Beruflich Dokumente
Kultur Dokumente
OSUMC Nausea Guideline
Hochgeladen von
umam fazlurrahmanCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
OSUMC Nausea Guideline
Hochgeladen von
umam fazlurrahmanCopyright:
Verfügbare Formate
Pathophysiology and Management of Nausea and Vomiting
Mechanisms of Nausea and Vomiting
There is a differential diagnosis to nausea which can be used to choose the most effective initial management.
Nausea and vomiting involves the stimulation of the VC in the medulla by one or more of the following pathways and is
mediated by varying neurotransmitters:
Peripheral Pathways
o Nausea triggered by mechanoreceptors and chemoreceptors in the GI tract, serosa, and viscera;
transmitted via the vagus and splanchnic nerves, sympathetic ganglia, and glossopharyngeal nerves to
the Chemoreceptor Trigger Zone (CTZ) and VC.
Vestibular System
o Nausea triggered by motion; transmitted via the vestibulocochlear nerve to the VC.
Chemoreceptor Trigger Zone (CTZ)
o Nausea triggered by toxins in both the blood stream and CSF.
Cortex
o Nausea triggered by sensory input, anxiety, meningeal irritation, and increased intracranial pressure.
The Vomiting Center (VC) is the final common pathway for vomiting. This center initiates coordinated responses from the
parasympathetic system and motor efferents to produce vomiting.
Benzodiazepines
Anticholinergics, Antihistamines
Corticosteroids
Phenothiazines, Butyrophenones, 5HT3
antagonists
Corticosteroids, Prokinetics Pharmacologic
intervention
PPIs, Phenothiazines
The Rational Approach to Nausea and Vomiting:
1. Identify all of the potential underlying causes/triggers
2. If possible, eliminate causes/triggers (medications, constipation, etc)
3. Identify the pathway and associated neurotransmitters (see Table 1 and Figure 1)
4. Choose the medications that best target the neurotransmitters involved (See Table 1 and Table 2)
5. Schedule medication ATC and titrate to effect
6. If symptoms are refractory despite adequate dosing, combine several therapies to block multiple pathways.
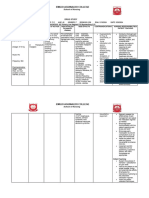
Table 1: Differential Diagnosis of Nausea and Vomiting
Differential Examples of Most Common Neural Pathway Receptors
Notable History/ Physical Exam Targeted Pharmacotherapy
Diagnosis Clinical Scenarios Involved to Block
Central Nervous System Origin
Motion sickness; Acoustic neuroma;
Vestibular Nausea worse with movement, Dizziness Vestibular Nucleus AChM, H1 Anticholinergics, antihistamines
Nystagmus; Vertigo
Toxins
Stimulation of CTZ (via 5HT3 &
NK1) See Chemo Guideline (hyperlink
5HT3, NK-
Chemotherapy Recent emetogenic chemotherapy Serotonin released in gut, this)
1, D2
stimulating peripheral pathways
Anxiety
Recent medication changes (additions or If possible, stop offending
Medications (antibiotics, opioids, digoxin, Direct effect on the CTZ via D2
deletions) D2 medication;Prokinetics;
SSRIs, TCAs) (central)
Butyrophenones; Phenothiazines
Metabolic abnormalities (uremia, liver
Treat underlying abnormalities;
failure, infection, ketoacidosis, electrolyte Direct effect on the CTZ via D2
Altered mental status D2 Butyrophenones; Phenothiazines;
abnormalities [hyper/hypocalcemia, (central)
Prokinetics
hyper/hyponatremia, hypokalemia])
Brainstem or cerebellar lesions;
a.m. symptoms, headache, neck stiffness, H1 and Corticosteroids; Antihistamines;
Intracranial Increased intracranial pressure via Cortex
papilledema, neurologic signs AChM Butyrophenones; Phenothiazines
inflammation/edema
Treat underlying anxiety
Nausea without vomiting or weight loss;
(benzodiazepines prn); Consider
Anticipatory nausea and vomiting; History of severe nausea post
Anxiety Cortex SSRIs for patients with chronic
Nausea as a manifestation of anxiety chemotherapy, mood/anxiety disorder,
anxiety (may contribute to
significant history of nausea in youth.
medication induced nausea)
Gastrointestinal Origin
Mechanical Stretch
Large/infrequent vomitus that relieves
nausea; Treat underlying constipation;
Constipation, Malignant Bowel
Crampy abdominal pain; Corticosteroids (for obstruction
Obstruction, Peritoneal carcinomatosis, Peripheral pathways: stimulation of D2,
Decreased frequency of BMs, abdominal and hepatic capsular distension);
Biliary obstruction, Hepatic capsular mechanoreceptors AchM/H1
fullness and distension, hard stools, Butyrophenones; Phenothiazines;
distension
straining with defecation, abnormal BS, Anticholinergics (for cramping)
fecal impaction.
Small-volume emesis, early satiety,
bloating, nausea with movement; h/o Peripheral pathways:
Gastroparesis D2 Prokinetics
neuropathy, hypothyroidism, or diabetes Mechanoreceptors
mellitus; peritoneal carcinomatosis
H2 blockers or PPI (GERD/ PUD)
Induced by GERD, PUD, Radiation, Esophageal burning, sour taste in mouth, Peripheral Pathways: 5HT3 antagonists (Chemo)
GI Mucosal AChM, H1,
Infection, Inflammation, Chemotherapy, worse when supine; epigastric pain Chemoreceptors via Serotonin Corticosteroids (Inflammation)
Irritation D2, 5HT3
Medications radiating to back, fever, diarrhea released in gut Anticholinergics (for cramping)
Treat underlying infection
Oropharyngeal cancer, Thick adherent Peripheral pathways via
Thrush, herpetic lesions; mucositis, Mouthcare (chlorhexidine
Glossopharyngeal mucus, Inflammation (gingivitis, dental stimulation of mechano and
gingivitis; h/o radiation; dysphagia, mouthwash),
Irritation caries), Infection (oropharyngeal chemoreceptors of the
odynophagia Treat the underlying infection
candidiasis, HSV), Radiation glossopharyngeal nerve
Table 2: Antiemetics
Receptor Affinities
Antiemetic Trade Name Neural Pathway Targeted Dosage Major Adverse Effects
D2 H1 AchM 5HT3
Prokinetics
Peripheral (Decreased Akathisia, EPS, colic in GI obstruction (Risk of
++ + (at high 5-20 mg PO/SC/IV before
Metoclopramide Reglan mechanoreceptor stimulation) ++ perforation in patients with complete GI
(agonist) doses) meals and at bedtime
CTZ obstruction)
Butyrophenones
0.5-2 mg PO/SC/IV/PR
Haloperidol Haldol CTZ +++ Akathisia, EPS, QT prolongation with high doses
q8h and q4h prn
Phenothiazines
CTZ 5-10 mg PO/IV q6h or 25
Prochlorperazine Compazine ++ + Akathisia, EPS, sedation (less than promethazine)
Vestibular mg PR q6h
CTZ 12.5-25 mg PO/IV q6h or Akathisia, EPS (less than haloperidol and
Promethazine Phenergan + + ++
Vestibular 25 mg PR q6h prochlorperazine), sedation
Anticholinergics
1.5 mg transdermal patch Sedation, dry mouth, urinary retention,
Scopolamine Transderm Scop Vestibular ++
every 3 days constipation, delirium
0.125 – 0.25 mg SL/PO Sedation, dry mouth, urinary retention,
Hyoscyamine Levsin Vestibular ++
q4h constipation, delirium
IV/SC: 0.1-0.2 mg q6h Sedation, dry mouth, urinary retention,
Glycopyrrolate Robinul Vestibular ++
PO: 1-2 mg q6h constipation
Antihistamines
25-100 mg/day in divided
Meclizine Antivert Vestibular ++ Sedation, dry mouth, urinary retention
doses TID
Diphenhydramine Benadryl Vestibular ++ + 25-50 mg PO/IV/SC q6h Sedation, dry mouth, urinary retention, delirium
5HT3 antagonists
1 CTZ
Ondansetron Zofran ++ 4-8 mg PO/IV q4-8h Headache, constipation
Peripheral pathways
2
Others
CTZ
Sedation, orthostatic hypotension, weight gain,
Olanzapine Zyprexa Peripheral Pathways ++ ++ ++ + 2.5-10 mg PO daily
hyperglycemia
Vestibular
Cortex Agitation, nausea, hyperglycemia,
Dexamethasone 2-32 mg PO/IV per day in
Corticosteroids Peripheral Pathways immunosuppression; Long term side effects with
(Decadron®) divided doses
(Inflammation) chronic use.
0.25-1 mg PO/SC/IV/PR
Lorazepam (Ativan®)
q4h prn anxiety
Benzodiazepines Cortex Sedation, delirium, agitation
2-10 mg PO/SC/IV/PR q4h
Diazepam (Valium®)
prn anxiety
Histamine2 Famotidine
Peripheral pathways +/0 20 mg PO/IV daily to BID Delirium (adjust dose for renal dysfunction)
Antagonists (Pepcid®)
Proton Pump Esomeprazole 20-40 mg PO/IV daily to
Peripheral pathways
Inhibitors (Nexium®) BID
1
Ondansetron is given as an example of a 5HT3 antagonist. 5HT3 antagonists are most effective for chemotherapy-induced nausea and vomiting. Other agents are available. See the Guidelines
for the Management of Chemotherapy induced Nausea and Vomiting for more specific information. (hyperlink this)
2
Select OSUMC formulary agents are included as examples. Other agents exist in each class of medications.
References:
1) Wood G. Management of intractable nausea and vomiting in patients at the end of life. JAMA 2007;298:1196-1207.
2) Weissman, D. Fast Fact and Concepts #05: Treatment of Nausea and Vomiting. June, 2000. End-of-Life Physician Education Resource Center www.eperc.mcw.edu
3) Jackson WC, Tavernier L. Olanzapine for intractable nausea in palliative care patients. J Pall Med 2003;6:251-5.
Author(s): Hartman, Gustin; Department: Pharmacy, Internal Medicine; Date Originated: May 2009; Committee(s) Approved:
This information has been developed by the authors and department listed above at The Ohio State University Medical Center and is intended for use only within the institution. The information is not meant to be applied rigidly and followed in all cases. Professional
judgment must remain central to the application of this information. All rights reserved, including right of reproduction, in whole or in part, in any form without permission from The Ohio State University Medical Center. Copyright: © 2009 The Ohio State University Medical
Center.
Das könnte Ihnen auch gefallen
- Surgery Shelf Notes 2021 PDFDokument43 SeitenSurgery Shelf Notes 2021 PDFBhandari SadikshyaNoch keine Bewertungen
- Pharmacology Quick Reference for Health Care ProvidersVon EverandPharmacology Quick Reference for Health Care ProvidersNoch keine Bewertungen
- Platelet Counting Fordirect Indirect MethodDokument30 SeitenPlatelet Counting Fordirect Indirect MethodShana Flame Haze100% (2)
- Nursing Health Assessment MnemonicsDokument20 SeitenNursing Health Assessment Mnemonicsmildred alidonNoch keine Bewertungen
- Drug Study FormatDokument2 SeitenDrug Study FormatEmilie CajaNoch keine Bewertungen
- NCP-Ineffective AirwayDokument5 SeitenNCP-Ineffective Airwayjava_biscocho1229Noch keine Bewertungen
- Spinal Cord Injury NCPDokument2 SeitenSpinal Cord Injury NCPEmmanuelRodriguez100% (1)
- Pharma Mod 11Dokument12 SeitenPharma Mod 11ANGELA SHANE AGUSTINNoch keine Bewertungen
- Prof BSP - Neurologic Paraneoplastic SyndromesDokument122 SeitenProf BSP - Neurologic Paraneoplastic SyndromesSavitha BasriNoch keine Bewertungen
- Anti EmeticsDokument29 SeitenAnti EmeticsBezawit TsigeNoch keine Bewertungen
- Drug Study - DigoxinDokument2 SeitenDrug Study - DigoxinKian Herrera50% (2)
- M.SC Yoga SyllabusDokument29 SeitenM.SC Yoga SyllabusSenthil KumarNoch keine Bewertungen
- A Development of Freudian Metapsychology For Schisophrenia Artaloytia2014Dokument26 SeitenA Development of Freudian Metapsychology For Schisophrenia Artaloytia2014Fredy TolentoNoch keine Bewertungen
- Drug AnalysisDokument49 SeitenDrug Analysisjomalaw6714Noch keine Bewertungen
- Jin Gui Yao Lue (Acupuncture)Dokument2 SeitenJin Gui Yao Lue (Acupuncture)Tim SchlankNoch keine Bewertungen
- Drug Study AsDokument3 SeitenDrug Study Askev mondaNoch keine Bewertungen
- Pharmacologic ClassDokument4 SeitenPharmacologic ClassBianca Nicole Gacad FernandezNoch keine Bewertungen
- AntiemeticsDokument25 SeitenAntiemeticsPridho GaziansyahNoch keine Bewertungen
- ANTIEMETIKDokument23 SeitenANTIEMETIKshabrinaNoch keine Bewertungen
- Clincal Practice Guidelines For ECT IJP-23Dokument26 SeitenClincal Practice Guidelines For ECT IJP-23JagadishaThirthalliNoch keine Bewertungen
- 1-Antiemetic DrugsDokument13 Seiten1-Antiemetic Drugsbwalyakangwa582Noch keine Bewertungen
- Psychiatric DrugDokument10 SeitenPsychiatric DrugKollebeng Pangda PasiwatNoch keine Bewertungen
- ER Drug StudyDokument4 SeitenER Drug StudyNecy Tessa C. AcostaNoch keine Bewertungen
- Bonilla Drug Study 2 20Dokument9 SeitenBonilla Drug Study 2 20YLA KATRINA BONILLANoch keine Bewertungen
- DepakoteDokument2 SeitenDepakotedana100% (1)
- Angiotensin-Converting Enzyme Inhibitors, Beta-Adrenergic Blockers: DecreasedDokument3 SeitenAngiotensin-Converting Enzyme Inhibitors, Beta-Adrenergic Blockers: DecreasedBianca Nicole Gacad FernandezNoch keine Bewertungen
- Anest Implication of PsikoaktifDokument5 SeitenAnest Implication of PsikoaktifjilieNoch keine Bewertungen
- Drug StudyDokument27 SeitenDrug StudyMariefer EsplagoNoch keine Bewertungen
- Antiemetic Drugs: PHR Sangita ShakyaDokument26 SeitenAntiemetic Drugs: PHR Sangita ShakyaCurex QANoch keine Bewertungen
- Anti-Emetic DrugsDokument10 SeitenAnti-Emetic DrugsLydia Alexandra LatumahinaNoch keine Bewertungen
- DRUGDokument6 SeitenDRUGjhoyorlyn22Noch keine Bewertungen
- Antiemitics & AntacidDokument22 SeitenAntiemitics & AntacidMohammad HayajnehNoch keine Bewertungen
- AntiemeticsDokument33 SeitenAntiemeticsSaiNoch keine Bewertungen
- Risperidone: Generic Name: ClassificationsDokument9 SeitenRisperidone: Generic Name: ClassificationsColeen Mae CamaristaNoch keine Bewertungen
- Guidelines For The Acute Assessment and Management of Amphetamine-Type Stimulant Intoxication and ToxicityDokument4 SeitenGuidelines For The Acute Assessment and Management of Amphetamine-Type Stimulant Intoxication and ToxicityTanani 102014007Noch keine Bewertungen
- Drug Induced VomitingDokument5 SeitenDrug Induced VomitingnimasNoch keine Bewertungen
- Standards of Laboratory Practice: Antiepileptic Drug MonitoringDokument11 SeitenStandards of Laboratory Practice: Antiepileptic Drug MonitoringDiegoAndrésYiZapataNoch keine Bewertungen
- Drug StudyDokument49 SeitenDrug StudyLexa Moreene Cu�adoNoch keine Bewertungen
- Psychotropic Substance Hallucinogens and Dissociatives - CompressedDokument39 SeitenPsychotropic Substance Hallucinogens and Dissociatives - CompressedshuyuichewNoch keine Bewertungen
- Drug Name Classification Mechanism of Action Indications Contra Indications Side Effects Nursing ResponsibilitiesDokument5 SeitenDrug Name Classification Mechanism of Action Indications Contra Indications Side Effects Nursing ResponsibilitiesJessica FabroaNoch keine Bewertungen
- Drugs For Gastrointestinal Disorders 2023Dokument23 SeitenDrugs For Gastrointestinal Disorders 2023aguilarjanicaNoch keine Bewertungen
- Antimicrobial Regimen Selection (Quick AnswersL Pharmacy Book)Dokument16 SeitenAntimicrobial Regimen Selection (Quick AnswersL Pharmacy Book)Yasmin ElsobkyNoch keine Bewertungen
- Neuropathic Pain: Emerging TreatmentsDokument11 SeitenNeuropathic Pain: Emerging TreatmentsFarhatNoch keine Bewertungen
- Antipsychotic Drugs - Pharmacology - An Illustrated ReviewDokument5 SeitenAntipsychotic Drugs - Pharmacology - An Illustrated ReviewDragutin PetrićNoch keine Bewertungen
- Finals Activity 1 - Drug StudyDokument5 SeitenFinals Activity 1 - Drug StudyElly LazaroNoch keine Bewertungen
- Adrenergic Drugs: Pharmacological Department Medical School - UNPAD Ike HusenDokument33 SeitenAdrenergic Drugs: Pharmacological Department Medical School - UNPAD Ike HusenHendra EfendiNoch keine Bewertungen
- The Serotonin Syndrome: D. BijlDokument6 SeitenThe Serotonin Syndrome: D. BijlBianca CaterinalisendraNoch keine Bewertungen
- Emergency Presentations of MDDokument10 SeitenEmergency Presentations of MDGustavo PestanaNoch keine Bewertungen
- AkathisiaDokument4 SeitenAkathisiaRindayu Julianti NurmanNoch keine Bewertungen
- Pharmacology Module For FinalsDokument11 SeitenPharmacology Module For FinalsCarlo GaradoNoch keine Bewertungen
- Phle Module 4Dokument135 SeitenPhle Module 4Margaret RNoch keine Bewertungen
- YAWAADokument10 SeitenYAWAAZyrene CapulongNoch keine Bewertungen
- Acute Pain Management: Bruce Ferrell, MD Brandon Koretz, MDDokument5 SeitenAcute Pain Management: Bruce Ferrell, MD Brandon Koretz, MDJayagopi KadarasenNoch keine Bewertungen
- Citicoline Drug StudyDokument2 SeitenCiticoline Drug StudyJC LumayaNoch keine Bewertungen
- Anti Emetics, Prokinetic and Digestive DrugsDokument46 SeitenAnti Emetics, Prokinetic and Digestive DrugsCynthia KeruboNoch keine Bewertungen
- Polytechnic College of Davao Del Sur, Inc.: Drug StudyDokument2 SeitenPolytechnic College of Davao Del Sur, Inc.: Drug StudyDayanaj OngNoch keine Bewertungen
- Cerenia InjectableDokument2 SeitenCerenia InjectableRue BensonNoch keine Bewertungen
- UntitledDokument2 SeitenUntitledPRINCESS KOBAYASHINoch keine Bewertungen
- Apt Aka 2015Dokument3 SeitenApt Aka 2015dzakiyah nurul israNoch keine Bewertungen
- Any Up-Dates Are To Be Completed in Different Color Ink. The Student Is Expected To Document All Meds The Client Is Currently ReceivingDokument1 SeiteAny Up-Dates Are To Be Completed in Different Color Ink. The Student Is Expected To Document All Meds The Client Is Currently Receivinggeorgeloto12Noch keine Bewertungen
- Drug-Induced Movement Disorders: TremorDokument6 SeitenDrug-Induced Movement Disorders: TremordentsavvyNoch keine Bewertungen
- Antidepressants, Antihistamines, General Anesthetics, MAO Inhibitors, OpioidsDokument3 SeitenAntidepressants, Antihistamines, General Anesthetics, MAO Inhibitors, Opioidskaycelyn jimenezNoch keine Bewertungen
- Antiemetic Drugs PDFDokument12 SeitenAntiemetic Drugs PDFDanisha Laila100% (2)
- PH - Karrar HaderDokument33 SeitenPH - Karrar HaderAdnan YassinNoch keine Bewertungen
- Adrenergic Agents: University of Negros Occidental-RecoletosDokument66 SeitenAdrenergic Agents: University of Negros Occidental-Recoletosmary grace trinidadNoch keine Bewertungen
- DrugsDokument8 SeitenDrugsJasmine J. FloresNoch keine Bewertungen
- DrUG STUDY PSYCHEDokument52 SeitenDrUG STUDY PSYCHELiza MPNoch keine Bewertungen
- NAUSEA AND VOMITING - ObatDokument8 SeitenNAUSEA AND VOMITING - ObatSri Ayu NingsihNoch keine Bewertungen
- Mental Health Proposal RevisedDokument7 SeitenMental Health Proposal Revisedapi-316749800Noch keine Bewertungen
- Exam Study Guide and Worksheet - Respiratory SystemDokument4 SeitenExam Study Guide and Worksheet - Respiratory SystemHailey PedenNoch keine Bewertungen
- Paediatric Consumer Health in IndiaDokument8 SeitenPaediatric Consumer Health in IndiaAkash GuruNoch keine Bewertungen
- IAEA Safety Standards: SSG-46Dokument340 SeitenIAEA Safety Standards: SSG-46Asiah HasanahNoch keine Bewertungen
- Electrotherapy: DR Ramaiah Choudhary PhysiotherapistDokument13 SeitenElectrotherapy: DR Ramaiah Choudhary Physiotherapistvenkata ramakrishnaiahNoch keine Bewertungen
- CompendiumDokument3 SeitenCompendiumKhuong LamNoch keine Bewertungen
- Sinusoidal CurrentDokument16 SeitenSinusoidal CurrentHareem Fatima100% (1)
- Clough K Oncoplasty BJSDokument7 SeitenClough K Oncoplasty BJSkomlanihou_890233161Noch keine Bewertungen
- Presented By: Christopher H. Wise, PT, DPT, MS, OCS, FAAOMPT, MTC, ATCDokument1 SeitePresented By: Christopher H. Wise, PT, DPT, MS, OCS, FAAOMPT, MTC, ATCemilNoch keine Bewertungen
- Risk Factors For Postoperative Nausea and VomitingDokument21 SeitenRisk Factors For Postoperative Nausea and VomitingmusafirlautNoch keine Bewertungen
- Conquering Interview AnxietyDokument4 SeitenConquering Interview AnxietySai Pavan KumarNoch keine Bewertungen
- Objectives: Therapeutic DietDokument17 SeitenObjectives: Therapeutic DietKBDNoch keine Bewertungen
- Stages of ReadingDokument12 SeitenStages of ReadingRolando Vilches GonzalezNoch keine Bewertungen
- Microfracture and Microfracture PlusDokument7 SeitenMicrofracture and Microfracture PlusdrjorgewtorresNoch keine Bewertungen
- Diabetic Retinopathy in PregnancyDokument109 SeitenDiabetic Retinopathy in PregnancyrayshahNoch keine Bewertungen
- Case ReportDokument50 SeitenCase ReportTajul AnshorNoch keine Bewertungen
- Mitral Valve ProlapseDokument4 SeitenMitral Valve Prolapseapi-306423962Noch keine Bewertungen
- Hypertensive Disorders of Pregnancy Teaching PlanDokument5 SeitenHypertensive Disorders of Pregnancy Teaching PlanMary Grace Belmonte100% (1)
- Draeger Evita V800 GE R860Dokument2 SeitenDraeger Evita V800 GE R860Billy IrawanNoch keine Bewertungen
- Program and Proceedings - 4th Caribbean Biomedical Research Days CBRD-2017, Jan 16-18, 2017, Rodney Bay, St. LuciaDokument18 SeitenProgram and Proceedings - 4th Caribbean Biomedical Research Days CBRD-2017, Jan 16-18, 2017, Rodney Bay, St. LuciaISBS_SocietyNoch keine Bewertungen
- Table AlkesDokument14 SeitenTable Alkesintan purnama sariNoch keine Bewertungen
- GBV Monthly Work PlanDokument20 SeitenGBV Monthly Work Planrachaelnamz19Noch keine Bewertungen