Beruflich Dokumente
Kultur Dokumente
JMD PPH Critical Thinking Map-1
Hochgeladen von
api-417952873Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
JMD PPH Critical Thinking Map-1
Hochgeladen von
api-417952873Copyright:
Verfügbare Formate
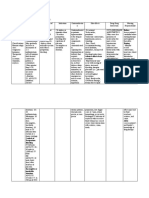
Priority Nursing Interventions (Basic Care & Comfort/ Safety &
Infection Control) (2.5 pts)
Name: Jeanine Diaz Critical Thinking Map Date: 6/10/2017
1. Message fundus until firm or have patient void.
Priority Assessments (Physiological Adaptation) (2.5
pts).
Concept: Post-Partum Hemorrhage 2. Initiate Oxytocin therapy if fundal message does not resolve
bleeding and if that does not work administer methergine and or
1. Assess for uterine atony by palpating fundus to Brief Pathophysiology (Physiological Adaptation) Hemabate.
check if firm or boggy, midline or deviated. Assess (2.5pts.) Post-Partum Hemorrhage (PPH) is blood loss greater
bladder for fullness and distention. Assess for any 3. Provide support to the patient and explain all procedures/answer
than 500ml in vaginal births, or more than 1000ml blood loss in any questions patient or family may have. Provide patient comfort
lacerations or hematomas. cesarean deliveries with a 10% decrease in H&H. It can occur as much as possible.
either early (within 24 hrs) or late (After 24hrs. -6 weeks
2. Assess amount of bleeding (saturating one pad in 15
postpartum). PPH can be caused by uterine atony, retained Medications (Pharmacological & Parenteral Therapies) (5pts)
minutes), clots (if any and the size), and for lochia that 1. Oxytocin 10 units IM if no IV access; 10-40 units in 1,000 cc
is sudden and massive or slow and steady. placental fragments, fibroids, lower genital track lacerations, and
crystalloid IV fluid (lactated Ringer’s solution or normal saline) SE:
subinvolution.
water intoxication causing confusion, drowsiness, and vomiting,
3. Assess vitals paying special attention to blood uterine cramping (desired), redness or irritation at injection site,
Priority Nursing Diagnosis (2.5pts.)
pressure and respirations (hypotension and tachypnea) runny nose, sinus pain or irritation. Contraindicted with
and skin for pale color or clammy feel. hypersensitivity.
1. Fluid volume deficient r/t blood loss secondary to uterine
Risk Factors (Health Promotion & atony, lacerations, retained placental fragments and 2. Methergine 0.1-0.2 mg IM q2-4 h followed by 0.2 mg PO q4-6
Maintenance/Reduction of Risk Potential) (1pt) coagulopathies AEB: decreased H&H, confusion, tachycardia and times 24 hours for 6 doses. SE: Dizziness, headache, tinnitus, nausea,
hypotension. vomiting, cramping (desired). Contraindicted in patients with current
1. Neonatal macrosomia: birth weight greater than elevation of BP, hypersensitivity.
4500, polydramnios, high parity. 2. Tissue perfusion: Ineffective r/t hypovolemia AEB: tachycardia
3. Hemabate 0.25mg(250 mcg) IM or directly into the uterus q 15-90
hypotension, pale and clammy skin. min; 8 doses maximum. SE: fever, diarrhea, vomiting. Contraindicted
2. Operative vaginal delivery, augmented or inducted in patients with asthma, hepatic, renal, and cardiac disease.
labor, prolonged first/second stage of labor. 3. Risk for bleeding r/t lack of information about signs of delayed
post-partum hemorrhage. Patient Teaching (Health Promotion &
3. Choriamniotitis, maternal obesity, congenital or
acquired coagulation defects. Maintenance/Safety & Infection Control/
Psychosocial Concerns (Psychosocial Integrity) (1 pt) Management of Care) (2.5 pt)
Potential & actual complications from treatments/
1. Anxiety due to fear and concern, fear of dying.
procedures (Physiological Adaptation/Reduction of 1. Teach patient signs and symptoms of PPH to report,
2. Depression and PTSD due to stressful situation and Risk Potential) (2pt) increased bleeding (blood changing back to bright red color),
traumatic birth process. 1. Complications from tamponade balloon include possible clots larger than a nickel, soaking a pad in less than 1 hr, fast
infection, perforation of uterus during placement, inflation and heartbeat, dizziness, and foul smelling lochia.
3. Negative memories of delivery and postpartum period. cervical trauma due to inflation and incorrect location.
Labs & Diagnostics (Reduction of Risk Potential) (2.5 pt) 2. Teach patient how to assess own fundus and report if
2. Complications from embolization of uterine artery include higher level than before or palpable beyond 7-10 days,
1. 10 % decrease in hemoglobin (11-13) and or hematocrit infection, amenorrhea, scare tissue formation and persistent pain tender, or has a fever.
(33-39%) post birth. lasting for months.
3. Teach patient how to perform fundal message in case of
2. Blood loss of more than 500ml for vaginal delivery or 3. Complications from hysterectomy include infection, bladder
greater than 1000ml for c-section (weigh pads and linens for
increased bleeding at home or boggy fundus. Also teach to
injury, bowel injury, hemorrhaging, blood clots, difficulty keep bladder empty and limit activity during initial
accurate blood loss (1ml blood =1 gram).
urinating and complications from anesthesia. postpartum weeks including driving.
3. Decreased platelets (150,000-400,000) and fibrinogen
(200-400).
Das könnte Ihnen auch gefallen
- Anaerobic Infections in HumansVon EverandAnaerobic Infections in HumansSydney FinegoldBewertung: 5 von 5 Sternen5/5 (1)
- NRN 202 Concept Map Patho-Altered Mental StatusDokument1 SeiteNRN 202 Concept Map Patho-Altered Mental StatusWendy Gilbert50% (2)
- Concept Map Critical CareDokument6 SeitenConcept Map Critical Careapi-498759347Noch keine Bewertungen
- CRITICAL CARE, March 2020Dokument47 SeitenCRITICAL CARE, March 2020Jonathan Yeoh100% (1)
- Nursing Care Plan Example NR450Dokument8 SeitenNursing Care Plan Example NR450J15Noch keine Bewertungen
- Neurologic Emergencies Stroke & Tia: Devin R. Harris, MD MHSC CCFP (Em)Dokument10 SeitenNeurologic Emergencies Stroke & Tia: Devin R. Harris, MD MHSC CCFP (Em)Samantha Lui100% (2)
- TraumaDokument10 SeitenTraumaNur Liyana Ahmad ZakiNoch keine Bewertungen
- NeuroVas Assessment.2Dokument2 SeitenNeuroVas Assessment.2ROxiie RakiztaNoch keine Bewertungen
- Foreign Body AspirationDokument3 SeitenForeign Body AspirationAsiya ZaidiNoch keine Bewertungen
- Bio 235 Midterm 1 NotesDokument53 SeitenBio 235 Midterm 1 NotesNita JosephNoch keine Bewertungen
- Wilkins 6 - Neurological Assessment - AssignmentDokument33 SeitenWilkins 6 - Neurological Assessment - AssignmentArifurRahman100% (1)
- Cns FormattedDokument59 SeitenCns FormattedbrihaspathiacademyNoch keine Bewertungen
- The Perioperative NursingDokument11 SeitenThe Perioperative NursingDa BondadNoch keine Bewertungen
- Bls HandoutDokument1 SeiteBls HandoutjeffNoch keine Bewertungen
- Chap.30 Med SurgDokument4 SeitenChap.30 Med SurgSheldon SloanNoch keine Bewertungen
- Nursing Memory Joggers PDFDokument2 SeitenNursing Memory Joggers PDFdummy damnNoch keine Bewertungen
- WWW Kenhub Com en Library Anatomy Endocrine SystemDokument20 SeitenWWW Kenhub Com en Library Anatomy Endocrine SystemIvana Odelia NainggolanNoch keine Bewertungen
- Uptake and Distribution of Volatile AnestheticsDokument22 SeitenUptake and Distribution of Volatile AnestheticsSuresh Kumar100% (3)
- Antibiotics - Classification & Mode of Action PDFDokument8 SeitenAntibiotics - Classification & Mode of Action PDFtarun paulNoch keine Bewertungen
- Anorectal Abscess: Principles of Internal Medicine, 18E. New York, Ny: Mcgraw-Hill 2012Dokument7 SeitenAnorectal Abscess: Principles of Internal Medicine, 18E. New York, Ny: Mcgraw-Hill 2012Irene SohNoch keine Bewertungen
- Nurse CertificationsDokument1 SeiteNurse CertificationsmirandasheaNoch keine Bewertungen
- NEURO2 1.02C Hemorrhagic Stroke - Dr. HiyadanDokument2 SeitenNEURO2 1.02C Hemorrhagic Stroke - Dr. HiyadanAra Diocos100% (1)
- Acute Cardiac AlterationsDokument38 SeitenAcute Cardiac AlterationsJoyce SiosonNoch keine Bewertungen
- Respiratory EmergenciesDokument21 SeitenRespiratory EmergenciesMohamed Anas SayedNoch keine Bewertungen
- Anasarca in The NICUDokument4 SeitenAnasarca in The NICUKarina Dwi SwastikaNoch keine Bewertungen
- NURS-FPX4010 - Maryam Maqsood - Assignment 2-1docxDokument8 SeitenNURS-FPX4010 - Maryam Maqsood - Assignment 2-1docxCaroline AdhiamboNoch keine Bewertungen
- Guillain Barre SyndromeDokument16 SeitenGuillain Barre SyndromeNeha Rathore100% (1)
- PICU BookDokument60 SeitenPICU BookJoão RosaNoch keine Bewertungen
- Fluid and ElectrolyteDokument2 SeitenFluid and Electrolytelilchibaby316150% (2)
- Management of Acute Metabolic Acidosis in The ICU Sodium BicarbonateDokument6 SeitenManagement of Acute Metabolic Acidosis in The ICU Sodium Bicarbonatecastillojess100% (1)
- W2 - MEDSURG Guidelines For Nursing Interventions On Coma PatientsDokument6 SeitenW2 - MEDSURG Guidelines For Nursing Interventions On Coma PatientsKyla L. Madjad100% (1)
- Sedative-Hypnotic Drugs - AMBOSSDokument8 SeitenSedative-Hypnotic Drugs - AMBOSSRuva Oscass JimmyNoch keine Bewertungen
- Brest Lump History TakingDokument3 SeitenBrest Lump History Takinganon_619577898Noch keine Bewertungen
- Word Part ReviewDokument6 SeitenWord Part ReviewRanee ToNoch keine Bewertungen
- Rayneilda Eleana Siew MLT U29 Unit Makmal Patologi Hospital Nukleus WP LabuanDokument17 SeitenRayneilda Eleana Siew MLT U29 Unit Makmal Patologi Hospital Nukleus WP LabuanValentine Brokenz Saintz100% (1)
- Psychiatric Nursing Notes: Psych MedsDokument59 SeitenPsychiatric Nursing Notes: Psych Medssurviving nursing schoolNoch keine Bewertungen
- TMS Lecture2Dokument33 SeitenTMS Lecture2ANTolaniNoch keine Bewertungen
- Pneumothorax: DR - Naveen Vennilavan R Pg-IiiDokument95 SeitenPneumothorax: DR - Naveen Vennilavan R Pg-Iiinaveen vennilavanNoch keine Bewertungen
- Chapter19-Birds NotesDokument8 SeitenChapter19-Birds Notesapi-195601294100% (1)
- Cardiology Flash Cards (EKG in A Nut Shell)Dokument62 SeitenCardiology Flash Cards (EKG in A Nut Shell)Nabeel Kouka, MD, DO, MBA, MPHNoch keine Bewertungen
- Acute Otitis Media: Jama Patient PageDokument1 SeiteAcute Otitis Media: Jama Patient PageS. JohnNoch keine Bewertungen
- Evidence-Based Prevention of Pressure Ulcers in The Intensive Care UnitDokument12 SeitenEvidence-Based Prevention of Pressure Ulcers in The Intensive Care Unitxxi_thNoch keine Bewertungen
- Pediatric Critical Care MedicineDokument107 SeitenPediatric Critical Care Medicinerahmawatusayu100% (1)
- Cns LectureDokument10 SeitenCns Lectureferg jeanNoch keine Bewertungen
- FilariasisDokument8 SeitenFilariasisTheeya QuigaoNoch keine Bewertungen
- CA2 Midterms Pharmacology-Part-1-Reviewer-2-colums PDFDokument8 SeitenCA2 Midterms Pharmacology-Part-1-Reviewer-2-colums PDFGensen Cu RoxasNoch keine Bewertungen
- Patient Assessment Marking SheetDokument2 SeitenPatient Assessment Marking SheetJim Courtney100% (4)
- Operating Room Attire 2018Dokument5 SeitenOperating Room Attire 2018andrea rabangNoch keine Bewertungen
- Hypersensitivity Nursing Students (BSC Nursing)Dokument25 SeitenHypersensitivity Nursing Students (BSC Nursing)Ikramul Hussain KhanNoch keine Bewertungen
- ICU DrugsDokument1 SeiteICU DrugsMimiNoch keine Bewertungen
- Safety Unfolding Nursing Case StudyDokument3 SeitenSafety Unfolding Nursing Case StudyclarimerNoch keine Bewertungen
- Journal Herpes Simplex EncephalitisDokument2 SeitenJournal Herpes Simplex EncephalitissavinaumarNoch keine Bewertungen
- Module 9 Student Activity SheetDokument6 SeitenModule 9 Student Activity SheetJenny Agustin FabrosNoch keine Bewertungen
- Ob2 Sas 13Dokument8 SeitenOb2 Sas 13Ralph Louie ManagoNoch keine Bewertungen
- OxytocinDokument2 SeitenOxytocinshefawNoch keine Bewertungen
- Oxytocin Induction or Stimulation of Labor BeforeDokument4 SeitenOxytocin Induction or Stimulation of Labor BeforeIrene Grace BalcuevaNoch keine Bewertungen
- Flowchart 1 Immediate Management of An AsphyxiatednewbornDokument3 SeitenFlowchart 1 Immediate Management of An Asphyxiatednewborndessy pratiwiNoch keine Bewertungen
- Postpartum ComplicationsDokument30 SeitenPostpartum ComplicationsOshNoch keine Bewertungen
- Postpartum ComplicationsDokument30 SeitenPostpartum ComplicationsJen Rhae LimNoch keine Bewertungen
- Drug Study OxytocinDokument3 SeitenDrug Study OxytocinSheena Marie M. TarleNoch keine Bewertungen
- Jeanine MDokument2 SeitenJeanine Mapi-417952873Noch keine Bewertungen
- Running Head: DISCHARGE PLAN 1Dokument11 SeitenRunning Head: DISCHARGE PLAN 1api-417952873Noch keine Bewertungen
- Nur 342 Goals Objectives WorksheetDokument2 SeitenNur 342 Goals Objectives Worksheetapi-417952873100% (3)
- Diaz Poster Presentation 1Dokument1 SeiteDiaz Poster Presentation 1api-417952873Noch keine Bewertungen
- Allentown EpidemiologyDokument14 SeitenAllentown Epidemiologyapi-417952873Noch keine Bewertungen
- CT and MR Angiography of The Peripheral Circulation - 1841846066 PDFDokument350 SeitenCT and MR Angiography of The Peripheral Circulation - 1841846066 PDFDididNoch keine Bewertungen
- Nursing Diagnosis: Risk For Deficient Fluid Volume R/T Traumatic InjuryDokument2 SeitenNursing Diagnosis: Risk For Deficient Fluid Volume R/T Traumatic Injuryarreane yookNoch keine Bewertungen
- M G University M.SC Applied Microbiology SyllabusDokument52 SeitenM G University M.SC Applied Microbiology SyllabusHermann AtangaNoch keine Bewertungen
- 07 04 2013 PDFDokument134 Seiten07 04 2013 PDFebrandeNoch keine Bewertungen
- (SGD) PathologyDokument6 Seiten(SGD) PathologyPaulene RiveraNoch keine Bewertungen
- Sally Aburumman Bushra SaleemDokument75 SeitenSally Aburumman Bushra SaleemAbdulrahman AlsayyedNoch keine Bewertungen
- Narcolepsy - Pathophysiology, Diagnosis and Treatment (Ed. Baumann, Bassetti, Scammell)Dokument416 SeitenNarcolepsy - Pathophysiology, Diagnosis and Treatment (Ed. Baumann, Bassetti, Scammell)kittygotclaws100% (1)
- Part I: Medical Microbiology Part II: Medical ParasitologyDokument36 SeitenPart I: Medical Microbiology Part II: Medical ParasitologyRamakrishna ShanbhogeNoch keine Bewertungen
- Module 6 IPM & Harmful Effect of Chemical Pesticides.Dokument6 SeitenModule 6 IPM & Harmful Effect of Chemical Pesticides.Nikhil BijuNoch keine Bewertungen
- Medical Terminology For Health Professions 7th Edition Ehrlich Test BankDokument26 SeitenMedical Terminology For Health Professions 7th Edition Ehrlich Test BankGregorySimpsonmaos100% (46)
- Septic ArthritisDokument5 SeitenSeptic ArthritisAtiqahNoch keine Bewertungen
- Chemical Safety TrainingDokument229 SeitenChemical Safety TrainingOmprakaash MokideNoch keine Bewertungen
- Sr. No. Cghs Treatment Procedure/Investigation List Non-NABH/Non - NABL Rates Nabh/Nabl RatesDokument49 SeitenSr. No. Cghs Treatment Procedure/Investigation List Non-NABH/Non - NABL Rates Nabh/Nabl RatesADDECC INFO INDIANoch keine Bewertungen
- 1 s2.0 S2772594422001637 MainDokument5 Seiten1 s2.0 S2772594422001637 MainCatarina CourasNoch keine Bewertungen
- Chapter 17 Unit IDokument23 SeitenChapter 17 Unit IGlory MimiNoch keine Bewertungen
- Cardiovascular SystemDokument9 SeitenCardiovascular SystemMayim LouiseNoch keine Bewertungen
- Unilag MSC FINANCE Past Questions PDFDokument2 SeitenUnilag MSC FINANCE Past Questions PDFbdianNoch keine Bewertungen
- Ictal and Postictal Psychiatric Disturbances - TrimbleDokument5 SeitenIctal and Postictal Psychiatric Disturbances - Trimblegoo99Noch keine Bewertungen
- 2021-05-15 New ScientistDokument62 Seiten2021-05-15 New ScientistAgenor Phillips100% (1)
- Video Recap of Mutations by Amoeba SistersDokument2 SeitenVideo Recap of Mutations by Amoeba Sistersapi-233187566Noch keine Bewertungen
- Acute Asthma Paed WaniDokument16 SeitenAcute Asthma Paed WaniNurul Syazwani RamliNoch keine Bewertungen
- Alternaria Species Causing Leaf Spot On Hemp (Cannabis Sativa) in Northern ChinaDokument14 SeitenAlternaria Species Causing Leaf Spot On Hemp (Cannabis Sativa) in Northern ChinaEsa PaundraNoch keine Bewertungen
- The Science of Sleep: A Brief Guide On How To Sleep Better Every NightDokument2 SeitenThe Science of Sleep: A Brief Guide On How To Sleep Better Every NightMark Anthony RaymundoNoch keine Bewertungen
- Life Expectancy Powerpoint PresentationDokument6 SeitenLife Expectancy Powerpoint PresentationAlejandro MendozaNoch keine Bewertungen
- Hemophilia and Its Treatment: Brief ReviewDokument7 SeitenHemophilia and Its Treatment: Brief ReviewSalsa BillaNoch keine Bewertungen
- Child Obesity Prevention Lit ReviewDokument28 SeitenChild Obesity Prevention Lit ReviewAisyahNurjannahNoch keine Bewertungen
- General Nursing Science 1 2020 PDFDokument95 SeitenGeneral Nursing Science 1 2020 PDFRicardo DomingosNoch keine Bewertungen
- Proteinuria A Guide To Diagnosis and AssDokument7 SeitenProteinuria A Guide To Diagnosis and AssMarcelliaNoch keine Bewertungen
- CBSE Class 11 English Sample Paper Set 5Dokument8 SeitenCBSE Class 11 English Sample Paper Set 5Shantam BasuNoch keine Bewertungen
- Derma OSCEDokument3 SeitenDerma OSCEUsama El BazNoch keine Bewertungen