ greater contact of the zonular fibers with the posterior iris surface → suppressants, mydriatics to inhibit PAS, and topical corticosteroids). If the
increase of pigment release) glaucoma can’t be controlled, surgical removal of the lens material is necessary.
3. When dilated, pigment deposits can be seen on the lens zonules and both
the anterior and posterior lens capsule. --------------------------------PHACOANAPHYLAXIS----------------------------------
• Pathogenesis: sensitization to own lens protein following surgery or penetrating
------------------------------PHACOLYTIC GLAUCOMA------------------------------ trauma → granulomatous inflammation.
• Pathogenesis: leakage of high-molecular weight lens protein through the • Clinical pictures: moderate anterior chamber reaction with KP on both the
capsule of a mature or hypermature cataract → the proteins precipitate an corneal endothelium and the anterior lens surface; low-grade vitritis, synechial
inflammatory reaction → lens material-filled macrophages and other formation, residual lens material in the anterior chamber.
inflammatory debris obstruct the trabecular meshwork → secondary glaucoma • Treatment: corticosteroids, aqueous suppressants. If medical therapy is
• Clinical picture: usually involves an elderly patient with a history of poor unsuccessful, residual lens material should be removed.
vision who has sudden onset of pain, conjunctival hyperemia, and worsening • Glaucoma, while it may occur, is not common in eyes with phacoanaphylaxis.
vision.
• Examination reveals an elevated IOP of 30-50mmHg, microcystic corneal ------------------------------INTRAOCULAR TUMORS--------------------------------
edema, prominent cell and flare reaction without KP, and open anterior chamber • Glaucoma can result from several different mechanisms:
angle. Wrinkling of the anterior lens-capsule. Cellular debris and white particles 1. Direct tumor invasion of the anterior chamber angle (e.g., primary or
can be seen in the anterior chamber angle. Hypopyon may be present. metastatic tumors of the ciliary body0
• The lack of KP helps distinguish phacolytic glaucoma from phacoanaphylaxis. 2. Angle closure by rotation of the ciliary body or by anterior displacement
• Therapy: medications and cataract extraction. of the lens-iris diaphragm (e.g., choroidal melanomas, other choroidal
and retinal tumors)
----------------------------LENS PARTICLE GLAUCOMA---------------------------- 3. Intraocular hemorrhage
• Occurs when the lens cortex obstructs the trabecular meshwork following 4. Neovascularization of the angle (e.g., choroidal melanomas, medulloepi-
cataract extraction, capsulotomy or ocular trauma. theliomas, retinoblastomas)
• The extent of the glaucoma depends on: 5. Deposition of tumor cells, inflammatory cells, and cellular debris within
1. The quantity of lens material released the trabecular meshwork
2. The extent of inflammatory response • Tumors causing glaucoma in adults include uveal melanoma, metastatic
3. The preexisting ability of the trabecular meshwork to clear the lens material carcinoma, lymphomas, and leukemia.
4. The functional status of the ciliary body which is often altered following • Glaucoma in children is associated with retinoblastoma, juvenile
surgery or trauma. xanthogranuloma, and meduloepithelioma.
• Usually occurs within weeks of the initial surgery or trauma, but it may occur
months or years later. ---------------------------INFLAMMATORY GLAUCOMA---------------------------
• Clinical findings: free cortical materior in the anterior chamber, elevated IOP, • A secondary glaucoma that often combines components of open-angle and
moderate anterior chamber reaction, microcystic corneal edema, and with time, angle-closure disease
the development of posterior and peripheral anterior synechia.
15 Sengdy Chandra Chauhari
• Occurs when the trabecular dysfunction exceeds the accompanying ciliary body 4. Secondary open-angle glaucoma
hyposecretion seen with acute inflammation. • The condition is insidious and unilateral, affecting the hypochromic eye, and
• Causes by a variety of mechanisms presents equally in middle-aged men and women.
1. Edema of the trabecular meshwork • The secondary open-angle glaucoma occurs in approximately 15% of cases.
2. Endothelial cell dysfunction • Gonioscopy reveals multiple fine vessels that cross the trabecular meshwork.
3. Blockage of the trabecular meshwork by fibrin and inflammatory cells These vessels do not appear to be associated with a fibrous membrane and
4. Prostaglandin-mediated breakdown of the blood-aqueous barrier. usually do not lead to PAS and secondary angle closure. They are fragile and
• The presence of KP and a miotic pupil suggests iritis as the cause of IOP may cause an anterior chamber hemorrhage.
elevation. • The glaucoma does not correspond to the degree of inflammation and may be
• Gonioscopic evaluation may reveal subtle trabecular meshwork precipitates. difficult to control. Corticosteroids are generally not effective. Aqueous
• Sometimes, PAS or posterior synechia with iris bombe may develop, resulting suppressants and alpha2-agonists are the agents of choice.
in angle closure.
• Treatment: corticosteroid → may raise IOP -------------------RAISED EPISCLERAL VENOUS PRESSURE-------------------
• Miotic agents should be avoided in patients with iritis, because they may • Normal episcleral venous pressure is approximately 9 mmHg.
aggravate the inflammation and cause posterior synechia. • Causes of increased episcleral pressure
1. Arteriovenous malformations (arteriovenous carotid-dural fistula,
GLAUCOMATOCYCLITIC CRISIS (POSNER-SCHLOSSMAN syndrome) orbital varix, Sturge-Weber syndrome).
• Characterized by: 2. Venous obstruction (retrobulbar tumor, thyroid ophthalmopathy).
1. Recurrent bouts of markedly increased IOP. The IOP is usually markely 3. Superior vena cava syndrome
elevated, in the 40-50 mmHg range. In between bouts the IOP usually • Clinical features: tortuous, dilated episcleral veins. Anterior segment appears
returns to normal, but with increasing numbers of attacks, a chronic normal in most of these patients, except for elevated IOP and the gonioscopic
secondary glaucoma may develop. finding of blood in Schlemm’s canal.
2. Low-grade anterior chamber inflammation. The iritis is mild with few • Medications that reduce aqueous humor formation are more effective than
KP that are small, discreet, and round in nature and usually resolve drugs that increase aqueous outflow. Laser trabeculoplasty is not effective
spontaneously within a few weeks. KP may be seen on the trabecular unless there are secondary changes in the outflow channels. Glaucoma filtering
meshwork on gonioscopy, suggesting a ‘trabeculitis’. surgery may be complicated by ciliochoroidal effusions or suprachoroidal
• Affects middle-aged patients and usually presents with unilateral blurred vision hemorrhage.
and mild eye pain.
• The etiology remains unknown. Prostaglandin-mediated mechanism! ----------------------ACCIDENTAL and SURGICAL TRAUMA--------------------
• Nonpenetrating, or blunt, trauma to the eye causes a variety of anterior segment
-----------------FUCHS HETEROCHROMIC IRIDOCYCLITIS------------------- injuries: hyphema, angle recession (cleavage), iridodialysis, iris sphincter tear,
• Characterized by: cyclodialysis, and lens subluxation.
1. Iris heterochromia (with loss of iris pigment in the affected eye) • Elevated IOP after blunt trauma may occur by several mechanisms
2. Low-grade anterior chamber reaction with small, stellate KP 1. Posttraumatic inflammation
3. Posterior subcapsular cataracts 2. Presence of blood and degenerative red blood cells (ghost cells)
16 Sengdy Chandra Chauhari
3. Direct injury to the trabecular meshwork. -------------------------------CYCLODIALYSIS CLEFT--------------------------------
This elevation tends to be short in duration but may be protracted with the risk • Definition: focal area of separation of the ciliary body from its attachment to
of corneal blood staining and glaucomatous optic nerve damage. the scleral spur.
• Acute secondary glaucoma caused by chemical injuries may result from: • When a cyclodialysis cleft is present, the eye is often hypotonus. The
1. Inflammation mechanism of hypotony is:
2. Shrinkage of scleral collagen 1. Increased uveoscleral outflow through the cleft into suprachoroidal space
3. Release of chemical mediators such as prostaglandins 2. Possibly reduced aqueous production as a result of vascular compromise
4. Direct damage to the chamber angle to the ciliary processes.
5. Compromise of the anterior uveal circulation • Closure of a cyclodialysis cleft may cause long-term elevation of IOP and
Trabecular damage or inflammation may cause glaucoma to develop months or glaucoma. Treatment is similar to POAG.
years after a chemical injury.
• Open-angle glaucoma is one of the long-term sequelae of siderosis or chalcosis ----------------------------------------HYPHEMA-------------------------------------------
from a retained intraocular metallic foreign body in penetrating or perforating • Increased IOP is a result of:
injuries. 1. Obstruction of the trabecular meshwork with red blood cells,
inflammatory cells, debris and fibrin
--------------TRAUMATIC or ANGLE-RECESSION GLAUCOMA-------------- 2. Direct injury to the trabecular meshwork from the blunt trauma
• An angle recession, or cleavage, is a tear in the ciliary body that splits between • Increased IOP is more common following recurrent hemorrhage or rebleeding
the longitudinal and circular muscle fibers. Angle recessions are often following a traumatic hyphema. Rebleeding usually occurs within 5-7 days after
associated with tears in the trabecular meshwork as well. the initial hyphema and may be related to normal clot retraction and lysis. The
• Angle-recession glaucoma is a chronic, unilateral secondary open-angle size of the hyphema associated with rebleeding is greater than the primary
glaucoma that usually occurs months to years following ocular trauma. hyphema. The larger the hyphema, the higher the incidence of increased IOP.
• Classic gonioscopic findings • Individuals with sickle cell hemoglobinopathies have an increased incidence of
1. Broad angle recess glaucoma following hyphema. The RBCs tend to sickle in the aqueous humor,
2. Absent or torn iris process and these more rigid cells have great difficulty passing out of the eye through
3. White glistering scleral spur the trabecular meshwork. The optic discs of these patients are much more
4. Depression in the overlying trabecular meshwork sensitive to elevated IOP and are prone to ischemic injury as a result of
5. Localized PAS at the border of the recession. compromised microvascular perfusion.
• The development of secondary glaucoma depends on: • Management of uncomplicated hyphema
1. The degree of angle involvement 1. Eyeshield (patching), limited activity (bed rest), head elevation.
2. Underlying patient predisposition 2. Topical and systemic corticosteroids → may reduce associated
• Treatment: aqueous suppressants, alpha2-agonists. Miotics may be useful, but inflammation
paradoxical responses with increased IOP may occur. Laser trabeculoplasty has 3. Cycloplegic agents → if significant ciliary spasm or photospasm occurs
a limited role and a low chance of success but may be considered prior to 4. Aminocaproic acid → reduce rebleeding
filtering surgery. • Management of elevated IOP in hyphema
1. Aqueous suppressants
17 Sengdy Chandra Chauhari
2. Alpha2-agonists 4. The conjunctiva tends not to be inflamed unless the IOP is markedly
3. Hyperosmotic agents elevated.
• CAIs should be avoided in sickle cell hemoglobinopathies because they 5. Gonioscopically, the angle appears normal except for the layering of
may increase the sickling tendency in the anterior chamber by increasing ghost cells over the trabecular meshwork inferiorly.
aqueous levels of ascorbic acid. 6. The vitreous has the appearance of old hemorrhage with characteristic
• Adrenergic agonists with significant alpha1 effects (apraclonidine, khaki coloration and clumps of extracellular pigmentation from
dipivefrin, epinephrine) should be avoided in sickle cell disease. degenerated hemoglobin.
• Parasympathomimetic agents should be avoided in all hyphema patients. • Both are generally self-limiting and resolve once the hemorrhage has cleared.
• Management of persistently elevated IOP • Treatment: Aqueous suppressants. If failed, consider irrigation of the anterior
1. Anterior chamber irrigation or washout procedure. chamber, pars plana vitrectomy, and/or trabeculectomy.
2. Iridectomy → if a total hyphema is present, to relieve pupillary block.
3. Trabeculectomy. -----------------------------------SURGICAL TRAUMA----------------------------------
• Operative procedures and laser surgery may be complicated by posttreatment
-----------------HEMOLYTIC and GHOST CELL GLAUCOMA------------------ IOP elevation. This elevation is usually transient, lasting from a few hours to a
• May develop after vitreous hemorrhage. few days.
• Hemolytic glaucoma • Mechanisms of elevated IOP following surgery
→ hemoglobin-laden macrophages block the trabecular outflow channels 1. Pigment release.
→ red-tinged cells are seen floating in the anterior chamber 2. Presence of inflammatory cells and debris
→ a reddish brown discoloration of the trabecular meshwork is often present 3. Mechanical deformation of the trabecular meshwork and angle closure
• Ghost cell glaucoma is a transient secondary open-angle glaucoma caused by • Agents used as adjuncts to intraocular surgery such as viscoelastic substances
degenerated RBCs (ghost cells) blocking the trabecular meshwork may cause secondary IOP elevations. Dispersive viscoelastics (sodium
• Ghost cell hyaluronate) may be more likely to cause IOP increases than retentive
1. RBCs that have lost their intracellular hemoglobin and appear as small viscoelastic agents (chondroitin sulfate).
khaki-colored cells that are less pliable than normal RBCs → Obstruction • Elevated IOP may increase the risk of retinal and optic nerve ischemia and
of the trabecular meshwork → Secondary glaucoma. cause damage in susceptible individual even in a short time. Thus, measurement
2. The cells develop within 1-3 months following a vitreous hemorrhage. of IOP soon after surgery or laser treatment is important. If a substantial rise in
3. They gain access to the anterior chamber through a disrupted hyaloid IOP does occur, therapy with beta-blockers, alpha2-agonists, or CAIs is
face, which can occur from previous surgery (pars plana vitrectomy, required.
cataract extraction, or capsulotomy), trauma, or spontaneous disruption. • The implantation of an intraocular lens (IOL) can lead to a variety of
• Clinical features of ghost cell glaucoma secondary glaucomas
1. Increased IOP and history of a recent vitreous hemorrhage resulting from 1. Uveitis-hyphema-glaucoma syndrome (UGH syndrome)
trauma, surgery, or preexisting retinal disease. 2. Secondary pigmentary glaucoma
2. The anterior chamber is filled with small circulating tan-colored cells. 3. Pseudophakic pupillary block
3. The cellular reaction appears out of proportion to the aqueous flare.
18 Sengdy Chandra Chauhari
• UGH syndrome
1. A form of secondary inflammatory glaucoma caused by chronic irritation
that is usually the result of a malpositioned anterior chamber IOL (the
chafing of the iris by the IOL or erosion of the lens haptics through the iris
or ciliary body).
2. Characterized by chronic inflammation, secondary iris neovascularization,
and recurrent hyphemas.
3. May also occur following implantation of a posterior chamber or suture-
fixated IOL.
-------------GLAUCOMA and PENETRATING KERATOPLASTY-------------
• Mechanisms of secondary glaucoma following penetrating keratoplasty
1. Open angle: inflammatory, corticosteroid induced, viscoelastic, wound
distortion of trabecular meshwork, fibrous/epithelial ingrowth
2. Closed angle: chronic PAS (angle closure), pupillary block, in
association with corticosteroid use, fibrous/epithelial ingrowth,
inflammatory
• Attempts to minimize these secondary glaucomas
1. Oversized donor grafts
2. Peripheral iridectomies
3. Surgical repair of the iris sphincter
--------------------------------DRUGS and GLAUCOMA--------------------------------
• Corticosteroid-induced glaucoma
• An open-angle glaucoma caused by prolonged use of topical, periocular,
inhaled, or systemic corticosteroids.
• It mimics POAG in its presentation and clinical course.
• The duration of time before the IOP rises and the extent of this rise depends
on: 1. the type and potency of the agent
2. the means and frequency of its administration
3. the susceptibility of the patient
• The elevated IOP is a result of an increased resistance to aqueous outflow in
the trabecular meshwork.
• Cycloplegic drugs can increase IOP in individuals with open angles.
19 Sengdy Chandra Chauhari
ANGLE-CLOSURE GLAUCOMA_________________________ in this position lens-iris apposition is maximal, setting the stage for pupillary
block and subsequent angle closure.
------MECHANISMS and PATHOPHYSIOLOGY of ANGLE CLOSURE-----
• Angle closure develops because apposition of the iris to the trabecular ACUTE PRIMARY ANGLE-CLOSURE GLAUCOMA__________________
meshwork blocks the drainage of aqueous humor. • Occurs when IOP rises rapidly as a result of relatively sudden blockage of the
• The mechanisms of angle closure fall into 2 general categories trabecular meshwork by the iris.
1. Mechanisms that push the iris forward from behind • Symptoms: pain, blurred vision, rainbow-colored haloes around lights, nausea
2. Mechanisms that pull the iris forward into contact with the trabecular and vomiting.
meshwork • Signs: high IOP; middilated, sluggish and often irregular pupil; corneal
• The most frequent cause of angle closure is pupillary block. epithelial edema; congested episcleral and conjunctiva blood vessels; shallow
Pupillary block → obstruction of aqueous flow from the posterior chamber anterior chamber; a mild amount of aqueous flare and cells.
through the pupil → pressure gradient between the posterior and anterior • Definitive diagnosis depends on the gonioscopic verification of angle closure.
chambers → forward bowing of the peripheral iris against the trabecular Compression gonioscopy is required to determine if the iris-trabecular
meshwork → closure of the anterior chamber angle. meshwork blockage is reversible (appositional closure) or irreversible
• Angle closure may also occur without pupillary block. The lens-iris diaphragm (synechial closure) and it may be therapeutic in breaking the attack of acute
can be pushed or rotated forward by several mechanisms: angle closure.
1. Ciliary body swelling, inflammation, or cysts. • Acute attack (high IOP) may cause:
2. Aqueous misdirection (malignant or ciliary block glaucoma) 1. glaucomatous optic nerve damage and/or retinal vascular occlusion
3. Posterior segment tumors 2. peripheral anterior synechiae (PAS)
4. Contracting retrolental tissue 3. sector atrophy of the iris → releases pigment and causes pigmentary
5. Scleral buckling procedures dusting of the iris surface and corneal endothelium.
6. Conditions predisposing to ciliochoroidal effusions (panretinal 4. ischemia of the iris sphincter muscle → causes the pupil to become
photocoagulation and nanophthalmos) permanently fixed and dilated.
Angle closure can occur when the iris is pulled forward by contraction of a 5. glaukomflecken (small anterior subcapsular lens opacities)
membrane or fibrovascular tissue, as with inflammation, neovascularization, or • Treatment
endothelial proliferation closing the anterior chamber angle. • Definitive treatment is an iridectomy, laser or surgical.
• Mild attacks may be broken by cholinergic agents (pilocarpine 1%-2%),
-------------------PRIMARY ANGLE-CLOSURE GLAUCOMA-------------------- which induce miosis that pulls the peripheral iris away from the trabecular
• Pathophysiology meshwork.
1. small anterior segments and short axial length → relative pupillary block • Stronger miotics should be avoided, as they may increase the vascular
2. age heightens the risk of relative pupillary block, as the lens grows and congestion of the iris or rotate the lens-iris diaphragm more anteriorly,
iridolenticular contact increases increasing the pupillary block. However, when the IOP is quite elevated, the
An angle-closure attack is often precipitated by some minor event, such as pupillary sphincter may be ischemic and unresponsive to miotic agents alone.
pupillary dilation. The dilation to midposition relaxes the peripheral iris so • The patient should be treated with some combination of a topical beta-
that it may bow forward, coming into contact with the trabecular meshwork; blockers; alpha2-agonists; an oral, topical, or intravenous CAI; and, when
20 Sengdy Chandra Chauhari
necessary, a hyperosmotic agent. This treatment is used to reduce IOP to the
point where the miotic agent will constrict the pupil and open the angle. SUBACUTE (INTERMITTENT, PRODROMAL) ANGLE-CLOSURE GLAUCOMA
• Globe compression and compression gonioscopy may also treat acute ACG. • Characterized by episodes of blurred vision, haloes, and mild pain caused by
• Nonselective adrenergic agonists or medications with significant alpha1- elevated IOP. These symptoms resolve spontaneously, especially during sleep-
adrenergic activity (apraclonidine) should be avoided to prevent further induced miosis. IOP is usually normal between the episodes, which occur
pupillary dilation and iris ischemia. periodically over days or weeks.
• Laser iridectomy is the treatment of choice for angle closure glaucoma • The typical history and the gonioscopic appearance of a narrow chamber angle
secondary to pupillary block. Surgical iridectomy is indicated when laser help establish the diagnosis
iridectomy cannot be accomplished. Once an iridectomy has been performed, • Laser iridectomy is the treatment of choice.
pupillary block is relieved and the iris is no longer pushed forward into • This condition can progress to chronic ACG or to an acute attack that does not
contact with the trabecular meshwork, as the pressure gradient between the resolve spontaneously.
posterior and anterior chambers approaches zero. If a laser iridectomy cannot
be performed, the acute attack may rarely be stopped by flattening the CHRONIC ANGLE-CLOSURE GLAUCOMA_________________________
peripheral iris through iridoplasty or by relieving pupillary block with laser • May develop either after acute angle closure in which synechial closure persists
pupilloplasty. or when the chamber angle closes gradually and IOP rises slowly as enough
• Once the attack is broken, a peripheral iridectomy should be performed as angle is compromised.
soon as possible. Following resolution of the acute attack, it is important to • The clinical course resembles that of open-angle glaucoma in its lack of
reevaluate the angle by gonioscopy for persistent residual angle closure that symptoms, modest elevation of IOP, progressive cupping of the optic nerve
may be amenable to laser gonioplasty. head, and characteristic glaucomatous loss of visual field.
• The IOP may remain low for weeks following acute ACG because of ciliary • Permanent PAS are present, as determined by indentation gonioscopy.
body ischemia and poor aqueous production, and it is a poor indicator of • Even if miotics and other agents lower IOP, iridectomy is necessary to relieve
angle function or anatomy. Repeat or serial gonioscopy is therefore the pupillary block and prevent further permanent synechial angle closure.
essential. Without iridectomy, closure of the angle progresses and becomes irreversible.
• Fellow eye • Laser iridectomy is the treatment of choice.
• Shares the anatomic predisposition for increased pupillary block. Gonioscopy • Argon laser gonioplasty or goniosynechialysis may be helpful in extensive
usually reveals a narrow, occludable angle. At high risk for developing acute PAS and elevated IOP following acute angle closure.
angle closure.
• The pain and emotional upset resulting from the involvement of the first eye THE NARROW ANTERIOR CHAMBER ANGLE_____________________
may increase sympathetic flow to the fellow eye and produce pupillary • Provocative tests are designed to precipitate a limited form of angle closure,
dilation. which can then be detected by gonioscopy and IOP measurement. The methods
• Peripheral iridectomy is recommended if a similar angle configuration is commonly used include pharmacologic pupillary dilation and prone-darkroom
present. If it is not, specific secondary ACGs must be strongly considered in testing. An IOP increase of 8 mmHg or more is considered positive. An
the differential diagnosis. asymmetric pressure rise between the two eyes with a corresponding degree of
• An untreated fellow eye has a 40%-80% chance of developing an acute attack angle closure is also considered a positive sign.
of angle closure over the next 5-10 years. • Various factors that cause pupillary dilation may induce ACG
21 Sengdy Chandra Chauhari
1. Drugs: mydriatics and miotics. • The process is much more rapid and is precipitated by marked lens swelling
2. Pain, emotional upset, or fright. (intumescence) as a result of cataract formation and the development of
• The effect of miotics is to pull the peripheral iris away from the chamber angle. pupillary block in an eye anatomically not disposed to closure.
However, miotics also cause the zonular fibers of the lens to relax, allowing the • (PACG → the process tends to occur slowly in hyperopes who undergo
lens to come forward. Furthermore, their use results in an increase in the progressive shallowing of the anterior chamber as a result of increasing
amount of iris-lens contact, thus potentially increasing pupillary block. anterior-posterior lens diameter)
• Alpha-blockers (moxisylyte or thymoxamine, dapiprazole) can reverse the • Disparities between the two eyes in the anterior chamber depths and degree of
effects of sympathomimetic dilating agents and minimize the chances of angle cataract should suggest a phacomorphic process.
closure → used as a diagnostic test for combined-mechanism glaucoma.
ECTOPIA LENTIS_________________________________________________
--------------------------------------PLATEAU IRIS---------------------------------------- • Definition: displacement of the lens from its normal anatomic position.
• Caused by anteriorly positioned ciliary processes that critically narrow the • Common causes: trauma, Marfan syndrome, homocystinuria, microsphero-
anterior chamber recess by pushing the peripheral iris forward. Following phakia, Weill-Marchesani syndrome.
dilation of the pupil, the peripheral iris bunches up and obstructs the trabecular • Anterior displacement of the lens → pupillary block → iris bombe →
meshwork. shallowing of the anterior chamber → secondary ACG.
• Should be suspected if: • May present clinically as acute or chronic ACG.
1. The central anterior chamber seems unusually deep and the iris plane • Laser iridectomy is the treatment of choice.
appears rather flat for an eye with angle closure. • Lens extraction is indicated if pupillary block is not relieved or when the
2. Angle closure occurs in younger myopic patients. anterior chamber progressively shallows following laser iridectomy.
• Can be confirmed with ultrasound biomicroscopy.
• Treatment APHAKIC or PSEUDOPHAKIC ANGLE-CLOSURE GLAUCOMA_______
1. Iridectomy → for plateau iris configuration. • Pupillary block in aphakic and pseudophakic eyes
2. Long-term miotic therapy → for plateau iris syndrome. 1. An intact vitreous face can block the pupil and/or an iridectomy in aphakic or
3. Laser peripheral iridoplasty → for plateau iris syndrome, to thin the pseudophakic eyes or in phakic eyes with dislocated lenses.
peripheral iris. 2. Shallow anterior chamber and iris bombe
3. Mydriatics → may restore the aqueous flow through the pupil
----SECONDARY ANGLE-CLOSURE GLAUCOMA with PUPILLARY BLOCK----- 4. Topical beta blockers, alpha-2 agonists, CAIs and hyperosmotic agents →
• Lens-induced ACG can be effective in reducing the IOP
1. Phacomorphic glaucoma 5. Laser iridectomy!
2. Ectopia lentis • Pupillary block with anterior chamber IOL
3. Aphakic or pseudophakic ACG 1. Pupillary block develops with apposition of the iris, vitreous face, and/or lens
• Nonrhegmatogenous retinal detachment optic. The lens haptic or vitreous may obstruct the iridectomy or the pupil,
and the peripheral iris bows forward around the anterior chamber IOL to
PHACOMORPHIC GLAUCOMA____________________________________ occlude the chamber angle. The central chamber remains deep in this
• Definition: secondary ACG arises from a swollen lens.
22 Sengdy Chandra Chauhari
instance, because the lens haptic and optic prevents the central portions of the NEOVASCULAR GLAUCOMA______________________________________
iris and vitreous face from moving forward. • Characterized by fine arborizing blood vessels on the surface of the iris and
2. Laser iridectomies trabecular meshwork, which are accompanied by a fibrous membrane. The
• Pupillary block after extracapsular cataract extraction contraction of the fibrovascular membrane results in the formation of PAS,
1. if an iridectomy has not been performed at the time of surgery → when the leading to the development of secondary ACG.
iris forms adhesions to a posterior chamber IOL or to the residual anterior or • Disorders predisposing to neovascularization of the iris and angle
posterior capsule. 1. Systemic vascular disease: carotid occlusive disease, carotid artery ligation,
2. when retained viscoelastic or fluid in the capsular bag pushes a posterior carotid cavernous fistula, giant cell arteritis, Takayasu (pulseless) disease
chamber IOL anteriorly 2. Ocular vascular disease: diabetic retinopathy, CRVO, CRAO, BRVO, SCR,
Coats disease, Eales disease, ROP, PHPV, syphilitic vasculitis, anterior
NONRHEGMATOGENOUS RETINAL DETACHMENT________________ segment ischemia
• The subretinal fluid accumulates and progressively pushes the retina forward 3. Other ocular disease: chronic uveitis, chronic retinal detachment, endophthal-
against the lens like a hydraulic press. The fluid or hemorrhage may accumulate mitis, Stickler syndrome, retinoschisis
rapidly, and as it pushes the bullous retinal detachment forward to a retrolenti- 4. Intraocular tumors: uveal melanoma, metastatic carcinoma, retinoblastoma,
cular position, it can flatten the anterior chamber completely. reticulum cell sarcoma
5. Ocular therapy: radiation therapy
------------------SECONDARY ANGLE-CLOSURE GLAUCOMA --------------- 6. Trauma
without PUPILLARY BLOCK • Classic pattern of neovascularization of the anterior segment: Fine vascular
Mechanisms of secondary angle closure tufts at the pupil that then extend radially over the iris, crosses the ciliary body
1. Contraction of a membrane, band, or exudate in the angle, leading to PAS and scleral spur as fine single vessels that then branch as they reach and involve
2. Forward displacement of the lens-iris diaphragma, often accompanied by the trabecular meshwork (reddish coloration). With contraction of the
swelling and anterior rotation of the ciliary body fibrovascular membrane, PAS develop and coalesce, gradually closing the
• Neovascular glaucoma angle. The PAS end at Schwalbe’s line because the fibrovascular membrane
• Iridocorneal endothelial (ICE) syndrome cannot grow over healthy corneal endothelium (distinguishing this condition
• Tumors from other secondary ACGs that result from an abnormal corneal endothelium
• Inflammation such as ICE syndrome)
• Aqueous misdirection • Clinical features: often present with an acute glaucoma.
• Epithelial and fibrous downgrowth • The most common cause of iris neovascularization is ischemic retinopathy.
• Trauma 1. Panretinal photocoagulation is the treatment of choice when the ocular
• Retinal surgery and retinal vascular disease media are clear. The resulting decrease in neovascularization after retinal
• Nanophthalmos ablation may reduce or normalize the IOP, depending on the degree of
synechial closure that has occurred. This procedure may improve the success
• Fuchs corneal endothelial dystrophy
rate of filtering surgery by eliminating the angiogenic stimulus and decrease
• Retinopathy of prematurity
the risk of hemorrhage at the time of surgery.
• Flat anterior chamber
23 Sengdy Chandra Chauhari
2. Medical therapy (topical beta blockers, alpha2-agonists, CAIs, cycloplegics 2. The corneal and angle findings predominate
and corticosteroids) may be useful in reducing IOP and decreasing • Cogan-Reese syndrome
inflammation. 1. The iris atrophy tends to be less severe
3. Filtering surgery has a better chance of success once neovascularization has 2. Tan pedunculated nodules or diffuse pigmented lesions on the anterior iris
regressed after panretinal photocoagulation. The use of the antimetabolites 5- surface
fluorouracil and mitomycin-C may increase the success rate. Tube-shunt • Causes: virus? (Epstein-Barr and herpes simplex viruses)
operations can also be effective in controlling the IOP. • Therapy
4. Cyclodestructive procedure. 1. Hypertonic saline solutions
2. Aqueous suppressants
IRIDOCORNEAL ENDOTHELIAL (ICE) SYNDROME_________________ 3. Filtering surgery (trabeculectomy or tube-shunt procedures)
• Definition: a group of disorders characterized by abnormal corneal endothelium
that causes variable degrees of iris atrophy, secondary ACG, and corneal TUMORS_________________________________________________________
edema. • The most common type is uveal melanomas.
• Three clinical variants • Mechanisms of angle-closure: forward displacement of the lens-iris diaphragm,
1. Chandler syndrome and neovascularization
2. Progressive iris atrophy
3. Cogan-Reese syndrome INFLAMMATION_________________________________________________
→ The corneal endothelium appears abnormal and takes on a beaten bronze • Pathogenesis
appearance. Specular microscopy! 1. Breakdown of the blood-aqueous barrier → fibrin and increased aqueous
• Clinical features: Unilateral, presents between 20 and 50 years of age, occurs proteins → posterior synechiae → iris bombe → secondary angle closure
more often in women. Decreased vision, pain or abnormal iris appearance. 2. PAS are formed through peripheral iris edema, organization of inflammatory
Microcystic corneal edema may be present without elevated IOP, especially in debris in the angle, and the bridging of the angle by large KP. PAS from
Chandler syndrome. The unaffected eye may have subtle changes of the corneal inflammatory disease occur most frequently in the inferior angle, and tend to
endothelium without other manifestations of the disease. be nonuniform in shape and height (PAS from primary angle closure → in the
• High PAS are characteristic of ICE syndrome (often extend anterior to superior angle, uniform in shape and height)
Schwalbe’s line). The PAS are caused by the contraction of the single layer of 3. Ischemia secondary to inflammation may rarely cause rubeosis iridis and
endothelial cells and surrounding collagenous-fibrillar tissue that extend from neovascular glaucoma
the peripheral cornea over the trabecular meshwork and iris. The PAS result in • Posterior uveitis → massive exudative retinal detachment → forward displace-
synechial closure of the anterior chamber and lead to an ACG ment of the lens-iris diaphragm → ACG. Treatment is aqueous suppressants
• Progressive iris atrophy and corticosteroids.
1. Characterized by severe iris atrophy • Interstitial keratitis → chronic inflammation, PAS formation, multiple cysts of
2. Resulting in heterochromia, corectopia, ectropion uveae, iris stromal and the iris pigment epithelium → ACG.
pigment epithelial atrophy, and hole formation.
• Chandler syndrome
1. Minimal iris atrophy and corectopia occurs
24 Sengdy Chandra Chauhari
AQUEOUS MISDIRECTION________________________________________ EPITHELIAL and FIBROUS DOWNGROWTH________________________
• Synonyms: malignant glaucoma, ciliary block glaucoma, posterior aqueous • Epithelial proliferation
diversion syndrome 1. ‘pearl’ tumors of the iris
• Cause: anterior rotation of the ciliary block and posterior misdirection of the 2. epithelial cysts → translucent, nonvascular anterior chamber cysts that
aqueous in association with a relative block to aqueous movement at the level of originate from the surgical or traumatic wound
the lens equator, vitreous face, and ciliary processes. 3. epithelial ingrowth → grayish sheetlike growth on the trabecular meshwork,
• Usually presents following ocular surgery in patients with a history of angle iris, ciliary body, and posterior surface of the cornea; often associated with
closure or PAS. May also occur spontaneously in eyes with an open angle wound incarceration, wound gape, ocular inflammation, and corneal edema.
following cataract surgery or various laser procedures. → The argon laser produces characteristic white burns on the epithelial
• Uniform flattening of the anterior chamber and elevated IOP. membrane on the iris surface, which helps to confirm the diagnosis of
• Clinical features epithelial downgrowth and to determine the extent of involvement.
1. The anterior chamber is shallow or flat with anterior displacement of the lens, → Cytologic examination of an aqueous aspirate can be performed to
pseudophakos, or vitreous face. confirm the diagnosis
2. Ciliary processes are seen to be rotated anteriorly and may be seen through an → Radical surgery is recommended to remove the intraocular epithelial
iridectomy to come in contact with the lens equator. membrane and the affected tissues and to repair the fistula.
3. Optically clear “aqueous” zones may be seen in the vitreous highlighting the • Fibrovascular tissue proliferation
underlying pathology. 1. Fibrous ingrowth progresses slowly and is often self-limited; appears as a
• Differential diagnosis: choroidal effusion, pupillary block, suprachoroidal thick, gray-white, vascular, retrocorneal membrane with an irregular border.
hemorrhage. Often the level of IOP, time frame following surgery, patency of 2. Fibrous ingrowth is a common cause of corneal graft failure
an iridectomy, or presence of a choroidal effusion or suprachoroidal 3. Fibrous ingrowth often involves the angle, resulting in PAS and the
hemorrhage help the clinician make the appropriate diagnosis and initiate destruction of the trabecular meshwork. The resultant secondary angle-
treatment. closure is treatment by medication, although surgical intervention may be
• Medical management required
1. cycloplegic therapy
2. beta blockers TRAUMA_________________________________________________________
3. alpha2-agonists • Mechanisms of ACG without pupillary block following ocular trauma
4. carbonic anhydrase inhibitors (CAIs) 1. Formation of PAS associated with angle recession
5. hyperosmotic agents 2. Contusion, hyphema and inflammation.
• Miotics should not be used and can make aqueous misdirection worse.
• Prostaglandin analogues would appear to be contraindicated, as they may RETINAL SURGERY and RETINAL VASCULAR DISEASE____________
increase inflammation. • Scleral buckling operations (especially encircling bands)
• In aphakic and pseudophakic eyes, the anterior vitreous can be disrupted with 1. Can produce shallowing of the anterior chamber angle and frank ACG. Often
the Nd:YAG laser. accompanied by choroidal effusion and anterior rotation of the ciliary body,
causing a flattening of the peripheral iris with a relatively deep central
• Surgical treatment: vitrectomy combined with anterior chamber deepening.
anterior chamber.
25 Sengdy Chandra Chauhari
2. Medical management: cycloplegics, anti-inflammatory agents, beta blockers, NANOPHTHALMOS_______________________________________________
CAIs, and hyperosmotic agents. • Definition: normal eye in shape, but unusually small, with a shortened antero-
3. If medical management is unsuccessful, argon laser gonioplasty, drainage of posterior diameter, a small corneal diameter, and a relatively large lens for the
suprachoroidal fluid, or adjustment of the scleral buckle is required. eye volume.
4. If scleral buckle compresses a vortex vein, increased episcleral venous • Thickened sclera may impede drainage from the vortex veins.
pressure and IOP occurs. This can be treated permanently only by shifting the • These eyes are markedly hyperopic and highly susceptible to PACG.
scleral buckle or releasing the band. • Intraocular surgery is frequently complicated by choroidal effusion and non-
• Following pars plana vitreous surgery rhegmatogenous retinal detachment. Choroidal effusion may occur sponta-
1. ACG may result from the injection of air, long-acting gases such as sulfur neously, and it can induce ACG.
hexafluoride and perfluorocarbons (perfluoropropane and perfluoroethane), or • Therapy for the glaucoma: laser iridectomy, argon laser peripheral iridoplasty,
silicone oil. These substances are less dense than water and rise to the top of and medical therapy.
the eye.
2. An iridectomy should be located inferiorly to prevent obstruction of the FUCHS CORNEAL ENDOTHELIAL DYSTROPHY____________________
iridectomy site by the oil or gas. • Mechanism of glaucoma: gradual thickening of the cornea from edema →
3. Eyes that have undergone complicated vitreoretinal surgery and have eventual closure of the anterior chamber angle.
developed elevated IOP require individualized treatment plans. Treatment
options include removal of silicone oil, releasing of the encircling element, RETINOPATHY OF PREMATURITY________________________________
removal of expansile gases, filtering surgery including tube-shunts, • Mechanism of glaucoma: contracting retrolental tissue → progressive
cilioablation. shallowing of the anterior chamber angle.
• Following panretinal photocoagulation • The onset of this complication usually occurs at 3-6 months of age during the
1. The ciliary body is thickened and rotated, and often an anterior annular cicatricial phase of the disease. However, the ACG may occur later in
choroidal detachment occurs. childhood.
2. Generally, this glaucoma is self-limited, and therapy is directed at temporary
medical management with cycloplegic agents, topical corticosteroids, and PERSISTENT HYPERPLASTIC PRIMARY VITREOUS (PHPV)________
aqueous suppressants.
• Usually unilateral; often associated with microphthalmos and elongated ciliary
• Central retinal vein occlusion (CRVO) processes
1. Sometimes causes early shallowing of the chamber angle, presumably
• Mechanism of glaucoma: contracture of the hyperplastic primary vitreous and
because of swelling of the choroid and ciliary body.
swelling of a cataractous lens → shallowing of the anterior chamber angle
2. Medical treatment of the glaucoma is topical corticosteroids and cycloplegia.
3. If the contralateral eye of a patient with CRVO has a potentially occludable
FLAT ANTERIOR CHAMBER______________________________________
anterior chamber angle, an underlying pupillary-block mechanism must be
• Following cataract surgery
considered and bilateral iridectomy is needed.
1. Hypotony with postoperative flat chamber often indicates a wound leak. A
Seidel test should be performed to locate the leak.
2. Simple pressure patching or bandage contact lens application will often
causes the leak to seal and the anterior chamber to re-form.
26 Sengdy Chandra Chauhari
3. If not, it should be repaired surgically to prevent permanent synechial closure
of the angle.
4. Some ophthalmologists repair the wound leak and re-form a flat chamber
following cataract surgery within 24 hours. Others prefer corticosteroid
therapy for several days to prevent synechiae formation.
5. The chamber should be re-formed without delay if:
• The hyaloid face or an IOL is in contact with the cornea
• There is corneal edema, excessive inflammation, or posterior synechiae
formation
27 Sengdy Chandra Chauhari
CHILDHOOD GLAUCOMA_____________________________ CLINICAL FEATURES____________________________________________
• Characteristic findings of infantile glaucoma
DEFINITIONS____________________________________________________ 1. Epiphora
• Primary congenital or infantile glaucoma is evident either at birth or within 2. Photophobia
the first few years of life. Both conditions are caused by dysplasia of the 3. Blepharospasm
anterior chamber angle without other ocular or systemic abnormalities. • Diagnosis of infantile glaucoma depends on careful clinical evaluation
• Secondary infantile glaucoma is associated with inflammatory, neoplastic, 1. IOP measurement
hamartomatous, metabolic, or other congenital abnormalities of the eye. 2. Measurement of corneal diameter
• Juvenile glaucoma is recognized later in childhood (after 3 years of age) or in 3. Gonioscopy
early adulthood. 4. Measurement of axial length of ultrasonography
• Developmental glaucoma includes primary congenital glaucoma and glaucoma 5. Ophthalmoscopy
associated with other development anomalies, either ocular or systemic. • External eye examination
Glaucoma associated with other ocular or systemic abnormalities may be 1. Buphthalmos with corneal enlargement greater than 12 mm in diameter
inherited or acquired. during the first year of life (The normal horizontal corneal diameter is 9.5-
• Buphthalmos (cow’s eye) refers to enlargement of the globe. This condition 10.5 mm in full-term newborns and smaller in premature newborns)
appears when the onset of elevated IOP occurs before the age of 3 in primary 2. Corneal edema (from mild haze to dense opacification of the corneal stroma)
congenital or infantile glaucoma or in the pediatric glaucomas associated with → present in 25% of affected infants at birth and in more than 60% by the
other ocular and/or systemic abnormalities. sixth month.
3. Haab’s striae (tears in Descemet’ membrane) → occurs acutely; results from
EPIDEMIOLOGY and GENETICS___________________________________ corneal stretching; typically oriented horizontal or concentric to the limbus.
• Congenital glaucoma → 50%-70% is isolated. • Reduced visual acuity → caused by optic atrophy, corneal clouding,
• Pediatric glaucoma cases → 60% are diagnosed by the age of 6 months and astigmatism, amblyopia, cataract, lens dislocation, or retinal detachment.
80% within the first year of life; 65% are male, 70% are bilateral. • Amblyopia → caused by corneal opacity or by refractive error.
• Pattern of inheritance: autosomal dominant (chromosome 1q21-31), autosomal • Myopia → caused by enlargement of the eye
recessive? • Large astigmatism → caused by tears in Descemet’s membrane
• Some patients may also have Axenfeld-Rieger syndrome, aniridia, or a • IOP measurement
multisystem genetic disorder. 1. Most general anesthetic agents and sedatives lower IOP. In general anesthesia
the infant may become dehydrated and the IOP may be reduced. As
PATHOPHYSIOLOGY_____________________________________________ anesthesia becomes deepens, IOP falls.
• Cellular or membranous abnormality in the trabecular meshwork → either an 2. The only exception to this rule is ketamine, which may raise IOP.
anomalous impermeable trabecular meshwork or a Barkan membrane covering 3. The normal IOP in an infant under anesthesia may range from 10 to 20mmHg
the trabecular meshwork. depending on the tonometer. A significant IOP elevation may occur in one
• Abnormal insertion of the ciliary muscle. eye only in 25%-30% of cases.
→ Developmental anomaly of the angle structures of 11-week fetus. • Gonioscopy
1. Under anesthesia, using a direct gonioscopic lens
28 Sengdy Chandra Chauhari
2. Isolated childhood glaucoma → deep anterior chamber with normal iris congenital dyskeratosis), optic nerve abnormalities (optic nerve pit, optic nerve
structure, high and flat iris insertion, absence of angle recess, peripheral iris coloboma, optic nerve hypoplasia, physiologic cupping)
hypoplasia, tenting of the peripheral iris pigment epithelium, thickened uveal
trabecular meshwork. LONG-TERM PROGNOSIS and FOLLOW-UP________________________
3. The angle is typically open with a high insertion of the iris root that forms a • Medications have limited long-term value for congenital or infantile glaucoma
scalloped line as result of abnormal tissue with a shagreened, glistening in most cases, and the preferred therapy is surgical.
appearance. This tissue holds the peripheral iris anteriorly. The angle is • The initial procedures of choice are:
usually avascular, but loops of vessels from the major arterial circle may be 1. goniotomy if the cornea is clear
seen above the iris root. 2. trabeculectomy ab externo if the cornea is hazy
4. The normal anterior chamber angle in childhood is different from the adult • Trabeculectomy and shunt procedures should be reserved for those cases
angle. where goniotomy or trabeculotomy has failed.
• Examination of the optic disc • Beta blockers, alpha2-agonists, or CAIs may be used as temporizing therapy
1. Using a direct ophthalmoscope and a direct gonioscopic or fundus lens on the prior to surgery to control IOP and help clear a cloudy cornea. These drugs must
cornea. Photographic documentation of the optic disc is recommended. be used with caution and at doses appropriate for the child’s weight to prevent
2. The optic nerve head of a normal infant is pink with a small physiologic cup. systemic side effects. The parents should be instructed to occlude the
3. Glaucomatous cupping in childhood resembles the cupping in adulthood, with nasolacrimal drainage system for at least 2 minutes immediately after
preferential loss of neural tissue in the superior and inferior poles. administering topical beta-blockers or alpha2 agonists and to be alert for apnea
4. In childhood the scleral canal enlarges in response to elevated IOP, causing and hypotension. Young children on CAIs require assessment for possible
enlargement of the cup. Cupping may be reversible if IOP is lowered, and acidosis, hypokalemia, and feeding problems.
progressive cupping indicates poor control of IOP. • Long-term prognosis has greatly improved with the development of effective
• Ultrasonography may be useful in documenting progression of glaucoma by surgical techniques, particularly for patients who are asymptomatic at birth and
recording increasing axial length. Increase in axial length may be reversible present with onset of symptoms before 24 months of age. When symptoms are
following reduction of IOP. present at birth or when the disease is diagnosed after 24 months of age, the
outlook for surgical control of IOP is more guarded.
DIFFERENTIAL DIAGNOSIS_______________________________________
• Excessive tearing: nasolacrimal duct obstruction, corneal epithelial defect or DEVELOPMENTAL GLAUCOMAS with ASSOCIATED ANOMALIES___
abrasion, conjunctivitis. Glaucoma associated with systemic congenital syndromes, with reported
• Corneal enlargement or apparent enlargement: X-linked megalocornea, high chromosomal abnormalities
myopia, exophthalmos, shallow orbits (e.g., craniofacial dysostoses) • Trisomy 21 (Down syndrome, trisomy G syndrome)
• Corneal clouding: birth trauma, inflammatory corneal disease, congenital → Mental deficiency, short stature, cardiac anomalies, hypotonia, atypical
hereditary corneal dystrophies, corneal malformations (dermoid tumors, facies
sclerocornea), keratomalacia, metabolic disorders with associated corneal • Trisomy 13 (Patau syndrome)
abnormalities (mucopolysaccharidoses, corneal lipidosis, cystinosis, and von → Mental retardation, deafness, heart disease, motor seizures
Gierke disease), skin disorders affecting the cornea (congenital ichthyosis and • Trisomy 18 (Edwards syndrome, trisomy E syndrome)
29 Sengdy Chandra Chauhari
→ low-set ears, high-arched hard plate, ventricular septal defects, rocker- • Cockayne syndrome
bottom feet, short sternum, hypertonia. → Autosomal recessive disorder, dwarfism, mental retardation, progressive
• Turner (XO/XX) syndrome wasting, “birdlike” facies
→ Short stature, postadolescent females with sexual infantilism, webbed neck, → Retinal degeneration, cataracts, corneal exposure, blepharitis, nystagmus,
mental retardation, congenital deafness, and multiple systemic anomalies. hypoplastic irides, irregular pupils
Glaucoma associated with systemic congenital disorders • Fetal alcohol syndrome
• Lowe (oculocerebrorenal) syndrome → Teratogenic effects of alcohol during gestation, facial abnormalities, mental
→ X-linked recessive disease, mental retardation, renal rickets, aminoaciduria, retardation, anterior segment involvement resembling Axenfeld-Rieger
hypotonia, acidemia, cataracts syndrome and Peters anomaly, optic nerve hypoplasia
• Stickler syndrome (hereditary progressive arthro-ophthalmopathy) Glaucoma associated with ocular congenital disorders
→ Autosomal dominant connective tissue dysplasia; ocular, orofacial, and • Congenital ectropion uveae
generalized skeletal abnormalities with high myopia; open-angle glaucoma; • Congenital corneal staphyloma
cataracts; vitreoretinal degeneration; retinal detachment • Cornea plana
• Zellweger (cerebrohepatorenal) syndrome • Iridoschisis
→ Congenital autosomal recessive syndrome; abnormal facies, cerebral • Megalocornea
dysgenesis, hepatic interstitial fibrosis, polycystic kidneys, CNS • Microcoria
abnormalities • Microcornea
→ Nystagmus, corneal clouding, cataracts, retinal vascular and pigmentary • Microphthalmos
abnormalities, optic nerve head lesions
• Persistent hyperplastic primary vitreous (PHPV)
• Hallermann-Streiff syndrome (dysephalic mandibulo-oculofacial syndrome, • Retinopathy of prematurity
Francois dysephalic syndrome)
• Sclerocornea
→ Micrognathia, dwarfism, microphthalmos, cataract, aniridia, optic atrophy
• Rubinstein-Taybi (broad-thumb) syndrome
Secondary glaucoma in infant and children
→ Mental and motor retardation, typical congenital skeletal deformities of
• Trauma
large thumbs and first toes
• Inflammation
→ Bushy brows, hypertelorism, epicanthus, anti-mongoloid slant of eyelids,
hyperopia, strabismus. • Retinopathy of prematurity with secondary ACG
• Oculodentodigital dysplasia (Meyer-Schwickerath and Weyers syndrome) • Lens-induced glaucoma
→ Autosomal dominant inheritance, hypoplastic dental enamel, microdontia, • Corticosteroid-induced glaucoma
bilateral syndactyly, thin nose, microcornea, microphthalmos • Pigmentary glaucoma
• Prader-Willi syndrome • Glaucoma secondary to intraocular tumors (retinoblastoma, juvenile
→ Chromosome 15 deletion, muscular hypotonia, hypogonadism, obesity, xanthogranuloma, medulloepithelioma)
mental retardation
→ Ocular albinism, congenital ectropion uveae, iris stromal hypoplasia, angle Children often develop glaucoma within 3 years following surgery for congenital
abnormalities cataract
30 Sengdy Chandra Chauhari
MEDICAL MANAGEMENT OF GLAUCOMA______________ 2. Parasympathomimetic (miotic) agents, including cholinergic and
anticholinesterase agents
• Two decisions arise in choosing an appropriate glaucoma therapy: 3. Carbonic anhydrase inhibitors (oral, topical)
1. when to treat 4. Adrenergic agonists (nonselective and selective alpha2 agonists)
2. how to treat 5. Prostaglandin analogues
• Primary angle-closure and infantile glaucoma are treated as soon as the 6. Combination medications
diagnosis is made. 7. Hyperosmotic agents
• Open-angle glaucoma is treated:
1. when damage to the optic nerve has been demonstrated in the form of BETA-ADRENERGIC ANTAGONISTS (BETA BLOCKERS)____________
progressive pathologic cupping and/or characteristic visual field defects • Mechanism of action of topical beta blockers
2. when IOP is elevated to an extent that it is likely to cause damage to the optic Inhibition of cAMP production in ciliary epithelium → reduction of aqueous
nerve humor secretion 20%-50% (2.5 ml/min to 1.9 ml/min) → IOP reduction of
• The goal of currently available glaucoma therapy 20%-30%.
1. To preserve visual function by lowering IOP below a level that is likely to • The effect of beta blockers on aqueous production occurs within 1 hour of
produce further damage to the nerve. instillation and can be present for up to 4 weeks after discontinuation.
2. The treatment regimen should have lowest risk, fewest side effects, and least • As systemic absorption occurs, a contralateral effect with lowering of the IOP in
disruption of the patient’s life the unilateral eye can also be observed.
• Target pressure goal • Beta blockers are additive in combination with miotics, adrenergic agonists,
1. Should actually be a range with an upper IOP limit that is unlikely to lead to CAIs (oral, topical) and prostaglandin analogues.
further damage of the nerve in a given patient • Approximately 10%-20% of the patients treated with topical beta blockers fail
2. The more advanced the glaucomatous process on initial presentation, the to respond with significant lowering of the IOP.
lower the target pressure generally needs to be prevent further progression. • If a patient is on systemic beta-blocker therapy, the addition of topical beta
3. An initial reduction in the IOP of 20%-30% from baseline is suggested, but blockers may be significantly less effective.
those patients who have progressive NTG may require a decrease of at least • Use of beta blockers for more than months to years may reduce their
30% from baseline. effectiveness, as the response of beta receptors is affected by constant exposure
4. The target pressure range needs to be reassessed or changed as comparisons to an agonist (long-term drift, tachyphylaxis). Similarly, receptor saturation
of IOP fluctuations, optic nerve changes, and/or visual field progression (drug-induced upregulation of beta receptors) may occur within a few weeks,
dictate. with loss of effectiveness (short-term escape)
• The anticipated benefits of any therapeutic regimen should justify the risks, and • Six topical beta blockers are approved for use for the treatment of glaucoma in
regimens associated with substantial side effects should be reserved for patients the US. All except betaxolol are noncardioselective beta1 and beta2 anta-
with a high probability of eventual severe visual dysfunction. gonists. Beta1 activity is largely cardiac and beta2 activity largely pulmonary.
• Ocular hypotensive agents are divided into several group based on chemical 1. Betaxolol → 0.25%, bid
structure and pharmacologic action: 2. Carteolol hydrochloride → 1.0%, qd, bid
1. Beta-adrenergic antagonists (nonselective and selective) 3. Levobunolol → 0.25%, 0.5%, qd, bid
4. Metipranolol → 0.3%, bid
31 Sengdy Chandra Chauhari
5. Timolol maleate → 0.25%, 0.5%. qd, bid → Because of the potential for significant ocular and systemic side effects,
6. Timolol hemihydrate → 5.12 mg/ml, qd, bid indirect-acting parasympathomimetic agents are used less commonly.
• Since betaxolol is a selective beta1 antagonist, it is significantly safer than the • Carbachol has both direct and indirect actions, although its primary mechanism
nonselective beta blockers when pulmonary, CNS, or other systemic conditions is direct.
are considered. Betaxolol may be useful in patients with a history of • Mechanism of IOP reduction by both direct- and indirect-acting agents
bronchospastic disorders, although other therapies should be tried in lieu of Contraction of the ciliary muscle, which pulls the scleral spur to tighten the
betaxolol, as beta selectivity is only relative and not absolute, and some beta2 trabecular meshwork, increasing the outflow of aqueous humor.
effect can therefore remain. In general, the IOP-lowering effect of betaxolol is • These agents can reduce the IOP by 10%-20%.
less than the nonselective beta blockers. • The currently accepted indications for miotic therapy
• Carteolol demonstrates intrinsic sympathomimetic activity, which means that, 1. Chronic treatment of increased IOP in patient with at least some filtering
while acting as a competitive antagonist, it also causes a slight to moderate angle
activation of receptors. Thus, even though carteolol produces beta-blocking 2. Prophylaxis for ACG prior to iridectomy
effects, these may be tempered, reducing the effect on cardiovascular and • Other actions of the parasympathomimetic agents
respiratory systems. Carteolol may also be less likely to adversely affect the 1. Reduce uveoscleral outflow. This action may actually worsen the glaucoma if
systemic lipid profile when compared with other beta blockers. miotics are used in patients with little to no trabecular outflow.
• Ocular and systemic side effects of beta blockers are bronchospasm, 2. Cause the pupillary sphincter to contract, stimulate secretory activity in the
bradycardia, increased heart block, lowered blood pressure, reduced exercise lacrimal and salivary glands, and disrupt the blood-aqueous barrier. These
tolerance, and CNS depression. Diabetic patients may experience reduced actions have little bearing on the IOP-lowering effect, except in ACG, where
glucose tolerance and masking of hypoglycemic signs and symptoms. Abrupt the mechanical action of the contracting pupillary sphincter may pull the iris
withdrawal of ocular beta blockers can exacerbate symptoms of away from the trabecular meshwork.
hyperthyroidism. Other side effects include lethargy, mood changes, depression, • Side effects of miotic agents
altered mentation, light-headedness, syncope, visual disturbance, corneal 1. Retinal detachment, especially in patients with peripheral retinal disease.
anesthesia, punctate keratitis, impotence, reduced libido, allergy and alteration 2. Induced myopia, brow ache, alteration of vision in dim light and in
of serum lipids. patients with lens opacities.
3. Paradoxical angle closure (indirect-acting miotics or the stronger direct-
PARASYMPATHOMIMETIC AGENTS______________________________ acting agents), caused by the contraction of ciliary muscle leads to forward
• Classifications movement of the lens-iris diaphragm, an increase in the anteroposterior
1. Direct-acting cholinergic agonists (e.g., pilocarpine) diameter of the lens, and a very miotic pupil. The concomitant administration
• Affect the motor end plates in the same way as acetylcholine, which is of an alpha-adrenergic agonist such as phenylephrine may cause a larger pupil
transmitted at postganglionic parasympathetic junctions, as well as at other without interfering with the reduction of IOP.
autonomic, somatic, and central synapses. 4. Generalized cataract formation in addition to anterior subcapsular
2. Indirect-acting anticholinesterase agents (e.g., echothiophate iodide, opacity (indirect-acting miotics). Direct-acting agents may also be weakly
demecarium bromide) cataractogenic.
• Inhibit the enzyme acetylcholinesterase, thereby prolonging and enhancing 5. Formation of iris pigment epithelial cysts (indirect-acting miotics)
the action of naturally secreted acetylcholine. 6. Ocular surface changes (pseudopemphigoid) (indirect-acting miotics)
32 Sengdy Chandra Chauhari
7. Increased inflammation following surgery (stronger miotics) → Anti- CARBONIC ANHYDRASE INHIBITORS_____________________________
cholinesterase agents should be discontinued and other agents substituted at • Mechanism of action
least 2-4 weeks prior to ocular surgery, because they cause significant 1. Direct antagonist activity upon ciliary epithelial carbonic anhydrase
bleeding during surgery and severe fibrinous iridocyclitis postoperatively. 2. Producing a generalized acidosis (?)
8. Breakdown of the blood-aqueous barrier. Thus, their use in treating uveitic • The enzyme carbonic anhydrase is also present in many other tissues, including
glaucoma should be limited. corneal endothelium, iris, retinal pigment epithelium, brain and kidney.
9. Systemic parasympathetic stimulation such as diarrhea, abdominal cramps, • Over 90% of the ciliary epithelial enzyme activity must be abolished to
increased salivation, bronchospasm and enuresis (indirect-acting miotics). decrease aqueous production and lower IOP.
Since cholinesterase is suppressed throughout the body, depolarization agents SYSTEMIC AGENTS
such as succinylcholine should be avoided while the patient is using these • Most useful in acute situations (e.g., acute ACG). Can be given orally,
eyedrops and for 6 weeks after discontinuation. intramuscularly, and intravenously.
• Preparations • Because of the side effects of the systemic CAIs, chronic therapy with these
1. Pilocarpine HCl 0.2%, 0.5%, 1.0%, 2.0%, 3.0%, 4.0%, 6.0%, bid-qid agents should be reserved for patients whose glaucoma cannot be controlled by
2. Pilocarpine nitrate 1.0% - 4.0%, bid-qid alternative topical therapy.
3. Pilocarpine membrane 20ug, 40ug, q5-7d → releases drug at a steady rate for • The oral agents most commonly used are acetazolamide and methazolamide.
approximately 1 week; the induced myopia is more stable and the miosis is The lowest dose that reduces the IOP to an acceptable range should be used.
less marked than with eyedrop therapy; the release of drug and the induced Methazolamide → has longer duration of action; less bound to serum protein;
symptoms are greatest during the first 24 hours; tolerated better when metabolized by liver, thereby decreasing the risk of systemic side effects; 25-50
administered at bedtime. mg 2-3 times daily.
4. Pilocarpine gel 4.0% qhs → loss of drug effect after 18-20 hours; induced Acetazolamide → not metabolized; excreted in urine; may be started at 62.5mg
myopia and miosis are less prominent than with drops. every 6 hours, and higher doses may be used if tolerated.
5. Carbachol 1.5%, 3.0%, bid, tid • Side effects are usually dose related. They include paresthesias of the fingers or
6. Echothiophate iodide 0.03%, 0.06%, 0.125%, 0.25%, qd, bid toes, lassitude, loss of energy, anorexia, weight loss, abdominal discomfort,
7. Physostigmine 0.25%, 0.5%, qd, bid diarrhea, loss of libido, impotence, unpleasant taste in the mouth, several mental
8. Demecarium bromide 0.125%, 0.25%, qd, bid depression, increased risk in formation of calcium oxylate and calcium
• Pilocarpine membrane and pilocarpine gel may be useful: phosphate renal stones, allergic reactions (sulfa derivatives), cross reactivity,
1. In some younger patients. hypokalemia, aplastic anemia, thrombocytopenia, agranulocytosis.
2. In patients bothered by variable myopia or intense miosis. • Preparations:
3. In older patients with lens opacities. 1. acetazolamide 62,5mg, 125mg, 250mg, 500mg, bid-qid (oral)
4. In patients who have difficulty complying with more frequent dosing regimen 2. acetazolamide 500mg (parenteral) 5-10mg/kg, usually ≤ 1qd q6-8hrs
• Indirect-acting agents are usually reserved for treatment of glaucoma: 3. methazolamide 25mg, 50mg, 100mg, bid, tid
1. In aphakic and pseudophakic eyes when IOP is not controlled by less toxic 4. dichlorphenamide 50mg, bid, tid
agents TOPICAL AGENTS
2. In phakic eyes when filtering surgery has failed. • Dorzolamide and brinzolamide are topical CAI agents available for chronic
treatment of IOP elevation. They reduce IOP (monotherapy) by 14%-17%.
33 Sengdy Chandra Chauhari
• Common adverse effects include bitter taste, blurred vision, punctate DIPIVEFRIN
keratopathy, and systemic lassitude. Ocular surface irritation with dorzolamide • A pro-drug that is chemically transformed into epinephrine by esterase enzymes
may be a result of the relative greater acidity (lower pH) when compared with in the cornea. Has greater corneal penetration, and its activity is relatively low.
brinzolamide. The brinzolamide solution may cause more blurring than the • Two major advantages over epinephrine salt
dorzolamide solution. 1. A lower topical concentration of dipivefrin has an intraocular effect similar to
• Preparations: a higher dosage of epinephrine salt.
1. dorzolamide 2.0%, bid, tid 2. Therapeutic effectiveness in they eye can be achieved with fewer topical and
2. brinzolamide 1%, bid, tid systemic side effects.
• Tolerated by some patients who are allergic to epinephrine salt.
NONSELECTIVE ADRENERGIC AGONISTS_________________________ • Its effectiveness may be diminished if an anticholinergic agent is added because
• Mechanism of action: increase conventional trabecular and uveoscleral outflow anticholinergic agent may prevent dipivefrin’s cleavage and activation by
• Epinephrine-related agents may initially increase aqueous production; with corneal esterases.
chronic use, they decrease it. • Preparation: 0.1%, bid
• Systemic side effects include headache, increase blood pressure, tachycardia,
arrhythmia, and nervousness. ALPHA2-ADRENERGIC AGONISTS_________________________________
• Ocular side effects • Alpha1 effects include vasoconstriction, pupillary dilation, and eyelid
1. Epinephrine causes adrenochrome deposits from oxidized metabolites in the retraction, while alpha2 effects are primarily IOP reduction and possible
conjunctiva, cornea and lacrimal system. It may stain soft contact lenses. neuroprotection.
2. Pupillary dilation as a consequence of alpha-agonist action that stimulates • Apraclonidine and brimonidine are relatively selective alpha2 agonists that have
norepinephrine receptors may precipitate or aggravate angle closure in been developed for glaucoma therapy. Brimonidine is much more highly
susceptible individuals. selective for the alpha2 receptor than apraclonidine. Apraclonidine has a much
3. Allergic blepharoconjunctivitis greater affinity for alpha1 receptor than does brimonidine.
4. Cystoid macular edema may be precipitated or exacerbated in aphakic and • Caution is recommended when using them in patients on a MAO inhibitor or
pseudophakic eyes without intact posterior capsules. tricyclic antidepressant therapy, in patients with severe cardiovascular disease,
5. Rebound conjunctiva hyperemia is common when they are discontinued. and concomitant with beta blockers, antihypertensives, and cardiac glycosides
EPINEPHRINE (alpha and beta agonist) (ophthalmic and systemic)
• Epinephrine and related compounds have less hypotensive effect in eyes with APRACLONIDINE HYDROCHLORIDE (PARA-AMINOCLONIDINE)
dark irides. • Mechanism of action
• The IOP-lowering effect begins at 1 hour and is maximal at 2-6 hours. 1. Prevents release of norepinephrine at nerve terminals.
• IOP reduction (monotherapy) by 15%-30%. 2. Decreases aqueous production and episcleral venous pressure
• Tolerance, or tachyphylaxis, is common with long-term use. 3. Improves trabecular outflow
• Epinephrine salts • May be effective for the short-term lowering of IOP (e.g., following argon laser
1. epinephrine hydrochloride → 1.0%, 2.0%, bid iridectomy, argon laser trabeculoplasty, Nd:YAG laser capsulotomy, and
2. epinephrine borate → 0.5%, 1.0%, 2.0%, bid cataract extraction)
3. epinephrine bitartrate → 2.0%, bid
34 Sengdy Chandra Chauhari
• Development of topical sensitivity and tachyphylaxis often limits long-term use. are light brown, blue-green, or two-toned may experience increased
More likely to produce vasoconstriction and can prolong iris sphincter ischemia pigmentation over the same time period.
• Preparation: 0.5%, 1.0%. bid, tid 2. Hypertrichosis of the eyelashes
BRIMONIDINE TARTRATE 3. Cystoid macular edema, uveitis, and possible herpetic keratitis.
• Encounters less tachyphylaxis in long-term use, and allergenicity such as • Topical application is performed at night to mitigate the conjunctival injection
follicular conjunctivitis and contact blepharitis-dermatitis is also lower. Cross and perhaps potentiate hypotensive effect.
sensitivity to brimonidine in patient with known hypersensitivity to • Preparation: latanoprost 0.005%, qd
apraclonidine is minimal. Less likely to induce vasoconstriction.
• Actions: COMBINED MEDICATIONS_______________________________________
1. IOP reduction, by: • Potential benefits:
• Decreased aqueous production 1. improved efficacy, convenience, and compliance
• Increased uveoscleral outflow 2. reduced cost
→ Its peak IOP reduction is approximately 26% (2 hour postdose) • Adrenergic agonists & parasympathomimetic agent (epinephrine & pilocarpine)
2. Neuroprotection, independent of IOP reduction by: • Adrenergic agonists & beta blockers (dipivefrin & levobunolol)
• Upregulation of a neurotrophin, basic fibroblast growth factor • Beta blockers & parasympathomimetic agent (timolol & pilocarpine)
• Cellular regulatory genes • Beta blockers & CAIs (timolol & dorzolamide)
• Preparation: 0.2%, bid, tid
HYPEROSMOTIC AGENTS________________________________________
PROSTAGLANDIN ANALOGUES_(PGF2α)___________________________ • Common hyperosmotic agents include:
LATANOPROST 1. Oral glycerin → 50% soln, 4-7oz
• A pro-drug that penetrates the cornea and becomes biologically active after 2. Oral isosorbide → particularly useful oral agent for diabetic patient because it
being hydrolyzed by corneal esterase. is not metabolized into sugar; 45% soln, 4-7 soln
• Mechanism of action: enhancing uveoscleral outflow. 3. Intravenous mannitol → 5.25% soln, 2 g/kg body wt
• Can reduce IOP by 25%-35%. • Used to control acute episodes of elevated IOP.
• Advantages of this agent: • Mechanism of action: Increasing the blood osmolarity → creating an osmotic
1. Once-daily dosing gradient between the blood and the vitreous humor → drawing water from the
2. Lack of cardiopulmonary effects vitreous cavity → reduction in IOP.
3. The additivity to other antiglaucoma medications except, perhaps, higher • They are rarely administered for longer than a few hours because the effects of
concentration miotic agents hyperosmotic agents are transient as a result of the rapid reequilibration of the
• Ocular side effects: osmotic gradient. They become less effective over time, and rebound elevation
1. Darkening of the iris and periocular skin in IOP may occur if the agent penetrates the eye and reverses the osmotic
→ Caused by increased numbers of melanosomes within the melanocytes. gradient.
→ The risk of iris pigmentation correlates with baseline iris pigmentation. • The larger the dose and the more rapid the administration, the greater the
Blue irides may experience increased pigmentation in 10%-20% of eyes reduction in IOP because of the increased gradient.
in the initial 18-24 months of therapy, whereas nearly 60% of eyes that
35 Sengdy Chandra Chauhari
• The substance distributed only in the extracellular water (e.g., mannitol) is more ANGLE-CLOSURE GLAUCOMA____________________________________
effective than a drug distributed in total body water (e.g., urea). • Medical treatment for acute ACG is aimed at preparing the patient for laser
• When the blood-aqueous barrier is disrupted, the osmotic agent enters the eye iridectomy. The goals of medical treatment are:
faster than when the blood-aqueous barrier is intact, thus reducing both the 1. To reduce IOP rapidly to prevent further damage to the optic nerve
effectiveness of the drug and its duration of action. 2. To clear the cornea
• Side effects include headache, mental confusion, backache, acute congestive 3. To reduce intraocular inflammation
heart failure, myocardial infarction, subdural and subarachnoid hemorrhage, 4. To allow pupillary constriction
hyperglycemia and ketaacidosis (glycerin → sugar + ketone bodies). 5. To prevent formation of posterior and PAS
• Treatment of chronic ACG is the same as POAG, although miotics may
--------------GENERAL APPROACH TO MEDICAL TREATMENT------------ induce a paradoxical increase in IOP if the angle is closed and the trabecular
meshwork is nonfunctional.
OPEN-ANGLE GLAUCOMA________________________________________
• Treatment is usually initiated with a single topical medication, unless the
starting IOP is extremely high, in which case combination therapy may be
indicated.
• A beta blocker is commonly the drug of choice for initial therapy, assuming
there is no medical contraindication. Initiation with a selective alpha2 agonist,
topical CAI, or PG analogue can also be considered.
• If one drug is not adequate to reduce IOP to the estimated desired safe level,
another agent should be tried, preferably as a therapeutic trial in one eye.
• If no single agent controls the pressure, a combination of topical agents should
be used. A beta blocker with an alpha2 agonist, topical CAI, or PG analogue
should be considered as second-line agents, and then miotic therapy followed
by systemic CAI may be used.
• Information for patients
1. How to space medications. Instructional charts.
2. How to administer eyedrops properly. Assistive drop device.
3. Eyedrops to given at the same time should be separated by at least 5 minutes
to prevent washout of the first by the second.
4. Nasolacrimal occlusion or gentle eyelid closure for 1 full minute after
instillation of the drop helps to promote corneal penetration and reduce
systemic absorption.
5. Topical and systemic side effects.
6. Compliance.
36 Sengdy Chandra Chauhari
SURGICAL THERAPY OF GLAUCOMA__________________ ------------------------LASER TRABECULOPLASTY (LTP) ------------------------
• Mechanism of action
• Surgery therapy of glaucoma is undertaken when: LTP stimulates the growth of trabecular meshwork endothelial cells → restores
1. medical therapy is not appropriate, not tolerated, not effective, or not properly trabecular meshwork function → improves the outflow facility
utilized by a particular patient • Indications
2. the glaucoma remains uncontrolled with either documented progressive 1. Patients with glaucoma on maximum tolerated medical therapy who require
damage or a very high risk of further damage. lower IOP and in whom the angle is open on gonioscopy.
• Surgery is usually the primary approach for infantile and pupillary-block 2. LTP effectively reduces IOP in patients with POAG, pigmentary glaucoma,
glaucoma. and exfoliation syndrome. Aphakic and pseudophakic eyes may respond less
• When surgery is indicated, the clinical setting must guide the selection of the favorably than phakic eyes; therefore, LTP may be more effective before than
appropriate procedure. after cataract surgery.
1. trabeculectomy and its variations 3. The role of initial LTP in POAG is at least as effective as medications for the
2. non-penetrating filtration procedures first 2 years. LTP may postpone the need for conventional surgery or
3. glaucoma drainage tube implants additional medications.
4. angle surgery for congenital glaucoma → When effective, LTP is expected to lower IOP 20%-25%.
5. ciliary body ablation. • Relative contraindications
6. iridectomy 1. Inflammatory glaucoma
7. gonioplasty 2. Membrane in the angle
3. Young patients who have developmental defects.
SURGERY FOR OPEN-ANGLE GLAUCOMA_________________________ 4. The lack of effect in the fellow eye
• Surgery is indicated when IOP cannot be maintained by nonsurgical therapies at • Preoperative evaluation
a level considered low enough to prevent further pressure-related damage to the 1. Optic nerve evaluation
optic nerve or visual field loss. Surgery has traditionally been considered only 2. Visual field examination
when medical therapy has failed and is associated with long-term risks of bleb- 3. Gonioscopy → the angle must be open. The amount of pigment in the angle
associated problems, cataracts, and infection. will help determine the laser settings for argon laser; a more pigmented angle
• The glaucoma may be uncontrolled for various reasons: responds to lower laser energy
1. Maximal medical therapy fails to adequately reduce IOP • Argon laser procedure
2. The amount of medical therapy necessary to control IOP is not well tolerance 1. Set at 300-1000 mW, 50 um, and 0.1 second.
or places the patient at unacceptable risk 2. Laser beam is focused through a goniolens at the junction of the anterior
3. Optic nerve cupping or visual field loss is progressing despite apparent unpigmented and the posterior pigmented edge of the trabecular meshwork.
“adequate” reduction of IOP with medical therapy. Laser energy was applied to the entire circumference (360˚) of the trabecular
4. The patient cannot comply with the necessary medical regimen meshwork. End point: blanching of the trabecular meshwork or production of
a tiny bubble. If a large bubble appears, the power is reduced.
3. Application to the posterior trabecular meshwork tends to produce
inflammation, pigment dispersion, prolonged elevation of IOP, and PAS.
37 Sengdy Chandra Chauhari
• Diode laser procedure: is similar; set at 600-1000 mW, 75 um, and 0.02 2. Active anterior segment neovascularization (rubeosis iridis) or active iritis →
second. the underlying problem should be addressed first, or a surgical alternative
• Complications such as tube implant surgery should be considered.
1. Transient rise in IOP (occurs in 20% of patients) → usually evident within the 3. Sustained extensive conjunctival injury or extremely thin sclera from
first 2-4 hours after treatment. Topical medications shown to blunt the IOP extensive prior surgery or necrotizing scleritis.
spikes include alpha2-agonists, beta blockers, pilocarpine, and topical CAIs. 4. Younger or aphakic/pseudophakic patients. Black patients.
Hyperosmotic agents, oral CAIs, and ice packs may be helpful in eyes with 5. Patients with uveitic glaucoma or with previously failed filtration procedures
IOP spikes not responsible to topical medication. • Preoperative evaluation
2. Low-grade iritis 1. The patient must be medically stable for an invasive ocular procedure under
3. Persistent elevation of IOP requiring filtering surgery local anesthesia.
4. Hyphema 2. Control of preoperative inflammation with corticosteroids helps to reduce
5. Formation of PAS postoperative iritis and scarring of the filtering bleb.
• Re-treatment of an angle that has been fully treated has a lower success rate and 3. Anticholinesterase agents should be discontinued if possible and replaced
a higher complication rate than does primary treatment. If initial LTP fails to temporarily by alternative medications at least 2-3 weeks before surgery to
bring IOP under control, a trabeculectomy should be considered. reduce bleeding and iridocyclitis.
4. IOP should be reduced as close as possible to normal levels before surgery is
-------------------SELECTIVE LASER TRABECULOPLASTY -------------------- performed, to minimize the risk of expulsive choroidal hemorrhage.
• Q-switched 532 nm Nd:YAG laser trabeculoplasty 5. Antiplatelet medications should be discontinued.
• The laser targets intracellular melanin 6. Systemic hypertension should be controlled.
7. Patient should be informed:
--------INCISIONAL SURGERY FOR OPEN-ANGLE GLAUCOMAS -------- • The purpose and expectations of surgery: to arrest or delay progressive
• The goal of filtering surgery (fistulizing procedure) is to create a new pathway visual loss caused by their glaucoma.
(fistula) for the bulk flow of aqueous humor from the anterior chamber through • Glaucoma surgery alone rarely improves vision.
the surgical defect in the sclera into the subconjunctival and sub-Tenon’s space. • Glaucoma medications may still be required postoperatively
• The filtering procedure most commonly used is guarded trabeculectomy. • Surgery may fail completely
• Indications: a patient with glaucoma on maximum tolerable medical therapy • Vision could be lost as a result of surgery
(MTMT) who has had maximal laser benefit and whose optic nerve function is • Glaucoma may progress despite successful surgery
failing or is likely to fail. • Patients with far advanced visual field loss or field loss that is impinging on
• The physician can determine that the patient is at MTMT only by advancing fixation are at risk for total loss of central acuity following a surgical
therapy beyond the tolerated level and documenting intolerance. An alternative procedure. The possible mechanism of this phenomenon include:
concept is core therapy, in which treatment consists of those medications likely 1. Cystoid macular edema
to work well in combination. 2. Early postoperative IOP spiking
• Relative contraindications 3. Shifting of the lamina, further compromising remaining axons
1. Blind eye → ciliary body ablation is a better alternative for lowering IOP 4. Optic nerve ischemia, possibly related to regional anesthesia
38 Sengdy Chandra Chauhari
• Trabeculectomy • A small amount of tissue should remain at the edges of the ostomy to allow
1. A guarded partial-thickness filtering procedure performed by removing a for resistance to outflow from the flap.
block of limbal tissue beneath a scleral flap. The scleral flap provides 7. Iridectomy
resistance and limits the outflow of aqueous, thereby reducing the • To lessen the risk of iris occluding the ostomy
complications associated with early hypotony (such as flat anterior chamber, • To reduce the risk of pupillary block
cataract, serous and hemorrhagic choroidal effusion, macular edema, and 8. Closure of scleral flap
optic nerve edema) • With the advent of laser suture lysis and releasable sutures, many surgeons
2. The use of antifibrotic agents (such as mitomycin-C and 5-fluorouracil), close the flap relatively tightly to avoid early shallow chambers. After a
combined with techniques of releasable sutures or laser suture lysis, enhances few days, flap sutures are released to promote filtration.
the longevity of guarded procedures. • Flow should be tested around the flap before closing the conjunctiva.
3. Succesful trabeculectomy surgery: • Leakage around the flap may be adjusted intraoperatively by the placement
• Involves reducing IOP and avoiding or managing complications of additional sutures, removal of sutures, or application of cautery to shrink
• Depends on appropriate and timely postoperative intervention to influence the wound edges.
the functioning of the filter. 9. Closure of conjunctiva
4. Complete healing of the epithelial and conjunctival wound with incomplete • Fornix-based flap → conjunctiva is secured at the limbus
healing of the scleral wound is the goal of this procedure. • Limbal-based flap → conjunctiva and Tenon’s capsule are closed
• Trabeculectomy procedures separately or in a single layer.
1. Preoperative evaluation 10. Postoperative management
2. Exposure. A corneal traction suture or superior rectus bridle suture can rotate • Topical antibiotics and corticosteroids
the globe down, giving excellent exposure of the superior sulcus and limbus. • Topical cycloplegic agents or mydriatics
3. Conjunctival wound.
• Sub-Tenon’s corticosteroids or a short course of systemic corticosteroids
• Fornix-based conjunctival flap → provides better exposure at the limbus;
• Antifibrotic agents
more difficult to achieve a water-tight closure. 1. 5-fluorouracil (5-FU), a pyrimidine analogue
• Limbal-based conjunctival flap → technically more challenging but allows
• 5-FU → deoxynucleotide 5-fluoro-2’-deoxyuridine 5’-monophosphate
for a secure closure well away from the limbus.
(FdUMP) → interferes with DNA synthesis through its action on
4. Scleral flap (3-4 mm trapezoidal or rectangular flap). thymidylate synthetase
• The flap is dissected anteriorly into clear cornea.
• Inhibits fibroblast proliferation; reduces scarring after filtering surgery.
5. Paracentesis
• 50 mg/ml on a surgical sponge is used intraoperatively.
• To control the anterior chamber through instillation of BSS or viscoelastic
• A total of 5 mg in 0.1-0.5 cc can be injected postoperatively.
• Allows for gradual lowering of IOP
2. Mitomycin-C (MMC), derived from Streptomyces caespitosus
• Intraoperative testing of the patency of the filtration site as well as of the • Acts as an alkylating agent after enzyme activation resulting in DNA cross-
integrity of the conjunctival closure.
linking.
6. Sclerotomy (with a punch or with sharp dissection).
• Most commonly administered intraoperatively by placing a surgical sponge
• The size of the ostomy is determined by the scleral flap and the amount of soaked in MMC within the subconjunctival space in contact with sclera at
overlap desired by the surgeon.
the planned trabeculectomy site.
39 Sengdy Chandra Chauhari
• Concentrations are typically between 0.2 and 0.4 mg/ml with a duration of 3. Cataract requiring extraction in a glaucoma patient requiring medications to
application from 1 to 4 minutes control IOP in whom medical therapy is poorly tolerated
3. They should be used with caution in primary trabeculectomies on young 4. Cataract requiring extraction in a glaucoma patient who requires multiple
myopic patients because of an increased risk of hypotony. medications to control IOP
• Techniques allowing tighter initial wound closure of the scleral flap help to • Contraindications
prevent early postoperative hypotony. 1. Glaucoma that requires a very low target IOP
1. The use of releasable flap sutures 2. Advanced glaucoma with uncontrolled IOP and immediate need for
2. The placement of additional sutures that can be cut postoperatively. successful reduction of IOP
3. Laser suture lysis → Glaucoma surgery alone is preferred.
• Early complications: infection, hypotony, flat anterior chamber, aqueous
misdirection, hyphema, formation or acceleration of cataract, transient IOP SURGERY FOR ANGLE-CLOSURE GLAUCOMA_____________________
elevation, cystoid macular edema, hypotony maculopathy, choroidal effusion, • The first clinical decision point following the diagnosis of ACG is to distinguish
suprachoroidal hemorrhage, persistent uveitis, dellen formation, loss of vision between angle closure based on a pupillary block mechanism and angle closure
• Late complications: leakage or failure of the filtering bleb, cataract, blebitis, based on another mechanism.
endophthalmitis (bleb infection), symptomatic bleb (dysesthetic bleb), bleb • The treatment of pupillary-block glaucoma, whether primary or secondary, is a
migration, hypotony. laser or an incisional iridectomy
• When an initial filtering procedure is not adequate to control the glaucoma and • For eyes with secondary angle closure not caused by pupillary block, an attempt
resumption of medical therapy is not successful, revision of original surgery, should be made to identify and treat underlying conditions.
repeat filtering surgery at a new site, and possibly cyclodestructive procedures
may be indicated. ---------------------------------LASER IRIDECTOMY-----------------------------------
• Indications
----------------------FULL-THICKNESS SCLERECTOMY ------------------------- 1. The presence of pupillary block
• A block of limbal tissue is removed with a punch, trephine, laser or cautery. 2. The need to determine the presence of pupillary block
• Advantages: IOP can be lowered and maintained at a lower level for long 3. To prevent pupillary block in an eye considered at risk, as determined by
periods of time. gonioscopic evaluation or because of an angle-closure attack in the fellow eye
• Disadvantages: higher incidence of postoperative flat anterior chamber, cataract, → This procedure provides an alternative route for aqueous trapped in the
hypotony, choroidal effusion, leakage of filtering blebs, and posterior chamber to enter the anterior chamber, allowing the iris to recede
endophthalmitis. from its occlusion of the trabecular meshwork.
• Contraindications: active rubeosis iridis, systemic anticoagulants consumption,
-----------COMBINED CATARACT AND FILTERING SURGERY ------------ angle closure not caused by a pupillary block mechanism
• Indications • Preoperative consideration
1. Glaucoma that is uncontrollable either medically or after laser trabeculoplasty 1. The glaucoma attack should be attempted medically, then proceed to surgery.
when visual function is significantly impaired by a cataract 2. Care should be taken to keep the iridectomy peripheral and covered by eyelid,
2. Cataract requiring extraction in a glaucoma patient who has advanced visual if possible, to avoid monocular diplopia.
field loss 3. Pilocarpine may be helpful by stretching and thinning the iris
40 Sengdy Chandra Chauhari
4. Apraclonidine or other agents can help blunt IOP spikes
• Technique ----------------INCISIONAL SURGERY FOR ANGLE-CLOSURE---------------
1. Set the argon laser at 800-1000 mW, 50 um, 0.02-0.1 second, using a • Peripheral iridectomy may be required if a patent iridectomy cannot be
condensing contact lens. There are a number of variations in technique, and achieved with a laser (cloudy cornea, flat anterior chamber, insufficient patient
iris color dictates which technique is chosen. Complications include localized cooperation)
lens opacity, acute rise in IOP, transient or persistent iritis, early closure of • Cataract extraction might be considered when pupillary block is associated
the iridectomy, and corneal and retinal burns with a visually significant cataract.
2. Q-switched Nd:YAG laser generally requires fewer pulses and less energy. • Chamber deepening and goniosynechialysis may break PAS.
The effectiveness of this laser is not affected by iris color. With a condensing
contact lens, the typical initial laser setting is 2-8 mJ. Complications include -----------------------------GLAUCOMA TUBE SHUNT-------------------------------
corneal burns, disruption of the anterior lens capsule or corneal endothelium, • Types of glaucoma drainage devices
bleeding, postoperative IOP spike, inflammation, and delayed closure of the 1. Resistance (valved) or flow-restricted devices: Krupin, Ahmed
iridectomy. 2. Nonresistance (nonvalved) devices: Molteno, Baelveldt
• Postoperative care 3. Anterior chamber tube shunt to an encircling band (ACTSEB) – Schocket
1. Bleeding → particularly with Nd:YAG laser; compression of the eye with the procedure
laser lens will tamponade the vessel, or argon laser can be used to coagulate • Indications
the vessel. 1. Trabeculectomy failure
2. IOP spikes → can be treated as described in the section on LTP 2. Failed trabeculectomy with antifibrotics
3. Inflammation → topical corticosteroids 3. Active uveitis
• Complications 4. Neovascular glaucoma
1. Focal lens damage → can be avoided by ceasing the procedure as soon as the 5. Inadequate conjunctiva
iris is penetrated 6. Impending need for penetrating keratoplasty
2. Retinal detachment → very rare, associated with Nd:YAG laser. 7. Others: poor candidate for trabeculectomy, potential for visual acuity, need
3. Bleeding and IOP spike for lower IOP
• Contraindications
----------LASER GONIOPLASTY or PERIPHERAL IRIDOPLASTY---------- 1. Eyes with very poor visual potential
• Indications 2. Patients unable to comply with self-care in the postoperative period.
1. ACG resulting from plateau iris syndrome and nanophthalmos. 3. Borderline corneal endothelial function
2. To open the angle temporarily, in anticipation of a more definitive laser or • Preoperative considerations
incisional iridectomy. 1. The status of the conjunctiva
• Contraindications: same as those for laser iridectomy 2. The health of the sclera at the anticipated tube and external reservoir sites
• Technique 3. The location of vitreous in the eye
1. Set the argon laser at 200-500 mW, 200-500 um, 0.1-0.5 second • Technique for implantation:
2. Stromal burns are created in the peripheral iris to cause contraction and 1. The superotemporal quadrant is preferred.
flattening.
41 Sengdy Chandra Chauhari
2. The extraocular plate or valve mechanism is sutured between the vertical and
horizontal rectus muscles posterior to the muscle insertions. ------------------------NONPENETRATING PROCEDURES-------------------------
3. The tube is routed anteriorly to enter in the chamber angle or through the pars 1. Deep sclerectomy with collagen implant
plana for posterior implantation in eyes that have had a vitrectomy. 2. Deep sclerectomy with injection of viscoelastic into Schlemm’s canal
4. The tube is covered with tissue such as sclera, pericardium, or dura to help (viscocanalostomy)
prevent erosion. • Involve creation of a superficial scleral flap and a deeper scleral dissection
• Postoperative management: topical steroids, antibiotics, and cycloplegics; IOP underneath to leave behind only a thin layer of sclera and Descemet’s
monitoring membrane.
• Complications: tube-corneal touch, flat chamber and hypotony, tube occlusion,
tube migration, valve malfunction, tube or plate exposure or erosion CONGENITAL OR INFANTILE GLAUCOMA________________________
--------------------CILIARY BODY ABLATION PROCEDURES------------------ ----------------------GONIOTOMY and TRABECULOTOMY-----------------------
• Procedures: cyclocryotherapy, diathermy, therapeutic ultrasound, thermal lasers • Indications: childhood glaucoma
(continuous Nd:YAG, argon, diode) • Contraindications: infants with unstable health, multiple anomalies with poor
• Goal: To reduce aqueous secretion by destroying a portion of the cilary body. prognosis and a grossly disorganized eye.
• Indications • Technique
1. Eyes that have poor visual potential or are poor candidates for incisional 1. The anterior chamber should be filled with viscoelastic to prevent collapse
surgery → generally reserved for eyes that have been or are likely to be and to tamponade bleeding.
unresponsive to other modes of therapy. 2. Goniotomy → A needle-knife is passed across the anterior chamber, and a
• Contraindications: eyes with good vision superficial incision is made in the anterior aspect of the trabecular meshwork
• Preoperative evaluation: same as for incisional glaucoma surgery under gonioscopic control.
• Postoperative management: analgesics, narcotics 3. Trabeculotomy → A fine wirelike instrument (trabeculotome) is inserted into
• Complications: prolonged hypotony, pain, inflammation, cystoid macular Schlemm’s canal from an external incision, and the trabecular meshwork is
edema, hemorrhage, phthisis bulbi torn by rotating the trabeculotome into the anterior chamber.
• Goniotomy is possible only in an eye with a relatively clear cornea, whereas
------------------------------------CYCLODIALYSIS-------------------------------------- trabeculotomy can be performed whether the cornea is clear or cloudy.
• Indications: aphakic patients who have not responses to filtering surgery.
• Techniques
1. A small scleral incision is made approximately 4 mm from the limbus.
2. A fine spatula is passed under the sclera into the anterior chamber.
3. This spatula disinserts a portion of the ciliary muscle from the scleral spur
and creates a cleft in the angle, providing direct communication between the
anterior chamber and the suprachoroidal space.
• Complications: bleeding, inflammation, cataract, stripping of Descemet’s
membrane, profound hypotony.
42 Sengdy Chandra Chauhari
Das könnte Ihnen auch gefallen
- Drug Use in Pregnancy & Lactation: Department of Pharmaceutical CareDokument39 SeitenDrug Use in Pregnancy & Lactation: Department of Pharmaceutical CareretnodwiNoch keine Bewertungen
- Regio Abdomen II.2020Dokument72 SeitenRegio Abdomen II.2020Anonymous 7rQI2K9deNoch keine Bewertungen
- JNC 8 Guideline Algorithm for Treating HypertensionDokument2 SeitenJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- GLAUCOMA American Academy of OphthalmoloDokument42 SeitenGLAUCOMA American Academy of OphthalmoloAnonymous 7rQI2K9deNoch keine Bewertungen
- Primary Angle Closure PPPDokument40 SeitenPrimary Angle Closure PPPAnonymous 7rQI2K9deNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Antibacterial Agents, NitrofuransDokument8 SeitenAntibacterial Agents, NitrofuransEmmanuel ChangNoch keine Bewertungen
- CPHQ Review Course Nov 28-29 2012Dokument195 SeitenCPHQ Review Course Nov 28-29 2012Khaskheli Nusrat100% (2)
- Assessment of Antimicrobial Activity of Cassia Fistula and Flacoartia Indica Leaves.Dokument5 SeitenAssessment of Antimicrobial Activity of Cassia Fistula and Flacoartia Indica Leaves.Eliana CaraballoNoch keine Bewertungen
- 10 0000@Www Quintpub Com@ejed@18638Dokument23 Seiten10 0000@Www Quintpub Com@ejed@18638Víctor Rodríguez67% (3)
- Shatavari (Asparagus Racemosus), Jivanti (Leptadenia Reticulata) and Methi (Trigonella Foenum-Graecum) : The Herbal Galactogogues For RuminantsDokument7 SeitenShatavari (Asparagus Racemosus), Jivanti (Leptadenia Reticulata) and Methi (Trigonella Foenum-Graecum) : The Herbal Galactogogues For RuminantsSanjay C. ParmarNoch keine Bewertungen
- Blessing IwezueDokument3 SeitenBlessing Iwezueanon-792990100% (2)
- Alconfactsheet CenturionDokument3 SeitenAlconfactsheet Centurionsudhakar.mrNoch keine Bewertungen
- Siddha Therapeutic Index - 18-Article Text-133-1-10-20210308Dokument7 SeitenSiddha Therapeutic Index - 18-Article Text-133-1-10-20210308Dr.kali.vijay kumkarNoch keine Bewertungen
- HHDBI7 W FX Xe 35 R DNJHN 6 Xsadtz 5 PQ9 ZSNI6 SXZXWDokument26 SeitenHHDBI7 W FX Xe 35 R DNJHN 6 Xsadtz 5 PQ9 ZSNI6 SXZXWleartaNoch keine Bewertungen
- Wound Management ProcedureDokument51 SeitenWound Management ProcedureSisca Dwi AgustinaNoch keine Bewertungen
- SOCA Blok 12Dokument21 SeitenSOCA Blok 12safiraNoch keine Bewertungen
- 1.agglutination ReactionDokument30 Seiten1.agglutination ReactionEINSTEIN2DNoch keine Bewertungen
- Aloe SCDokument3 SeitenAloe SCnitkolNoch keine Bewertungen
- Chapter - 3 Medical Negligence and It'S Relation With Consumer Protection Act, 1986Dokument67 SeitenChapter - 3 Medical Negligence and It'S Relation With Consumer Protection Act, 1986Soumiki GhoshNoch keine Bewertungen
- Yoga y AyurvedaDokument50 SeitenYoga y AyurvedaManuel100% (1)
- Ban Biblio NumberedDokument23 SeitenBan Biblio NumberedYayangAsanggaNoch keine Bewertungen
- Significant Prognostic Impact of Improvement in VeDokument10 SeitenSignificant Prognostic Impact of Improvement in VeFIA SlotNoch keine Bewertungen
- Ha Ema To PoiesisDokument38 SeitenHa Ema To PoiesisEmma Joel OtaiNoch keine Bewertungen
- Clinical Guidelines For Treating Caries in Adults Following A Minimal Intervention Policy-Evidence and Consensus Based Report PDFDokument11 SeitenClinical Guidelines For Treating Caries in Adults Following A Minimal Intervention Policy-Evidence and Consensus Based Report PDFFabian ArangoNoch keine Bewertungen
- SAR Training Suggested ReadingDokument1 SeiteSAR Training Suggested Readingsesse_mNoch keine Bewertungen
- Cirugia BariatricaDokument9 SeitenCirugia BariatricaedwardmenesesNoch keine Bewertungen
- Sirenomelia: A Case Report of A Rare Congenital Anamaly and Review of LiteratureDokument3 SeitenSirenomelia: A Case Report of A Rare Congenital Anamaly and Review of LiteratureInt Journal of Recent Surgical and Medical SciNoch keine Bewertungen
- Pain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalDokument50 SeitenPain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalPrathiba PrassaddNoch keine Bewertungen
- Minutes Prac Meeting 26 29 October 2020 - enDokument80 SeitenMinutes Prac Meeting 26 29 October 2020 - enAmany HagageNoch keine Bewertungen
- Disorders of Orgasm in Women A LiteraturDokument15 SeitenDisorders of Orgasm in Women A Literaturкостя100% (1)
- Med school memes that are medically funnyDokument1 SeiteMed school memes that are medically funnylostinparadise0331Noch keine Bewertungen
- Bioactive Compounds in Phytomedicine BookDokument228 SeitenBioactive Compounds in Phytomedicine BookAnil KumarNoch keine Bewertungen
- A Comparison of Muscle Strength and Flexibility Between The Preferred and Non Preferred Leg in English Soccer PlayersDokument10 SeitenA Comparison of Muscle Strength and Flexibility Between The Preferred and Non Preferred Leg in English Soccer PlayersMalikiNoch keine Bewertungen
- Pathophysiology Tia VS CvaDokument6 SeitenPathophysiology Tia VS CvaRobby Nur Zam ZamNoch keine Bewertungen
- Netter 39 S Internal Medicine 2nd Edition Pages 65, 68Dokument2 SeitenNetter 39 S Internal Medicine 2nd Edition Pages 65, 68Burca EduardNoch keine Bewertungen