Beruflich Dokumente
Kultur Dokumente
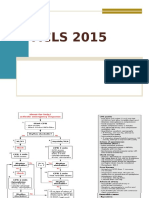
Pulseless Arrest Algorithm For Managing Asystole
Hochgeladen von
Lady MuffinsOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pulseless Arrest Algorithm For Managing Asystole
Hochgeladen von
Lady MuffinsCopyright:
Verfügbare Formate
(https://www.acls.net) Login (https://lms.acls.
net/login/)
Call us at 1-877-560-2940
Or mail support@acls.net (mailto:support@acls.net?
%20for%20ACLS%2C%20BLS%2C%20and%20PALS.%20I%27d%20also%20like%20to%20know%20more%20about%20your%20other%20medical%20courses.)
ACLS Algorithms (aclsalg.htm) / Pulseless Arrest Algorithm for Managing Asystole
Pulseless Arrest Algorithm for (https://www.facebook.com/aclstrainingcenter) (https://twitter.com/aclstraining)
Managing Asystole
Apr 27, 2018
Version control: This document is current with respect to 2015 American Heart Association® Guidelines for CPR and ECC. These guidelines are current until they are
replaced on October 2020. If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net (mailto:support@acls.net?
subject=Pulseless%20Arrest%20Algorithm%20for%20Managing%20Asystole&body=Hi%2C%20I%20had%20questions%20about%20your%20Pulseless%20Arrest%20Algorithm
for an updated document.
Management of a patient in cardiac arrest with asystole follows the same pathway as management of PEA. The top priorities stay the same: Following the steps in the ACLS
Pulseless Arrest Algorithm and identifying and correcting any treatable, underlying causes for the asystole. The algorithm assumes that scene safety has been assured,
personal protective equipment is being used, and no signs of obvious death are present.
Begin with the primary survey to assess the patient's condition:
In the absence of respirations and a pulse in the presence of asystole (present in two leads) consideration of termination of efforts should take place.
Follow the ACLS Pulseless Arrest Algorithm for asystole:
Check the patient's rhythm, taking less than 10 seconds to assess.
Verify the presence of asystole in at least two leads.
Resume CPR at a compression rate from 100-120 per minute. Rotate team members every 2 minutes with rhythm breaks to help maintain high quality CPR.
As soon as IV or IO access is available, administer epinephrine 1mg IV/IO. Do not stop CPR to administer drugs.
During CPR, search for and treat possible contributing causes (see "Reversible Causes", H's and T's in the PDF version (/images/algo-arrest.pdf)).
Check rhythm.
If no electrical activity is present (patient is in asystole), resume CPR.
If electrical activity is present, see if the patient has a pulse.
If the patient does not have a pulse or there is some doubt about the pulse, resume CPR.
If a good pulse is present and the rhythm is organized, begin post-resuscitative care.
IV/IO access is a priority over advanced airway management. If an advanced airway is placed, change to continuous chest compressions without pauses for breaths. Give 10
breaths per minute (once every 6 seconds) and check rhythm every 2 minutes.
Without a pulse or electrical activity on the ECG, the emergency care team needs to decide when resuscitation efforts should stop. The patient's wishes and the family's
concerns need to be considered.
(https://www.acls.net/judy-bio.html) Written by Judy Haluka (https://www.acls.net/judy-bio.html) and last updated May 7, 2017
© 2018 ACLS Training Center | Privacy (/privacy.html) | Terms (/terms.html) | Returns (/returns.htm)
Das könnte Ihnen auch gefallen
- ACLS Advanced Cardiovascular Life Support Provider Manual 2023Von EverandACLS Advanced Cardiovascular Life Support Provider Manual 2023Noch keine Bewertungen
- How to Apply StarkTape Kinesiology Tape. Best Kinesiology Taping TechniquesVon EverandHow to Apply StarkTape Kinesiology Tape. Best Kinesiology Taping TechniquesBewertung: 5 von 5 Sternen5/5 (1)
- ACLS Bradycardia AlgorithmDokument1 SeiteACLS Bradycardia AlgorithmLady MuffinsNoch keine Bewertungen
- ACLS PEA Asystole AlgorithmDokument3 SeitenACLS PEA Asystole AlgorithmSafira RNoch keine Bewertungen
- Basic Life Support (BLS) Primary Survey For Respiratory ArrestDokument6 SeitenBasic Life Support (BLS) Primary Survey For Respiratory ArrestRifqi MuhammadNoch keine Bewertungen
- KMR ACLS Helpful Hints 2015 Guidelines Version 1 0 Revised 1 PDFDokument2 SeitenKMR ACLS Helpful Hints 2015 Guidelines Version 1 0 Revised 1 PDFSheenaMilesNoch keine Bewertungen
- ACLS Study GuideDokument30 SeitenACLS Study GuidemmmmzNoch keine Bewertungen
- ACLS Tachycardia Algorithm For Managing Unstable TachycardiaDokument2 SeitenACLS Tachycardia Algorithm For Managing Unstable TachycardiaLady MuffinsNoch keine Bewertungen
- Xoluxezuxuve Aha Acls Manual PDF Free Download TopepuwisDokument4 SeitenXoluxezuxuve Aha Acls Manual PDF Free Download TopepuwisRidma Irsyam SeptadiNoch keine Bewertungen
- Basic Life Support and Advanced Cardiovascular Life SupportDokument90 SeitenBasic Life Support and Advanced Cardiovascular Life SupportRakhshanda khan100% (1)
- 1008 1400 ACLS - StudyGuide Print PDFDokument54 Seiten1008 1400 ACLS - StudyGuide Print PDFWaqar HassanNoch keine Bewertungen
- Pacing Week PresentationsDokument54 SeitenPacing Week PresentationsjoejenningsNoch keine Bewertungen
- (Advanced Cardiac Life Support) : ACLS Algorithms 2018Dokument18 Seiten(Advanced Cardiac Life Support) : ACLS Algorithms 2018cristina100% (1)
- ACLS-Study-Guide-2011 MADE EASYDokument2 SeitenACLS-Study-Guide-2011 MADE EASYFrances Albaña TevesNoch keine Bewertungen
- Bls and Acls-2020 Guidelines: Presented by - Unit 2 Interns Department of Medicine Kims, BBSRDokument32 SeitenBls and Acls-2020 Guidelines: Presented by - Unit 2 Interns Department of Medicine Kims, BBSRsidraNoch keine Bewertungen
- ACLS DrugsDokument4 SeitenACLS DrugsEduard Espeso Chiong-Gandul Jr.Noch keine Bewertungen
- Catheter Ablation For AFDokument12 SeitenCatheter Ablation For AFPeny Ruth Jessica DamanikNoch keine Bewertungen
- Henti JantungpptwebinarDokument28 SeitenHenti JantungpptwebinarTandangSusantoNoch keine Bewertungen
- Henti JantungpptwebinarDokument28 SeitenHenti JantungpptwebinarTandangSusantoNoch keine Bewertungen
- ACLS and MegacodeDokument33 SeitenACLS and MegacodeMark Joseph100% (1)
- 2021.06.26 L6. Resuscitation Management in Operating Theatre - Ms. Carmen LUIDokument71 Seiten2021.06.26 L6. Resuscitation Management in Operating Theatre - Ms. Carmen LUIElaine LeeNoch keine Bewertungen
- Code BlueDokument4 SeitenCode BlueKatrina JankiewiczNoch keine Bewertungen
- AclsDokument73 SeitenAclsKamel Hady50% (2)
- Defibrillation Report InputDokument8 SeitenDefibrillation Report InputChrisnel CaoileNoch keine Bewertungen
- 2014 February ALS Cardiac Arrest and ROSCDokument37 Seiten2014 February ALS Cardiac Arrest and ROSCAuliaFadhilahTasruddinNoch keine Bewertungen
- Advanced Cardiovascular Life SupportDokument16 SeitenAdvanced Cardiovascular Life SupportSarah Mohd YusofNoch keine Bewertungen
- Guidelines Adult Advanced Life SupportDokument34 SeitenGuidelines Adult Advanced Life SupportParvathy R NairNoch keine Bewertungen
- BLS, ACLS DR Dagmawi FebrauruyDokument33 SeitenBLS, ACLS DR Dagmawi FebrauruyTemesgen GeletaNoch keine Bewertungen
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDokument49 SeitenAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamNoch keine Bewertungen
- Basic Life SupportDokument6 SeitenBasic Life SupportbhongskirnNoch keine Bewertungen
- Guidelines Adult Advanced Life SupportDokument35 SeitenGuidelines Adult Advanced Life SupportindahNoch keine Bewertungen
- EXCGDokument1 SeiteEXCGTran FamNoch keine Bewertungen
- Advance Cardiovascular Life Support Recky Rahman Haqiki Fadulrahman NaufalDokument44 SeitenAdvance Cardiovascular Life Support Recky Rahman Haqiki Fadulrahman Naufalmuhammad_khan_326Noch keine Bewertungen
- Acls Study Guide 2016 For Pulse 2016Dokument8 SeitenAcls Study Guide 2016 For Pulse 2016eng78ineNoch keine Bewertungen
- Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS)Dokument35 SeitenBasic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS)rajNoch keine Bewertungen
- Pals Study GuideDokument8 SeitenPals Study Guidefredyromanreyes100% (2)
- Alteplase: Umair - M030 Farrakh - M036Dokument30 SeitenAlteplase: Umair - M030 Farrakh - M036Farrakh AliNoch keine Bewertungen
- Ischemic Stroke ManagementDokument8 SeitenIschemic Stroke ManagementBa LitNoch keine Bewertungen
- Bls - Acls Update American Heart Association 2020: Ns. Anastasia Hardyati., Mkep., Sp. KMBDokument26 SeitenBls - Acls Update American Heart Association 2020: Ns. Anastasia Hardyati., Mkep., Sp. KMBcelvin sohilait100% (1)
- ATLS Powerpoint YoDokument29 SeitenATLS Powerpoint YobharatNoch keine Bewertungen
- 2021 ACLS Study GuideDokument20 Seiten2021 ACLS Study GuideShane Brown83% (12)
- FREE 2022 ACLS Study Guide - ACLS Made Easy! PDFDokument18 SeitenFREE 2022 ACLS Study Guide - ACLS Made Easy! PDFkumar23Noch keine Bewertungen
- Anaesthetic Crisis ManualDokument63 SeitenAnaesthetic Crisis ManualkushishaNoch keine Bewertungen
- Advanced Life Support-RESSU CouncilDokument30 SeitenAdvanced Life Support-RESSU CouncilGigel DumitruNoch keine Bewertungen
- Acls 2015Dokument13 SeitenAcls 2015I Gede Aditya100% (5)
- Basic Life Support Program - Andhra Medical CollegeDokument6 SeitenBasic Life Support Program - Andhra Medical CollegeRajasekhar BandiNoch keine Bewertungen
- Asystole CaseDokument6 SeitenAsystole CaseAsep BageurNoch keine Bewertungen
- ACLS Algorithms 2020 (Advanced Cardiac Life Support)Dokument1 SeiteACLS Algorithms 2020 (Advanced Cardiac Life Support)evelyn k100% (2)
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDokument50 SeitenAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNoch keine Bewertungen
- PALS Nitty Gritty Study Guide FINALDokument11 SeitenPALS Nitty Gritty Study Guide FINALuncmikee1997100% (1)
- ACLS Exam ADokument8 SeitenACLS Exam AAgil Rumboko Sumitro100% (3)
- Ecg in Emergency: Adi SulistyantoDokument41 SeitenEcg in Emergency: Adi Sulistyantomech_pilot2203Noch keine Bewertungen
- CardiacDokument18 SeitenCardiacAya Mohamed100% (1)
- ALS Practical Assessment Tool 2018Dokument5 SeitenALS Practical Assessment Tool 2018MorganeNoch keine Bewertungen
- Code Blue (Autosaved)Dokument24 SeitenCode Blue (Autosaved)irfan taibNoch keine Bewertungen
- Dih AlteplaseDokument13 SeitenDih AlteplasewidiaNoch keine Bewertungen
- Advanced Cardiac Life Support (ACLS) Provider HandbookVon EverandAdvanced Cardiac Life Support (ACLS) Provider HandbookBewertung: 5 von 5 Sternen5/5 (1)
- M E D I C a L a B B R E V I a T I O N S D I C T I O N a R Y: (Mad)Von EverandM E D I C a L a B B R E V I a T I O N S D I C T I O N a R Y: (Mad)Noch keine Bewertungen
- اخلاق طبابتDokument230 Seitenاخلاق طبابتAziz Ahmad NaseriNoch keine Bewertungen
- Brad Blanton - Radical HonestyDokument10 SeitenBrad Blanton - Radical HonestyraduNoch keine Bewertungen
- Liposuction: Immediately After SurgeryDokument1 SeiteLiposuction: Immediately After SurgeryScott J. Zevon, MD, FACSNoch keine Bewertungen
- Bosanquet Etal DMCN 2013Dokument9 SeitenBosanquet Etal DMCN 2013ramopavelNoch keine Bewertungen
- Differential Diagnosis of Cervical CancerDokument8 SeitenDifferential Diagnosis of Cervical Cancerrey martinoNoch keine Bewertungen
- Deep Sleep ExperimentsDokument12 SeitenDeep Sleep ExperimentsCristina Lemoing100% (1)
- Tratado de Psicofarmacologia PDFDokument20 SeitenTratado de Psicofarmacologia PDFNsndndfkNoch keine Bewertungen
- MastoiditisDokument3 SeitenMastoiditisPrincess GyasiNoch keine Bewertungen
- Asuhan Keperawatan DiareDokument32 SeitenAsuhan Keperawatan Diareandreas winda adityaNoch keine Bewertungen
- Fecal Occult BloodDokument9 SeitenFecal Occult BloodRipu DamanNoch keine Bewertungen
- 2018 ESMO Handbook of Interpreting Oncological Study PublicationsDokument219 Seiten2018 ESMO Handbook of Interpreting Oncological Study PublicationsAlex Lugli100% (1)
- Jan 5, 2021 TDIR Worksheet (COG 2)Dokument122 SeitenJan 5, 2021 TDIR Worksheet (COG 2)Clarabelle Mae Dela RosaNoch keine Bewertungen
- Understanding COVID - 19 PandemicDokument10 SeitenUnderstanding COVID - 19 PandemicShyam KantNoch keine Bewertungen
- Behcet DiseaseDokument6 SeitenBehcet DiseasejbahalkehNoch keine Bewertungen
- Hili MallDokument7 SeitenHili Mallvenkatesh snkNoch keine Bewertungen
- 1 Positive Psychology Module 1Dokument7 Seiten1 Positive Psychology Module 1diether780Noch keine Bewertungen
- By Trevor Hiltbrand - Reviwed By: Free Shipping On Orders $150+ (U.S. Only.)Dokument4 SeitenBy Trevor Hiltbrand - Reviwed By: Free Shipping On Orders $150+ (U.S. Only.)Bruno ManestarNoch keine Bewertungen
- Diabetes Chart.1Dokument6 SeitenDiabetes Chart.1dr_vidyasagar41Noch keine Bewertungen
- June 2021Dokument90 SeitenJune 2021SEIYADU IBRAHIM KNoch keine Bewertungen
- Thomas Szasz On Freedom and Psychotherapy: Browse Articles & InterviewsDokument4 SeitenThomas Szasz On Freedom and Psychotherapy: Browse Articles & InterviewsGeorge RoseNoch keine Bewertungen
- Drug Study: Phinma University of PangasinanDokument1 SeiteDrug Study: Phinma University of PangasinanVoid LessNoch keine Bewertungen
- Maritime Declaration of Health: Safety Management System FormsDokument2 SeitenMaritime Declaration of Health: Safety Management System FormsTJames PaulinNoch keine Bewertungen
- Summary - Hyaline Membrane DiseaseDokument1 SeiteSummary - Hyaline Membrane DiseaseJet BautistaNoch keine Bewertungen
- CH 23 Infectious Diseases Skill WSDokument2 SeitenCH 23 Infectious Diseases Skill WSChing Man TamNoch keine Bewertungen
- Ncezid FRM Pass Attest Eng 508Dokument5 SeitenNcezid FRM Pass Attest Eng 508GO STUDY ABROAD OFFICIALNoch keine Bewertungen
- MMHA - Decriminalization & Thresholds - CPT Members - April 21, 2022Dokument6 SeitenMMHA - Decriminalization & Thresholds - CPT Members - April 21, 2022Tyler HarperNoch keine Bewertungen
- Surgery KGMU Proff Chapterwise by Arif Naseem 2009-2021Dokument4 SeitenSurgery KGMU Proff Chapterwise by Arif Naseem 2009-2021DR. PARDEEP SHARMANoch keine Bewertungen
- Group 33 Module 7 ManuscriptDokument56 SeitenGroup 33 Module 7 ManuscriptMARIA KHIM ROSE BALCITANoch keine Bewertungen
- Bacterial Vaginosis Treatment - UpToDateDokument12 SeitenBacterial Vaginosis Treatment - UpToDateAlex Esteban Espinoza CevallosNoch keine Bewertungen
- Power of Plants 1Dokument14 SeitenPower of Plants 1api-399048965Noch keine Bewertungen