Beruflich Dokumente
Kultur Dokumente
Trauma Bedah Saraf
Hochgeladen von
andikaisnaeniCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Trauma Bedah Saraf
Hochgeladen von
andikaisnaeniCopyright:
Verfügbare Formate
In
Invvestigation for clinically important br
brain
ain
injuries in patients with head injury
NICE Pathways bring together all NICE guidance, quality standards and other NICE
information on a specific topic.
NICE Pathways are interactive and designed to be used online. They are updated
regularly as new NICE guidance is published. To view the latest version of this pathway
see:
http://pathways.nice.org.uk/pathways/head-injury
Pathway last updated: 16 December 2016
This document contains a single pathway diagram and uses numbering to link the
boxes to the associated recommendations.
Copyright © NICE 2016. All rights reserved
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
Head injury path
pathwa
wayy Page 2 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
1 Person with head injury
No additional information
2 Choosing type of imaging
The current primary investigation of choice for the detection of acute clinically important brain
injuries is CT imaging of the head.
For safety, logistic and resource reasons, do not perform magnetic resonance imaging (MRI)
scanning as the primary investigation for clinically important brain injury in patients who have
sustained a head injury, although it is recognised that additional information of importance to the
patient's prognosis can sometimes be detected using MRI.
Ensure that there is appropriate equipment for maintaining and monitoring the patient within the
MRI environment and that all staff involved are aware of the dangers and necessary precautions
for working near an MRI scanner.
Do not use plain X-rays of the skull to diagnose significant brain injury without prior discussion
with a neuroscience unit. However, they are useful as part of the skeletal survey in children
presenting with suspected non-accidental injury.
3 Good radiation management
In line with good radiation exposure practice, make every effort to minimise radiation dose
during imaging of the head and cervical spine, while ensuring that image quality and coverage
is sufficient to achieve an adequate diagnostic study.
4 Adults
No additional information
Head injury path
pathwa
wayy Page 3 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
5 When to perform a CT head scan within 1 hour
For adults who have sustained a head injury and have any of the following risk factors, perform
a CT head scan within 1 hour of the risk factor being identified:
GCS less than 13 on initial assessment in the emergency department. See
recommendations on GCS [See page 9].
GCS less than 15 at 2 hours after the injury on assessment in the emergency department.
Suspected open or depressed skull fracture.
Any sign of basal skull fracture (haemotympanum, 'panda' eyes, cerebrospinal fluid leakage
from the ear or nose, Battle's sign).
Post-traumatic seizure.
Focal neurological deficit.
More than 1 episode of vomiting.
A provisional written radiology report should be made available within 1 hour of the scan being
performed.
Quality standards
The following quality statements are relevant to this part of the interactive flowchart.
1. CT head scans
4. Provisional radiology reports
6 When to perform a CT head scan within 8 hours
For adults with any of the following risk factors who have experienced some loss of
consciousness or amnesia since the injury, perform a CT head scan within 8 hours of the head
injury:
Age 65 years or older.
Any history of bleeding or clotting disorders.
Dangerous mechanism of injury (a pedestrian or cyclist struck by a motor vehicle, an
occupant ejected from a motor vehicle or a fall from a height of greater than 1 metre or 5
stairs).
More than 30 minutes' retrograde amnesia of events immediately before the head injury.
Head injury path
pathwa
wayy Page 4 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
A provisional written radiology report should be made available within 1 hour of the scan being
performed.
7 Children
No additional information
8 When to perform a CT head scan within 1 hour
For children who have sustained a head injury and have any of the following risk factors,
perform a CT head scan within 1 hour of the risk factor being identified:
Suspicion of non-accidental injury.
Post-traumatic seizure but no history of epilepsy.
On initial emergency department assessment GCS less than 14, or for children under 1
year GCS (paediatric) less than 15 (see recommendations on GCS [See page 9]).
At 2 hours after the injury, GCS less than 15.
Suspected open or depressed skull fracture or tense fontanelle.
Any sign of basal skull fracture (haemotympanum, 'panda' eyes, cerebrospinal fluid leakage
from the ear or nose, Battle's sign).
Focal neurological deficit.
For children under 1 year, presence of bruise, swelling or laceration of more than 5 cm on
the head.
A provisional written radiology report should be made available within 1 hour of the scan being
performed.
For information on sedation for imaging in children and young people see the NICE pathway on
sedation in children and young people.
Quality standards
The following quality statements are relevant to this part of the interactive flowchart.
1. CT head scans
4. Provisional radiology reports
Head injury path
pathwa
wayy Page 5 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
9 CT head scan versus observation
CT head scan
For children who have sustained a head injury and have more than 1 of the following risk
factors (and none of those in when to perform a CT head scan within 1 hour [See page 5]),
perform a CT head scan within 1 hour of the risk factors being identified:
Loss of consciousness lasting more than 5 minutes (witnessed).
Abnormal drowsiness.
Three or more discrete episodes of vomiting.
Dangerous mechanism of injury (high-speed road traffic accident either as pedestrian,
cyclist or vehicle occupant, fall from a height of greater than 3 metres, high-speed injury
from a projectile or other object).
Amnesia (antegrade or retrograde) lasting more than 5 minutes (assessment of amnesia
will not be possible in preverbal children and is unlikely to be possible in children aged
under 5 years).
A provisional written radiology report should be made available within 1 hour of the scan being
performed.
Observation
Children who have sustained a head injury and have only 1 of the risk factors in the
recommendation above (and none of those in when to perform a CT head scan within 1 hour
[See page 5]) should be observed for a minimum of 4 hours after the head injury.
If during observation any of the risk factors below are identified, perform a CT head scan within
1 hour:
GCS [See page 9] less than 15.
Further vomiting.
A further episode of abnormal drowsiness.
A provisional written radiology report should be made available within 1 hour of the scan being
performed. If none of these risk factors occur during observation, use clinical judgement to
determine whether a longer period of observation is needed.
For information on sedation for imaging in children and young people see the NICE pathway on
sedation in children and young people.
Head injury path
pathwa
wayy Page 6 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
Quality standards
The following quality statements are relevant to this part of the interactive flowchart.
1. CT head scans
4. Provisional radiology reports
10 Patients having warfarin treatment
For patients (adults and children) who have sustained a head injury with no other indications for
a CT head scan and who are having warfarin treatment, perform a CT head scan within 8 hours
of the injury. A provisional written radiology report should be made available within 1 hour of the
scan being performed.
Quality standards
The following quality statement is relevant to this part of the interactive flowchart.
2. CT head scans for people taking anticoagulants
11 When to involve a neurosurgeon
Discuss with a neurosurgeon the care of all patients with new, surgically significant
abnormalities on imaging. The definition of 'surgically significant' should be developed by local
neurosurgical centres and agreed with referring hospitals, along with referral procedures.
Regardless of imaging, other reasons for discussing a patient's care plan with a neurosurgeon
include:
Persisting coma (GCS [See page 9] 8 or less) after initial resuscitation.
Unexplained confusion which persists for more than 4 hours.
Deterioration in GCS score after admission (greater attention should be paid to motor
response deterioration).
Progressive focal neurological signs.
A seizure without full recovery.
Definite or suspected penetrating injury.
A cerebrospinal fluid leak.
Head injury path
pathwa
wayy Page 7 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
12 Return to assessment path
See head injury / assessment in the emergency department for patients with head injury
Head injury path
pathwa
wayy Page 8 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
Glasgow coma score
Base monitoring and exchange of information about individual patients on the three separate
responses on the GCS (for example, a patient scoring 13 based on scores of 4 on eye-opening,
4 on verbal response and 5 on motor response should be communicated as E4, V4, M5).
If a total score is recorded or communicated, base it on a sum of 15, and to avoid confusion
specify this denominator (for example, 13/15).
Describe the individual components of the GCS in all communications and every note and
ensure that they always accompany the total score.
In the paediatric version of the GCS, include a 'grimace' alternative to the verbal score to
facilitate scoring in preverbal children.
In some patients (for example, patients with dementia, underlying chronic neurological disorders
or learning disabilities) the pre-injury baseline GCS may be less than 15. Establish this where
possible, and take it into account during assessment.
Focal neurological deficit
problems restricted to a particular part of the body or a particular activity, for example, difficulties
with understanding, speaking, reading or writing; decreased sensation; loss of balance; general
weakness; visual changes; abnormal reflexes; and problems walking
High-energy head injury
for example, pedestrian struck by motor vehicle, occupant ejected from motor vehicle, fall from a
height of greater than 1 metre or more than 5 stairs, diving accident, high-speed motor vehicle
collision, rollover motor accident, accident involving motorised recreational vehicles, bicycle
collision, or any other potentially high-energy mechanism
Skull fracture or penetrating head injury
signs include clear fluid running from the ears or nose, black eye with no associated damage
around the eyes, bleeding from one or both ears, bruising behind one or both ears, penetrating
injury signs, visible trauma to the scalp or skull of concern to the professional
Head injury path
pathwa
wayy Page 9 of 10
Copyright © NICE 2016.
In
Invvestigation for clinically important br
brain
ain injuries in patients with head injury NICE Pathways
Sources
Head injury: assessment and early management (2014) NICE guideline CG176
Your responsibility
The guidance in this pathway represents the view of NICE, which was arrived at after careful
consideration of the evidence available. Those working in the NHS, local authorities, the wider
public, voluntary and community sectors and the private sector should take it into account when
carrying out their professional, managerial or voluntary duties. Implementation of this guidance
is the responsibility of local commissioners and/or providers. Commissioners and providers are
reminded that it is their responsibility to implement the guidance, in their local context, in light of
their duties to avoid unlawful discrimination and to have regard to promoting equality of
opportunity. Nothing in this guidance should be interpreted in a way which would be inconsistent
with compliance with those duties.
Copyright
Copyright © National Institute for Health and Care Excellence 2016. All rights reserved. NICE
copyright material can be downloaded for private research and study, and may be reproduced
for educational and not-for-profit purposes. No reproduction by or for commercial organisations,
or for commercial purposes, is allowed without the written permission of NICE.
Contact NICE
National Institute for Health and Care Excellence
Level 1A, City Tower
Piccadilly Plaza
Manchester
M1 4BT
www.nice.org.uk
nice@nice.org.uk
0845 003 7781
Head injury path
pathwa
wayy Page 10 of 10
Copyright © NICE 2016.
Das könnte Ihnen auch gefallen
- Azzi in Between - ActivitesDokument17 SeitenAzzi in Between - ActivitesSusanaGM0% (1)
- Case Report On The JokerDokument5 SeitenCase Report On The Jokersloppyjoes14Noch keine Bewertungen
- MmmGiuseppe Micieli, Anna Cavallini, Stefano Ricci, Domenico Consoli, Jonathan A. Edlow - Decision Algorithms For Emergency Neurology-Springer (2021)Dokument631 SeitenMmmGiuseppe Micieli, Anna Cavallini, Stefano Ricci, Domenico Consoli, Jonathan A. Edlow - Decision Algorithms For Emergency Neurology-Springer (2021)Bulbucan Iulia-Denisa0% (1)
- Food Safety ChecklistDokument4 SeitenFood Safety Checklistjalali007Noch keine Bewertungen
- Ages and Stages 24 Months QuestionairreDokument8 SeitenAges and Stages 24 Months QuestionairreandikaisnaeniNoch keine Bewertungen
- Tchokov-Gemiu - El PIano 2º MetodologíaDokument5 SeitenTchokov-Gemiu - El PIano 2º MetodologíaGenara Pajaraca MarthaNoch keine Bewertungen
- Teaching Cooperative Learning The Challenge For Teacher EducationDokument249 SeitenTeaching Cooperative Learning The Challenge For Teacher EducationBambang Sulistyo90% (10)
- Philosophy and Education in MalaysiaDokument42 SeitenPhilosophy and Education in MalaysiaThiyya SylviaNoch keine Bewertungen
- The True Rosicrucian & Holy Grail Traditions - Online CoursesDokument8 SeitenThe True Rosicrucian & Holy Grail Traditions - Online CoursesPanther PantherNoch keine Bewertungen
- Minor Ped Head TraumaDokument25 SeitenMinor Ped Head Traumalaila.forestaNoch keine Bewertungen
- RCH DEM Head Injury GuidelinesDokument4 SeitenRCH DEM Head Injury GuidelinesJerry LeeNoch keine Bewertungen
- Head Injury Management of PediatricDokument22 SeitenHead Injury Management of PediatricIrma KusumaNoch keine Bewertungen
- NICE Guidlines For Head InjuryDokument20 SeitenNICE Guidlines For Head InjuryMuhammed al-jumailyNoch keine Bewertungen
- The Management of Traumatic Brain InjuryDokument6 SeitenThe Management of Traumatic Brain InjuryDeli IndahNoch keine Bewertungen
- Indications For CT Scanning in Minor Head Injuries: A ReviewDokument6 SeitenIndications For CT Scanning in Minor Head Injuries: A ReviewariqNoch keine Bewertungen
- Basis 1Dokument5 SeitenBasis 1Sasmita MahadewiNoch keine Bewertungen
- Approach To HeadacheDokument61 SeitenApproach To Headachesabahat.husainNoch keine Bewertungen
- Indikasi Skull XrayDokument9 SeitenIndikasi Skull XrayHesti Nurmala RizqiNoch keine Bewertungen
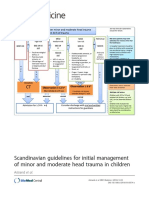
- Scandinavian Guidelines For Initial Management of Minor and Moderate Head Trauma in ChildrenDokument20 SeitenScandinavian Guidelines For Initial Management of Minor and Moderate Head Trauma in ChildrenRafael Mujica OreNoch keine Bewertungen
- Research: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryDokument8 SeitenResearch: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryCarlos Martin Yafac RiscoNoch keine Bewertungen
- Indications For CT Brain or Neck in Head InjuriesDokument4 SeitenIndications For CT Brain or Neck in Head InjuriesMehrine MehrNoch keine Bewertungen
- Guia Tec NiceDokument63 SeitenGuia Tec NiceAlexander BenavidesNoch keine Bewertungen
- Management Head Injury in ICUDokument5 SeitenManagement Head Injury in ICUIrma KusumaNoch keine Bewertungen
- Tayal 2007Dokument7 SeitenTayal 2007Candra YogiswaraNoch keine Bewertungen
- Poster No.: Congress: Type: Authors: Keywords:: Page 1 of 20Dokument22 SeitenPoster No.: Congress: Type: Authors: Keywords:: Page 1 of 20adityaNoch keine Bewertungen
- Lee 2018Dokument6 SeitenLee 2018fachriybalafifNoch keine Bewertungen
- Head Injury: Which Patients Need Imaging? Which Test Is Best?Dokument5 SeitenHead Injury: Which Patients Need Imaging? Which Test Is Best?crushnaNoch keine Bewertungen
- How Should Mild Head Injuries Be Assessed?Dokument4 SeitenHow Should Mild Head Injuries Be Assessed?anjarwatiNoch keine Bewertungen
- Growing Skull Fractures: Guidelines For Early Diagnosis and Surgical ManagementDokument6 SeitenGrowing Skull Fractures: Guidelines For Early Diagnosis and Surgical Management相壮壮Noch keine Bewertungen
- 2011 PEDIATRIC HEAD Imaging GuidelinesDokument56 Seiten2011 PEDIATRIC HEAD Imaging GuidelinesElena BelonosovNoch keine Bewertungen
- NIH Public Access: Predictors of Positive Head CT Scan and Neurosurgical Procedures After Minor Head TraumaDokument13 SeitenNIH Public Access: Predictors of Positive Head CT Scan and Neurosurgical Procedures After Minor Head TraumadenisNoch keine Bewertungen
- Initial Treatment For Closed Head Injuries PDFDokument1 SeiteInitial Treatment For Closed Head Injuries PDFdiaga081Noch keine Bewertungen
- Stroke Transient Ischaemic AttackDokument15 SeitenStroke Transient Ischaemic AttackAarif RanaNoch keine Bewertungen
- Management of Mild and Moderate Head Injuries in Adults: Dana Turliuc, A. CucuDokument11 SeitenManagement of Mild and Moderate Head Injuries in Adults: Dana Turliuc, A. CucuSarrah Kusuma DewiNoch keine Bewertungen
- CPG Early Management of Head Injury in AdultsDokument84 SeitenCPG Early Management of Head Injury in Adultsizwan taufikNoch keine Bewertungen
- Surgical Management: SurgeryDokument5 SeitenSurgical Management: SurgeryKarl Angelo MontanoNoch keine Bewertungen
- Cranial TraumaDokument46 SeitenCranial TraumaBhaskar SatsangiNoch keine Bewertungen
- NeuroVISION ArticleDokument8 SeitenNeuroVISION ArticleDanielle de Sa BoasquevisqueNoch keine Bewertungen
- Material paraDokument89 SeitenMaterial pararoberto gomesNoch keine Bewertungen
- Minor Head Trauma in Infants and Childre ManagmentDokument12 SeitenMinor Head Trauma in Infants and Childre ManagmentRita ValenteNoch keine Bewertungen
- ABSTRAK MilusDokument1 SeiteABSTRAK MilusIjah HaeraniNoch keine Bewertungen
- Routine NS ConsultDokument5 SeitenRoutine NS Consultyasser.yasser.yaNoch keine Bewertungen
- Imaging of Head Trauma: Part 1: IntroductionDokument28 SeitenImaging of Head Trauma: Part 1: Introductiondrnancy1786Noch keine Bewertungen
- Research Manuscript FinalDokument12 SeitenResearch Manuscript FinalTHESSNAVARRONoch keine Bewertungen
- Acep Head Mild Trauma PoliceDokument35 SeitenAcep Head Mild Trauma PolicehaithamNoch keine Bewertungen
- Head Injury 2022.Dokument45 SeitenHead Injury 2022.Alia QNoch keine Bewertungen
- Adult Routine Head CTDokument17 SeitenAdult Routine Head CTAvan IchsanNoch keine Bewertungen
- CT Head AnatomyDokument57 SeitenCT Head AnatomyMaajid Mohi Ud Din MalikNoch keine Bewertungen
- Pone 0211599Dokument12 SeitenPone 0211599HILA GINANoch keine Bewertungen
- CtscanchildDokument3 SeitenCtscanchildGautamu ZalavadiyaNoch keine Bewertungen
- Evaluation of The Relationship Between Binocular Anomaly and Headache Prospective Cross Sectional StudyDokument7 SeitenEvaluation of The Relationship Between Binocular Anomaly and Headache Prospective Cross Sectional StudyEstefania GuerreroNoch keine Bewertungen
- Peripheral VertigoDokument18 SeitenPeripheral VertigoJohan Andrea Arguello PeñaNoch keine Bewertungen
- Kasturi - Head InjuryDokument18 SeitenKasturi - Head InjuryRazak GhaniNoch keine Bewertungen
- The Team in A Nutshell : Dr. Haim EzerDokument22 SeitenThe Team in A Nutshell : Dr. Haim EzerHaim EzerNoch keine Bewertungen
- Head Injuries in Infants and Children CA5041 Id 7883 v2.1Dokument9 SeitenHead Injuries in Infants and Children CA5041 Id 7883 v2.1bhanugorijala28Noch keine Bewertungen
- Recommendations: Level 1b Level 1bDokument5 SeitenRecommendations: Level 1b Level 1bIbrahem Y. NajjarNoch keine Bewertungen
- Trauma Management - Classified by Organs & Systems Group C33Dokument139 SeitenTrauma Management - Classified by Organs & Systems Group C33ziadalmomany99Noch keine Bewertungen
- Thenan - Danial - AinaDokument33 SeitenThenan - Danial - AinaThenan SankarNoch keine Bewertungen
- Head Injury With Craniotomy A Case Presentation of BSN 3 YB 7Dokument90 SeitenHead Injury With Craniotomy A Case Presentation of BSN 3 YB 7MARIA STEPHANY DELA CRUZNoch keine Bewertungen
- Clinical Guideline SPPDDokument6 SeitenClinical Guideline SPPDBejoku lanangnyaNoch keine Bewertungen
- Guidelines For Safe Transfer of The Brain-Injured Patient: Trauma and Stroke, 2019Dokument13 SeitenGuidelines For Safe Transfer of The Brain-Injured Patient: Trauma and Stroke, 2019VasFel GicoNoch keine Bewertungen
- Tirado-Bsn 4d-Journal Summary and ReflectionDokument3 SeitenTirado-Bsn 4d-Journal Summary and ReflectionJeniper Marie Cute29Noch keine Bewertungen
- Neuro-Ophthalmological Biomarkers of Visual Outcome in Newly Diagnosed Idiopathic Intracranial HypertensionDokument8 SeitenNeuro-Ophthalmological Biomarkers of Visual Outcome in Newly Diagnosed Idiopathic Intracranial HypertensionMira TamilaNoch keine Bewertungen
- SCIWORA-Spinal Cord Injury Without Radiological Abnormality: Veena Kalra, Sheffali Gulati, Mahesh Kamate and Ajay GargDokument3 SeitenSCIWORA-Spinal Cord Injury Without Radiological Abnormality: Veena Kalra, Sheffali Gulati, Mahesh Kamate and Ajay GargnsatriotomoNoch keine Bewertungen
- Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and AdultsDokument231 SeitenHead Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adultsakunkeren2023Noch keine Bewertungen
- Good Morning EveryoneDokument6 SeitenGood Morning EveryoneRichlle CortesNoch keine Bewertungen
- Echography and Doppler of the BrainVon EverandEchography and Doppler of the BrainChiara RobbaNoch keine Bewertungen
- Interventional Management of Head and Face Pain: Nerve Blocks and BeyondVon EverandInterventional Management of Head and Face Pain: Nerve Blocks and BeyondNoch keine Bewertungen
- PIC Oprator Excavator PC RIYANTODokument1 SeitePIC Oprator Excavator PC RIYANTOandikaisnaeniNoch keine Bewertungen
- List Staff Subkont (Rapid Ag 1 Feb 2021) List Staff Subkont (Rapid Ag 14 Feb 2021)Dokument1 SeiteList Staff Subkont (Rapid Ag 1 Feb 2021) List Staff Subkont (Rapid Ag 14 Feb 2021)andikaisnaeniNoch keine Bewertungen
- Site Walk Finding Report 30 Juni 2020Dokument4 SeitenSite Walk Finding Report 30 Juni 2020andikaisnaeniNoch keine Bewertungen
- List Karyawan Swab Antigen 1 Februari 2021 No Nama Dept JabatanDokument2 SeitenList Karyawan Swab Antigen 1 Februari 2021 No Nama Dept JabatanandikaisnaeniNoch keine Bewertungen
- Site Walk Finding Report 30 Juni 2020Dokument4 SeitenSite Walk Finding Report 30 Juni 2020andikaisnaeniNoch keine Bewertungen
- Chart and Cheklist Hygiene and Risk Matrix 20 Oktober 2020Dokument2 SeitenChart and Cheklist Hygiene and Risk Matrix 20 Oktober 2020andikaisnaeniNoch keine Bewertungen
- PIC Oprator Excavator PC SOLEMANDokument1 SeitePIC Oprator Excavator PC SOLEMANandikaisnaeniNoch keine Bewertungen
- Site Walk Finding Report 13-Mei-2020Dokument10 SeitenSite Walk Finding Report 13-Mei-2020andikaisnaeniNoch keine Bewertungen
- Suggested Checklist For RestaurantsDokument11 SeitenSuggested Checklist For Restaurantsaarshshah10100% (1)
- Dialy MP ARKM The StatureDokument1 SeiteDialy MP ARKM The StatureandikaisnaeniNoch keine Bewertungen
- Food Safety and Sanitation ChecklistDokument5 SeitenFood Safety and Sanitation ChecklistandikaisnaeniNoch keine Bewertungen
- Dialy MP ARKM The StatureDokument1 SeiteDialy MP ARKM The StatureandikaisnaeniNoch keine Bewertungen
- LUPUS Scientificarticle PDFDokument31 SeitenLUPUS Scientificarticle PDFDwi Astika SariNoch keine Bewertungen
- SC ManagementDokument8 SeitenSC ManagementandikaisnaeniNoch keine Bewertungen
- IMCA-Briefing-428 (Medical Examination of Divers)Dokument20 SeitenIMCA-Briefing-428 (Medical Examination of Divers)Ernesto CarmonaNoch keine Bewertungen
- Jurnal Personal Hygiene 2Dokument6 SeitenJurnal Personal Hygiene 2andikaisnaeniNoch keine Bewertungen
- Presentation Corona VirusDokument11 SeitenPresentation Corona Virusandikaisnaeni100% (2)
- ECG Changes During Septic Shock PDFDokument10 SeitenECG Changes During Septic Shock PDFandikaisnaeniNoch keine Bewertungen
- Vankova 2014Dokument6 SeitenVankova 2014andikaisnaeniNoch keine Bewertungen
- Vasopressors and Inotropes in ShockDokument8 SeitenVasopressors and Inotropes in ShockRiska PashaNoch keine Bewertungen
- Abdominal HysterectomyDokument5 SeitenAbdominal HysterectomyandikaisnaeniNoch keine Bewertungen
- Guidelines For The Management of Acute Cervical Spine and Spinal Cord InjuriesDokument259 SeitenGuidelines For The Management of Acute Cervical Spine and Spinal Cord InjuriesMedstudent JombloNoch keine Bewertungen
- The e Ect of Zinc Sulfate On Prevention, Incidence, and Severity of Mucositis in Leukemia Patients Undergoing ChemotherapyDokument8 SeitenThe e Ect of Zinc Sulfate On Prevention, Incidence, and Severity of Mucositis in Leukemia Patients Undergoing ChemotherapyandikaisnaeniNoch keine Bewertungen
- First Aid 2016 Guidelines - EN PDFDokument192 SeitenFirst Aid 2016 Guidelines - EN PDFKai HarukaNoch keine Bewertungen
- Asuhan Keperawatan: Diabetic Ketoacidosis Hyperglycemic Hyperosmolar StateDokument50 SeitenAsuhan Keperawatan: Diabetic Ketoacidosis Hyperglycemic Hyperosmolar StateandikaisnaeniNoch keine Bewertungen
- Post Op Cabg CareDokument31 SeitenPost Op Cabg CareYeria Rayanti100% (1)
- KDIGO AKI Guideline DownloadDokument141 SeitenKDIGO AKI Guideline DownloadSandi AuliaNoch keine Bewertungen
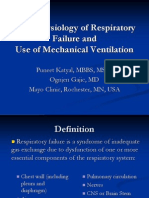
- Respiratory Failure Mechanical VentilationDokument37 SeitenRespiratory Failure Mechanical Ventilationawakepull312Noch keine Bewertungen
- Homework 1Dokument10 SeitenHomework 1Nam Anh KiraiNoch keine Bewertungen
- Krznaric R 2012 CH 03 How To Find Fulfilling Work Giving Meaning To WorkDokument24 SeitenKrznaric R 2012 CH 03 How To Find Fulfilling Work Giving Meaning To WorkAline BitencourtNoch keine Bewertungen
- Sharma Ishan Final DraftDokument5 SeitenSharma Ishan Final Draftapi-242143314Noch keine Bewertungen
- Schizophrenia: by Byawele Jairus WangusaDokument30 SeitenSchizophrenia: by Byawele Jairus WangusaAYO NELSONNoch keine Bewertungen
- Camera Shot TypeDokument3 SeitenCamera Shot TypeJulie Ann PajarillaNoch keine Bewertungen
- Abetare and Dancing 230109Dokument11 SeitenAbetare and Dancing 230109Adelina GjNoch keine Bewertungen
- Gestalt TherapyDokument15 SeitenGestalt TherapyJoy Caniete BermudezNoch keine Bewertungen
- s3 Lesson PlanDokument4 Seitens3 Lesson Planapi-230087515Noch keine Bewertungen
- CAS Evaluation FormsDokument2 SeitenCAS Evaluation FormsprandayNoch keine Bewertungen
- Gentile Formative Assessment - Psiii sp25Dokument6 SeitenGentile Formative Assessment - Psiii sp25api-321979646Noch keine Bewertungen
- Syllabus: FOR (Compulsory, Elective & Pass)Dokument61 SeitenSyllabus: FOR (Compulsory, Elective & Pass)Jogendra meherNoch keine Bewertungen
- Age Term Date Student Instrument Teacher: E E G GDokument1 SeiteAge Term Date Student Instrument Teacher: E E G GAustin SalsburyNoch keine Bewertungen
- The Mayans: Vade Mecum, Volventibus AnnisDokument11 SeitenThe Mayans: Vade Mecum, Volventibus AnnisOnenessNoch keine Bewertungen
- The 21st Century TeacherDokument23 SeitenThe 21st Century TeacherJessa LoronoNoch keine Bewertungen
- Individual Differences NotesDokument4 SeitenIndividual Differences NotesCiku CakNoch keine Bewertungen
- Individual Performance Commitment and Review Form (IPCRF) : To Be Filled in During PlanningDokument7 SeitenIndividual Performance Commitment and Review Form (IPCRF) : To Be Filled in During PlanningRofil AlbaoNoch keine Bewertungen
- ??? Seashell MagickDokument3 Seiten??? Seashell MagickBarbra AntonNoch keine Bewertungen
- HapticityDokument19 SeitenHapticitySauda DarNoch keine Bewertungen
- 4.labov's Narrative CategoriesDokument1 Seite4.labov's Narrative Categorieslilamy84100% (1)
- Jail Faces Mental Health Challenges: Ef GHDokument8 SeitenJail Faces Mental Health Challenges: Ef GHDavid PenticuffNoch keine Bewertungen
- Demographic, Personality, and Social Cognition Correlates of Coronavirus Guideline Adherence in A U.S. SampleDokument11 SeitenDemographic, Personality, and Social Cognition Correlates of Coronavirus Guideline Adherence in A U.S. Samplesayyid cbrNoch keine Bewertungen
- Eng 3rd Q Week 4Dokument23 SeitenEng 3rd Q Week 4Sarah Visperas RogasNoch keine Bewertungen
- Gontarski-Beckett's Voice(s) PDFDokument21 SeitenGontarski-Beckett's Voice(s) PDFTrad AnonNoch keine Bewertungen
- Communication Styles: 4 Basic Types Which Type Describes You?Dokument44 SeitenCommunication Styles: 4 Basic Types Which Type Describes You?amritaNoch keine Bewertungen