Beruflich Dokumente
Kultur Dokumente
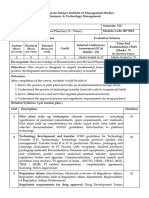
Five Content Areas and Percent of Scored Test Items (Range) in Each Area
Hochgeladen von
সোমনাথ মহাপাত্রOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Five Content Areas and Percent of Scored Test Items (Range) in Each Area
Hochgeladen von
সোমনাথ মহাপাত্রCopyright:
Verfügbare Formate
Five Content Areas and Percent of Scored Test Items (Range) in Each Area
This table shows the percent of scored test questions that are included in each major content area.
Percent of Scored Test
Five Content Areas
Items (Range)
Ethical Principles / Informed Consent /
20% - 25%
Safety
Institutional Review Board / Independent
Ethics Committee (IRB/IEC) Roles and 7% - 11%
Responsibilities
Clinical Trial Protocol and Protocol
4% - 8%
Amendments
Investigator Roles and Responsibilities 28% - 32%
Sponsor Roles and Responsibilities 31% - 35%
Ethical
Principles /
Informed
Sponsor Roles Institutional
Consent /
and Review Board /
Safety
Responsibilities Independent
Ethics
Committee
(IRB/IEC) Roles
and
Investigator
Responsibilities
Roles and
Responsibilities Clinical Trial
Protocol and
Protocol
Amendments
\\NAS1\George\Docs\SoCRA\CCRP communications\Study guide management
Detailed CCRP® Examination Outline
The CCRP certification examination content is arranged into five major content areas (listed below). The examination
outline has been expanded to be more descriptive of the topics that are included within the major content areas of the
exam. It is our hope that these descriptions will further assist you in your study process.
Five Content
Topic Areas
Areas
Nuremberg Code Abstracting/verification of information from medical records
Ethical Belmont Report related to informed consent and safety reporting
Declaration of Helsinki Vulnerable subjects
Principles/
Informed consent including development, content, Safety Reporting (adverse events, serious adverse drug
Informed
review, approval, discussion, documentation and experiences, unanticipated adverse device effects)
Consent/Safety ongoing updates. Financial disclosure
Maintenance of informed consent documents
(paper/electronic)
Knowledge Of:
Ethical principles described in the
Nuremberg Code, Belmont Report and
Declaration of Helsinki
Regulatory Requirements:
Informed consent/assent process including development, content, review, approval,
discussion, documentation and ongoing updates
Submission (obtain approval) of informed consent documents to reviewing IRB/IEC- original
and updates
Essential elements/information to be provided to subjects
Safeguards for children in clinical trials
Exemption for informed consent for emergency research
Permission by parents or guardians and for assent by children
Protection of vulnerable subjects
Obtaining consent with use of a short form written consent
Informing subjects of safety concerns and any relevant changes to the study
Subject safety issues –definitions, documentation, and reporting of adverse events, serious
adverse events/serious adverse drug reaction, and unanticipated adverse device effects
including the following:
Documentation
Expected or unexpected results associated with investigational products
Investigator’s plan/protocol of action for management of adverse event (e.g., stop
investigational product; call, retest, treat subject)
Follow-up to determine resolution of adverse event
Definition / classification of: adverse event, adverse drug reaction, serious adverse
event, and unanticipated adverse device effects
Documentation of serious adverse events/serious adverse drug reaction, and
unanticipated adverse device effects and relevant information on source documents
and CRFs
Regulatory requirements for reporting serious adverse event/serious adverse drug
reaction, and unanticipated adverse device effects to Sponsor/CRO and IRB/IEC
Regulatory requirements for documenting reasons for subject
discontinuation/termination
Regulatory requirements for documenting follow-up medical care for study subjects
Safety monitoring/reporting activities
Un-blinding
Requirements for documentation and reporting financial disclosure for clinical investigators
including:
Form FDA 3454 and 3455
Definition of significant equity interest and significant payments in clinical trial
Definition of covered clinical trial
Record maintenance
\\NAS1\George\Docs\SoCRA\CCRP communications\Study guide management
Institutional Roles and Responsibilities etc. of IRB/IEC Membership
Review Board/ Determination that the rights, welfare and safety of Protocol review
Independent study subjects including vulnerable populations are Significant Risk/Non Significant Medical Device study
Ethics protected determination
Committee Development and implementation of Standard Documentation
(IRB/IEC) Roles Operating Procedures (SOPs) Development, maintenance of IRB/IEC related documents
(paper/electronic)
and
Record retention IRB/IEC
Responsibilities
Knowledge Of:
Regulatory Requirements Related to:
Responsibilities and obligations of the IRB/IEC
Development and review of informed consent documents, recruitment materials, safety
reports, continuing review of investigational device exemptions (IDEs) (significant risk, non-
significant risk, and exempt studies)
Standard operating procedure development and implementation for the IRB/IEC
IRB / IEC membership
IRB / IEC protocol review
IRB / IEC protocol amendment review
IRB / IEC expedited protocol review
Significant risk/non significant medical device study determination
Documentation of IRB/IEC meeting minutes, reviews and decisions
Communication of IRB/IEC decisions
Record retention for IRB/IEC
Protocol development including: Development, review protocol amendments
Clinical trial phases Submission of protocol amendment(s) to applicable authorities,
Clinical Trial Study design characteristics (e.g., double- IRB/IEC
Protocol and blind, crossover, randomized) Investigational New Drug (IND) and Investigational Device
Protocol Study objectives and purpose Exemption (IDE) Amendment submission to applicable
Amendments Inclusion/exclusion criteria authorities and approval
Description of procedures
Statistical plan
Knowledge Of:
Development of protocols (including study design with consideration of methods to reduce bias,
objectives, endpoints, data safety monitoring)
Clinical trial phases (e.g. drug trials- phase 1, 2, 3 and medical devices- feasibility, pivotal)
Randomization and blinding
Development and review of protocol amendment(s)
Regulatory requirements for submission of protocol amendment(s) to applicable authorities,
IRB/IEC
\\NAS1\George\Docs\SoCRA\CCRP communications\Study guide management
Roles, responsibilities and obligations of the Study visits and follow up care
investigator Investigational site source documentation
Study conduct in accordance with investigational Documentation/Reporting discontinuation of study subjects
plan, investigator agreement and applicable Investigational site study related reports (i.e. progress reports,
regulations protocol changes, protocol deviations, final reports
Protocol(s) and protocol related document(s) (i.e., source documentation/case report forms
Investigator’s informed consent documents, recruitment Maintenance of essential study related documents
Roles and materials, safety reports, continuing reviews) (paper/electronic)
Responsibilities development, review, and submission for reviewing Abstracting/verification of information from medical records
authorities Record retention requirements for clinical sites
Recruitment, screening, enrollment, and retention Quality control, quality assurance and corrective and
of subjects preventive action plans (CAPA) at investigational site
Investigational site Investigational product
accountability including training of subjects
Knowledge Of:
Roles, responsibilities and obligations of the clinical investigator
Regulatory requirements for compliance to conduct study in accordance with investigational plan,
investigator agreement, and applicable regulations
Regulatory requirement for protocol(s) and protocol related document(s) (i.e., informed consent
documents, recruitment materials, continuing reviews) development, review, and submission for
reviewing authorities
Subject Scheduling, Screening, Recruitment, and Retention including:
Recruitment plan/strategies (including regulatory requirements for recruitment materials)
Subject compliance
Subject visits
Subject retention
Subject discontinuation
Regulatory requirements related to receipt and distribution of investigational product and other
supplies at study site:
Documentation of randomization of subjects and investigational product
Packaging and labeling of investigational products
Evaluation and documentation of Investigational product compliance (e.g., according to
protocol)
Documentation of Investigational Product Accountability
Subject training for study agents
Regulatory requirements related to source documentation (paper/electronic) -completion/review of
source documentation and case report forms of subject participation in a study including:
Subject eligibility
Informed consent
Safety- adverse events, adverse drug reaction, serious adverse effect, unanticipated adverse
device effect
Study related visits, procedures, and assessments
Discontinuation/termination of study subject
Regulatory requirements for Investigational site study reports development and submission to
reviewing authorities (i.e. progress reports, safety reports, final reports protocol changes, protocol
deviations)
Regulatory requirements for essential documents
Regulatory requirements for record retention
Quality control, quality assurance and corrective and preventive action plans (CAPA)
\\NAS1\George\Docs\SoCRA\CCRP communications\Study guide management
Regulatory documents (i.e. FDA Forms, 1572, 3454, 3455,
Roles, responsibilities and obligations of the Medwatch [3500 and 3500A])
sponsor Study Plan
Investigator/site qualifications Maintenance of essential study related documents
Investigator Brochure (paper/electronic) for sponsors
Investigational site training, management, oversight Development, verification, maintenance of electronic records
and investigator compliance and electronic record systems
Sponsor’s
Protocol(s) and protocol related document(s) (i.e., Monitoring including study coordination, record verification and
Roles and quality assurance
informed consent documents, recruitment
Responsibilities materials, safety reports, continuing reviews) Maintenance of essential study related documents
development, review, and submission for reviewing (paper/electronic) for sponsors
authorities Verification of information from medical records
Site/investigator training (GCP, investigational
product, study, reporting requirements)
Record Retention (Sponsor)
Sponsor Investigational product accountability Corrective Action Plans (CAPA)
Standard Operating Procedures Regulatory Agency inspections
Knowledge Of:
Roles, responsibilities and obligations of the sponsor
Evaluating clinical site and personnel for qualification to conduct the clinical study
Investigator meetings
Development and review of investigational product brochure
Regulatory requirement for protocol(s) and protocol related document(s) (i.e., informed consent
documents, recruitment materials, safety reports, continuing reviews) development, review, and
submission to reviewing authorities
Site/investigator training (GCP, investigational product, study, reporting requirements, compliance
with protocol)
Regulatory requirements related to shipment and disposition of investigational products including:
Investigational product (e.g., package insert, report of prior investigations, Investigator's
Brochure)
Documentation of randomization of investigational product
Investigational product accountability
Packaging and labeling of investigational products
Evaluation and documentation of investigational product compliance (e.g., protocol, standard
operating procedures, local governance)
Documentation of investigational product accountability
Standard operating procedure (SOP) development and implementation
Regulatory requirements related to the development, submission and review of regulatory
documents (i.e. FDA Forms 1572, 3454, 3455, Medwatch 3500 and 3500A, annual reports, safety
reports, final reports)
Data Safety Monitoring Boards (DSMB)
Regulatory requirements related to electronic record systems
Review of accuracy and completeness of site records including monitoring source
documentation/case report forms: eligibility, product dosing and accountability, adverse events,
study related visits and follow up care, and informed consent
Regulatory requirements related to essential documents for clinical studies (sponsor)
Preparation and follow-up for study site and sponsor regulatory agency inspections (including FDA
forms 482 and 483)
Knowledge of principles of Quality Assurance and Corrective and Preventive Action Plans (CAPA)
\\NAS1\George\Docs\SoCRA\CCRP communications\Study guide management
Das könnte Ihnen auch gefallen
- Acrp CP DcoDokument24 SeitenAcrp CP Dcopopatlilo2Noch keine Bewertungen
- Ethical Issues in Clinical TrialsDokument16 SeitenEthical Issues in Clinical TrialsPranjal KothaleNoch keine Bewertungen
- Site AssessmentDokument7 SeitenSite AssessmentRehab KhanNoch keine Bewertungen
- Chapter-Ii: By: J. Jayasutha Lecturer Department of Pharmacy Practice SRM College of Pharmacy SRM UniversityDokument15 SeitenChapter-Ii: By: J. Jayasutha Lecturer Department of Pharmacy Practice SRM College of Pharmacy SRM UniversityHamid RazaNoch keine Bewertungen
- GCP Participant ManualDokument36 SeitenGCP Participant ManualNatalie FanNoch keine Bewertungen
- Doc10-14 App H QSE 8 Occur MGTDokument4 SeitenDoc10-14 App H QSE 8 Occur MGTajee doNoch keine Bewertungen
- A Comprehensive and Practical Guide to Clinical TrialsVon EverandA Comprehensive and Practical Guide to Clinical TrialsBewertung: 3 von 5 Sternen3/5 (1)
- Compatibility of Pharmaceutical Solutions and Contact Materials: Safety Assessments of Extractables and Leachables for Pharmaceutical ProductsVon EverandCompatibility of Pharmaceutical Solutions and Contact Materials: Safety Assessments of Extractables and Leachables for Pharmaceutical ProductsNoch keine Bewertungen
- Equipment Qualification in the Pharmaceutical IndustryVon EverandEquipment Qualification in the Pharmaceutical IndustryBewertung: 3.5 von 5 Sternen3.5/5 (3)
- 2 National Guidelines and RegulationsDokument31 Seiten2 National Guidelines and RegulationsLarissa Miguel SeveraNoch keine Bewertungen
- SOP 032 Handling of Non-Compliance v1.1 24 FEB 2017 PDFDokument15 SeitenSOP 032 Handling of Non-Compliance v1.1 24 FEB 2017 PDFHaroon RasheedNoch keine Bewertungen
- Sample Management in Clinical TrialsDokument8 SeitenSample Management in Clinical TrialstheanhdbtNoch keine Bewertungen
- Jira TrainingDokument22 SeitenJira Trainingkasalasurya16Noch keine Bewertungen
- Regulatory Binder ChecklistDokument4 SeitenRegulatory Binder ChecklistOscar Pompa MeraNoch keine Bewertungen
- Root Cause Analysis Template 22Dokument9 SeitenRoot Cause Analysis Template 22Devi ChintyaNoch keine Bewertungen
- COMPASSIONATE 3A CLINPATH Activity 1 Comparison of AO 037 and ISO 15189Dokument17 SeitenCOMPASSIONATE 3A CLINPATH Activity 1 Comparison of AO 037 and ISO 15189Adrian CaballesNoch keine Bewertungen
- Audiology: Test at A GlanceDokument13 SeitenAudiology: Test at A Glanceabdullah hussinyNoch keine Bewertungen
- Code of Professional Conduct For NursesDokument3 SeitenCode of Professional Conduct For NursesherbertNoch keine Bewertungen
- Sop Title: Assessing Protocol Feasibility: Sop No: Effective DateDokument7 SeitenSop Title: Assessing Protocol Feasibility: Sop No: Effective Datetiara rengganis100% (1)
- Handbook of Nanosafety: Measurement, Exposure and ToxicologyVon EverandHandbook of Nanosafety: Measurement, Exposure and ToxicologyUlla VogelBewertung: 4 von 5 Sternen4/5 (1)
- AMC CBD Form Final Version 2Dokument2 SeitenAMC CBD Form Final Version 2Everymed WorldwideNoch keine Bewertungen
- Anctioning Reference Points Instruction Manual: Behavioral Sciences BoardsDokument12 SeitenAnctioning Reference Points Instruction Manual: Behavioral Sciences Boardslamarrokina22Noch keine Bewertungen
- Chart Audit ToolDokument3 SeitenChart Audit ToolshkjnuNoch keine Bewertungen
- Innovative and Efficient Laboratory ManagementVon EverandInnovative and Efficient Laboratory ManagementNoch keine Bewertungen
- Title: Constitution of An IECDokument11 SeitenTitle: Constitution of An IECprabhaNoch keine Bewertungen
- Description of Technology Readiness Levels (TRL)Dokument8 SeitenDescription of Technology Readiness Levels (TRL)TonyNoch keine Bewertungen
- FMR No 4Dokument7 SeitenFMR No 4Dwi RatihNoch keine Bewertungen
- BACR Presentation GCP Jan-2018-002Dokument72 SeitenBACR Presentation GCP Jan-2018-002MilenNoch keine Bewertungen
- An Introduction To Good Laboratory Practices: Melissa Elliott, BS, RQAP-GLPDokument54 SeitenAn Introduction To Good Laboratory Practices: Melissa Elliott, BS, RQAP-GLPHimanshu BarmanNoch keine Bewertungen
- Document Title: HSE Performance: DistributionDokument7 SeitenDocument Title: HSE Performance: DistributionAbdellatef HossamNoch keine Bewertungen
- NPA SITXWHS007 Assessment 1 Short Answer FinalDokument13 SeitenNPA SITXWHS007 Assessment 1 Short Answer FinalJoshua Estrada AbellaNoch keine Bewertungen
- IIN311-B - Case Study and Reading Control Form - Case 2 - 1069349Dokument7 SeitenIIN311-B - Case Study and Reading Control Form - Case 2 - 1069349Juanito alachofaNoch keine Bewertungen
- Pediatric Non-Clinical Drug Testing: Principles, Requirements, and PracticeVon EverandPediatric Non-Clinical Drug Testing: Principles, Requirements, and PracticeAlan M. HobermanNoch keine Bewertungen
- Hrec Icq 150611 PDFDokument11 SeitenHrec Icq 150611 PDFCarlos Eduardo C. da SilvaNoch keine Bewertungen
- 0969733011420096-Moral DelibrationDokument13 Seiten0969733011420096-Moral DelibrationAnonymous RJZcGzMNoch keine Bewertungen
- FDA Administrative Order No. 2020-0010 Regulations On The Conduct of Clinical Trials For Investigational Products Clinical Trial/ Clinical StudyDokument14 SeitenFDA Administrative Order No. 2020-0010 Regulations On The Conduct of Clinical Trials For Investigational Products Clinical Trial/ Clinical StudyFrietzyl Mae GeneralaoNoch keine Bewertungen
- Chinese General Hospital and Medical Center Department of Medical Education and Research Research Ethics Review Board (Rerb)Dokument11 SeitenChinese General Hospital and Medical Center Department of Medical Education and Research Research Ethics Review Board (Rerb)Reda SoNoch keine Bewertungen
- Nonclinical Study Contracting and Monitoring: A Practical GuideVon EverandNonclinical Study Contracting and Monitoring: A Practical GuideWilliam F. SalminenNoch keine Bewertungen
- 4 Federici AIES 2018Dokument15 Seiten4 Federici AIES 2018martinsmicaelribeiroNoch keine Bewertungen
- Research and Ethical CommitteeDokument8 SeitenResearch and Ethical Committeefarha naazNoch keine Bewertungen
- NMRR Data Elements For Submission Version 2Dokument12 SeitenNMRR Data Elements For Submission Version 2Yeoh Jia LimNoch keine Bewertungen
- Ich-Gcp & Schedule yDokument38 SeitenIch-Gcp & Schedule ySahiti PendyalaNoch keine Bewertungen
- Industrial Pharmacy II - TheoryDokument3 SeitenIndustrial Pharmacy II - TheoryAlana KhanNoch keine Bewertungen
- Chapter 3.1 Introduction To Industrial Hygiene and Occupational HealthDokument27 SeitenChapter 3.1 Introduction To Industrial Hygiene and Occupational HealthHafizudin DaudNoch keine Bewertungen
- 3-KP 17 Önleyici Faaliyet-EnDokument5 Seiten3-KP 17 Önleyici Faaliyet-EnErdinç KuşçuNoch keine Bewertungen
- ISM General Awareness FinalDokument17 SeitenISM General Awareness FinalSudhakaran JayaramNoch keine Bewertungen
- IP Accountability SOP - 4 23 2019Dokument5 SeitenIP Accountability SOP - 4 23 2019JulianaCerqueiraCésarNoch keine Bewertungen
- Nov 25 Consultation FormDokument3 SeitenNov 25 Consultation FormJC LumayaNoch keine Bewertungen
- Swab Instrument and Sharps Count Policy Page 1 of 3 Quality, Safety and Experience CommitteeDokument37 SeitenSwab Instrument and Sharps Count Policy Page 1 of 3 Quality, Safety and Experience CommitteeGina AprianaNoch keine Bewertungen
- Checklist Clinical Office Endos PDFDokument20 SeitenChecklist Clinical Office Endos PDFBABBY ZBOURGNoch keine Bewertungen
- 2003 BPS - KAI's Test ReviewDokument11 Seiten2003 BPS - KAI's Test ReviewriobocabotdNoch keine Bewertungen
- Basic Course in Biomedical Research Handbook: March 2021Dokument89 SeitenBasic Course in Biomedical Research Handbook: March 2021Ayush GuptaNoch keine Bewertungen
- Document Title: Control of Substances Hazardous To Health (COSHH)Dokument13 SeitenDocument Title: Control of Substances Hazardous To Health (COSHH)Abdellatef HossamNoch keine Bewertungen
- Module 2.2 - Concept of EBP PDFDokument24 SeitenModule 2.2 - Concept of EBP PDFvincyNoch keine Bewertungen
- Element 4 - Environmental Risk Evaluation and ControlDokument43 SeitenElement 4 - Environmental Risk Evaluation and ControlAla Eldin YassenNoch keine Bewertungen
- Ethics For Speech-Language Pathologists and Audiologists: An Illustrative CasebookDokument17 SeitenEthics For Speech-Language Pathologists and Audiologists: An Illustrative CasebookJesus Mata CastroNoch keine Bewertungen
- Nondestructive Evaluation Indication, Evaluatio and Disposition Guide LinesDokument126 SeitenNondestructive Evaluation Indication, Evaluatio and Disposition Guide LinesEdison Walit100% (1)
- BT-11-202 eTMF Maintenance Plan - Version1.0 - 05apr2021 - Final - Fully - SignedDokument20 SeitenBT-11-202 eTMF Maintenance Plan - Version1.0 - 05apr2021 - Final - Fully - SignedAdnan MuharemagicNoch keine Bewertungen
- ASHA Guidelines For Early Intervention IncludeDokument10 SeitenASHA Guidelines For Early Intervention IncludeMayraNoch keine Bewertungen
- CBT 15 1029Dokument13 SeitenCBT 15 1029সোমনাথ মহাপাত্রNoch keine Bewertungen
- 1201020895PL IMillerDokument26 Seiten1201020895PL IMillerসোমনাথ মহাপাত্রNoch keine Bewertungen
- Account Statement As of 04-05-2020 19:48:27 GMT +0530Dokument11 SeitenAccount Statement As of 04-05-2020 19:48:27 GMT +0530সোমনাথ মহাপাত্রNoch keine Bewertungen
- Risk of 2nd Malig in NHLDokument11 SeitenRisk of 2nd Malig in NHLসোমনাথ মহাপাত্রNoch keine Bewertungen
- BD Biosciences Support - Protocols - Intracellular Staining of Human Red Blood CellsDokument1 SeiteBD Biosciences Support - Protocols - Intracellular Staining of Human Red Blood Cellsসোমনাথ মহাপাত্রNoch keine Bewertungen
- Brandtzaeg 1981Dokument14 SeitenBrandtzaeg 1981সোমনাথ মহাপাত্রNoch keine Bewertungen
- Chapter 3 Haemoglobin Pattern Analysis: 3.1. Chromatographic Methods (For Hba Determination)Dokument27 SeitenChapter 3 Haemoglobin Pattern Analysis: 3.1. Chromatographic Methods (For Hba Determination)সোমনাথ মহাপাত্রNoch keine Bewertungen
- East Bank MapDokument1 SeiteEast Bank Mapসোমনাথ মহাপাত্রNoch keine Bewertungen
- My OwnDokument1 SeiteMy Ownসোমনাথ মহাপাত্রNoch keine Bewertungen
- Globalizarea Nimicului - RitzerDokument27 SeitenGlobalizarea Nimicului - RitzerAlina PetreNoch keine Bewertungen
- 149 FullDokument10 Seiten149 Fullসোমনাথ মহাপাত্রNoch keine Bewertungen
- Chap1 - Units, Dimensions & Vectors PDFDokument61 SeitenChap1 - Units, Dimensions & Vectors PDFসোমনাথ মহাপাত্রNoch keine Bewertungen
- Immune Recognition of Self Nucleic Acids Driven by Endogenous Antimicrobial Peptides: Role in AutoimmunityDokument176 SeitenImmune Recognition of Self Nucleic Acids Driven by Endogenous Antimicrobial Peptides: Role in Autoimmunityসোমনাথ মহাপাত্রNoch keine Bewertungen
- Result Sheet PDFDokument41 SeitenResult Sheet PDFManohar ManuNoch keine Bewertungen
- Anxiety Disorders Treatment ProtocolDokument25 SeitenAnxiety Disorders Treatment Protocolসোমনাথ মহাপাত্রNoch keine Bewertungen
- DHR-ICMR Funded Workshops FormatDokument3 SeitenDHR-ICMR Funded Workshops Formatসোমনাথ মহাপাত্রNoch keine Bewertungen
- DHR-ICMR Funded Workshops FormatDokument3 SeitenDHR-ICMR Funded Workshops Formatসোমনাথ মহাপাত্রNoch keine Bewertungen
- Icmr Talent FormDokument2 SeitenIcmr Talent Formসোমনাথ মহাপাত্রNoch keine Bewertungen
- 1 This Is System WiseDokument1 Seite1 This Is System Wiseসোমনাথ মহাপাত্রNoch keine Bewertungen
- Cell-Cell Interactions: Concept OutlineDokument18 SeitenCell-Cell Interactions: Concept Outlineসোমনাথ মহাপাত্রNoch keine Bewertungen
- EBv Neg Epidemiology Leblond JCO.1998.16.6Dokument8 SeitenEBv Neg Epidemiology Leblond JCO.1998.16.6সোমনাথ মহাপাত্রNoch keine Bewertungen
- Observership Policy Saint Agnes HospitalDokument3 SeitenObservership Policy Saint Agnes HospitalNilay BhattNoch keine Bewertungen
- Griffin Observership ApplicationDokument7 SeitenGriffin Observership Applicationসোমনাথ মহাপাত্রNoch keine Bewertungen
- Boards and Beyound Step 2 Cs PalpitationsDokument4 SeitenBoards and Beyound Step 2 Cs Palpitationsসোমনাথ মহাপাত্রNoch keine Bewertungen
- Cs Info ManualDokument20 SeitenCs Info Manualসোমনাথ মহাপাত্রNoch keine Bewertungen
- Medical AbbreviationsDokument4 SeitenMedical AbbreviationsNelly PaniaguaNoch keine Bewertungen
- Chemo For HematologyDokument1 SeiteChemo For Hematologyp monica aneeshaNoch keine Bewertungen
- UWORLD Biostatistics Book Review PDFDokument93 SeitenUWORLD Biostatistics Book Review PDFসোমনাথ মহাপাত্র50% (2)
- Chemo For HematologyDokument1 SeiteChemo For Hematologyp monica aneeshaNoch keine Bewertungen
- Rguhs Thesis Topics in Pediatric DentistryDokument5 SeitenRguhs Thesis Topics in Pediatric Dentistrylhydupvcf100% (2)
- Pengantar FarmakologiDokument18 SeitenPengantar FarmakologiHaidar AdiNoch keine Bewertungen
- Appendix 2 - Application Checklist - ICH CTDDokument17 SeitenAppendix 2 - Application Checklist - ICH CTDWilliam ChandraNoch keine Bewertungen
- Classification of Dosage FormsDokument25 SeitenClassification of Dosage FormsNimit Jain100% (1)
- CIOMS Guideline Preparing Clinical and Safety InformationDokument4 SeitenCIOMS Guideline Preparing Clinical and Safety InformationNataliaNoch keine Bewertungen
- Theories of Drug Receptor Interactions: by Lee Eun JinDokument42 SeitenTheories of Drug Receptor Interactions: by Lee Eun Jinsky.blueNoch keine Bewertungen
- Guideline Reporting Physiologically Based Pharmacokinetic PBPK Modelling Simulation - enDokument16 SeitenGuideline Reporting Physiologically Based Pharmacokinetic PBPK Modelling Simulation - enLay LylyNoch keine Bewertungen
- BIODATA GauravDokument11 SeitenBIODATA Gauravgaurav tiwariNoch keine Bewertungen
- PharmacologyDokument271 SeitenPharmacologysweta suman100% (3)
- E.g., Phenylephrine Is Full Agonist at Alpha-Adrenoceptors. E.g., Aripipraxole Is Partial Antagonist at Selected Dopamine ReceptorsDokument1 SeiteE.g., Phenylephrine Is Full Agonist at Alpha-Adrenoceptors. E.g., Aripipraxole Is Partial Antagonist at Selected Dopamine ReceptorsSafura IjazNoch keine Bewertungen
- Agency DOD Program Charts Aug 2017Dokument269 SeitenAgency DOD Program Charts Aug 2017jpd1015Noch keine Bewertungen
- @jeeneetprep PGMEE Test SeriesDokument410 Seiten@jeeneetprep PGMEE Test SeriesL.ABHISHEK KUMARNoch keine Bewertungen
- 2017 Guidelines WebDokument291 Seiten2017 Guidelines Webrini setyawatiNoch keine Bewertungen
- CBR A Drug DevelopDokument2 SeitenCBR A Drug DevelopAlfieNoch keine Bewertungen
- Lesson Plan DFDDokument2 SeitenLesson Plan DFDRajwinder Onkar SinghNoch keine Bewertungen
- Recent Progress in Drug DeliveryDokument18 SeitenRecent Progress in Drug DeliveryAyush SapkotaNoch keine Bewertungen
- Lecture 01 PDFDokument71 SeitenLecture 01 PDFKimNoch keine Bewertungen
- 1-En-Introduction To Pharmaceutical Technology and MixingDokument72 Seiten1-En-Introduction To Pharmaceutical Technology and Mixingsedasunkar100% (1)
- B.P.P.K - Course OutcomesDokument3 SeitenB.P.P.K - Course OutcomesDr. B. Sree Giri PrasadNoch keine Bewertungen
- Pharmacy Time Table 2023-2024 1st IsseDokument8 SeitenPharmacy Time Table 2023-2024 1st IsseIhtisham SafdarNoch keine Bewertungen
- Introduction To PharmacologyDokument21 SeitenIntroduction To Pharmacologyderic100% (12)
- G1e121020 - Ghery Arrahman - Bahasa InggrisDokument4 SeitenG1e121020 - Ghery Arrahman - Bahasa InggrisGhery Arrahman100% (1)
- QC Tests For Tablet Dosage FormsDokument8 SeitenQC Tests For Tablet Dosage FormsSai Krishna ManchikantiNoch keine Bewertungen
- Day 1-5 James Butler FinalDokument22 SeitenDay 1-5 James Butler FinalPedro MaiaNoch keine Bewertungen
- 2.02 - Quality and Bioequivalence Guideline - Jul19 - v7 1Dokument35 Seiten2.02 - Quality and Bioequivalence Guideline - Jul19 - v7 1vinayNoch keine Bewertungen
- Daftar PustakaDokument5 SeitenDaftar PustakaFaisal MNoch keine Bewertungen
- 4 Oct 2019 Hisfarma DIY (Lisa Aditama)Dokument71 Seiten4 Oct 2019 Hisfarma DIY (Lisa Aditama)Marni BandurNoch keine Bewertungen
- Introduction To PharmacologyDokument2 SeitenIntroduction To PharmacologyJoy Ann Akia PasigonNoch keine Bewertungen
- Karnataka Aayush ListDokument14 SeitenKarnataka Aayush ListplanetsandtarotNoch keine Bewertungen
- Mechanistic Models of Cmap Drug Perturbation Functional ProfilesDokument36 SeitenMechanistic Models of Cmap Drug Perturbation Functional ProfilesMacarenaLópezSánchezNoch keine Bewertungen