Beruflich Dokumente
Kultur Dokumente
Old Carts
Hochgeladen von
inggitluthfiazahraCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Old Carts
Hochgeladen von
inggitluthfiazahraCopyright:
Verfügbare Formate
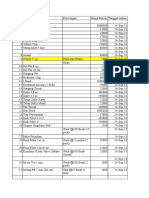
Table 1
MODULE 17: Cardiology Causes of chest pain 3
PART 9 Cardiovascular
• Myocardial infarction
Assessment of • Unstable angina pectoris
• Pericarditis
• Dissecting aortic aneurysm
chest pain • Myocarditis
• Apical ballooning syndrome (Tako tsubocardiomyopathy)
Pulmonary
• Pleurisy
by Kate O’Donovan
• Pulmonary embolism
• Pneumothorax
The final part in this series will focus on the assessment of • Pneumonia
chest pain. This symptom is one of the most common present-
Haematological
ing complaints seen in primary and secondary care1,2 and is the
• Sickle cell anaemia
leading cause of emergency department visits after abdominal
pain. Assessment and differentiation of the various chest pain Musculoskeletal
presentations can be challenging due to variation in clinical • Costochondritis
presentation, patient history of the symptom and the potential • Trauma
for atypical presentation in women, older people, and those with
diabetes or chronic kidney disease. Through structured nursing Gastrointestinal
assessment it is possible to identify those at high risk. The aim of • Reflux
this article is to provide an overview of the assessment of chest • Ulcers
pain and differential diagnosis of chest pain. • Gallstones
• Pancreatitis
There are many causes of chest pain as outlined in Table 1 but
acute coronary syndrome is one of the potentially more serious
Non organic
causes that require rapid identification and implementation of • Anxiety
treatment in an attempt to preserve myocardial function and pre-
vent the development of arrhythmias, heart failure or cardiogenic patient assessment must be systematic and comprehensive with-
shock. Acute coronary syndromes are an umbrella term used to out the use of leading questions. In the author’s experience the
describe the clinical presentation of ischaemic heart disease and tool ‘OLD CARTS’ (see Table 2) is most commonly used in clinical
encompasses unstable angina pectoris, non ST segment eleva- practice when assessing chest pain. The following is an overview
tion myocardial infarction and ST segment elevation myocardial of ‘OLD CARTS’.
infarction. It is defined by the European Society of Cardiology Onset
Guidelines4 as a life threatening manifestation of atherosclerosis Establishing the onset of chest pain is vital in helping to
caused by rupture of a vulnerable atherosclerotic plaque with differentiate between acute and chronic pain. Patients with mus-
subsequent thrombus formation, which causes a sudden com- culoskeletal pain caused by injury or chronic conditions may
plete or critical reduction in coronary blood flow, which results in present to the emergency department days after the injury has
the clinical presentation of chest pain. occurred as a consequence of inability to carry out routine daily
Assessment of chest pain should focus on the history of the tasks or worsening of the chronic condition.6 Ischaemic chest
pain, cardiovascular risk factor profile, previous personal history pain in comparison may occur with exertion and relieve with rest
of ischaemic heart disease and prior relevant investigation. All or with sublingual GTN spray.
but the history of chest pain has been presented in part one and Location
two of this series. A clear history of chest pain and its associated Despite popular belief left sided chest pain is unlikely to indi-
symptoms are pivotal in guiding investigations and treatment. cate a cardiac origin. 1 Ischaemic chest pain is located central
There are numerous chest pain assessment tools and scores and or slightly to the left of central chest, but according to Hamm 7
a sample of these are presented in Tables 2 and 3, which can aid ischaemic chest pain may be experienced anywhere from the
in the assessment of chest pain pubis region to the top of the head and in some people they may
According to Oriolo and Albarran1 there is no specific recom- only experience pain in the areas of radiation such as arm, neck,
mendation as to which is the most appropriate tool to use, but jaw and not in the chest. Atypical symptoms include absence of
Sponsored by an unrestricted grant from Merck Sharp & Dohme Ireland (Human Health) Ltd
CardioWINNov-SM-KOD-AM.indd 1 21/10/2011 11:45:39
Continuing Education
Table 2
Example of assessment using OLD CARTS framework 5
Description Patient report
Onset When did the pain begin?
Location Where is the pain?
Duration How long does the pain last?
Characteristics Describe the pain? Crushing, stabbing, indigestion like, dull, ache for example.
Associating factors Other symptoms associated with the pain such as nausea and/or vomiting, weakness, fatigue,
breathlessness, syncope, cold and clammy?
Relieving factors/radiation Does the pain radiate such as down the arm, up into the neck for example?
Relieving factors: pain stops when activity ceases, relieved by sitting forward or resting?
Treatment/temporal factors Use of GTN, pain was relieved by rest or decrease in physical activity. Pain non comparable to
previous ischaemic chest pain
Severity (intensity) A numerical scale (1 no pain – 10 worse pain experienced ) is used to gauge pain severity
pain but instead epigastric fullness, fatigue and indigestion. These Table 3
symptoms may be seen in those who experience autonomic
neuropathy secondary to diabetes. In addition atypical presenta- Chest Pain Assessment Tools5
tion maybe experienced in younger (25-40 years) and older (>75 P – precipitating or provoking factors
years) patients, women and in those with chronic renal failure or Q – quality (intensity/pain score)
dementia. Absence of chest pain leads to under recognition of R – radiation, region
the disease and under treatment.7 S – severity/symptoms/duration
Duration T – timing
Differentiating chest pain according to duration of pain can
C – commenced when
be helpful marker in aiding diagnosis. According to Oriolo and
H – history/evidence of risk factors
Albarran1 if the pain is continuous or prolonged, eg. after exer-
E – extra/additional symptoms
cise, it is unlikely to be anginal in nature. In addition, pain that S – stays/radiation
rapidly comes and goes lasting less than a minute is also unlikely T – timing, how long has it lasted?
to be cardiac related. In contrast pain caused by ischaemic heart
disease can last for as long as 20 minutes or more and it is usu- P – place/location
A – what alleviates/aggravates the pain
ally relieved by GTN within one to five minutes of administration.
I – intensity scoring
But remember pain caused by oesophageal spasm can also be
N – nature and characteristics
relieved by GTN spray.
Character itate chest pain symptoms. Despite knowledge of ACS related to
Ischaemic chest pain has several descriptors depending on the substance abuse it is not routinely asked about or documented
patient’s perception of pain. Descriptors include pressure, heavy in clinical notes.
feeling, feeling of indigestion stabbing and sharp pain. Pain that Other associated symptoms related to chest pain include nau-
is reproducible on palpation, sharp or pleuritic pain, pain worse sea, vomiting, diaphoresis, shortness of breath, syncope or pre
on inspiration or coughing is unlikely to be ischaemic in nature syncope. If present then the presence of acute coronary syn-
although cannot be excluded. drome should be high.
Typical angina pain is defined as chest discomfort that is aggra- Relieving factors/radiation
vated by exertion and relieved by rest or GTN. It is necessary to It is necessary to enquire about how the chest pain is relieved. As
explore other aggravating/associating factor to aid in differential mentioned previously pain relieved by change in body position
diagnosis.2 Classically ischaemic pain maybe described as exer- or respiratory pattern or by antacids tend not to be ischaemic
tional pain, pressure or discomfort in the neck shoulder or arm. in nature. In comparison pain relieved by GTN or rest suggest
Atypical descriptors include cramping, grinding, pricking. Rarely ischaemia.
is tooth or jaw pain experienced as ischaemia. Hamm7 describes the radiation pattern of ischaemic chest pain
Associating factors as common in the left arm, neck or jaw. Radiation is less common
Typical ischemic pain is normally relieved by rest and/or GTN. in the right arm or both arms simultaneously, the back, abdomen
Pain that is relieved by change in body position, adjusting breath- and the teeth.
ing pattern or by antacids is unlikely to be cardiac in nature. 1 Temporal factors
When assessing the patient about the nature of their chest pain it From clinical experience people with a prior history of ischae-
is also important to obtain information regarding the use of rec- mic heart disease are able to recognise their ischaemic chest pain
reational drugs, herbal or over the counter medications as these from other forms of chest pain. For those who present for the
may interfere with patient’s prescribed medication and/or precip- first time with chest pain this is impossible and provides a chal-
34 WIN November 2011 Vol 19 Iss 9
CardioWINNov-SM-KOD-AM.indd 2 21/10/2011 11:46:37
Continuing Education
lenge when assessing the pain. Also temporal factors address the pared with an ECG recorded when the patient is pain free.
treatment used to relieve pain and how often the treatment is In addition to the ECG routine bloods such as full blood count,
administered in order to obtain relief. coagulation screen, renal function should be observed to rule
Severity out non-cardiac causes of chest pain and also to gain insight
Pain is subjective so the use of pain scores, visual analogues into how other systems are functioning. Cardiac markers such as
and pain scales are helpful in quantifying the severity of chest troponins should also be noted, these serve to identify and risk
pain and the effectiveness of the treatment administered. In our stratify patients into high, intermediate and low risk. Troponins
clinical practice the pain scale is used and for those that can- are highly sensitive for myocardial necrosis caused by occlusion
not use the pain scale due to communication barriers a visual of the coronary artery.
analogue is available. The pain scale is recorded in the nursing Conclusion
documentation along with the assessment of chest pain. Chest pain is a common presenting complaint with numerous
In addition, recording the vital signs is essential and underpins possible causes. A systematic approach as outlined above, sup-
the subsequent physical examination. Vital signs that directly plemented with vital signs, ECG and the relevant bloods will aid
relate to the cardiovascular system are the pulse and blood pres- in diagnosis, risk stratification and treatment options.
sure, but respiratory rate, temperature and level of consciousness Kate O'Donovan is course co-ordinator for the postgraduate diploma in
maybe beneficial in establishing differential diagnoses. Regarding cardiovascular nursing in the Mater Hospital, Dublin
the recording of blood pressure Tough3 advises recording blood References
pressure in both arms when a patient presents with chest pain. A 1. Oriolo V, Albarran JW. Assessment of acute chest pain. Br J Cardiac Nurs 2010; 5(12): 587-593.
difference of greater than 20mmHg may indicate aortic dissec- 2. Bickley LS. The cardiovascular system. Bates Guide to Physical Examination and History Tak-
ing (10th Ed). Lippincott Williams & Wilkins: Philadelphia 2009: 323-389.
tion and can assist in formulating a diagnosis. 3. Tough J. Assessment and management of chest pain. Nursing Standard 2004; 18(26): 45-53
Attaching the patient to a cardiac monitor to observe for 4. Bassand JP, Hamm CW, Ardissino D Et al. Guidelines for the diagnosis and treatment of non
st-segment elevation acute coronary syndromes. Task force for diagnosis and treatment of non
ST segment deviation or occurrence of arrhythmias is also st-segment elevation acute coronary syndromes of European Society of Cardiology. Eur Heart
recommended. J 2007; 28: 1598-1660
Recording 12 lead ECG has a central role in the early assess- 5. Seidel HM, Ball JW, Dains JE, Benedict GW. Mosby’s Guide to Physical Examination (6th Ed).
Mosby: St Louis, 2003.
ment of patients with suspected ischaemic chest pain. It is 6. Hoskins R. Assessing and managing the patient with musculoskeletal chest pain. In: Albar-
recommended that recording and interpreting a 12 lead ECG ran JW, Tagney J (eds). Chest Pain: Advanced Assessment and Management Skills. Blackwell
Publishing: Oxford, 2007.
within 10 minutes of patient presentation is best practice.7 Ideally 7. Hamm CW, Mollmann H, Bassand JP, Van de Werf F. (2009)Acute Coronary Syndromes.
an ECG should be recorded when the patient has pain and com- The ESC Textbook of Cardiovascular Medicine. Oxford 2009: 535-596.
CardioWINNov-SM-KOD-AM.indd 3 21/10/2011 11:47:05
Das könnte Ihnen auch gefallen
- ACLS Exam ADokument8 SeitenACLS Exam ASean Johnson83% (30)
- Costochondritis: Rapid Evidence ReviewDokument7 SeitenCostochondritis: Rapid Evidence ReviewDiana FlorezNoch keine Bewertungen
- Chan, Johnson - TreatmentGuidelines PDFDokument0 SeitenChan, Johnson - TreatmentGuidelines PDFBogdan CarabasNoch keine Bewertungen
- Cardio InternetDokument46 SeitenCardio InternetnaimNoch keine Bewertungen
- Checklist CPR 2018 PDFDokument2 SeitenChecklist CPR 2018 PDFCarissa Tirtania100% (3)
- CvsDokument35 SeitenCvsVISS11Noch keine Bewertungen
- DD Chest Pain DR M Yusuf Suseno SPJPDokument246 SeitenDD Chest Pain DR M Yusuf Suseno SPJPMatthew christopherNoch keine Bewertungen
- Cardiovascular System Diseases Part 1Dokument22 SeitenCardiovascular System Diseases Part 1Prince Rener Velasco PeraNoch keine Bewertungen
- Slide Set Chest PainDokument77 SeitenSlide Set Chest PainPragnesh ShahNoch keine Bewertungen
- Chest Pain ProtocolDokument7 SeitenChest Pain Protocolomar kmr97Noch keine Bewertungen
- Angina Pectoris (Stable Angina) Nursing Care Management - Study GuideDokument8 SeitenAngina Pectoris (Stable Angina) Nursing Care Management - Study GuideSachin Singh100% (1)
- Angina Pectoris, SeminarDokument18 SeitenAngina Pectoris, SeminarMuslim GrdkhiwatyNoch keine Bewertungen
- PDX - Cardio Part 1Dokument45 SeitenPDX - Cardio Part 1LUAPLRAKNoch keine Bewertungen
- 100 Clinical Cases in Medicine - PasTest - Cardiac OnlyDokument30 Seiten100 Clinical Cases in Medicine - PasTest - Cardiac OnlySsNoch keine Bewertungen
- Chest Pain EvaluationDokument23 SeitenChest Pain Evaluationhjuarez1102Noch keine Bewertungen
- Diagnosing Chest Pain Diagnosing Chest Pain: HistoryDokument4 SeitenDiagnosing Chest Pain Diagnosing Chest Pain: HistorySuhaib Bin SinanNoch keine Bewertungen
- MI + Unstable AnginaDokument9 SeitenMI + Unstable AnginaJessica CainNoch keine Bewertungen
- Reading Reference 3-Approach To Chest PainDokument14 SeitenReading Reference 3-Approach To Chest PainVarshini Tamil SelvanNoch keine Bewertungen
- Winzenberg, T. (2015) - Musculoskeletal Chest Wall Pain.Dokument5 SeitenWinzenberg, T. (2015) - Musculoskeletal Chest Wall Pain.Tom StevensNoch keine Bewertungen
- 2005 Chronic Stable AnginaDokument11 Seiten2005 Chronic Stable AnginaAlma EscobarNoch keine Bewertungen
- NSTMIDokument16 SeitenNSTMIrio kharismaNoch keine Bewertungen
- 5+2 Chest PainDokument27 Seiten5+2 Chest PainMazen HossamNoch keine Bewertungen
- Acute Chest PainDokument103 SeitenAcute Chest PainYajjat GargNoch keine Bewertungen
- Angina PectorisDokument7 SeitenAngina PectorisTruptilata SahooNoch keine Bewertungen
- AnginaDokument33 SeitenAnginaJai Singhrandhawa100% (1)
- Chest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsDokument16 SeitenChest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsJose AnaconaNoch keine Bewertungen
- Dolor ToracicoDokument11 SeitenDolor ToracicoSandy A.Noch keine Bewertungen
- Week 2 Individual AssignmentDokument1 SeiteWeek 2 Individual AssignmentPaul SahagunNoch keine Bewertungen
- Cme Acute Chest PainDokument38 SeitenCme Acute Chest PainDzillah MazaNoch keine Bewertungen
- Chest Pain: SV Hoàng Khương Duy Y2014dDokument32 SeitenChest Pain: SV Hoàng Khương Duy Y2014dDavid WilliamNoch keine Bewertungen
- Cardiac PPT SeminarDokument129 SeitenCardiac PPT SeminarjoashannNoch keine Bewertungen
- Cardiovascular Disease: Chest Pain: Cardiac or NotDokument7 SeitenCardiovascular Disease: Chest Pain: Cardiac or Notmahaberani_zNoch keine Bewertungen
- Angina: by Maureen Narayan-RamDokument8 SeitenAngina: by Maureen Narayan-RamMirandaNoch keine Bewertungen
- 53Dokument8 Seiten53George EstreganNoch keine Bewertungen
- General Medicine and Surgery For Dental Practition PDFDokument7 SeitenGeneral Medicine and Surgery For Dental Practition PDFAnnanyaNoch keine Bewertungen
- 1Dokument4 Seiten1Mirla Castellanos JuradoNoch keine Bewertungen
- Outpatient MedicineDokument0 SeitenOutpatient Medicineclaragustin_53768590Noch keine Bewertungen
- Chest PainDokument31 SeitenChest PainMarwan GamaleldinNoch keine Bewertungen
- Approach To Chest PainDokument37 SeitenApproach To Chest Painمصطفى عادل موسى احمدNoch keine Bewertungen
- Kelompok 14 Skenario 2Dokument30 SeitenKelompok 14 Skenario 2Rachmad SammuliaNoch keine Bewertungen
- Resident Chest Pain ModuleDokument7 SeitenResident Chest Pain ModuleFatima ShoukatNoch keine Bewertungen
- Case Report ASMIHA 2022Dokument1 SeiteCase Report ASMIHA 2022Ghina NinditasariNoch keine Bewertungen
- Coronary Artery Disease: Aleson Claire A. Llanes, MDDokument94 SeitenCoronary Artery Disease: Aleson Claire A. Llanes, MDFly LlanesNoch keine Bewertungen
- Slide 3: American Heart Association (AHA) in 2016 Stated That 15.5 Million Americans HaveDokument19 SeitenSlide 3: American Heart Association (AHA) in 2016 Stated That 15.5 Million Americans HaveChia LengkeyNoch keine Bewertungen
- Care of Clients With Angina PectorisDokument8 SeitenCare of Clients With Angina PectorisaryshamyleeNoch keine Bewertungen
- IIA - Altered Tissue PerfusionDokument14 SeitenIIA - Altered Tissue PerfusionDharylle CariñoNoch keine Bewertungen
- Evaluation of Chest Pain: William Norcross, M.DDokument16 SeitenEvaluation of Chest Pain: William Norcross, M.DAbhinit RiddhiNoch keine Bewertungen
- Internal Diseases Propedeutics. Part II. Diagnostics of Cardiovascular DiseasesDokument100 SeitenInternal Diseases Propedeutics. Part II. Diagnostics of Cardiovascular DiseasesХассан ЯасирNoch keine Bewertungen
- Chest Pain Pediatrics: Pediatric CardiologyDokument15 SeitenChest Pain Pediatrics: Pediatric CardiologygladyannNoch keine Bewertungen
- The Cardiovascular SystemDokument7 SeitenThe Cardiovascular SystemRex HuangNoch keine Bewertungen
- Chest Pain: Clinical Practice Guideline For Primary Health Care PhysiciansDokument70 SeitenChest Pain: Clinical Practice Guideline For Primary Health Care PhysiciansrajesheravankaraNoch keine Bewertungen
- Acs SGD 8 - 20240308 - 051618 - 0000Dokument13 SeitenAcs SGD 8 - 20240308 - 051618 - 0000Sarah JesikaNoch keine Bewertungen
- Chest Pain ManagementDokument55 SeitenChest Pain Managementztt64nmvvpNoch keine Bewertungen
- Cardiology HX - PEDokument34 SeitenCardiology HX - PEjjNoch keine Bewertungen
- Symtomps and SignDokument6 SeitenSymtomps and SignSartika AkibNoch keine Bewertungen
- Angina PectorisDokument36 SeitenAngina PectorisBardahWasaLamahNoch keine Bewertungen
- Chest Pain: Dr. Rakesh Gupta MD Specialist: Pulmonologist Lifecare Hospital: MusaffahDokument71 SeitenChest Pain: Dr. Rakesh Gupta MD Specialist: Pulmonologist Lifecare Hospital: Musaffah491970Noch keine Bewertungen
- Angina PectorisDokument8 SeitenAngina PectorisPrince DuNoch keine Bewertungen
- ودالشمال6Dokument241 Seitenودالشمال6Karren FernandezNoch keine Bewertungen
- Unstable Angina, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandUnstable Angina, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- A Simple Guide to Chest Pain, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Chest Pain, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- Summary of Data Base Clue and Cue Problem List Initial Diagnosis Planning Diagnosis Therapy Monitoring EducationDokument2 SeitenSummary of Data Base Clue and Cue Problem List Initial Diagnosis Planning Diagnosis Therapy Monitoring EducationinggitluthfiazahraNoch keine Bewertungen
- PenyemaianDokument32 SeitenPenyemaianinggitluthfiazahraNoch keine Bewertungen
- Comatose: Coma Due To Cerebral Mass Lesions and HerniationsDokument3 SeitenComatose: Coma Due To Cerebral Mass Lesions and HerniationsinggitluthfiazahraNoch keine Bewertungen
- Referred Pain (Nyeri Menjalar)Dokument1 SeiteReferred Pain (Nyeri Menjalar)inggitluthfiazahraNoch keine Bewertungen
- Post-ACLS Megacode Flashcards - QuizletDokument9 SeitenPost-ACLS Megacode Flashcards - QuizletMaya LaPradeNoch keine Bewertungen
- 2018 Slides Bradycardia and Cardiac Conduction DelayDokument108 Seiten2018 Slides Bradycardia and Cardiac Conduction DelayalynNoch keine Bewertungen
- Ecg CompiledDokument65 SeitenEcg CompiledVstreamhdNoch keine Bewertungen
- DR Russell Blaylock On Devastating Health Effects of MSG Aspartame and ExcitotoxinsDokument40 SeitenDR Russell Blaylock On Devastating Health Effects of MSG Aspartame and Excitotoxinsdplant100% (1)
- Cardiac Rehab BookletDokument32 SeitenCardiac Rehab BookletAbu Bakr Siddique100% (1)
- Tutorial Antianginal DrugsDokument2 SeitenTutorial Antianginal DrugsAbdul MosheenNoch keine Bewertungen
- Biohemija 2Dokument4 SeitenBiohemija 2mirzaNoch keine Bewertungen
- Ischemic Heart Disease PWDokument13 SeitenIschemic Heart Disease PWEunica RamosNoch keine Bewertungen
- Medication: Expected Pharmacological Action Therapeutic UseDokument1 SeiteMedication: Expected Pharmacological Action Therapeutic UseMike EveretteNoch keine Bewertungen
- Cardiac UltrasoundDokument72 SeitenCardiac Ultrasoundramon100% (6)
- ABC of Clinical Electrocardiography Bradycardias and Atrioventricular Conduction BlockDokument5 SeitenABC of Clinical Electrocardiography Bradycardias and Atrioventricular Conduction BlockIgnacio Aguilar ValdiviesoNoch keine Bewertungen
- ACLS PEA Asystole AlgorithmDokument3 SeitenACLS PEA Asystole AlgorithmSafira RNoch keine Bewertungen
- A Combined Algorithm For Identification and Differentiation of Atrial Flutter and Atrial Fibrillation Based On ECG AnalysisDokument4 SeitenA Combined Algorithm For Identification and Differentiation of Atrial Flutter and Atrial Fibrillation Based On ECG AnalysisOana DrăganNoch keine Bewertungen
- Test Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce ShadeDokument11 SeitenTest Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce ShadeLisaTurnerMDkfym100% (27)
- Plabable-Gems-19. Cardiology Plabable GemsDokument64 SeitenPlabable-Gems-19. Cardiology Plabable GemsAli RazaNoch keine Bewertungen
- Guias ESC para Insuficiencia Cardiaca CronicaDokument128 SeitenGuias ESC para Insuficiencia Cardiaca CronicaKarla HernandezNoch keine Bewertungen
- Arrhythmias: Domina Petric, MDDokument22 SeitenArrhythmias: Domina Petric, MDMwaba PeterNoch keine Bewertungen
- 2019 Catheter Ablation of VA PDFDokument153 Seiten2019 Catheter Ablation of VA PDFyusupNoch keine Bewertungen
- Modifiable Risk Factors Non - Modifiable Risk Factors: LegendDokument2 SeitenModifiable Risk Factors Non - Modifiable Risk Factors: LegendWendy Escalante100% (1)
- 2013 ACC/AHA Guideline On The Assessment of Cardiovascular RiskDokument25 Seiten2013 ACC/AHA Guideline On The Assessment of Cardiovascular RiskaxxoNoch keine Bewertungen
- Cardiac CTDokument7 SeitenCardiac CTdaniel7pintiliiNoch keine Bewertungen
- Systematic Approach To ECGDokument12 SeitenSystematic Approach To ECGAmr El TaherNoch keine Bewertungen
- Shanae J DownerDokument2 SeitenShanae J Downerapi-367795334Noch keine Bewertungen
- 100 Questions in Cardiology-, PDFDokument241 Seiten100 Questions in Cardiology-, PDFditairinaNoch keine Bewertungen
- Acute Myocardial InfarctionDokument14 SeitenAcute Myocardial InfarctionJardee DatsimaNoch keine Bewertungen
- Kothari 1992Dokument5 SeitenKothari 1992Intan Robi'ahNoch keine Bewertungen
- Av BlockDokument38 SeitenAv BlockLanna Harumiya100% (1)
- Acs BTCLSDokument23 SeitenAcs BTCLSAnonymous mj4onk5Z5jNoch keine Bewertungen