Beruflich Dokumente
Kultur Dokumente
Differentiation Between Complex Tic and Eyelid Myoclonia With Absences: Pediatric Case Report and Brief Review of The Literature
Hochgeladen von
Aperito InternationalOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Differentiation Between Complex Tic and Eyelid Myoclonia With Absences: Pediatric Case Report and Brief Review of The Literature
Hochgeladen von
Aperito InternationalCopyright:
Verfügbare Formate
Received: Jan 05, 2015
Neurological Research and Therapy Accepted: Feb 28, 2015
Open Access Published: Mar 04, 2015
http://dx.doi.org/10.14437/NRTOA-2-111 Case Report Tanya Murphy, Neurol Res Ther 2015, 2:2
Differentiation between Complex Tic and Eyelid Myoclonia with
Absences: Pediatric Case Report and Brief Review of the
Literature
Diana M Gerardi1, Caroline De Oleo Brozyna2, S Parrish Winesett3, 4, Maria Gieron Korthals1, 3 and Tanya Murphy1, 2*
1
Department of Pediatrics, University of SouthFlorida, Tampa, Florida
2
Department of Psychiatry, University of South Florida, Tampa, Florida
3
Department of Neurology, University of South Florida, Tampa, Florida
4
Department of Neurology, All Children’s Hospital, St. Petersburg, Florida
Abstract *Corresponding Author: Tanya Murphy, USF
th
Eyelid Myoclonia with Absences (EMA) can often be Department of Pediatrics, Rothman Center, 880 6 St.
clinically mistaken for a tic disorder. This case report South, Suite 460, Box 7523 St. Petersburg, Florida 33701;
describes a 4-year-old female who presented with eye Tel: 727-767-8230; Fax: 727-767-7786; E-mail:
fluttering and blinking accompanied by a hand gesture tmuphy@health.usf.edu
described as a “brow wipe” that was exacerbated by
sunlight, warm temperatures, anxiety, and excitement. She Introduction
was diagnosed with a transient tic disorder, and aripiprazole Eyelid Myoclonia with Absences (EMA), also known as
and clonazepam treatment partially decreased symptom Jeavons syndrome, is an epileptic syndrome characterized by
intensity. She was stable for months, after which symptoms eyelid myoclonia associated with brief absences and
worsened with constant tics while in the sun and seeking
photosensitivity [1, 2]. EMA was originally classified as reflex
light stimuli to induce an episode. Video electroencephalogr
syndrome of idiopathic generalized epilepsy, but is currently
-am confirmed self-induced photosensitive seizures with
identified as a myoclonic form of epilepsy [3, 4]. Typical age of
generalized epileptiform discharges consistent with
onset is between 6 and 8 years, and more females are affected
generalized seizures. The EMA diagnosis was confirmed by
than males [5]. The etiology of EMA is thought to be genetic [5-
these characteristic eye closure-related discharges, and the
10].
patient was successfully treated with valproate. We also
present a brief review of the literature that underscores the
During an episode, a patient with EMA will assume a posture of
clinical similarities between EMA and tics, as well as the
head slightly bent backwards when he/she is staring at the sun
importance of timely implementation of appropriate
or a source of bright light while shaking a hand in front of their
treatment in EMA.
face [11-13]. The patient’s eyelids exhibit rhythmic jerks and
consciousness is impaired only mildly and briefly following
Keywords: Absence Seizures; Eyelid Myoclonia with
eyelid closure. These absences, which can occur more than three
Absences; Jeavons Syndrome; Pediatric Absence Seizures;
times daily, last approximately three to six seconds in the
Pediatric Seizure Disorders
Copyright: © 2015 NRTOA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, Version 3.0, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Volume 2 • Issue 2 • 111 www.aperito.org
Citation: Tanya Murphy (2015), Differentiation between Complex Tic and Eyelid Myoclonia with Absences: Pediatric Case
Report and Brief Review of the Literature. Neurol Res Ther Open Access 2:111
http://dx.doi.org/10.14437/NRTOA-2-111 Page 2 of 5
presence of uninterrupted light; this is in contrast with other psychiatry. After evaluation, the patient was started on
forms of photosensitive epilepsies that are sensitive to flickering clonazepam 0.25mg one-quarter tablet once a day, and
lights. Approximately 50% of patients with EMA will display eventually increased to 0.25mg one tablet twice a day. Two
myoclonic limb jerks and tonic-clonic seizures triggered by months later, aripiprazole 1.5mg daily was added to her
sleep deprivation, fatigue, and/or alcohol intake [14]; however, medication regimen, as well as behavior intervention. She was
this is more common in adults than children [15, 16]. stable for six months, after which her behaviors worsened, as
Photosensitivity often decreases with age and antiepileptic drug she began to seek sunlight to induce the repetitive movements
(AED) treatment [14]. that eventually became nonstop when exposed to the sun. In
addition, the patient’s social functioning began to suffer, as she
EMA diagnosis is confirmed through video EEG, which will displayed constant brow swiping during recreational outdoor
typically display frequent high-amplitude 3-6 Hz generalized time and lost interest in social activities. The possibility of a
polyspike-slow-wave discharges and therefore rule out non- seizure disorder characterized by the self-induction of repetitive
epileptic paroxysmal eyelid movements [4, 5]. Notably, behaviors and brow swiping through seeking sunlight, a
neuroimaging and clinical examination will be normal in condition known as EMA, was then considered, and she was
patients with EMA [15]. Reports suggest that EMA is often referred to a pediatric neurologist specializing in seizure
misdiagnosed as a tic disorder, [17-19] and it is essential that disorders. Per neurology, findings from the evaluation revealed
patients, especially school-age females who present with a normal neurological examination. Video EEG displayed
photosensitivity, be evaluated comprehensively to rule out generalized polyspikes and maximal bioccipitally in conjunction
photosensitive epilepsy through video EEG. The goal of this with her episodes. The patient’s habitual episodes of brow
paper is to aid in differential diagnosis by calling attention to the wiping were recorded. Clinically, the patient would stare at the
clinical features of EMA that differentiate it from other light and move her left hand from the thumb to the pinky across
conditions by presenting a case report of a 4-year-old girl who her face. The spike was usually at the time her pinky cleared the
was initially diagnosed with a tic disorder. Further investigation left eye. On the EEG, generalized spikes at 1.5 and 2 Hz were
suggested a diagnosis of EMA, which was subsequently present. The EEG showed a normal background. Photic
confirmed through video EEG and appropriate treatment was stimulation was performed without abnormality. The patient
implemented. was then allowed to do her “tic movements;” these distinctly
showed reactivity in the background with bilateral parasagittal
Case Report spike and wave discharges at approximately 1 Hz. Spikes were
The patient is a previously healthy 4-year-old female with a not present in the absence of this “brow wiping” movement, and
family history significant for motor tics and autism. She were more pronounced when the patient was next to a window
presented with eye fluttering and repetitive blinking that and performed the movement looking into the sunlight,
occurred throughout the day and worsened when anxious or suggesting features of self-induced photosensitive epilepsy with
exposed to warmer temperatures. The eye fluttering occurred generalized epileptiform discharges. The patient was
concurrently with a complex movement of a hand gesture subsequently treated with lamotrigine and levetiracetam without
described as a brow wipe that became more frequent and intense symptom relief. However, successful treatment with valproate
in the sunlight. Her neurologist considered stereotypic followed and patient was doing well on follow-up.
movement disorder and transient tic disorder, but when her
episodes continued to worsen, the patient was referred to child
Volume 2 • Issue 2 • 111 www.aperito.org
Citation: Tanya Murphy (2015), Differentiation between Complex Tic and Eyelid Myoclonia with Absences: Pediatric Case
Report and Brief Review of the Literature. Neurol Res Ther Open Access 2:111
http://dx.doi.org/10.14437/NRTOA-2-111 Page 3 of 5
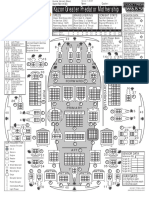
EEG before and during typical Eye Brow wiping (Referenitial montage)
Same EEG epoch with bipolar Montage
Volume 2 • Issue 2 • 111 www.aperito.org
Citation: Tanya Murphy (2015), Differentiation between Complex Tic and Eyelid Myoclonia with Absences: Pediatric Case
Report and Brief Review of the Literature. Neurol Res Ther Open Access 2:111
http://dx.doi.org/10.14437/NRTOA-2-111 Page 4 of 5
Discussion controlling myoclonic jerks and generalized tonic-clonic
This case demonstrates a challenge in appropriate and timely seizures, [14] as was the case in our patient.
diagnosis of EMA in a child. The reasons for misdiagnosing EMA diagnosis is confirmed when the characteristic seizures,
EMA for tic disorder stems from various similarities between photosensitivity, and a video EEG demonstrating eye closure-
EMA and tic disorders. For example, patients with EMA often related EEG discharges are present [25]. Due to similar clinical
report inducing seizures by waving their fingers within their line presentations, EMA is often misdiagnosed as tics, [17, 18] and
of vision or repetitively blinking their eyes, [20, 21] which are reassessment of a patient with tic-like movements who also
often signs that are mistaken for tics. Notably, the movements presents with photosensitivity is advisable. Child psychiatrists
observed in tic disorders are often less rhythmic and do not and neurologists should be aware of EMA and appropriately
involve tonic muscle contractions. An urge towards sunlight to differentiate it from non-epileptic conditions, such as tics,
induce tics has been reported in cases of Tourette’s syndrome stereotypies, and exaggerated normal eye movements. Making
[22]. Also similar to tic patients, pediatric EMA patients report the timely diagnosis could spare the patient from inappropriate
premonitory sensations and sense of relief after the absence therapies and potential deterioration in emotional and
[23]. The compulsive need to induce a seizure may be intellectual function if seizures go untreated.
analogous to the compulsory tic behavior in patients with tics
[23]. This type of presentation shares overlap with stereotypic References
movement disorder, in that these complex repetitive movements 1. Covanis A. Jeavons syndrome. Atlas of Epilepsies:
can be triggered by an environmental event. Despite similarities Springer; 2010:1081-1091.
in clinical presentation, a patient with EMA will have EEG 2. Jeavons P. Nosological problems of myoclonic epilepsi
characteristic abnormalities, unlike a patient with tics or -es in childhood and adolescence. Developmental
stereotypies. Medicine & Child Neurology. 1977; 19(1):3-8.
EMA treatment can also present a clinical challenge. The effect 3. Engel Jr J. ILAE classification of epilepsy syndromes.
of uncontrolled seizures on neurocognitive development and the Epilepsy research. 2006; 70:5-10.
potential adverse effects of appropriate pharmacotherapy on a 4. Striano S, Capovilla G, Sofia V, et al. Eyelid
child's physical, emotional, and intellectual well-being will need myoclonia with absences (Jeavons syndrome): A well-
to be considered. A case series has described patients with EMA defined idiopathic generalized epilepsy syndrome or a
who did not respond to AEDs developing EMA-associated spectrum of photosensitive conditions? Epilepsia.
intellectual disability as a consequence of uncontrollable 2009; 50:15-19.
seizures [9]. In contrast, the patients who did respond to AEDs 5. Striano S, Striano P, Nocerino C, et al. Eyelid
did not display impairment neurological or executive function, myoclonia with absences: an overlooked epileptic
as their seizures were controlled. Specifically, absences have syndrome? Neurophysiologie Clinique/Clinical
been successfully controlled with valproic acid, lamotrigine, Neurophysiology. 2002; 32(5):287-296.
levetiracetam, ethosuximide, and clonazepam [14, 24]. 6. Sadleir LG, Vears D, Regan B, Redshaw N, Bleasel A,
However, ethosuximide and lamotrigine have demonstrated Scheffer IE. Family studies of individuals with eyelid
some worsening of myoclonic jerks, and ethosuximide, as well myoclonia with absences. Epilepsia. 2012;
as clonazepam to a lesser extent, has been known to exacerbate 53(12):2141-2148.
generalized tonic-clonic seizures [14]. As well as exhibiting 7. Adachi M, Inoue T, Tsuneishi S, Takada S, Nakamura
benefit in absences, valproic acid has demonstrated efficacy in H. Eyelid myoclonia with absences in monozygotic
Volume 2 • Issue 2 • 111 www.aperito.org
Citation: Tanya Murphy (2015), Differentiation between Complex Tic and Eyelid Myoclonia with Absences: Pediatric Case
Report and Brief Review of the Literature. Neurol Res Ther Open Access 2:111
http://dx.doi.org/10.14437/NRTOA-2-111 Page 5 of 5
twins. Pediatrics international : official journal of the 16. Giannakodimos S, Panayiotopoulos CP. Eyelid
Japan Pediatric Society. Jun 2005; 47(3):343-347. Myoclonia with Absences in Adults: A Clinical and
8. Capovilla G, Striano P, Gambardella A, et al. Eyelid Video-EEG Study. Epilepsia. 1996; 37(1):36-44.
fluttering, typical EEG pattern, and impaired 17. Camfield C, Camfield P, Sadler M, et al. Paroxysmal
intellectual function: a homogeneous epileptic eyelid movements A confusing feature of generalized
condition among the patients presenting with eyelid photosensitive epilepsy. Neurology. 2004; 63(1):40-42.
myoclonia. Epilepsia. Jun 2009; 50(6):1536-1541. 18. Malafosse A. Idiopathic Generalized Epilepsies:
9. Caraballo RH, Fontana E, Darra F, et al. A study of 63 Clinical, Experimental, and Genetic Aspects. Vol 9.
cases with eyelid myoclonia with or without absences: London: John Libbey Eurotext; 1994.
type of seizure or an epileptic syndrome? Seizure : the 19. Sun Y, Chen H, Chang H, Zhu Y. [Misdiagnosis of
journal of the British Epilepsy Association. Jul 2009; eyelid myoclonia as Tic's disorder: a case report].
18(6):440-445. Zhonghua Er Ke Za Zhi. Nov 2004; 42(11):839.
10. Yang T, Liu Y, Liu L, Yan B, Zhang Q, Zhou D. 20. Binnie C, Jeavons P. Photosensitive epilepsies.
Absence status epilepticus in monozygotic twins with Epileptic syndromes in infancy, childhood, and
Jeavons syndrome. Epileptic disorders: international adolescence. London: John Libbey. 1992:299-305.
epilepsy journal with videotape. Sep 2008; 10(3):227- 21. Darby CE, de Korte RA, Binnie CD, Wilkins AJ. The
230. Self-induction of Epileptic Seizures by Eye Closure.
11. Ames FR, Saffer D. The sunflower syndrome: a new Epilepsia. 1980; 21(1):31-42.
look at “self-induced” photosensitive epilepsy. Journal 22. Kobylski T, Licamele W. Sun gazing by patients with
of the neurological sciences. 1983; 59(1):1-11. Tourette's Disorder. The American journal of
12. Bettoni L, Bortone E, Ghizzoni P, Juvarra G. The psychiatry. 1991; 148(3):394.
sunflower syndrome. Functional neurology. 1985; 23. Kent L, Blake A, Whitehouse W. Eyelid myoclonia
1(2):175-181. with absences: phenomenology in children. Seizure:
13. Ng BY. Psychiatric aspects of self‐induced epileptic the journal of the British Epilepsy Association. 1998;
seizures. Australian and New Zealand journal of 7(3):193-199.
psychiatry. 2002; 36(4):534-543. 24. Striano P, Sofia V, Capovilla G, et al. A pilot trial of
14. Panayiotopoulos C. Treatment of typical absence levetiracetam in eyelid myoclonia with absences
seizures and related epileptic syndromes. Paediatric (Jeavons syndrome). Epilepsia. Mar 2008; 49(3):425-
Drugs. 2001; 3(5):379-403. 430.
15. Panayiotopoulos CP. Syndromes of idiopathic 25. Joshi CN, Patrick J. Eyelid myoclonia with absences:
generalized epilepsies not recognized by the Routine EEG is sufficient to make a diagnosis. Seizure:
International League against Epilepsy. Epilepsia. 2005; the journal of the British Epilepsy Association. 2007;
46(s9):57-66. 16(3):254-260.
Volume 2 • Issue 2 • 111 www.aperito.org
Das könnte Ihnen auch gefallen
- Rifle May 2015 USADokument72 SeitenRifle May 2015 USAhanshcNoch keine Bewertungen
- Classification: Epilepsy (Sometimes Referred To As A Seizure Disorder) Is A Common ChronicDokument11 SeitenClassification: Epilepsy (Sometimes Referred To As A Seizure Disorder) Is A Common ChronicChristian BartolomeNoch keine Bewertungen
- Kazon Greater Predator MothershipDokument1 SeiteKazon Greater Predator MothershipknavealphaNoch keine Bewertungen
- A Simple Guide to Facial Palsy, Diagnosis, Treatment, and Related ConditionsVon EverandA Simple Guide to Facial Palsy, Diagnosis, Treatment, and Related ConditionsNoch keine Bewertungen
- Hans Belting - The End of The History of Art (1982)Dokument126 SeitenHans Belting - The End of The History of Art (1982)Ross Wolfe100% (7)
- Enochian Dragon Ritual PDFDokument4 SeitenEnochian Dragon Ritual PDFDenis NantelNoch keine Bewertungen
- Epilepsy Syndromes inDokument24 SeitenEpilepsy Syndromes inEdwin AlvarezNoch keine Bewertungen
- EpilepsyDokument16 SeitenEpilepsysapphireNoch keine Bewertungen
- Inside:: Issue 4 - February 2004 Bi-Monthly Warhammer E-ZineDokument40 SeitenInside:: Issue 4 - February 2004 Bi-Monthly Warhammer E-ZineJoe BloggsNoch keine Bewertungen
- Configuring BGP On Cisco Routers Lab Guide 3.2Dokument106 SeitenConfiguring BGP On Cisco Routers Lab Guide 3.2skuzurov67% (3)
- Infantile, Childhood, and Adolescent Epilepsies.9Dokument34 SeitenInfantile, Childhood, and Adolescent Epilepsies.9Silviana IlieNoch keine Bewertungen
- Presentation EpilepsyDokument38 SeitenPresentation EpilepsypertinenteNoch keine Bewertungen
- Evolution Army 3 R DadDokument341 SeitenEvolution Army 3 R DadStanisław DisęNoch keine Bewertungen
- Adult Focal EpilepsyDokument22 SeitenAdult Focal EpilepsyzhoujNoch keine Bewertungen
- Seizures in Children - Pediatric in Review 2020Dokument29 SeitenSeizures in Children - Pediatric in Review 2020Apple B RaiwaaNoch keine Bewertungen
- Seizures in Children JULIO 2020Dokument29 SeitenSeizures in Children JULIO 2020Elizabeth HendersonNoch keine Bewertungen
- Re Ex Myoclonic Epilepsy of Infancy: Seizures Induced by Tactile StimulationDokument8 SeitenRe Ex Myoclonic Epilepsy of Infancy: Seizures Induced by Tactile StimulationOziNoch keine Bewertungen
- Epilepsia FocalDokument17 SeitenEpilepsia FocalVíctor CalzadaNoch keine Bewertungen
- Epilepsy and Oral Health: Department of Pedodontics, Faculty of Dentistry, Atatürk University, Erzurum TurkeyDokument17 SeitenEpilepsy and Oral Health: Department of Pedodontics, Faculty of Dentistry, Atatürk University, Erzurum TurkeyNila Kusuma SuriNoch keine Bewertungen
- 94 - CH 10 - Symptoms in Heterophoria and Heterotropia and The Psychological Effects of Strabismus P. 153-157Dokument5 Seiten94 - CH 10 - Symptoms in Heterophoria and Heterotropia and The Psychological Effects of Strabismus P. 153-157Catleya ProtacioNoch keine Bewertungen
- Antiepileptic Drug Treatment of Epilepsy in ChildrenDokument27 SeitenAntiepileptic Drug Treatment of Epilepsy in ChildrenYunierNoch keine Bewertungen
- Scheffer 2019Dokument4 SeitenScheffer 2019Maria Teresa CruzNoch keine Bewertungen
- Epilepsysurgeryinchildren: Luis E. Bello-Espinosa,, Greg OlavarriaDokument12 SeitenEpilepsysurgeryinchildren: Luis E. Bello-Espinosa,, Greg OlavarriaAzizah HalidNoch keine Bewertungen
- Epileptic Disorders - 2023 - Nascimento - Focal Epilepsies Update On Diagnosis and ClassificationDokument17 SeitenEpileptic Disorders - 2023 - Nascimento - Focal Epilepsies Update On Diagnosis and ClassificationIvan MihailovicNoch keine Bewertungen
- Status Epilepticus: Presentasi Bed Site TeachingDokument29 SeitenStatus Epilepticus: Presentasi Bed Site TeachingDinda Dwipermata PutriNoch keine Bewertungen
- Approach To Refractory Childhood SeizuresDokument10 SeitenApproach To Refractory Childhood SeizureskholisahnasutionNoch keine Bewertungen
- Epilepsy DR LindaDokument8 SeitenEpilepsy DR LindaLaylaNoch keine Bewertungen
- 06 Neonatal SeizuresDokument10 Seiten06 Neonatal SeizuresSivanathan SubramaniamNoch keine Bewertungen
- The Diagnosis and Management of Epilepsy: Journal of Tropical Pediatrics January 2002Dokument9 SeitenThe Diagnosis and Management of Epilepsy: Journal of Tropical Pediatrics January 2002Roy MarechaNoch keine Bewertungen
- Evaluation of The Neonate With Seizures 2020Dokument7 SeitenEvaluation of The Neonate With Seizures 2020Eduardo Rios DuboisNoch keine Bewertungen
- CASEPRESDokument37 SeitenCASEPRESNathaniel GanapinNoch keine Bewertungen
- Neonatal SeizuresDokument13 SeitenNeonatal SeizuresGaby CorletoNoch keine Bewertungen
- Clinical Management of Seizures in Newborns: Diagnosis and TreatmentDokument10 SeitenClinical Management of Seizures in Newborns: Diagnosis and TreatmentfitriNoch keine Bewertungen
- Care Study Chapter 1Dokument49 SeitenCare Study Chapter 1bose olajuyinNoch keine Bewertungen
- Abdulsalam Mohammed Yakasai Physiotherapy Intervention in Children With EpiDokument17 SeitenAbdulsalam Mohammed Yakasai Physiotherapy Intervention in Children With Epinaveen chaudharyNoch keine Bewertungen
- Adult Epilepsy and Anaesthesia: Eleanor L Carter Frca and Ram M Adapa MD PHD FrcaDokument7 SeitenAdult Epilepsy and Anaesthesia: Eleanor L Carter Frca and Ram M Adapa MD PHD FrcaSnehaNoch keine Bewertungen
- Common Problems in Pediatric NeurologyDokument19 SeitenCommon Problems in Pediatric NeurologyPaul ManaloNoch keine Bewertungen
- Progressive Myoclonus EpilepsiesDokument11 SeitenProgressive Myoclonus Epilepsiesbirriederesse42Noch keine Bewertungen
- Epilepsy Research Paper ConclusionDokument7 SeitenEpilepsy Research Paper Conclusionzpyrufrif100% (1)
- Panayiotopoulos Syndrome: A Common Benign But Underdiagnosed and Unexplored Early Childhood Seizure SyndromeDokument2 SeitenPanayiotopoulos Syndrome: A Common Benign But Underdiagnosed and Unexplored Early Childhood Seizure SyndromeNensy AnggrainyNoch keine Bewertungen
- Unverricht-Lundborg Disease A Case Report and LiteDokument4 SeitenUnverricht-Lundborg Disease A Case Report and LiteAndreea CimpoiNoch keine Bewertungen
- Aroxysmal Isorders: Approach To Paroxysmal DisordersDokument46 SeitenAroxysmal Isorders: Approach To Paroxysmal DisordersblwNoch keine Bewertungen
- Psychogenic Non-Epileptic Seizures: Indian Pediatrics November 2004Dokument4 SeitenPsychogenic Non-Epileptic Seizures: Indian Pediatrics November 2004Nico NicoNoch keine Bewertungen
- Epilepsi 1Dokument12 SeitenEpilepsi 1Ima SoniaNoch keine Bewertungen
- Peds 20 Annals 20 ArticleDokument13 SeitenPeds 20 Annals 20 ArticleLeah Mariz RocaNoch keine Bewertungen
- Bell's Palsy: Submitted By: Twinkle Singh & Kinjalika VarmaDokument34 SeitenBell's Palsy: Submitted By: Twinkle Singh & Kinjalika Varmatwinklestar1396Noch keine Bewertungen
- British Medical JournalDokument2 SeitenBritish Medical Journalpatricia roseNoch keine Bewertungen
- Adult Epilepsy and AnaesthesiaDokument8 SeitenAdult Epilepsy and AnaesthesiaHainey GayleNoch keine Bewertungen
- Status EpilepticusDokument13 SeitenStatus EpilepticusDiana Yactayo SilvaNoch keine Bewertungen
- The Severe Epilepsy Syndromes of Infancy: A Population-Based Study - 2021Dokument13 SeitenThe Severe Epilepsy Syndromes of Infancy: A Population-Based Study - 2021Ana CostaNoch keine Bewertungen
- Evaluation and Management of Drug Resistant Epilepsy in ChildrenDokument10 SeitenEvaluation and Management of Drug Resistant Epilepsy in ChildrenAzizah HalidNoch keine Bewertungen
- Frontal Lobe SeizuresDokument11 SeitenFrontal Lobe Seizuresjhonny churata huarachiNoch keine Bewertungen
- Indian Guidelines On Epilepsy: Mrinal Kanti Roy, Dhiman DasDokument6 SeitenIndian Guidelines On Epilepsy: Mrinal Kanti Roy, Dhiman DasNurhafizah IbrahimNoch keine Bewertungen
- Progressive Myoclonic - Genetic Therapeutic - Lancet 2005 (Shahwan)Dokument10 SeitenProgressive Myoclonic - Genetic Therapeutic - Lancet 2005 (Shahwan)chintanNoch keine Bewertungen
- Pedia - Seizure Final PDFDokument8 SeitenPedia - Seizure Final PDFPrakkash SJNoch keine Bewertungen
- NEUROLOGICDokument11 SeitenNEUROLOGICinah krizia lagueNoch keine Bewertungen
- The Epilepsies: Support For Education and Learning: Clinical Case Scenarios-Children and Young People With EpilepsyDokument42 SeitenThe Epilepsies: Support For Education and Learning: Clinical Case Scenarios-Children and Young People With EpilepsyNinia MNoch keine Bewertungen
- Evaluation of First Seizure and Newly Diagnosed.4Dokument31 SeitenEvaluation of First Seizure and Newly Diagnosed.4veerraju tvNoch keine Bewertungen
- NDT 6 297Dokument12 SeitenNDT 6 297Chema ToledoNoch keine Bewertungen
- The New Basic Classification: Defining Where Seizures BeginDokument9 SeitenThe New Basic Classification: Defining Where Seizures Begininah krizia lagueNoch keine Bewertungen
- 2020 Epilepsy With Myoclonic-Atonic Seizures (Doose Syndrome)Dokument8 Seiten2020 Epilepsy With Myoclonic-Atonic Seizures (Doose Syndrome)Florian LamblinNoch keine Bewertungen
- Biology 2 JournalDokument5 SeitenBiology 2 JournalKadymars JaboneroNoch keine Bewertungen
- A Practical Guide To Treatment of Childhood Absence EpilepsyDokument10 SeitenA Practical Guide To Treatment of Childhood Absence EpilepsyLorenz BelloNoch keine Bewertungen
- Epilepsy: Neurological DisorderDokument8 SeitenEpilepsy: Neurological DisorderAJPEDO LIFENoch keine Bewertungen
- Biology: Investigatory ProjectDokument22 SeitenBiology: Investigatory ProjectNarayana BaipadithayaNoch keine Bewertungen
- Epilepsy: Bassel F. Shneker, MD, and Nathan B. Fountain, MDDokument53 SeitenEpilepsy: Bassel F. Shneker, MD, and Nathan B. Fountain, MDDiane Mx100% (1)
- 40 People vs. Rafanan, Jr.Dokument10 Seiten40 People vs. Rafanan, Jr.Simeon TutaanNoch keine Bewertungen
- Export Management EconomicsDokument30 SeitenExport Management EconomicsYash SampatNoch keine Bewertungen
- Eggermont 2019 ABRDokument15 SeitenEggermont 2019 ABRSujeet PathakNoch keine Bewertungen
- AMULDokument11 SeitenAMULkeshav956Noch keine Bewertungen
- Case Study 2Dokument5 SeitenCase Study 2api-247285537100% (1)
- Quiz 140322224412 Phpapp02Dokument26 SeitenQuiz 140322224412 Phpapp02Muhammad Mubeen Iqbal PuriNoch keine Bewertungen
- SLA in PEGA How To Configue Service Level Agreement - HKRDokument7 SeitenSLA in PEGA How To Configue Service Level Agreement - HKRsridhar varmaNoch keine Bewertungen
- Progressive Muscle RelaxationDokument4 SeitenProgressive Muscle RelaxationEstéphany Rodrigues ZanonatoNoch keine Bewertungen
- Evs ProjectDokument19 SeitenEvs ProjectSaloni KariyaNoch keine Bewertungen
- How To Block HTTP DDoS Attack With Cisco ASA FirewallDokument4 SeitenHow To Block HTTP DDoS Attack With Cisco ASA Firewallabdel taibNoch keine Bewertungen
- Z-Purlins: Technical DocumentationDokument11 SeitenZ-Purlins: Technical Documentationardit bedhiaNoch keine Bewertungen
- Continue Practice Exam Test Questions Part 1 of The SeriesDokument7 SeitenContinue Practice Exam Test Questions Part 1 of The SeriesKenn Earl Bringino VillanuevaNoch keine Bewertungen
- 8051 NotesDokument61 Seiten8051 Notessubramanyam62Noch keine Bewertungen
- Determination Rules SAP SDDokument2 SeitenDetermination Rules SAP SDkssumanthNoch keine Bewertungen
- Perancangan Crushing Plant Batu Andesit Di PT Nurmuda Cahaya Desa Batujajar Timur Kecamatan Batujajar Kabupaten Bandung Barat Provinsi Jawa BaratDokument8 SeitenPerancangan Crushing Plant Batu Andesit Di PT Nurmuda Cahaya Desa Batujajar Timur Kecamatan Batujajar Kabupaten Bandung Barat Provinsi Jawa BaratSutan AdityaNoch keine Bewertungen
- CV & Surat Lamaran KerjaDokument2 SeitenCV & Surat Lamaran KerjaAci Hiko RickoNoch keine Bewertungen
- Cooperative Learning: Complied By: ANGELICA T. ORDINEZADokument16 SeitenCooperative Learning: Complied By: ANGELICA T. ORDINEZAAlexis Kaye GullaNoch keine Bewertungen
- Sveba Dahlen - SRP240Dokument16 SeitenSveba Dahlen - SRP240Paola MendozaNoch keine Bewertungen
- ELEVATOR DOOR - pdf1Dokument10 SeitenELEVATOR DOOR - pdf1vigneshNoch keine Bewertungen
- Apron CapacityDokument10 SeitenApron CapacityMuchammad Ulil AidiNoch keine Bewertungen
- RFID Seminar AbstractDokument2 SeitenRFID Seminar Abstractanushabhagawath80% (5)
- Close Enough To Touch by Victoria Dahl - Chapter SamplerDokument23 SeitenClose Enough To Touch by Victoria Dahl - Chapter SamplerHarlequinAustraliaNoch keine Bewertungen
- Model 255 Aerosol Generator (Metone)Dokument20 SeitenModel 255 Aerosol Generator (Metone)Ali RizviNoch keine Bewertungen