Beruflich Dokumente
Kultur Dokumente
2017 Clinical Guideline For The Management of Immune Thrombocytopenia (Itp) in Children PDF
Hochgeladen von
Fernando FernándezOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
2017 Clinical Guideline For The Management of Immune Thrombocytopenia (Itp) in Children PDF
Hochgeladen von
Fernando FernándezCopyright:
Verfügbare Formate
CLINICAL GUIDELINE FOR THE
MANAGEMENT OF IMMUNE
THROMBOCYTOPENIA (ITP) IN
CHILDREN V3.0
Clinical Guideline Template
Page 1 of 16
1. Aim/Purpose of this Guideline
1.1. This guideline applies to medical staff caring for children with Immune
Thrombocytopenia (ITP).
2. The Guidance
2.1. Acute Childhood Immune thrombocytopenia is usually a benign and self-
limiting condition, where there is an isolated thrombocytopenia of <
100.10< /l, in the absence of any underlying cause. The time from symptom
onset to return of normal platelet counts ranges from a few days to six
months with an average of three weeks.
In 4% of patients resolution of the disease is followed by recurrent episodes of
thrombocytopenia.
Persistent or chronic ITP develops in 10% of patients. The mechanism is
immune mediated with increased destruction of platelets most notably
occurring in the spleen, recent evidence also suggest impaired production
also occurs< . The majority of children require no intervention. Treatment is
based on bleeding severity. Bone marrow assessment is indicated in only
some cases.
2.2. Differential Diagnosis: see appendix 4
ITP should be distinguished from other causes of (a) thrombocytopenia and
(b) bruising/petechiae.
2.3. Presentation of ITP:
Usually abrupt onset of bruises and petechiae in an otherwise healthy
child.
An antecedent viral illness is often reported in the two or three weeks prior
to diagnosis or in some cases it may follow vaccination –MMR,
DT/IPV/Hib/MenC
Less frequent presentations include epistaxis and gross haematuria
Platelet count is usually < 20 x 10 /l at presentation in ITP
2.4. Grading of Severity:
Mild: ( 54% of cases³ ) Bruising/petechiae/minor epistaxis
Moderate: (42%³) More severe skin manifestations, large bruises>
5cm; mucosal lesions and intermittent bleeds from gums, lips buccal
mucosa orophaynx or GI tract;, troublesome epistaxis-longer than 20
minutes; menorrhagia; haematuria; malaena; haematemesis without
hypotension and HB fall < 2gm/dl
Severe: (4%³) Severe epistaxis, melaena, menorrhagia requiring
admission and/or blood transfusion; fall in Hb >2gm/dl; suspected
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 1 of 11
internal haemorrhage; life threatening bleeding if intracranial
haemorrhage or continuous or high volume bleeding resulting in
hypotension or prolonged capillary refill and requiring fluid resuscitation
or blood transfusion>10ml/kg.
2.5. Risk of intracranial haemorrhage:
The risk is small, 0.1-0.5% and is not related to whether a patient has
had treatment previously or not.
2.6. Risk of other serious bleeding:
Epistaxisis or gastrointestinal bleeds in 4%.
2.7. Investigations:
FBC
Blood film - Contact haematologist to confirm film has been examined
and is normal
Clotting studies
Consider according to presentation
GP and save/cross match
U+E, LFT
Detailed coagulation factor assays (discuss with lab first)
DCT particularly if anaemia and high reticulocyte count
Viral serology: EBV, CMV, HIV, HCV, Parvo, VZV
Autoantibodies ANA, anti-DNA, lupus anticoagulant, ANCA
Immunoglobulins, lymphocyte subsets
TFT’s.
2.8. Management:
Platelets are young and ‘sticky’ so management should not be based on
count alone (grade B recommendation –level IIb evidence), symptoms of
bleeding or special circumstances need to be considered.
If typical features of acute ITP [i.e. no pan -cytopenia, acute onset of bruising,
normal white cell count and normal blood film except for reduced platelet count]:
Give parents/ patient information about support l see appendix 3.
Advise avoidance of formal contact sports or activities where there is a
risk of trauma. Otherwise normal activities encouraged.
Avoid asprin and non-steroidal anti-inflammatory drugs.
Relapses may occur during intercurrent viral infections.
Advice on what to do in the event of injury - open door access card
or letter (copy letter to assessment unit/ward.)
Provide information about the UK Childhood ITP registry: give
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 2 of 11
information and consent form for parents and child to read (download
from www.uk- itp.org.) Consent can be obtained at next review. Email Dr
S Harris/ Paediatric research nurses the details of patient once
consented. They will enter data. Data is anonymised and there is no
change to usual management.
Parent or patient to carry card /letter/medical alert particularly if
ITP persists.
2.9. Treatment:
Most children with ITP do not require specific treatment. Treatments do not
resolve the condition faster but can temporarily raise platelet count. Treatment
should be tailored to the individual considering presence and severity of
bleeding, co-morbidities that may increase risk of bleeding, specific instances
such as surgery, and side effects of treatment.
Consideration should be given to performing a bone marrow examination prior
to treatment to exclude other diagnoses such as leukaemia.
Advice about treatment and investigations can be sought from Paediatrician
with benign haematology interest or Bristol Paediatric Haematologists.
If no treatment is given the child should be monitored closely for the first 2
weeks to exclude any emerging serious marrow disorder. Repeat blood count
up to daily initially, but child may not need to stay in hospital if clinically well.
After 2 weeks tests can be less frequent and continued until normal counts.
2.10. Bone marrow tests:
This is not needed for most cases, but is recommended if there are other
abnormalities in the blood count/smear, if systemic features e.g. bone pain or
unexplained large spleen. Discuss with the Associate Specialist in Paediatric
Oncology (or Haematology consultant) if a BM is required. This is usually done
under general anaesthesia. The usual bone marrow list is Thurs pm, if required
at other times co-ordinate between Consultant Anaesthetist (via Anaesthetic
secretary) and doctor performing BM. BM would be indicated in a child with
Trisomy 21 due to increased incidence of leukaemia and myelodysplasia.
BM is also recommended in:
Chronic ITP to ensure there is no slowly progressive myelodysplasia
or marrow failure.
Those failing to respond to treatment.
The presence of excessive or persistent bleeding despite a
platelet count>20.10< /l.
2.11. Treatment options:
Immunoglobulin
Steroids
Platelet transfusion
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 3 of 11
Immunoglobulin
IVIg is only recommended in children with moderate to severe symptomatic ITP
–overt mucosa bleeding or suspected internal bleeding or prior to procedures
likely to induce bleeding( Grade A level1b).
Response is more rapid than steroids.
Dose- Intravenous IG 0.8 g/kg ( to 1gm/kg) this may be repeated depending on
platelet response.
Intravenous immunoglobulin is a pooled blood product. Side effects during and
after infusion may occur e.g. flu like symptoms. There is also potential risk of
transmission of infective agents.
Steroids
2mg/kg/day for one - two weeks, then tail steroids over 5 days regardless of
FBC.
High dose steroids 4mg/kg for 3-4 days can raise count within 72hrs ( 72-
88% cases)
Bristol Haematology team still recommends bone marrow prior to steroids.
Emergency treatment in organ or life threatening situations
Platelet transfusion using 2-3 fold usual volume together with
IV high dose corticisteroids (iv methyl prednisolone 30mgkg/day) and /or IV
immunoglobulin.
Special circumstances Immunoglobulin/ steroids may be given to raise platelet
count prior to surgery (see also appendix 3).
Menorrhagia Tranexamic acid may help reduce bleeding ( TA contraindicated if
haematuris). The Oral Combined contraceptive pill may be considered.
Other treatments
Intravenous anti-D immunoglobulin for RhD positive children but high incidence
of side effects.
Rutiximab in chronic ITP.
Romiplastin unlicienced in children currently.
Splenectomy if >5-10years old with > 12 months history and significant
reduction in quality of life. ( Give Hib, Pneumovax and meningococcal
vaccination preoperatively and lifelong penicillin V postoperatively).
2.12. Post vaccination ITP:
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 4 of 11
If ITP follows within 3 weeks of the first dose of MMR ,then serology to these
viruses should be evaluated and second doses of MMR components only given
if non immune.
2.13. Follow Up:
Children should not be kept in hospital unnecessarily. If platelet count greater
than 10 to 20 and asymptomatic, can be followed as out-patients. Arrange
follow up FBC at 10-14 days to ensure no evolving serious marrow disorder.
There is no need to test FBC’s frequently after this. A repeat FBC on resolution
of symptoms is helpful to confirm remission.
If atypical features emerge at any point e.g. lassitude, pan-cytopenia, limp,
abdominal pain, limb pain, pallor
Arrange bone marrow aspirate under general anaesthesia.
Tests for persistent ITP
Bone marrow evaluation (recommended if ITP persists and no prior response)
Tests to identify infection (HIV/HCV/H pylori) if clinical suspicion or high local
prevalence.
ANA Testing for APLA including ACA and LAC
Serum immunoglobulins (IgG, IgA, IgM)
Review of medication usage.
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 5 of 11
3. Monitoring compliance and effectiveness
Element to be Compliance with sections 2.7,2.8 and 2.9
monitored
Lead Audit lead, paediatric consultants
Tool Individual patient review
Frequency At patient contact
Reporting Paediatric consultants Child health audit and guidelines
arrangements
Acting on Paediatric consultants Child health audit and guidelines
recommendations Required actions will be identified and completed in 3-6 months.
and Lead(s)
Change in Required changes to practice will be identified and actioned within3-
practice and 6 months. A lead member of the team will be identified to take each
lessons to be change forward where appropriate. Lessons will be shared with all
shared the relevant stakeholders
4. Equality and Diversity
4.1. This document complies with the Royal Cornwall Hospitals NHS Trust
service Equality and Diversity statement which can be found in the 'Equality,
Diversity & Human Rights Policy' or the Equality and Diversity website.
4.2. Equality Impact Assessment
The Initial Equality Impact Assessment Screening Form is at Appendix 2.
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 6 of 11
Appendix 1. Governance Information
CLINICAL GUIDELINE FOR THE
MANAGEMENT OF IMMUNE
Document Title
THROMBOCYTOPENIA (ITP) IN CHILDREN
V3.0
Date Issued/Approved: 10th Nov 2017
Date Valid From: 10th Nov 2017
Date Valid To: 10th Nov 2020
Directorate / Department responsible
Dr.S.Harris – paediatric consultant
(author/owner):
Contact details: 01872253041
Clinical Guideline for the management of
Brief summary of contents
Immune Thrombocytopenia (ITP) in children.
ITP
Suggested Keywords: Children
Immune Thrombocytopenia
RCHT PCH CFT KCCG
Target Audience
Executive Director responsible for
Medical Director
Policy:
Date revised: 10th Nov 2017
CLINICAL GUIDELINE FOR THE
This document replaces (exact title of MANAGEMENT OF IMMUNE
previous version): THROMBOCYTOPENIA (ITP) IN CHILDREN
V2.0
Approval route (names of Paediatric consultants
committees)/consultation: Child health audit and guidelines meeting
Divisional Manager confirming
David Smith
approval processes
Name and Post Title of additional
Not Required
signatories
Name and Signature of {Original Copy Signed}
Divisional/Directorate Governance
Lead confirming approval by specialty
and divisional management meetings Name: Caroline Amukusana
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 7 of 11
Signature of Executive Director giving
{Original Copy Signed}
approval
Publication Location (refer to Policy
on Policies – Approvals and Internet & Intranet Intranet Only
Ratification):
Document Library Folder/Sub Folder Clinical / Paediatrics
ITP Support Association
www.itpsupport.org.uk there
is an information page both
for children and teenagers
About ITP for
Links to key external standards kidswww.itpkids.org/content/about_itp.h
tml includes advice on ITP and sport
www.bpl.co.uk provides information
on blood products including
immunoglobulin
1.Guidelines for the investigation of ITP in adults ,
children and pregnancy. British committee for
standards in Haematology task force. B.J.Haem
2003.120574-596
2.Idiopathic thrombocytopenic purpura. PHB
Bolton- Maggs. Arch Dis Child 2000;83:220-222
3. Changing trends in the UK management of
childhood ITP. Grainger el al. Arch Dis Child 2011;
Related Documents: 184234
4. International consensus report on the investigation
and management of primary immune
thrombocytopenia. Provan et al. Blood 2010;115:168-
186
American Society of Haematology 2011 evidence- based
guideline for immune thrombocytopenia. Neuert el al.
Blood 2011; 117: 4190-4205.
Training Need Identified? No
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 8 of 11
Version Control Table
Version Changes Made by
Date Summary of Changes
No (Name and Job Title)
Dr.S.Harris-
Dec 2012 V1.0 Initial Issue
paeditatric consultant
Tabitha Fergus-
Feb 2014 V2.0 Re format only Deputy ward manager
Reformat only.
Nov 2017 V3.0 Reviewed with no changes Sian Harris, Paediatric
Consultant
All or part of this document can be released under the Freedom of Information
Act 2000
This document is to be retained for 10 years from the date of expiry.
This document is only valid on the day of printing
Controlled Document
This document has been created following the Royal Cornwall Hospitals NHS Trust
Policy on Document Production. It should not be altered in any way without the
express permission of the author or their Line Manager.
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 9 of 11
Appendix 2. Initial Equality Impact Assessment Form
This assessment will need to be completed in stages to allow for
adequate consultation with the relevant groups.
Name of Name of the strategy / policy /proposal / service function to be assessed
CLINICAL GUIDELINE FOR THE MANAGEMENT OF IMMUNE THROMBOCYTOPENIA (ITP)
IN CHILDREN V3.0
Directorate and service area: Is this a new or existing Policy?
Child Health existing
Name of individual completing assessment: Telephone:
Sian Harris 01872252800
1. Policy Aim* Clinical Guideline for the management of Immune Thrombocytopenia
(ITP) in children.
Who is the strategy /
policy / proposal /
service function aimed
at?
2. Policy Objectives* Clinical Guideline for the management of Immune Thrombocytopenia
(ITP) in children.
3. Policy – intended Evidenced based and standardised practice
Outcomes*
4. *How will you Patient review
measure the
outcome?
5. Who is intended to Children and families
benefit from the
policy?
6a Who did you Workforce Patients Local External Other
consult with groups organisations
x
Please record specific names of groups
b). Please identify the
groups who have
Clinical Guideline Group
been consulted about
Child Health Directorate
this procedure.
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 10 of 11
What was the Guideline agreed
outcome of the
consultation?
7. The Impact
Please complete the following table. If you are unsure/don’t know if there is a negative
impact you need to repeat the consultation step.
Are there concerns that the policy could have differential impact on:
Equality Strands: Yes No Unsure Rationale for Assessment / Existing Evidence
Age X
Sex (male, X
female, trans-gender /
gender reassignment)
Race / Ethnic X
communities
/groups
Disability - X
Learning disability,
physical
impairment, sensory
impairment, mental
health conditions and
some long term health
conditions.
Religion / X
other beliefs
Marriage and X
Civil partnership
Pregnancy and X
maternity
Sexual X
Orientation,
Bisexual, Gay,
heterosexual, Lesbian
You will need to continue to a full Equality Impact Assessment if the following have
been highlighted:
You have ticked “Yes” in any column above and
No consultation or evidence of there being consultation- this excludes any policies which have
been identified as not requiring consultation. or
Major this relates to service redesign or development
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 11 of 11
8. Please indicate if a full equality analysis is recommended. Yes No
X
9. If you are not recommending a Full Impact assessment please explain why.
No areas indicated
Signature of policy developer / lead manager / director Date of completion and submission
Sian Harris 10th November 2017
Names and signatures of 1. Sian Harris
members carrying out the 2. Human Rights, Equality & Inclusion Lead
Screening Assessment
Keep one copy and send a copy to the Human Rights, Equality and Inclusion Lead
c/o Royal Cornwall Hospitals NHS Trust, Human Resources Department, Knowledge Spa,
Truro, Cornwall, TR1 3HD
This EIA will not be uploaded to the Trust website without the signature of the
Human Rights, Equality & Inclusion Lead.
A summary of the results will be published on the Trust’s web site.
Signed Chris Warren
Date 10/11/2017
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 12 of 11
Appendix 3: Causes of Thrombocytopenia:-
Destructive Thrombocytopenia:-
1.Immune Mediated;
Immune thrombocytopenia
Post-viral infection
HIV
Drug induced e.g. quinine, heparin, teicoplanin
Post-transfusion purpura
Post BMT
Collagen vascular disease
Allo immune thrombocytopenia in the newborn
Maternal chronic ITP
Post vaccination e.g. MMR (1 in 23,000)
Varicella Zoster infection ( additional antibodies to protein S and C can cause purpura
fulminans)
CVID
2. Vasculitis with Endothelial Cell Injury;
Haemolytic uraemic syndrome
Thrombotic thrombocytopenic purpura
DIC
3. Vascular Abnormalities;
Catheters, prosthetic heart valve
Congenital heart disease
Haemangiomas [Kasabach-Merritt syndrome]
Venous malformations
Hyposplenism
Decreased Platelet Production:-
1. Congenital;
Fanconi aplastic anaemia
Thrombocytopenia and absent radii [TAR]
Amega -karyocytic thrombocytopenia
Wiskott-Aldrich syndrome
Paroxysmal nocturnal haemoglobinuria
Von Willibrands type IIB
2. Acquired;
Neoplastic bone marrow disease particularly ALL
Acquired aplastic anaemia
Drug induced
Bruises with Normal Platelet Counts:-
Child non accidental injury
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 13 of 11
Henoch-Schonlein purpura
Increased vascular leak
Collagen tissue disorders eg Ehlers Danlos
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 14 of 11
Appendix 4: Recommended safe platelet counts in adults ( no
equivalent Paediatric guidance available)
Dentrstry platelets>10. 109/l
Dental extractions >30. 109/l
Regional dental block >30. 109/l
Minor surgery >50. 109/l
Major surgery >80. 109/l
Clinical Guideline for the management of Immune Thrombocytopenia (ITP) in children.
Page 15 of 11
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hepatitis Viral en Niños - Que Conocemos en 2021Dokument7 SeitenHepatitis Viral en Niños - Que Conocemos en 2021Fernando FernándezNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Manejo de Emergencia de Fiebre y Neutropenia en Niños Con CancerDokument6 SeitenManejo de Emergencia de Fiebre y Neutropenia en Niños Con CancerFernando FernándezNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Infeccion Osteoarticular Bacteriana Hematogena en NiñosDokument19 SeitenInfeccion Osteoarticular Bacteriana Hematogena en NiñosFernando FernándezNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Avances Recienes en DBP Fisiopatologia, Prevencion y TtoDokument10 SeitenAvances Recienes en DBP Fisiopatologia, Prevencion y TtoFernando FernándezNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Virus y M. Pneumoniae Son Los Ppales Agentes Etiologicas de NAC en Pacientes Hospitalizados en EspañaDokument11 SeitenVirus y M. Pneumoniae Son Los Ppales Agentes Etiologicas de NAC en Pacientes Hospitalizados en EspañaFernando FernándezNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Actualización en Virus Zyka Sfadi2017Dokument4 SeitenActualización en Virus Zyka Sfadi2017Fernando FernándezNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Inr Como Pnto Final de Tto en Niños Con Intoxicacion Por AcetaminofenDokument3 SeitenInr Como Pnto Final de Tto en Niños Con Intoxicacion Por AcetaminofenFernando FernándezNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Prescribiendo en Injuria Renal Aguda PedDokument5 SeitenPrescribiendo en Injuria Renal Aguda PedFernando FernándezNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Cochrane Manejo de La Fiebre en Niños Meremikwu2003Dokument25 SeitenCochrane Manejo de La Fiebre en Niños Meremikwu2003Fernando FernándezNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- Angioedema Pediatrico 2018Dokument8 SeitenAngioedema Pediatrico 2018Fernando FernándezNoch keine Bewertungen
- Accidentes Cerbrovasculares en Neonatos y Edad Infantil Bernsonleung2016Dokument17 SeitenAccidentes Cerbrovasculares en Neonatos y Edad Infantil Bernsonleung2016Fernando FernándezNoch keine Bewertungen
- Bone and Joint Infections.18Dokument12 SeitenBone and Joint Infections.18Fernando FernándezNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Enfermedad Meningocócica 2017Dokument14 SeitenEnfermedad Meningocócica 2017Fernando FernándezNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Abcdef en Cuidado CriticoDokument19 SeitenAbcdef en Cuidado CriticoFernando FernándezNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Bronquiolitis N.E.J.M. Enero 2016Dokument11 SeitenBronquiolitis N.E.J.M. Enero 2016Fernando FernándezNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Bronquiolitis N.E.J.M. Enero 2016Dokument11 SeitenBronquiolitis N.E.J.M. Enero 2016Fernando FernándezNoch keine Bewertungen
- 16-Pediatric Infections - Volume 1 - VaricellaDokument24 Seiten16-Pediatric Infections - Volume 1 - VaricellaFernando FernándezNoch keine Bewertungen
- Approach To Pediatric EmergencyDokument516 SeitenApproach To Pediatric EmergencyFernando Fernández100% (3)
- Enfermedad de KawasakiDokument538 SeitenEnfermedad de KawasakiFernando FernándezNoch keine Bewertungen
- Desordenes Respiratorios en El Neonato Pediatrics in Review 2010Dokument12 SeitenDesordenes Respiratorios en El Neonato Pediatrics in Review 2010Fernando FernándezNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Manual de Cuidados NeonatalesDokument679 SeitenManual de Cuidados Neonatalesgabyriveraamaya100% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Pathology Lecture 7 - LiverDokument11 SeitenPathology Lecture 7 - Livercgao30Noch keine Bewertungen
- Gout N C P BY BHERU LALDokument1 SeiteGout N C P BY BHERU LALBheru LalNoch keine Bewertungen
- Protocols Sepsis Treatment Stony BrookDokument6 SeitenProtocols Sepsis Treatment Stony BrookVicky Chrystine SianiparNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Pedia CaseDokument65 SeitenPedia CaseJason MirasolNoch keine Bewertungen
- Geriatric PsychiatryDokument91 SeitenGeriatric PsychiatryVipindeep SandhuNoch keine Bewertungen
- Study On The Effect of Vatajstanyadushti in ChildrenDokument8 SeitenStudy On The Effect of Vatajstanyadushti in ChildrenRadha DeviNoch keine Bewertungen
- Journal On Respiratory Disorders in PregnancyDokument7 SeitenJournal On Respiratory Disorders in PregnancyallyssaNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Fading Kitten Emergency Protocol: Hypothermia HypoglycemiaDokument1 SeiteFading Kitten Emergency Protocol: Hypothermia HypoglycemiaJose Emmanuel MNoch keine Bewertungen
- Ear MedicationDokument15 SeitenEar MedicationPascalina Monts'onyaneNoch keine Bewertungen
- Homeopathic Remedy Pictures Alexander Gothe Julia Drinnenberg.04000 1Dokument6 SeitenHomeopathic Remedy Pictures Alexander Gothe Julia Drinnenberg.04000 1BhargavaNoch keine Bewertungen
- Pancreatic Cancer Therapeutics in Major Developed Markets To 2021Dokument7 SeitenPancreatic Cancer Therapeutics in Major Developed Markets To 2021Kanchan JagtaniNoch keine Bewertungen
- Swami Karmamurti Saraswati, DC, DO, Director of Satyananda Ashram, MelbourneDokument5 SeitenSwami Karmamurti Saraswati, DC, DO, Director of Satyananda Ashram, MelbourneJacklynlim LkcNoch keine Bewertungen
- Emergency Department Case Management: Second EditionDokument39 SeitenEmergency Department Case Management: Second EditionsadikinNoch keine Bewertungen
- Dermoscopy Seborrheic Keratosis-2017Dokument7 SeitenDermoscopy Seborrheic Keratosis-2017kikiNoch keine Bewertungen
- Pneumonia Clinical Case Study BSN 2 2 Group 4Dokument43 SeitenPneumonia Clinical Case Study BSN 2 2 Group 4Precious Jenichris TamayoNoch keine Bewertungen
- Introduction to Pakistan's National Essential Drug ListDokument16 SeitenIntroduction to Pakistan's National Essential Drug ListUmair MazharNoch keine Bewertungen
- Jurnal Ebn Managemen 1Dokument7 SeitenJurnal Ebn Managemen 1KohakuNoch keine Bewertungen
- Download John Murtaghs General Practice Companion Handbook 7Th Edition John Murtagh full chapter pdf scribdDokument67 SeitenDownload John Murtaghs General Practice Companion Handbook 7Th Edition John Murtagh full chapter pdf scribdderrick.ayala232100% (4)
- PE 3 ReviewerDokument5 SeitenPE 3 ReviewerZac GarciaNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Dual Antiplatelet Therapy Vs Alteplase For Patients With Minor NondisablingDokument10 SeitenDual Antiplatelet Therapy Vs Alteplase For Patients With Minor Nondisablingbetongo Bultus Ocultus XVNoch keine Bewertungen
- Chapter 1 Introduction FinalDokument5 SeitenChapter 1 Introduction FinalDivine Grace Cabungcag0% (1)
- Some Applications of Genetic EngineeringDokument9 SeitenSome Applications of Genetic Engineeringshibi sharmaNoch keine Bewertungen
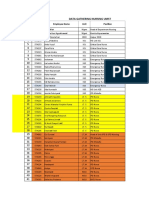
- Data Peserta Gartheting LT 3aumst Final 2022Dokument11 SeitenData Peserta Gartheting LT 3aumst Final 2022Doni IrawanNoch keine Bewertungen
- Tinnitus Today December 1998 Vol 23, No 4Dokument29 SeitenTinnitus Today December 1998 Vol 23, No 4American Tinnitus AssociationNoch keine Bewertungen
- Anaesthetic Considerations for Day Care SurgeryDokument8 SeitenAnaesthetic Considerations for Day Care SurgerySirisha Ckv100% (1)
- B R Robbins and Cotran: Pathologic Basis of Disease, 8th EditionDokument1 SeiteB R Robbins and Cotran: Pathologic Basis of Disease, 8th EditionabdallhNoch keine Bewertungen
- Diabetes in Pregnancy: Management ofDokument8 SeitenDiabetes in Pregnancy: Management ofdiana rossNoch keine Bewertungen
- Application of Nursing ProcessDokument2 SeitenApplication of Nursing ProcessClarence ViboraNoch keine Bewertungen
- Metabolic Stress PDFDokument30 SeitenMetabolic Stress PDFNurul Latifa MuhammadNoch keine Bewertungen
- WVSU Adult Nursing ProcessDokument9 SeitenWVSU Adult Nursing ProcessMark ArconadaNoch keine Bewertungen
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (13)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)