Beruflich Dokumente
Kultur Dokumente
Rapid Sequence Intubation
Hochgeladen von
Parth PatelCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Rapid Sequence Intubation
Hochgeladen von
Parth PatelCopyright:
Verfügbare Formate
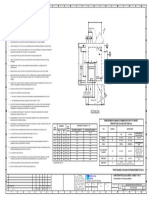
Rapid Sequence Intubation
o Preparation
Check monitors, IVs (2>1), equipment to see if they’re working
Patient’s external canal meatus should be level with sternal notch
Do this by placing bed linens to create a ramp under patient’s head
o Preoxygenation
3 minutes on 100% O2 nonrebreather mask or 6 vital capacity breaths
o Premedication – blunts adverse effect of laryngoscopy
Only if PREMED:
Pediatric – use ATROPINE 0.02 mg/kg
Reactive Airway Disease (asthma) – use LIDOCAINE 1.5 mg/kg
Elevated ICP (strokes) – use LIDOCAINE
MI – use FENTANYL 3 ug/kg
Elevated blood pressure
Dissection - FENTANYL
Give pretreatment 3 minutes before induction medications
o Paralysis with Induction
Induction meds first, then immediately give paralytic meds
Etomidate MC used
Use KETAMINE if CAD (causes tachycardia and thus demand
ischemia)
For paralytics, choose between succinylcholine and nondepolarizing agents
If crush injury (forearm fracture or diffuse bruising), use
VECURONIUM, ROCURONIUM (nondepolarizing agents)
o To reverse nondepolarizing agents, once you see partial
motor activity regained, give ATROPINE 1st (0.01 mg/kg IV),
then EDROPHONIUM (0.5-1 mg/kg IV)
Avoid succinylcholine for anything that may cause HYPERkalemia
o ALS, MS, muscular dystrophy, myasthenia gravis
o Stroke, spinal cord injury
o Major burns
o Sepsis > 5 days (esp. abdominal)
o Malignant hyperthermia history
o Caution with ESRD
o Placement of Tube (intubate)
o Postintubation
Confirm tube with ETCO2 and auscultation
ETCO2 confirms placement, NOT position and cannot r/o main stem
intubation
ETCO2 is most sensitive after SIX manual breaths
False negative ETCO2 can occur with massive PE, MI, or severe
pulmonary edema
Sedate with BENZOS or PROPOFOL to minimize agitation
OPIATES to control pain and blunt sympathetic response to intubation
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Stanford CA-1 ReviewDokument342 SeitenStanford CA-1 ReviewParth Patel100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Enochian Dragon Ritual PDFDokument4 SeitenEnochian Dragon Ritual PDFDenis NantelNoch keine Bewertungen
- Chapter 1 - Central Venous CathetersDokument6 SeitenChapter 1 - Central Venous CathetersParth PatelNoch keine Bewertungen
- 2022 Mable Parker Mclean Scholarship ApplicationDokument2 Seiten2022 Mable Parker Mclean Scholarship Applicationapi-444959661Noch keine Bewertungen
- IEC TC 56 Dependability PDFDokument8 SeitenIEC TC 56 Dependability PDFsaospieNoch keine Bewertungen
- Introduction To Screenwriting UEADokument12 SeitenIntroduction To Screenwriting UEAMartín SalasNoch keine Bewertungen
- Toeic: Check Your English Vocabulary ForDokument41 SeitenToeic: Check Your English Vocabulary ForEva Ibáñez RamosNoch keine Bewertungen
- Meno's Paradox of Inquiry and Socrates' Theory of RecollectionDokument10 SeitenMeno's Paradox of Inquiry and Socrates' Theory of RecollectionPhilip DarbyNoch keine Bewertungen
- Synthesis, Analysis and Simulation of A Four-Bar Mechanism Using Matlab ProgrammingDokument12 SeitenSynthesis, Analysis and Simulation of A Four-Bar Mechanism Using Matlab ProgrammingPedroAugustoNoch keine Bewertungen
- Viscerosomatic Reflexes: System/Organ Sympathetic ParasympatheticDokument2 SeitenViscerosomatic Reflexes: System/Organ Sympathetic ParasympatheticParth PatelNoch keine Bewertungen
- Measurement Assignment EssayDokument31 SeitenMeasurement Assignment EssayBihanChathuranga100% (2)
- Cisco UCS Adapter TroubleshootingDokument90 SeitenCisco UCS Adapter TroubleshootingShahulNoch keine Bewertungen
- Maxillomandibular FixationDokument9 SeitenMaxillomandibular FixationParth PatelNoch keine Bewertungen
- Padi Open Water Scuba Diver Manual: Table of ContentDokument2 SeitenPadi Open Water Scuba Diver Manual: Table of ContentParth PatelNoch keine Bewertungen
- A Randomized Comparison Between Interscalene and Small-Volume Supraclavicular Blocks For Arthroscopic Shoulder SurgeryDokument6 SeitenA Randomized Comparison Between Interscalene and Small-Volume Supraclavicular Blocks For Arthroscopic Shoulder SurgeryParth PatelNoch keine Bewertungen
- OMM - Galbreath PDFDokument1 SeiteOMM - Galbreath PDFParth PatelNoch keine Bewertungen
- Notes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0MDokument1 SeiteNotes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0Mسجى وليدNoch keine Bewertungen
- CHAPTER 1 SBL NotesDokument13 SeitenCHAPTER 1 SBL NotesPrieiya WilliamNoch keine Bewertungen
- Summary of Bill of Quantities ChurchDokument52 SeitenSummary of Bill of Quantities ChurchBiniamNoch keine Bewertungen
- Week-3-Q1-Gen Chem-Sep-11-15-DllDokument12 SeitenWeek-3-Q1-Gen Chem-Sep-11-15-DllJennette BelliotNoch keine Bewertungen
- Peer PressureDokument13 SeitenPeer PressuremightymarcNoch keine Bewertungen
- Close Enough To Touch by Victoria Dahl - Chapter SamplerDokument23 SeitenClose Enough To Touch by Victoria Dahl - Chapter SamplerHarlequinAustraliaNoch keine Bewertungen
- Food ResourcesDokument20 SeitenFood ResourceshiranNoch keine Bewertungen
- Case Study 2Dokument5 SeitenCase Study 2api-247285537100% (1)
- KsDokument5 SeitenKsnurlatifahNoch keine Bewertungen
- SweetenersDokument23 SeitenSweetenersNur AfifahNoch keine Bewertungen
- HatfieldDokument33 SeitenHatfieldAlex ForrestNoch keine Bewertungen
- Sample - SOFTWARE REQUIREMENT SPECIFICATIONDokument20 SeitenSample - SOFTWARE REQUIREMENT SPECIFICATIONMandula AbeyrathnaNoch keine Bewertungen
- LM2576/LM2576HV Series Simple Switcher 3A Step-Down Voltage RegulatorDokument21 SeitenLM2576/LM2576HV Series Simple Switcher 3A Step-Down Voltage RegulatorcgmannerheimNoch keine Bewertungen
- The cardioprotective effect of astaxanthin against isoprenaline-induced myocardial injury in rats: involvement of TLR4/NF-κB signaling pathwayDokument7 SeitenThe cardioprotective effect of astaxanthin against isoprenaline-induced myocardial injury in rats: involvement of TLR4/NF-κB signaling pathwayMennatallah AliNoch keine Bewertungen
- Cyber Briefing Series - Paper 2 - FinalDokument24 SeitenCyber Briefing Series - Paper 2 - FinalMapacheYorkNoch keine Bewertungen
- SLA in PEGA How To Configue Service Level Agreement - HKRDokument7 SeitenSLA in PEGA How To Configue Service Level Agreement - HKRsridhar varmaNoch keine Bewertungen
- John L. Selzer - Merit and Degree in Webster's - The Duchess of MalfiDokument12 SeitenJohn L. Selzer - Merit and Degree in Webster's - The Duchess of MalfiDivya AggarwalNoch keine Bewertungen
- Pidsdps 2106Dokument174 SeitenPidsdps 2106Steven Claude TanangunanNoch keine Bewertungen
- QSP 04bDokument35 SeitenQSP 04bakrastogi94843Noch keine Bewertungen
- Sample Resume For Supply Chain Logistics PersonDokument2 SeitenSample Resume For Supply Chain Logistics PersonAmmar AbbasNoch keine Bewertungen
- The Influence of Irish Monks On Merovingian Diocesan Organization-Robbins BittermannDokument15 SeitenThe Influence of Irish Monks On Merovingian Diocesan Organization-Robbins BittermanngeorgiescuNoch keine Bewertungen