Beruflich Dokumente
Kultur Dokumente
Aminoglycosides PDF
Hochgeladen von
Ashiqul Islam0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
43 Ansichten41 SeitenOriginaltitel
Aminoglycosides.pdf
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
43 Ansichten41 SeitenAminoglycosides PDF
Hochgeladen von
Ashiqul IslamCopyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 41
Aminoglycosides
Aminoglycosides are a group of natural and
semisynthetic antibiotics having polybasic
aminogroups linked glycosidically to two or
more aminosugar (streptidine, 2-deoxy
streptamine, garosamine) residues
Unlike penicillin, which was a chance
discovery, aminoglycosides are products of
deliberate search for drugs effective against
gram negative bacteria
Aminoglycosides include:
– Streptomycin (Streptomyces griseum)
– Neomycin (S. fradiae)
– Kanamycin (S. kanamyceticus)
– Tobramycin (S. tenebrarius)
– Amikacin (semisynthetic derivative of
kanamycin)
– Gentamicin (Micromonospora purpurae)
– Sisomicin (similar to C1a component of
gentamicin)
– Netilmicin (semisynthetic derivative of
sisomicin)
Chemical structure
Aminoglycosides have a hexose ring
(aminocyclitol ring), either streptidine
(in streptomycin) or 2-
deoxystreptamine (other
aminoglycosides), to which various
(two or more) amino sugars are
attached by glycosidic linkage. That’s
why they are called aminoglycosides
Common properties
Polycations
Highly polar (water soluble)
Stable in solution. They are used as sulphate
salts, which are highly water soluble. Solutions
are stable for months
More active in alkaline than in acid pH
All are bactericidal
Common toxicity profile like ototoxicity &
nephrotoxicity
Poor oral absorption
Volume of distribution approximately the
extracellular space (0.26 L/kg)
Tissue distribution variable (poor CNS
penetration)
Negligible metabolism
Ranally eliminated (filtered, with a small
amount of proximal reabsorption)
Elimination t½ 2-3 hours (if renal function is
normal)
Can cross placenta (teratogenic)
Have concentration dependent killing property
Exhibit post antibiotic effect
They act by interfering with bacterial protein
synthesis
All are active primarily against aerobic gram
negative bacilli. No activity against anaerobic
microorganism or facultative bacteria. Limited
activity against gram positive bacteria,
observed only when combined with β-lactams
or glycopeptides. Streptococci highly resistant
There is only partial cross resistance among
them. An organism resistant to one
aminoglycoside may still respond to another.
Resistance – 1st kanamycin, then
gentamicin, then tobramycin. Amikacin is
less vulnerable to those enzyme because it is
developed as poor substrate of these enzymes
They have relatively narrow margin of safety
Antibacterial activity
Antibacterial activity directed against aerobic
gram-negative bacilli, including Pseudomonas
aeruginosa
No activity against anaerobic microorganism or
facultative bacteria
Limited activity against gram-positive bacteria.
To achieve an additive or synergistic effect
aminoglycosides are often combined with a β-
lactams antibiotic or glycopeptides or a drug
active against anaerobic bacteria
Streptococci highly resistant (used in blood
agar to isolate)
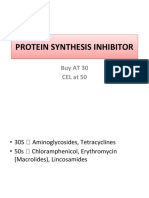
Mechanism of action
Aminoglycosides are irreversible inhibitors of
protein synthesis, but the precise mechanism
for bactericidal activity is not known
The initial event is passive diffusion via porin
channels across the outer cell membrane
Aminoglycosides then enters the bacterial cell
cytoplasm via O2 dependent active transport
system.
– The transmembrane electrochemical gradient
supplies the energy for this process &
transport is coupled to a proton pump
– Low extracellular pH & anaerobic conditions
inhibit transport by reducing the gradient
– Transport may be enhanced by cell wall-
active drugs such as penicillin or vancomycin
Inside the cell, aminoglycosides irreversibly
binds with the specific receptor protein on the
30S subunit ribosomal protein
Protein synthesis is inhibited by
aminoglycosides in at least three ways
– Aminoglycosides interfere with the normal
activity of the “initiation complex” of peptide
formation
– They induce *misreading of mRNA
template, which causes incorporation of
incorrect amino acid into the peptide,
resulting in a nonfunctional or toxic
protein
– Amino acid attachment results the
breakup of polysomes into nonfunctional
monosomes which is incapable of
protein synthesis
These activities occur more or less
simultaneously, & the overall effect is
irreversible & lethal for the cell
Mechanisms of resistance:
– Three principal mechanisms have been
established:
Production of a transferase
(aminoglycosidase) enzyme or enzymes
inactivates the aminoglycoside by
adenylation, acetylation, or
phosphorylation (bind with the amino
group of the drug). Each of these enzymes
has its own aminoglycoside specificit;
therefore, cross resistance is not an
invariable rule. This is the principal type of
resistance encountered clinically.
Commonly occurs in hospital setting.
There is impaired entry of aminoglycoside
into the cell. This may be genotypic, i.e.,
resulting from mutation or deletion of a
porin protein or proteins involved in
transport & maintenance of the
electrochemical gradient; or phenotypic,
e.g. resulting from growth conditions
under which the oxygen-dependent
transport process is not functional
The receptor protein on the 30S ribosomal
subunit may be deleted or altered as a
result of a mutation. So there is low affinity
for ribosome
Resistance:
–First Kanamycin,
–then Gentamycin &
–then Tobramycin
Netilmicin & Amikacin are less
vulnerable to these enzymes
because it is developed as a poor
substrate of these enzymes
Once daily administration of Aminoglycosides:
– Traditionally, aminoglycosides have been
administered in two or three equally divided
daily dose for patients with normal renal
function.
– However, once-daily aminoglycoside dosing
called extended interval aminoglycoside dose
(EIAD) may be preferred in certain clinical
situations
– Once daily administration recommended:
Gram negative bacilli infection: urinary,
abdominal, pelvic, lower respiratory tract
& soft tissue
– Once daily administration may be more
effective:
Mild to moderate renal insufficiency (Ccr
>40 ml/min)
Fever in neutropenic patient (in a setting of
low incidence of P. aeruginosa infection)
– Aminoglycosides have concentration
dependent killing – i.e., increasing
concentrations kill an increasing proportion
of bacteria & at a more rapid rate
– They also have a significant postantibiotic
effect, such that the antibacterial activity
persists beyond the time during which
measurable drug is present. The
– postantibiotic effect of aminoglycosides can
reach several hours.
– Because of these properties, a given total
amount of aminoglycoside may have better
efficacy when administered as a single large
dose than when administered as multiple
smaller doses
– There is no difference in incidence &
intensity of any of the adverse effects in
EIAD
– A trough concentration above 2μg/mL is
predictive of toxicity. At clinically relevant
doses, the time above this threshold will be
greater with multiple smaller doses of drug
– than with a single large dose
– Single daily dose of aminoglycoside is just as
safe, effective & no more (& often less) toxic
than multiple smaller doses. Therefore many
authorities now recommend that
aminoglycosides be administered as a single
daily dose in many clinical situations with
the following exceptions:
Severe renal insufficiency
Severe burn
Ascitis
Severe sepsis syndrome
The efficacy of once daily aminoglycoside
dosing in combination therapy of
enterococcal, streptococcal &
staphylococcal endocarditis remains to be
defined
Myocardial disease
Pregnancy
Neonates/children
Hemodialysis
Concomitant nephrotoxic drugs
Culture document predominant P.
aeruginosa infection in neutropenic patient
The standard low-dose, thrice daily
administration is still recommended
Once-daily dosing has potential practical
advantages:
– Determination of serum concentrations is
probably unnecessary unless aminoglycoside
is given for more than 3 days
– A drug administered once a day rather than 3
times a day saves time
– Less nursing time is required to give a drug
once a day instead of 3 times a day
– Once a day dosing lends itself to outpatient
therapy
Clinical uses:
– Gentamicin (preferred among
aminoglycosides). If it is resistant then
Tobramycin (similar to gentamicin. Slightly
more active against P aeruginosa), Amikacin,
Netilmicin (less ototoxic, less active against P
aeruginosa)
For blind therapy of serious undiagnosed
infection usually with penicillin or
metronidazole
Urinary tract infection (effective but used
only in seriously ill pyolonephritis)
Pneumonias (community acquired
pneumonia is susceptible to beta lactam,
however combination is required in
hospital acquired pneumonia)
Meningitis (ceftriaxone preferred, but
required in Pseudomonas)
Peritonitis (peritoneal dialysis)
Sepsis (anti-pseudomonal Penicillin with
Gentamicin or Amikacin or Tobramycin or
Netilmicin)
Penicillin-aminoglycoside combinations
also are used to achieve bactericidal
activity in treatment of enterococcal
endocarditis & to shorten duration of
therapy for viridans streptococcal &
staphylococcal endocarditis
Topical (slowly as ointment, but rapid as
cream)
Streptomycin:
– Bacterial endocarditis (with Benzyl penicillin)
– Tularemia (tetracycline is preferred)
– Plague (tetracycline & chloramphenicol)
– Tuberculosis (one of the combination in
MDRTB) 2nd line agent I/M or I/V
Neomycin: broad spectrum. Too toxic for
parenteral use
– Topical administration in ulcers, wounds &
burns
– Used orally to reduce intestinal load of
Enterobacteriaceae (preferred one is Lactulose)
– Bowel preparation along with erythromycin
base to reduce incidence of wound infection
after elective colorectal surgery
Unwanted effects:
– All aminoglycosides are ototoxic &
nephrotoxic
– Ototoxicity & nephrotoxicity are more likely
to be encountered when
Therapy is continued for more than 5 days
At higher doses
In the elderly
In the setting of renal insufficiency
– Concurrent use with loop diuretics
(frusemide, ethacrynic acid) or other
nephrotoxic antimicrobial agents (e.g.
vancomycin or amphotericin) can potentiate
nephrotoxicity & should be avoided if
possible
– It is important to monitor plasma levels of
gentamicin, tobramycin, netilmicin &
amikacin to avoid concentrations that cause
dose-related toxicities
– When the drugs are administered two or
three times daily, both peak & trough levels
are measured
– Peak levels are defined as those obtained
thirty minutes to one hour after infusion
– Trough levels are obtained immediately
before the next dose
– When once daily dosing is employed, only
the trough concentrations are monitored
Ototoxicity (irreversible):
– Is directly related to high peak plasma levels
& the duration of treatment
– Progressive accumulation of drug in
perilymph & endolymph of the inner ear
– Half-lives in otic fluid is six times longer than
plasma
– Toxicity depends on the Area Under the
Curve (AUC)
– Damage of the hair cells begins at central
part of cochlea (high-frequency)
– Toxicity correlates with the number of
– destroyed hair cells in the organ of Corti
– Deafness may be irreversible & has been known
to affect fetuses in utero
– Aminoglycoside ear drops can cause ototoxicity
when instilled in patients with perforated
eardrum; are contraindicated in them
– Clinical feature of cochlear damage
Tinnitus & high frequency hearing loss
initially
Conversation is not interfered at early stage
Delayed diagnosis as people can continue for
some days with normal conversation that is of
low frequency
– Clinical features of vestibular damage
Intense headache, vertigo, ataxia, loss of
balance (specially in patients receiving
streptomycin), mental past pointing
– Streptomycin & Gentamicin produce
predominantly vestibular effects
– Amikacin, Kanamycin & Neomycin
primarily affect auditory function
– Tobramycin affects both
– Patients simultaneously receiving another
ototoxic drug, such as the loop diuretics
frusemide, bumetanide, or ethacrynic acid or
cisplatin, are particularly at risk
Nephrotoxicity (reversible)
– Accumulation & retention of aminoglycoside in
proximal tubular cells
– These cells have the capacity to regenerate. That’s
why the effects are reversible
– Related to inhibition of intracellular
phospholipases
– Disrupt calcium-mediated transport processes, &
this results in kidney damage ranging from mild,
reversible renal impairment to severe, acute
tubular necrosis, which can be irreversible
– Aminoglycosides interfere with the production of
prostaglandins in the kidney & this is causally
related to reduced GFR
– However, the exact biochemical processes
that lead to the toxicity remain to be
elucidated
– Associated factors: hypotension,
dehydration, duration of therapy,
concomitant liver disease, advanced age,
other nephrotoxins
– Nephrotoxicity results in rising serum
creatinine levels or reduced creatinine
clearance, although the earliest indication
often is an increase in trough serum
aminoglycoside concentrations
– Reduced excretion of drug may lead to
ototoxicity later
– Order of nephrotoxicity
Neomycin is highest toxic
Streptomycin is the least toxic
Tobramycin & Gentamicin are in between
& equal
Neuromuscular paralysis:
– In very high doses, aminoglycosides can
produce a curare-like effect with
neuromuscular blockade that results in
respiratory paralysis
– The mechanism responsible is a decrease in
both the release of acetylcholine (results from
inhibition of calcium uptake necessary for the
exocytotic release of acetylcholine) from
– prejunctional nerve endings & the sensitivity
of the postsynaptic site
– This side effect most often occurs after the
direct intraperitoneal or intrapleural
application of large doses of aminoglycosides
– Only observed when given concurrently with
other neuromuscular blocking drugs or along
with anesthesia
– Neomycin is particularly criminal with this
ability
– Patients with myasthenia gravis are
particularly at risk
– Prompt administration of calcium gluconate
or neostigmine can reverse the block
Allergic reactions:
– Hypersensitivity occurs infrequently
– Contact dermatitis is a common reaction to
topically applied neomycin
Other:
– Bone marrow depression, hemolytic anemia
& bleeding due to antagonism of factor V
– Teratogenicity: risk of 8th cranial nerve
damage to fetus
– GIT: nausea, vomiting, loose motion
Precautions & interactions of Aminoglycosides
– Avoid aminoglycosides during pregnancy: risk of
fetal ototoxicity
– Avoid concurrent use of other nephrotoxic drugs, e.g.
NSAIDs, Amphotericin B, Vancomycin, Cyclosporine,
Cisplatin
– Cautious use of other ototoxic drugs like vancomycin,
minocycline & furosemide, though clinical evidence
of potentiated ototoxicity is meagre
– Cautious use in patients > 60 years age & in those
with kidney damage
– Cautious use of muscle relaxants in patients receiving
an aminoglycoside
– Do not mix aminoglycoside with any drug in the
same syringe/infusion bottle
Streptomycin
Isolated from a strain of streptomyces griseus
Antibacterial spectrum & mechanism of
resistance are typical of that of other
aminoglycosides
Clinical uses:
– Mycobacterial infections: mainly as second
line agent for treatment of TB. It should be
used only in combination with other agents
to prevent emergence of resistance
– Nontubercular infections: in plague,
tularemia, & sometimes bruellosis,
streptomycin given in combination with
tetracycline
Gentamicin
Isolated from Micromonospora purpurea
Antibacterial activity:
– Inhibits in vitro many strains of
staphylococci & coliform & other gram-
negative bacteria
– It is active alone, but also as a synergistic
companion with β-lactam antibiotics, against
pseudomonas, proteus, enterobacter,
klebsiella, serratia, stenotrophomonas &
other gram-negative rods
– It has no activity against anaerobes
(bacteroides)
Clinical uses:
– I/M or I/V administration:
For severe infections (e.g. sepsis &
pneumonia) caused by gram-negative
bacteria that are likely to be resistant to
other drugs, especially pseudomonas,
enterobacter, serratia, proteus,
acinetobacter, & klebsiella. It usually is
used in combination with a second agent,
as an aminoglycoside alone may not be
effective for infections outside the urinary
tract
– Aminoglycosides should not be used for
single agent therapy of pneumonia because
penetration of infected lung tissue is poor &
local conditions of low pH & low oxygen
tension contribute to poor activity
Topical administration:
– Creams, ointments, & solutions containing
0.1-0.3% gentamicin sulfate have been used
for the treatment of infected burns, wounds,
or skin lesions & the prevention of I/V
catheter infections
– 10 mg can be injected S.C. for treatment of
ocular infections
Intrathecal administration:
– Meningitis caused by gram-negative bacteria
has been treated by the intrathecal injection
of gentamicin sulfate
– However, neither intrathecal nor
intraventricular (toxic) gentamicin was
beneficial in neonates with meningitis
– Moreover, the availability of third-generation
cephalosporins for gram-negative meningitis
has rendered this therapy obsolete in most
cases
Amikacin
Semisynthetic derivative of kanamycin
Less toxic than the parent molecule
Resistant to many enzymes that inactivate
gentamicin & tobramycin, & it therefore can be
used against some microorganisms resistant to
the latter drugs
Many gram-negative enteric bacteria, including
many strains of proteus, pseudomonas,
enterobacter, & serratia, are inhibited by
amikacin in vitro
Strains of MDRTB including streptomycin-
resistant strains, are usually susceptible to
amikacin
Neomycin & Kanamycin
Paromomycin is also a member of this group
Antibacterial activity & resistance:
– Active against gram-positive & gram-
negative bacteria & some mycobacteria
– Pseudomonas & streptococci are generally
resistant
– The wide spread use of these drugs in bowel
preparation for elective surgery has resulted
in the selection of resistant organisms &
some outbreaks of enterocolitis in hospitals
Clinical use:
– Limited to topical & oral use
– Topical administration:
Used on infected surfaces or injected into
joints, the pleural cavity, tissue spaces, or
abscess cavities where infection is present
Ointments, often formulated as a
neomycin-polymyxin-bacitracin
combination, can be applied to infected
skin lesions or in the nares for suppression
of staphylococci but they are largely
ineffective
– Oral administration:
In preparation for elective bowel surgery,
often combined with erythromycin base.
This reduces aerobic bowel flora with little
effect on anaerobes
In hepatic coma (supplemented by
lactulose)
Das könnte Ihnen auch gefallen
- Aminoglycosides 23099Dokument27 SeitenAminoglycosides 23099TES SENNoch keine Bewertungen
- AMINOGLYCOSIDESDokument15 SeitenAMINOGLYCOSIDESGareth BaleNoch keine Bewertungen
- Department of Pharmacology: Prof. Dr. Asya RehmanDokument15 SeitenDepartment of Pharmacology: Prof. Dr. Asya RehmanGareth BaleNoch keine Bewertungen
- DP On AglDokument12 SeitenDP On AglDeepikaNoch keine Bewertungen
- Pharma URO AminoglycosidesDokument8 SeitenPharma URO AminoglycosidesHussein AlhaddadNoch keine Bewertungen
- AMINOGLYCOSIDEDokument18 SeitenAMINOGLYCOSIDEVinayKumarNoch keine Bewertungen
- AminoglycosidesDokument36 SeitenAminoglycosidesIqbal V MohammadNoch keine Bewertungen
- Inhibitor of Bacterial Protein SynthesisDokument83 SeitenInhibitor of Bacterial Protein SynthesisNdayisaba CorneilleNoch keine Bewertungen
- AMINOGLYCOSIDES AND MACROLIDES: MECHANISMS AND CLINICAL USESDokument45 SeitenAMINOGLYCOSIDES AND MACROLIDES: MECHANISMS AND CLINICAL USESAbdullah EmadNoch keine Bewertungen
- Antibacterials IiDokument8 SeitenAntibacterials IiPatrick JnrNoch keine Bewertungen
- P'cology of Amin & Spect (2022-P)Dokument42 SeitenP'cology of Amin & Spect (2022-P)Tewodros TeshomeNoch keine Bewertungen
- Antibacterial Drugs: B.K. SatriyasaDokument56 SeitenAntibacterial Drugs: B.K. SatriyasaVicNoch keine Bewertungen
- Aminoglycosides: Amlan GangulyDokument14 SeitenAminoglycosides: Amlan GangulyAli Akand AsifNoch keine Bewertungen
- Aminoglycoside AntibioticsDokument36 SeitenAminoglycoside AntibioticsGeneral InquiriesNoch keine Bewertungen
- Protein Synthesis Inhibitors 1Dokument23 SeitenProtein Synthesis Inhibitors 1Johnathan DevidNoch keine Bewertungen
- Aminoglycosides.: Chapter No. 02 Week # 07Dokument2 SeitenAminoglycosides.: Chapter No. 02 Week # 07Alee Iz HarNoch keine Bewertungen
- AminoglycosidesDokument20 SeitenAminoglycosidesHassan.shehri100% (5)
- 46 Aminoglycosides-2023Dokument16 Seiten46 Aminoglycosides-2023deo okiaNoch keine Bewertungen
- Protein Synthesis Inhibitors: Aminoglycosides and TetracyclinesDokument78 SeitenProtein Synthesis Inhibitors: Aminoglycosides and Tetracyclinesansam hirbaweNoch keine Bewertungen
- Aminoglycosides KunjDokument17 SeitenAminoglycosides KunjDeepak kumarNoch keine Bewertungen
- 5 AminoglycosidesDokument7 Seiten5 AminoglycosidesNashat SaadiNoch keine Bewertungen
- Aminoglycosides (17.07.2017)Dokument44 SeitenAminoglycosides (17.07.2017)Habibul Kowser (Rishat)Noch keine Bewertungen
- ZetamycinDokument6 SeitenZetamycinelcapitano vegetaNoch keine Bewertungen
- Aminoglycoside: From Wikipedia, The Free EncyclopediaDokument11 SeitenAminoglycoside: From Wikipedia, The Free Encyclopediaawajahat100% (3)
- Buy The Book PDA DownloadDokument9 SeitenBuy The Book PDA Downloadneilbert_jayNoch keine Bewertungen
- Aminoglycosides: Dr. Amit ShahDokument29 SeitenAminoglycosides: Dr. Amit ShahAmit ShahNoch keine Bewertungen
- Aminoglycosides ResearchDokument12 SeitenAminoglycosides Researchتارا للطباعة والترجمةNoch keine Bewertungen
- Aminoglycosides: Official Reprint From Uptodate ©2021 Uptodate, Inc. And/Or Its Affiliates. All Rights ReservedDokument17 SeitenAminoglycosides: Official Reprint From Uptodate ©2021 Uptodate, Inc. And/Or Its Affiliates. All Rights ReservedVanessa GomesNoch keine Bewertungen
- Newer Antibiotics: Guide: DR Saroja A ODokument51 SeitenNewer Antibiotics: Guide: DR Saroja A OparahulNoch keine Bewertungen
- Gentamicin: Gentamicin 80mg/2mL Injection As Gentamicin SulphateDokument7 SeitenGentamicin: Gentamicin 80mg/2mL Injection As Gentamicin SulphateGraciano Aristides MaturbongsNoch keine Bewertungen
- Antibiotics Aminoglycosides: Dr. Ahmed Faris Behia Clinical Pharmacology and Forensic ToxicologyDokument25 SeitenAntibiotics Aminoglycosides: Dr. Ahmed Faris Behia Clinical Pharmacology and Forensic Toxicologyصادق رستم هادي -Noch keine Bewertungen
- Anti - TB DrugsupdatedDokument35 SeitenAnti - TB DrugsupdatedgNoch keine Bewertungen
- CLINICAL USE OF ANTIBIOTICS IN VETERINARY PRACTICEDokument83 SeitenCLINICAL USE OF ANTIBIOTICS IN VETERINARY PRACTICEhansmeet100% (1)
- Anti Parasit A RiosDokument59 SeitenAnti Parasit A RiosMaxiNoch keine Bewertungen
- Aminoglycoside: Systemic AminoglycosidesDokument47 SeitenAminoglycoside: Systemic AminoglycosidesPawan PatelNoch keine Bewertungen
- Aminoglikosida Farkol 2 2023Dokument20 SeitenAminoglikosida Farkol 2 2023ghazialghifariNoch keine Bewertungen
- Principles of Antimicrobial TherapyDokument19 SeitenPrinciples of Antimicrobial TherapyMERVENoch keine Bewertungen
- Aminoglycosides AntibioticsDokument2 SeitenAminoglycosides AntibioticsHlaSoe WinNoch keine Bewertungen
- Antibacterial Agents (1)Dokument44 SeitenAntibacterial Agents (1)belindasithole965Noch keine Bewertungen
- AntibioticDokument84 SeitenAntibioticDr. Kalavati PrajapatiNoch keine Bewertungen
- Antimicrobials Revision: Gram Staining, MIC, Antibiotic Misuse & MechanismsDokument5 SeitenAntimicrobials Revision: Gram Staining, MIC, Antibiotic Misuse & MechanismsDanny LeeNoch keine Bewertungen
- Antibacterial Class 03Dokument80 SeitenAntibacterial Class 03tsegaab yosephNoch keine Bewertungen
- Aminogycoside AntibioticsDokument31 SeitenAminogycoside AntibioticsNurul Febrina100% (2)
- Aminoglycoside - WikipediaDokument52 SeitenAminoglycoside - WikipediaRustam LoharNoch keine Bewertungen
- 9 ATB Protein Synthesis Inhibitors &anti-MetabolitesDokument118 Seiten9 ATB Protein Synthesis Inhibitors &anti-Metaboliteskamal abu ajamiehNoch keine Bewertungen
- Antimicrobials MD 3 GISDokument26 SeitenAntimicrobials MD 3 GISmus zaharaNoch keine Bewertungen
- Pharmacology: Fast and Dirty Board ReviewDokument7 SeitenPharmacology: Fast and Dirty Board ReviewRochelleth7278Noch keine Bewertungen
- Aminoglycoside & Cephalosporin Antibiotics: Uses, Mechanisms & ToxicitiesDokument30 SeitenAminoglycoside & Cephalosporin Antibiotics: Uses, Mechanisms & ToxicitieskrishnakumarNoch keine Bewertungen
- 6-Protein Synthesis InhibitorDokument71 Seiten6-Protein Synthesis InhibitorAlexa Joy InguilloNoch keine Bewertungen
- Antibiotics-2 Cology 2Dokument25 SeitenAntibiotics-2 Cology 2Manthan ChauhanNoch keine Bewertungen
- Aminoglycosides: Aminoglycoside Is CategoryDokument6 SeitenAminoglycosides: Aminoglycoside Is CategoryAnonymous RJwbBCkrHNoch keine Bewertungen
- AminoglycosidesDokument12 SeitenAminoglycosidesTayyab JabbarNoch keine Bewertungen
- Nursing 3703 Pharmacology: Antimicrobials by Linda SelfDokument78 SeitenNursing 3703 Pharmacology: Antimicrobials by Linda Selfdon yenNoch keine Bewertungen
- Amikacin Drug ProfileDokument2 SeitenAmikacin Drug ProfileErum JanNoch keine Bewertungen
- AntibioticsDokument30 SeitenAntibioticsRoza RahbeniNoch keine Bewertungen
- The AminoglycosidesDokument8 SeitenThe AminoglycosidesVangenique Nieves AgrudaNoch keine Bewertungen
- Pharma URO MacrolidesDokument6 SeitenPharma URO MacrolidesHussein AlhaddadNoch keine Bewertungen
- AntibioticsDokument53 SeitenAntibioticsMaheen IdreesNoch keine Bewertungen
- Protein Synthesis InhibitorsDokument35 SeitenProtein Synthesis InhibitorsHarsha MaheshwariNoch keine Bewertungen
- Adult Infectious Disease Bulletpoints HandbookVon EverandAdult Infectious Disease Bulletpoints HandbookBewertung: 4.5 von 5 Sternen4.5/5 (9)
- Singular and Plural NounsDokument3 SeitenSingular and Plural NounsJosé BulquesNoch keine Bewertungen
- Chapter 20: Sleep Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDokument4 SeitenChapter 20: Sleep Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNoch keine Bewertungen
- Bylaw 16232 High Park RezoningDokument9 SeitenBylaw 16232 High Park RezoningJamie_PostNoch keine Bewertungen
- ms360c Manual PDFDokument130 Seitenms360c Manual PDFEdgardoCadaganNoch keine Bewertungen
- Lehman BrothersDokument10 SeitenLehman BrothersJaikishin RuprajNoch keine Bewertungen
- Calculate Capacity of Room Air Conditioner: Room Detail Unit Electrical Appliances in The RoomDokument2 SeitenCalculate Capacity of Room Air Conditioner: Room Detail Unit Electrical Appliances in The Roomzmei23Noch keine Bewertungen
- Download C How To Program An Objects Natural Approach 11E 11Th Edition Paul Deitel full chapter pdf scribdDokument67 SeitenDownload C How To Program An Objects Natural Approach 11E 11Th Edition Paul Deitel full chapter pdf scribdjack.bowlin207100% (4)
- Dice Resume CV Narendhar ReddyDokument5 SeitenDice Resume CV Narendhar ReddyjaniNoch keine Bewertungen
- PhysicsLab PreReport201Dokument9 SeitenPhysicsLab PreReport201Giuliana SchulzNoch keine Bewertungen
- Vox Latina The Pronunciation of Classical LatinDokument145 SeitenVox Latina The Pronunciation of Classical Latinyanmaes100% (4)
- Sine and Cosine Exam QuestionsDokument8 SeitenSine and Cosine Exam QuestionsGamer Shabs100% (1)
- All Paramedical CoursesDokument23 SeitenAll Paramedical CoursesdeepikaNoch keine Bewertungen
- Barker-Choucalas, Vida PDFDokument176 SeitenBarker-Choucalas, Vida PDFAnn GarbinNoch keine Bewertungen
- Gr.10 Music History ModuleDokument45 SeitenGr.10 Music History ModuleKyle du PreezNoch keine Bewertungen
- PronPack 5 Sample MaterialDokument13 SeitenPronPack 5 Sample MaterialAlice FewingsNoch keine Bewertungen
- Boat DesignDokument8 SeitenBoat DesignporkovanNoch keine Bewertungen
- Documentation Control HandbookDokument9 SeitenDocumentation Control Handbookcrainvictor 45Noch keine Bewertungen
- A Secret Baby by The Bratva by Lexi AsherDokument184 SeitenA Secret Baby by The Bratva by Lexi Asheralisa sanchez100% (1)
- List of Psychotropic Drugs Under International ControlDokument32 SeitenList of Psychotropic Drugs Under International ControlRadhakrishana DuddellaNoch keine Bewertungen
- Vestax VCI-380 Midi Mapping v3.4Dokument23 SeitenVestax VCI-380 Midi Mapping v3.4Matthieu TabNoch keine Bewertungen
- Facebook Facing Off Againt TencentDokument6 SeitenFacebook Facing Off Againt TencentWai Shan Lee0% (1)
- Effects of Zero Moment of Truth On Consumer Behavior For FMCGDokument14 SeitenEffects of Zero Moment of Truth On Consumer Behavior For FMCGBoogii EnkhboldNoch keine Bewertungen
- Aluminium FOil SearchDokument8 SeitenAluminium FOil SearchAtul KumarNoch keine Bewertungen
- UEME 1143 - Dynamics: AssignmentDokument4 SeitenUEME 1143 - Dynamics: Assignmentshikai towNoch keine Bewertungen
- Schedule For Semester III, Class of 2021Dokument7 SeitenSchedule For Semester III, Class of 2021Jay PatelNoch keine Bewertungen
- ADD MATH ProjectDokument13 SeitenADD MATH Projectmegazat27Noch keine Bewertungen
- CV. Anderson Hario Pangestiaji (English Version)Dokument5 SeitenCV. Anderson Hario Pangestiaji (English Version)Anderson PangestiajiNoch keine Bewertungen
- #1Dokument7 Seiten#1Ramírez OmarNoch keine Bewertungen
- Chapter 9 Screw ConveyorsDokument7 SeitenChapter 9 Screw ConveyorsMarew Getie100% (1)
- BA50BCODokument6 SeitenBA50BCOpedroarlindo-1Noch keine Bewertungen