Beruflich Dokumente
Kultur Dokumente
477556
Hochgeladen von
reneOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
477556
Hochgeladen von
reneCopyright:
Verfügbare Formate
Commentary
Acta Cytologica 2017;61:359–372 Received: May 17, 2017
Accepted after revision: May 18, 2017
DOI: 10.1159/000477556
Published online: July 11, 2017
The Bethesda System for Reporting
Cervical Cytology: A Historical Perspective
Ritu Nayar a David C. Wilbur b
a
Department of Pathology, Northwestern University Feinberg School of Medicine and Northwestern Medicine,
Chicago, IL, and b Department of Pathology, Massachusetts General Hospital and Harvard Medical School,
Boston, MA, USA
Keywords have carried on the legacy of this seminal work, even as mo-
The Bethesda System · Reporting terminology · Pap test · lecular methods are being closely integrated into cervical
Cervical cytology cancer screening, triage, and prevention.
© 2017 S. Karger AG, Basel
Abstract
The aims of The Bethesda System (TBS) were to provide ef- The Bethesda System (TBS) was the direct result of a
fective communication from the laboratory to the clinical series of articles published in 1987 in The Wall Street Jour-
provider; facilitate cytologic-histologic correlation; facilitate nal by investigative reporter Walt Bogdanich, about lax
research into the epidemiology, biology, and pathology of practices and inaccuracies in medical laboratories. In
cervical disease; and provide reproducible and reliable data spite of the well-accepted contribution of the Papanico-
for national and international statistical analysis compari- laou (Pap) test in reducing the incidence of cervical can-
sons. Dr. Diane Solomon and colleagues’ contribution to cer- cer, much of this breaking news focused on so called “Pap
vical cancer screening, diagnosis, and management began mills” in which cervical cytology specimens were being
with the inception and dissemination of TBS for reporting processed under less than optimal conditions. Public out-
cervical cytology in 1988, as detailed in the accompanying cry and legislative action ensued. In response to the pub-
article [Solomon et al.: Acta Cytol 1989;33:567–574]. The sig- lic’s concerns about the quality of laboratory testing, par-
nificance of TBS for the further development and implemen- ticularly in physician’s office laboratories and concerning
tation of standardized terminology in pathology, and the re- Pap test interpretation, the US Congress passed the Clin-
search/management of cervical cancer have continued to ical Laboratory Improvement Amendments (CLIA) in
evolve over the past three decades. TBS has always been a 1988. The CLIA detailed a number of quality assurance
multidisciplinary effort and acknowledgement needs to be practices that laboratories must comply with, based on
given to several stakeholders who, over the years, have con- the type and complexity of testing they perform.
tributed to its success. It has been our privilege and honor to
© 2017 S. Karger AG, Basel Correspondence to: Dr. Ritu Nayar
Northwestern Memorial Hospital
Cytopathology Galter 7–132B, 251 East Huron Street,
E-Mail karger@karger.com
Chicago, IL 60611 (USA)
www.karger.com/acy
E-Mail r-nayar @ northwestern.edu
Prior to TBS, US laboratories used a variety of nonre- er reproducibility over that seen with 3-tier systems. A
producible terms for reporting cervical cytology includ- major component of TBS 1988 was a clarification of the
ing Pap test class numbers (which were completely non- misunderstood term “atypia.” As an equivocal finding,
descriptive) amongst other terminologies, e.g., 3-tier dys- atypia had been overused and applied in a highly incon-
plasia (mild/moderate/severe, or carcinoma in situ) and sistent manner, leading to considerable confusion about
cervical intraepithelial neoplasia (CIN). Much was made its appropriate management. In TBS, atypia was specifi-
of the clinically and biologically irrelevant morphologic cally defined to include only cases in which the cytologic
distinctions between human papillomavirus (HPV) cyto- findings were of “undetermined significance”; the term
pathic effects and low-grade dysplasia as well as the non- was not to be used for cases in which inflammatory, reac-
reproducible distinction between the grades of precancer, tive, preneoplastic, or neoplastic changes were clearly
and these differences were often used as a clinical thresh- present. This definition was also applied to cases of glan-
old for significant interventions. To address these issues, dular epithelial abnormality. This gave rise to the now-
the National Cancer Institute (NCI) convened a work- familiar terms “atypical squamous cells of undetermined
shop, under the leadership of Drs. Diane Solomon and significance” (ASCUS) and “atypical glandular cells of
Robert Kurman, with the aim of developing a system for undetermined significance” (AGUS).
reporting Pap tests that would communicate the cytology Within a few years of its introduction, TBS gained
findings to clinicians in a clear and relevant fashion. A widespread acceptance in clinical practice in the USA
group of individuals, with expertise in gynecologic cyto- and, thereafter, internationally. Encouraged by the early
pathology, histopathology, and patient management, met benefits of this new standardized terminology, the NCI
in Bethesda, MD, USA, in December 1988, and formu- organized a follow-up workshop in Bethesda, MD, in
lated the first version of TBS [1]. This lexicon for practice April 1991 to critically evaluate TBS and consider areas
was founded on 3 basic principles that continue to hold for improvement. The 1991 Workshop was attended by
true today – 3 decades and 3 updates later! Terminology 182 invited experts in cytopathology and gynecology, and
must be (1) clinically relevant, (2) reasonably reproduc- approximately 65 presentations were made by various
ible and flexible, and (3) reflect the most current under- laboratories to share experiences regarding the use of TBS
standing of cervical neoplasia. in clinical practice. The discussions resulted in the refine-
TBS 1988 created a standardized framework for cervi- ment of the report format and terminology, and the de-
cal cytology reports that included an evaluation of speci- velopment of precise criteria for the evaluation of adequa-
men adequacy, an optional general categorization, and a cy and specific diagnostic terms. A discussion about the
descriptive diagnosis. The inclusion of recommendations management of abnormalities detected by cervical cytol-
for adequacy limitations or elaborations on morphologic ogy acknowledged the need to have clinical trial data to
findings to guide management, as appropriate, was sug- help in development, so interim management guidelines
gested. The introduction of adequacy has been consid- were published in 1991 which would be finalized after
ered by many to be the most important quality assurance further data was gathered. The updates were presented to
component of TBS. The general categorization, although the cytopathology community in the form of the first
optional, clearly separated “normal” from “abnormal” re- Bethesda Atlas “blue book” in 1994 [2].
ports and is aimed at assisting clinical providers in triag- Of all the changes introduced by TBS, the concept of
ing reports for subsequent patient management. The de- ASCUS proved to be by far the most controversial for cli-
scriptive diagnosis, on the other hand, is designed to be nicians and pathologists alike. It highlighted the intrinsic
the essential interpretive component of the report that limitations of morphologic interpretation, and led to sig-
details the morphologic findings, i.e., infection, reactive/ nificant variability in management and outcomes which
reparative changes, and/or epithelial cell abnormalities, caused frustration amongst clinical providers. With in-
both squamous and glandular. For squamous lesions, creasing implementation of TBS terminology in the early
TBS introduced a new 2-tier terminology for reporting 1990s, it became clear that the vast majority of abnormal
HPV-associated squamous intraepithelial lesions (SIL): cervical cytology results fell into the equivocal categories
low-grade (LSIL) and high-grade (HSIL). It also allowed of ASCUS or LSIL. In light of the increasing clarity of
for a period of transition during which previously used HPV biology, the large volume of women with ASCUS/
grades of CIN, degrees of dysplasia, and the presence of LSIL cytology, which had the potential to overburden the
HPV cytopathic changes could be appended. The new available colposcopy resources, and the recent availability
2-tier terminology was expected to improve interobserv- of HPV testing for potential triage, the NCI conceived the
360 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
ASCUS-LSIL Triage Study (ALTS) to determine how best 1. General. (a) The terms “interpretation” or “result”
to manage women with these equivocal results. The ALTS were recommended in lieu of “diagnosis” in the head-
was designed as a randomized multicenter trial to com- er of the cervical cytology report, since it is a screening
pare the 3 management strategies available: immediate test, which serves as a medical consultation by provid-
colposcopy, HPV triage, and conservative follow-up. ing an interpretation that contributes to a diagnosis
Women were recruited between 1996 and 1998, with the when integrated with patient history, clinical findings,
aim of establishing how best to avoid overreferral and and the results of other laboratory tests such as cervical
overtreatment for the majority of women with clinically biopsy. (b) Acknowledging that TBS was developed
insignificant changes, while providing a safety net for the primarily for cervical cytology, it was decided that
small percentage of women with underdiagnosed high- specimens from other sites in the lower anogenital
grade lesions [3]. tract, such as the vagina and anus, could also be re-
The ALTS was a pivotal trial that not only achieved its ported using this terminology.
main goal, but greatly informed our understanding of 2. Terminology. (a) Squamous lesions: consideration
cervical cancer biology, which, in turn, significantly im- was given to the possibility of eliminating the ASCUS
pacted clinical practice patterns. The study results estab- interpretive category, but this was not done due the
lished molecular testing for high-risk HPV as the most unacceptable loss of sensitivity and positive predictive
cost-effective approach to clarify equivocal cytologic value for HSIL that it would portend. Instead, it was
findings. Follow-up data showed that the risk of CIN2+ modified to ASC, with a narrower definition and a
for high-risk HPV-positive ASCUS is the same as for LSIL simple dichotomous system of qualifiers, i.e., ASC-US
and should therefore be managed as such, while HPV- and ASC-H, which also mirrored HPV biology. (b)
negative ASCUS is relatively safe and does not require Glandular lesions: while TBS emphasizes that cervical
immediate colposcopy. The implementation of reflex cytology is not a screening test for adenocarcinoma,
HPV testing for ASCUS decreased colposcopy referrals improvements in sampling devices and experience
by up to 50%. From the ALTS, we were also able to dem- with cytomorphologic recognition of glandular ab-
onstrate that in screening and diagnostic workup for cer- normalities led to the addition of “endocervical ade-
vical cancer, there is no gold standard, and, indeed, cy- nocarcinoma in situ” (AIS) as a distinct interpretative
tology, colposcopy, and histology are all subject to vari- category, and the “atypical glandular cells” (AGC) cat-
able performance. Interobserver “non-reproducibility” of egory was refined to specify the glandular cell type and
pathologic interpretations was shown to be comparable, better reflect concern for neoplasia so as to provide
for both histopathology and cytology and, at best, average more guidance for management.
[4]. Similarly, intake colposcopy in the ALTS had a sensi- The NCI and the American Society of Cytopathology
tivity of 53% for subsequent CIN2+ and an overall sensi- collaborated, under the leadership of Drs. Diane Solomon
tivity of 70% for CIN3+. Thus colposcopy, like cytology and Ritu Nayar, to facilitate the dissemination of the TBS
and histology, was found to be subjective and detected 2001 update. Three educational methods were utilized:
only about 2/3rd of CIN3+ [5]. 1. The 2nd edition of the Bethesda print atlas addressed
From the onset, TBS was expected to continue to the reporting changes, and was significantly expanded
evolve with time in response to advances in the under- with a new chapter-based format and the addition of
standing of cervical neoplasia and the changing needs of background, detailed interpretive criteria, ample illus-
the cytopathology and clinical communities. In 2001, the trations, explanatory notes, management guidelines,
third TBS workshop was held to consider updates based and sample reports. New technologies such as liquid-
on practice changes, and advances in science and technol- based cytology, automation, computer-assisted imag-
ogy. In order to broaden participation both within the ing, and HPV testing were also included [6].
USA and internationally, draft recommendations were 2. A companion Bethesda Web atlas was established in
posted on an Internet bulletin board, and over 2,000 com- conjunction with the print atlas. It had more images
ments were considered prior to the multidisciplinary than the print atlas, and the ability to perform search-
workshop. TBS 2001 was attended by over 400 people es by morphology, preparation type, etc., as well as a
from 24 countries and 44 professional societies. A num- self-test [7].
ber of significant updates occurred in 2001 that can be 3. The Web-based Bethesda Interobserver Reproducibil-
summarized as follows: ity Study (BIRST), using a subset of images from the
2nd edition of the Bethesda atlas prior to its publica-
TBS: History and Significance Acta Cytologica 2017;61:359–372 361
DOI: 10.1159/000477556
tion, was undertaken to gain additional insight into published in print and electronic formats in 2015 [12,
consensus among cytologists with varied training and 13]. It was also accompanied by a companion Bethesda
experience, and to identify specific cytomorphologic 2014 website which contains images from the BIRST-2
features and reporting categories that represented project conducted in conjunction with this update [14,
sources of poor agreement. The results confirmed that 15]. It was gratifying to see that the prior educational ef-
the a priori difficulty of the image was a more impor- forts and experience resulted in a marked improvement
tant determinant of agreement than the characteristics in almost all interpretative categories when compared to
of the participant [8]. BIRST-1, although the performance of glandular lesions
Immediately following the 2001 Bethesda Workshop, is still less reproducible than that of squamous lesions
the American Society for Colposcopy and Cervical Pa- and the image difficulty remains the main determinant
thology (ASCCP) held a multidisciplinary consensus of agreement.
conference to develop management strategies for cyto- One of the most significant contributions of the pro-
logic abnormalities conforming to TBS categories [9]. cess is that TBS has served as a model for the development
The results of ALTS and other clinical research formed of other standardized reporting systems in cytopathology
the basis for guideline development. This was a historic and histopathology. The Bethesda System for Thyroid
event where, for the first time, reporting terminology cor- Cytopathology, the Paris System for Urinary Cytopathol-
related with both biology and clinical management. These ogy, the Milan System for Salivary Gland Cytology, and
evidence-based management guidelines were updated in the Papanicolaou Society of Cytopathology Guidelines
2006 and 2012, based on additional data from subsequent for Pancreaticobiliary Cytology have all followed educa-
trials and clinical experience in the USA, and they are tional efforts similar to TBS [16–19]. Extension of the
now widely accepted as the standard of care [10, 11]. 2-tiered terminology of LSIL and HSIL is now recognized
Between 2001 and 2014, with the approval and imple- by the World Health Organization, and by the ASCCP,
mentation of prophylactic HPV vaccination and primary and College of American Pathologists for reporting his-
HPV screening as an alternative option for the secondary topathology of specimens from the lower anogenital tract
prevention of cervical cancer, the role and performance [20, 21].
characteristics of cervical cytology were gradually but The success of TBS rests on sound principles that were
surely changing in various parts of the world. In vacci- key to adopting and implementing it as an international
nated populations, the removal of the HPV16 and HPV18 standardized reporting terminology for cervical cytology.
genotypes will lead to a subsequent decreased prevalence TBS (a) is based on evidence, inclusion and consensus; (b)
of high-grade lesions. In the primary HPV screening al- correlates with biology and management; (c) is concise
gorithm with reflex cytology only for women who are and practical; (d) is flexible enough to be adopted by dif-
HPV-positive but do not have HPV16/18, the Pap test ferent geographic/laboratory settings; (e) allows for
will take on more of a “diagnostic” role. Thus, it will be change with the increase of knowledge and experience;
imperative to maintain the sensitivity of cytology for it to and (f) incorporates multiple educational endeavors (at-
be utilized in this application. In addition, another decade lases, websites, and BIRST). Editors and authors of the
of experience with liquid-based cytology, and other tech- cervical cytology Bethesda atlases have always been com-
nologic advances such as immunocytochemistry and mo- mitted to making the educational materials affordable,
lecular process was gained, leading to the need for an- and therefore widely accessible, by foregoing all hono-
other TBS update. raria or royalties.
The 2014 TBS revision, which occurred under the In summary, TBS serves as a landmark and exemplary
leadership of Drs. Ritu Nayar and David C. Wilbur, an- contribution to standardized reporting. The following ex-
ticipated minimal changes in terminology, and it was cerpts are an appropriate end to this discourse:
largely undertaken to provide cytologists and clinicians
It is paradoxical that instead of TBS responding to new devel-
with an extensive educational resource to include basic
opments and changes, it has actually led the way in many areas.
concepts, more morphologic clues, pitfalls, and histolog- TBS played a vital role in initiating research in the biology of cervi-
ic correlations, and also to update management guide- cal cancer, in exploring new approaches and strategies in patient
lines. An additional non-morphologic chapter was also management and in incorporating new technologies into cervical
added, detailing the current conceptual approach to cancer screening. (Foreword by Robert Kurman in the 2nd edition
of The Cervical Cytology Bethesda Atlas, 2004 [6].)
overall risk assessment-based management. The 3rd edi-
tion of the Bethesda atlas was significantly larger and
362 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
I never imagined that a small meeting on the campus of the Na- Disclosure Statement
tional Institutes of Health in Bethesda, Maryland, one snowy week-
end in December 1988 would begin a process that has changed the The authors have no conflicts of interest to declare.
practice of cervical cytology – in both the laboratory and the clini-
cian’s office – around the world. (Preface by Diane Solomon to the
3rd edition of The Cervical Cytology Bethesda Atlas, 2015 [13].)
TBS: History and Significance Acta Cytologica 2017;61:359–372 363
DOI: 10.1159/000477556
364 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
TBS: History and Significance Acta Cytologica 2017;61:359–372 365
DOI: 10.1159/000477556
366 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
TBS: History and Significance Acta Cytologica 2017;61:359–372 367
DOI: 10.1159/000477556
368 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
TBS: History and Significance Acta Cytologica 2017;61:359–372 369
DOI: 10.1159/000477556
370 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
TBS: History and Significance Acta Cytologica 2017;61:359–372 371
DOI: 10.1159/000477556
References
1 Solomon D, et al: The 1988 Bethesda System 8 National Cancer Institute, American Society 16 Ali SZ, Cibas ES (eds): The Bethesda System
for reporting cervical/vaginal cytologic diag- of Cytopathology: Bethesda System Website for Reporting Thyroid Cytopathology. Defi-
noses. Developed and approved at the Na- Atlas. http://nih.techriver.net/ (accessed May nitions, Criteria, and Explanatory Notes. New
tional Cancer Institute Workshop, Bethesda, 9, 2017). York, Springer, 2010.
Maryland, USA, December 12–13, 1988. Acta 9 Wright TC, Cox JT, Massad LS, Twiggs LB, 17 Layfield LJ, Pitman MB, DeMay RM, Shid-
Cytol 1989;33:567–574. Wilkinson EJ: 2001 Consensus guidelines for ham VB: Pancreaticobiliary tract cytology:
2 Kurman RJ, Solomon D (eds): The Bethesda the management of women with cervical cy- journey toward “Bethesda” style guidelines
System for Reporting Cervical/Vaginal Cyto- tological abnormalities. JAMA 2002; 287: from the Papanicolaou Society of Cytopathol-
logic Diagnoses. Definitions, Criteria, and Ex- 2120–2129. ogy. Cytojournal 2014;11:18.
planatory Notes for Terminology and Speci- 10 Wright TC Jr, Massad SL, Dunton CJ, Spitzer 18 Rosenthal DL, Wojcik EM, Kurtycz DFI (eds):
men Adequacy. New York, Springer, 1994. M, Wilkinson EJ, Solomon D: 2006 Consen- The Paris System for Reporting Urinary Cy-
3 Schiffman M, Adrianza ME: ASCUS-LSIL tri- sus guidelines for the management of women tology. New York, Springer, 2016.
age study. Design, methods and characteris- with abnormal cervical cancer screening tests. 19 Rossi ED, Faquin WC, Baloch Z, Barkan GA,
tics of trial participants. Acta Cytol 2000; 44: Am J Obstet Gynecol 2007;197:346–355. Foschini MP, Pusztaszeri M, Vielh P, Kurtycz
726–742. 11 Massad LS, Einstein MH, Huh WK, Katki DFI: The Milan system for reporting salivary
4 Stoler MH, Schiffman M: Interobserver vari- HA, Kinney WK, Schiffman M, Solomon D, gland cytopathology: analysis and suggestions
ability of cervical cytologic and histologic in- Wentzensen N, Lawson H: 2012 Updated from initial survey. Cancer Cytopathol 2017
terpretations: realistic estimates from the consensus guidelines for the management of (in press).
ASCUS-LSIL triage study. JAMA 2001; 285: abnormal cervical cancer screening tests and 20 Darragh TM, Colgan TJ, Cox JT, Heller DS,
1500–1505. cancer precursors. J Low Genit Tract Dis Henry MR, Luff RD, McCalmont T, Nayar R,
5 Gage JC, Hanson VW, Abbey K, Dippery S, 2013;17(5 suppl 1):S1–S27. Palefsky JM, Stoler MH, Wilkinson EJ, Zaino
Gardner S, Kubota J, Schiffman M, Solomon 12 Nayar R, Wilbur DC: The Pap test and Bethes- RJ, Wilbur DC; LAST Project Work Groups:
D, Jeronimo J: Number of cervical biopsies da 2014. Cancer Cytopathol 2015: 123: 271– The lower anogenital squamous terminology
and sensitivity of colposcopy. Obstet Gynecol 281. standardization project for HPV-associated
2006;108:264–272. 13 Nayar R, Wilbur DC (eds): The Bethesda Sys- lesions: background and consensus recom-
6 Solomon D, Nayar R (eds): The Bethesda Sys- tem for Reporting Cervical Cytology, ed 3. mendations from the College of American
tem for Reporting Cervical Cytology. Defini- Definitions, Criteria, and Explanatory Notes. Pathologists and the American Society for
tions, Criteria, and Explanatory Notes. New New York, Springer, 2015. Colposcopy and Cervical Pathology. Arch
York, Springer, 2004. 14 The 2014 Bethesda Cervical Cytology Web Pathol Lab Med 2012;136:1266–1297.
7 Sherman ME, Dasgupta A, Schiffman M, Atlas. https://bethesda.soc.wisc.edu/ (ac- 21 Stoler M, Bergeron C, Colgan TJ, Ferenczy
Nayar R, Solomon D: The Bethesda Interob- cessed May 10, 2017). AS, Herrington CS, Kim K-R: Epithelial tu-
server Reproducibility Study (BIRST): a web 15 Kurtycz DFI, Staats P, Chute D, Russell D, mours, part of tumours of the uterine cervix;
based assessment of the Bethesda 2001 System Pavelec D, Monaco SE, Friedlander MA, Wil- in Kurman RJ, Carcangiu ML, Herrington CS,
for classifying cervical cytology. Cancer Cyto- bur DC, Nayar R: Bethesda Interobserver Re- Young RH (eds): WHO Classification of Tu-
pathol 2007;111:15–25. producibility Study-2 (BIRST-2): Bethesda mours of Female Reproductive Organs, chapt
System 2014. J Am Soc Cytopathol 2017;6: 7, ed 4. Lyon, IARC, 2014, pp 172–198.
131–144.
372 Acta Cytologica 2017;61:359–372 Nayar/Wilbur
DOI: 10.1159/000477556
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- CHC33015-Sub 1 AssessmentDokument102 SeitenCHC33015-Sub 1 AssessmentMaimuna100% (8)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- DM No. 2022-0287 Updated Moa and Tor PRDPDokument8 SeitenDM No. 2022-0287 Updated Moa and Tor PRDPDRMC Infirmary100% (1)
- Hospital Case StudyDokument3 SeitenHospital Case StudyShashi88% (8)
- Carmen Best Background InformationDokument15 SeitenCarmen Best Background InformationKING 5 NewsNoch keine Bewertungen
- Negative Impact of Social Media: A Qualitative Inquiry Towards Student of Arellano University Jose Rizal CampusDokument30 SeitenNegative Impact of Social Media: A Qualitative Inquiry Towards Student of Arellano University Jose Rizal Campusisabel ysaNoch keine Bewertungen
- Test Bank For Medical Assisting Administrative and Clinical Competencies 8th Edition by BlesiDokument18 SeitenTest Bank For Medical Assisting Administrative and Clinical Competencies 8th Edition by BlesiMary Lawson100% (33)
- Time: 45 Minutes Instructions To CandidatesDokument12 SeitenTime: 45 Minutes Instructions To CandidatesHegi Ann AlcalaNoch keine Bewertungen
- Brach y TherapyDokument3 SeitenBrach y Therapydincy danielNoch keine Bewertungen
- LYRA Value Impact Workforce HealthDokument13 SeitenLYRA Value Impact Workforce HealthThomas WhittyNoch keine Bewertungen
- PMFIAS CA 2019 05 12 SciDokument107 SeitenPMFIAS CA 2019 05 12 SciShivy SwarnkarNoch keine Bewertungen
- History: Middle AgesDokument2 SeitenHistory: Middle AgesAyinNoch keine Bewertungen
- Mobile Phone Addiction Among YouthDokument10 SeitenMobile Phone Addiction Among Youthda dadadfgNoch keine Bewertungen
- Non-Toxic GoiterDokument17 SeitenNon-Toxic Goiterabigaille chua100% (1)
- Physical Education Cambridge Progression Test P1 - ST6 (2022)Dokument14 SeitenPhysical Education Cambridge Progression Test P1 - ST6 (2022)Givemore MuromboNoch keine Bewertungen
- Review of LitreatureDokument10 SeitenReview of Litreaturekuttivasanth50% (2)
- Recommendations For Cardiovascular Prevention DuringDokument5 SeitenRecommendations For Cardiovascular Prevention DuringRaiyanNoch keine Bewertungen
- Veterans Affairs Presumptive Service Connection and Disability CompensationDokument33 SeitenVeterans Affairs Presumptive Service Connection and Disability CompensationChuck Achberger100% (1)
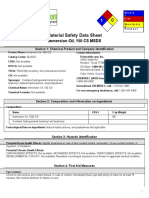
- 0 Material Safety Data Sheet: Immersion Oil, 150 CS MSDSDokument5 Seiten0 Material Safety Data Sheet: Immersion Oil, 150 CS MSDSA.N. MNoch keine Bewertungen
- K5 - Sistem Informasi KesehatanDokument29 SeitenK5 - Sistem Informasi KesehatanPusvaNurmalaSariNoch keine Bewertungen
- Health and Fitness - Unit 8: Ms. Pilar Gonzales-A09Dokument87 SeitenHealth and Fitness - Unit 8: Ms. Pilar Gonzales-A09Antonio Palacios OrihuelaNoch keine Bewertungen
- BNO72122 - v2 - 161956 Focal Spasticity Workbook - FINAL - PIDokument51 SeitenBNO72122 - v2 - 161956 Focal Spasticity Workbook - FINAL - PIAli Radhi MutarNoch keine Bewertungen
- Cleaning Policy 6.0Dokument27 SeitenCleaning Policy 6.0saadNoch keine Bewertungen
- Antipsycotic DrugDokument21 SeitenAntipsycotic DrugShashank SatheNoch keine Bewertungen
- 7724 (11) The Hospital and Pertinent Laws and RegulationsDokument24 Seiten7724 (11) The Hospital and Pertinent Laws and RegulationsnewazNoch keine Bewertungen
- Mini Case Study For MR ADokument3 SeitenMini Case Study For MR Aapi-300133703Noch keine Bewertungen
- Babe 2Dokument17 SeitenBabe 2Sathish SizzyNoch keine Bewertungen
- Chain of Hope Teams With Gift of LifeDokument1 SeiteChain of Hope Teams With Gift of LifeJonathan DanosNoch keine Bewertungen
- Piriformis Syndrome: DefinitionDokument3 SeitenPiriformis Syndrome: DefinitionMd Sherajul HaqueNoch keine Bewertungen
- Computer in Community Pharmacy HDokument13 SeitenComputer in Community Pharmacy HMayan Khan100% (2)
- Myanmar Regulatory and Market ProfileDokument15 SeitenMyanmar Regulatory and Market ProfileMaaz Khan100% (1)