Beruflich Dokumente
Kultur Dokumente
Diabetic Foot Ulcers: Local Management of
Hochgeladen von
RohmatullahOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diabetic Foot Ulcers: Local Management of
Hochgeladen von
RohmatullahCopyright:
Verfügbare Formate
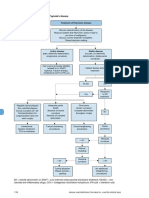
Principles of local management of DFUs1
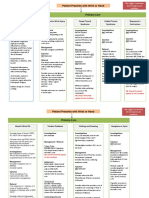
Indications for referral of a patient with diabetes to a specialist
foot service2,3
Priority Indications Timing of Suggested
QUICK GUIDE
Local management of
Standard local DFU management consultation or frequency of
n Debridement referral follow-up*
n Cleansing Urgent n Open wound +/- signs of Immediate As determined
diabetic foot ulcers
n Management of exudate levels (active infection consultation by specialist
n Treatment of infection pathology) n New neuropathic pain or
n Offloading/protection pain at rest
n Active Charcot deformity
(red, hot swollen midfoot or
Monitor regularly, e.g. weekly ankle)
n Is the wound making positive progress?* n Vascular compromise
(sudden absence of DP/PT
Yes pulses or gangrene)
No
High n Previous history of DFU or Immediate or Every 12 months Management of
Reassess patient and wound Continue standard (ADA risk lower extremity amputation ‘next available’
treatment diabetic foot ulcers
No category 3) n Chronic venous insufficiency outpatient
n At 4 weeks, has the consultation is complex, and
wound area reduced
by≥50%? Moderate n PAD +/- LOPS Referral within Every 2–3
requires a
Refer/amend management Yes (ADA risk n DP/PT pulse diminished 1–3 months months multi-disciplinary
as appropriate to correct category 2) or absent team approach to
problems Consider treatment n Lower limb swelling or
and reassess oedema avoid serious
n Second-line (advanced) therapies
may be indicated if wound area
regularly Low n LOPS +/- longstanding Referral within 1 Every 4–6 and expensive
reduction at 4 weeks is <50% (ADA risk non-changing foot deformity month months complications, such as
despite optimised management category 1) n Patient requires specialist
footwear infection and amputation1
of blood glucose and ischaemia, Once DFU healed
concordance with offloading/ (diabetic foot in remission) Very low n No LOPS or PAD Referral within As a minimum,
protection and exclusion of n Ongoing surveillance in remission (ADA risk n Education about foot 1–3 months annually
infection n Protective footwear category 0) care, exercise, footwear,
preventing injury, etc.
*All patients with diabetes should be seen by a foot specialist at least once per year.
*Triggers for reassessment include increasing wound size, new pain or discomfort, ADA: American Diabetic Association; DP: dorsalis pedis; LOPS: loss of protective sensation; PAD:
signs of infection peripheral arterial disease; PT: posterior tibial
© Wounds International 2017 All rights reserved. Unless otherwise designated,
References 3. Miller JD et al. J Fam Pract 2014; 63(11): 646–56 all trademarks are proprietary to KCI Licensing,
1. WUWHS. Florence Congress, Position Document. Local 4. Chadwick P, Armstrong DG. Local management of diabetic Inc., its affiliates and/or licensors.
management of diabetic foot ulcers. Wounds International, 2016 foot Made Easy. Wounds International, 2017 Supported by Acelity
PRA001748-R0-OUS, EN (12/17)
2. Boulton AJM et al. Diabetes Care 2008; 31(8): 1679-85 5. Téot L et al. Int Wound J 2017; 14(5) 842-8 www.acelity.com
LOCAL MANAGEMENT OF DFUs1,4
Dry, black Sloughy Granulating
TIELLETM Packing Hydropolymer Foam Dressing with LIQUALOCKTM Technology; † SILVERCEL™ NON-ADHERENT hydro alginate antimicrobial dressing with EASYLIFT™
*World Union of Wound Healing Societies (WUWHS), Florence Congress, Position Document. Local management of diabetic foot ulcers. Wounds International, 2016
Mostly or completely
(due to ischaemia) Yellow, brown, grey or black Clean, red
epithelialised
Cleanse: according to local protocol. V.A.C. VERAFLO CLEANSE CHOICE™ Dressing provides a wound cleansing Red, pink
option for clinicians when surgical debridement must be delayed or is not possible or appropriate5
Debridement (as appropriate), e.g. for removal of callus and devitalised tissue
To separate toes without Dry to low exudate Moderate to high exudate Dry to low Moderate to high exudate Protect new tissue
retaining moisture or n TIELLETM Lite n BIOSORBTM Gellling Fibre Dressing exudate n BIOSORBTM Gelling Fibre Dressing growth to allow wound
Technology; SILVERCEL™ hydro alginate antimicrobial dressing
hydrating tissues: Hydropolymer Adhesive n TIELLETM Plus Hydropolymer Adhesive n ADAPTIC TOUCHTM n TIELLETM Plus Dressing maturation and prevent
ADAPTIC TOUCHTM Foam Dressing Foam Dressing with LIQUALOCKTM Dressing n TIELLETM Non Adhesive Hydropolymer from drying out
Non-Adhering Silicone with LIQUALOCKTM Technology Dressing with LIQUALOCKTM Technology n ADAPTIC TOUCHTM Dressing
Dressing Technology n TIELLETM Non Adhesive Dressing n Use low adherent contact layer with dressings n Emollient
n TIELLETM Non Adhesive n Use low adherent dressings below if above if appropriate: ADAPTIC TOUCHTM Dressing n Reassess regularly
Dressing appropriate: ADAPTIC TOUCHTM Dressing n Consider skin barrier
n Ensure ongoing surveillance
n NU-GEL™ Hydrogel with n Consider skin barrier
n Provide protective footwear
Primary dressing
Alginate n V.A.C. VERAFLO CLEANSE CHOICE™ Dressing
n NU-DERM™ Thin Hydrocolloid
Deep wounds: BIOSORBTM Dressing or TIELLETM Packing Dressing**; NPWT: V.A.C.® Therapy System (V.A.C.ULTA™ Therapy System and ACTIV.A.C.™ Therapy System) Wound Dressing
If there is a risk of infection,
consider an iodine-
Infection: SILVERCELTM Dressings†; V.A.C. VERAFLO™ Therapy in conjunction with good clinical practice such as antibiotic therapy and debridement PLEASE NOTE
impregnated dressing, e.g.
This algorithm is based on
INADINETM (PVP-I) Non
Odour: consider a dressing containing activated charcoal, e.g. ACTISORB™ Silver 220 Activated Charcoal Dressing with Silver the WUWHS DFU Position
Adherent Dressing Document* and is a guide only.
Fragile periwound skin: TIELLE ESSENTIALTM Silicone Foam Dressings or TIELLETM Non Adhesive Dressing The choice of dressings and
devices must be based on local
protocols and clinical judgement
**
Reassess the wound, periwound skin and suitability of the dressing for the patient and the wound at each review.
If area reduction is <50% at 4 weeks consider: PROMOGRANTM Protease Modulating Matrix or PROMOGRAN PRISMATM Wound Balancing Matrix
Protect/offload: Ensure dressing is compatible with mode of offloading and can be accommodated without bulk or creasing
Das könnte Ihnen auch gefallen
- SBARDokument1 SeiteSBARCindy Deeann StarkeyNoch keine Bewertungen
- Nursing Care Plan - Posterior Hip Dislocation LeftDokument1 SeiteNursing Care Plan - Posterior Hip Dislocation LeftJasmin Jacob100% (7)
- Sas 3Dokument3 SeitenSas 3Dummy AccountNoch keine Bewertungen
- Evidence Based Oral MedicineDokument13 SeitenEvidence Based Oral MedicineShantanu DixitNoch keine Bewertungen
- NICE 2023Dokument3 SeitenNICE 2023hatem newishyNoch keine Bewertungen
- Venous Thromboembolism: Diagnosis and Anticoagulation TreatmentDokument3 SeitenVenous Thromboembolism: Diagnosis and Anticoagulation TreatmentArjun KumarNoch keine Bewertungen
- 19.guidelines DVTDokument2 Seiten19.guidelines DVTRed DevilNoch keine Bewertungen
- NifedipineDokument1 SeiteNifedipinelaude.francesNoch keine Bewertungen
- Fever in Children Dr. Red Dr. BantasanDokument2 SeitenFever in Children Dr. Red Dr. Bantasanmaki RemularNoch keine Bewertungen
- Cts Refmgt Pathway v2-6 With Backing SmallerDokument11 SeitenCts Refmgt Pathway v2-6 With Backing Smalleraime_meldaNoch keine Bewertungen
- DVT and PE What To DoDokument3 SeitenDVT and PE What To DoSpj JjNoch keine Bewertungen
- Head Nursing TemplateDokument10 SeitenHead Nursing TemplateBianca MaeNoch keine Bewertungen
- Benztrop, Congentin: Drug StudyDokument4 SeitenBenztrop, Congentin: Drug StudyHamimah Bint AliNoch keine Bewertungen
- EAU Guidelines On Sexual and Reproductive Health 2022 - 2022 03 29 084141 - Megw (110 111)Dokument2 SeitenEAU Guidelines On Sexual and Reproductive Health 2022 - 2022 03 29 084141 - Megw (110 111)CRISTH KIMBERLY ENEQUE DE LA CRUZNoch keine Bewertungen
- Hand and Wrist PathwayDokument2 SeitenHand and Wrist PathwaydrsadafrafiNoch keine Bewertungen
- Drug StudyDokument3 SeitenDrug StudyRamiel ChristopherNoch keine Bewertungen
- CP-07 Workflow For Daycare Ambulatory CareDokument1 SeiteCP-07 Workflow For Daycare Ambulatory CareNatasha BhasinNoch keine Bewertungen
- SOP Alur Kegawat Daruratan No Dokumen PKM Rwl. Ugd - 52 No Revisi 00 Halaman 1/2Dokument3 SeitenSOP Alur Kegawat Daruratan No Dokumen PKM Rwl. Ugd - 52 No Revisi 00 Halaman 1/2Maryo FeliksNoch keine Bewertungen
- Elimination Diarrhea ManagementDokument7 SeitenElimination Diarrhea ManagementKristiene Kyle AquinoNoch keine Bewertungen
- Drug Dose Route Indication Contraindication Action Sideeffects NursingDokument3 SeitenDrug Dose Route Indication Contraindication Action Sideeffects NursingAnaliza Vios YaoNoch keine Bewertungen
- Nursing Interventions to Manage Postpartum Pain and Prevent ComplicationsDokument6 SeitenNursing Interventions to Manage Postpartum Pain and Prevent ComplicationsAna LuisaNoch keine Bewertungen
- CSBP Post Stroke Checklist ENDokument2 SeitenCSBP Post Stroke Checklist ENEduardo BessoloNoch keine Bewertungen
- LOSARTAN (ARBs) Drug Study (GERIATRICS)Dokument5 SeitenLOSARTAN (ARBs) Drug Study (GERIATRICS)CHRISTIE MONTANONoch keine Bewertungen
- NCP Acute PainDokument3 SeitenNCP Acute PainjrilleraNoch keine Bewertungen
- DIABETIC FOOT ULCER TXDokument31 SeitenDIABETIC FOOT ULCER TXRichard BunNoch keine Bewertungen
- Place ICP Monitor + Supportive Care and Avoidance of Secondary Brain InjuryDokument31 SeitenPlace ICP Monitor + Supportive Care and Avoidance of Secondary Brain Injuryvirus coronaNoch keine Bewertungen
- Hemophilia MX SOPDokument1 SeiteHemophilia MX SOPdhvanishah0313Noch keine Bewertungen
- Philippine Urological Association, Inc.: Executive Committee and Board Members 1997Dokument12 SeitenPhilippine Urological Association, Inc.: Executive Committee and Board Members 1997mits98Noch keine Bewertungen
- Stroke Physician: Discharge ChecklistDokument4 SeitenStroke Physician: Discharge ChecklistEllaNoch keine Bewertungen
- De Manuel NCPDokument2 SeitenDe Manuel NCPSkynet DivineNoch keine Bewertungen
- 03 - CVDS - 0036 Appendix C Wells Score TablesDokument4 Seiten03 - CVDS - 0036 Appendix C Wells Score TablesgabrimarteNoch keine Bewertungen
- Alternative Learning System Related Learning Experience Surgical WardDokument13 SeitenAlternative Learning System Related Learning Experience Surgical WardRoshin TejeroNoch keine Bewertungen
- Drug StudyDokument21 SeitenDrug Studydelpozo100% (3)
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDokument2 SeitenSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanNoch keine Bewertungen
- NCP FractureDokument3 SeitenNCP Fracturesarzlasco09Noch keine Bewertungen
- Nursing Care PlanDokument11 SeitenNursing Care PlanLovely Hope LugatimanNoch keine Bewertungen
- JaneDokument2 SeitenJaneJane DianoNoch keine Bewertungen
- Head Nursing TemplateDokument9 SeitenHead Nursing TemplateBianca MaeNoch keine Bewertungen
- Constipation DiarrhoeaDokument2 SeitenConstipation DiarrhoeaMaría RecioNoch keine Bewertungen
- WTAAbdStabWoundsDokument1 SeiteWTAAbdStabWoundsMariyam AlblooshiNoch keine Bewertungen
- Assessment Diagnosis Planning Implementation Evaluation Interventions Rationale Subjective Data: Na Independent: Goal MetDokument34 SeitenAssessment Diagnosis Planning Implementation Evaluation Interventions Rationale Subjective Data: Na Independent: Goal MetHydie Mae AlcabedosNoch keine Bewertungen
- GENERIC NAME: Clonazepam BRAND NAME: RivotrilDokument2 SeitenGENERIC NAME: Clonazepam BRAND NAME: RivotrildanaNoch keine Bewertungen
- Vicpostoporderform WebDokument2 SeitenVicpostoporderform WebJunaid ShahNoch keine Bewertungen
- DRUG STUDY CIPROFLOXACIN AND ALUMINUM HYDROXIDEDokument7 SeitenDRUG STUDY CIPROFLOXACIN AND ALUMINUM HYDROXIDEDelle KairuzNoch keine Bewertungen
- Clinical Suspicion of DVT: An Approach To Symptoms Suggestive of Lower Limb Deep Vein Thrombosis (DVT)Dokument1 SeiteClinical Suspicion of DVT: An Approach To Symptoms Suggestive of Lower Limb Deep Vein Thrombosis (DVT)Ari Setiyawan NugrahaNoch keine Bewertungen
- XXXDokument13 SeitenXXXtiaraNoch keine Bewertungen
- Mabini Colleges College of Nursing and Midwifery Drug Study on DiclofenacDokument1 SeiteMabini Colleges College of Nursing and Midwifery Drug Study on DiclofenacMa. Sheenadel Zamudio100% (4)
- Asiw The GreatDokument3 SeitenAsiw The GreatLoveline Kate AlcedoNoch keine Bewertungen
- Holy Child School of Davao Nursing Care Plan: E. Jacinto St. Davao CityDokument2 SeitenHoly Child School of Davao Nursing Care Plan: E. Jacinto St. Davao CityMaxileo Villareal AbeciaNoch keine Bewertungen
- KetorolacDokument2 SeitenKetorolacDayanaj OngNoch keine Bewertungen
- nnnnDokument1 Seitennnnnuguitnorelyn30Noch keine Bewertungen
- NCP-Spinal Cord InjuryDokument2 SeitenNCP-Spinal Cord InjuryJohn LineroNoch keine Bewertungen
- NCP, Medication (Cont.), Affective LearningDokument4 SeitenNCP, Medication (Cont.), Affective LearningRosenda GonzalesNoch keine Bewertungen
- 10.1 New Era in DVT Management Single Drug Approach J Nugroho MD FIHADokument32 Seiten10.1 New Era in DVT Management Single Drug Approach J Nugroho MD FIHAEmdan SengadjiNoch keine Bewertungen
- Renal Medicine Brochure - v1.1 Edited SH 2017 Oct 25Dokument2 SeitenRenal Medicine Brochure - v1.1 Edited SH 2017 Oct 25Rye CalderonNoch keine Bewertungen
- Fin DRUG STUDYDokument4 SeitenFin DRUG STUDYKc AcainNoch keine Bewertungen
- Prostate Cancer NCPDokument1 SeiteProstate Cancer NCPKathleen Dimacali0% (1)
- 5 Year Financial PlanDokument29 Seiten5 Year Financial PlanFrankieNoch keine Bewertungen
- King and QueenDokument3 SeitenKing and QueenRohmatullahNoch keine Bewertungen
- Timers Management LukaDokument52 SeitenTimers Management LukaRohmatullahNoch keine Bewertungen
- Assessment of A Patient With A Wound: Core CurriculumDokument4 SeitenAssessment of A Patient With A Wound: Core CurriculumRohmatullahNoch keine Bewertungen
- WRP Australia 2017 Case Study-1newDokument10 SeitenWRP Australia 2017 Case Study-1newRohmatullahNoch keine Bewertungen
- Quality Control of Radiology ServicesDokument12 SeitenQuality Control of Radiology ServicesMariaDoresiaSidabungkeNoch keine Bewertungen
- B Konsep Manajemen KeperawatanDokument3 SeitenB Konsep Manajemen KeperawatanRohmatullahNoch keine Bewertungen
- Acquisition Team Charter TemplateDokument5 SeitenAcquisition Team Charter TemplateRohmatullahNoch keine Bewertungen
- 3011 DalamDokument6 Seiten3011 DalamRohmatullahNoch keine Bewertungen
- Jurnal 15904 PDFDokument8 SeitenJurnal 15904 PDFRohmatullahNoch keine Bewertungen
- Coldplay The ScientistDokument2 SeitenColdplay The ScientistRohmatullahNoch keine Bewertungen
- You Want To Develope A Comprehensive Wound Assesment Tool For Use in Your HospitalDokument1 SeiteYou Want To Develope A Comprehensive Wound Assesment Tool For Use in Your HospitalRohmatullahNoch keine Bewertungen
- From: EdoDokument1 SeiteFrom: EdoRohmatullahNoch keine Bewertungen
- 5 Year Financial PlanDokument29 Seiten5 Year Financial PlanFrankieNoch keine Bewertungen
- Problem SolverDokument2 SeitenProblem SolverRohmatullahNoch keine Bewertungen
- ICD-10 2010 Volume 1 & 3Dokument1.999 SeitenICD-10 2010 Volume 1 & 3aprilNoch keine Bewertungen
- Clinical Protocol For Wound Management 2013Dokument17 SeitenClinical Protocol For Wound Management 2013Moloce BeatriceNoch keine Bewertungen
- Standart P Carol PDFDokument1 SeiteStandart P Carol PDFRohmatullahNoch keine Bewertungen
- Working To Prevent Diabetes-Related Amputations: EditorialDokument1 SeiteWorking To Prevent Diabetes-Related Amputations: EditorialRohmatullahNoch keine Bewertungen
- Working To Prevent Diabetes-Related Amputations: EditorialDokument1 SeiteWorking To Prevent Diabetes-Related Amputations: EditorialRohmatullahNoch keine Bewertungen
- GooglepreviewDokument72 SeitenGooglepreviewRohmatullahNoch keine Bewertungen
- WRP Australia 2017 Case Study-1newDokument10 SeitenWRP Australia 2017 Case Study-1newRohmatullahNoch keine Bewertungen
- Exploring The Impact of Mindfulness-Based Meditation On The Quality of Life, Symptoms of Depression and Anxiety, and Wound Healing For Individuals With DFUDokument1 SeiteExploring The Impact of Mindfulness-Based Meditation On The Quality of Life, Symptoms of Depression and Anxiety, and Wound Healing For Individuals With DFURohmatullahNoch keine Bewertungen
- Fast and Effective Wound Healing: Negative Pressure Wound TherapyDokument12 SeitenFast and Effective Wound Healing: Negative Pressure Wound TherapyRohmatullahNoch keine Bewertungen
- Fast and Effective Wound Healing: Negative Pressure Wound TherapyDokument12 SeitenFast and Effective Wound Healing: Negative Pressure Wound TherapyRohmatullahNoch keine Bewertungen
- Clinical Protocol For Wound Management 2013Dokument17 SeitenClinical Protocol For Wound Management 2013Moloce BeatriceNoch keine Bewertungen
- Nutrition 411: The Diabetic Foot Ulcer - Can Diet Make A Difference?Dokument4 SeitenNutrition 411: The Diabetic Foot Ulcer - Can Diet Make A Difference?RohmatullahNoch keine Bewertungen
- Winners SupplementDokument32 SeitenWinners SupplementRohmatullahNoch keine Bewertungen
- Wound Care Handbook: Patient Teaching GuideDokument26 SeitenWound Care Handbook: Patient Teaching GuideRohmatullahNoch keine Bewertungen
- PICOT AmbulansiDokument2 SeitenPICOT AmbulansiEviliaNoch keine Bewertungen
- Fnsa Final Convention ScheduleDokument4 SeitenFnsa Final Convention ScheduleFNSANoch keine Bewertungen
- Introduction RHDDokument5 SeitenIntroduction RHDapriellejoyjovenaNoch keine Bewertungen
- RCL Physical Exam Guidelines For Examining Physician 11-2014Dokument4 SeitenRCL Physical Exam Guidelines For Examining Physician 11-2014George Mihalache100% (1)
- CPR: Lifesaving Technique for Cardiac & Respiratory EmergenciesDokument5 SeitenCPR: Lifesaving Technique for Cardiac & Respiratory EmergenciesMukesh KumarNoch keine Bewertungen
- Rehabilitation Following Partion Glossectomy and Neck DissectionDokument10 SeitenRehabilitation Following Partion Glossectomy and Neck DissectionnotmelbrooksNoch keine Bewertungen
- Meckel's Diverticulum Location IleumDokument1 SeiteMeckel's Diverticulum Location Ileumidk broNoch keine Bewertungen
- Causality assessment of single case reportsDokument11 SeitenCausality assessment of single case reportsM LyaNoch keine Bewertungen
- B.N. Mitra's Tissue Remedies guideDokument2 SeitenB.N. Mitra's Tissue Remedies guideSoumen PaulNoch keine Bewertungen
- Prescription Template 02Dokument2 SeitenPrescription Template 024NM19CS099 KUMAR NISHANTNoch keine Bewertungen
- Immunolgy Unit1 Q AQADokument21 SeitenImmunolgy Unit1 Q AQAKajana Sivarasa ShenthanNoch keine Bewertungen
- Heart Disease in PregnancyDokument5 SeitenHeart Disease in PregnancyAngeliqueNoch keine Bewertungen
- Research OUTPUTDokument10 SeitenResearch OUTPUTjoedlaranoiiiNoch keine Bewertungen
- Ear - WikipediaDokument15 SeitenEar - WikipediadearbhupiNoch keine Bewertungen
- Biochemical Biomarkers in Alzheimer's DiseaseDokument150 SeitenBiochemical Biomarkers in Alzheimer's DiseaseInternational Medical PublisherNoch keine Bewertungen
- Minutes 2ND QuarterDokument6 SeitenMinutes 2ND QuarterBarangay LiwaywayNoch keine Bewertungen
- Cholesteatoma Definition and Classification: A Literature ReviewDokument6 SeitenCholesteatoma Definition and Classification: A Literature ReviewRobertNoch keine Bewertungen
- FINAL People BrochureDokument19 SeitenFINAL People BrochureWilliam PerkinsNoch keine Bewertungen
- Surgical Versus Medical Treatment of Drug-Resistant Epilepsy: A Systematic Review and Meta-AnalysisDokument10 SeitenSurgical Versus Medical Treatment of Drug-Resistant Epilepsy: A Systematic Review and Meta-AnalysisSebastianNoch keine Bewertungen
- Dafpus IskDokument4 SeitenDafpus IskmarsyaNoch keine Bewertungen
- CNL Final Exam Study GuideDokument15 SeitenCNL Final Exam Study GuideGelsey Gelsinator JianNoch keine Bewertungen
- CISF SCREENING GUIDELINES PRESENTATION - TO BE FOLLOWED BY CISF SECURITY STAFF FOR PASSENGERS WITH DISABILITIES AT INDIAN AIRPORTS - Cisf PPT FinalDokument36 SeitenCISF SCREENING GUIDELINES PRESENTATION - TO BE FOLLOWED BY CISF SECURITY STAFF FOR PASSENGERS WITH DISABILITIES AT INDIAN AIRPORTS - Cisf PPT FinalDisability Rights Alliance100% (1)
- Director - ProfileDokument2 SeitenDirector - ProfileHimanshu GoyalNoch keine Bewertungen
- 2016 Issue 1Dokument86 Seiten2016 Issue 1Fareesha KhanNoch keine Bewertungen
- Antiprotozoal and Antihelminthic Drugs - HandoutDokument21 SeitenAntiprotozoal and Antihelminthic Drugs - HandoutdonzNoch keine Bewertungen
- Test Bank For Ethics and Law in Dental Hygiene 3rd Edition by BeemsterboerDokument36 SeitenTest Bank For Ethics and Law in Dental Hygiene 3rd Edition by Beemsterboertyphous.madrierdvfzai100% (46)
- Musictherapy in Dental Medicine: Dr. Gabriela Iorgulescu, MDD, Ma, Ba, PHDDokument6 SeitenMusictherapy in Dental Medicine: Dr. Gabriela Iorgulescu, MDD, Ma, Ba, PHDMarco Antonio García LunaNoch keine Bewertungen
- Uri Flush 3 Liquid Stones ProblemDokument4 SeitenUri Flush 3 Liquid Stones ProblemSourabh KoshtaNoch keine Bewertungen