Beruflich Dokumente
Kultur Dokumente
GRP
Hochgeladen von
flying highOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
GRP
Hochgeladen von
flying highCopyright:
Verfügbare Formate
REVIEWS
Vascular heterogeneity and
specialization in development
and disease
Michael Potente1–3 and Taija Mäkinen4
Abstract | Blood and lymphatic vessels pervade almost all body tissues and have numerous
essential roles in physiology and disease. The inner lining of these networks is formed by a single
layer of endothelial cells, which is specialized according to the needs of the tissue that it supplies.
Whereas the general mechanisms of blood and lymphatic vessel development are being defined
with increasing molecular precision, studies of the processes of endothelial specialization remain
mostly descriptive. Recent insights from genetic animal models illuminate how endothelial cells
interact with each other and with their tissue environment, providing paradigms for vessel type-
and organ-specific endothelial differentiation. Delineating these governing principles will be
crucial for understanding how tissues develop and maintain, and how their function becomes
abnormal in disease.
Organ homeostasis depends on the function of two hier- In this Review, we discuss the molecular and func-
archically branched vessel networks: the blood and the tional heterogeneity within the vasculature and highlight
lymphatic vasculatures. The blood vasculature is a closed emerging concepts of endothelial specialization. We first
circulatory system that consists of arteries, veins and provide an overview of the origins and the develop-
interconnecting capillaries. It transports gases, nutrients, ment of blood and lymphatic vessels and then explain
metabolites and cells, and provides paracrine signalling how they become remodelled into functionally special-
molecules to adjacent tissues. The lymphatic system, con- ized networks. We also discuss how vessels reciprocally
versely, is blind-ended and unidirectional, and comprises instruct tissue differentiation and function, as well as the
lymphatic vessels, lymph nodes and associated lymphoid mechanisms that underlie vessel type- and vascular
organs. This ‘second vascular system’ is coupled to the bed-specific diseases.
1
Angiogenesis & Metabolism blood vasculature as it returns extravasated fluid and
Laboratory, Max Planck
macromolecules to the blood circulation. Moreover, Blood and lymph vessel architecture
Institute for Heart and Lung
Research, Ludwigstr. 43, lymphatic vessels participate in fat absorption, tissue Blood vessels organize into tree-like structures. Large
D-61231 Bad Nauheim, cholesterol clearance and immune cell trafficking 1. arteries carry oxygenated blood away from the heart
Germany. Endothelial cells (ECs) line the interior of all blood and branch into smaller calibre arterioles that feed into
2
International Institute of and lymphatic vessels. Despite sharing a mesodermal extensive capillary networks (FIG. 1). Venules drain capil
Molecular and Cell Biology,
02–109 Warsaw, Poland.
origin and some common functions, these cells are not laries and converge into larger veins to return oxygen-
3
DZHK (German Center for all alike. Depending on the type of vessel or organ in depleted blood to the heart. Blood is transferred via
Cardiovascular Research), which they reside, ECs exhibit distinct molecular and the pulmonary artery to the lungs for re‑oxygenation.
partner site Frankfurt functional properties, which give rise to substantial Lymphatic vessels are similarly organized into a hierar-
Rhine‑Main, D-13347 Berlin,
heterogeneity in the vascular tree. The mechanisms by chy of blind-ended lymphatic capillaries, pre-collecting
Germany.
4
Department of Immunology, which ECs specialize to fulfil their tissue-specific tasks vessels and collecting vessels. Lymphatic capillaries
Genetics, and Pathology, are poorly understood but are essential for normal organ clear excess interstitial fluid and provide an entry site
Uppsala University, development and function. Endothelial specialization for tissue-resident immune cells into the lymphatic
Dag Hammarskjölds väg 20, has been linked to cell-intrinsic developmental pathways system. By contrast, collecting vessels are specialized
75185 Uppsala, Sweden.
michael.potente@mpi‑bn.
and transcriptional programmes, as well as to signals for fluid transport, and drain lymph into the thor
mpg.de; from the microenvironment. Examples of these micro acic and right lymphatic ducts, which connect to the
taija.makinen@igp.uu.se environment signals include growth f actors, mechanical venous circulation. All of these vessel types have dis
doi:10.1038/nrm.2017.36 forces and metabolic stimuli, as well as cell–matrix and tinctive morphological and functional c haracteristics
Published online 24 May 2017 cell–cell interactions. (FIG. 1).
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 1
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Blood capillary Lymphatic capillary
Continuous Fenestrated Discontinuous
Pericyte Oak-leaf shape of EC
with button junctions
Discontinuous Anchoring
BM filaments
BM
EC
Capillary bed
Arteriole Venule
Collecting
lymphatic vessel
Artery Vein
BM BM
Tunica intima BM Tunica intima
Tunica media SMC Tunica media
(SMCs and (SMCs and
elastic fibres) Valve elastic fibres) Valve
Tunica Tunica
adventitia adventitia
Endothelium
Endothelium Endothelium
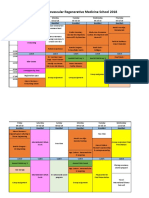
Figure 1 | Organization of the vasculature. The vasculature is organized into hierarchical networks
Nature Reviews of arteries
| Molecular Cell(red),
Biology
veins (blue) and interconnected capillaries, as well as blind-ended lymphatic capillaries and collecting vessels (green)
that drain fluid into the venous circulation. Arterioles, capillaries and venules constitute the microvasculature, the site
where most intercellular communication occurs. Large arteries and veins are characterized by a continuous lining of
endothelial cells (ECs), basement membrane (BM) and layers of smooth muscle cells (SMCs). Blood capillary ECs can be
continuous, fenestrated or discontinuous, and they have a varying extent of BM and pericyte coverage. Lymphatic
capillaries consist of oak-leaf-shaped ECs with specialized button-like junctions and anchoring filaments that pull the
ECs apart and allow the entry of fluid under conditions of high interstitial pressure. Collecting lymphatic vessels have
a sparse SMC coverage and luminal valves that help with pumping and that prevent the backflow of lymph, respectively.
The anatomy of capillary vessels is shown at the top of the figure and larger vessels are shown at the bottom. The tunica
adventitia is the outer connective tissue covering of the vessel.
Heterogeneity in vessel morphology. Vessel walls can control osteoprogenitor cells, while connected sinusoidal
be morphologically diverse, both within a certain part capillaries in the bone marrow are highly branched and
of the network and between different parts of the net- irregular and interact with haematopoietic cells3. ECs are
work. For example, the endothelium of arteries and enwrapped by a basement membrane (BM), the shape and
veins forms a continuous monolayer, whereas capil- composition of which differs across the vascular tree4.
lary ECs can be continuous, fenestrated or discontin- It varies from a thick elastic lamina in large arteries to a
uous (FIG. 1). Fenestrated endothelium is found in tissues thin, discontinuous BM in lymphatic capillaries (FIG. 1).
that are involved in filtration and secretion, including Vessels also differ in their coverage by mural cells,
Fenestrated endothelium
Endothelium that is permeated exocrine and endocrine glands, kidney glomeruli and which comprise vascular smooth muscle cells (vSMCs),
with pores (fenestrae). the intestinal mucosa; discontinuous endothelium is pericytes and hepatic stellate cells. The walls of larger
characteristic of sinusoidal vascular beds that are found calibre blood vessels contain vSMCs, which are essen-
Basement membrane in the liver and bone marrow 2. Even within a given tial for vascular stability and tone, and blood pressure
(BM). Sheet-like extracellular
matrix structure that separates
capillary network, ECs can have distinct characteristics. regulation. Blood capillaries and venules, however, are
endothelium from the In the bone vasculature, capillaries close to the growth encased by pericytes. Pericytes make contacts with the
underlying tissue. plate form densely packed column-like structures that endothelium to regulate vessel stability, transendothelial
2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
transport and blood–brain barrier (BBB) formation5,6. specialized for the absorption of dietary lipids1. By con-
Pericytes have also been reported to possess contrac- trast, collecting lymphatic vessels have continuous
tile properties and to contribute to cerebral blood flow ‘zipper’ junctions14, which prevent leakage and ensure
regulation7, although this finding could not be con- the delivery of lymph and dendritic cells (DCs) to lymph
firmed in another study 8, possibly owing to differences nodes. Despite considerable insights into the functions
in pericyte definition. Mural cells have several different of junctional proteins, little is currently known about the
embryonic origins in different organs6, but whether they composition of endothelial junctions that would explain
have tissue-specific properties is mostly unknown. In the the barrier properties of different blood and lymphatic
lymphatic system, mural cell coverage is also different. vessel types.
Collecting lymphatic vessels have an SMC layer that Besides permeability, organ-specific vasculature
enables lymphatic vessel pumping through its unique also differs in its capacity to deliver nutrients to tissues.
ability to undergo both phasic and tonic contractions. In organs with energy-consuming functions, ECs adapt
Lymphatic capillaries lack mural cell support 9. Other to metabolic demands by adjusting capillary density and
vessel type-specific features are luminal valves, which by controlling endothelial nutrient transfer. The myo-
are only present in veins and collecting lymphatic vessels cardium, for example, relies on fatty acid catabolism
to prevent backflow. to produce ATP for its contractile performance, and
its ECs express high levels of the fatty acid transporter
Heterogeneity in vessel function. Heterogeneity in CD36 (REF. 15). Transendothelial fatty acid transport
morphology is coupled to heterogeneity in function has been shown to be regulated by vascular endothe-
(TABLE 1). The regulation of vascular tone is an arterial lial growth factor B (VEGFB), a growth factor that is
function that occurs primarily at the level of the enriched in contractile tissues16. Other studies have
arterioles, whereas veins, specifically post-capillary suggested a primary role for VEGFB in the regulation
venules, are the primary sites of leukocyte extravasation of cardiac metabolism and vascularization rather than
during inflammation. transendothelial transport17,18. Conversely, neurons rely
The barrier function of ECs also varies among dif- on glucose as the major energy source. Consequently,
ferent vascular beds. In the brain, for example, ECs BBB ECs preferentially express the glucose transporter
establish the highly selective BBB, which protects neu- GLUT1 (also known as SLC2A1), which facilitates the
rons from toxic molecules, immune cells and patho- transfer of glucose from the blood to the brain10. The
gens. Its barrier properties are based on a continuous importance of tissue-dependent transendothelial trans-
endothelium that is linked by specialized tight junctions port becomes evident in disorders in which the expres-
and adherens junctions, a low rate of transcytosis, and the sion or the function of transporters is compromised.
suppression of leukocyte adhesion10. The formation and For example, endothelial GLUT1 levels are decreased in
maintenance of the BBB depend on pericytes that con- Alzheimer disease, in response to a high-fat diet and
trol EC transcytosis5 and on the expression of sodium- in GLUT1‑deficiency syndrome, resulting in reduced
dependent lysophosphatidylcholine symporter 1 (NLS1; brain glucose availability, neuronal dysfunction and
encoded by MFSD2A), a selective transporter of essential neurodegeneration10,19,20. Additional substrate-specific
omega‑3 fatty acids, the expression of which is restricted transporters in the BBB endothelium include solute
Blood–brain barrier to BBB ECs11,12. carrier family 7 member 5 (SLC7A5), which main-
(BBB). A selective permeability The barrier properties of ECs differ dramatically tains normal levels of branched-chain amino acids in
barrier that restricts the in organs that are involved in absorption and filter- the brain. Its EC‑selective inactivation causes autism
passage of solutes from the
circulating blood to the brain.
ing. Examples include the kidney and small intestine, spectrum disorders21.
in which fenestrated ECs enable the rapid exchange, Functional endothelial heterogeneity is particularly
Tight junctions uptake and secretion of fluids, solutes and molecules2. important for the regulated trafficking and homing of
Intercellular junctional Endothelial permeability is even higher in liver sinu immune cells. For example, specialized high endothelial
complexes that are composed
soidal ECs (LSECs). LSECs are discontinuous, have venules (HEVs) in lymph nodes express molecules for the
of claudins, occludin and
junctional adhesion molecules, large non-diaphragmed fenestrae that are organized in recruitment and transendothelial migration of lympho-
and that function as sieve plates, and that lack an organized BM, allowing the cytes22,23. Moreover, tissue-specific differentiation of HEV
diffusion barriers. passage of small particles from the blood to hepatocytes2. ECs underlies organ-specific homing of leukocytes to
Interestingly, the barrier properties of blood vessels also distinct anatomical sites. An example is CD22‑mediated
Adherens junctions
Adhesive structures that are
influence their stem cell niche function. In the bone homing of B cells into gut-associated lymphoid tissue
formed through the association marrow, the less permeable arteries maintain haemato- through HEVs expressing β-galactoside α-2,6‑sialyl-
of cadherins, which link actin poietic stem cells (HSCs) in a quiescent state, whereas transferase 1 (ST6GAL1), a glycosyltransferase that
filaments between cells. the more permeable sinusoidal vessels promote HSC generates ligands for CD22 (REF. 22). Lymphatic vessels
activation and differentiation, as penetrating blood are also critically involved in immune cell trafficking
Transcytosis
Transport of macromolecules plasma increases reactive oxygen species formation13. into and exit from lymph nodes. For example, lymphatic
across the cell. Unlike most blood vessels, lymphatic capillaries are capillaries express the chemokine CCL21 to recruit
tasked with fluid uptake and are thus highly perme DCs from the peripheral tissues. Within lymph nodes,
Stem cell niche able. They are equipped with button-like junctions specialized lymphatic ECs (LECs) in the subcapsular
A microenvironment that
supports the undifferentiated
and anchoring filaments, which together facilitate fluid or cortical and medullary sinuses express molecules for
and self-renewable state uptake when interstitial pressure is high1,14. In the small the regulated entry of antigens and DCs, or the egress of
of stem cells. intestine, lymphatic capillaries (lacteals) are further lymphocytes, respectively 23.
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 3
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 1 | Examples of organ-specific endothelial specialization
Type Location EC phenotypes Specialized function Molecular Molecular regulation Refs
of ECs and characteristics markers
BBB ECs Central • Continuous • Highly selective barrier • MFSD2A Pericyte-derived 5,10–12,
nervous • Specialized tight junctions to protect neurons from • GLUT1 signals induce 21
system (occludins, claudins and toxic molecules, cells • SLC7A5, others and maintain BBB
JAMs) and pathogens properties and
• Inhibition of fenestrae, • Specialized for efficient integrity
pinocytosis and bulk-flow glucose transport to
transcytosis the brain
• Suppression of leukocyte • Substrate-specific
adhesion transporters for selective
transfer (nutrients
and metabolites)
Myocardial Heart • Continuous • Preferential fatty acid • CD36 • MEOX and TCF15 15–18
capillaries • Ratio of ECs to uptake and transfer to • LPL heterodimers induce
cardiomyocytes 3:1 the myocardium • PPARγ fatty acid transport
• Distance of EC from • Support cardiomyocyte genes
cardiomyocyte = 1 μm survival • VEGFB increases
fatty acid transfer and
vessel growth
Pulmonary Lung • Dense network through Specialized for efficient • ACE Unknown Reviewed
capillaries which blood flows as a sheet gas exchange at the • ALCAM in 186
• Extremely thin blood–air blood–air barrier (also known as
barrier CD166)
• Large number of caveolae
Liver Liver • Discontinuous • Dynamic filter for fluids, • Stabilin 1 Hepatocyte- 187,188
sinusoidal • Fenestrated (pore solutes and particles • Stabilin 2 derived VEGF
Reviewed
ECs size 100–200 nm, • Clearance of soluble • HGF and autocrine
in 186
non-diaphragmed) waste macromolecules • WNT2 WNT2 promote
• Fenestrae arranged as sieve by receptor-mediated differentiation of
plates endocytosis LSECs
• Lack of organized basement • Hepatic immune
membrane tolerance
• Control hepatocyte
proliferation
Glomerular Kidney • Fenestrated (pore size • Size- and ND Podocyte-derived 131
ECs 60–80 nm) charge-selective VEGF induces and
• Fenestrae cover 20% of EC filtration barrier maintains fenestrations
surface • Vasomotor tone control
• Thick endothelial glycocalyx
(60–300 nm)
Type H ECs Metaphysis • Organized as • Mediate bone High levels of HIF1 and DLL4–Notch 3
and interconnected vessel angiogenesis PECAM1 and signalling induces type
endosteum of columns • Control bone-forming endomucin H ECs
long bones • Direct arterial supply osteoprogenitor cells
• Well oxygenated through the release of
• Associated with osteogenic factors
osteoprogenitor cells
Type L ECs Diaphysis • Highly branched sinusoidal • Interaction with cells Low levels of Emerges from type H 3
of long network of the haematopoietic PECAM1 and ECs
bone (bone • Connected to the central system endomucin
marrow) vein • Niche for haematopoietic
• Hypoxic stem cells
• Surrounded by densely
packed haematopoietic cells
HEV ECs Lymph • Plump appearance Control homing and entry HEV sialomucins CD11c+ DC-derived 22
nodes and • Support tethering, rolling of lymphocytes and other (addressins), with lymphotoxin regulates
Reviewed
secondary and transmigration of immune cells (including 6‑sulpho sialyl HEV phenotype and
in 23
lymphoid immune cells precursors of conventional Lewis X on O- function in lymph
organs • Clonal expansion during DCs and NK cells) and N‑glycans, nodes
(except inflammation-induced and molecules
spleen); expansion of the lymph node involved in
non-lymphoid vasculature their synthesis
organs during (for example,
chronic GLYCAM1 and
inflammation FUT7), CD63,
and cancer CCL21
4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 1 (cont.) | Examples of organ-specific endothelial specialization
Type Location EC phenotypes Specialized function Molecular Molecular regulation Refs
of ECs and characteristics markers
Lymph Lymph nodes Different phenotypes in • Control size-selective CCL1 (SCS), VEGFC regulates Reviewed
node different parts of the LN entry of antigens (SCS) CCRL1 (also growth in 23,189
LECs: • DC entry (SCS) known as
• SCS • Lymphocyte egress ACKR4) (ceiling
• MS (MS and CS) of SCS), LYVE1
• CS • Antigen presentation and (all but ceiling
induction of peripheral of SCS), PLVAP,
immune tolerance S1P, PDL1
Lacteal Villi of • Lymphatic capillary-type ECs • Absorption of dietary Lymphatic VEGFC and DLL4 83,190
ECs the small • Combination of zipper and fats (chylomicrons) and capillary markers, maintain lacteals
intestine button-like junctions fat-soluble vitamins including LYVE1
• Continuous (low-level) • Entry for tissue-derived and CCL21
proliferation and sprouting DCs to mesenteric lymph
nodes allows induction
of oral tolerance
Meningeal Meninges Lymphatic capillary-type ECs • Drainage of Lymphatic VEGFC regulates 191,192
LECs cerebrospinal fluid capillary markers, growth
• Delivery of antigens and including LYVE1
immune cells to cervical and CCL21
lymph nodes
Schlemm’s Eye Circular ‘lymphatic-like’ vessel Drainage of aqueous LEC markers • Forms by postnatal 164,165,
canal ECs humour in between the except for PDPN migration of 166
lens and the cornea and LYVE1 venous-derived ECs
• VEGFC and ANG–
TIE2 regulate growth
ACE, angiotensin-converting enzyme; ALCAM, activated leukocyte cell adhesion molecule; ANG, angiopoietin; BBB, blood–brain barrier; CCL21, CC-chemokine
ligand 21; CCRL1, CC-chemokine receptor-like 1; CS, cortical sinus; DCs, dendritic cells; DLL4, Delta-like protein 4; ECs, endothelial cells; FUT7, fucosyl transferase 7;
GLUT1, glucose transporter 1; GLYCAM1, glycosylation-dependent cell adhesion molecule 1; HEV, high endothelial venule; HGF, hepatocyte growth factor;
HIF1, hypoxia-inducible factor 1; JAMs, junctional adhesion molecules; LECs, lymphatic ECs; LN, lymph node; LPL, lipoprotein lipase; LSECs, liver sinusoidal ECs;
LYVE1, lymphatic vessel endothelial hyaluronic acid receptor 1; MFSD2A, sodium-dependent lysophosphatidylcholine symporter 1; MS, medullary sinus; ND, not
determined; NK, natural killer; PDL1, programmed cell death 1 ligand 1; PDPN, podoplanin; PECAM1, platelet endothelial cell adhesion molecule; PLVAP,
plasmalemma vesicle-associated protein; PPARγ, peroxisome proliferator-activated receptor-γ; SCS, subcapsular sinus; SLC7A5, solute carrier family 7 member 5;
TCF15, transcription factor 15; TIE2, tyrosine kinase with Ig and EGF homology domains 2; VEGF, vascular endothelial growth factor.
The development of the vasculature arterial- and venous-fated ECs, which express ephrin B2
The development and growth of the vasculature are and ephrin type B receptor 4 (EPHB4), respectively 29,30.
intimately linked to the homeostatic needs of the t issue More recent studies have suggested that arterial and
that it serves. A shortage in nutrient and oxygen avail- venous ECs are derived from different pools of angio-
ability is the primary stimulus to form blood vessels, blasts that arise at distinct locations31. The existence
and increased interstitial fluid pressure is a driver of of additional angioblast pools is also suggested by the
lymphatic vessel growth in the developing embryo24. observation that loss‑of‑function mutants of Npas4l in
Depending on the developmental state, vascular bed zebrafish lead to a loss of most but not all ECs25.
or pathophysiological context, blood and lymphatic In mice, the first ECs similarly differentiate from
vessels can form through different mechanisms and mesodermal progenitors and coalesce into primitive
from v arious cellular origins. vessel networks at extra-embryonic and intra-embryonic
sites (FIG. 2a). NPAS4, the closest mammalian homologue
The formation of the first blood vessels through vasculo of Npas4l, is transiently expressed during EC lineage
genesis. The first blood vessels in development form by differentiation but is dispensable for mouse embryonic
a process known as vasculogenesis (FIG. 2a). In zebra development 25. The difference between fish and mice
fish, the basic helix–loop–helix-Per–ARNT–Sim might be rationalized by compensation through other
(bHLH-PAS) protein neuronal PAS domain-containing bHLH-PAS proteins, but could also indicate that a pre-
protein 4‑like protein (Npas4l) is at the top of a tran- dominantly NPAS4‑independent pool of angioblasts
Angioblasts scriptional hierarchy that instructs multipotent meso- forms the mammalian vasculature. Irrespective of the
Endothelial cell precursor cells dermal cells to differentiate into endothelial precursors precise origins, angioblast differentiation and function
that differentiate from the
known as angioblasts25. These angioblasts arise from the are controlled by several tissue-derived factors, including
mesoderm and form the first
embryonic blood vessels. posterior and anterior lateral plate mesoderm and assem- fibroblast growth factor 2 (FGF2), bone morphogenetic
ble into the large axial and cranial vessels, as well as the protein 4 (BMP4) and VEGF. FGF2 and BMP4 regulate
Mesoderm transient pharyngeal arch arteries26–28. Assembly of the mesoderm specification and EC differentiation, and
The middle layer of the three axial vessels is coupled to the establishment of the first VEGF seems to have a primary role in EC propagation
germ layers in the early
embryo, which forms
major artery and vein: the dorsal aorta and the cardinal and survival32. Another regulator is the hormonal pep-
connective tissues (including vein. Angioblasts were reported to first assemble into tide Elabela, which guides angioblasts to their proper
endothelium) and muscle. a common precursor v essel and to then segregate the position in the zebrafish embryo33.
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 5
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Lumen formation Expansion of the blood vasculature through angio ECs, known as tip cells, are migratory and invasive,
The formation of the interior genesis. Further growth of both the embryonic and and are thought to guide new sprouts. Tip cells are
space of a vessel through the adult vasculature is achieved through angiogenesis. followed by stalk cells, which elongate, proliferate and
which blood or lymph flows. Angiogenesis describes the formation of new vessels stabilize the nascent vessel and establish a lumen34,35
Membrane blebbing
from existing ones, during which ECs sprout, branch (FIG. 2b). Depending on the location and organism, lumen
Bulge or protrusion of the and connect, and subsequently remodel into functional formation can occur through different mechanisms,
plasma membrane, vessel circuits (FIG. 2b). This process requires ECs to including cord hollowing, vacuolar fusion and inverse
which is characterized adopt specialized phenotypes and functions. Leading membrane blebbing36,37. Lumenized sprouts eventually
by a spherical morphology.
a Vasculogenesis c Lymphangiogenesis
Intra-embryonic E10 cardinal vein
Dorsal aorta
PLLV
LEC differentiation
Cardinal vein and migration
pTD
Angioblasts Extra-embryonic
Sprouting and primary
plexus formation
Sprout
Blood islands
Primitive capillary
plexus E14 skin,
postnatal ear skin
b Angiogenesis CNS,
postnatal retina d Lymphvasculogenesis
Tip
Sprout
Stalk
Non-venous
(Primitive) capillary plexus LEC progenitor
E13–14 mesentery Primary plexus
e Tip and stalk cell specification
BMP9
VEGFC VEGFA BMP10
CCBE1
ADAMTS3 TGFβ
VEGF Mature
gradient VEGFC
VEGFR3 VEGFR2 NRP1 ALK1 ALK5
Tip cell Tip cell PFKFB3
specification
Tip cell
competiton DLL4 High glycolysis SMADs
Tip cell function Stalk cell
Tip cell and competition specification
DLL4
Stalk NOTCH1
cells Stalk cell ALK1 ALK5
VEGFR2
sVEGFR1 VEGFR3
NICD1 PFKFB3
NRP1
VEGFR1 SMADs
Canonical Notch targets
VEGFA (HES, HEY, NRARP)
VEGFR1
VEGFR2 Stalk cell specification
Nature Reviews | Molecular Cell Biology
6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Progenitor cells anastomose (that is, they fuse and become connected) from low-flow (veins) to high-flow (arteries) areas42
Early descendants of stem cells to neighbouring sprouts to generate new vascular (FIG. 3). Arteriovenous plasticity is also observed in other
that can divide a limited loops, either through sprout hollowing (generating a vascular beds that form via sprouting. For example, the
number of times and can multicellular tube) or through membrane invagination arterial and venous components of the gastrointestinal
differentiate into a few
cell types.
(resulting in a unicellular tube)38. The resulting blood vasculature in zebrafish have a common venous origin as
flow stabilizes new connections, and non-p erfused this vasculature arises from a pool of specialized angio-
segments regress39. Through iterative cycles of this blasts residing in the floor of the posterior cardinal vein
sprouting behaviour, ECs progressively expand the pri- (PCV)43 (FIG. 3). Other late-forming vascular beds also
mary vascular network. Pre-existing vasculature can emerge from various cellular sources. The coronary
also expand by vessel splitting — a process known as vasculature of the heart, for example, is formed by ECs
intussusception40. However, the cellular mechanisms of derived from the sinus venosus, pro-epicardium and
intussusception are poorly defined. endocardium that populate complementary regions of
the heart 44. The contribution of the endocardium to the
Tissue-specific mechanisms of vessel formation. coronary vasculature is only minimal in the embryonic
As development proceeds, new vascular beds form to heart 45. However, a population of endocardium-derived
support the growth and the function of various organs ECs generated through lineage conversion during
(FIG. 2). Some vascular beds arise through a combin trabecular compaction forms a substantial proportion
ation of vasculogenesis and angiogenesis, and others are of postnatal coronary vessels46. The formation of a vas-
formed exclusively by angiogenesis, such as the brain cular bed from various endothelial sources is an effective
and the retina. In these organs, angiogenic sprout- mechanism to ensure adequate vascularization of essen-
ing generates a plexus intermediate that subsequently tial organs, such as the heart. Interestingly, heart ECs are
remodels into a network of arteries, veins and capillar- also a source of mural cells, as endocardial ECs can con-
ies. Depending on the tissue characteristics, the cellular vert into progenitors of pericytes and vSMCs through
mechanisms of angiogenesis can differ. In the rigid bone endothelial-to‑mesenchymal transition47.
tissue, ECs do not form motile sprouts but instead organ- Although it is thought that most ECs have the ability
ize into columnar structures with multicellular buds that to proliferate and to contribute to the growth of vascular
fuse to form vessel arches41. The cellular dynamics of ECs beds, clonal expansion of ECs has also been reported
are also important for artery formation. In the retina, (FIG. 3). During inflammation-induced growth of the
for example, vein-derived tip cells continuously migrate lymph node vasculature, ECs of HEVs represent local
progenitors that undergo clonal proliferation to gen-
erate new lymph node capillaries and HEVs48. Studies
◀ Figure 2 | Mechanisms of vascular development. a | Endothelial progenitor cells, known in adult mice also suggested the existence of circula-
as angioblasts, differentiate from mesoderm, acquire arterial or venous fate, and assemble tory and vessel wall-resident progenitor cells that can be
into the first embryonic blood vessels: the dorsal aorta and the cardinal vein. In the activated to promote vessel growth on demand49 (FIG. 3).
extra-embryonic yolk sac, angioblasts first assemble into blood islands that fuse to form a However, their overall contribution to vascular growth
primary vessel network. b | Expansion of the network is achieved through angiogenesis
remains debatable.
that generates new vessels and vascular circuits from pre-existing ones through vessel
sprouting, branching and anastomosis. c | The first lymphatic endothelial cells (LECs)
transdifferentiate from venous endothelial cells in the cardinal vein between embryonic The development of the lymphatic vasculature.
day 9.5 (E9.5) and E9.75 and migrate out of the veins to form the first primitive lymphatic Lymphatic development begins only after functional
structures, the primordial thoracic duct (pTD) and the peripheral longitudinal lymphatic blood circulation is established. The first LECs are gen-
vessel (PLLV). Further expansion of the vasculature occurs through lymphangiogenic erated through transdifferentiation of blood ECs (BECs).
sprouting that generates a primary vascular plexus. d | Certain lymphatic vascular beds, This process is instigated by the transcription factor
such as the mesenteric vasculature, form through the lymphvasculogenic assembly of prospero homeobox protein 1 (PROX1) and occurs in
vessels from non-venous-derived progenitors. Lymphvasculogenesis is thought to be certain veins, such as the cardinal vein50. VEGFC, bind-
restricted to embryonic development, although lymphangiogenesis also occurs during ing to its receptor VEGF receptor 3 (VEGFR3), stimu-
postnatal development. Examples of tissues vascularized by the processes from parts a–d
lates the migration of LECs out of veins51. After exiting
are indicated in the cartoon illustrations of the mouse embryos. e | Key signalling
pathways that control blood vessel sprouting and tip cell and stalk cell specification. the veins as streams of cells, LECs assemble in the jugular
Tip cells express high levels of vascular endothelial growth factor receptor 2 (VEGFR2), region of the embryo into the first primitive vessels, the
VEGFR3 and the downstream target Delta-like protein 4 (DLL4) that activates Notch primordial thoracic ducts and the peripheral longitu-
signalling and establishes stalk cell behaviour in neighbouring cells. Stalk cell behaviour dinal lymphatic vessels50,52 (FIG. 2c). Venous sprouting
is actively suppressed in the tip cells by neuropilin 1 (NRP1)‑mediated inhibition of bone takes place in a few other locations in the embryo and
morphogenetic protein (BMP)–activin receptor-like kinase (ALK) signalling. Tip cells generates four additional primitive lymphatic structures
also show high glycolytic activity that promotes tip cell function and competitiveness. known as lymph sacs, which expand further through
Note that collagen and calcium-binding EGF domain-containing protein 1 lymphangiogenic sprouting (FIG. 2c). In zebrafish, the
(CCBE1)–a disintegrin and metalloproteinase with thrombospondin motifs 3 ventral wall of the cardinal vein was shown to harbour
(ADAMTS3)-mediated proteolytic processing and activation of VEGFC has so far only
specialized angioblasts that are a source of LECs53.
been shown in the context of lymphangiogenesis. Dashed arrow indicates reduced
signalling. CNS, central nervous system; HES, hairy and enhancer of split protein; Another study identified bi‑potential PROX1‑expressing
HEY, HES-related with YRPW motif protein; NICD1, NOTCH1 intracellular domain; precursors on the dorsal side of the vein that give rise to
NRARP, Notch-regulated ankyrin repeat-containing protein; PFKFB3, 6‑phosphofructo‑ LECs through differential daughter-cell fate determin
2‑kinase/fructose‑2,6‑bisphosphatase 3; SMAD, mothers against decapentaplegic ation following VEGFC-induced division54. Whether
homologue; sVEGFR1, soluble VEGFR1; TGFβ, transforming growth factor-β. ventral and dorsal precursors represent independent
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 7
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Clonal expansion of specialized ECs generates high Pre-existing ECs expand the vascular
endothelial venules and capillaries (lymph node) network by proliferation and migration
Tip cell Venous tip cells migrate against the
Integration of circulatory or flow and provide ECs for arteries
vessel wall-resident progenitors
Stalk cells
Capillary
network Lymphatic
capillaries
LECs migrating from
veins form lymphatic
Non-venous-derived LECs vasculature
of unknown origin contribute
to lymphatic vessels
Artery Collecting Vein
lymphatic vessel Progenitors from blood-
forming haemogenic
endothelium contribute
to lymphatic vessels by
lymphvasculogenesis
Specialized angioblasts
establish lymph vessels
and gastrointestinal
vasculature (zebrafish)
Blood islands
Different pools of angioblasts
form the first blood vessels
by vasculogenesis
Figure 3 | Origins and sources of ECs during vascular development. Mesoderm-derived angioblasts form the first
major vessels: the dorsal aorta and the cardinal vein. Expansion of the vasculature occurs through the proliferation of
pre-existing endothelial cells (ECs). Clonal expansion of local progenitors withinNature Reviews | Molecular
high endothelial venules hasCell
beenBiology
reported in the adult lymph node. Incorporation of circulating or vessel wall-resident endothelial progenitor cells may
also contribute to neovascularization in the adult. Vein-derived tip cells migrate against the blood flow and contribute
to the formation of arteries. The first LECs are generated through the transdifferentiation of venous ECs in the
cardinal vein (zebrafish, mammals) and the intersomitic vein (mammals). Specialized angioblasts on the floor of
the cardinal vein form both the gastrointestinal vasculature and LECs in zebrafish embryos. Non-venous-derived LEC
progenitors of haemogenic endothelial origin, or of as yet unknown origin, additionally contribute to the lymphatic
vasculature of certain organs.
pools of LEC progenitors, and whether they are also Together, these findings suggest that heterogeneity
present in mammalian veins, is unknown. in endothelial origin may contribute to tissue-specific
In addition to the venous source of LECs, alterna- formation and specialization of vessels. However, further
tive cellular origins have been described in the chick55, studies are needed to refine our understanding of the
as well as in the murine mesentery, skin and heart 56–59. different EC origins, their organ-specific contributions
The exact cellular origins are unclear except for the and their functional importance.
mesenteric vasculature, which was shown to form
Haemogenic endothelium through vasculogenic differentiation and assembly Regulation of vascular patterning
Specialized endothelial cells (lymphvasculogenesis) of Kit lineage cells derived from Newly formed vascular beds use signalling mechanisms
present in certain embryonic blood-forming haemogenic endothelium59 (FIG. 2d). The to adapt blood and lymphatic patterning to t issue
blood vessels, which can give
rise to haematopoietic cells
contribution of macrophages to lymphatic vasculature architecture and demand. Vessel density regulation fol-
during a restricted window has also been suggested, but could not be confirmed by lows some general principles but is also regulated in a
of development. lineage-tracing studies58,60. tissue-specific manner.
8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Regulation of vessel sprouting and branching by ECs use guidance molecules such as slits, netrins and
VEGFR signalling. A key trigger of the formation of ephrins, which bind to roundabout, UNC5 and EphB
new vessel branches is tissue hypoxia, which leads to receptors, respectively, to navigate nascent vessels77.
the secretion of pro-angiogenic growth factors and In some organs, vessels have been shown to co‑pattern
cytokines. The most extensively studied among these with nerves, with vessel-derived signals promoting the
is VEGF, which binds to VEGFRs on ECs to promote extensions of nerves and vice versa78. Reciprocal guid-
migration, proliferation and tip cell formation61. ECs ance mechanisms also exist between different types
with high activation of VEGFR2 and the VEGFC of vessels, as shown during the formation of zebrafish
receptor VEGFR3 become tip cells, and in these cells trunk and murine and chick mesenteric lymphatic
the expression of the Notch ligand Delta-like protein 4 vessels, where artery-derived CXC-chemokine ligand 12
(DLL4) is upregulated62 (FIG. 2e). DLL4 induces stalk cell (CXCL12; also known as SDF1) regulates the migration
behaviour in adjacent ECs by activating NOTCH1 sig- of CXCR4+ LECs57,79. Of note, vessel growth is also regu-
nalling, resulting in decreased expression of VEGFR2 lated in a vascular bed-specific manner. Growth factors
and VEGFR3 and increased expression of VEGFR1 such as VEGFB promote vascular expansion in certain
— a decoy receptor that sequesters VEGF. Tip cell and tissues, such as the heart and adipose tissue17,80. Another
stalk cell specification thus relies on differential VEGFR example is sprouting from the axial vein in zebrafish,
expression and relative VEGF sensitivities, which are which requires BMP but not VEGF signalling 81. In addi-
established through DLL4–NOTCH1 signalling 62,63. tion, canonical developmental pathways can have vas-
During sprouting, the levels of VEGFRs are constantly cular bed-specific roles. This is exemplified in the
changing as ECs face different environments, meet new blood vasculature of the bone and in the lacteals of the
cellular neighbours or undergo asymmetric cell divi- intestinal villi, where Notch does not restrict but rather
sion64–66. As a result, stalk cells can become tip cells and promotes (lymph)angiogenic sprouting 82,83.
vice versa, allowing dynamic position changes in the
growing vessel64. The dynamics of this tip cell and stalk Mechanical forces and metabolism regulate vessel
cell shuffling also led to the model that ECs acquire a sprouting and branching. In addition to hardwired
tip cell phenotype when DLL4–NOTCH1 is inactive. signal transduction cascades, mechanical forces that
However, more recent reports suggest that the stalk cell are imposed by blood flow provide another layer of
phenotype needs to be actively suppressed to allow tip regulation. In vitro and in vivo studies showed that
cell formation. This suppression is mediated by neuro both luminal and transmural flow regulate angiogenic
pilin 1 (NRP1), a co‑receptor for VEGF and semaphor- sprouting 84–86. Endothelial metabolism is also emerg-
ins, which establishes differential responsiveness to ing as a major determinant of tip and stalk behaviour
transforming growth factor-β (TGFβ)–BMP signalling 67 in the blood vasculature. This idea stems from the
(FIG. 2e). Consistent with these data, BMP9 and BMP10 realization that angiogenic sprouting is metabolically
support stalk cell specification by activating Notch demanding 87. BECs rely primarily on glycolysis and they
downstream target genes, and their inhibition causes increase flux through this pathway when activated by
endothelial hypersprouting 68–70. pro-angiogenic signals88. Enhanced glycolysis provides
As discussed above, another member of the VEGF a competitive advantage for BECs to become tip cells,
family, VEGFC, is the key regulator of lymphatic v essel as glycolysis-derived ATP drives EC rearrangement and
sprouting. It binds to the VEGF receptor VEGFR2, directional migration88. Conversely, reducing glycolysis
as well as to VEGFR3, which is mainly expressed in compromises vascular expansion, as shown by blockade
LECs. VEGFC activity is regulated by collagen and of the glycolytic activator 6‑phosphofructo‑2‑kinase/
calcium-binding EGF domain-containing protein 1 fructose‑2,6‑bisphosphatase 3 (PFKFB3)88. ECs also
(CCBE1)‑controlled and a disintegrin and metallo require fatty acid β‑oxidation (FAO) for vessel sprouting.
proteinase with thrombospondin motifs 3 (ADAMTS3)- FAO-derived carbons are used for nucleotide synthe-
mediated proteolytic cleavage (FIG. 2e), which ensures sis, which is required for DNA replication during EC
Transmural flow that lymphangiogenesis is spatially and temporally proliferation89. Emerging evidence suggests that LECs
Fluid flow through the controlled 71–73. Analogous to the requirement for also rely on FAO during lymph vessel growth90.
endothelial layer. NRP1 as a co‑receptor for VEGFR2 during VEGF-
induced blood vessel sprouting 61, NRP2 is essential Vessel regression contributes to vessel remodelling.
Glycolysis
An oxygen-independent
for VEGFC–VEGFR3‑induced lymphatic sprouting 74. Vessel density regulation involves not only the forma-
metabolic pathway that Several other known regulators of lymphatic sprouting tion of new vessel connections but also the removal of
converts glucose into pyruvate also exert their effect by influencing VEGFC–VEGFR3 unnecessary connections. This process is known as vessel
to generate energy and signalling. For example, TGFβ-mediated activation of regression. EC apoptosis underlies the programmed
biomass precursors.
TGFβ receptor type 2 (TGFBR2) and activin receptor- regression of the transient hyaloid vasculature and pupil-
Fatty acid β‑oxidation like kinase 5 (ALK5; also known as TGFBR1) promotes lary membrane in the eye91, but does not account for
(FAO). A catabolic process LEC sprouting by regulating VEGFR3 and NRP2 physiological regression in other vascular beds92. Instead,
in mitochondria during which expression75. Much less is known about the cellular dynamic rearrangements of ECs have been proposed as
fatty acids are broken down mechanisms of lymphatic vessel formation. Existing the central mechanism of regression that leads to retrac-
to generate substrates for
the tricarboxylic acid (TCA)
evidence suggests that, at least in certain vascu tion of ECs from non-perfused vessel segments93–96.
cycle and the electron lar beds, a similar tip cell and stalk cell-dependent Lymphatic vasculature is believed to undergo similar
transport chain. process occurs76. remodelling events, as illustrated by the process through
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 9
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Box 1 | Vascular instructive functions signalling, which are the major mitogenic signalling
cascades. Activating mutations in phosphatidylinositol-
Endothelial cells (ECs) are specialized by signals from the tissue environment, but they 4,5-bisphosphate 3-kinase catalytic subunit alpha
can also influence the tissue that they invade. Independently of their tissue-nourishing (PIK3CA), which encodes the p110α catalytic subunit of
function, ECs secrete growth factors, chemokines and extracellular matrix components, PI3K, drive venous and lymphatic malformations104–108,
or present signalling molecules on their cell surface, which act on cells in their vicinity.
and the inactivation of RAS p21 protein activator 1
These ‘angiocrine factors’ signal in a paracrine manner and instruct organ
morphogenesis, homeostasis and regeneration124,125. In the developing embryo, (RASA1), a negative regulator of RAS, causes capillary
for example, the formation and patterning of the heart, pancreas, liver, lung and kidney malformation-arteriovenous malformation109,110 and lym-
are regulated by EC‑derived signals, which leads to morphogenesis defects when ECs are phatic vessel hyperplasia111. RAS signalling seems to be a
absent . Organ homeostasis in adult mice is also instructed by angiocrine signals.
125 pivotal antagonist of LEC quiescence112,113, which couples
Studies in the liver have shown that the renewal of hepatocytes is guided by WNT signals growth factor signalling to the PI3K pathway 114.
that are deployed by ECs in the central vein of the liver lobule181. By producing WNT2 The phosphatase PTEN, a negative regulator
and WNT9B, these ECs maintain adjacent AXIN2‑expressing precursor cells that renew of PI3K–AKT signalling, and the transcription factor
the liver under homeostatic conditions. A different pattern of angiocrine signals forkhead box protein O1 (FOXO1), which is inactiv
mediates liver regeneration in response to injury. Liver sinusoidal ECs (LSECs) release ated by AKT-mediated phosphorylation, are critical
WNT2, hepatocyte growth factor (HGF) and angiopoietin 2 (ANG2), which together
drivers of quiescence in BECs115,116. PTEN is induced by
support the reconstitution of liver mass and function182,183. Interestingly, ANG2
coordinates hepatocyte and EC proliferation, thereby ensuring an adequate vascular DLL4–NOTCH1 and arrests cell cycle progression in
supply to the newly forming parenchyma183. However, unbalanced angiocrine signalling stalk cells115, and FOXO1 slows proliferative and meta
can also drive pathology, as shown in chronic liver injury in which prevalent bolic activity in ECs116. FOXO1‑induced quiescence relies
signalling by the stromal cell-derived factor 1 (SDF1) receptor CXCR4 causes fibrosis184. on the suppression of MYC, itself a potent activator of
Endothelial-derived signals also establish niches for stem and progenitor cells, endothelial proliferation, growth and metabolism116.
including haematopoietic stem cells, neural stem cells and spermatogonial stem cells124. Similar regulation of the metabolic and cell cycle machin-
A prime example is bone, in which specialized ECs help to sustain osteoprogenitor ery is caused by physiological laminar shear stress,
cells, the precursors of bone-forming cells, and haematopoietic stem cells (HSCs), which a well-known instigator of EC quiescence. The effects of
establish the haematopoietic system124,125. Osteoprogenitor cells associate with so‑called shear stress are transmitted by the transcription factor
type H endothelium that is found at the distal end of the bone arterial network. Type H
Krueppel-like f actor 2 (KLF2), which suppresses glyco-
ECs are characterized by the high expression of the endothelial markers PECAM1 and
endomucin and release essential osteogenic signals (for example, fibroblast growth lytic (for example, PFKFB3) and angiogenic (for example,
factors (FGFs), platelet-derived growth factors (PDGFs) and bone morphogenetic proteins VEGFR2) genes, among others117. Other quiescence-
(BMPs)), thereby promoting osteogenesis3. Of note, age-induced bone loss can be promoting factors in BECs are the BMP9 and BMP10
reversed by boosting type H vessel formation through hypoxia-inducible factor (HIF) proteins, which signal through ALK1 (also known as
and Notch3,82, suggesting that type H vessel-derived angiocrine signalling is essential for SKR3) and endoglin, and the cerebral cavernous malfor-
maintaining bone function. Endothelial Notch signalling also promotes the expansion of mation proteins (CCM1–3), the inactivation of which
HSC niches in the bone and involves type H ECs, the formation of arterioles and arteries, causes hyperplastic vascular malformations68,69,118,119.
and the expansion of perivascular cells185. Together, these data highlight the gatekeeper Unlike BECs, LECs promote quiescence in response to
function of the endothelium, and demonstrate that endothelial manipulation is sufficient oscillatory shear, mimicking disturbed flow, through a
to alter tissue differentiation, homeostasis and regeneration.
FOXC2‑dependent mechanism120. The inactivation of the
transcription factor FOXC2 causes a loss of quiescence,
which mesenteric collecting vessels form from a plexus which involves junction disassembly and TAZ-dependent
intermediate97,98. However, it is interesting to note that re‑entry into the cell cycle120.
although airway inflammation-driven changes in blood Of note, ECs in certain tissues maintain a proliferative
vessel remodelling subside after the resolution of the state or seem to be more susceptible to the re‑induction
inflammatory response, hyperplasia of lymphatic vessels of growth after they have become quiescent. For exam-
persists99,100. This suggests that there are different mech- ple, LECs in lacteals continuously proliferate, presumably
anisms of vessel remodelling in blood and lymphatic to cope with the permanently renewing environment of
vessels, at least during pathological conditions. the small intestine83. In addition, the activation of mech-
A key determining factor of regression is flow- anistic target of rapamycin complex 1 (mTORC1) or the
induced shear stress93–95, which has also been implicated inhibition of DLL4–NOTCH1 in adult mice causes loss of
in the functional specialization of both blood and lym- quiescence and vascular neoplasms in the skin and liver,
phatic vessels101–103. The influence of flow-dependent although other organs seem to be less affected121–123. It is
mechanical forces on vessel specialization is further unknown whether this tissue preference is a consequence
discussed below. of a particular tissue environment, vessel structure or
endothelial identity.
Vessel quiescence is important to maintain a functional
vascular network. After having established new vascu- Vessel specialization
lar networks, ECs resume quiescence. Quiescence is a Vascular specialization involves differentiation not only
reversible, non-dividing and non-migrating state that into arteries, veins and lymphatic vessels but also into
is common to most ECs in adult blood and lymphatic tissue-specific endothelia. Specialized ECs recipro
vessels, although relatively little is known about its regu cally shape their tissue environment by providing
lation. The importance of this regulation is, however, angiocrine signals that support organ development
highlighted in vascular pathologies that are caused by and function124,125 (BOX 1). Endothelial specialization
the aberrant activation of PI3K–AKT and RAS–MAPK can be instructed either by cell-intrinsic mechanisms,
10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Notochord which exhibit organ-restricted expression or activity, or sensory nerves are another source of VEGF that is
A transient midline structure by external tissue-derived signals, which act locally and required for arterial differentiation in the skin blood
that forms in chordate are dependent on the microenvironment. A few of these vasculature126. Arterial specification by VEGF depends
embryos, and which provides mechanisms are discussed below. on the activation of ERK signalling downstream of its
signals for the patterning
of the surrounding tissues.
receptors VEGFR2 and NRP1 (REF. 126). Sympathetic
Tissue-derived biochemical signals drive endothelial innervation can also promote arterial specification127.
differentiation. Biochemical signals have a key role Sympathetic nerve terminals produce noradrenaline that
in the first developmental event of EC specialization activates the ERK pathway through binding to endothe-
— the differentiation into arteries and veins (FIG. 4a). lial α1 and α2 adrenergic receptors127. Interestingly,
Notochord-derived sonic hedgehog induces VEGF, which ERK activation is also important for the specifica-
subsequently evokes arterial specification of angioblasts tion of LEC fate downstream of VEGFC–VEGFR3
that receive the highest VEGF signalling 31,32. Peripheral signalling 73,128,129 (FIG. 4a).
a
SHH VEGF Noradrenaline SOXF VEGFC
VEGFR2–NRP1 α1 and α2 NR2F2 NR2F2–SOX18 VEGFR3
SOXF FOXC
NR2F2
DLL4-dependent ERK Suppression of ERK
Notch signalling signalling Notch signalling PROX1 signalling
Arterial specification Venous specification Lymphatic specification
(e.g. SOX17, ephrin B2, NRP1) (e.g. NR2F2, EPHB4, NRP2) (e.g. PROX1, VEGFR3, LYVE1)
b Pericyte Steady
Immune
Tonic cell exit
Immune
cell entry
Capillary bed
Pulsatile
Lymphatic
capillary
Laminar flow
Reciprocating flow Phasic
Transmural flow and tonic
Tissue contraction Collecting
lymphatic vessel
Circumferential stretch
Artery Vein
SMC contraction
Intraluminal pressure
Figure 4 | Signals and mechanisms of specialization in the blood and lymph vasculature. a | The key signalling
pathways and transcriptional programmes that control endothelial cell (EC) identity. Dashed
Nature arrows
Reviews indicate that
| Molecular Cell VEGFC–
Biology
VEGFR3 signalling is required for the initiation of PROX1 expression in zebrafish but not in mice. b | ECs are confronted
with different types of mechanical forces that are generated by tissue elasticity and the pulling forces of neighbouring
cells, as well as flow-driven shear stress, luminal pressure, cyclic circumferential stretch, and cellular transmigration.
The magnitude and patterns of these forces differ depending on the organ or the vessel in which the ECs reside. Arteries
form a high-pressure system, which enables the directed transportation of blood to the capillary bed, whereas veins and
lymphatics face low-pressure gradients and have valves to prevent back flow. Organ function also generates mechanical
forces. Muscle contractions in skeletal muscle or in the heart exert strain on the vessel wall. ECs sense and transmit
different types of external forces primarily through their cell–cell and cell–extracellular matrix (ECM) adhesions, which
also generate intrinsic traction forces. The different types of forces exerted on ECs of different vessel types are indicated
by colour-coded arrows. α1, α1 adrenergic receptor; DLL4, Delta-like protein 4; EPHB4, ephrin type B receptor 4;
FOXC, forkhead box protein C; LYVE1, lymphatic vessel endothelial hyaluronic acid receptor 1; NR2F2, nuclear receptor
subfamily 2 group F member 2; NRP, neuropilin; PROX1, prospero homeobox protein 1; SHH, Sonic hedgehog;
SOXF, SRY-box group F; VEGF, vascular endothelial growth factor; VEGFR, VEGF receptor.
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 11
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Compared with our understanding of arteriovenous sets of transcription factors143, suggesting that combin
fate specification, much less is known about signals and atorial responses restrict endothelial phenotypes to
pathways that regulate the functional specialization of specific tissue compartments. However, the transcrip-
vessels. Examples include extracellular matrix (ECM)- tional patterns that establish tissue-specific endothelial
derived cues and signalling through β1 integrins, which differentiation have not yet been determined.
control EC subtype specification in the developing
bone130. Additional examples include the requirement of Mechanical forces as determinants of endothelial
continuous VEGF signalling for the maintenance of fenes- specialization. ECs face different types of mechan-
trated endothelium in adult tissues131, as well as the role of ical forces that are generated by the elasticity of the
the angiopoietin (ANG)–tyrosine kinase with Ig and EGF ECM, the pulling forces of their neighbours, as well as
homology domains 2 (TIE2) system in vessels adopting a flow-driven shear stress, luminal pressure, cyclic cir-
post-capillary venule phenotype that enables leukocyte cumferential stretch, and cellular transmigration9,144
adhesion during inflammation132. The formation of lym- (FIG. 4b). ECs sense and transmit external forces through
phatic valves is perhaps one of the best-described mech their cell–cell and cell–ECM adhesions, which also
anisms of functional specialization and involves several generate intrinsic traction forces. Endothelial glycocalyx
pathways, which include FOXC2–calcineurin– nuclear and primary cilia have additionally been implicated in
factor of activated T cells, cytoplasmic 1 (NFATC1), EC force sensing 145,146. Signalling pathways that convert
ephrin B2–EPHB4, connexin, α9 integrin–FN‑EIIIA mechanical information into biological responses — that
(fibronectin-EIIIA) and ANG–TIE signalling 9,133. is, mechanotransduction — and the effects of different
Signalling by ANG2–TIE2 is also crucial for the formation force types on BECs and LECs, have been reviewed
of button-like junctions in lymphatic capillaries134. elsewhere9,144,147. We focus below on the shear stress-
driven processes that are specifically implicated in vessel
Transcriptional programmes determine endothelial remodelling and specialization.
cell identity and specification. Transcriptional mech- Studies in chick embryos have demonstrated the piv-
anisms are essential not only for endothelial lineage otal role of blood flow in driving the remodelling of the
specification (FIG. 4a), but also for determining vessel- primitive yolk sac vasculature and the specialization of
and organ-specific EC identities. A prime example is the the arteries32,148. Shear stress controls the expression of
acquisition of arterial-venous differentiation, which is EC lineage-specific genes in a dosage-dependent manner.
co‑determined by a network of transcriptional regula- For example, ECs exposed to high shear stress show
tors. Among these are the FOXC and SOXF families of increased expression of the arterial genes EFNB2, NRP1
transcription factors, which drive arterial differentiation and GJA5 (which encodes connexin 40) (REFS 32,148).
partly by enhancing endothelial Notch signalling 135,136. Conversely, PROX1, which defines the identity of the
SOX17, for example, is enriched in the arterial endothe- low-flow lymphatic vessels, is downregulated under
lium of mice, and its deletion results in a failure to form high shear 149.
arteries137. Venous identity, conversely, is regulated by As discussed above, physiological laminar flow has
nuclear receptor subfamily 2 group F member 2 (NR2F2; a stabilizing effect and promotes EC quiescence, and
also known as COUPTF2), a transcriptional regulator long-term exposure to high or low shear induces vessel
that is expressed in venous and lymphatic ECs, but not in remodelling to adjust lumen diameter. Both blood ECs
arterial ECs32. Consistent with the central role of Notch and LECs respond to physiological laminar shear by
in determining arterial identity, NR2F2 promotes venous reorganizing their actin cytoskeleton and focal adhesions,
differentiation by suppressing Notch signalling. NR2F2 and by aligning in the direction of flow. However, under
is also involved in lymphatic differentiation. In venous high shear stress, ECs align perpendicular to the flow
LEC progenitors, NR2F2 and SOX18 transactivate the direction150. Although progress has been made in under-
master regulator of LEC fate, PROX1 (REFS 138,139), standing the general flow-sensing mechanisms144,147,
which subsequently drives its own expression by inter- much less is known about how ECs interpret shear
Haemangiomas acting with NR2F2 (REFS 140,141). In complex with stress magnitude and what determines the differential
Benign vascular tumours that PROX1, NR2F2 is u nable to suppress Notch target genes flow responses in endothelial subtypes. It has been pro-
are composed of an increased and instead supports LEC-specific gene expression140. posed that arterial ECs, venous ECs and LECs exhibit
number of endothelial cells. Although these transcription factors are crucial for different shear stress sensitivities, so-called set points,
Endothelial glycocalyx
specifying the general EC identity of vessel types, other that determine the range of shear stress within which to
Coating of the apical surface of transcription factors endow ECs with organ-specific respond9,144. The set point was suggested to be determined
endothelial cells, which is attributes. Examples include mesenchyme homeobox 2 by the levels of VEGFR3 (REF. 150), a component of the
composed of proteoglycans (MEOX2) and transcription factor 15 (TCF15), which platelet endothelial cell adhesion molecule 1 (PECAM1)–
and glycoproteins and which
programme heart ECs to efficiently transfer fatty acids to VE‑cadherin–VEGFR mechanosensory complex, which
has a role in mechanotransduc-
tion, signalling, haemostasis the myocardium15. Consistent with such tissue-restricted is highly expressed in low-flow lymphatic vessels, but
and blood cell interactions. transcriptional activities, the genetic manipulation of which has generally low expression in blood endothelia.
certain transcription factors leads to organ-specific vas- Different regions of the vascular tree face not only
Primary cilia cular phenotypes; for example, the inactivation of FOXOs different magnitudes but also different patterns of flow,
A non-motile
microtubule-based
causes organ-restricted haemangiomas that correlate with which range from pulsatile flow in arteries to lower con-
antenna-like sensory and organ-specific gene expression changes142. Furthermore, stant flow in veins, as well as complex flow patterns in
signalling organelle. ECs of each organ have been shown to express unique venous and lymphatic valves. The pattern of flow regulates
12 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Glaucoma
endothelial gene expression and cellular responses. For Tissue metabolites can also function as paracrine sig-
A group of eye diseases that is example, disturbed flow at vessel branch points provides nalling molecules. 3‑hydroxybutyrate is an intermediate
caused by damage to the optic a signal for the initiation of valve morphogenesis through of branched-chain amino acid metabolism that is prod
nerve and that results in loss the upregulation of the transcription factors FOXC2 uced in skeletal muscle and that stimulates fatty acid
of vision.
and GATA2 (REFS 102,120,151). Distinct flow patterns in transport across the endothelium to fuel lipid catabo
different regions of mature valves may further explain lism in myofibres160. Another example is lactate, the end
region-specific molecular and morphological differences product of glycolysis. ECs take up lactate from the extra-
and may determine the unique identity of valve ECs. This cellular milieu via the monocarboxylate transporter
has been highlighted by the shared expression of genes MCT1, which activates HIF signalling 161. ECs exposed
that were previously thought to be restricted to lym- to lactate also increase the expression of VEGF and other
phatic and/or to arterial endothelium, such as PROX1, receptor tyrosine kinase ligands, thus promoting their
FOXC2, ITGA9 and EFNB2, in both venous and lym- angiogenic behaviour 162.
phatic valves120,152,153. Besides intraluminal shear stresses,
lymphatic vessels and lymphatic capillaries, in particular, Vessel type- and vascular bed-specific diseases
are exposed to transmural flow, which was shown to pro- Vascular heterogeneity is apparent in many diseases2.
mote permeability and cell–cell junction reorganization154. For example, inflammatory blood vessel diseases often
Transmural flow may thus contribute to the specialization affect specific vessels or vascular beds, and systemic dis-
of button-like junctions in lymphatic capillaries. eases such as diabetes and hyperlipidaemia show pre-
Flow also regulates various aspects of vessel morpho- dilection sites for atherosclerotic lesion development.
genesis and function in disease states. Disturbed blood Certain tumours metastasize preferentially through
flow in vessel branch points, bifurcations and curvatures particular vascular beds, and signals from the tumour
promotes BEC proliferation and inflammatory activa- microenvironment determine tumour vessel hetero-
tion, and predisposes these sites to atherosclerosis144,155. geneity, which influences responsiveness to therapy 163.
Furthermore, the aetiology of certain vascular malfor- Perhaps the clearest examples of vessel type-restricted
mations is linked to abnormal flow regulation, which is or organ-restricted disease manifestation are vascular
further discussed below. malformations. These diseases commonly arise from
abnormalities in ECs and are categorized according to
Metabolism influences endothelial cell heterogeneity. the vessel type that is perturbed (TABLE 2). Sequencing
ECs are exposed to various environments that differ in efforts have identified causative mutations for each
oxygen tension, nutrient abundance and metabolite accu- type of malformation (TABLE 2). For example, activating
mulation. For example, ECs at the blood–air b arrier in mutations in TIE2 or in its downstream effector PIK3CA
the lung face high oxygen levels, whereas ECs in the bone cause the majority of venous malformations that lead
marrow cavity or in the lymphatic vessels are confronted to the most common vascular malformations104,107–109.
with relatively hypoxic conditions. The influence of Somatic activating mutations in PIK3CA also account
such metabolic environments on endothelial specializa for the majority of lymphatic malformations 105,106.
tion has not yet been studied in detail. However, given Mutations in TIE2 have not been observed in lymphatic
the ability of ECs to sense and to respond to metabolic malformations but have been found in another organ-
cues87, it seems likely that tissue metabolism provides a type-specific vascular disease that affects the Schlemm’s
range of signals that contribute to EC heterogeneity. For canal — a lymphatic-like vessel that collects aqueous
example, the differentiation of mesodermal progenitors humour from the eye164–166. TIE2 haploinsufficiency
into angioblasts is stimulated by low levels of oxygen causes Schlemm’s canal hypoplasia that provokes
and involves signalling by hypoxia-inducible factors primary congenital g laucoma in humans167.
(HIFs)156. Oxygen abundance also affects EC metabo- In addition to affecting specific vessel types, vas-
lism, with consequences for endothelial bioenergetics cular malformations can manifest in an organ-specific
and function. A shortage of oxygen impedes enzymatic manner. Cerebral cavernous malformations (CCMs),
reactions that require oxygen (for example, FAO) and for example, are vascular malformations of venous
disrupts the redox balance157. In addition to oxygen, origin that primarily affect the central nervous system
altered nutrient availability can redirect metabolic fluxes (CNS)119. The enlarged and rupture-prone lesions arise
and can thereby lead to the accumulation of metabolites from loss‑of‑function mutations in one of the three
that affect signalling and gene expression. An example CCM genes (CCM1–3). The proteins encoded by these
is acetyl coenzyme A (acetyl-CoA), which is a central genes function in a complex that controls junctional
metabolite of energy metabolism, and which contains organization and polarity. Increased RHOA activation in
an acetyl group that is required for the post-translational CCM lesions has been found to contribute to junctional
modification of proteins157. Studies in LECs have shown disintegration168, and defective flow responses, aberrant
that FAO-derived acetyl-CoA contributes to lymphatic angiogenesis and TGFβ–BMP-induced endothelial-
gene expression, as it is used by the acetyltransferase p300 to-mesenchymal transition were shown to promote
to acetylate histones at PROX1‑target genes90. Other stud- lesion formation169–171. Further studies have shown
ies have demonstrated that non-histone proteins such as that the loss of CCM proteins results in the increased
VEGFR2 and NOTCH1 are also regulated by acetyl- activity of MAPK/ERK kinase kinase 3 (MEKK3) and
ation158,159, which suggests that endothelial function is its flow-responsive targets Krüppel-like factor 2 (KLF2)
modulated in tune with metabolic resources. and KLF4 (REFS 171–173). The proangiogenic versus the
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 13
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
vasoprotective roles of KLF2 in low-flow versus high- increases in lesion number 174. Interestingly, angio-
flow vessels, respectively, were proposed to be a potential genic stimuli are also required for the induction of
explanation for why veins are more prone to forming arteriovenous malformations (AVMs) in mice lacking
CCM lesions171. However, the reasons for the CNS- the TGFβ type I receptor, ALK1, which model human
restricted occurrence of CCMs are not clear. Factors hereditary haemorrhagic telangiectasia (HHT)175. The
from the neurovascular microenvironment may be rupture-prone AVMs in HHT form from direct connec-
important. As lesion formation requires on‑going angio tions between arteries and veins and are found in the
genesis170,174, it is possible that the brain vasculature, brain, as well as in the lungs, liver and gastrointestinal
owing to its late development, is particularly sensitive tract. Defective BMP–ALK1–endoglin-dependent, flow-
to CCM formation. Cerebral ischaemia-induced angio induced inhibition of EC proliferation and mural cell
genesis could additionally explain ageing-associated recruitment was suggested to underlie AVM formation
Table 2 | Examples of organ- and vessel type-specific vascular abnormalities and their underlying mutations
Affected Main affected Disease Disease manifestation and proposed Gene Type of mutation Refs
vessel type organs mechanism
Vein Mucosa, skin and Cutaneomucosal Dilated veins with thick fibrotic walls TIE2 Inherited and somatic 193
muscle venous malformation and irregular SMC coverage; defective (second-hit) activating
(VMCM) communication between ECs and SMCs
Vein Skin, subcutis; Sporadic venous Dilated veins with thick fibrotic walls TIE2 Somatic activating 194
also mucosa, malformation and irregular SMC coverage; defective
muscle, joints, communication between ECs and SMCs
gastrointestinal
tract, lung and brain
Vein Subcutis, mucosa, Sporadic venous Dilated or interconnected veins with PIK3CA Somatic activating 104,
muscle and joints malformation thick fibrotic walls and irregular SMC 107,
coverage; defective communication 108
between ECs and SMCs
Vein Skin (palms Blue rubber bleb nevus Dilated veins with thick fibrotic TIE2 Two somatic activating 195
and soles), (BRBN) syndrome walls and irregular SMC coverage, mutations on the same
gastrointestinal haemorrhaging; defective allele
tract communication between ECs and SMCs
Vein Skin, subcutis in Glomeruvenous Undifferentiated SMCs (glomus cells) GLMN Inherited and somatic 196
extremities malformation (GVN) around distended vein-like channels; (second-hit)
defect in SMC differentiation leading to inactivating
defective vessel maturation
Lymphatic Any tissue except Lymphatic Malformed, dilated and dysfunctional PIK3CA Somatic activating 105,
vessel brain malformation lymphatic channels (microcystic) or 106
large cyst-like cavities containing lymph
(macrocystic)
Lymphatic Feet (up to the Milroy disease (primary Swelling of lower limbs; lack of FLT4 Inherited heterozygous 197
vessel knees) lymphoedema) lymphatic drainage due to hypoplasia or (which inactivating
(capillary) dysfunction of lymphatic capillaries encodes
VEGFR3)
Lymphatic Lower limbs Lymphoedema Swelling of lower limbs; retrograde FOXC2 Inherited heterozygous 198,
vessel distichiasis (LD; lymph flow due to lack of lymphatic inactivating 199
(collecting) primary lymphoedema) valves
Mixed CM: skin; AVM: Capillary malformation- Overactivation of RAS–MAPK RASA1 Inherited heterozygous 110
CNS, extremities arteriovenous signalling leading to abnormal vessel and somatic (second-
malformation (CM‑AVM) development hit) inactivating
Mixed Telangiectasias: Hereditary Dilatation of post-capillary venules ENG, Inherited heterozygous 200–
skin, mucosa; AVM: haemorrhagic with excessive layers of SMCs. AVMs ALK1, inactivating 202
lung, liver, brain telangiectasia (HHT) due to defects in flow-induced vascular SMAD4
stabilization
Mixed CNS Cerebral cavernous Dilated blood vessels with multiple CCM1–3 Somatic (sporadic); or 203–
(capillary- malformation (CCM) caverns; defect in EC cell–cell junctions inherited and somatic 206
venous) (second-hit)
inactivating (familial)
Schlemm’s Eye Primary congenital Hypoplasia of Schlemm’s canal TIE2 Inherited heterozygous 167
canal glaucoma inactivating
(haploinsufficiency)
ALK1, activin receptor-like kinase 1; AVM, arteriovenous malformation; CCM, cerebral cavernous malformations; CM, capillary malformation; CNS, central nervous
system; EC, endothelial cell; ENG, endoglin; FOXC2, forkhead box C2; GLMN, glomulin; PIK3CA, phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit
alpha; RASA1, RAS p21 protein activator 1; SMAD4, mothers against decapentaplegic homologue 4; SMC, smooth muscle cell; TIE2, tyrosine kinase with Ig and EGF
homology domains 2; VEGFR3, vascular endothelial growth factor receptor 3.
14 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Lymphoedema
in mice118. Imaging of the initial flow-dependent stages are beginning to provide insights into the mechanisms
Fluid accumulation and tissue of AVM formation in zebrafish176,177 instead revealed the that govern organ- and vessel type-specific endothelial
swelling due to dysfunction impaired migration of ALK1‑deficient cells against differentiation, and they point to the complexity of the
of the lymphatic vessels. the flow, leading to an increase in distal arterial calibre mechanisms involved. However, our understanding of
and EC n umber 178. Overall, these studies suggest endothelial heterogeneity is in its infancy, and numer-
that disruption of endothelial flow response mech ous fundamental questions remain. For example, what
anisms contributes to the f ormation of different types of are the origins and sources of organ-specific ECs and
vascular malformations. how do they influence vessel specialization? Is endothe-
In addition to lymphatic malformations, genetic lial specialization bounded by cell-autonomous mech
diseases of the lymphatic system include hereditary anisms or is it imposed by the microenvironment?
lymphoedema, the clinical forms of which are classified What are the key signals and pathways and how are
according to the underlying mutation and the disease they regulated? Although the role of growth factor sig-
phenotype, including the affected body part179. Currently, nalling cascades and transcription factors is currently
more than 20 causative genes have been identified, many the best-understood aspect of tissue-specific endothelial
of which centre on VEGFR3 signalling and the resultant differentiation, it seems likely that the role of mechanical
reduction in pathway activity 180. Interestingly, some of forces and metabolism will continue to gain increasing
these mutations primarily affect either collecting vessels attention in the future. Although these signals are not
or lymphatic capillaries. For example, Milroy disease, EC‑specific, they may establish a particular environ-
which is caused by inactivating mutations in VEGFR3, ment or cellular state that is permissive for endothelial
is characterized by hypoplasia and/or by dysfunction of differentiation. In this context, it will be of particular
the lymphatic capillaries133. Of note, VEGFR3 is pres- interest to investigate the link between tissue environ-
ent in all LECs, and it remains unclear what determines ment, endothelial epigenetic state and phenotype, given
vessel-type specific disease manifestation. recent studies that highlight the influence of metabolism
on epigenetics and cellular differentiation157. Such stud-
Conclusions and perspectives ies will also need to take into account the source of ECs
Molecular, morphological and functional heterogene- used for analysis. Until now, most in vitro studies in the
ity within the endothelium is increasingly recognized vascular field have been based on a limited number of
in both normal and disease conditions, and it is now EC model systems (for example, human umbilical vein
established that this heterogeneity affects the vascular ECs (HUVECs) and human dermal LECs (HDLECs)),
architecture, structure and function. The diversity of which ignore tissue-specific differences in phenotype
phenotypes that ECs can adopt suggests substantial and function. Addressing these questions and chal-
plasticity and indicates that heterogeneity is a core lenges promises to reveal exciting new perspectives on
endothelial property that allows ECs to fulfil their multi the mechanisms of vascular development and function,
ple tasks. Tissue- and cell type-specific genetic models with implications for a variety of vascular diseases.
1. Aspelund, A., Robciuc, M. R., Karaman, S., 10. Zhao, Z., Nelson, A. R., Betsholtz, C. & Zlokovic, B. V. 21. Tarlungeanu, D. C. et al. Impaired amino acid
Makinen, T. & Alitalo, K. Lymphatic system in Establishment and dysfunction of the blood–brain transport at the blood brain barrier is a cause of
cardiovascular medicine. Circ. Res. 118, 515–530 barrier. Cell 163, 1064–1078 (2015). autism spectrum disorder. Cell 167, 1481–1494.
(2016). 11. Ben-Zvi, A. et al. Mfsd2a is critical for the formation e18 (2016).
2. Aird, W. C. Endothelial cell heterogeneity. Cold Spring and function of the blood–brain barrier. Nature 509, This study demonstrates a crucial function
Harb. Perspect. Med. 2, a006429 (2012). 507–511 (2014). of endothelial SLC7A5 in transporting
3. Kusumbe, A. P., Ramasamy, S. K. & Adams, R. H. 12. Nguyen, L. N. et al. Mfsd2a is a transporter for the branched-chain amino acids across the BBB
Coupling of angiogenesis and osteogenesis by essential omega‑3 fatty acid docosahexaenoic acid. and thereby maintaining normal brain function.
a specific vessel subtype in bone. Nature 507, Nature 509, 503–506 (2014). 22. Lee, M. et al. Transcriptional programs of lymphoid
323–328 (2014). 13. Itkin, T. et al. Distinct bone marrow blood vessels tissue capillary and high endothelium reveal control
These studies characterize two distinct differentially regulate haematopoiesis. Nature 532, mechanisms for lymphocyte homing. Nat. Immunol.
capillary subtypes in the bone vasculature, 323–328 (2016). 15, 982–995 (2014).
which have key roles in maintaining the cells 14. Baluk, P. et al. Functionally specialized junctions 23. Girard, J. P., Moussion, C. & Forster, R. HEVs,
of the bone- and blood-forming system. between endothelial cells of lymphatic vessels. lymphatics and homeostatic immune cell trafficking
4. Di Russo, J. et al. Vascular laminins in physiology J. Exp. Med. 204, 2349–2362 (2007). in lymph nodes. Nat. Rev. Immunol. 12, 762–773
and pathology. Matrix Biol. 57–58, 140–148 15. Coppiello, G. et al. Meox2/Tcf15 heterodimers (2012).
(2016). program the heart capillary endothelium for cardiac 24. Planas-Paz, L. et al. Mechanoinduction of lymph
5. Armulik, A. et al. Pericytes regulate the blood–brain fatty acid uptake. Circulation 131, 815–826 (2015). vessel expansion. EMBO J. 31, 788–804 (2012).
barrier. Nature 468, 557–561 (2010). 16. Hagberg, C. E. et al. Vascular endothelial growth This study implicates interstitial fluid
In this study, the critical regulatory role of factor B controls endothelial fatty acid uptake. Nature pressure-induced cell stretching in the
pericytes at the BBB is demonstrated. 464, 917–921 (2010). activation of VEGFR3 and the induction
6. Armulik, A., Genove, G. & Betsholtz, C. Pericytes: 17. Kivela, R. et al. VEGF‑B‑induced vascular growth of lymphatic vascular expansion.
developmental, physiological, and pathological leads to metabolic reprogramming and ischemia 25. Reischauer, S. et al. Cloche is a bHLH-PAS
perspectives, problems, and promises. Dev. Cell 21, resistance in the heart. EMBO Mol. Med. 6, transcription factor that drives haemato-
193–215 (2011). 307–321 (2014). vascular specification. Nature 535, 294–298
7. Hall, C. N. et al. Capillary pericytes regulate cerebral 18. Dijkstra, M. H. et al. Lack of cardiac and high-fat diet (2016).
blood flow in health and disease. Nature 508, 55–60 induced metabolic phenotypes in two independent This study identifies Npas4l as the gene that
(2014). strains of Vegf‑b knockout mice. Sci. Rep. 4, 6238 is mutated in the avascular zebrafish cloche
8. Hill, R. A. et al. Regional blood flow in the normal (2014). mutant.
and ischemic brain is controlled by arteriolar smooth 19. Winkler, E. A. et al. GLUT1 reductions exacerbate 26. Paffett-Lugassy, N. et al. Heart field origin of great
muscle cell contractility and not by capillary pericytes. Alzheimer’s disease vasculo-neuronal dysfunction vessel precursors relies on nkx2.5‑mediated
Neuron 87, 95–110 (2015). and degeneration. Nat. Neurosci. 18, 521–530 vasculogenesis. Nat. Cell Biol. 15, 1362–1369
9. Sabine, A., Saygili Demir, C. & Petrova, T. V. (2015). (2013).
Endothelial cell responses to biomechanical forces 20. Jais, A. et al. Myeloid-cell-derived VEGF maintains 27. Proulx, K., Lu, A. & Sumanas, S. Cranial vasculature
in lymphatic vessels. Antioxid. Redox Signal. 25, brain glucose uptake and limits cognitive impairment in zebrafish forms by angioblast cluster-derived
451–465 (2016). in obesity. Cell 165, 882–895 (2016). angiogenesis. Dev. Biol. 348, 34–46 (2010).
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 15
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
28. Siekmann, A. F., Standley, C., Fogarty, K. E., 53. Nicenboim, J. et al. Lymphatic vessels arise from 78. Jones, C. A. & Li, D. Y. Common cues regulate neural
Wolfe, S. A. & Lawson, N. D. Chemokine signaling specialized angioblasts within a venous niche. Nature and vascular patterning. Curr. Opin. Genet. Dev. 17,
guides regional patterning of the first embryonic 522, 56–61 (2015). 332–336 (2007).
artery. Genes Dev. 23, 2272–2277 (2009). 54. Koltowska, K. et al. Vegfc regulates bipotential 79. Cha, Y. R. et al. Chemokine signaling directs trunk
29. Herbert, S. P. et al. Arterial-venous segregation by precursor division and Prox1 expression to promote lymphatic network formation along the preexisting
selective cell sprouting: an alternative mode of blood lymphatic identity in zebrafish. Cell Rep. 13, blood vasculature. Dev. Cell 22, 824–836 (2012).
vessel formation. Science 326, 294–298 (2009). 1828–1841 (2015). 80. Robciuc, M. R. et al. VEGFB/VEGFR1‑induced
30. Lindskog, H. et al. Molecular identification of venous This study demonstrates that LEC differentiation expansion of adipose vasculature counteracts obesity
progenitors in the dorsal aorta reveals an aortic origin is achieved through differential daughter cell fate and related metabolic complications. Cell Metab. 23,
for the cardinal vein in mammals. Development 141, determination following venous progenitor cell 712–724 (2016).
1120–1128 (2014). division in zebrafish. 81. Wiley, D. M. et al. Distinct signalling pathways
31. Kohli, V., Schumacher, J. A., Desai, S. P., Rehn, K. 55. Wilting, J. et al. Dual origin of avian lymphatics. regulate sprouting angiogenesis from the dorsal
& Sumanas, S. Arterial and venous progenitors of Dev. Biol. 292, 165–173 (2006). aorta and the axial vein. Nat. Cell Biol. 13, 686–692
the major axial vessels originate at distinct locations. 56. Klotz, L. et al. Cardiac lymphatics are heterogeneous (2011).
Dev. Cell 25, 196–206 (2013). in origin and respond to injury. Nature 522, 62–67 82. Ramasamy, S. K., Kusumbe, A. P., Wang, L.
32. Marcelo, K. L., Goldie, L. C. & Hirschi, K. K. Regulation (2015). & Adams, R. H. Endothelial Notch activity promotes
of endothelial cell differentiation and specification. 57. Mahadevan, A. et al. The left–right Pitx2 pathway angiogenesis and osteogenesis in bone. Nature 507,
Circ. Res. 112, 1272–1287 (2013). drives organ-specific arterial and lymphatic 376–380 (2014).
33. Helker, C. S. et al. The hormonal peptide Elabela development in the intestine. Dev. Cell 31, 690–706 83. Bernier-Latmani, J. et al. DLL4 promotes continuous
guides angioblasts to the midline during (2014). adult intestinal lacteal regeneration and dietary fat
vasculogenesis. eLife 4, e06726 (2015). 58. Martinez-Corral, I. et al. Nonvenous origin of dermal transport. J. Clin. Invest. 125, 4572–4586 (2015).
34. Potente, M., Gerhardt, H. & Carmeliet, P. Basic lymphatic vasculature. Circ. Res. 116, 1649–1654 84. Galie, P. A. et al. Fluid shear stress threshold regulates
and therapeutic aspects of angiogenesis. Cell 146, (2015). angiogenic sprouting. Proc. Natl Acad. Sci. USA 111,
873–887 (2011). 59. Stanczuk, L. et al. cKit lineage hemogenic 7968–7973 (2014).
35. Betz, C., Lenard, A., Belting, H. G. & Affolter, M. endothelium-derived cells contribute to mesenteric 85. Ghaffari, S., Leask, R. L. & Jones, E. A. Flow dynamics
Cell behaviors and dynamics during angiogenesis. lymphatic vessels. Cell Rep. 10, 1708–1721 (2015). control the location of sprouting and direct elongation
Development 143, 2249–2260 (2016). 60. Gordon, E. J. et al. Macrophages define dermal during developmental angiogenesis. Development
36. Charpentier, M. S. & Conlon, F. L. Cellular and lymphatic vessel calibre during development by 142, 4151–4157 (2015).
molecular mechanisms underlying blood vessel lumen regulating lymphatic endothelial cell proliferation. 86. Song, J. W. & Munn, L. L. Fluid forces control
formation. Bioessays 36, 251–259 (2014). Development 137, 3899–3910 (2010). endothelial sprouting. Proc. Natl Acad. Sci. USA 108,
37. Gebala, V., Collins, R., Geudens, I., Phng, L. K. 61. Simons, M., Gordon, E. & Claesson-Welsh, L. 15342–15347 (2011).
& Gerhardt, H. Blood flow drives lumen formation Mechanisms and regulation of endothelial VEGF 87. Potente, M. & Carmeliet, P. M. The link between
by inverse membrane blebbing during angiogenesis receptor signalling. Nat. Rev. Mol. Cell Biol. 17, angiogenesis and endothelial metabolism. Annu. Rev.
in vivo. Nat. Cell Biol. 18, 443–450 (2016). 611–625 (2016). Physiol. 79, 43–66 (2017).
This study identifies a novel mechanism of lumen 62. Blanco, R. & Gerhardt, H. VEGF and Notch in tip and 88. De Bock, K. et al. Role of PFKFB3‑driven glycolysis
formation in the angiogenic sprout, which involves stalk cell selection. Cold Spring Harb. Perspect. Med. in vessel sprouting. Cell 154, 651–663 (2013).
pressure-driven inverse membrane blebbing 3, a006569 (2013). In this study, the importance of metabolic
of ECs. 63. Zarkada, G., Heinolainen, K., Makinen, T., Kubota, Y. regulation and 6-phosphofructo-2-kinase/fructose-
38. Herwig, L. et al. Distinct cellular mechanisms of blood & Alitalo, K. VEGFR3 does not sustain retinal 2,6-bisphosphatase 3 (PFKFB3)‑driven glycolysis
vessel fusion in the zebrafish embryo. Curr. Biol. 21, angiogenesis without VEGFR2. Proc. Natl Acad. for endothelial sprouting is revealed.
1942–1948 (2011). Sci. USA 112, 761–766 (2015). 89. Schoors, S. et al. Fatty acid carbon is essential for
39. Korn, C. & Augustin, H. G. Mechanisms of vessel 64. Jakobsson, L. et al. Endothelial cells dynamically dNTP synthesis in endothelial cells. Nature 520,
pruning and regression. Dev. Cell 34, 5–17 (2015). compete for the tip cell position during angiogenic 192–197 (2015).
40. Gianni-Barrera, R., Trani, M., Reginato, S. & Banfi, A. sprouting. Nat. Cell Biol. 12, 943–953 (2010). 90. Wong, B. W. et al. The role of fatty acid beta-
To sprout or to split? VEGF, Notch and vascular 65. Nakayama, M. et al. Spatial regulation of VEGF oxidation in lymphangiogenesis. Nature 542, 49–54
morphogenesis. Biochem. Soc. Trans. 39, 1644–1648 receptor endocytosis in angiogenesis. Nat. Cell Biol. (2017).
(2011). 15, 249–260 (2013). 91. Lobov, I. B. et al. WNT7b mediates macrophage-
41. Ramasamy, S. K. et al. Blood flow controls bone 66. Costa, G. et al. Asymmetric division coordinates induced programmed cell death in patterning of
vascular function and osteogenesis. Nat. Commun. collective cell migration in angiogenesis. Nat. Cell Biol. the vasculature. Nature 437, 417–421 (2005).
7, 13601 (2016). 18, 1292–1301 (2016). 92. Watson, E. C. et al. Apoptosis regulates endothelial
42. Xu, C. et al. Arteries are formed by vein-derived This study demonstrates that asymmetric cell number and capillary vessel diameter but not
endothelial tip cells. Nat. Commun. 5, 5758 (2014). cell division contributes to tip cell and stalk vessel regression during retinal angiogenesis.
This paper shows that venous tip cells contribute cell selection. Development 143, 2973–2982 (2016).
to the formation of arteries by migrating against 67. Aspalter, I. M. et al. Alk1 and Alk5 inhibition by Nrp1 93. Chen, Q. et al. Haemodynamics-driven developmental
the direction of flow. controls vascular sprouting downstream of Notch. pruning of brain vasculature in zebrafish. PLoS Biol.
43. Hen, G. et al. Venous-derived angioblasts generate Nat. Commun. 6, 7264 (2015). 10, e1001374 (2012).
organ-specific vessels during zebrafish embryonic 68. Larrivee, B. et al. ALK1 signaling inhibits angiogenesis 94. Franco, C. A. et al. Dynamic endothelial cell
development. Development 142, 4266–4278 (2015). by cooperating with the Notch pathway. Dev. Cell 22, rearrangements drive developmental vessel
44. Chen, H. I. et al. The sinus venosus contributes to 489–500 (2012). regression. PLoS Biol. 13, e1002125 (2015).
coronary vasculature through VEGFC-stimulated 69. Ricard, N. et al. BMP9 and BMP10 are critical for 95. Kochhan, E. et al. Blood flow changes coincide with
angiogenesis. Development 141, 4500–4512 (2014). postnatal retinal vascular remodeling. Blood 119, cellular rearrangements during blood vessel pruning
45. Zhang, H. et al. Endocardium minimally contributes 6162–6171 (2012). in zebrafish embryos. PLoS ONE 8, e75060 (2013).
to coronary endothelium in the embryonic ventricular 70. Moya, I. M. et al. Stalk cell phenotype depends on 96. Lenard, A. et al. Endothelial cell self-fusion during
free walls. Circ. Res. 118, 1880–1893 (2016). integration of Notch and Smad1/5 signaling cascades. vascular pruning. PLoS Biol. 13, e1002126 (2015).
46. Tian, X. et al. Vessel formation. De novo formation Dev. Cell 22, 501–514 (2012). 97. Bazigou, E. et al. Integrin‑alpha9 is required for
of a distinct coronary vascular population in neonatal 71. Jeltsch, M. et al. CCBE1 enhances lymphangiogenesis fibronectin matrix assembly during lymphatic valve
heart. Science 345, 90–94 (2014). via A disintegrin and metalloprotease with morphogenesis. Dev. Cell 17, 175–186 (2009).
47. Chen, Q. et al. Endothelial cells are progenitors of thrombospondin motifs‑3‑mediated vascular 98. Norrmen, C. et al. FOXC2 controls formation and
cardiac pericytes and vascular smooth muscle cells. endothelial growth factor‑C activation. Circulation maturation of lymphatic collecting vessels through
Nat. Commun. 7, 12422 (2016). 129, 1962–1971 (2014). cooperation with NFATc1. J. Cell Biol. 185, 439–457
48. Mondor, I. et al. Clonal proliferation and stochastic 72. Bui, H. M. et al. Proteolytic activation defines distinct (2009).
pruning orchestrate lymph node vasculature lymphangiogenic mechanisms for VEGFC and VEGFD. 99. Baluk, P. et al. Pathogenesis of persistent lymphatic
remodeling. Immunity 45, 877–888 (2016). J. Clin. Invest. 126, 2167–2180 (2016). vessel hyperplasia in chronic airway inflammation.
This study identifies local progenitor cells within 73. Le Guen, L. et al. Ccbe1 regulates Vegfc-mediated J. Clin. Invest. 115, 247–257 (2005).
high endothelial venules, which proliferate clonally induction of Vegfr3 signaling during embryonic 100. Yao, L. C., Baluk, P., Feng, J. & McDonald, D. M.
during inflammation-induced expansion of the lymphangiogenesis. Development 141, 1239–1249 Steroid-resistant lymphatic remodeling in chronically
lymph node vasculature. (2014). inflamed mouse airways. Am. J. Pathol. 176,
49. Basile, D. P. & Yoder, M. C. Circulating and tissue 74. Xu, Y. et al. Neuropilin‑2 mediates VEGF‑C‑induced 1525–1541 (2010).
resident endothelial progenitor cells. J. Cell. Physiol. lymphatic sprouting together with VEGFR3. J. Cell 101. Sweet, D. T. et al. Lymph flow regulates collecting
229, 10–16 (2014). Biol. 188, 115–130 (2010). lymphatic vessel maturation in vivo. J. Clin. Invest.
50. Yang, Y. et al. Lymphatic endothelial progenitors 75. James, J. M., Nalbandian, A. & Mukouyama, Y. S. 125, 2995–3007 (2015).
bud from the cardinal vein and intersomitic vessels TGFbeta signaling is required for sprouting 102. Sabine, A. et al. Mechanotransduction, PROX1,
in mammalian embryos. Blood 120, 2340–2348 lymphangiogenesis during lymphatic network and FOXC2 cooperate to control connexin37 and
(2012). development in the skin. Development 140, calcineurin during lymphatic-valve formation. Dev. Cell
51. Karkkainen, M. J. et al. Vascular endothelial growth 3903–3914 (2013). 22, 430–445 (2012).
factor C is required for sprouting of the first lymphatic 76. Zheng, W. et al. Notch restricts lymphatic vessel 103. Noble, F. et al. Flow regulates arterial–venous
vessels from embryonic veins. Nat. Immunol. 5, sprouting induced by vascular endothelial growth differentiation in the chick embryo yolk sac.
74–80 (2004). factor. Blood 118, 1154–1162 (2011). Development 131, 361–375 (2004).
52. Hagerling, R. et al. A novel multistep mechanism 77. Adams, R. H. & Eichmann, A. Axon guidance 104. Limaye, N. et al. Somatic activating PIK3CA mutations
for initial lymphangiogenesis in mouse embryos based molecules in vascular patterning. Cold Spring Harb. cause venous malformation. Am. J. Hum. Genet. 97,
on ultramicroscopy. EMBO J. 32, 629–644 (2013). Perspect. Biol. 2, a001875 (2010). 914–921 (2015).
16 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
105. Luks, V. L. et al. Lymphatic and other vascular 129. Deng, Y., Atri, D., Eichmann, A. & Simons, M. 154. Miteva, D. O. et al. Transmural flow modulates cell
malformative/overgrowth disorders are caused Endothelial ERK signaling controls lymphatic fate and fluid transport functions of lymphatic
by somatic mutations in PIK3CA. J. Pediatr. 166, specification. J. Clin. Invest. 123, 1202–1215 (2013). endothelium. Circ. Res. 106, 920–931 (2010).
1048–1054.e5 (2015). 130. Langen, U. H. et al. Cell-matrix signals specify bone 155. Morbiducci, U. et al. Atherosclerosis at arterial
106. Osborn, A. J. et al. Activating PIK3CA alleles and endothelial cells during developmental osteogenesis. bifurcations: evidence for the role of haemodynamics
lymphangiogenic phenotype of lymphatic endothelial Nat. Cell Biol. 19, 189–201 (2017). and geometry. Thromb. Haemost. 115, 484–492
cells isolated from lymphatic malformations. 131. Kamba, T. et al. VEGF-dependent plasticity of (2016).
Hum. Mol. Genet. 24, 926–938 (2015). fenestrated capillaries in the normal adult 156. Ramirez-Bergeron, D. L. et al. Hypoxia affects
107. Castillo, S. D. et al. Somatic activating mutations in microvasculature. Am. J. Physiol. Heart Circ. Physiol. mesoderm and enhances hemangioblast specification
Pik3ca cause sporadic venous malformations in mice 290, H560–H576 (2006). during early development. Development 131,
and humans. Sci. Transl Med. 8, 332ra43 (2016). 132. Fuxe, J. et al. Angiopoietin/Tie2 signaling transforms 4623–4634 (2004).
108. Castel, P. et al. Somatic PIK3CA mutations as a driver capillaries into venules primed for leukocyte trafficking 157. Pavlova, N. N. & Thompson, C. B. The emerging
of sporadic venous malformations. Sci. Transl Med. 8, in airway inflammation. Am. J. Pathol. 176, hallmarks of cancer metabolism. Cell Metab. 23,
332ra42 (2016). 2009–2018 (2010). 27–47 (2016).
109. Uebelhoer, M., Boon, L. M. & Vikkula, M. Vascular 133. Koltowska, K., Betterman, K. L., Harvey, N. L. 158. Zecchin, A. et al. Reversible acetylation regulates
anomalies: from genetics toward models for & Hogan, B. M. Getting out and about: the emergence vascular endothelial growth factor receptor‑2 activity.
therapeutic trials. Cold Spring Harb. Perspect. Med. 2, and morphogenesis of the vertebrate lymphatic J. Mol. Cell Biol. 6, 116–127 (2014).
a009688 (2012). vasculature. Development 140, 1857–1870 (2013). 159. Guarani, V. et al. Acetylation-dependent regulation of
110. Eerola, I. et al. Capillary malformation-arteriovenous 134. Zheng, W. et al. Angiopoietin 2 regulates the endothelial Notch signalling by the SIRT1 deacetylase.
malformation, a new clinical and genetic disorder transformation and integrity of lymphatic endothelial Nature 473, 234–238 (2011).
caused by RASA1 mutations. Am. J. Hum. Genet. 73, cell junctions. Genes Dev. 28, 1592–1603 (2014). 160. Jang, C. et al. A branched-chain amino acid
1240–1249 (2003). 135. Corada, M., Morini, M. F. & Dejana, E. Signaling metabolite drives vascular fatty acid transport and
111. Lapinski, P. E. et al. RASA1 maintains the lymphatic pathways in the specification of arteries and veins. causes insulin resistance. Nat. Med. 22, 421–426
vasculature in a quiescent functional state in mice. Arterioscler. Thromb. Vasc. Biol. 34, 2372–2377 (2016).
J. Clin. Invest. 122, 733–747 (2012). (2014). 161. Vegran, F., Boidot, R., Michiels, C., Sonveaux, P.
112. Ichise, T., Yoshida, N. & Ichise, H. H−, N− and Kras 136. Hermkens, D. M. et al. Sox7 controls arterial & Feron, O. Lactate influx through the endothelial cell
cooperatively regulate lymphatic vessel growth specification in conjunction with hey2 and efnb2 monocarboxylate transporter MCT1 supports
by modulating VEGFR3 expression in lymphatic function. Development 142, 1695–1704 (2015). an NF‑kappaB/IL‑8 pathway that drives tumor
endothelial cells in mice. Development 137, 137. Corada, M. et al. Sox17 is indispensable for angiogenesis. Cancer Res. 71, 2550–2560 (2011).
1003–1013 (2010). acquisition and maintenance of arterial identity. 162. Ruan, G. X. & Kazlauskas, A. Lactate engages receptor
113. Roth Flach, R. J. et al. Endothelial mitogen-activated Nat. Commun. 4, 2609 (2013). tyrosine kinases Axl, Tie2, and vascular endothelial
protein kinase kinase kinase kinase 4 is critical 138. Srinivasan, R. S. et al. The nuclear hormone receptor growth factor receptor 2 to activate phosphoinositide
for lymphatic vascular development and function. Coup-TFII is required for the initiation and early 3‑kinase/Akt and promote angiogenesis. J. Biol. Chem.
Mol. Cell. Biol. 36, 1740–1749 (2016). maintenance of Prox1 expression in lymphatic 288, 21161–21172 (2013).
114. Gupta, S. et al. Binding of ras to phosphoinositide endothelial cells. Genes Dev. 24, 696–707 (2010). 163. Phoenix, T. N. et al. Medulloblastoma genotype
3‑kinase p110alpha is required for ras-driven 139. Francois, M. et al. Sox18 induces development dictates blood brain barrier phenotype. Cancer Cell
tumorigenesis in mice. Cell 129, 957–968 (2007). of the lymphatic vasculature in mice. Nature 456, 29, 508–522 (2016).
115. Serra, H. et al. PTEN mediates Notch-dependent stalk 643–647 (2008). 164. Park, D. Y. et al. Lymphatic regulator PROX1
cell arrest in angiogenesis. Nat. Commun. 6, 7935 140. Aranguren, X. L. et al. COUP-TFII orchestrates determines Schlemm’s canal integrity and identity.
(2015). venous and lymphatic endothelial identity by J. Clin. Invest. 124, 3960–3974 (2014).
116. Wilhelm, K. et al. FOXO1 couples metabolic activity homo- or hetero-dimerisation with PROX1. J. Cell Sci. 165. Aspelund, A. et al. The Schlemm’s canal is a
and growth state in the vascular endothelium. Nature 126, 1164–1175 (2013). VEGF‑C/VEGFR‑3‑responsive lymphatic-like vessel.
529, 216–220 (2016). 141. Lee, S. et al. Prox1 physically and functionally J. Clin. Invest. 124, 3975–3986 (2014).
This paper identifies the forkhead transcription interacts with COUP-TFII to specify lymphatic 166. Kizhatil, K., Ryan, M., Marchant, J. K., Henrich, S.
factor FOXO1 as a key driver of endothelial endothelial cell fate. Blood 113, 1856–1859 (2009). & John, S. W. Schlemm’s canal is a unique vessel
quiescence, which lowers EC metabolism through 142. Paik, J. H. et al. FoxOs are lineage-restricted with a combination of blood vascular and lymphatic
the suppression of MYC signalling. redundant tumor suppressors and regulate phenotypes that forms by a novel developmental
117. Doddaballapur, A. et al. Laminar shear stress inhibits endothelial cell homeostasis. Cell 128, 309–323 process. PLoS Biol. 12, e1001912 (2014).
endothelial cell metabolism via KLF2‑mediated (2007). 167. Souma, T. et al. Angiopoietin receptor TEK mutations
repression of PFKFB3. Arterioscler. Thromb. Vasc. 143. Nolan, D. J. et al. Molecular signatures of tissue- underlie primary congenital glaucoma with variable
Biol. 35, 137–145 (2015). specific microvascular endothelial cell heterogeneity expressivity. J. Clin. Invest. 126, 2575–2587 (2016).
118. Baeyens, N. et al. Defective fluid shear stress in organ maintenance and regeneration. Dev. Cell 26, 168. Stockton, R. A., Shenkar, R., Awad, I. A.
mechanotransduction mediates hereditary 204–219 (2013). & Ginsberg, M. H. Cerebral cavernous malformations
hemorrhagic telangiectasia. J. Cell Biol. 214, This paper exemplifies the molecular heterogeneity proteins inhibit Rho kinase to stabilize vascular
807–816 (2016). within the endothelium showing that organ-specific integrity. J. Exp. Med. 207, 881–896 (2010).
119. Fischer, A., Zalvide, J., Faurobert, E., Albiges-Rizo, C. ECs express unique combinations of transcription 169. Maddaluno, L. et al. EndMT contributes to the onset
& Tournier-Lasserve, E. Cerebral cavernous factors and signalling molecules. and progression of cerebral cavernous malformations.
malformations: from CCM genes to endothelial cell 144. Baeyens, N., Bandyopadhyay, C., Coon, B. G., Yun, S. Nature 498, 492–496 (2013).
homeostasis. Trends Mol. Med. 19, 302–308 (2013). & Schwartz, M. A. Endothelial fluid shear stress 170. Mleynek, T. M. et al. Lack of CCM1 induces
120. Sabine, A. et al. FOXC2 and fluid shear stress stabilize sensing in vascular health and disease. J. Clin. Invest. hypersprouting and impairs response to flow.
postnatal lymphatic vasculature. J. Clin. Invest. 125, 126, 821–828 (2016). Hum. Mol. Genet. 23, 6223–6234 (2014).
3861–3877 (2015). 145. Tarbell, J. M., Simon, S. I. & Curry, F. R. 171. Renz, M. et al. Regulation of beta1
This study shows how mechanical forces generated Mechanosensing at the vascular interface. Annu. Rev. integrin‑Klf2‑mediated angiogenesis by CCM proteins.
by recirculating flow in valve regions define identity, Biomed. Eng. 16, 505–532 (2014). Dev. Cell 32, 181–190 (2015).
and how the mechanosensitive transcription factor 146. Goetz, J. G. et al. Endothelial cilia mediate low flow 172. Cuttano, R. et al. KLF4 is a key determinant in the
FOXC2 maintains the quiescence and integrity sensing during zebrafish vascular development. development and progression of cerebral cavernous
of the lymphatic endothelium. Cell Rep. 6, 799–808 (2014). malformations. EMBO Mol. Med. 8, 6–24 (2015).
121. Sun, S. et al. Constitutive activation of mTORC1 147. Kutys, M. L. & Chen, C. S. Forces and 173. Zhou, Z. et al. Cerebral cavernous malformations arise
in endothelial cells leads to the development and mechanotransduction in 3D vascular biology. from endothelial gain of MEKK3–KLF2/4 signalling.
progression of lymphangiosarcoma through VEGF Curr. Opin. Cell Biol. 42, 73–79 (2016). Nature 532, 122–126 (2016).
autocrine signaling. Cancer Cell 28, 758–772 (2015). 148. Buschmann, I. et al. Pulsatile shear and Gja5 174. Boulday, G. et al. Developmental timing of CCM2 loss
122. Yan, M. et al. Chronic DLL4 blockade induces vascular modulate arterial identity and remodeling events influences cerebral cavernous malformations in mice.
neoplasms. Nature 463, E6–E7 (2010). during flow-driven arteriogenesis. Development 137, J. Exp. Med. 208, 1835–1847 (2011).
123. Liu, Z. et al. Notch1 loss of heterozygosity causes 2187–2196 (2010). 175. Park, S. O. et al. Real-time imaging of de novo
vascular tumors and lethal hemorrhage in mice. 149. Chen, C. Y. et al. Blood flow reprograms lymphatic arteriovenous malformation in a mouse model of
J. Clin. Invest. 121, 800–808 (2011). vessels to blood vessels. J. Clin. Invest. 122, hereditary hemorrhagic telangiectasia. J. Clin. Invest.
124. Rafii, S., Butler, J. M. & Ding, B. S. Angiocrine 2006–2017 (2012). 119, 3487–3496 (2009).
functions of organ-specific endothelial cells. Nature 150. Baeyens, N. et al. Vascular remodeling is governed 176. Corti, P. et al. Interaction between alk1 and blood flow
529, 316–325 (2016). by a VEGFR3‑dependent fluid shear stress set point. in the development of arteriovenous malformations.
125. Ramasamy, S. K., Kusumbe, A. P. & Adams, R. H. eLife 4, e04645 (2015). Development 138, 1573–1582 (2011).
Regulation of tissue morphogenesis by endothelial cell- 151. Kazenwadel, J. et al. GATA2 is required for lymphatic 177. Laux, D. W. et al. Circulating Bmp10 acts through
derived signals. Trends Cell Biol. 25, 148–157 (2015). vessel valve development and maintenance. J. Clin. endothelial Alk1 to mediate flow-dependent arterial
126. Simons, M. & Eichmann, A. Molecular controls of Invest. 125, 2979–2994 (2015). quiescence. Development 140, 3403–3412 (2013).
arterial morphogenesis. Circ. Res. 116, 1712–1724 152. Munger, S. J. et al. Segregated Foxc2, NFATc1 178. Rochon, E. R., Menon, P. G. & Roman, B. L. Alk1
(2015). and Connexin expression at normal developing venous controls arterial endothelial cell migration in
127. Pardanaud, L. et al. Sympathetic innervation valves, and connexin-specific differences in the valve lumenized vessels. Development 143, 2593–2602
promotes arterial fate by enhancing endothelial phenotypes of Cx37, Cx43, and Cx47 knockout mice. (2016).
ERK activity. Circ. Res. 119, 607–620 (2016). Dev. Biol. 412, 173–190 (2016). 179. Connell, F. C. et al. The classification and diagnostic
128. Shin, M. et al. Vegfc acts through ERK to induce 153. Bazigou, E. et al. Genes regulating lymphangiogenesis algorithm for primary lymphatic dysplasia: an update
sprouting and differentiation of trunk lymphatic control venous valve formation and maintenance in from 2010 to include molecular findings. Clin. Genet.
progenitors. Development 143, 3785–3795 (2016). mice. J. Clin. Invest. 121, 2984–2992 (2011). 84, 303–314 (2013).
NATURE REVIEWS | MOLECULAR CELL BIOLOGY ADVANCE ONLINE PUBLICATION | 17
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
180. Brouillard, P., Boon, L. & Vikkula, M. Genetics of 192. Louveau, A. et al. Structural and functional features haemorrhagic telangiectasia type 1. Nat. Genet. 8,
lymphatic anomalies. J. Clin. Invest. 124, 898–904 of central nervous system lymphatic vessels. Nature 345–351 (1994).
(2014). 523, 337–341 (2015). 203. Sahoo, T. et al. Mutations in the gene encoding KRIT1,
181. Wang, B., Zhao, L., Fish, M., Logan, C. Y. & Nusse, R. This study, together with reference 189, a Krev‑1/rap1a binding protein, cause cerebral
Self-renewing diploid Axin2+ cells fuel homeostatic identifies lymphatic vessels in the meninges and cavernous malformations (CCM1). Hum. Mol. Genet.
renewal of the liver. Nature 524, 180–185 (2015). demonstrates their role in draining cerebrospinal 8, 2325–2333 (1999).
182. Ding, B. S. et al. Inductive angiocrine signals fluid and immune cells from the brain, thus 204. Liquori, C. L. et al. Mutations in a gene encoding
from sinusoidal endothelium are required for liver challenging the immune-privileged status a novel protein containing a phosphotyrosine-
regeneration. Nature 468, 310–315 (2010). of the CNS. binding domain cause type 2 cerebral cavernous
183. Hu, J. et al. Endothelial cell-derived angiopoietin‑2 193. Limaye, N. et al. Somatic mutations in angiopoietin malformations. Am. J. Hum. Genet. 73, 1459–1464
controls liver regeneration as a spatiotemporal receptor gene TEK cause solitary and multiple (2003).
rheostat. Science 343, 416–419 (2014). sporadic venous malformations. Nat. Genet. 41, 205. Laberge‑le Couteulx, S. et al. Truncating mutations
184. Ding, B. S. et al. Divergent angiocrine signals from 118–124 (2009). in CCM1, encoding KRIT1, cause hereditary
vascular niche balance liver regeneration and fibrosis. 194. Vikkula, M. et al. Vascular dysmorphogenesis caused cavernous angiomas. Nat. Genet. 23, 189–193
Nature 505, 97–102 (2014). by an activating mutation in the receptor tyrosine (1999).
185. Kusumbe, A. P. et al. Age-dependent modulation of kinase TIE2. Cell 87, 1181–1190 (1996). 206. Bergametti, F. et al. Mutations within the programmed
vascular niches for haematopoietic stem cells. Nature 195. Soblet, J. et al. Blue rubber bleb nevus (BRBN) cell death 10 gene cause cerebral cavernous
532, 380–384 (2016). syndrome is caused by somatic TEK (TIE2) mutations. malformations. Am. J. Hum. Genet. 76, 42–51
186. Aird, W. C. Phenotypic heterogeneity of the J. Invest. Dermatol. 137, 207–216 (2017). (2005).
endothelium: II. Representative vascular beds. 196. Brouillard, P. et al. Mutations in a novel factor,
Circ. Res. 100, 174–190 (2007). glomulin, are responsible for glomuvenous Acknowledgements
187. LeCouter, J. et al. Angiogenesis-independent malformations (“glomangiomas”). Am. J. Hum. Genet. There is much outstanding work in the field that could not be
endothelial protection of liver: role of VEGFR‑1. 70, 866–874 (2002). cited in this Review owing to space constraints and so the
Science 299, 890–893 (2003). 197. Karkkainen, M. J. et al. Missense mutations interfere authors ask the forbearance of their colleagues. The authors
188. Klein, D. et al. Wnt2 acts as a cell type-specific, with VEGFR‑3 signalling in primary lymphoedema. thank M. Fiedler for assistance with the artwork. M.P. is
autocrine growth factor in rat hepatic sinusoidal Nat. Genet. 25, 153–159 (2000). supported by the Max Planck Society, the European Research
endothelial cells cross-stimulating the VEGF pathway. 198. Finegold, D. N. et al. Truncating mutations in FOXC2 Council (ERC) Starting Grant ANGIOMET (311546), the
Hepatology 47, 1018–1031 (2008). cause multiple lymphedema syndromes. Hum. Mol. Deutsche Forschungsgemeinschaft (SFB 834), the Excellence
189. Ulvmar, M. H. & Makinen, T. Heterogeneity Genet. 10, 1185–1189 (2001). Cluster Cardiopulmonary System (EXC 147/1), the LOEWE
in the lymphatic vascular system and its origin. 199. Fang, J. et al. Mutations in FOXC2 (MFH‑1), grant Ub‑Net, the DZHK (German Center for Cardiovascular
Cardiovasc. Res. 111, 310–321 (2016). a forkhead family transcription factor, are responsible Research), the Stiftung Charité and the European Molecular
190. Nurmi, H. et al. VEGF‑C is required for intestinal for the hereditary lymphedema-distichiasis syndrome. Biology Organization Young Investigator Programme. The
lymphatic vessel maintenance and lipid absorption. Am. J. Hum. Genet. 67, 1382–1388 (2000). work of T.M. is funded by the Swedish Research Council, the
EMBO Mol. Med. 7, 1418–1425 (2015). 200. Gallione, C. J. et al. A combined syndrome of juvenile Swedish Cancer Foundation, the European Research
191. Aspelund, A. et al. A dural lymphatic vascular polyposis and hereditary haemorrhagic telangiectasia Council (ERC‑2014‑CoG‑646849) and Knut and Alice
system that drains brain interstitial fluid and associated with mutations in MADH4 (SMAD4). Wallenberg Foundation.
macromolecules. J. Exp. Med. 212, 991–999 Lancet 363, 852–859 (2004).
(2015). 201. Johnson, D. W. et al. Mutations in the activin Competing interests statement
This study identifies lymphatic vessels in the receptor‑like kinase 1 gene in hereditary The authors declare no competing interests.
meninges and demonstrates their role in draining haemorrhagic telangiectasia type 2. Nat. Genet. 13,
cerebrospinal fluid and immune cells from the 189–195 (1996). Publisher’s note
brain, thus challenging the immune-privileged 202. McAllister, K. A. et al. Endoglin, a TGF-beta binding Springer Nature remains neutral with regard to jurisdictional
status of the CNS. protein of endothelial cells, is the gene for hereditary claims in published maps and institutional affiliations.
18 | ADVANCE ONLINE PUBLICATION www.nature.com/nrm
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Clinical Pathways Dan Sistem Drgs Casemix SMF Jantung & Kedokteran Vaskular Rsud Kota Cilegon 2018 Unstable Angina Pektoris (ICD 10: ..)Dokument3 SeitenClinical Pathways Dan Sistem Drgs Casemix SMF Jantung & Kedokteran Vaskular Rsud Kota Cilegon 2018 Unstable Angina Pektoris (ICD 10: ..)flying highNoch keine Bewertungen
- Goland Et Al 2016 Angiogenic Imbalance and Residual Myocardial Injury in Recovered Peripartum Cardiomyopathy PatientsDokument7 SeitenGoland Et Al 2016 Angiogenic Imbalance and Residual Myocardial Injury in Recovered Peripartum Cardiomyopathy Patientsflying highNoch keine Bewertungen
- Recent Advances in Pulmonary HypertensionDokument12 SeitenRecent Advances in Pulmonary Hypertensionflying highNoch keine Bewertungen
- Takahashi2016Dokument11 SeitenTakahashi2016flying highNoch keine Bewertungen
- 47 PH in Patient With Hyperthyroidism-Dres - Niemeyer EN PDFDokument4 Seiten47 PH in Patient With Hyperthyroidism-Dres - Niemeyer EN PDFflying highNoch keine Bewertungen
- Incidence of Pulmonary Hypertension in Hyperthyroid PatientsDokument4 SeitenIncidence of Pulmonary Hypertension in Hyperthyroid Patientsflying highNoch keine Bewertungen
- Stem CellDokument22 SeitenStem Cellflying highNoch keine Bewertungen
- Anti-Inflammatory Nanomedicine For Cardiovascular DiseaseDokument13 SeitenAnti-Inflammatory Nanomedicine For Cardiovascular Diseaseflying highNoch keine Bewertungen
- Hubungan Kelas Nyha Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu/Rsup Prof. Dr. R.D. Kandou ManadoDokument8 SeitenHubungan Kelas Nyha Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu/Rsup Prof. Dr. R.D. Kandou Manadoflying highNoch keine Bewertungen
- Mesenchymal Stem Cells in Cardiac Regeneration: A Detailed Progress Report of The Last 6 Years (2010 - 2015)Dokument25 SeitenMesenchymal Stem Cells in Cardiac Regeneration: A Detailed Progress Report of The Last 6 Years (2010 - 2015)flying highNoch keine Bewertungen
- Colloids and Surfaces B: Biointerfaces: Christina Mckee, G. Rasul ChaudhryDokument16 SeitenColloids and Surfaces B: Biointerfaces: Christina Mckee, G. Rasul Chaudhryflying highNoch keine Bewertungen
- hubungan Kadar Tnf-α Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu - rsup Prof. Dr. r.d. Kandou ManadoDokument6 Seitenhubungan Kadar Tnf-α Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu - rsup Prof. Dr. r.d. Kandou Manadoflying highNoch keine Bewertungen
- Educational Program Cardiovascular Regenerative Medicine School 2018Dokument3 SeitenEducational Program Cardiovascular Regenerative Medicine School 2018flying highNoch keine Bewertungen
- Mesenchymal Stem Cell Paracrine Factors in Vascular Repair and RegenerationDokument9 SeitenMesenchymal Stem Cell Paracrine Factors in Vascular Repair and Regenerationflying highNoch keine Bewertungen
- s2 2016 354560 BibliographyDokument4 Seitens2 2016 354560 Bibliographyflying highNoch keine Bewertungen
- Rupture of Vulnerable Atherosclerotic Plaques: Micrornas Conducting The Orchestra?Dokument8 SeitenRupture of Vulnerable Atherosclerotic Plaques: Micrornas Conducting The Orchestra?flying highNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Kawasaki Disease: BackgroundDokument10 SeitenKawasaki Disease: BackgroundAmarantoNoch keine Bewertungen
- Gram Positive Vs Gram NegativeDokument9 SeitenGram Positive Vs Gram NegativeOdior VictorNoch keine Bewertungen
- In Text Citation: Reference/Bibliography StyleDokument6 SeitenIn Text Citation: Reference/Bibliography StyleStanley_Ipviss_4553Noch keine Bewertungen
- Alpha InterferonDokument7 SeitenAlpha InterferonLAURA MARCELA BARRENECHE CALLENoch keine Bewertungen
- Manor Supplementary Notes PCOGDokument32 SeitenManor Supplementary Notes PCOGBenjamin TNoch keine Bewertungen
- 833Dokument169 Seiten833MarcNicaNoch keine Bewertungen
- Lesson Plan-Parts of A CellDokument8 SeitenLesson Plan-Parts of A Cellapi-298069969Noch keine Bewertungen
- Biological Classification - Grade 11 & 12Dokument26 SeitenBiological Classification - Grade 11 & 12Ishita Singh100% (1)
- Immunology (Levinson)Dokument93 SeitenImmunology (Levinson)ECFMGNoch keine Bewertungen
- Christine Schaffner 2020 Beginners Guide To Your Lymphatics BBMDokument14 SeitenChristine Schaffner 2020 Beginners Guide To Your Lymphatics BBMLauren100% (1)
- PicornavirusDokument23 SeitenPicornavirusMj BrionesNoch keine Bewertungen
- CH 49 MedsurgDokument18 SeitenCH 49 MedsurgJiezl Abellano AfinidadNoch keine Bewertungen
- Prepared For The Coronavirus - 9 Simulations, Drills & Laws Planned For It - 28-04-2020 - Makia Freeman - Thefreedomarticles PDFDokument29 SeitenPrepared For The Coronavirus - 9 Simulations, Drills & Laws Planned For It - 28-04-2020 - Makia Freeman - Thefreedomarticles PDFWolf GantNoch keine Bewertungen
- IMSEDokument5 SeitenIMSEharith r donovanNoch keine Bewertungen
- What Is Gene Therapy?Dokument2 SeitenWhat Is Gene Therapy?Alister KingNoch keine Bewertungen
- Cambridge International AS & A Level: Biology 9700/21Dokument18 SeitenCambridge International AS & A Level: Biology 9700/21Lavanya EaswarNoch keine Bewertungen
- Food IrradiationDokument53 SeitenFood Irradiationapi-3700321Noch keine Bewertungen
- Campeel IutDokument86 SeitenCampeel IutRosa TorresNoch keine Bewertungen
- اسئلة امتحان الأحياء ف2 ثنائية اللغةDokument118 Seitenاسئلة امتحان الأحياء ف2 ثنائية اللغةomanfastsolutionNoch keine Bewertungen
- Sesiones Carteles-1Dokument92 SeitenSesiones Carteles-1Manuel Nolasco QuirogaNoch keine Bewertungen
- Bio Cell TheoryDokument22 SeitenBio Cell TheoryCHLOE BEA DILLANoch keine Bewertungen
- Diploma in Medical Lab. Technology - 2 YearsDokument20 SeitenDiploma in Medical Lab. Technology - 2 YearsTeamGGxKick EsportsNoch keine Bewertungen
- UVR Whitepaper6 Airstream InDuct Disinfection 90000630 REV A 083120Dokument4 SeitenUVR Whitepaper6 Airstream InDuct Disinfection 90000630 REV A 083120JUANNoch keine Bewertungen
- Transplantation PDFDokument18 SeitenTransplantation PDFChandan Kumar100% (1)
- Lab Tests and Diagnostic TestDokument14 SeitenLab Tests and Diagnostic TestZhailyn Joy DumlaoNoch keine Bewertungen
- DIB - Week 01 - 02 - Anatomy & Physiology PDFDokument99 SeitenDIB - Week 01 - 02 - Anatomy & Physiology PDFFaisal MujibNoch keine Bewertungen
- Dunaliella Salina As A Novel Host For The Production of Recombinant ProteinsDokument9 SeitenDunaliella Salina As A Novel Host For The Production of Recombinant ProteinsMarcusNoch keine Bewertungen
- Why The Covid Vaccines Are DangerousDokument36 SeitenWhy The Covid Vaccines Are DangerousGustavo Iac100% (4)
- Neurological Complications of COVID-19: Underlying Mechanisms and ManagementDokument21 SeitenNeurological Complications of COVID-19: Underlying Mechanisms and ManagementAngelita Torres LlacsahuangaNoch keine Bewertungen
- Identificação Bacteriológica em Banheiros de Unidades Básicas de Saúde de Municípios Do Noroeste Paulista, BrasilDokument5 SeitenIdentificação Bacteriológica em Banheiros de Unidades Básicas de Saúde de Municípios Do Noroeste Paulista, BrasilLiana Maia100% (1)