Beruflich Dokumente
Kultur Dokumente
Typhoid Fever in Children Aged Less Than PDF
Hochgeladen von
Aulia NurhanifaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Typhoid Fever in Children Aged Less Than PDF
Hochgeladen von
Aulia NurhanifaCopyright:
Verfügbare Formate
Typhoid fever in children aged less than 5 years
Anju Sinha, Sunil Sazawal, Ramesh Kumar, Seema Sood, Vankadara P Reddaiah, Bir Singh, Malla Rao,
Abdolla Naficy, John D Clemens, Maharaj K Bhan
Summary Introduction
Typhoid fever is a waterborne and foodborne disorder.
Background Calculation of the incidence of typhoid fever
Unlike most other gastrointestinal infections, which
during preschool years is important to define the optimum
predominantly affect children aged 6 months to 3 years,
age of immunisation and the choice of vaccines for public-
the incidence of typhoid fever peaks between 5 and 12
health programmes in developing countries. Hospital-based
years.1 According to hospital-based data and limited
studies have suggested that children younger than 5 years
information from field studies that used passive
do not need vaccination against typhoid fever, but this view surveillance for case detection, typhoid fever is infrequent
needs to be re-examined in community-based longitudinal under 3 years of age.2–5 This finding is repeated in
studies. We undertook a prospective follow-up study of standard medical texts.6 A consequence of this
residents of a low-income urban area of Delhi, India, with epidemiological profile is that antityphoid vaccines
active surveillance for case detection. currently available have been assessed only in children of
Methods A baseline census was undertaken in 1995. school age and in older people, and the optimum age for
Between Nov 1, 1995, and Oct 31, 1996, we visited 8172
immunisation as part of public-health programmes
remains unclear.
residents of 1820 households in Kalkaji, Delhi, twice weekly
Several factors may explain the low rates of detection of
to detect febrile cases. Blood samples were obtained from
typhoid fever in preschool years. Typhoid fever may be
febrile patients, and those who tested positive for
milder or atypical in presentation at this age,3,7,8 and as
Salmonella typhi were treated with ciprofloxacin. such, it may be under-reported when case detection is
Findings 63 culture-positive typhoid fever cases were passive, as was the case in most previous studies.
detected. Of these, 28 (44%) were in children aged under 5 Subclinical or atypical presentation may be the result of
years. The incidence rate of typhoid per 1000 person-years an underdeveloped reticuloendothelial system, the nidus
was 27·3 at age under 5 years, 11·7 at 5–19 years, and 1·1 for multiplication of Salmonella typhi. Difficulties in
between 19 and 40 years. The difference in the incidence of collecting the recommended 5 mL blood from preschool
typhoid fever between those under 5 years and those aged children for conventional blood culture methods used in
endemic settings may also lead to underdiagnosis.9,10
5–19 years (15·6 per 1000 person-years [95% CI
For these reasons, it is important to re-examine the
4·7–26·5]), and those aged 19–40 years (26·2 [16·0–36·3])
incidence of typhoid fever, particularly in infants and
was significant (p<0·001 for both). The difference between
young children, by means of active surveillance11–13 and by
the incidence of typhoid at 5–19 years and the incidence at
use of isolation methods that are highly sensitive even
19–40 years was also significant (10·6 [6·3–14·8], when the amount of blood available for testing is small.
p<0·001). Morbidity in those under 5 and in older people These data would help determine a suitable age for
was similar in terms of duration of fever, signs and immunisation in public-health programmes, and would
symptoms, and need for hospital admission. enable assessment of the effectiveness of antityphoid
Interpretation Our findings challenge the common view that vaccines currently available.14
typhoid fever is a disorder of school-age children and of We therefore undertook a prospective surveillance
adults. Typhoid is a common and significant cause of study of a community-based cohort aged up to 40 years.
Blood culture for every eligible febrile episode used a
morbidity between 1 and 5 years of age. The optimum age of
medium that gives high sensitivity when only a small
typhoid immunisation and the choice of vaccines needs to
amount of blood is available for tests, as is common with
be reassessed.
preschool children.
Lancet 1999; 354: 734–37
See Commentary page 698 Methods
Study population
We studied residents of low socioeconomic status in an urban
area of Kalkaji, New Delhi, India, between Nov 1, 1995, and
Indian Council for Medical Research, Advanced Centre for Oct 31, 1996. The local climate has three distinctive seasons—a
Diarrhoeal Disease Research, Division of Paediatric hot dry summer (April–June), a wet and humid monsoon
Gastroenterology (A Sinha MD, S Sazawal MD, R Kumar MD, (July–October), and a cool dry winter (November–March).
Prof M K Bhan MD ), Department of Microbiology (S Sood MD ), and Residents of Kalkaji are migrants from neighbouring states.
Centre for Community Medicine (V P Reddaiah MD , B Singh MD), All Families live in jhuggies—clay structures with one or two rooms.
India Institute of Medical Sciences, New Delhi, India; Department 66% of water comes from hand pumps, and 34% from a piped
of International Health, School of Hygiene and Public Health, Johns supply. The drainage system for sewage and wastewater is
Hopkins University, Baltimore, MD (S Sazawal); and Department of inadequate. Typhoid immunisation is not a part of routine
Health and Human Services, National Institute of Child Health and health-care. We have undertaken continuous study of this
Human Development, Bethesda, MD, USA (M Rao MPH, population for several years, which has enabled us to establish a
A Naficy MPH, J D Clemens MD) detailed demographic sampling frame.
Correspondence to: Prof M K Bhan, Department of Pediatrics, In 1995, a computerised census of the population of Kalkaji
All India Institute of Medical Sciences, New Delhi 110-029, India showed a total of 19 585 residents living in 4361 dwellings. All
734 THE LANCET • Vol 354 • August 28, 1999
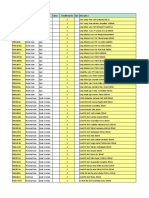
Age at follow-up Total follow-up Culture-confirmed Typhoid incidence∗ vials, respectively (Becton Dickson, MD, USA). The latter
(years) (years) cases (n) (95% CI) medium contains antibiotic absorbing resins that enhance
Under 5 1027 28 27·3 (17·2 to 37·4)
isolation of bacteria if the patient has taken antibiotics before
0–1 166 0 ·· sampling. Specimens were transported to the laboratory
>1–2 202 5 24·8 (3·1 to 46·5) immediately and processed (Bactec NR 730, Becton Dickson).
>2–3 213 11 51·6 (21·1 to 82·2) The vials were probed for growth value twice on the first 2 days,
>3–4 225 5 22·2 (2·7 to 41·7) once on day 3 and day 4, and once on day 10. Positive vials were
>4–5 221 7 31·7 (8·2 to 55·2)
Over 5–19 2743 32 11·7 (7·9 to 15·7)
subcultured on blood, MacConkey, and chocolate agar plates.
肁5–12 1579 22 13·9 (8·1 to 19·8) Smears were gram-stained, and if gram-negative bacilli were
>12–19 1164 10 8·6 (3·3 to 13·9) found, further processing was done by the Sceptor MIC/ID
Over 19–40 2684 3 1·1 (⫺0·1 to 2·4) panel (Becton Dickson) for enteric bacilli. The panel was
Total 6454 63 9·8 (7·4 to 12·2) inoculated with the Sceptor inoculator (Becton Dickson) and
*Incidence per 1000 person-years. biochemical reactions, and minimum inhibitory concentration
Table 1: Age-specific incidence of culture-confirmed typhoid endpoints were then recorded by use of the template. The results
detected by active surveillance over a 1-year period in urban of biochemical and tests of minimum inhibitory concentration
Dehli were processed by a computer that used Sceptor software
(version 3.0) to identify the most likely organism present and to
residents were assigned a unique identification number, and this
calculate confidence values. Confirmation of Salmonella spp was
gave us the sample population for the study. To ensure uniform
done by agglutination with factor O, H, and Vi antiserum
distribution of randomly selected residents throughout the
(Murex Biotech, Dartford, UK). Culture-positive typhoid was
population and to prevent biases due to case clusters, the
defined as a febrile episode that yielded S typhi in blood culture.
population was divided into clusters of 70 households with a
mean of 4·49 people per household, and 26 such clusters were
randomly selected by computer for active surveillance. Statistical analysis
Ethical approval was obtained from the Institutional Review We estimated a sample size of 8000 people for active surveillance
Boards of the All India Institute of Medical Sciences, New which would give 7000 person-years of follow-up on the
Delhi, India, and the National Institute of Child Health and assumption of 12% loss to follow-up. By enumeration of all
Development, Bethesda, MD, USA—the two participating possible outcomes from our binomial distribution, we estimated
institutions. Informed consent was obtained from the study that the follow-up of 7000 person-years would give an 85%
participants before enrolment. probability that the lower limit of the 95% CI for the incidence
of typhoid fever would be at least six cases per 1000 person-
years, assuming an incidence of ten cases per 1000 person-years.
Fieldwork
We estimated the incidence of typhoid for those people under
Between Nov 1, 1995, and Oct 31, 1996, residents in active surveillance by dividing the number of episodes by the
households selected for active surveillance were visited at home actual number of years of follow up, which was calculated to
twice a week by trained field assistants. During these visits, the allow for people to move to higher age categories. Incidence was
continuing residence status of each study participant was calculated per 1000 person-years. Age at typhoid onset was used
verified, and newcomers to the households were enrolled if they to categorise cases in age groups. We estimated 95% CIs for
proposed to stay for the duration of the study. Each resident was incidence rates and differences across age categories using
questioned about any fever. Duration of fever in children was conventional methods.15 We compared proportions using 2, 2
determined by parental assessment. People reported to be ill but for trend, and Fisher’s exact tests.
not available at the visit were revisited in the evening, as were
those households that were found locked. If residents could not
be contacted, we recorded them as “not available” until the next Results
scheduled visit. The total population number studied was 8172, of whom
When fever was reported, core body temperature was 7159 were less than 40 years old. We visited these 7159
measured by tympanic thermometer (Thermoscan Pro-LT, San initially enrolled residents at their households twice
Diego, CA, USA). Blood samples were obtained if body weekly for 12 months: 1126 were under 5 years old; 2908
temperature was 38°C or more for those 5 years or younger, aged between 5 and 19 years, and 3125 were over 19
irrespective of the duration of fever. People older than 5 years years of age. Only 11 880 (6·8%) of 174 720 visits failed
had to have had continuous fever for the past 3 days. Patients to yield morbidity information. During the year there
eligible for blood sampling were referred to the study clinic for
were 171 births and 47 deaths, and 383 people
examination by a physician and for blood sampling after
informed consent was obtained. Patients gave only one sample
outmigrated. The new births and 1798 immigrants were
during a febrile episode. included in the surveillance.
All febrile cases were followed up by a physician twice during Overall, there were 1454 febrile episodes eligible for
the first week of illness, and weekly thereafter until recovery. On blood culture. Of these, cultures were actually obtained
each follow-up visit, patients were assessed for vital signs, in 1217 cases. S typhi were isolated in 63 cases,
duration and character of fever, toxic effects, presence of salmonella other than S typhi in 24 cases, and other
palpable spleen, and other relevant physical signs. Febrile cases bacteria were isolated in 18 cases. Of the total culture-
were initially given an antipyretic and antimalarial drugs. positive S typhi cases in the cohort, 16 (25%) occurred in
Patients whose blood culture was positive for S typhi, or those children under 3 years of age and 28 (44%) in those
whose clinical profile was consistent with typhoid fever, were under 5 years. During 1 year of active surveillance, 63
treated with oral ciprofloxacin 15 mg per kg bodyweight for at
culture-positive cases were observed. The overall
least 7 days, and for 4 days after the cessation of fever.
Ciprofloxacin is currently used for primary treatment of typhoid incidence of typhoid fever in patients up to 40 years of
fever in India because multidrug resistant strains are common. age was 9·8 per 1000 person-years.
Analysis of age-specific incidence showed some
Laboratory methods unexpected results (table 1). The difference between the
Blood sampling used aseptic precautions. 3–5 mL blood was incidence of typhoid fever at age under 5 years and the
taken from patients older than 5 years, at least 2 mL blood was incidence at 5–19 years (15·6 cases per 1000 person years
taken from children under 5 years, and samples were inoculated [95% CI 4·7–26·5]) and at 19–40 years (26·2
into Bactec 26 A plus (aerobic) and Bactec red plus (aerobic) [16·0–36·3]) was significant (p<0·001). The difference
THE LANCET • Vol 354 • August 28, 1999 735
Indicator of Age Difference in p from patients under 5 years and in 47% of isolates from
severity
<5 years 肁5 years
proportions (95% CI) those older than 5 years. Sensitivity to ciprofloxacin
(n=28) (n=35) occurred in 96% of isolates from those aged under 5 years
Toxicity 18 (64%) 19 (54%) 10 (⫺34·2 to 14·2) 0·59 and 97% of isolates from those aged over 5 years. The
Splenomegaly 4 (14%) 9 (26%) ⫺12 (⫺30·9 to 8·0) 0·42 phage types of all the S typhi isolates were determined by
Diarrhoea 4 (14%) ·· ·· ··
Vomiting 1 (4%) 1 (3%) 1 (⫺9·5 to 8·1) 1·0
standard procedures at the National Reference Centre for
Hospital admission 5 (18%) 1 (3%) 15 (⫺0·2 to 30·2) 0·08 salmonella phage typing. The strains were of several
Fever duration (days) different phage types, predominantly E1 (54·7%), A
聿3 1 (4%) 1 (3%) 1 (⫺9·5 to 8·1) 0·7† (15%), and 35 (15%). All phage types were distributed
>3–7 ·· 3 (9%) ·· ··
>7–10 9 (32%) 4 (11%) 21 (⫺0·4 to 40·9) ·· evenly throughout the study area.
>10 18 (65%) 27 (77%) ⫺12 (⫺35·4 to 9·7) ·· Nine patients did not recover after a 10-day course of
Loss of 1 or more full 22 (78%) 33 (94%) ⫺16 (⫺32·7 to 1·3) 0·12 ciprofloxacin despite sensitivity to the drug in vitro.
days normal activity*
These patients were admitted to hospital and treated with
*For workers=loss of full workday, for children=loss of full day at school, for preschool
children=loss of full day of normal activity needing special attention of mother. † 2 for
ceftriaxone. Seven of the nine patients were under 5 years
trend. old.
Table 2: Severity of culture-confirmed typhoid cases detected
in active surveillance during a 1-year period in urban Delhi Discussion
between typhoid incidence at 6–19 years and later ages Our findings challenge the common view of typhoid fever
was also significant (10·6 [6·3–14·8], p<0·001). The as a disorder that affects mainly children of school age
incidence of culture-positive typhoid peaked at age and adults.16 These findings also contradict the current
3 years at 51·6 cases per 1000 person-years (95% CI view that typhoid in children under 5 years is mild and
subclinical. Typhoid infection can be a significant cause
21·1–82·2). No case was confirmed by culture in the first
of morbidity between 1 and 5 years of age. In Kalkaji,
year of life.
44% of all S typhi infections occurred in children aged
Incidence rates of typhoid varied seasonally. The
between 1 and 5 years. We suggest that current strategies
maximum incidence (18·8 cases per 1000 person-years)
for vaccination against typhoid fever need urgent review.
occurred during the monsoon (July–October), and lower
The relatively mild and atypical nature of illness related
rates of 5·4 and 4·7 per 1000 person-years occurred
to S typhi in preschool children may explain the low
during summer and winter seasons, respectively.
number of hospital admissions in this age group.3,7,8,17
We studied a dynamic population cohort, in which
However, the data on severity in our study should be
estimates of disease incidence may be biased by different
judged in the context of the early and aggressive
incidence rates among immigrants. To assess whether
treatment provided. Although we found no cases of
this bias affected our results we also calculated the
perforation and haemorrhage, our findings show that
incidence of typhoid in the fixed cohort of 6849 people
typhoid infection in young children does not cause a
for whom data were available at the beginning and the merely transient, benign bacteraemia.
end of 1 year’s surveillance. The age-specific incidence Two moderately effective and well tolerated vaccines
rates under 5 years of age in this fixed cohort (24·1 per against typhoid fever are currently available, but neither is
1000 person-years in the under 5 years, 4·5 in those older being used in public-health programmes in developing
than 5 years) were similar to the rates in the dynamic countries. Our data and experience of feasibility suggest
cohort. that the optimum age for initial immunisation against
We took blood samples from children under 5 years old typhoid in a setting such as Kalkaji is the same age as
from the first day of fever, but in older patients the measles immunisation.18 Ty21a typhoid vaccine, which
sample was obtained only after at least 3 days of fever. To has been tested for efficacy only in school children and
assess whether this method accounted for differential adults,19,20 is not suitable for large-scale use in developing
incidence rates in those under 5 and those older we countries for logistical and cost reasons. This vaccine
analysed rates of culture positively by day of fever at the requires at least three oral doses and cannot, therefore, be
time of blood collection. At 1–2 days, 3–7 days, and more given at one visit alone at 9 months of age. The Vi
than 7 days, the positivity rates in children up to 5 years polysaccharide vaccine could be given, but it is not
of age were 2·0%, 4·3%, and 30·4% respectively. In older sufficiently and durably immunogenic at this age since it
patients, blood samples were not obtained on fever days is a T-independent antigen,21 although data on this issue
1–2, and the positivity rates at 3–7 days and more than are sparse. Our findings support the need for
7 days from blood collection were 6·5% and 15·2%. In development of new vaccines such as conjugates of the Vi
both age groups, maximum culture positivity rates polysaccharide and others that may be effective when
occurred after 7 days of fever. Therefore, early blood given in late infancy.
sampling did not affect the positivity rate. The incidence of typhoid fever and the age distribution
The clinical profiles of typhoid fever in children under of cases varies between developing countries.22 Therefore,
5 years and in older patients are compared in table 2. the age patterns of typhoid fever observed in our urban
There was no significant difference in any indicators of study area may differ from those in rural areas within
typhoid severity between these two age categories. India or in other developing countries. Ferreccio and
However, typhoid fever was associated with significant colleagues3 showed a low incidence of mild typhoid in
morbidity in children under 5 years of age. 18 of 28 infants and young children in an endemic area in
patients under 5 years old had signs of toxicity, all but Santiago. Similar epidemiological data on typhoid fever
one had fever for more than 7 days despite prompt are required in different regions of the world and other
treatment, and five needed admission to hospital. developing countries to allow estimates of cost
The minimum inhibitory concentration technique effectiveness and formulation of rational public-health
showed sensitivity to chloramphenicol in 64% of isolates policy for typhoid immunisation.
736 THE LANCET • Vol 354 • August 28, 1999
Contributors 8 Arora RK, Gupta A, Joshi NM, et al Multidrug resistant typhoid fever:
Maharaj K Bhan was the principal investigator in India and was involved study of an outbreak in Calcutta. Indian Pediatr 1992; 29: 61–66.
in protocol design, study conduct, and data interpretation. Sunil Sazawal 9 Edelman R, Levine MM. Summary of an international workshop on
was involved in study conception and design, obtained all baseline data typhoid fever. Rev Infect Dis 1986; 8: 329–49.
used in defining sampling strategy, and contributed to statistical analysis 10 Mishra S, Patwari AK, Anand VK, et al. A clinical profile of multidrug
and preparation of the paper. Anju Sinha supervised the fieldwork, and resistant typhoid fever. Indian Pediatr 1991; 28: 1171–74.
assisted in data analysis and preparation of the paper. Ramesh Kumar and
11 Acharya IL, Lowe CU, Thapa R, et al. Prevention of typhoid fever in
Seema Sood supervised the laboratory work. Vankadara P Reddaiah and
Nepal with the Vi capsular polysaccharide of salmonella typhi. N Engl
Bir Singh provided statistical assistance. John D Clemens, Malla Rao, and
Abdolla Naficy, our US collaborators, helped at all stages of the study, J Med 1987; 317: 1101–04.
particularly during data analysis. 12 Klugman KP, Koornhof HJ, Schneerson R, et al. Protective activity of
Vi capsular polysaccharide vaccine against typhoid fever. Lancet 1987;
Acknowledgments ii: 1165–69.
The study was supported by the Indo-US vaccine action programme. 13 Chuttani CS, Prakash K, Vergese A, et al. Controlled field trials of
We thank Charles Lowe of NIH for help with design; Dharmendra oral killed typhoid vaccines in India. Int J Epidemiol 1972; 1: 39–43.
Kashyap for computer software development and data management; 14 Gupta A, Jalla S, Sazawal S, et al. Advances in vaccines for typhoid
Geeta Mehta of the National Reference Centre for salmonella phage fever. Indian J Pediatr 1994; 61: 321–39.
typing at the Lady Hardinge Medical College, New Delhi, India; the
15 Smith PG, Morrow RH. Methods for field trials of interventions
Department of Biotechnology, India and National Institutes of Health,
against tropical diseases: a ‘toolbox’. Oxford: Oxford University Press,
Bethesda, MD, USA, for financial support; and the Norwegian University
1991: 292–93.
Committee for Development Research and Education, for core support.
16 Levine MM, Tacket CO, Galen JE, et al. Progress in development of
new attenuated strains of Salmonella typhi as live oral vaccines against
References typhoid fever. In: Levine MM, Woodrow GC, eds. New generation
vaccines. New York: Marcel Dekker, 1997: 437–46.
1 Patnaik KC, Kapoor PN. A note on incidence of typhoid in Delhi.
Indian J Med Res 1967; 55: 228–39. 17 Middlekamp JN. Typhoid fever in infants and children. Med Times
1965; 93: 956–62.
2 Sen SK, Mahakur AC. Enteric fever—a comparative study of adult
and paediatric cases. Indian J Pediatr 1972; 39: 354–60. 18 Ivanoff B, Levine MM, Lambert PH. Vaccination against typhoid
3 Ferreccio C, Manterola A, Prenzel I, et al. Benign bacteremia caused fever: present status. Bull World Health Organ 1994; 72: 957–71.
by Salmonella typhi and parathypi in children younger than 2 years. 19 Ferreccio C, Levine MM, Rodriguez H, et al.Comparative efficacy of
J Pediatr 1984; 104: 899–901. two, three, or four doses of Ty21a live oral vaccine in enteric coated
4 Kapoor JP, Mohan M, Talwar V, et al. Typhoid fever in young capsules: a field trial in an endemic area. J Infect Dis 1989; 159:
children. Indian Pediatr 1985; 22: 811–13. 766–69.
5 Mahle WT, Levine MM. Salmonella typhi infection in children 20 Hackett J. Salmonella-based vaccines. Vaccine 1990; 8: 5–11.
younger than five years of age. Pediatr Infect Dis J 1993; 12: 627–31. 21 Plotkin SA, Cam NB. A new typhoid vaccine composed of the Vi
6 Levine MM. Typhoid fever vaccines. In: Plotkin S, Mortimer E. capsular polysaccharide. Arch Intern Med 1995; 155: 2293–99.
Vaccines (2nd ed). Philadelphia: WB Saunders, 1994: 601. 22 Simanjuntak CH, Paleologo FP, Punjabi NH, et al. Oral
7 Mulligan TO. Typhoid fever in young children. BMJ 1971; 4: immunisation against typhoid fever in Indonesia with Ty21a vaccine.
665–67. Lancet 1991; 338: 1055–59.
THE LANCET • Vol 354 • August 28, 1999 737
Das könnte Ihnen auch gefallen
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsVon EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsBewertung: 5 von 5 Sternen5/5 (9)
- Typhoid Fever in Children Aged Less Than 5 Years: The Lancet August 1999Dokument5 SeitenTyphoid Fever in Children Aged Less Than 5 Years: The Lancet August 1999Marian SplashNoch keine Bewertungen
- Management of Tuberculosis: A guide for clinicians (eBook edition)Von EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Noch keine Bewertungen
- A Study of Typhoid Fever in Five Asian Countries: Disease Burden and Implications For ControlsDokument4 SeitenA Study of Typhoid Fever in Five Asian Countries: Disease Burden and Implications For ControlsPutu SuartiniNoch keine Bewertungen
- Children at Risk of Giardiasis in Auckland: A Case-Control AnalysisDokument8 SeitenChildren at Risk of Giardiasis in Auckland: A Case-Control AnalysisMegbaruNoch keine Bewertungen
- Apid 8 2 98735Dokument5 SeitenApid 8 2 98735ko naythweNoch keine Bewertungen
- 5 SudharshanDokument5 Seiten5 SudharshaneditorijmrhsNoch keine Bewertungen
- New England Journal Medicine: The ofDokument11 SeitenNew England Journal Medicine: The ofDevina Indah PermatasariNoch keine Bewertungen
- Etiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesDokument11 SeitenEtiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesAlexandra Duque-DavidNoch keine Bewertungen
- Jurnal Imun RisaDokument11 SeitenJurnal Imun RisaYulianti Risa TonapaNoch keine Bewertungen
- Literature Review On Typhoid FeverDokument4 SeitenLiterature Review On Typhoid Feverc5h4drzjNoch keine Bewertungen
- 0148607115626921Dokument8 Seiten0148607115626921AndreannaNoch keine Bewertungen
- JCDR 10 LC08Dokument6 SeitenJCDR 10 LC08kurniawan martNoch keine Bewertungen
- Typhoid WidalDokument4 SeitenTyphoid WidalamaliamldNoch keine Bewertungen
- Original Article: Pulmonary Tuberculosis in Childhood Nephrotic Syndrome (A Cross Sectional Study)Dokument5 SeitenOriginal Article: Pulmonary Tuberculosis in Childhood Nephrotic Syndrome (A Cross Sectional Study)Maghfirah RahimaNoch keine Bewertungen
- A Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsDokument28 SeitenA Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsPatrick NunsioNoch keine Bewertungen
- 44 RevDokument14 Seiten44 RevAsshiddiqie ColectionNoch keine Bewertungen
- Jounal Siklus Anak 5Dokument6 SeitenJounal Siklus Anak 5dwi-148502Noch keine Bewertungen
- The Rationality of Antibiotics Therapy Toward Children With Typhoid Fever at M.M. Dunda HospitalDokument4 SeitenThe Rationality of Antibiotics Therapy Toward Children With Typhoid Fever at M.M. Dunda HospitalaisyahNoch keine Bewertungen
- Tuberculosis in Children Exposed at Home To MultidrugDokument12 SeitenTuberculosis in Children Exposed at Home To MultidrugElsa HasibuanNoch keine Bewertungen
- 838 3348 1 PBDokument7 Seiten838 3348 1 PBararapiaNoch keine Bewertungen
- Neonatal Group A Streptococcus Meningitis. Case Report and Literature ReviewDokument6 SeitenNeonatal Group A Streptococcus Meningitis. Case Report and Literature ReviewJessyMomoNoch keine Bewertungen
- Extensively Drug-Resistant Tuberculosis in Children With HumanDokument12 SeitenExtensively Drug-Resistant Tuberculosis in Children With Humanromeoenny4154Noch keine Bewertungen
- Immunogenicity of Fractional-Dose Vaccine During A Yellow Fever Outbreak - Preliminary ReportDokument9 SeitenImmunogenicity of Fractional-Dose Vaccine During A Yellow Fever Outbreak - Preliminary Reportrizki agusmaiNoch keine Bewertungen
- Uti PediaDokument8 SeitenUti PediaNeenya SisonNoch keine Bewertungen
- Journal GastroenteritisDokument4 SeitenJournal GastroenteritisRian KurniawanNoch keine Bewertungen
- OJMM Pattern of Acute Parasitic Diarrhoea in ChildrenDokument6 SeitenOJMM Pattern of Acute Parasitic Diarrhoea in ChildrenriskaNoch keine Bewertungen
- Association Between Age and Severity To Leptospirosis in ChildrenDokument5 SeitenAssociation Between Age and Severity To Leptospirosis in ChildrenNurafni DewiNoch keine Bewertungen
- Intestinal Parasites in Children With Diarrhea in Delhi, IndiaDokument5 SeitenIntestinal Parasites in Children With Diarrhea in Delhi, IndiaOva OlegnaNoch keine Bewertungen
- Research Article: Viral Agents of Diarrhea in Young Children in Two Primary Health Centers in Edo State, NigeriaDokument6 SeitenResearch Article: Viral Agents of Diarrhea in Young Children in Two Primary Health Centers in Edo State, NigeriariniNoch keine Bewertungen
- A Comparative Study of Typhidot and Widal Test For Rapid Diagnosis of Typhoid FeverDokument5 SeitenA Comparative Study of Typhidot and Widal Test For Rapid Diagnosis of Typhoid FeverArbusa86Noch keine Bewertungen
- Respiratory Syncytial Virus Infections in Children With Acute Myeloid Leukemia: A Report From The Children's Oncology GroupDokument3 SeitenRespiratory Syncytial Virus Infections in Children With Acute Myeloid Leukemia: A Report From The Children's Oncology GrouperickmattosNoch keine Bewertungen
- Typhoid BangladeshDokument11 SeitenTyphoid BangladeshMarindaRamadhanyNoch keine Bewertungen
- Clinical Profile of Acute BronchiolitisDokument4 SeitenClinical Profile of Acute BronchiolitisInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Clinical Profile and Outcome of Dengue Fever CasesDokument2 SeitenClinical Profile and Outcome of Dengue Fever CasesValencius SunandarNoch keine Bewertungen
- BMC Infectious DiseasesDokument7 SeitenBMC Infectious DiseasesRaffaharianggaraNoch keine Bewertungen
- 7611 193 16003 1 10 20180511 PDFDokument6 Seiten7611 193 16003 1 10 20180511 PDFUkhti Aisha Syafa Az-zahraNoch keine Bewertungen
- 7611 193 16003 1 10 20180511 PDFDokument6 Seiten7611 193 16003 1 10 20180511 PDFEltriNoch keine Bewertungen
- Incidence of Diarrhea and Contributing Factors in Nakaloke Town Council, Eastern Uganda, Among Children Below 5 Years of AgeDokument18 SeitenIncidence of Diarrhea and Contributing Factors in Nakaloke Town Council, Eastern Uganda, Among Children Below 5 Years of AgeKIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- Paediatrica Indonesiana: Darnifayanti, Guslihan Dasa Tjipta, Rusdidjas, Bugis Mardina LubisDokument5 SeitenPaediatrica Indonesiana: Darnifayanti, Guslihan Dasa Tjipta, Rusdidjas, Bugis Mardina LubisQonitina HafidhaNoch keine Bewertungen
- JurnalDokument7 SeitenJurnalRahmi SilviyaniNoch keine Bewertungen
- Mendeley 03Dokument5 SeitenMendeley 03faraNoch keine Bewertungen
- First Line FluDokument6 SeitenFirst Line Flu419022 MELA ANANDA PUTRIANANoch keine Bewertungen
- Pre-Hospital Management of Febrile Seizures in Children Seen at The University College Hospital, Ibadan, Nigeria Feature ArticleDokument5 SeitenPre-Hospital Management of Febrile Seizures in Children Seen at The University College Hospital, Ibadan, Nigeria Feature Articlechaz5727xNoch keine Bewertungen
- Nakalema Et Al IAA Journal of Biological Sciences 9 (1) :39-60, 2022. ISSN: 2636-7254 ©iaajournalsDokument22 SeitenNakalema Et Al IAA Journal of Biological Sciences 9 (1) :39-60, 2022. ISSN: 2636-7254 ©iaajournalsKIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- 12701-50629-1-PB-1 AnakDokument4 Seiten12701-50629-1-PB-1 AnakAni RoseNoch keine Bewertungen
- Multidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceDokument7 SeitenMultidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceAldy RinaldiNoch keine Bewertungen
- Sitasi Jurnal 4Dokument8 SeitenSitasi Jurnal 4ninikNoch keine Bewertungen
- Article On DengueDokument6 SeitenArticle On Dengueاحمد احمدNoch keine Bewertungen
- Epidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudyDokument9 SeitenEpidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudydouwesdNoch keine Bewertungen
- SkrofulodermaDokument4 SeitenSkrofulodermabangunazhariyusufNoch keine Bewertungen
- Apgh 2 1Dokument8 SeitenApgh 2 1Rashmi Ranjan BeheraNoch keine Bewertungen
- Cit230 PDFDokument4 SeitenCit230 PDFJoyBoyXNoch keine Bewertungen
- Community Medicine Last Moment RevisionsDokument17 SeitenCommunity Medicine Last Moment RevisionsDeepak Maini100% (2)
- Tugas Ipg UlfaDokument8 SeitenTugas Ipg UlfaUlfa Mukhlisa Putri UlfaNoch keine Bewertungen
- Adiutarini 2Dokument7 SeitenAdiutarini 2Eva Tirtabayu HasriNoch keine Bewertungen
- Jurnal 2Dokument12 SeitenJurnal 2zingioNoch keine Bewertungen
- Safety and Immunogenicity of Tetanus-Diphtheria-Acellular Pertussis Vaccine Administered To Children 10 or 11 Years of AgeDokument5 SeitenSafety and Immunogenicity of Tetanus-Diphtheria-Acellular Pertussis Vaccine Administered To Children 10 or 11 Years of AgeaulianmediansyahNoch keine Bewertungen
- Efficacy of Zinc Therapy in Acute Diarrhea in ChilDokument4 SeitenEfficacy of Zinc Therapy in Acute Diarrhea in ChilKusuma IntanNoch keine Bewertungen
- Pmid 36550736 IpiDokument6 SeitenPmid 36550736 Ipiajaya basnetNoch keine Bewertungen
- Subgroup 3Dokument12 SeitenSubgroup 3John Mervin OliverosNoch keine Bewertungen
- Concepts and Prevention of Disease PDFDokument41 SeitenConcepts and Prevention of Disease PDFAna Rika Javier Harder100% (1)
- Health and Safety CeritficationsDokument10 SeitenHealth and Safety Ceritficationsapi-384371999Noch keine Bewertungen
- Housekeeping Module 7 DaysDokument2 SeitenHousekeeping Module 7 DaysfaquinitoNoch keine Bewertungen
- Maret 18 PDFDokument178 SeitenMaret 18 PDFAnonymous vLgCd0U7Noch keine Bewertungen
- G 12 STEM HRPTA Minutes of The MeetingDokument3 SeitenG 12 STEM HRPTA Minutes of The MeetingAlvin Ray GarciaNoch keine Bewertungen
- JSA FormDokument23 SeitenJSA Formbayu dwi wkNoch keine Bewertungen
- Arrival-Registration-M7365667 Shaik Umar Farook RahamathullaDokument1 SeiteArrival-Registration-M7365667 Shaik Umar Farook Rahamathullamrcopy xeroxNoch keine Bewertungen
- Treatment of Latent Tuberculosis InfectionDokument9 SeitenTreatment of Latent Tuberculosis InfectionRoberto López MataNoch keine Bewertungen
- Knowledge Regarding Cervical Cancer Among Married Women in Rural Telangana: A Cross Sectional StudyDokument5 SeitenKnowledge Regarding Cervical Cancer Among Married Women in Rural Telangana: A Cross Sectional StudySrideviRaviNoch keine Bewertungen
- Obstetric Haemorrhage: EsmoeDokument43 SeitenObstetric Haemorrhage: EsmoeLana LocoNoch keine Bewertungen
- Association Between Prenatal Smoking and Gestational Diabetes MellitusDokument11 SeitenAssociation Between Prenatal Smoking and Gestational Diabetes Mellitusนีล ไบรอันNoch keine Bewertungen
- TrachomaDokument6 SeitenTrachomaSpislgal PhilipNoch keine Bewertungen
- ObesityDokument11 SeitenObesityDesembri Wahyuni0% (1)
- SS II.1.1 Update On Typhoid Management - Dr. Adityo Susilo, SpPD-KPTI PDFDokument34 SeitenSS II.1.1 Update On Typhoid Management - Dr. Adityo Susilo, SpPD-KPTI PDFWisnu Yudho HNoch keine Bewertungen
- Activity Sheet No. 8Dokument5 SeitenActivity Sheet No. 8Blexx LagrimasNoch keine Bewertungen
- Keyword: Acute Resporitory Infection, Under Five Children Characteristic, Physical Condition of House, Occupant BehaviorDokument10 SeitenKeyword: Acute Resporitory Infection, Under Five Children Characteristic, Physical Condition of House, Occupant BehaviorPutri Permatasari WakidiNoch keine Bewertungen
- STDs An Its Effects To The Mother and ChildDokument25 SeitenSTDs An Its Effects To The Mother and Childalixyshanjf.rvNoch keine Bewertungen
- CHN MergedDokument261 SeitenCHN MergedRej h100% (1)
- Assessment Exam Nle Enhancement Second Semester With AnswersDokument105 SeitenAssessment Exam Nle Enhancement Second Semester With AnswersPRINCESS TAHANoch keine Bewertungen
- Matriz CargaDokument80 SeitenMatriz CargaRodnei MacedoNoch keine Bewertungen
- Health Problems Illnesses Sickness Ailments Injuries Wordsearch Puzzle Vocabulary WorksheetDokument2 SeitenHealth Problems Illnesses Sickness Ailments Injuries Wordsearch Puzzle Vocabulary Worksheetpepac414100% (7)
- Early Incident Reporting TBTDokument1 SeiteEarly Incident Reporting TBTRichard SmithNoch keine Bewertungen
- Emhj 16 1 2010Dokument134 SeitenEmhj 16 1 2010Muhammad SaeedNoch keine Bewertungen
- Role of Nursing in Infection ControlDokument54 SeitenRole of Nursing in Infection Controltummalapalli venkateswara rao75% (4)
- Health Quarter 3 Grade 10Dokument5 SeitenHealth Quarter 3 Grade 10Jan Paul Santos100% (1)
- Soal B Inggris Bidan UAS Desember 2019Dokument7 SeitenSoal B Inggris Bidan UAS Desember 2019DewiBatubaraNoch keine Bewertungen
- To Be DiscussedDokument5 SeitenTo Be DiscussedJamal P. AlawiyaNoch keine Bewertungen
- Pi Is 0002937811009379Dokument9 SeitenPi Is 0002937811009379Mirza FinandarNoch keine Bewertungen
- Remarkable Story of VaccinesDokument111 SeitenRemarkable Story of Vaccinescallisto3487Noch keine Bewertungen
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (46)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4.5 von 5 Sternen4.5/5 (6)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingVon EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingBewertung: 1 von 5 Sternen1/5 (1)