Beruflich Dokumente
Kultur Dokumente
Accelerated Orthodontics
Hochgeladen von
Miguel Soni CasillasCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Accelerated Orthodontics
Hochgeladen von
Miguel Soni CasillasCopyright:
Verfügbare Formate
R evi e w A r tic le
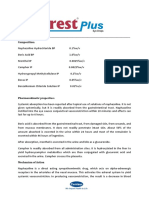
Accelerated Orthodontics – A Review
Shailesh Shenava1, 1
M.D.S, Professor and Head, Department of Orthodontics and Dentofacial Orthopaedics, Terna Dental
College and Hospital, Mumbai, India, 2M.D.S, Professor and Head, Department of Orthodontics and
U S Krishna Nayak2,
Dentofacial Orthopaedics, A.B.Shetty Memorial Institute of Dental Sciences, Mangalore, India, 3Post
Vivek Bhaskar3, Graduate Student, Department of Orthodontics and Dentofacial Orthopaedics, A.B.Shetty Memorial
Arjun Nayak4 Institute of Dental Sciences, Mangalore, India, 4Post Graduate Student, Department of Orthodontics
and Dentofacial Orthopaedics, A.B.Shetty Memorial Institute of Dental Sciences, Mangalore, India
Corresponding Author: Dr. Vivek Bhaskar, Post Graduate Student, Department of Orthodontics
and Dentofacial Orthopaedics, A.B.Shetty Memorial Institute of Dental Sciences, Mangalore, India.
E-mail: vivek.libra@gmail.com
Abstract
The duration of orthodontic treatment is the primary concern of most patients. Unfortunately, long orthodontic treatment time poses
several disadvantages like higher predisposition to dental caries, gingival recession and root resorption. Therefore this increases
the demand to find the best method to increase rate of tooth movement with the least possible disadvantages. Orthodontic
treatment is based on the premise that when force is delivered to a tooth and thereby transmitted to the adjacent investing
tissues, certain mechanical, chemical, and cellular events take place within these tissues, which allow for structural alterations
and contribute to the movement of that tooth. Conventionally, this process is slow and orthodontic treatment times can range
anywhere between 12-48 months. By enhancing the body’s response to these forces, tooth movement can be accelerated. Many
methods are available to accelerate tooth movement, such as surgical methods (corticotomy, piezosurgery etc), mechanical/
physical stimulation methods (vibration, lasers), drugs, magnets etc. These methods have been successfully proven to reduce
treatment times by up to 70%. Hence, this article aims to review the latest methods to accelerate orthodontic tooth movement.
Keywords: Accelerated orthodontic tooth movement, Corticotomy, Microosteoperforations, Lasers, Piezosurgery, Vibration
INTRODUCTION conventional corticotomy, but with reduced invasiveness
and morbidity.
Orthodontic force induces a cellular response in
the periodontal ligament, which brings about bone Mechanical or physical stimulation of the periodontal
resorption on the pressure side and bone deposition ligament has also been shown to increase the speed of bone
on the tension side. This happens via induction of remodelling. Many methods have been used for this purpose,
osteoclasts via the RANK-RANKL pathway and out of which lasers and vibration seem to show most promise.
presence of various inflammatory mediators such as They have been proven to act by inducing osteoclastogenesis
IL-1, IL-8, TNF-alpha etc.1-4 Surgical methods have by inducing the RANK/RANKL pathway and induction
been used since long to accelerate tooth movement. of signalling molecules such as MAPK (Mitogen Activated
These methods were based on the principle that when Protein Kinase), c-fos, and nitric oxide.6,7 These modalities
the bone is irritated surgically, an inflammation cascade have also been shown to reduce relapse, and pain and root
is initiated which caused increased osteoclastogenesis, resorption caused due to orthodontic forces.
hence causing faster tooth movement (Regional
Acceleratory Phenomenon or Periodontally Accelerated Methods to accelerate orthodontic tooth movement can be
Osteogenic Orthodontics). 5 However, these were broadly studied under the following categories:
invasive and not well accepted by the patients. Hence,
newer surgical methods have arrived with the help 1. Drugs.
of piezosurgery, fiberotomy, microosteoperforations 2. Surgical Methods.
etc. which achieve the same results as achieved by 3. Physical/ Mechanical stimulation methods.
35 International Journal of Scientific Study | February 2014 | Vol 1 | Issue 5
Shenava, et al.: Accelerated Orthodontics
I. Drugs spongiosa (Sebaoun et al 2008). Surgery results in
Various drugs have been used since long to accelerate a substantial increase in alveolar demineralization,
orthodontic tooth movement, and haveachieved successful a transient and reversible condition. This will result
results. 8-10 These include vitamin D, prostaglandin, in osteopenia (temporary decrease in bone mineral
interleukins, parathyroid hormone, misoprostol etc. But, density). The osteopenia enables rapid tooth movement
all of these drugs have some or the other unwanted because teeth are supported by and moved through
adverse effect. For example, vitamin D when injected in trabecular bone. As long as tooth movement continues,
the PDL increases the levels of LDH and CPK enzymes; there is prolongation of RAP. When RAP dissipates,
prostaglandin causes a generalized increase in the the osteopenia disappears and the radiographic image
inflammatory state and causes root resorption. Hence, as of of normal spongiosa reappears. Then when orthodontic
today, no drug exists that can safely accelerate orthodontic tooth movement is completed, an environment is
tooth movement. created that favors alveolar re-mineralization
• Simply stated, when bone is surgically irritated, a
II. Surgical Methods wound is created. This wound initiates a localised
• In 1931, Bichlmayr introduced a surgical technique for inflammatory response. Due to the presence of the
rapid correction of severe maxillary protrusion with inflammatory markers, osteoclasts migrate to the area
orthodontic appliances. Wedges of bone were first and cause bone resorption.
removed to reduce the volume of bone through which
the roots of the maxillary anterior teeth would need to This effect, however, is temporary, and lasts for about
be retracted. In 1959, Kole expanded on this philosophy 4 months,12 and the procedure needs to be repeated, in
by addressing additional movements, including space case faster tooth movement is still required.
closure and crossbite correction. They suggested that
bony blocks (bone-teeth unit) were created as a result of The various surgical methods available are:
the corticotomy, hence causing faster tooth movement. 1. Corticotomy
This concept prevailed till 2001, when Wilcko et al The conventional corticotomy procedure involves elevation
showed a transient demineralization-remineralization of full thickness mucoperiosteal flaps, bucally and/or
process taking place after corticotomy.11 This was lingually, followed by placing the corticotomy cuts using either
termed as PAOO (Periodontally Accelerated Osteogenic micromotor under irrigation, or piezosurgical instruments.
Orthodontics). This concept was earlier described This can be followed by placement of a graft material,
by Frost in 1983, and was called as RAP (Regional wherever required, to augment thickness of bone. In 2001,
Acceleratory Phenomenon).5 Wilcko et alreported that a surface-computed tomographic
evaluation of corticotomized patients clearly showed a
What is RAP or PAOO? How does it work? transient localized demineralization-remineralization process
• Regional Acceleratory Phenomena (RAP) is local consistent with the accelerated wound-healing pattern of the
response to a noxious stimulus, which describes a regional acceleratory phenomenon.11
process by which tissue forms faster than the normal
regional regeneration process. By enhancing the Advantages
various healing stages, this phenomenon makes healing a. It has been proven successfully by many authors, to
occur 2–10 times faster than normal physiologic accelerate tooth movement.
healing (Frost, 1983).5 b. Bone can be augmented, thereby preventing periodontal
• Many studies have reported an increase in the defects, which might arise, as a result of thin alveolar
activity of inflammatory markers such as chemokines bone.
and cytokines in response to orthodontic forces.
Chemokines play an important role in the recruitment Disadvantages13
of osteoclast precursor cells, and cytokines, directly a. High morbidity associated with the procedure.
or indirectly, through the prostaglandin E2 pathway b. Invasive procedure.
and the RANK/RANKL pathway, leading to the c. Chances of damage to adjacent vital structures.
differentiation of osteoclasts from their precursors d. Post-operative pain, swelling, chances of infection,
cells into mature osteoclasts. Therefore, it is logical to avascular necrosis.
assume that increasing the expression of these factors, e. Low acceptance by the patient.
by surgically irritating the bone should accelerate tooth
movement.1-4 • Park et al in 2006, and Kim et al in 2009, introduced the
• A histological study showed that selective alveolar corticison technique, as a minimally invasive alternative
decortication induced increased turnover of alveolar to surgically injure the bone without flap elevation.
International Journal of Scientific Study | February 2014 | Vol 1 | Issue 5 36
Shenava, et al.: Accelerated Orthodontics
They used a reinforced scalpel and mallet to go • This device comes as ready-to-use sterile disposable
through the gingiva and cortical bone. This technique device. The device has an adjustable depth dial and
did induce RAP effect, but had drawbacks such as; indicating arrow on the driver body. The adjustable
inability to place grafts, and the malleting procedure depth dial can be positioned to 0 mm, 3 mm, 5 mm, and
was shown to cause dizziness after surgery.14 7 mm of tip depth, depending on the area of operation.
Previous animal studies have shown that performing
2. Piezocision micro-osteoperforations (MOPs) on alveolar bone
• To reduce the morbidity associated with conventional during orthodontic tooth movement can stimulate
corticotomy, Dibart et al in 2009, introduced a flapless the expression of inflammatory markers, leading to
method of corticotomy, using piezosurgery.13 increases in osteoclast activity and the rate of tooth
• In the technique described by them, the surgery was movement.
performed 1 week after placement of orthodontic • Mani Alikhani et al (2013)15, performed a single center
appliance, under local anaesthesia. Gingival vertical single blinded study to investigate this procedure
incisions, only bucally, were made below the interdental on humans. They used a Ni-Ti closed coil spring,
papilla, as far as possible, in the attached gingiva delivering a constant force of 100 g to distalize the
using a No.15 scalpel. These incisions need to be maxillary canine after first premolar extraction. The
deep enough so as to pass through the periosteum, spring was anchored to a TAD distal to the second
and contact the cortical bone. Next, using ultrasonic premolar, and attached to the canine using a power
instrumentation (they used a BS1 insert Piezotome), arm through the vertical slot of the canine bracket.
to perform the corticotomy cuts to a depth of 3 mm Gingival crevicular fluid (GCF) samples were collected
through the previously made incisions. At the areas from each subject to evaluate the level of inflammatory
requiring bone augmentation, tunnelling is performed response. GCF was collected before orthodontic
using an elevator inserted between the incisions, to treatment, immediately before the start of canine
create sufficient space to accept a graft material. No retraction, and at each subsequent visit, between 10
suturing is required, except for the areas, where the AM and 12 noon. These samples were taken from
graft material needs to be stabilized. Patient is placed the distobuccal crevices of the maxillary canine. GCF
on an antibiotic, mouthwash regimen. samples were collected with filter-paper strips (Oraflow,
Smithtown, NY) inserted 1 mm below the gingival
Advantages margin into the distobuccal crevices of the canine for
a. Minimally invasive. 10 seconds. Cytokine levels were measured using a
b. Better patient acceptance. custom protein array for the following cytokines: CCL-
2 (MCP1), CCL-3, CCL-5(RANTES), IL-8 (CXCL8),
Disadvantages IL-1a, IL-1b, IL-6, and TNF-a (Raybiotech, Norcross,
a. Risk of root damage, as incisions and corticotomies Ga) according to the manufacturer’s instructions.
are “blindly” done. • Alginate impressions were taken at the beginning
of the study, immediately before canine retraction,
• To reduce the risk of root damage, however, Jorge et al and 28 days after canine retraction began to
in 2013,14 suggested a method, called MIRO (Minimally monitor the rate of tooth movement. The
Invasive Rapid Orthodontic procedure) by using impressions were immediately poured up with
metal wire as a guide to placement of the incisions, plaster (calcium sulfate). Vertical lines were drawn
and subsequently the corticotomy cuts. He placed on the cast over the palatal surface of the canine
metal guides in between each tooth, perpendicular to and lateral incisor from the middle of the incisal
the main arch wire, and took digital radiographs, to edge to the middle of the cervical line. The
ensure that the metal guides did not project over the distance between the canine and the lateral incisor
tooth roots. Once this was confirmed, incisions and was assessed before and after canine retraction at
piezoelectric corticotomy was done using the pins as 3 points: incisal, middle, and cervical thirds of the
a guide. crowns. All cast measurements were made using an
electric digital caliper (Orthopli Corp, Philadelphia,
3. Micro-Osteoperforations (MOP) Pa) with an accuracy of 0.01 mm. They concluded
• To further reduce the invasive nature of surgical their study by stating that:
irritation of bone, a device called Propel, was • MOPs significantly increased the expression
introduced by Propel Orthodontics. They called this of cytokines and chemokines known to recruit
process as Alveocentesis, which literally translates to osteoclast precursors and stimulate osteoclast
puncturing bone.15 differentiation.
37 International Journal of Scientific Study | February 2014 | Vol 1 | Issue 5
Shenava, et al.: Accelerated Orthodontics
• MOPs increased the rate of canine retraction 2.3- (model LA3D0001.1;LAMBDA S.p.A., Vicenza,
fold compared with the control group. Italy) emitting infrared radiation with a wavelength of
• Patients reported only mild discomfort locally at 808±10 nm operated according to the manufacturer’s
the spot of the MOPs. At days 14 and 28, little to recommendations. They also aimed to study the
no pain was experienced. analgesic properties of laser therapy. For analgesic
• MOPs are an effective, comfortable, and safe purposes, the settings were adjusted to a wavelength of
procedure to accelerate tooth movement during 800 nm, a continuous wave mode, an output power of
orthodontic treatment. 0.7 mW, and an exposure time of 30 seconds. For bio-
• MOPs could reduce orthodontic treatment time stimulation, the parameters were set at a wavelength
by 62%. of 800 nm, a continuous wave mode, an output power
• However, this was the first study investigating this of 0.25 mW, and an exposure time of 10 seconds.
method, and certain issues were not addressed, such The total energy density (dose) at each application
as, effect on root resorption, number of perforations was 8 J (2 × 40 s × 100 mW). After 6 months, the laser
required, long term effects (this study had a duration side (experimental) and the control side canines were
of only 28 days). examined with periapical radiographs, which showed
no undesirable changes in the adjacent periodontal
III. Physical/Mechanical Stimulation ligaments and alveolar bones. Vitality tests of the
• Surgical methods, regardless of technique, are retracted canines were also positive.
still invasive to some degree, and hence have their
associated complications. Hence, non-invasive Three models were made for each patient. On the models,
methods have come to the fore. These modalities the mesial cusp tips of first molar and the canine were the
include lasers, vibration, direct electric current etc. reference points. The distance between the first molar and
Laser the canine was measured on all 3 models for each patient
• Saito and Shimizufound that low intensity laser therapy with a digital caliper accurate to 0.02 mm. These distances
can accelerate bone regeneration in the midpalatal were recorded at T0 (after completion of alignment and
suture during rapid palatal expansion and stimulate leveling: day 1 of canine retraction), T1 (at the end of 3
the synthesis of collagen, which is major matrix months of canine retraction), and T2 (on completion of
protein in bone. In the last decade, many histologic canine retraction on the experimental side).
studies have attempted to determine the effect of
low-intensity laser therapy on the histochemical There was a highly significant positive difference in the rates
pathways directly associated with orthodontic tooth of tooth movement on the experimental side compared
movement. Increased osteoblastic and osteoclastic with the control side. The mean increase in the rates of
activity after low-level laser therapy was observed tooth movement at 3 months was 54% in the maxillary arch
in vivo and in vitro. The mechanism involved in the and 58% in the mandibular arch. Mean increase in the rate
acceleration of tooth movement is by the production of tooth movement after canine retraction was 29% in the
of ATP and activation of cytochrome C, as shown maxillary arch and 31% in the mandibular arch. There was
in that low-energy laser irradiation enhanced the a significant decrease in the pain score recorded, using a
velocity of tooth movement via RANK/RANKL Visual Analog Scale.
and the macrophage colony-stimulating factor and
its receptor expression.6 In this study, they used the semiconductor with a wavelength
• In 2004, Cruz et alwas the first to carry out a human of 800 nm, a continuous wave mode, an output power of
study on the effect of low-intensity laser therapy on 0.25 mW, and an exposure time of 10 seconds because the
orthodontic tooth movement. They showed that the results of Takedaand Bradley et alhad indicated significant
irradiated canines were retracted at a rate 34% greater bio-stimulatory effects on bone metabolism around this
than the control canines over 60 days.16 dosage, whereas higher dosages had bio-inhibitory effects,
• Gauri Doshi Mehta et al in 2013 16, in a split mouth and lower dosage showed nonsignificant results.16
design, used a laser at 800 nm for 10 sec on the
canine, both bucally and lingually, which had to be • Limpanichkul et al in 2006, however obtained a
distalized after first premolar extraction. They used result that low level laser had no additive effect on
a Ni-Ti closed coil spring delivering a constant force orthodontic tooth movement. The reason could be the
of 150 g from the first molar tube hook to the power higher energy density of 25 J per square centimeter
arm of the canine bracket and also secured with a that they used.(16)
ligature tie to the bracket. The laser type used was a • Various studies on low level laser therapy, have shown
semiconductor (aluminium gallium arsenide) diode orthodontic tooth movement to be increased by
International Journal of Scientific Study | February 2014 | Vol 1 | Issue 5 38
Shenava, et al.: Accelerated Orthodontics
30-60%. The variations amongst the studies seems REFERENCES
to arise from variations in frequency of application
of laser, intensity of laser, and method of force 1. Taddei SR, Andrade I Jr, Queiroz-Junior CM, Garlet TP, Garlet GP, Cunha
Fde Q, et al. Role of CCR2 in orthodontic tooth movement. Am J Orthod
application on the tooth. Dentofacial Orthop 2012;141:153-60.
2. Uematsu S, Mogi M, Deguchi T. Interleukin (IL)-1 beta, IL-6, tumor
Vibration necrosis factor-alpha, epidermal growth factor, and beta 2-microglobulin
levels are elevated in gingival crevicularfluid during human orthodontic
• Nishimura et al in 2008, used a Ni-Ti expansion spring tooth movement. J Dent Res 1996;75:562-7.
on the 1st molar of Wistar rats, and applied a vibration 3. Garlet TP, Coelho U, Silva JS, Garlet GP. Cytokine expression pattern
of 60 Hz, 1 m/s2. They stated that the rats that received in compression and tension sides of the periodontal ligament during
orthodontic tooth movement in humans. Eur J Oral Sci 2007;115:355-62.
the vibration showed increased orthodontic tooth
4. Bletsa A, Berggreen E, Brudvik P. Interleukin-alpha and tumor necrosis
movement. In the sectioned samples, they showed factor-alpha expression during the early phases of orthodontic tooth
increased RANKL expression in the fibroblasts and movement in rats. Eur J Oral Sci 2006;114:423-9.
osteoclasts of the periodontal ligament of the rats that 5. Frost, H. M. The regional acceleratory phenomenon: a review. Henry Ford
Hospital Medical Journal. 1983;31(1):3.
received vibration.17 6. Nimeri, G., Kau, C. H., Abou-Kheir, N. S., Corona, R. Acceleration of
• Liu et al in 2009 conducted a study on thirty mice, in tooth movement during orthodontic treatment-a frontier in Orthodontics.
which they used an omega shaped Ni-Ti expander to Progress in orthodontics. 2013;14(1):42.
7. Nishimura, M., Chiba, M., Ohashi, T., Sato, M., Shimizu, Y., Igarashi,
deliver a force of 20 g on the 1st molar. Mechanical K., Mitani, H. Periodontal tissue activation by vibration: intermittent
vibration (4 Hz for 20 min/day) was applied stimulation by resonance vibration accelerates experimental tooth
perpendicular to the occlusal surface of the first molar. movement in rats. American Journal of Orthodontics and Dentofacial
Orthopedics. 2008;133(4):572-583.
This regimen was repeated seven times, every 3 days.
8. Sekhavat, A. R., Mousavizadeh, K., Pakshir, H. R., Aslani, F. S. Effect of
Upon micro-CT examination of the jaws of the killed misoprostol, a prostaglandin E1 analog, on orthodontic tooth movement
mice, it showed that the mice that received vibration in rats. American journal of orthodontics and dentofacial orthopaedics.
showed 40% more tooth movement.18 2002;122(5): 542-547.
9. Collins, M. K., & Sinclair, P. M. The local use of vitamin D to increase the
• Recently, a product by the name Acceledent has arrived rate of orthodontic tooth movement. American Journal of Orthodontics and
at the market, which makes use of this technology. Dentofacial Orthopedics. 1988; 94(4):278-284.
This device consists of an activator, which is the 10. Bartzela, T., Türp, J. C., Motschall, E., Maltha, J. C. Medication effects
on the rate of orthodontic tooth movement: a systematic literature
active part of the appliance that delivers the vibration review. American Journal of Orthodontics and Dentofacial Orthopedics.
impulses with a USB interface through which it can be 2009;135(1):16-26.
connected to a computer to review the patient usage 11. Wilcko, W. M., Wilcko, M. T., Bouquot, J. E., Ferguson, D. J. Rapid
orthodontics with alveolar reshaping: two case reports of decrowding.
of the appliance, a mouthpiece that contacts the teeth. International Journal of Periodontics and Restorative Dentistry.
It is a portable device that can be charged similar to 2001;21(1):9-20.
any other electronic device, and has to be worn for 20 12. MOVEMENT, A. O. T. Accelerating tooth movement: The case against
minutes a day. Various case studies using this device corticotomy-induced orthodontics. American Journal of Orthodontics and
Dentofacial Orthopedics. 2013;144(1):4-13.
have shown the treatment times to be reduced by up 13. Dibart, S., Sebaoun, J. D., & Surmenian, J. Piezocision: a minimally
to 30-40%. invasive, periodontally accelerated orthodontic tooth movement procedure.
Practical Osseous Surgery in Periodontics and Implant Dentistry 2011;195.
14. Clínicas, P. E. Rapid Orthodontics with Flapless Piezoelectric Corticotomies:
First Clinical Experiences. Int. J. Odontostomat. 2013;7(1):79-85.
CONCLUSION 15. Alikhani, M., Raptis, M., Zoldan, B., Sangsuwon, C., Lee, Y. B., Alyami,
B., Teixeira, C. Effect of micro-osteoperforations on the rate of tooth
Since long, orthodontic patients have been asking for movement. American Journal of Orthodontics and Dentofacial Orthopedics.
2013;144(5):639-648.
shorter treatment times, and today, we do have methods 16. Doshi-Mehta, G., Bhad-Patil, W. A. Efficacy of low-intensity laser therapy
that can accelerate orthodontic tooth movement in reducing treatment time and orthodontic pain: a clinical investigation.
safely. The current methods such as piezocision, American Journal of Orthodontics and Dentofacial Orthopedics.
2012;141(3):289-297.
microosteoperforations, lasers and vibration have reduced 17. Nishimura, M., Chiba, M., Ohashi, T., Sato, M., Shimizu, Y., Igarashi,
or eliminated the invasive nature of previous procedures K., Mitani, H. Periodontal tissue activation by vibration: intermittent
used to achieve the Regional Acceleratory Phenomenon. stimulation by resonance vibration accelerates experimental tooth
movement in rats. American Journal of Orthodontics and Dentofacial
Also, they come with additional advantages such as
Orthopedics. 2008;133(4):572-583.
reduced rates of relapse, reduced orthodontic pain and 18. Liu D et al. Acceleration of Orthodontic tooth movement by mechanical
reduced root resorption. vibration. 2010 AADR Annual meeting Washington D.C.
How to cite this article: Shailesh Shenava, US Krishna Nayak, Vivek Bhaskar, Arjun Nayak. "Accelerated Orthodontics – A Review".
International Journal of Scientific Study. 2014;1(5):35-39.
Source of Support: Nil, Conflict of Interest: None declared.
39 International Journal of Scientific Study | February 2014 | Vol 1 | Issue 5
Das könnte Ihnen auch gefallen
- Psychiatric Case History NotesDokument8 SeitenPsychiatric Case History NotesTysle100% (1)
- Parental Alienation Is SERIOUS Child Abuse 2018 Wilfrid Von Boch-Galhau Parental Alienation Is in The DSMDokument15 SeitenParental Alienation Is SERIOUS Child Abuse 2018 Wilfrid Von Boch-Galhau Parental Alienation Is in The DSML9at100% (6)
- Principles of Transactional Analysis - by Eric BerneDokument8 SeitenPrinciples of Transactional Analysis - by Eric BernecornelpcNoch keine Bewertungen
- Functional ApplianceHGHDFGDokument40 SeitenFunctional ApplianceHGHDFGmustafa_tambawalaNoch keine Bewertungen
- V-Bend and Anchorage in Orthodontics: Mehak Arya Iyrmds Dept of OrthodonticsDokument37 SeitenV-Bend and Anchorage in Orthodontics: Mehak Arya Iyrmds Dept of OrthodonticsMehak AryaNoch keine Bewertungen
- Self LigationDokument2 SeitenSelf Ligationdavidrocks81Noch keine Bewertungen
- Supplementary DIagnostic AidsDokument186 SeitenSupplementary DIagnostic AidsRajshekhar Banerjee100% (1)
- Margaret Moore Bob Tschannen-Moran Erika JacksonDokument201 SeitenMargaret Moore Bob Tschannen-Moran Erika JacksonBella100% (18)
- Finishing and Detailing: The Keys to Ideal OcclusionDokument92 SeitenFinishing and Detailing: The Keys to Ideal Occlusiontanmayi minniNoch keine Bewertungen
- Curing Lights in OrthodonticsDokument31 SeitenCuring Lights in OrthodonticsPerthish sharmaNoch keine Bewertungen
- Vertical Maxillary ExcessDokument125 SeitenVertical Maxillary ExcessYuvashreeNoch keine Bewertungen
- CROSSBITE According To GraberDokument29 SeitenCROSSBITE According To GraberAslamCv100% (1)
- Saudi Prometric Latest Questions AndanswerDokument67 SeitenSaudi Prometric Latest Questions AndanswerGloria Jaison100% (4)
- Adult Orthodontics SeminarDokument52 SeitenAdult Orthodontics Seminaravanthika krishnaraj100% (2)
- Lingual orthodontics (LO) versus buccal orthodontics (BO): biomechanical and clinical differencesDokument8 SeitenLingual orthodontics (LO) versus buccal orthodontics (BO): biomechanical and clinical differencesenzorodriguez50% (2)
- Thesis LDDokument4 SeitenThesis LDashishNoch keine Bewertungen
- Retention and Relapse SeminarDokument51 SeitenRetention and Relapse SeminarShabeel Pn100% (2)
- Roth Vs MBT PDFDokument8 SeitenRoth Vs MBT PDFandiiperezNoch keine Bewertungen
- Begg's and Tip Edge PhilosophyDokument74 SeitenBegg's and Tip Edge PhilosophyNeel Lalmani MauryaNoch keine Bewertungen
- History of Science and Technology in The PhilippinesDokument12 SeitenHistory of Science and Technology in The PhilippinesQuerobin Gampayon100% (1)
- Loop MechanicsDokument9 SeitenLoop MechanicsMohammed HussainNoch keine Bewertungen
- Root Resorption Causes and AssessmentDokument89 SeitenRoot Resorption Causes and AssessmentRajshekhar BanerjeeNoch keine Bewertungen
- Construction Bite / Orthodontic Courses by Indian Dental AcademyDokument62 SeitenConstruction Bite / Orthodontic Courses by Indian Dental Academyindian dental academyNoch keine Bewertungen
- Skeletal Anchorage Systems in Orthodontics Absolute Anchorage Adream or RealityDokument10 SeitenSkeletal Anchorage Systems in Orthodontics Absolute Anchorage Adream or RealitySoe San KyawNoch keine Bewertungen
- 9-Miniscrews in Orthodontics Biomechanics-Case Report-Oussama Sandid - Mohamad Aboualnaser-Awatef Shaar-Miniscrews Mini-Implant en Orthodontie PDFDokument19 Seiten9-Miniscrews in Orthodontics Biomechanics-Case Report-Oussama Sandid - Mohamad Aboualnaser-Awatef Shaar-Miniscrews Mini-Implant en Orthodontie PDFAnonymous oD9H6T8p100% (1)
- Functional Matrix HypothesisDokument14 SeitenFunctional Matrix Hypothesispriyab710Noch keine Bewertungen
- Beggs Philosophy Ortho / Orthodontic Courses by Indian Dental AcademyDokument81 SeitenBeggs Philosophy Ortho / Orthodontic Courses by Indian Dental Academyindian dental academyNoch keine Bewertungen
- Intrusion Arches ShinuDokument66 SeitenIntrusion Arches ShinuYuvashreeNoch keine Bewertungen
- Tweed - A Philosophy of Orthodontic TreatmentDokument30 SeitenTweed - A Philosophy of Orthodontic TreatmentriofrankfurtNoch keine Bewertungen
- Beggs TechniqueDokument24 SeitenBeggs TechniqueGAURAV VARMANoch keine Bewertungen
- Biomechanics and Types of Movement 9b670d85Dokument41 SeitenBiomechanics and Types of Movement 9b670d85NamBuiNoch keine Bewertungen
- Bioprogressive Therapy: DR Hiten KalraDokument100 SeitenBioprogressive Therapy: DR Hiten Kalralingual courseNoch keine Bewertungen
- Uttar Pradesh Empanelment List for Minilap 2018-19Dokument19 SeitenUttar Pradesh Empanelment List for Minilap 2018-19Vijay KumarNoch keine Bewertungen
- Orthodontic Handbook for Dental AssistantsVon EverandOrthodontic Handbook for Dental AssistantsBewertung: 1 von 5 Sternen1/5 (1)
- Roth Versus MBTDokument23 SeitenRoth Versus MBTJose Antonio Figuroa AbadoNoch keine Bewertungen
- Friction in OrthodonticsDokument71 SeitenFriction in OrthodonticsNimisha SharmaNoch keine Bewertungen
- The Necessity of Gnathostatic Diagnoses in Orthodontic PracticeDokument15 SeitenThe Necessity of Gnathostatic Diagnoses in Orthodontic Practicesauriua100% (1)
- Edgewise AppDokument27 SeitenEdgewise AppReshamIrshadNoch keine Bewertungen
- Various Intrusive ArchsDokument10 SeitenVarious Intrusive ArchsmutansNoch keine Bewertungen
- Muscle Physiology / Orthodontic Courses by Indian Dental AcademyDokument93 SeitenMuscle Physiology / Orthodontic Courses by Indian Dental Academyindian dental academyNoch keine Bewertungen
- Centre of Resistance of MaxillaDokument2 SeitenCentre of Resistance of MaxillasameerorthoNoch keine Bewertungen
- Extraction Vs Non Extraction Controversy: A Review: January 2018Dokument9 SeitenExtraction Vs Non Extraction Controversy: A Review: January 2018Jawad TariqNoch keine Bewertungen
- Intrusion ArchDokument105 SeitenIntrusion Archaa bbNoch keine Bewertungen
- Kriya For Balancing The ChakrasDokument5 SeitenKriya For Balancing The ChakrasFedra Fox Cubeddu100% (2)
- ANCHORAGE CONTROL IN ORTHODONTICSDokument83 SeitenANCHORAGE CONTROL IN ORTHODONTICSMothi KrishnaNoch keine Bewertungen
- Orthodontics in the Vertical Dimension: A Case-Based ReviewVon EverandOrthodontics in the Vertical Dimension: A Case-Based ReviewNoch keine Bewertungen
- Few ControversiesDokument9 SeitenFew Controversieshassankhan9849Noch keine Bewertungen
- Scissors Bite-Dragon Helix ApplianceDokument6 SeitenScissors Bite-Dragon Helix ApplianceGaurav PatelNoch keine Bewertungen
- Paradigm Shift in Orthodontics PDFDokument28 SeitenParadigm Shift in Orthodontics PDFHardiklalakiya0% (1)
- Biomechanics of Deep Bite TreatmentDokument66 SeitenBiomechanics of Deep Bite TreatmentMaitreye PriyadarshiniNoch keine Bewertungen
- Diagnostic Elements For Tooth Extraction in OrthodonticsDokument24 SeitenDiagnostic Elements For Tooth Extraction in OrthodonticsLanaNoch keine Bewertungen
- Friction in OrthodonticsDokument9 SeitenFriction in Orthodonticsaa bbNoch keine Bewertungen
- Functional Occlusion in Orthodontics: ClinicalDokument11 SeitenFunctional Occlusion in Orthodontics: ClinicalNaeem MoollaNoch keine Bewertungen
- Evolution of Treatment Mechanics PDFDokument9 SeitenEvolution of Treatment Mechanics PDFJunaid Israr - OrthodonticsNoch keine Bewertungen
- Extractions in Orthodontics: An Update on Indications and PatternsDokument10 SeitenExtractions in Orthodontics: An Update on Indications and Patternsdrzana78100% (1)
- Asymmetric Headgear 2Dokument5 SeitenAsymmetric Headgear 2Ali HmoudNoch keine Bewertungen
- Occlusion - DevelopmentDokument33 SeitenOcclusion - Developmentsameerortho100% (1)
- Molar UprightingDokument8 SeitenMolar UprightingNguyen AnhNoch keine Bewertungen
- KLoop Molar Distalizing AppDokument7 SeitenKLoop Molar Distalizing AppAngie Römer HaroNoch keine Bewertungen
- Attachments & Auxiliaries in Begg's TechniqueDokument117 SeitenAttachments & Auxiliaries in Begg's TechniqueswapniljunnarkarNoch keine Bewertungen
- The Snail Loop For Low-Friction Space Closure PDFDokument3 SeitenThe Snail Loop For Low-Friction Space Closure PDFAthira JithendranathNoch keine Bewertungen
- P.R. Begg - Peter C. Kesling - The Differential Force Method of Orthodontic TreatmentDokument39 SeitenP.R. Begg - Peter C. Kesling - The Differential Force Method of Orthodontic TreatmentNizam Muhamad100% (1)
- Spaceclosurebyfrictionlessmechanics2 140303231146 Phpapp01Dokument109 SeitenSpaceclosurebyfrictionlessmechanics2 140303231146 Phpapp01Nadia YactayoNoch keine Bewertungen
- 1947 Howes CASE ANALYSIS AND TREATMENT PLANNING BASED UPON THE Relationship of Tooth Material To Its Supporting BoneDokument35 Seiten1947 Howes CASE ANALYSIS AND TREATMENT PLANNING BASED UPON THE Relationship of Tooth Material To Its Supporting BoneRockey ShrivastavaNoch keine Bewertungen
- Ideal Arch Force Systems - A Center-Of-resistance PerspectiveDokument9 SeitenIdeal Arch Force Systems - A Center-Of-resistance PerspectivemutansNoch keine Bewertungen
- Anchorage in OrthodonticsDokument123 SeitenAnchorage in Orthodonticsdrimtiyaz123Noch keine Bewertungen
- Fixed Orthodontic Appliances: A Practical GuideVon EverandFixed Orthodontic Appliances: A Practical GuideBewertung: 1 von 5 Sternen1/5 (1)
- EORTC QLQ-C30 Into Indonesian VersionDokument11 SeitenEORTC QLQ-C30 Into Indonesian VersionHendryNoch keine Bewertungen
- Latest Guideline on Caries-risk Assessment and ManagementDokument8 SeitenLatest Guideline on Caries-risk Assessment and ManagementPriscila Belén Chuhuaicura SotoNoch keine Bewertungen
- Chemicals Zetag MSDS Powder Zetag 4139 - 1010Dokument6 SeitenChemicals Zetag MSDS Powder Zetag 4139 - 1010PromagEnviro.comNoch keine Bewertungen
- Psychology All Case Studies PDFDokument54 SeitenPsychology All Case Studies PDFArmeen AmirNoch keine Bewertungen
- Ocurest Plus2018Dokument4 SeitenOcurest Plus2018rotastrainNoch keine Bewertungen
- Continuous Passive Motion (CPM) : Theory and Principles of Clinical ApplicationDokument10 SeitenContinuous Passive Motion (CPM) : Theory and Principles of Clinical ApplicationlaurentiaNoch keine Bewertungen
- Nuclear Associates User ManualDokument20 SeitenNuclear Associates User ManualvandarsNoch keine Bewertungen
- Microsoft Word Document جديدDokument3 SeitenMicrosoft Word Document جديدHisham EssamNoch keine Bewertungen
- Beta Blockers: Selective and Non-Selective TypesDokument22 SeitenBeta Blockers: Selective and Non-Selective TypesJewelyn ConolNoch keine Bewertungen
- Register Now for the 3rd Hematology Forum 2023Dokument1 SeiteRegister Now for the 3rd Hematology Forum 2023modather sanosiNoch keine Bewertungen
- American Society For Biochemistry and Molecular BiologyDokument23 SeitenAmerican Society For Biochemistry and Molecular BiologyShishui UchihaNoch keine Bewertungen
- Huntingtons Disease ProjectDokument9 SeitenHuntingtons Disease Projectapi-306544419Noch keine Bewertungen
- PCRL 627: Clinical Microbiology and Immunology 2016: Email: Shilling@uic - EduDokument45 SeitenPCRL 627: Clinical Microbiology and Immunology 2016: Email: Shilling@uic - Edui24youNoch keine Bewertungen
- A Brief History of Evidence-Based Medicine in Four PeriodsDokument31 SeitenA Brief History of Evidence-Based Medicine in Four PeriodsSaad MotawéaNoch keine Bewertungen
- 53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Dokument9 Seiten53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Dina AyupnNoch keine Bewertungen
- Essential hygiene and safety practices for body, home and cookingDokument3 SeitenEssential hygiene and safety practices for body, home and cookingNorma Nieves QuesadaNoch keine Bewertungen
- NUS Medicine Admission Brochure 2019Dokument12 SeitenNUS Medicine Admission Brochure 2019Glenden KhewNoch keine Bewertungen
- Detyre Kursi: Lenda:AnglishtDokument11 SeitenDetyre Kursi: Lenda:AnglishtFjorelo FeroNoch keine Bewertungen
- Synthesis of Novel Amino Acid Derivative of 7-AVCADokument4 SeitenSynthesis of Novel Amino Acid Derivative of 7-AVCAIOSRjournal0% (1)
- Mayo HospitalDokument1 SeiteMayo HospitalTooba SaeedNoch keine Bewertungen
- MSWORD PronunciationDokument3 SeitenMSWORD PronunciationStephen ThomsonNoch keine Bewertungen
- Bapat Et Al. - 2006 - Quantification of Metabolically Active Biomass Using Methylene Blue Dye Reduction Test (MBRT) Measurement of CFU IDokument10 SeitenBapat Et Al. - 2006 - Quantification of Metabolically Active Biomass Using Methylene Blue Dye Reduction Test (MBRT) Measurement of CFU IJosé Matías ZapiolaNoch keine Bewertungen