Beruflich Dokumente
Kultur Dokumente
Clinical Interpretation of Laboratory Tests - Edition Fifth
Hochgeladen von
Teodora Polgar100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
188 Ansichten796 SeitenA practical manual about clinical interpretation of laboratory tests and the principles behind them. Very useful!
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenA practical manual about clinical interpretation of laboratory tests and the principles behind them. Very useful!
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF herunterladen oder online auf Scribd lesen
100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
188 Ansichten796 SeitenClinical Interpretation of Laboratory Tests - Edition Fifth
Hochgeladen von
Teodora PolgarA practical manual about clinical interpretation of laboratory tests and the principles behind them. Very useful!
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 796
CLINICAL
INTERPRETATION.
of LABORATORY
TESTS
Fifth Edition
Preface to the Fifth Edition
There have been numerous changes and advances in clinical
pathology smce the last edition of this book appeared 1 have
attempted to evaluate these changes and adyances and to incorporate
those that appear to be both pracucal and valuable mto the text
At the same ume I have removed tests that have been superseded
by newer and better methods I hope that this has resudted in a
book that will be a useful reference for physicians, medical students,
and technologists
‘The advances in enzyme chemistry warranted a separate chapter
for this subject. The use of radioactive isotopes, parucularly in the
diagnosis of thyroid disease, resulted in the addition of much new
material Discussion of abnormal hemoglobm and newer concepts
of the blood-clotung mechanism were also imcluded Blood groups
and tests pertaming to the musculoskeletal system were separated
and placed in new chapters
I wish to express my deep appreciation to Margaret K Johnson
for her painstaking work in the preparation of the manuscript
Lam also deeply grateful to the publishers for therr cooperation in
preparation of the reviston
RaymMonp H Goopare, MD
vu
Preface to the First Edition
The numerous advances m xi branches of clinical pathology have
created a demand for ready information on interpretation of labora
tory tests and on the most helpful laboratory procedures applicable
to the diagnosis of a gren disease It 1s hoped that ch1s book will
fill such a need by bringrng together the laboratory and the clinic
Medical students :mterns and medical technologists as well as
chnicrans should find it a valuable reference work for their particu
Jar problems in tlus field
Part 1 deals with the physiology normal values and the signifi
cance of abnormal values of the various body fluids and excreta
Thus section also includes chapters on bas1l metabolic rates I:ver
function tests bacteriologic virus and mycotic examinations shin
tests and poisons Chemotherapy and anttbiotic therapy in relation
to bicterrology are discussed in Chapter 13 Bacteriologic Rami
nations
In Part 2 diseases with associated laboratory findings are dis
cussed according to the various systems eg the Blood and Bone
Marrow Lach disease which lends tself to laboritory diagnosis 1s
bmefiy outhned ‘Tins 15 followed by a hst of changes to be expected
in the pertinent laboratory examinations These examinations are
given in the order of importance with the most important first
1”
x Preface to First Edition
Although it is hoped that other atomic bombs will not be used,
the blood changes resulting from those dropped on Japan ate listed.
These sequelae are similar to those which have been seen in radia-
tion sickness following overexposure to x-rays.
Part 2 ends with methods of preparing body fluids, excreta, and
tissues for the laboiztory. The proper methods of preparing speci-
mens is important in order that accurate results may be obtained.
For example, the blood glucose level drops when tt 1s Kept at room
temperature unless a preservative is added.
Although: certain tests are pathognomonic, clinicians should not
rely entirely upon the laboratory for a diagnosis, The laboratory
and x-ray department are helpful adjuncts in the modern doctor's
diagnostic armamentarium, but they should not replace a careful
history and physical examination. The history and physical exam-
ination are also important so that the laboratory tests requested will
be pertinent to the diagnosis. Certain routine tests are desirable
for the protection of the patient because certain diseases may be
symptomless at the time. Thus, most hospitals perform routine
urinalyses, blood-count estimations, and serological tests for syphi-
ls However, it should be remembered that frequent venipunceures
may work a hardship on the patient.
Dr. Alexander §. Wiener was hind enough to help me in organiz
ing the material on blood groups and the Rh factor. For this, I am
most appreciative. Dr. William T, Carleton reviewed Chapter 12,
Liver-Function Tests, and made several valuable suggestions.
T wish to thank Mfrs, Isabel Baker Carleton for her painstaking
work in preparing certain illustrations. The original photographs
were taken by Mr. Matthew D. Carrigan, who has always been most
cooperative, .
Here J wish to express my gratitude to my secretary, Miss Agnes
M. O'Hare, who spent many hours in preparing the manuscript
and in checking references.
Finally, 1 wish to express my appreciation to the publishers for
their help in the many details about which I have asked their advice.
Raymonp H. Goopace, M.D.
Table of Contents
Part 1
Body Fluids, Excreta, and Functional Tests
HEMATOLOGY
Bone Marrow
Blood
Erythrocytes
Hemoglobin
Leukocytes
Platelets
Coagulation of Blood
Tests for Hemorrhagic Disorders
New Terminology of Blood Cells
Broop CHEMstry
Grouping of Chemical Constituents
Physiology of Acid-Base Equilibrium
Chlorides
Sodium .
Potassium
Magnesium
Calcium
Phosphorus
Tron
xi
ii Table of Contents
CHAPTER PACE
2 Broop Cuexusrey (Continued)
Tron Binding 105
Copper 106
Todine 106
Protein Bound Iodine 107
Lipids 107
Bilirubin 110
Therapeutic Drugs 14
Miscellaneous Tests 1G
3 Bioop Cuemistry (Continued) 127
Enzymes 197
4 SPROLOcY . 140
Acquired Antibodies 140
Cold Autohemagglatinins 44
Nonspecific Antibodies 144
Bacterial Agglutnation Tests 145
Nonspecific Agglutination Tests 150
Complement Fixation 157
Flocculation Reactions 162
Precipitin Tests 166
Antistreptolysin 167
Antihyaluronidase 168
’
5 Bioop Grours 172
6 Urine 192
Physiology of Urine Formation 192
Normal Urine 192
Volume 192
Color 195
Odor 196
Specific Gravity 196
Reaction 200
17-Ketosteroids (Usinary Androgens) ae
Proteins .
Table of Contents veces xiii
a4 oI
CHAPTER PAGE
6 Urine (Continued)
Nonprotein Nitrogenous Products tee 205
Sugars ae ee nee . 207
Products of Acidosis oe 220
Pigments eee ee 2u1
Inorganic Constituents : : 215
Sediment + : os 217
Casts . . 219
Crystals . 222
Bacteriological Examination : 225
Ova and Parasites soe 225
Special Tests 225
Kidney-Function Tests . os : 228
Drugs and Poisons . : 235
7 Gastric aNp DUODENAL CONTENTS 238
Physiology of the Stomach oe 238
Normal Gastric Contents 239
Tubeless Detection of Gastric Acidity (Diagnex
Blue Test) 242
Abnormal Findings in Gastric Contents 243
Duodenal Contents : 247
Abnormal Duodenal Fluid : 248
Biliary System 249
Bacteriological Examination of Gastric and
Duodenal Contents oa 250
8 GEREBROSPINAL FLUID : 251
Physiology - . 251
Spinal Puncture 252
Physical Characteristics . . 254
Chemical Composition 257
Precipitation Tests... - : : 260
Miscellaneous Tests . : 263
Bacteriological Examination . 264
9 Sruruat AND SALIVA . : 266
Source of Sputum . 266
xiv
CHATTER
9
10
MW
12
13
14
Table of Contents
Spurun anp Sativa (Continued)
Collection :
Physical Characteristics
Microscopic Examination
Bacteriological Examination
Fungus Examination
Saliva
Frers
Macroscopic Examination
Chemical Examination
Microscopic Examination
Bacteriological Examination
Ova and Parasites
Helminths
‘TRANSUDATES AND EXUDATES
Transudates
Exndates
Bacteriological Examination
SPERMATOZOA
Ongin
Examination
‘Tests ror Liver AND Bruiary Funcrigy
Physiology of Liver Function
Classification of Tests
Changes in Urine and Feces Secondary to Liver
Damage and Biliary Obstruction
Liver Biopsy
BAcTERIOLOGICAL EXAMINATIONS
Chemotherapeutic Drugs in Relation to Bacteriology
Antibiotic Drugs in Relation to Bacteriology
Resistance of Organisms to Chemotherapeutic
Agents
Blood
PAGE
266
267
268
272
272
272
275
275
277
280
281
281
284
292
292
295
296
297
297
297
302
302
309
323
326
329
329
529
332
335
Table of Contents x
catAPTER PAGE
14 BACTERIOLOGICAL Exaninations (Continued)
Urine coke eee 337
Gastric and Duodenal Contents 339
Cerebrospinal Fluid 340
Sputum 342
Feces 344
Transudates and Exudates 347
Orifices and Tissues 349
15 RIcKETTSIAS AND VIRUSES 357
Rickettsias 357
Viruses 361
16 MycoLocicaL ExaMInaTIONS 378
Dermatomycoses : : 378
Fungous Infections of Skin or Mucous Membrane
with Frequent Systemic Involvement 383
Primary Systemic Infections 386
17 ‘Tesrs FoR ALLERGY AND IMMUNITY 389
Types 389
For Primary Allergenic Diseases 391
For Bacterial Infections 392
For Fungous Infections 396
For Parasitic Infections 397
For Viral Infections 399
18 Toxico.ocic EXAMINATIONS 402
Gaseous Poisons 403
Inorganic Poisons 405
Organic Poisons 410
Part 2
Diseases with Associated Laboratory Findings
19 Tue Broop ann HEMATOPOIETIC ORGANS 417
The Anemias Al7
434
Hemoglobinopathies
Table of Contents
xvi
CHAPTER PACE
20 9 THE Bioop axp Hesatoroirtic Orcans (Continued)
Hemorrhagic Diseases 457
Polycythemia 472
Leukemias 476
Leukemoid Reactions 485
Agranulocytosis 485
Effects of Atomic Bomb Explosion 487
Infectious Mononucleosis 490
Acute Infecuous Lymphocytosis 492
Lymphoblastoma 492
Parasitic Diseases 493
21 HEART anv Boop VEssELs 500
Infections of the Heart 500
Diseases Causing Cardiac Insufficiency 504
Diseases of Blood Vessels 506
22 Tilt Respiratory SysTes 510
Infections of Throat and Larynx 510
Lungs 513
23 GASTROINTESTINAL TRACT AND PANCREAS 530
Mouth and Pharynx 530
Esophagus 530
Stomach and Duodenum 531
Intestines 534
Pancreas 550
24° Liver Ann Brurary TRAcT 557
Selection of Tests 557
Diseases of the Liver 562
Parasites 569
Extrahepatic Biliary Discases 569
25 THe GentrouriNary SYSTEM 572
Kidneys 572
Bladder 592
Genitalia 593
599
Pregnancy
Table of Contents xvii
CHAPTER PAGE
26 MuscuLoskeLeral SYSTEM aan » . , 603
‘ Myasthenia Gravis : . oe 603
Muscular Dystrophy . 604
+ Periodic Muscular Paralysis 605
Dermatomyositis . 605
Osteomyelitis 605
Paget's Disease (Osteitis Deform man ) : 606
Osteogenic Sarcoma . 606
Osteitis Fibrosa Cystica . 606
Multiple Myeloma. 608
Arthritis 609
7 EnpocrixE GLANDS 618
Pituitary Gland 618
Placenta 626
Ovaries : 627
Adrenal Gland : 629
. Thyroid 642
Parathyroid 658
Islands of Langerhans 660
28 CENTRAL NeRvous SYSTEM 669
Bacterial Infections 669
Mycotic Infections 675
Parasitic Infections . 676
Viral Infections 677
Tumors G8t
Trauma 682
Subarachnoid Hemorrhage . 683
Ruptured Disk 683
Multiple Sclerosis 684
Cerebral Hemorrhage and Thrombosis : 634
Intrathecal Injections soe 685
29 BacrexioLocican Discasrs avp Diseases oF DousrruL
Cause . . .. . §87
Systemic Infections 687
Infections of Intestines 703
Collagen Diseases . 708
xviii
CHAPTER
30
31
32
INDEX,
Table of Conte
Viraman Dericiency
Vitamin-A Deficiency
Vitamin-B Deficiency
Vitamin-G Deficiency
Vitamin-P Deficiency
Viramin-D Deficiency
Vitamin-K Deficiency
Merasouic Disorpres
Fluid and Electrolyte Balance
Fluid and Electrolyte Imbalance
Edema
Shock
Burns
Glycogen Storage Disease
Hemochromatosis
Miscellaneous Meliturias
Alkaptonuria
Poiphyrra
Primary Essential Xanthomatoses
Kwashiorkor
COLLECTION AND Care or Lanoratory SrrciMEeNs
Hematology
Blood Chemustry
Serology
Blood Cultures
Urine
Gastric and Duodenal Contents
Cerebrospinal Fluid
Sputum
Feces
Transudates and Exudates
Qulrarass nd. Sears
Cytological Studies for Tumor Cells
Surgical Specimens
Part 1
Body Fluids, Excreta,
_and Functional Tests
1
Hematology
BONE MARROW
Anatomy:
The bone marrow lies in all of the bones and is surrounded
by the endosteum, The functioning bone marrow is made up of
young and adult blood cells and their precursors, blood vessels, fat
cells, and reticulum. The reticulum is connected with the endos-
teurn and is closely bound with the blood vessels. Most of the
reticulum cells are fixed, but they are capable of rounding off to
become large free macrophages. Lymph vessels have not been
found in the bone marrow, and nerve structures have been demon-
strated only in connection with the larger blood vessels. Lymph
follicles have been seen and are generally considered to be normal
bone marrow structures.
The blood supply of the marrow is made up of a series of
branching thin-walled vessels which connect with the nutrient
artery of the bone and its vein. ‘The blood supply is further derived
from, the axteries af the shaft af the hone and af the eniphysce. The
finer divisions of these vessels are capillaries, some of which are
collapsed, while others are dilated. The intravascular or extra-
vascular origin of blood cells has not been definitely settled. Many
investigators believe that all blood cells have an extravascular?
origin in the bone marrow.
Almost all of the bone marrow is red and is functioning during
the first few years of life. From five years of age, fat cells appear
3
4 Body Fluids, Exereta, and Functional Tests
in the marrow of the long boncs so that ultimately hematopoietic
marrow is found only in the proximal ends of the femur and
humerus. The red marrow in adult life is limited mostly to the
bones of the trunk and head; namely, the skull, vertebrae, ribs,
sternum and innominate bone. In adults, the total bone marrow
has been estimated to weigh from 1600 to 3700 gm. (314 to 8
pounds). However only about half of it is in an active state in
the normal adult.
The nonfunctioning marrow of the long bones retains the essen-
tial hematopoietic structures; and with proper stimulation it will
start to function. Exiension of hematopoiesis to the long bones is
stimulated by pernicious anemia, myelogenous leukemia, and to
a certain extent during residence at high altitudes.
Extramedullary Hematopoiesis:
Extramedullary hematopoiesis may on occasion supplement the
formation of cells by the bone marrow, Foci of hematopoiesis have
been seen in the spleen, lymph nodes, adrenals, cartilage, broad
ligament, organizing thrombi, and fat tissue. These blood forming
foci may be made up of erythroblasts or their precursors, myelo-
cytes, megakaryocytes or all three types. Extramedullary hema-
topoiesis occurs particularly in anemia of infants and young chil-
dren,? pernicious anemia,3.4 macrocyte anemia of Jiver disease,
metastatic carcinoma,?, ° malignant granuloma (Hodgkin's disease)
of the bone marrow,® bone marrow injury by a toxin, anemia
resulting from severe sepsis,27 leukemia,¢ & and osteosclerosis.?
Function of Bone Marrow:
The bone marrow forms erythrocytes, granulocytes, and plate-
Jets These cells are formed from special precursor cells, and nor-
mally enter the blood stream only after they have matured. The
method whereby the cells enter the circulation is stil] debated. One
view2° contends that the red cells arise within the endothelial lin-
ing, while the leukocytes are formed outside the vascular spaces.
One of the reasons advanced to support this thcory is the fact that
the erythrocytes possess no means of locomotion and could not
Hematology 5
reach the blood stream if they were produced extravascularly. It is
held by Klima and Rosegger1? that all blood formation is extra-
vascular, the new cells being released into the circulation by
diapedesis or by temporary dissolution of the capillary wall.
Sabin!2 found that granulocytes enter the blood stream at
regular intervals with small hourly increases and larger daily in-
creases in the afternoon and at midnight. Chemotactic factors
probably play an important role in drawing the leukocytes out of
the bone marrow. As for the erythrocytes many contend that
anoxemia is the stimulus which brings them into the blood stream.
Such anoxemia may be brought about by deficient pulmonary
ventilation, deficiency of oxygen in the air as in high altitudes,
fixation of hemoglobin (¢.g., carbon monoxide poisoning), or by
anemia. This, however, is apparently not the sole factor, as is sug-
gested by observationst? which show that there is imperfect corre-
lation between anoxemia and marrow hyperplasia.
Control of Hematopoiesis:
There is also evidence that certain hormones influence hema-
topoiesis. According to Gordon and Charipper!4 castration of
female rats raises the red cell count and, of male rats lowers the red
cell count. Evidence that other endocrine glands influence erythro-
poiesis is seen in the anemia which is associated with hypethyroid-
ism, hypoadrenalism (Addison's disease) and hypopituitarism (Sim-
monds’ disease) and by the increased red cell count which may be
found in hyperadrenalism (Cushing’s syndrome). Influence of
endocrine glands on other blood cells is noted in the lymphocyto-
penia, the decrease or disappearance or eosinophils and rhe mncrease
in the number of polymorphonuclear leukocytes which follow the
administration of adrenocorticotropic hormone or adrenal cortical
hormones. It ts possible that these hematopoietic effects are mani-
festations of their action on general metabolism which influences
the growth of cells.
The specific influence of iton and liver extract on erythro-
poiesis in various types of anemia must also be recognized. They
are, however, not governing factors in erythrocyte formation; rather
6 Body Fluids, Excrefa, and Functional Tests
they are materials of which the red cell is composed or are concerned
with its construction and development.
Examination of the Bone Marrow:
Frevious investigators had studied the bone marrow from
trephine specimens of che long bones and sternum, but Arinkin?®
in 1929 was the first to propose the technic of needle operation.
The aspiration technic has been improved and is generally pre-
ferred over trephining. In fact trephine specimens are taken only
when repeated aspirations have failed. Aspiration specimens are
usually taken from the sternum because of its accessibility and
because active bone marrow may be obtained at all ages. Other
sites for bone marrow aspiration are the iliac crests, the spinous
processes of the vertebrae, ribs, and in children the upper tibiae.
Technic: The skin over the midsternum is shaved if necessary,
and carefully sterilized with an appropriate antiseptic. Aseptic
technic is observed throughout by the operator. The skin, subcu-
taneous tissue, and periosteum are anesthetized. A short, beveled 18
gauge needle with a guard and a stylet is used. The guard 1s set at
Tem from the tip for an adult and 0.6 to 0.2 cm. for a child. When
the anesthesia is effective, insert the needle vertically into the
middle of the sterntum between the second and third ribs, using a
boring motion. When the cortex is pierced, a “give” is felt as the
point encounters the soft marrow. The stylet is removed and a 5 cc.
syringe 1s attached. Suction is then applied and marrow pulp is
pulled into the syringe. If no specimen 1s visible in the syringe, the
stylet is replaced, and the needle is forced deeper into the marrow.
After remova! of the needle, a sterile bandage is placed over the
puncture wound.
Smears, contact smears or imprints, and supravital stain prepara-
tions may be made from the material. Satisfactory tissue for sec:
tioning is nat usually obtained by this method, but small bits of tis-
sue may be fixed and blocked together. The smears may be stained
by Wright or Giemsa stains.
Sternal puncture is contraindicated in serious hemorrhagic con
ditions including hemophilia.
Hematology 7
Normal Bone Marrow: :
Erythrocyte counts and leukocyte counts may be made on mar-
row material, but there are marked fluctuations. Erythrocyte counts
and hemoglobin determinations on marrow material are about the
same as the patient's peripheral blood or slightly lower. The white
cell count, however, ranges from 10,000 to 190,000 per cu. mm.
according to Segerdahl.1¢ The leukocyte count tends to be higher
the Jess the amount of marrow withdrawn. It would appear, there-
fore, that marrow cel! counts are of little or no value.
The differential count yields the most information. For a sat
isfactory differential count, at least 300 to 500 cells must be counted.
Table I shows the ranges to be expected in the normal adult, It
must be realized that the ranges of the normal bone marrow cells
as given by different investigators vary widely. For example, Osgood
and Seaman have lower values for myeloblasts (0-2.4), promyelocytes
(0-8) and erythroblasts (3-21), and higher values for lymphocytes
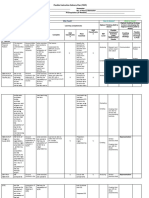
Tapis 1; Percenraces or Cenis 1x Bone Manzow or
Norman Aputts*
Range Average
Myeloblasts ... . woe +. [003 to 50] 2.0
Promyelocytes... eae . - $10 to 80) 50
Myelocytes:
Neutrophilie.. . . ws . . . | 50 to19.0] 12.0
Eosinophilic.... -.. - : : : . 7005 to 80] 15
Basophilic.... 0. wee eee . 000 to 00.5] 00.3
Metamyelocytes (juyenile” forms). - -}13.0 to320} 22.0
Polymorphonuclear neutrophils. . . «f 78 to800) 200
Polymorphonuelear posinop his soe oe --- 00.5 to 4Q} 20
Polymorphonuclear basophils. . «+» {00.0 to 00.7; 00.2
Lsinpboeytes. . . 3.0 to17.0] 100
Plasma cells . hoe +» +-/00.0 to 2.0; 00.4
Monocytes .. . oe + . 005 to 50] 20
Reticulum cells . nae soe 00.1 to 2.0} 00.2
Megakaryoeytes wee . . 00 03 to 30 00.4
Pronormoblasts (maeroblasts) . -| 1.0 to 4.0
Normoblasts (basophilic, polychromatophilic, andacidophi lic)! 7.0 to Py ° isd
* Wintrobe, M. M,: Clinical Hematology. Fifth Ed. Lea & Febiger, Philadel-
phia, 1961, p, 65,
8 Body Fluids, Excreta, and Functional Tests
(7-30). Custer on the other hand uses as normal! a higher range of
myetocytes {up to 34), and a lower range of polymorphonuciear
neutrophils (up to 20) and lymphocytes (up to 7).
Bone Marrow Changes in Disease:
Careful microscopic examination and intelligent interpretation
of bone marrow smears yield information in certain blood disorders
in which the peripheral blood shows little or no change. In evaluat-
ing a bone marrow smear, attention should be given to the follow-
ing criteria: (I) The myeloid: erythroid ratio (MLE. ratio). The
normal M:E ratio excluding adult leukocytes is 0.56:1, A normal
M:E ratio may be found in myelosclerosis, aplastic anemia and
multiple myeloma as well as in the normal smear. If the proportion
of myeloid cells to erythroblasts is increased, leukopoiesis from
infection, leukemoid reaction or leukemia may be suspected. The
altered ratio may also be due to decrease of erythroblasts. If rhe
proportion of erythroblasts is increased, it may be due to depression
of myeloid activity as in agranulocytosis, or to hyperplasia of the
erythropoietic tissue. Such erythroblastic hyperplasia may be nor-
moblastic and due to blood loss, increased blood destruction, iron
deficiency, polycythemia vera, plumbism or cirrhosis of the liver.
It may be megaloblastic such as is seen in pernicious anemia, sprue
and other macrocytic anemias. (2) The number and shape of
megakaryocytes. It should also be noted whether or not they are
breaking up to form platelets. (3) The presence of cells which are
normally not found in marrow smears, ¢.g., tumor cells from meta-
static neoplasm such as carcinoma or Hodgkin's disease, plasma or
“myeloma” cells, Gaucher's cells, lupus erythematosus, (L-E.) cells
and foam cells of Niemann-Pick disease. (4) Note the presence of
parasites such as malaria, Leishmania, and Histoplasma capsulatum.
(5) Note the presence of pathological processes such as sarcoidosis,
tuberculosis and brucellosis. (6) 1f inadequate material is obtained
alter repeated aspirations, a bone marrow biopsy with a trephine is
indicated.
Kolmer!? has summarized the important changes in many of
these diseases as follows:
Hematology
Disease
Pernicious and related anemias ....
Aplsstic anemia
Aeute hemolytie anemias
Chronie hemolytic anemias
Sickle-cell anemia ..
Hypochromic microeytic anemia
Congenital hemolytic jaundice .
‘Thrombopenic purpura. .. ..
Erythremia........ -
Important Changes
Untreated or during relapse: (1) increase of
nucleated erythrocytes; (2) preponder-
ance of megaloblasts; (3) increase of
reticulum (Ferrata) cells; (4) abnormal
lenkopoiesis, especiatly lymphocytes; (5)
reduction in megakaryocytes
Chiefly red blood corpuscles: relative lym-
phocytosis constituting from 60 to 100
per cent of the nucleated cells; striking
immaturity of the red and white cor-
puscles; they may be normally cellular or
hyperplastic
Markedly hyperplastic: 60 per cent or more
of the nucleated cells belong to the eryth-
rocytic series; leukocytes relatively re-
duced.
. Normoblastie hyperplasia characteristic
(normoblasts or macroblasts): no megalo-
blasts
. Largely nucleated red cells (chiefly normo-
blasts): there may be moderate shift to
the left of the myeloid leukocytes;
eosinophils relatively increased; megakar-
yocytes may be increased
Hyperplastic: increase of normoblasts;
no megaloblasts; granulopoiesis usually
normal
Erythropoietic hyperplasia. of the normo-
blastic type: no megaloblasts or giant,
abnormal leukocytes .
Many megakaryocytes: usually an increase
of erythroid elements due tosevere hemor-
rhage and anemia
Dark red and very cellular: hyperplasia of
all elements, moderate increase of nucle-
ated erythrocytes; sometimes an increase
of megakaryocytes, myelocytes, and
royeloblasts
Myeloblastic and myelocytic leukemia 9Marked hyperplasia» crowded with myelo-
blasts and more primitive cells; in eosino-
philic leukemia, preponderance of cosino-
phils; in monocytic leukemia, myelocytes
and myeloblasts; also “monoblasts” and
“monocytes” in some cases; in chronic
myelocytic leukemia, the differential
count is similar to that of the blood
10
Body Fluids, Excreta, and Functional Tests
Disease
Lymphocytic leukemia .
Aleukemic Icukemia
Tafectious mononucleosis
Agranulocytosis.
Mahgnant granufoms
(Hodgkin’s disease)
Multiple myeloma,
Composition of Blood:
Important Changes
. .-May be only shghtly changed: ‘usually,
however, a sell-marked lymphorytosis
(80 to 90 per cent of the cells}
Of great value in diagnosis’ frequently the
changes are identical with those of typical
blood findings; sometimes musleading
when only a few cells are obtained, but
pronounced unmaturity of the leukocytes
may be observed when cellularity is
reduced; in leukopenic cases of lymphocy-
tic leukemia, marrow lymphocytosis may
‘be shght or absent.
Increase of lymphocytes or moderate shift
to left of myeloid leukocytes chiefly of
value from » negative standpoint in the
sense that findings characteristic of leu-
kernia are absent
Normal erythropoietic tissue and normal
numbers of megakaryocytes. striking
lack of granulocytes; plasma cells, lym-
phocytes, and reticulum cells may be
increased
Findings variable and nonspecific. there
may be slight shift to left in the myeloid
celis; also sught monocytosis or moderate
eosinophilia; 50 lymphocytosis; relative
reiiuction in nucleated ted cells
Various types described such as myelo-
blastic, lymphoblastic, and erythroblastie,
with “plasms cells” the usual designation:
myeloma cells most characteristic, can-
stituting from 5 to 65 per cent of all cells
present
BLOOD
The blood is a fluid in which cells are free and suspended. The
fluid part is “plasma™ before clotting occurs and “serum” after
clotting accurs, Plasma is made up of water from 91 to 92 per cent
and solids from 8 to 9 per cent. The solids consist of serum albumin,
serum globulin, fibrinogen, sodium, calcium, potassium, magnesium,
phosphorus, the nonprotein nitrogen group, neutral fats, phospho-
Plate 1
Smear of bone morrow as obtained by sternal puncture. (From Tice:
Practice of Medicine. W. F. Prior Co., Hagerstown, Md.)
Key: Mt, myeloblast; Pro, promyelocyte, Me, myelocyte (differentiated), J, juvenile or
metamyelocyte; E, ecsinophit, 1, lymphocyte; P, plarme cell; N, normoblan.
Hematology nN
lipids, glucose, cholesterol, oxygen, and carbon dioxide. Plasma also
contains such substances as antibodies, complement, hormones, and
enzymes. In adults the plasma constitutes from 53 to 58 per cent of
the blood volume.
The cellular part of the blood consists of leukocytes, erythrocytes,
and platelets. As determined by centrifugation these cells constitute
45 to 47 per cent of the total blood volume in mates and 42 per cent
in females, This percentage of packed blood cells is Known as the
hematocrit.
Blood Volume:
Keith, Rountree and Geraghty!® introduced a simple dye
dilution method for the estimation of plasma volume. They first
used brilliant vital red, Evans’, but this had the disadvantages of
incomplete mixing of the dye and blood, elimination of some of the
dye during the mixing period, and difficult matching in the pres-
ence of hemolysis. These difficulties were largely overcome by the
substitution of a nontoxic slowly diffusing blue dye (Evans’ blue
dye or T-1824), The technic of using Evans’ blue has been modi-
fied and improved by Gregersen, ef al.,1° Price and Longmire,?¢
and Morris.2 Whereas this method is useful for comparing values
obtained in the same patient at different times, it cannot be con-
sidered a precise method for measuring plasma volume, according
to Courtice and Gunton.??
The use of radioactive elements has added other means for
determining blood volume. Radioactive phosphorus (P?2) with a
“half-life” of 14.8 days can be introduced into red cells in vitro and
then they can be put back into the circulation where the extent of
their dilution can be measured.2* Serum albumin has been tagged
with radioactive iodine?4 °5 (1251) with a “half-life” of eight days,
and by this method the plasma volume rather than the erythrocyte
volume has been determined. Another tracer substance, radioactive
chromium (Cr®1) with a “half-life” of 26.5 days will tag both plasma
protein and erythrocytes according to Gray and Sterling.?6 Blood
volume determination has been further refined by the use of radioac-
tive iodine attached to normal serum albumin. A known amount of
12 - Body Fluids, Exereta, and Functional Tests
radioactive iodine with albumin is given intravenously. After
sufficient mixing time, a sample of blood is withdrawn and placed in
a scintiHation detector such as the Volemetron, The blood volume
in liters can be computed in 15 to 20 minutes by this method.
Normal Values: In normal human adults the total blood volume
ranges from 60 to 88 cc. per kilogram of body weight, depending
on the method used for its determination. It represents from 6 to 8
per cent of the total body weight, Table 2 shows the normal values
of plasma volume and total blood volume for man by various
methods.
Taste 2. Normar Vatues or Torar Broop Votume 4Np
Pruasma VOLUME In Man
Total Blood Plasma
Autharity Afethod Volume vince. | Volume ince
per kg body wt. per kg
. body wet.
Rountree, Brown, and Roth” | Vitel red 88 51
Sunderman and Austin®......f Vital red = 43 (scrum)
Gibson and Evans®. . . . | Evans’ blue 7S (males) 43 (males)
66 (females) { 42 (females)
Hurtado, Merino, and Delgado") Evans’ blue 85 (males) 46 (mates)
Hopper, Taber, and Winkler! | Evans’ blue 80 45
Courtice and Gunton’, .... Evans’ blue _ aL
Hopper, Taber, and Winkler™ | Carbon monovade ; 80 45
Salvesen™.. ca ee Carbon monoxide | 60 =
Chang and Harrop® .. Carbon monoxide ) 67 (males) ~
Berlin et alts... . 2. ++ | Radioactive
phosphorus 69 (males) 38.7 (males)
44 (females) } 27 (females)
The Application of Blood Volume Determination: Blood
volume determinations are of most value in surgery, ¢.g., surgical
or traumatic hemorrhage, surgical or traumatic shock. They are
also of value in gastrointestinal hemorrhage, chronic infection or
chronic anemia. From the preoperative and postoperative blood
volumes and the amount of blood and plasma transfused, the
amount of blood, red cells, and plasma lost can be calculated.
Hematology .
oe
Berlin et al.34 have computed the total blood loss, red cell loss, at
plasma loss in a series of surgical cases representing both thoracic
and abdominal surgery as shown in Table 3. As a result of blood
volume determinations, transfusions, fluids and plasma expanders
can be used quantitatively with some degree of precision as to the
needs of the individual patient. ~
Taste 3, Bioop, Rep Cert, AND PLasmMA Loss IN
THoracia AND ABDOMINAL SURGERY
No. of Blood Red Celi | Plasma
Operation Cases Loss Loss Loss
ce. ee. ec.
Thoracoplasty.. . 12 910 467 468
Pneumonectomy. . 4 2840 1267 1603
Lobectomy .. .. 8 2680 1156 1628
Gall bladder procedure... 6 690 270 420
Large bowel procedure..... 4 1630 460 1190
Gastric resection..... : ir 1870 440 1490
Specific Gravity:
The specific gravity of blood is the ratio of the weight of blood
to the weight of the same volume of water at a temperature of 4°C,
The normal specific gravity of blood is reported as 1.048 to 1.066
with averages given as 1.052 to 1.063. Men have a slightly higher
specific gravity (1.057) than women (1.053). The specific gravity
of the blood depends upon the number of red cells and their hemo-
globin content, also upon the amount of protein in the plasma. The
specific gravity of serum is 1.026 to 1.031.
Phillips ef al.88 developed a simple method of determining the
specific gravity of whole blood, plasma, or serum by the use of
copper sulfate of graded specific gravities. A drop of blood or
plasma entering the copper su/fate solution becomes surrounded by
a layer of copper proteinate and remains as a discrete drop for
15 t0 20 seconds. During this time it rises or falls and thus reveals
its specific gravity relative to that of the solution. If the drop is
14 Body Fluids, Excrelo, and Functional Tests
lighter than the test solution, it will rise a few millimeters and will
subsequently sink to the bottom. If the drop is of the same specific
gravity as the test solution it will become stationary and then fall,
TE the drop is heavier, it will continue to fall. In addition to the
specific gravity of the blood, the plasma protein level, volume of
picked red cells, and hemoglobin concentration can be determined.
Functions af Blood:
The blood has numerous functions, which under normal condi-
tions maintain proper body metabolism. These functions are listed
by Best and Taylor36 as follows:
Respiratory: The transportation of oxygen from the air in the
lungs to the tissues, and of carbon dioxide from the tissues to the
lungs.
Nturitive: The conveyance of food materials, glucose, amino
acids, and fats from the alimentary canal to the tissues.
Excretory: The removal of waste products of metabolism, for
example, urea, uric acid, creatinine, and so on.
Maintenance of Water Content of Tissues: Though the blood
itself is contained within vascular channels, a constant interchange
of fluid through the vessel walls takes place. This fluid, which has
left the blood vessels and has come into direct contact with the
tissue cells, is known as the “lymph,” or tissue juice. It closely re-
sembles the blood fiuid in chemical composition, The final stage in
the transportation of oxygen and food materials to the tissnes, and
the first stage in the journey of carbon dioxide and waste products
from the tissues, arc made through the medium of the transuded
fluid. It is the very high solvent and ionizing powers of water, of
which the blood fluid and lymph are chiefly constituted, which make
these such admirable media for the carrying our of the complex
chemical processes of the body.
Body-Temperature Regulation: The body owes its ability to
regulate its temperature largely to the water of the blood and the
tissue fluids, Water possesses three qualities that fit it preeminently
to Fulfill this purpose:
Fe oe we
ARROW.
_— CRS Merge ERAN Ree ORL Fae maT Da we et be
'E-CELIS OF THE BONEM
oe AORMOBLAST C”
A nosmaitacr wf
t
Z v,
of Yor
Se
4
th
RETICULOCYTE nonce
Plate 2
Celis of the Bone Marrow Red Cells The hushocyte or hemohisticblast is probably the
forerunner of all the blood cells erythreblastic, myeloblaste, lymphoblastic, and monocytic. The
Pp 2 red cell—erythrogone—is seen with red cell hyperplasia. Normoblast “A“ i: usually called
mocroblast, “B," erythreblast, “C,” nermoblast. The approximate proporhons of these celts in the
normal morrow are these erythrogones, 0, normoblast “A,” © to 3 per cent; “B," 10 10 20 per cent,
“C" 70 t9 90 per cent. (Dameshek.)
THE CELLS OF THE BONE-MARROW
MYELO
woke 4 ;
MATURE FOLYMORFHONUCLEAR IE” MNETAMIYELOCYTE femop
Plote 3
Cells of the Bone Morrow: White Cells The opprozimate proportions of theve cells tn
the normal marrow are there myeloblasts, 1 te 5 per cent, promyelocytes, 2 fo 10 per cent,
myototytes, 40 to 80 per cont, metamyelocytes, 20 to 30 per cent, meture palymorphonuclears,
Sto 10 percent. Ar the cells moture, the cytoplasm becomes more pink ond the nucleus more ond
more shrunken Knowledge of these cells becomes Important in the atudy of acute Enfections with
“ght to the left" (Dameshek )
. ERYTHROGENESIS
IRON DEFICIENCY
HYPOCHROMIC, ATEN
TIORMAL HYPERPLASIA
am \ ERYTHROGONE
tegen
normostasT °A”
Wi “LIVER periciency
PERNICIOUS ANEMIA
SPRUE
VITAMINE’B’ DEFiclEncy
NORMOBLAST “B*
(@) \
NORMOBLAST C a
Ss None
’ MEGALOBLAST ‘C”
, g
wt OK
NORMOCYTE menocyte
aout MACROCYTE
Plate 4
Erythrogenesis. Two types of red blood cell formation may be seen in the marrow:
(Q) Normoblastice—seen normally and in normal hyperplasia, (2) megaloblastic, os in peratcious
anemia and ossociated states (Cf. Dameshek and Valentine. Arch. Path. 23:359, 1937). The most
primitive cell in either cose Is the erythrogone (promegaloblest). Nermoblast “A,” Macreblast, Nor
moblast "8," Erythroblast, Normoblast “C,"" Nosmoblast,
: 0
CS 7
Plate 5
Abnormal erythrocytes. (From Davidsohn, |., ond Wells, B, B.: Tadd-
Sanford’s Clinical Diagnosis by Laboratory Methods. Ed. 13. W. B.
Saunders Co., 1962.)
All drawn from actvol specimens end off stained with Wright's ston except where noted
1,000) (1 mm = micron), 1 Varlations in atze, shape and hemaglobia eantent, fram cases
of pernicioun anemia and chlorosis. 2. Polychromatephilia and besophske cranvter degeneration
in cares of lead paxtoning and pernicious anemia 3. Normablosts, reticulated erythrocytes and
one qicrablast, the top row represents stoges in the development of the normablast The two
Feticulated erythtecytes org stained wih brlliont cresyt blus, 4 Maegolsblosts in pernicious
anemia. Two show polychromatophila and fairly typical nuclei, two have condensed nuclei ond
one of these hox boscphulic oyioplasmic granules 5, Nuclear porticles er Howell Jolly bodies,
One cell olso shows batophite granular degeneration. 4. Mitohe Figures, bvo from myelogenous
leukemia and one with polychtometophalie cyloptoem, from von Jelath’s onemia Tha tout wer sioined
with Leishman's stole. 7. Cabor's ring bodies in von Jaksch’s enema Two cells olso eon
suctene particles and one shows bosophilie granuior degenerstion {Leuhhmar’s slain).
Hematology 15
HIGH srEciric HEAT: The specific heat of water is considerably
higher than that of any other liquid or solid. Because of this great
heat-storage power of water, sudden changes of bady temperature
are avoided. Even a cold-blooded animal, such as the frog, has—
because of this purely physical quality—some ability to maintain
a relatively constant body temperature against transient fluctua:
tions in environmental temperature. A man of average weight
develops 3000 Calories in 24 hours. This amount of heat is
capable of raising the temperature of his tissues (which are mostly
water) only about 89.60°F. (32°C). Heat elimination (radiation
and so on) is able to keep pace with heat production, and the body
temperature varies but slightly within normal limits. It has been
pointed out by L. J. Henderson, however, that if the tissues had the
low heat-storage capacity (specific heat) of most substances, an
amount of heat equal to 3000 Calories wold raise the temperature
of the tissues and fluids of the body by from 212° to 302° F. (100°
to 180° G).
HIGH ConDucTIVITY: The thermal! conductivity of water is greater
than that of any other ordinary liquid. The advantage of this in the
dissipation of heat from deeply situated regions of the body is
obvious.
HIGH LATENT HEAT OF EVAPORATION: More heat is required for
the vaporization of water than for that of an equivalent amount
of any other liquid. About 0.6 Calorie (large) is required for the
vaporization ot 1 cc. of water. This figure is 50 per cent higher
than that of water's closest competitor. Fluid is constantly lost from
the body through evaporation from the lungs and skin. A large
amount of heat is lost in the process.
These physical properties of water, which make it ideal as a
heat-regulating medium, are enhanced by other purely physiologi-
cal factors. The mobility of the blood and the readiness with which
it may be quickly redistributed in the body, combined with the
unique physical properties of the fluid itself, make it highly efficient
as a regulator of body temperature. The blood may, in a moment,
be brought from deeper to superficial regions and spread out in
16 Body Fluids, Exereta, ond Functional Tests
fine vessels over a broad axea just beneath the skin. In this way, it
greatly increases the radiation of heat. At another instant, in order
that heat may be conserved, the Muid is drained from the surface
areas and collected in the deeper parts of the body, in the internal
organs, muscles, and so on.
Protective and Regulatory: The blood and lymph contain cer-
tain chemical substances of a complex nature, antitoxins, lysins, and
other antibodies, which are the basis of the body's defense against
injurious agents of various hinds. The circulating fluids also bring
the endocrine principles {rom the ductiess glands into direct contact
with the cells of the tissues.
Taste 4: Sumstary or Normat Boop VaLurs
ADULTS
Erythrocytes : Temales 4,600,000 to 4,800,000 per cu. mm
Males. . 5,400,000 to 5,800,000 per cu, mm,
Retiewlorytes 05 to 15 per cent of erythrocytes
Hemoglabin ... . Females. 14 (£2) Gm per 100 ec. of blood
Mates 16 (£2) Gm. per 100 ce. of blood
Hematocrit (volume of packed
erythrocytes). 1, Females 42 (4:5) ce per 100 ce. of blood
Males .... . 47 (27) ce per 100 ce. of blood
Mean corpuscular volume Females, .. . : 86 1u. merons
Males 82 cu. microns
Color index. vee 1 (in absolute terms)
Mean corpuscular hemoglobin 29 (2) micromicrograms
Mean corpuscular hemoglobin
concentration . S4 (2) Gin, per 100 ce,
Saturation index . 09 to 12 (in absolute terms)
Sedimentation rate. . Males Females
(mm fall in i bour) . .. Otv8 mm. 0 to 10 mm, (Cutler)
0 fo 15 mm. Oto 2mm (Westergren}
Oto 651mm. Oto 15mm (\Wentrobe)
Fragilty of erythrocytes... . Minirstns resistance (slight
hemolysis) 0,48 to 0.4 per cent sodtum chlonde
‘Maximum resistance (coraplete.
hemolysis) 0 36 to 0 3 per eent sodtum chloride
Leukocytes. ..-. -. - —- 6000 to 16,000 per eu, mm.
Hematology 7
Tasix 4; Suamrary oF Normat Boop Vatues (Continued)
{per cent)
Percentages of leukocytes. Nonsegmented neutrophils
(metamyelocytes)..........6.0068 2tod
Segmented neutrophils (mature
neutrophils) 54 to 60
Eosinophils 1to3
Basophils 0.25 to 0.5
Lymphocytes... -. 25t033
Monocytes (arge mononuclear ‘cells) 3to7
Platelets .. . . . 250,000 per cu. mm. Figures vary with different
technies; for example, Dameshek’s method’?
gives 500,000 to 900,000 per cu. mm.
Bleeding time ~ . 1 to 3 minutes (Duke)
Coagulation time. Capillary tube .. . . 1to7 minutes
Howell method. 10 to 30 minutes
Lee and White method 5 ta 8 minutes
Clot retraction time .. Begins in | hour; marked in 18 hours
Prothrombin time... - -10 to 20 seconds (Quick**); 12.5 per cent plasma,
37 to 42 seconds
Prothrombin level. . 300 units per ce. of plasma
Prothrombin index . . 70 to 100 per cent
Capillary fragility... 2. . Suction cup .. ~-20 to —35 em. of mercury
“LE.” Capus erythematosts
cells... 0 0.0... . «Normally negative
Tagce 5: Summary oF NorMaL BLoop VaLues
INFANTS AND CHILDREN
Erythroblasts . ... . Atbrth. . 1 to § per 100 WBC
After seventh day , 0 per 100 WBC
Erythrocytes .... 0... .. . Under 2weeks
of age.. .. 5,100,000 to 5,660,000 per eu. mm
One to 15
years.... 4,600,000 to 4,700,000 per cu. mm’
Reticulocytes | At birth. 2 to G per cent
Second week and Tater. 0.5 to 1.5 per cent
Hemoglobin ........ . . At birth: capillary . 19.85 Gm. per 100 cc,
venous.... 17.0 Gm. per 100 ce.
Children: males. . 16 (+2) Gm. per 100 ec.
females.... 14 (42) Gm, per 100 cc.
Hematocrit (volume of packed
erythrocytes).......-.-2.05 Infants. .49 to 54 (4:10) ce. per 100 ec. of blood.
Children, .35 to 39 ce. per 100 ec. of blood
18 Body Fluids, Excreta, and Functional Tests
Tate 5: Suntary or Noamar Broo Vauues (Continued)
Mean corpuscular volume.... Infants. . Sf eu. microns
Children. 2. 2... . . 72 eu microns
‘Mean corpuscular hemoglobin .. Chitdren.,., 26 to 28 micromucrograms
Mean corpuscular hemoglobin
concentration . wee Children... 32 to 34 Gm _ per 100 ec
Sedimentation rate Landau’ .
method}. oe Under 2 years. . + 1to6mm.
(rom. fal} in 4. hour) Over 2 years .. . te 9mm.
Fragility of erythyvooytes . .. Minimum resistance. . O48 fo 0,42 per cent
of sodium chloride
Maximum resistance 0.39 to 03 per cent
of sodium chloride
Leukocytes. «. » Infants .. 10,008 to 22,500 per cu, mm
Children. , 8300 to 10,800 per cu. mm
Percentages of leukocytes Nonsepmented neutrophils per cent
(metamyelocytes) . stos
Segmented neutrophils (mature
neutrophils}. . 16 to 60
Eosinopluls 1to3
Basophils. : 025 00.5
Lymphgeytes. . ns . 42 tods
Monocytes (Jarge mononuclear cells), 3to 5
Platelets. At birth 140,000 to 290,000 per cy mm.
Atl month. 200,000 to 370,000 per cl. mm
Ata months 200, 000 to 480,000 per cu. min
Bleeding time Atbirth. . 2minates
Second week 2 to 3 minutes
Coagulation time : _At birth 2 ta 3 minutes (occasionally up
fo 12 rainutes}
Second week 2 to § minutes
Prothrombin time At birth . 43 seconds (Kato & Poncher')
Second week —-25 seconds
Children, 13-20 seconds
ERYTHROCYTES
Life Cycle of Erythrocytes:
The normal erythrocyte is a non-nucleated round cell which
originates in the bone marrow from a nucleated cell called an
“erythroblast.” Although the nuclei are normally not present in
the circulating blood, a few cells retain a blue reticulum when
Hematology 7
stained with a vital stain such as brilliant cresyl blue. These are
called “reticulocytes” and are found in normal blood in values
varying from 0.5 to 1.5 per cent.
Opinions differ on the length of the life span of erythrocytes.
Dekkers*? has estimated it to be from 50 to 75 days, while Ashby#?
believes they function for from 80 to 100 days. Vischer#3 has
Fig. 1: Red corpuscles of normal blood. Wright's stain (photograph,
x 750). (From Davidsohn, |, and Wells, B. B.: Todd-Sanford‘s Clinical
Diagnosis by Laboratory Methods, Ed. 13. W. B. Saunders Co., 1962.)
calculated that transfused erythrocytes function only 12 to 13 days.
Shemin and Rittenberg!# concluded that the average life span of
human erythrocytes was about 127 days by following the isotope
concentration of heme in red cells after feeding glycine labelled
with N15. Bale e¢ al.45 calculated an average life of 115 days for the
red cell protein of the dog by using C1 labelled di-tysine. Finch and
his colleagues*6 followed transfused red cells tagged with radioactive
iron in subjects in whom the reunhzation of the iron was blocked.
Thus the life span of a red cell population of a single age could be
followed. It was found that the red cell turnover in both man and
20 Body Fluids, Excreta, and Functional Tests
in the dog was approximately 1 per cent a day. It would seem
therefore that the length of life of human erythrocytes in the normal
individua) is about 120 days.
Apparently the nonfunctioning cells are removed by the phago-
cytic cells of the reticuloendothelial system after they have under-
gone fragmentation. The phagocytic cells of the liver, spleen,
bone marrow, and subcutaneous tissues carry on this process. The
hemoglobin of the erythrocytes is probably broken up into globin
and an iron-containing pigment, hemochromogen in its reduced
form, and hematin when oxidized. This pigment is freed of iron and
as changed to bilirubin, which is a normal constituent of the plasma.
Bilirubin gives plasma its yellowish tinge and is normally present
at a level of 0.7 mg. per 100 cc. (quantitative van den
Bergh test). The fate of globin is not known at present, but it is
assumed chat it is converted into amino acids and used again in
manufacturing hemoglobin.
Normal Erythrocytes;
The normal erythrocyte is 2 round non-nucleated cell with a
thinner central portion. The normal mean diameter of red cells is
reported as from 7.2 to 7.9 microns.47 The normal mean thickness
varies, according to diflerent reports, from 1,84 to 2.14 micrens.48
Certain physiological changes take place in the erythrocyte
count and hemoglobin level, There is apparently a diurnal “varia-
tion equivalent to 11 per cent of the mean hemoglobin for the
day. Such variation must be correlated with the activity of the per-
son, since there is little or no variation in xed cell count and hemo-
globin during complete rest.49 Muscular activity is usually asso-
ciated with an increase in red-blood cell count and hemoglobin
value. The ingestion of a large amount of water may temporarily
lower the red-blood cell count, while dehydration will increase this
value because of hemo-concentration, Excitement and fear cause
an increase in the number of red blood cells, which is higher than
would be expected from technical variations, Adult males have
Hematology 21
higher counts than adult females. Low barometric pressure, which
is experienced at high altitudes, causes anoxemia and an associated
increase in both red blood cells and hemoglobin.
Abnormal Erythrocytes (Plate 2):
A differential count should not be considered complete unless a
report is made concerning the presence of any abnormal erythro-
cytes. Certain findings will help the clinician in making a diagnosis.
Certain erythrocytes stain a light blue, polychromatophilia,
which is seen in unripe macrocytes or in degenerated nucleated red
cells, Variation in size, anisocytosis, is seen in both primary and
secondary anemia. Variation in shape, poikilocytosis, is scen in
more advanced anemias.
A deficiency of hemoglobin is called “hypochromia.” It may be
so marked that only a rim is left. These forms occur in hypochromic
anemia, sickle-cell anemia, and erythroblastic anemia. Red blood
cells may also contain an excess of hemoglobin, hyperchromia.
These cells are seen characteristically in macrocytic anemia, such
as pernicious anemia.
Basophilic stippling is seen in certain cells. The action of toxins
on regenerating red blood cells results in the formation of residual
chromatin dots, which take the basic stain. These forms are present
in lead poisoning, malaria, and in marked primary and secondary
anemias.
Nuclear remnants are sometimes seen. They may appear as blue
dots; chromatin particles; spherical, eccentrically located, datk-
staining granules; Howell’s bodies; and blue-staining, threadlike,
twisted rings, Cabot's ring bodics.
Confusing bodies are seen in degenerating red cells: (1) A round
body, Maragliano body, has the appearance of a vacuole, and is
in che center of the cells; (2) bacillary degeneration, rodlike hyaline
areas with a vibratory motion; and (3) Ehrlich’s hemoglobinemic
degeneration, dark bodies in the centers of red blood cells.
A peculiar cell, called a “target” corpuscle, may be found in
hypochromic anemia, sickle-cell anemia, Cooley’s anemia, and in
22 Body Fluids, Excreta, and Functional Tests
jaundice without anemia, This cell is characterized by a central
round region of pigmented material, surrounded by a clear zone
without pigment, and this in turn is surrounded by the outer border
of the cell.
Erythrocytes that take the shape of a sickle when deprived of
oxygen are found in sickle-cell anemia, which is peculiar to the
Negro race.
Decrease in Number of Erythrocytes:
A reduction below normal of the number of erythrocytes per
cu, mm., the amount of hemoglobin and the volume ot packed red
cells is called anemia. The oxygen carrying capacity of the blood
is reduced with the reduction in the number of erythrocytes. In
anemia from sudden blood loss or from chronic slow blood loss
there is a tendency ta make up the blood volume by increasing the
fluid portion of the bload.
Anemia has the time-honored division inte primary and second
ary types, but such division is not considered satisfactory today.
Primary anemia referred to anemia resulting from fundamental dis-
ease of the hematopoietic organ itself and also to anemia of un
known etiology. Secondary anemia included those anemias which
are the indirect result of disease of other organs and also those
anemias of known etiology.
Anemia can occur as a result of (1) acute or chronic blood loss;
(2) excessive blood destruction; (3) decreased blood production
from deficiency of substances concerned in erythropoiesis or some
fault in the construction of red cells; and (4) congenital “dystro
phies” of the erythron. {The “erythron” includes the circufating
red cells arid the bone marrow from which they originate.)
Increase in Number of Erythrocytes (Polycythemia):
Polycythemia is 2 condition in which the red cell mass is mcreased
above norma}. There is also a concomitant increase in hemoglobin
(more than 17.5 Gm. per 100 cc.), in hematocrit (more than 52
per cent), and red cell count (more than 6,000,000 per ct. mm.) ,
Hematology 23
The polycythemias can be conveniently divided into absolute
and relative types as follows:
Absolute
1. Primary Polycythemia vera
2. Secondary
a. Compensatory polycythemia High altitude
Alveolar hypoventilation
Chrome pulmonary insufficiency
Congenital heart disease
Methemoglobinemia
Carboxy hemoglobinemia
b, Chemical agents and drugs Coal tar derivatives
Cobalt
Manganese
Mercury
Iron
Arsenic
Bismuth sulbnitrate
Digitalis
Caffeine
Nicaune
Testosterone .
c, Neoplasms Neoplasms of kidneys, liser and uterus
Subtentorial neoplasms
d. Miscellaneous
Relative (pseudopolycythemia) Hemoconcentration secondary to
dehydration.
See page 472 for discussion
Reticulocytes:
Reticulocytes are seen in the blood smear only when the blood
is stained with a vital stain, such as briffiant cresyl blue. They are
characterized by a faint blue reticulum in erythrocytes which are
larger than normal. The reticulum may appear as a pale blue band,
it may be distributed evenly throughout the cell as fragments or it
may be so densely packed that it can be mistaken for a nucleus. As
a rule there is a large amount of reticulum in reticulocytes which
have just emerged from the nucleated stage and very little in those
which are approaching maturity.
Reticulocytes will last 24 hours in oxalated blood at room
temperature, However, if the blood is Lept in a refrigerator, Heath
24 Body Fluids, Excrefa, ond Functional Tests
and Daland5? report that the reticulocytes retain demonstrable
reticulum for six months,
The normal range for reticulocytes is 0.6 to 1.5 per cent in
healthy persons, Friedlander and Wiedemer®! reported that they
Fig. 2: Reticulated erythrocytes (x 1000). (From Davidsehn, 1, and
Wells, B. Ba Todd-Sanford’s Clinical Diagnosis by Laboratory Methods,
Ed. 13. W. 8. Saunders Co, 1962,
are slightly increased in the spring. Newborn infants have from
2 to 6 per cent, but this drops to from 0.5 to 1.5 per cent in two to
five days. an |
An increased reticulocyte count is indicative of increased
erythropoiesis, and is a helpful guide an proving the adequacy of
liver therapy in primary macrocytic anemia. The reticulocyte
response is in inverse ratio to the original erythrocyte count; that
1s, the lower the original erythrocyte count, the higher the reticulo-
cyte response.
Hematology 25
Reticulocytes are also increased in congenital! hemolytic jaun-
dice, sickle-cell anemia, in cases of chronic blood loss of short dura-
tion (from two to four months), and in anemic premature infants.
There is a slight increase in leukemia, myelophthisic anemia, lead
and mercury poisoning, malaria, and in the full-term infant at birth.
There is a decrease below low normal (0.5 per cent) in both
idiopathic and symptomatic aplastic anemia.
Stippled Cells:
Basophilic stippling is not seen in a smear of normal blood. It
does occur in severe anemia, lead and mercury poisoning, leukemia,
and chronic malaria. The granules of stippled cells are stained by
Wright’s stain and are characteristically deep blue. They are not
to be confused with the reddish granules seen in erythrocytes con-
taining Plasmodium vivax.
Heinz Bodies:
Heinz bodies are refractile inclusions varying in size from 1 to
4 microns and are found in red cells under certain conditions.
They may be demonstrated by dark field or phase microscopy and
may be stained by 0.5 per cent methyl violet in 0.85 per cent sodium
chloride. ,
Heinz bodies are found in patients with hemolytic anemia
resulting from exposure to certain drugs or chemicals. Among these
are Pamaquine and primaquine (antimalarial drags) which affect
the red cells of susceptible patients, most of whom are Negroes.
Adults habituated to acetanilid or phenacetin and children suffi-
ciently exposed to fumes of mothballs may develop hemolytic anemia
and positive Hemz bodies.
Hemolytic anemia with many Heniz bodies with no exposure to
drugs has been reported in 14 premature or underweight infants by
Gasser.52 In postsplenectomy cases, small numbers have been
found, according to Dacie.®%
Siderocytes:
Siderocytes are red blood cells which show blue granules after
the Prussian blue stain. These granules are thought to contain
26 Body Fluids, Excreta, and Functional Tests
jonized ferric iron and can be demonstrated in orthochromic
normoblasts and occasionally in reticulocytes. Siderocytes up to 20
per cent or more are found in che blood of hemolytic anemias and
in hematologically normal blood after splenectomy.
Indices Derived from Erythrocyte Values:
Hematocrit: The hematocrit or volume of packed cells in
terms of cubic centimeters per 100 cc. is of value in determining
alteration in size of erythrocytes. The normal values for cell volume
are as follows: infants, 49 to 54 (+10); children from one to 15
years, 35 to $9; adult males, 4? (+: 7); and adult females, 42 (+ 5).
It gives clinical infonnation similar to that given by the red-blood-
cell count and hemoglobin,
Mean Corpuscular Volume: The mean corpuscular volume may
be determined from the volume of packed cells and the erythrocyte
count as follows:
volume of packed blood cells, ce, per 100 ce,
red blood cell count, millions per eu, mm.
The value for infants is approximately 84; children, 72; adult males,
82; and adult females, 86 cu. microns. The values are increased to
more than 100 in macrocytic anemia and are decreased in microcytic
anemia,
Volume Index: The volume index may also be determined by a
slightly different formula:
volume of packed blood cells, ce. per 100 ec. x 23
red blood cell count, millions per cu. mm, x 20.
The volume index is the relative mass of circulating red blood cells
as compared to the normal. The values for children are from 0.68 to
0.82 and for adults from 6.8 to 1. In macrocytic anemias, values
from 1.20 to 1.60 or higher are found.
= number of cubic microns
Sedimentation Rate:
The sedimentation rate or index is the fall of the red cell column
in one hour measured in millimeters. It is a nonspecific test which
is accelerated in a variety of diseases and in pregnancy. ‘The underly-
ing reason for this change in rate of fall is not clearly understood.
Hematology
27
Various protein fractions such as alpha and beta globulin®+ have
been added to plasma with some acceleration of the sedimentation
rate. However, the effect is less marked than that produced by the
addition of fibrinogen.35 This fact, plus the observation that plasma
fibrinogen is usually increased when the sedimentation rate is
accelerated, led to the conclusion that increased sedimentation rate
SEDIMENTATION RATE, MM. IN ONE HOUR
30
70 a
60
50
40
a 5 "10 «15° «20 25 30 35 40 45 50 55
VOLUME OF PACKED RED CELLS, CC. PER 100 Cc, BLOOD
Fig. 3—Chert for correction of sedimentation rate according to volume of packed
red cells. The fogarithmie curve on which this chart is based fs heavily outlined. The
mean pormal volume of packed red cells for men (47 cc} and for women (42 cc.) are
ako heavily outlined and the range of normat sedimentation is represented by solid
and open cofumns for each sex, respectively,
To “correct” sedimentation rate, find on the chart the horizontal line corresponding
to the sedimentation rate for the potient; find also the vertical line corresponding to
the yolume of the packed red cells in the patient's bleed. Select the curve lying
nearest to the point of junction of the horizontal ond the vertical fines and follow
this to the sormal line for the sex of the patient, The horizontal fing corresponding
to this lost potnt of juncture gives the corrected sedimentation rate, Since the rence
hetween the normal sedimentation rates in men end women is largely due to the
difference in volume of packed red cells, all sedimentation rates moy ho corrected to
@ volume of 47 cc. and a single standard of normal (0 to 6 mm.) used. Thir chart
should not be ysed to “correct” polycythemic blood fo a normal level. (Wintrcbe and
landsberg, Am. Jour. Med. Sef)
90
80
70
50
20
10
238 Body Fluids, Excreta, and Functional Tests
is the result of an increased level of fibrinogen.# 57 Since the addi-
tion of pure albumin inhibits the fall of erythrocytes and the
globulins and fibrinogen cause varying increases in rate of fall,
it seems likely that the sedimentation rate depends upon the ratio
of the various protein fractions to each other.
It is customary to correct the sedimentation rate for anemia
because there is an increased rate of fail when there are fewer
erythrocytes. Sickle-cell anemia fs an exception because the peculiar
shape of the red cells prevents the formation of rouleaux. In order
that the clinician may evaluate the findings properly, it is advisable
to Teport the uncorrected and corrected sedimentation rates together
with the hematocrit. The method of correction of sedimentation
rate according to volume of packed red cells (hematocrit) is shown
in Figure 3,
The normal results vary with the method used as indicated in
Table 6, Certain precautions should be taken in carrying out a
sedimentation rate, viz: (1) The test should be done within two
Taste 6; Variations or Normat SrpiMENtTATION Ratrs
Cutler Westergren Wrntrohe
(Mm in One Hour) | (Aten.in One Hour) | (Mim. in One Hour)
Children .. : — Oto 10 3 to 130
Men .. Oto8 Oto 15 O65
(average 37)
Women. Oto 10 Oto 20 0 to 15.0
{average 9.6)
hours of the time of collection of the specimen. (2) The test should
be carried out within a temperature range of 22° C. to 27° C,, since
the rate increases with increase in temperature. Blood which has
been kept in a refrigerator should be allowed to reach this tempera.
ture range befare starting the test. (3) The tube should be kept in
an exact vertical position during the test because any deviation in-
creases the rate of fall.
The sedimentation rate remains within normal range in func.
tional nervous disease, benign tumors such as uncomplicated
Hematology 29
fibroids and cysts, asthma, hay fever, essential hypertension, diabetes
mellitus, cirrhosis of the liver, simple peptic ulcer, hydronephrosis,
uncomplicated cholelithiasis, and nephrolithiasis, early acute appen-
dicitis, head colds, and hypertrophic arthritis.
Changes in the sedimentation rate in various conditions are
shown in Table 7.
TABLE 7: CHANGES IN SEDIMENTATION RATE
Increased Decreased
Physiological. Malaria during paroxysms
Pregnancy after second mouth Erythremis
Menstruation Sickle-cell anemia,
. Certain cases of severe liver disease
Infectious processes.
Acute general and localized infection
Chronic active infections
Tuberculosis
Syphilis
Rheumatic carditis
Blood dyserasias
Leukemias
Anemias
Poisoning:
Lead
Arsenic
Alcohol
Miscellaneous:
Coronary thrombosis
Hemorrhage
Advanced malignancy
Hyperthyroidism
Nephritis and nephrosis
Certain cases of severe liver disease
Hemolysis of Erythrocytes:
Hemolysis is a phenomenon which is sometimes preceded by
agglutination. Red cells have a tendency to agglutinate under cer-
tain conditions, and under other conditions they tend to hemolyze.
30 Body Fluids, Excreta, and Functional Tests
‘The role of these peculiarities of red cells in the development of
disease is not entirely understood, but helpful diagnostic procedures
have been developed in which the agglutination and hemolysis
potentials have been used. Agglutination of red cells will be dis.
enssed in Chapter 5.
Osmotic Fragility Test; The fragility test as originally described
is a measure of resistance of red cells to hemolysis by hypotonic
sodium chloride solutions, When normal venous whole blood is used,
hemolysis just begins at 0.46 to 0.40 per cent sodium chloride; this
is called “minimum resistance.” Hemolysis with such blood is usu-
ally complete in solutions varying from 0,36 to 0 30 per cent sodium
chloride; this is called “maximum resistance.”
Increased Fragility in Hypotonic Sodium Chloride: Increased
fragility is marked in congenital hemolytic jaundice (familial hemo-
lytic jaundice). This test helps to differentiate this disease from
various types of obstructive jaundice. There is some increase in
fragility in aplastic anemia. This may help to differentiate it from
pernicious anemia and hypochromic anemia.
Decreased Fragility in Hypotonic Sodium Chloride: Decreased
fragility is found in erythroblastic anemia, pernicious anemia, sickle-
cell anemia, hypochromic anemia, hemolytic anemias, polycythemia
vera (erythremia), and obstructive jaundice.
In hemolytic jaundice, after splenectomy, the fragility of
erythrocytes may be increased or decreased.
Fragility in Other Reagents: It is sometimes helpful to employ
a modification of the standard fragility test by determining the
resistance of erythrocytes to dilute hydrochloric acid, lysolecithin,
or saponin. Dilute hydrochloric acid reveals increased fragility in
nocturnal hemoglobinuria. The reaction of erythrocytes in tyso-
lecithin is the same as in hypotonic saline except in acquired
hemolytic jaundice. In this disease saline fragility may be increased
while lysolecithin fragility remains normal according to Singer.5%
In pernicious anemia, saponin hemolysis is increased while saline
Fragility is decreased.
Mechanicai Fragility: Mechanical fragility may be determined
by shaking blood in a flask containing glass beads."? Congenital
Hematology 31
hemolytic jaundice and sickle-cell anemia show increased mechan-
ical fragility.
HEMOGLOBIN
Hemoglobin Formation and Destruction:
Hemoglobin gives the red color to the blood. The red blood
cells are, for the most part, made up of water (64 per cent), and the
remainder of hemoglobin. Hemoglobin is composed of globin, which
is a sulfur-bearing portion (96 per cent), and hematin, a ferrous
complex of protoporphyrin (4 per cent). Hemoglobin is formed
in the bone marrow in the maturing red blood cells, but the detailed
steps are not known.
In the lungs, hemoglobin combines readily with oxygen, form-
ing a compound known as “oxyhemoglobin,” which gives arterial
blood its bright-red color, The oxygen is given up readily in the
Ussues, since it is only in Joose combination with hemoglobin.
Hemoglobin then becomes reduced hemoglobin and. carries carbon
dioxide from the tissues to che lungs, which accounts for the dark
color of venous blood.
After erythrocytes have lived their normal span of life, they
undergo fragmentation. Hemoglobin is released and destroyed by
the cells of the reticuloendothelial system of the liver (Kupffer’s
cells), spleen, and bone marrow. The destruction of hemoglobin
consists first of separating globin from hematin. Globin is broken
down into amino acids. Hematin is broken up by separating the
iron, which is stored in the liver and spleen to be used again in
the manufacture of hemoglobin, The remaining iron-free product,
porphyrin, is converted to bilirubin and transported to the liver to
be excreted in the bile. A small amount of bilirubin is excreted in
the urine by the Kidneys.
Normal Hemoglobin:
In the past, the level of hemoglobin has been expressed in per-
centage, but this is unsatisfactory because of the variation in dif-
ferent sexes and at different ages, which would require the establish-
ment of arbitrary normals to insure accuracy, In expressing hemo-
a2 Body Fluids, Excreta, and Functional Tests
globin in percentage, it is assumed that §,000,000 red blood cells
per cubic millimeter of blood contain 100 per cent hemoglobin,
Hemoglobin is preferably expressed in grams per 100 cc. of blood,
using normal values that are corrected for age and sex.
At birth the normal hemoglobin level in capillary blood is 19.85
Gm, and in venous blood is 17.9 Gm. Both cells and hemoglobin
are about 15 per cent less concentrated in venous blood than
in capillary blood at birth. However, this difference gradually dis-
appears ducing the first week. In male children the normal
hemoglobin level is 16 (2) Gm. and in female children 14
(2) Gm. These figures are the same in adults, viz: 16 (+2) Gm.
for males and 14 (+ 2) Gm. for females,
Abnormal Hemoglobin Values:
Hemoglobin is increased (hyperchromernia) in those conditions
in which there is an increase in erythrocytes. These are erythremia,
compensatory polycythemia at high altitudes, and dehydration such
as is associated with burns and diarrhea. Hemoglobin is increased
in macrocytic anemia because each erythrocyte carries more hemo-
globin than normat (hyperchromia), although the erythrocyte count
is lower than normal.
Hemoglobin values are reduced (oligochromemia) in all anemias.
In hypochromic ancmias particularly, the hemoglobin is low, not
only because there is a reduction in total erythrocytes, but also
because the individual cells have a decreased amount of hemoglobin.
Indices Derived from Hemoglobin Values:
Golar Index: In computing the color index, it is assumed that
5,000,000 red blood cells per cubic millimeter of blood have a hemo-
globin value of 100 per cent, The color index is determined by
dividing the percentage of hemoglobin by the first two figures of
the erythrocyte count multiplied by 2, A hemoglobin value of
70 per cent with a red-bland cell count of 4,000,000 would give
a color index of eS ar 0.87, which would suggest hypochromic
anemia. A color index greater than | is indicative of macracytic
anemia.
Hematology 33
Mean Corpuscular Hemoglobin: This index is computed by
dividing the hemoglobin value in grams per 1000 ce., by the erythro-
cyte level, in millions per cubic millimeter, and expressing the
results in micromicrograms, The normal for adults is 29 (=: 2);
for children, from 26 to 28.
Mean Corpuscular Hemoglobin Concentration: This index is
calculated by dividing hemoglobin, in grams per 100 cc., by the
volume of packed cells, in cubic centimeters per 100 cc. of blood,
and multiplying by 100. The results are given in grams per 100
cc. The normal for adults is 34 (+ 2); for children, from 32 to 34.
The mean corpuscular hemoglobin and mean corpuscular hemo-
globin concentration are decreased in hypochromic anemias and
increased in macrocytic anemias.
Saturation Index: The saturation index measures the concentra-
tion of hemoglobin in the average erythrocyte, as if it carried hemo-
globin in solution.
The saturation index is computed as follows:
hemoglobin, per cent (gm per 100 cc. % 6.9)
Saturation index = Volume packed red blood cells (cc. per 100 ce. x 2.3)
The saturation index is decreased in hypochromic and micracytic
anemias, and increased in macrocytic anemias.
Hemoglobinopathies:
See page 434,
LEUKOCYTES
Types of Leukocytes:
Leukocytes of the peripheral blood are divided into two gen-
eral groups, the granulocytes and the nongranulocytes. The cells in
these two categories are:
Granulocytes Nongranulocytes
Polymorphonuclear neutrophils Lymphocytes
Eosinophils Monocytes (large mononuclear
Basophils cells)
34 Body Fluids, Excreta, and Functional Tests
Functions of Leukocytes:
Polymorphonucleay Neubopkils: The chief function of these
cells is chat of phagocytosis particularly of bacteria and tiny par-
ticles. This function is well illustrated in the opsonocytophagic
index for B. abortus. They also destroy antigen and distribute anti-
body, “Their function in the production of antibody is problem-
atical.
Eesinophils: These cells are thought to have an important role
in detoxification, and in the disintegration and removal of protein.
Their function in relation to allergy and hypersensitivity is not
yet clear.
In persons with normal pituitary and adrenals, injection of
25 mg. of adrenacorticowropic hormone (ACTH) or 0.3 ce. of
epinephrine will cause an eosinopenia.®® 6! The mechanism which
brings about this fall in circulating eosinophils is not as yet com-
pletely understood. It is known that ACTH stimulates the adrenal
cortex which releases steroid hormones in lage quarttities, Of
these steroids, those with an oxygen atom at I} and 17 carbon
positions (“11-17 oxysteroids”) produce a decrease in circulating
eosinophils by a mechanism as yet unknown.®?
~~ Basophils: Although these cells may be funerionless, there is
some evidence that in inflammation they bring an anticoagulant
(heparin) to prevent the clotting of blood in the inflamed tis-
stig, 61, 62
Lymphocytes: The function of these cells is not completely
understood. They may help to destroy the toxic products of protein
metabolism.¢2- 03. ¢4 They are increased during convalescence from
infections, and, therefore, must have some function in connection
with the process of healing. They have been shown experimentally
to participate in resistance to tuberculosis.
Monocytes: These cells phagocytize some bacteria, pavticulste
matter, and protozoa. In an inflammatory process the neutrophils
predominate for about three days, then they break up and the
monocytes remain to phagocytize fragments of cells, ete. Because
monocytes contain lipases they are able to digest bacteria with a
lipoid capsule such as Mycobacteritan tuberculosis and Mycobac-
tertum leprae.
Hematology 35
Normal Total Leukocyte Values:
The total! leukocyte count varies normally with age, exercise,
relationship to a meal, relationship to hot bath, high altitudes, and
dehydration. There may also be physiological changes in the leuko-
cyte count from day to day. Normal values for various age groups
are as follows:
Number per cu. num.
Infants .. . . 10,000 to 22,500
Children : 8,300 to 10,800
Adults . 6,000 to 10,000
Leukocytosis:
Leukocytosis is the term applied to an increase in the total
leukocyte count above the upper limit of normal. Leukocytasis is
the result of an absolute increase in number of one of the white
cells; thus an increase in neutrophils (neutrophilia) in acute appen.
dicitis or of eosinophils (eosinophilia) in trichinosis will result in an
increase in the total white count.
It is important ¢o do a differential count in addition to a total
white count in order to detect an increase in number of one of the
white cells, ‘his sometimes gives a clue to the cause of the under:
lying condition as indicated in the following pages.
Origin and Significance of Granulocytes:
Polymorphonuclear Neutrophils: The youngest recognized forms
of this series are the myeloblasts. Normally, these cells occur only
in the bone marrow where they go through certain stages to reach
maturity. In the myeloblast stage differentiation from lymphoblasts
and monoblasts is difficult, The myeloblast next develops into the
tmyelocyte, which is characterized by the presence of tiny, pale, red
staining granules in the cytoplasm. Myeloblasts and myelocytes are
Not in the peripheral blood except in conditions that stimulate
great activity in the bone marrow, such as severe infections, myelog-
cnous leukemia, and erythroblastosis foetalis.
Nonsegmented Neutrophils (Band Forms): Normal values are
as follows: adults from 2 to 5 per cent; children from three to ten
years old, from 3 to 8 per cent. The myelocyte becomes a meta-
36 Body Fluids, Exereta, and Functional! Tests
myelocyte by the indentation of the nucleus and later assumes the
shape of a horseshoe. The fine pale-red granules remain in the
cytoplasm. Metamyelocytes may be divided into young forms (with
nucleoli and dark staining nuclei) and adult forms (without
nucleoli). Metamyelacytes are the youngest forms that are found
normally in the peripheral blood. They are also known as “band
forms” and “nonsegmented" or “non-filamented” neutrophils. These
forms are increased in acute infectious processes with or without an
incease in the total leukocyte count. An increase in metamyelocytes
constitutes a “shift 10 the left’ as described by Schilling.
Segmented Polymorphonuclear Neutrophils: Normal values are
as follows: adults from 54 to 62 per cent; children from three to
ten years old, fram 16 to 60 per cent. The nucleus of the metamyel-
ocyte becomes pinched off into from two to six or even ten lobes
connected by threads of chromatin, Normally, the granutes remain
pale red, but in severe infections they may take the basophilic stain
and increase in size. These are known as toxic granules and are
thought to be due to the effect of toxins in the cells.
Taste 8; NormMat. VALUES OF LEUKOCYTES IN
PERIPHERAL Boop
Children. (8-10 years) Adults
Absolute Count Absolute Count
Per | Aver- Range Per | Aver- Range
cent age cent age
Granulocytes
Nonseemented 1
trophils (band
forms) ¥ ‘ 280 | 150-300 25 30g | 150-100
Segmented or mature
reutropbils 16-60 | 3250 | 3000-8000 | 54-62 | 4000 | 3000-5500
Eosinophils... 13 300 50-700 1-3 200 50-250
Basophuls.. . 00.75, 35 0-50 0-0.75 25 15-50
te
aioli “ 49-48 | 4000 | 3250-5000 | 25-33 | 2100 | 1500-3000
Monocytes. . 3-5 350 | 250-700 BT 375} 285-500
RS,
Hematology 37
When an increase in white cells (leukocytosis) is due to an
increase in neutrophils, it is called neutrophilia. In this instance
leukocytosis and neutrophilia are synonymous. Usually the increase
in neutrophils is “absolute”; that is, both the total number of
neutrophils per cu. mm. and the percentage are increased. Neutro-
penia is a reduction below normal of the total number of neutro-
phils.
An increase in neutrophils is found in the following;
1. Infectious processes, systemic: Septicemia, pyemia, - pneumonia,
meningitis, gonorrhea, diphtheria, tularemia, actinomycosis, Weil's dis-
ease, anterior poliomyelitis, rabies, typhus, herpes zoster, coccidioidomyco-
sis, acute rheumatic fever, smallpox, chickenpox, scarlet fever, erysipelas,
valvular heart disease, peritonitis, anthrax, plague, cholera, and tetanus,
2. Infectious processes, localized: Pyogenic abscess, carbuncle, furun-
culosis, tonsillitis, mastoiditis, otitis media, sinusitis, ulcer, empyema,
cholecystitis, pyelitis, pyelonephritis, salpingitis, appendicitis,
8. Metabolic disorders: Acidosis of diabetes mellitus, uremia, gout,
and eclampsia.
4, Drugs and poisons: Digitalis, epinephrine, foreign proteins,
venoms, mercury, lead, carbon monoxide, potassium chlorate, camphor,
coal tar products, pyridine, pyrogallol, benzol compounds, turpentine.
5. Acute hemorzhage: Neutrophilia occurs particularly when the
hemorrhage is into a body cavity, e.g., ruptured tubal pregnancy.
6. Diseases of the hemopoietic system: Myelogenous leukemia, ery-
thremia, erythroblastosis foetalis, incompatible transfusions, sudden
hemolysis.
7, Miscellancous conditions: Coronary occlusien, rapidly growing
carcinoma, for 12 to 36 hours after a major operation, burns.
8. Physiological conditions: Strenuous exercise, pregnancy, labor,
puerperium, during digestion, after a hot bath, fear, pain, dehydration,
extreme sunlight and high altitude.
Lupus Erythematosus Cells (“L.E.” Cells): These cells are
usually neutrophils containing one or more masses of purplish-
staining material which fills the cell and compresses the nucleus,
These cells are thought to form as follows: When injured leukocytes
come in contact with an abnormal globulin in the serum, their
nuclei absorb protein, lose their normal chromatin structure and
become homogencous masses that seem to be composed largely of
38 Body Fluids, Excreta, and Functional Tests
desovyribanucleaprotcin, These masses became fiee by either
extrusion or disintegration of the surrounding cytoplasm. They are
then phagocytized by healthy neutrophils, forming “L.E." cells.
These cells are found in stained bone marrow smears, and by
appropriate incubation and concentration technic they may be
found in the peripheral blood. “L.E.” cells are usually indicative of
lupus erythematosus, but similar cells may be tound in rheumatoid
arthritis and in toxic reactions to certain drugs.
Eosinophils: Normal values of eosinophils in both adults and
children are from 1 to 3 per cent. Eosinophils originate from
myeloblasts; when they develop into myelocytes, large acid staining
granules form in the cytoplasm thus differentiating them from
neutrophilic myelocytes. The adult cells rarely have more than two
lobes, but they retain the characteristic coarse acid-staining granules,
Eosinophils are increased in the following conditions:
1. Blond diseases: Easinaphilic leukemia, myelogenous leukemia,
polycythemia vera, and slightly in pernicious anemia.
2. Parasitic discases: Trichinosis, hydatid cyst, especially after rup-
ture, schistosomiasis, infestation with Clonorchis sinensis, infestation with
some intestinal parasites particularly in strongyloidiasis and ancylos
tomiasis, infestation with Zasciola hefatica and in massive infestauon
with Taena solium and amebiasis.
3. Skin diseases: Psoriasis, pemphigus, dermatitis herpetiformis, ery-
thema multiforme, mycosis fungoides. and cutancous allergies such as
urticaria and angioneurotic edema. .
4, Neoplasms: Some cases of malignant granuloma (Hodgkin's dis
ease), certain ovarian and bone neoplasms, neoplasms impinging upon
se1ous surfaces, and neoplasms showing extensive nectosis.
5. Allergic diseases of the respirator tract: Bronchial asthma, hay
fever, and pollinosis.
6 Poisons: Phosphorus, copper sulfate, camphor, and pilocarpme
7. Disease of unknown or doubtful etiology: Loefller’s syndrome
some cases Of periarteritis nodosa, chorea, scarlet fever, tropical eosino
philia, and familial eosinophilia. ;
8. Specific infections: Brucellosis, tuberculosis, coccidioidomycosis.
Eosinophils are decreased (cosinopenia), or disappear entirely
in severe infections and reappear upon recovery. ‘They are decreased
Hematology 39
also in shock, major surgical operations, severe alarm reactions,
Cushing’s disease, and following injection of adrenal cortica! hor-
mones, or substances that increase the output of these hormones,
e.g., ACTH and epinephrine.
For more accurate enumeration of the eosinophils to determine
the percentage of decrease in the Thorn test, they are counted in
a counting chamber and the total per cu. mm. is reported. (See
page 635). The normal range is usually 150 to 250 per cu. mm.
Basophils: Normal values of basophils in both adults and chil-
dren are from 0 to 0.75 per cent. Basophils originate from myelo-
blasts, but the mature nuclei do not become lobulated. The cyto-
plasm is characterized by coarse basic-staining granules.
Basophils are increased in the following conditions:
1. Blood diseases: Basophilic leukemia, myelogenous leukemia,
polycythemia vera and chronic hemolytic anemia.
2. Miscellaneous conditions: Sometimes in Hodgkin's disease,
chickenpox, smallpox, chronic infections of the bony sinuses, follow-
ing splenectomy, and sometimes after administration of nonspecific
proteins.
Origin and Significance of Nongranulocytes:
Lymphocytes: Normal values of lymphocytes are as follows:
Adults, from 25 to 33 per cent; children from three to ten years old,
from 42 to 48 per cent. Lymphocytes supposedly originate from
lymphoblasts in the spleen, lymph glands, tonsils, thymus, and
possibly the bone marrow. Lymphoblasts are not found normally in
the peripheral blood, but they are found in blood smears of acute
lymphatic leukemia.
Lymphocytes are sometimes classified as “large” and “small,” the
large form representing the more immature stage. Some authorities
assert, however, that the large forms originate in the spleen, while
the small forms originate in the lymph glands.
Abnormal lymphocytes, sometimes called “atypical lymphocytes”
are found characteristically in blood smears of infectious mononu-
cleosis. These cells are usually large, have an oval, kidney-shaped or
40 Body Fluids, Excreta, and Functional Tests
lobulated nucleus and a vacuolated or foamy nongranular cyto-
plasm. The nucleus is a coarse network of strands and masses of
chromatin. These are thought to be well differentiated, mature
lymphocytes by most hematclogists.
Lymphocytes are increased in the following conditions with an
increased white cell count:
Blood diseases: Lymphocytic leukemia and sometimes in pur-
pura hemorthagica.
Acute infections: Infectious mononucleosis, acute infectious
lymphocytosis, pertussis, and during convalescence from acute pyo-
genic infections.
Chronic infections: Tuberculosis in persons with good resistance,
congenital syphilis, and secondary syphilis.
Metabolic diseases: Rickets, thyrotoxicosis, and malnutrition.
Normal increase in infants and children.
Lymphocytes are increased in the following conditions with a
normal or decreased white cell count:
Blood diseases: Pernicious anemia and familial splenic anemia
{Gaucher's disease).
Acute infections: Typhoid fever, influenza, undulant fever
(brucellosis), infections hepatitis, German measles, and mumps.
Monocytes {Large Mononuclear Cells): Normal values are as
follows: Adults from 8 to 7 per cent; children from three to ten
years old, from 3 to 5 per cent. Monocytes are believed to originate
in the bone marrow from monoblasts. These develop into pre-
monocytes, which in tarn become adult monocytes.
Monocytes are increased in the following conditions:
Blood diseases: Monocytie leukemia.
Acute infections: Brucellosis, subacute bacterial endocarditis,
typhus fever, Rocky Mountain spotted fever.
Certain parasitic infestations: Kala-azar, cutaneous leishmaniasis,
malaria, and trypanosomiasis.
Miscellaneous conditions: Sometimes in Hodgkin's disease,
familial splenic anemia (Gaucher's disease), Niemann-Pick’s dis-
ease, Hand-Schiller-Christian’s disease, and poisoning by tetra-
chlorethane.
Hematology 4t
Plasma Cells: Plasma cells are not found normally in the per-
ipheral blood. They are thought to originate from lymphocytes or
primitive connective tissue cells.6 They are round cells with deep
blue cytoplasm and an eccentric nucleus containing deep-staining
chromatin arranged like the spokes of a wheel.
Plasma cells are found in the peripheral blood in the following
conditions:
Blood diseases: Plasma cell leukemia.
Exanthematous diseases: Rubella, slight increase in measles,
scarlet fever, and chickenpox.
Miscellaneous conditions: They may be present in multiple
myeloma and serum reactions.
Leukopenia:
Leukopenia is a reduction in the total number of leukocytes
below the lower limit of normal. It is usually due to a decrease in
granulocytes, particularly neutrophils.
Causes of Leukopenia: The important causes of leukopenia may
be grouped as follows:
1. Certain acute and chronic infections: Typhoid and paratyphoid
fever, brucellosis, miliary tuberculosis, overwhelming pyogenic infections.
2. Ceitain viral and rickettsial diseases: Measles, rubella, smallpox
up to about the fourth day, influenza after third or fourth day, infectious
hepatitis, dengue, psittacosis, scrub typhus {tsutsugamushi fever), sand
fly fever (pappataci fever), sometimes in infectious mononucleosis.
3. Certain protozoa! infestations: Systemic leishmaniasis, cutaneous
leishmaniasis, malaria except during a paroxysm.
4. Diseases of the hemopoietic s}stem: Aplastic anemia, agranulocyto-
sis, aleukemic leukemia, relapse of pernicious anemia, chronic hypo-
chromic anemia, Banti's syndrome, familial splenic anemia (Gaucher's
disease).
5. Certain drugs and poisons: Sulfonamides, barbiturates, amido
pyrine, benzol, dinitrophenol, thiouracil compounds, tridione, pyri
benzamine, arsenic, plasmochin, quinine, Chloromycetin, salol and thio-
glycolic acid, nitrogen mustards.
6. Radiation: X-rays, radium, and radiation from atomic disintegra-
tion.
7. Miscellaneous conditions: Portal cirrhosis, anaphylactoid shock,
nonspecific protein therapy, rheumatoid arthritis, splenic neutropenia,
Felty’s syndrome, cachexia, and debilitated states.
42 Body Fluids, Exereta, ond Functional Tests
- PLATELETS
The Life Cycle of Platelets:
Platelets are thought to originate from the megakaryocytes in
the bone marrow during adult life. The mechanism of their forma
tion is not clear, but apparently the cytoplasm of the megakaryo-
cytes undergoes fragmentation to form platelets. Wright®* came
to this conclusion in 1906 and his work has been confirmed by
Runting®? and Downey.s
Platelets have a short span of life of eight to nine days. In fact,
all of the platelets in the peripheral blood can be replaced in three
to five days, forming at the rate of approximately 100,000 per day.s?
Function of Platelets:
Platelets are concerned in the clotting of blood and also in clot
retraction (syneresis) .
Physical Function: By virtue of their adhesiveness, platelets tend
to stick to such surfaces as injured endothelium and form numerous
pseudopods. Thus, a mass of platelets in a strictly physical way can
plug openings in capillaries.
In connection with clot retraction, it has been observed that when
the platclet count is low, the clot is less firm, less rigid and less
adhesive than normal. Tocantins*® demonstrated experimentally
that clot retraction is absent when the platelet count is 70,000 per
cu. mm. or lower. It is felt, therefore, that platelets play an important
role in clot retraction probably by contraction of the pseudopods
thrown out by the platelets into the fibrin network.7%
Capillary Fragility: Those conditions in which there is a marked
dmombocytopenia are associated with increased capillary fragility
resulting in capillary hemorrhages when the tourniquet test is
applied. At the present time the mechanism whereby platelets
maintain the integrity of capillary endothelium is not clear.
Chemical Function. Platelets contain a number of active amines,
among which is serotonin. This was originally discovered as the
vasopressor agent released from clotted blood?9 and is now thought
to reinforce local vasoconstrictive mechamusms following trauma.
Hematology . 43
Platelet Coagulation Factors: The following platelet factors have
been partially purified: 7 .
Factor 1, a factor which resembles plasma proaccelerin also known
as Factor V; Factor 2, which accelerates the formation of fibrin by
the action of thrombin on fibrinogen; Factor 3, the lipoid platelet
thromboplastic factor; Factor 4, an antiheparin. Factor 3, the
thromboplastic factor, appears to be most important in blood
coagulation.
Normal Platelet Values:
The counting of platelets is not satisfactory because of their
small size, agglutination potential and tendency to break up
Normal adults are said to have 250,000 to 500,000 per cu. mm.
Figures vary depending on the technic used as indicated below:
Olef?? 437,000 to 586,000 per cu. mm.
Dameshek?t 500,000 to 900,000 per cu. mm,
Tocantins® cutaneous blood 250,000 + 7458, standard deviation
58,500
venous blood 310,000 = 11,937, standard deviation
110,750
arterial blood 350,000 + 13,889, standard deviation
128,000
Thrombocytosis:
‘Thrombocytosis is an increase in platelets above the upper limits
of normal. Due consideration must be given for the variation in
different methods as shown above.
Causes of Thrombocytosis: Thrombocytosis is noted in the fol-
lowing:
PHYSIOLOGICAL CONDITIONS: High altitudes, severe exercise,
cachexia, and malnutrition. .
DISEASES OF THE HEMOPOIETIG SYSTEM: Polycythemia vera, hemo-
lytic anemias, acute hemorrhage, chronic myelogenous leukemia,
and. chlorosis.
INFECTIONS: Suppurative processes and acute rheumatic fever.
MISCELLANEOUS: After surgical operations, particularly splenec-
tomy, after fractures, particularly of the neck of the femur, and
during asphyxia.
44 Body Fluids, Exereta, and Functional Tests
Thrombocytopenit
A decrease in the total platelet count below the lower limit of
normal is called thrombocytopenia and is generally associated with
protonged bleeding time, normal coagulation time, increased
capillary fragility and reduced prothrombin consumption. This
condition is found mostly in primary and secondary purpura
hemorrhagica as follows:
1, Idiopathic thrombocytopenic purpura.
2. Symptomatic thrombocytopenic purpura caused by the following:
Chemical and physical agents, acute and chronic leukemias; hypo
chromic, aplastic, pernicious, and myclophthisic anemias; certain infec
tions, such as septicemia, typhoid fever, early pneumonia, diphtheria and
bacterial endocarditis; hemolytic jaundice; Banti’s disease; familial
splenic anemia (Gaucher's disease); and on the first day of menstruation
COAGULATION OF BLOOD
‘The clotting of blood appears as a very simple reactton, but it is
in reality a very complex process. The most widely accepted concept
is that it @kes place in three steps or stages:
Stage 1
Interaction of platelet fac-
tor, antihemophilic factor Calcium and Plasma
(AHF), plasma thrombo + accesiory > thromboplastin
platin component (PTC) factors
Stage 2
Prothrombin -+ Thromboplastin,
calcium and ~ Thrombin
accessory Jactors
Stage 3
Fibrinogen’ + Thrombin 2 Fibrin
{blood dot)
Clotting Factors:
Confusion in terminology is one of the major problems in
studying blood coagulation. Dilferent investigators have given
different names to the same factor. Following is a list of international
numbers with synonyms:
Hematology 45
Factor F Fibrinogen
Factor 1 Prothrombin °
Factor HI = Thromboplastin (tissue)
‘Thrombokinase
Factor IV) Calcium
Factor V Labile factor
Proaccelerin
Plasma Ac globulin
Factor VE Serum Ac globulin
Accelerin
Factor VIL Stable factor
Proconyertin
Serum prothrombin conversion accelerator (SPCA)
Co-thromboplastin
Autoprothrombin I
+Factor VIL Antihemophilic factor (AHF)
Thromboplastinogen
Platelet co-factor I
Plasma thromboplastic factor A
Factor IX Plasma thromboplastin component (PTC)
Christmas factor
Platelet co-factor J]
Plasma thromboplastic factor B
Autoprothrombin JI
Factor X Stuart-Prower factor
Factor XI Plasma thromboplastin antecedent (PTA)
Factor XII Hageman factor
Following is a description of the nature of the various factors:
FACTOR I. FI8RINOGEN: This is a molecule of large molecular weight,
in plasma but not in serum. Fibrinogen is changed to fibrin by the proteo-
lytic action of thrombin.
FACTOR 11. PROTHROWBIN: This is a stable plasma glycoprotein which
is converted to thrombin by thromboplastin, calcium and certain other
factors. It is virtually absent from normal serum. .
FACTOR Il. TISSUE THROMBOPLASTIN: Tissues which show the greatest
thromboplastic activity are brain, ]ung and placenta. Tissue thrombo-
plastin can be fractionated into a heat-stable lipoid substance which seems
closely related chemically to platelet factor 3, and a heat labile protein
which seems to resemble the product of the interaction of AHF, PTC,
PTA and other plasma factors.75
FAcToR Iv. CALGIUM: Calcium secms to be required in many phases
of the clotting process. Calcium and accessory factors are necessary for
46 Body Fluids, Excreto, ond Funetional Tests
the completion of stages 1 and 2 of blood clotting. Details of the inter-
actions which take place must await further research.
FAGIOR V. PROACCELERIN: This has the character of 2 globulin which
is necessary for the formation of thrombin from prothrombin by throm.
boplastin and calcium. One group in ute United States has called it
plasma accelerator globulin,?® while another has called it labile factor.?7
Ta Australia, Fantl and Nance’® designated it accelerator substance, and
in Norway, Owren?? used the term Factor V. It disappears rapidly during
coagulation, hence fresh serum contains virtually none.
FACTOR vi, AccILIRIN: This facto. was named aceelerin because it
was considered to be the active form of proaccelerin, Factor V.
TAGTOR VII, PROCONVERTIN: This is a stable B globulin which is found
in both plasma and serum. Owren?? described it as Factor VII, Ware and
Scegers*? as serum Ac-globulin and Alexander®? as prothrombin con-
version accelerator, It can correct the prolonged prothrombin times of
certain patients treated with coumarin, of infants during the neonatal
period, of those with liver cell damage, and of those rare patients who
have a congenital Factor VII deficiency.
FACTOR Vill. ANTIHEMOPHILIG rAGroR (Ar): This factor is 2 glebulin
which corrects the clotting in true hemophiliacs. It is normally present
in plasma and is used up in the process of clotting, hence is not present
in serum.
FACTOR 1X. PLASMA THROMBOPLASTIN COMFONENT: This factor is 2
betas globulin found sn normal serum and plasma. It corrects the clotiing
defect in Christmas disease and is also known as Christmas Tactor
FACTOR X. STUART-PROWER 1 AcToR‘®} This is an alpha globulin which
ip found in both serum and plasma. Ie is necessary for the formation of
thromboplastin and the action of tissue thromboplastin in converting
prothrombin to thrombin.
FACTOR XI. PLASMA ‘THROMBOPLASTIN ANTECEDENT (FTA): This is a
globulin which is present in normal serum and plasma. The lack of this
globulin causes a hemophiha-like disease, but it oceurs in esther sex
FACTOR Xit M1AGEMAN FACTOR:64 This 15 a2 heatlabile globulin witch
is present in both serum and plasma. The lack of this factor causes no
clinical symptoms.
Thrombin:
Thrombin is formed from prothrombin by the acuon of
thromboplastin, calcium and certain other factors. [t appears that
plasma thromboplastin reacts with calcium and Factor V (proac-
celerin) to form an unstable product, prothrombinase, which can
carry aut the final change of prothrombin to thrombin in the
Hematology 47
presence of calcium. From the reaction of tissue thromboplastin,
calcium, Factor V, Factor VII and Stuart Factor an apparently similar
prothrombinase is formed.
Thrombin not only forms fibrin from fibrinogen, but it speeds
up the disruption of platelets and activates Factor V, thus catalyzing
the first two stages of blood coagulation.
Fibrin:
Fibrin is formed from fibrinogen which acts as the substrate for
the proteolytic action of thrombin. Fibrin strands are then formed
by polymerization.85
TESTS FOR HEMORRHAGIC DISORDERS
Platelet Count:
The platelet count yields information which may be of help in
evaluating a hemorrhagic condition, In addition to counting
platelets, they should be evaluated qualitatively, ¢.g., for the presence
of giant forms. Both thrombocytosis and thrombocytopenia may be
associated with a hemorrhagic disorder. If the platelet count is
sufficiently reduced, there 1s usually an associated prolonged bleeding
time, increased capillary fragility and poor clot retraction. However,
the clotting time is within normal limits, and prothrombin con-
sumption is reduced.
Coagulation Time:
Coagulation time is the measurement of the clotting of blood
in vitro without tissue juices. This may be done in several ways, but
the same technic and the same caliber glassware should be used each
time.
Capillary-Tube Method: A common technic is the capillary-tube
method. Five pieces of capillary tubing are filled with fresh blood
from a deep cut. A section of tube is broken off at each one-half.
minute interval. The end-point is the appearance of a thin thread
of fibrin between the fragments as they are pulled apart. The nor-
mal coagulation time by this method is from three to seven minutes.
Lee and White Method: Another popular method is that of Lee
and White, in which 1 ec. of blood is placed in a tube with a di-
ameter of 8 mm. (%o inch). The tube should be absolutely clean
48 Body Fluids, Excreta, and Functional Tests
and should be rinsed with isotonic saline solution, It is advisable
to use at least three tubes so chat one tube is undisturbed while
the others are being examined. The test is best carried out at 98.6°
F, (37° C) The normal range by this method is from six to 15
minutes. A normal coagulation time does not exclude a clotting
defect and does not prove adequacy of plasma thromboplastin
formation.
The coagulation time may be shortened by the accidental inuo
duction of tissue fluids, rapid passage of blood through the needle,
introduction of air bubbles, or unclean or rough glassware. It may
be prolonged by very low or high pH, very low or high temperature,
the use of ordinary plastic, silicone, or paraffin-lined tubes, or after
administration of hepain. In a silicone tube the normal range 1s
19 to 60 minutes,
The coagulation time is prolonged under the following condi-
tions:
Hypoprothrombinemia in which there is a deficiency of
Factors Il, V, VII or X, vitamin K deficiency or inability to
absorb it,
Hemophilia, Factor VIII deficiency.
Plasma ‘thromboplastin component deficiency, Factor XI
deficiency.
Hageman wait, Factor XII deficiency.
Fibrinogenopenia or afibrinogenemia.
Hyperheparinemia in heparin therapy, peptone and anaphy
lactic shack. 2
Circulating anticoagulants against factors V, VIII and 1X
Clot-Retraction Time:
Determinalion: Determination of clot-retraction time may be
made by placing I cc. of venous blood in each of three small rubes
(8 mm. [3%o inch] in diameter) and § cc, in a fourth, All tubes are
placed in a 98.6° F. (87° C.) incubator and inspected (not handled)
after one-half, one, two, four, and 24 hours for evidence of retrac-
tion from the side, There is retraction of normal blood in from 30
to GO minutes.
Hematology . 49
Clot retraction is prolonged and is not satisfactory in the follow-
ing conditions:
Primary thrombocytopenia. .
Thrombocytopenia secondary to aplastic anemia, pernicious
anemia, hemorrhagic disease of the newborn, acute leukemias,
multiple mycloma and malignant granuloma (Hodgkin's disease)
of the bone marrow.
Bt
Fig. 4: Clot retraction. A: Normal retraction of clot, B: No retraction of lot,
Thrombasthenia in which the platelet count is normal, but
there is imparred platelet aggregation.
Development of fibrinolysin in shock may confuse the result
by dissolution of the clot.
$0 Body Fluids, Excreta, and Functional Tests
Factors Influencing Glot Retraction: (1) A decrease in the
amount of fibrinogen results in the formation of a small clot which
gives the impression of normal clot retraction. (2) A decrease in the
number of red cells gives the impression of normal clot retraction.
(3) An increase in the number of red cells (polycythemia) results
in an apparently poor clot retraction, since the clot is large and the
amount of clear serum is small.
Dissolution of Clot:
Fibrinolysins may be detected in whole blood or im plasma by
observing shrinkage of a clot kept at 37° C. for 24 hours. A normal
clot docs not change in this time. Fibrinolysins da not usually
produce a severe bleeding disorder unless they can cause lysis of a
clot in two hours or less, An increase in fibrinolysins may be found
in major surgery of the lung, prostate or uterus, shock, premature
separation of the placenta, death of fetus in utero, advanced hver
disease and carcinomatosis,
Fibrinogen Level:
‘The normal plasma fibrinogen level is 150 to 300 mg. per 100 cc.
Blood congulation is not usually defective unless the plasma
fibrinogen level is less than 100 mg. per 100 cc. Clinically significant
reduction of fibrinogen levels fs seen in abruptio placentae, retention
of a dead fetus, amniotic fluid embolism, congenital afibrino
genemia, liver discases, severe malnutrition, typhoid fever, marked
anemia and for a short time after extensive hemorrhage.
Bleeding Time:
‘The normal bleeding time is one to three minutes.
The bleeding time is protonged in the following conditions:
Primary thrombocytopenia.
Thrombocytopenia secondary to pernicious anemia, aplastic
anemia, hemorrhagic disease of the newborn, acute lerhemias,
chronic lymphocytic leukemia, multiple myeloma and Hodghin’s
disease of the bone marrow.
Vascular hemophilia.
Thrombocytopathia, a condition in which there is a decrease
in platelet factor 3.
Hematology 51
Value of Bleeding and Clotting Time:
The concept of the value of bleeding and clotting time has
undergone a change. With the availability of more specific tests,
bleeding and clotting times as screening tests have little to offer
except in severe disorders of blood clotting.
Capillary Fragility Test:
Determination: The capillary fragility test is also Known as the
“tourniquet test.” A blood-pressure cuff is applied above the elbow,
and the pressure is maintained at a point just above the diastolic
pressure. In a positive test, a large number of tiny hemorrhages
develop within a few minutes.
The test is positive in idiopathic thrombocytopenic purpura and
in some cases of secondary thrombocytopenic purpura, scurvy,
scarlet fever, measles, influenza, achylia gastrica, vitamin-K defi-
ciency, and chronic nephritis.
Prothrombin Determination:
Schofield’s8* discovery of the part played by spoiled sweet clover
in hemorrhagic disease of cattle was followed by isolation and
synthesis of the active principle, dicoumarin. Dicoumarin under
various trade names, such as Dicumarol, now has an important
role in the prevention and treatment of coronary thrombosis,
phlebothrombosis and thrombophlebitis. In such cases, the blood-
clotting mechanism is too efficient. The use of Dicumarol is an
attempt to reduce the efficiency of this mechanism to the lower limit
of safety. This is done by giving an initial dose of from 200 to 300
mg. (3 to 414 grains) of Dicumarol, which does not become effective
for 48 hours. A prothrombin time or prothrombin activity (Fig. 5)
is determined at this time to establish a base line, or normal, for the
patient. To eliminate confusion, the prothrombin time only is re-
ported in seconds, The complete report should inclide the pro-
thrombin time of the control as well as that of the patient. The
range of the normal prothrombin time is usually from 12 to 14
seconds.
In view of the fact that a difference of a few seconds in pro-
thrombin time is indicative of wide differences in prothrombin
52 Body Fluids, Excreto, ond Functional Tests
concentration, procedures have been developed in which the plasma
is diluted, thus creating a longer coagulation time and making it
easier to detect minor variations in prothrombin concentration. The
optimal dilution appears to be 12.5 per cent plasma in isotonic
saline solution, and this is said to increase the sensitivity and relia-
bility of the test. The normal range using diluted plasma according
to the method ot Shapiro4? is fiom 37 to 42 seconds
® |
| TT
coe 1
je -—— 4
i
Fig. 5: Prothrombin activity curve for plasma with prothrombin time
of 12 seconds, Curve is determined by tests on serial dilutions of plasma.
(Quiek, A. Ja Am, J. Clin. Path., 10:222, 1940.)
The prothrombin time is prolonged in the following conditions:
Treatment with anticoagulants which reduce prothrombin Factors
Vil and X.
Parahemophitia in which there isa deficiency of Factor V.
Serum prothrombin conversion accelerator (SPCA), Tactor VII
deficiency.
Hemorrhagic disease of the newborn,
Liver disease in which there 1s suficient reduction of Factors V, VI
and X and fibrinogen.
Circulating antiprothrombin and anuthromboplastin
Hematology 53
Sources of Error: The physician as well as the technician should
be aware of the sources of error in determining the prothrombin
time.
I. Fresh plasma should be used. Plasma allowed to stand at room
or refrigerator temperature for more than two or three hours may give
clotting times slightly higher than fresh plasma.
2. Hemolysis of the specimen of blood.
3. Inadequate amount of blood resulting in an excess of the antico-
agulant.
4. The use of old thromboplastin extract. It should be used within
four hours after preparation. Prolonged aging results in a loss of potency
and prolonged clotting time.
5. Metallic fons, such as copper, in the distilled water used in mak-
ing the saline solution for extraction of the thromboplastin may lead to
prolonged clotting time,
6. Failure to recognize the end-point.
7. Glassware must be chemically clean. Soaps and other detergents
used in cleaning glassware, if net properly rinsed off, will tend to give
prolonged clotting time.
8. The calcium chloride, sodium chloride, sodium oxalate, potassium
oxalate, and ammonium oxalate must be anhydrous and of reagent
grade. Prolonged clotting times have been traced frequently to faulty
calcium chloride. {: should be used in an anhydrous state.
9. Failure to mix the reagents thoroughly with the plasma at the
time of addition may result in a prolonged clotting time.
10, The storage of thromboplastin at room temperature may result
in slight loss of potency in one to two months. It is, therefore, advisable
to store it in the refrigerator.
IL. The use of improper technic, such as improper use of the pipet,
neglecting to blow into it after each transfer, and neglecting to wipe the
outside of the pipet at each transfer.
Prothrombin Consumption Test:*
The prothrombin consumption test is really a measure of the
available plasma thromboplastin. By determining the prothrombin
before and after coagulation is complete one obtains a measure of
the thromboplastin that reacts with prothrombin.
54 Body Fluids, Excreta, and Functional Tests
Prothrombin consumption and thromboplastin generation are
reduced in the following conditions:
Hemophilia in which there is a deficiency of Factor VIE.
Deficiency of Factors V, IX, X, XL or XL,
Thrombocytopenia with impaired thromboplastin formation,
Thrombocytopathia, a condition in which thee is a deficiency of
platelet factor 3.
Circulating anuithromboplastin
Thromboplastin Generation Test (TGT);**™
This test is of value in differentiating blood coagulation
abnormalities in which there is deficient formation of thambo.
plastin. Such abnormalities are found in hemophiha with deficiency
of Factor VIII (AHG), deficiency of Factor IX (PTC) and in
abnormality of platelet function. It is based upon the fact that
normal plasma treated with aluminum hydroxide which contains
Factor VHI (AHG), Factor V (proaccelerin), Factor XI (PTA),
Factor XII (Hageman Factor), platelets plus normal serum which
supphes Factors IX (PFC) and X (Stuart-Prower Factor) as well as
Factor XI (PTA) and XII (Hageman Factor) react to form
thromboplastin in the presence of calaum chloride. A Jack of any
ol these seven factors will cause abnormal thromboplastin formation
1, When patient's adsorbed plasma, normal serum and normal plate-
lets are incubated, then deficiency of Factor V or VIII is present. They
are differentrated by the prothrombin time. I{ prothrombin time 1s pro-
longed, Factor V deficiency exists, but not Factor VIII deficiency
2. When patient's serum and normal adsorbed plasma and normal
platelets are incubated, then deficiency of Factor IX or X is present.
Differentiate by prothrombin time which is normal in Factor IX defi-
erency and prolonged in Factor X deficiency.
3. Patient's adsorbed plasma plus patient's serum: and patient's or
normal platelets are incubated, then deficiency of Factor NJ or XII is
present .
4, When patent's platelets plus normal adsorbed plasma and normal
serum are incubated, thrombocytopenia or thrombocytopathia is present.
Hf the platelet count 1s normal, the cause 1s thrambocytopathia.
Hematology 55
Partial Thromboplastin Time (PTT):
This is an overall screening test of the total coagulation
mechanism except for platelet factor deficiency and Factor VII
deficiency. It is based on the observation that with whole thrombo-
plastin (saline extract of rabbit brain) the results obtained with
hemophilic plasma are the same as with normal plasma, while with
partial thromboplastin (cephalin) the results with hemophilic
plasma are much longer than those with normal plasma. In carrying
out the test, a standardized amount of platelet-like reagent is added
to plasma. The reaction is initiated by the addition of calcium
chloride, and a stopwatch is started simultaneously. The tube is
incubated in a 37° C. waterbath for 30 seconds and is then checked
periodically for clot formation. The normal range is 40 to 100
seconds.
NEW TERMINOLOGY OF BLOOD CELLS
The first two reports*!. 92 of the Committee for Clarification of
the Nomenclature of Cells and Diseases of the Blood and Blood-
Forming Organs recommend certain changes in names and defini-
tions of blood cells. It seems advisable to give a summary of these
recommendations here with the hope that it will help to promote a
universal adoption of some form of standard nomenclature.
The following terms are recommended for the cells of the differ-
ent series and for diseases affecting any cell of that series: Lympho-
cytic, granulocytic, monocytic, plasmacytic, thrombocytic, and
erythrocytic.
Table 9 gives recommended terms for each of the white cells
and thrombocytes.
The definitions decided on are as follows:
Lymphoblast:
Any cell of the lymphocytic series having fine chromatin struc-
ture in the nucleus. Cells of blast morphology associated with pro-
lymphocytes should be tentatively classified as lymphoblasts.
Prolymphocyte:
Any cell of the lymphocytic series intermediate in morphology
56
Body Fluids, Exereta, and Functional Tesis
Taste 9: RecoMMENDED Terms AnD TERMS TO BE AVOIDED
WHEN REFERRING TO SreciFic CELLs oF BLoop AND
Bioop-Forminc OrcANS
eee
Nase of Series| Term to be Used Terms to be Avoided
Lymphocytic. .} Lymphoblast Myeloblast, hemocytoblast, Iymphoidocyte,
stem cell, lymphocyte
Prolymphocyte Large lymphocyte, pathologie large lympho-
eyte, atypical leukocytoic lymphocyte,
monocyte, immature lymphocyte
Lymphocyte Small, medium, or large lymphocyte, normal
lymphocyte, smalt, medium, or large
mononuclear
Monocytic. ...| Monoblast Myeloblast, hemocytoblast, lymphoidocyte,
lymphocyte, stem cell, immature monocyte
Promenocyte Premonocyte, hemohistioblast, immature
monocyte, Ferrata cell
Monocyte Large mononuelest, transitional, plasmato-
oyte, endothelial leukocyte, histtocyte,
resting wandering cell
Granulocytic. .| Myeloblast Granuloblast, hemocytoblast, lymphoidocyte,
lymphocyte, stem cell
Progranulocyte Promyclocyte Il, levkoblast, myeloblast,
premyelocyte, promyelocyte, progranulo-
eyteA
Myelocyte Granulocyte, myelocyte B, nonfilament,
class I
eS
Hematology
57
TABLE 9: (Continued)
Name of Series| Term to be Used Terms to be Avoided
Granulocytic. | Metamyelocyte Metagranulocyte, juvenile, myelocyte C,
Continued nonfilament, ¢elass I
Band cell Staff cell, stab cell, nonfilament, class I, rod
nuclear, polymorphonuclear, stabkernige,
thabdocyte, nonsegmented
Segmented Polymorphonuclear, filamented, class IT, Ii,
IV, or V, loboeyte
Plasmacytic. ..]| Plasmablast Myeloblast, hemocytoblast, lymphoidocyte,
lymphocyte, stem cell, lymphoblastic
plasma cell, myeloma cell
Proplasmacyte Tork cell, Turk irritation form, lympho-
blastic or myeloblastic plasma cell,
myeloma cell
Plasmacyte Plasma cell, Unna’s plasma cell,
Marschalko’s plasma cell, plasmacytoic
lymphocyte, myeloma cell
Thromboeytic | Megakaryoblast | Megalokaryoblast
Promegakaryocyte | Premegalokaryocyte
Megakaryocyte Megalokaryocyte
Thrombocyte Platelet, thromboplastid
Disintegrated cell
Senile cell, smudge, basket cell, smear cell,
degenerated cell
58 Body Fluids, Exereta, ond Functional Tests
between the lymphoblast and the lymphocyte. It will always have
toa coarse a chromatin structure to fit the criteria for a blast and to0
fine a chromatin structure or too large a cell diameter to be classed
as a lymphocyte. Usually, but not always, prolymphocytes are larger
than 15 microns in diameter, which is the upper limit for the
lymphocyte.
Lymphocyte:
Any cell of the lymphocytic series having the morphology of
those commonly found in the blood of healthy adults.
Monoblast:
Any cell of the monocytic series having fine chromatin structure,
Usually nucleoli are visible. Cells of blast morphology found in
association with promonocytes should be tentatively classed as
monoblasts.
Promonocyte:
Any cell intermediate in morphology between the monoblast and
the monocyte. It is differentiated from the monoblast by having an
irregularly shaped nucleus and somewhat coarser chromatin struc-
ttre, and from the monocyte by the presence of one or more
nucleoli.
Monocyte:
Any cell of the monocytic series having the morphology of these
commonly found in the blood of healthy adults. Ic is differentiated
from the promonocyte by the absence of nucleoli,
Myeloblast:
Any cell of the granulocytic series having fine chromatin stru
ture and containing no specific granules. Usually nucleoli are vi
ble. Cells of blast morphology found in association with progranu-
locytes should tentatively be classed as myeloblasts.
Progranulocyte:
Any cell of the granulocytic series which has a nuclear structure
too coarse for that of a blast cell and which has not yet developed
Hematology 59
discernible, specific granules. This term was selected rather than
“promyelocyte” because of its clear relationship to the definition of
granulocyte, given below, and because the term “promyelocyte”
has been in wide use for cells which do contain specific granules.
The reason that the terms granuloblast, granulocyte, and meta
granulocyte were not chosen was that the terms myeloblast and mye-
locyte were already in general use with essentially the definitions
here given. This is true also for the term granulocyte, which would
otherwise have to be synonymous with the term myelocyte.
Specific Granules:
Neutrophilic, eosinophilic, or basophilic granules. This term
does not include azurophilic granules.
Granulocyte:
An inclusive term to apply to any cell containing specific gran-
ules. The plural form “granulocytes” would therefore include all
myelocytes, metamyelocytes, band cells, and segmented cells whether
neutrophils, eosinophils, or basophils.
Myelocyte:
Any cell containing specific granules, with a round or oval nu-
cleus. It is distinguished from the progranulocyte by the presence of
specific granules and from the metamyelocyte by the absence of
indentation in the nucleus, It may be further subdivided, at the
option of the user, into early and Jate stages, but the definition of
early or late should be clearly stated in any publication.
This and all subsequent cells of the granulocytic series should
be additionally characterized as neutrophil, eosinophil, or basophil.
Metamyelocyte:
Any cell of the granulocytic series having specific granules in the
cytoplasm and a nucleus intermediate in shape between that of
the myelocyte and the band cell. The nucleus usually has an in-
dented oval shape, resembling 2 bean or kidney.
Band Cell:
Any cell of the granulocytic series which has a nucleus that
could be described as a curved or coiled band, no matter how
60 Body Fluids, Exereta, one Functional Tests
marked the indentation, if it does not completely segment the
nucleus into lobes connected by a filament, It is differentiated from
the metamyelocyte by an appreciable length of the nucleus having
parallel sides, and from the segmented neutrophil by having no
indentation which could be described as a filament.
Segmented Cell:
Any cell containing specific granules in which the lobes of the
nucleus are connected by a filament. A filament is defined as a
thread-like structure, Since at times, in viewing a three-dimensional
object from one direction, it is impossible to be certain whether
two parts of the nucleus are connected by 2 filament or band, it is
suggested chat such cells always be placed in the segmented category
since this is the more differentiated and more common cell.
The term “toxic neutrophils,” followed by 2 1 to 4-4 designa
tion, is recommended for the grading of toxic granules, basophilia
of the cytoplasm, vacuoles, and condensation of nuclear chromatin
in the neutrophils, since its meaning is clear, although it is recog-
nized that it is not an adequately descriptive term. The grading
should depend more on the degree of change than on the percenage
of the cells involved and should be recorded in the report whenever
the degree of change exceeds 2--.
Plasmablast:
Any cell of the plasmacytic series having fine chromatin structure
in the nucleus. Cells of blast morphology found in association with
proplasmacytes are usually seen only in plasmacytic leukemia or
plasmacytic sarcoma. The cytoplasm tends to be more opaque in
staining than in the other Icukocytic blast cells.
Proplasmacyte:
Any cell of the plasmacytic series with a nuclear structure too
coarse for that of a blast cell but with one or more nucleoli present.
Plasmacyte:
A cell characterized by extremely coarse chromatin structure,
Hematology 61
with the deeply staining chromatin of the nucleus aggregated into
large, sharply demarcated clumps. It is differentiated from the pro-
plasmacyte by the absence of nucleoli. The cytoplasm of all cells of
the plasmacytic series tends to be deeply basophilic and opaque in
appearance. Azurophilic granules may be present or absent, but
are more commonly absent.
Megokaryoblast:
Any cell of the thrombocytic series having a nucleus with fine
chromatin structure. Usually these are larger than the other blast
cells.
Promegakaryocyte:
Any cell of the thrombocytic series with a nucleus containing
nucleoli but having a chromatin structure too coarse for a blast cell.
The nucleus is usually similar in shape to that of the megakaryocyte.
Fine azurophilic granules are usually diffusely scattered through the
cytoplasm.
Megakaryocyte:
Any nucleated cell of the thrombocytic series in which nucleoli
are not discernible, The azurophilic granules are often aggregated
into clumps. Megakaryocytes and promegakaryocytes are typically
much larger than other cells found in the marrow.
Thrombocyte:
Any cell of the thrombocytic series containing no nucleus; in
other words, any non-nucleated fragment of megakaryocytic cyto-
plasm containing azurophilic granules similar to those of the mature
megakaryocyte.
The term “thromboplastid” was recognized as being anatomi-
cally correct, but it was felt that to be consistent with the use of
the term “erythrocytic” and to permit the use of “thrombocytic”
and “erythrocytic” in describing these cell series, the suffix “cyte”
was preferable for these two non-nucleated forms.
62 Body Fluids, Excreta, and Functional Tests
Disintegrated Cell:
Any cell of any series in which the cytoplasmic outline has been
disrupted or the nuclear chromatin is no longer surrounded by a
membrane, excluding the changes in the nucleus that occur in
mitotic division. Disintegrated cells should be recorded as such in
the differential report, even though they could be identified by
dispersed granules. They should be counted even if only shreds of
nuclear material are discernible, since they are undoubtedly in-
cluded in the total leukocyte count.
Table 10 gives the recommended terms for cells of the erythro-
cytic series.
‘The definitions of cells of the erythrocytic series are as follows:
Rubriblast:
Any cell of the erythrocytic series having fine chromatin struc-
ture in the nucleus. Nucleoli are usually discernible. A stippled
chromatin pattern is more common than the lace-net pattern usually
seen in other blast cells.
Tate 10; RecomMenpen Terms anp Terms To BE Avoipep
Wuen Rererring To Speciric Cetrs oF EryrHrocytic Series
Name of Series | Term ta be Used Terms to be Avorded
Erythroeytic | Rubriblast Crythroblast, megaloblast, pronormoblast,
promegaloblast, normoblast, hemocyto-
blast, stem cell, myeloblast, lymphordo-
eyte, karyoblast.
Prorubricyte Erythroblast, megaloblast, pronormoblast,
normoblast, macronermoblast, macrablast,
prokaryocyte
Normoblast, pronormoblast, macronormo-
blast, erythroblast, polychtomatophilic
wormoblast, karyooyte
Metarubrieyte Normoblast, erythroblast, metakaryocyte
Reticulocyte*
Erythrocyte Red blood cell, erythroplastid, normocyte,
akaryocyte
"Tt is recommended that the reticulocyte stage be considered a subdivision of the
erythrocyte stage.
Hemotclogy 63
Prorubricyte:
Any cell of the erythrocytic series in which one or more nucleoli
are discernible in the nucleus and which has a chromatin structure
tao coarse to be classified as a rubriblast.
Rubricyte:
Any cell of the erythrocytic series having definite structure of
the nuclear chromatin, but containing no discernible nucleoli. This
stage is differentiated from the prorubricyte by the absence of
nucleoli in the nucleus, and from the metarubricyte by net having
a pyknotic, fragmented, or partially extruded nucleus. Some may
wish to subdivide and qualify this stage—or other stages—further
into basophilic, polychromatic, or normochromatic rubricytes, ac-
cording to the amount of hemoglobin present in the cytoplasm.
Metarubricyte:
Any nucleated cell of the erythrocytic series having a pyknotic,
fragmented, partially extruded, or partially autolyzed nucleus. Pyk-
notic describes a dense, solid, structureless nuclear mass. The phe-
nomenon of karyorrhexis, or fragmentation of uuclei, should be
clearly distinguished from the occurrence of double, well-formed
nuclei, which are occasionally seen in prorubricytes and rubricytes,
as well as in other cells which may divide amitotically.
Reticulacyte:
Any non-nucleated cell of the erythrocytic series in which, when
supravitally stained—usually with brillant cresyl blue—one or more
granules or a diffuse network of fibrils are discernible. All reticulo-
cytes are included under the term “erythrocytes” since, without a
special stain, reticulocytes are indistinguishable from erythrocytes.
Erythrocyte:
Any non-nucleated cell of the erythrocytic series.
Pemicious-Anemia Type:
The qualifying adjective phrase to be applied to any cell of the
erythrocytic or granulocytic series, and to the marrow and blood
64 Body Fluids, Exereta, and Functional Tests
pictures as a whole, to indicate the presence of the morphologic
changes characteristically seen in pernicious anemia and other
macrocytic anemias which respond to liver extract or folicacid
therapy. In the nucleated cells of the erythrocytic series, the major
feature of this change is a relative increase in the palestaining para
chromatin with a corresponding decrease in the deep-staining basi-
chromatin. In the cells of the granulocytic series, the characteristic
change is the presence of giant forms having very bizarre nuclei; and
in the segmented neutrophils, the occurrence of many cells with
more than five lobes,
REFERENCES
1, Dacie, J. V. and White, J. C.: Exythropoiesis with Particular Refer-
ence to Its Study by Biopsy of Human Marrow. J. Clin. Path,
2:1, 1949.
2. Brannan, D.: Extramedullary Hematopoiesis in Anemias. Bull
Johns Hopkins Hosp., 41:104, 1927.
3. Lyall, A.: Massive Extramedullary Bone Marrow Formation in a
Case of Pemicious Anemia. J. Path. & Bact., 41:469, 1935.
4. Meyer, E. and Heineke, A. Uber Blutbildung in Milz und Leber
bei schweren Anamien. Verhandl. d. deutsch pat. Gesellsch, 9:224,
1905.
5. Wintrobe, M, M.: Relation of Discasc of the Liver to Anemia. Arch
Int. Med., 57:289, 1936,
G. Jordan, H. E.: Extramedullary Blood Production. Physiol. Rev.,
22:375, 1942.
7. Blaisdell, J. L.: Extramedullary Hematopoiesis in a Retroperitoneal
Tumor. Arch, Path. 16:643, 1933.
8. Schiller, W.: Local Myelopoiesis in Myeloid Leukemia. Am. J, Path,
19:809, 1943.
9, Donhauser, }. L.: The Human Spleen as an Haemoplastic Organ,
as Exemplified in a Case of Splenomegaly with Sclerosis of the
Bone Marrow. Jour. Exper. Med., 10:559, 1908.
10. Moeschlin, S: Phasenkontrastuntersuchungen in der Hamatologie
Acta Haematol., 2:399, 1949.
11. Klima, R. and Rosegger, H.: Untersuchungen uber Farbbarkeit,
Resistenz und Formeigenheiten der menschlichen Retikulozyten
Tolia Haematol, 51-414, 1934.
J2. Sabin, F. R : Bone Marrow. Physiol Rev., 8:191, 1928.
13. Shillingford, J. P.: The Red Bone Marrow in Heart Failure. Jour.
. Path., 3:24, 1950.
Hematology 65
14, Gordon, A. S. and Charipper, H. A: The Endocrine System and
Hemopoiesis. Ann. New York Acad. Sci., 48:615, 1947.
15, Arinkin, M,. J.: Intravitale Untersuchungens methodika des Kno-
chenmarks. Folia Haematol , 38:233, 1929.
16. Segerdahl, E.: Uber Sternalpunktionen, Uppsala, Appelbergs Bok-
tryckeriaktiebolag, 1935.
17, Kolmer, J. A.: Clinical Diagnosis by Laboratory Examinations. C.
Appleton-Century Co., Inc, New York, 1944, p. 44.
18. Keith, N. M., Rountree, L. G., and Geraghty, J. T.: A Method for
the Determination of Plasma and Blood Volume. Arch. Int. Med.,
16:547, 1915.
19. Gregersen, M. L., Gibson, J. G., and Stead, E, A.: Plasma Volume
Determinations with Dyes; Errors in Colorimetry; Use of the Blue
Dye T-1824. Am. J. Physiol. (Proc), 118:54, 1935; also Am. Jour.
Physiol. 120:494, 1937; Jour, Lab, and Clin. Med., 23:423, 1938;
ibid., 168:517, 1950.
20. Price, P. B. and Longmire, W. P.: The Use of T-1824 in Plasma
Volume Determinations. Bull. Johns Hopkins Hosp., 69:327, 1941;
ibid., 71:51, 1942; ibid., 75:14, 1944.
21. Morris, C. J. O. R.: Chromatographic Determinations of Evans’ Blue
in Plasma and Serum. Biochem. Jour., $8:203, 1944.
22. Courtice, F. C. and Gunton, R. W.: The Determination of the Blood
Volume in Man by the Carbon Monoxide and Dye Methods. Jour.
Physiot., 108:142, 1949,
23. Reid, A. F. and Orr, M, K.: A Rapid Method for Determining Blood
Volumes by the Use of P32—Labelled Red Cells. Jour. Clin, In-
vest, 29:313, 1950.
24. Crispell, K. R., Porter, B.. and Nieset, R. T.: Studies of Plasma
Volume Using Human Serum Albumin Tagged with Radioactive
Jodine. Jour. Clin. Invest., 29:513, 1950.
25. Storaasli, J. P., Krieger, H., Friedell, H. L., and Holden, W. D.: The
Use of Radioactive Jodinated Plasma Protein in the Study of
Blood Volumes. Surg., Gyn., and Obstet., 91:458, 1950.
26. Gray, S. J. and Sterling, K.: The Tagging of Red Cells and Plasma
Proteins with Radioactive Chromium, Jour. Clin. Invest., 29:1604,
1950.
27. Rountree, L. G., Brown, G. E., and Roth, G. M.:; The Volume of
Blood and Plasma in Health and Disease. W. B. Saunders Co.,
Philadelphia and London, 1929.
28. Sunderman, T. W. and Austin, J, H.: The Measurement of Serum
Volume. Am, Jour. Physiol., 117:474, 1936.
66
29,
30,
31.
32.
33.
34,
35.
36.
37.
38.
39.
40.
41.
42,
43,
a}
Body Fluids, Exereta, and Functional Tests
Gibson, J. G. and Evans, W. A.: The Relation of Plasma and Total
Blood Volume to Venous Pressure, Blood Velocity Rate, Physical
Measurements, Age and Sex in Ninety Normal Humans. Jour.
Clin, Invest., 16:317, 1987.
Hurtado, A., Merino, C., and Delgado, E.: Influence of Anoxemia
on the Hemopoietic Activity. Arch, Int. Med., 75:284, 1945.
Hopper, J., Jr. Tabor, H, and Winkler, A. W.: Simultaneous Meas-
urements of the Blood Volume in Man and Dog by Means of
Exans Blue Dye, T1824, and by Means of Carbon Monoxide; Nor-
mal Subjects Jour, Clin Invest,, 23:628, 194.
Salvesen, H. A.: The Determination of Blood Volume by the Carbon
Monoxide Method. Jour. Biol. Chem., 40:109, 1919.
Chang, H. C. and Harrop, G. A.: The Determination of the Circulat
ing Blood Volume with Carbon Monovide, Jour. Clin. Invest,
5:393, 1928,
Berlin, N. 1, Hyde, G. M., Parson, R. J., and Lawrence, H. H:
The Blood Volume in Various Medical and Surgical Conditions
NE, Jour. Med., 247:675, 1952.
Phillips, R. A. Van Slyke, D. D., Hamilton, P. V., Dole, V. P,
Emerson, K., Jr, and Archibald, R. M.: Measurement of Specific
Gravities of Whole Blood and Plasma by Standard Copper Sulfate
Solutions, Jour. Biol. Chem. 183:305, 1950,
Best, C. H. and Taylor, N. B.: The Physiological Basis of Medical
Practice. Seventh Edition, The Williams & Wilkins Co, Balt
more, 1961, p. 2.
Dameshek, Ws: A Method for the Simultaneous Examination of
Blood Platelets and Reticulocytes. Arch, Int. Med., 50:579, 1932.
Quick, A. J., Stanley-Brown, M., and Bancroft, F. Wa A Study of
the Coagulation Defect in Hemophiha and Jaundice. Am Jour.
Med. Sci, 190:501, 1935
Landau, A. Microsedimentation (Linzenmeier-Raunert method)
Am, J. Dis, Child. 45:691, 1933.
Kato, K. and Voncher, H. G.: The Prothrombin in the Blood of
Newborn Mature and Immature Infants as Determined by Micro
Prothrombin Test. JAMA, U4:749, 1040,
Dekkers, H. J, Nu Fate of Transiused Red Blood Cells Acta Med.
Scandinav., 9! 7, 1939.
Ashby, W.: Determination of Length of Life of Transfused Blood
Corpuscles in Man. J. Exper. Med., 29:267, 1919.
Vischer, A.: Uber die Lebensdauer der Erythrocyten, Beobachtungen
bei ‘Transfusionen mit Obalocytan blue. Zeschr. £ Min. med., 135:
133, 1938.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Developing ListeningDokument24 SeitenDeveloping ListeninggildejcaduNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Presentation On Health and HygieneDokument14 SeitenPresentation On Health and HygieneShekh Muhsen Uddin Ahmed100% (1)
- Reiki For Depression and Anxiety (Review) : Joyce J, Herbison GPDokument36 SeitenReiki For Depression and Anxiety (Review) : Joyce J, Herbison GPHenry CogoNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- DopeDokument30 SeitenDopeAlyssa NavarroNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Risk Based Inspection (RBI) - How To DoDokument44 SeitenRisk Based Inspection (RBI) - How To DoAna Marks100% (8)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Iron Ore TalingsDokument8 SeitenIron Ore TalingsUday BoddepalliNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- In The PhilippinesDokument9 SeitenIn The PhilippinesWilliam Buquia100% (2)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Leuven University Press - The Artistic Turn A Manifesto - 2013-08-08Dokument3 SeitenLeuven University Press - The Artistic Turn A Manifesto - 2013-08-08Lixo Electronico100% (1)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Blackbook AssignmentDokument6 SeitenBlackbook AssignmentAbhishek SureshNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Lethal in Disguise - The Health Consequences of Crowd-Control WeaponsDokument53 SeitenLethal in Disguise - The Health Consequences of Crowd-Control Weapons972 Magazine100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Models Relating Mixture Composition To The Density and Strength of Foam Concrete Using Response Surface Methodology - Nambiar & Ramamurthy 2006 PDFDokument9 SeitenModels Relating Mixture Composition To The Density and Strength of Foam Concrete Using Response Surface Methodology - Nambiar & Ramamurthy 2006 PDFalexnlima852Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Fidp FabmDokument5 SeitenFidp FabmEve Intapaya100% (1)
- MBA Liverpool Research Thesis, Gufran KhurshidDokument79 SeitenMBA Liverpool Research Thesis, Gufran KhurshidGufran KhurshidNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- On The Phenomenon of Burnout: The Lived Experiences of Teachers During The Current Global PandemicDokument7 SeitenOn The Phenomenon of Burnout: The Lived Experiences of Teachers During The Current Global PandemicPsychology and Education: A Multidisciplinary JournalNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Module 1.2 Engineering Data AnalysisDokument8 SeitenModule 1.2 Engineering Data AnalysisDirect XNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- 統計ch6 solutionDokument33 Seiten統計ch6 solutionH54094015張柏駿Noch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Agg Lika 2005Dokument3 SeitenAgg Lika 2005Georgia GiampoylakiNoch keine Bewertungen
- Midterm Study Guide & History of Rhetoric QuestionsDokument2 SeitenMidterm Study Guide & History of Rhetoric Questionsapi-262025468Noch keine Bewertungen
- EssayDokument1 SeiteEssaymanya bediNoch keine Bewertungen
- Water Security PlanDokument22 SeitenWater Security PlanMuzamil Maqbool RatherNoch keine Bewertungen
- Certified Human Resource Management Professional (CHRMP)Dokument9 SeitenCertified Human Resource Management Professional (CHRMP)Shamail AhmedNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- University of Birmingham Dissertation FormatDokument4 SeitenUniversity of Birmingham Dissertation FormatGhostWriterCollegePapersUK100% (1)
- MMS/M06 Management Training and Development Paper: HRM403 Time: Three Hours Maximum Marks: 70 All Questions Carry Equal MarksDokument4 SeitenMMS/M06 Management Training and Development Paper: HRM403 Time: Three Hours Maximum Marks: 70 All Questions Carry Equal Marksvikizza100% (1)
- Câu hỏi và đáp ánDokument2 SeitenCâu hỏi và đáp ánMai Trâm TốngNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Statexer#5Dokument6 SeitenStatexer#5Ghost31Noch keine Bewertungen
- CultiVitae Cover Letter W - Sample TemplateDokument3 SeitenCultiVitae Cover Letter W - Sample TemplateHafsoh larasatiNoch keine Bewertungen
- Schwartz and Weiss, 1978aDokument2 SeitenSchwartz and Weiss, 1978aAtika WulandariNoch keine Bewertungen
- The Meaning and Value of Supervision in Social Work Field EducationDokument18 SeitenThe Meaning and Value of Supervision in Social Work Field EducationmohammedNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)