Beruflich Dokumente
Kultur Dokumente
Transmission of Salmonella Bacteria
Hochgeladen von
Amy EstacioCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Transmission of Salmonella Bacteria
Hochgeladen von
Amy EstacioCopyright:
Verfügbare Formate
Transmission of Salmonella Bacteria
Food is the most common vehicle for the spread of Salmonella, and eggs are the
most common food implicated. [26] As one authority points out, “Studies showed
that the internal contents of eggs can be contaminated with [Salmonella], and this
contamination has been identified as a major risk factor in the emergence of human
illness.” [26]. Part of this risk stems from the variety of ways that Salmonella can
contaminate an egg. For example, the FDA has documented the following:
Bacteria can be on the outside of a shell egg. That’s because the egg exits the hen’s body
through the same passageway as feces is excreted. That’s why eggs are required to be washed at
the processing plant. All USDA graded eggs and most large volume processors follow the
washing step with a sanitizing rinse at the processing plant. It is also possible for eggs to become
infected by Salmonella Enteritidis fecal contamination through the pores of the shells after
they’re laid. SE also can be inside an uncracked, whole egg. Contamination of eggs may be due
to bacteria within the hen’s reproductive tract before the shell forms around the yolk and white.
SE doesn’t make the hen sick. [29]
Chicken is also a major cause of Salmonella. Beginning in 1998, the publisher
of Consumer Reports magazine has conducted surveys and tested chicken at
retail for Salmonella and Campylobacter. Its 2009 study found 14% of broiler
chickens at grocery stores to contain Salmonella. [28] A USDA Baseline Data
Collection Program report done in 1994 documented Salmonella contamination
on 20.0% of broiler-chicken carcasses [16]. However, in 2009 the same
USDA data collection survey showed the prevalence of Salmonella in broiler
chickens at 7.5%. [17] Additionally, turkey carries a lower risk with a
prevalence of 1.66%.
While Salmonella comes from animal feces, fruits and vegetables can become
contaminated. A common source is raw sprouts, which have been the
subject of at least 30 reported outbreaks of foodborne illnesses since 1996.
[30] The U.S. Department of Health and Human Services cautions against
consuming raw sprouts under any circumstances: “Unlike other fresh
produce, seeds and beans need warm and humid conditions to sprout and
grow. These conditions are also ideal for the growth of bacteria,
including Salmonella, Listeria, and E. coli.” [30]
http://www.about-salmonella.com/salmonella_transmission/
Symptoms of Salmonella infection include painful abdominal cramps, diarrhea and
often fever.
Salmonella infections can have a broad range of illness, from no symptoms to
severe illness. The most common clinical presentation is acute
gastroenteritis. Symptoms include diarrhea and abdominal cramps, often
accompanied by fever of 100°F to 102°F (38°C to 39°C). [4, 5] Other
symptoms may include bloody diarrhea, vomiting, headache and body
aches.
The incubation period, or the time from ingestion of the bacteria until the
symptoms start, is generally 6 to 72 hours; however, there is evidence that
in some situations the incubation can be longer than 10 days. [6, 7] People
with salmonellosis usually recover without treatment within 3 to 7 days. [5]
Nonetheless, the bacteria will continue to be present in the intestinal tract
and stool for weeks after recovery of symptoms—on average, 1 month in
adults and longer in children. [6]
S. Typhi and Paratyphi generally cause a bacteremic illness—Salmonella found
in the blood—of long duration. This illness is called enteric, typhoid, or
paratyphoid fever. [5] Symptoms start gradually, and include fever,
headache, malaise, lethargy, and abdominal pain. In children, it can present
as a non-specific fever. The incubation period for S. Typhi is usually 8 to 14
days, but it can range from 3 to 60 days. [5, 6] For S. Paratyphi infections,
the incubation period is similar to that of non-typhoidal Salmonella, 1 to 10
days. [5,6]
http://www.about-salmonella.com/salmonella_symptoms_risks/
Always wash your hands before you start preparing food.
Cook poultry until it reaches an internal temperature of 165 ºF. [33]
Cook beef and pork until they reach 160ºF. High quality steaks (not needle or blade tenderized) can be safely
cooked to 145ºF. [33]
Cook eggs until they reach 160ºF or until the yoke is solid. Pasteurized eggs are available in some grocery
stores. [33]
Do not eat or drink foods containing raw eggs. Examples include homemade eggnog, hollandaise sauce, and
undercooked French toast. [32]
Never drink raw (unpasteurized) milk. [32]
Avoid using the microwave for cooking raw foods of animal origin. Microwave-cooked foods do not reach a
uniform internal temperature, resulting in undercooked areas and survival of Salmonella.
If you are served undercooked meat, poultry, or eggs in a restaurant don’t hesitate to send your food back to the
kitchen for further cooking.
Avoid cross-contamination. That means that you should never allow foods that will not be cooked (like salads)
to come into contact with raw foods of animal origin (e.g., on dirty countertops, kitchen sinks, or cutting boards).
Wash hands, kitchen work surfaces, and utensils with soap and water immediately after they have been in
contact with raw foods of animal origin. [33]
Wash hands with soap after handling reptiles, amphibians or birds, or after contact with pet feces. Infants and
persons with compromised immune systems should have no direct or indirect contact with such pets.[32]
Reptiles, amphibians or birds, or any elements of their housing (such as water bowls) should never be allowed in
the kitchen.
Avoid eating in animal barns, and wash your hands with soap and water after visiting petting zoos or farm
settings.
Always wash your hands after going to the bathroom. The hands of an infected person who did not wash his or
her hands adequately after using the bathroom may also contaminate food.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Nursing Care Plan For Myocardial InfarctionDokument7 SeitenNursing Care Plan For Myocardial Infarctionmariejo95% (125)
- Case StudyDokument6 SeitenCase StudyApoorv Jain100% (1)
- Brain TumorDokument24 SeitenBrain TumorAmy EstacioNoch keine Bewertungen
- Easy ChairDokument11 SeitenEasy ChairVinod RushinathNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Resources DistributionDokument10 SeitenResources DistributionDarshan KanganeNoch keine Bewertungen
- Building System Design Plate 3-Ground Floor PLanDokument1 SeiteBuilding System Design Plate 3-Ground Floor PLanLester de GuzmanNoch keine Bewertungen
- Project On IDA NgoDokument20 SeitenProject On IDA NgoMayank SarafNoch keine Bewertungen
- Measure UP! Worksheet: Name - Date - ClassDokument2 SeitenMeasure UP! Worksheet: Name - Date - ClassnangungunaNoch keine Bewertungen
- Ybannag Customs and TraditionsDokument15 SeitenYbannag Customs and TraditionsNena de Alban100% (1)
- Reviion Sheet 16Dokument6 SeitenReviion Sheet 16tarekmosbahi mosbahiNoch keine Bewertungen
- English Quiz 2Dokument19 SeitenEnglish Quiz 2Yulia Nurfajar AiniNoch keine Bewertungen
- Why Do You Need NattoDokument13 SeitenWhy Do You Need NattoGwyneth100% (1)
- Nutrient Analysis of Raw and Processed Soybean and DevelopmentDokument6 SeitenNutrient Analysis of Raw and Processed Soybean and DevelopmentMounia TahriNoch keine Bewertungen
- QuestionnaireDokument8 SeitenQuestionnaireMelvin HonorioNoch keine Bewertungen
- Rules of Subject Verb Agreement Are All You NeedDokument8 SeitenRules of Subject Verb Agreement Are All You Needalexandra jacobNoch keine Bewertungen
- WORKSHEET 4.4 Types of CarbohydratesDokument3 SeitenWORKSHEET 4.4 Types of Carbohydratesmira bonzay100% (1)
- Organic Farming in The Philippines: and How It Affects Philippine AgricultureDokument6 SeitenOrganic Farming in The Philippines: and How It Affects Philippine AgricultureSarahNoch keine Bewertungen
- Science Section A UPSRDokument2 SeitenScience Section A UPSRvinno8556% (9)
- Talking GreeksDokument401 SeitenTalking Greekstwerkter100% (2)
- Cookery (Tvl-He) : Name of Learner: Grade/Section: Learning Strand: Date SubmittedDokument4 SeitenCookery (Tvl-He) : Name of Learner: Grade/Section: Learning Strand: Date SubmittedRonigrace Sanchez100% (3)
- Gess 209Dokument6 SeitenGess 209api-309501342Noch keine Bewertungen
- Leaflet Actiwave 140Dokument2 SeitenLeaflet Actiwave 140AnalystNoch keine Bewertungen
- Form of Past Perfect SimpleDokument3 SeitenForm of Past Perfect SimpleDagmardv ValyNoch keine Bewertungen
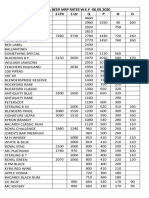
- Liquor & Beer MRP Rates Wef 17.12.2019 (1) - 1Dokument2 SeitenLiquor & Beer MRP Rates Wef 17.12.2019 (1) - 1Kondu Krishna Vamsi ChowdaryNoch keine Bewertungen
- Design and Fabrication of Paddy Cleaning MachineDokument5 SeitenDesign and Fabrication of Paddy Cleaning MachineDave RoneNoch keine Bewertungen
- EJERCICIOS4ESODokument29 SeitenEJERCICIOS4ESOLidia GutiérrezNoch keine Bewertungen
- Hussain Kapadawala 1Dokument56 SeitenHussain Kapadawala 1hussainkapda7276Noch keine Bewertungen
- EF3e Elem Progresstest 7 12 AnswerkeyDokument8 SeitenEF3e Elem Progresstest 7 12 AnswerkeyCarlos Júlio92% (13)
- Ingredients: Ep 18 - Rhubarb Trifle With Champagne Jelly and MascarponeDokument6 SeitenIngredients: Ep 18 - Rhubarb Trifle With Champagne Jelly and Mascarponegrupo077Noch keine Bewertungen
- Praveenkumar Pol KMF ProjectDokument57 SeitenPraveenkumar Pol KMF ProjectPraveenkumar. B. Pol83% (6)
- EjerciciosPresentTenses 210907 171536Dokument10 SeitenEjerciciosPresentTenses 210907 171536Andrea Martinez JiménezNoch keine Bewertungen
- 0877 Joel - 1Dokument3 Seiten0877 Joel - 1jesudossNoch keine Bewertungen
- Tcs Ninja NQT Previous Year PapersDokument210 SeitenTcs Ninja NQT Previous Year PapersVellasamy karthickNoch keine Bewertungen
- 12 Ways To Maximize Everyday in RamadanDokument12 Seiten12 Ways To Maximize Everyday in Ramadanthe_TRUTHNoch keine Bewertungen