Beruflich Dokumente
Kultur Dokumente
PAMI Pain Mangement and Dosing Guide 02282017
Hochgeladen von
HawsinCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
PAMI Pain Mangement and Dosing Guide 02282017
Hochgeladen von
HawsinCopyright:
Verfügbare Formate
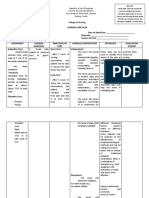
Pain Management
and Dosing Guide
Updated November 2016
Pain Management and Dosing Guide Includes:
1. Principles of Pain Management, Discharge and Patient Safety
http://pami.emergency.med.jax.ufl.edu/ Considerations, Analgesic Ladder
https://goo.gl/4Yh1cB 2. Non-opioid Analgesics, Opioid Prescribing Guidelines and
Equianalgesic Chart, Opioid Cross-Sensitivities, Intranasal
Medications
Send your feedback on all PAMI materials and how you 3. Nerve Blocks, Neuropathic Pain Medications, Muscle Relaxer
use them to improve patient safety and clinical care. Medications, Ketamine Indications
If you would like to adapt this guide for your 4. Topical and Transdermal Medications
institution or have recommendations contact PAMI at
emresearch@jax.ufl.edu or 904-244-4986. 5. Procedural Sedation and Analgesia (PSA) Medications
6. Stepwise Approach to Pain Management and PSA
Disclaimer
The PAMI dosing guide, website, learning modules, and resources are for educational and informational purposes only and are not intended as a substitute for professional medical diagnosis or management
by a qualified health care professional. PAMI is not responsible for any legal action taken by a person or organization as a result of information contained in or accessed through this website or guide whether
such information is provided by PAMI or by a third party. As new research and clinical experience becomes available, patient safety standards will change. Therefore, it is strongly recommended that
physicians, nurses and other healthcare professionals remain current on medical literature and national standards of care and structure their treatment accordingly. As a result of ongoing medical advances
and developments, information on this site is provided on an “as is” and “as available” basis. Patient care must be individualized. The use of information obtained or downloaded from or through this website,
module, or product is at the user’s sole discretion and risk.
Funding provided by Florida Medical Malpractice Joint Underwriting Association (FMMJUA) and University of Florida College of Medicine-Jacksonville, Department of Emergency Medicine
Principles of Pain Management Pain Management Considerations Analgesic Ladder and Treatment Basics
• Type of pain: nociceptive, neuropathic, inflammatory
Establish realistic pain goals • Acute vs. chronic vs. acute on chronic pain exacerbation Step 3: Severe Pain
Will vary depending on patient and type of • Pain medication history: OTC, Rx and herbal Step 1 and Step 2 Strategies +/- Scheduled
• Patient factors: genetics, culture, age, previous Opioid Analgesics
pain - goal of zero may not be feasible
pain experiences, comorbidities
• Verify dosing for < 6 mo and > 65 yo
Treatment Options
Educate patient/caregivers on pain • Pharmacotherapy: systemic, topical, transdermal - Step 2: Moderate Pain
management goals and regimen nerve blocks Step 1 Strategy + Intermittent Dose of Opioid
• Non-pharmacologic modalities Analgesics (PO, IV) +/-
• Refer to pain, palliative or other specialists for Interventional (Blocks & Procedures)
advanced treatment
Consider pharmacologic and Non-pharmacological modalities
non-pharmacologic treatment options and Splinting, distraction, hot/cold therapy, Step 1: Mild Pain
initiate therapy exercise, massage, imagery, and others Non-opioid Analgesic (APAP, NSAIDs, COX-2
Inhibitors) +/- Local/Topical Anesthetics
Discharge and Patient Safety Considerations
• Assess and counsel regarding falls, driving, work
safety, and medication interactions Ladder Basics
Continually reassess patient’s pain • Bowel regimen for opioid induced constipation 1. Use oral route when possible
and monitor for medication efficacy and • Vital signs and oral intake before discharge 2. Give analgesics at regular intervals
side effects • Document all pain medications administered and 3. Prescribe according to pain intensity
response at time of discharge or disposition
• Use same scale to reassess pain • Consider OTC and non-pharmacologic options
4. Dosing must be adapted to individual
• Use scale that is age and cognitively appropriate • Can patient implement pain management plan? 5. Analgesic plan must be refined and
• If no improvement, adjust regimen - insurance coverage, transportation, etc. communicated with patient and staff
Non-Opioid Analgesics* Opioid Prescribing Guidelines and Equianalgesic Chart
Generic Adult Pediatric Onset (O) and Approximate Recommended STARTING Recommended STARTING
(Brand) (<12 yo) Generic (Brand) Duration (D) Equianalgesic Dose dose for ADULTS dose for CHILDREN (> 6 mo)
Acetaminophen 325-650 mg 15 mg/kg Oral IV Oral IV Oral IV Oral IV
(Tylenol®) Max:PO q 4-6 h PO q 4-6 h
4 g/d or 1 q 4 h Max: 90 mg/kg/d O: 30-60 min O: 5-10 min 15-30 mg 2-10 mg 0.3 mg/kg 0.1 mg/kg
Morphine (MSIR®) [CII] D: 3-6 h D: 3-6 h 30 mg 10 mg q 2-4 h q 2-4 h q4h q 2-4 h
Acetaminophen <50 kg
1 g IV q 6 h 15 mg/kg IV q 6 h Morphine extended release O: 30-90 min 15-30 mg 0.3-0.6 mg/kg
IV (Ofirmev®) Max: — 30 mg 10 mg — —
Use only if not mg q 44 g/d or 650 or 12.5 mg/kg (MS Contin®) [CII] D: 8-12 h q 12 h q 12 h
tolerating PO h prn pain IV q 4 h prn pain
Max: 75mg/kg/d Hydromorphone (Dilaudid®) [CII] O: D:
15-30 min O: 15 min
4-6 h D: 4-6 h 7.5 mg 1.5 mg 2-4 mg
q4h
0.5-2 mg
q 2-4 h
0.06 mg/kg
q4h
0.015 mg/kg
q4h
Celecoxib 100-200 mg >2 yo Hydrocodone/APAP 325 mg
(Celebrex®) PO daily to q 12 h
Max: 400 mg/d 50 mg PO BID (Norco 5, 7.5, 10®) [CII] O: 30-60 min — 30 mg — 5-10 mg — 0.1-0.2 mg/kg —
Hycet (7.5 mg/325 mg per 15 mL) D: 4-6 h q6h q 4-6 h
400-800 mg 10 mg/kg
Ibuprofen PO q 6 to 8 h Fentanyl [CII] Transdermal Transdermal Transdermal 1-2 mcg/kg
(Motrin®) PO q 6 to 8 h Max: 40 mg/kg/d O: 12-24 h O: immediate 100 mcg 50 mcg
Max: 3200 mg/d or 2400 (Sublimaze® Duragesic®) D: 72 h per D: 30-60 min — (0.1 mg) 12-25 mcg/h q 1-2 h 12-25 mcg/h q 1-2 h
mg/d Patch for opioid tolerant patients ONLY q 72 h q 72 h (max 50 mcg/dose)
patch
1-2 mg/kg O: 30-60 min
25-50 mg PO q 6 to 12 h Methadone (Dolophine®) [CII] D: >8 h — Variable Variable 5-10 mg — 0.7 mg/kg/d PO/SC/IM/IV divided
Indomethacin PO q 6 to 12 h >6 mo Opioid tolerant patients ONLY q 8-12 h q 4-6 h prn severe chronic pain
(Indocin®) (chronic use)
Max: 200 mg/d Max: 4 mg/kg/d
or 200 mg/d Oxycodone 5, 15, 30 mg (Roxicodone®), 5-10 mg q 6 h
Oxycodone 5, 7.5, 10 mg/ APAP 325 mg O: 10-15 min — 20-30 mg — — 0.05-0.15 mg/kg —
15-30 mg IV/IM 0.5-1
dose
mg/kg/
IM/IV
(Percocet®), D: 4-6 h ER 10 mg q 12 h q 4-6 h
Ketorolac† q6h ER=Oxycontin® [CII]
(Toradol®) q 6 h
Max: 120 mg/d Max: 15-30 mg O: 1 h 50-100 mg q 6 h
x5d Tramadol (Ultram®) [CIV] D: 3-6 h — 300 mg — Max: 400 mg/d — — —
q6hx5d
Naproxen 250-500 mg PO
q 8 to 12 h
5 mg/kg PO
q 12 h Codeine * 15, 30, 60 mg/APAP O: 1-2 h
D: 4-6 h — 200 mg — 30-60 mg
q4h — — —
(Naprosyn®) Max: 1500 mg/d Max: 1000 mg/d 300 mg
Meloxicam 7.5-15 mg PO daily *Codeine is often ineffective. Use for cough and cold is contraindicated in children. Not recommended for < 12 yo or 12-18 yo with respiratory condition or nursing mothers.
(Mobic®) Max: 15 mg/d — Opioid Cross-Sensitivities Intranasal Medications*
*Doses can be scheduled or PRN pain. Avoid NSAIDs in renal Phenanthrenes (related to morphine): morphine, Generic Dose Max Dose Comments
dysfunction, PUD, CHF, and if < 6 mo of age. Use with caution codeine, oxycodone, hydrocodone, hydromorphone
in elderly patients. Phenylpiperidines (related to meperidine): Fentanyl 1.5-2 mcg/kg q 1-2 h
3 mcg/kg or 100 mcg Divide dose equally between each nostril
†For patients < 65 yo, 60 mg IM or 30 mg IV x 1, followed by 30 meperidine, fentanyl 10 mg or 1 mL per
mg IV/IM q 6 h PRN up to a max daily dose of 120 mg for 5 days. Midazolam 5 mg/mL 0.3 mg/kg nostril (total 2 mL) Divide dose equally between each nostril
Risk of cross-sensitivity in patients with allergies is
For patients >65 yo, <50 kg, and/or with renal impairment, 30 greater when medications from the same opioid Ketamine+ 0.5-1.0 mg/kg Large range Limited data Use with caution until further studied
mg IM or 15 mg IV x 1, followed by 15 mg IV/IM q 6h PRN up to
a max daily dose of 60 mg for 5 days. family are administered. *Use the MOST concentrated form available with an atomizer. + Dosing not well established. Studies have used 0.5-9 mg/kg.
NERVE BLOCKS Neuropathic Pain Medications
Type of Block General Distribution of Anesthesia Generic (Brand) Beginning Dose Max Dose
Gabapentin* (Neurontin®) 300 mg PO QHS to TID 3600 mg/d
Interscalene Plexus Block Shoulder, upper arm, elbow and forearm
Pregabalin* (Lyrica®) 50 mg PO TID 300 mg/d**
Supraclavicular Plexus Block Upper arm, elbow, wrist and hand
SNRIs: Duloxetine (Cymbalta®) 30 mg PO daily† 60 mg/d**
Infraclavicular Plexus Block Upper arm, elbow, wrist and hand Venlafaxine ER (Effexor XR®) 37.5 mg PO daily 225 mg/d
Axillary Plexus Block Forearm, wrist and hand. Elbow if including musculocutaneous nerve TCAS: Amitriptyline (Elavil®) 25 mg PO QHS 200 mg/d
Median Nerve Block Hand and Forearm Nortriptyline (Pamelor®) 25 mg PO QHS 150 mg/d
†30 mg daily for at least 7 days to decrease nausea
Radial Nerve Block Hand and Forearm *Requires dose adjustment based on renal function **Varies depending on indication
Ulnar Nerve Block Hand and Forearm
Muscle Relaxer Pain Medications
Femoral Nerve Block Anterior thigh, femur, knee and skin over the medial aspect below the knee
Generic (Brand) Beginning Dose Max Dose
Popliteal Nerve Block Foot and ankle and skin over the posterior lateral portion, distal to the knee Baclofen (Lioresal®) 5 mg PO TID 80 mg/d
Tibial Block Foot and ankle Cyclobenzaprine
5 mg PO TID 30 mg/d
Deep Peroneal Block Foot (Flexeril®)
Saphenous Nerve Block Foot Methocarbamol 1-1.5 g PO TID to 4x/day x 48-72 h,
8 g/d
(Robaxin®) then 500-750 mg PO TID to 4x/day
Sural Nerve Block Foot
Adult: 2-10mg PO TID-QID;
5-10mg IV/IM Ped: 0.6 mg/
Max Dose Max Dose Diazepam
Duration Duration Ped: (6-12yo): 0.12-0.8 mg/kg/day PO kg/8h IV/IM to
(Valium®)
Local Anesthetics† Onset without Epi, with Epi, divided q 6-8 h; 0.04-0.2 mg/kg IV/IM adult max
without Epi (h) with Epi (h)
mg/kg mg/kg q 2-4 h prn;
Lidocaine (1%) Rapid 0.5–2 1–6 4.5 (300 mg) 7 (500 mg)
Ketamine (Ketalar®) Indications
Bupivicaine (0.5%)* Slow 2-4 4-8 2.5 3 Indications Starting Dose
Mepivicaine (1.5%) Rapid 2-3 2-6 5 7 IV: Adult 0.5-1.0 mg/kg, Ped 1-2mg/kg;
Procedural Sedation IM: 4-5 mg/kg
2-Chloroprocaine (3%) Rapid 0.5-1 1.5-2 10 15 IV: 0.1 to 0.3 mg/kg, max initial dose ≤ 10 mg
Sub-dissociative Analgesia
Ropivicaine (0.5%) Medium 3 6 2-3 2-3 IM: 0.5-1.0 mg/kg; IN*: 0.5-1.0 mg/kg
*Most cardiotoxic †1% = 10mg/ml, 0.5% = 5mg/ml Excited Delirium Syndrome IV: 1 mg/kg; IM: 4‐5 mg/kg
*Dosing not well established. Studies have used 0.5-9 mg/kg.
Topical and Transdermal Medications*
Generic (Brand) Indications Onset (O) and Recommended STARTING Recommended STARTING Maximum Dose
Duration (D) dose for ADULTS dose for CHILDREN
Diclofenac sodium 1.5%, 2% w/w 1.5% soln: 40 drops QID 1.5% soln: 40 drops QID
topical solution (Pennsaid) 2% soln: 2 pumps (40mg) BID 2% soln: 2 pumps (40mg) BID
Osteoarthritis Variable to affected knee — 1% gel (2g): 8 g/d to single joint of upper
extremity; 1% (4g): 16 g/d to single joint of
1% gel (Voltaren gel) 1% gel: 2 or 4g QID lower extremity
Diclofenac epolamine 1.3% patch Acute pain from sprains, Variable 1 patch (180 mg) BID — 1 patch BID
(Flector patch) strains, contusion
Lidocaine 5% patch Postherpetic neuralgia Variable 1-3 patches applied once daily, — 3 patches in a 12 h period per day
(Lidoderm patch) remove after 12 h
Fentanyl (Duragesic®) Persistent moderate to severe O: 12-24 h 12-25 mcg/h q 72 h Variable
chronic pain D: 72 h per patch
Capsaicin cream (Theragen®, Zostrix®, Apply a thin layer to the >12 yo: Apply a thin layer to
Salonpas) Exists as several OTC formulations Strains, sprains, backache or
arthritis Variable affected area and gently the affected area and gently Up to QID
in combination with camphor and menthol massage up to QID massage up to QID
Minor cuts, scrapes, burns, Externally 3-4 times per day. Apply in area less
Lidocaine 4% (L.M.X.4®) sunburn, insect bites, and minor O: 20-30 min Apply externally than 100cm2 for children less than 10kg. Apply
skin irritations D: 60 min in area less than 600cm2 for children between
10 and 20kg
LET (Lidocaine Epinephrine Tetracaine) O: 10 min Topical 3 mL
(gel or liquid) Wound repair (non-mucosal) D: 30-60 min 4% Lidocaine, 1:2,000 Epinephrine, 0.5% Tetracaine (not to exceed maximal Lidocaine
dosage of 3-5 mg/kg)
EMLA (2.5% Lidocaine 2.5% Prilocaine) O: 60 min 3-12 mo (>5 kg): 2 gm 3-12 mo max area 20cm2
Cover with occlusive dressing Dermal analgesic (intact skin) D: 3-4 h 20 gm 1-6 yo (>10kg): 10 gm 1-6 yo max area 100cm2
Maximum application time 4 hours 7-12 yo (>20kg): 20 gm 7-12 yo max area 200cm2
Pain-Ease® Cooling intact skin and mucus O: immediate Spray for 4-10 sec from distance
Vapocoolant/Skin Refrigerant membranes and minor open D: few sec to — of 8-18 cm. Stop when skin turns white to avoid frostbite
wounds 1 min Not recommended for < 3 yo
Foley catheter and nasogastric O: 2-5 min 2% topical gel/jelly, 5% topical ointment, 2% oropharyngeal
Lidocaine tube insertion; intubation; nasal D: 30-60 min viscous topical solution 3-5 mg/kg
packing; gingivostomatitis
*Dosages are guidelines to avoid systemic toxicity in patients with normal intact skin and with normal renal and hepatic function
Stepwise Approach to Pain Management
Procedural Sedation and Analgesia Medications
and Procedural Sedation Analgesia (PSA)
Generic (Brand) Adult Pediatric Comments http://pami.emergency.med.jax.ufl.edu/resources/
educational-materials/procedural-sedation/
>3 mo: IV 1-2 mg/kg; Risk of laryngospasm increases with active upper respiratory
Ketamine IV 0.5-1.0 mg/kg additional doses 0.5 mg/kg infection and procedures involving posterior pharynx; vomiting 1. Situation Checkpoint
(Ketalar®) IM 4-5 mg/kg IV q 10-15 min prn; common - consider premedication with Ondansetron (Zofran).
IM 4 - 5 mg/kg Not recommended in patients <3 mo. What are you trying to accomplish?:
IV 0.05-0.1 mg/kg analgesia, anxiety, sedation, procedure, etc.
Midazolam IV 0.05-0.1 mg/kg Initial max dose 2 mg. Max total dose in >60 yo is 0.1 mg/kg
IN 0.2-0.3 mg/kg
(Versed®) IV slow push over 1-2 min Decrease dose by 33-50% when given with opioid
(IN max 10 mg) 2. Developmental/Cognitive Checkpoint
IV 0.5-1 mg/kg slow push What is the patient’s development stage?
Propofol IV 1 mg/kg slow push (1-2 min); Risk of apnea, hypoventilation, respiratory depression, rapid changes
(1-2 min); additional doses 0.5
(Diprivan®) additional doses 0.5 mg/kg in sedative depth, hypotension; provides no analgesia
mg/kg
3. Family Dynamic Checkpoint
Risk of myoclonus (premedication w/ benzo or opioid can decrease),
Etomidate Who is caring for the patient?
IV 0.1 - 0.2mg/kg; additional doses 0.05mg/kg pain with injection, nausea and vomiting, risk of adrenal suppression;
(Amidate®)
provides no analgesia What are the family dynamics?
IV ketamine 0.75 mg/kg +
propofol 0.75 mg/kg. Additional 4. Facility Checkpoint
Ketamine + Propofol — See ketamine and propofol comments respectively
doses: ketamine 0.5 mg/kg, Type of staffing and setting, team
propofol 0.5-1 mg/kg
experience, facility policies, etc.
IV 1 mcg/kg loading dose (over IV 0.5–2 mcg/kg loading dose
Dexme-
10 min) followed by 0.5 to 2 mcg/ (over 10 min) followed by 0.5 to Risk of bradycardia, hypotension, especially with loading dose or 5. Patient Assessment Checkpoint
detomidine
kg/h continuous infusion. Use 2 mcg/kg/h continuous infusion rapid infusions, apnea, bronchospasm, respiratory depression
(Precedex®) Review patient’s risk factors and history.
0.5 mcg/kg for geriatric patients IN 2-3 mcg/kg
Do not use if acute asthma exacerbation, suspected pneumothorax/other
Nitrous oxide — 50% N2O/50% O2 inhaled 6. Management Checkpoint
trapped air or head injury with altered level of consciousness
Monitor mental status, hemodynamics, and histamine release. Requires Choose your “ingredients” for pharmacologic
IV 0.05-.0.1 mg/kg or IV 0.1-0.2 mg/kg,
longer recovery time than fentanyl. Difficult to titrate during procedural and non-pharmacologic “recipe.”
Morphine sedation due to slower onset and longer duration of action. Reduce
5-10 mg titrated to effect
dosing when combined with benzodiazepines (combination increases risk
of respiratory compromise) 7. Monitoring & Discharge Checkpoint
100 times more potent than morphine; Rapid bolus infusion may Joint Commission standards, reassessments,
Fentanyl IV 0.5-1 mcg/kg
1-3 yo: 2 mcg/kg; lead to chest wall rigidity. Reduce dosing when combined with facility policies, discharge and transportation
3-12 yo 1-2 mcg/kg benzodiazepines and in elderly. Preferred agent due to rapid onset considerations.
and short duration.
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Symptom Management Guidelines: ORAL MUCOSITIS: Focused Health AssessmentDokument11 SeitenSymptom Management Guidelines: ORAL MUCOSITIS: Focused Health AssessmentVincent Paul SantosNoch keine Bewertungen
- Penanganan Nyeri Kanker Dengan OksikodonDokument26 SeitenPenanganan Nyeri Kanker Dengan OksikodonMuhammad ArifNoch keine Bewertungen
- APM 21 1989 FinalDokument15 SeitenAPM 21 1989 FinalRuben HerediaNoch keine Bewertungen
- Dave Parth YogeshbhaiDokument97 SeitenDave Parth YogeshbhaiMaharshi PandyaNoch keine Bewertungen
- End of Life Care PPPDokument43 SeitenEnd of Life Care PPPElaine SUNoch keine Bewertungen
- Literature Review of Momordica CharantiaDokument7 SeitenLiterature Review of Momordica Charantiavvomvqwgf100% (1)
- Greyhounds Pain ManagementDokument5 SeitenGreyhounds Pain ManagementPeterNoch keine Bewertungen
- Jur Nista TabDokument17 SeitenJur Nista Tabnela sharonNoch keine Bewertungen
- Republic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteDokument6 SeitenRepublic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteYellowNoch keine Bewertungen
- Acute Pain Management - Scientific Evidence - Third Edition PDFDokument540 SeitenAcute Pain Management - Scientific Evidence - Third Edition PDFCharity Clarke100% (1)
- PARACETAMOLDokument8 SeitenPARACETAMOLRayhan Amin 2212830042Noch keine Bewertungen
- The Use of Medical Cannabis To Treat Post Traumatic Stress DisorderDokument15 SeitenThe Use of Medical Cannabis To Treat Post Traumatic Stress DisorderRay SternNoch keine Bewertungen
- Dolor CVNADokument15 SeitenDolor CVNAStephania MendozaNoch keine Bewertungen
- The Preoperative EvaluationDokument25 SeitenThe Preoperative Evaluationnormie littlemonsterNoch keine Bewertungen
- Precision Med PPT ExplainationDokument2 SeitenPrecision Med PPT ExplainationSeemron BiswalNoch keine Bewertungen
- Chemical BurnDokument14 SeitenChemical BurnSyidah RoslanNoch keine Bewertungen
- Essential Notes in Pain Medicine Oxford Speciality Training Rev Notes Sep 14 2022 - 0198799446 - Oxford University Press Enrique Collantes Celador Full ChapterDokument68 SeitenEssential Notes in Pain Medicine Oxford Speciality Training Rev Notes Sep 14 2022 - 0198799446 - Oxford University Press Enrique Collantes Celador Full Chaptermargaret.jones429100% (4)
- Nature's First "Atypical Opioids": Kratom and Mitragynines.Dokument5 SeitenNature's First "Atypical Opioids": Kratom and Mitragynines.Anonymous kdfP21Noch keine Bewertungen
- Chapter 18Dokument11 SeitenChapter 18missy23pap100% (1)
- Askep HivDokument17 SeitenAskep Hivputri d dianiNoch keine Bewertungen
- Pathophysiology of OsteoarthritisDokument41 SeitenPathophysiology of OsteoarthritisghaziaNoch keine Bewertungen
- Pain Management After Complex Spine Surgery A.10Dokument10 SeitenPain Management After Complex Spine Surgery A.10Ahida VelazquezNoch keine Bewertungen
- Drug Cards CNSDokument23 SeitenDrug Cards CNSChristine Schroeder100% (2)
- Pharmacologic Therapy For Acute PainDokument11 SeitenPharmacologic Therapy For Acute PainDiana Florez100% (1)
- Pain ManagementDokument18 SeitenPain ManagementEimhie Lee CasiNoch keine Bewertungen
- Anesthetic Management For Laparoscopic CholecystectomyDokument6 SeitenAnesthetic Management For Laparoscopic CholecystectomyibunqumairaNoch keine Bewertungen
- Management of Pain Associated With The Insertion of Intrauterine ContraceptivesDokument9 SeitenManagement of Pain Associated With The Insertion of Intrauterine ContraceptivesLeonardo Daniel MendesNoch keine Bewertungen
- Purity of OsteoarthritisDokument31 SeitenPurity of OsteoarthritisZeeshan IslamNoch keine Bewertungen
- Medical Surgical Nursing ExamsDokument4 SeitenMedical Surgical Nursing ExamsRoanne LaguaNoch keine Bewertungen
- PT - Mapeh 6 - Q4Dokument6 SeitenPT - Mapeh 6 - Q4Michelle AcostaNoch keine Bewertungen