Beruflich Dokumente
Kultur Dokumente
Management of Diabetes
Hochgeladen von
Twinkle SalongaCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Management of Diabetes
Hochgeladen von
Twinkle SalongaCopyright:
Verfügbare Formate
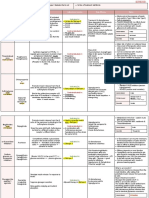
Hypoglycemic drugs
• Older drugs are cheaper and have established benefits for reducing microvascular disease therefore usually recommended as first-line therapy ( Metformin
etformin and Sulphonylureas )
• Newer drugs using is not supported by evidence for reduction in microvascular disease (because the trials have not yet been done) an
andd they are much more expensive so are often reserved for later therapy
after failure of metformin and sulphonylureas. ( One guideline which follows these principles is shown in (Figure )
Mechanism of action Clinical Use
1- Increases insulin sensitivity ‘insulin sensitiser’ because it lowers insulin levels
levels. Use:
Biguanides 2-
3-
It reduces the rate of gluconeogenesis, and hence hepatic glucose output
It has effects on gut glucose uptake and utilisation.
output. • It is employed as first-line
line therapy in all patients who tolerate it, and
• its use is maintained when additional agents are added as glycaemia deteriorates.
deteriorates
4- At the molecular level, metformin acts as a weak inhibitor of mitochondrial Dose:
respiration, which (AMP) and (ATP). This has : • Introduced
ntroduced at low dose (500 mg twice daily) to minimise risk of GIT side effects.
Metformin : a- Direct effects on flux
lux through gluconeogenesis.
gluconeogenesis • The usual maintenance dose is 1 g twice daily.
• It's the only biguanide now available. b- It activates intracellular energy sensor AMP-kinase,
kinase, which is involved in :
Side effects :
- GLUT4 metabolism and
• It is now widely used as first-line
line • GIT side-effects with metformin:
metformin
- Fatty
atty acid oxidation,
therapy for type 2 diabetes, - Diarrhoea,
BUT its mechanism of action remains unclear at a cellular level.
irrespective of body weight. - Abdominal cramps,
• It given adjunct to insulin therapy in It does not : - Bloating
obese pa ents with type 1 diabetes. 1- Affect
ffect insulin secretion, - nausea.
2- Induce hypoglycaemia • Lactic acidosis in renal impairment , hepatic impairment , alcohol excess :
3- Predispose
redispose to weight gain. helpful on obese people & normal weight. - Dose halved if GFR 30–45
30 mL/min
N.B. has established benefits in microvascular disease - Shouldn’t used if GFR< 30 mL/min , hepatic impairment , alcohol excess.
• Their action is to bind to the sulfonylurea receptor on the cell membrane, Use:
Sulphonylureas which closes ATP-sensitive
sensitive potassium channels and blocks potassium efflux
resulting in depolarization which promotes influx of calcium, a signal for insulin
• Often used as an add-on
on to metformin, if glycaemia is inadequately controlled on
metformin alone (see Fig. above).
insulin secretagogues release.
( They promote pancreatic β-cell
cell insulin secretion ) Dose:
They are ineffective in patients without a functional beta-cell
beta cell mass & their effect wears The dose–response of all sulphonylureas is steepest at low doses.
dose
off as the beta-cell
cell mass declines.
Side effects :
It does cause : - Weight gain not preferred to be used in obese individuals.
1- Hasten beta-cell apoptosis.
apoptosis - Hypoglycaemia Hypoglycaemia occurs because the closure of KATP
2- Induce hypoglycemia. channels brings about unregulated insulin secretion, even with normal or low
3- Promote weight gain. blood glucose levels.
Sulfonylureas should be used with care in patients with liver disease.
N.B. has established benefits in microvascular disease. Patients with renal impairment should only be given those primarily excreted by liver.
• They reduce insulin resistance by bind and activate peroxisome proliferator
proliferator-activated A number of adverse effects become apparent and their use has declined.
receptor-γ (PPAR γ), a nuclear receptor present mainly in adipose tissue that 1- Rosiglitazone :
regulates the expression of several genes involved in metabolism. - Increase the risk of MI ( withdrawn in 2010).
1- TZDs potentiate the effect of endogenous or injected insulin.: 2- Pioglitazone :
- Directly
irectly (in the adipose cells) and Uses :
- Indirectly
ndirectly (by altering release of ‘adipokines’, such as adiponectin, which
Thiazolidinediones alter insulin sensitivity in the liver).
- More
- Has
ore effective in insulin-resistant
insulin patients.
as a beneficial effect in reducing fatty liver and NASH
'glitazones' or 'PPARγ agonists
agonists' 2- Act indirectly via the glucose–– fatty acid cycle, lowering free fatty acid levels and thus - usually added to metformin with or without sulphonylurea therapy
promoting glucose consumption by muscle.
muscl
- may be given with insulin therapy
3- Reduce hepatic glucose production, (effect
effect that is synergistic with that of metformin)
Side effects : (Does
oes not appear to increase the risk of myocardial infarction BUT)
It doesn't & Does cause : - it causes :
1- Hypoglycaemia does not occur (Plasma insulin concentrations are not increased) • Exacerbation of cardiac failure by causing fluid retention,
2- TZDs increase pre-adipocyte
adipocyte differentiation, resulting in an increase in fat • Increases
ncreases the risk of bone fracture,
mass and in body weight. • Bladder cancer.
The "incretin effect" is :
• The
he augmentation of insulin secretion seen when a glucose stimulus is given orally rather than IV, and
d reflects the release of incretin peptides from the L cells in intestine:
1- Glucagon-like
like pep7de 1 (GLP-1)
(GLP
2- Gastric inhibitory polypeptide (GIP).
Incretin-based
based therapies:
- DPP-4
4 (dipep7dyl pep7dase 4) rapidly inactivates GLP-1.
- GLP-1 analogues
The incre n effect is diminished in type 2 diabetes, and this has s mulated the development of two incretin-based
based therapeutic approaches :
- DPP-4 inhibitors
1- ‘gliptins’, or DPP-4
4 inhibitors :
- Prevent breakdown enhance concentrations of endogenous GLP-1
GLP & GIP.
- Drugs : 1- Sitaglip n 2- Vildaglip
V n 3- Saxaglip n 4-Linagliptin.
inagliptin.
Doesn't cause hypoglycemia :
Unlike sulphonylureas, they only :
promote insulin secretion when there is a 2- GLP-1
1 receptor agonists :
glucose ‘trigger’ for insulin secretion. - have a similar structure to GLP-1
GLP 1 but have been modified to resist breakdown by DPPDPP-4.
- These agents are not orally active and have to be given by subcutaneous injection
injection.
Thus, when the blood glucose is normal, the
insulin secretion is not augmented and so
- They
hey have a key advantage over the DPP-4
DPP inhibitors: because the GLP-11 ac vity aachieved is supra-physiological :
these agents do not cause hypoglycaemia. • it delays gastric emptying and,
• at the level of the hypothalamus, decreases appetite.
Thus, injectable GLP-1
1 analogues lower blood glucose and result in weight loss – an appealing therapy, as the majority of patients with type 2 diabetes are obese.
- Drugs: Exenatide (twice daily) / Liraglutide (once daily).
inhibitor Dapagliflozin
The sodium and glucose transporter 2 (SGLT2) inhibitor: apagliflozin ( licensed for use in 2012 ).
• Glucose is filtered freely in the renal glomeruli and reabsorbed
reabsorbed in the proximal tubules via SGLT2.
SGLT2 inhibitors • Inhibition results in about 25% of the filtered
ed glucose not being reabsorbed with consequent glycosuria S.E: increased urinary tract and genital fungal infections.
• This
his helps to lower blood glucose AND results in calorie loss and subsequent weight loss
loss.
• α-glucosidase inhibitors ( Acarbose taken with each meal ) competitively inhibits alpha
alpha-glucosidase
glucosidase enzymes situated in the brush border of the intestine,
α -glucosidase
glucosidase reducing absorption
orption of dietary carbohydrate
1- Abdominal discomfort
So, undigested
ndigested starch then enter the large intestine where it will be broken down by fermentation causing (S.E.) :
inhibitors 2- Flatulence
3- Diarrhoea
iarrhoea can result
Das könnte Ihnen auch gefallen
- Wa0009.Dokument1 SeiteWa0009.Yael riveroNoch keine Bewertungen
- Practical Insulin: A Handbook for Prescribing ProvidersVon EverandPractical Insulin: A Handbook for Prescribing ProvidersBewertung: 5 von 5 Sternen5/5 (2)
- 4A Drug SheetDokument14 Seiten4A Drug SheetTherese PagayNoch keine Bewertungen
- GLYBURIDEDokument3 SeitenGLYBURIDEJohn Carlo SamsonNoch keine Bewertungen
- Diabetes Dosing Tip SheetDokument11 SeitenDiabetes Dosing Tip SheetYas PurohitNoch keine Bewertungen
- Drug Study ProglinDokument2 SeitenDrug Study ProglinChris Denver BancaleNoch keine Bewertungen
- Janumet-Xr MakassarDokument49 SeitenJanumet-Xr MakassarSuardy CiayadiNoch keine Bewertungen
- Metformin in 2019Dokument2 SeitenMetformin in 2019Juaan AvilaNoch keine Bewertungen
- Diabetes Drug Chart: Drug Action Use Side Effects Nursing ImplicationsDokument2 SeitenDiabetes Drug Chart: Drug Action Use Side Effects Nursing ImplicationspulmonologistNoch keine Bewertungen
- Drug StudyDokument5 SeitenDrug StudyLyhNoch keine Bewertungen
- Medication Administration WorksheetDokument6 SeitenMedication Administration WorksheetCheska CarrionNoch keine Bewertungen
- Drug Study TemplateDokument2 SeitenDrug Study TemplateMary hope DomalaonNoch keine Bewertungen
- DM AND DI DrugsDokument13 SeitenDM AND DI DrugsAisha MarieNoch keine Bewertungen
- Topic: DM Section: 4 Group NamesDokument8 SeitenTopic: DM Section: 4 Group NamesTurkish DizilerNoch keine Bewertungen
- FINAL Diabetes Medication Summary SSDokument1 SeiteFINAL Diabetes Medication Summary SSronique reidNoch keine Bewertungen
- Diabetes Treatment: PancreatitisDokument2 SeitenDiabetes Treatment: PancreatitisSafiya JamesNoch keine Bewertungen
- Endo Pharma ElhDokument14 SeitenEndo Pharma Elhodiodi57Noch keine Bewertungen
- Leaflet JARDY MET Tablet RangeDokument1 SeiteLeaflet JARDY MET Tablet RangeijackaliceNoch keine Bewertungen
- ADA 2023.-154-159 - OrganizedDokument6 SeitenADA 2023.-154-159 - OrganizedEfren BalsecaNoch keine Bewertungen
- Finals PHARMACOTHERAPHY OF DIABETES MELLITUS 2017Dokument8 SeitenFinals PHARMACOTHERAPHY OF DIABETES MELLITUS 2017Sheryl Layne Lao-SebrioNoch keine Bewertungen
- Final Magnesium SulfateDokument3 SeitenFinal Magnesium SulfateGwyn RosalesNoch keine Bewertungen
- Drugs For DiabetesDokument8 SeitenDrugs For DiabetesUsmanNoch keine Bewertungen
- 5.CHAPTER 5 Using Oral MedicationsDokument6 Seiten5.CHAPTER 5 Using Oral MedicationsGautam ManoharNoch keine Bewertungen
- Pancreatic Hormones Antidiabetic Drugs Part 2Dokument24 SeitenPancreatic Hormones Antidiabetic Drugs Part 2jenet soleilNoch keine Bewertungen
- ANTI-DIABETIC AGENTS (OHAs)Dokument42 SeitenANTI-DIABETIC AGENTS (OHAs)Prajwal Rao KNoch keine Bewertungen
- Antidiabetic Drugs - AMBOSSDokument13 SeitenAntidiabetic Drugs - AMBOSSOpio IsaacNoch keine Bewertungen
- Pomr Mik SK 4 NeewwDokument4 SeitenPomr Mik SK 4 NeewwDewi Ayu CahyaningrumNoch keine Bewertungen
- Getformin Tab Leaflet PakistanDokument2 SeitenGetformin Tab Leaflet PakistanMuhammad Vaqar HussainNoch keine Bewertungen
- Danuglipron (2023) : Activate GLP-1 ReceptorsDokument2 SeitenDanuglipron (2023) : Activate GLP-1 Receptorseslambasuony98Noch keine Bewertungen
- Lamirax Lamotrigina: Comprimidos DispersablesDokument2 SeitenLamirax Lamotrigina: Comprimidos DispersablesFlorenciaNoch keine Bewertungen
- Magnesium SulfateDokument2 SeitenMagnesium SulfateGwyn Rosales100% (1)
- Anti DepressantDokument6 SeitenAnti Depressantyahyaahmed152000Noch keine Bewertungen
- 9+10. Oral Antidabetic DrugsDokument3 Seiten9+10. Oral Antidabetic Drugsmohammed alrubaiaanNoch keine Bewertungen
- DiabetesAlgorithm Stanford2018Dokument7 SeitenDiabetesAlgorithm Stanford2018Rogelio MoscosoNoch keine Bewertungen
- MetoclopramideDokument1 SeiteMetoclopramideJack SolomonNoch keine Bewertungen
- Drug StudyDokument6 SeitenDrug StudyBea Lee VenturanzaNoch keine Bewertungen
- Blood Glucose Control Pathway in Type 2 Diabetes Apr 2013Dokument2 SeitenBlood Glucose Control Pathway in Type 2 Diabetes Apr 2013J WongNoch keine Bewertungen
- Drug StudyDokument4 SeitenDrug StudyhsiriaNoch keine Bewertungen
- Review of Pharmacology (PGMEE) Paperback - 2018 (PDFDrive)Dokument1 SeiteReview of Pharmacology (PGMEE) Paperback - 2018 (PDFDrive)Muez AlkeblawiNoch keine Bewertungen
- PHARMA-RATIONALE-R4.2-Pancreatic Hormones and Antidiabetic DrugsDokument3 SeitenPHARMA-RATIONALE-R4.2-Pancreatic Hormones and Antidiabetic Drugscharmainemargaret.parreno.medNoch keine Bewertungen
- Diabetes Mellitus Treatment ProtocolDokument1 SeiteDiabetes Mellitus Treatment ProtocolPuja Zarkar100% (1)
- Linagliptin, Norgesic ForteDokument4 SeitenLinagliptin, Norgesic FortehahahaNoch keine Bewertungen
- Emilio Aguinaldo College: School of NursingDokument3 SeitenEmilio Aguinaldo College: School of Nursingbryan.zabala.mnlNoch keine Bewertungen
- Drug Interactions ActivityDokument5 SeitenDrug Interactions ActivityPatricia Camryne AmbidaNoch keine Bewertungen
- Pharma Revision FileDokument21 SeitenPharma Revision Filemaxwell amponsahNoch keine Bewertungen
- Medication Dosage and Availability Classification Mechanism of Action Indication Action Contraindication Adverse Effect Nursing Responsibility DoseDokument3 SeitenMedication Dosage and Availability Classification Mechanism of Action Indication Action Contraindication Adverse Effect Nursing Responsibility Dosebambem aevanNoch keine Bewertungen
- Drug Interaction DMT2Dokument12 SeitenDrug Interaction DMT2Dhonat FlashNoch keine Bewertungen
- Endocrine CologyDokument124 SeitenEndocrine CologyBehailu TejeNoch keine Bewertungen
- Oral Diabetes Mellitus MedicationsDokument43 SeitenOral Diabetes Mellitus MedicationsSanjeev Harry BudhooramNoch keine Bewertungen
- Oral Management of Diabetes Type IIDokument34 SeitenOral Management of Diabetes Type IIYasser Gebril100% (1)
- Pharmacotherapy of Diabetes Mellitus: Dr. Ave Olivia Rahman, Msc. Bagian Farmakologi Fkik UnjaDokument42 SeitenPharmacotherapy of Diabetes Mellitus: Dr. Ave Olivia Rahman, Msc. Bagian Farmakologi Fkik UnjaGita Tanbao SuselinNoch keine Bewertungen
- Icjpir-15-103 9-14Dokument6 SeitenIcjpir-15-103 9-14Sriram NagarajanNoch keine Bewertungen
- Drug StudyDokument4 SeitenDrug StudyAilah Mae Dela Cruz0% (1)
- Algorithm For Blood Glucose Lowering Therapy in Adults With Type 2 Diabetes PDF 2185604173Dokument1 SeiteAlgorithm For Blood Glucose Lowering Therapy in Adults With Type 2 Diabetes PDF 2185604173AlessioNavarraNoch keine Bewertungen
- Antimicrobial Agents Mucosal Protective Agents: Amoxicillin Clarithromycin SucralfateDokument2 SeitenAntimicrobial Agents Mucosal Protective Agents: Amoxicillin Clarithromycin SucralfateAlexandra AlexaNoch keine Bewertungen
- Generic NameDokument5 SeitenGeneric NameJanika BecieraNoch keine Bewertungen
- Oral Antidiabetic DrugsDokument46 SeitenOral Antidiabetic Drugscarms100% (1)
- Amaryl M PI - May 2018marylDokument11 SeitenAmaryl M PI - May 2018marylvicky upretiNoch keine Bewertungen
- How To RecoverDokument3 SeitenHow To RecoverSterr LiingNoch keine Bewertungen
- Wellness Lecture: How To Have A Healthy Work-Life Balance in The New NormalDokument41 SeitenWellness Lecture: How To Have A Healthy Work-Life Balance in The New NormalTwinkle SalongaNoch keine Bewertungen
- Alcohol, Drugs and The Workplace - The Role of Medical ProfessionalsDokument40 SeitenAlcohol, Drugs and The Workplace - The Role of Medical ProfessionalsTwinkle SalongaNoch keine Bewertungen
- Booster VaccinesDokument40 SeitenBooster VaccinesTwinkle SalongaNoch keine Bewertungen
- TIPS For Workplace & Home Holiday Celebrations: Worker Health Advisory On COVID-19Dokument1 SeiteTIPS For Workplace & Home Holiday Celebrations: Worker Health Advisory On COVID-19Twinkle SalongaNoch keine Bewertungen
- How To Manage Sleep DisordersDokument19 SeitenHow To Manage Sleep DisordersTwinkle SalongaNoch keine Bewertungen
- 2 Teleconsultation For Filipino CliniciansDokument25 Seiten2 Teleconsultation For Filipino CliniciansTwinkle Salonga0% (1)
- Zones For Rate & Transit Times (Outbound)Dokument2 SeitenZones For Rate & Transit Times (Outbound)Twinkle SalongaNoch keine Bewertungen
- Diseases of The Immune SystemDokument3 SeitenDiseases of The Immune SystemTwinkle SalongaNoch keine Bewertungen
- Surgery - Pediatric GIT, Abdominal Wall, Neoplasms - 2014ADokument14 SeitenSurgery - Pediatric GIT, Abdominal Wall, Neoplasms - 2014ATwinkle SalongaNoch keine Bewertungen
- Calcium Lactat Bisoprolol 5 MG Cetirizine 10 MGDokument7 SeitenCalcium Lactat Bisoprolol 5 MG Cetirizine 10 MGtitis agustinaNoch keine Bewertungen
- Makalah Singkat FarmasiDokument6 SeitenMakalah Singkat FarmasiArul DarmansyahNoch keine Bewertungen
- Sinarest AF SyrupDokument5 SeitenSinarest AF SyrupImshan TalibNoch keine Bewertungen
- St. Paul College of Ilocos SurDokument3 SeitenSt. Paul College of Ilocos SurMarie Kelsey Acena MacaraigNoch keine Bewertungen
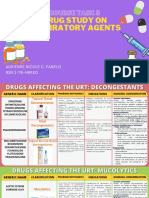
- Course Task 8 Drug Study On Respiratory AgentsDokument23 SeitenCourse Task 8 Drug Study On Respiratory AgentsAdrienne Nicole PaneloNoch keine Bewertungen
- Vasquez, Julianne Gabrielle G. Pharmacology BSN 2-A-7 Course Task #1Dokument6 SeitenVasquez, Julianne Gabrielle G. Pharmacology BSN 2-A-7 Course Task #1PagodNoch keine Bewertungen
- TDM Basic PrinciplesDokument10 SeitenTDM Basic PrinciplesabinchandrakumarNoch keine Bewertungen
- Package Insert - BOOSTRIXDokument40 SeitenPackage Insert - BOOSTRIXmiguelNoch keine Bewertungen
- Pulmicort Respules (Budesonide Inhalation Suspension) Vs Singulair, Children - Full Text View - ClinicalTrials - GovDokument5 SeitenPulmicort Respules (Budesonide Inhalation Suspension) Vs Singulair, Children - Full Text View - ClinicalTrials - GovHanna PurwaningsihNoch keine Bewertungen
- HTN Protocol 6.05Dokument2 SeitenHTN Protocol 6.05Sergiu CiurdariuNoch keine Bewertungen
- Brief Review On Clinical TrialsDokument23 SeitenBrief Review On Clinical TrialssallurajNoch keine Bewertungen
- Anti Biotics: Acive Princble Indication Family NameDokument61 SeitenAnti Biotics: Acive Princble Indication Family NameAhmed FekryNoch keine Bewertungen
- Anaesthetic and Muscle Relaxant Agents: DR David N.MusyokaDokument43 SeitenAnaesthetic and Muscle Relaxant Agents: DR David N.MusyokaIrene Zae MwandotoNoch keine Bewertungen
- Running Head: 1: PolypharmacyDokument3 SeitenRunning Head: 1: PolypharmacyjosephNoch keine Bewertungen
- Sublingual Tablet Tapentadol HCL 2Dokument80 SeitenSublingual Tablet Tapentadol HCL 2Maharshi PandyaNoch keine Bewertungen
- Kelompok 1Dokument14 SeitenKelompok 1Aurent WidjanarkoNoch keine Bewertungen
- RH Sayana Press FaqsDokument7 SeitenRH Sayana Press Faqsolga_bravo_19Noch keine Bewertungen
- How To Do Drug CalculationsDokument7 SeitenHow To Do Drug Calculationsjk centralNoch keine Bewertungen
- Use of Atypical Antipsychotics in The Elderly: A Clinical ReviewDokument11 SeitenUse of Atypical Antipsychotics in The Elderly: A Clinical ReviewGianNoch keine Bewertungen
- Pharmacovigilance - Sem VIIIDokument4 SeitenPharmacovigilance - Sem VIIIkuttiappan anithaNoch keine Bewertungen
- The National Pharmacy Week 2015 Quiz Bee QsDokument7 SeitenThe National Pharmacy Week 2015 Quiz Bee QsPamella JadeNoch keine Bewertungen
- ANALSIKDokument4 SeitenANALSIKDianpratiwi22Noch keine Bewertungen
- FANTANYLDokument3 SeitenFANTANYLTanuj VermaNoch keine Bewertungen
- TramadolDokument7 SeitenTramadolFlauros Ryu JabienNoch keine Bewertungen
- KAPS Ques - July 2022Dokument2 SeitenKAPS Ques - July 2022majid tariq100% (1)
- PKPADokument22 SeitenPKPAYola SafitriNoch keine Bewertungen
- Somali Essential Medicines List 2019Dokument36 SeitenSomali Essential Medicines List 2019Usama MohaNoch keine Bewertungen
- Stock Conversion 02142022Dokument427 SeitenStock Conversion 02142022tiaraNoch keine Bewertungen
- Epilepsy and PregnancyDokument57 SeitenEpilepsy and Pregnancyninjahattori1Noch keine Bewertungen
- Dr. Reddy's API Product List PDFDokument9 SeitenDr. Reddy's API Product List PDFROUNAK PALNoch keine Bewertungen