Beruflich Dokumente
Kultur Dokumente
Bio Physio
Hochgeladen von
سامي التريكيCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bio Physio
Hochgeladen von
سامي التريكيCopyright:
Verfügbare Formate
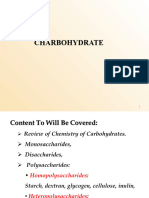
carbohydrates
Sugars that contain aldehyde groups that are _ _ _ to carboxylic acids are
classified as sugars.
• oxidized, non-reducing
• oxidized, reducing
SAADDES
• reduced, non-reducing
• reducing, oxidizing
copyright Cl 20 13-2014 Dental Decks
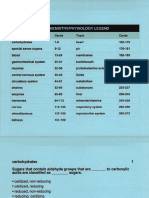
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• oxidized, reducing
*** Examples include: lactose, maltose, g lucose, galactose, and fructose.
Reducing sugars contain a free anomeri c carbon (oxygen on Cl atom is available for
redox reaction) that can be oxidized. If the oxygen on the anomeric carbon (the
carbonyl group) of a sugar is not attached to any other structure, that sugar is a
reducing sugar. The carbonyl group of the monosaccharides has reducing
properties. The reducing properties are lost when the carbonyl carbon forms a
glycosidic bond.
Important point: This reaction is the basis of a reducing-sugar test, which was
SAADDES
classically used by clinical laboratories to screen for diabetes (presence of excess free
glucose in the blood) and other inborn errors involving the inability to metabolize
other reducing sugars.
• Most current clinical tests for blood glucose utilize glucose oxidase linked
reactions.
• Because the reducing groups of both glucose and fructose are involved in the
glycosidic bond, sucrose is not a reducing sugar. In other words, sucrose contains
no free anomeric carbon.
• Monosaccharides combine into larger molecules by forming glycosidic bonds.
These bonds form when the hydroxyl group on the anomeric carbon of a mono-
saccharide reacts with an -OH or -NH group of another compound (typi ca lly an al-
cohol, purine, pyrimidine, or in this case another sugar).
• Glucosuria, the presence of glucose in the urine, can be caused by low
insulin levels, high blood sugar levels, impaired tubular reabsorption, or a high
glomerular filtration rate. Note: The threshold for glucosuria is 160-180mg/dl.
Saad Alqahtani, Twitter @saaddes
Glucose
H
I
C= O
I Open Chain
H - C - OH
I
HO - C - H
I
H - C - OH
I
H - C - OH
I
H - C - OH
I
SAADDES
H
l Anomeric Carbon
4
Cyclic form
H OH H OH
a - D-Glucopyranose ~-0-Giucopyranose
Saad Alqahtani, Twitter @saaddes
Cl-0 -Giucose !3-D-Glucose
SAADDES
Comparison of alpha and beta configuration of 0-Giucose
~
A g lycosidic bond, also known as a glycosid ic
linkage is the two-bond link between the rings
in an oligosaccharide or polysacchcaride.
Sucrose
Glycosidic bond
0
HOC~2 O
HO
lA-1
CH 20H
OH
Saad Alqahtani, Twitter @saaddes
carbohydrates
Which of the following glycosaminoglycans can be found functioning in syn-
ovial fluid?
• hepari n
• keratan sulfate
SAADDES
• hyaluronate
• dermatan sulfate
• chondroitin sulfate
• heparan sulfate
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hyaluronate
Glycoproteins are conjugated proteins, w hich contain one or more saccha rides lacking a serial repeat unit
and are bound covalently to a protein. There i s a class of complex macromol ecules t hat may contain 95%
or more of carbohydrates, and it resembles polysaccharides more than it resembl es proteins. To d istinguish
them from other glycoproteins, they are called proteoglycans. Their ca rbohydrate chains are called gly-
cosaminoglycans. Proteoglycans consist of many d ifferent g lycosaminoglycan chains linked coval ently to
a protein core. Six d istinct classes are recognized: chondroitin sulfate, dermatan sulfate, keratan sulfate, he-
paran sulfate, heparin, and hyaluronate.
Certain features are common to the d ifferent classes of g lycosaminoglycans (GAGs). The long unbranched
heteropolysaccha ride chains are made up l argely of d isaccha ride repeating units, consi sting of a hex-
osamine and a uronic acid. Common consti tuents of GAGs are sul fate groups, linked by ester bonds to cer-
tain monosaccharides or by amide bonds to the amino g roup of g lucosamine. Only hyaluronate is not
SAADDES
sulfated and is not covalently attached to protein. The carboxyl s of uronic acids and the sulfate groups con-
tribute to the highly charged nature of GAGs.Their el ectrical charge and their macromolecular structure are
important in the their rol e as lubricants and support elements in connective t issue. GAGs are predomi-
nantly components of the extracellular matrices and cell surfaces, and they participate in cell adhesion and
signaling.
( h,u <u:ttn"~olu.:s uf<. \{.'!.
LouUulion Cunmuntll
Hyaluronalc Synovial Omd. vitreous humor. I!LM Large polymers, shock absori>mg
of loose oonnc-c-ti\'C Iissue
Chondroitin suliate Cartilage. bone, hc:art \'alvcs Mos1 abundant <1AG
Hcpamn sulfate Basc-mcnl membranes. components of ConlaUlS h1g.her tu:ctylatcd glucosanunc
cell suriae>cs than hcpann
Heparin Component oiinlracdlular granules of Scn•es as an antu:oagulant. more sulfn1cd
mast cdls limng the nrtclics oithc than hcparan sulfate
lungs.li\'cr. and skm
D«matan sulfate Skin. blood vessels. heart valves
Kttntan suli3tc: Cornea, bone, c-artilage ag~gtll<'d With Mos1 hcl«ogenous GAG
chondroitin sui rates
Saad Alqahtani, Twitter @saaddes
carbohydrates
Which intestinal enzyme breaks down the 0 -glycosidic bond between
glucose and fructose?
• maltase
• lactase
SAADDES
• sucrase
• none of the above
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• sucrase
A disaccharide is a carbohydrate cons isting of two sugar units in a covalent bond.
Examples include:
• Maltose ("beer sugar") - cons ists of two glucose molecules j oined together by a
reaction (condensation reacti on) in which a molecule of water is removed. Th is reaction
produces a bond between the two glucose molecules called a glycosidic bond. The
intestinal enzyme maltase p romotes the conversion of maltose into glucose.
• Lactose ("milk sugar") - consists of glucose and galactose. The intestinal enzyme
lacta se p romotes the conversion of lactose into glucose and galactose.
• Sucrose ("table sugar")- consists of glucose and fructose. The intestinal enzyme sucr-
SAADDES
ase (invertase) promotes the conversion of sucrose into glucose and fructose.
Remember: The final digestion of these substances (d isaccharides) to absorbable
monosaccharides is completed by enzymes of the small intestine (maltase, sucrase, and
lactase). These monosaccharides can then be absorbed by enterocytes.
Important: Monosaccharides can be linked by glycosidic bonds to create larger
structures (disaccharides, oligosaccharides, and polysaccharides). These bonds form when
the hydroxyl group on the anomeric carbon of a monosaccharide reacts w ith an - OH or
-NH group of another compound (typically an alcoho l, purine, pyrimidine, or in this case
another sugar). Maltose, lact ose, and sucrose consist of monosaccharides joined by an 0-
glycosidic bond.
1. If oxygen is involved, this bond is classified as 0-glycosidic (found in
polysaccharides); if nitrogen is involved, this bond is classified as N-glycosidic
(found in glycoproteins and nucleotides).
2. 0-glucose is a monosaccharide, the most important of the aldohexoses.
Saad Alqahtani, Twitter @saaddes
carbohydrates
Glucose, fructose, and galactose are classified as:
• monosaccharides
• disaccharides
• oligosaccharides
SAADDES
• polysaccharides
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• monosaccharides
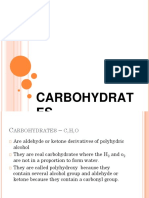
The simplest of the carbohydrates are the monosaccharides, which can be classified according
to the number of carbon atoms they contain. Those with three carbons are called trioses (for ex-
ample, glyceraldehyde and dihydroxyacetone); four, tetroses (for example, erythrose); five, pen-
toses (for example, ribose); and six, hexoses (for example, glucose).
Monosaccharides with an aldehyde as t heir most oxidized functional group are called aldoses
(for example, glyceraldehyde); those with a keto group as t heir most oxidized function al group
are called ketoses (for example, d ihydroxyacetone). Mon osaccharides wit h five, six, seven, or
eight carbon atoms occur as cyclic rings in nature (e.g., ribose, glucose, fructose, galactose).
Remember: The naming of configuration s of simple sugars (monosaccharides) and amino
SAADDES
acids is based on t he absolute configuration of glyceraldehyde. The sym bols L and D refer to
the absolute configuration of the four constituents around a specific chiral carbon
(asymmetric carbon) in monosaccharides and amino acids (see 0-Giyceraldehyde diagram
below). In a Fisher proj ection, t he 0 form has the hydroxyl group on the right; t he L form has
the hydroxyl group on the left. Sugars of the D form, which are related to 0-glyceraldehyde,
are the most common in nature.
Other monosaccharides include: man nose, ribose, and xylose.
CHO CHO
I I
H-C-OH H0-0 - H
I I
CH 20 H CH20H
0 -Giyceraldehyde L-Giyceraldehyde
Fischer projection formulas
Saad Alqahtani, Twitter @saaddes
carbohydrates
Which of the following polysaccharides is hydrolyzed by glucan transferase?
• starch
• glycogen
• cellu lose
SAADDES
• glycosaminoglycans
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• glycogen
Polysaccharides are carbohydrates that are p olymers of monosaccharides.
Polysaccharides are made up of many sugar units covalently bonded by condensation
reactions (wh ich results in 0 -glycos idic b onds). Since polysaccharides have large
molecules, they are insoluble. Their main functions in living organisms are to act as
storage molecu les (starch and glycogen) or as st ructu ral materials (cel lulose).
Homopolysaccharides (starch, glycogen, dextrans, and glucans) contain only a single
monosaccharide species. Heteropolysaccharides (g lycosaminoglycans) contain a number
of different monosaccharide species. The two most important storage polysaccharides are
starch and glycogen.
• Starch is a large, insoluble carbohydrate that forms an important energy store in
plant s. Starch is a polymer and consists of a large number of a-glucose molecul es
SAADDES
j oined together by condensation reactions. It consists of two main components
that may be present in different prop orti ons. Amylose (wh ich is unbranched)
forms long straight chains wh ile amylopectin has highly branched chains with a
a-1,6 linkages. Note: Both amylose and amylopectin are rapidly hydrolyzed by t he
enzyme alpha amylase, wh ich is secreted by the parotid glands and t he pancreas.
• Glycogen is a branched polymer of between 10,000 and 40,000 glucose residues
held together by a-1,4 glycosid ic bonds. Approxim ately one in 12 glucose residues
serves as a branch point forming an a-1,6 glycosidic bond with another glucose residue.
It is especially abundant in the liver. Note: The glucose unit s of glycogen can enter the
glycolytic pathway after removal by t he action of glycogen phosphorylase. Note: The
cleavage of glycogen b eyond a branching point requi res the activity of
glucantransferase and amylo-alpha-1 , 6-glucosidase.
Cellulose is the most common organ ic co mpound on earth. Cellul ose is not digestible by
h umans and is often referred to as "dietary fiber" or "roughage:' acting as a hydrophilic
bulking agent for feces. Cellulose is still a glucose polymer chain, but linked differently w ith
81-41inkages. The term glycan refers to a polysaccharide or an oligosaccharide.
Saad Alqahtani, Twitter @saaddes
carbohydrates
The ground substance ofthe extracellular matrix is made up of:
• type II collagen
• type Ill collagen
• p roteoglycan molecules
• fibri lli n
SAADDES
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• proteoglycan molecules
Proteoglycans consist of a co re protein w ith glycosaminog lycans (GAGs) attached in
a brush-like fashion and are 95% polysacchari de and 5% protein. Major functions
include: lubricants, extracellular matrix, and being a molecular "sieve:· Note: Six
distinct classes are recognized: chondroitin sulfate, dermatan sulfate, keratan sulfate,
heparan sulfate, heparin, and hyaluronate.
Glycoproteins are conjugated proteins, which conta in one or more saccharides lack-
ing a seri al repeat unit and are bound covalently to a protein. The carbohydrate portion
of most g lycoproteins d iffers from that of p roteoglycans in that it is shorter and
SAADDES
branched. They serve as enzymes, hormones, antibodies, and structural proteins. Gly-
coproteins are often components of cel l membranes and are involved in cell-to-cell in-
teractions.
Glycolipids (or sph ingolipids) are found in the cel l membrane with the
carbohyd rate portion extending into the extracellular space. They are derived from
the lipid ceramide, and th is class of com pounds includes cereb rosides,
globosides, and gangliosides.
Molecule Components C haracteristic Role
Proteoglycan Protein + GAGs l ong & straight lubrication, ECM, Molecular "sieve''
Glycoprotein Protein + Carbohydrate Short & branched Enzymes, honnones, antibodies,
structural prote ins
Glycolipids l ipid + Carbohydrate NIA Cell membrane receptors
Saad Alqahtani, Twitter @saaddes
carbohydrates
The most abundant glycosaminoglycan in the body is:
• keratan sulfate
• dermatan sulfate
• chond roitin sulfate
SAADDES
• heparan sulfate
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• chondroitin sulfate
Chondroitin su lfate is a major constituent in various connective tissues, especially in the
ground substance of blood vessels, bone, and cartilage. In cartilage chondroitin sulfate,
provides structure by holding water and nutrients, and allowing other molecul es to move
through cartilage - an important property, as there is no blood supply to cartilage. Chon-
droitin may work by acting as a buil ding b lock for proteog lycan molecules, and may also
have anti-inflammatory pro perties. Important: In our joints, chondroitin sulfate contrib-
utes to strength, fl exibility, and shock absorption.
Remember: The extracellular space in animal t issues is filled with a gel-like material,
the extracellular matrix, also called ground substance, which holds the cells of a t issue
SAADDES
together and provides a porous pathway for the diffusion of nutrients and oxygen to
individual cell s. The ground substance is composed of an interlocking meshwork of
heteropolysaccharides (glycosaminog lycans), most covalently linked to protein forming
proteog lycans, and fibrous proteins.
Important: Hyaluronidase will promote depolymerization of the extracellul ar matrix
(ground substance). Hyaluronidase is an enzyme that splits hyaluronic acid
(g lycosaminoglycan) and so lowers its viscosity and increases the p ermeability of
connective t issue and the absorption of fluids.
1. Heparin contains the largest proport ion of sulfate (yes, even more than
heparan su lfate).
2. Only hyaluronate is not sulfated and is not covalent ly attached to a protein.
3. Remember: GAGs are the long unbranched heteropolysaccharide chains made
u p largely of disaccharide repeating units, consisting of a hexosamine and a uronic
acid. Common constituents of GAGs are sulfate groups, linked by ester bonds to
certa in monosaccharides or by amide bonds to the amino group of glucosamine.
Saad Alqahtani, Twitter @saaddes
carbohydrates
For each Jetter, choose the most appropriate answer to fill in the blank.
Dextrans are (A) _ _ of (B) _ _ produced extracellularly by bacteria and
yeast. The enzyme used to produce dextrans is (C) __, and the substrate
is (D) _ _ . A side product of dextran production is (E) _ _ , which is
formed into (F) _ _ and stored intracellularly as reserve nutrients.
SAADDES
• (A) monosacchari des I polysaccharides I oligosacchari des
• (B) glucose I fructose I galactose
• (C) dextran synthase I glucosyl transferase I fructosyl t ransferase
• (D) maltose I sucrose I lactose
• (E) glucose I fructose I galactose
• (F) starch I glycogen I !evans
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
(A) polysaccharides
(B) glucose
(C) glucosyl transferase (dextran sucrase)
(D) sucro se
(E) f ructose
(F ) levans (fructan s)
Dextrans are polysaccharides of glucose produced extracellularly by bacteria and
yeast. The enzyme used to produce dextrans is glucosyl transfera se (dextran sucrase),
and the substrate is sucrose. A side product of dextran production is fructose which
SAADDES
is formed into I evans (fructans) and stored intracellularly as reserve nutrients.
A few bacteria, notably Streptococcus mutans, produce dextran from sucrose.
Dextran is a "sticky" polymer of glucose molecules linked together in a.- (1,6) linkages
with some a- (1 -3) branches. It is produced outside bacterial cells by the enzyme
glucosyl transferase (dextran sucrase). This enzyme splits sucrose into glucose and
fructose and links the glucose molecules into a dextran polymer. The dextran is
deposited as a th ick glycocalyx around the cel l and seems to be essential fo r the
ca ri ogenicity of Streptococcus mutans.
Note: Fructan s (Ievans) also increase the adhesion of bacteria to surfaces of the teeth
and promote the formation of dental plaque. It is formed from the f ructose moiety
of sucrose by the enzyme fructosyl transferase (levan sucrase). Fructans are
considered to be reserve nutrients for bacteria.
Saad Alqahtani, Twitter @saaddes
special sense organs
All of the following statements are true EXCEPT one. Which one is the EXCEP-
TION?
• rods contain rhodopsin -a photopigment
• cones are responsible for color vision
SAADDES
• rods are used for dark adaptation
• rods and cones are located in the retina
• cones are more abundant than rods
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• cones are more abundant than rods
The retina is the innermost layer (nervous tissue) of the eye. The retina receives visual
stimuli and sends the information to the brain. Photoreceptor cells ca lled rods and
cones compose the visual receptors (for the optic nerve) of the retina. Rods and
cones contain photopigments. There are four different photopigments, each
consisting of a protein called an opsin to which a chromophore molecule cal led
retinal is attached. Opsins differ from pigment to pigment and confer specific light-
sensitive properties on each photopigment. Note: Retinal is produced from vitam in
A and is added to an opsin to synthesize rhodopsin.
SAADDES
Rods contain a photopigment called rhodopsin. Their response indicates d ifferent
degrees of brightness, but the entire rod system is characterized by a relative lack of
color discrimination. Rods are numerous in the periphery of the retina.
Cones are primarily responsible for color vision. There are three d ifferent types of
cones (red, g reen, and blue). Each one contains a different photopigment and is
selectively sensitive to a particula r wavelength of light. They are concentrated in the
center of the retina, especially in the fovea .
1. Duri ng dark adaptation (night vision), rhodopsin is synthesized in the
rods. Severe vitamin A deficiency over many months causes night blindness.
2. Cones are the principal photo receptors during daylight or in brightly lit
areas.
3. Rods are more abundant, have higher sensitivity, and lower acuity com-
pared to cones.
Saad Alqahtani, Twitter @saaddes
special sense organs
Which of the following structures of the eye functions like a shutter in the
camera analogy, allowing more or less light into the eye?
·lens
• retina
SAADDES
• cornea
• iris
10
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• iris
Ba sic anatomy of the eye:
• Cornea- The crystal clear dome that covers the front of the eye. The maj ority (70%) of
the bending (refracting) of li ght rays is accompli shed by the cornea. The shape of the
cornea does not change (with t he except ion of small changes that occur over a life-
time). Remember: The majority of the focusing is done by the cornea, not the lens.
• Lens- The crystalline lens finishes the focusing of light. The lens helps to "fine -tune"
vision, and it is able to change shape to allow focus on near objects. When the lens
becomes cloudy, it is called a cataract.
• Pupil -This is the opening in the middle of the iris.
SAADDES
• Iris -This is t he part of the eye that gives it co lor (i.e., b lue, green, brown). The iris
functions like a shutter in the camera analogy, allowing more or less light into the eye.
• Retina - Th is is a th in layer of nerve t issue that senses light. Specialized cell s called
rods and cones convert light energy into nerve signals t hat travel through t he opt ic
nerve to the brain. The retina is analogous to the film in a camera.
• Fovea- This is the center of t he retina that receives the focus of the object of regard.
Nerve cells are more densely packed in this area, especially cones, so im ages that are
focused on the fovea can be seen in greater detail.
• Opt ic nerve- This is the nerve that runs from the eyeball to t he brain. The opti c nerve
carries information f rom the ret ina to the brain for interpretation.
Note: The eyeball itself is divided into two segments, each fill ed w ith fluid. The anterior
segment has two chambers (anterior and posterior), which are both fill ed with aqueous
humor (watery fluid), and the posterior segment is fi lled w ith vitreou s humor (thick,
gelatinous material).
Saad Alqahtani, Twitter @saaddes
Anterior chamber
lridocorneal angle
I"<-- - Canal of Schlemm
::::,....-~--- Posterior
chamber
SAADDES
Vitreous body
Sclera
Lamina cribrosa 1().1
Central retinal artery
Saad Alqahtani, Twitter @saaddes
special sense organs
A sound wave will strike the first.
• membrane of the oval w indow
• membrane of the round w indow
• tectoria l membrane
SAADDES
• tympanic membrane
11
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• t ympanic m embrane
Sound waves strike the tympanic membrane and cause it to vibrate. This causes the
membrane of the oval window to vibrate, which causes the perilymph in the bony
labyrinth of the cochlea and endolymph in the membranous labyrinth of the cochlea to
move. This movement of the endolymph causes the ba silar membrane to vibrate, which,
in turn, stimulates hair cells on the organ of Corti to transmit nerve impulses along the
cran ial nerve. Eventually, nerve impu lses reach the auditory cortex and are interpreted as
sound.
Parts of the Ear:
External ear- consists of the external part (pinna) and the ear canal
SAADDES
• Auricle (pinna)- directs sound waves
• External auditory canal (meatus) - contains hair and cerumen (brown earwax);
serves as a resonator
Middle ear (tympanic cavity)- an air-fi lled cavity in the temporal bone
• Auditory tube - equalizes pressure
·Ossicles (mall eus, incus, stapes) - link together to transmit sounds to the oval win -
dow and create a 22 fold amplification of sound fro m the tympanic membrane to the
oval w indow
Inner ear - formed by a membranous labyrinth w ith in a bony labyrinth
• Vestibule (saccule and utricle) - associated with sense of balance
• Semicircular canals - concerned w ith equilibrium
• Cochlea (contains two membranes, vestibular and basilar) - portion of inner ear
responsible for hearing. The spiral organ (organ of Corti) conta ins the receptors
(called hair cells) for hearing. The cochlea is the basic functional unit of hearing
because this portion t ransforms flui d vibrations from sound waves (mechanical
energy) into a nerve impulse (electrical energy).
Saad Alqahtani, Twitter @saaddes
Outer Middle Inner
Semicircular canal
Vestibular
SAADDES
nerve
Cochlear
nerve
lExrema~l
auditory canf l
Tympanic Tympanic
membrane cavity
lH
Saad Alqahtani, Twitter @saaddes
special sense organs
Your patient just returned from an ophthalmology appointment where
she received tropicamide to induce mydriasis. What significance does
this have on her dental appointment?
• the patient can't d istinguish colors when choosing denture teeth
SAADDES
• the patient will be extra sensitive to the overhead dental light
• the patient will have trouble seeing without bri ght light
• the patient will experience blurry vision
12
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the patient will be extra sensitive to the overhead dental light
Remember:
1. Miosis is the constriction of the pupil of the eye. M iosis can be caused by a
normal response to an increase in light, certa in d rugs, or pathological conditions.
2. Mydriasis is the prolonged abnormal dilation of the pupil of the eye induced
by a drug or caused by a disease and causes the eyes to become extra sensitive to
light.
In myopia (nearsightedness), the eye is too long for the refractive power of the lens,
and far objects are focused at a point in front of the retina. The eye can focus on
very near objects. This is caused by a cornea that is steeper, or an eye that is longer,
SAADDES
than a normal eye. Nearsighted people typica lly see well up close but have difficulty
seeing far away. To treat myopia, concave lenses are used.
Farsightedness, or hyperopia, occurs when light entering the eye focuses behind
the retina, instead of d irectly on it. This is caused by a cornea that is flatter, or an eye
that is shorter, than a normal eye. Farsighted people usually have trouble seeing up
close but may also have difficulty seeing far away as well. To treat hyperopia, convex
lenses are used.
Astigmatism occurs when the cu rvature of the lens is not uniform and is corrected
with cylindric lenses.
Presbyopia is the inability of the eye to focus sharply on nearby objects, resulting
from the loss of elasticity of the lens with advancing age. Presbyopia is corrected w ith
bifocals.
Saad Alqahtani, Twitter @saaddes
blood
The normal range for hemoglobin is different between the sexes and is
approximately _ _ _ for men and _ _ _ for women.
• 5-8 grams per deciliter, 2-3 grams per deciliter
• 9-11 grams per decili ter, 7-9 grams per deciliter
SAADDES
• 13-18 grams per decili ter, 12-16 grams per deciliter
• 20-22 grams per decili ter, 18-21 grams per deciliter
13
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• 13-18 gram s per deciliter, 12-16 grams per deciliter
Hemoglobin is a quaternary protein consisting of four tertiary (folded) polypept ide chains - two
alpha chains and two beta chains. Each chain has an associated iron-containing heme group.
Oxygen can bind to the iron of the heme group or carbon dioxide can bind to amine groups of the
amino acid s in the polypeptid e chains. Hemoglobin is essential to the ability of erythrocytes to
transport oxygen and carbon dioxide; and a single erythrocyte contains up to 300 million
hemoglobin molecules.
Important point: Each hemoglobin molecule contains four iron atoms. Each atom binds one
diatomic oxygen molecule for a maximum capacity of eight oxygen atoms per hemoglobin
molecule.
Normal Blood Values of Hemoglobin (* 100 ml =1 dl)
SAADDES
• Women: 12 to 16 grams per deciliter
• Men: 13 to 18 grams per deciliter
• Newborn: 14 to 20 grams per deciliter
Important:
• The Hgb value depends on the number of RBCs and the amount of Hgb in each RBC
• A low Hgb value is found in anemia, in hyperthyroidism and in cirrhosis of the liver
• A high Hgb value is found in polycythemia, in COPD, and in congestive heart failure
1. Hemoglobin carries oxygen to tissue from the lungs and carbon dioxide away from
8 tissue to the lungs. (Remember: the Bohr effect refers to a mechanism whereby acid in
the tissues assists in 0 2 unloading from Hb, to promote 0 2 delivery to the tissues; the Bohr
effect is very strong in the fetus.
2. Blood leaving the lungs is 98% saturated with oxygen. However, the hemoglobin of
normal venous blood returning to the lungs is only 75% saturated.
3.Carbaminohemoglobin is hemoglobin that is carrying carbon dioxide from the tissues
to t he lungs. Whereas about 97% of the oxygen is tra nsported by hemoglobin, only about
30% of the carbon dioxide iscarried by hemoglobin; the rest is transported as bicarbonat e
or as carbon dioxide.
Saad Alqahtani, Twitter @saaddes
blood
Although albumin accounts for only 60% of the total plasma protein, it pro-
vides 80% of the colloid osmotic pressure of the plasma.
The colloid osmotic pressure is necessary to prevent edema.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
14
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Albumin is a single tightly packed polypeptide with 585 amino acids, without any covalently
bound carbohydrate. Its shape minimizes its effect on plasma viscosity. In general, compact
proteins do not increase the plasma viscosity to the same extent as more elongated proteins
of the same molecular weight. With its molecular weight of 66,000 D and an acidic isoelectric
point (pi), it is able to avoid renal excretion, but it does cross the vascular endothelium of most
tissues to a limited extent. Therefore, it is present in interstitial fluid and lymph but at lower
concentrations than in the plasma.
Because the interstitial fluid volume is fa r larger than the plasma volume (1 2% versus 4.5% of the
body volume, respectively), the total amount of albumin in the interstitial spaces slightly exceeds
that in the vascular compartment. Thisalbumin is returned to the blood by the lymph.
Although albumin accounts for only 60% of the total plasma protein, it provides 80% of the colloid
SAADDES
osmotic pressure of the plasma. This is because the col loid osmotic pressure depends on the
amount of water and elect rolytes that a protein attracts to its surface, and albumin is one of the
most hydrophilic plasma proteins. Loss of albumin can result in hyperbi lirubinemia and manifest
as jaundice.
The colloid osmotic pressure is necessary to prevent edema. In the capillaries, the hydrostatic pres-
sure of the blood forces fluid from the blood into the interstitial spaces. The colloid osmotic pressure
of the albumin and other plasma proteins is necessary to draw this fluid back into the capillary. Fluid
balance across the endothelium is maintained as long as these two forces cancel each other.
Usually, edema develops when the albumin concentration drops below 2.0 g/dl. Edema can also be
ca used by an increase in capil lary permeability, venous obstruction, impaired lymph flow, and con-
gestive heart failure with an increased venous pressure.
l .The kidney is the organ that is chiefly responsible for the regulation of the osmotic
pressure in the body fluids by regulating the reabsorption of water in response to anti-
diuretic hormone (ADH or vasopressin).
2. As a binding protei n, albumin is extremely versatile, with binding sites for fatty
acids, thyroxine, cortisol, heme, bilirubi n, and many other metabolites. With the
exception of albumin, almost all plasma proteins are glycoproteins.
Saad Alqahtani, Twitter @saaddes
blood
The principal hormone for serum calcium regulation is:
• ca lcitonin
• parathyroid hormone
• thyroid hormone
SAADDES
• vasopressin/antidiuretic hormone
15
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• parathyroid hormone
The human body contains 1-1.5 kg Ca'•, most of which (about 98%} is located in the mineral
substance of the bone. Calcium levels are regulated primarily by parathyroid hormone (PTH}, and
also by vitamin D and calcitonin. PTH and vitamin D increase serum calcium, while calciton in
decreases ("tones down"} blood calcium levels (see table below}.
Patients with hyperparathyroidism will have decreased renal calcium excretion and will also be
predisposed to an increased likelihood of bone fracture because PTH's primary purpose is to
increase the concentration of serum calcium .The bone resorption seen in elderly patients with low
dietary ca lcium is intensified by pa rathyroid hormone. Calcium blood levels are increased in
hypervitaminosis 0, in hyperparathyroidism, in bone cancer and other bone diseases. Calcium
blood levelsare decreased in severe diarrhea, in hypopa rat hyroidism, and in avitaminosis D (rickets
and osteomalacia}.
SAADDES
Note: Remember that calcitonin and PTH are complimentary hormones that work together to keep
a balance within serum calcium levels. Recall that if PTH increases serum calcium, calcitonin "tones•
down the serum calcium level by depositing more in bone as well as increasing its excretion.
Plasma phosphorus concentration (normal is approximately 4 mg%} is also regulated by
parathyroid hormone. Increased hormone causes the kidneys to increase the rate of phosphate
excretion, which decreases plasma phosphate concentration.
Frll \ ' ifa1ai1t 0 C.kJtoni11
Stilnutusru r o.:~:u:nnn(Ca~) i>«TcM<:so:nun(C.)I~) ln('f'Q.'I<:llcnnn(C.'ll!<-)
So:cr~i•• n ln~ l'1ll
D«-1-c~J.t" so:rum pbo!!pbatc
Aniunun:
Bum: lrn:n::l.'lci'C'llurptwn ln~rc$0rplwn O.:ac:uc u~sorptwn
K1dn~ o.:~ r~phllll'llll n:ab,;orpbun In~ rbullphuru..,; r-:ab~rpboo N/A
lrn:n:a'!o:Ca1• rt'ab,;orphlllll In~ Crl· n:-ab~hoo
c.:· ~,;orpboo (''~a
lmc~llrn: lrn:ra.'lo:
ac:th-abun of vit11mm l)l ::: : ~~'!=~~rptUln N/A
In~
In~ N fA
Saad Alqahtani, Twitter @saaddes
blood
Which of the following blood equations is correct?
• serum = plasma- fibri nogen
• plasma = serum -fibri nogen
• serum = hematocrit + plasma
SAADDES
• hematocrit = fibrinogen - plasma
16
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• serum =plasma - fibrinogen
Human blood constitutes about 8% of the body's weight. Blood consists of cells and
cell fragments in an aqueous medium, the blood plasma. The proportion of cellula r
elements, known as hematocrit, in the total volume is approximately 45%. The blood
is the most important transport medium in the body. Blood maintains homeostasis
and plays a decisive role in defending the body against pathogens.
Serum is the clea r, thin, and sticky flu id portion of the blood obtained after removal
of the fibri n clot and blood cel ls. Serum differs from the plasma in that serum lacks
fibrin and other coagu lation products.
SAADDES
Plasma is blood m inus the formed elements. It is the flu id portion of the blood
(plasma makes up 55% of the blood). Plasma also conta ins no cells.
Plasma contains:
• Proteins (7%)- consist of albumins, globulins, and fibrinogen
• Water (91%)
• Other solutes (2%) -consist of metabolic end products, food materials,
respiratory gases, hormones, and ions
1. Remember: The other 45% of the blood consists of formed elements -
erythrocytes (red blood cells), leukocytes (white blood cel ls), and
thrombocytes (platelets).
2. The function of platelets in hemostasis is that they agglutinate and plug
small ruptured vessels.
Saad Alqahtani, Twitter @saaddes
blood
The general term for reactions that prevent or minimize loss of blood
from the vessels if they are injured or ruptured is:
• erythropo iesis
• syneresis
SAADDES
• homeostasis
• hemostasis
17
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hemostasis
Th rough a three-part process, the circulatory system guards against excessive blood loss. In this
process, vascular injury activates a complex chain of events - vasoconstriction, platelet
aggregation, and coagulation - that leads to clotting. Th is process stops bleeding without
stopping blood flow through the inj ured vessel.
Three essential steps for blood clotting:
1. The production of thrombin from prothrombin during the clotting process requ ires a
prothrombin activator (Factor Xa-Factor V complex), which is formed either by way of
an extrinsic pathway or by way of an intrinsic pathway. Remember: The only protease of
the extrinsic pathway is factor VIla, which is formed from the inactive factor VII by thrombin
on factor X. However, proteolytic activation is not sufficient. Factor VIla is active only in the
SAADDES
presence of tissue factor, a membrane glycoprotein in subendothelial tissue. Tissue factor
and factor VIla come in contact only after vascular inj ury. The intrinsic pathway requires only
factors already present in the blood (e.g., kininogen, kallikrein, and Hageman factor [F XII)), how-
ever, it on ly becomes activated on contact with a negatively cha rged surface - the exposed
extracellular matrix in the body offers this negatively cha rged surface.
2. Prothrombin activator (Factor Xa-Factor V complex) acts enzymat ically to catalyze the form-
ation of thrombin (Factor lla) from prothrombin (Factor II).
3. Thrombin (Factor lla) acts as an enzyme to convert fibrinogen (Factor I) into fibrin (Factor Ia)
threads that enmesh red blood cells and plat elets to form the clot itself.
1. When blood vessels are ruptured and tissues are damaged, both the extrinsic and
intrinsic pathways are usually act ivated.
2. In cirrhosis of the liver, prothrombin and fibri nogen levels w ill be deficient and
cause impaired clot formation. Remember: The liver synthesizes factors II, VII, IX, and X.
3. Homeostasis - tendency toward equilibrium between different but interdependent
elements of an organism.
4. Erythropoiesis- the production of red blood cells.
5. Syneresis -liquid separating from a gel due to further solidification or coagulation.
Saad Alqahtani, Twitter @saaddes
(1) Tissue trauma
!
Tissue Factor
(2) VII
r: Vll•i
SAADDES
x -------.:...---~~-Jio- Activated X (Xa)
L A c.- Prothrombin )
(3) activator
Platelet
phospholipids t I
't
Prothrombin ------~~ Thrombin
Ext rinsic pathway for initiat ing blood clotting.
t 17-1
Saad Alqahtani, Twitter @saaddes
Blood trauma or
contact with collagen
XII ~Activated XII (XIIa)
t -+- (HMW kininogen, prekallikrein)
(2) XI ---+- Activated XI (XIa)
t ( Ca..
(3)
Thrombin~!
VIlla
j
IX ~ Activated IX (IXa)
Ca••
SAADDES
(4) X
t Activated X (Xa)
(5)
Thrombin -+- Ca..
t
v----.-
Prothrombin
Platelet activator
phospholipids ) ~
Prothrombin - "":'t-+- Thrombin
Int rinsic pat hway for init iating blood clotting. 17 A· l
Saad Alqahtani, Twitter @saaddes
blood
Iron, the most important mineral in the formation of hemoglobin, is absorbed
mainly in the _ _ _ and is only absorbed as _ _ _ .
• ascending colon, Fe 3•
• sigmoid colon, Fe2 •
SAADDES
• duodenum, Fe3•
• jejunum, Fe2•
18
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• duodenum, Fe2 •
Iron is quantitatively the most important trace element. The human body contains
4-5 grams of iron, which is almost exclusively present in protein-bound form .
Approximately 75% of the total amount is found in heme p roteins, mainly
hemoglobin and myoglobin. In addition to hemoglobin and myoglobin, 15% to 25%
of iron is stored in the liver, spleen, and bone marrow, mainly in the form of
intracellular iron-protein complexes called ferritin and hemosiderin (a complex of
ferritin, denatured ferritin, and other proteins).
Iron is absorbed almost entirely in the upper part of the small intestine, primarily in
the duodenum. Here iron immediately combines in the blood plasma with a beta
SAADDES
globulin apotransferrin, to form transferrin, which is then transported in the
plasma. Iron is bound loosely with transferrin and can be released to any of the tissue
cells at any point in the body. Approximately 60% of excess iron is stored in the liver.
The iron stored in ferritin is ca lled storage iron.
Important: Iron can only be absorbed by the bowel in bivalent form (i.e., as Fe 2• ). For
this reason, reducing agents in food such as ascorbate (vitamin C) promote iron
uptake.
l.The dominant factor controlling absorption of iron from the Gl tract is the
8 saturation of mucosal cells with iron particularly dictated by the rate at
which the transferrin complex is able to exit the epithelial cell into the
vascular system.
2. Hemochromatosis is an iron-storage d isease that results in the deposit-
tion of iron-containing pigments in the peri pheral tissues with characteri stic
bronzing of the skin, diabetes and weakness.
3. Bilirubin is a product of heme degradation.
Saad Alqahtani, Twitter @saaddes
blood
0 blood type is referred to as:
• universal donor
• universal recipient
• neither of t he above
SAADDES
19
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• universa l donor
Type 0 people do not produce AB antigens. Therefore, type 0 people's blood normally will
not be rejected when it is g iven to others with d ifferent 0-A-B blood types. As a result, type 0
people are universal donors for transfusion s. AB blood type people do not make any AB
antibodies. The blood of AB type people does not discriminat e against any other 0 -A-B blood
type. Therefore, they are universal receivers for transfusions.
All humans and many other primat es can be typed by the 0 -A-B blood group. There are four
types: A, B, AB, and 0. There are two antigens and tw o antibodies that are mostly respon sible
for the 0-A-B blood types. The specific combination of these four components determines an
individual's blood type. The table below shows the possible permutat ions of antigens and
antibod ies with the correspond ing ABO types ("yes" indicates the presence of a com ponent,
SAADDES
and "no" indicates its absence in the blood of an ind ividual).
ABO Blood Type Antigen A Antigen B Antibody Antibody
Anti-A Anti-B
A Y es No No Yes
B No Y es Y es No
0 No No Y es Yes
AB Y es Y es No No
For instance, type A people have the A antigen on the surface of their red cells (as shown in t he
ta ble above). As a result, anti-A antibodies will not be produced because they would cause t he
destruction of their own blood. However, if B-type blood is injected into their systems, anti-S
antibod ies in the plasma will recognize the blood as alien and burst or agglutinate t he
introduced red cells in order t o cleanse the blood of alien protein.
Saad Alqahtani, Twitter @saaddes
blood
The most important feature of the hemoglobin molecule is its ability to
combine loosely and reversibly with oxygen.
Oxygen does not combine with the two positive bonds of the iron in the
hemoglobin molecule. Instead it binds loosely with one of the so-called
coordination bonds of the iron atom.
SAADDES
• both statements are true
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
20
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
The primary fu nction of hemoglobin (Hgb) in the body is to combine with oxygen in the lungs and
t hen to release this oxygen readily in the peripheral tissue capillaries, where the gaseous tension of
oxygen is much lower tha n in the lungs.
Hemoglobin is the oxygen-bearing protein of red blood cell s and exists in two conformational
states - tense (T) or relaxed (R). The T conformation has a weaker affinity for oxygen (e.g., in t he
capillaries), while the Rconformation has a stronger affinity for oxygen (e.g., in the lungs (150-300
fold increase over the T state)).
The combination of hemoglobin (Hb) with oxygen (02) is reversible, and whether Hb binds with or
releases 0 2 depends in large part on the oxygen partial pressure (Po2). When the Po 2, is
relatively high, (as in the pulmonary capillaries), Hb has a higher affinity for 0 2 and is 98%
SAADDES
saturated. At a lower Po2, (as in the tissue capillaries), Hb has a lower affinity for 0 2 and is only
pa rtially saturated.
Important: The oxyhemoglobin dissociation curve illustrates the relationship between Po 2 in t he
blood and the number of 0 2 molecules bound to Hgb. This curve can be shifted in numerous clinical
conditions either to the right or the left. The curve is shifted to t he right when the affinity of Hgb for
0 2 decreases, which enhances 0 2 dissociation. Thisresult s in decreased Hgb binding to 0 2 at a given
Po 2, thus increasing the P50 (which is t he point on the curve where 50% of Hgb issaturated with 0 2
and is 27 mm Hg in normal adults). When the affinity of Hgb for 0 2 increases, the curve is shifted to
t he left, which reduces the P50.1n this state, 0 2 dissociation and delivery to tissues are inhibited.
Factors that cause a shift of the oxyhemoglobin dissociation curve:
• Decrease in pH causes a shift to the right, conversely, an increase in pH shift s the curve to t he
left.
• All of the following cause a shift of the curve to the right:
l .lncreased hydrogen ions
2. Increased temperature
3. Increased BPG
4.1ncreased C02
Saad Alqahtani, Twitter @saaddes
100
90 18
Oxygenated blood
~
80 .. leaving the lungs ···-·-··- 16
~
--~-1--k---i --- '--4- -
c: 70 14
0
:;::
...::J
Ill
iii
60 1- - 12 ~
VI
VI 50 1 i 10 ~
SAADDES
1
t--
c:
:0 40 ·- -hi--/' - Reduced blood returning ! so>
:I
0
c,
0 30 6
E
Gl
l: 20 r ojmt"'"l ---1---- ----- 4
10 1 l ' 2
0
! ' ! 0
0 10 20 30 40 50 60 70 80 90 100 110 120 130 140
Pressure of oxygen in blood (Po2) (mm Hg)
Oxygen-hemoglobin dissociation curve
20-1
Saad Alqahtani, Twitter @saaddes
--g
100
'#. 90
80
~ 70
.a
CIS
60
~ 50
SAADDES
:g 40
g 30
~ 20
:I:
10
0~,-~~-r~~-,~~r-r-~~~~
0 10 20 30 40 50 60 70 80 90100110120130140
Pressure of oxygen in blood (P02) (mm Hg)
Shift of the oxygen-hemoglobin dissociation cun'e to the right caused by an increase in
hydrogen ion concentration (decrease in pH). BPG, 2,3 -biphosphoglycerate.
20A· I
Saad Alqahtani, Twitter @saaddes
blood
All of the following are common subunit hemoglobin chains EXCEPT one.
Which one is the EXCEPTION?
• alpha
• beta
SAADDES
• gamma
• delta
• epsilon
21
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• epsilon
A molecule of hemoglobin Is composed of the following:
1. Globin (protein) portion
• Consists of four polypeptid e chains- two alpha chains and two beta chains
• The normal adult globin portion of Hb consists of two alpha and two beta chains, and the
normal fetal globin portion of Hb consists of two alpha and two gamma chains
2. Four ring-shaped heme molecules (non-protein groups)
• Each heme is a nitrogen-containing organic pigment molecule that has a single atom of
iron in the reduced state (Fe''or ferrous iron) in its center, which can combine with one
SAADDES
molecule of oxygen. These heme groups are attached to the globin polypeptide cha ins.
Each iron atom can bind reversibly with one molecule of oxygen; therefore, a hemoglobin
molecule can potentially associate with four oxygen molecules. When it is combined with oxygen,
the compound is cal led oxyhemoglobin. When the hemoglobin molecule is not combined with
oxygen, the compound is ca lled deoxyhemoglobin (reduced hemoglobin).
1. Hemoglobin combines reversibly with carbon dioxide at the protein portion of the
hemoglobin molecule.
2. Carbon monoxide decreases the amount of oxygen that can be tra nsported by hemo-
globin by competing with oxygen for hemoglobin binding sites. Ca rbon monoxide has a
much higher affinity (240 x stronger) for hemoglobin tha n does oxygen.
3. As pH decreases, so does the affinity of hemoglobin for oxygen.
4. Methemoglobin conta ins iron in the ferric state (Fe,.) and cannot function as an oxy-
gen carrier.
5. Hemoglobin is a major H· buffer of the blood. Deoxygenated hemoglobin is less acidic
than oxygenated hemoglobin and therefore ideally suited to buffer the H' ions (coming
from tissue C02).
Saad Alqahtani, Twitter @saaddes
blood
The most common form of hemoglobin in the adult human being i s:
• hemoglobin H
• hemoglobin S
• hemoglobin M
SAADDES
• hemoglobin A
• hemoglobin C
22
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hemoglobin A
Hemoglobin H is an abnormal hemoglobin composed of four beta chains; it is
usually associated with a defect in three of the four alpha chain genes resulting in
alpha-thalassemia.
Hemoglobin S is an abnormal hemoglobin in which valine has replaced glutamic
acid in t he beta chain. The presence of hemoglobin S causes the red blood cell to
deform and assume a sickle shape when exposed to decreased amounts of oxygen
(such as might happen when someone exercises or in the peri pheral circulation).
Sickled red blood cells can bl ock small blood vessels, causing pain and impaired
SAADDES
circu lation, decrease the oxygen-carrying capacity of the red bl ood cel l and decrease
the cell's life span. HemoglobinS is the predominant form of hemoglobin in persons
with sickle-cell anemia. Important: A major effect of sickle cell anemia is the
decreased solubility of the deoxy fo rm of hemoglobin.
Hemoglobin M is a g roup of abnormal hemoglobins in wh ich a single amino acid
substitution favors the formation of methemoglobin and is thus associated w ith
methemoglobinemia.
Hemoglobin A is a combination of two alpha chains and two beta cha ins.
Hemoglobin Cis abnormal hemoglobin in wh ich lysine has replaced glutamic acid,
causing reduced plasticity of the red blood cells.
Saad Alqahtani, Twitter @saaddes
blood
In the normal person, about 90o/o of all erythropoietin is formed in the
- --'· the remainder is formed mainly in the _ __
• kidneys, liver
•liver, kidneys
SAADDES
· bone marrow, kidneys
· kidneys, bone marrow
23
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• kidneys, liver
Any cond ition that causes the quantity of oxygen transported to the tissues to decrease ord ina rily
increases the rate of red blood cell p roduction by the bone marrow. The principal stimulus for red blood
cell production in low oxygen states is a circulating hormone called erythropoietin, a glycoprotein.
Important: The p roduction of eryth ro poietin and thus erythrocytes, is regulated by a negative-feedback
mechanism that is sensitive to the amount of oxygen delivered to the tissues (particularly the kid neys).
~ 1. Inadequate erythropoiesis leads to anemia, increased cardiac output and hypoxia.
NotH 2. Anoxia (low oxygen) leads to greater production, while an increased oxygen supply leads to
decreased production. The site of action of this hormone appears to be at the hemocytoblast (a
pl uripotent stem cell).
3. Excessive erythropoiesis can lead to polycythemia, an increase in blood viscosit y and
sluggish blood flow.
SAADDES
4. Important: Anemic individuals have normal oxygen tension but reduced oxygen content in
t heir systemic arterial blood.
Characteristics of erythrocytes:
1. Biconcave d iscs, about 7.8 microns in d iameter, lack nuclei and mitochondria.
2. Contain hemoglobin and a large quantity of carbonic anhydrase which converts carbon d ioxide
and water to bicarbonate and proteins
3. Have a lipid membrane containing lipoproteins and specific blood g roup substances (A. B, 0 ).
4. The principal function is to transport hemoglobi n, which in turn carries oxygen from the lungs to
the tissues.
5. The proportion of erythrocytes in a sample of blood is called the hematocrit (46.2% for males and
40.6% for females is the normal range).
6. The amount of bile pigments excreted by the liver is a good ind ication of the amount of erythrocyte
destruction per day.
7. Ufe span of erythrocytes = 105 to 120 days.
Source of erythrocyte production:
• Early Embryo - yolk Sac
• Mid Gestation - mostly liver, but also spleen and lymph nodes
• Final Month of Gestation to about 20 yea rs o ld - exclusively in the bone marrow
• 20 years old and older- marrow of membranous bones, such as the vertebrae, sternum. ribs, and ilia
Saad Alqahtani, Twitter @saaddes
blood
Which ofthe following will shift the oxygen-hemoglobin dissociation curve to
the right?
Select all that apply.
• increased ca rbon dioxide concentration
SAADDES
• increased blood temperature
• increase in pH
• increased 2,3-biphosphoglycerate (BPG)
24
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• increased carbon dioxide concentration
• increased blood temperature
• increased 2,3-biphosphoglycerate (BPG)
The influences of pH, Pco 2, and temperature on the oxygen binding by hemoglobin (Hb)
operates to ensure adequate deliveries of oxygen to active tissues. When a muscle is actively
contracting, t he following events occur: lactic acid is produced (lowering the pH), C0 2 is
prod uced by the tissues (increasing Pco 2 and further decreasing pH through formation of
carbonic acid: H20 + C02 - H2C0 3 - H• + HC03t and heat is produced (thereby
increasing blood tem perature). Therefore, the by-products of exercise are also the exact
factors that stimulate 0 2 relea se from oxyhemoglobin .
SAADDES
Active tissues have the following characteristics:
• Lower pH
Note: Acidic conditions will decrease the affinity of Hb for 0 2. The higher the H+ ion
concentration (lower pH), t he less 0 2 is bound to Hb.
• Increased arterial Pco 2
Note: The partial pressure of carbon d ioxide (Pco2) affects t he binding of 0 2 to Hb
because carbon di oxide molecul es bin d with Hb molecul es and alter the Hb
conformation from the R state (high 0 2 affinity) to the T state (low 0 2 affinity). Therefore, t he
higher t he Pco 2, the less 0 2 is bound to Hb.
• Increased temperature
Note: The higher the temperature, t he less 0 2 is bound to Hb at any given Po 2.
• Increased 2,3-biphosphoglycerate (BPG)
Note: Hypoxia increases the formation of BPG, which also shifts the oxyhemoglobi n
d issociation curve to the right.
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
The substance intrinsic factor, essential for absorption of vitamin B12 in the
ileum, is secreted by the:
• ch ief cells
• parietal cells
SAADDES
• gastrin cells
• mucous cel ls
25
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• parietal cells
The lining of the stomach is covered with a columnar epithelium folded into gastric pits; each
pit is the opening of a duct into which one or more gastric gland s empty. The gastric mucosa
is divid ed into three distinct regions based on the structu re of the glands. The small cardiac
glandular region, located just below the lower esophageal sph incter (LES), primarily contains
mucus-secreting gland cells. The remainder of the gastric mucosa is divided into the oxyntic
or parietal (acid-secreting) gland region, located above the gastric notch (equivalent to t he
proximal part of th e stomach), and th e pyloric gland region, located below th e notch
(equivalent to the distal part of the stomach).
The stomach mucosa has two important types of tubular glands: oxyntic glands (also called gastric
gland s) and pyloric glands. The oxyntic glands secrete hydrochloric acid, pepsinogen, intrinsic fac-
tor, and mucus. The pyloric glands secrete mainly mucus but also the hormone gastrin.
SAADDES
An oxyntic gland is composed of th ree main types of cells: (1) mucous neck cells, which secret e
mainly mucus;(2) peptic (or chief) cells, which secrete large quantities of pepsinogen; and (3) pari-
etal (or oxyntic) cells, which secrete hydrochloric acid and intrinsic factor.
The pyloric glands are structurally similar to the oxyntic gland s, but contain few peptic cells and al-
most no parietal cells. Instead, they contain mostly mucous cells that are id entical with the mucous
neck cells of the oxynt ic glands. These cells secrete a small amount of pepsinogen, and a large
amount of thin mucus.The pyloric glands also contain Gcells (enteroendocrine cells) that secrete the
hormone gastrin.
Important:
1. Oxyntic gland salso contain enterochromaffin-like (ECL) cells which secrete histamine, and 0
cells, which secrete somatostatin.
2. Secretion of intrinsic factor is the only gastric function that is essential for human life.
3. Gast ric juice consists of inorganic and organic constituents together with water. The predomi-
nant organic constituent of gastric juice is pepsinogen, the inactive proenzyme of pepsin.
4. Parasympathetic innervation via the vagus nerve is the strongest stimulant of gastric H+ secre-
tion. In addition, vagal stimulation results in t he secretion of pepsinogen, mucus, HC0 3·, and
intrinsic factor.
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
All of the following slow gastric emptying EXCEPT one. Which one is the
EXCEPTION?
• gastri c inhibitory peptide
• activation of the sympathetic nervous system
SAADDES
• secretin
• activation of the enteric nervous system
• cholecystokinin
• activation of the parasympathetic nervous system
26
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• activation ofthe parasympathetic nervous system
Foodstuffs enterin g the duod enum, especially fats and acidic chym e, stimulate the
release of hormones, in cluding cholecystokinin, secretin, and gastric inhibitory
peptide (GIP), that inhibit the pyloric pump. Note: Stomach emptying is enhanced by
the presence of food in the stomach and gastrin.
The small intestine sends inhibitory signals to the stomach to slow secretion and
motili ty. Two types of sig nals are used: nervous and endocrine. Distension of the
small intestine, as well as chemical and osmotic irritation of the mucosa, is transduced
into gastric inhibitory impulses in the enteric nervous system. Th is nervous pathway
is called the enterogastric reflex. Secondly, enteric hormones such as cholecystokinin
and secretin are released from cells in the small intestine (specifically the duodenum) and
SAADDES
contribute to suppression of gastric activity.
Remember: In general, sympathetic stimulation causes inhibition of gastrointestinal
secretion and motor activity, and contraction of gastrointestinal sphincters and blood
vessels. Conversely, parasympathetic stimuli and acetylcholine typically stimulate
these digestive activities.
There are two major types of contractions in the Gl tract, peristalsis and mixing
(segmentation) contractions. Peristaltic contractions generate propu lsive movements. Mix-
ing contractions serve to spread out the food stuffs and increase the surface area available for
d igestion and absorption.
1. The principal function of the small intestine is to digest and absorb the nutrients
contained in a meal.
2. The presence of chyme in the duodenum retards additional gastric emptying.
3. Digestion and absorption in the small intestine are aided by two d igestive juices
derived from the pa ncreas (pancreatic j uice) and liver (bile). These secretions are trig-
gered by hormonal and neural signals activated by the presence of the meal in the
small intestine.
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
Three of the following signaling molecules are important in causing
pancreatic secretion. Which of the following is NOT one of them?
• cholecystokinin
• secretin
SAADDES
• acetylcholine
• epinephri ne
27
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• epinephrine
Three signaling molecules important for pancreatic secret ion:
1. Acetylcholine, is released from parasympathetic vagus nerve endings and from other cholin-
ergic nerves in the enteric nervous system.
2. Cholecystokinin, is secreted by the duodenal and upper jej unal mucosa when food enters the
small intestine.
3. Secretin, is also secreted by the duodenal and jejunal mucosa when highly acidic food enters
the small intestine.
The first two of the signaling molecules, acetylcholine and cholecystokinin, stimulate the acinar
cells of the pancreas, cau sing production of large quantities of pancreatic digestive enzymes but
relatively small quantities of water and electrolytes to go with the enzymes. Without the water, most
SAADDES
of the enzymes remain temporari ly stored in the acini and ducts until more fl uid secretion comes
along to wash them into the duodenum. Secretin, in contrast to the two other signaling molecules,
stimulates secretion of large quantities of water solution of sodium bicarbonate by the pan-
creatic ductal epithelium.
Pancreatic secretion s (daily secretion = 1.5 liters; with a pH bet ween 7.5 and 8.8) from pancreatic
acinar cells include enzymes involved in protein breakdown (trypsin, chymotrypsin, and
ca rboxypeptid ase), carbohydrate breakdown (amylase), and fat breakdown (lipase, cholesterol
esterase, phospholipase). Pancreatic enzymes are secreted in an inactive form called a zymogen,
and are then activated in the small intesti ne. Note: Pancreatic duct cells secrete a fluid that is high
in bicarbonate ion. Quantitatively, the pancreas is the largest contributor to the supply of
bicarbonate ion s needed to neutralize the gastric acid load.
1. The secretions of the exocrine gastric glands, composed of the mucous, parietal,
8 and ch ief cells, make up the gastric juice (daily secretion 2-3 liters; with a pH bet ween
1.0 and 3.0). Gastric secretions include HCI. mucous, pepsinogen, and intrinsic factor.
2. Intestinal secretions (daily secretion unknown with a pH between 6.5 and 7.8),
mainly mucou s, are secreted by goblet cells and enterocytes.
3. Bile (pH around 7.8) is produced by the liver and stored in the gallbladder. Bile aids
in the emulsification, digestion and absorption of fats.
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
Your patient comes in and says that his physician has diagnosed him with per-
nicious anemia. As you know, this is caused by the malabsorption of vitamin
812.
1. What protein is crucial in the absorption of vitamin B12?
• gastrin
SAADDES
• intrinsic fact or
• pepsin
2. What cell is res ponsible for the faulty glycoprotein impli cated in pernicious anemia?
• ch ief cell s
• parietal cell s
• mucous neck cell s
•gcells
3. What type of glands w ithin the stomach contain these cells?
• pyloric glands
• gastric glands
• cardiac glands
• none of the above 28
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. intrinsicfactor
2. parietal ce lls
3. gastric glands
The stomach mucosa has two important types of t ubul ar glands: oxyntic glands (also called
gastric glands) and pyloric glands. The oxyntic glands secrete hydrochloric acid, pepsino-
gen, intrinsic facto r and mucous. The pyloric glands secrete mainly mucous but also the
hormone gastrin.
An oxyntic gland is composed ofthree main types of cell s: (1) mucous neck cells, which se-
crete mainly mucou s;(2) peptic (or chief) cells, wh ich secrete large quantities of pepsino-
gen; and (3) parietal (or oxyntic) cells, which secrete hydrochloric acid and intrin sic
factor.
SAADDES
The pyloric glands are struct urally similar to the oxyntic glands, but contain few pepti c
cells and almost no parietal cells. Instead, they contain mostly mucous cells that are iden-
tical w ith the mucous neck cell s of t he oxyntic glands. These cells secrete a small amount
of pepsinogen and a large amount ofthin mucou s. The pyloric glands also contain G cells
(enteroendocrine cell s) that secrete the hormone gastrin.
Functions of secretions:
• Hydrochloric acid- p roduces an acid environment t hat helps to kill bact eria and to
activate pepsin. Th is solu bil izes connective t issue. Secretion is increased by
acetylcholine, gastrin and histamine.
• Pepsin- proteolytic enzyme secreted in an inactive form (pepsinogen) and converted
by stomach acidity or by autocatalysis to pepsin. It is activated rat her t han inhibited by
low pH.
• Mucous- viscous and alkaline, produces a barrier along t he wall s of t he stomach to
p rotect the stomach from the acid and from abrasion.
• Intrinsic factor - a glycoprotein that is essential for normal absorpti on of vitamin B12
in the intestine. Without intrinsic factor, pernicious anemia w ill develop.
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
Distension of the intestine by chyme and parasympathetic neural activity
_ _ _ the contractile force, while sympathetic neural activity it.
• decrease, increases
• increase, decreases
SAADDES
• have no effect on, increases
• none of the above
29
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• incre ase, de creases
Coordinated contractions of smooth muscle, ca lled segmentation, are controlled by
neural, mechanical, and hormonal factors. Segmentation facil itates digestion and
absorption in the small intestine in several ways:
• Foodstuffs are mixed w ith digestive enzymes from the pancreas and bile salts
from the biliary system
• Nutri ent molecules in the lumen are constantly dispersed, allowing them to
contact the epithelium, where enzymatic digestion is completed and absorption
occurs
• Chyme is moved down the d igestive tube, making way for the next load and
SAADDES
eliminating undigestible, perhaps toxic, substances
Following a meal, when the lumen of the small intestine contains chyme, two types
of motility predominate: segmentation contractions chop, mix, and roll the, chyme
and peristalsis slowly propels the chyme toward the large intestine.
1. Chyme is the semiflu id contents of the stomach consisting of partially
digested food and gastric secretions.
2. Gastric emptying is fastest when its contents are isotonic. The following
gastric contents delay gastric emptying:
1. Hypertonic or hypotonic contents
2. Fat (by stimulating cholecystokinin __. causes receptive relaxation)
3. H· in the duodenum (stimulates neural reflexes to stomach)
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
Which of the following pairings regarding the absorption in the small
intestine is INCORRECT?
• fructose - - facilitated diffusion
• free fatty acids - - simple diffusion
SAADDES
• dipeptides - - primary active transport
• glucose - - secondary active transport
30
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• dipeptides - - primary active transport
*** Dipeptides are absorbed by secondary active transport.
The bulk of dietary lipid is neutral fat or triglyceride, composed of a glycerol
backbone with each carbon linked to a fatty acid. Additionally, most foodstuffs
contain phospholipids, sterols like cholesterol and many minor lipids, including
fat-soluble vitamins. In order for the triglyceri de to be absorbed, two processes
must occur:
•large aggregates of dietary triglyceride, which are virtually insoluble in an aque-
ous environment, must be broken down physically and held in suspension (a proc-
ess called emulsification)
SAADDES
• Triglyceride molecules must be enzymatically digested to yield monoglycerides
and free fatty acids, both of which can efficiently diffuse into the enterocyte
*** The key players in these two t ransformations are bile salts and pancreatic
lipase, both of which are mixed with chyme and act in the lumen of the small
intestine.
Dipeptides and amino acids are t he end products of protein digestion. The final
digestive stage occurs by brush border peptidases and absorption immediately
follows. Absorption across the brush border occurs by multiple secondary active
transporters utilizing either sodium-dependent cotransport (amino acids) or
hydrogen-dependent cotransport (di- and tri -peptides).
Disaccharides and small glucose polymers are hydrolyzed at the brush border by
lactase, sucrase, maltase and alpha-dextrinase. The resultant monosaccharides
(glucose and galactose) are then absorbed by secondary active transporters driven by
the sodium gradient. Fructose absorption is mediated by facilitated diffusion.
Saad Alqahtani, Twitter @saaddes
gastrointestinal system
Place the following phases of gastric secretion in their proper order:
• intestinal phase
• gastric phase
• cephalic phase
SAADDES
31
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. cephalic phase
2. gastric phase
3. intestinal phase
Phases of Gastric Secretion:
• Cephalic phase ("wake up call"): sensations of thoughts about food are relayed to
the brainstem where parasympathetic signals to the gastric mucosa are initiated.
This d irectly stimulates gastri c juice secretion and stimulates the release of gastrin,
which prolongs and enhances the effect.
• Gastric phase ("full steam ahead"): the presence of food, specificall y the d isten-
sion food t riggers local and parasympathetic nervous reflexes that increase these-
SAADDES
cretion of gastri c juice and gastrin (which fu rther amplifies gastric juice secretion).
Products of protein digestion can also tri gger the gastrin mechanism.
• Intestinal phase ("step on the brakes"): as food moves into the duodenum, the
presence of fats, carbohydrates and acid stimulates hormonal and nervous reflexes
that inhibit stomach activity.
Saad Alqahtani, Twitter @saaddes
muscles
As an action potential reaches a skeletal muscle cell, what is the order of
activation by which the signal is transmitted internally through the muscle
cell so that contraction results?
• acetylcholine, ca lcium, troponin, tropomyosin, myosin heads
SAADDES
• calcium, acetylcholine, troponin, tropomyosin, myosin heads
• acetylcholine, ca lcium, tropomyosin, t roponin, myosin heads
• calcium, acetylcholine, tropomyosin, t roponin, myosin heads
32
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• acet ylcholine, calcium, troponin, tropomyosin, myosin head s
When an action potential arrives at a muscle cell, the action potential causes Ca'• to be
released from the sarcoplasmi c reticulum. As intracellul ar Ca>< is increased, Ca'• begins to
bind to troponin C on the thin filaments, causing a conformational change in troponin
that permits the interaction between actin and myosin.
After calcium b inds with troponin, tropomyosin moves from its b locking position,
permitting actin and myosin to interact. In the first stage of the cross-bridge cycle, myosin
is bound t ightly to actin. As ATP binds myosin, the myosin-actin bond is broken, and the
myosin head is cocked toward the plus end of actin (away from theM-line [the center of
the sarcomere)). Next, an inorganic phosphate (Pi) group is hydrolyzed from ATP in the
SAADDES
myosin-ATP complex (myosin-ATP __. myosin-ADP + Pi), at wh ich time the myosin-ADP
complex rebinds actin at a new site further from the M -li ne. After the myosin-ADP
complex b inds to actin, ADP is released from the actin -myosin-ADP complex, causing a
conformational rebound in the "cocked" myosin to return to its original posit ion, pulling
the actin filament toward the M-line thereby causing the muscle fiber to shorten
(contract). This process is called the Sliding Filament Theory.
Note: This process is repeated as long as calcium ions are bound to troponin and ATP is
available. Once calciu m ions are returned to the sarcoplasmic reticulum, tropomyosin
moves back into its b locking position and prevents further interaction between high-
energy myosin and actin subunits. Contraction ceases and the muscle fi bers relax.
Important: In the contractile cycle, the dissociation of the actin-myosin complex results
from ATP binding to the myosin head (actin -myosin + ATP __. actin+ myosin-ATP).
Remember: Composition of myofilaments
• Thick filament - co mposed mainly of the protein myosin
• Thin filaments- composed mainly of the protein actin
Saad Alqahtani, Twitter @saaddes
I A I
~
1111111 1111111 1111111 1111111
1111111
1111111 II IIIII 1111111 1111111
I I IIIII
1111111 1111111 1111111 1111111
1111111
1111111 1111111 1111111 111111 I
1111111
Relaxed
SAADDES
Relaxed and contracted slates of a myollbril s howing (top) sliding of the actin fi laments (thinner) into
the spaces between the mysosin filaments (thicker), and (bottom) pulling of the Z membranes toward
each other.
Saad Alqahtani, Twitter @saaddes
Head
A
~
SAADDES Cross-bridges Hinges
Mysoin filament
Body
A, Myosin molecule. B, Combination of many myosin mole-
cules to form a myosin fi lament. Also shown are thousands of
myosin cross-bridges and interaction between the heads of the
cross-bridges with adjacent actin filaments.
~~ F-aciin Tropomyosin
Actin fi lament, composed of two helical strands of F-actin molecules and two strands 32A-I
of tropomyosin molecules that fit in the grooves between the actin strands. Anached to
one end of each tropomyosin molecule is a troponin complex that initiates contraction.
Saad Alqahtani, Twitter @saaddes
muscles
The immediate source of energy for muscle contraction is ATP binding to
myosin. The ATP pool, however, is extremely small and has three sources
of replenishment. Which of the following is NOT a source?
• creatine phosphate
SAADDES
• lactic acid
• glycogen
• cellular respiration
33
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• lactic acid
The hydrol ysis of ATP (adenosine tri phosphate) provides the immediate source of
energy for muscle contraction. Although a muscle fiber conta ins only enough ATP to
power a few twitches, its ATP "pool" is replenished as needed. The three sources of
high-energy phosphate to keep the ATP"pool"filled are creatine phosphate, g lycogen
and cellula r respiration in the m itochondri a of the muscle fibers.
Creatine phosphate - the phosphate group in creatine phosphate is attached by a
"high-energy" bond like that in ATP. Creatine phosphate deri ves its high-energy phos-
phate from ATP and can donate the phosphate back to ADP to form ATP.
SAADDES
Note: Creatine phosphate + ADP ~ creatine + ATP. The pool of creatine
phosphate in the fiber is about 10 times larger than that of ATP and thus serves as a
modest reservoir of ATP.
Glycogen - skeletal muscle fibers conta in about 1% glycogen. The muscl e fiber can
degrade th is glycogen by g lycogenolysis, producing glucose-1-phosphate. This
enters the glycolytic pathway to yield two molecules of ATP for each pair of lactic acid
molecules produced. Not much, but enough to keep the muscle functioning if it fails
to receive sufficient oxygen to meet its ATP needs by respiration. However, this
source is lim ited, and eventually the muscle must depend on cellular respiration .
Cellular respiration - cellular respiration not only is required to meet the ATP needs
of a muscle engaged in prolonged activity (thus causing more rapid and deeper
breathing), but is also required afterwards to enable the body to resynthesize glyco-
gen from the lactic acid produced earli er (deep breathing continues for a time after
exercise is stopped). Note: The body must repay its oxygen debt.
Saad Alqahtani, Twitter @saaddes
muscles
As you complete the seating of a crown, you ask your patient to tap lightly on
the articulating paper. Which of the following statements correctly describes
the physiology responsible for a patient's light tapping on the articulating
paper?
• the "all or nothing" phenomenon occurs; all fibers in the masseter and medial
pterygoid are partially stimulated, causing a light contraction
SAADDES
• fractionation occurs; each muscle fiber involved is stimulated only by a fraction of
the alpha-motor neurons innervating the fiber, and so the fibers contract lightly
• fractionation occurs; only a few small alpha-motor units are recruited, and the mas-
seter and medial pterygoid muscles contract lightly
• the"al l or nothing" phenomenon occurs; the muscles that close the mouth are stimu-
lated ful ly but are countered by stimulation of the muscles that open the mouth,
causing a slight closing of the mouth
34
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• fractionation occurs; only a few small alpha-motor units are recruited,
and th e ma sseter and medial pteryg oid mu scles contract lightl y
Th e motor unit is t he alpha-mot or neuron and all of the muscle fibers t hat it innervat es:
• Each muscle is composed of several muscle fibers
• Each muscle fiber is innervated by a single alpha-motor neuron
• Each alpha-mot or neuron innervates many muscle fibers
• All of the fibers innervat ed by a motor neuron contract when that motor neuron fires
an action potenti al
Remember: The Size Principle - motor unit s are recruited in order of t he size of the motor
unit. If only a small amount of t ension is required to perform t he movement, then only small
SAADDES
motor units will be activated. If greater force is required, more and larger motor units will be
recruited. Important: When a patient bites down rapid ly on an unexpect ed hard surface
wh ile chewing, the cessation of mot or unit recruitment in the jaw closing muscles is caused
by periodontal mechanoreceptors. Fractionation means that it is not necessary to
activate all of the motor unit s in a muscle.
The contraction of skelet al muscle is controlled by t he nervous system. Action pot entials
t raveling down somati c alpha mot or neurons cause depolarization of the skeletal muscle
fibers at which they terminate. The juncti on between t he terminal of a motor neuron and a
muscle f iber is called a neuromuscular junction. When an action potential arrives at a
neuromuscular j unction, calcium ions enter the nerve terminal, causing the release of
acetylcholine from synaptic vesicles w ithin t he motor neuron. Acetylcholine then binds to
t he nicot inic cholinergic recept ors in the muscle fiber plasma membrane. This causes
depolarization, which triggers an action pot ential (the action potenti al travels along the
membrane and the t-tubules). This action potential triggers t he release of calcium ions from
t he sarcoplasmic reticulum. This leads to crossbridge formation between actin and myosin.
These interactions are responsible for the development of t ension and t he short ening of t he
fibers.
Saad Alqahtani, Twitter @saaddes
muscles
All of the follow ing statements comparing fast and slow-twitch muscle fibers
are true EXCEPT one. Which one is the EXCEPTION?
• fast-twitch fibers are about twice as large in diameter than slow-twitch muscle fibers
• slow-twitch fibers have a g reater resistance to fatigue than fast-twitch muscle fibers
SAADDES
• the enzymes of oxidative phosphorylation are considerably more active in slow-
twitch fibers than in fast-twitch fibers
• fast-twitch fibers contain more mitochondria and myoglobin than slow-twitch
muscle fibers
• fast-twitch fi bers can deliver extreme amounts of power for a few seconds to a
minute versus slow-twitch fibers
35
copyright C 2011·2014 Dental Deets
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• fast-twitch fibers contain more mitochondria and myoglobin
than slow-twitch muscle fibers
*** This is false; (see chart below}
( haractcristics of Skeletal \lusclc Fibers
Characte rist ic Slow Twitch (Type I) Fast 1\vitcb (Type II)
Myosin-ATPase activity Low High
Speed/I ntensity of contraction Slow/Low Fast/High
Resistance to fatigue High Low
SAADDES
Oxidative capacity Hig h Low
Enzymes for a naerobic glycolysis Low High
Mitochondria Many Few
Sarcoplasmic retic ulum Less extensive More extensive
Capillaries Many Few
Myoglobin content High Low
Glycogen content Low High
1. "Fast" muscles are for rapid, powerful actions (jumping, short distance
Notes runn ing) while "slow" muscles are for prolonged activity (body postu re, running
a marathon).
2. Oxidative capacity is related to (1) the number of capillaries, (2) the
myoglobin content, (3) the number of mitochondria.
Saad Alqahtani, Twitter @saaddes
muscles
All of the following statements concerning muscle spindles are true
EXCEPT one. Which one is the EXCEPTION?
• they are found within the belly of muscles
• they consist of small, encapsulated intrafusal fibers and run in parallel with the
main muscle fibers (extrafusal fibers)
muscle
SAADDES
• the finer the movement required, the smaller the number of muscle spindles in a
• they detect both static and dynamic changes in muscle length
36
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the finer the movement required, the smaller the number
of muscle spindles in a muscle
***This is false; the finer the movement required, the greater the number of muscle
spindles in a muscle.
Muscle tone is "fine-tuned" by t wo sensory organs:
1. Muscle spindle (measures muscl e length) has three components:
1. Specialized muscle fibers: (intrafusal fibers)
2. Sensory terminals: g roup Ia and II afferents
3. Motor terminals: gamma motor (efferent) neurons
SAADDES
*** Activates alpha motor neuron when stretched.
2. Golgi tendon organ (measures muscle tension): innervated by a single-group lb
sensory (afferent) fiber.
*** Inhibits alpha motor neuron.
1.The muscle spindle is a small, highly differentiated part of muscle tissue
8 located w ithin the belly of muscles and runs parallel w ith t he main muscle
fibers.
2.The annulospiral endings (sensory term inals) are wrapped around spec-
ialized muscle fibers that belong to the muscle spindle (intrafusal fibers)
and are quite separate from the fibers that make up the bulk of the muscle
(extrafusal fibers).
3. Motor (efferent) neurons can be fu rther classified as alpha or gamma
motor neurons. Alpha motor neurons innervate and stimulate skeletal mus-
cle. Gamma motor neurons innervate the muscl e spindle.
4. Activation of the gamma motor neuron maintains the spindle sensitivity.
Saad Alqahtani, Twitter @saaddes
muscles
When a muscle is , the _ _ _ reflex reacts. This reflex is consid-
ered _ _ _ , and the result is _ __
• contracted/ golgi tendon/ monosynaptic/contraction
• stretched/golgi tendon/ disynaptic/ relaxation
SAADDES
• stretched/ stretch/ monosynaptic/contraction
• contracted/ stretch/disynaptic/relaxation
• stretched/ stretch/ monosynaptic/ relaxation
37
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• stretched /stretch /monosynaptic/contraction
The stretch reflex, also known as the myotatic reflex, responds to passive stretching of
the muscle. The muscle stretch is detected by muscle spindles whose afferents (1a
fibers) synapse with lower motor neurons (alpha-motor neurons) and interneurons
(1a inhibitory interneurons). The reflex is important for the automatic maintenance of
posture and muscle tone. When the muscle is stretched, so is the muscle spindle. The
muscle spindle depolarizes in response to stretching (senses the change in length)
and sends action potentials to the spinal cord where it synapses w ith a motor neuron.
This triggers the stretch reflex, causing the muscle to contract. The basic function of
the muscle spindle is to convey information to the centra l nervous system
concern ing muscle length and tension. Important: The sensory receptors serving the
SAADDES
stretch reflex are classified as proprioceptors.
Reflex Number of Stimulus Afferent R esponse
Syn apses Fibers
Stretch reflex Monosynaptic Muscle is Ia Contraction o f the muscle
(knee j erk) stretched
GoJgi tendon reflex Disynaptic Muscle contracts lb RcJa.xation o f the muscle
(clasp knife)
Flcxor·withdrawal Polysynaptic Pain 11, Ill, and Ipsilateral flexion, contralatcraJ
reflex (atler touch · IV extension
ing a hot stove)
1. The Golgi tendon reflex is the reverse of the stretch reflex. Golgi tendon
organs also depolarize in response to muscle stretch but inhibit the motor
neuron, causing the muscle to relax.
2. The flexor-withdrawal reflex is a polysynaptic reflex that is used when a
person touches a hot object or steps on a needle.
Saad Alqahtani, Twitter @saaddes
muscles
Most reflex arcs have:
• th ree basic elements
• fou r basic elements
• five basic elements
SAADDES
• six basic elements
38
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• six basic elements
The reflex arc is a simple neural pathway connecting receptors to an effector. A
receptor detects a stimulus or environmental change. An effector is an organ of
response (i.e., skeletal muscl e). It produces a response called a reflex. Reflexes are
quick because they involve few neurons. Reflexes are either somatic (resulting in
contraction of skeletal muscle) or autonomic (activation of smooth and ca rdiac
muscle). Most reflex arcs have six basic elements: a receptor, sensory (afferent)
neuron, integration center (CNS), interneuron, motor (efferent) neuron, and effector.
Spinal reflexes are somatic reflexes mediated by the spinal cord. Two important
SAADDES
spinal reflexes influence the contraction of skeletal muscles. These are:
1. Stretch reflex - it is initiated at receptors called muscle spindles that are
sensitive to muscle length and tension. This reflex stimulates the stretched
muscle to contract. An example is the patellar reflex (knee jerk reflex), in wh ich
the striking of the patellar tendon at the knee causes the quadriceps muscles to
contract and swing the lower leg forward.
2. Tendon reflex - it is initiated at recepto rs called neurotendinous organ s
(Golgi tendon o rgans) that are sensitive to tension that occurs as a result of
muscular contraction. This reflex stimulates the contracted muscl e to relax.
Note: When the stretch reflex stimulates the stretched muscle to contract, antag-
onistic muscles that oppose the contraction are inhibited. This occurrence is cal led
reciprocal inhibition and the neuronal mechanism that causes this reciprocal
relationship is ca lled reciprocal innervation.
Saad Alqahtani, Twitter @saaddes
muscles
In a single muscle, there are both intrafusal and extrafusal fibers. All of the
following statements are true in the description of intrafusal fibers EXCEPT
one. Which one is the EXCEPTION?
• contain nucl ear bag fibers that detect fast, dynamic changes
SAADDES
• innervated by gamma-motor neurons
• contain nuclear linking fibers that transmit afferent signals
• encapsulated in sheaths to form muscle spindles
• contain nuclear cha in fibers that detect static changes
39
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• contain nuclear linking fibers that transmit afferent signals
Two Types of Muscle Fibers:
1. Extrafusal Fibers
• Fibers that make up the bulk of the muscle
• Innervated by alpha-motor neurons (efferent neurons)
• Provide t he force for muscle contraction
2. lntrafusal Fibers
• Are encapsulated in sheaths to form muscle spindles
• Innervated by gamma-motor neurons (efferent neurons)
SAADDES
Two Types of lntrafusal Fibers:
1. Nuclear bag fibers
• Detect fast, dynamic changes in muscle length and tension
• Innervated by group Ia afferents - fastest in the body
2. Nuclear chain fibers
• Detect static changes in muscle length and tension
• Innervated by the slower group II afferents as well as the group Ia
afferents
Remember:
1. A sensory (afferent) neuron transm its afferent nerve impulses from the recept-
or (peripheral ending of a sensory neuron) to the spinal cord.
2. A motor (efferent) neuron transm its efferent nerve impulses from the integrat-
ing center (in the spinal cord) to an effector (muscle cell).
Saad Alqahtani, Twitter @saaddes
central nervous system
Within the spinal cord, the H-shaped mass of gray matter is divided into
horns, which consist mainly of neuron cell bodies. Cell bodies in the
posterior (dorsal) horn relay:
• voluntary motor impulses
SAADDES
• reflex motor impulses
• sensory impulses
• all of the above
40
[refer to AS card 211 -1for illustration]
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• sensory impulses
*** Those cell bodies in the anterior (ventral) horn transmit motor impulses.
The white matter surrounding these horns consists of myelinated nerve fibers, wh ich
form the ascending and descending tracts. A tract represents a group of axons w ithin
the central nervous system having the same origin, termination and function; it is often
named for its origin and termination (e.g., spinothalamic tract).
Axons of cells that run on the same side as their cell bodies of origin are referred to as
ipsilateral. Axons of cells that run on the opposite side of their cell bodies of origin are
referred to as contralateral.
SAADDES
Note: Sensory pathways are ascending systems (e.g., spinothalamic and DC-ML systems);
motor pathways are descending systems (e.g., pyramidal and extrapyramidal systems).
Remember: The white matter refers to those parts of the brain and spinal cord that are
responsible for communication between the various gray matter regions and between
the gray matter and the rest of the body. In essence, the gray matter is where the
processing is done and the white matter is the channels of communication. By analogy,
the gray matter is like the CPU in a computer, and the white matter is like t he p rinted
circuit board that connects it to the other parts of the computer.
White Matter vs. Gray Matter (both the spinal cord and the brain consist of):
• White Matter = bundles of axons each coated with a sheath of myelin
• Gray Matter = masses of the cell bodies and dendrites, each covered w ith
synapses
In the spinal cord, the white matter is at the surface, and the gray matter inside. In the
brain of mammal s, th is pattern is reversed.
Saad Alqahtani, Twitter @saaddes
central nervous system
Which of the following structures plays a role by associating with the
corticospinal system to control complex patterns of motor activity?
• hypothalamus
• hippocampus
SAADDES
• basal ganglia
• thalamus
41
[refer to AS card 197 B-1, 204-1for illustration I copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• basal ganglia
Collections of nerve cells (nuclei) lie at the base of the cerebrum (subcortical) in structures called
the:
• Basal ganglia -like the cerebellum, constitutes anot her accessory motor system that functions
usually not by itself but in close association with the cerebral cortex and corticospinal motor
system. ln fact, the basal ganglia receives most of its input signals from the cerebral cortex itself
and also returns almost all of its output signals back to the cortex. On each side of the brain, these
ganglia consist of the striatum (caud ate nucleus and putamen), globus pallid us, substantia nigra
and the subthalamic nucleus. They are located mainly lateral to and surrounding the thalamus.
The function of the basal ganglia is to control complex patterns of motor activity.
Note: An example is t he writing of letters of the alphabet When there is serious damage to
the basal ganglia, the cortical system of motor control can no longer provide these patterns.
SAADDES
Instead one's writing becomes crude.
Important: The basal ganglia are a group of anatomically closely related subcortical nuclei. Damage
to these nuclei does not cause weakness, but can cause dramatic motor abnormalities. Clinical
syndromes associated with damage to these nuclei include Parkinson's disease and Huntington's dis-
ease (Huntington's chorea).
• Thalamus -a large ovoid collection of nuclei (gray matter) that relays all sensory stimuli
(except olfactory) as they ascend to the cerebral cortex. Output from the cortex also can synapse
in the thalamus. General functions include sensory and motor relay to the cerebral cortex,
regulation of cort ical activation and visual input. Key point: The thalamus is a distribution
center that controls activity in specific regions of the cerebral cortex.
• Hypothalamus - controls many homeostatic processes, which are often associated with the
autonomic nervous system. The hypothalamus is involved in regulating body temperature, water
balance, appetite, gastrointestinal activity, sexual activity, sleep and even emotions such as fear
and rage. The hypothalamus also regulates the release of the hormones of the pituitary gland;
and thu s the hypothalamus greatly affects the endocrine system. Important: Sti mulation of the
posterior hypothalamus by a reduction in core temperature will produce shivering.
• Hippocampus - functions in the consolidation of memories and in learning.
Saad Alqahtani, Twitter @saaddes
central nervous system
The main structures of the hindbrain include which of the following?
Select all that apply.
• medulla oblongata
• pons
SAADDES
• cerebral hemispheres
• cerebellum
42
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• medulla oblongata
• pons
• cerebellum
The human forebrain (prosencephalon) is made up of:
• A pair of cerebral hemispheres called the telencephalon
• A group of structures located deep within the cerebrum t hat make up the diencephalon (com-
posed of the epithalamus, dorsal thalamus and hypothalamus; it forms the central core of the
brain)
Main Structures of the Hindbrain (rhombencephalon):
• Cerebellum- is the large brain mass lying posterior to t he ponsand medulla and inferior to the
posterior part of the cerebrum. The cerebellum's functions include motor coordination, motor
SAADDES
learning and equilibrium.
• Pons - connects the cerebellum with the cerebrum and links the midbrain to the medulla
oblongata. CN V is associated with the pons. General funct ions includ e: respiratory/uri nary
control, control of eye movement and facial sensation/motor control.
• Medulla oblongata- the medulla looks like a swollen tip to the spinal cord. General funct ions
include: cardiovascular and respiratory control, auditory and vestibular input and brainstem
reflexes. CN IX, X, and XII are associated with the medulla, whereas CN VI-VIII are associat ed with
the j unction of pons and medulla.
Note: The neurons controlling breathing have mu (!J) receptors, the receptors to which opiates,
like heroin, bind. This accounts for the suppressive effect of opiates on breath ing.
The brain stem lies immediately inferior to the cerebrum, j ust anterior to the cerebellum. The brain
stem consists of the midbrain, pons and medulla oblongata. The midbrain (mesencephalon)
connects dorsally with the cerebellum and contains large voluntary motor nerve tracts.
The limbic system is a pri mitive brain area deep within the temporal lobe. Besides initiating basic
drives (hunger, aggression, emotional feelings and sexual arousal), the limbic system screensall
sensory messages traveling to the cerebral cortex.
Saad Alqahtani, Twitter @saaddes
central nervous system
For each of the following patient complaints, match the most appro-
priate lobe of the cerebrum that may not be functioning properly.
Patient's complaints are: A. Frontal lobe
l. I always Jorgct if I bmshcd my teeth already. B. Temporal lobe
I just cannot remember if I a lready d id so I just assume I d id.
a
C. Occipital lobe
SAADDES
2. I ... ummm ... j ust cannot make my wrist move the bmsh ... um D. Parietal lobe
... but ... and ... why do I need ... to brush my teeth'!
3. Every time I grasp my brush, it won't fit in my mouth.
It also hurts to have the water on my teeth.
4. I brush every day, but I have trouble getting toothpaste on
my brush. I have no trouble. getting my brush to my mouth,
but I just cannot manage to sec the toothpaste and the brush.
43
[refer to AS card 197-1, 197 C-1for illustration]
copyright Cl 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. B (Temporal lobe) -this patient will also have trouble hearing you respond
2. A (Frontal lobe) -motor trouble and trouble with language expression
3. D (Parietal lobe)- sensations
4. C (Occipital lobe)- patient has vision troubles -tell him or her to put toothpaste
directly on his/her teeth and use the brush as normal
The cerebrum (cerebral cortex), the largest region of the brain, occupies t he superior
portion of the cranial cavity. The cerebrum con sists of right and left hem ispheres. The
right hemisphere controls the left side of the body; the left hemisphere control s the right side.
The corpus callosum is a mass of nerve fibers connecting the hemispheres. Each cerebral
hemisphere is divided into four lobes, based on anatomical landmarks and functional differ-
ences. The lobes are named for the cranial bones that overlie them.
SAADDES
Note: In addition to the functions of the primary areas in each lobe, the vast majority of the
cerebral cortex is involved in associative and higher order functioning such as ideation, lang-
uage, and thought.
Lobes of the Cerebrum
Frontal Contains the primary motor (movement) area and infl uences
personal ity, judgment, abstract reasoning, social behavi or and
language expression.
Temporal Controls hearing, language comprehens ion, storage and recall
of memories.
Parietal Interprets and integrates sensations of: pain, temperature and
touch - particular! y in regards to size, shape, distance and
texture; impOitant for awareness of body shape.
Occipital Functions mainly to interpret v isual sti muli.
Saad Alqahtani, Twitter @saaddes
Parietal Lobe
Frontal Lobe
Occipital
Lobe
SAADDES Temporal
Lobe
Medulla Oblongata
Spinal Cord
197-1
Lobes of the Brain - Lateral view
Saad Alqahtani, Twitter @saaddes
PARIETAL LOBE
intelligE>.,ce
behaviour
language
Intelligence
reading
memory
sensation
movement
SAADDES
TEMPORAL LOBE
beh· I!LJr CEREBELLUM
h anng balance
poeeh coor dination
VISiOn
mt ry
BRAIN STEH
bloCid pre ou-- P
brcathmg
consciOusness
heartbeat
swallowing 197 C-1
Saad Alqahtani, Twitter @saaddes
circulatory system
For the following questions, use the same answer choices.
1. Which of the following has the thickest layer of muscle?
2. Which of the following is the major regulator of blood flow?
3. Which of the following contain valves?
4. Which of the following are large vessels that contain deoxygenated
blood? Is there an EXCEPTION to this rule?
5. Which has higher compliance, veins or arteries?
• veins
• arteries
SAADDES
• capillaries
• arterioles
• venu les
44
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. arteries
2. arterioles
3. veins
4. veins- EXCEPTION - (pulmonary veins carry oxygenated blood and
pulmonary arteries carry deoxygenated blood )
5. veins have higher compliance and arteries have a lower compliance
Systemic arteries - transport oxygenated blood under high pressure away from the heart to
tissues of the body. These arteries have strong muscular walls to withstand the high pressure
and low compliance.
Note: The pulmonary and umbilical arteries are the on ly arteries that contain deoxygenated
blood.
SAADDES
Systemic veins -function as conduits for the tra nsport of deoxygenated blood from the
tissues back to the heart. These veins have larger lumens and thinner walls than the arteries
the veins accompa ny but a higher compliance and act as volume reservoirs. Some contain
valves (especially the veins of the limbs) that allow blood to flow toward the heart but not
away from it.
Note: The pulmonary and umbilical veins are the only veins that contain oxygenated blood.
Capillaries - this is where the exchange of fluid, nutrients and metabolic waste products
occurs between the blood and t he interstitial spaces. The capillary walls are very thin. They
consist of a single layer of endothelial cells surrounded by a thin basal lamina of the tunica
intima.
Note: The amount of blood that flows th rough the capillaries per minute is equal to the
amount of blood that flows through the aorta per minute.
Arterioles - regulate the flow of blood into capillaries. Blood flow is regulated to meet tissue
metabolic needs.
Venules- are very small veins that collect blood from the capillaries; venules gradually coalesce
into progressively larger veins.
Saad Alqahtani, Twitter @saaddes
Pulmonary Circulation
Left
Pulmonary
veins
Lobar arteries
to right lung -"tilio'IJ'Ifii~~~l::~L.-±::;:;;1?
Superior
vena cava
Pulmonary_-'~=~~. .~~~
SAADDES
veins
Right
atrium
~~~:icle 1"'~:-+,1/--1-;fl--lt-JHP-'Hr-1:-
lnferior
vena cava
• Oxygenated blood
• Unoxygenated blood
Pulmonary circulation showing the pulmonary trunk dividing into right and left pul-
monary arteries, which in turn divide into lobar arteries.
44-1
Rcproduc~d with pcrmis..-.ion from Spcacx AI', Mason EB: Httma11 AntiiMIJ' Ond Phy.tinlogJ~ ed 4; St Paul. 1992. Wesl Publit>lung Company.
Saad Alqahtani, Twitter @saaddes
circulatory system
Which structures are the site of highest resistance in the cardiovascular
system?
• veins
• arteries
• arterioles
• venules
SAADDES
When these structures are acted on by nitric oxide or adenosine, they will:
• constrict
• d il ate
• stay the sam e
This will affect total peripheral resistance in what way?
• increase
• decrease
• stay the sam e
45
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. arterioles
2. dilate
3. decrease
Arterioles are the last small branches of the arterial system and act as control valves
through which b lood is released into the capillaries. Arterioles vary in diameter ranging
from 30 ~~ m to 400 ~~ m. Any artery smaller than 0.5 mm in diameter is considered to be an
arteriole.
They have a sma ll lumen and a relatively thick tunica media that is composed almost
entirely of smooth muscle, w ith very little elastic tissue. The intima of an arteriole is
composed of endothelial cells lying on a basement membrane w ith an underlying fine
SAADDES
internal elastic lamina in the larger arterioles.
Arterioles p lay a major role in regulating the flow of b lood into the capillaries. Blood flow
to tissue is mainly regulated by arteriolar diameter. Constriction of the arterioles restricts
the flow of blood into the capillaries, while dilation allows the blood to enter the
capillaries more freely. Important: Arterioles are the primary resistance vessels and
determine the distribution of cardiac output. Arteriolar res istance is regulated by the
autonomic nervous system. Remember: Alpha 1-adrenerg ic receptors are found on the
arterioles of the skin and splanchnic circulations. BetaTadrenergic receptors are found on
arterioles of skeletal muscle. Beta 1-adrenergic receptors are found primarily in the heart
muscle and kidneys. Beta b lockers are comm only p rescribed for their antihypertensive
effects.
Local blood flow is regulated by t issue metabolism. Various humoral factors can also
affect arteriolar diameter, including endothelins (vasoconstrictor), nitric oxide and
adenosine (vasodilators). Sympathetic activation results in an overall vasoconstriction of
arterioles and an increase in total peripheral resistance (TPR).
Key Point: An increase in arteriolar resistance will increase TPR.
Saad Alqahtani, Twitter @saaddes
circulatory system
For the following questions, use the same answer choices.
1. Which circuit supplies the alveoli of the lungs?
2. Which circuit supplies the connective tissue of the lungs?
3. Which has a lower blood pressure?
4. Which has a greater volume of blood flow per minute?
5. Which circuit involves the thick-walled left ventricle?
SAADDES
• pulmonary circuit
• systemic circuit
• both
• neither
46
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. pulmonary circuit
2. systemic circuit
3. pulmonary circuit
4. neither (they have the same, about 5 L/ min)
5. systemic circuit
The vessels of the circulatory system can be divided into two separate circuits, each of which
leaves and return s to the heart. The pump for the pulmonary circuit, which circulates blood
through the lungs, is the right ventricle. The left ventricle is the pump for the systemic circuit,
which provid es the blood supply for the tissue cells of the body.
1. Pulmonary ci rcu it - pulmonary circulation tra nsports oxygen-poor blood from the
rig ht ventricle to the lungs where blood picks up a new blood supply. Then the pulmonary
circulation returns the oxygen-rich blood to the left atriu m. Note: The vessels of this circuit
SAADDES
supply only the alveoli.
2. Systemic circuit - the systemic circulation provides t he functional blood supply to all
body tissue. The systemic circulation ca rries oxygen and nutrients to the cell s and picks
up carbon dioxid e and waste products. Systemic circulat ion carries oxygenated blood from
the left ventricle, through the arteries, to the capillaries in the tissues of t he body. From t he
t issue capillaries, the deoxygenated blood returns through a system of veins to the right
atriu m of the heart.
Note: The vessels of this circuit transport blood to all tissues of the body except the alveoli of
the lungs.
Note: The volume of blood flow per minute (5 L/min) is the same in both circuits.
Remember:
1. Mean arterial blood pressure = Cardiac output x Total peripheral resistance
2. Vascular compliance = Increase in Volume /Increase in pressure
3. Blood pressure in the pu lmonary circuit is much lower than that of the systemic circu lation,
because pu lmonary arterioles are usually dilated and have little resistance to blood flow. The
pulmonary vessels are highly compliant, allowing the pulmonary circuit to store blood volume
without changing blood pressure.
Saad Alqahtani, Twitter @saaddes
Blood C irculation
Lung
capillaries
Pulmonary
circuit
Left
atrium
Right Left
ventricle ventricle
SAADDES
Hepatic
portal
system
Systemic capillary
46-1
beds
The right heart chambers propel blood into the pulmonary circuit (dashed arrows), and
the left heart chambers propel blood into the systemic circuit (solid arrows).
Rcproduc~d with pcnn is..-.ion from Spcae< AP, Mason EB: HmtlliJI Anammyand Phy:tin!Og)~ ed 4; St Paul. 19<)2. Wc:sl Publislung Company.
Saad Alqahtani, Twitter @saaddes
circulatory system
Your patient tells you that he just had a heart bypass operation. He says that
they used a vein from his leg and re-routed blood that previously flowed
through his left anterior descending coronary artery (often referred to as the
widow maker). Which of the following explanations is correct in answering
how a vein can adequately replace an artery?
SAADDES
• although veins have higher compliance norm ally, when under high pressure, compliance
decreases and so t he vein acts very simil ar to an artery when put in these conditions
• although veins have lower co mp li ance normally, when under the high pressure, compli-
ance increases and so the vein acts very similar to an artery when put in these conditions
• although veins have higher resistance norm ally, when under the high pressure, resistance
decreases and so t he vein act s very simil ar to an artery when put in t hese conditions
• although veins have lower resistance norm ally, when under high pressu re, resistance in-
creases and so the vein acts very similar to an artery when put in these conditions
47
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• although veins have higher compliance normally, when under high
pressure, compliance decreases and so the vein acts very similar to
an artery when put in these conditions
Total peripheral resistance (TPR) regulates the flow of b lood from the systemic arterial
circulation into the venous circulation. Cardiac output regulates the flow of blood from
the veins back into the arterial side. The amount of blood located in the systemic veins is
reg ulated by their compliance. Sympathetic activation decreases venous compliance and
returns more b lood back to the heart, increasing cardiac output and blood pressure, thus
causing more blood to be pushed t hrough the arterial circulation.
The ability of a b lood vessel wall to expand and contract passively with changes in
SAADDES
pressure constitutes an important functi on of large arteries and veins. Th is ability of a
vessel to distend wit h increasing trans mu ral pressure (inside minus outside pressure ) is
quantified as vessel compliance (C), which is the change in volum e (DV) divided by the
change in pressure (DP).
Important points about compliance: (1) Compliance decreases at higher pressures and
volu mes (i.e., vessels become "stiffer" at higher p ressures and volum es); (2) At lower
p ressures, the compliance of a vein is about 10 to 20 t im es greater than that of an artery.
Therefore, veins can accommodate large changes in b lood volum e w ith on ly a small
change in pressure. However, at higher pressures and volum es, venous compliance
becomes similar to arterial compliance. This makes veins suitable for use as arterial by-
pass grafts.
Re lative volumes of blood at rest in different parts of the adult cardiovascular
system:
• 66% - in the systemic veins, venules • 6%- in the heart
• 11 % - in the systemic arteries, arterioles • 5%- in the capillaries
• 12% - in the pulmonary loop
Saad Alqahtani, Twitter @saaddes
circulatory system
Your patient presents with stage 1 hypertension. His blood pressure is
1 SO mmHg/99 mmHg, confirming his diagnosis.
l. ls his pulse pressure norm al, high, or low?
2. To bring his b lood p ressure down to norm al, he coul d attempt to do what to the total
SAADDES
peripheral resistance?
• increase it
• decrease it
3. Norm ally, the mean pressure in the aorta is about 100 mmHg. Eventually, the blood w ill
return via the vena cava at a pressure of 4 mmHg. Where did the blood pressure decrease
the most as b lood traveled through the body?
• large veins
• large arteries
• arterioles
• venules
• capillaries
48
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
l.high
2. decrease it
3. arterioles- the site of highest resistance
Although capillaries have a smaller diameter than arteri oles, there are vastly more
capillaries arranged in parallel than there are arterioles. Thus, most of the pressure
drop in the systemic circu lation occurs in the arterioles.
Pressure decreases as blood moves through the systemic ci rcu lation. This pressure
gradient is required for blood flow.
Remember: blood flow= pressure gradient/resistance
SAADDES
The resistance to the flow of blood offered by the entire systemic circu lation is
ca lled the total peripheral resistance (TPR).
The target systolic blood pressure is 120 mmHg and the recommended diastolic
blood pressure is 80 mmHg. However, as blood enters arterioles the pressure can
drop to as low as 30 mmHg.
The pulse pressure equals the systolic pressure minus the diastolic pressure (Pulse
pressure = SBP-DBP). The most important determinant of pulse pressure is stroke
volume.
1. The pressure is highest in the aorta and lowest in the venae cavae.
2. Mean pressure is as follows: in the aorta _ . 100 mmHg; at the end of
the arterioles - . 30 mmHg; and in the vena cava - . 4 mmHg.
Saad Alqahtani, Twitter @saaddes
circulatory system
There are two general causes of extracellular fluid edema:
(1) abnormal leakage of fluid from the plasma to the interstitial spaces
across the capillaries, and (2) failure of the lymphatics to return fluid from
the interstitium back into the blood.
The most common clinical cause of interstitial fluid accumulation is
excessive capillary fluid filtration.
SAADDES
• both statements are true
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
49
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Edema refers to the presence of excess fluid in the body tissues. In most instances, edema occurs
mainly in the extracellular fluid compa rtment, but it can involve intracell ular fluid as well.
Two conditions are especially prone to cause intracellular swelling: (1) depression of the metabolic sys-
tems of the tissues, and (2) lack of adequate nutrition to the cells. Note: Intracellular edema can also
occur in inflamed tissues. Inflammation usually has a direct effect on the cell membranes to increase
their permeability, allowing sodium and other ions to diffuse into the interior of the cell, with subse-
quent osmosis of water into the cells.
Ext racellular fluid edema occurs when there is excess fluid accumulation in the extracellular
spaces. There are two general causes of extracellularfluid edema: (1) abnormal leakage of fluid from
t he plasma to the interstitial spaces across the capillaries, and (2) failure of the lymphatics to return
fluid from the interstitium back into the blood. The most common clinical cause of interstitial fluid ac-
SAADDES
cumulation is excessive capillary fluid filtration.
Any one of the following cha nges can increase the capillary filtration rate:
• Increased capillary filtration coefficient
• Increased capillary hydrostatic pressure
• Decreased plasma colloid osmotic pressure
Important:Two major forces influence fluid movement between capillaries and interstitial fluid: Hy-
drostatic Pressure and Colloid Osmotic Pressure (Oncotic Pressu re). Increased hydrostat ic pres-
sure pushes fluid out of a system, while increased colloid osmotic pressure draws fluid into a system.
Netfluid movement between the capillary and interstitial fluid can be determined by the following
equation: Net Pressure= [Pc - Pi] - [nc- nil
P= Hydrostatic Pressure; n= Colloid Osmotic Pressure; c= capillary; i= interstitial fluid
A positive Net Pressure number means filtration (fluid moves out of capillaries) will occur; while a
negative Net Pressure number indicates absorption (fluid moves into capillaries) will take place.
Generally, hydrostatic pressure is higher in the capillaries than the interstitial fluid, so hydrostatic
pressure tends to favor filtration . On the other hand, colloid osmotic pressure usually favors ab-
sorption because the colloid osmot ic pressure isalso higher in the capillaries (remember: higher col-
loid osmotic pressure draws fluid into a system!).
Saad Alqahtani, Twitter @saaddes
circulatory system
Your patient has just finished her 2-hour appointment and is eager to get
out of the office. She stands up from the chair very fast, and quickly becomes
dizzy and nearly faints. This is termed orthostatic hypotension.
1. Wh ich of the following receptors a re most important in the short-term regul ation of her
blood p ressure and returning it to normal?
• stretch receptors in the carotid sinus
SAADDES
• chemoreceptors in the aortic bodies
• chemoreceptors in the carotid bod ies
• stretch receptors in the p ulm onary circul ation
2. This d rop in blood pressure will cause what to happen?
• sympathetic impulses to increase
• parasympathetic impulses to increase
• both to increase
• neither to increase
3. The effect on the heart will be:
• increased heart rate, decreased stroke volume
• increased heart rate, increased stroke vo lu me
• decreased heart rate, decreased stroke vo lum e
50
• decreased heart rate, increased stroke volume copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. stretch receptors in the carotid sinus
2. sympathetic impulses to increase
3. increased heart rate, increased stroke volume
The baroreceptor regulatory system is composed of two groups of stretch receptors: (1) one
group in the carotid sinuses near the bifurcations of the common carotid arteries in the neck,
and (2) a second group in the arch of the aorta. These receptors detect changes in blood
pressure and feed the information back to the cardiac control center and the vasomotor center
in t he medulla. In response, these control centers alter the ratio between sympathetic and
parasympathetic output. If t he pressure is too high, a dominance of parasympathetic impulses
will reduce the pressure by slowing the heart rate, red ucing stroke volume and dilating blood
"reservoir" vessels. If the pressure is too low, a dominance of sympathetic impulses will
SAADDES
increase the pressure by increasing the heart rate, stroke volume and constricting "reservoir"
vessels.
Stretch receptors in the carotid sinus are stimulated by elevated blood pressu re,
resulting in the activation of the para sympathetic nervous system and inhibition of the
sympathetic nervous system to reduce blood pressure back toward its set point.
Chemoreceptors in the carotid and aortic bod ies, as well as chemoreceptive neurons in the
vasomotor center of the medulla itself, detect increases in carbon dioxide, decreases in blood
oxygen and decreases in pH (which is really an increase in hydrogen ion concentration). This
information feeds back to the cardiac control center and vasomotor control center of the
medulla, which in t urn, alters the ratio of parasympathetic and sympathetic output. When
oxygen drops, carbon dioxide increases, and/or pH drops, a dominance of sympathetic
impulses increases heart rate and stroke volume and constricts "reservoir" vessels, in response.
Stretch receptors in t he atria and pulmonary circul ations are stimulated by an
expansion of blood volume. They DO NOT directly respond to changes in systemic
arterial blood pressure.
Saad Alqahtani, Twitter @saaddes
circulatory system
It's 4 o'clock on a Friday afternoon, and you are about to do a quick preparation and
restoration. When you give the injection, the patient complains of severe discomfort. You
realize you forgot to aspirate the needle first, and you have just injected into an artery.
1. Your needle passed through the artery layers in which order?
• tunica adventitia, tunica media, tunica intima
• tunica media, tunica intima, tunica adventitia
• tunica intima, t unica media, tunica adventitia
• tunica adventitia, tunica intima, tunica media
SAADDES
2. Judging by their relative thicknesses, which is the toughest vessel to puncture?
• artery
• vein
• capillary
3. Which layer is thicker: tunica media or t unica adventitia?
4. Which layer is innervated by the autonomic nervous system?
• tunica intima
• tunica media
• tunica adventitia
5. By puncturing this artery, you have hit the vessel with the greatest:
• resistance
• pressure
• cross-sectional area
51
• blood volume
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. tunica advent itia, tunica media, tunica int ima
2. artery
3. tunica media
4. tunica media
5. pressure
Type of Vessel Tunica Intima Tunica Media Tunica Adventitia
(Endothelium) (Smooth :\'luscle; (Fibrous Connective T issue)
Elastic Connective Tis.-.ue)
Arteries Smooth lining Allows constriction and dilation of Provides flexi ble support rhat
vessels: thicker than in veins; resists collapse or i 1~ury;
muscle innervated by autonomic th icker than in veins; thinner
SAADDES
fi bers than nmic-.a media
Veins Smooth lining with Allows constriction and dilation of Provides flexi ble support that
semilunar valves to vessels; thinner than in arterie..'i; resists collapse or inj ury;
ensure one.way flow muscle innervated by autonomic more prominent than tunic-.a
fi bers media
Capillaries Makes up entire wall of Absent Absent
capillary; thinness
pennits ease of transport
across vessel wall
Properties of Vessels
Arteries Largest pressure
Arterioles Largest resistance
Capillaries Largest cross-sectional area
Veins Largest blood volume
Saad Alqahtani, Twitter @saaddes
dna/rna
In your practice, you see quite a few HIV/AIDS patients. These patients have a
virus that has the unique ability to:
• produce(+) ssRNA from a(- ) ssRNA molecule
• produce(- ) ssRNA from a(+) ssRNA molecule
SAADDES
• produce DNA from an mRNA molecule
• produce dsRNA from an ssRNA molecule
52
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• produce DNA from an mRNA molecule
***Using the enzyme "reverse transcriptase"
Reverse transcriptase is a DNA polymerase that uses RNA as its template. Thus, the
enzyme is able to make genetic information flow in the reverse (RNA ~ DNA) of its
normal d irection (DNA ~RNA).
Certain RNA viruses conta in w ithin the viral particle a unique RNA-directed DNA
polymerase that is ca lled reverse transcriptase. On infection, the single-stranded
RNA viral genome and t he enzyme enter t he host and the reverse transcriptase
catalyzes the synthesis of a DNA strand complementary to the viral RNA .
SAADDES
Reverse t ranscriptase enzymes are found naturally in certa in vi ruses cal led
retroviruses. These are viruses in which the genetic information is carried on an RNA
molecule. When one of these viruses infects a host cell, it uses this enzyme to make a
complementary DNA (eDNA) copy of its genetic information, which is then
incorporated into the host DNA.
1. The human immunodeficiency vi rus (HIV), the causative agent of AIDS, is
a retrovirus .
2. The d rug AZT (a thymidine analog) is a competitive inhibitor of the HIV
reverse transcri ptase. The w ild-type reverse transcri ptase seems to have a
high affinity for AZT and other base analogs.
3. Reverse transcriptase is one of the enzymes used in genetic engineering,
in which t he enzyme can be used to obtain a copy of a particular gene from
the relevant mRNA.
Saad Alqahtani, Twitter @saaddes
dna/rna
Ribosomes are surrounded by a membrane and form a separate cellular com-
partment.
In bacteria, they are either free-floating in the cytoplasm or attached to the
plasma membrane, and in eukaryotes they are either free floating in the cy-
toplasm or bound to the membrane of the endoplasmic reticulum.
SAADDES
• both statements are true
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
53
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false. the second is true
Although they enjoy the prestigious status of organelles, ribosomes are not surrounded by
a membrane and do not form a separate cellular compartment. They are simply large, cat-
alytically active, ribonucleoprotein particles.
Important: Ribosomes are the protein-synthesizing machines of the ceii.They translate
the information encoded in messenger RNA (mRNA) into a polypeptide.
In bacteria, they are either free -fl oating in the cytoplasm or attached to the plasma mem-
brane. In eukaryotes they are either free floating in the cytoplasm or bound to the mem-
brane of the endoplasmic reticulum (called rough endoplasmic reticulum [RER)).
SAADDES
At a ribosome, amino acids are linked together in the order specified by mRNA to form a
polypeptide or protein (this process is ca lled protein synthesis or translation). Ribosomes
have enzymatic activity. They catalyze the formation of peptide bonds, which link amino
acids to one another. Many ribosomes in different stages of translation can be attached to
a single mRNA strand (call ed a polyribosome), thus multiplying its effect. Proteins formed
by ribosomes attached to the RER are destined for secretion from the cell, incorporation
into the plasma membrane or formation of lysosomes. Since all protein synthesis begins on
free ribosomes, attachment of a ribosome to the ER requires the presence of a specific se-
quence at the amino end of the growing protein chain to signal the attachment of the ri-
bosome to the ER.
1. The 70s ribosomes are the sites of protein synthesis (translation) in bacterial
8 cells and chloroplasts and are composed of two rRNA subun its (30s & 50s) and 55
proteins.
2. The 80s ribosomes are the sites of protein synthesis (translation) in the cyto-
p lasm of eukaryotic cell s and are composed of two rRNA subunits (40s & 60s) and
84 proteins.
Saad Alqahtani, Twitter @saaddes
dna/rna
Genetic recombination experiments depend heavily upon the action of
which enzymes?
Select all that apply.
• dna ligases
SAADDES
• alkaline phosphatase
• creatine kinase
• restriction endonucl ease
54
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• dna ligases
• restriction endonucleases
The nuclea se is used to cleave both the DNA to be cloned and a plasmid DNA. The specificity
of the nuclease is such that, when mixed, the DNA to be cloned and the plasmid DNA will
anneal (base pair) and can then be joined together by a DNA ligase.
Southern blotting is a technique that can be used to detect mutations in DNA and can also
identify DNA restriction fragments. It combines the use of restriction enzymes and DNA
probes.
Advances in this technology (DNA cloning) are revolutionizing many aspects of medicine,
agriculture and other industries. Commercial products of recombinant DNA technology
SAADDES
include human insulin (for diabetes}, anticoagulants (tissue plasminogen factor},
erythropoietin (for anemia) and human growth hormone (for dwarfism}.
1. The first organism used for DNA cloning was E. coli, and it is still the most common
host cell. Bacterial cloning vectors include plasmids, bacteriophages and cosmids.
2. Some other enzymes that are used in recombinant DNA technology (gene
cloning) are:
• DNA polymerase I -fills in t he gaps in duplexes by step-wise addition of nucleo-
tides to 3' -end
• Reverse transcriptase - makes a DNA copy of an RNA molecule
• Exonucleases - remove nucl eotides from 3'- or 5'-end of DNA depending on
the specific exonuclease
3. A nuclease is an enzyme that cleaves phosphodiest er bonds in a nucleic acid.
DNases cleave DNA, and RNases cleave RNA. Nucleases that cleave internal phospho-
diester bonds are called endonucleases, and t hose t hat cleave bond s at t he 5' end or
3' end are called exonucleases.
Saad Alqahtani, Twitter @saaddes
dna/rna
All of the follow ing statements are true EXCEPT one. Which one is the
EXCEPTION?
• the replication of DNA involves some RNA intermediates
• the replication of DNA involves DNA ligase linking DNA molecules together
SAADDES
• the replication of DNA requires unzipping of the DNA molecule
• the replication of DNA involves the building of the new ssDNA strand from 3' to 5'
55
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the replication of DNA involves the building of the new ssDNA strand from 3' to 5'
***RNA intermediates are involved to prime the DNA polymerase and then are later re-
placed by DNA.
Replication is the process of completely duplicating the DNA within a cell. The
primary enzyme in this process is DNA polymerase, which reads a single strand of
DNA from the 3'-end toward the 5'-end whi le forming the new, complementary,
continuous strand from the 5'-end toward its 3'-end. As the DNA polymerase complex
moves along the DNA molecule, the original complementary strand (lagging strand)
is also duplicated. The DNA polymerase that is moving along the lagging strand from
SAADDES
the 5'-end towa rd the 3'-end thus cannot form a continuous copy of the lagging
strand. Instead, the DNA polymerase fo rms approximately 1,000 to 5,000 base long
multiple segments (Okazaki fragments), wh ich are joined together by DNA ligase to
form a continuous strand.
DNA polymerase can only add nucl eotides to a pre-existing piece of nucl eic acid
(primer). Duri ng replication, the primer is provided by RNA polymerase. The short
10-base segments created by RNA polymerase are removed, once the DNA has been
added to it, by an exonuclease; and the gap in the sequence is filled in by a DNA
polymerase. Important point: RNA polymerase synthesizes RNA primer chains fo r
DNA polymerase and does not require a primer cha in.
Note: Topoisomerases are responsible for unwinding supercoiled DNA to allow DNA
polymerase access to replicate the genetic code. The enzyme DNA gyrase re-forms
the supercoiled structure once the repl ication fo rk has passed.
Saad Alqahtani, Twitter @saaddes
dna/rna
Which of the following enzymes is NOT involved in unwinding, unzipping
and rezipping the DNA molecule during replication?
• topoisomerases
• helicases
SAADDES
• gyrases
• polymerases
56
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• polymerases
*** Polymerases are used in replication itself.
Helicases unwind the helix. Topoisomerases are responsible for unwinding super-
coiled DNA so as to allow DNA polymerase access to replicate the genetic code. The
enzyme DNA gyrase re-forms the supercoiled structure once the replication fo rk has
passed.
1. Ribose and uracil are the only d ifferences between the products of RNA
and DNA hydrolysis.
SAADDES
2. DNA is double-stranded; RNA is single-stranded.
3. Replication forks are sites at which DNA synthesis (replication) occurs.
4. The hydrolysis of DNA (deoxyribonu cl eic acid) will yield:
• Phosphoric acid
• Deoxyribose (sugar)
• Nitrogenous base (adenine, guanine, thymine, and cytosine)
5. The hydrolysis of RNA (ri bonucleic acid) w ill yield:
• Phosphoric acid
• Ribose (sugar)
• Nitrogenous bases (adenine, guanine, uracil, and cytosine)
Saad Alqahtani, Twitter @saaddes
dna/rna
Which of the following is contained in a nucleoside?
Select all that apply.
• nitrogen base
• phosphate
SAADDES
• ribose/deoxyribose sugar
• serine
• nitrate
57
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• nitrogen base
• ribose/deoxyribose sug ar
Note: A nucleotide also contains the phosphate.
A single base-sugar-phosphate unit is called a nucleotide. Without the phosphate group,
the molecule is called a nucleoside. These individual nucleotides are linked together to
form a polynucleotide chain (the link or bond is between a phosphate group of one
nucleotide and the sugar of the next and is called a phosphodiester bond).
If the polynucleotide chain contains the sugar ribose, the chain is called ribonucleic acid
(RNA); if the polynucleotide chain contains the sugar deoxyribose, the chain is called
deoxyribonucleic acid (DNA).
SAADDES
Nucleic acid s store and transmit information to synthesize the polypeptides and proteins
present in the body's cells. Nucleic acids are complex molecules composed of structures
known as nitrogenous bases (purines and pyrimidines), five-carbon sugars (pentoses)
and phosphate groups (which conta in phosphorus and oxygen).
Important: The backbone of nucleic acid s is made up of alternating phosphate and
pentose units, w ith a p urine or pyrimidine base attached to each.
Remember: The catabolism of a nucleotide (sing le base -sugar-phosphate unit) results in
no energy production in the form of ATP (as opposed to the catabolism of a lipid,
protein, or carbohydrate, wh ich do).
Hum ans obtain nearly all of their purines and pyrimidines from endogenous synthesis
rather than from the diet. Ribonucleotides are synthesized first, and are the precursors of
the corresponding 2-deoxyribonucleotides. Purine nucleotides are catabolized to free bases
first, and are then either oxidized to the excretory product uric acid or recycled to the cor-
respond ing nucleotides in PRPP-dependent salvage reactions. Uric acid is poorly so luble in
water. Therefore, it can cause kidney stones, and it causes gout when it forms crystals of
sodium urate in the gout j oints.
Saad Alqahtani, Twitter @saaddes
dna/rna
Which of the following are the same in RNA and DNA molecules?
• the purines
• the pyri midines
• both the purines and pyrimidines
SAADDES
• neither the puri nes and pyrimidines
58
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the purines
***The purines (A and G) are the same.
In DNA, the pyrimidine bases are thymine (T) and cytosine (C). In RNA, the pyrimidine
bases are uracil (U) and cytosine (C).
***The phrase "CUT down the pyramid s" may help you remember that cytosine, uracil,
and t hymine are all pyrimi dines.
Remember: The backbone of the DNA molecule consists of the deoxyriboses linked by
phosphodiester b ridges (i.e., the 3'-0H group of the sugar of one is linked to the 5'-0H of
the next sugar by a phosphate). The va riable part of the DNA is the sequence of the bases
SAADDES
and the p recise sequence of the purine and pyrimid ine bases carry the geneti c
information to express t he characteristics of the organism.
After t he form ation of the DNA molecule, there is a polarity with the 5'-0H group at one end
of the helical structure and the 3'-0H group at the other end. The base sequence is written
in t he 5' ..... 3' direction. A resulting spiral double helical structure results.
1. Purine ba ses t hat are cons umed in the human diet in the form of DNA or
RNA are mostly excreted in t he form of uric acid. Xanthine oxidase catalyzes this
formation of uric acid from p urine bases.
2. The use of tetrahydrofolic acid (TFA) by several of the enzymes in purine and
pyrimid ine synt hesis has made TFA metabolism a prime target for a number of
antimetabolites, such as methotrexate, used in cancer chemotherapy.
3. Ultraviolet light produces pyrimidine dim ers in DNA, which interfere w ith
replication and transcription. These lesions are removed via the acti on of an
endonuclease, an enzyme that excises a 12 bp (base pair) fragment surrounding
the dim er. Then DNA polymerase I fill s in the gap and DNA ligase seals the
seams.
Saad Alqahtani, Twitter @saaddes
dna/rna
Which of the following RNA mutations is least likely to have a significant
effect on the product protein?
• the elimination of the th ird nucleotide of a codon
• the elimination of the first nucleotide of a codon
SAADDES
• a substitution of the third nucleotide of a codon
• a substitution of the first nucleotide of a codon
59
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• a substitution of the third nucleotide of a codon
*** Due to the "wobble" effect.
Degeneracy of the genetic code: There are 64 d ifferent triplet codons and only 20 amino
acids. Unless some am ino acids are specified by more than one codon (sometimes referred to
as a triplet), some codons would be com pletely meaningless. Therefore, some redundancy is
built into the system: some am ino acids are coded for by multiple codons. In some cases, t he
red undant codons are related to each other by sequence; for example, leucine is specified by
the codons CU U, CUA, CUC, and CUG. Note how the codons are the same except for the
third nucleotide position (at the 3'-end). This third position is known as the "wobble"
position of t he codon. This is because in a number of cases, the ident ity ofthe base at the third
position can wobble and the same amino acid will still be specified. This property allows some
SAADDES
protection against mutation __. if a mutation occurs at the third position of a codon, there is
a good chance t hat the amino acid specified in t he encoded protein won't change.
Important: Only tryptophan, methionine, and selenocysteine are coded by just one codon.
The other 17 amino acids are coded by two or more. Codon s that specify the same amino acid
are called synonyms.
Several of the codons serve special functions:
1. Initiation codon (AUG) - signals the beginning of polypeptide chains and codes for
methionine: thus all proteins begin with methionine.
2. Termination codons (UAA, UAG, and UGA)- signal the end of polypeptide chain synthe-
sis. These codons are also referred to as stop codons or nonsense codons.
1. An anticodon is a specific sequence of three nucleotides in a transfer RNA,
8 complementary to a codon for an amino acid in a messenger RNA.
2. Remember: The two RNAs (tRNA and mRNA) are paired antiparallel - the first
base of the codon (always reading in the 5'- 3' d irection) pairing with t he third base
of the anticodon. For example, if the anticodon on a transfer RNA is 5' ACG 3; then its
corresponding codon on the messenger RNA would be 5' CG U 3'.
Saad Alqahtani, Twitter @saaddes
dna/rna
A sequence of DNA reads "A-T-T-G-C-A:' How many hydrogen bonds would you
expect to see holding this sequence to its complementary strand?
·12
·14
SAADDES
·16
·18
60
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• 14 (2 in each A-T pairing and 3 in each G-C pairing)
The t wo antiparallel pol ynucleotide chains of double-helical DNA are not identical
in either base sequence or composition. Instead, they are complementary to each
other. Wherever adenine appears in one chain, thymine is found in the other; sim ilarly,
wherever guanine is found in one chain, cytosine is found in the other.
Important point: Separated DNA strands are able to reassociate because DNA
strands are complementary.
Note: Watson and Crick deduced this specificity of ba se pairing because of stearic
and hydrogen-bonding facto rs.
SAADDES
In the Watson-Crick structure, the two cha ins or strands of the heli x are antiparallel,
such that one strand runs 5' to 3' ("five prime to three pri me") wh ile the other runs 3'
to 5'.
The DNA double helix is held together by two sets of forces: hydrogen bonding
between complementary base pairs and base-stacking interactions facili tated by
phosphodiester bonds.
The helix structure results in a major and a m inor g roove being formed along the DNA
molecule. The major groove is the binding region for many proteins that control the
transcri ptional activity of the DNA molecule.
Important: Three hydrogen bonds can form between G and C, but only two can
form between A and T. The weaker bonding between A and T (or U in RNA) is used in
transcri ption to aid in the release of the newly formed RNA from the DNA template.
Saad Alqahtani, Twitter @saaddes
dna/rna
A sequence of DNA is " T-A-G-T-A-T-C-A-T". What would the complementary
RNA sequence be?
• A-T-C-A-T-A-G-T-A
• A-U-C-A-U-A-G-U-A
SAADDES
• U-T-C-U-T-U-G-T-U
• A-G-C-A-U-A-G-T-U
61
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• A-U-C-A-U-A-G-U-A
A complete DNA molecule consists of two polynucleotide chains that run in
opposite directions to one another.
The two strands of DNA form a double helix that runs antiparallel such that one
strand runs S'to 3' ("five prime to three prime") while the other one runs 3' to 5~
The purine and pyrimidine bases that are opposite one another (adenine w ith
thym ine and guanine with cytosine) in each polynucleotide chain are linked together
by hydrogen bonds. The A-T base pair has two hydrogen bonds wh ile the G-C base
pair has three. This base pairing (A w ith T and G with C) is known as complementary
SAADDES
base pairing.
Remember: This complementary base pairing can also occur in RNA and between
RNA and DNA; however, uracil substitutes for thymine in RNA. Uracil base pairs w ith
adenine.
Important point: The A-T base pair promotes helix stabilization in DNA but does
not do so in RNA.
l .ln all DNA, the number of thymine residues equals the number of adenine
residues. Also, the number of guanine residues equals the number of
cytosine residues.
2. Puri nes are the larger of the two types of bases found in DNA.
3. In addition, the sum of purine residues equals the sum of pyrimidine
residues (A + G = T + C).
4. The melting temperature of the double helix is a function of the base
composition with a higher GC content having a higher melting temperature.
Saad Alqahtani, Twitter @saaddes
dna/rna
All of the following statements concerning the backbone of DNA are true
EXCEPT one. Which one is the EXCEPTION?
• it is constant th roughout the molecule
• it consists of deoxyriboses linked by "phosphodiester bri dges" or "phosphodiester
bonds"
SAADDES
• it is hydrophobic
• it is highly polar
62
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• it is hydrophobic
*""*This is false; it is hydrophilic.
The backbone of DNA, which is constant throughout the molecule, consists of deoxyriboses
linked by phosphodiester bonds. Note: The backbone of RNA consists of riboses linked by the
same phosphodiester bonds.
Specifically, the 5'-hydroxyl group of one nucleotide unit is joined to the 3'-hydroxyl group of the
next nucleot ide by a phosphodiester linkage. Thus, the covalent backbones of nucleic acids
consist of alternating phosphate and pentose residues and a purine or pyrimidine base is attached
to each pentose. The 5'-0H group and the 3'-0H moiety are linked in a condensation reaction.
The most prominent features of the DNA Double Helix:
• The two strands of the double helix have opposite polarity. Base-pairing is always antiparallel,
not only in the DNA double helix but also in other base-pai red structures formed by DNA or RNA.
SAADDES
• The 2-deoxyribose/phosphate backbones of the t wo strands form two ridges on the surface of
the molecule. The phosphate groups are negatively charged.
• The bases face inward to the helix axis, but their edges are exposed. They form the lining of two
grooves that are framed by the ridges of the sugar-phosphate backbone. The two grooves are of
unequal size. They are called the major and minor groove.
• In each of the two strands, successive bases lie flat. one on top of the other, like a stack of pan-
cakes. The flat surfaces of the bases are hydrophobic and successive bases in a strand form numer-
ous van der Waals interactions. This base stacking is the strongest noncovalent force in t he
double helix.
• Bases in opposite strands interact by hydrogen bonds. Note: The base sequence of one strand
predicts exactly the base sequence of the opposite strand. This is essential for DNA replication and
DNA repair.
• The double strand is wound into a right-handed helix with about 10.4 base pairs per turn.
1. The backbones of both DNA and RNA are hydrophilic and highly polar.
2. The hydroxyl groups of the sugar residues form hydrogen bonds with water.
3. The ribose phosphate portion of purine and pyrimidine nucleotides comes from 5-
phosphoribosyl-1-pyrophosphate (PRPP). PRPP is synthesized from ATP and ribose
5-phosphate, which is primarily formed by the pentose phosphate pathway.
Saad Alqahtani, Twitter @saaddes
dna/rna
Which type of RNA is the least abundant in the cell?
• messenger RNA
• t ransfer RNA
• ri bosomal RNA
SAADDES
63
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• messenger RNA
* **Ribosomal RNA is the most abundant fo llowed by t ransfer RNA.
Types of RNA:
1. Messenger RNA (mRNA) molecules carry information (genetic code) from
DNA in the nucleus to ribosomes in the cytoplasm, where polypeptides and
proteins are synthesized (translation). Important: mRNA is the template for pro-
tein synthesis and contains the codon.
2. Transfer RNA (tRNA) molecules carry the amino acids to ribosomes, where
the amino acids are linked together in the order specified by mRNA to form
SAADDES
particular polypeptides and proteins. Note: Amino acyl -tRNA synthetase is a
group of ligases (enzymes) that ensures that the correct amino acid is attached to
the tRNA w ith the correct anticodon to be used during protein synthesis.
Individual enzymes are highly specific for one amino acid. No error checking
occurs during the translation process on the ri bosome.
3. Ribosomal RNA (rRNA) molecules are the major component of ribosomes,
which are the physical and chem ical structures on wh ich protein molecules are
actually assembled.
4. Other RNA: a vast group of other RNA molecules specifically regulatory RNA
species such as small nuclear ribonucleoproteins (SNRPs), microRNA (miRNA),
small interferi ng RNA (siRNA), ribozymes and other RNA molecules.
Remember: Transcription is the process in wh ich DNA serves as a template fo r the
assembly of molecules of RNA (all three types). This process involves the enzyme RNA
polymerase.
Saad Alqahtani, Twitter @saaddes
dna/rna
The activity level of which enzyme controls the rate of glycolysis?
• aldolase
• phosphoglucose isomerase
• phosphofructokinase
SAADDES
• triose phosphate isomerase
64
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• phosphofructokinase
Phosphofructokinase (PFK} is a glycolytic enzyme that catalyzes the irreversible transfer of a
phosphate from ATP to fructose-6-phosphate. This is the most important control point of
glycolysis. Important point: The phosphofructokinase reaction is the rate-limiting step in
glycolysis. The reaction which is shown below, requires an input of energy from ATP.
fructose-6-phosphate + ATP phosphofructokinase fructose-1,6-bisphosphate + ADP
This allosteric enzyme is up-regulated by ADP and AMP and is inhibited by ATP, H+ and
citrate. In other words, the enzyme is most active when t he energy of a cell is low. Fructose-
2,6-bisphosphate is an important allosteric activator of this enzyme and an allosteric inhibitor
of fructose-1,6-bi sphosphatase, which physiologically reverses this reaction at the end of
SAADDES
gluconeogenesis (g lucose synthesis}.
Aldola se converts fructose-1,6-bisphosphate (6-carbon metabolite} into two 3-carbon
metabolites, dihydroxyacetone phosphate and glyceraldehyde-3-phosphate. This is called
the aldolytic reaction of glycolysi s. Aldolase is plentiful in skeletal and heart muscle t issues.
Glycolysis occurs in the cytoplasm in the absence of oxygen and involves the following:
1. Two molecules of ATP are used to phosphorylate glucose and start glycolysis.
2. The phosphorylated molecule is then broken down in a series of reactions into two, three
carbon molecules (lysis}.
3.Two molecules of NAD• capture Wand are reduced to 2 molecules of NADH + W.
4. Four molecules of ATP are produced by substrate phosphorylation.
5. The end product pyruvate may then either undergo aerobic respiration in the mitochon-
dria or anaerobic respiration (fermentation}.
*** Net Gain of 2 ATP
1. Fluoride inhibits bacterial enolase, decreasing pyruvate synthesis and in turn,
Notes
decreases bacterial acid production.
2. Lactate dehydrogenase converts pyruvate to lactate (lactic acid} under anaerobic
condit ions.
Saad Alqahtani, Twitter @saaddes
Hexoldnase or
glucokinase
Glycolysis Glycoraldohydo ~ 2H 2PO..+ 2NAD'
3·phos photo
ATP ADP
dehydrogenase ~2NADH+2H'
Glucose _ _\.::.,._,.:
/ ;__ _ Glusosc 6·phosphate
1,3· blsphoaphoglycerate (2)
~.::::.::"'~·1l Phosphoglycoroto
kin ase
~ 2ADP
~ 2ATP
Fructose &.phosphate
3-phoaphQ91yterate ( 2)
ATP
F
Phosphofructokinase 1
ADP Phosphoglycoroto1 l
mutase
SAADDES
Fructose 1, 6·bisphosphate
2·phosphoglyeerato (2)
Eno/as•1'
~H2 o
Glyceraldehyde + Dlhydroxyac:•tone
3-phosphate phosphate Phosphoenolpyruvate (2)
\____/ 2ADP
F
Triose phosphate Pyruvate kinese
isomerase 2ATP
1 Pvruvate l 2l
Second phase: oxidation coupled to generation of
high-energy phosphate and high-energy electrons.
First pha.se: phosporylation • 2 triose phosphate oxidized to pyruvate
and splitting. • 1 H2P04 consumed 64-t
• 2 triose phosphate consumed • 2 NADPH generated
• 2 ATP consumed • 4 ATP generated
Saad Alqahtani, Twitter @saaddes
enzymes
All of the following are the most useful enzymes for the diagnosis of acute
myocardial infarction EXCEPT one. Which one is the EXCEPTION?
• creatine kinase (CK)
• lactate dehydrogenase (LDH)
SAADDES
• alanine t ransaminase (ALT)
• aspartate transaminase (AST)
65
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• alanine transaminase (ALT)
In the diagnosis of acute myocardial infarction, enzyme determinations can provide only esti mates
of the extent of the damage, whereas an ECG can locate the site of the infarction. However, an ECG
does not distinguish between old defects and a recent infarction, whereas enzyme elevations are
diagnostic for recent and ongoing tissue damage.
*""* Creatine kinase (specifically CK-2 along with CK-3) is the first heart enzyme to appear in the
blood after a heart attack, followed by AST and LDH.
Some enzymes show relatively high activity in only one or a few tissues. The presence of increased
levels of these enzymes in plasma thu s reflects damage to the corresponding tissue.
For example:
In the liver:
SAADDES
• Alanine transaminase (ALT) and aspartate transaminase (AST) are most abundant in the
liver. They are not secreted in t he blood and t herefore any elevation of their plasma levels
isdue to leakage from the damaged cells. The transaminase levels are used for the diagnosis
of liver diseases.
In the heart:
• Creatine kinase (CK): CK-2 along with CK-3
• Lactate dehydrogenase (LDH): specifically H subunits
• Aspartate transaminase (AST)
1. Levels of lipase and amylase are elevated in acute pancreatitis and their main use is the
B differential diagnosis in patients who present with severe abdominal pain of sudden onset.
2. CK is used for the diagnosis of muscle diseases. Along with LDH, AST and myoglobin lev-
els, CK level is elevated in dermatomyositis, polymyositis and muscular dystrophies.
3. Elevated LDH with more or less normal AST and CK levels is typical for pulmonary in-
farction.
4. Glutamyl transferase (GGT) is used as a sensitive indicator of biliary obstruction.
5. Acid phosphatase (ACP) and prostate-specific antigen (PSA) are tumor markers used
for the diagnosis and follow-up of patients with prostatic cancer.
Saad Alqahtani, Twitter @saaddes
enzymes
All ofthe following statements concerning transamination reactions are true
EXCEPT one. Which one is the EXCEPTION?
• these reactions involve the transfer of an amino g roup from one amino acid to an
a-keto acid
• the enzymes that cata lyze these reactions are known as t ransaminases o r
SAADDES
aminotransferases
• glutamate and a-ketoglutarate are often involved in these reactions, serving as one
of the amino acid/a-keto acid pairs
• pyridoxal phosphate (PLP), which is derived from vitamin B6 serves as the cofactor
for these reactions
• all amino acids participate in these reactions at some point in their catabolism
66
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• all amino acids participate in these reactions at some point in their catabolism
*** This is false; serine and threon ine are not transaminated. They are oxidatively
deaminated (release NH3) by a dehydratase enzyme to form pyruvate and propionyl coA
respectively.
The first step in the catabolism of most amino acids involves the removal of the a -amino
group. Once removed, th is nitrogen can be incorporated into other compounds or
excreted.
Nitrogen is transferred from one amino acid to another by transamination reactions,
which always involve two different pairs of amino acids and t heir corres pond ing a -keto
acids.
SAADDES
Note: Glutamate and a -ketoglutarate usually serve as one of t he pairs; tran saminases
(aminotransferases) catalyze the t ransfer of amino groups; all transaminases require the
coenzyme pyridoxal phosphate.
In contrast to transamination reactions that t ransfer amino groups, oxidative
deamination reacti ons result in the liberation of the amino group as free ammonia (NHl
These reactions occur primarily in the liver and ki dney and provide a -ketoacids (for
energy) and ammonia (wh ich is a source of nitrogen in urea synt hesis). Note: Enzymes
involved in deamination reactions include glutamate dehydrogenase (for glutamate),
histida se (for h istidine) and serine dehydratase (for serine and threonine).
All aminotransferases (transaminases) share a comm on prost hetic group, pyridoxal
phosphate (PLP). PLP is t he coenzyme form of pyridoxine or vitamin B6. It functions as an
intermediate carrier of amino grou ps at t he act ive site of aminotransferases. PLP
undergoes reversible transformations between its aldehyde form, pyridoxal phosphate
(PLP), which can accept an amino group and its aminated form, pyridoxamine
phosphate (PMP), wh ich can donate its amino acid to an a -keto acid.
Saad Alqahtani, Twitter @saaddes
enzymes
All of the following are true of oxidative deamination reactions EXCEPT one.
Which one is the EXCEPTION?
• p rovide a-ketoacids fo r energy
• p rovide ammonia fo r urea synthesis
SAADDES
• occur mainly in t he liver and kidney
• p rovide a detoxification mechan ism
67
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• provide a detoxification mechanism
Deamination is also an oxidative reaction that occurs under aerobic conditions in all tissues
but especially t he liver and kidneys. During oxidative deamination, an amino acid is converted
into t he corresponding keto acid (for energy) by the removal of the amine group as ammonia
and being replaced by a ketone group. The ammonia eventually goes into the urea cycle.
Oxidative deamination occurs primarily on glutamic acid because glutamic acid is t he end
product of many transamination reactions.
Glutamate dehydrogenase is an enzyme of the oxidoreductase class that catalyzes the
oxidative deamination of glutamate. Ammon ia is released and <x-ketoglutarate is formed.
SAADDES
Glutamate dehydrogenase is unusual in that it can use either NAD• or NADP• as a coenzyme.
The reversible reaction has a major fu nction in both the synthesis and degradation of glutamic
acid and, via transaminases, other amino acids as well.
*** Important: Both aspartate aminotransferase (AST) and alanine aminotransferase (ALT)
are transaminases (aminotransferases). They are not involved in oxidative deamination
reactions. In contrast to transamination reactions that transfer amino groups, oxidative
deamination results in t he liberation of the am ino group as free ammon ia.
1. Glutaminase deaminates glutamine to glutamate and ammonium ion;
asparaginase deaminates asparagine to aspartate and ammonium ion.
2. Glutamate is unique in that it is t he only am ino acid that undergoes rapid oxidat-
ive deamination.
3. Histidine is deaminated by histidase to form ammonium ion (NH',J and urocan-
ate.
4. Serine and threonine are deaminated by serine dehydratase. Serine is converted
to pyruvate and threonine to a-ketobutyrate (which is decarboxylated oxidatively
to form propionyl CoA); ammon ium ion is released.
Saad Alqahtani, Twitter @saaddes
enzymes
Carbonic anhydrases are _ _ _ -containing enzymes that catalyze the
reversible reaction between carbon dioxide hydration and bicarbonate
dehydration.
• manganese
• selenium
• zinc
• mercury SAADDES
68
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• zinc
Carbon dioxide (C0 2) is a key metabolite in all living organism s. Carbon dioxide exists in
equilibrium with bicarbonate (HC0 3"), which is poorly soluble in l ipid membranes com-
pared to carbon dioxide; carbon dioxide can freely diffuse in and out of the cell, while bi-
carbonate must be transported. The conversion of bicarbonate to carbon dioxide facilitates
its transport into the cell, wh ile the conversion of carbon dioxide to b icarbonate helps trap
the carbon dioxide in the cell. The interconversion of carbon dioxide and b icarbonate pro-
ceeds slowly at physiological pH, so organisms produce enzymes to speed up the process.
Carbonic anhydrases are zinc-containing enzymes that catalyze the reversible rea ction
between carbon dioxide hydration and bicarbonate dehydration.
SAADDES
Carbonic anhydrase catalyzes the following reaction: H20 + C0 2 - H+ + HC03•
Carbonic anhydrase is one of the fastest known enzym es (one molecule of carbonic
anhydrase can process one milli on molecules of C0 2 each second) and is found in great
concentration in erythrocytes. Carbonic anhydrase is an enzyme that enables red b lood
cells to transport carbon dioxide from the t issues to the lungs.
1. Within the erythrocyte, carbon ic anhydrase facilitates the combination of car-
bon dioxide and water to form carbonic acid.
2. Carbonic anhydrase also functions in the kidney with the reabsorption of bicar-
bonate ion.
3. Although not required for carbon dioxide and water to form carbon ic acid,
carbonic anhydrase greatly increases the reaction in both respects (formation
and dissociation).
4. Most of the carbon dioxide (C0 ) is transported in the b lood as bicarbonate
2
ion (HC0 3·). It is converted to carbonic acid (H C0 ) more rapidly in whole
2 3
blood than in plasma. The reason for this is that whole blood contains erythro-
cytes with carbonic anhydrase while plasma does not contain erythrocytes.
Saad Alqahtani, Twitter @saaddes
enzymes
Which of the following components of the electron transport chain accepts
only electrons?
• FMN (flavin mononucleotide)
• coenzyme Q (ubiquinone)
SAADDES
• cytochrome b
• oxygen
69
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• cytochrome b
***The cytoch romes accept only electrons. The other components accept hydrogen and
electrons.
The majority of the energy conserved during catabolism reactions occurs near the end of
the metabolic series of reacti ons in the electron trans port chain. The electron tran sport,
or respiratory chain, gets its name fro m the fact that electrons are transported to meet
up with oxygen from respiration at the end of the chain. This chain is present in the inner
mitochondrial membrane and is the fi nal common pathway by which electrons derived
from different fuels of the body flow to oxygen. Elect ron transport and ATP synt hesis by
oxidative phosphorylation proceed continuously in all cells of the body that contain
SAADDES
mitochondria.
Components of the electron t ransport chain:
• FMN: receives electrons from NADH and transfers them through Fe-5 centers to
coenzyme Q. FMN is derived from riboflavin. Remember: NAD• is derived fro m n iacin.
• Coenzyme Q: receives electrons from FMN and also through Fe-5 centers from
FADH 2. Coenzyme Q is not derived from a vitamin (the body synthesizes it).
• Cytochromes (b, c, a and a 3): receive electrons from the reduced form of coenzyme
Q. Each cytochrome consists of a heme group associated with a protein; cytochrome a
+ a is also called cytochrome oxida se. Heme is synthesized from glycine and succinyl
3
CoA in humans. Heme is not derived from a vitamin.
• Oxygen: ultimately receives the elect rons at the end of the chain and is reduced to
water.
Remember: A coenzyme is a nonprotein substance (organic cofactor) that combines
w ith an apoenzyme (the protein portion of a co mplex enzyme) to form a haloenzyme (a
complete, cata lytically active enzyme system).
Saad Alqahtani, Twitter @saaddes
Complex I
NADH dehydrogenase
Complex JJ
Succinate dehydrogenase
In the mitochondrial elec-
t ron t ransport system
SAADDES
(ETS) electrons pass fi·om
Complex JJJ NADH or FADH2 to ulti-
Ubiquinone-cytochrome c mately reduce 02 and pro-
oxidoreductase duce H20
Complex IV
Cy tochrome oxidase
Diagrammatic representation of the mitochondrial electron transport syst em (ETS). The
path of the electrons is indicated by the broad, shaded arrows. UB= ubiquinone; C= cy-
tochrome C.
69- 1
Reproduced with p..-nnission from Wilcox RB: Hig1• Yield Bioclu~mistry. ed 1: Bnhimorc:. 2004, Lippincolt Willinms & Wilkins..
4
Saad Alqahtani, Twitter @saaddes
enzymes
Which ofthe following is NOT an enzyme classification?
• oxidoreductase
·ligase
• transferase
• oxygenase
• hydrolase SAADDES
• isomerase
70
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
•oxygenase
***Oxygenase is an enzyme but not an enzyme classification. It belongs to the oxidoreduc-
tase enzyme class.
Enzymes are catalysts. Most are very large proteins. Enzymes b ind temporarily to one or
more of the reactants of the reaction the enzymes catalyze.ln doing so, the enzyme intro-
d uces a new reaction pathway, which lowers the amount of activation energy needed and
thus speeds up the reaction. The functioning of the enzyme is determined by the shape of
the protein. Enzymes are substrate specific. For example, the enzyme pepti dase (which
breaks peptide bonds in proteins) will not work on starch (which is b roken down by human-
produced amylase in the mouth). The arrangement of molecules on the enzyme prod uces
an area known as the active site w ithin which the specific substrate(s) w ill "fit". It recog-
SAADDES
nizes, confines, and orients the substrate in a particular direction.
Classification of enzymes:
• Oxidoreductases: catalyze redox reactions
• Transferases: transfer functional groups
• Hydrolases: cause hydrolysis reactions
• Lyases: break C-0, C-C, or C-N bonds
• Isome rases: rearrange functional groups
• Ligases: join two molecules, for example, DNA ligase joins p ieces of DNA
1. Substrate concentration, pH, temperature and enzyme concentration all have
an effect on the activity of an enzyme.
2. The enzymatic mo del that assumes that enzymes have flexible conformations
is called induced fit.
3. The inactive precursor of an enzyme is called a proenzyme.
4. A catalytically inactive p rotein formed by removal of the cofactor from an active
enzyme is called an apoenzyme.
Saad Alqahtani, Twitter @saaddes
enzymes
Which of the following enzymes is responsible for dissolving blood clots?
• prothrombin
• thrombin
• fibri nogen
• plasmin
SAADDES
71
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• plasmin
Plasmin (aka fibrinolysin) is normally present in the blood in an inactive form ca lled
plasminogen. Substances known as plasminogen activators (for example, urokinase
produced in the kidney) can convert plasminogen to plasmin, which will cleave the
peptide bond in fibri n, leading to its breakdown and dissolution of clots.
Fibrinogen is a soluble protein normally present in the plasma that is essential to the
blood clotting process. Fibrinogen is converted into an insoluble, th read-like polymer
ca lled fibrin by the enzyme thrombin. Thrombin is produced from the inactive
plasma protein precursor prothrombin, which is formed in the liver. In the presence
SAADDES
of thromboplastin and ca lcium ions, prothrombin is converted to thrombin.
Deficiency in plasmin can lead to thrombosis and defective wound healing.
Note: Research has shown that thrombin acts upon the arginyl-glycine linkages
(specific peptide bonds) in fibrinogen to produce a fibrin monomer.
Saad Alqahtani, Twitter @saaddes
enzymes
A zymogen is converted to its active enzyme form by which of the following
mechanisms?
• removal of a peptide fragment
• addit ion of a peptide fragment
SAADDES
• addit ion of an amino group
• removal of an amino group
72
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• removal of a peptide fragment
Zymogens are enzymatically inactive precursors of proteolytic enzymes. The
digestive enzymes that hydrolyze proteins are produced and secreted as zymogens in
the stomach and pancreas. They are converted to their active forms by removal of a
peptide fragment in the lumen of the digestive tract. Proteolytic enzymes are
synthesized as inactive zymogen precursors to prevent unwanted destruction of
cellu lar proteins, so as to regulate when and where the enzyme becomes activated.
Note: The release and activation of the pancreatic zymogens is mediated by the
secretion of cholecystokinin, secretin and the parasympathetic nervous system.
SAADDES
A good example of what occurs when some zymogens become active enzymes inside
the cells is seen in acute pancreatitis, in which the premature activation of some ofthe
pancreatic enzymes such as trypsin, phospholipase A2 and elastase, p roduce the
autodigestion of the pancreas.
Z~mog<•ns
Site of Synt hesis Zymogen Active E nzyme
Stomach Pepsinogen Pepsin
Pancreas Chymotlypsinogen Chymotrypsin
Pancreas Trypsinogen T rypsin
Pancreas Procarboxypeptidase A Carboxypeptidase A
Pancreas Procarboxypeptidase B Carboxypeptidase B
Pancreas Proelastase Elastase
Saad Alqahtani, Twitter @saaddes
enzymes
Starch molecules are broken down by enzymes known as:
• oxygenases
• isomerases
• peroxidases
• amylases
SAADDES
73
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• amylases
Amylase is the name given to glycoside hydrolase enzymes that break down starch into glu-
cose molecules. Amylase is also known as ptyalin. Although the amylases are designated by
d ifferent Greek letters, they all act on et- 1.4-glycosidic bonds.
Classifi cation of amylases:
• et-a myiases: by acting at random locations along the starch chain, a -amylase breaks
down long-chain carbohydrates, ultimately yielding maltotriose and maltose from amyl-
lose, or maltose, glucose, and "limit dextrin" from amylopectin. Because a-amylase can
act anywhere on the substrate, a-amylase tends to be faster acting than [3-amylase. In
animals, a-amylase is a major digestive enzyme.
SAADDES
Note: In human physiology, both the sa livary and pancreatic amylases are a-amylases.
• ~-amylase: working from the non-reducing end, [3-amylase catalyzes the hydrolysis
of the second <x-1A-g lycosidic bond, cleaving off two glucose units (maltose) at a time.
• y-amylase: in addition to cleaving the last a-1,4-glycosidic linkages at the non reducing
end of amylose and amylopectin yield ing glucose, y-amylase will cleave a-1,6-glycosidic
linkages.
1. "Limit dextrins" are various branched polysaccharide fragments that remain fol-
lowing the hydrolysis of starch.
2. Disaccharides and small glucose polymers are hydrolyzed at the intestinal brush
border by lactase, sucrase, maltase and alpha-dextrinase.
3. Remember: Only monosaccharides (e.g., glucose, galactose, fructose) are absorbed
in the small intestine. Lactase degrades lactose to glucose and galactose, isomaltase
cleaves a glucose linked 1,6 to another glucose as is found at the branch points in
starch and glycogen and sucrase degrades sucrose to glucose and fructose.
4. a-1,4 linkages are the predom inant linkages between glucose units within
glycogen molecules.
Saad Alqahtani, Twitter @saaddes
enzymes
Your patient's medical history says that she has von Gierke's disease. She is
missing the enzyme which converts _____
• g lucose-6-phosphatase, g lucose-6-phosphate to glucose
• g lucose-6-phosphatase, glucose-6-phosphate to fructose-6-phosphate
SAADDES
• pyruvate ca rboxylase, pyruvate to phosphoenolpyruvate
• pyruvate carboxylase, pyruvate to 2-phosphoglycerate
74
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• glucose-6-phosphatase, glucose-6-phosphate to glucose
Glucose -6-phosphatase (G6P) is the liver enzyme that converts glucose-6-phosphate into
glucose. G6P is vital for the release of glucose into the bloodstream from glycogen
breakdown (g lycogenolysis).
Important: Glucose-6-phosphatase, like pyruvate carboxylase, is present in the liver and
kidneys but not in muscle. Therefore, any glucose released from glycogen stores of
muscle will be oxid ized in the glycolytic pathway. In the liver, the acti on of glucose -6-
phosphatase allows glycogenolysis to generate free glucose for maintaining b lood
glucose levels.
Gluconeogenesis is a b iochemical process in which glucose is made fro m molecul es that
SAADDES
are not carbohydrates (primarily from amino acids but not fatty acids). This p rocess occurs
prim arily in the liver and the p rocess p rovides glucose for export to other tissues when
o t her sou rces of glucose are exhausted. Typically, gluconeogenesis involves the
conversion of lactic acid or amino acids into pyruvate or phosphoenolpyruvate, which
is then converted to glucose.
Some key reactions of gluconeogenesis:
• Pyruvate - oxaloacetate (catalyzed by pyruvate carboxylase)
• Oxaloacetate - phosphoenolpyruvate (catalyzed by phosphoenolpyruvate
carboxykinase)
• Fructose-1,6-bisphosphate - fructose-6-phosphate (catalyzed by fructose -1 ,6-
bisphosphatase)
• Glucose-6 -phosphate -glucose (catalyzed by glucose-6-phosphatase)
1. Glucose-6-phosphate does not contain a high-energy bond.
2. In glycolysis, glucose is converted to pyruvate; glycolysis is the first part of
the respiratory pathway. In gluconeogenesis, pyruvate is converted to glucose.
Saad Alqahtani, Twitter @saaddes
Sequential reactions in gluconeogenesis starting from pyruvate
Pyruvate + JiCo 3· + ATP oxaloacetate + AOP + P; + tr x2
Oxaloacetate + GTP phosphoenolpyruvate + C0 2 + GOP x2
Phosphoenolpyruvate + H20 2-phosphoglycerate x2
2-Phosphoglycerate 3-phosphoglycerate x2
3-Phosphoglycerate + ATP I ,3-bisphosphoglycerate + ADP + H' x2
I,3-Bisphosphoglycerate + NADH + 1-I' ~ glyceraldehyde-3-phosphate + NAD• + P; x2
SAADDES
Glyceraldehyde-3-phosphate dihydroxyacetone phosphate
Glyceraldehyde-3-phosphate + dihydroxyacetone phosphate ~ fi-uctose- 1,6-bisphosphate
Fructose-1 ,6-bisphospb ate + H20 fructose-6-phosphate + P;
Fructose-6-phosphate glucose-6-phosphate
Glucose-6-phosphate + H20 glucose + P;
Summary:
2 Pyruvate + 4ATP + 2GTP + 2NADH + 4H20 --- glucose + 4ADP + 2GDP + 6P; + 2 NAD + 2H '
The bypass reactions are in bold; a ll other reactions are reversible steps of g lycolysis. The
figures at the right indicate that the reaction is to be counted twice, because two three-carbon
precursors are required to make a molecule of glucose. Note that the reactions required to re-
place the cytosol ic NADH consumed in the glycera ldehyde-3-phosphate dehydrogenase re-
action (the conversion of lactate to pyruvate in the cytoso l or the transport of reducing
equiva lents from the mitochondria to the cytosol in the fom1 of malate) are not considered in
this summary. 7 .,_ 1
Saad Alqahtani, Twitter @saaddes
enzymes
Km is the substrate concentration at which the enzyme is half-saturated with
its substrate.
Km is also the substrate concentration at which the reaction is half maximal.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
75
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
In Michaelis -Menton kinetics, there are a few simple (or simplistic) assumptions about en-
zymatic catalys is:
1. The reaction has only one substrate.
2. The molar concentration of the substrate is much higher than that of the enzyme.
3. Only the initial reaction is considered.
4. The course of the reaction is observed for only a very short t ime period.
Km is equivalent to that substrate concentration at wh ich V0 (initial reaction velocity) is
one-half Vmax· Note: Km has units of molarity.
The Km values of enzymes range w idely. For most enzymes, Km li es between 1o-• and
SAADDES
10.. M. The Km value for an enzyme depends on the particular substrate and also on
environmental cond itions such as the temperature and ionic strength.
The Michaelis Menton constant (Kml is frequently and incorrectly said to be equivalent
to the dissociation constant of the enzyme-substrate complex. For most reactions, the
Michaelis constant is a co mp lex function of many different reaction constants, but this
constant does give a method by which to compare the affinity (reciprocal of dissociation)
of an enzyme for different substrates or different enzymes for the same substrate. The
lower the Km the higher the relat ive affinity.
1. Km va lues for enzyme-substrate reactions:
• Increase in the presence of a compet itive inhibitor
•Are not affected in the presence of a noncompetitive inhibitor; however,
Vmax is reduced in the presence of a noncompetitive inhibitor
Important: The maximal rate (V max> is attained when the enzyme sites are saturated
with substrate.
Saad Alqahtani, Twitter @saaddes
enzymes
All of the following statements concerning allosteric enzymes are true
EXCEPT one. Which one is the EXCEPTION?
• they frequently catalyze a comm itted step early in a metabolic pathway
• they often have two or more subunits, each with substrate binding sites that exhibit
cooperativity
SAADDES
• allosteric activators cause the enzyme to bind substrate more readily
• allosteric inhibitors cause the enzyme to bind substrate less readily
• they follow the Michaelis-Menton kinetics
76
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• they follow the Michaelis-Menton kinetics
***This is false; allosteric enzymes usually show a complex relationship between the
velocity and substrate concentration.
The reg ulation of metabolic processes is achieved through 2 mechanisms acting directly
on enzymes: allosteric regulation and covalent modification.
Allosteric regulation: an allosteric enzyme is a regulatory enzyme and has both an
active site for the substrate and an allosteric site for an effector (non-active site) of the
enzyme. In the absence of the enzyme's effector, the substrate is able to b ind to the
enzyme's active site and end products are produced. If the effector is present, it w ill b ind
to the enzyme's allosteric site. Effectors cause conformational changes that are
SAADDES
trans mitted through the bulk of the protein to the catalytically active site(s).
The hallmark of effectors is that when they b ind to enzymes, the effectors alter the
catalytic properties of an enzyme's active site. Those that increase cata lytic activity are
known as positive effectors. Effectors that reduce or inhibit cata lytic activity are
negative effectors. These modifiers may be either the substrate itself or some other
metabolite. For example, ATP inhibits phosphofructokinase (an allosteric enzyme) even
though ATP is also a substrate for this enzyme.
Covalent modification (the reversible covalent modification of an enzyme): enzyme
phosphorylation is the most comm on form of covalent modification. Phosphorylation
occurs on either Ser-OH, Thr-OH or Tyr-OH groups. Adding or removing a phosphate
group (a bulky, heavily negatively-charged functional group) has dramatic effects on
protein conformation. Enzymes exist in 2 states, mod ified (phosphorylated) and
unmodified (un phosphorylated), where one is active and the other is inactive. Enzyme
phosphorylation is catalyzed by ATP-dependent protein kinases. Phosp horylated
enzymes are dephosphorylated by phosphoprotein phosphatases.
Saad Alqahtani, Twitter @saaddes
enzymes
What is the substrate for glycogen synthesis?
• UDP-glucose
• TOP-glucose
• ADP-glucose
• CTP-glucose
• GTP-glucoseSAADDES
77
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• UDP-gluco se
The synthesis of glycogen from glucose is carried out by the enzyme glycogen synthase.
It is the key regulatory enzyme for glycogen synthesis and utilizes UDP-glucose as one
substrate and the non-reducing end of glycogen as another.
Note: Glycogen synthase is respon sible for making the a -1,4linkages in glycogen.
UDP-glucose is the substrate for glycogen synthesis. Glucose enters the cell and is
p hosphorylated to g lucose -6-phosphate by hexokinase (in most tissues) or by
glucokinase (in the liver). To initiate glycogen synthesis, the glucose-6-phosphate is
reversibly converted into glucose -1-phosphate by phosphoglucomutase. Th is glucose-
SAADDES
1-phosphate is then converted to UDP-glucose by the action of UDP-glucose
pyrophosphoryla se.
1. Glycogen syntha se occurs in both phosphorylated and dephosphorylated
8 forms. The active enzyme, glycogen synthase A, is the dephosphorylated and
active form and is activated (dephosphorylated) by insulin. Glycogen synthase
B, is the phosphorylated and inactivated form of the enzyme and is inactivated
(phosphorylated) by epinephrine (in muscle and liver) and glucagon (in liver).
2. Glycogen phosphorylase, wh ich breaks down glycogen, also has two forms;
(a) and (b): however, in th is case the phosphorylation of this enzyme (wh ich
happens in liver cell s) forms the active enzyme (a) and the dephosphorylation
forms the inactive enzyme (b). Glycogen phosphorylase is activated (phosphor-
ylated) by glucagon and epinephrine and inactivated (dephosphorylated) by
insulin.
3. Important: Both enzymes (glycogen synthase and phosphorylase) are phos-
phorylated at specific serine residues.
Saad Alqahtani, Twitter @saaddes
enzymes
Which of the following best describes an "uncompetitive inhibitor"?
• essentially a noncompetitive inhibitor that can bind only when the substrate is
attached
• essentially a competitive inhibitor that can bind only when the substrate is attached
SAADDES
• a noncompetitive inhibitor that can be overcome by increasing substrate concentra-
tion
• an irreversible inhibitor (the two are synonyms)
78
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• essentially a noncompetitive inhibitor that can bind only when
the substrate is attached
Enzymes are subject to the fol lowing types of inhibition:
Reversible:
1. Competitive inhibition: the competitive inhibitor resembles the substrate and
binds to the active site of the enzyme. The substrate is then prevented from bind-
ing to the same active site. The hallmark of competitive inhibition is the inhibit-
ion can be overcome by increasing the substrate concentration.
2. Noncompetitive inhibition: the inhibitor and substrate can bind simultaneous-
ly to an enzyme molecule. This means that their binding sites do not overl ap.
SAADDES
Because the inhibitor and substrate do not compete for the same site, noncompet-
itive inhibition cannot be overcome by increasing the substrate concentration. A
noncompetitive inhibitor is by definition an allosteric inhibitor.
3. Uncompetitive inhibition: like noncompetitive, t he inhibitor and substrate
bind at d ifferent sites which do not overlap. However, an uncompetitive inhibitor
will bind only to an enzyme that has a substrate already attached (ES complex).
4. Mixed inhibition: the inhibitor binds to a site other than t he active site, but has
a different affinity for the lone enzyme (E) versus the enzyme-substrate complex
(ES).
Remember: The noncompetitive inhibitor binds to either a free enzyme or t he ES
complex.
Irreversible inhibitors are those that combine with or destroy a functional group on
the enzyme that is essential for its activity. A classic example is the irreversible
inhibition of cyclooxygenase (COX) by aspirin (acetylsalicylate), which acetylates the
active site serine residue.
Saad Alqahtani, Twitter @saaddes
enzymes
A competitive inhibitor of an enzyme:
• increases Km without affecting Vmax
• decreases Km without affecting Vmax
• increases Vmax w ithout affecting Km
SAADDES
• decreases both Vmax and Km
79
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• increases Km without affecting V max
Competitive inhibition:
• Inhibitor and substrate compete for the same binding • Vmax remains the same
site on the enzyme • Km is increased
• Is overcome by increasing substrate
Noncompetitive inhibition:
• Inhibitor and substrate bind at different sites on the • Vmax is decreased
enzyme • Km is unchanged
• Is not overcome by increasing substrate
Mixed Inhibition:
• Inhibitor and substrate bind at different sites and inhibitor • Km is increased
SAADDES
has different affinity for enzyme versus enzyme-substrate • Vm is decreased
complex
Uncompetitive Inhibition:
•Inhibitor binds only to enzyme-subst rate complex at a site • Km andVm are both decreased
other than the active site
The rate at which an enzyme works is influenced by several factors:
• The concentration of substrate molecules (the more of them available, the quicker the enzyme
molecules collide and bind with them). The concentration of substrate is designated [S] and is
expressed in unit of molarity.
• The temperature: As the temperature rises, molecular motion and hence, collisions between
enzyme and substrate speed up. But as enzymes are proteins, there is an upper limit beyond
which the enzyme becomes denatured and ineffective.
• The presence of inhibitors (competitive and noncompetitive)
• pH : The conformation of a protein is influenced by pH and as enzyme activit y is crucially
dependent on the protein's conformation, the enzyme's activity is likewise affected.
1. The velocity of a reaction increases with the substrate concentration if the enzyme
Notes concentration is constant.
2. AtVmax all of the active sites are saturated with substrate.
Saad Alqahtani, Twitter @saaddes
enzymes
Trypsinogen is activated either by trypsin or by the duodenal enzyme:
• endopeptidase
• alanine aminotransferase
• enteropeptidase
SAADDES
• pancreatic lipase
80
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• enteropeptida se
The presence of amino acids (from protein digestion) in the small intestine (specifically t he
d uoden um) stimulates the release of cholecystokinin (CCK). This hormone causes the release
of the pancreatic zymogens (e.g., trypsinogen, chymotrypsinogen, proelastase,
procarboxypeptidases and prophospholipases) and the contraction of the gallbladder to
deliver bile to the duodenum.
To prevent self-digestion, the dangerous enzymes (not the lipases and glycosidases) are
synthesized and secreted as inactive precursors called zymogens. The zymogens are
synthesized at the rough endoplasmic reticulum, stored in secretory vesicles, released by
exocytosis and activated by selective proteolytic cleavage in t he lumen of the Gl tract.
Remember:
SAADDES
• Trypsinogen is activated either by trypsin or by enteropeptidase
• Trypsin converts trypsinogen, chymotrypsinogen, proelastase and procarboxypeptidase
A and B to their active forms. Important point: Trypsin can act as an activator for all zym-
ogens of pancreatic proteases.
1. Pepsinogen (secreted by ch ief cells of the stomach) is activated to pepsin by the
B low pH in the stomach or other activated pepsin molecules.
2. Trypsin cleaves peptide bonds in which the carboxyl group is contributed by
lysine and arginine (basic amino acids).
3. Chymotry psin cleaves peptide bonds in which the carboxyl group is contributed
by the aromatic amino acids or by leucine.
4. Elastase cleaves at the carboxyl end of amino acid residues with small, uncharged
(hydrophobic) side chains such as alanine, glycine or serine.
5. Carboxypeptidase A has little activity on aspartate, glutamate, arginine, lysine or
proline; carboxypeptidase B cleaves basic amino acids, lysine and arginine.
6. Endopeptidase (for example, trypsin) refers to any of a large group of enzymes
that catalyze the hydrolysis of peptide bonds in the interior of a polypeptide chain
or protein molecule.
Saad Alqahtani, Twitter @saaddes
enzymes
Which enzyme is derived from osteoblasts and its serum level rises in bone
conditions with increased osteoblastic activity?
• lactate dehydrogenase
• alanine t ransaminase
SAADDES
• alkaline phosphatase
• acid phosphatase
81
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• alkaline phosphatase
Alkaline phosphatase is abundant in bone, placenta, intestine and the hepatobil iary system.
Each of these organs contains a different isoenzyme.The bone and liver enzymes are the most
abundant in the normal serum. The bone enzyme is derived from osteoblasts and its serum
level rises in bone conditions with increased osteoblastic activity: rickets, osteomalacia, hy-
perparathyroidism, osteitis deformans, neoplastic di seases with bone metastases and healing
fractures. Note: The liver enzyme level is increased in patients with biliary obstruction.
Remember: The levels of only a limited number of enzymes are determined on a rout ine basis
in most clinical laboratories. The most important of these are as follows:
1. Plasma cholinesterase is one of the few diagnostically important enzymes whose major
SAADDES
place of residence is in the plasma. It is decreased in severe liver diseases, includ ing viral
hepatitis and liver cirrhosis. More important is its use in the diagnosis of organophos-
phate poisoning. Respon sible for metabolism of ester anesthetics used in dentistry.
2. Alanine transaminase (ALT) and aspartate transaminase (AST): these enzymes are
most abu ndant in the liver. They are not secreted into the blood and therefore any eleva-
tion of their plasma levels is due to leakage from damaged cells. The transaminase levels are
used for the diagnosis of liver diseases.
3. -y-Giutamyl transferase (GGT): although present in most tissues, it is most abundant in
liver and kidney. GGT is used as a sensitive indicator of biliary obstruction.
4. Acid phosphatase (ACP) and prostate-specific antigen (PSA) are tumor markers, used
for the diagnosis and follow-up of patients with prostatic cancer.
5. Creatine kinase (specifically CK-2 along with CK-3) is the first heart enzyme to appear in
the blood after a heart attack, followed by aspartate transaminase (AST) and lactate
dehydrogenase (LDH).
6. Levels of lipase and amylase are elevated in acute pancreatitis and their main use is the
d ifferential diagnosis in patients who present with severe abdominal pain of sudden onset.
Saad Alqahtani, Twitter @saaddes
enzymes
Which of the following equations is correct?
• haloenzyme +cofactor = coha loenzyme
• apoenzyme+ cofactor = haloenzyme
• coenzyme + cofactor = enzyme
SAADDES
• coenzyme+ apoenzyme = coapoenzyme
82
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• apoenzyme+ cofactor= halo enzyme
Cofactors are organic molecul es (coenzymes) or ions (usually metal ions) that are
required for its activity. They may be attached either loosely or tightly (prosthetic group)
to the enzyme. A cofactor binds w ith its associated protein (apoenzymes), which is
functionally inactive, to form the active enzyme (haloenzyme).
Sumt.· t.'lll\ mt.·scunl.tinml!, n· quinn~ murl!.tnh:
t.'lcntcnh .t\ (UI.tcturs
Cofactor Enzymes
Fc1 ' or Fe3 " Cytochrome oxidase
Catalase
SAADDES
Peroxidase
Ferredoxin
Cul• Cytochrome oxidase
Pyruvate phosphokinase
Zn2 Carb<lnic anhydrase
Alcohol dehydrogenase
Mg' Hexokinase
Glucose-6-phosphatasc
Pyruvate kinase
Mn 2 Arginase
Rib<lnuelcotide reductase
K Pyruvate
Ni1..- Urease
Mo Dinitrogcnasc
Se Glutathione peroxidase
Saad Alqahtani, Twitter @saaddes
enzymes
Which ofthe following functions as a coenzyme vital to tissue respiration?
• pyridoxal phosphate
• biocytin
• thiamine pyrophosphate
SAADDES
• tetrahydrofolate
83
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• thiamine pyrophosphate
Thiamine pyrophosphate functions as a coenzyme vital to tissue respiration. It is req uired as a
cofactor for the enzyme pyruvate dehydrogenase, which catalyzes the oxidative decarboxylation
of pyruvate, to form acetyi-CoA, which then enters into the Krebs cycle for the generation of energy.
Thiamine pyrophosphate is also a coenzyme for transketolase, which functions in the pentose
phosphate pathway, an alternate pathway for glucose oxidation.
Suml' COl'llL\ nu·s sen i n~ a~ tr.uhn·nt carriers uf spccit1c atoms ur tunctwnal groups
Coenzyme Derived from Functions
Tltiamine pyrophosphate (TPP) Thiamine (vitamin 8 1) Vital to tissue re$piration. Plays a role in the
removal of carboxyl ( -COOH) grouJ>S from
organic acids, releasing the. c.arbon and oxygen
SAADDES
atoms as carbon dioxide (C02) .
Flavin adenine dinucleotide Riboflavin (vitamin B2) Functions in certain oxidation I reduction reactions
(FAD) in the body.
Nicotinamide adenine. Nic.otinic acid (niacin/ Utilized altemately with NADH as an oxidizing or
dinucleotide (NAD) vitamin 8.1) reducing agent in various metabolic processes.
Coenzyme A Pantothenic acid Functions as an acyl group carrier and is nece~~sa ry
(vitamin Bs) for fa tty acid synthesis and oxidation, pyruvate
oxidation and other acetylation re-actions.
Pyridoxal phosphate (PLP) Pyridoxine (vitam in 8 6) Is essential fo r many enzymatic reactions, almost
all of which are associate.d with amino acid
metabolism.
Tetrahydrofolate folic acid (vitamin~) Participates. in the transfer of various c.arbon
fragments from one mol«:ule to another · for
instance.• involved in the synthesis of methionine
and thymine.
Lipoate Not required in diet Cofactor for the pyruvate dehydrogenase complex,
which bre.aks down pyruvate to form acetyi-CoA.
Coenzyme. B u Vitamin Bu Is an essential cofactor for several enzymes.
Saad Alqahtani, Twitter @saaddes
hormones
All of the major anterior pituitary hormones, EXCEPT for growth hormone
exert their principal effects by stimulating target glands such as the
thyroid gland, adrenal cortex, ovaries, testicles and mammary glands.
Growth hormone, in contrast to other hormones, does not function
through a target gland but exerts its effects directly on all or almost all
tissues of the body.
SAADDES
• both statements are true
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
84
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Growth hormone (GH), also cal led somatotrophic hormone or somatotropin, is a small protein
molecule that contains 191 amino acids. It is synthesized and secreted by cells cal led somatotropes
in the anterior pituitary and is part of the hypothalamus-pituitary-liver axis. GH stimulates body
growth, secretion of IGF-1 and lipolysis; it however inhibits the actions of insulin on carbohydrate
and lipid metabolism.
A major target of GH is the liver, where it causes t he liver to form several small proteins called
somatomedins that have the potent effect of increasing all aspects of bone growth. Many of the
somatomedin effects on growth are similar to the effects of insulin on growth. Therefore, t he
somatomedins are also called insulin-like growth factors (IGFs). By far t he most important of t he
somatomedins is somatomedin C (also called IGF-I).Its concentration in the plasma closely follows
the rate of GH secretion.
SAADDES
Aside from its general effect in causing growth, GH has multiple specific metabolic effects, including
(1) increased rat e of protein synthesis in most cells of the body; (2) increased mobilization of fatty
acids from adipose t issue, increased free fatty acids in the blood and increased use of fatty acid s for
energy; (3) decreased rate of glucose utilization throughout the body. Th us in effect, GH enhances
body protein, uses up fat stores and conserves carbohyd rates.
1. GH raises blood glucose levels by decreasing peripheral tissue utilization. It is protein
anabolic and lipolytic. Excessive GH ca n lead to gigantism and acromegaly (after growth
plates are closed)
2. The following factors stimulate GH secretion:
• Decreased blood glucose • Exercise
• Decreased blood free fatty acids • Testosterone, estrogen
• Starvation or fasting, protein deficiency • Deep sleep (stages II and IV)
• Trauma, stress, excitement • Growth hormone-releasing hormone
3. The following factors inhibit GH secretion:
• Increased blood glucose • Growth hormone inhibitory hormone
• Increased blood free fatty acids (somatostati n)
• Aging • Growth hormone (exogenous)
• Obesity • Somatomedins (insulin-l ike growth factors)
Saad Alqahtani, Twitter @saaddes
hormones
Testosterone and pituitary FSH are required for normal sperm production.
Many cells express the androgen receptor and the FSH receptor.
• both statements are true
SAADDES
• both statements are fa lse
• the fi rst statement is t rue, the second is fa lse
• the fi rst statement is fa lse, the second is t rue
85
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is true, the second is fal se
***Only Sertoli cells express the androgen recepto r and the FSH receptors, so these hor-
mones regu late spermatogenesis indirectly through their actions on Sertoli cell s.
H ormone~ of the P itmtar~ G land
Hormone Source Tat·get Action (s)
Thyroid-stimulating Ante rior pituitary 11tyroid gland S timulates synthesis and secretion of thyroid
honnone honnone.~
FoJlicle·stimulating Ante rior pituitary Ovary S timulates growth o f graafian foJlicles and
honnone e~"itrogen secretion
Testis Promotes speml maturation (testis)
SAADDES
Luteinizing hormone Anterior pituitary Ovary S timulates ovulation, formation o f corpus lute.um
and synthe$is of estrogen and progesterone
(ovary)
Testis Stimulates synthesis and se<:retion of testosterone.
(testis)
Growth hom1one Anterior pituitary Bone S timulates protein synthesis and overall growth
Prolactin Ante rior pituitary Mammary gland~ S timulates milk production and breast
deveJopment
Adrenocorticotropic Ante rior pituitary AdrenaJ cortex S timulates synthesis a nd secretion of adrenaJ
honnone cortical honn ones
Melanocyte· Ante rior pituitary Skin S timulates melanin synthesL~
stimulating hom1one
Oxytocin Posterior pituitary Mammary glandc; Milk ejection
Uterine smooth Uterine contraction
musc]e
Antidiuretic honnone Posterior pituitary Kidney tubules S timulates water reabsorption a t rena] collecting
(vac;opressin) ducts
Saad Alqahtani, Twitter @saaddes
hormones
All of the following hormones use the adenylyl cyclase-cAMP second mes-
senger system EXCEPT one. Which one is the EXCEPTION?
• adrenocorticotropic hormone (ACTH)
• calcitonin
SAADDES
• glucagon
• somatostatin
• thyroid-releasing hormone
86
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• thyroid-releasing hormone
Second messengers are small, diffusible molecules that mediate the intracellular effects of
hormones. These "second messenger• molecules intervene between the original message (the
neurotransmitter or hormone) and the ultimate effect on the cell.
The following second messenger systems play critical roles in hormone-mediated cell regulation:
adenylate cyclase (cAMP), ca lcium ions and associated calmodulin and products of membrane
phospholipid breakdown (e.g., inositol triphosphate [IP3 1and diacylglycerol [DAG]). Note: Not
only do multiple hormones ut ilize the same second messenger system, but a single hormone can
also utilize more tha n one system. lmportant: Hormones that utilize second messengers are usually
water soluble peptide/protein hormones.
SAADDES
Se-cond messengel' system Hormones that use system
Adenylyl Cyclase-cAMP Adrenoc011icotropic honnone, Angiotensin II (epithelial cells), Calcitonin,
Cat~h ol am ines (beta rece.ptors), Follicle·s timulating honnone, Glucagon,
Lute.i nizing hormone, Parathyroid hormone, Thyroid·stimulating honnone,
Secretin, Somtostatin
Inositol triphosphate (JP,)
Angiotensin Jl (vascular smooth muscle), Cate.cltolamines (alpha re.c eptors),
and diacylglycerol (OAG) Gonadotrop i n ~ rele.asing honnone, Gro\\1h hormone·rele.asing honnone., Oxytocin,
and/or calcium--calmodulin Thyroid·re.leasing honnone, Vasopressin (V 1 receptor, vascular smooth nnL~c l e)
Important: cAMP is released into the cytoplasm after a first messenger G protein bind sto its recep-
tor on the catalytic domains of adenylyl cyclase. Once adenylyl cyclase forms cAMP and releases it into
the cytoplasm, the cAMP binds to ion channels or to an enzyme, such as protein kinase, to expose
this enzyme's active site, which continues the commu nication pathway.
Remember:
1. cAMP issynthesized from adenosine triphosphat e (ATP) by adenylate cyclase, a hormone-con-
trolled enzyme in the plasma membrane.
2. cAMP is degraded by a group of enzymes that are collectively known as phosphodiesterases.
3. The most important target of cAMP is protein kinase A.
Saad Alqahtani, Twitter @saaddes
hormones
Which of the following is the best-known stimuli for increasing the rate of
thyroid-stimulating hormone (TSH) secretion by the anterior pituitary
gland?
• exposure to heat
SAADDES
• exposure to cold
• exposure to stress
• exposure to relaxation
87
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• exposure to cold
Thyroid-stimulating hormone (TSH), also called thyrotropin, is secreted by cel ls called thyrotropes
of the anterior pituitary gland. TSH controls the rate of secretion of thyroxine (T4 ) and
triiodothyronine (T 3 ) by the thyroid gland and t hese hormones control the rates of most
intracellular chemical reactions in the body.
Various types of stress can inhibit TSH secretion, most likely by way of neural influences that inhibit
the secretion ofthyrotropin-releasing hormone (TRH) from the hypothalamus.
Remember: TSH secretion is stimulated by TRH. There are several negative feedback loops that
regulate the secretion of thyroid hormones, including the following:
1. High levels of circulating thyroid hormone decreases the secretion of both TRH and TSH.
SAADDES
2. Elevated levels ofTSH decreases the secretion ofTRH.
Causes of Hyperthyroidism (e.g., Toxic Goiter, Thyrotoxicosis, Graves' disease): In the patient with hy-
perthyroidism the entire thyroid gland is usually markedly hyperplastic. These changes in the t hy-
roid gland are similar to those ca used by excessive thyroid-stimulating hormone. However,
radioimmunoassay studies have shown the plasma TSH concentrations to be less than normal rather
than enhanced and often to be essentially zero. On the other hand, another substance that has an
action similar to that ofTSH is found in the blood of most patients. This substance, called long-act-
ing thyroid stimulator (LATS), has a prolonged stimulating effect on the thyroid gland.
Note: In hypothyroidism (whether it is manifested as myxedema in adults or as cretinism in chil-
dren), there is decreased serum free T4 and increased serum TSH.
Remember: About 93% of the metabolical ly active hormones secreted by the t hyroid gland is t hy-
roxine, and 7% triiodothyronine. However, almost all of the thyroxine is eventually converted to tri-
iodothyronine in the tissues, so that both are functionally important. The functions of these two
hormones are qualitatively the same, but they differ in rapidity and intensity of action. Triiodothyro-
nine is about four times as potent as t hyroxine, but it is present in the blood in much smaller quanti-
t ies and persists for a much shorter t ime than does thyroxine.
Saad Alqahtani, Twitter @saaddes
hormones
Releasing hormones are synthesized in the:
• posterior pituitary
• hypothalamus
• anterior pituitary
• ovary
SAADDES
88
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hypothalamus
The secretions of the anterior pituitary are controlled by hypothalamic releasing and inhibitory
hormones (factors), which are secreted within the hypothalamus itself and then conducted to the
anterior pituitary through min ute blood vessels called t he hypothalamic-hypophyseal portal
system .
The hormones of the posterior pituitary (ADH and oxytocin) are synthesized in neuroendocrine
cells located within the supraoptic and paraventricular nuclei of the hypothalamus. The synthesized
hormones are packaged in granules that are transported dow n the axon of the cell and stored in
nerve terminals located in the neurohypophysis (posterior pituitary).
Uonnones of tlu: lh poth.ll.unus
Jlormo.nt Sou ret Tar~CI Acljon ($)
SAADDES
Growth hormone- llypothalamus Adenohypophysis Stimulates secretion of growth hormone
releasing; hormone (somatotropes)
(GRI I)
Growth hormone- llypothalamus Adenohypophysis Inh ibits Sc(>n:lion of growth honnone
inhibiting: hormone (somatotropes)
(SontatOSLatin)
Cortic.oLropin- llypothalamus Adenohypophysis Stimulates secretion of adrenO<:urlicotropic
releasing; hormone ((."'rticotropes) hormone (ACTI1)
(CRII)
Th>•rotropin- llypothalamus Adenohypophysis Stimulates secretion of thyroid -stimuhlling
releasing; hormone (thyrotrop«) hormone (TSI I) and prolactin
(TRH)
Gonad otropin- llypothalamus Adenohypophysis Stinml at~s rd~as~ of FSI I and LJI
re leasin~ hormone (gonadotropes)
(GNRII)
Prola<:1in- ll)'pOthalamus Ad~nOh)'pOphysis Stimulates se~,-et ion of prolactin
rtlc.asing hormone (lac1o1ropes)
(PRH)
Prola<:1in- ll)'pOthalamus Ad~nOh)'pOphysis Inh ibits sccn:lion of prolactin
inhibiting hormone (lac1o1ropes)
(Pil l)
Saad Alqahtani, Twitter @saaddes
hormones
ADH is formed primarily in the paraventricular nuclei and oxytocin is formed
primarily in the supraoptic nuclei of the hypothalamus.
ADH and oxytocin are secreted by the posterior pituitary.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
89
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false. the second is true
Remember: ADH (also called vasopressin) and oxytocin are synthesized in neuroendo-
crine cell s located within the supraoptic and paraventricular nuclei of the hypothalamus.
The synthesized hormones are packaged in granules that are transported down the axon
of the cell and stored in nerve terminals located in the neurohypophysis (posterior
pituitary).
Note: ADH is formed prim arily in the supraoptic nuclei and oxytocin is formed primarily
in the paraventricular nuclei of the hypothalamus.
ADH acts on the kidneys to regulate the volume and osmolality of urine. When plasma ADH
levels are low, a large volum e of urine is excreted (d iuresis) and the urine is dilute. When
SAADDES
plasma levels are high, a small volum e of urine is excreted (antidiuresis) and the urine is
concentrated. Note: ADH decreases the production of u rine by increasing the reabsorp-
tion of water by the renal tu bules (ADH increases the water permeability of the collecti ng
ducts and distal t ubules). Without ADH, there would be ext reme loss of water into the u ri ne.
Oxytocin is secreted by t he posterior portion of the pituitary (neurohypophysis) in
response to dilation of t he cervix and to suckling. Oxytocin stimulates the smooth muscle
of the uterus. Oxytocin also p romotes the contracti on of myoepithelial cell s surrounding
the sac-like alveoli of the mamm ary glands, resulting in the ej ection of milk during breast-
feeding.
Oxytocin release causes a positive feedback mechanism to begin. Uterine contractions
push t he fetus against the cervical opening, which causes more oxytocin to be secreted.
The rise in oxytocin causes greater uterine contractions and the cycle continues until
parturition is co mplete.
Saad Alqahtani, Twitter @saaddes
hormones
All of the following are factors and conditions that decrease insulin secretion
EXCEPT one. Which one is the EXCEPTION?
• decreased blood glucose
• fasting
SAADDES
• somatostatin
• increased blood free fatty acids
• alpha-adrenergic activity
90
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• increased blood free fatty acids
** * Increased blood free fatty acids increases insulin secretion.
Insulin is the primary anabolic hormone that is responsible for maintaini ng the upper limit of blood
glucose and free fat ty acid levels. Insulin achieves t his objective by promoting glucose uptake and
utilization by muscle and adipose ti ssue, increasing glycogen storage in liver and muscle and reducing
glucose output by the liver. Insulin promotes protein synthesis from amino acids and inhibits protein
degradation in peripheral tissues. Insuli n also promotes triglyceride synthesis in the liver and ad ipose
tissue and represses lipolysis of adipose triglyceri de stores. Finally. insulin regulat es metabo lic
homeostasis through effect s on satiety. Note: Partial or complete loss of insuli n's action result s in severe
hyperglycemia, dyslipidemia and d iabetes mellitus.
Insulin lowers blood sugar by binding to tyrosine-kinase receptors on striated muscle (skeletal and car-
d iac) and adipose cell membranes, resulti ng in a cascade that translocates GLUT-4 glucose transporters to
SAADDES
the cell membrane. GLUT-4 transporters allow facil itated d iffusion of glucose into the muscle and fat cells.
ln!.'rea!led blood glucosc- Ikcrcascd blood gluco~c
lncrcas.cd bliXId free fany adds Fasting
ln~Yca!Oed blood ami1\0 acids Som:uos:t.:uin
Gl hom\O"e:~ (gascrin, o:'holccyl!tokini.n.. GIP) o.-:.drcnergic acti\'ity
Glucagoo.. Growth OOtmo.,e. rot1isul LCJ)Iin
Parasympathetic s•imulatioo. ai,'!Ct)'lcholi.n.c
P·adtMcrgk s-timulatio"
lnsuli.nres-i llta.nce (o~,.-ityl
Sulfooylurca.i d1ugs (glyburidc. tolbutamide)
1. Insulin is secreted by the beta cells in the islets of Langerhans of the pancreas.
8 2. Maj or stimuli for insulin secretion include increased serum g lucose and some amino acids
(particularly arg inine and lysine).
3. Key point: Insulin promotes the utilization of carbohyd rates for energy, whereas it
depresses the utilization of fats. Conversely, lack of insulin causes fat util ization mainly to the
exclusion of glucose util ization, except for brain tissue.
4. Clinical manifestations of hypoglycemia include: hunger, nervousness, shakiness,
perspiration, dizziness or lightheadedness. sleepiness, confusion, d ifficult y speaki ng and
feeling anxious or weak. Important: Seizures can occur as a result of severely low glucose
levels.
Saad Alqahtani, Twitter @saaddes
hormones
Glucagon, a hormone secreted by the alpha cells of the islets of Langerhans
when blood glucose concentration falls, has several functions that are
diametrically opposed to those of insulin.
The most important function of glucagon is to increase the blood glucose
concentration, an effect that is exactly the opposite that of insulin.
SAADDES
• both statements are true
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
91
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Glucagon is the primary "counterregulatory" hormone that increases blood g lucose
levels through its effects on liver g lucose output. The major effects of g lucagon on
glucose metabolism are ( 1) breakdown of liver g lycogen (glycogenolysis) and
(2) increased gluconeogenesis in the liver. Both of these effects greatly enhance the
availability of glucose to the other organs of the body. For these reasons, glucagon is
found in emergency medical kits. It can be used on an emergency patient who has
diabetes and is suffering from hypoglycemia.
Glucagon is secreted by the alpha cell s in the islets of Langerhan s of the pancreas
in response to a fall in the blood glucose level. Glucagon is frequently ca lled the
SAADDES
hyperglycemic facto r. Glucagon has many of the opposite effects of insulin.
Note: Insulin is secreted in response to a rise in the blood glucose level and causes
glycogenesis in the liver (conversion of g lucose to g lycogen).
Glucagon release by alpha cells is promoted by the following:
• A fall in blood glucose level (hypoglycemia) - this is by far the most
potent factor that controls glucagon secretion
• Sympathetic stimulation
• Circulating catechol amines via ~ 2-adrenergic receptors
• Increased level of amino acids (especially arginine and alanine) in the blood
plasma. *** In this instance, the glucagon and insulin responses are not
opposites.
Factors that decrease glucagon secretion: a rise in blood g lucose level, insulin,
somatostatin, free fatty acids and ketoacids.
Note: Somatostatin (aka, growth hormone inhibitory hormone) acts locally within the
islets of Langer hans themselves to depress the secretion of insulin and glucagon.
Saad Alqahtani, Twitter @saaddes
hormones
As the acidic stomach contents pass into the small intestine, the low pH
triggers secretion of the hormone _ _ _ into the blood.
• cholecystokinin
• gastric inhibitory peptide
SAADDES
• gastrin
• secretin
92
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• secretin
Several hormones control Gl secretion and moti lity of the Gl tract:
• Secretin: was the first Gl hormone discovered and is secreted by the "S" cells in the mucosa of
the duodenum in response to acidic gastric juice emptying into the duodenum from the pylorus
of the stomach. Secreti n functions as a type of firefighter: secretin stimulates the pancreas to
release a flood of bicarbonate base which neutralizes the acid. Secretin has the following
functions:
•Inhibits stomach moti lity and gast ric acid secretion
• Stimulates the pancreatic duct cells to secrete a fluid that contains a lot of bicarbonate ions
but is low in enzymes
• Stimulates the secretion of bile from the gallbladder
• Cholecystokinin plays a key role in facilitating digestion within the small int estine. Cholecys-
SAADDES
tokinin is secreted by the "I" cells in the mucosa of the duodenum and jejunum mainly in response
to digest ive product s of fat. fatty acids and monoglycerides in the intest inal contents. This hor-
mone strongly contracts the gallbladder, expelling bile into the small intestine where the bile in
turn plays important roles in emulsifying fatty substances, allowing them to be digested and ab-
sorbed. Cholecystokinin also inhibits stomach contraction moderately. Therefore, at the same
time that this hormone causes emptying of the gallbladder, it also slows the emptying of food
from the stomach to give adequate time for digestion of the fats in the upper intestinal tract.
• Gastric inhibitory peptide (GIP) is secreted by the mucosa of the upper small intesti ne mainly
in response to fatty acids and amino acids but to a lesser extent in response to carbohydrates. It
has a mild effect in decreasing motor activity of the stomach and therefore slows emptying of gas-
t ric contents into the duodenum when the upper small intestine is already overloaded with food
products.
• Gastrin is a major physiological regulator of gastric acid secretion. Gastrin also has an important
trophic or growth-promoting influence on the gastric mucosa. Gastrin is secreted by "G" cells of
the antrum of the stomach in response to sti muli associated with ingestion of a meal (e.g., disten-
sion of the stomach, productsof protein degradation and gastrin releasing peptide, which itself
is released by nerves of gastric mucosa during vagal stimulation). The pri mary actions of gastrin
are (1) stimulation of gastric acid secretion and (2) sti mulation of growth of the gastric mucosa.
Saad Alqahtani, Twitter @saaddes
hormones
The enterogastric reflex. which is initiated when the duodenum fills with
_ _ _ , inhibits the "pyloric pump:' thereby inhibiting gastric motility and
emptying.
• bicarbonate
SAADDES
• acid chyme
• enkephalins
• water
93
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• acid chyme
As acid chyme enters the duodenum, the decreasing pH inhibits gastrin secretion and
causes the release of negative o r "stop" signals in the duodenum. These take the form
of hormones cal led enterogastrones, which include cholecystokinin (the most im-
portant"stop" signal), secretin and gast ric inhibitory peptide (GIP). These hormones
inhibit stomach secretion and motility and allow time for the digestive process to
proceed in the duodenum before it receives more chyme.
The enterogastric reflex also reduces motili ty and forcefully closes the pyloric sphinc-
ter. Eventuall y, as the chyme is removed, the pH increases, and gastrin and the"go" sig-
SAADDES
nal resumes, and the process of digestion occurs all over again. The process of"go" and
"stop" signals continues until stomach emptying is complete.
Important point: Enterogastrones are released by the small intestine in response to
the acidity of the duodenal chyme, the presence of amino acids and the presence
of free fatty acids in the chyme.
Saad Alqahtani, Twitter @saaddes
hormomes
All of the following statements concerning aldosterone are true EXCEPT one.
Which one is the EXCEPTION?
• causes Na• retention
• causes K• excretion
SAADDES
• renin controls it
• acts at the distal tubu le
• is produced in the kidney
94
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• is produced in the kidney
*** This is false; aldosterone is produced in the adrenal cortex.
Aldosterone is the principal mineralocorticoid and is secreted by cells located in the zona
glomerulosa of the ad renal cortex. Aldosterone promot es reabsorption of sodium into t he
blood from the glomerular filtrate. Potassium is lost in t he urine. Note: Increased blood
aldosterone levels will result in high plasma volume and low potassium levels in the plasma.
The major target of aldosterone is the distal tubule of t he kidney, where aldosterone
stimulates exchange of sodium and potassium. Three primary physiologic effects result:
• Increased resorption of sodium: sodium loss in urine is decreased under aldosterone
stimulation
• Increased resorption of water, with consequent expansion of extracellular fluid
SAADDES
volume. This is an osmotic effect directly related to increased resorption of sodium.
• Increased renal excretion of potassium
The two most significant regulators of aldosterone secretion are:
1. Concentrations of potassium ion in extracellular fluid: Small increases in blood levels
of potassium strongly stimulate aldosterone secretion.
2. Angiotensin II: Activation of the renin-angiotensin system as a result of decreased
renal blood flow (usually due to decreased vascular volume) results in release of
angiotensin II, which stimulates aldosterone secretion. Important: Decreased sodium
concentration causes the j uxtaglomerular cells of t he kidneys to secrete renin, which
converts angiotensinogen to angiotensin I. Angiotensin I is converted to angiot ensin II,
which in turn, stimulates t he adrenal cortex to release aldosterone.
Remember: ANP's (atrial natriuretic peptide) physiologic effects are opposite to that of
aldosterone.
Note: Addison's di sease is adrenocortical insufficiency. Common sym ptoms include
hypotension, hyperpigmentation, muscle weakness, anorexia, hypoglycemia and hyperkalem ic
acidosis.
Saad Alqahtani, Twitter @saaddes
hormones
Oral contraceptives work by:
• inhibiting foll icle formation by eliminating the LH surge
• inhibiting ovulation by eliminating the LH surge
• inhibiting foll icle fo rmation by eliminating the FSH surge
SAADDES
• inhibiting ovulation by eliminating the FSH surge
95
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• inhibiting ovulation by eliminating th e LH surge
Oral contraceptives ("the pill") are pills consisting of one or more female sex
hormones taken by women to prevent pregnancy. Most oral contraceptives are
combined pills that contain synthetic estrogen-like (ethinyl estradiol and mestranol)
and progesterone-like (norethindrone,norethynodrel, ethynodiol and norgestrel)
substances.
These synthetic hormones apparently prevent the rise in luteinizing hormone. This
in turn, prevents ovulation. The exact mechanism is thought to be as follows: In the
presence of either estrogen or progesterone (or a synthetic substitute), the
SAADDES
hypothalamus fa ils to secrete the normal surge of LH-releasing factor (also called
gonadotropin-releasing factor) . This then inhibits the release of luteinizing hormone
from basophils of the anterior pituitary gland. Subsequently, ovulation does not
occur.
1. The main reason for using synthetic estrogens and progestins is that the
natural hormones are almost entirely destroyed by the liver within a short
t ime after they are absorbed from the Gl tract and portal circulation.
However, many of the synthetic hormones can resist this destructive
propensity of the liver, thus allowing oral administration.
2. Ovulation occurs as a result of the estrogen-induced LH surge.
3. Unlike other steroid hormones, all estrogens have an aromatic A ring.
Saad Alqahtani, Twitter @saaddes
hormones
About 93% of the metabolically active hormones secreted by the thyroid
gland is thyroxine (T4 ), and 7% triiodothyronine (T3 ).
T4 is deiodinated and then T3 typically binds to the TH receptor.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
96
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
The thyroid secretes two major hormon es, thyroxine and triiodothyronine, commonly called
T4 and T3, respectively. Both of these hormon es profoundly increase the metabolic rate of the
body.Thyroid secretion is controlled primarily by thyroid-stimulating hormone (TSH) secreted
by the anterior pitu itary gland. Note: Thyrotropin-releasing hormone (TRH) is a hormone re-
leased by the hypothalamus that communicates with the pituitary gland and stimulates release
of thyroid-stimulating hormone.
Follicular cells of the thyroid gland synthesize thyroglobulin conta ining tyrosine and secrete it
into the colloid-containing regions of the foll icles. Here the tyrosine residues of thyroglobulin
are iodinated. Iodinated tyrosine molecules bind to one another forming thyroglobul in bound
SAADDES
triiodothyronine (T3) and thyroxine (T4) which remain stored in the colloid region of the
follicle. When thyroid stimulating hormone (TSH) is present, the T3 and T4 bound
thyroglobu lin is transported back into the follicular cells and lysosomes release T3 and T4 from
thyroglobulin into t he circulation.
About 93% of the metabol ically active hormones secreted by t he thyroid gland is thyroxine, and
7% triiodothyronine. However, almost all of the thyroxine is eventually converted to triiodothy-
ronine in the tissues, so t hat both are functionally importa nt. The functions of these two hor-
mones are qualitatively t he same, but they differ in rapidity and intensity of action.
Triiodothyronine is about four times as potent as thyroxine, but it is present in the blood in much
smaller quantit ies and persists for a much shorter t ime than does thyroxine.
These hormones enter the bloodstream and produce the following actions:
• Important for normal growth and development (especially the brain)
• Affect many metabolic processes and the metabolic rate
• Increase oxygen consumption and heat production
Note: A dietary iodine deficiency will increase the secretion of thyroglobulin (as opposed to
thyroxine, triiodothyronine or TSH).
Saad Alqahtani, Twitter @saaddes
hormones
Catecholamines are synthesized from:
• alanine
• tyrosine
• proline
• arginine
SAADDES
97
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• t yro sine
The water-soluble co mpounds epinephrine (adrenaline) and norepinephrine (noradrena-
line) are catecho lamines. They are synthesized from tyrosine.
Secretion of these hormones is stimulated by acetylcholine release from pregangli onic
sympathetic fibers innervating the adrenal medulla. Common stimuli for secretion of
adrenomedullary hormones include exercise, hypoglycemia, hemorrhage and emotional
distress. Following release into blood, these hormones b ind adrenergic receptors on
target cell s where the hormones induce essentially the same effects as direct sympathetic
nervous stimulation.
Outside t he nervou s system, norepinephrine and its methylated derivative epinephrine
SAADDES
act as regulators of carbohydrate and lipid metabolism. Norepinephrine and
epinephrine increase the degradation of triacylglycerol and glycogen as well as increase
the output of the heart (specifically, epinephrine) and blood pressure. These effects are
part of a coordinated response to prepare the individual for emergencies and are often
called the "fight or flight" reactions.
Norepinephrine can be released in 2 ways:
• By the adrenal medulla into the bloodstream (as discussed above)
• Directly onto an organ by a postgangli onic sympathetic (adrenergic) neuron that
stores norepinephrine
Important: The effects are more widespread when norepinephrine is released into the
bloodstream by the adrenal medulla as opposed to directly onto an organ by a
postganglionic sympathetic neuron.
Note: Pheochromocytoma is a tu mor of the adrenal medulla with signs and symptoms
caused by excessive catecholamines (epinephrine &norepinephrine) including tachycardia,
hypertension, anxiety and sweating. It is usually associated with excessive excretion of 3-
methoxy-4-hydroxymandelic acid (VMA).
Saad Alqahtani, Twitter @saaddes
hormones
All of the following are affected by epinephrine and/or norepinephrine
EXCEPT one. Which one is the EXCEPTION?
• blood g lucose
• tota l peripheral resistance
SAADDES
• heart rate
• kidney function
98
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• kidney function
The adrenal medulla is a specialized ganglion of the sympathetic nervous system.
Preganglionic fibers synapse d irectly on chromaffin cells in the adrenal medulla.
These cells secrete epinephrine (80%) and norepinephrine (20%) into t he
circulation. Both of these hormones are water-soluble, direct-acting adrenergic
agonists and are biosynthesized from the amino acid tyrosine. Water-soluble
hormones cannot pass through t he plasma membrane and must have a plasma
membrane receptor.
Epinephrine (adrenalin) has the fol lowing effects:
SAADDES
• Stimulates glycogenolysis and gluconeogenesis, which tend to raise blood
glucose levels. Also stimulates lipolysis in adipose tissue (break-down oftriglycer-
ides into glycerol and fatty acids)
• Increases the rate, force and amplitude of the heartbeat
• Constricts blood vessels in skin, mucous membranes and kidneys
• Dilates bronchioles in the lungs, dilates blood vessels in skeletal muscle and
relaxes bronchiolar smooth muscle
• Activates muscle glycogen phosphorylase
Norepinephrine (noradrenalin) has t he following effects:
• Increases the heart rate and the force of contraction of heart muscle
• Promotes lipolysis in adipose tissue
• Constricts blood vessels in almost all areas of the body, thus increasing total
peripheral resistance
Saad Alqahtani, Twitter @saaddes
hormones
Parathyroid hormone causes which of the following to occur?
• removal of ca lcium via the kidney
• removal of ca lcium from bone
• removal of calcium via the Gl system
SAADDES
• none of the above
99
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• removal of calcium from bone
Parathyroid hormone (PTH) is secreted by chief cells in the parathyroid gland in
response to decreased plasma-calcium levels. The plasma-calcium level is the major
controller of parathyroid hormone secretion. PTH is a principal controller of calcium
and phosphate metabolism and is involved in the remodeling of bone. PTH increases
the plasma-calcium concentration and decreases the plasma-phosphate concentra-
tion.
PTH has three modes of action:
1. Increases calcium removal from storage in bone and increases absorption of
SAADDES
calcium by intestines, increasing blood calcium levels.
2. Acts on the kidneys to decrease calcium excretion and increase phosphate ex-
cretion in the urine. Also stimulates 1-alpha-hydroxylase in the kidneys.
3. Increases the absorption of calcium in the Gl tract indirectly by causing the
kidney to produce vitamin D (1 ,25-dihydroxycholecalciferol).
1. Hyperparathyroidism causes extensive bone decalcification and is
Notes marked by extremely high blood calcium levels and low blood phosphate
levels. This leads to muscular weakness.
2. Hypoparathyroidism (tetany) causes decreased bone resorption,
decreased renal Ca•· reabsorption, increased renal phosphate reabsorption
and decreased production of the active form of vitamin D (1,25-
dihydroxycholecalciferol). Together these effects decrease serum calcium
and increase serum phosphate.
***A diet deficient in calcium will result in production of PTH and bone resorption.
Saad Alqahtani, Twitter @saaddes
hormones
Which of the following hormones' secretion is stimulated by stomach disten-
tion?
• gastrin
• cho lecystokinin (CCK)
SAADDES
• secretin
• gastric inhibitory peptide (GIP)
• all of the above
100
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• gastrin
Gastrin is a maj or physiological regulator of gastric acid secretion. Gastrin also has an impor-
ta nt trophic or g rowth-promoting influence on t he ga stric mucosa. Gastrin is synthesized in G
cells, which are located in gastric pits, primarily in the antrum region of the stomach and bi nds
receptors found predom inantly on parietal and enterochromaffin-like cell s.
G l U oJ moncs
Hormone Source S timuli for Release Action (s)
Gastrin .. C .. cells of the antrum Stimuli associa[ed with Stimulates gastric acid sec-re[ion
o f the S[Oil\ilCh ingestion of a meal, such Stimulation of growth of the gastric- muc.os.a
SAADDES
as distension of the
stom.ach. the products of
proteins and GRP
Cholecys[OJcinin ••r · ctlb in the-muc-.os.a Digestive- pi'Oducts of Contract." the gallbladder expelling bile into the-
of the duodenum and fat, fany acids, and small imestine
jejunum monoglyc.erides in the Inhibits S[Om.ach contraction moderately
inteslinal contem.s
Secretin "S.. celb in the mucosa Acidic gastric j uice- Principal stimulus fo r the pancre-as [0 secrete a
of the duodenum emptying i nto the bic.arbona[e-rich fluid which neurralizes the acid
duode.num
Gastric inhibitory Mucosa of the upper Mainly fatcy acid.~ and Mild et)"'ec[ of decre-asing 11\0[0r acti\'ity of the
peptide small imestine amino acid.~ but [0 a stomach and £here fore slows emptying o f gastric
lesser extem in response con tent.~ imo the duodenum when t11e uppe-r small
[0 carbohydrate intestine is already overloaded with food produC[S
1. The five (-term inal amino acids of gastrin and cholecystokinin are identical, which
explains their overlapping biological effects.
2. Excessive secretion of gastrin, or hypergastrinemia, is a well-recognized cause of
a severe d isease known as Zollinger-Ellison syndrome.
Saad Alqahtani, Twitter @saaddes
hormones
Which of the following gastrointestinal hormones seems to be the most
potent in causing a moderate increase in insulin secretion?
• gastrin
• gastric inhibitory peptide (GIP)
SAADDES
• cholecystokinin (CCK)
• secretin
101
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• gastric inhibitory peptid e (GIP)
These hormones are released in the gastrointestinal tract after a person eats a meal.
They then cause an "anticipatory" increase in blood insulin in preparation for the glu-
cose and amino acids to be absorbed from the meal. These gastrointestinal hormones
generally act the same way as amino acids to increase the sensitivity of insulin response
to increased blood g lucose, almost doubling the rate of insulin secretion as the blood
glucose level rises.
Remember: Gastric inhibitory peptide (GIP) is secreted by the mucosa of the upper
small intestine, mainly in response to fatty acids and amino acids but to a lesser extent
in response to carbohydrates. It has a m ild effect in decreasing motor activity of the
SAADDES
stomach and therefore slows emptying of gastri c contents into the duodenum when
the upper small intestine is already overloaded w ith food products.
Important: Other hormones that either d irectly increase insulin secretion or potenti-
ate the glucose stimulus for insulin secretion include glucagon, growth hormone, cor-
t isol and, to a lesser extent, progesterone and estrogen. The importance of the
stimulatory effects of these hormones is that prolonged secretion of any of them in
large quantities can occasionally lead to exhaustion of the beta cells of the islets of
Langer hans and thereby increase the risk for developing d iabetes mellitus.
1. GIP is also thought to have significant affects on fatty acid metabolism
through stimulation of lipoprotein lipase activity in adipocytes.
2. GIP receptors are seven-transmembrane proteins found on beta cells in the
pancreas.
3. It has been found that type 2 d iabetics are not responsive to GIP.
Saad Alqahtani, Twitter @saaddes
hormones
A tumor of the adrenal gland is causing your patient to conserve sodium in
the renal tubules causing increased blood volume, pressure and edema.
Where is the location of this adenoma?
• zona glomerulosa of the adrenal cortex
SAADDES
• zona fasciculata of the adrenal cortex
• zona reticu laris of the adrenal cortex
• adrenal medulla
102
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• zona glomerulosa of the adrenal cortex
Hurmuru.·s of Ihe \dn·n.tl Glamh
Hor mone Source Ta rget Action (s)
A ldosterone AdrenaJ col'lex Kidney Stimulate$ kidney tubules 10 consen•e sodium, which
(zona glomerulosa) in. rum, rriggers the release of ADH and the resulting
conservation of water by the kidney
Conisol Adrenal conex General Promotes gluconeogenesis, lipolysis, proteolysis, and
(zona fasciculata) inununosuppression
Jn large amounts, it has an anti·innam matory e fte ct
Adr enal androgens AdrenaJ col'lex Sex organs E.xact role uncenain, but may suppon sexual ftmction
(zona reticularis) Other effectors
SAADDES
Adrenal estrogens Adre.nal conex Sex organs Thought to be physio1ogica1ly insignificant
(zona reticularis)
Epinephrine Adrenal medulla Sympathetic Enhance$ and prolong..~ the effects of the.sympathetic
effectors division of the autonomic nervous system
Norepinephrine /\drena1 medulla Sympathetic Enhance$ and prolong..~ the effects ofrhe sympathetic
effectors division of the autonomic nervous system
Important point: Cortisol (glucocorticoid} influences carbohydrate, lipid and protein
catabolism. Glucocorticoid s promote gluconeogenesis by inducing synthesis of the enzyme
phosphoenolpyruvate carboxykinase (PEPCK}.
1. The mineralocorticoid aldosterone and the glucocorticoids are collectively called
the corticosteroids.
2. All steroid hormones are synthesized from cholesterol.
3. Mineralocorticoids have an aldehyde group at C-18.
4. Estrogens are di stinguished by the aromatic nature of ring A.
5. The corticosteroids are d istinguished from the progestins by the presence of
additional hydroxyl groups.
6. Testosterone is a precursor oftwo other hormones, DHT and estradiol.
Saad Alqahtani, Twitter @saaddes
hormones
Cortisol is the primary glucocorticoid produced by the adrenal cortex gland.
Cortisol's principal physiological actions include all of the following EXCEPT
one. Which one is the EXCEPTION?
• increase hepatic gluconeogenesis
SAADDES
• increase hepatic glycogenolysis
• increase protein catabolism
• stimulation of fat deposition and inhibition of lipolysis
• inhibit ACTH secretion (negative feedback mechanism)
• maintenance of blood pressure by sensitizing arteri oles to the action of noradrena-
line
• rena l excretion
103
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• stimulation of fat deposition and inhibition of lipolysis
*** This is false; g lucocorticoids (mainly, cortisol) promote mobilization of fatty
acids from adipose tissue and stimulate lipolysis.
Hormones I h.tt \ffl't:l \h·l.thuli!r!int
Horrnone Metabolic EffHts
Insulin Promotes: Glucose uptake into cells
Amino acid uptake into cells
Glycogenesis, lipogenesis, protein synthesis
Inhibits: Lipolysis, gluconeogenesis
SAADDES
Glucagon Promotes : Glycogenolysis, gluconeogenesis
Thyroxine Promotes : Glycogenolysis, gluconeogenesis, lipolysis
Growth honnone Promotes: Amino acid uptake into cells, protein synthesis, glycogenolysis, lipolysis
Cortisol P romotes : Gluconeogenesis, lipolysis, breakdown of protein
Testosterone Promotes : Protein synthesis
Remember: Cushing's syndrome results from hypercortisolemia. If the basis of
the disorder is increased pituita ry adrenocorticotropin secretion, t he d isorder is cal led
Cushing's disease. Common symptoms of Cushing's syndrome include centripetal
fat distribution, muscl e wasting, proximal muscle weakness, t hin skin with abdominal
striae, capillary fragility, insulin resistance and polycythemia.
Note: Individuals with Cushing's syndrome can develop "moon facies:·
Saad Alqahtani, Twitter @saaddes
hormones
Which of the follow ing is classifi ed as a "stress hormone"?
• growth hormone (GH)
• thyroid-stimulating hormone (TSH)
• adrenocorticotropic hormone (ACTH)
SAADDES
• follicle-stimul ating hormone (FSH)
This hormone stimulates the excretion of:
• cortisol
• adrenal in
• aldosterone
• two of the above
104
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. adrenocorticotropic hormone (ACTH)
2. cortisol
ACTH secretion is controlled by the hypothalamus, to w hich t he pituita ry gland is
attached. When the body is stressed, corticotropin-releasing hormone (CRH)
produced by the hypothalamus travels throug h a portal system to the anteri or lobe
of the pituitary, w here the hormone induces the production and secretion of ACTH by
the basophils of the pars distalis. ACTH in turn stimulates the adrenal cortex to
synthesize and secrete cortisol.
1. The secretion of aldosterone from t he adrenal cortex is not induced by
SAADDES
ACTH. Major stimuli fo r aldosterone production are a rise in angiotensin II
and a ri se in serum [K•]. The major inhibitory signal against the secretion of
aldosterone is ANP (atrial natriuretic peptide). Aldosterone's primary effect
is on the kidney tubu les, where it stimulates sodium retention and potassium
excretion.
2. Ana lysis of ACTH is used as an indicator of pituitary function and is use-
fu l in the differential diagnosis of the following: Add ison's disease, congenital
adrenal hyperplasia and Cushing's syndrome.
3. ACTH deficiency is characterized by adrenal insufficiency symptoms such
as weight Joss, Jack of appetite (anorexia), wea kness, nausea, vom iting and
low blood pressure.
4. Adrenocortical insufficiency - acute adrenal crisis can occur in patients
who have been t reated w ith long-term corticosteroids. This impairs the
adrenal cortex from producing co rtisol.
Saad Alqahtani, Twitter @saaddes
hormones
Cortisol (hydrocortisone) has a direct inhibitory effect on which structures?
Select all that apply.
• adrenal cortex
• hypothalamus
SAADDES
• anterior pituitary gland
• posterior pituitary gland
105
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hypothalamus
• anterior pituitary gland
The release of cortisol is controlled primarily by ACTH, which is secreted by
basophils in the pars distalis of the anterior pituitary gland. The release of ACTH in
turn, is influenced by co rticotropin-releasing hormone (CRH) from the
hypothalamus. Cortisol exerts an inhibitory influence on both ACTH and CRH
release by way of negative feedback.
Feedback circuits are at the root of most control mechanisms in physiology and are
particularly prominent in the endocri ne system. Instances of positive feedback cert-
ainly occur, but negative feedback is much more common. Negative feedback is
SAADDES
seen when the output of a pathway inhibits input to the pathway. The heating system
in your home is a simple negative feedback circuit. When the furnace produces
enough heat to elevate the temperatu re above the set point of the thermostat, the
thermostat is tri ggered and shuts off the furnace (heat is feeding back negatively on
the source of heat). When the temperature drops back below the set point, negative
feedback is gone and the furnace comes back on.
Cortisol is the main glucocorticoid produced and secreted by the cells of the zona
fasciculata in the adrenal cortex. Cortisol allows glucagon and epinephri ne to work
more effectively at their ta rget t issues, but antagonizes the actions of insulin. By fa r
the best-known metabolic effect of cortisol and other glucocort icoids on
metabolism is their ability to stimulate gluconeogenesis (formation of carbohyd rate
from proteins and some other substances) by the liver, often increasing the rate of
gluconeogenesis as much as 6- to 10-fold.
Important: A patient taking cortisol for a long period of time may experience
atrophy of the adrenal cortex due to inhibition of ACTH production.
Saad Alqahtani, Twitter @saaddes
hormones
The placenta secretes five hormones that are essential to pregnancy. Which of
the following is NOT one of them?
• oxytocin
• progesterone
SAADDES
• relaxin
• estrogen
• human chori onic gonadotropin (hCG)
• human placental lactogen (hPL)
106
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• oxytocin
llormunrs ol Othl·r \ laJor Endocrilll' G lands
Hor mone Source Target Action (s)
Testosterone Testis Spermatogenic cells Promotes the de.velopment of male
Muscle reproductive system and male secondary
Bone tissue se.xual characteristics
Other tissues
Estrogen Ovarian follicles U tenL'i Promotes the development of female
Mammary glands reproductive. system, female breasts and
Other tissue~'i female secondary sexual characteristics
Proge,'iterone Corpus luteum U terus Stimulates secretion of ..uterine milk" by the
SAADDES
Other tissues uterine endometrial gland<; and promotes
development o f secretory ap~.,aratus of breasts
Human chorionic Chorion (fetal Ovary Promotes growth of corpus luteum and
gonadotropin tissue component se.cretion of estrogens and progesterone. by
(hCG) of the placenta) corptL'i luteum
During pregnancy, human chorionic gonadotro pin (hCG) is secreted by the placenta and
circulates both in the mother and fetus. It promotes growth of the corpus luteum and
secretion of estrogens and progesterone by corpus luteum.
The ovaries of a female produce ova, the female sex hormones (progesterone and estro-
gen) and follicles. The corpus lute um is a yellowish mass of cell s that forms from an
ovarian follicle after the release of a mature egg (ovul ation). If the mature egg is not
fe rtilized and pregnancy does not occu r, the corpus luteum retrogresses to a mass of
scar tissue (corpus albicans) which eventually disappears. If the mature egg is fertilized
and pregnancy does occur, the corpus luteum does not degenerate but pe rsists for
several months.
Saad Alqahtani, Twitter @saaddes
hormones
Somatostatin acts by both endocrine and paracrine pathways to affect its tar-
get cells. A majority of the circulating somatostatin appears to come from the
and ___.
• gallbladder, large intestine
SAADDES
• pancreas, gastrointestinal tract
• stomach, adrenal medulla
• bladder, small intestine
107
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• pancreas, gastrointestinal tract
Somatostatin was fi rst discovered in hypothalamic extracts and ident ified as a hormone t hat inhibited secre-
tion of grow th hormone. Subsequently, somatostatin was found to be secreted by a broad range oftissues in-
cluding the: pancreas, intestinal tract and regions of the central nervous system outside the hypothalamus.
Somatostatin acts by both endocrine and paracrine pathways to affect its t arget cells. A majority of the circu-
lating somatostatin appears to come from t he pancreas and gastrointestinal tract. If one had to summarize the
effects of somatostatin in one phrase, it would be: "somatostatin inhibits the secreti on of many other hor-
mones:'
Effects of somatostatin (growth hormone inhibitory hormone):
• Inhibits the secretion of growth hormone from the pitui tary gland
• Acts locally within the isl ets of langerhans t hemselves to depress the secretion of insulin and glucagon
• Inhibits t he secretion of many of t he other Gl hormones including gastrin, cholecystokinin, secretin and
vasoactive intestinal peptide
SAADDES £xcns
Action
Hype.rglyc-emia
Hypoglycemia
Ga..<>lrin Jnducc acid producing
4
Poorly defined Stomach ulcers
cells of the stomach to
produce acid intestines stomach and
iniC$tinC$
Causes intestinal cdls Unclear Unclear No symptoms
to s.«n:te water and
salts into the intestine
Saad Alqahtani, Twitter @saaddes
hormones
Prolactin is said to be under "predominant inhibitory control:' Which ofthe
following explains why?
• In normal cond itions, prolactin is constantly synthesized in the anterior pituitary.
Only when prolactin is not needed does the inhibitory mechanism kick in.
• In normal conditions, prolactin inhibitory facto r is produced by the hypothalamus.
SAADDES
Only when prolactin is needed does the hypothalamus stop synthesis and secretion.
• In normal conditions, prolactin is synthesized by the hypothalamus. However, pro-
lactin inhibitory hormone prevents the secretion unless prolactin is needed.
• In normal conditions, prolactin inhibitory factor is produced by the anterior pituitary.
Only when prolactin is needed does th is stop and the ovaries are able to produce
prolactin.
108
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• In normal conditions, prolactin inhibitory factor is produced by the hypothalamus.
Only w hen prolactin is needed does the hypothalamus stop synthesis and secretion.
Prolacti n is a sing le-chain protein hormone this is structurally related to growth hormone.
Prolacti n is secreted by lactotropes in the anterior p ituitary.
The primary acti on of prolactin is related to breast development and function during
pregnancy and lactati on.
The hypot halamus synthesizes a prolacti n inhibitory factor (dopamine). Under normal
conditions, large amounts of dopamine are continually transmit ted to the anterior
p ituitary gland so that the normal rate of prolactin secretion is slight. Important: This is
why prolactin is said to be under predominant inhibitory control by t he hypothalamus.
SAADDES
However during pregnancy and lactation, the formati on of dopamine itself is suppressed,
t hereby allowing the anterior pituitary gland to secrete an elevated amount of prolactin.
Factors that increa se p rolactin secretion:
• Estrogen (pregnancy), breast-feeding, sleep, stress, thyrotro pin-releasing hormone
(TRH) and dopamine antagonists (e.g., many antihypertensive drugs and tricyclic
antidepressant s)
Factors that decrease prolactin secretion:
• Dopamine, bromocript ine (do pamine agonist), somatostati n, TSH and GH
Note: Dopamine serves as the major pro lactin-inhibiting factor or "brake" on prolactin
secreti on.
In contrast to what is seen with all the other p ituita ry hormones, t he hypot halamus ton ic-
ally su ppresses prolacti n secretion from the p ituitary. In other words, there is usually a hy-
pot halamic "brake" set on the lactotrope cells of the hypothalamus, and pro lacti n is se-
creted on ly when the b rake is released. If the pituitary stalk is cut, p rolactin secretion
increases, wh ile secretion of all the other pituitary hormones fall dramati cally due to loss of
hypothalami c releasing hormones.
Saad Alqahtani, Twitter @saaddes
hormones
Steroid hormones are synthesized by a series of enzymatic modifications of:
• trii odothyronine
• thyroxine
• cholesterol
SAADDES
• 5-dihydrotestosterone
109
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• cholesterol
Steroid hormones are crucial substances for the proper function of t he body. They mediate a
wide variety of vital physiological functions ra nging from anti-inflammatory agents to regulat-
ing events during pregnancy. Steroid hormones are synthesized and secreted into t he blood-
stream by endocrine glands such as the adrenal cortex and the gonad s (ovary and testis). Steroid
hormones are all characterized by t he steroid nucleus, which is composed of three six- member
rings and one five-member ring.
Cholesterol is a sterol, which is a natura l prod uct derived from the steroid nucl eus. In addition
to being the building block for steroid hormon es, cholesterol is also a component of the cell
membrane. It is thought that the cholesterol present in the cell membrane is responsible for al-
SAADDES
lowing steroid hormones to enter the cell, bind to the hormone receptor and ultimately to a
specific site on the chromatin, in t urn activating the gene in question.
Five classes of steroid hormones:
1. Androgens: originate in the adrenal cortex and gonads and pri marily affect maturation
and function of secondary sex organs (male sexual determination).
2. Estrogens: originate in the adrenal cortex and gonads and primarily affect maturation
and function of secondary sex organs (female sexual determination).
3. Progestins: originat e from both ovaries and placenta and mediate the menstrual cycle
and maintain pregnancy.
4. Mineralocorticoids: originate in adrenal cortex and maintain t he balance of salt and water.
5. Glucocorticoids: originate in the adrenal cortex and affect mainly metabolism in diverse
ways; decrease inflammation and increase resistance to stress.
Note: The production and secretion of steroid hormones are controlled by trophic hormones,
which themselves are either proteins or peptides.
Important: Steroid hormones, which are non-polar molecules, are not stored in tissues and
generally cross cell membra nes relatively read ily. They act t hrough intracellular receptors.
Saad Alqahtani, Twitter @saaddes
hormones
Calcitonin, a peptide hormone secreted by the thyroid gland, tends to
decrease plasma calcium concentration.
In general, calcitonin has effects opposite to those of parathyroid hormone.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
110
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are tru e
Three hormones (parathyroid hormone, calcitriol and calcitonin) regulate the distribution
of [Ca' ') between bone and extracellular fluid (ECF) and thereby reg ulate p lasma calciu m.
PTH is secreted by the parathyroid glands and its secretion is regulated by the [Ca••] in ECF.
The p roduction of calcitriol, a metabolite of vitamin D3 produced in the proxim al tubule
of the kidney is stimulated by hypocalcemia and hypophosphatemia. Calcitonin is secreted
by thyro id C cells (aka, parafollicular cells) and its secretion is stimul ated by hypercalcemia.
Calcitonin decreases plasma [Ca' ') mainly by stimulating bone formation (i.e., deposition of
[Ca'•) in bone).
Note: Calciton in inhibits tubular reabsorpti on of calcium and phosphate, leading to in-
SAADDES
creased rates of their loss in urine and decreased plasma concentrations.
Important: Calcitonin is not required in adult humans. Although it is important during
bone development, the major regulator of plasma calcium levels in the adult is
parathyroid hormone.
Hormont'~ ol tht' I h\ 1 01d and J•ar.tth\ nud C.land~
Hormone Source Target Action (s)
Triiodothyronine 'f hyroid gland Ge.neral Increases rate of metabolism
(f,) (foll icular cells)
Terraiodothyronine o1· Thyroid gland Ge.neral Increases rate of metabolism (usually converted to
thy,-oxine (T,) (follicular cells) T, fir.;t)
Calcitonin 'Thyroid gland Bone tissue Increase calcium storage in bone, lowering blood
(parafollicular Kidneys Ca2"" levels
c.ells)
Paralhyroid hom10ne Parathyi'Oid glands Bone tissue Increases calcium removal from storage in bone
(PTH) hne.•ainal tract and increases abso1·~tion of calcium by intestines,
increasing blood Ca1+1evels
Saad Alqahtani, Twitter @saaddes
hormones
The amount ofT4 produced and released by the thyroid gland is controlled
by which of the following?
• hypothalamus
• medulla oblongata
SAADDES
• parathyroid gland
• pituitary g land
111
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• pituitary g land
The thyroid gland is a small g land, norm ally weighing less than one ounce, located in the
front of the neck. The thyroid g land is m ade up of two halves, called lobes, that lie along
the trachea and are j oined together by a narrow band of thyroid t issue, known as the isth-
mu s.
The thyroid gland is under the contro l of the pituitary gland, a small g land the size of a
peanut at the base of the brain. When the level of thyroid hormones (T3 and T4) drops too
low, the pitu itary g land produces thyroid -stimulating hormone (TSH or thyrotrop in),
which stimulates the thyro id g land to produce m ore horm ones.
SAADDES
The pituitary g land itself is reg ulated by the hypothalam us. The hypothalamus prod uces
thyroid-relea sing hormone (TRH), which tell s the p itu itary gland to stimulate the thyroid
g land (by releasing TSH).
The function of the thyroid g land is to take iodine, fo und in m any foods, and convert it into
thyroid horm ones: thyroxine (T4) and triiodothyronine (T3). Thyroid cells are the only cells
in the body that can absorb iod ine. These cell s combine iodine and the amino acid tyrosine
to make T3 and T4 . T3 and T4 are then released into the bloodstream and are transported
throughout the body where they control metabolism.
1. Thyroid horm ones increa se glycogenolysis, g luconeogenesis, lipolysis, protein
8 synthesis and degradation. The hormones overall effects are catabolic.
2. Thyroid hormones stimulate bone maturation as a result of ossification and
fusion of the growth p lates.
3. Thyroid hormones are lipophilic hormones that exert their effects via trans-
criptional processes.
Saad Alqahtani, Twitter @saaddes
hormones
On his 21st birthday, John celebrates with his first few beers. He notices
(along with other symptoms of inebriation) that he has an increased need to
urinate. This is physiologically caused by a decrease in production of:
• oxytocin
SAADDES
• antidiuretic hormone (ADH)
• parathyroid hormone (PTH)
• aldosterone
112
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• antidiuretic hormone (ADH)
Antidiuretic hormone, also known common ly as vasopressin, is a nine-amino acid peptide
secreted from the posterior pituitary. Within hypothalamic neurons (supraoptic nuclei), the
hormone is packaged in secretory vesicles with a carrier protein called neurophysin and bot h
are released upon hormone secretion.
The single most important effect of antidiuretic hormone is to conserve body water by reduc-
ing the loss of water in urine. Antidiuretic hormone bind s to receptors on cells in the collecting
d ucts of the kidn ey and promotes reabsorption of water back into th e circulation. In the ab-
sence of antidiuretic hormone, the collecting ducts are virtually impermeable to wat er and it
flows out as urine.
Antidiuretic hormone stimulates water reabsorption by stimulating insertion of"water chan-
SAADDES
nels; or aquaporins, into the membranes of kidney tu bules. These channels t ransport solute-
free water through tubular cells and back into blood, lead ing to a decrease in plasma osmolarity
and an increased osmolarity of urine.
The most important variable regulating antidiuretic hormone secretion is plasma osmo-
larity, or the concentration of solutes in blood . Osmolarity is sensed in the hypothalamus by
neurons known as an osmoreceptors, which in turn, stimulate secretion from th e neurons that
produce antidiuretic hormone.
Secretion of antidiuretic hormone is stimulated by decreases in blood pressure and volume,
conditions sensed by stretch receptors in the heart and large arteries. Another potent stimulus
of antidiuretic hormon e is nausea and vomiting, both of which are controlled by regions in
the brain with links to the hypothalamus.
1. Ethanol and caffeine decrease ADH release while nicoti ne increases its release.
2. Sweating causes an increase in ADH, while drinking large amounts of water
causes a decrease in ADH.
3. Hyposecretion of ADH results in diabetes insipidus (polyuria, polydipsia, and
polyphagia). Diabetes insipid us wou ld also result from the hypoactivity of the post-
erior pituitary gland.
Saad Alqahtani, Twitter @saaddes
hormones
Polypeptide and protein hormones are stored in secretory vesicles until needed.
Steroid hormones are usually synthesized from cholesterol and are not stored.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
113
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
There are three g eneral classes of hormones:
1. Proteins and polypeptides, including hormones secreted by the anterior (GH. TSH. FSH,LH, and pro-
lactin), and posterior (ADH and oxytocin) pituitary gla nd, the pancreas (insulin and glucagon), the
parathyroid gland (parathyroid hormone) and many others.
2. Steroids secreted by the adrenal cortex (cortisol and aldosterone). the ova ries (estrogen and proges-
terone). the testis (testosterone) and the p lacenta (est rogen and progesterone).
3. Derivatives of the amino acid tyrosine, secreted by the thyroid (thyroxine and tri iodothyronine) and
the adrenal medullae (epinephrine and norepinephrine). Note: There are no known polysaccharides or
nucleic acid hormones.
M ost of the hormones in the body are polypeptides and proteins. Proteins and peptide hormones are
SAADDES
synthesized on the rough end of the endoplasmic reticulum of the different endocrine cells, in the same
fashion as most other proteins. They are usually synthesized first as larger proteins that are not biologically
active (preprohormones) and are cleaved to form small er prohormones in the endoplasmic reticulum .
These are then transferred to the Golgi apparatus for packaging into secretory vesicles. These vesicles are
stored w ithin the cytoplasm unti l their secretion is needed. Note: Peptide hormones are w ater soluble, al-
lowing them to enter the ci rculatory system easi ly, w here they are carried to their target tissues.
The chemical structure of steroid hormones is similar to that of cholesterol and in most instances they are
synthesized from cholesterol itself. They are lipid soluble. Al though there is usually very little hormone
storage in steroid-producing endocrine cells, large stores of cholesterol esters in cytoplasm vacuoles can
be rapid ly mobilized for steroid synthesis after a stimulus. Much of the cholesterol in steroid-producing
cell s comes from the plasma. Because the steroids are highly lipid soluble, once they are synthesized, they
simply diffuse across the cell membrane and enter the interstitial fluid and then the blood.
The two group s of hormones derived from tyrosine, the thyroid and adrenal medulla ry hormones, are
formed by the actions of enzymes in the cytoplasmic comp artments of the glandular cells. Thyroid hor-
mones are synthesized in foll icular cell s and stored in follicular colloid as thyroglobulin. They cross cell
membranes and associate w ith nuclear receptors. Catecholamines are synthesized in the cytosol and se-
cretory granules and do not readily cross cell membranes. They act through cell membrane-associated re-
ceptors.
Saad Alqahtani, Twitter @saaddes
nerves
All cells have a resting potential.
During the upstroke of the action potential, the cell repolarizes, or becomes
Jess positive.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
114
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is true, the second is false
All cells (not j ust excitable cells) have a resting potential: an electrical charge across the
plasma membrane, with the interior of the cell negative w ith respect to the exterior. The
size of the resti ng potential varies b ut in excitable cells runs about (-)70 mV.
Note: Excitable cells include neurons and muscle cells. In neurons, the action potential is
also called the nerve impulse.
Depolarization of a membrane occurs when sodium channels open, allowing sodium to
move to an area of lower concentration (and more negative charge) inside the cell which
reverses the polarity to an inside-posit ive state.
Important point: During the upstroke of the action potential, the cell depolarizes, or
SAADDES
becomes less negative. The dep olarization is caused by inward current (i.e., the
movement of positive charge into the cell). In nerve and in most types of muscl e, this
inward current is carried by sodium (Na•).
Note: As sodium (Na•) fl oods the cell during initial depolarization, the membrane
potential can reach as high as (+)55 mV (inside positive).
Certa in external stimuli reduce the charge across the p lasma membrane.
• Mechanical stimu li (e.g., stretching, sound waves) activate mechanically gated
sodium channels
• Certain neurotransmitters (e.g., acetylcholine) open ligand-gated sodium channels
In each case, the facilitated diffusion of sodium into the cell reduces the resting potential
at that spot on the cell creating an excitatory postsynaptic potential or EPSP. If the
potential is reduced to the threshold voltage (about -50 mV in mammali an neurons), an
action potential is generated in the cell. Important: If the neuron does not reach this
crit ical threshold level, then no action potential will occur (all or none). So long as
suprathreshold stimuli can reach the thresho ld of the cell, they produce the same action
potential that threshold stimuli do.
Saad Alqahtani, Twitter @saaddes
SAADDES
Depolarization
Depolarization and repolarization. A. Resting membrane potential (RMP) resu lts fro m
an excess of positive ions on the outer surface of the plasma membrane. More Na+ ions
are on the outside of the membrane than K+ ions are on the inside of the membrane. B.
Depolarization of a membrane occurs when Na+ channels open, allowing Na+ to move to
an area of lower concentration (and more negative charge) inside the cell -reversing the
polarity to an inside-positive state. C, Repolarization of a membrane occurs w hen K+ chan-
nels then open, allowing K+ to move to an area of lower concentration (and more negative
charge) outside the cell- reversing the polarity back to an inside-negative state. Each volt-
meter records the changing membrane potential as a red line. n•-•
Saad Alqahtani, Twitter @saaddes
nerves
All of the follow ing statements are true EXCEPT one. Which one is the
EXCEPTION?
• peripheral nerve fibers can sometimes regenerate if the soma (cell body) is not
damaged and some of the neurilemma rema ins intact
• the neurilemma forms a regeneration tube through which the growing axon
SAADDES
reestablishes its original connection
• if the nerve o riginally led to a skeletal muscl e, the muscle atrophies in the absence
of innervation but regrows when the connection is re-established
• nerve fibers of the CNS (brain and spinal cord) possess the th ickest neurilemma
115
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• nerve fibers of the CNS (brain and spinal cord )
possess the thickest neurilemma
***This is false; nerve fibers of the CNS (brain and spinal cord) are not enclosed by
a neurilemma. This is why regeneration of severed axons is more d ifficult in the CNS
(brain and spinal cord).
The neurilemma (also cal led a sheath of Schwann, Schwann's membrane o r
neurolemma) is the thin membrane spirally enwrapping the myelin layers of certa in
fibers, especially those of the peripheral nerves, or the axons of certain
unmyelinated nerve fibers.
SAADDES
1. All axons of the PNS have a sheath of Schwann cells (and thus a neuri-
8 lemma, made up of the outer layer of Schwann cells) around them.
2. When a Schwann cell is w rapped successively around an axon, it becomes
a myelin sheath. In the CNS, the sheath cells are called oligodendrocytes.
Remember: Right-sided lesions of the spinal cord result in loss of motor activity on
the same (ipsilateral) side and pain and temperature sensations on the opposite
(contralateral) side.
Saad Alqahtani, Twitter @saaddes
nerves
The primary action of local anesthetics in producing a conduction
block is to decrease the permeability of the ion channels to:
• calcium ions
• ch loride ions
SAADDES
• potassium ions
• sodium ions
116
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• sodium ions
Local anesthetics selectively inhibit the peak permeability of sodium, whose value is normally
about five to six times greater than the minimum necessary for impul se conduction. The
following sequence is a proposed mechanism of action of local anesthetics:
1. Displacement of calcium ions from the sodium channel receptor site, which permits ...
2. Binding of local anesthetic molecule to t hi s receptor site, which thus produces ...
3. Blockade of the sodium channel, and a...
4. Decrease in sodium conductance, which leads to ...
5. Depression of the rate of electrical depolarization, and a...
6. Failure to achieve the threshold potential level, along with a...
7. Lack of development of propagated action potentials, which is called ...
8. Conduction blockade
SAADDES
The mechanism whereby sodium ions gain entry to the axoplasm of the nerve, t hereby initiat-
ing an action potential, is altered by local anesthetics. The nerve membrane remains in a polar-
ized state because ionic movements responsible for the action potential fail to develop. Nerve
block produced by local anesthetics is called a nondepolarizing nerve block.
1. Local anesthetics reversibly block nerve impulse conduction and produce
reversible loss of sensation at their administration site. The site of action of local
anesthetics is at the lipoprotein sheath of the nerves.
2. Local anesthetics are clinically effective on both axons and free nerve endings.
3. Important: Small, myelinated nerve fibers which conduct pain and tempera-
ture sensations are affe.cted first, followed by touch, proprioception and skeletal
muscle tone.
4. Emergence from a local anesthetic nerve block follows the same diffusion patterns
as induction does; however, it does so in reverse order.
5. Recovery is usually a slower process than induction because the anesthetic is
bound to t he drug receptor site in the sodium channel and t herefore is released
more slowly than it is absorbed.
6. Potassium, calcium and chloride conductance's remain unchanged.
Saad Alqahtani, Twitter @saaddes
nerves
Match the major ascending tract of th e spinal cord on the left with the
function on the right.
Tract Fu nction
l. Latera l spinothalamic A. Discriminating touch and pressure
sensations
SAADDES
2. Anterior spinothalamic
B. Unconsc ious kinesthes ia
3. Fasciculi grac ilis and cuneatus
C. Pain, temperature, and cmde touch;
4. Anterior and posterior spinocerebell ar oppos ite s ide
D. Crude touch and pressure
117
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• 1. C, 2 . D, 3. A, 4 . B
The white matter of the spinal cord contains tracts that travel up and down the
cord. Many of these tracts travel to and from the brain to provide sensory input to
the brain or bring motor stimuli from the brain to control effectors. Ascending
tracts, those that t ravel toward the brain are sensory; descending tracts are
motor. For most, the name will indicate if it is a motor or sensory tract. Most
sensory tracts' names begin with spino, indicating origin in the spinal cord, and
their names end with the part of the brain where the tract leads. For example, the
spinothalamic tract travels from the spinal cord to the thalamus. Tracts whose
names begin with a part of the brain are motor. For example, the corticospinal
tract begins with fibers leaving the cerebral cortex and travels down toward motor
SAADDES
neurons in the cord.
\lajor \seen ding Tracts of the Spinal ( ord
Name Function Location Origin Te1·mination
La teral Pain, temperature. and crude Lateral white Posterior gray c.olumn; Thalamus
spinothalamic touch; opposite side coJumns opposite side
A nterior Crude touch and pressure Anterior w hite Posterior gray c.olumn; Thalamus
spinothalamic coJumns opposite side
FascicuJi gracilis and Discriminating touch and Posterior Spina] gangJia; same Medulla
n meatus pressure sensations wh ite co]umns s ide
Anterior and posterior Unconscious kinesthesia Lateral white Anterior or posterior Ce rebe llum
spinocerebeJlar coJumns gray coJumn
The origin refers to the location of cell bodies of neurons from which the axons of
tract ari se.
The termination refers to the structure in which the axons of the tract terminate.
Saad Alqahtani, Twitter @saaddes
nerves
Spatial summation occurs when:
• two inhibitory inputs arrive at a postsynaptic neuron within 1 m inute of each other
• two excitatory inputs arrive at a postsynaptic neuron simultaneously
• two inhibitory inputs arrive at a postsynaptic neuron 10 seconds apart
SAADDES
• two excitatory inputs arrive at a postsynaptic neuron in rapid succession
118
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• two excitatory inputs arrive at a postsynaptic neuron simultaneously
Neurotransmitters may be excitatory, increasing the probability of causing an action
potential in the postsynaptic neuron (an excitatory postsynaptic potential or EPSP), or
inhibitory, decreasing the probability of an action potential in the postsynaptic
neuron (an inhibitory postsynaptic potential or IPSP). Note: Neurotransmitter
molecules may have excitatory or inhibitory effects depending upon t heir binding
to d ifferent subtypes of receptors.
There are two forms of summation by which EPSPs may combine to reach threshold
and initiate an action potential:
SAADDES
1. Spatial summation occurs when two excitatory inputs arrive at a postsynaptic
neuron simultaneously. Together these two inputs produce greater depolarization.
It is the result of a converging circuit and is dependent upon t he simultaneous
arri val of impulses from multiple presynaptic fibers.
2. Temporal summation occurs when two excitatory inputs arrive at a postsynap-
tic neuron in rapid succession. In temporal summation, t here is an increase in the
frequency of nerve impulses in a single presynaptic fi ber.
Note: An action potential initiated at the m idpoint along the length of an axon will
spread toward the cell body (soma) and nerve ending.
Saad Alqahtani, Twitter @saaddes
nerves
Saltatory conduction happens in myelinated neurons only. Which of the
following are effects of saltatory conduction compared to conventional
conduction?
Select all that apply.
• conduction is faster
SAADDES
• conduction is slower
• conduction is at the same rate
• conduction consumes more energy
• conduction consumes less energy
• conduction consumes the same energy
119
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• conduction is faster
• conduction consumes less energy
In an unmyelinated neuron, the impulse t ravels along the entire membrane surface
and is known as continuous conduction. Note: This conduction is relatively slow
(1.0 m/sec) compa red to saltatory conduction (up to 100m/sec).
In a myelinated neuron, the myelin sheath decreases membrane capacitance and
increases membrane resistance, preventing movement of sodium and potassium
through the membrane. If the myelin sheath were continuous, action potentials could
not be produced. However, the myelin sheath is interrupted by nodes of Ranvier.
The distance between these nodes is between 0.2 and 2 mm. Action potentials
SAADDES
traveling down the axon "jump" or "leap" from node to node. This is called saltatory
conduction.
Saltatory conduction is of value for two reasons:
1. Increases velocity of nerve t ransmission in myelinated fibers.
2. Conserves energy for the axon because only the node depolarizes. Thus, it takes
less energy fo r the sodium/potassium ATPase to re-establish resting ion g radients.
Important point: Saltatory conduction is not only faster but also consumes less
energy, since t he pumping of sodium and potassium ions need occur only at the
nodes.
Conduction velocity depends on:
1. Diameter of the nerve fiber - the larger the d iameter, the faster t he conduction
velocity because an increase in diameter reduces resistance to current flow down
the axon.
2. Presence of myelin sheath -which of course, increases conduction velocity.
Saad Alqahtani, Twitter @saaddes
nerves
In most instances, acetylcholine has an inhibitory effect.
GABA is believed always to cause inhibition.
• both statements are t rue
SAADDES
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is false, the second is true
120
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
Release of excitatory neurotransmitters from the presynapt ic membrane openschannels in the post-
synaptic membrane and leads to an increase in the concentration of sodium ions withi n the postsy-
naptic cell and a decrease in potassium ions. This leads to a depolarization of the postsynaptic cell,
which is propagated furt her along the cell membrane by an action potent ial.
Inhibitory neurotransmitters encourage the hyperpolarization of the postsynaptic cell, making it
less likely to generate an act ion potential. This hyperpolarized state is achieved either by increasing
n flow into the cell (GABAA receptors) or increasing K• flow out of the cell (GABA8 receptors).
Whether a neurotransmitter acts in an excitatory or inhibitory manner is determined by the reaction
of t he receptor to its binding. Thus a given chemical can be exci tatory at some receptors and in -
hibitory at others.
SAADDES
Some of the most important small-molecule transmitters are:
• Acetylcholine - in most instances, acetylcholine has an excitatory effect; however, it is known to
have inhibitory effectsat some peripheral parasympathetic nerve endings, such as inhibition of the
heart by the vagus nerves
• Norepinephrine- in most areas, NE probably activates excitatory receptors; but in a few areas, it
activates inhibitory receptors instead
• Dopamine- the effect of dopamine is usually inhibitory
• Serotonin - act s as an inhibitor of pain pathways in the spinal cord; also has an inhibitory effect
on higher nervous system struct ures which help control mood
• Glutamate- it is believed always to cause excitation
• GABA- it is believed always to cause inhibition
• Glycine - it is believed always to act as an inhibitory transmitter
• Nitric oxide - changes intracellular metabolic functions that modify neuronal excitability for sec-
onds, minutes, or perhaps even longer
Note: Monoamine oxidase (MAO) is an enzyme that catalyzes the oxid ative deamination of
monoamines such as norepinephrine, serotonin and epinephrine. This deamination process aids in
metabolizing excess neurotransmi tters that may build up at postsynaptic terminals.
Saad Alqahtani, Twitter @saaddes
nerves
A patient of yours presents with symptoms similar to Parkinson's disease. He
claims that the physicians have not diagnosed him with Parkinson's because
it was due to trauma. The trauma affected which part of his brain?
• pons
SAADDES
• pari etal lobe
• basal ganglia
• tha lamus
121
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• basal gan g lia
The basal ganglia include several deep telencephalic nuclei (including the caudate
nucleus, putamen and globus palli dus). The basal gangli a interacts w ith the cerebral
cortex, subthalamic nucleus, substantia nigra and thalamus. They are functionally
important, at a minimum, for controlling voluntary movements and establi shing postures.
When the basal gangli a are altered, say in disorders like Parkinson's disease and
Huntington's disease, the person has unwanted movements, such as involuntary jerking
movements of an arm or leg or spasmodic movement of facial muscles.
The term striatum, derived from the striated appearance of these nuclei, refers only to the
caudate nucleus and putamen. The striations are produced by the fi ber bundles formed
by the anterior limb of the internal capsule, as it separates the caudate nucleus and
SAADDES
putamen. The combination of putamen and globus pallidus is often referred to as the
lentiform nucleus.
The basa l ganglia and cere be llum are large collections of nuclei that modify movement
on a minute -to -minute basis. The cerebral (motor) cortex sends information to both, and
both structures send information back to the cortex via the thalamus. This
communication occurs via two opposing pathways - a direct and an indirect path
both which use dopamine as a neurotransmitter. Dopamine is inhibitory in the indirect
path and excitatory in the direct path w ith an overall net excitatory role. The basal ganglia
is located deep to the cerebral cortex. Note: The output of the cerebellum is excitatory,
while the basal gangli a are inhibitory.
Remember: The cere bellum is situated below and posterior to the cerebrum and above
the pons and medulla. It is morphologically divided into two lateral hemispheres and a
middle portion. Its f unction is to maintain equilibrium and mu scle coordination.
Note: The major parts of the extrapyramidal system are the "subcortical nuclei':Th is
includes the caudate nucleus, putamen and globus pallidus (which are also known as the
basal ganglia).
Saad Alqahtani, Twitter @saaddes
nerves
The two classes of acetylcholine receptors in autonomic ganglia are:
• nicotinic and alpha
• alpha and beta
• nicotinic and muscari nic
SAADDES
• muscarinic and beta
122
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• nicotinic and muscarinic
The main type of neuron in autonomic ganglia is the postganglionic neuron. These cells receive
synaptic connections from preganglionic neurons and they project to autonomic effector cells.
The classic neurotransmitter of autonomic ganglia, whether sympathetic or parasympathetic, is
acetylcholine. The two classes of acetylcholine receptors in autonomic ganglia are:
Nicotinic Receptors
• Stimulated by ACh and nicotine, not stimulated by muscarine
• Found at all ganglionic synapses
• Also found at neuromuscular junctions and the adrenal medulla
• Produce excitation
• The fast EPSP (excitatory postsynaptic potentials) results from activation of nicotin ic recep-
tors, which cause ion channels to open
SAADDES
• Blocked by hexamethonium and curare
Muscarinic Receptors
• Stimulated by ACh and muscarine, not stimulated by nicotine
• Found at target organs when ACh is released by postganglionic neurons (all of parasymp-
athetic and some sympathetic) including heart, smooth muscle and glands
• The slow EPSP is mediated by muscarinic receptors that inhibit theM current, a current pro-
duce by conductance of potassium
• Blocked by at ropine
Note: Those fibers that secrete acetylcholine are said to be cholinergic. Those that secrete norepi-
nephrine are said to be adrenergic.
The cholinergic effect s of preganglionic autonomic neurons (both sympathetic and
parasympathet ic) are excitatory. The cholinergic effects of postganglionic parasympathetic
fibers can be either excitatory or inhibitory.
Important: All preganglionic neuronsare cholinergic in both the sympathetic and the parasympa-
thetic nervous systems. Either all or almost all of the postganglionic neurons of the parasympa-
thetic system are also cholinergic. Conversely, most of the postganglionic sympathetic neurons are
adrenergic, except for the postganglionic sympathetic nerve fibers to the sweat glands, to the pi-
loerector muscles of the hairs, and to a very few blood vessels which are cholinergic.
Saad Alqahtani, Twitter @saaddes
ome target tissue
Sympathetic division Cholinergic Adrenergic re stim ulated, other
(nicotinic) (alpha or beta) re inhibited. For ex
Ach receptors NE rec{2Jptors mple, blood vessel
release4·······h rele~ including those i
Pregangllonicne~{~~ ~n
A keletal muscle) ar
timulated to vaso
onstrict, and stom
"·····" Effector ch glands are inhib-
cell ted.
Cholinergic Cholinergic
(nicotinic) (muscarinic) weat glands ar
~====~r:e:le::se=d~ r~
timulated and skele
al m uscle blood ves
SAADDES
els are inhibited
B
Postganglionic neuron ~ vasodilate) during
Effector
cell
Cholinergic
(nicotinic)
eneral response i
xcitatory but som
c arget tissues are in
itied (e.g., the heart
cell
Locations of neurotransmitters and receptors of the autonomic nervous system. In all pathways.
p reganglionic fibers are chol inergic, secreting acetylcholine (ACh), which stimulates nicotini c receptors
in the postganglionic neuron. Most sympathetic postganglionic fibers are adrenerg ic (A), secreting nor-
epinephrine (NE), thus sti mulating alpha or beta adrenerg ic recep tors. A few sympathetic postganglionic
fibers are choli nergic, stimulating muscarinic receptors in effector cells (8). All parasympathetic post-
ganglionic fibers are choli nergic (C), stimulating muscarinic receptors in effector cells. l22-l
Saad Alqahtani, Twitter @saaddes
nerves
Motor signals are transmitted directly from the cortex to the spinal cord
through the corticospinal tract and indirectly through multiple accessory
pathways that involve the basal ganglia, cerebellum and various nuclei of
the brain stem.
The most important output pathway from the motor cortex is the cortico-
spinal tract, also called the pyramidal tract.
SAADDES
• both statements are t rue
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is false, the second is true
123
Irefer to AS card 195-1for illustration] copyngh t 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
The corticospinal tract (aka. pyramidal tract) is a group of fibers that carries messages for volun-
tary motor movement (fine skilled movement s of skeletal muscle) to the lower motor neurons in the
b rain stem and spinal cord. The corticospi nal tract orig inates about 30% from the primary motor cortex.
30% from the premotor and supplementary motor areas and 40% from the somatosensory areas
posterior to the central sulcus.
This tract is direct and monosynaptic, meaning that the axons of its neu rons do not synapse with other
cell s until they reach their final destination in the brain stem or spinal cord. These d irect connections
bet ween the cortex and the lower motor neurons allow messages to be transmitted very rapid ly from
the central nervous system to the periphery.
The fibers of the pyramidal tract that synapse with cranial nerves located in the brain stem form the
SAADDES
corticobulbar tract. This is the part of the pyramidal tract that carries the motor messages that are most
important for speech and swallowing. The fibers of the pyramidal tract that synapse with spinal nerves
sendi ng information about voluntary movement to the skeletal muscles form the corticospinal tract. At
the pyramids in the inferior part of the medulla, 85% to 90% of corticospinal fibers decussate, or cross to
the other side of the brain. The remaining 10% to 15% conti nue to descend ipsilaterally. The fibers that
decussate are called the lateral corticospinal tract or the crossed pyramidal tract. Because t hey
descend along the sides of the spinal cord, the uncrossed or direct fibers that synapse with spinal nerves
on the ipsilateral side of the body are called the direct pyramidal tract. They may also be referred to as
the ventral pyramidal tract or the anterior corticospinal tract since they travel down the ventral aspect
of the spi nal cord.
1. Descending pathways can be subd ivided into (1) a lateral system, which ends on motor neu-
8 rons to li mb muscles and on the lateral group of interneurons, and (2) a medial system, which
ends on the medial group of interneurons.
2. The lateral system incl udes the lateral corticospinal tract and part ofthe corticobulbar tract .
These pathways infl uence the contralateral motor neurons that supply the musculature of the
limbs, especially the d igits and the muscles of the lower part of the face and the tongue.
3. The medial system incl udes the ventral corticospi nal, lateral and medial vestibulospinal, retic-
ulospinal and tectospinal tracts. These pathways mainly affect posture and provide the motor
background for movement of the limbs and digits.
Saad Alqahtani, Twitter @saaddes
nerves
The effectors of the autonomic nervous system include all of the following
EXCEPT one. Which one is the EXCEPTION?
• smooth muscle
• cardiac muscle
SAADDES
• glands
• skeletal muscle
124
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• skeletal muscle
The autonomic nervous system (ANS} is a motor system that controls smoot h muscle, cardiac muscle and
glands. It helps maint ain homeostasis and coordinates responses to external stimuli . lts components are the
sympathetic, pa rasympatheti c and enteri c nervous systems. Autonomic motor pathways have pregan-
glionic and postganglionic neurons. Preganglionic neurons reside in the CNS, whereas postganglionic
neu rons lie in peripheral ganglia.
Important Points to Remember:
1. Sympathetic preganglionic neurons are located in the thoracolumbar region of the spinal cord and
sympathetic postganglionic neurons are located in paravertebral and prevertebral ganglia.
2. Parasympathetic preganglionic neurons are l ocated in crani al nerve nuclei or in the sacral spinal
cord. Parasympathetic postganglionic neurons reside in ganglia locat ed in or near the target organs.
3. Sympathetic pregangl ionic axons are short while their postgangluionic axons are long. Parasympa-
SAADDES
thetic axons are the opposite ~the preganglionics are longer and the postganglionics are shorter.
4. The ANS is activat ed mainly by centers located in the spinal cord, brain stem and hypot halamus. Al so
portions of the cerebral cortex, especially of the limbic system, can transmit signal s to the lower cen-
ters and in this way influence autonomic control.
5. The enteric nervous system includes the myenteric and submucosal pl exuses in the wall of the gas-
trointestinal tract. The myenteric pl exus regulates motility and the submucosal pl exus regulates ion and
water transport and secretion.
6. Neurotransmitters at the synapses of preganglionic neurons in autonomic ganglia include acetyl-
choline (acting at both nicotini c and musca rinic receptors) and a number of neuropeptides. lnterneu-
rons in the ganglia release catecholamines. Sympathetic postganglionic neurons generally release
norepinephrine (acting on adrenergic receptors) as thei r neurotransmitter. Sympathetic postgan-
glionic neurons that supply sweat glands rel ease acetylcholine. Parasympathetic postganglionic
neurons rel ease acetylcholine (acting on muscarinic receptors}.
Note: Those fibers that secrete acetylcholi ne are said to be cholinergic.Those that secrete norepinephrine
are sai d to be adrenergic. Quick summary: All preganglionic neurons are cholinergic in both the sym-
pathetic and the parasympathetic nervous systems. Either all or almost all of the postganglionic neu-
rons of the parasympathetic system are also cholinergic. Conversel y, most of the postganglionic
sympathetic neurons are adrenergic, except for the postganglionic sympat hetic nerve fibers to the sweat
glands, to the piloerector muscles of the hairs and to a very few blood vessel s which are cholinergic.
Saad Alqahtani, Twitter @saaddes
Central Somatic Nervous Autonomic Nervous
Nervous System (SNS) System (ANS)
System
(CNS) Somatic Autonomic
Brain and Integration cente rs
spinal cord
Peripheral
Nervous
System Pa s pathetic
di sion
(PNS)
• rent)
Cranial nerves
SAADDES
and
spinal nerves
(cardiac and smooth
muscle; glands)
Stimulus Response Stimulus Response
Organizational plan of the nervous system. This diagram summarizes the scheme used by most neu-
robiologists in s tudying the nervous system. Both the somatic nervous system (SNS) and the autonomic
nervous system (ANS) include components in the central nervous system (CNS) and peripheral nervous
system (PNS). Somatic sensory pathways conduct information toward integrators in the CNS, and so-
matic motor pathways conduct info nnation toward somatic effectors. In the ANS, visceral sensory path-
ways conduct infonnation toward CNS integrators, whereas the sympathetic and parasympathetic
pathways conduct information toward autonomic effectors. 12 .,.1
Saad Alqahtani, Twitter @saaddes
nerves
The action potential is generated by the rapid opening and subsequent
voltage inactivation of voltage-dependent _ _ channels and the delayed
opening and closing of voltage-dependent _ _ channels.
• Na•, K·
SAADDES
125
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• Na ·, K·
The action potential is generated by the rapid open ing and subsequent voltage inactivation of volt-
age-dependent Na• channels and the delayed open ing and closing of voltage-dependent K•channels.
lon channels are integral m embrane proteins that have ion-selective pores. Different regions of an ion
channel protein act as gates to activate and inactivate the channel. An ion channel typi cally has t wo
states: high conductance (open) and zero conductance (closed). The channel oscillates randomly be-
tween the open and closed states. For the voltage-dependent channel, the fraction oftime that the chan-
nel spends in the open state is a function of the transmembrane potential difference.
Remember: After the action potential is over, for a few milliseconds, the increased potassium
conductance allows for additional potassium efflux, leaving the interior of the cell even more
negative than the origi nal resting membrane potential. This is called hyperpolarization. Gradually, the
ion concentrations go back to resting levels and the cell membrane returns to (-) 70 mV.
SAADDES
The importance of the hyperpolarization is that the cell remains in a•hypoexcitabl e state~ the relative
refractory period. Thi s means that, in order to trigger a second action potential, t he depolarizing
stimulus must be of a greater magnitude to achieve th reshold.
Important point to remember: Duri ng the absolute refractory period t he membrane will not
respond to any stimulus. Duri ng the relative refractory period, however, a very strong stimul us may
elicit a response in the membrane.
Voltage inactivation of Na• channels and membrane hyperpolarization due to slow closure of K•
channels are t he major factors determining the absolute and relative refractory periods that limit the
maximum fi ring rate of action potentials.
1. Presynaptic neurons transmit information toward a synapse; postsynaptic neurons
8 transmit information away from a synapse.
2. Nerve impulses travel in only one direction because of the fact that synapses are
polarized.
3. Electrical synapses are rare in the CNS (common in cardiac and smooth muscle).
They are connected by gap junctions, which allow local electrical currents resulting
from action potentials in the p resynaptic neuron to pass directly to the postsynaptic
neuron.
Saad Alqahtani, Twitter @saaddes
nerves
A patient of yours lists a selective 13-blocker in her medication list. You know
that this is for her hypertension. What is the mechanism of this drug?
• blocks 13 1 -adrenergic receptors in the heart, causing a decrease in heart rate and
force of contraction
• blocks 13 2-cholinergic receptors in the heart, causing a decrease in heart rate and
SAADDES
force of contraction
• blocks 13 1-cholinergic receptors in the heart, causing a decrease in heart rate and
force of contraction
• blocks 13 2-adrenergic receptors in the heart, causing a decrease in heart rate and
force of contraction
126
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• blocks 1} 1-adrenergic receptors in the heart, causing
a decrease in heart rate and force of contraction
~-blockers "block" the effects of adrenaline on t he body's p-receptors. This slows the
nerve impulses that travel th roug h the heart. As a result, the heart does not have to work as
hard because it needs less blood and oxygen. P-blockers also block the impu lses that can
cause an arrhythmia. The body has two main beta receptors: P 1and p 2.
• Some P-blockers are selective, which means that they block P1 receptors more than they
block PTreceptors. P 1-receptors are responsible for heart rat e and the strength of your
heartbeat
• Nonselective P-blockers block both P1andp 2 -receptors. p2-receptors are responsible for
t he function of your smooth muscles
SAADDES
Adrenergic receptors are membrane receptor proteins located on autonomic effector organs
that are regulated by catecholamines (epinephrine and norepineph rine).
Two main types of adrenergic receptors:
a.-receptors:
• a. 1 : located in sympathetic postsynaptic nerve terminals- increase vascular smooth
muscle contraction
• a.2 : located in sympathetic presynaptic nerve term inals; beta cell of pa ncreatic islets-
inhibit NE release; inhibit insulin release
~-receptors:
• ~ 1 : located in the heart - increase cardiac outpu t
• ~ 2 : located in liver; smooth muscle vasculature, bronchioles and uterus - increase
hepatic glucose output; decrease contraction of blood vessels, bronchioles and uterus
Important:
1. Norepinephrine stimulates mainly a. -receptors.
2. Epinephrine stimulates both a. and 13 -receptors.
Saad Alqahtani, Twitter @saaddes
nerves
All cells, including neurons, have a resting membrane potential that is
typically around (-)70mV.
An action potential is propagated with the same shape and size along the
entire length ofthe axon.
SAADDES
• both statements are t rue
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is false, the second is true
127
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Resting membrane potential (RMP) results from an excess of positive ions on the
outer surface of the plasma membrane. More Na• ions are on the outside of the
membrane than K• ions are on the inside of the membrane.
The size of the resting membrane potential varies but in excitable cells runs between
(-) 40 and(-) 85 millivolts. The resting membrane potential ari ses from t wo activities:
1. leakage of potassium and sodium through nerve membranes. There are
channel proteins in the nerve membrane through which potassium and sodium
ions can leak, called a potas sium-sodium "leak" channel. The emphasis is on
potassium because, on average, the channels are far more permeable to
SAADDES
potassium than to sodium, normally about 100 t imes as permeable. This
differential in permeability is exceedingly important in determining the level of
the normal resting membrane potential.
2. The sodium /pota ssium pump establishes the sodium and potassium
g radients across the membrane using ATP. Important: This pump is an
electrogenic pump because more positive charges are pumped to the outside
than to the inside (three Na• ions to the outside for each two K· ions to the
inside), leaving a net deficit of positive ions on the inside; this causes a negative
potential inside the cell membrane.
Remember:
1. The action potential is propagated rather than merely being conducted; it is
regenerated as it moves along the axon. In this way an action potential remains the
same size and shape as it is conducted.
2. Visceral smooth muscle and cardiac pacemaker cells lack a stable resting
membrane potential.
Saad Alqahtani, Twitter @saaddes
nerves
Exteroreceptors signal internal events.
Sensory receptors can be classified in terms of the types of energy that they
transduce or according to the sources of the input.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second statement is false
• the first statement is fa lse, the second statement is true
128
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second statement is true
Sensory receptors can be classified in terms of the t ype of energy that they transduce (e.g ., photore-
ceptors transd uce light, mechanoreceptors transduce d isplacement and force) or accord ing to the source
of the input (e.g., extero receptors signal external events, p roprioceptors signal t he position of the body
part with respect to space o r another body part).
Central pathways are usually named by their origi n and termi nation o r for the type of information con-
veyed. The motor neuron is the only means of communication between the CNSand effectors, like mus-
cles and g land s. It is often referred to as "the final common pathway" as it is the only way for the CNS
to express its operati ons as behavior. Note: The term pathway is similar to tract but is generally used to
suggest a particular function (e.g., t he auditory pathway: a series of neuron-to -neu ron links, across sev-
eral synapses, that convey and p rocess auditory information).
Sensory receptors include exteroreceptors, interoreceptors and proprioceptors. Stimuli are environ-
SAADDES
mental events that excite sensory receptors. Responses are the effects of sti muli and sensory transduc-
tion is the p rocess by w hi ch stimuli are detected. Note: lnteroreceptors (aka, viscero receptors) are
associated with the viscera or organs and provide information about the int ernal environment. For ex-
ample, mechanoreceptors detect d istension of the gut and fullness of the bladder.
All receptors are linked to sensory neurons. When a receptor responds to a stimulus, a signal is sent
along the sensory neu ron to t he CNS (brain o r spinal cord). Wit hin the CNS, the stimulus is identified
and if a response is required to maintain homeo stasis, signals are sent to effectors along motor neurons.
1. Adaptation, a change in the way that a recepto r respond s to sequential o r p rolonged
stimulation, is a characteristic property of sensory receptors that makes t hem better suited to
evaluate and determi ne pa rticular kind s of sensory info rmation.
2. Free nerve endings respond to itch, movement, pain and temperatu re. Examples include
nociceptors (detect painful stimuli), Merkel d isks and root ha ir plexuses.
3. Proprioceptors are found in the j oi nt s, muscles, and tendons.
4. Each spinal reflex is elicited by t he activati on of one or more classes of sensory receptors.
Muscle stretch r& eptors (muscle spindles) and Golgi tendon organs are important
receptors for both spinal reflexes and as a source of the proprioceptive information that gives
us an aw areness of our limbs and helps guide vol untary movement.
5. The parasympathetic nervous system includes p rimary afferent neurons and the sensory
receptors that they innervate, somatic moto r neurons and autonomic neu rons.
Saad Alqahtani, Twitter @saaddes
nerves
When scaling and root planing, you are using a firm finger rest for minutes at
a time.
1. Which of the following are the receptors that are used in sensing this
continuous pressure?
2. Which of the following are the receptors used when you are manipulat-
ing an instrument in your fingers?
SAADDES
• pacinian corpuscles
• meissner's corpuscles
• ruffini's corpuscles
• krause's corpuscles
129
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. ruffini's corpuscles
2. pacinian corpuscles
Somatic Sensory Receptors
Classification by structure Bl' Location and Type By Activation By Sensation and Function
Stimulus
Free Nerve Endings
Nociceptors Both extt-roceptors and Almost any no:<ious Pain: tel'nperarure; itl.'h;
Visl.'t-roceptors (most stimulus; tt1nperature tickle-; stretching
body lis..o;ue$) ehange; mechanical
Merkeldisk.o; Exteroc.eptors Light pressure; meehanical Oiscrintinative touch
Root hair plexu..o;e..o; Exteroc.eplors Jlair movement; meehanical Sense of"detlection·• type
movt-1~-.ent of hair
SAADDES
EncapsulatW Nerve Endings
Touch and Press ure Receptors
Meissnet's corpuscle. Exteroc.eptors: t -pidennis.. Light pressure; mechanical Ois.crintinative touch: low
hairlt$S skin ftequt -ncy vibration
Krause's COI'puscle tvlul.'ous mt-1nbrane Mechanical; thermal Touch; low-frequtncy
vibration; cold
Rutlini's COI'J)lt..•K·Ie Dennis. of skin. Mechanical; thermal Crude and persistent touch:
e--xteroc.eptors heat
Paeinian corpu.•;c::·le Dennis. of skin. joint Deep prt$Sul'e, 1nechanical Deep prt$Sure; high freque--ncy
caps.l1les vibration; strerch
Stretch receptors
Muscle spindles Skeleral musde Sttctl~h. me<.~hankal Sense of musd e lt-ngth
Golgi tendon receplors tvlus.culotendinous Force of oonttaction and Sense of musdt tension
junction (endon s.ttetd'l. mechanical
Important: Skin contains low-threshold mechanoreceptors, thermoreceptors and nociceptors. Mus-
cle, joints and viscera have mechanoreceptors and nociceptors. Low-threshold mechanoreceptors
may be rapidly or slowly adapting.
Remember: Baroreceptors are special ly adapted groups of nerve fibers within the walls of the
carotid sinus and the aortic arch . Baroreceptors are stretch receptors that respond to changes in
blood pressure.
Saad Alqahtani, Twitter @saaddes
nerves
The primary functional unit of the sympathetic and parasympathetic
nervous systems is the:
• one-neuron motor pathway
• two-neuron motor pathway
SAADDES
• three-neuron motor pathway
• fou r-neuron motor pathway
130
Irefer to AS card 212-1, 212 A-1for illustration)
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• two-neuron motor pathway
The nervous system can be divided into centra l (CNS) and peripheral (PNS) parts, each with fu rther
subd ivisions.The peripheral nervous system (PNS) provides an interface between the environment
and the central nervous system (CNS). The CNS includes the spinal cord and brain.The brain includes
the medulla, pons, cerebellum, midbrain, thalamus, hypothalamus, basal ganglia and cerebral cortex.
The PNS includes primary afferent neurons and the sensory receptors that they innervate, somatic
motor neurons and autonomic neurons.
The PNS is subdivided into the:
• Somatic Nervous System- includes all nerves controlling t he muscular system and external
sensory receptors. External sense organs (including skin) are receptors. Muscle fibers and gland
cellsare effectors.
• Autonomic Nervous System- the organs(the "viscera") of our body, such as the heart, stomach
SAADDES
and intestines, are regulated by a part of the nervous system called the autonomic nervous
system (ANS). The ANS works largely unconsciously and integrates information from the internal
and external environments to maintain total body homeostasis. The ANS has t wo divisions, the
sympathetic nervous system (also called the thoracolumbar or adrenergic division) and the
parasympathetic nervous system (also called the craniosacral or cholinergic division).
• The enteric nervous system includes the myenteric and submucosal plexuses in the wall ofthe
gastrointestinal tract. The myenteric plexus regulates motility and the submucosal plexus regulates
ion and water transport and secretion.
Remember: The primary functional unit of the sympathetic and parasympathetic nervous systems
is the two-neuron motor pathway, which consists of a preganglionic neuron, whose cell body is lo-
cated in the CNS, and a postganglionic neuron, whose cell body islocated in one of the autonomic
ganglia.
Important:
1. Motor neurons in the ANS do not reach their targets directly (as do those in the somatic system)
but rather connect to a secondary motor neuron which in turn innervates the target organ.
2. Motor neuronsof the somatic system are distinct from those of the autonomic system. Inhibitory
signals cannot be sent through the motor neuronsof the somatic system.
Saad Alqahtani, Twitter @saaddes
nerves
All preganglionic neurons are _ _ _in both the sympathetic and the
parasympathetic nervous systems.
• dopaminergic
• serotonergic
SAADDES
• cholinergic
• adrenergic
131
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• cholinergic
All preganglionic neurons are cholinergic in both the sympathetic and the parasympathetic
nervous systems. Eith er all or almost all of the postganglionic neurons of the parasympa-
thetic system are also cholinergic. Conversely, most of the postganglionic sympathetic neu-
rons are adrenergic, except for the postga nglionic sympathetic nerve fibers to the sweat
glands, to the piloerector muscles of the hairs and to a very few blood vessels which are
cholinergic. Note: Those fi bers that secrete acetylcholine are said to be cholinergic. Those that
secrete norepinephrine are said to be adrenergic.
Note: Each sympathetic preganglionic neuron bra nches extensively and synapses with
numerous postganglionic neurons. It is this high ratio of postgang lionic to preganglionic
fibers that results in widespread effects throughout the body.
SAADDES
Remember:
1. The presynaptic sympathetic nerve fibers originate in the lateral horn s of spinal cord
segments T1 -L2. From the lateral horns, all of these fibers must reach the sympathetic trunk.
Presynaptic sympathetic fibers exit the spinal cord in the ventral roots (because they are
motor fibers), pass through the spinal nerves and eventually enter the ventral primary rami
of spi nal cord segments T1-L2. Shortly after entering the ventral primary rami, the
presynaptic sympathetic fibers exit the ventral primary rami via white rami communicantes
which carry the presynaptic sympathetic fibers to the sympathetic trunk.
2. The main nerves of the PNS are the vagus nerves. They originate in the medulla oblong-
ata. Eac h preganglionic parasympathetic neuron synapses with ju st a few postganglionic
parasympathetic neurons, which are located near or in the effectors (organs, muscles or
glands).
Dysfunction of the ANS causes organ-specific or organ system-specific disease. In Horner's syn-
drome, a lack of sympathetic tone causes miosis, ptosis and anhydrosis on the affected side.
Excessive PNS activity carried by the vagus nerve can cause a vasovagal episode with hy-
potension and possible syncope. In dentistry this can be most commonly seen with standing up
very quickly after sitting for a long period of time, known as orthostatic hypotension.
Saad Alqahtani, Twitter @saaddes
nerves
Nerves connect with muscles at the . There, the ends of nerve
fibers connect to special sites on the muscle's membrane called _____
These plates contain receptors that enable the muscle to respond to
• gap junction, motor end plates, norepinephri ne
SAADDES
• mucocutaneous junction, visceral end plates, epinephrine
• neuromuscular junction, motor end plates, acetylcholine
• neuromuscular junction, sensory end plates, norepinephrine
132
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• neuromuscular junction, motor end plates, acetylcholine
Acetylcho line is released by the nerve to transmit a nerve impu lse across the neuromuscu-
lar junction. After a nerve stimulates a muscle at this junction, an electrical impul se fl ows
through the muscle causing it to contract.
Acetylcholine (ACh) is the neurotransmitter released from the presynaptic terminal and
the postsynapt ic membrane contains a nicotinic receptor. ACh is synthesized in the
neurons from which it is released. Choline acetyltransferase catalyzes the formation of
acetylcholine from acetyi-CoA and choline in the presynaptic terminal. The terminals of
motor axons contain thousands of synaptic (storage) vesicles fi lled w ith acetylcholine.
The action potential conducted along the motor nerve causes depolarization and an
SAADDES
influx of calcium. The influx of calciu m stimulates the release of ACh from storage
vesicles into the synapse. ACh binds to nicotinic receptors on the motor end plate.
Stimulation of the ACh receptor results in the opening of sodium channels (and some
potassium channels), thereby leading to an infl ux of sodium and an effl ux of potassium
through the cell membrane that resu lts in a small net depolarization termed "miniature
end plate potentials" (mEPP). If enough mEPPs occur simultaneously, their summation
creates a full-fledged "end plate potential" (EPP, not an action p otential) which
generates current in adjacent muscle tissue. This sparks an action potential in the muscle
fiber followed by muscle contraction.
Important: Following its release from the presynaptic terminal, ACh is rapidly broken
down into acetate and cho line by the enzyme acetylcholinesterase (AChE) on the motor
end-plate. Note: If acetylcholinesterase is inhibited, there w ill be prolongation of the
end-plate potential (EPP), which can lead to tetanus of the affected muscle fibers.
Note: The neuromuscular junction (NMJ) is the synapse between the presynaptic
motor neuron and the postsynaptic muscle membrane.
Saad Alqahtani, Twitter @saaddes
nerves
The entry of which of the following into the presynaptic terminal
triggers the release of neurotransmitter?
• sodium
• potassium
SAADDES
• chloride
• ca lcium
133
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• calcium
An axon terminal of a presynapt ic neuron closely app roaches a dendrite or cell body of a
postsynaptic neuron; however, the two cells are separated by a small synaptic cleft.
Neurotransmitters are stored w ithin the axon terminal of a presyna ptic neuron in
synaptic vesicles. When an action potential depolarizes the presynaptic membrane,
voltage-gated calcium channe ls are op ened, causing an increase in intracellular
calciu m. Calcium causes the synaptic ves icles to empty the neurotransmitter molecules
into the synapt ic cleft. These neurotransmitters diffuse across the synaptic cleft and
bind to specific receptors on the postsynaptic cell, causing a change to the cell
membrane's ion permeability and subsequent membrane potential. This p rocess is called
synaptic transmission and the time required is called the synaptic delay. The final step
SAADDES
is enzymatic deactivati on of the neurotransmitter through conformati onal change or
removal from the synapt ic cleft.
A synapse is an anatomical junction between two neurons where t he depolarization of
the presynaptic cell initiates a response in the postsynaptic cell. Both electrical and
chemical synapses are important means of cellu lar communication in the nervous system.
Electrical synap ses directly connect the cytosol of two neurons and allow rapid
bidirectional current flow between neurons. They act as low-pass filters.
Standard chemical synaptic transmission involves the release of transmitter from a
presynaptic terminal, diffusion of transmitter across a synapti c cleft and b inding of the
transmitter to receptors on the opposed postsynaptic membrane. Note: The entry of
calcium into t he presynapt ic terminal t riggers t he release of neurotransmitter.
Note: Gap junctions are the morphological correlate of electrical synapses. Gap junctions
contain channels formed by hemichannels called connexons. Connexons are formed by
proteins called connexins.
Saad Alqahtani, Twitter @saaddes
nerves
Strictly speaking, the all-or-none principle refers to the:
• strength of muscle contraction
• resting potential
• action potential
SAADDES
• excitatory postsynaptic potential
134
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• action potential
Any stimulus strong enough to initiate a nerve impulse is referred to as a threshold stimulus.
A single nerve cell, j ust like a sing le muscle fiber, transmits an action potential according to
t he ali-or-none principle. The principle states that if a stimulus is strong enough to generate
a nerve action potential, the impulse is conducted along the entire neuron at maximum
strength, unless conduction is altered by conditions such as toxic materials in cells or fatigue.
SAADDES
6 After a brief pe riod of hype rpoJarization, the re sting potential is restored by the sodium·potassium
pump and the return of ion channcJs to their resting state.
The action potential differs from the subthreshold and passive responses in t hree important
ways: (1 ) it is a much larger response in which the polarity of the membrane potential actually
overshoots (the cell interior becomes positive with respect to the exterior), (2) the action poten-
t ial is propagated down the entire length of the nerve fiber, and (3) t he action potential is prop-
agated without decrement (i.e., it maintains its size and shape as it is regenerated along the
axon).ln addition, when a stimulus even larger than the t hreshold stimulus is applied, the act-
ion potential remains the same and does not increase wit h greater stimulus strength. A stimu-
lus either produces a full-sized action potential or fails to do so.
Saad Alqahtani, Twitter @saaddes
nerves
Tracts descending to the spinal cord are concerned with voluntary motor
function, muscle tone, reflexes, equilibrium, visceral innervation and
modulation of ascending sensory signals. The largest and most important
of these tracts that controls skilled voluntary movement is the:
• rubrospinal tract
SAADDES
• vestibu lospinal t ract
• reticulospinal tract
• corticospinal tract
135
Irefer to AS card 195-1for illustration] copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• corticospinal tract
Universally regarded as the single most important tract concerned w ith skilled vo lun-
ta ry activity, t he corticospinal t ract ori ginates from pyramid-shaped cells in the pre-
motor, primary motor and primary sensory motor.
Name Fun ction Location Origin T ermination
Lateral Voluntary movement, Lateral white Motor areas or Lateral or anterior
corticospinal contraction of individual or columns cerebral cortex gray columns
small groups of muscles, opposite side from
SAADDES
particularly those moving tract location in cord
hand'i, fingers, feet and toes
of opposite side
Anterior Same as late ral corticospinal Anterior white Motor cortex but on Lateral or anterior
corticospinal except ma inly musc les of columns same side as location gray columns
same side in cord
Lateral rcticulospinal Mainly facilitatory influence Lateral white Reticular formation, Lateral or anterior
on motor neurons to skeletal columns midbrain, pons and gray columns
muscles medulla
Medial reticulospinal Mainly inhibitory influence Anterior white Reticular formation, Lateral or anterior
on motor neurons to skeletal columns medulla mainly gray columns
muscles
Rubrospinal Coordination of body move .. Lateral white Red nucJcus Lateral or anterior
ment and posture columns (of midbrain) gray columns
V<-<tibulospinal Mediates the influences of Lateral white Lateral vestibular Lateral or anterior
the vestibular e nd organ and columns nuc leus gray columns
the cerebe llum upon (4th ventricle)
extensor muscle tone
Saad Alqahtani, Twitter @saaddes
nerves
There are two major groups of descending tracts from the brain: the corti-
cospinal, or pyramidal tracts, and the extrapyramidal tracts.
The pyramidal tracts descend directly without synaptic interruption, from the
cerebral cortex to the spinal cord.
SAADDES
• both statements are true
• both statements are false
• the first statement is t rue, the second is false
• the first statement is false, t he second is t rue
136
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Remember: Sensory information from receptors throughout most of the body is relayed to the brain
by means of ascending tracts of fibers that conduct impulses up the spinal cord. When the brain di-
rects motor activities, these directions are in the form of nerve impulses that travel down the spinal
cord in descending tracts of fibers.
The spinal cord extend s from the level of the foramen magnum of the skull to the first lumbar verte-
bra. Unlike the brain, in which the gray matter forms a cortex over white matter, the gray matter of
the spinal cord is locat ed centrally, surrounded by white matter. The central gray matter of the spinal
cord isarranged in the form of an H, with two dorsal horns and two ventral horns (also called poster-
ior and anterior horns, respectively). The white matter of the spinal cord is composed of ascending
and descending fiber tracts. These are arranged into six columns of white matter called funiculi .
SAADDES
The ascending fiber tracts convey sensory information from cutaneous receptors, proprioceptors
(muscle and joint senses) and visceral receptors. Most of the sensory information that originatesin the
right side of the body crosses over and eventually reach the region on the left side ofthe brain, which
analyses thisinformation. Similarly, the information arising in the left side of the body isultimately an-
alyzed by the right side of the bra in. This decussation occurs in the medulla oblongata for sensory
modalities, or in the spinal cord for other modalities of sensation.
There are t wo major groups of descending tracts from the brain: the corticospinal, or pyramidal
tracts, and the extrapyramidal tracts. The pyramidal tract sdescend directly wi thout synapt ic inter-
ruption f rom the cerebral cortex to the spinal cord. The cell bodies that contribute fibers to these py-
ramidal tracts are located pri marily in the precentral gyrus(also called the motor cortex). Other areas
of the cerebral cortex however, also contribute to these tracts.
Note: The corticospinal tract scarry voluntary motor stimuli from the cerebral cortex to motor neu-
rons in the spinal cord . They are called the "pyramidal tracts" because some of them cross in th e
pyramids of the medulla. The other t racts (i.e., tectospinal, vestibulospinal, anterior corticospinal, lat-
eral and anterior reticulospinal and rubrospinal) come from a variety of locations in the brain, as a
group are termed the "extra-pyramidal tracts:' and are generally associated with balance and mus-
cle tone.
Saad Alqahtani, Twitter @saaddes
miscellaneous
Which of the following characteristics is shared by simple and facilitated
diffusion of glucose?
• it is saturable
• requires metabolic energy
SAADDES
• occurs down an electrochemical gradient
• require a Na• g radient
137
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• occurs down an electrochemical gradient
*** Both types of transport occur down an electrochemica l gradient ("downhill") and do
not require metaboli c energy.
Processes by which substances are transferred across cell membranes:
• Diffusion: the process by which molecules spread from areas of high concentration, to areas
of low concentration. Oxygen enters the cell in this manner. Oxygen moves from the blood,
where it is concentrated, to the inside of the cell, where it is not concentrated. Note: When
the molecules are even throughout a space it is called equilibrium.
• Osmosis: a type of diffusion, but involving on ly the movement of water across the mem-
brane. The water moves to the side of the membra ne that contains the most molecules of
solute d issolved in it.
SAADDES
***Diffusion and osmosis are both types of passive transport (that is, no energy is required
for the molecules to move into or out of the cell}.
• Facilitated diffusion: a process whereby a substance passes through a membrane with t he
aid of an intermediary or a facilitator. The facilitator is an integral membrane protein that
spa ns the width of the membrane. The force that drives the molecule from one side of the
membra ne to the other is diffusion.
• Active transport: the pumping of molecules or ions throug h a membrane aga inst their
concentration gradient. It requires a transmembrane protein (usually a complex of them)
called a transporter and energy. The source of this energy is ATP (primary active transport} or
another molecule with a favorabl e concentration grad ient (secondary active transport; e.g.,
cotransporters and antiporters}.
Important: Most mammalian cells transport g lucose through a family of membrane proteins
known as glucose transporters (Glut or SLC2A family). Glut- 1 mediates glucose transport into
red cell s and throug hout the blood brain barrier. It is ubiquitously expressed and transports
glucose in most cells. Glut-2 provides glucose to the liver and pa ncreatic cells. Glut-3 is the
main transporter in neurons, whereas Glut-4 is primarily expressed in muscle and adipose
t issue and is regulated by insulin. Glut-S transports fructose in t he intestine and testis.
Saad Alqahtani, Twitter @saaddes
miscellaneous
Which of the following patients has the least chance of edema formation?
• a patient with inflammation
• a patient who is standing
• a patient with venous constriction
SAADDES
• a patient with arteri olar constriction
138
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• a patient w ith arteriolar constriction
***Constriction of arterioles causes decreased capillary hydrostatic pressure and as a
result, decreased net pressure (Starling forces) across the capillary wa ll.
Note: Arteriolar dilation increases the likelihood of edema. Venous constriction and
standing cause increased capill ary hydrostatic pressure and tend to cause edema.
Inflammation causes local edema by dilating arterioles and increasing permeability.
Condition s that w ill cause extrace llular fluid e dema:
• Increased capillary pressure due, for example, to b lockage of a vein
• Decreased plasma colloid osmotic pressure due to decreased p lasma protein
SAADDES
concentration
• Increased interstitial fluid colloid osmotic pressure caused by a lymphatic
obstruction
• Increased capillary permeability, which may occu r in certain allergic responses
Edema occurs when the volu me of interstitial fluid exceeds the capacity of the lymphatics
to return the flui d to the circulation or the accumul ation of fluid in a third space, such as
the peritoneum (ascites), pleural cavity (hydrothorax) or pericardia! sac (pericardia!
effusion). Important: The physical cause of edema is positive pressure within the
interstitial spaces (see note below). Systemi c, or generalized edema, may be due to heart
failure or renal disease. Massive systemi c edema is called ana sarca.
Note: Under normal cond itions, negative pressure is p resent in t he interstitium. Nega-
tive pressure is maintained by the co mb ination of oncoti c forces and lymphatic drainage,
w ith a combined drainage capacity that exceeds hydrostatically induced shifts of water
from the intravascular compartment When factors associated with this relationship are
changed, the outcome is often abnormal interstitial water retenti on creating a positive
interstitial pressure.
Saad Alqahtani, Twitter @saaddes
miscellaneous
Match the scenario to the solution options.
So lution Options Scenarios
I. Isotonic A. A solution that when placed on the outs ide of the cell will
2. Hypoton ic cause osmos is out of the cell
3. Hypertonic B. A solution that when p laced on the outs ide of the cell wall will
SAADDES
cause osmos is into the cell
C. A solution that when p laced on the outs ide of the cell will not
cause osmos is
139
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. C, 2. B, 3. A
An isotonic solution is a solution that has the same salt concentration as t he normal
cells of t he body and the blood. This solution, when placed on the outside of a cell,
wi ll not cause osmosis and the cel l will not shrink or swell.
Note: A 0.9% solution of sodium chlori de or a 5% g lucose solution are both
approximately isotonic to plasma.
A hypotonic solution is a solution w ith a lower salt concentration t han in normal
cells of the body and the blood. This solution, when placed on the outside of a cell,
will cause osmosis into the cell and lead to swelling and lysis of the cell.
SAADDES
Note: Any solution of sodium ch loride w ith less than 0.9% concentration is hypotonic.
A hypertonic solution is a solution with a higher salt concentration than in normal
cells ofthe body and the blood. This solution, when placed on the outside of a cell will
cause osmosis out of the cell and lead to shrinkage of the cel l.
Note: Sodium ch loride solutions of g reater than 0.9% concent ration are all
hypertonic.
Isotonic solutions have the same solute concentrations as each other. If isotonic
solutions are separated by a partially permeable membrane, the water potential will
be the same on either side. There w ill be no net osmotic movement of water between
the two solutions. The amount of water that moves in one direction will be exactly
balanced by the amount that moves back in the other.
Saad Alqahtani, Twitter @saaddes
miscellaneous
Which of the following is NOT an oncogene?
• HER-2/neu
• ras
•myc
• src
·CAAT SAADDES
140
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
· CAAT
*** CAAT is the binding site for RNA transcription factors.
An oncogene is a defective gene t hat is involved in tr iggering cancer cell
growth. Oncogenes are altered forms of genes (proto-oncogenes) that normally are
involved in stimulating cell division. These normal genes are mutated and function in
an inappropriate manner in cancer cells. Important: One or more oncogenes are
mutant in all forms of cancer.
Note: A proto-oncogene is a gene that has functions to promote cell division. When
these genes are mutated, defective versions of these genes are formed (oncogenes),
which may produce products that promote cell division in an abnormal fashion .
SAADDES
A key feature of oncogene activity is that a single altered allele leads to unregula-
ted growth. This is in contrast with tumor suppressor genes, in which both alleles
must be defective to lead to abnormal cell division.
The following selected oncogenes have been associated with numerous cancer
types:
• HER-2/neu: a growth factor receptor - it has been identified in up to 30% of
human breast cancers
• ras: a signal transduction molecule - it has been identified in cancers of many dif-
ferent origins including pancreas (90%), colon (SO%), lung (30%), thyroid (SO%), blad-
der (6%), ovarian (lS%), breast, skin, liver, kidney and some leukemias
• myc: a transcription factor - mutations in the myc gene have been found in many
different cancers, including Burkitt's lymphoma, B-cell leukemia, and lung cancer
• src: a protein tyrosine kinase - it was t he first oncogene ever d iscovered. It has
been identified in human neuroblastoma, small-cell lung cancer, colon and breast
ca rcinomas and rhabdomyosarcoma
Saad Alqahtani, Twitter @saaddes
miscellaneous
The organic part of bone matrix is mainly composed of type Ill collagen.
The collagen fibers provide bone with great tensile strength, while the
inorganic salts allow bone to withstand compression.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is false
• the first statement is fa lse, the second is true
141
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
The organic part of bone matrix is mainly composed of type I collagen. Osteoblasts
are mononucleate bone-forming cells that descend from osteoprogenitor cells.
Osteoblasts are located on the surface of osteoid seams and make a protein mixture
known as osteoid, which mineralizes to become bone. Osteoid is pri maril y composed
of type I collagen.
The intercellular matrix of bone conta ins both organic components
(glycosaminoglycans in the ground substance and collagen fibers) and inorganic
salts. The inorganic salts consist primarily of calcium phosphate, wh ich is present in
SAADDES
the form of highly insoluble crystals of hydroxyapatite. The collagen fibers provide
bone w ith great tensile strength, while the inorganic salts allow bone to withstand
compression.
Some of the common g lycosaminoglycans present in the intercellular matrix of bone
include hyaluronic acid and chondroitin sulfate. The intercellular matrix also
conta ins a calcium-bind ing protein called osteocalcin as well as a calcium and
collagen-binding protein called osteonectin.
Age, race and gender affect bone mass, structural integri ty and bone loss. For exam-
ple, blacks commonly have denser bones than wh ites, and men commonly have
denser bones than women. Point to remember: Bone density and structural integrity
(ability to withstand stress) decrease after age 30 in women and 45 in men. Thereafter,
a relatively steady quantitative loss of bone matrix occurs.
Saad Alqahtani, Twitter @saaddes
miscellaneous
All of the following bonds are considered to be weak bonds EXCEPT one.
Which one is the EXCEPTION?
• hydrogen bonds
• ionic bonds
• covalent bonds
• van der Waa ls forces
SAADDES
Weak bonds are involved in all of the following EXCEPT one. Which one is the
EXCEPTION?
• secondary structure of proteins
• cell membrane
• dsDNA structure
• amino acid linkage
142
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• covalent bonds
• amino acid linkage
Covalent bonds are t he strongest possible type of chemical bond. Other chemical
bonds include ionic bonds, hydrogen bonds and the van der Waals force. There are nu-
merous other types of rare and exotic bonds, but the first fou r are by far t he most com-
mon.
Covalent bonds are created between atoms w ith similar electronegativity. In general,
electronegativity increases as you move to the right of the periodic table and decreases
as you move down the peri odic table. Electronegativity is not an atomic property, but
emerges when atoms interact w ith other atoms.
SAADDES
Covalent bonds are forces that hold atoms together. The forces are formed when the
atoms of a molecule share electrons. Two examples of covalent bonds are peptide
and disulfide bonds. Note: Hydrogen, oxygen, nitrogen and ca rbon are capable of
forming one, two, three and fou r cova lent bonds, respectively. Carbon is very
versatile and can form cova lent single, doubl e and t ri ple bonds.
Weak bonds may be easily broken but are very important because they help to
determ ine and stabilize the shapes of biological molecules. For example weak bonds
are important in stabilizing t he secondary structure (a-helix and ~-sheets) of
p roteins. Hydrogen bonds keep complementa ry strands of DNA together and
participate in enzymatic catalysis. These interactions are individually weak but
collectively strong.
Note: Denaturing agents (organic solvents, urea and detergents) act primarily by
disrupting the hydrophobic interactions that make up t he stable core of g lobular
proteins.
Saad Alqahtani, Twitter @saaddes
miscellaneous
The pitch of a sound is related mainly to which of the following
characteristics of a sound wave?
• amplitude of the sound wave
• frequency of the sound wave
SAADDES
• superimposed wave
• secondary waves
•length of the sound wave
143
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• frequency of the sound wave
A sound can be characterized according to its pitch, loudness and timbre (quality).
As mentioned, the pitch is related to the frequency of the sound wave. In general,
the higher t he frequency of a sound wave, t he higher t he pitch of the sound wave.
Note: Frequency is measured in hertz (Hz) or cycles per second.
The loudness of a sound is related to t he intensity and the amplitude of the wave.
Usuall y, the greater the amplitude of a particular sound wave, the greater the
SAADDES
intensity of the wave and the louder t he sound.
Note: Intensity is measured in decibels (dB).
The timbre or quality of a sound is related to the presence of additional sound-wave
frequencies superimposed on the principal frequency.
Saad Alqahtani, Twitter @saaddes
miscellaneous
The major intracellular cation is:
• sodium
• potassium
• magnesium
• chrom ium
SAADDES
144
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• potassium
Functionally, the body's water is effectively compartmentalized into two major fluid compart-
ments:
Intracellular Fluid (ICF) comprises 2/3 of t he body's water.
• If the body has 60% water, the ICF is about 40% of the weight
• The ICF is primarily a solution of potassium and organic anions, proteins, etc.
• The cell membranes and cellular metabolism control the constituents of t his ICF
• The ICF is not homogeneous in the body. The ICF represents a conglomeration of fluids from
all the different cells
Extracellular Fluid (ECF) is t he remaining 1/3 of t he body's water.
• The ECF is about 20% of the weight
SAADDES
• The ECF is primarily a NaCI and NaHC0 3 solution
• The ECF is fu rther subdivided into t hree subcompartments:
1. 1nterstitial fluid (I SF) surrounds the cells, but does not circulate. It comprises about
3/4 ofthe ECF.
2. Plasma circulates as the extracellular component of blood. Plasma makes up about 1/4
of the ECF.
3. Tran scellular fluid is a set of fluids that are outside of the normal compartments.
These 1-21iters of fluid make up the CSF, d igestive juices, mucous, etc.
The 60-40-20 Rule:
• 60% of body weight is water
• 40% of body weight is intracellular fluids
• 20% of body weight is extracellular fluid
1. All t he body's fluid compartments are in osmotic equili brium (except for transient
8 changes).
2. The ions and small solutes that constitute the ECF are in equilibrium with similar
concentrations in each subcompartment.
3. The ECF volume is proportional to the total Na• content.
Saad Alqahtani, Twitter @saaddes
miscellaneous
The temperature of the body is regulated by neural feedback mechanisms
that operate primarily through the hypothalamus.
Shivering is the most potent mechanism for increasing heat production.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is false
• the first statement is fa lse, the second is true
145
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
The temperature of the body is reg ulated by neural feedback mechanisms that operate
primarily through the hypothalamus. The hypothalamus conta ins not only the control
mechanisms but also the key temperature sensors. Under control of these mechanism s,
sweating begins alm ost precisely at a skin temperature of 37•c and increases rapidly as
the skin temperature rises above this value. The heat production of the body under these
cond itions remains almost constant as the skin temperature rises. If the skin temperature
drops below 37•c, a variety of responses are initiated to conserve the heat in the body
and to increase heat production. These include: vasoconstriction to decrease the flow of
heat to the skin, cessation of sweating, shivering to increase heat production in the
muscles and the secretion of norepinephrine, epinephrine and thyroxine to increase heat
SAADDES
production.
***Shivering is the most potent mechanism for increasing heat production.
The human body has the remarkable capacity for regulating its core temperature
somewhere between 98°F and too•F when the ambient temperature is between
approximately 68°F and 130•F.
When the amb ient temperature is above body temperature, then radiation, conduction
and convection all transfer heat into the body rather than out. Since there must be a net
outward heat transfer, the on ly mechanisms left under those cond itions are the
evaporation of perspiration from the skin and the evaporative cooling from exhaled
moisture.
Radiation is heat transfer by the emission of electromagnetic waves that carry energy
away from the emitting object. Conduction is heat transfer by means of molecular
agitation w ithin a material without any motion of the material as a whole. Convection
is heat transfer by mass motion of a flu id such as air or water when the heated fluid is
caused to move away from the source of heat, carrying energy with it .
Saad Alqahtani, Twitter @saaddes
miscellaneous
Which of the following solutions has an osmotic pressure different from the
other two solutions?
• 1M glucose
• 1M sodium chloride
SAADDES
• 1M potassium chlori de
• they all have the same osmotic pressure
146
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• 1M glucose
***The key to this question is the fact that osmotic pressure of a solution depends on
the number of solute particles present and not on their various properties. Sodium
chloride and potassium ch loride wil l ionize into two ions per molecule, whereas
glucose will remain a single molecule in solution.
• Osmosis is the net d iffusion of water through a semipermeable membrane
caused by a concentration difference.
• Osmotic pressure is the pressure that develops in a solution as a result of net
osmosis into that solution; osmotic pressure is affected by the number of d issolved
SAADDES
particles per unit volume of flu id. Note: Intracellular (fluid w ithin cells) and extra-
cellular (interstitial flu id and plasma) fluids have similar total osmotic pressures.
Osmolarity is expressed in units of osmoles per liter of solution (osmoi/ L), wh ile osmo-
lality is defined as osmoles per kilogram solvent (osmol/kg).
While similar, osmolarity and tonicity are not the same. The key d ifference between
the two is that osmolarity is a measure of all solutes in solution, whereas tonicity is a
measure of impermeable solutes. Osmolarity compares the amount of solutes in
two solutions, whereas tonicity compares the osmotic pressure gradient. If a
solution in compartment A is hyperton ic to a solution in compartment B, water will
flow from compa rtment B to compartment A in an effort to dilute the solutes in
compa rtment A. This allows the two compa rtments to have equal solute concentra-
tion.
Saad Alqahtani, Twitter @saaddes
miscellaneous
Which of the following statements concerning the two principal laws of
thermodynamics is FALSE?
Select all that apply.
• they apply only to closed systems, that is, entities within which there can be no
loss of energy or of mass
SAADDES
• the f irst law says that the total quantity of energy in the universe remains
constant (this is the pri nciple of the conservation of energy)
• the second law states that the quality of this energy is degraded irreversibly
(this is the principle of the degradation of energy)
• the second law, known as Carnot's principle, is controlled by the concept of
entropy
• the two laws describe the concept that Delta G is positive in an exergonic
reaction
147
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the two laws describe the concept that Delta G is
positive in an exergonic reaction
The principle energy laws that govern every organization are derived from the two
famous laws of thermodynamics. Heat, being a form of energy, is subject to the
princip le of energy conse rvation; th is p ri nciple is called the fi rst la w of
thermodynamics - the tota l energy, including heat, in a closed system is conserved.
Heat, being a form of energy can be transformed into work and other forms of
energy, and vice versa. However, this t ransformation of heat energy is subject to a
very important restriction, called the second law of thermodynamics.
SAADDES
It can be given in three equiva lent fo rms:
1. Heat flows spontaneously from a hot body to a cool one
2. One cannot convert heat completely into useful work
3. Every isolated system becomes disordered in time
*** Entropy is a measure of the degree of randomness or d isorder of a system.
Certain chemica l reactions proceed spontaneously until equilibrium is reached.
Reactions that proceed with the release of energy are exergonic. Because the
products of such reactions have less free energy than the reactants, the free-energy
change (D.G) is negative. Chemical reactions in wh ich the products have more free
energy than the reactants are enderg onic. For these reactions, the D.G is positive,
and heat is con sumed as a reactant.
Saad Alqahtani, Twitter @saaddes
miscellaneous
Isotopes of an element:
• have di fferent chemica l properties but t he same weights
• have the same chemical properties but different weights
• have d ifferent chemica l properties and weights
SAADDES
• have the same chemical properties and weights
143
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• have the same chemical properties but different weights
Atoms of the same element can have d ifferent numbers of neutrons; the d ifferent
possible versions of each element are called isotopes. For example, the most
common isotope of hydrogen (protium) has no neutrons at all; there's also a hydrogen
isotope ca lled deuterium, w ith one neutron, and another, tri tium, with two neutrons.
Isotopes are stable or radioactive forms of an element that differ in atomic weight
but are otherw ise chemically identica l to the naturally abundant form of the element.
Isotopes of a given element have the same number of protons but differ in the
number of neutrons. Important point: Isotopes have the same atomic number but
SAADDES
different mass numbers.
Remember: The atomic number is the number of protons and the mass number is
the sum of protons and neutrons.
Note: The radioactive forms of isotopes are often used as tracers in medical radio-
graphy
Saad Alqahtani, Twitter @saaddes
miscellaneous
Growth and preparation of the chromosomes for replication occurs in
which phase of the cell cycle?
•5
•M
SAADDES
149
copyright 0 201}·2014 Oental Dt<:ks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
The cell cycle is an ordered set of event s, culminating in cell growth and division into two
daughter cells. The stages are G 1 - S- G2 - M .
• The G 1 stage stands for "GAP 1"
• The S stage stands for "Synthesis" (the stage when DNA replication occurs)
• The G2 stage stands for "GAP 2"
• The M stage stands for "Mitosis" [t he stage when nuclear chromosomes separate
and cytoplasmic (cytokinesis) division occur). Mitosis is further divided into: p ro-
phase, prometaphase, metaphase, anaphase and telophase. Interphase is often
included in discussions of mitosis, b ut interphase is techn ically not part of mitosis, but
SAADDES
rather encompases stages G1, 5 and G2 of the cell cycle.
The cell cycle consists of the follow ing:
• G 1 = growth and preparation of t he chromosomes for replication
• S = synthesis of DNA (and centrosomes)
• G2 = p reparati on for mitosis
• M = mitosis
The period between M and 5 is called G 1; that between 5 and M is G2 . Note: Many t im es
a cell will leave the cell cycle, temporarily or permanently. The cell exits the cycle at G1 and
enters a stage designated G0 (G zero). Many G0 cells are busy carrying out their functions
in the organism (e.g., secretion, attacki ng pathogens).
Important: Protein and RNA synthesis occu r in all phases of the cell cycle except M
(mitosis). A eukaryotic cell cannot divide into two, t he two into four, etc. unless two
p rocesses alternate: • doubling of its genome (DNA) in S pha se (synthesis phase) of t he
cell cycle
• halving of that genome during mitosis (M phase)
Saad Alqahtani, Twitter @saaddes
-<M II
SAADDES GO
(/
Cell Cycle
Schematic of the cell cycle. M =Mitosis, G J=Gap I, G2=Gap 2, S=Synthesis; not in
ring: GO=Gap 0/Resting
149· 1
Saad Alqahtani, Twitter @saaddes
miscellaneous
Which class of antibody is the first antibody to appear in the circulation after
antigen stimulation?
•lgA
•lgD
SAADDES
•lgE
•lgG
•lgM
150
copyngh t 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• lgM
Antibodies are protein molecules produced by plasma cells in the spleen and lymph
nodes in response to stimulation by antigens. Antibodies leave the immune system
environment and travel through the circulation to the infection site. Here they
interact with microorganisms or other biochemicals and exert a specific immune
response. Antibody molecules are composed solely of protein; a typical antibody
molecule consists of two "heavy" chains of 400 amino acids and two "light" chains
of 200 amino acids.
SAADDES
lgG Most common antibody; important antibody of the secondary antibody response; passes the
placenta and enters d1e fetal c irculation.
lgA Second most abundant; occurs in body secretions and protects surface tissues; synthesized by
the plasma cells in the mucous membranes of the GI, respiratory and urinary tracts.
IgO Serves as the receptor site on the surface of the B lymphocytes; function is unknown or not
fully understood .
JgM Large antibody consisting o f five antibody units; important in the primary antibody response;
first antibody to appear in the circulation after antigen stimulation; does not pass the placenta
or enter the fetal circulation. Important in complement activation and primary antibody against
A and B antigens on red blood cells
lgE Is present in only trace amounts in serum; reaginic activity resides in the immunoglobulin;
protects extemal mucosal surfaces; tightly bound to its receptors on mast cells and basophils;
responsible for type I hypersensitivity reactions (allergic and anaphylactic).
Saad Alqahtani, Twitter @saaddes
kidneys
Three patients ingest three different substances. Match the substance to the
description of the patient's urine.
Description Substance
I. J im are a substance that is fi ltered into the renal tubules A. Inu lin
bur is then reabsorbed fully
B. Glucose
2. Art are a substance that is filtered and secreted, so the
SAADDES
C. Para-am inohippurate (PAH)
entire amount of substance was released in the first pass
3. Mau are a substance that was freely filtered and neither
secreted or reabsorbed
Which patient is being tested for his glomerular filtration rate (GFR)?
• Jim
• Art
• Matt
151
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. B, 2. C, 3. A
• Matt
Inulin is a starch that is given by mouth. Inulin is freely fil tered from t he g lomerular
capillaries into Bowman's capsu le, but inulin does not undergo tubu lar secretion or
reabsorption. The glomerular filtration rate (GFR) can be calcu lated by the clearance
of inulin from plasma. The rate at which a substance is cleared from plasma =
plasma volume completely cleared I unit time = (the uri ne concentration of the
substance * urine vo lume) I plasma concentration ofthe substrate.
Important: If t he clearance of a substance that is freely filtrated is less than that of
inulin, then there is a net reabsorption of the substance. If t he cl earance of a
SAADDES
substance t hat is freely fil tered is greater than that of inulin, t hen there is a net
secretion of the substance. If the cl earance of a freely filtered substance is equal to
that of inulin, then (1) it is neither secreted nor absorbed or (2) it is both secreted
and absorbed in equal amounts.
1. PAH is both filtered and secreted and is used to estimate rena l plasma
flow. Glucose and sodium chloride are filtered and subsequently reab-
sorbed.
2. Assessment of blood urea nitrogen (BUN) and serum creatinine can also
be used to estimate t he GFR. Some literatu re states that the most accurate
measure of GFR is creatinine clearance. Patients w ith chronic kidney disease
are staged according to GFR and proteinuria. Risk factors incl ude diabetes,
high bl ood pressure, fami ly history, and smoking. Staged 1 through 5- Stage
5 (requiring dialysis).
3. If t he amount of a substance excreted in the urine is less than the amount
filtered, then the substance is reabsorbed.
Saad Alqahtani, Twitter @saaddes
kidneys
The thick ascending limb of the loop of Henle is called the "diluting
segment" because:
• sodium ch loride (NaCI) is reabsorbed with a proportional amount of water
• water is reabsorbed from the tubu lar lumen
SAADDES
• water is secreted into the tubu lar lumen
• sodium chloride (NaCI) is reabsorbed without water
• sodium ch loride (NaCI) is reabsorbed and water is secreted
152
Irefer to AS card 21-1for illustration) copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• sodium chloride (NaCI) is reabsorbed without water
The nephron is the basic structural and functional unit of the kidney. The nephron's chief function is
to regulate the concentration of water and soluble substances like sodium saltsby filtering the blood,
reabsorbing what is needed and excreting the rest as urine.
Two general classes of nephrons are cortical nephrons and juxtamedullary nephrons. Cortical
nephron shave their renal corpuscle in the superficial renal cortex, while the renal corpuscles of j ux-
tamedullary nephrons are located near the renal medulla. Functionally, cort ical and j uxtamedullary
nephronshave dist inct roles. Cortical nephrons (85%of all nephrons) mainly perform excretory and
regulatory functions, while juxtamedullary nephrons (15% of nephrons) concentrate and dilute
uri ne.
The flow of the renal tubule is as follows:
SAADDES
• The proximal tubule: Fluid in the filtrate entering the proxi mal convoluted tubule is reabsorbed
into the peritubular capillaries, including approximately two-thirds of the filtered salt and wat er
and all filtered organic solutes (primarily glucose and amino acids).
• The loop of Henle extend s from the proximal tube and consists of a descending limb and ascend-
ing limb. The loop of Henle begins in the cortex, receiving filtrate from the proximal convoluted
tubule, extends into the medulla and then returns to the cortex to empty into the distal convoluted
tubule.The loop of Henle's primary role is to concentrate the salt in the interstitium, the tissue sur-
rounding the loop.
l . lts descending limb is permeable to water but completely impermeable to salt and thus
only indirectly contributes to the concentration of the interstitium.
2. Unlike the descending limb, the ascending limb of the loop of Henle is impermeable to
water, a critical feature of the countercurrent exchange mechanism empl oyed by the loop.
The ascending limb actively pumps sodium out of the filtrate, generating the hypertonic in-
terstiti um that drives countercurrent exchange.
• Much of the ion transport taking place in the distal convoluted tubule is regulated by the en-
docrine system. In the presence of parathyroid hormone, the distal convoluted tubule reabsorbs
more calcium and excretes more phosphate. When aldosterone is present, more sodiu m is reab-
sorbed and more potassium excreted.
Saad Alqahtani, Twitter @saaddes
kidneys
The kidneys regulate acid-base balance by the:
• secretion of bicarbonate ions (HC0 3-) into the rena l tubu les and the reabsorption of
hydrogen ions (H ')
• secretion of hydrogen ions (W) into the rena l tubu les and the reabso rption of
SAADDES
bicarbonate ions (HC0 3-)
• secretion of both hydrogen (W) and bicarbonate ions (HC0 3-) into the rena l tubu les
• reabsorption of both hydrogen (W) and bica rbonate ions (HC0 3-)
153
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• secretion of hydrogen ions (H') into the renal tubules and the
reabsorption of bicarbonate ions (HCo 3 ·)
There are three primary systems that regulate the hydrogen ion concentration in the body flu-
ids:
1. The chemical acid base buffer system of the body fluids, which immediately com bi ne
with acid or base to prevent excessive changes in hydrogen ion concentration.
2.The respiratory center, which regulates the removal of C02 (and therefore H2C0 3) from the
extracellular fluid.
3. The kidneys, which can excrete either acid or alkaline urine, thereby readjusting t he extra-
cellular fluid hydrogen ion concentration toward normal during acidosis or alkalosis.*** The
kidneys, although providing t he most powerful of all the acid-base reg ulatory systems, re-
SAADDES
q uire many hours to several days to readjust t he hydrogen ion concentration.
The hydrogen ions are secreted into t he tubules by tubu lar cells. The secretion mechanism
derives hydrogen ions from carbonic acid. The enzyme carbonic anhydrase is present within
tubular cells and it catalyzes the formation of carbonic acid from carbon dioxide and water. The
carbonic acid dissociates into hydrogen ions (H+) and bicarbonate ions (HC0 3'). The H· ions are
secreted into the t ubules, and the HC0 3· ions pass out of the tubu lar cells and into the blood.
This leads to a net reabsorption of HC0 3·, but not a net secretion of H+.
Phosphate compounds (HP04 ·) and ammonia (NH 3) act as buffers to tie up hydrogen ions in
t he tubular fluid and are responsible for the net secretion of H+. Phosphate compounds are
excreted in combination with a cation such as sod ium (Na+), Ammonium ions are excreted in
combination with anions such as chloride (Cr).
1. Ammonia is form ed in t he tubular cells by the d eamination of certain am in o
Notes
acids, particularly glutamic acid.
2. Phosphate and ammonium excretion measurements provide good information
on how much acid is being eliminated by t he kidneys.
Saad Alqahtani, Twitter @saaddes
kidneys
_ _ _ is the best overall index of kidney function.
• CPR
• TFR
•APR
• GFR
SAADDES
154
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• GFR
The glomerular filtration rate (GFR) is the rate at which the glomeruli filter blood, normally
about 120 ml/minute. Clinically, the GFR is evaluated by measuring plasma [creatinine). GFR
depends on:
• Permeability of capi llary walls
• Vascular pressure
• Filtration pressure
• Clearance
The GFR is increased by:
• Vasodi lation of afferent arterioles: increases t he glomeru lar capillary hydrostatic
pressure and increases renal blood flow (RBF)
SAADDES
• Vasoconstriction of efferent arterioles: also increases the glomerular capi llary hyd ro-
static pressure
• Decreased hydrostatic pressure in Bowman's capsu le: blockage of urine transport
th rough t he ureters will increase hydrostatic pressure in Bowman's capsule and cause a
decrease in GFR
• Decreased plasma colloid osmotic pressure: associated with a decrease in the concen-
t ration of plasma proteins
Important: Autoregulation allows GFR and RBF to remain constant despite changes in arterial
blood pressure between 90 and 180 mm Hg.
Remember:
• If t he tubules neither reabsorb nor secrete the substance, as happens with inulin or
creatinine, clearance equals the GFR
• If the tubules reabsorb the substance, clearance is less than the GFR
• If the t ubules secrete the substance, clearance exceeds t he GFR
• lfthe t ubules reabsorb and secrete the substance, clearance may be less than, equal to,
or greater than the GFR
Note: Excessive constriction of the afferent arteriole will decrease RBF and GFR.
Saad Alqahtani, Twitter @saaddes
kidneys
The countercurrent mechanism is a system in the renal _ _ that facilitates
the _ _ of the urine. The system is responsible for the secretion of _ _
urine in response to _ _ plasma osmolarity.
• cortex/concentration/hyperosmotic/elevated
SAADDES
• medulla/dilution/hypo-osmotic/depressed
• cortex/dilution/hypo-osmotic/depressed
• medulla/concentration/hyperosmotic/elevated
155
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• medulla/concentration /hyperosmotic/elevated
The countercurrent mechanism is a system in the rena l medulla that facilitates
concentration of the urine as it passes through the rena l tubules. This mechanism is
responsible for the secretion of hyperosmotic urine in response to elevated plasma
osmolari ty and requires the penetration of the loop of Henle into the rena l medulla
for the development of a medullary osmotic gradient. The mechanism depends on
the special anatomical arrangement and transport properties of the loop of Henle.
Important: The kidney dialysis machine is an example of a countercurrent
mechanical system.
SAADDES
The countercurrent multiplier in the loop of Henle is dependent upon the active
reabsorption of sodium chloride by the thick ascending loop of Henle, the osmotic
equilibrium between interstitial fluid and tubular fluid in the descending loop of
Henle and continued inflow of new sodium chloride from the proximal tubule into
the loop of Henle. The sodium chloride reabsorbed from the ascending loop of Henle
keeps adding to the newly arrived sodium chlori de, thus "multiplying" its
concentration in the medullary interstitium.
Countercurrent exchange occurs in a region of the peritubular capillary bed called
the "vasa recta:'
Important point: The vasa recta do not create the medullary hyperosmolari ty but
do prevent it from being dissipated and can carry away the water that has been
reabso rbed.
Saad Alqahtani, Twitter @saaddes
kidneys
Reabsorption of glomerular filtrate would be most affected if modifications
were made to the permeability of which section of the nephron?
• descending loop of Henle
• distal convo luted tubu le
SAADDES
• proximal convo luted tubu le
• ascending loop of Henle
156
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• proximal convoluted tubule
*** Approximately 2/3 of the glomerular filtrate is reabsorbed in the proximal
convoluted tubule. This includes almost 100% of the filtered glucose and amino
acids.
Glomerular filtration is the filtration process as blood flows through the kidney.
Some of the plasma (16% to 20%) is fi ltered out of the g lomerular capillaries and into
the g lomerular capsules of the renal tubules as the g lomerular filtrate. This filtrate
contains most plasma components but is free of large protein s.
SAADDES
Excretion Rate =Filtration Rate- Reabsorption + Secretion
Reabsorption is the movement of solutes from tubular flu id into interstitial flu id.
Reabsorption takes place not only in the proximal tubule but also in the loop of
Henle, the d istal convoluted tubule and the collecting duct.
Processes include: pri mary active transport, secondary active transport, faci litated
diffusion, simple d iffusion and solvent drag. Transport can be either transcellular or
paracellular.
Secretion is the movement of solutes from the interstitial fluid into the tubular flu id.
Saad Alqahtani, Twitter @saaddes
kidneys
Your afternoon patient complains that she has consumed "tons of liquids"
today. The patient asks ifthis will have an effect on her urine concentration.
What would you say in response to this question?
• Your plasma osmolarity is lower than normal, and yo u will likely excrete a large amount
of concentrated urine
• Your plasma osmolarity is lower than normal, and yo u will likely excrete a large amount
of dilute u rine
SAADDES
• Yo ur plasma osmolarity is higher than normal, and you will likely excrete a large amount
of concentrated urine
• Yo ur plasma osmolarity is higher than normal, and you will likely excrete a large amount
of dilute u rine
What are the normal values for daily glomerular filtrate amount and
excretion amount, respectively?
• 1SO - 2SO L; 1 - 2 L
• 1SO - 2SO L; 12 L
• 4S - 7S L; 1 - 2 L
• 4S - 7S L; 12 L
157
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• Your plasma osmolarity is lower than normal, and you
will likely excrete a large amount of dilute urine
• 1 SO to 2SO L; 1-2 l
When tu bular secretion and reabso rption processes are completed, the fluid
remaining w ithin the tubu les is transpo rted to other components of t he uri nary
system to be excreted as urine. Urine consists of water and other materi als that were
filtered or secreted into the tubu les but not reabso rbed.
Although the daily GFR in normal individuals is variable, with a range of 1 SO to 2SO
L/24 hr., the kidneys normally excrete only 1 to 2 L of urine per day. Approximately
SAADDES
99% of the filtrate is returned to the vascular system, while 1% is excreted as urine.
Water and substances t he body needs are retu rned to the blood, w hereas waste
products and excess flu id and solutes remain in the tubu les and are excreted from the
body as urine.
Note: In response to elevated plasma osmolarity, a small vo lume of concentrated
uri ne w ill be produced. If plasma osmolarity is lower than normal, a large volume of
dilute urine wi ll be excreted.
Saad Alqahtani, Twitter @saaddes
kidneys
Ammonia is produced from the metabolism of a variety of compounds.
1. Which compound listed below is quantitatively the most important source
of ammonia?
2. Which compound is not a source of ammonia?
3. Which compound is converted to ammonia mainly in the kidney?
SAADDES
• glutamine
• amino acids
• amines
• puri nes and pyrimidines
• triglycerides
158
copyngh t 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• amino acids
• triglycerides
• glutamine
Sources of ammonia:
1. From amino acids: many tissues, but particula rl y the liver, form ammonia
from amino acids by the aminotransferase and glutamate dehydrogenase react-
ions.
2. From glutamine: the kidneys (specifically, the tubular cells) form ammonia
from glutamine by the action of rena l glutaminase. Most of this ammonia is
excreted into the urine as NH4 • , which is an important mechanism for maintaining
SAADDES
the body's acid-base balance.
3. From amines: amines obtained from the d iet and monoamines that serve as
hormones or neurotransmitters give rise to ammonia by the action of amine oxi-
dase.
4. From purines and pyrimidines: in the catabolism of purines and pyrimidines,
amino groups attached to the rings are released as ammonia.
Note: The formation of urea (which is a main product of protein nitrogen
metabolism) in the liver is qualitatively the most important disposal route for
ammonia. Urea travels in the blood from the liver to the kidneys, where urea passes
into the glomerular filtrate.
Important: Excessive accumulation of uric acid crystals in the blood causes gout.
Remember: Arginase directly catalyzes urea formation in a cell.
Saad Alqahtani, Twitter @saaddes
kidneys
1. Which of the following processes is not involved in the formation of urine?
2. Which two of the following processes in the formation of urine involve the
most similar amounts of fluid transport?
3. Which two processes supplement each other, working in the same
"direction"?
SAADDES
4. Which process is most affected by levels of ADH?
5. Which process occurs in Bowman's capsule?
• filtration
• reabsorption
• excretion
• secretion
159
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. excretion- urine is excreted once it is formed, excretion is not part of formation
2. filtration and reabsorption- about 99% of the filtrate is reabsorbed
3. filtration and tubular secretion- both send substances from blood to tubules
4. reabsorption
5. filtration
The formation of urine has th ree processes: filtration, reabsorption and tubula r secretion.
During filtration, or glomerular excretion, blood pressure forces all the small molecules in the
blood into the lumen of the nephron through the pores both in the walls of the glomerular
capillaries and in t he wall of the Bowman's capsule. The filtrate has the same concentration of
d issolved substances as the blood minu s the formed elements and the plasma proteins t hat
are too large to fit through the pores of t he capillaries and the Bowman's capsule. As the filtrate
SAADDES
passes through the tubules of t he nephron, water and many dissolved materials are reabsorb-
ed by t he blood. In fact, during the filtrate's passage through the tubules, up to 99% of the
water is reabsorbed. In addition, the t ubules also remove substances from the blood. This
process, called tubular secretion, supplements the initial g lomerular fi ltration.
Normal urine is clear, straw-colored and slig htly acidic, and has the characteristic odor of
urea. The formation of urine is important in the regulation of acid-base balance, maintenance
of ECF volume and blood pressure and in maintaining the normal osmolarity of ECF.
Diuresis results from a decrease in the tubu lar reabsorption of water.
Possible Causes of Dilute Urine Possible Causes of Con centrated Urine
0 Absence of ADH 0 Decreased plasma volume
0 Diabetes insipidus 0 Cellular dehydrat ion
0 Diabetes mell itus
0 Excess ADH
Saad Alqahtani, Twitter @saaddes
heart
Cardiac muscle has a shortened action potential compared to skeletal
muscle.
In cardiac muscle, the action potential is caused by opening oftwo types of
channels.
SAADDES
• both statements are t rue
• both statements are fa lse
• the first statement is true, the second is fa lse
• the first statement is false, the second is true
160
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
The action potential in a ventricular muscle fi ber, averages ab out 1OS m illivolts, which means t hat the
intracellular potenti al ri ses from a very negative value, about ·85 millivolts, bet ween beats to a slightly
positive value, about +20 millivolts, du ring each beat After an initi al spike, the membrane remains de·
polarized for about 0.2 second, exhi biti ng a plateau, foll owed at the end of the pl ateau by ab rupt re·
polarization. Important point: The presence of the plateau in t he action potential causes ventricular
contraction to last as much as 15 times as long in cardiac muscle as in skeletal muscle.
At least t wo maj or d ifferences bet ween the membrane properties of card iac and skeletal muscle ac·
count for the prolonged action potential and the plateau in cardiac muscle:
1. First, the action potential of skeletal muscle iscaused almost entirely by sudden opening of large
numbers of so-called fast sodium channels that all ow a tremendous amount of sodium to enter
the muscle fi ber. These channels are called fast channels because they remain open only for a very
SAADDES
short period of time and then abruptly close. At the end of this cl osu re, repolarization occurs and
the action potential is over within another thousandth of a second or so. In cardiac muscle, t he ac·
tion potential is caused by opening of two types of channels: (1) t he same fast sodium channels as
those in skeletal muscle and (2) an entirely d ifferent population of slow calcium channels, which
are also called calcium-sodium channels. This second population of channels d iffers from t he fast
sodium channels in that they are slower to open and, even more important, remain open for several
tenths of a second.
2. Secondly, a major functional d ifference between cardiac muscle and skeletal muscle t hat helps ac·
count for both the pro longed action potential and its plateau is the fact that immediately after t he
onset of the action potential, the permeability of the card iac muscle membrane for the potassium
ions decreases about five-fold, an effect t hat does not occu r in skeletal muscl e.
Important: The strength of card iac muscle contracti on is directly proportional to intracell ular Ca2 •
concentration.
1. The refracto ry period of atrial muscle is much shorter t han that for the ventricles (about
0.15 second for the atria compared with 0.25 to 0.30 second for the ventricles). Therefore,
the rhythmical rate of contraction of t he atria can be much faster than t hat of the ventricles.
2. Skeletal muscle cells have a short refractory period t hat allows them to be stimulated
to contract a second time before they have relaxed from an initial contraction.
Saad Alqahtani, Twitter @saaddes
heart
The bicuspid or mitral valve is located between which two chambers of the
heart?
• the right and left ventricl es
• the right atri um and the left ventricle
• the right and left atri a
• the left atrium and the left ventri cle
SAADDES
Which valve is unique in having a different number of cusps than the others?
• mitral valve
• tri cuspid va lve
• pulmonary semilunar va lve
• aortic semilunar valve
161
Irefer to AS card 167-1, 167 B-1for illustration] copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the left atrium and the left ventricle
• mitral valve
The heart consists of fou r chambers: two atria (upper chambers} and two ventricles (lower
chambers}. There is a valve through which blood passes before leaving each chamber of the
heart. The valves prevent the backward flow of blood. These valves are actual flaps t hat
are located on each end of the two ventricles (lower chambers of the heart}. They act as one
way inlets of blood on one side of a ventricle and one-way outlets of blood on the other side
of a ventricl e. The atrioventricular valves are tough, fibrous flaps of endocard ium. Both are
secured to pa pillary muscles of the ventricular walls by chordae tendineae.
• The tricuspid valve is located between the right atrium and right ventricle, surrounding
the AV orifice. The tricuspid valve is composed of three cusps that prevent a backflow of
SAADDES
blood from the right ventricl e into the right atrium during ventricular contraction.
• The mitral (bicuspid} valve is located between the left atrium and the left ventricle,
surrounding the AV orifice. The mitral valve is composed of two cusps t hat prevent a
backflow of blood from the left ventricle to the left atrium d uring ventricular contraction.
Note: These valves are open during ventricular diastole, but they are forced sh ut during
systole as the pressure in the ventricles increases, thu s preventing the flow of blood back into
the atria while the ventricles are contracting.
The pulmonary semilunar valve is located at t he entrance to t he pu lmonary trunk. It is
composed of three cusps that prevent the backflow of blood from the pulmonary artery into
the right ventricle d uring ventricular relaxation. The aortic semilunar valve is located at the
entrance to the ascending aorta. It is composed of three cusps that prevent a backflow of
blood from the aorta into the left ventricle d uring ventricular relaxation. These valves are open
during ventricular systole.
Important: At no time during the cardiac cycle are all the valves of the heart open at the same
time. The first heart sound (5 1} corresponds to closure of the AV valves; the second heart
sound (5 2} corresponds to closure of the semilunar valves.
Saad Alqahtani, Twitter @saaddes
heart
An electrocardiogram is a graphic illustration of the:
• ca rdiac cycle
• cardiac conduction system
• ca rdiac output
SAADDES
• systemic and pulmonary circuits
162
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• cardiac conduction system
An electrocardiogram (ECG or EKG) is a test that measures the electrical activity of the
heart. The signals that make the heart's muscle fibers contract come from the
sinoatrial node, which is the natural pacemaker of the heart . The principal ECG
interva ls are between the P, QRS and T waves.
Remember:
1. The P wave is the electrical recording from the body surface of atrial depolar-
ization and precedes atri al contraction.
2. The T wave of an electrocardiogram wave segment represents the repolariza-
SAADDES
tion of the ventri cles.
3. The QRS complex represents ventricular depolarization.
4. The first heart sound represents closure of the AV va lves at the onset of systole.
5. The second heart sound represents closure of the semilunar va lves at the onset
of diastole.
*** There is no d istinctly visible wave representing atrial repolarization in the
ECG because atrial repola rization occurs during ventri cula r depolarization and is
thus obscured.
1. An ECG that shows extra P waves before each QRS compl ex indicates
B partial heart block (or second-degree block).
2. An ECG that shows the P wave and the QRS complex being dissociated
is indicative of complete heart block; that is, there is no correlation between
the P wave and the QRS-T complex on the ECG.
Saad Alqahtani, Twitter @saaddes
heart
Cardiac function is the volume of blood pumped each minute, and is
expressed by which equation?
• CO = SV- HR
• CO = SV + HR
SAADDES
• CO = SVx HR
• CO = SV I HR
163
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
· CO=SVxHR
Where:
• CO is cardiac output expressed in L/min
• SV is stroke volume per beat
• HRis the number of beats per minute
Cardiac output (CO) is perhaps the single most important factor that is used in relation to the
circulation, for it is the CO that is responsible for t ransport of substances to and from the tissues.
The average resting cardiac output is about 5.6liters per minute for men and 10% to 20% less for
women. CO varies depending upon the level of body activity, age, body size, condition of the heart,
etc.
SAADDES
Heart Rate (HR) is directly proportional to cardiac output; an adult HR is normally 80-100 beats per
minute (bpm). Heart rate is an intri nsic factor of the SA (pacemaker) node in the heart and is modi-
fied by autonomic, humoral and local factors.
Stroke Volume (SV) is determined by three factors: preload, afterload and contractility.The preload
gives the volume of blood that the ventricle has available to pump, as well as the end diastolic length
of the muscle (increased preload increases stroke volume).The contractility is the force that the mus-
cle can create at the given length- increased contractility increases stroke volume. Afterload is the
arterial pressure again st which the muscle will contract (increased afterload decreases stroke vol-
ume). SV = End Diastolic Volume - End Systolic Volume
"'** The average SV is 70 to 80 ml
Important: The cardiac output of the left and right sides of the heart is equal. Blood ejected from
the left side of the heart to the systemic circulation must be oxygenated by passage through the
pulmonary circulation.
Tota l peripheral resistance (TPR) is the sum of the resistance of all peripheral vasculature in the
systemic circulation. Thus we have the equation, BP = CO x TPR. This is one of the fundamental
equations of cardiovascular physiology. You can see from the equation that blood pressure can be
maintained by altering cardiac output and/or total peripheral resistance.
Saad Alqahtani, Twitter @saaddes
heart
The Bainbridge Reflex is a positive feedback mechanism in which there is a
compensatory increase in heart rate, due to a rise in right atrial pressure.
It is commonly referred to as an Atrial Reflex.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is false
• the first statement is fa lse, the second is true
164
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
The Bainbridge Reflex is a positive feedback mechanism in w hich there is a compen-
satory increase in heart rate, due to a rise in right atrial pressure. It is commonly re-
ferred to as an Atrial Reflex.
The stretch receptors of the atria that elicit the Bainbridge Reflex t ransmit their
afferent signals throug h the vagus nerves to t he medulla of the brain. Then efferent
signals are transmitted back t hrough vaga l and sympathetic nerves to increase heart
rate and strength of heart contraction. Thus, this reflex helps prevent damming of
blood in the veins, atria, and pulmonary circu lation.
SAADDES
Remember: The baroreceptors in the internal carotid arteries and aorta are tonic-
ally active and regu late bl ood pressure on a moment-to-moment basis. An increase in
arterial pressure stretches these receptors to initiate a reflex that inhibits t he medullary
vasoconstrictor center and induces vasod ilation. Conversely, a decrease in arterial pres-
sure d isinhibits the vasoconstricto r center and induces vasoconstriction. The barore-
ceptors in the internal carotid arteries predominate over those in the aorta and t hey
respond more vigorously to changes in pressure (stretch) than they do to elevated or
reduced nonpulsatile pressure.
Note: Peripheral chemoreceptors (carotid and aortic bodies) and central chemore-
ceptors in the medulla oblongata are stimulated by a decrease in blood P0 2 and by an
increase in blood PC0 2. Stimulation of these chemoreceptors increases the rate and
depth of respiration, but it also produces peripheral vasoconstriction. Cardiopulmonary
baroreceptors are also present in t he cardiac chambers and large pulmonary vessels.
They have Jess influence on blood pressure but participate in regulation of blood vol-
ume.
Saad Alqahtani, Twitter @saaddes
heart
Use the same answer options for the following questions.
1. Your patient has a defective mitral valve, allowing backflow. Which of the
following cardiac phases will be least affected by this defect?
2. Normally, which phase would have the highest ventricular pressure?
SAADDES
• isovolumetric contraction
• fill ing phase
• isovolumetric relaxation
• ejection phase
165
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• filling phase (because the mitral valve is open through this phase normally)
• ejection phase (isovolumetric contraction would have an increasing pressure
right up until the ejection where the pressure would be the highest)
The spontaneous generation of an action potential within the SA node initiates a sequence of events
known as the cardiac cycle. Each cardiac cycle lasts approximately 0.8 seconds and spans the inter-
val from the end of one heart contraction to the end of the subsequent heart contraction.
There are two phases of the cardiac cycle.ln t he diastole phase, the heart ventricles are relaxed and
the heart fills with blood. In the systole phase, the ventricles contract and pu mp blood into the ar-
teries.
Duri ng the diastole phase, the atria and ventricles are relaxed. Blood flows into the right and left
atria. The valves located between the atria and ventricles (AV valves) are open once blood pressure
in the at ria exceeds the pressure in the ventricles, allowing blood to fl ow through to the ventricles.
SAADDES
Here is a summary of the events that occur during the diastole phase:
• Atrioventricular valves are open
• The sinoatrial node, which startscardiac conduction, contractscausing atrial contraction
• The atria empt y blood into the ventricles
• Semilunar valves close, preventing backflow into the ventricles
During the systole phase, the ventricles contract pumping blood into the arteries. The right ventri-
cle sends blood to the lungs via the pulmonary artery. The left ventricle pumps blood to the aorta.
Here is a summary of the events that occur during the systole phase:
• The ventricles contract
• Atrioventricular valves close and semilunar valves open
• Blood flows to either the pulmonary artery or aorta
1. Blood flow to the coronary arteries woul d be greatest during ventricular relaxation
in a resting individual.
2. Ventricular volume is greatest following atrial systole.
3. Ventricular pressure is greatest during ventricular ejection.
4. 1ncreased ventricular volume increases end-diastolic fiber length. This is why an
increased fi lling of the ventricle during diastole causes a more forceful heartbeat.
Saad Alqahtani, Twitter @saaddes
heart
The first heart sound ("Lub") is associated w ith the closure of the:
• aortic and m itral va lves
• m itral and tri cuspid va lves
• aortic and pulmonary valves
SAADDES
• tri cuspid and pulmonary valves
166
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• mitral and tricu spid valves
The first heart sound ("Lub") is associated with the closure of the atrioventricular
valves (mitral and tricuspid va lves) at the beginning of ventricular contraction. This
sound is largely due to vibrations of the taut A-V va lves immediately after closu re and
to the vibration of the wal ls of the heart and major vessels around the heart.
1. It is louder and longer than the second heart sound.
2. Ventricu lar systole starts with the first heart sound.
3. Ventricu lar d iastole ends with the first heart sound.
SAADDES
The second sound ("Dub") is associated w ith the closure of the semilunar valves
(aortic and pulmonary valves) as the ventricles begin to relax fol lowing thei r
contraction. This sound is due largely to vibrations of the taut, closed semilunar
va lves and to the vibration of the wal ls of the pulmonary artery, the aorta, and to
some extent, the ventri cles.
1. Diastole begins with the second heart sound.
2.The aortic valve closes before the pulmonary va lve; this causes"splitting"
of the second heart sound.
Saad Alqahtani, Twitter @saaddes
heart
You have four patients with the following heart defects. For each patient,
choose which portion of the cardiac conduction system that is most likely
malfunctioning.
1. Craig has a higher than normal heart rate (tachycardia).
2. Gary's ventricles contract nearly simultaneously with the atria.
3. Ashley's right ventricle does not contract on the lateral side.
4. Jimmy's entire left ventricle does not contract.
SAADDES
• sinoatrial node
• atrioventricula r node
• internodal pathways
• atrioventricula r bundle
• purkinje fibers
167
[refer to AS card 160-1for illustration]
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. Craig- Sinoatrial node (the pacemaker of the heart)
2. Gary- Atrioventricular node (the portion responsible for delaying impulse s as
they pass from the atria to the ventricles)
3. Ashley- Purkinje fibers (they are not transmitting impulses to the lateral side of
the right ventricle)
4. Jimmy- Atrioventricular bundle (the AV bundle is divided, and the left bundle is
not transmitting impulses). Note: Technically he could have a problem with all Pur-
kinje fibers on the left side of his heart, but the most likely problem would be at the
source of the split (the AV bundle).
The cardiac conduction system arises from the fact that cardiac myocytes are electrically
coupled to one another via gap j unctions.
SAADDES
• SA node (pacemaker): located within the superior lateral wall of the right atrium near the
opening of the superior vena cava. Specialized pacemaker cells depolarize at an intrinsic
rate that drives the depolarization of the remainder of the heart.
• Internodal pathways: rapidly transmit the wave of depolarization to the left atrium and
to the AV node.
• Atrioventricular node (AV node): located in t he posterior wall of the right atrium behind
t he tricuspid valve within the lower right interatrial septum. An impulse is delayed in the AV
node for about 0.13 seconds to allow the atrial blood to empty into t he ventricles before
ventricular contraction occurs. Aside from the AV node, t he atria and ventricles are elec-
trically isolated.
• AV bundle (bundle of Hi s): originates in the AV node, passes su bendocardially down
the right side of t he interventricular septum fo r about 1 em and t hen d ivides into t he
right and left b undle branches.
• Purkinje fibers: originate from t he right and left bundle branches, extending to t he
papillary muscles and lateral walls of the ventricles. The wave of depolarization travels
extremely fast t hrough t he bundle branches and purkinje fibers (total elapsed time of 0.03
seconds).
Saad Alqahtani, Twitter @saaddes
heart
Use the same answer options for the following questions.
1. The ventricles are completely depolarized during which isoelectric
portion of the ECG?
2. This portion of the ECG represents atrial depolarization.
3. This portion of the ECG represents the segment between depolarization of
the atria and depolarization of the ventricle.
• QRS complex
• Q-T interval
SAADDES
• S-T segment
• P wave
• P-R interval
168
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• S-T segment
• P wave
• P- R interval
The ECG, wh ich is recorded from the surface oft he body, traces the conduction of the
cardiac impulse throughout the heart. The ECG may be used to detect and analyze
certain card iac arrhythmias, such as altered sinoatrial rhythms, AV conduction blocks,
premature depolarizations, ectopic tachyca rdias and atrial and ventricu lar fibrill ation.
The Normal Electrocardiogram (ECG) Is Compo sed of:
• P wave: represents atrial depolarization prior to the atria's contraction
SAADDES
• T wave: represents ventricular repolarization
• QRS complex: represents ventricular depolarization
• S-T segment: represents the period when the ventri cles are depolarized; is iso-
electric
• P-R interval: represents the length of time between depolarization of the atria
and depolarization of the ventricles (approximately 0.16 seconds) Note: Varies w ith
heart rate; when HR increases, the P-R interva l decreases.
• Q-T interval: represents the period between ventricu lar depolarization and
ventri cular repolarization (approximately 0.35 seconds)
Note: The ECG is also isoelectric between the T and P waves (the ventricle is at resting
membrane potential). This peri od of ventricular diastole, when the ventricle is fi lling
with blood, greatly diminishes at high heart rates.
Saad Alqahtani, Twitter @saaddes
CARDIAC CYCLE. NORMAL LIMITS OF WAVES AND INTERVALS
P wave- 80ms
P-Q interval - 120 to 200ms
P-R segment- 50 to 120ms
SAADDES
QRS complex- 80 to 120ms
ST segment - 80 to 120ms
T wave - 160ms
ST interval - 320ms
QT interval - 300 to 430ms
168· 1
Saad Alqahtani, Twitter @saaddes
heart
Venous return (VR) is the flow of blood back to the heart. Under steady-state
conditions, venous return must equal when averaged over time
because the cardiovascular system is essentially a closed loop.
• sv
SAADDES
·CO
• HR
• BP
169
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• CO (cardiac output)
**"*Otherwise, blood would accumulate in either the systemic or pulmonary ci rculations. Although
ca rdiac output and venous return are interdependent, each can be independent ly regulated.
The circulatory system is made up of two circulations [pulmonary and systemic) situated in series be-
t ween the right ventricle (RV) and left ventricle (LV). Balance is achieved, in large part, by the Frank-
Starling relationship. For example, if systemic venous return is suddenly increased [e.g., changing
from supine to upright position), right ventricular preload increases, leading to an increase in stroke
volume and pulmonary blood flow. The left ventricle experiences an increase in pulmonary venous
return, which in turn increases left ventricular preload and stroke volume by the Frank-Starling rela-
t ionship. In this way, an increase in venous return can lead to a matched increase in cardiac output.
SAADDES
l .ln ventricular contraction, preload is stretch of the fibers by blood during vent ricular fill-
ing. Afterload is the arterial pressure against which the ventricle ejects the blood. An in-
crease in myocardial fiber length, as occurs with augmented ventricular filli ng (preload)
during diastole, produces a more forceful ventricular contraction. This relationship between
fiber length and strength of contraction is known as the Frank-Starling relationship or
Starling's law of the heart.
2. Preload value is related to right atrial pressure. The most important determining factor
for preload is venous return.
3. Afterload for the left ventricle is determined by aortic pressure; afterload for the right
ventricle is determined by pulmonary artery pressure.
4. Contractility is an expression of cardiac performa nce at a given preload and afterload.
Contractility can be modulated by the autonomic nervous system.
S. lncreases in heart rate will also increase cardiac output, EXCEPT at very high heart rates
where there will be less ti me for filling.
6. Sympathetic activation of the heart will increase heart rate, conduction velocity in the
heart and contractility of the card iac muscle.
7. The myocardium functions only aerobically and in general, it uses substrates in
proportion to their arterial concentration.
Saad Alqahtani, Twitter @saaddes
heart
Which of the following equations correctly defines blood flow through the
vasculature?
· flow = (in itial pressure - fina l pressure) x resistance
• flow = (init ial p ressu re - final pressure ) I resistance
SAADDES
• flow = resistance I (initial pressure - fina l pressure)
170
copynght 0 2013·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• flow= (initial pressure- final pressure) I resistance
Blood flow is directly proportional to the pressure difference between the two ends of
the vessel (the pressure gradient) and is inversely proportional to the resistance of the
vessel.
This relationship indicates that:
1) t he greater the pressure gradient, the greater t he flow rate; and
2) the flow rate decreases with increased resistance
Factors influencing resistance are expressed as:
Resistance = viscosity (of bl ood) x length (of vessel)
SAADDES
(radius)•
Important: The larger the vessel, the less the resistance.
Note: It is the fourth power of the radius. This means that if the radius is doubled
the resistance will decrease by a factor of 16. Thus, the major physiological
regulation of blood flow is via the activation of vascu lar smooth muscl e (vasocon-
striction). This fact explains why arterioles, w ith their ability to quickly constri ct o r
dilate, are the most critical factor in controlling blood flow to peri pheral t issues.
Regulators of vascu lar smooth muscle include the sympathetic nervous system,
ci rcu lating hormones and local factors.
Pressure is the d ri ving force of the blood flow. When blood vessels are connected,
the b lood flows from the higher pressure site to the lower p ressure site and the
rate of flow is proportional to the pressure difference. The overall pressure
difference is between the ascending aorta and the entrance to the ri ght atrium
(the circulatory pressure [about 100 mmHg]).
Saad Alqahtani, Twitter @saaddes
heart
Changes in vessel _ _ are most important quantitatively for regulating
blood flow within an organ, as well as for regulating arterial pressure.
· thickness
•length
SAADDES
• diameter
• viscosity
171
copyngh t 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• diameter
Resistance to blood flow within a vascu lar network is determined by the size of individ-
ual vessels (length and diameter), the organization of the vascular network (series and
parallel arrangements), physical cha racteristics ofthe blood (viscosity, laminar flow ver-
sus turbu lent flow) and extravascular mechanical forces acting upon the vasculature.
Changes in vessel diameter, particularly in small arteries and arterioles, enable or-
gans to adjust their own blood flow to meet the metabolic requirements of the t issue.
Therefore, if an organ needs to adjust its blood flow (and therefore, oxygen delivery),
cel ls surrounding these blood vessels release vasoactive substances that can either
SAADDES
constrict or dilate the resistance vessels.
The ability of an organ to regulate its own blood flow is termed local regulation of
blood flow and is mediated by vasoconstri ctor and vasodilator substances released
by the tissue surrounding blood vessels (vasoactive metabolites) and by the vascula r
endothelium. There is also a mechanism intrinsic to the vascular smooth muscle (myo-
genic mechanism) that is involved in local blood flow regulation.
In organs such as the heart and skeletal muscle, mechanical activity (contraction and
relaxation) produces compressive forces that can effectively decrease vessel d iameters
and increase resistance to flow during muscle contraction.
Important: C0 2, N02, W, K•, lactate and adenosine are metabolites that cause local va-
sodilation. Hormones regulating local blood flow include histamine and bradykinin
(cause arteri olar d ilation and venous constriction), serotonin (causes arteri olar con-
stri ction) and prostaglandins (cause constriction or dilation depending on specific
type).
Saad Alqahtani, Twitter @saaddes
heart
Fill in the blanks so that each statement correctly describes a situation that
will increase venous return to the heart.
• the contraction of (skeletal I card iac I smooth) muscle
• a(n) (increase I decrease) in intrathoracic pressure
SAADDES
• the presence of venous (valves I peristalsis)
• a(n) _ _ _ _ _ _ (increase I decrease) in venous compliance
172
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• skeletal
• decrease
• valves
• decrease
Venous return is influenced by several factors.
• Muscle contraction. Rhythmical contraction of limb muscles as occurs during normal
locomotory activity (walking, running, swimming) promotes venous return by the muscle
pump mechanism.
• Decreased venous compliance. Sympathetic activation of veins decreases venous
compliance, increases central venous pressure and promotes venous return indirectly by
augmenting cardiac output t hrough t he Frank-Starling relationship, which increases the
SAADDES
total blood flow through t he circulatory system.
• Respiratory activity. During respiratory inspiration, the venous return increases because
of a decrease in right atrial pressure.
• Vena cava compression. An increase in the resistance of t he vena cava decreases venous
return.
Remember: Under normal circumstances, the rate of venous return is the major factor that
determines cardiac output as stated in Starling's law of the heart (or the Frank-Starling
relationship).
1. Contraction of the skeletal muscles, especially in the limbs, squeezes the veins
8 and t his pushes blood in the extremities towards the heart; back flow is prevented
by the presence of numerous one-way valves in t he vein s. Thus, rhythmic
contractions of the leg muscl es will counteract t he force of gravity, which tends to
cause pooling of blood in the feet in standing persons.
2. Veins have a great degree of compliance t hat can be regulated by the
sympathetic nervous system. An increase in sympathetic activation decreases
venous compliance and increases venous return .
Important: An increase in intrathoracic pressure will decrease venous return.
Saad Alqahtani, Twitter @saaddes
heart
Which ofthe following parameters is decreased during exercise?
• heart rate
• cardiac output
• total peripheral resistance
• stroke volume
SAADDES
• arteria l pressure
173
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• total peripheral resistance
*** This is caused by t he accumulation of vasodilator metabolites (e.g., lactate,
potassium ions and adenosine). These metabolites accumulate because of an
increasing metabolic rate w ithin the exercising muscle. This arterial vasodilation
accounts for the overall decrease in TPR.
Three major effects are essential for t he circulatory system to supply t he
t remendous blood flow to the muscl es during exercise:
1. Mass discharge of the sympathetic nervous system t hroughout t he body w ith
consequent stimulative effects on the circu lation.
2. Increase in card iac output.
SAADDES
3. Increase in arterial pressure.
During exercise, t he d ilation of blood vessels in active skeletal muscles g reatly
increases blood flow to t he muscl es. At the same time, sympathetic vasoconstrictor
activity causes a compensatory constri ction of vessels elsewhere in t he body. There
is also an increase in the activity of the sympathetic nerves to the heart and a
decrease in the activity of t he parasympathetic nerves.
In addition, venous return is enhanced by the increased pumping effects of the
contracting skeletal muscles and by the sympathetic vasoconstrictor effects. As a
result, both heart rate and stroke volume increase, causing an increase in cardiac
output.
During exercise, the increase in ca rdiac output is somewhat greater than the
decrease in total peri pheral resistance. Therefore, the mean arterial pressure rises.
Important: An anxious dental patient may have a higher systolic blood pressure than
previously noted; th is is most likely due to decreased arterial compliance.
Saad Alqahtani, Twitter @saaddes
heart
Parasympathetic fibers innervate the heart by way of the vagus nerves.
The right vagus nerve goes to the AV node while the left vagus nerve goes to
the SA node.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is false
• the first statement is fa lse, the second is true
174
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is true, the second is fal se
Heart rate is controlled primarily by the autonomic nervous system. Sympathetic
(norepinephrine) stimulation causes an increase in heart rate and parasympathetic
(acetylcholine) stimulation causes a decrease in heart rate. The main centers for
autonomi c cardiac control are located in the medulla oblongata of the brain stem.
Sympathetic cardiac effects:
1. An increase in the rate of discharge of the sinoatrial node (S -A node).
2. An increase in the rate at wh ich the depolarization spreads throughout the heart.
The heart then contracts more uniformly, which increases its pu mping effectiveness.
3. An increase in ICF (intracellul ar fl uid) calcium, wh ich increases the force of
SAADDES
ventricu lar contractions.
Parasympathetic fibers innervate the heart by way of the vagus nerves. The right
vagu s nerve goes to the SA node while the left vagus nerve goes to the AV node.
Parasympathetic activation decreases heart rate and de creases the spread of
depolarization from the atria to the ventricles.
l .The SA node serves as the cardiac pacemaker to initiate the cardiac impulse.
This impu lse is propagated from the SA node to the atria and ultim ately reaches
the AV node. After a delay in the AV node, the cardiac impul se is propagated
throughout the ventricles.
2. Velocity of conduction: highest in Purkinje system; slowest in AV node.
3. The properties of automaticity (the ability to init iate its own beat) and rhyth-
micity (the regularity of pacemaker activity) allow a perfused heart to beat even
when it is comp letely removed from the body.
4. Automaticity: greater in SA node than in AV node which is greater than in
Purkinje system.
Saad Alqahtani, Twitter @saaddes
heart
If a patient's SA and AV nodes fail, what is the most likely situation the patient
will be in?
• dead; the patient's heart wil l fail immediately
• both the atria and ventricl es wi ll continue to contract on the pace of the bundle
of His (30-40 impulses per m inute)
period
SAADDES
• the ventricles w ill contract and passively fill, keeping the patient alive for a short
• the atri a will ta ke over and contract; the ventricles will allow the blood to flow
through and out to the periphery of t he body
175
[refer to AS card 160-1for illustration] copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both the atria and ventricles will continue to contract on the
pace of the bundle of His (30-40 impulses per minute)
The bundle of His (AV bundle) is located in the proxim al intraventricular septum. The bun-
d le of His em erges from the AV node to begin the conduction of the impulse from the AV
node to the ventricles.
The AV node together w ith the b undle of His make up the AV nodal tissue. The AV nodal
tissue is considered supraventricular (above the ventricles). The AV nodal tissue has an in-
trinsic rate of 40-60 beats per minute. If the SA node is injured, AV nodal tissue can take
over control of heart rate and rhythm.
The bundle of His (AV b undle) passes subendocardially down the right side of the interven-
SAADDES
tricular septum for about 1 em and then divides into the right and left bundle branches.
The right bundle branch, a direct continuation of the b undle of His, proceeds down the
right side of the interventricular septum. The left bundle branch, wh ich is considerably
thicker than the right, arises almost perpendicular from the bundle of His and perforates the
interventricular septum. On the subendocardial surface of the left side of the interventric-
ular septum, the left bundle branch splits into a thin anterior division and thick posterior
division.
The right bundle branch and the t wo divisions of the left bundle branch ultim ately subdi-
vide into a co mp lex network of conducting fibers, called Purkinje fibers that spread out
over the subendocardial surfaces of both ventricles. Collectively, the bundle branches and
Purkinje network comprise the ventricular conduction system. Note: It takes about 0.03-
0.04 seconds for the impulse to travel fro m the bundle of His to the ventricular m uscle.
Remember: The ventricular conducting system is capable of intrinsic pacem aker activity at
a rate of 30-40 impulses per minute. If the SA and AV nodes are injured, the ventricular
conducting system can take over control of heart rate and rhythm.
Saad Alqahtani, Twitter @saaddes
pH
The isoelectric point (pi):
• is the pH at which the number of positive and negative charges on a molecule equal
each other
• is the pH at wh ich the number of positive and negative charges in a solution equal
each other
SAADDES
• can be determined using the Henderson-Hasselbalch equation
• is the pKa of a solution at wh ich it is neither basic nor acidic
• two of the above
176
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• is the pH at which the number of positive and negative
charges on a molecule equal each other
Another way of stating it is: the isoelectric point (also cal led the isoelectric pH) is
the pH at which a solute has no net electric charge and thus does not move in an
electric field. It is designated pi for that solute.
This information has practical importance - for a solution containing a mixture
of amino acids, the d ifferent amino acids can be separated on the basis of the
direction and relative rate of their migration when placed in an electric field at a
known pH. The same applies to protein molecules and is frequently used to separate
proteins.
SAADDES
Note: Whereas the pK (the negative logarithm of the dissociation constant of an acid)
is the property of an individual ionizable group, the pi is a property of the whole mol-
ecule.
Example:
The amino acid g lycine has a net negative charge at any pH above glycine's pi and
wi ll thus move toward the positive electrode (the anode) when placed in an electric
field. At any pH below g lycine's pi, g lycine has a net positive charge and will move
toward the negative electrode (the cathode). The farther the pH of a glycine solution
is from its isoelectric point (pi), the greater the net electric charge of the population
of glycine molecules.
Note: At physiologic pH, all amino acids have both a negatively cha rged carboxyl
group (-Coo·) and a positively cha rged amino group (-NH 3+). They are therefore,
dipolar ions (in this state, the compound is said to be a zwitterion).
Saad Alqahtani, Twitter @saaddes
Amino acid pKa 1 pi
Table of pKa and pi values
Glycine 2.34 5.97
• The pKa values and the isoelectric
point (pi), are given for the 20 a-amino Alanine 2.34 6.00
acids. Valine 2.32 5.96
• pKa 1= a-carboxyl group Leucine 2.36 5.98
Isoleucine 2.36 6.02
Methionine 2.28 5.74
Proline 1.99 6.30
SAADDES
Phenylalanine 1.83 5.48
Tryptophan 2.83 5.89
Asparagine 2.02 5.41
Gluta mine 2.17 5.65
Serine 2.21 5.68
Threonine 2.09 5.60
Tyrosine 2.20 5.66
Cysteine 1.96 5.07
Aspartic acid 1.88 2.77
Glutamic acid 2.19 3.22
Lysine 2.18 9.74
Arginine 2.17 10.76 176-1
Histidine 1.82 7.59
Saad Alqahtani, Twitter @saaddes
pH
Which of the following represents the pH of a solution that has a 10-4 M
concentration of OH- ion?
•5
SAADDES
·8
·7
·10
177
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
· 10
This type of problem is solved by using the following equation:
=
Kw [H+) [OH -)
• Kw is the ion product of water and always equals 10"14
• [H+) is the hydrogen ion concentration (pH= -log (H+))
• [OH-) is the hydroxide ion concentration (pOH = -log [OH- ))
Therefore, by taking the negative log of both sides, the equation can be rewritten as
SAADDES
follows:
14 = pH+ pOH
Solving the problem on the front of the card - 14 = pH+ 4
pH = 10
Saad Alqahtani, Twitter @saaddes
pH
Carbonic acid/bicarbonate is the most important physiological buffer
system in the body.
Proteins also participate in pH buffering, mainly through their histidine side
chains.
• both statements are t rue
SAADDES
• both statements are false
• t he fi rst statement is true, t he second is false
• t he fi rst statement is fa lse, the second is t rue
178
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Most biomolecules contain weakly ionizabl e groups that are subject to protonation and
deprotonation. Conseq uently, all biological processes depend on t he pH value of the
environment. The maintenance of an optimal pH is t herefore essential for survival and optimal
function.
The pH of plasma is approximately 7.40 in arterial blood and 6.35 in venous blood. This
d ifference is caused by the higher concent ration of carbonic acid in venous blood. Carbonic
acid is formed spontaneously from carbon d ioxide and water, but the react ion is accelerated
d ramatically by the enzyme carbonic anhydrase in erythrocytes.
Carbonic acid/ bicarbonate is the most important physiological buffer system in the body. It
SAADDES
is important because C0 2 and HC0 3·are present in high concentrations in the body, not only in
the plasma but also in the interstitial and int racellular compartments. Also, the C0 2 level can
be regulated by the lungs and t he HC0 3·1evel by the kidneys.
Phosphate groups provide an additional buffer system: Only H2P04 '· is present in appreciable
q uantities at physiological pH values. The ph osphate buffer is important only in t he intracellu-
lar compartments, in which phosphate is the major inorganic anion.
Proteins also participate in pH buffering, mainly through their histidine side chains: Serumal-
bumin for example, has 16 histid ine residues with pK values not far from t he blood pH of 7.4. Like
phosphate, protein s are more important buffer systems in t he cells than in the plasma.
Remember: Buffer systems most common ly consist of a weak acid (the proton donor) and a
"salt'; or conjugate base of that acid (the proton acceptor}. These systems minimize pH
changes brought about by a change in the acid or base content of the solution. These buffer
systems reduce the effect of an abrupt change in W ion concentration by releasing W ions
when t he pH rises and accepting Wions when the pH drops.
Note: Hemoglobin is a major intracellular buffer.
Saad Alqahtani, Twitter @saaddes
pH
The famous relationship stated in the Henderson-Hasselbalch equation can
be used to:
• predict the pH that acid buffers work best at
• predict the pKa that acid buffers work best at
SAADDES
• predict the d issociation constant of a weak acid only
• predict the d issociation constant of a strong acid only
• predict the d issociation constant of any acid
179
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• predict the pH that acid buffers work best at
*..,. The relationship cannot predict any dissociation constants
Buffers must be chosen for the appropriate pH range that they are called on to control. The pH range
of a buffered solution is given by the Henderson-Hasselbalch equation. Th is equation describes the
relationship bet ween the pH, pK (the negative log of the dissociation constant) and the
concentrations of an acid and its conjugate base. The equation is simply a useful way of restating
t he expression for t he dissociation constant of an acid (Kal-
The dissociation constant of an acid (Kalis:
[H+) [A-)
Ka = - - -
SAADDES
[HA)
Note: The larger the Ka, the stronger the acid because most of the HA has been converted into W
and A'. Conversely, the smaller the Ka, the less acid has dissociated and therefore, the weaker the
acid.
The Henderson-Hasselbalch Equation was derived from the equation for the dissociation
constant:
[A·]
pH = pK. + log - -
[HAl
1. The Henderson-Hasselbalch equation shows that pH=pK when an acid is half neutral-
Not.. ized.
2. The pH of a buffer system depends on the pK of the weak acid and the ratio of molar
concentrations of salt and weak acid .
3. The optimum pH for an enzyme is the pH that facilitates the most rapid reaction rate.
4. A buffer is most effective when the pH of the solution equals the buffer's pKa, though it
still works well within 1 pH unit of its pKa.
Saad Alqahtani, Twitter @saaddes
pH
All of the following are mechanisms the body uses to control the blood's
acid-base balance EXCEPT one. Which one is the EXCEPTION?
• excess acid is excreted by the kidneys
• pH buffers are found in the blood
SAADDES
• excretion of carbon dioxide
• filtering blood by the spleen
180
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• filtering blood by the spleen
The body employs regulatory systems that are designed to restore the normal blood
pH. There are three lines of defense against acidosis and alkalosis:
1. The buffer systems act immediately to prevent excessive fluctuations of the
blood pH.
2. Al veolar ventilation increases in acidosis and decreases in alkalosis. The respira-
tory center in the medulla oblongata of the brain responds d irectly to pH and C0 2.
This mechanism works on a time scale of m inutes.
3. The kidneys excret e excess W in acidosis and excess HC03· in alka losis. This is a
SAADDES
long term mechanism that acts on a time scale of hours to days.
Note: From the Henderson-Hasselbalch relationship, we can see how plasma pH is
determined by the plasma levels of ca rbon dioxide and bicarbonate. The pK. of the
bicarbonate-carbon dioxide buffer system is 6.1.
pH = 6.1 +log [bicarbonate] I (0.03 X partial pressure of carbon dioxide)
*** The 0.03 multipl ier is the solubili ty constant of C0 2 in blood. The multiplier
converts the PC0 2 measurement to C0 2 concentration in mmoi/ L. This is necessary
to ensure that both the HCo3· and C0 2 concentration have the same units.
Saad Alqahtani, Twitter @saaddes
pH
Respiratory acidosis results from hyperventilation.
Metabolic acidosis results from excessive vomiting.
• both statements are t rue
SAADDES
• both statements are fa lse
• the first statement is t rue, the second is fa lse
• the first statement is fa lse, the second is true
181
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are false
Even small deviations from the normal blood pH lead to severe cl inical disturbances.
An arteri al pH lower than 7.35 is called acidemia and an arteria l pH exceeding 7.45 is
ca lled alkalemia. The pathological states leading to these outcomes are ca lled
acidosis and alkalosis, respectively.
Respiratory acidosis is caused by any impairment in t he d isposal of C02 . Conversely,
respiratory alkalosis results from hyperventilation. For example, a doubling in the
rate of alveolar ventilation raises the blood pH from 7.40 to 7.62. A 50% reduction in
alveolar ventilation lowers t he blood pH from 7.40 to 7.12. Note: If you administer a
SAADDES
high nitrous-oxygen mixture (for example, 90:10) to a patient, th is will cause respiratory
depression and result in respiratory acidosis.
Metabolic acidosis is caused either by an overproduction of o rganic acids or by an in-
ability of t he kidneys to excrete excess acid. The normal urinary pH va ri es over a range
of 4.0 to 7.0, depending on the need to excrete excess protons. Conversely, metabolic
alkalosis is caused by the abnormal loss of acids from t he body: for exampl e, as a re-
sult of excessive vomiting.
The most important laboratory test for t he distinction between metabolic and respira-
tory acidosis is t he determination of the tota l plasma carbon dioxide (C0 2 + H2C0 3 +
HC03lln respiratory acidosis, the total carbon dioxide is elevated because C0 2 reten-
tion is by definition, the cause of the acidosis; in metabolic acidosis, it is reduced be-
cause the patient hyperventilates in an attempt to eliminate excess ca rbonic acid. The
converse applies to alkalosis.
Saad Alqahtani, Twitter @saaddes
membranes
The cell (plasma) membrane is a fluid mosaic of:
• lipids and carbohydrates
• proteins and carbohydrates
• lipids and proteins
SAADDES
• carbohyd rates
182
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• lipids and proteins
The cell membrane (plasma membrane) is composed mainly of lipids and proteins.
The lipids form a bilayer, t heir hydrophilic head groups interact w ith water on both
intracellular and extracellular surfaces while the hydrophobic fatty acyl chains of the
lipids interact with in t he central portion of t he membrane. Peripheral proteins do
not cross the length of the membrane and are either embedded within the outer or
inner layer of the membrane; integral proteins span from one side of the membrane
to the other side.
1. Carbohydrates are attached to proteins and lipids on the exterior side of
the cell membrane.
SAADDES
2. Integral proteins are associated w ith the hydrophobic phase of the
bilayer.
Important point: The membrane is said to be a "fluid-mosaic" since lipids and
proteins can diffuse laterally w ithin the plane of the membrane. However, peri pheral
proteins seldom flip from the outer to the inner membrane or vice versa.
The lipids that make up the bulk of a cell's surface membrane fall into three classes:
phospholipids, steroids (primarily cholesterol) and g lycolipids. About half of the
molecules in an average membrane are phospholipids. Examples of phospholipids
include: phosphatidylethanolamine, phosphatidylserine and phosphatidylinositol.
Examples of glycolipids includes phosphatidylcholine and sphingomyelin.
Phospholipids are amphiphilic with the hydrocarbon ta il of t he molecule
hydrophobic and its polar head hydrophilic. As the plasma membrane faces watery
solutions on both sides, its phospholipids accommodate this by form ing a
phospholipid bilayer with t he hydrophobic tails facing each other.
Saad Alqahtani, Twitter @saaddes
membranes
Proteins account for about one quarter of the total mass in most membranes.
Membrane proteins are globular proteins.
• both statements are true
SAADDES
• both statements are false
• the first statement is t rue, the second is false
• the first statement is fa lse, the second is true
183
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is fal se, the second is true
Proteins account for about one half of the total mass in most membranes. Membrane p ro-
teins are globular proteins. Accord ing to the fluid -m osaic model of membrane structure,
they associate with the lipid b il ayer in different ways:
• Integral membrane proteins: are embedded in the lipid b ilayer. In most cases, the
polypept ide traverses the lipid b il ayer by means of a transmembrane helix. The nonpo-
lar side chains of these amino acids interact w ith the membrane lipids.
Note: Integral membrane proteins can be solu bilized only w ith treatments that destroy
the lipid b ilayer (action of detergents).
• Peripheral membrane proteins: interact with integral membrane proteins or the hy-
SAADDES
drophilic head groups of the memb rane lipids, but they do not t raverse the lipid b ilayer.
Note: They can be detached from the membrane by manipu lating pH or salt concentra-
tions.
Six Common Features of Biological Membranes:
1. Sheetlike structures, only a few molecul es thick (60 to 100 At hick).
2. Consist mainly of lip ids and proteins (carbohydrates are attached to exterior).
3. The membrane lipids are small molecules w ith hydrophobic and hydrophilic groups
that form lip id bilayers in aqueous media. The hydrophobic center of the bilayer forms
a barrier to t he flow of polar molecul es across the membrane.
4. The proteins function as transporters, enzymes, receptors, and mediators.
S.They are non covalent assemblies. The protein and lipid molecules are held together
by many noncovalent interactions.
6. Their lipi d distribution in t he membrane is asymmetrical, meaning they contain
most of their phospholipids (phosphatidylethanolamine, p hosphatidylserine and
phosphatidylinositol) in the cytoplasmic (inner) leaflet and most of their glycolipids
(phosphatidylcholine and sphingomyelin) in the exoplasmic (outer) leaflet.
Saad Alqahtani, Twitter @saaddes
membranes
What is the name of the structure shown below?
Hint: It is the basic structure of cell membranes.
SAADDES
184
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• lipid bilayer
In an aqueous environment (water), phospholipid molecules form lipid bilayers (also called
bimolecular sheets), in which t he polar regions (phosphate group that is negatively charged)
are located at the surfaces of the bilayer, where the molecules interact with water (hydrophilic).
The nonpolar regions (fatty acid portion) are hydrophobic and orient themselves toward the
interior of the bilayer so as to minimize contact with t he aqueous portion. In this lipid bilayer,
globular proteins (peripheral and integral) are embedded at irregular intervals, held by
hydrophobic interactions between the membrane lipids and hydrophobic domains in the
proteins.
1. lipids, when suspended in water, spontaneously form bilayer structures that are
SAADDES
stabilized by hydrophobic interactions.
2.This lipid bilayer serves as a permeability barrier, yet it is quite fluid. The membrane
mosaic is fluid because the interactions among lipids and between lipids and proteins,
are noncovalent, leaving individual lipid and protein molecules free to move laterally
in the plane of the membrane.
3. Bilayers arise through the operation of two opposing forces: (1) attractive forces
between hydrocarbon chains (van der Waals forces) caused by the hydrophobic effect
forcing such chains together and (2) repulsive forces between the polar head groups.
4. The lipid bilayer is impermeable to small inorganic ions such as sodium and protons.
5. All noncovalent structures are fragile. Biological membranes are especially vulner-
able to agents that disrupt hydrophobic interactions. Exposed membranes tolerate
neither nonpolar organic solvents nor detergents. Many disinfectants, including phen-
ol, ethanol and cationic detergents, act by disrupting the membranes of microorgan-
isms.
6. Gases such as oxygen and carbon dioxide diffuse freely across membranes, but most
nutrients, metabolic intermediates and coenzymes are water soluble and can-not
cross the lipid bilayer. Also because inorganic ions cannot cross, the electrical conduct-
ivity of lipid bilayers is very low.
Saad Alqahtani, Twitter @saaddes
membranes
Molecules that can easily penetrate a biologic membrane are usually:
• large and nonpolar
• small and polar
• large and polar
SAADDES
• small and nonpolar
185
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• small and nonpolar
The most important property of the lipid bilayer is that it is a highly impermeable structure.
Impermeable simply means that it does not allow molecules to freely pass across it. On ly water
and gases (for example 0 2, C0 2) can easily pass through the bilayer. This property means that
large molecules and small polar molecules cannot cross the bilayer and thus the cell
membrane, without the assistance of other structures. To penetrate a lipid bilayer, a substance
has to pass from the aqueous solution through the region of the hydrophilic head groups, then
across the hydrophobic core and out between the head groups on the opposite side.
In most membranes, passive diffusion is limited to lipid-soluble molecules. Water soluble
molecules require carrier-mediated transport. Membrane carriers are integral membrane
proteins that form a gated channel across the lipid bilayer. Unlike a simple pore, the gated
SAADDES
channel has a specific binding site for the transported molecule. The channel undergoes con-
formational changes that allow the substrate to bind on one side and dissociate on the oppo-
site sid e of the membrane. Note: Some types of carrier-mediated transport are passive and
others are driven by the hydrolysis of ATP, either directly or indirectly.
Facilitated diffusion is a type of carrier-mediated transport in which an external energy source
is not used. Therefore, the net transport of the substrate is always down its electrochemical gra-
dient. For example, the glucose carrier in the erythrocyte membrane is a gated channel with a
binding site for glucose. Note: Most cell s in the human body take up g lucose by thi s cost-effi-
cient mechanism. The transport of a single substrate by a membrane carrier, as in the facilitated
diffusion of glucose, is called uniport.
Another important property of the lipid bilayer is its fluidity. The lipid bilayer contains lipid
molecules. The bi layers' fluidity allows these structures mobility within the lipid bilayer. This
fluidity is biologically important, influencing membrane transport. Fluidity is dependent on
both the specific structure of the fatty acid chains, the presence of cholesterol and
temperature (fluidity decreases with lower temperature and in creases w ith increased
temperature).
Saad Alqahtani, Twitter @saaddes
tooth/mouth
The organic matrix of enamel is made from noncollagenous proteins only
and contains several enamel proteins and enzymes.
Of the enamel proteins, 90% are a heterogenous group of low-molecular-
weight proteins known as amelogenins.
• both statements are true
SAADDES
• both statements are false
• the fi rst statement is true, the second is false
• the fi rst statement is fa lse, the second is true
186
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
The organic matrix of enamel is made from noncollagenous proteins only and conta ins several
enamel proteins and enzymes. Of the ena mel proteins, 90% are a heterogenous group of low-
molecu lar-weight proteins known as amelogenins. The remaining 10% cons ist s of
nona melogen ins such as enamelin and ameloblast.in.
• Amelogenins: are hydrophobic proteins rich in proline, histidine and glutamine. Represent t he
main protein present in form ing enamel; expression stops w hen enamel reaches full thickness.
Loss of function: A thin hypoplastic enamel layer is formed that lacks enamel rods.
• Ameloblast.in: this protei n is present in much smaller amounts compared with amelogenin; it
is found mostly in newly formed (secretory stage) ena mel and more so at the outer surface t han
in deeper areas closest to t he DEJ. Loss of function: terminal d ifferent iating ameloblasts detach
from the dentin and enamel formation aborts.
SAADDES
• Enamelin: this protein is the largest and the least abundant of the enamel matrix proteins; is
present only at t he growing enamel surface. Loss of function: not known .
Ameloblasts produce an enamel matrix (organic matrix) w ith protein components called
amelogenins and enamel ins. Th is organ ic matrix makes up about 1% to 2% of enamel and water
makes up about 4%.
Enamel is a highly mineralized structure conta ining approximately 95% inorganic matter. The
hydroxyapatite crystals, which are made up of calciu m and phosphate, are the largest mineral
constituents (90% to 95%) of this inorganic matter.
Note: Enamel is semipermeable; it is this property of enamel that allows fluoride ions to be
absorbed on the hydroxyapat ite crystals, forming fluorapatite via fluoride ion displacement of a
hydroxyl group. The tooth becomes more resistant to bacteria-producing acids because
fluorapatite has a lower solubility product constant than hydroxyapatite (another way of saying
t his is hydroxyapatite has a higher solubility than fluorapatite).
Remember: Enamel is harder tha n bone. The main reason for this is that enamel hydroxyapatite
crystals are larger and more firmly packed. These tightly packed masses of hydroxyapatite crystals
are keyhole-shaped rods called enamel prisms and form the structural found ation of enamel.
Actually, these hydroxyapatite crystals in enamel are four times larger than those in bone, dentin
and cementum.
Saad Alqahtani, Twitter @saaddes
tooth/mouth
All of the following statements concerning enamel hypoplasia are true
EXCEPT one. Which one is the EXCEPTION?
• it is a defect in the m ineralization of the formed enamel matrix
• the enamel of primary and permanent teeth appear pitted
SAADDES
• rad iographically, the enamel is either absent o r very thin over tips of cusps and
interproximal areas
• it can be caused by nutritional deficiencies
187
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• it is a defect in the mineralization of the formed enamel matrix
***This is fal se; it is a defect in the formation of the enamel matrix.
Enamel hypoplasia is a general term referring to all quantitative defects of enamel
thickness. They range from single or multiple pits to small fu rrows and wide troughs to
entirely missing enamel. Note: Hypocalcification and opacities are qualitative de-
fects.
Hypoplasia results only if the assault occurs during the time the teeth are
developing. Either dentition may be involved. The teeth appear pitted, yellow to dark
brown in color, and have open contacts. Radiographically, the enamel appears to be
SAADDES
absent or very th in, especially over the cusp tips and interproximally.
The enamel is hard in context but thin and deficient in amount. The etiology may be
hereditary or environmental. Examples of environmental causes include a vitam in
deficiency (A and D), inadequate ca lcium intake, fluorosis, congenital syphilis, high
fever, injury o r trauma to the mouth.
1. Enamel hypocalcification is a defect in the mineralization of the formed
S enamel matrix.
2. Tooth erosion in bulimic patients is due to the solubility of hydroxyap-
atite in acid.
3. Enamel hypoplasia is strongly associated with amelogenesis imperfecta;
w ith the subsets being:
• Hypoplastic- pitting
• Hypo maturation -normal thickness enamel that chips/abrades
• Hypocalciflcation- normal th ickness, enamel ch ips/ abrades
Saad Alqahtani, Twitter @saaddes
tooth/mouth
Caries activity is directly proportional to all of the following EXCEPT one.
Which one is the EXCEPTION?
• the consistency of fermentable carbohydrates ingested
• the quantity of fermentable carbohydrates ingested
SAADDES
• the frequency of ingesting fermentable carbohydrates
• the o ral retention of fermentable carbohydrates ingested
188
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• th e quantity of fe rmentable carbohydrates ing este d
Dental caries has been an intractable disease in spite of intense dental research. The meta-
bolic acids p roduced by streptococci mutans demineralize the tooth surface and lead to
dental caries. The enzyme glucosyltransferase (aka, dextran sucrase) produced by strep-
tococci mutans is the key factor in this process. Oral bacterial g lucosyltransferases (GTFs) use
sucrose as a substrate in synthesis of either water-soluble or insoluble g lucans (e.g., dex-
trans, mutans, and !evans).
Remember: S. Sanguis (which is the most frequently iso lated Streptococcus in the oral
cavity), S. Salivarius and Lactobacillus species also produce g lucosyltransferase. This
SAADDES
enzyme catalyzes the formation of extracellular glucans from d ietary sucrose. Glucan
production contributes to the formation of dental plaque. Th is dental plaque holds the
lactic acid wh ich is p roduced by these Streptococci against the tooth. This acid disso lves
the hydroxyapatite crystals which form the enamel of the tooth, creating caries.
Each time that plaque bacteria come into contact with food or drink conta in ing simple
sugars (monosaccharides such as glucose and fructose, and d isaccharides such as sucrose,
lactose and maltose), the plaque bacteria use the sugars for the bacteria's metabolic
needs, making organic acids (i.e., lactic acid) a metabo lic by-product. If these acids are not
buffered by sa liva, they d issolve the surface of the a patite crystals of adjacent tooth
structure. This is called demineralization (this occurs when the pH level of the mouth
drop s be low 5.5). Caries depends on the ba lance between demineralization and
remineralization, i.e., on the frequency of eating (and on the microbial co mposition of
the p laque and its chemical nature and th ickness, on the local fl uoride concentration and
on the b uffering capacity of saliva). A frequent pattern of eating therefore increases caries
risk.
Saad Alqahtani, Twitter @saaddes
tooth/mouth
The primary physiologic control of the salivary glands is by the sympathetic
nervous system.
Control of salivary secretion is exclusively neural.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is false
• the first statement is fa lse, the second is true
189
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
The main functions of sa liva in digestion include lubrication and moistening offood for swallowing,
solubilization of material for taste, initiation of ca rbohydrate digestion and clearance and
neutralization of refluxed gastric secretions in the esophagus. Saliva also has antibacteria l actions
that are important for overall health of the oral cavity and teeth.
There are three pa irs of major salivary glands: parotid, submand ibular and sublingual. In addition,
many smaller glands are found on the tongue, lips and palate. These glands are typical tu buloalveo-
lar glands. The acinar portion of the gland is classified according to its major secretion: serous, mu-
cous or mixed. The parotid gland produces mainly serous secretion, the sublingual gland secretes
mainly mucous and the submandibular gland produces a mixed secretion.
Two Secretions:
SAADDES
1. Mucous secretion: contains mucins (glycoproteins), which are proteins that have poly-
saccharides attached to them. Lubricates the mouth and food.
2. Serous secretion: contains the enzyme salivary amylase (ptyalin). This enzyme splits starch
into alpha-dextrin, maltotriose and maltose.
Stimulation of the parasympathetic nerves to salivary glands increases blood flow by dilati ng the
vasculature of the glands. Vasoactive intestinal polypeptide (VIP) and acetylcholine are released
from parasympathetic nerve terminals in the salivary glands and are vasodilatory during secretion.
Control of salivary secretion is exclusively neural. In contrast, control of most other Gl secretions is
primarily hormonal. Salivary secretion is st imulated by both the sympathetic and parasympathetic
subd ivisions of the autonomic nervous system. The pri mary physiological control of t he salivary
glands is by the parasympathetic nervous system. Note: Sympathetic fibers to the salivary glands
stem from the superior cervical ganglion. Preganglionic parasympathetic fibers travel via branches
of the facial and glossopharyngeal nerves. These fibers form synapses with postganglionic neurons
in ganglia in or near the salivary glands.
Note: Vagal stimulation increases saliva production, so vagotomy (or at ropine) inhibits saliva
production and produces dry mouth.
..,.* Atropine prevents the action of acetylcholine on the secreting cells in the oral cavity.
Saad Alqahtani, Twitter @saaddes
tooth/mouth
All of the following characterize saliva EXCEPT one. Which one is the
EXCEPTION?
• low K+concentration
• low osmolarity
SAADDES
• the inorganic composition is entirely dependent on the stimulus and the rate of
salivary flow
• it is always hypotonic
190
copynght 0 20 13·2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• low K• concentration
The important p roperties of saliva are a large flow rate relative to the mass of gland, low
osmolarity, high K+concentration and organic constituents - including enzymes (amy-
lase, lipase), mucin and growth factors. The inorganic co mposition is entirely dependent
on the stimulus and the rate of sa livary flow, which is stimulated during a meal. The major
components are Na•, K•, Hco3·, Ca 2• , Mg 2• and cr.
Note: In humans, salivary secretion is always hypotonic due to the fact that the salivary
ductal cell s reabsorb sodium and chloride in exchange for potassium and bicarbonate.
The organic constituents of saliva, p roteins and glycoproteins, are synthesized, stored
SAADDES
and secreted by the acinar cells. The major p roducts are amylase (an enzyme that in itiates
starch digestion), lipase (important for lipid di gestion), glycoprotein (mucin, which forms
mucus when hydrated) and lysozyme (attacks bacterial cell wa ll s to limit colonization of
bacteria in the mouth).
Note: Saliva supplies calcium and p hosphate, which are important for remineralization of
the enamel.
Remember: Caries is modified by saliva. High flow-rate saliva is a very effective buffer. The
balance between demineralization and remineralization can therefore be altered
substantially by the rate of salivary flow. Flow is decreased by salivary gland pathology (as
occurs in several connective tissue disease and w hich can follow radiotherapy and cancer
chemotherapy), by many mood-altering drugs and so me drugs used in other medical
treatment, in dehydration and during sleep. Flow increases naturally during vigorous
chewing. A maximum salivary flow rate of less than 0.7 ml/min. is associated with
high caries risk.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
The nonessential amino acids are synthesized either from common
metabolic intermediates or from other amino acids.
Only three amino acids: leucine, lysine and histidine, are exclusively
ketogenic.
SAADDES
• both statements are true
• both statements are false
• the first statement is t rue, the second is false
• the first statement is fa lse, the second is true
191
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is true, the second is false
Only eleven of the 20 amino acids can be synthesized in the human body. Those that cannot
be synthesized are ca ll ed essential amino acid s. The nonessential amino acids are
synthesized either from common metabolic intermediates or from other amino acid s.
The essential amin o acid s include: valine, threonine, leucine, methionine, isoleucine, lysine,
phenylalanine, histid ine and tryptophan. The nonessential am ino acids include: alanine, as-
paragine, cysteine, g lutamine, proline, tyrosine, arginine, aspartate, glutamate, glycine and ser-
ine.
Amino acids are used for th ree major pu rposes:
• They are substrates for the generation of metabolic energy
• They are substrates for protein synthesis
SAADDES
• They are substrates for the synthesis of many products including heme, purines, pyrim-
idines, several coenzymes, melanin and t he biogenic a mines
Amino acids can also be classified as ketogenic, glucogenic, or both according to the natu re
of their metabol ic end products.
• The seven amino acid s (phenylalanine, tyrosine, isoleucine, leucine, tryptophan, th reonine
and lysine) that are degraded ent irely or in part to acetoacetyi-CoA and/or acetyi-CoA can
yield ketone bodies in the liver, where acetoacetyl-Co-A is converted to acet oacetate and
then to acetone and p-hydroxybutyrate. These are the ketogenic amino acids.
• The amino acids that are degraded t o pyruvate, a-ketog lutarat e, succinyi-CoA, fumarate,
and/or oxaloacetate can be converted to glucose and glycogen. They are the glucogenic
amino acids.
Note: The division between ketogenic and glucogenic amino acids is not sharp, five amino acids
(tryptophan, phenylalanine, tyrosine, t hreonine and isoleucine) are both ketogenic and gluco-
genic. Only leucine and lysine are purely ketogenic.
Important: The nitrog en of the amino acid s is incorporated in urea, a soluble, nontoxic prod-
uct that is excret ed in the urine.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
In eukaryotes, DNA does not exist free; it is complexed with an approximately
equal mass of basic proteins called histones. These histones contain a large
portion of:
• cysteine and lysine
SAADDES
• arginine and lysine
•lysine and glutamine
• glutamine and arginine
192
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• arginine and lysine
The nucleus contains the chromosomes of the cell. Each chromosome consists of a
single molecule of DNA complexed with an equal mass of proteins. Collectively, the
DNA of the nucleus with its associated proteins is ca lled chromatin. Most of the
protein consists of multiple copies of 5 kinds of hi stones (H l , H2A, H2B, H3 and H4).
These are basic proteins, bristling with positively charged arginine and lysine
residues. Important: Both Arg and Lys have a free amino group on thei r R group,
which attracts protons (W), giving them a positive cha rge (perfect amino acids to
bind tightly to the negatively-charged phosphate g roups of DNA).
SAADDES
Note: These histones help neutralize the large negative charge of the DNA phosphate
groups and stabilize DNA in a compact form.
Remember: Histones package and order the DNA into structural units called
nudeosomes. Nucleosomes are repeating subunits of chromatin, consisting of a DNA
cha in coiled around a core of histones.
1. Chromatin also contains small amounts of a w ide variety of nonhistone
proteins. Most of these are transcription factors (e.g., the steroid receptors)
and their association with the DNA is more transient.
2. Activation of DNA for replication or t ranscription requ ires breakup of the
nucl eosomestructure. Phosphorylation of serine and th reonine residues in
histones is part of the process for replication, w hile acetylation of lysine
residues in the histones is used for transcriptional activation.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Which one of the following statements about protein structure is correct?
• proteins consisting of one polypeptide can have quaternary structure
• the formation of a disulfide bond in a protein requires that the two participating
cysteine residues be adjacent to each other in the primary sequence of the protein
SAADDES
• the stability of quaternary structure in proteins is mainly due to covalent bonds
among the subunits
• the information required for the correct folding of a protein is contained in the
specific sequence of amino acids along the polypeptide chain
193
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• th e information required for the correct folding of a protein i s contained
in th e specific sequence of amino acids alon g th e polypeptid e chain
*** The correct folding of a protein is guided by specific interactions among the side
chains of the amino acid residues of a polypeptide chain.
Proteins are polymers b uilt from amino acids j oined by peptide bonds. The resulting chain
of amino acids (called a polypeptide) is then folded in different ways and to different
extents. Generally, amino acids have a central or alpha carbon to which is attached a
hydrogen atom (H), a carboxyl group (COOH), an amino group (NH 2) and a fourth
group that differs from one amino acid to another and is often indicated by the letter R.
App roxim ately 20 different amino acids (they possess different R groups) are common ly
found in proteins of the body.
SAADDES
Proteins are formed from amino acids by reactions that bond the alpha amino group of
one amino acid to the alpha carboxyl group of another. This bond is called a peptide
bond. Two amino acids joined together by a pept ide bond form a dipeptide. Ten or more
amino acids linked in a chain by peptide bonds form a polypeptide chain. A protein is a
polypeptide chain of approxim ately 100 or more amino acids linked by peptide bonds.
The order of amino acids in a protein from the amino terminal to the carboxy terminal of
the protein chain is referred to as the primary structure of the protein. Higher-order
structures are dependent on the prim ary structure.
1. The two cysteine residues that react to form the disulfide bond (a covalent
bond) may be a great distance apart in the primary structure but are brought
into close proximity by the three-dimensional folding of the polypeptide chain.
2. Many proteins are composed of two or more polypept ide chains, generally
referred to as subunits, which associate through non covalent interaction s and
occasionally, disulfide bonds to form protein quaternary structu res. It has been
known for long that the functions of proteins are closely related to their
quaternary structure.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Most plasma proteins are derived from the:
• kidney
•liver
• plasma cells
• T cells
SAADDES
194
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• liver
Most plasma proteins are derived from the liver.ln all, the liver synthesizes about 25 g of plasma
proteins every day, which accounts for nearly 50% of the total protein synthesis in the liver. Only
the immunoglobulins are not produced by the liver. They are synthesized by plasma cells.
Most plasma proteins (exception: albumin) are glycoproteins. They circulate for several days
and are eventually removed from the circulation when their oligosaccharide chains are worn
down.
Although albumin accounts for only 60% of the total plasma protein, it provides 80% of the col-
loid osmotic pressure of the plasma. This is because the colloid osmotic pressure depends on
the amount of water and electrolytes that a protein attracts to its surface and albumin is one of
the most hydrophilic plasma proteins. Remember: The colloid osmotic pressure is necessary
SAADDES
to prevent edema. Usually, edema develops when the albumin concentration drops below 2.0
g/dl. Edema can also be caused by an increase in capillary permeability, venous obstruction, im-
paired lymph flow and CHF with an increased venous pressure.
Globulins (are soluble in salt solutions but not pure water) make up 35% of plasma protein and
are used in the transport of ions, hormones and lipids. They also assist in immune function. Fib-
rinogen accounts for 4% of plasma protein and is essential in the clotting of blood and can be
converted into insoluble fibrin. Regulatory proteins, which make up less than 1% of plasma
protein, are proteins such as enzymes, proenzymes and hormones.
Remember: Plasma proteins act as buffers that help stabilize the pH of the internal
environment. Intracellular proteins absorb hydrogen ions generated by the body's metabolic
processes.
Note: Other plasma proteins include the following:
1. Lipoproteins (chylomicrons, VLDL, LDL, HDL) that are responsible for the transport in the
blood of triglycerides, phospholipid s, cholesterol and cholesterol esters from the liver to
tissues or organs.
2. Transferrin (for iron transport)
3. Prothrombin (a blood-clotting protein)
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
A peptide bond forms between the _ _ group of one amino acid and the
_ _ group of the adjacent amino acid.
• amino; amino
• carboxyl; carboxyl
SAADDES
• ca rboxyl; amino
195
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• carboxyl; amino
Amino acids are j oined together in proteins by peptide bonds. A peptide bond is a chemical
bond formed between two molecules when the carboxyl group of one molecule reacts with the
amino group of the other molecule, thereby releasing a molecule of water. This is a condensa-
tion reaction and usually occurs between amino acids. The resulting CO-NH bond is called a
peptide bond and t he resulting molecule is an amide.
Important Characteristics of the Peptide Bond:
• The bonds involving the <x-carbon can rotate freely
• Unlike its components (the a-amino and a-carboxyl group), the components of the pep-
t ide bond do not accept or give off protons; therefore it does not ionize at physiologic pH
• It is not cleaved by organic solvents or urea, but is susceptible to strong acids. They are ex-
SAADDES
tremely stable.
• It is generally a trans bond (occurs in trans configu ration as opposed to cis configuration)
• It is uncharged but polar
• Proline d ue to formation of a tertiary amine restricts the range of rotation of the a-carbon
in the peptide bond
Remember: Another type of covalent bond that occurs in many proteins is the disulfide bond.
It is formed from the sulfhydryl group (-SH) of each of two cysteine residues, to produce a
cystine residue. It is widely thought t hat these strong, covalent bonds help stabilize the
structure of proteins and prevent them from becoming denatured in the extracellular
environment. Exa mples include the hormone insulin and the immunoglobulins.
1. A residue is a single amino acid unit within a polypeptide chain.
8 2. Cystine is an amino acid that is found in many proteins.
3. Hydroxyproline is a constituent of collagen and is rarely found in any other pro-
tein. Hydroxyproline provides stability to the triple-helical structure of collagen via
hydrogen bonding. Vitamin C is required for hydroxylation of proline (otherwise,
collagen is not formed properly).
4. Glycine is the only non-chira l amino acid.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Both hemoglobin in RBCs and myoglobin in the muscles employ heme as a
prosthetic group.
Myoglobin consists of a single polypeptide with a noncovalently bound
heme group while hemoglobin has four polypeptides, each with its own
heme.
SAADDES
• both statements are true
• both statements are false
• the first statement is t rue, the second is false
• the first statement is false, the second is t rue
196
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Humans need oxygen-binding proteins because molecular oxygen is poorly soluble in body fluid s.
Both hemoglobin in RBCs and myoglobin in the muscles employ heme as a prosthetic group. Myo-
globin consists of a single polypeptide w ith a noncova lently bound heme group while hemoglobin
has fou r polypeptides, each with its own heme. Adult hemoglobin (HbA) has t wo alpha chains and
two beta chains and feta l hemoglobin (HbF) has two alpha chains and two gamma chains. Myoglo-
bin has a far higher oxygen-binding affinity tha n do the hemoglobins, and HbF has a slig htly higher
affin ity than does HbA.
Myoglobin and hemoglobin are heme proteins whose physiological importance is principally
related to their abil ity to bind molecular oxygen. Myoglobin is a monomeric heme protein (it
contains on ly one heme unit, not fou r like hemoglobin) found ma inly in muscle tissue w here
myoglobin serves as an intracellular storage site for oxygen . During periods of oxygen deprivation,
SAADDES
oxymyoglobin releases its bound oxygen, which is then used for metabolic pu rposes. It is also
called muscle hemoglobin.
Important point to remember: Hemoglobin contains four hemes and can potentially associate
with four oxygen molecules.
Myoglobin has a m uch greater affinity for oxygen than does hemoglobin . This makes myoglobin
well suited for its biolog ical function within muscle cells, which is to store oxygen and make
myoglobin's available to the mitochondria. Myoglobin is in fact, much bet ter at this than
hemoglobin because its very high affinity for oxygen at low P0 2 enables myoglobin to bind and
store oxygen effectively. In summary, hemoglobin and myoglobin are specialized proteins,
adapted for different kinds of oxygen-binding fu nctions.
Important: The heme iron in hemoglobin and myoglobin binds molecular oxygen on ly in the ferrous
(Fe'•) state. Its oxidation to the ferric (Fe'•) form produces useless methemoglobin. The enzyme
methemoglobin reductase reduces methemog lobin back to normal hemoglobin, using the coen-
zyme NADH as a reductant.
Note: Carbon monoxide also binds coordinately to heme iron atoms in a manner similar to that of
oxygen, but the binding of carbon monoxide to heme is much stronger than that of oxygen. The
preferential binding of carbon monoxide to heme iron is largely responsible for the asphyxiation
that results f rom carbon monoxide poison ing.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
All amino acids found in proteins are of the:
• D-configuration
•l-configuration
• F-configuration
SAADDES
• (-configuration
197
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• L-configuration
Stereoisomers (optical isomers or enantiomers) are compounds that have the same
composition and the same order of atomic connections, but different molecular
arrangements. In all standard amino acids (except glycine), the a-carbon is
asymmetric, bonded to four different substituent groups (a carboxyl group, an amino
group, an R group and a hydrogen atom). This carbon is ca lled a chiral center. The
fou r different substituent groups can occupy two different arrangements in space,
which are non-super-imposable mirror images of each other. These two forms are
ca lled stereoisomers (optical isomers or enantiomers). Note: All molecules with a
chiral center are also optically active.
SAADDES
The classification and naming of stereoisomers are based on the absolute
configuration of the fou r substituents of the asymmetric carbon atom. The reference
compound to which all other optically active compounds are compared is the
smallest sugar to have an asymmetric carbon (glyceraldehyde). The naming of
configurations of both simple sugars and amino acids is based on the absolute
configuration of glyceraldehyde, as established by x-ray diffraction analysis.
Important: The stereoisomers of all chiral compounds having a configuration related
to L-glyceraldehyde are designated L ("levorotatory") and the stereoisomers related
to D-glyceraldehyde are designated D ("dextrorotatory"). The right and left
designations for glyceraldehyde refer to the manner in which the two forms rotate
plane-polarized light.
Note: 0-amino acids are found in some antibiotics and in bacterial cell walls.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
In contrast to hemoglobin and myoglobin where the iron is always in the
ferrous state (Fe 2 • ), the heme iron of the cytochromes:
• is always in the Fe3 • state
• is always in the Fe<+ state
SAADDES
• is always in the Fe5 • state
• switches back and forth between Fe2 • and Fe 3 •
198
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• switches back and forth between Fe 2 • and Fe ••
The cytochromes contain iron in the form of an iron-porphyrin, usually the heme group. In cont rast
to hemoglobin and myoglobin where the iron is always in the ferrous state, the heme iron of the cy-
tochromes switches back and forth between Fe 2• and Fe ••. Also most cytochromes (but not cy-
tochrome a/a3), the heme iron is bound to two amino acid side chains rather than one. This prevents
t he binding of molecular oxygen, carbon monoxide and other potential ligands.
Cytochromes are in general, membrane-bound hemoproteins that conta in heme groups and carry
out electron transport. They are found either as monomeric proteins (e.g., cytochrome c) or as
subu nits of bigger enzymatic complexes that catalyze redox reactions. Cytochromes are found in
the mitochondrial inner membrane and endoplasmic reticu lum of eukaryotes, in the chloroplasts of
plants, in photosynthetic microorganisms and in bacteria .
SAADDES
The electron transport chain is the final common pathway by which electrons derived from
different fuels of the body flow to oxygen. Note: Electron transport and ATP synthesis by oxidative
phosphorylation proceed continuously in all cells of the body that contain mitochondria.
Cytochromes receive electrons from the reduced form of coenzyme Q (ubiquinone). Each contains
a heme group made of a porphyrin ring containing an atom of iron. This cytochrome iron atom is
t he electron carrier and is reduced when the cytochrome accepts an electron (Fe••, Fe2• ) .
Cytochromes are distinguished by differences in their light-absorption spectra and are designated
b, c1, c, a3 and a. These differences are a result of the heme prosthetic group. Note: Cytochromes
a3 and a are the terminal members of the electron transport chain. They exist as a complex which is
called Complex IV or cytochrome oxidase complex.
Note: The prosthetic groups of cytochromes have four five-membered, nitrogen-containing rings
in a cyclic structure called a porphyrin. The four nitrogen atoms are coordinated with a central Fe
ion that can be either Fe 2• or Fe'•. Remember: These porphyrins are also found in the heme proteins
hemoglobin and cytochrome P450. Glycine and succinyi-CoA are the precu rsors to the
biosynthesis of these rings.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
All amino acids have a carboxyl group and an amino group, both bound
to the same carbon. This carbon is called the:
• a-carbon
• f3 -carbon
SAADDES
•y-carbon
• ),-carbon
199
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• a.-carbon
General structure of the amino acids found in proteins
¥1¥ [9
H- Ni-C- tC- OH
~"'- 1Carboxylic Acid
1
' Amino ,
Group l.al ~ Group
Sid'e Chain ex -carbon
L With the except ion of the nature of the R group, this structure is common
SAADDES
to all the a-amino acids, The central or a.-carbon is in the center, Attached
to this is a hydrogen atom (H), a carboxyl group (COOH), an amino group
(NH 2) and the R group, In all amino acids except glycine, the a-carbon atom has
four different substituent groups (in glycine, the R group is a hydrogen atom),
2, Amino acids can lose their n itrogen-contain ing amino groups and be
converted to a-keto acids (alpha -keto acids) that can ultimately enter the
Krebs cycle (for example, by way of pyruvic acid or the Krebs cycle co mp-
onent oxaloacetic acid, both of which are a-keto acids), An a -keto acid is
simil ar to an amino acid, except that an a -keto acid has oxygen rather than
an amino group bonded to its a -carbon,
3, When proteins are broken down and used for energy, most of this energy
is derived from the oxidation of a-keto acids (Le,, pyruvate, oxaloacetate and
a-ketoglutarate), These substances can then enter the Krebs cycle,
4, Dipept ides are formed by a reaction between the carboxyl group of one
amino acid and the amino group of another amino acid, The substituted
amide bond thus formed is called the pept ide bond,
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Glutamate can be synthesized by the addition of ammonia to a -ketoglutar-
ate. All of the following amino acids can be derived from glutamate EXCEPT
one. Which one is the EXCEPTION?
• asparagine
SAADDES
• glutamine
• proline
• arginine
200
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• asparagine
Synthesis of amino acids:
•CL-ketoglutarate gives rise to glutamate, which in turn is the precursor of glut-
amine, proline and arginine
• 3-phosphoglycerate gives rise to serine, which in turn is the precursor of gly-
cine and cysteine
• Oxaloacetate gives rise to aspartate, which in turn is the precursor of aspara-
gine, methionine, threonine and lysine
Note: Threonine is the precursor of isoleucine.
SAADDES
• Pyruvate gives rise to alanine, valine, leucine and isoleucine
Note: Isoleucine can be formed by either pyruvate or th reonine.
• Phosphoenolpyruvate and erythrose-4-phosphate produce shikimate, wh ich
is converted to chorismate. Chorismate then gives rise to tryptophan, tyrosine
and phenylalanine. This biosynthetic pathway only occurs in plants and bacteria
not in humans.
Note: Tyrosine is synthesized from phenylalanine in humans.
• Ribose-5-phosphate gives rise to histidine
Remember: Humans can only synthesize 11 ofthe 20 common amino acids. The other
9 amino acids must be consumed in the diet and include: histidine, isoleucine, leucine,
lysine, methionine, phenylalanine, th reonine, t ryptophan and valine.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Elastin has an aberrant amino acid composition, with high proportions of:
• valine, phenylalanine and lysine
• tryptophan, histidine and methionine
• glycine, alanine and proline
SAADDES
• threonine, cysteine and g lutamate
201
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• glycine, alanine and proline
The elastic fibers of the extracellular matrix have two components: an inner core of
amorphous elastin and a layer of 10-nm microfibrils surrounding t he elastin. Elastin
has high proportions of g lycine (31%), alanine (22%) and proline (11%). Some
hyd roxyproline (1%; a derivative of proline) is also present, but t here is no
hydroxylysine. Like collagen, elastin conta ins covalent crosslinks that are derived
from allysine. Therefore, lysyl oxidase is required for the synthesis of elastin as well
as of collagen. The covalent cross links of elastin are similar to those of collagen except
for desmosine, which is present in elastin but not collagen.
In contrast to collagen, which forms fibers t hat are toug h and have high tensile
SAADDES
strength, elastin is a connective tissue protein w ith rubber-li ke properties. Elastic
fibers can be stretched to several t imes their normal length (it is the elastin that gives
these fibers the capacity of return ing to their ori ginal lengths after being stretched).
These fibers are found in the skin, ligaments and the walls of arteri es, where t he fibers'
elastic properties are important.
1. The polypeptide subunit of elastin fibrils is tropoelastin.
2. Elastin fibers are fo rmed as a t hree-dimensional network of cross-linked
polypeptides. The cross-links involve lysine and oxidized lysine residues
(a Ilysine), wh ich are covalently linked to produce a desmosine cross-link.
3. The oxidation of lysine residues in both col lagen and elastin is an extra-
cellular process catalyzed by lysyl oxidase (a copper requiring enzyme).
4. The amorphous elastin is surrounded by microfibrils. The most important
microfibril protein, fibrillin-1, is defective in Marfan syndrome.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Which of the following amino acids carry a positive charge on the side chain
which makes them basic?
Select all that apply.
• lysine
SAADDES
• glutamate
• arginine
• histidine
• aspartate
• tyrosine
202
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
· lysine
• arginine
• histidine
Each of the 20 amino acids found in proteins can be distinguished by the R-group substitution on
the a-carbon atom . There are two broad classes of amino acids based upon whether the Rgroup is
hydrophobic or hydrophilic.
The hydrophobic (non-polar) amino acids tend to repel the aqueous environment and therefore,
resid e predominantly in the interior of proteins. This class of amino acid s does not ion ize or
participate in the formation of H-bonds. Hydrophilic (polar) amino acid s tend to interact with the
aqueou senvironment, are often involved in the formation of H-bonds and are predominantly found
on the exterior surfaces proteins or in the reactive centers of enzymes.
The functions of amino acid s in proteins are determined by the noncovalent int eractions and the
SAADDES
cova lent bonds that their side chains can form:
• The small amino acids (glycine and alanine) occupy little space. In proteins they are often
found in places where two polypeptide chains have to come close together.
• The branched-chain amino acids valine, leucine and isoleuci ne have hydrophobic sid e chains.
• The hydroxyl amino acids seri ne and threonine form hydrogen bonds with their hydroxyl
group. This group also forms covalent bonds with carbohydrate in glycoprotein sand with phos-
phate in phosphoproteins.
• The sulfur amino acids cysteine and methionine are quite hydrophobic, although cysteine also
has weak acidic properties.
• The aromatic amino acids phenylalanine, tyrosine and tryptophan are hydrophobic, although
the sid e chains of tyrosine and tryptophan can also form hydrogen bonds.
• The acidic amino acids glutamate and aspa rtate have a carboxyl group in the side chain that
is negatively charged at pH 7. The corresponding carboxamid e groups in glutamine and aspara-
gine are not acidic but can form strong hydrogen bonds.
• The basic amino acids lysine, arg inine and histidine carry a positive cha rge on the sid e chain,
although the pK value of the histidine side chain is quite low.
• Proline is a freak among amino acids with its nitrogen tied into a ring structure as a second ary
amino group. Being stiff and angled, it is often found at bends in the polypeptide.
Saad Alqahtani, Twitter @saaddes
OH
l
[.......(',.........
-~]·
/
Aromatic
CH>
amino
acids J-ilN- CH- COo-
Tyroslne
0
II
0 y-NH,
SAADDES
coo- I
Acidic C-NH<! 9Hl
amino
acids
CH;. Cll" 9~
f-t,N-CH-coo- ~r< - CH - coo- ~N-CH-Cco·
Aspartate Asparagine Glutamine
~li~ WH;
r•·r, H~- C - NH7
N -.
Basic
amino
TH" TH' / \
acids
?H> TH'
""/NH
r
CH,
TH' YH' Imino acid
H3N- CH COO H;;r.t -tH-coo- >t,N - cH coo-
Lysine Arginine Histidine
Structure of the Amino Acids in Proteins
202 A· l
Saad Alqahtani, Twitter @saaddes
OH
l
[.......(',.........
-~]·
/
Aromatic
CH>
amino
acids J-ilN- CH- COo-
Tyroslne
0
II
0 y-NH,
SAADDES
coo- I
Acidic C-NH<! 9Hl
amino
acids
CH;. Cll" 9~
f-t,N-CH-coo- ~r< - CH - coo- ~N-CH-Cco·
Aspartate Asparagine Glutamine
~li~ WH;
r•·r, H~- C - NH7
N -.
Basic
amino
TH" TH' / \
acids
?H> TH'
""/NH
r
CH,
TH' YH' Imino acid
H3N- CH COO H;;r.t -tH-coo- >t,N - cH coo-
Lysine Arginine Histidine
Structure of the Amino Acids in Proteins
202 A· l
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
The primary st ructure of a protein refers to the spatial a rrangement of a portion
of a polypeptide chain determined by the amino acids present.
The secondary structure of a protein refers to the irregular folding of a polypep-
tide chain (the overall three-dimensional conformation of the polypeptide).
SAADDES
• both statements are true
• both statements are false
• the first statement is t rue, the second is false
• the first statement is fa lse, the second is true
203
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are false
Proteins differ from each other because each has a distinctive number and sequence
of amino acid residues. The amino acids are the alphabet of protein structure. No
other property so clearly d istinguishes one protein from another.
The primary structure consists of a sequence of amino acids linked together by
cova lent peptide bonds.
The secondary structure refers to t he spatial arrangement of a portion of a
polypeptide chain determined by the amino acids present (pri mary structure). The
SAADDES
most common types of secondary structures are the a -helix (coiled conformation of
a peptide chain), j}-pleated sheets (an extended, zigzag arrangement of a polypep-
tide chain) and 13-hairpin turns (reverse turns).
The tertiary structure refers to the irregular folding of a polypeptide chain (the
overall three-dimensional conformation of the polypeptide [e.g., globular, fibrous
and pleated sheet]). Note: The best method for determining the three-dimensional
structure of a protein is by x-ray diffraction.
The quaternary structure refers to the spatial arrangement of subunits in a protein
that consists of more than one polypeptide chain. Two examples of proteins w ith
quaternary structures are the hemoglobin and antibody molecules found in the
blood of a mammal.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Patients with vitamin C deficiency (scurvy) form a collagen with insufficient:
• isoleucine
• hydroxylysine
• valine
SAADDES
• hydroxyproline
204
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hydroxyproline
*** The hydroxylation of prolyl and lysyl side chains in procollagen req uires ascorbic acid
(vitamin C). As a result, patients with vitamin C deficiency (scurvy} form a collagen wit h
insufficient hydroxyproline t hat denatures spontaneously at room temperature.
Collagen accounts for approximately 25% of the body protein in adults and 15% to 20% in
children. It is most abundant in strong, tough connective tissues. Type I collagen is by far t he
most abundant collagen in the body. lt has a most unusual am ino acid composition, with 33%
glycine and 10% proline. It also contains hydroxyproline and hydroxylysine.
The basic structural unit of collagen fibrils, t he tropocollagen molecule, consists of t hree
intertwined polypeptides. In t he case of type I collagen, it has a very unusual am ino acid
seq uence, with glycine in every third position. Tropocollagen is the longest known protein and
SAADDES
is formed from procollagen, which is secreted by fibroblasts. The t hree helical polypeptides
of the tropocollagen molecule are wound around each other in a right-handed triple helix.
Note: The long, ropelike tropocollagen molecules form fibrils by aligning t hemselves in paral-
lel. Once secreted outside the cell tropocollagen units are crosslinked through covalent
bonding between adjacent lysine residues to produce mature collagen.
Remember: Vitamin C influences t he formation of collagen, which is t he organic matrix found
in dentin and cementum (see note #1 below).
~ 1. Hydroxyproline and hydroxylysine are nonstandard amino acids that are
f!1P~J present in few other proteins. For t his reason, t heir concentration in a particular tis-
~ sue is a good estimate of the collagen content as well. They are not used directly
in the reactions of protein synthesis. These amino acids are formed by t he hydroxyla-
tion of proline and lysine (by lysyl hydroxylase}. This hydroxylation involves a-keto-
glutarate, oxygen, Fe'• and vitamin C (ascorbic acid), which is required because it
restores iron to its reduced state (Fe,.).
2. Collagen and reticular fibers make up the stroma of all lymphoid tissues except
the thymus.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
Which of the following serves as a principal source of carbon for nonessen-
tial amino acids?
• fats
• water
SAADDES
• ca rbohydrates
• urea
205
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• carbohydrates
***Ten of the nonessential amino acids contain carbon skeletons that can be derived
from glucose. Note: Tyrosine, the 11th nonessential amino acid, is synthesized by the
hydroxylation of the essential amino acid phenylalanine.
Remember: The essential amino acids include: valine, threonine, leucine, methionine,
isoleucine, lysine, phenylalanine, histidine and tryptophan. The nonessential amino acids
include: alanine, asparagine, cysteine, glutamine, proline, tyrosine, arginine, as partate,
glutamate, glycine and serine. Note: Although cysteine's carbon skeleton can be formed
from carbohydrates, cysteine requires the essential amino acid methionine to supply the
sulfhydryl group.
SAADDES
Important: Nonessential amino acids can be synthesized from the corresponding
a-keto acids, an a-amino acid (as the NH 3• donor), a specific transaminase enzyme and
pyridoxal phosphate ([PLP), the coenzyme form of vita min Bl)l. These amino acids
include alanine, aspartate and glutamate. The other nonessential amino acids are
synthesized by amidation (g lutamine and asparagine).
Amino acids are degraded to carbon dioxide, water and urea. The separation of the amino
nitrogen f rom the carbon skeleton is an early event in the cata bolism of most amino acids.
In most cases, the amino group is initially transferred to a-ketoglutarate in a t ransamina-
tion reaction. The glutamate formed in these reactions is oxidatively deaminated by gluta-
mate dehydrogenase, forming free ammon ia. Note: Because ammonia is toxic, it has to be
converted to nontoxic urea in the urea cycle. This pathway is present on ly in the liver.
Note: The carbon skeletons of the amino acids are channeled either into gluconeogene-
sis (glucogen ic amino acids) or into ketogenesis (ketogenic amino acids).
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
A patient of yours suffers from phenylketonuria (PKU). Your dental assistant
offers her a bottle of soda. The patient, a relatively intelligent dental stud-
ent, responds by saying:
•I cannot have th is because it conta ins tyrosine, wh ich I am unable to metabolize
• I cannot have this because it conta ins phenylalanine, which I am unable to
metabolize
SAADDES
• Thank you, I need to drink this to supplement my phenylalanine levels
• Thank you, I need to drink this to supplement my tyrosine levels
Which supplement would you expect this patient to be taking?
• tyros ine
• phenylalanine
• both tyrosine and phenylalanine
• neither, no supplement needed
206
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• I cannot have this because it contains phenylalanine,
which I am unable to metabolize
• tyrosine (she cannot produce this amino acid)
Tyrosine is formed from phenylalanine, wh ich is an essential amino acid that is need-
ed for optimal growth in infants and for nitrogen equilibrium in adults.
Hydrophobic amino acids have side chains that conta in:
• Aliphatic groups: val ine, leucine and isoleucine
• Aromatic groups: phenylalanine, tyrosine and tryptophan
Dopamine, the thyroid hormones (tri iodothyronine and thyroxine), melanin,
SAADDES
norepinephrine and epinephrine are all synthesized from the amino acid tyrosine.
Remember: Melanin is the natural substance that gives color (pigment) to hair, skin
and the iris of the eye.
5-hydroxytryptamine (serotonin), melatonin, niacin and the nicotinamide moiety of
NAD+ and NADP+ are formed from the essential amino acid tryptophan.
1. When the enzyme (phenylalanine hydroxylase) that cata lyzes the trans-
formation of phenylalanine to tyrosine is not active because of a hereditary
defect, the serious disease known as phenylketonuria (PKU) results.
2. Negative nitrogen balance (nitrogen output exceeds intake) may be
caused by a dietary lack of essential amino acids.
3. Albinism is a genetic disease caused by the absence of tyrosinase (a crit-
ical enzyme necessary for the synthesis of melanin from tyrosine in melano-
cytes). Albinos do not have problems w ith epinephrine synthesis, despite
melanin and epinephrine having DOPA as a common intermediate, because
a different enzyme is used in DOPA for melanin synthesis.
Saad Alqahtani, Twitter @saaddes
proteins/amino acids
All G proteins exist in two forms:
• an inactive GTP-bound form that acts on the effector and an active GOP-bound form
that does not
• an active GTP-bound form that acts on the effector and an inactive GOP-bound form
that does not
SAADDES
• an active ATP-bound form that acts on the effector and an inactive AOP-bound form
that does not
• an inactive ATP-bound form that acts on the effector and an active AOP-bound form
that does not
207
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• an active GTP-bound form that acts on the effector and an
inactive GOP-bound form that does not
Many neurotransmitters manipulate the membrane potential of their target cell directly by opening
a ligand-gated ion channel in the plasma membrane. Water-soluble hormones however, trigger
lengthy signaling cascades. Most hormone receptors activate a G protein which triggers the synthe-
sis of a second messenger. cAMP, cGMP, IP3 (acting th rough Ca" ) and 1-2-diacylglycerol (DAG) are
most important. The second messengers activate protein kinases, including kinases A (cAMP-acti-
vated), C (Ca'•-diacylglycerol-activated), G (cGMP-activated) and the calmodulin-dependent protein
kinases (Ca'•-activated).
G proteins (guanine nucleot ide-binding proteins) play a pivotal role in the signal transduction
pathways for numerous hormones and neurotransmitters. The G protein is loosely bound to the
SAADDES
cytoplasmic surface of the plasma membrane and it consists of three subunits designated a, fl
andy. The a subunit has a nucleotide binding site that can accommodate either GDP or GTP. fl and
y subunits function as a single unit, but the a subunit isonly loosely associated with fly.
The inactive G protein is associated with the unstimulated receptor, with GDP bound to the a
subunit. Hormone binding induces a conformational change both in the receptor and the
attached G protein. This conformat ional change greatly reduces the affinity of the a subunit for
GDP. GDP dissociates away and is quickly replaced by GTP.
Once GTP is bound, the G protein leaves the receptor and breaks up into the a-GTP subunit and the
fly complex. Both the a-GTP subunit and the fly complex diffuse along the inner surface of the
plasma membrane, where they bind to target proteins known as effectors.
1. The GTP bound a subunit of the G protein activates adenylate cyclase.
2. Active adenylate cyclase converts ATP to cAMP. cAMP further binds and activates PKA.
3. Active protein kinase A (PKA) phosphorylates specific proteins which up or down-reg-
ulates cellular processes depending on the cell type.
4. The components of the activated G protein are membrane-bound messengers that
t ransmit a signal from t he receptor to the effector.
5. All G proteins exist in two forms: an active GTP-bound form that acts on the effector
and an inactive GOP-bound form that does not.
Saad Alqahtani, Twitter @saaddes
lipids
In saturated fatty acids, the carbons are linked exclusively by single bonds.
Monounsaturated fatty acids have one carbon-carbon double bond and
polyunsaturated fatty acids have more than one.
• both statements are true
SAADDES
• both statements are false
• the first statement is t rue, the second is false
• the first statement is fa lse, the second is t rue
208
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statem e nts are tru e
A "standard" fatty acid is an unbranched hydrocarbon chain with a carboxyl group at one
end. Most naturally occurring fatty acids have an even number of carbons; chain lengths of
16 and 18 are the most common.
Fats can be classified by the n umber of double bonds between carbon atoms in their fatty
acid molecules:
• Saturated fat: conta ins no double bonds between carbon atoms
• Monoun saturated fat: has one double bond between carbon atoms
Note: Most monounsaturated fatty acids are in the CIS (same -side) form.
• Polyunsaturated fat: has multiple double bonds between carbon atoms
Essential fatty acids cannot be synthesized because humans lack the enzymes to p lace
SAADDES
double bonds at certa in positions (omega-3 and omega-6) and must therefore obtain
them fro m the diet. All fatty acids are building b locks of phospholipids and glycolipids
and are therefore needed for the synthesis of membranes. Note: Cell s derive energy
from fatty acids through beta-oxidation.
Satur ated Fatty Acids Monounsatur ated Fatty Acids Polyunsaturated Fatty Acids
Arachidic acid Caprylic acid Emcic acid Arachidonic acid
Behenic acid Lauric acid OJeic acid Linoleic acid
Butyric acid Myristic acid PahnitoJcic acid Linolenic acid
Capric acid Palmitic acid
Caproic acid Stearic acid
Important: Some of the polyunsaturated fatty acids, notably linoleic acid and linolenic
acid, are nutritionally essential. Arachidonic acid can be synthesized from dietary linoleic
acid.
Saad Alqahtani, Twitter @saaddes
lipids
Dietary triglycerides are digested and broken down to free fatty acids and 2-
monoacylglycerol by pancreatic lipase which are absorbed with the help of:
• elastase
• pepsinogen
SAADDES
• trypsinogen
• bile salts
209
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• bile salts
Unlike t he tri glycerides, t he products of fat d igestion are slightly soluble in water. The
efficient absorption of the fatty acids and 2-monoacylglycerol requ ires bile salts as
emulsifiers. Between 20 and sog of bile salts reach the intestine every day.
Like a detergent, bile salts contain hydrophobic and hydrophilic components. The
hydrophobic portions of the molecule associate with the fat and t he hydrophilic parts
associate w ith water, serving to solubilize (emulsify) the otherwise insoluble fat. The
micelles, wh ich are tiny m icrodroplets emulsified by bile salts, travel to the m icrovilli
of the intestinal epithelial cells, w hich absorb t he fatty acids. The bile salts are
resorbed in the distal ileum via Na•/bile acid cotransporters, recycled by the liver and
are resecreted into the gut during subsequent digestive cycl es. ***Up to 95% of bile
SAADDES
salts are recycled.
Bile salts perform two important actions in t he intestinal tract:
1. Most important, bile salts help in the absorption of fatty acids, monoglycerides,
cholesterol, fat-soluble vitamins and other lipids from the intestinal tract (form water-
soluble complexes, called micelles, w ith fatty acids and g lycerides).
2. Bile salts also have a detergent action on the fat particles in the food, w hich de-
creases the surface tension of the particles and allows agitation in the intestinal t ract
to break the fat globules into minute sizes.
In general, lipids with the lowest water solubility are most dependent on bile salts fo r
their absorption.
Bile acids are usually conjugated in amide linkage w ith the amino acid glycine or
taurine, giving bile salts. The chol ic acid conjugates with glycine and tau rine are
ca lled glycocholate and taurocholate, respectively.
Note: Fat malabsorption can result from pancreatic fai lure, lack of bile salts, or exten-
sive intestinal diseases. This condition is called steatorrhea.
Saad Alqahtani, Twitter @saaddes
lipids
A membrane phospholipid that does NOT contain glycerol is:
•lecithin
• sphingomyelin
• cerebroside
• cardiolipin
SAADDES
210
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• sphingomyelin
*** Most membrane phospholipids contain glycerol (lecithin, cerebroside and
ca rdiolipin). Sphingomyelin is an exception and is based on sphingosine.
Phospholipids are lipids. Each molecule is made up of one glycerol molecule
attached to two fatty acids and a phosphate group. Structurally, phospholipids
are similar to t riglycerides except that a phosphate g roup replaces one of the
fatty acids. Phospholipid molecules have one end that is attracted to water while the
other is repelled by it. This property is important in plasma membranes. The fatty acid
end that is not attracted to water is said to be hydrophobic. At the other end of the
SAADDES
molecule, the phosphate group that is attracted to water is said to be hydrophilic.
Three major types of body phospholipids:
1. The lecithins: are a group of phospholipids that upon hydrolysis yield two fatty
acid molecules and a molecule each of glycerol, phosphori c acid and choline. They
are water soluble emulsifiers and membrane constituents.
2. The cephal ins: are a group of phospholipids having hemostatic properties and
found especially in the nervous tissue of the brain and spinal cord. The cephal ins
resemble lecithin, except they contain either 2-ethanolamine or L-seri ne in the
place of cho line.
3. The sphingomyelins: are a group of phospholipids that are found especially in
nerve t issue and yield sphingosine, choline, a fatty acid and phosphoric acid upon
hydrolysis. They are membrane constituents. Note: The neurologic disturbances
seen in Niemann-Pick disease are associated with the accumulation in CNS tissue
of sphingomyelin.
Saad Alqahtani, Twitter @saaddes
lipids
Which one of the following sequences places the lipoproteins in the order of
most dense to least dense?
• HDL- VLDL- chylom icrons- LDL
• LDL-chylom icrons-HDL-VLDL
SAADDES
• HDL-LDL-VLDL-chylom icrons
• VLDL-chylomicrons-LDL-HDL
• chylomicrons-HDL-LDL-VLDL
211
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• HDL-LDL-vLDL-chylomicrons
Lipids (triglycerides and cholesterol) are not able to move in body fluids due to their
hydrophobic nature so they are packaged in micellar st ructu res called lipoproteins. The
various lipoproteins are class ified in terms of density. Note: Since lipids are much less
dense than proteins, there is an inverse relationship between the lipid content and
density (i.e., high lipid content means low density particle). The maj or component s of
lipoproteins are triacylglycerols (triglycerides), cho lesterol and cholesterol esters, which
are the components being transported, and phospholipids and proteins which make up
the micellar memb rane (the protein component alone is ca lled an apolipoprotein).
Types of lipoproteins:
SAADDES
• Chylomicrons: least dense lipoprotein; most trig lyceride and the least protein con-
tent. Transport dietary t riacylglycero ls from the Gl tract to muscle, adipose tissue and
liver.
• VLDLs (very low-density lipoproteins): more dense than chylomicrons; high content
of trig lycerides. Transport endogenous triacylglycerols from the liver to various ti ssues
(primarily muscle and adipose tissue).
• LDLs (low-density lipoproteins): denser than VLDLs; less triglyceride and more protein
content. Has h ighest content of cholesterol. They are the primary plasma carriers of
cholesterol for delivery to all tissues b ut especially to the liver.
• HDLs (high-density lipoproteins): most dense lipoprotein; has the lowest t rig lycer-
ide and highest protein content. Transfers cholesterol as an acyl ester derivative from
other t issues back to the liver.
Note: These lipoproteins are transported into the cells by way of receptor-mediated
endocytosis.
Saad Alqahtani, Twitter @saaddes
lipids
Which of the following statements about plasma lipoproteins are correct?
Select all that apply.
• chylomicrons are synthesized in the intestinal mucosal cells and transport
triacylglycerol to the peripheral tissues
• HDL particles are produced from LDL particles in the circulation by the action of
SAADDES
lipoprotein lipase
• HDL competes with LDL for binding to receptors on the surface of cells in
extrahepatic tissues
• very low density lipoprotein (VLDL) particles are the precursors of LDL in the
circulation
212
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• chylomicrons are synthesized in the intes tinal mucosal cells and
t ran s port triac ylg lycerol to the peripheral ti ssue s
• very low de nsity lipoprotein (VLDL) particles are the precursors of
LDL in the circulation
Chylomicrons are plasma lipoproteins consisting of a large d roplet of triacylglycerols
that a re stabilized by a coat of protein and phos pholipid. Chylomi crons carry fatty acids
o bta ined in the diet to the tissues where they are consumed or stored as fuel. The
remnants of chylo mi crons, depleted of their triacylg lycerols (trig lycerides) but still
containing cholesterol, move through the bloodstream to the liver, where they a re taken
up, degraded in lysosomes and their constituents recycled.
SAADDES
Note: Chylomicrons are the least de nse of the blood lipoproteins because chylomi crons
have the most triacylglycerols and the lea st protein content.
Remember: Lipoproteins are lipid-bind ing proteins, responsible for the transport in the
blood of triglycerides, phospholipids, cholesterol and cholesterol esters from the liver to
tissues or organs. Other lipoproteins include the foll owing:
• Very low-density lipoproteins (VLDL): these contain a high concentration of trigly-
cerides and moderate concentrations of both phospholipids and cholesterol
• Low-density lipoproteins (LDL): are ve ry rich in cholesterol. They are the major
cholesterol carrier in the blood and are derived from VLDL
• High-density lipoproteins (HDL): are protein rich with relatively little free cholest-
e rol; most of the cholesterol is present as acyl ester derivatives
1. HDL particles a re produced de novo in the liver.
2. HDL and LDL pa rticles each have their o wn s pecific binding sites on cell
membranes (HDL on the liver, and LDL on the liver and extrahepatic tissues).
3. Lovastatin ("statin" d rug) lowers blood cholestero l levels by inhibiting
HMG CoA reductase, a key regulatory enzyme in cholestero l biosynthesis.
Saad Alqahtani, Twitter @saaddes
lipids
Ketone bodies are formed only in the:
• stomach
• kidney
• pancreas
· li ver
SAADDES
213
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• liver
liver mitochondria have the capacity to divert any excess acet yi-CoAderived from fatty acid or pyruvate
oxidation into ketone bodies. The compounds classified as ketone bod ies are acetoacetate, P· hydroxy·
butyrate and acetone (a non metabolizable side p rod uct). Ketone body prod uction is regulated p rima·
rily by availabi lity of acetyi-CoA. Duri ng conditions of low glucose availability (a period of starvation or
fasting, or a case of d iabetes mell itus}, the mobi lization otfatt y acids from adipose tissue ishigh such that
hepatic beta-oxidation will occur at a high rate and so will synthesis of ketone bodi es from the resulting
acetyi-CoA. These ketone bod ies are then transported in the blood to peripheral ti ssues, where the ke-
tone bod ies can be reconverted to acetyi-CoA and oxid ized by the citric acid cycle (Krebs cycle). They are
important sources of energy for the peri pheral tissues.
Synthesis of ketone bodies by the liver is a three-step process:
• The first st ep is formation of acetoacetyi· CoA in a reversal of the thiolase step of beta-oxidation
SAADDES
• In the second step, a thi rd molecule of acetyi-CoA condenses with the acetoacet yi-CoA, formi ng 3·
hydroxy· 3· methylglutaryl CoA (HMG CoA) in a reaction catalyzed by HMG-CoA synthase
Note: This enzyme, HMG-CoA synthase, is the rate-limiting step in the synthesis of ketone bodies
and is present in significant q uantities only in the liver.
• In the third step, HMG-CoA is cleaved to yield acetoacetate (a ketone body) and acet yi-CoA in a re-
action catalyzed by HMG·CoA lyase (HMG·CoA cleavage enzyme)
Note: Acetoacetate can be red uced to form f3·hydroxybutyrate o r can be spontaneously decar·
boxylated to form acetate (which cannot be metabolized by t he body). It is vol atil e and can be
blown out in the b reath.
1. Ketone bodies are utilized exclusively by extrahepatic tissues (hea rt and skeletal muscle
use ketone bodi es parti cularly effectively). Unlike fatty acids, ketone bodies can be
oxid ized by the brain. Note: Fatty acids are unable to cross the blood-brain barrier, but
ketone bodies can.
2. When the rate of formation of ketone bodies is g reater than the rate of their use, their
levels begi n to rise in t he blood (ketonemia) and eventually in the u rine (ketonu ria). These
t wo cond itions are seen most often in cases of starvation o r severe d iabetes mell it us.
3. Extrahepatic ti ssues convert ketone bodies back to acetyl CoA by using succinyl CoA as a
CoA donor and the enzyme thiophorase. The liver itself lacks t hiophorase and thus cannot
use ketone bodies for its own energy needs.
Saad Alqahtani, Twitter @saaddes
lipids
All of the following are sources of acetyi -CoA for fatty acid synthesis EXCEPT
one. Which one is the EXCEPTION?
• creatinine
• pyruvate
SAADDES
• glucose
• citrate
214
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• creatinin e
***Glucose is the major source of acetyi-CoA for fatty acid synthesis.
Acetyi-CoA for fatty acid synthesis comes mostly from the glycolytic breakdown of
glucose when high amounts of glucose are consumed (e.g., a high ca rbohydrate diet).
Fatty acid synthesis occurs primarily in the cytoplasm of the liver, lactating mammary
glands and to a lesser extent, in adipose tissue and kidney. The process incorporates
ca rbons from acetyl CoA into the growing fatty acid cha in, utilizing ATP and reduced
nicotinamide adenine dinucleotide phosphate (NADPH).
Important points to remember for fatty acid synthesis:
SAADDES
• Glucose is first degraded to pyruvate by glycolysis in the cytoplasm.
• Pyruvate is then t ransported into the mitochondria, where pyruvate
dehydrogenase oxidatively decarboxylates pyruvate, form ing acetyi-CoA and
other products.
• Acetyi-CoA can then serve as a substrate for citrate synthesis.
• Citrate is transported out of the m itochond ri a to the cytoplasm (where fatty
acid synthesis occurs) via the citrate -malate-pyruvate shuttle. Finally, citrate
splits to generate cytoplasmic acetyl-Co A for fatty acid synthesis.
Summary of fatty acid synthesis: Acetyi-CoA --+ Malonyi-CoA --+ Malonyi-ACP-+
Acetyi-ACP-+ Acetoacetyi-ACP-+ Butyryi-ACP-+ Fatty acid
***The carboxylation of acetyi-CoA to form malonyi-CoA is catalyzed by acetyi-CoA
carboxylase (an allosteri c enzyme that is the pri ncipal regulator of the pathway).
Remember: Malonyi-CoA is the th ree-carbon intermediate that participates in the
biosynthesis of fatty acids but not in their breakdown.
Saad Alqahtani, Twitter @saaddes
SAADDES
• n Although NAD & FAD
play important roles in these
pathways, t hey have been
left out of t his d iag ram fo r
the sake of simplicity.
Summary of Glucose Metaboli.sm
Glucose is catabolized to pyruvic acid in the process of glycolysis. If oxygen is available, pyruvic acid is
converted to acetyi-CoA and then enters t he citric acid cycle and transfers energy to the maximum num-
ber of ATP molecules via oxidative phosphorylation .lf oxygen is not available, pyruvic acid is converted
to lactic acid, incurring an oxygen debt. The oxygen debt is later repaid when ATP p roduced via oxidative
phosphorylation is used to convert lactic acid back into pyruvic acid or all the way back to g lucose. If
there is an excess of g lucose, the cell may convert it to glycogen (glycogenesis). later, individ ual glucose
molec ules can be removed from the g lycogen chain by t he p rocess of glycogenolysis. 214-1
Saad Alqahtani, Twitter @saaddes
lipids
Which of the following is involved in both fatty acid catabolism and
synthesis?
• carnitine
• coenzyme A
SAADDES
• malonyi-CoA
• alcohol dehydrogenase
215
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• coenzyme A
Fatty Acid Catabolism (summary):
The fat ty acid is transported to the mitochondria by employing carnitine as a carrier substance. Once
inside the mitochondria, the fatty acid is transferred from the carnitine to a CoA and is oxidized (via
beta oxidati on) to acetyi-CoA. The acetyi-CoA molecules enter into the citric acid cycle (Krebs cycle)
to form carbon d ioxide and reducing equivalents (NADH, FADH 2). The reducing equivalents are then
reoxid ized by electron transport system and the energy released by that process is used by the
oxidative phosphorylation system to form ATP. Note: Fatty acids are the predominant source of ATP for
moderate levels (lasting longer than 1 hour) of activity.
Biosynthesis of Fatty Acids (summary):
This occurs in the cytosol. It involves two carbon additions from acet yi-CoA and an acyl protein (ACP).
A key intermed iate in the synthesis of fatty acids is malonyi-CoA, which is formed from acetyi-CoA,
SAADDES
bicarbonate and ATP. This irreversible reaction is the committi ng step in fatty acid synthesis.
< ompml\o n ol J<:tth \nd ~\nlh•SJ\ .:and l>• l!• adatwn
Synthesis O~radatinn
Crcatcst flux through pathway ARcr carbohydratc·rich meal In star.•atJon
Hormonal state favorin)l: pathway High insulin/glucagon raiio Low msuhnlglucagon riltio
Majortissucs.itc Primarily liver Muscle. liver
Subct'lluln location Primnnly cytosol Pn maril>• mit<Khondna
Carriers of acyllact't)'l groups CJtrtalc (mJtocbondrin to cytosol) Cnmilinc ( C)'I0$01 to mitochondria)
bdwccn mito<'hondria and cytosol
Phosphopantctbcinc-t'onhaininJ,t A<:yl cnrri« protein domam. Coenzyme A
ac-tive u rritrs coenzyme A
Oxidation/reduction cofa ctors NAOPH NAn•. P'A D
TwCH'arbon donor/ product Malonyl Cot\: dooorof Acet)'l CoA: product
one acetyl group
Acth·ator C1tralc
lobibitor Falty acyl CoA (inhibits acetyl Malonyl CoA (inhibils camilinc
CoA carboxylase) acyltransfcrasc)
P1·oduct nfpathway Palnutalc Acetyl Cot\
Saad Alqahtani, Twitter @saaddes
lipids
A patient of yours has uncontrolled diabetes mellitus. This causes ketosis, or
high levels of ketone bodies, in the body tissues and fluid. Which of the
following is NOT a symptom of this condition?
• fruity breath
• lowered pH of the blood
SAADDES
• decreased potassium in the urine
• ketone bodies in the urine
216
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• decreased potassium in the urine
Ketosis is a cond ition characterized by an abnormally elevated concentration of ketone
bodies in the body t issues and fluids. Ketosis occurs when fatty acids are incompletely
metabolized, a complication of starvation, fasting and alcoholism. It is characterized by
ketones in the urine (ketonuria), ketone bodies in the blood (ketonemia), potassium loss
in the urine and a fruity odor of acetone on the breath.
Important: The complete absence of insulin in type 1 diabetes leads to diabetic
ketoacidosis w ith severe ketonemia, acidosis and b lood glucose levels as high as 1000
mg/dl. Large amounts of glucose and ketone bodies are lost in the urine and osmotic
diuresis causes dehydration and electrolyte imbalances. The co ma is caused by
dehydration, electrolyte disturbances and acidosis. Untreated ketoacidosis is fatal.
SAADDES
Proper treatment includes fl uid replacement, correction of the acidosis and generous
insulin injections. Note: Glucose i s effective in reversing ketosis in a non-diabetic patient.
Hyperglycemia and ketoacidosis are hallm arks of untreated diabetes mellitus. Hyper-
glycemia is caused by increased hepatic production of glucose combined w ith diminished
peripheral utilization. Ketosis results from increased mobilization of fatty acids fro m adi-
pose tissue combined with accelerated hepatic synthesis of 3-hydroxybutyrate and ace-
toacetate.
1. The overtreatment of diabetes w ith insulin or oral antidiabetic drugs leads to
8 hypoglycemic shock.
2. Acetone is not utilized by the body as a fuel (fruity, "acetone" smelling breath
is a hallm ark of diabetic ketoacidosis).
3. In a healthy diet, most acetyi-CoA is processed through the citric acid cycle.
During fasting, the normal balance between carbohydrate and fatty acid
metaboli sm is disrupted and activity of the citric acid cycle is reduced. Then some
of the acetyi-CoA produced from fats will be converted to ketone bodies.
Saad Alqahtani, Twitter @saaddes
lipids
All of the following statements concerning fatty acid synthesis are true
EXCEPT one. Which one is the EXCEPTION?
• fatty acid synthesis involves two ca rbon additions primarily from acetyi-CoA
• the important step in fatty acid synthesis is the fi rst one in which acetyi-CoA, ATP
and bica rbonate form malonyi-CoA
SAADDES
• fatty acid synthesis is not a simple reversal of j:l-oxidation used for the catabo lism of
fatty acids
• fatty acid synthesis takes place in the mitochondria while fatty acid breakdown
(catabolism) occurs in the cytosol (cytoplasm)
217
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• fatty acid synthesis takes place in the mitochondria while fatty
acid breakdown (catabolism) occurs in the cytosol (cytoplasm)
*** This is false; fatty acid synthesis ta kes place in t he cytosol w hile fatty acid
breakdown (catabolism) occurs in the mitochondria.
Remember: Fatty acids are oxidized by the pathway of j:l-oxidation, w hich is active in
the mitochondria of most cells. j:l-oxidation produces acetyi-CoA for the TCA cycle.
On a high-carbohydrate, low-fat d iet, ca rbohydrates are converted into fat by the
sequential action of glycolysis, pyruvate dehydrogenase and fatty acid biosynthesis.
This sequence is most active in the liver. The endogenously synthesized fat is
SAADDES
transported from the liver to adipose tissue in VLDL.
A fat o r triglyceride, contains th ree molecules of fatty acid combined w ith one
molecule of glycerol. A fatty acid is a long-chain com pound with an even number of
ca rbon atoms and a terminal COOH group. Fatty acids can be saturated (no double
bonds), monounsaturated (has one double bond between ca rbon atoms) o r
polyunsaturated (has multiple double bonds between carbon atoms).
The "tail" of a fatty acid is a long hydroca rbon chain, making it hydrophobic. The
"head" of the molecule is a carboxyl group, w hich is hydrophilic. Fatty acids are the
main component of soap, where their ta ils are soluble in oily dirt and their heads are
soluble in water to emulsify and wash away t he oily d irt. However, w hen the head end
is attached to glycerol to form a fat, that w hole molecule is hydrophobi c.
Note: Lipids are organic compounds that do not d issolve in water but do dissolve in
alcohol and other organic solvents. The major lipids include triacylglycerols (the
most common lipids), phospholipids and steroids.
Saad Alqahtani, Twitter @saaddes
lipids
The molecule picture below plays a major role:
• as an energy source
Fatty acid
• as a membrane component
• as a signal mechanism Fatty acid
SAADDES
• two of the above
• all of the above
Fatty acid
218
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• as an energy source (it is a triglyceride)
A triglyceride is a naturally occurring ester of three fatty acids and glycerol that is the chief
constituent of fats and oil s. Triglycerides provide more than half the energy requirements
of so me organs - particularly the liver, heart and skeletal muscle. Note: Triglycerides are
not membrane constituents as are phospholipids and steroids.
Triglycerides play an important role in metabolism as energy sources. Triglycerides
contain twice as much energy (9.3 kcal/g) as carbohydrates (4 kcal/g). In the intestine,
triglycerides are split into glycero l and fatty acids (with the help of lipases and bile
secretions), which can then move into blood vessels. The triglycerides are rebuilt in the
blood from their fragments and become constituents of lipoproteins. Various tissues can
release the free fatty acids and take them up as a source of energy. Fat cell s can synthesize
SAADDES
and store triglycerides. When the body requires fatty acids as an energy source, the
hormone glucagon signals the breakdown of the triglycerides by hormone-sensitive
lipase to release free fatty acids.
Note: The human body is a machine fueled by food. During their oxidation to carbon diox-
ide and water, carbohydrates yield about 4 kcal/g, trig lycerides - 9.3 kcal!g, proteins- be-
tween 4.0 and 4.5 kcal/ g, and alcohol - 7.0 kcal/g. Molecular oxygen is consumed during
oxidative metabolism and carbon dioxide is produced.
Remember: In the human body, high levels of triglycerides in the bloodstream have been
linked to atherosclerosis, and by extension, to the risk of heart disease and stroke.
1. In the triglycerides, all three hydroxyl groups of glycerol are esterified with a
fatty acid.
2. The long hydrocarbon chains of the fatty acid residues ensure that triglycerides
are insoluble in water. In the body, triglycerides minimize contact w ith water by
forming fat droplets.
3. The trig lycerides are used only as a storage form of metabolic energy, but other
lipids serve more specialized functions.
Saad Alqahtani, Twitter @saaddes
lipids
Choline is required for synthesis and release of acetylcholine.
Choline is also a precursor for synthesis of the phospholipids phosphatidyl-
choline (lecithin) and sphingomyelin.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is true
219
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statem e nts are tru e
Choline and carnitine have traditionally been considered as nonessential because they
can be synthesized de novo. However, choline has recently been reclassifi ed as essential
and carnitine as conditionally essential.
Functions of choline:
• Choline is required for synthesis and release of acetylchol ine, an important
neurotransmitter involved in memory storage, muscle contro l and other functions
• It is also a precursor for synthesis of the phospholipids phosphatidylcholine (lecithin)
and sp hingomyelin, which are important for membrane function, intracellular
signaling and hepatic export of very-l ow-density lipoproteins
SAADDES
• Phosphatidylcho line is also important in removal of cholestero l from t issues because
it is a substrate for lecithin-cholesterol acyltransferase in reverse cholesterol transport
• Choline is a precursor for the methyl donor betaine
Note: Because choline can b e synthesized de novo (from phosphatidylserine in
membranes) and is abundant in food, choline deficiency is very rare. However, a
deficiency of cho line in the diet can cause abnormalities in the metabolism of fats and
can lead to fatty liver disease and eventually hepatic cirrhosis.
Carnitine is required for transport of fatty acids across the mitochondrial membrane, so it
is essential for normal fatty acid metabolism. Because carn it ine can be synthesized de novo,
it is nonessential for normal healthy adults. However, it is considered cond itionally essen-
tial because h um an genetic disorders of carnitine metaboli sm have been described and
some of them respond to carn it ine supplementation.
Saad Alqahtani, Twitter @saaddes
lipids
The binding of glucagon to its receptor:
• deactivates adenylate cyclase
• activates adenyl ate cyclase
• causes the breakdown of cyclic AMP to ATP
SAADDES
• causes the production of ATP from cAMP
• deactivates protein kinase
220
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• activates adenylate cyclase
The secretion of glucagon from the pancreatic alpha cells is increased two to threefold
by hypoglycemia and reduced to half of the basal release by hyperglycem ia. Acting
through its second messenger, cyclic AMP (cAMP), g lucagon up-regulates the blood
glucose level when dietary ca rbohydrate is in short supply. Its actions on the pathways
of g lucose metabolism are opposite to those of insulin, but unlike insulin, glucagon
acts almost exclusively on the liver; it has negligible effects on adipose tissue, muscle
and other extrahepatic tissues.
When hormones signal the need for metabolic energy, t ri glycerides stored in adipose
tissue are brought out of storage and transported to those tissues (skeletal muscle,
SAADDES
heart and renal cortex) in which fatty acids can be oxidized for energy production.
Important: The hormones glucagon and epinephrine activate adenyl ate cyclase in
the adipocyte plasma membrane, raising the intracellular concentration of cAMP. A
cAMP-dependent protein kinase in turn, phosphorylates and thereby activates horm-
one-sensitive triacylglycerollipase, which then ini tia lizes the hydrolysis of the ester
linkages of triglycerides- fo rmi ng free fatty acids and glycerol. The fatty acids that are
released bind to serum albumin and travel to the tissues, where the fatty acids dissoc-
iate from albumin and diffuse into the cells in which the fatty acids will serve as fuel.
Note: The glycerol released by t ri acylglycerol lipase action is phosphorylated by
glycerol kinase and the resu lting glycerol-3-phosphate is oxidized to dihydroxy-
acetone phosphate. This compound is then converted to glycera ldehyde-3-phos-
phate by the enzyme triose phosphate isomerase. Glyceraldehyde-3- phosphate is
then oxidized via glycolysis.
Remember: Insulin causes activation of a phosphorylase that dephosphorylates the
hormone sensitive lipase and thereby diminishes lipolysis.
Saad Alqahtani, Twitter @saaddes
metabolism
The electron transport or respiratory chain gets its name from the fact that
electrons are transported to meet up with oxygen from respiration at the
end of the chain. The overall electron chain transport reaction is:
SAADDES
• 2 H++ 2 e+ + 1/ 2 0 2 ~ Hp +energy
• 3 W + 3 e• + 1 0 2 ~ HP + energy
221
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
The majority of the energy conserved during cataboli sm reactions occurs near the end of the
metabolic series of reactions in the electron transport chain (also called the respiratory chain).
Notice that 2 hydrogen ions, 2 electrons and an oxygen molecule react to form as a product
water with energy released in an exothermic reaction.Thi s relatively straight forward reaction
actually requires eight or more steps. The energy released is coupled with the formation of three
ATP molecules per every use of t he electron transport chain.
Four reactions of the tricarboxylic acid (TCA) cycle (aka citric acid cycle or t he Krebs cycle)
transfer electrons to either NAD'" or FAD•. The resulting NADH or FADH 2 is then oxidized by t he
mitochondrial electron transport chain to generate energy that is used to form ATP by
SAADDES
oxidative phosphorylation. Important: The enzymes of the electron transport chain and
those involved in ATP synthesis are exclusively localized in mitochondria.
In summary, the substrate of the TCA cycle is t he two-carbon unit acetyl Co A and the products
of a complete t urn of the cycle are two C0 2, one high-energy phosphate bond (as GTP) and
t hree NADH and one FADH 2. The NADH and FADH 2 are subsequently oxidized by the electron
transport chain with t he production of 10 ATPs.
1. Oxidative phosphorylation occurs in the mitochondrial inner membrane,
8 glycolysis occurs in the cytoplasm and t he TCA cycle occurs in t he mitochondrial
matrix. Remember: Red blood cells do not contain an active mitochondrial electron
transport system.
2. The electron carriers (flavoproteins, iron-sul fur proteins, coenzyme Q and
cytochromes) make up the electron transport syst em. During oxidative
phosphorylation, the proton gradient, created using energy from the electron
transport system, is used to produce ATP. The proton gradient is created by
increasing the proton concentration outside the inner membrane of the
mitochondria.
Saad Alqahtani, Twitter @saaddes
SAADDES (4) 2H" + 2e· (reducing equivalents)
10 ATP
Ge neral description of synthesis of ATP within mitochondria. Acetyi-CoA p roduced by
oxidation of pyruvate and fatty acids is metabolized by the tricarboxylic acid cycle to re -
ducing equiva lents, wh ich are oxidized by the electron trans port system. Energy released
during the oxidative process is used to drive synthesis of ATP.
221-1
Saad Alqahtani, Twitter @saaddes
metabolism
Which complex contains cytochromes b and c 1 and an Fe-S center?
• complex I
• complex II
• complex Ill
• complex IV
SAADDES
222
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• complex Ill
The electron carriers in the respiratory assemb ly of the inner mitochondrial membrane are
quinones, flavins, iron -sulfur co mplexes, hem e groups of cytochrom es and copper ions.
Electrons fro m NADH are transferred to the FMN prosthetic group of NADH-Q oxidoreduc-
tase (Complex 1), the first of four complexes. This oxidoreductase also contains Fe-5 centers.
The electrons emerge in QH 2, the reduced form of ubiquinone (Q). The citric acid cycle en-
zyme succinate dehydrogenase is a component of the succinate-Q reductase com plex
(Complex II), which donates electrons from FADH 2 to Q to form QH 2. This highly mobile hy-
drophobic carrier transfers its electrons to Q-cytochrome c oxidoreductase (Complex Ill ),
a complex that contains cytochromes b and c1 and an Fe -5 center. This com plex reduces
cytochro me c, a water-soluble peripheral membrane protein. Cytochrom e c, like Q is a mo-
SAADDES
bile carrier of electrons, which it then transfers to cytochrome c oxidase (Complex IV). This
complex contains cytochromes a and a 3 and three copper ions. A heme iron ion and a
copper ion in this oxidase transfer electrons to 0 2, the ultimate acceptor, to form H20.
The flow of electrons through Complex I, Ill and IV leads to transfer of protons fro m the ma-
trix side to the cytoplasm side of the inner mitochondrial membrane. A proton-motive force
consisting of a pH gradient (m atrix side basic) and a m embrane potential (matrix side neg-
ative) is generated. The flow of protons back to the matrix side th rough ATP synth ase
drives ATP synthesis.
Important: The flow of two electrons through NADH-Q oxidoreductase, Q-cytochrom e c
oxidoreductase and cytochrome c oxidase generates a gradient sufficient to synthes ize 1,
0.5 and 1 m olecule of ATP, respectively. Hence, 2 .5 molecules of ATP are formed per mol-
ecu le of NADH oxidized in the mitochondrial matrix, whereas on ly 1.5 molecules of ATP
are made per molecule of FADH 2 oxidized, because its electrons enter the chain at QH 2,
after the first proton -pumping site.
Saad Alqahtani, Twitter @saaddes
metabolism
All of the following statements concerning the citric acid cycle (Krebs cycle)
are true EXCEPT one. Which one is the EXCEPTION?
• the cycle starts w ith the 4-carbon compound oxaloacetate, adds 2 carbons from
acetyi-CoA, loses 2 carbons as C0 2 and regenerates the 4-carbon compound oxalo-
acetate
SAADDES
• the pyruvate that enters this cycl e is generated by the glycolysis of glucose or pro-
tein catabolism
• this cycle is controlled by regulation of several enzyme activities. The most import-
ant of these regulated enzymes are citrate synthase, isocitrate dehydrogenase and
a-ketoglutarate dehydrogenase complex
• the enzymes involved in the citric acid cycle are found in the cytoso l
• aspartic acid and oxaloacetic acid are interconvertible
223
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the enzymes involved in the citric acid cycle are found in the cytosol
••• This is false; the enzymes involved in this cycle are found in the mitochondria.
Acotyt CoA
After glycolysis takes
place in the cell's cy-
toplasm, the pyruvic
acid molecules travel Oxaloacotate
NADH~
into the interior of
the mitochondrion .
Once the pyruvic Malate
acid is inside, carbon dehydrogenase
SAADDES r
NAO•
d ioxide is enzymati-
cally removed from
each three -carbon Malate
lsocltrate
pyruvic acid mole- ~
cule to form acetic Citric Acid /soc/Irate NAO'
acid. The enzyme dehydrogenase
then combines the HzO Fumarase
Cycle
NAOH
acetic acid with an • co,
enzyme (coenzyme
A) to produce acetyl
coenzyme A, also Fumarate
known as acetyi-
CoA. Once acetyi- ~~ydrogenase
FADH,
~~~c/nate NAO• + CoASH
CoA is formed, the Succlnyl CoA
Krebs cycle begins. synthetase
FAD Succinate ~~) ~ci,~ PI Succlnyl CoA
~ CoASH
Saad Alqahtani, Twitter @saaddes
metabolism
1. Which of the following is the pace-setting enzyme of glycolysis?
2. Which of the following is the first step to use energy rather than produce it?
3. Which of the following is the enzyme that produces two distinct carbon-based
molecules?
• hexokinase
• phosphog lucose isomerase
SAADDES
• phosphofructokinase
• aldolase
• triose phosphate isomerase
• glyceraldehyde-3-phosphate dehydrogenase
• phosphog lycerate kinase
• phosphog lyceromutase
• enolase
224
• pyruvate kinase copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
1. phosphofructokinase
2. hexokinase (traps glucose into the cell)
3. aldolase
Enz~ mcs ot Gl~ col~ sis
Enzyme Function
Hexokinase Converts glucose into glucosc-6-phosphate
Phosphoglucose isomerase Converts glucosc·6·phosphate into fructosc-6·phosphate
Phosphofruc tokinase Converts fructosc·6·phosphate into fructose I ,6·b isphosphate
Aldolase Converts fructose 1,6·bisphos phate into d ihydroxyacctonc
phosphate and glyceraldehyde 3·phosphate
SAADDES
Triose phosphate isomerase Converts dihydroxyacctone phos phate into glyceraldehyde
3·phospha tc
Glyceraldehyde 3·phosphatc dehydrogenase Converts glyceraldehyde 3·phosphate into
1,3 b isp hosphoglyccrate
Phosphoglycerate kinase Converts I ,3·bisphosphoglyccratc into 3-phosphoglycerate
Phosphoglyccromutasc Converts 3·phosphoglyc.e rate into 2·phosphoglycerate
Enolase Converts 2·phosphoglyc.e rate into phosphoenolpyruvate
Pyruvate kinase Converts phosphoenolpyruvate into pyruvate
Nine reactions, each catalyzed by a specific enzyme, make up the process we call glycolysis. All or-
ganisms have glycolysis occurring in t heir cytoplasm .
At steps 1 and 3, ATP is converted into ADP, inputting energy into the reaction as well as attaching
a phosphate to the glucose. At steps 6 and 9, ADP is converted into the higher energy ATP. At step
5, NAD• is converted into NADH + W.
The end of the glycolysis process yields two pyruvic acid molecules with a net gain of 2 ATP and two
NADH per glucose.
Saad Alqahtani, Twitter @saaddes
metabolism
Which of the following is the metabolic pathway in which there is a shuttling
of glucose and lactate between muscle and liver during physical exercise?
• hydrologic cycle
• cori cycle
SAADDES
• ca rbon cycle
• glucose cycle
225
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• Cori cycle (sometimes referred to as the "lactic acid cycle")
Lactate is released into the blood by cells that lack mitochondria, such as red blood cells, and
by exercising skeletal muscle. In the Cori cycle, blood-borne glucose is converted by exercising
muscle to lactate, which diffuses into the blood. This lactate is taken up by t he liver and
converted to glucose, which is released back into the circulation (see diagram below).
The cycle's importance is based on t he prevention of lactic acidosi s in the muscle under anaer-
obic conditions. The accumulation of lactic acid causes muscle pain and cramps; however, nor-
mally before this happens the lactic acid is moved out of the muscles into the liver.
The cycle is also important in producing ATP, an energy source, during muscle activity. The Cori
cycle functions more efficiently when muscle activity has ceased because t he oxygen debt can
be made up so that t he citric acid cycle and electron transport chain also work.
SAADDES In Liver In Muscle
The Cori cycle. Lactate formed by active muscle is converted into glucose by t he liver.
Thi s cycle shifts part of t he metabolic burden of active muscle to the liver.
Saad Alqahtani, Twitter @saaddes
metabolism
Lactic acid fermentation is a reaction which occurs in cells without or
in cells when is limited.
• nucleoli; C0 2
• mitochond ri a; 0 2
SAADDES
• cytoplasmic granules; W
• mitochond ri a; C0 2
226
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• mitochondria; 0 2
Lactic Acid Fermentat ion:
Reaction occurs in cells w ithout mitochondria (RBC) or in cells when 02 is limited (m uscle
cells during exercise). The entire purpose of th is reaction is to convert the NADH produced
in step 6 of g lycolysis back to NAD• so that glycolysis can continue. This is simp ly a redox
reaction in which pyruvate is reduced to lactate by the enzyme lactate dehydrogenase.
Pyruvate ~===== Lactate
NADH + H· NAD•
SAADDES
Lactate can then enter the bloodstream and travel to the liver where it is converted back
to g lucose through the g luconeogenesis pathway.
Conversion of Pyruvate to Acetyi-CoA:
Much more energy can be obtained from glucose if it is oxid ized com pletely to C02 and H20
through the TCA cycle and electron transport system (requires 0 2 and mitochondria). The
entry to the TCA cycle is through acetyi-CoA. Pyruvate is converted into acetyi-CoA by the
enzyme pyruvate dehydrogenase (multi-enzyme complex) which is located inside the mi-
tochondria.
NADH
NU coenzymeA
Pyruvate ~\
.---_ _ _\_,_.,~ Acetyl CoA
C02
Saad Alqahtani, Twitter @saaddes
Glycolysis splits one molecule
of glucose (six carbon atoms)
into two molecules of pyruvic
acid (three carbon atoms each).
The glyco lytic pathway does
not require oxygen, so it is
termed anaerobic. A transition
reaction removes a carbon
dioxide molecule, converting
each pyruvic acid molecule into
a two-carbon acetyl group that
SAADDES
is escorted by coenzyme A
(CoA) into the citric acid cycle.
There, two more carbon diox-
ide molecules (one carbon
atom each) are released. The
carbon and oxygen atoms in
the original glucose molecule
are thus released as waste
products. However, the real
metabolic prize is energy,
which is released as the mole-
cu le is broken down. Because
th is part of the pathway re-
quires oxygen, it is termed aer-
obic.
226·1
Catabolism of Glucose
Saad Alqahtani, Twitter @saaddes
metabolism
The most common pathway of glycolysis is:
• the Entner-Doudoroff pathway
• the Embden-Meyerhof pathway
• the Pentose Phosphate pathway
SAADDES
• the Urea pathway
227
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the Embden-Meyerhof pathway
The Embden-Meyerhof pathway is a specific glycolytic pathway by which glucose is
converted to pyruvate. This is t he most common pathway and is used by a large
number of anaerobic and facu ltatively anaerobic bacteria. Important: Oral bacteria
use this pathway. The pyruvate is reduced to lactic acid via fermentation. This lactic
acid is cariogenic. Note: This glycolytic pathway resu lts in the net production of 2
ATP molecules per molecule of g lucose metabolized.
The Entner-Doudoroff pathway is an alternative to glycolysis used by many
obligate aerobic bacteria. It results in the net production of only one ATP molecule
SAADDES
per molecule of glucose metabolized by substrate level phosphorylation compared
to the 2 formed in the Embden-Meyerhof pathway. The pathway ends w ith the
formation of a pyruvate and a g lyceraldehyde-3-phosphate (which is converted by
enzymes outside the pathway to pyruvate). Note: These bacteria lack either of the
key enzymes 6-phosphofructokinase or aldolase of the Embden-Meyerhof
pathway.
The pentose phosphate pathway (also called the pentose shunt, the hexose
monophosphate pathway or the phosphogluconate pathway) is a pathway of hexose
oxidation whereby glucose-6-phosphate generates five-carbon sugars. This pathway
plays a major role in generating reducing equivalents, in the form of NADPH, fo r
reductive biosynthesis reactions w ithin cells (e.g., fatty acid synthesis, steroid
synthesis).
Saad Alqahtani, Twitter @saaddes
metabolism
All of the follow ing are characteristic of the pentose phosphate pathway
EXCEPT one. Which one is the EXCEPTION?
• it produces C02
• it is controlled by inhib ition of glucose 6-phosphate dehydrogenase by NADPH
SAADDES
• it requires ATP fo r phosphorylation
• it produces ribose 5-phosphate
• it involves the breakage and formation of C-C bonds
228
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• it requires ATP for phosphorylation
The pentose phosphate pathway consists of two irreversible oxidative reactions, followed by a
series of reversible sugar-phosphate interconversions. No ATP is directly consumed or produced in
the cycle. Ca rbon 1 of glucose 6-phosphate is released as C0 2, and two NADPH are produced for
each glucose 6-phosphate entering the oxidative part of the pathway. Unlike glycolysis or the citric
acid cycle in which the direction of the react ions is well defined, the interconversion reactions of the
pentose phosphate pathway can function in several different directions. The rate and direction of
the reactions at any given time are determined by the supply of and demand for intermediates in
the cycle.
Important: The pentose phosphate pathway occurs in the cytosol of the cell. The pathway provides
a major portion of the cell's NADPH, which functions as a biochemical reductant. The pathway also
SAADDES
produces ribose-5-phosphate, required for biosynthesis of nucleotides, and providesa mechanism
for the metabolic uti lization of five-carbon sugars ingested as food.
1. The oxidative branch of this pathway is concerned with the synthesis of NADPH.
Glucose-6-phosphate dehydrogenase catalyzes the committed and rate-limiting step.
This enzyme is regulated by availability of the substrate NADP•. This reaction sequence is
irreversible.
2. The nonoxidative branch of this pathway links ribulose-5-phosphate, the product of
the oxidative branch, to the glycolytic and gluconeogenic pathways. The most important
enzymes in this reversible reaction sequence are transketolase and transaldolase.
3. Pentose phosphate pathway activity is minimal in muscle and the brain in which
almost all the glucose is degraded by glycolysis. It is particularly important in liver and
mammary glands, which are active in the biosynthesis of fatty acid s, and in the adrenal
cortex, which is active in the NADPH-dependent synthesis of steroid s.
4. Th is pathway is also important in cells that are exposed to a high oxygen partial
pressure. In the cornea of the eye for example, it accounts for 60% of the total glucose
consu mption.
5. Increased consumption of NADPH results in an increased act ivity of the oxidative
branch.
Saad Alqahtani, Twitter @saaddes
Glusose 6-phosphate G6-P
Ribulose 5-phosphate
NAOP• ~
1
Phosphopentose / ' - Ph~sphopentose
Glucose 6-phosphate tsomerase / ' eptmerase
NADPH + w dehydrogenase
Ribose s-phosphate x xylulose
5-phosphat
i '""""'
6-Phosphogluconolactone Transketolase
Glyceraldehyde
3-phosphate
(G3·P) . E Sedo7-P
SAADDES
H,o lase
Ery-4-P ~
6-Phosphogluconate Transketolase
~~~:~ons r
~
uctose 6-p.h ospha,P)-- G/f;.p
NAD::::. 6-Phosphog/uconate
dehydrogenase glycolysis G6·P /
C02 Nonoxidativc portion {reversible)
T his ponion rearranges the sugars so they can
Ribulose 5-phosphate
reenter the glycolytic pathway.
Oxidative portion (not rever.<ible)
This poni on generates NADPH, wh ich is
needed for biosynthetic pathways such as
fatty acid and cholesterol synthesis.
2211·1
This pentose phosphate pathway may function as an alternate form of glycolysis or may be the
route for the complete oxidation of glucose (it begins with glucose 6-phosphate).
Saad Alqahtani, Twitter @saaddes
metabolism
Oxidative phosphorylation is the major source of ATP in aerobic organisms.
The generation of GTP from succinyl CoA is an example of substrate level-
phosphorylation in which the production of high-energy phosphate is
coupled to the conversion of substrate to product, rather than resulting
from oxidative phosphorylation.
SAADDES
• both statements are true
• both statements are false
• the first statement is true, the second is fa lse
• the first statement is fa lse, the second is t rue
229
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statem ents are true
The t hree main t ypes of phosphorylation:
• Substrate-level phosphorylation: high-energy phosphate intermediates are formed
and are transferred to ADP to produce ATP. Examples of th is are found in glycolysis and
the citric acid cycle (Krebs cycle). Glycolysis is the fi rst phase and the citric acid cycle
is the second phase of the res piratory metaboli sm of glucose.
• Electron-transport/ oxidative phosphorylation: electrons move down the electron
transport chain and chemios mosis occurs. Because the electrochemical gradient gen-
erated by the transfer of electrons through the electron transport chain to 0 2 is used in
the production of ATP, the overall process is known as electron transport/oxidative
SAADDES
phosphorylation. It is the third and final phase of respiratory metabolism of glu-
cose and other substrates. Reduced coenzymes (NADH and FADH 2 ) generated earlier
in glyco lysis and the Krebs cycle are reoxidized; the electrons these processes release
are transported through a series of membrane bound carriers (flavoproteins, iron-sulfur
proteins, coenzyme Q and cytochromes) to establish a proton gradient across a mem-
brane, a terminal acceptor such as ox ygen is reduced, and ATP is synthesized by
chemiosmosis.
Note: Oxidative phosphorylation is the major source of ATP in aerobic organism s.
• Photophosphorylation: occurs as a result of photosynthesis (which also involves an
electron trans port chain)
Note: Oxygen u ptake, which is dependent on the presence of ADP, phosphate and an
electron donor, is termed coupled respiration.
Saad Alqahtani, Twitter @saaddes
metabolism
Theoretically, in most human cells, one glucose molecule produces enough
usable chemical energy to synthesize:
• 30-32 ATP molecules
• 32-34 ATP molecules
SAADDES
• 36-38 ATP molecules
• 44-48 ATP molecules
230
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• 36-38 ATP mol e cul es
***Some cells, such as heart and liver cells, shuttle electrons more efficiently and may be
able to synt hesize up to 38 ATP m olecul es.
A net profit of 4 ATP is p roduced by substrate -level phosphorylation during glycolysis
(2 ATP) and the Krebs cycle (2 ATP) and 32-34 ATP are produced by oxidative phosphory-
lation during electron transport.
ATP Derived from Glucose
1. No 0 2 ava ilable o r no mitochond ria:
Glucose + 2Pi + 2ADP ~ 2 lactate+ 2 ATP + H 20
Glucose m ust be converted to lactate, 2 ATP produced.
SAADDES
2. Complete oxidation of Glucose to C0 2 and H 20
Conversion Products ATPformed
Glucose~ 2 Pyruvate 2ATP 2ATP
2NADH 4 ATP (a-GP shuttle) or 6 ATP (M-A shuttle)
2 Pyruvate ~ 2 acetyi-CoA 2NADH 6ATP
2 acetyi-CoA into TCA cycle 2GTP 2ATP
6NADH 18ATP
2 FADH2 i.AIL
36 or 38ATP
Important: A Na• gradient across the luminal m embrane provides the imm ediate energy
sou rce for the transport of glucose into intestinal epithelial cells.
Note: Theoretically, 36-38 ATP per g lucose m olecul e is possible. In reality, cell s only p ro-
duce 30 -32 ATP per g lucose because each NADH produces 2.5 ATP (not the theoretical3
ATP) and FADH 2 produces 1.5 ATP (not the theoretical 2 ATP).
Saad Alqahtani, Twitter @saaddes
metabolism
Gluconeogenesis is the reverse of glycolysis.
Gluconeogenesis produces glucose from amino acids, lactate and glycerol.
• both statements are true
SAADDES
• both statements are false
• the first statement is t rue, the second is false
• the first statement is fa lse, the second is true
231
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
Gluconeogenesis produces glucose from amino acid s, lactate and glycerol. This pathway uses
the reversible reactions of glycolysis while bypassing the irreversible ones. It is the only source
of glucose during long-term fasting. Only the liver and kidneys have a complete gluconeogenic
pathway.
Gluconeogenesis is a pathway consisting of 11 enzyme-catalyzed reactions and involves the fol-
lowing key steps:
• Gluconeogenesis begins in the mitochondria with the formation of oxaloacetate through
carboxylation of pyruvate at the expense of one molecule of ATP. This reaction is catalyzed by
pyruvate carboxylase, which is stimulated by high levels of acetyi-CoA (when fatty acid ox-
idation is high in the liver) and inhibited by high levels of ADP.
SAADDES
• Oxaloacetate must then be reduced into maltate using NADH in order to be transported
out of the mitochondria.
• In the cytoplasm, malate is oxidized to oxaloacetate using NAD•, where the remaining
steps of gluconeogenesis occur.
• Oxaloacetate is then decarboxylated and phosphorylated to produce phosphoenolpyru-
vate by phosphoenolpyruvate carboxykinase. One molecule of GTP is hydrolyzed to GDP
in the course of thi s reaction.
• The next steps in the reaction are the same as reversed g lycolysis. However, fructose-1,6-
bisphosphatase converts fructose-1,6-bisposphate to fructose-6-phosphate. The purpose of
this reaction is to overcome the large negative .C.G.
• Glucose-6-phosphate is formed from fructose-6-phosphate by phosphoglucoisomerase.
Glucose-6-phosphate can then be used for glucose generation or in other metabolic path-
ways. Free glucose is not generated automatically because glucose, unlike glucose-6-phos-
phate, tends to freely diffuse out of the cell.
• The final reaction of gluconeogenesis, the formation of glucose, is then carried out in the
lumen of the endoplasmic reticulum. Glucose-6-phosphate is hydrolyzed by glucose-6-phos-
phatase to produce glucose. Glucose is then shuttled into the cytosol by glucose transporters
located in the membrane of the endoplasmic reticulum.
Saad Alqahtani, Twitter @saaddes
metabolism
Which of the following cells in the body metabolize glucose only through
anaerobic pathways?
• muscle cells
• red blood cells
SAADDES
• hepatocytes
• neural cells
232
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• red blood cells
***Though they are never really in an oxygen-deprived environment, they do not have mito-
chondria and t herefore cannot send pyruvate to the citric acid cycle.
The oxidation of g lucose to pyruvate is known as glycolysis. Pyruvate is then either oxidized to
acetyi-CoA or reduced to lactic acid. Under aerobic conditions, the fate of pyruvate in most tis-
sues is oxidation to acetyi-CoA via the pyruvate dehydrogenase enzyme in the mitochon-
d ria. When oxygen is depleted, as for instance during prolonged vigorous exercise, t he fate of
pyruvate in many tissues is reduction to lactate (lactic acid) via the lactate dehydrogenase en-
zyme in t he cytosol and the process is known as lactic acid ferm entation.
Glycolysis occurs in the cytosol of all cells in the body. Glycolysis starts with a molecule of
SAADDES
glucose and then performs 10 stepwise chemical t ransformations. During thi s process, the
sugar molecule is primed with two phosphates (using up two ATP molecules), then broken in-
to two pieces, and finally reshaped and dehydrated, forming four ATP molecules in the process.
Overall, glycolysis builds two new ATP molecules using the energy of th is partial breakdown
of sugar. The ATP may then be used to power molecular processes throughout the cell. In
addition, one step in glycolysis also extracts four hydrogen atoms from the sugar molecule,
which may be used for biosynthesis or to create addi tional chemical energy.
Pyruvate is the end product o f glycolysis in cells with mitochondria and an adeq uate supply
of oxygen. This series of 10 reactions is called aerobic glycolysis because oxygen is required
to reoxidize the NADH formed during the oxidation of glyceraldehyde-3-phosphate. Aerobic
glycolysis sets the stage for the oxidative decarboxylation of pyruvate to acetyi-CoA, a major
fuel of the citric acid cycle.
Alternatively, glucose can be converted to pyruvate, which is red uced by NADH to form lactate.
This conversion is called anaerobic glycolysis because there is no net formation of NADH and
t herefore, this conversion can occur in the absence of oxygen. Anaerobic glycolysis allows the
production of ATP in tissues that lack mitochondria (for example, red blood cells) or in cells
deprived of sufficient oxygen.
Saad Alqahtani, Twitter @saaddes
substances
The common precursor of all three aromatic amino acids is:
• chorismate
• phosphoenolpyruvate
• shikimate
SAADDES
• ribose 5-phosphate
233
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• chorismate
Among the essential amino acids, t he aromatic amino acids (phenylalanine, tyrosine
and tryptophan) form by a pathway in which chorismate occupies a key branch point.
Tyrosine is not essential to t he human d iet, since this amino acid can be synthesized
in the body from phenylalanine. Tyrosine is a precursor of t he adrenal hormones
epinephrine and norepinephrine as wel l as of the thyroid hormones, including
thyroxine. Tyrosine is also the precursor to the neurotransmitter dopamine. Melanin,
the skin and hair pigment, is also derived from th is amino acid.
_...Tryptophan ~ Serotonin
SAADDES
Chorismate
"'-
Prephenate
-
t
Tyrosine - Dopa - Dopamine ....,Norepinephrine ._Epinephrine
~Phenylalanine
Remember: Serotonin (also ca lled 5-hydroxytryptamine) is synthesized from the
amino acid tryptophan. Serotonin is released from platelets upon damage to the
blood vessel wa lls. Serotonin acts as a potent vasoconstrictor and increases vascular
peripheral resistance. In gastric mucous membranes, serotonin is secreted by the
enteroendocrine cells and causes the smooth muscle to contract. In the brain,
serotonin acts as a neurotransmitter.
Note: Lysergic acid diethylamide interferes w ith the action of serotonin in the brain.
Saad Alqahtani, Twitter @saaddes
substances
A patient of yours fails to tell you about his or her allergy to latex. You walk
into the room and begin treatment. The allergic reaction presenting causes
histamine release. All of the following are responses to this EXCEPT one.
Which one is the EXCEPTION?
• vasod ilation (particularly the arterioles)
SAADDES
• secretion of HC L
• bronchoconstriction
• increased blood pressure
• increased vascu lar permeability (particularly in capillaries and venu les)
234
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• increased blood p ressure
*** This is false; histamine causes decreased blood pressure.
As a maj or mediator of allergic res ponses, histamine is released by circulating basophils
and their sedentary cousins, the mast cells. Histamine dilates small b lood vessels,
increases capillary permeability, contracts bronchial and intestinal smooth muscle,
stimulates gastric secretion and nasal fluid discharge and regulates the cells of the
immune system.
Histamine is an important protein involved in many allergic reactions. Allergies are caused
by an immune response to a normally innocuous substance (i.e., pollen, dust) that co mes
in contact with lymphocytes specific for that substance, or antigen. In many cases, the
lymphocyte triggered to res pond is a ma st cell. For this response to occur, a free-floating
SAADDES
lgE (an immunoglobulin associated w ith allergic response) molecule specific to the
antigen must first be attached to cell surface receptors on mast cells. Antigen b inding to
the mast cell-attached lgE then triggers the mast cell to respond or become activated.
(Note: Degranulation describes the action of the mast cell when it is activated.) This
response often includes the release of histamine. Th is increases the local blood flow and
increases the permeability of the capillaries and venules, all owing large quantities of fl uid
and protein to leak into the tissues (the characteristic "wheal").
Histamine has powerful pharmacologic action s, wh ich are mediated by two specific
receptor types:
1. H1 receptors mediate the typical allergic and anaphylactic responses to hista-
mine (e.g., bronchoconstriction, vasodilation and increased capillary permeability).
2. H2 receptors mediate other responses to histamine, such as the increased secretion
of gastric acid and pepsin.
Import ant: The actions of bradykinin (a vasodi lating kinin) are simi lar to h istamine.
Bradykinin increases vascu lar permeability, dilates b lood vessels and causes the t issue
swell ing associated with inflamm ation.
Saad Alqahtani, Twitter @saaddes
substances
All of the following statements concerning heparin are true EXCEPT one.
Which one is the EXCEPTION?
• unlike other g lycosaminoglycans that are extracellular compounds, heparin is an
intracellular component of mast cells that line arteri es, especiall y in the liver, lungs
and skin
SAADDES
• it serves as a powerful anticoagulant
• it is used in the treatment of certa in types of lung, blood vessel and heart disorders,
and during or after certain types of surgery (open heart or bypass surgeries)
• small quantities are produced by basophil cells of the blood
• it is usually found in large quantities in the blood
235
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• it is usually found in large quantities in the blood
***This is false; its concentration in the blood is normally slight, so that only under
limited physiologica l conditions does heparin have significant anticoagu lant effects.
Heparin is conta ined in secretory vesicles or granules within mast cells and the
basophil cells of the blood, wh ich are functionally almost identical to the mast cells.
Heparin occurs in greatest concentration in the tissues surrounding the capillaries of
the lungs and the liver.
Hepari n is a naturally occurring sulfated glycosaminoglycan that is used to reduce clot-
SAADDES
ting tendency of patients. Both in vivo and in vitro, hepari n prevents the activation of
clotting factors by binding with an inhibitor of the coagu lation process. The inhibitor
is antithrombin Ill, a plasma protein inhibitor of serine proteases. In the absence of
heparin, antithrombin Ill slowly (10-30 m in) combines with several clotting factors,
yielding complexes devoid of proteolytic activity; in the presence of heparin, inac-
tive complexes are formed within a few seconds. Note: Antith rombin Ill conta ins an
arginine residue t hat combines with t he active site serine of factors Xa and IXa; thus
the inhibition is stoichiometric.
1. Heparin prevents the activation of factor IX (Christmas factor) and inter-
B feres w ith thrombin action.
2. Heparin can also enhance t he removal of lipoproteins from the blood by
binding apolipoprotein E (protein found on some liposomes) and by activat-
ing lipoprotein lipase.
Saad Alqahtani, Twitter @saaddes
substances
An apprehensive dental patient comes in and states that he already took
ibuprofen for the pain he anticipates from the appointment today. As you
know, this inhibits the synthesis of prostaglandins. All of the following
statements are true about prostaglandins EXCEPT one. Which one is the
EXCEPTION?
• they have a very short half-life
SAADDES
• they generally act locally on or near the tissue that produced them
• they are synthesized only in the liver and the adrenal cortex
• the common precursor of prostaglandins is arachidonic acid (an unsaturated fatty
acid)
• thei r synthesis can be inhibited by a number of unrelated compounds, including
aspirin and cortisol
236
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• they are synthesized only in the liver and the adrenal cortex
***This is false; prostaglandins are synthesized by a broad variety of tissues.
Prostaglandins are any of a group of components derived from unsaturated 20-carbon fatty
acids, primarily arachidonic acid, via the cyclooxygenase pathway; prostaglandins are potent
mediators of numerous d ifferent physiologic processes. Prostaglandins belong to a subcl ass of
lipids known as the eicosanoids (along with t hromboxanes and leukotrienes) because of t heir
structural similarities to the C-20 polyunsaturated fatty acids, the eicosanoic acids. In general,
prostagland ins act in a manner similar to that of hormones, by stimulating target cells into
action. However, prostaglandins differ from hormones in that they act locally, near their site
of synthesis and they are metabolized very rapidly. Also the same prostaglandins act
SAADDES
d ifferently in different t issues. Prostaglandins are 20-carbon fatty acids that contain a five-
carbon ri ng.
Prostaglandins are synthesized in the cell from arachidonic acid mobilized by phospholipase
A2. The intermediate is then passed into one of either the cyclooxygenase or lipoxygenase
pathways to form either prostaglandins and thromboxanes or leukotrienes. The cyclooxygen-
ase pathway produces thromboxanes, prostacycl ins and prostaglandins D, E and F. The lip-
oxygenase pathway is active in leukocytes and in macrophages and prod uces leukotrienes.
Prostaglandins are released through the prostaglandin transporter on t he cell's plasma
membrane.
1. Prostaglandins seem to modulate the action of hormones rather than act as hor-
mones themselves.
2. Aspi rin, indomethacin, ibuprofen and phenylbutazone, which are NSAIDs, inhibit
the biosynthesis of prostaglandins by interfering with the enzyme cyclooxygenase,
the enzyme that initiates the formation of prostaglandins from arachidonic acid.
3. Prostaglandins enhance inflammatory effects, whereas aspiri n diminishes them.
Saad Alqahtani, Twitter @saaddes
substances
All of the following are formed via the cyclooxygenase pathway EXCEPT one.
Which one is the EXCEPTION?
• prostaglandins
• prostacyclin
SAADDES
• leukotrienes
• thromboxanes
237
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• leukotrienes
The prostaglandins and a number of related substances (prostacyclin, thromboxanes
and leukotrienes) are chem ica l messengers. One of these messengers is present in
almost every body t issue. They act primarily as local messengers that exert their
effects in the tissues that synthesize prostaglandins.
Note: Leukotrienes are potent bronchoconstrictors and cause airway wall edema,
increasing mucus production. They also attract eosinophils into the tissues and
amplify the inflammatory process.
Arachidonic acid (an unsaturated fatty acid) is the major compound from wh ich
prostaglandins, prostacyclin, th romboxanes and leukotri enes are derived. Arachidon-
SAADDES
ic acid is a part of phospholipids in the plasma membranes of cells. Va ri ous com-
pounds activate a plasma membrane enzyme ca lled phospholipase A2 , and th is en-
zyme splits arachidonic acid from the membrane phospholipids.
Different metabolic pathways utilize different enzymes that convert arachidonic
acid into the different messengers:
• To form prostaglandins, prostacyclin or thromboxanes, the cyclooxygenase
pathway utilizes the enzyme cyclooxygenase
• To form leukotrienes, the lipoxygenase pathway utilizes the enzyme lipoxygen-
ase
Note: Many NSAIDs including aspirin, block the cyclooxygenase pathway. The benefit
of th is blockade comes from the ability to slow the synthesis of prostaglandins, thus
reducing their inflammatory ability.
Remember: Prostacyclin is a prostaglandin produced in the walls of blood vessels
that acts as a vasodilator and inhibits platelet aggregation.
Saad Alqahtani, Twitter @saaddes
liver
The liver synthesizes all of the so-called nonessential amino acids.
The liver plays an important role in glucose metabolism by engaging in
gluconeogenesis.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is t rue, the second is fa lse
• the first statement is fa lse, the second is true
238
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Hepatocytes (liver cells) are metabolic super-achievers in the body. Their fu nctions include the
following:
• Hepatocytes contribute to metabolism of the major nutrients: carbohydrates, lipids and pro-
teins. Thus, the liver plays an important role in glucose metabolism by engaging in gluconeogen-
esis, the conversion of the sugars to glucose. The liver also stores glucose as glycogen at times of
glucose excess (such as in the postprandial period) and then releases stored glucose into the
bloodstream as it is needed. This process is referred to as the "glucose buffer function of the
liver:'
• Hepatocytes also participate in lipid metabolism. They are a particularly rich source of the meta-
bolic enzymes engaged in fatty acid oxidation to supply energy for other body functions. Hep-
atocytes also convert products of carbohydrate metabolism to lipids that can be stored in adipose
SAADDES
tissue and synthesize large quantities of lipoproteins, cholesterol and phospholipids. In addition,
hepatocytes convert a considerable portion of synthesized cholesterol to bile acid s.
• The liver also plays a vital role in protein metabolism. The liver synthesizes all of the nonessent-
ial amino acids. With the exception of immunoglobulins, the liver synthesizes almost all of the
proteins present in plasma, especially albumin, which determines plasma oncotic pressure, as
well as most of the important clotting factors.
• The liver is the critical site for disposal of the ammonia generated from protein catabolism. This
is accomplished by converting ammonia to urea, which can then be excreted by the kidneys.
• The liver also serves as a gatekeeper, by limiting the entry of toxic substances into the blood-
st ream, and as a garbage disposal, by extracting potentially toxic metabolic products produced
elsewhere in the body and converting them to chemical forms that can be excreted. Note: The
liver fulfills these fu nctions in part, because of its unusual blood supply. Unlike all other organs,
the majority of blood arriving at the liver is venous in nature and is supplied by the portal vein
from the intestine.
Note: The nonessential amino acids ca n all be synthesized in the liver. To do this for most amino
acids, an a -keto acid having the same chemical composition (except at the keto oxygen) as that of
the amino acid is first synthesized. Then the amino radica l is transferred through transamination
from an available amino acid to the keto acid to take the place of the keto oxygen.
Saad Alqahtani, Twitter @saaddes
liver
In a cotton-candy-eating competition, you consume 14 moderately sized
and overpriced bags of threaded sugar. This causes your portal vein to
drop tremendous loads of glucose to your hepatocytes soon after. Which of
the following enzymes functions only when this happens?
• pyruvate kinase
SAADDES
• glucokinase
• phosphofructokinase
• hexokinase
239
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• glucokinase
Glucokinase is the liver isoenzyme of hexokinase. Like hexokinase, glucokinase catalyzes
the ATP-dependent phosphorylation of glucose to form glucose-6-phosphate (G6P) and
ADP. This is the first step of glycolysis. The enzyme w ill act on a variety of 6-carbon sugars,
producing moieties phosphorylated at position six.
The most important kinetic difference between glucokinase and the other isoenzymes of
hexokinase is the Michaelis Menten constant (I<,) for glucose. Whereas the other forms
of hexokinase have Km values near 0.1 mmol/ liter (2 mg/dl), glucokinase has a Km near 10
mmol/liter (200 mg/dl). Note: Th is difference is very important in the liver, which is a major
source of glucose from gluconeogenesis.
SAADDES
By phosphorylating glucose, glucokinase creates glucose -6-phosp hate. Glucose-
6-phosphate can then be used by the l iver through the glycolytic p athway. Along
with th is process in the liver, glucokinase also facilitates glycogen synthesis. Through
th is, the majority of the body's glucose is stored.
1. Glucokinase is inhibited by the CoA-th ioesters of long -chain fatty acids. These
products are most abundant during fasting, when the liver metabolizes large
amounts of fatty acids from adipose tissue.
2. Glucokinase is not involved in the process of gluconeogenesis. Instead, the
enzyme glucose-6-phosphatase catalyzes the hydrolysis of glucose-6-phos-
phate to glucose and phosphate.
3. Glucokinase is also the predominant enzyme for the phosphorylation of gluc-
ose in beta cells of the pancreas.
4. Other tissues use hexokinase to do the same thing as glucokinase.
5. Hexokinase, phosphofructokinase and pyruvate kinase are the three regula-
tory enzymes of glycolysis.
Saad Alqahtani, Twitter @saaddes
liver
The liver releases glucose back into the circulating blood during exercise.
Which organs take up this extra glucose?
Select all that apply.
• kidneys
SAADDES
• muscle
• heart
• brain
•lungs
240
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• muscle
• brain
Glucose Facts:
• Main fuel source of brain. The brain uses about 120 g of glucose per day.
Only fuel source for red blood cells, cornea, lens (because these cells have no mitochondria).
Kidney, medulla, testes, leukocytes, white muscle fibers use a lot of glucose because these cells
have very few mitochondria.
• Starch is the storage form of glucose in plants, and glycogen is the storage form of glucose in an-
imals. The liver and the muscles are the main storage sites for glycogen. We only store enough
glycogen to survive on for about 1 day.
• The body maintains a constant level of glucose in the blood.
1) Ingest glucose
SAADDES
2) Glucose passes through cells of intestinal tract and enters portal blood ~bloodstream
3) Pancreas monitors the level of glucose in the bloodstream and produces hormone regulators
of blood glucose levels
• levels too low, produces glucagon which signals the liver to put more glucose into the blood
stream
•levels too high, produces insulin which signals cells to increase uptake of glucose and sig-
nals liver to take in glucose and store it as glycogen
The liver releases glucose into the blood during muscular activity and in the interval between
meals. The released glucose is derived from two sources:
(1) The breakdown of stored glycogen
(2) The formation of new glucose by the process of gluconeogenesis
1.1n skeletal muscle, the glucose is phosphorylated and then degraded by glycolysis to
8 pyruvate, which is converted to acetyi-CoA and oxidized via the citric acid cycle.
2. Glucose is the major end product of carbohydrate ingestion.
3. The presence of glucose in the urine proves a person has exceeded his or her renal
threshold for glucose.
4. Fasting leads to decreased liver glycogen.
Saad Alqahtani, Twitter @saaddes
liver
One of the two nitrogen atoms in urea comes from ammonia via carbamoyl
phosphate; and the other from:
• valine
• glycine
SAADDES
• aspartate
• isoleucine
241
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• aspartate
..,.* The aspartate nitrogen is derived either from ammonia, through the glutamate dehydrogenase
reaction followed by transamination with oxaloacetate, or directly from transa mination reactions.
Most amino acid catabolism takes place in the liver. The liver is also the only import ant site for
ammonia detoxification in the urea cycle. One of the substrates of the urea cycle is carbamoyl
phosphate, which is synthesized from ammonia, carbon dioxide and ATP.
The use of two ATP molecules makes this reaction irreversible. The carbamoyl phosphate synthetase
catalyzi ng this reaction requires N-acetylglutamate as an activator. This regulatory metabolite is
formed by a separate enzyme from glutamate and acetyi·CoA. Carbamoyl phosphate synthetase is
abundant in liver mitochondria and its Michaelis Menten constant (Kml for ammonia (250 mmol/liter)
SAADDES
is much higher than the physiological ammonia concentration (30 to 60 mmol/liter). Therefore, it can
maintain ammonia at th is low level.
1. The synthesis of one urea molecule requires four high-energy phosphate bonds. Two
ATP molecules are converted to ADP in the ca rbamoyl phosphate synthetase reaction and
another t wo phosphate bonds are consumed for the formation of argininosuccinate when
one ATP molecule is hydrolyzed to AMP and inorganic pyrophosphate.
2. The two nitrogens enter the urea cycle as ammonia and aspartate.
3. Urea is produced by the hydrolysis of arginine.
4. The urea cycle occurs partly in the mitochondria.
5. A complete block of any step in t he urea cycle is fatal since there is no known alternative
pathway for the synthesis of urea.
6.1nherited disorders from defective enzymes may cause a partia l block in some of there-
actions and results in hyperammonemia, which can lead to mental retardation.
7. Extensive ammonia accumulation leads to extensive liver damage and death.
8. Liver cirrhosiscaused by alcoholism creates an interference in the enzymes that produce
carbamoyl phosphate in the first step in the cycle.
9. The level of nonprotein nitrogen in the blood is due primarily to the level of urea.
10. Death from advanced liver disease is primari ly due to the inhibition of urea synthesis.
Saad Alqahtani, Twitter @saaddes
2 ATP
2 AOP
+Pi
l
NH; + C02
Carbomoy/
phosphate
synthase/
(mitochondria)
Pi1
Citrulline
The Urea Cycle
Aspartate
Arglnlnosucc/nate
synthetase
(cytosol)
ATP AMP+ PPi
Carbamoyl . Vorntth/ne transcarbamoytase
phosphate ~(mitochondra)
SAADDES
Ornithine Arglnlnosucclnate
lyase
(cytosol)
Arginase
cytosol)
Fumarate
H20 Arginine
Urea
Degrades amino acids into a mino groups. Accounts for 90% of nitrogen in urine.Urea
cycle occurs in the liver, carbamoyl phosphate incorporation occurs in the mitochondria;
the remaining steps occur in the cytosol.
241-1
Saad Alqahtani, Twitter @saaddes
liver
The major regulatory enzyme of cholesterol synthesis is:
• thiolase
• HMG-CoA reductase
• HMG-CoA synthase
SAADDES
• HMG-CoA kinase
242
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• HMG-CoA reductase
Although cholesterol is synthesized in most tissues of the body, where cholesterol
serves as a component of cell membranes, it is produced mainly in the liver.
Cholesterol is synthesized from acetyi-CoA; key intermediates in cholesterol
biosynthesis are HMG-CoA, mevalonic acid, isopentenyl pyrophosphate and
squalene.
In the liver, bile salts are fo rmed from cholesterol; in certain endocrine tissues,
cholesterol is converted to steroid hormones (e.g., testosterone, cortisol, progester-
one, and estradiol [which is the most potent naturally occurring human estrogen]).
SAADDES
Vitamin D is also formed from cholesterol by a series of reactions requiring the skin,
liver, and kidney.
1. Cholesterol absorption depends upon the presence of bile salts in the
8 intestinal lumen.
2. Cholesterol is mostly esterified with fatty acids when circu lating in
blood plasma.
3. Circu lating cholesterol is taken up into liver cells where it inhibits synthe-
sis of additional cholestero l from acetyi-CoA via allosteric inhibition of HMG-
CoA reductase.
*** This provides an intrinsic feedback control system to reduce excess
cholesterol synthesis.
4. Thiolase and HMG-CoA synthase are both involved in the synthesis of chol-
esterol. The reactions these enzymes catalyze are reversible and do not com-
m it the cell to the synthesis of cholesterol.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Which of the following is a cofactor required for the hydroxylation of lysine
and proline?
• riboflavin
• vitamin E
SAADDES
• vitamin C
• folacin
243
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• vitamin C
Summar~ of\ ita min C
Dietary Sources Citrus fruits, tomatoes, green peppers, broccoli, spinach,
strawberries, melon
Major Body Functions • Synthesis of connective tissues. Essential for the
hydroxylation of lysine and proline in collagen
synthesis
• Essential for integrity for capillaries and oral mucosa
•
SAADDES
Needed for normal bone matrix formation
• Needed for normal phagocytic function and ant ibody
synthesis in host defense system
Deficiency • Scurvy (degeneration of skin, teeth, blood vessels,
epithelial hemorrhages)
• Delayed wound healing
• Anem ia
1. Vitam in Cis also ca lled ascorbic acid.
8 2. It is an antioxidant.
3. Vitam in C deficiency primarily affects connective tissue (as opposed to
hematopoietic, epithelial, muscular or nervous tissue)
4. Vitam in C is essential for the normal elaboration and maintenance of
bone matrix, cartilage and dentin.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Which of the following is a part of active cytochrome oxidase?
• zinc
• vitamin C
• copper
• vitamin K
• magnesium SAADDES
244
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• copper
Cytochrome oxidase is one of a superfamily of proteins that act as the terminal en-
zymes of respiratory chains. Copper is also important in the maturation of col lagen
and elastin as copper is a cofactor for the enzyme lysyl oxidase. The oxidized lysine
residues formed in collagen and elastin by this enzyme form the cross-links that
stabilize these molecules.
Minerals are inorganic elements that are essential to life. They serve both structural
and regulatory functions. Minerals may be classified as:
• Major minerals (more than 0.005% of body weight) include calcium, ch loride,
SAADDES
magnesium, phosphorus, potassium, sodium, and sulfu r
• Trace minerals (less than 0.005% of body weight) include ch romium, cobalt, cop-
per, fluoride, iodine, iron, manganese, molybdenum, selenium and zinc
General Functions of Minerals:
• Maintenance of acid-base balance
• Coenzymes or catalysts fo r biologic react ions
• Components of essential body compounds
• Transmission of nerve impulses and regulation of muscle contractions
• Maintenance of water balance
• Growth of oral and other body tissues
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
A patient of yours with a PhD in nutrition tries to trip you up by saying that he
supplements every morning with tocopherol. What is he talking about?
• ri boflavin
• vitamin E
SAADDES
• vitamin C
• fo lacin
245
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• vitamin E
Summar~ of\ ita min E
Dietary Sources Vegetable oi l and seeds, green leafy vegetables,
margarines, shortenings
Major Body Functions Is an antioxidant and scavenger of free radicals
Deficiency Is a lmost entirely restricted to premature infants
1. Vitamin E is also cal led tocopherol.
SAADDES
2.1 t prevents free radicals from oxidizing compounds such as polyunsatur-
ated fatty acids.
3. Being lipid soluble, vitamin E associates w ith plasma lipoproteins, mem-
branes and storage fat.
4. In membranes, fat depots and lipoproteins vitam in E reacts w ith the free
radicals that are formed during lipid peroxidation, t hereby interrupting free
rad ical chain reactions. The inactive oxidized deri vatives of vitam in E formed
in these reactions are reduced back to the active fo rms by reducing agents,
including ascorbate and glutathione.
S. lt is t he least toxic of the fat-soluble vitam ins (vitamin D is the most toxic
of all vitam ins).
6. Vitam in E supplementation has been proposed to be of benefit in preven-
t ion of heart d isease and cancer; however, controlled studies have been un-
able to show a link between vitamin E supplementation and t he prevention
of these diseases.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Which of the following is a severe thiamine-deficiency syndrome found in
areas where polished rice is the major component of the diet?
• pellagra
• megaloblastic anemia
SAADDES
• pernicious anemia
• beri-beri
246
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• beri-beri
Summar~ ot T hiamine( \ itamin 8 1 )
Dietary Sources Yeast, lean pork and legume seeds
Major Body Functions Involved in the metabolism of carbohydrates and many amino acids
Deficiency Beriberi, manifests with severe muscle weakness and muscle
wasting, delirium, ophthalmoplegia (paralysis of the eye muscles)
and memory loss. This is accompanied by peripheral vasodilation
and an increased venous return to the heart. Myocardial contractility
is impaired and death can result from high-output cardiac failure.
Thiamine pyrophosph ate (TPP) is the biologically active form of the vitamin, formed by the
SAADDES
t ransfer of a pyroph osphate group from ATP to thiam ine. Thiamine pyrophosphate serves as a
coenzyme in t he oxidative decarboxylation of a-keto acids, and in the formation or degrada-
tion of a-ketols by t ransketolase.
Thiamine, also called vitamin B1, is used in many d ifferent body functions and deficiencies may
have far-reaching effects on the body. Very li ttle of th is vitamin is stored in the body and
depletion of this vitamin can happen within 14 days.
Today, t hiamine deficiency is most common in alcoholics who have poor intestinal absorption
in addi tion to an inadeq uate dietary in take. In this context, thiamine deficiency causes not
beriberi but Wernicke-Korsakoff syndrome. In the acute stage, kn own as Wernicke en-
cephalopathy, the patient presents with mental derangement and delirium, ataxia and paral-
ysis of t h eye muscles. The chronic stage, known as Korsakoff psychosis, is a severely
debilitating anterograde amnesia.
Note: The oxidative decarboxylation of pyruvate and a -ketog lutarate plays a key role in energy
metabolism of most cells, but is particularly important in t issues of the nervous system. In thi-
amine deficiency t he act ivity of these two dehydrogenase reactions is decreased, resulting in a
decreased production of ATP, and t hus impaired cellular function.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Which of the following statements concerning niacin are correct?
Select all that apply.
• a deficiency causes pellagra
• it is the precursor of FAD
SAADDES
• pork, whole grains, and legumes are the richest sources of niacin
·limited quantities of niacin can be obtained from the metabolism of t ryptophan
247
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• a deficiency causes pellagra
• limited quantities of niacin can be obtained
from the metabolism of tryptophan
The term niacin, originally applied to nicotinic acid, is now often used as a generic term for the
vitamin-active pyri midine derivatives nicotinic acid and nicotinamide. Both in the human body
and in dietary sources, niacin is present as a constituent of NAD• and NADP•. The dietary coen-
zymes are hydrolyzed in the Gl tract and free nicotinic acid and nicotinamide are absorbed in the
small intestine. After their transport to t he tissues, the vitamin forms are incorporated into the
coenzymes. Excess niacin is readily excreted by t he kidneys.
NAD+ and NADP• can also be synthesized from dietary tryptophan, but the pathway is ineffic-
ient. Sixty milligrams of tryptophan, w hich is nutritionally essential itself, is required for the syn-
SAADDES
thesis of 1 mg of niaci n. Also the pathway of endog enous niacin synthesis requires ri boflavin, thi-
amine and pyridoxine and is therefore impa ired in patients with multiple vitamin deficiencies.
Summ~H) ot Nt~tun
Dietary Sources Yeast, liver, meat, peanuts and o ther legume seeds, and
enriched cereals
Major Body Functions Component of NAD• and NADP+, which serve as
coenzymes in oxidation-reduction reactions
Deficiency Pellagra, which is c haracterized by diarrhea, dermatitis
and dementia (the 3 D's)
1. Pellagra is seen only with a d iet low in both niacin and tryptophan.lt is most often
associated with corn based diets. Early deficiency signs include weakness, lassitude,
anorexia, indigestion and g lossitis similar to that in riboflavin deficiency. The signs of
severe deficiency are dermatitis, diarrhea and dementia, and, if untreated, death.
2. High supplemental doses are effective in treati ng hyperlipidemia.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Pernicious anemia is caused by the malabsorption of:
• vitam in A
• vitam in B12
• vitam in C
• vitamin E
SAADDES
243
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• vitamin 8 12
Vitamin B12, or cobalamin, is chemically the most complex of all vitamins. The absorption of dietary
B12 requires intrinsic factor, a glycoprotein secreted by the parietal cells of the stomach. Vitamin B12
binds tightly to intrinsic factor and in this form, it is absorbed from the ileum. In t he blood it binds
t ightly to transcobalamin II and other plasma proteins. The cobalamin-transcoba lamin II complex
is taken up into the cells by receptor-mediated endocytosis. Transcoba lamin II directs the vitamin to
t he tissues in which it is needed and prevents its renal excretion.
Only two reactions are known to require cobalamin coenzymes in human tissues. The cytoplasmic
methylation of homocysteine to methionine requires methylcobalamin and the mitochondrial
methylmalonyi-CoA mutase reaction requires deoxyadenosylcobalami n.
SAADDES
Dietary Sources
Major Body Functions
Summar~ ofYitamin 8 12
Muscle and organ meats, eggs, dairy products, fish
Required for two reactions in the body:
I. Involved in the format ion of methionine
2. Involved in the conversion ofmethylmalonyl CoA to
succinyl CoA
Deficiency Pernicious anemia, neurologic disorders, glossitis
1. Pernicious anemia is an autoimmune disease that destroys the parietal cells in the
8 stomach. This deprives the patient of intrinsic factor and neither dietary nor biliary vitamin
B12 can be absorbed.
2.1t is the only vitamin that contains essential mineral element sand is the first substance
containing cobalt that is found to be vital to life.
3. It may be present in inadequate quantities in a strictly vegetarian diet.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Which vitamin plays a key role in amino acid metabolism?
• vitamin A
• vitamin B6
• vitamin K
• vitamin B12
SAADDES
249
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• vitamin 8 6
Vitamin B6 is a generic name for the d ietary precursors of the active coenzyme form,
pyridoxal phosphate (PLP). They include pyridoxine, pyridoxal and pyridoxamine, as
well as their phosphorylated derivatives. Note: The phosphate is removed by
intestinal alkaline phosphatase and the dephosphorylated forms are absorbed.
Several dozen enzymes of amino acid metabolism contain PLP as a tightly bound
prosthetic group. In these reactions, the aldehyde group of PLP forms an aldimine
derivative with the amino group of the amino acid. The aid imine is stabilized by an
intramolecular hydrogen bond w ith the phenolic hydroxyl group.
SAADDES
Vitam in B6 assists in the balancing of sodium and potassium as well promotes red
blood cel l production. Vitamin B6 is further involved in the nucleic acids RNA as
well as DNA. It has been linked to cancer immunity and fights the formation of the
toxic chem ica l homocysteine, wh ich is detri mental to the heart muscle.
Dietary sources of vitamin B6 include liver, fish, nuts, whole grains, legumes, egg
yolk and yeast.
Serious deficiency is rare, but when it occurs, it is characterized by peripheral neurop-
athy, stomatitis, glossitis, irritability, psychiatric symptoms and especially in children,
epileptic seizures.
Note: Vitamin B6 deficiency is most common in alcoholics, in whom it contributes to
sideroblastic anemia, peripheral neuropathy and seizures.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Which of the following plays a key role in one-carbon metabolism, and is
essential for the biosynthesis of the purines and the pyrimidine, thymine?
• biotin
• riboflavin
SAADDES
• pantothenic acid
• folic acid
250
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• folic acid
Folic acid consists of pteroic acid (pteridine +para-am inobenzoic acid (PABA)) and one to seven
y-linked glutamate residues. Dietary polyglutamate forms of folic acid are hydrolyzed to pteroyl
monoglutamate in the intestinal lumen. The monog lutamate is absorbed and reduced to the
active coenzyme form tetrahydrofolate (THF) by dihydrofolate reductase in the intestinal mu-
cosa. The monoglutamate conjugate of methyi-THF is the major circulating form ofTHF, but
intracellularTHF is present in the form of polyglutamate conjugates.
Important: The clinical signs of folate deficiency are caused by impairment of DNA replication
in dividing cells, resulting from reduced synthesis of purine nucleotides and thymine.
Summar~ of Folic \cid
SAADDES
Dietary Sources Liver, yeast, some fntits and green vegetables
Major Body Functions Involved in the synthesis of purines and thymine,
w hich are required for ON A formation
..
Deticiency Megaloblastic anemia
. Diarrhea
Glossitis
1. Folic acid is stored in the liver and may be synthesized by the bacterial flora of the
Gl tract. Their growth can be inhibited by sulfonam ides and trimethoprim.
2. Folic acid deficiency is probably t he most common vitamin deficiency in the
U.S., particularly among pregnant women and alcoholics.
3. Because of folic acid's importance in the synthesis of purines and thymine, the
metabolism of folic acid is the target of a number of antimetabolite drugs such as
methotrexate.
4. Folate supplements are recommended for t he prevention of neural tube defe.cts
(spina bifida and anencephaly).
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
The determination of the prothrombin time is the most important
laboratory test for the evaluation of the vitamin Kstatus.
Vitamin K deficiency is most common in the elderly.
• both statements are true
SAADDES
• both statements are fa lse
• the first statement is t rue, the second is fa lse
• the first statement is fa lse, the second is true
251
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is true, the second is fal se
Vitamin K participates in the enzymatic carboxylation of glutamyl residues during the
synthesis of prothrombin and other clotting factors (II, VII, IX and X) in the liver. The only
important deficiency sign is a clotting disorder. Note: The determination of the pro-
thrombin time is the most important laboratory test for the evaluation of the vitamin K
status.
Summa11 of\ ita min K
Dietary Sources Green and yellow vegetables, small amount in cereals,
fruits and meats
SAADDES
Major Body Functions Required for synthesis of prothro mb in and ce11ain other
clotting factors in the liver
..
Deficiency Retarded blood clotting
Excessive bleeding
1. Humans get some of their vitamin K as phylloquinone and some as mena-
quinone produced by intestinal bacteria.
2. Vitamin K has no specific binding protein in the plasma, but is transported
from the intestine to the liver in chylomicrons.
3. Unlike the other fat-soluble vitamins, vitamin k is not stored to any great ex-
tent.
4. Vitamin K deficiency is most common in newborn s. This is known as hemorr-
hagic disease of the newborn. It is the most common nutritional deficiency in
newborns.
5. Vitamin K deficiency in adults is usually caused by fat malabsorption.
6. Vitamin K decreases coagulation time and is present in low concentrations in
milk.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Pantothenic acid is a component of which of the following?
Select all that apply.
• pyridoxal phosphate
• coenzyme A
SAADDES
• retinoic acid
• fatty acid synthase
252
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• coenzyme A
• fatty acid synthase
Pantothenic acid is a component of coenzyme A, which functions in the t ransfer of
acyl g roups. Coenzyme A conta ins a thiol group that carri es acyl compounds as acti-
vated thiol esters. Examples of such stru ctures are succinyl CoA, fatty acyl CoA, and
acetyl CoA. Pantothenic acid is also a component of fatty acid synthase (which cata-
lyzes reactions of fatty acid synthesis).
Summ:u~ of Pantothenic Acid
SAADDES
Dietary Sources Widely d istributed in all foods
Major Body Functions • Component of coenzyme A, wh ich functions in the
entry of pyruvic acid into the Krebs cycle and in the
degradation of fatty acids
• Also a component of fatty acid synthase
Deficiency • Fatigue
***Very rare • Sleep d isturbance
• Impaired coordination
• Diarrhea
• G l, rena l problems
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Biotin is a prosthetic group of:
• pyruvate carboxylase
• acetyi-CoA carboxylase
• propionyi-CoA carboxylase
SAADDES
• all of the above
253
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• all of the above
Biotin is a prosthetic group of pyruvate ca rboxylase, acetyi-CoA carboxylase, propi-
onyi-CoA ca rboxylase and other AlP-dependent carboxylases. These multiunit en-
zymes conta in biotin covalently bound to thee-am ino g roup of a lysine residue.
Summar~ of Biotin
Dietary Sources Is present in almost a ll foods, particularly li ver, milk and
egg yolk
Major Body Functions . Essential tor the activity of many enzyme systems
. that are involved in amino acid and protein synthesis
Required tor the carboxylation of acetyl CoA to
SAADDES
malonyl CoA, an intermediate in fatty acid synthesis
Deficiency .. Fatigue
.. Depression
Nausea
.. Dermatitis
Muscular pains
Loss of hair
1. The proteolytic degradation of biotin-containing enzymes both in the in-
8 testinal lumen and in the tissues, produces the biotin-lysine conjugate bio-
cytin. Biotin is released from biocytin by biotinidase. Biotinidase deficiency
causes non dietary biotin deficiency.
2. A large percentage of the biotin (sometimes ca lled vitamin H) requirement
in humans is supplied by intestinal bacteria.
3. Egg white contains the protein avidin, so called because it binds biotin
avidly, preventing its intestinal absorption.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
The biologically active forms of vitamin A are the flavoproteins.
In vitamin A deficiency, columnar epithelia are transformed into heavily
keratinized squamous epithelia, a process known as squamous metaplasia.
• both statements are true
SAADDES
• both statements are false
• the first statement is true, the second is false
• the first statement is false, the second is true
254
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
The retinoids (i.e., retinol, retinal and retinoic acid) are the active forms of vitamin A. Retinal
and retinoic acid are t he most important biologically active forms. Retinal is the prosthetic
group of t he rhodopsins, the visual pigments of rods and cones. Retinoic acid is a gene reg u-
lator that acts through nuclear receptors, similar to the steroid hormones. Note: Retinoic acid is
required for the maintenance of epithelial tissues.
Sumnur~ of\ •t~tmm \
Dietary Source$ Live r, mea t, eggs, dairy products and cod Jivcr oil provide vita min A in the fonn
..
of retinol e sters and vegetables (yellow, orange and leafy green) supply carotenes
Major Body Functions Cons tituent of rhodopsin (visua l pigment)
. Maintenance of e pithelia l tissue$
SAADDES
Has a ro]c in muc.o poJysaccharide synthc~'ii s , bone growth ~md rcmodeJing
Dcfidency .. Xe rophthalmia ("dry eyes")
..
Night b lindness
Microcytic ~memi a
. Susceptibility to infections
Jmpainnent o f reproductive function both in men a nd wo me n
1. Vitamin A, along with vitamins C and D, is req uired for the normal production of
8 sound dentin and enamel; however, a deficiency of vitamin A will most likely affect
the enamel more than the dentin. Whereas, a deficiency in vitamin C will affect the
dentin more, due to the role of vitamin C in collagen synthesis.
2. ~-Carotene, the orange pigment of carrots and many other vegetables, is t he
major vitamin A precursor in plants.
3. In vitam in A deficiency, columnar epithelia are transformed into heavily keratin-
ized squamous epithelia, a process known as squamous metaplasia. Follicular
hyperkeratosis (goosefl esh) is an early sign, together wit h night blindness. This often
leads to xerophthalmia ("dry eyes").
4. Both vitamin A deficiency and vitam in A excess are teratogenic.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
All of the following vitamins have little to no risk of overdose EXCEPT one.
Which one is the EXCEPTION?
• niacin
• biotin
SAADDES
• vitamin C
• vitamin K
255
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• vitamin K
***The others are water soluble and thus have little, if any, risk of overdose.
The water-soluble vitamins, excluding vitamin C, popularly are termed the B-complex
B-complex vitamins. There are eight of them, namely: B1 (thiamine), B2 (riboflavin),
B3 (niacin), B5 (pantothenic acid), B6 (pyri doxine), B7 (biotin/vitamin H), B9 (folic acid/
folacin) and B12 (cobalamin). The water-soluble vitamins, inactive in their so-called
free states, must be activated to their coenzyme forms. B complex vitamins and vita-
min C are water-soluble vitamins that are not stored in the body and must be
replaced each day, preferably through a high-quality liquid multivitam in.
SAADDES
Remember: The water-soluble vitamins are absorbed in our intestine, pass d irectly
to the blood and are carried to the t issues in which the vitam ins will be utilized.
Vitamin B12 requires a substance known as "intrinsic factor" for absorption.
Water-soluble vitamins usually are excreted in the urine on a daily basis.
Thiamine (B,), ri boflavin (B2), pyridoxine (B6), ascorbic acid (C), pantothenic acid
(B 5) and biotin (B 7) appear in urine as free vitam ins. The t issue storage capacity of
water-soluble vitam ins is limited, and as the tissues become saturated, the rate of
excretion increases sharply. This keeps us from overdosing, but this is also why
we need to take these vitamins daily. Unlike the other water-soluble vitam ins
however, vitamin 8 12 is excreted solely in the feces.
Remember: Fat-soluble vitamins include vitamins A, D, Eand K. They are carri ed in fat
and can be stored in the body. It is possible to overdose on fat-soluble vitamins.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Vitamin Dis required in the diet of individuals exposed to sunlight.
Cholecalciferol is not the active form of vitamin D and needs to be converted
to active 1,25-dihydroxycholecalciferol (calcitriol) by successive hydroxyla-
tions in the liver and kidney.
SAADDES
• both statements are true
• both statements are fa lse
• the first statement is t rue, the second is fa lse
• the first statement is fa lse, the second is true
256
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the first statement is false, the second is true
Vitam in D is nutritionally essential only for people who stay out of the sun. Otherwise, it is
synthesized photochemically in the skin, by the action of ultraviolet radiation on the minor
membrane steroid 7-dehydrocholesterol.
The initial product of t his reaction, cholecalciferol (vitamin 0 3), is transferred to a specialized
vitamin D-binding plasma protein. Cholecalciferol is not the active form of vitamin D and
needs to be converted to active 1,25-dihydroxycholecalciferol (calcitriol) by successive
hyd roxylations in the liver and kidney.
Calcitriol is a hormone-like substance. Calcitriol assists PTH in mobilizing calcium and phosphate
from the bones and in stimulating calcium reabsorption by the kid neys. Its most important
SAADDES
effect however, is the stimulation of intestinal calcium and phosphate absorption.
Vitamin D deficiency is called rickets in children and osteomalacia in adults. The immediate
effect is reduced intestinal calcium absorption, which tends to red uce the plasma calcium
concentration. The maintenance of the blood calcium level has top priority and therefore, PTH
is released. Even in long-standing vitamin D deficiency, plasma calcium can be maintained at
a near-normal level by PTH (at t he expense of t he bones, which are gradually drained of t heir
mineral content). As a result, affected child ren have soft, cartilaginous bones that bend easily
and affected adults have brittle bones that break easily.
Summar~ of\ it:unin J)
Dietary Sources Liver, egg yolk and saltwater fish (cod liver oil), as well as fortified foods
Major Body Functions .. Promotes growth and mineralization of bones and teeth
Calcium and phosphorus metabolism (bone formation)
Deficiency .. Rickets in children
Osteomalacia in adults
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Riboflavin is a precursor of:
• NAD• and NADP•
• ATP and ADP
• pyri doxal phosphate (PLP)
• FMN and FAD
SAADDES
257
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• FMN and FAD
Vitamin B2, commonly ca lled riboflavin, consists of a d imethyl isoalloxazine ring t hat
is covalently bound to a sugar alcohol ri bitol. Its only biological function is as a pre-
cursor of flavin adenine d inucl eotide (FAD) and flavin mononucleotide (FMN), the
prosthetic groups of t he flavoproteins.
Dietary riboflavin is absorbed by an energy-dependent transporter in the upper small
intestine and transported to the tissues, in wh ich it is converted to the coenzyme forms
FMN and FAD. The excess is excreted in the uri ne o r metabolized by m icrosoma l
enzymes in the li ver.
SAADDES
Riboflavin deficiency usually occurs along w ith other vitamin deficiencies and is most
common in alcoholics. The symptoms incl ude glossitis, angular stomatitis, sore th roat
and a moist (seborrheic) dermatitis of the scrotum and nose. This deficiency may be ac-
compan ied by a normochromic normocytic anemia.
Sum m ar~ of Rihotla\ in (\ ita min B,)
Dietary Sources Liver, yeast, eggs, meat, em iched bread and cereals and milk
Maj or Body Functions Precursor of FAD and FMN, the prosthetic groups of the tlavoproteins
De ficiency .. Angular stomatitis
. Moist (seborrheic) dermatitis o f the scrotum and nose
Glossitis
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
All of the following statements concerning fluoride are true EXCEPT one.
Which one is the EXCEPTION?
• it may have some protective effect in osteoporosis
• it can be incorporated in the inorganic substance of bones and teeth
SAADDES
• it hardens tooth enamel
• although not absolutely essential, it strengthens teeth and bones
258
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• it hardens tooth enamel
Fluoride does not make t he enamel harder, but reduces the solubility of enamel due to t he
incorporation of fluoride into the apatite structure of the enamel. The concentration of fluoride
in the body fluids is reg ulated by an equilibrium relationship between bone and urinary
excretion. A deficiency of fluoride can lead to an increased incidence of dental caries and
toxicity leads to tooth enamel mottling and discoloration, increased bone density and
calcification.
Facts about fluoride:
• It inhibits bacterial enola se (a key enzyme in glycolysis) which can decrease caries activ-
ity
• It is excreted by the kidney
SAADDES
• It is deposited in calcified tissues (i.e., skeletal)
• At 1 ppm, fluoride is tasteless, colorless and odorless. One ppm is the equivalent of
1 mg/L, or 1 inch in 16 miles
• It converts hydroxyapatite to fluoroapatite by the substitut ion of the OH ion wit h the
fluoride ion
• Fluoridation of community water has been credited with reducing tooth decay by 50%-
60% in the United States since World War II. More recent estimates of this effect show decay
reduction at 18%-40%, which reflects that even in communities t hat are not optimally
fluoridated, people are receiving some benefits from other sources (e.g., bottled beverages,
toothpaste).
• Fluoride works by stopping or even reversing the tooth decay process. Fluoride keeps
t he tooth enamel strong and solid by prevent ing t he loss of (and enhancing t he reattach-
ment of) important minerals from the tooth enamel.
• Water fluoridation costs, on average, 72 cents per person per year in U.S. commun ities.
• Children under age 6 years may develop enamel fluorosis if they ingest more fluoride
t han needed. A common source of extra fluoride is unsupervised use of toothpaste in
very young children.
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Your dental assistant comes in one day all smiles. At lunch, she announces
that she is pregnant. You recommend that she makes sure to keep her intake
of this mineral high because it helps her immune system, as well as the
growth and development of her and her unborn child. She often comes in
with loads of perfume on and you are hoping that this change in diet might
also improve her sense of smell, so she tones it down a notch. Which mineral
are we talking about?
• phosphorus
• cobalt
SAADDES
• copper
• zinc
259
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• zinc
Zinc is the most abundant trace mineral in the body after iron. lt is a constituent of the zinc
metalloenzymes, which include carbonic anhydrase, the cytoplasmic (copper-zinc) super-
oxide dismutase, alcohol dehydrogenase, carboxypeptidase A and B, DNA and RNA poly-
merases and in many others.
Zinc is absorbed incompletely in the small intestine. It is also present in pancreatic juice
and excess zinc is excreted in the stools. Transport in the blood is in association with seru m
albumin.
Zinc supports a healthy immune system, is needed for wound healing, helps maintain
your sense of taste and smell and is needed for DNA synthesis. Zinc also supports normal
SAADDES
growth and development during pregnancy, childhood, and adolescence.
Nutrient/Mineral Functions
Iron Constituent of hemoglobin and enzymes involved in e nergy metabolism
Jodinc Constituent of thyroid hormones, regulates energy metabolism
Calcium Bone and tooth fonnation, blood clotting , nerve trans mission, muscle contraction
Phosphoms Bone and tooth fom1ation, acid-base balance, release o f energy (ADP, ATP)
Sulfur Cons tituent of active tissue compounds, cartilage and tendon
Potassium Acid·base balance, body water balance, nerve function, muscle relaxation
Sodium Acid·base balance, body water balance, nerve function
Magnesium Key cofactor in kinases involved in protein synthesis
CobaJt Constituent of vitamin 8 12
Copper Constituent of enzymes associated with iron me tabolism and nerve function
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Summary of fat-soluble vitamins
Vitamin Major Function Deficiency Symptoms
A Helps form skin and mucous membrane-..~ Night b lindness
and keep them healthy, thus increasing Abnormal drynt\'is of the skin, eyes or mucous
resistance to infections membranes
Essential fo r night vision Keratomalacia
Promote-s bone a nd tooth development Perifollicular hyperkeratosis
Beta carotene is an a ntioxidant and
SAADDES
Anorexia
protects agains t cancer Bone changes
D Promotes hardening of bone..~ a nd teeth Osteomalacia in adults
Increase-s the absorption of calcium Rickets in children
Deformity of bone and pathologic fractures
E Protects vitamins A and C and fatty acids • Neurologic syndromes including arcOcxia
Prevents damage to cell membranes (absence of rcllcxes) and gait disturbances
Antioxidant May contribute to hemolytic anemia
K Major impo rtance in b lood clot !Ormation • H ypothrombincmia and hemorrhagic disease
260
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
SAADDES
Saad Alqahtani, Twitter @saaddes
minerals/vitamins
Summary of water-soluble vitamins
Vitamin Major Function Deficiency Symptoms
c Formation of collagen. helps hold them Bleeding gums
together and keep them healthy Failed wound healing
Wound healing Bruise easily
Maintaining blood vessels, bones. [ee[h Dry. rough skin
Absorption of ii'On, calcium, folacin Scurvy
Production of brain honnones, immune Sore joint<; and bone.o;
factors Increased infec[ion..<;
Antioxidant
SAADDES
Thiamine He-lps relea.o;e ene-rgy from foods Beriberi
Promote.s nol'lllal appetite Ede-ma. heart tililure
Important in function of[he nervou..<; sys[em • Wernicke·s enc.ephalopathy
Peripheral neuropathy
Riboflavin He-lps relea.o;e. ene.rgy from foods Oroac.uloge.niml area.o; are reddened.
Promote.s good vision and healthy skin greasy. sc.aly and pnu itic
Seborrheic derma[itis
Angular stomatitis
Cheilosis
Magenta tongue
Niacin Energy production fl·om fOods Pellagra
Aid.o; digestion Diarrhea
Promo[t.S normal appetite Photosensitive de•·matiris
Promote.s healthy skin and ne-rves Mucosal inflammation
Dememia
Beefy red tongue
261
copyright 0 20 t l -1014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
Summary of water-soluble vitamins (continued)
Vitamin Major Function Deficiency Symptoms
Folate .. Aids in protein metabolism .. Megaloblastic anemia
.. Promotes red blood cell fonnation
Prevents birth defects o f the spine and brain
wwers homocysteine levels and thus
.. Glossitis
Diarrhea
Neural tube defects
coronary heart disease risk
B, .. Aids in building of genetic material .. Mega loblastic anemia
.
Aids in development o f normal red blood
cells .. Glossitis
Anorexia
Maintenance of nervous system
. Sensory neuropathy
SAADDES
Dementia
Pantothenic .. Involved in energy production .. Burning foot syndrome
acid Aids in fonnation o f hormones
.. Fatigue
Abdominal pain and vomiting
Insomnia
Biotin .. Helps release energy from carbohydrates .. Scaly dermatitis
Aids in fat synthesis
.. Alopecia
Muscle pain
. Depression
Anemia
B. .. Aids in protein metabolism, abso•·ption .. Seborrheic dennatitis
. Aids in red blood cell fonnation
Helps body use fat .. Glossitis
Cheilosis
. Angular stomatitis
Peripheral neuropathy
Saad Alqahtani, Twitter @saaddes
respiratory system
Which of the following terms means air in the chest?
• hemothorax
• pyothorax
• pneumothorax
• pulmothorax
SAADDES
• pulmonary inflation
28
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• pneumothorax
A penetration wound of the chest wall can lead to a pneumothorax (air in the pleural cavity) or a
hemothorax (blood in the pleural cavity).ln both of these situations, the surface tension that binds
t he lungs to the chest wall is eliminated, and the lung will instantly shrink to the size of a tennis ball.
The lungs fill the pleural divisions of the thoracic cavity; they extend from the root of the neck to
the diaphragm. The lungs are the main component of the respiratory system; they distribute air and
exchange gases. The right and left lungs are separated by the mediastinum, which contains t he
heart, blood vessels, and other midline structures; fissures divide each lung into Jobes. Each
primary bronchus enters its respective lung at the hilus, an indentation on the mediastinal surface.
The bronchi and pu lmonary blood vessels are bound together by connective tissue to form the root
of the lung. The base, the inferior surface of the lung, rests on the diaphragm. The apex, the most
superior portion of the lung, projects above the clavicle.
SAADDES
Right lung:
• Has three Jobes (superior, middle, and inferior) and three secondary (lobar) bronchi
• Contains ten bronchial segments (corresponding to the t ertiary bronchi)
• Usually receives one bronchial artery
• Has a slightly larger ca pacity than the left lung
• The azygos vein leaves an impression on the right lung as the vein arches over the root
Left lung:
• Has two Jobes (superior and inferior) and two secondary (lobar) bronchi
• Contains eight bronchial segments (corresponding to the tertiary bronchi)
• Contains a cardiac notch (on its superior lobe), which is an indentation providing room for
the heart
• Usually receives two bronchial arteries
• Contains a lingula, which is a tongue-shaped portion of its superior lobe that corresponds to
the middle lobe of the right lung
Each lung is enclosed in a double-layered pleural sac. One layer is called the visceral pleura; t he
other is called the parietal pleura. Between t he two layers is the pleural cavity, which is filled with
serous fluid.
Saad Alqahtani, Twitter @saaddes
fissure Inferior
..._ __L_~_Card lac Middle ._~-- ...::c~ lobe
notch lobe
Inferior Cardiac
lobe notch
Right lung
(B) L~tcrat views
SAADDES
28·1
Costal surfaces of lungs. The lungs arc shown in isolation in antcrior(A) and lateral views (B), demon-
strating lobes and fissures. C. The heart and lungs are s hown in situ.
Reproduced with permission from 1\>loorc KL. Dalley AF. and Agur AMR. Clinit<llfy Oriftu('({An(llonty. 00 6. Wolters Kluwer. Baltimore. 2010.
Saad Alqahtani, Twitter @saaddes
respiratory system
The ridge that marks the bifurcation of the trachea into the right and left pri-
mary bronchi is the:
• carina
•lingula
SAADDES
• mediastinum
• bronchial t ree
29
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• carina
The trachea connects the upper respiratory tract to the lower respiratory tract. It is about 9-1 5 em in length.
It is located in front of the esophagus and behi nd the thyroid g land in the neck. It is considered to be in the
superior and middle mediastinum. It is made up of 16-20 incomplete hyaline cartilaginous rings that are
open posteriorly. The trachea bifurcates into the right and left main stem bronchi at a location called the
carina, which is located at the level ofthe sternal angle (T4-T5). A series of ( -shaped rings of hyaline car-
tilage strengthen the trachea and prevent it from collapsing during inspiration. The trachea is lined with
ciliated pseudostr atified columnar epithelium and mucous-secreting goblet cells, which trap inhaled
debris. Ciliary action moves debris toward the oropharynx for removal by coughing.
The trachea branches off into t wo main bronchi, the left and right p rimary bronchi, which lead to the left
and right lung respectively. The right lung is larger and heavier than the left, but it is shorter and wider
SAADDES
because the right dome of the d iaph ragm is higher and the heart and pericardi um bulge more to the left .
The right and left mainstem bronchi branch from the trachea at different angles, the right more vertical
and more di rectly in line with the trachea, thus the right b ronchus is more likely to receive aspi rated
material. At this point in breathing, the air has been moistened, purified and warmed . Each bronchi enters
its lung and begins on a series of branches, called the bronchial or respiratory tree. The first of these
b ranches is the lobar (secondary) b ranch. On the left, there are t wo lo bar branches, while on the right,
there are three. Each lobar branches into one lobe. The next branch is called the segmental (tertiary)
b ranch. Each b ranch conti nues to branch into smaller and smaller b ronchioles. The final branch is called
the terminal bronchioles. These bronchio les are smaller than 0.5 mm in diameter. Each of these terminal
b ronchioles gives rise to several respiratory bronchioles. Note: The first few levels of bronchi are
supported by rings of cartilage. Branches after that are supported by irregularly shaped d iscs of cartilage,
while the latest levels of the tree have no support whatsoever.
Note: The right main bronchus divides into three lobar bronchi, and the left main bronchus divides
into two lobar bronchi. Each secondary or lobar bronchus serves one of the five lobes of the t wo lungs.
Each respiratory bronchiole subd ivides into several alveolar ducts, which end in clusters of small, thin-
walled air spaces called alveoli. These cl usters of alveoli are called alveolar sacs and form the functional
unit of the lung.
Saad Alqahtani, Twitter @saaddes
primary bronchus
SAADDES
Bronchi in situ -Anterior view
29· 1
Saad Alqahtani, Twitter @saaddes
respiratory system
Which of the following components of the respiratory system does NOT have
cilia?
• tertiary bronchioles
• primary bronchioles
SAADDES
• alveo lar ducts
• respiratory bronchioles
• terminal bronchioles
30
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• alveolar ducts
Conducting bronchioles are smaller extensions of bronchi (little bronchi). Those devoid
of alveoli in their walls are nearer the hilum of the lung. These conducting passageways
deliver air to passageways that have alveoli. The last generations of conducting
bronchio les are called terminal bronchioles.
Respiratory bronchioles, continuing from terminal bronchioles, branch nearer to the
alveolar ducts and sacs and have occasional alveoli in their wall s. These bronchio les
capable of respiring are the first generation of passageways of the respiratory portion
of the bronchial tree.
Remember:
SAADDES
• The conducting zone of the respiratory system is made u p of the nose, pharynx, lar-
ynx, t rachea, bronchi, bronch ioles, and termina l bronchioles; their functi on is to filter,
warm, and moisten air and conduct it into the lungs. It's also called the dead zone be -
cause there is no 0 2 exchange happens here.
• The respiratory zone is the site of oxygen and carbon dioxide gas exchange, and is
composed of t he respiratory bronchioles, alveolar ducts, and alveoli.
Bronchioles are characterized by:
• A diameter of one millimeter or less
• An epithelium that progresses fro m ciliated pseudostratified columnar to simple
cuboidal (respiratory bronchioles)
• Small bronchioles have non-ciliated bronchiolar epithelial cells (Clara ce lls) that
secrete a surface-active lipoprotein
• Walls devoid of gland s in the underlying connective t issue
• Woven bundles of smooth muscle to regu late t he bronchiolar diameter
• Walls de void of cartilage (small diameter p revents them from collapsing at end of
expiration)
Saad Alqahtani, Twitter @saaddes
SAADDES
(A) (B)
The Trachea, Bronchi, Bronchioles, and Alveoli
(A) The trachea and bronchi
(B) The termination of bronchioles into alveoli
30-1
Saad Alqahtani, Twitter @saaddes
respiratory system
Which of the following vessels supply blood to the bronchi?
• pulmonary arteries
• pulmonary veins
• subclavian arteries
SAADDES
• none of the above
31
Irefer to card 29-1, 30-1for illustration! copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• none of the above- the bronchial arteries supply blood to the bronchi
Each lung is shaped like a cone. It has a blunt apex, a concave base (that sits on the diaphragm), a
convex costal surface, and a concave mediastinal surface. At the middle of the mediastinal surface, the
hilum is located, which is a depression in which the bronchi, vessels, and nerves that form the root enter
and leave the lung.
The root of the lung contains the following structures:
• Primary bronchus: the right and left bronchi arise from the trachea and carry air to the hilum of the
lung du ring inspiration and carry ai r from the lung during expi ration
• A pulmonary artery: enters the hilum of each lung carrying oxygen-poor blood
• Pulmonary vein(s): a superior and inferior pair for each lung leave the hilum carrying oxygen-rich
b lood
1. The small bronchial arteries (which are branches of the thoracic portion of the descending
SAADDES
aorta) also enter the hilum of each lung and deliver oxygen-rich blood to the tissues. The
bronchial arteries tend to follow the bronchial tree to the respiratory bronchioles where the
bronchial arteries anastomose with the pulmona ry vessels.
2. Branches of the vagus nerve pass behind the root of each lung to form the posterior pul-
monary plexus.
Innervation of the lung: The lung is innervated by parasympathetic nerves via the vagus and sympathetic
nerves derived from the second to fourth thoracic sympathetic ganglia. These nerves form plexuses around
the hilus of the lung and give rise to intrapulmonary nerves accompanying the bronchial tree and blood
vessels. Both sympathetic and parasympathetic nerves to the lung contain efferent and afferent fibers.
Important: When foreign objects are aspirated into the trachea, they usually pass into the right primary
bronchus because it is larger, straighter, and shorter than the left. It is also in a more di rect li ne w i th the tra-
chea (important in a dental cha ir because if a patient swallows an object it tends to lodge in the right
bronchus).
Tuberculosis seems to be more common in the right lung than the left due to the shorter right bronchus.
The reason that the disease is usually restricted to the apex of the lungs is due to the fact that venti la-
tion/ perfusion ratio is high as the blood flow is reduced leading to higher alveolar P0 2 this provides a bet-
ter environment for the obligate aerobes to g row.
Saad Alqahtani, Twitter @saaddes
respiratory system
Which of the following is NOT a part of the lower respiratory tract?
•laryngopharynx
• trachea
• primary bronchus
SAADDES
• alveolar duct
32
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• laryngopharynx
The mediastinum lies between the rig ht and left pleura in and near the median sagittal plane of the
chest. It extends from the stern um in front to the vertebral column behind, and contains all the tho-
racic viscera except the lungs. It may be divided for purposes of description into two parts:
• An upper portion, above the upper level of the pericardium, which isnamed the superior me-
diastinum
• A lower portion (inferior mediastinum) which is subdivided into three parts:
- that in front of the pericardium, the anterior mediastinum
-that containing the pericardium and its contents, the middle mediastinum
-a nd that behind the pericard ium, the posterior mediastinum
SAADDES
The respiratory system consists of the upper and lower respiratory tracts, the lungs, and the thoracic
cage. The respiratory system is designed to exchange the ca rbon dioxide accumulated in the blood
for oxygen in the airways, which enters the lungs as air from the surrounding atmosphere.
Blood travels continuously through t wo different circulations: the pulmonary and the systemic cir-
cu lations. The heart pumps deoxygenated blood from the veins of the systemic circulation into the
arteries of the pulmonary circulation. This blood is oxygenated by the lungs, and then flows back to
the heart to be pumped into the arteries of the systemic circu lation.
The structures of the upper respiratory tract include the nose, mouth, nasopharynx, oropharynx,
laryngopharynx, and larynx. Besides warming and humidifying inhaled air, these structures provide
for taste, smell, and the chewing and swallowing of food.
The lower respiratory tract structures are the trachea, bronchi, and lungs. Bronchi branch into bron-
chioles, which in turn branch into lobules. The lobule includes the terminal bronchioles and alveoli.
A mucous membrane containing hair-like cilia lines the lower tract. Functionally, the lower tract is
subdivided into conducting airways (the trachea and the primary, lobar, and segmental bronchi)
and alveoli, the sites of gas excha nge.
Saad Alqahtani, Twitter @saaddes
primary bronchus
SAADDES
Diaphragm
32· 1
Respiratory System
Reproduced with perm1ssion from BaJTon·s Ant11omy fo1 :bh Card.;;:. Australia. 2009. Global Book l'ubl•shing.
Saad Alqahtani, Twitter @saaddes
respiratory system
All of the paranasal sinuses drain into one of the three meatuses (superior,
middle, and inferior) EXCEPT one. Which one is the EXCEPTION?
• maxillary sinus
• frontal sinus
SAADDES
• ethmoidal sinus
• sphenoidal sinus
33
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• sphenoidal sinus- which drains into sphenoethmoidal recess
Air enters through the nostrils (external nares) that lead to the vestibu les of the nose.
The bony roof of the nasal cavity is formed by the cribriform plate ofthe ethmoid bone.
The lateral walls have bony projections cal led conchae (superior, m iddle, and inferior),
wh ich are also referred to as the nasal tu rbinates. These conchae form shelves that have
spaces (or grooves) beneath them cal led meatuses (superior, middle, and inferior). All
of the paired paranasal sinuses drain into the nasal cavity by way of these meatuses
except for the sphenoidal sinus wh ich drains into the sphenoethmoidal recess. The na-
solacrimal duct, which d rains tears from the surface of the eyes, also empties into the
nasal cavity by way of the inferior meatus. The floor is formed by the hard palate. The
SAADDES
nasal cavity opens posteri orly into the nasopharynx via funnel-like openings called the
choanae (posterior nares). The maxillary sinus drains into the m iddle meatus through
the semilunar hiatus.
1. The vestibules are lined w ith nonkeratinized stratified squamous ep-
ithelium.
2. The conchae of the nasal fossae are lined with pseudostratified ciliated
columnar epithelium.
3.The olfactory epithelium is very prominent in the upper medial portion of
the nasal cavity. Both olfactory and respiratory epithelium are cha racterized
as pseudostratified columnar epithel ium; olfactory epithelium is unique in
that it conta ins olfactory sensory cells.
4. The nasal cavity receives sensory innervation from the olfactory nerve fo r
smell and from the trigeminal nerve for other sensations. The nasal cavity's
blood supply is from branches of the ophthalmic and maxillary arteries.
Saad Alqahtani, Twitter @saaddes
SAADDES Nasal
vestibule
Inferior
nasal
meatus
La teral Wall of Nose
33· 1
Reproduced with pcnmssion from Atlll.1 ojH11man AlllJtiJmy: Springhouse:. 2001. Springhouse.
Saad Alqahtani, Twitter @saaddes
respiratory system
While ascending to 30,000 feet, the passengers on a commercial flight expe-
rience the sensation of their ears "popping:' The swallowing or yawning that
triggers this equalizes the pressure of the middle ear with the surrounding
atmosphere via the eustachian (auditory) tube. The pharyngeal opening for
this tube, along with the salpingopharyngeal fold, pharyngeal recess, and
pharyngeal tonsils (adenoids) are all located in the:
SAADDES
•laryngopharynx
• oropharynx
• nasopharynx
• none of the above
34
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• nasoph arynx
The ph arynx (the throat) is a t ube that serves as a passageway for the respiratory and di-
gestive tracts. It extends from the mouth and nasal cavities to the larynx and esophagus.
The pharynx is divided into three regions:
1. Nasopharynx- is the most superior division of the pharynx. It is inferior to the sphe -
noid bone and li es at the level of the soft palate. The pharynx is lined with ciliated pseu-
dostratified epithelium (respiratory epithelium). The nasopharynx has four open ings:
• two auditory (eustachian) tubes: each opening out of a lateral wall and connecting
with the mi ddle ear (tympanic cavity)
• two openings of the posterior nares (choanae)
Note: nasopharynx -location of the pharyngeal tonsils
SAADDES
The soft palate and uvula form the anterior wall of the nasopharynx. Note: The tensor veli
palatini and the levator veli palatini muscles prevent food from entering the nasophar-
ynx.
2. Oropharynx - the middle division of the pharynx; is continuous w ith the posterior
oral cavity and is lined with stratified squamous epithelium. The oropharynx extends in-
feriorly from the soft pa late to the hyoid bone. The opening into the oropharynx from the
mouth is called the fauces. The lingual tonsils protrude into the oropharynx from the
oral cavity at the base of the tongue. The anterolateral walls of the oropharynx support
the palatine tonsils. It is a food and air pa ssageway.
3. La ryngopharynx- is the most inferior division of the pharynx; the laryngopharynx ex-
tends from the hyoid bone to the opening of the esophagus. The laryngopharynx is lined
w ith stratified squamous epitheliu m. extends from the oro pharynx above to the larynx
and esophagus. The laryngopharynx also serves as a passageway for food and air. Air
entering the laryngopharynx goes to the larynx while food goes to the esophagus.
Note: Food entering the larynx would be expelled by violent coughing.
Saad Alqahtani, Twitter @saaddes
Pharyngeal tonsil (adenoids)
Middle turbinate
SAADDES
Inferior turbinate
Vestibule
34-1
Pharynx
Saad Alqahtani, Twitter @saaddes
respiratory system
A women in Ethiopia who has a human papillomavirus infection, starts to
grow warts on her larynx and respiratory tract. In order to allow her to breathe
an emergency airway maybe established by opening into the trachea:
• th rough the thyrohyoid membrane
SAADDES
• between the thyroid and crico id cartilage
• between thyroid cartilages
• above the level of thyroid cartilage
35
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• between the thyroid and cricoid cartilage
An emergency tracheotomy (tracheostomy) is most easil y made by an incision
through the median cricothyroid ligament. This ligament runs from the cricoid ca rtilage
to the thyroid ca rtilage and is inferior to the space between the vocal cords (rima glot-
tid is) w here aspirated objects usuall y get lodged. The tracheotomy allows for air to
pass between the lungs and the outside air. Important: The space entered is cal led
the cricothyroid space.
Important: A cricothyrotomy is preferabl e to tracheostomy for non-surgeons in
emergency respiratory obstructions. In t his procedure, an incision is made throug h
SAADDES
the skin and cricothyroid membrane for t he relief of acute respiratory obstruction.
Note: A tracheotomy (tracheostomy) is rarely performed and is limited to patients with
extensive laryngeal damage and infants w ith severe airway obstruction. Because of
the presence of major vascu lar structures (carotid arteries and internal jugular vein), t he
thyroid g land, nerves (recurrent laryngeal branch of the vagus nerve), the pleural cav-
ities, and the esophagus, meticulous attention to anatomical detail has to be observed.
Laryngeal prominence (Adam's apple) is a protuberance that is formed by the angle
ofthe thyroid cartilage surround ing the larynx. This protuberance is more pronounced
in men.
Saad Alqahtani, Twitter @saaddes
respiratory system
Which of the following describes the function of the surfactant?
• increases the surface area of the alveoli
• reduces the attractive forces of 0 2 molecules and increases surface tension
• reduces the cohesive force of H 20 molecules and lowers surface tension
SAADDES
• increases the cohesive force of air molecules and raises surface tension
• none of the above
36
copyright Cl 20 13-2014 Dental Decks
ANATOMIC SCIENCES
Saad Alqahtani, Twitter @saaddes
• reduces the cohesive force of H 20 molecules and lowers surface tension
Surfactant is a complex substance containing phospholipids and a number of apopro-
teins. This essential fluid is produced by the Type II alveolar cells, and lines the alveoli
and smallest bronchioles. Surfactant reduces surface tension throughout the lung,
thereby contributing to its general compliance. It is also important because it stabi-
lizes the alveoli.
Neonatal respiratory distress syndrome (or respiratory d istress syndrome of new-
born) is a syndrome in premature infants caused by developmental insufficiency of
surfactant production and structural immaturi ty in the lungs. It begins shortly after
birth and is manifest by tachypnea, tachyca rdia, chest wall retractions (recession), ex-
SAADDES
piratory grunting, nasal fl aring and cyanosis during breathing efforts.
Cells of respiratory mucosa:
• Clara cells are dome-shaped cells w ith short m icrovilli found in the small airways
(bronchioles) of the lungs. Clara cells are found in the ci liated simple epithelium.
These cells may secrete glycosaminoglycans to protect t he bronchiole lining.
• Type I pneumocytes (simpl e squamous alveola r cells) are responsible for gas ex-
change in the alveoli and cover a majority of t he alveolar surface area (>95%).
• Type II pneumocytes are granular and roughly cubo idal in shape. They cover a
much smaller surface area t han type I cells (<5%). Their function is t he production
and secretion of surfactant (the majority of which are d ipalm itoylphosphatidyl-
choline), a g roup of phospholipids t hat reduce the alveola r surface tension.
• Alveolar macrophages (or dust cells) are type of macrophages found in the pul-
monary alveolus, near t he pneumocytes, but separated from the wall. Dust cells are
another name for monocyte derivatives in the lungs that reside on respiratory sur-
faces and cl ean off particles such as dust or microorganisms.
Saad Alqahtani, Twitter @saaddes
reproductive system
Ovulation occurs as a result of:
• the progesterone-induced LH surge
• the estrogen-induced FSH surge
• the progesterone-induced FSH surge
SAADDES
• the estrogen-induced LH surge
271
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• the estrogen-induced LH surge
High levels of estradiol occur around midcycle and exert positive feedback on gonadotropi n
secretion. This induces the LH (and a smaller FSH} surge. The midcycle gonadotropin surge
induces (a} meiotic maturation of the primary oocyte so that is prog resses to a secondary
oocyte (with on e polar body} arrested at metaphase of the second meiotic division, (b) break-
down of the ovarian and follicular wall so that the oocyte-cumulus complex is extruded (called
ovulation}, and (c) differentiation of t he remaining foll icular cell s into a corpus luteum. The
corpus luteum produces high levels of progesterone, estradiol and inhibin.
1. Without LH, even though large quantities of FSH are available, the follicle will not
progress to the stage of ovulation.
SAADDES
2.1f pregnancy does not occur, the corpus luteum will d ie in 14 days. This constitutes
the luteal phase of the menstrual cycle.
3. The oviducts capture the ovulated cumulus-oocyte complex and transport it med-
ially into the oviduct and toward the uterus. Important: Estrogen promotes ciliation
and transport; progesterone inhibits transport.
4. The uterine mucosa, called the endometrium, is the normal site of embryonic im-
plantation. The mucosa is increased in thickness in prepa ration for implantation and
is sloughed away if no pregnancy occurs.
5. One dominant follicle is selected per menstrual cycle (usually the largest follicle
with the most FSH receptors}.
6. FSH and LH are both glycoproteins and act in both the ovaries (in females} and
the testes (in males}.
Two significant results of the female sexual cycle are:
1. Only a single mature ovum is normally released from t he ovaries each month so that only
a single fetus can begin to grow at a time.
2. The uterine endometrium is prepared for implantation of the fertilized ovum at t he re-
quired time of the month.
Saad Alqahtani, Twitter @saaddes
Female Reproductive Cycles
cortex
Gonadotropin
cycle
This diagram illus trates the
SAADDES
interrelationships among the
cerebral, hypothalamic, pitu-
itary, ovarian, and uterine
functions throughout a stan-
dard 28-day menstrual cycle.
l11e variations in basal body
temperature are also illus-
trated.
Menstrual Postmenstrual Postmenstrual Menstru8.1 271·1
phase (proliferative Ovulation (secretory phase
phase) phase)
Saad Alqahtani, Twitter @saaddes
reproductive system
GnRH is produced by the:
• pituitary g land
• adrenal gland
• hypothalamus
• thyroid gland
SAADDES
273
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• hypothalamus
The reproductive systems are composed of gonads, an internal reproductive tract with associated
gland s and external genitalia. Mammary glands are accessory reproductive glands in women. Go-
nads have two main functions: production of gametes and production of hormones. Hormones (pri-
marily sex steroid s) are absolutely necessary for normal function of the reproductive system and t heir
production is regulated by a hypothalamic-pituitary-gonadal axis.
Seminiferous tubules in the testiscontain Sertoli cells and developing sperm cells. Spermatogen-
esis refers to the progression of sperm cells from spermatogonia through the processes of meiosisand
spermiogenesis to form mature spermatozoa.
Testosterone and pituitary FSH are required for normal sperm production. Only Sertoli cells express
the androgen receptor and the FSH receptor, so these hormones regulate spermatogenesis indirectly
SAADDES
through their actions on Sertoli cells. Sertoli cells produce the hormone inhibin, which negatively
feeds back on pituitary FSH production. Note: Sertoli cells have many functions, including the pro-
duction of androgen-binding protein (ABP) and fluid and creat ion of the blood-testis barrier. Leydig
cells are stromal cells that reside outside the seminiferous tubu les. They respond to LH by producing
testosterone.
Leydig cells are regulated within a hypothalamic-pituitary-test icular axis. The hypothalamus
produces GnRH, which sti mulates pituitary gonadotropes to secrete LH and FSH. Testosterone,
DHT and estradiol negatively feedback at the pituitary and hypothalamus and inhibit LH more than
FSH secretion. Important: lnhibin from the Sertoli cells selectively inhibits FSH.
Testosterone, DHT and estradiol have numerous actions on the male reproductive tract, external gen-
italia and male secondary sex characteristics, as well as on other organ systems (e.g., blood cell pro-
duction, lipoprotein production, bone maturat ion).
The male tract includ es tubal structures (epididymis, ductus deferensand male urethra), accessory
sex glands (seminal vesicles, prostate) and the penis. The seminal vesicles and the prostate produce
most of the ejaculate, which nourishes, buffersand protects sperm.
Remember: A male chil d is considered to have reached his full adult sexual capabilities at the end
of puberty. This means that after puberty the male child is capable of reproduction .
Saad Alqahtani, Twitter @saaddes
Spermatogenesis
~miniferous tubule
Type A
spermatogonia
Type A
spermatogonium
SAADDES
Meiosis I
~condary
spermatocytes
Melo51511
11 n n n n Spermatids
\, t t , "' 7 (2stagesof
n u u/ differentiation)
Spermiogenesis ( ( . ( (
++ t +
n LLLL Spermatozoa
lumen
273·1
Saad Alqahtani, Twitter @saaddes
reproductive system
Initiation of the onset of puberty has long been a mystery. But now it has
been determined that during childhood the hypothalamus simply does not
secrete significant amounts of GnRH.
For reasons still not understood, at the time of puberty, the secretion of
hypothalamic GnRH breaks through the childhood inhibition and adult
sexual life begins.
SAADDES
• both statements are true
• both statements are false
• the first statement is true, the second is false
• the first statement is false, the second is true
274
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are true
Initiation of the onset of puberty has long been a mystery. But now it has been determined that
duri ng childhood the hypothalamus simply does not secrete significant amounts of GnRH. One of
the reasons for this is that during childhood, the slightest secretion of any sex hormones exerts a
strong inhibitory effect on hypothalamic secretion of GnRH (gonadotropin releasing hormone).
Yet for reasons still not und erstood, at the time of puberty, the secretion of hypothalamic GnRH
breaks throug h the childhood inhibition and adult sexual life begins.
On average, females reach puberty 1 or 2 years earlier than males. In females, puberty is marked
by the first episode of menstrual bleeding, which is called menarche. The period of puberty is
caused by a grad ual increase in GnRH secretion by the hypothalamus, beginning in about the eighth
year of life and culminating in the onset of puberty and menstruation between the ages 11 and 16
SAADDES
years in girls (average, 13 years). Note: In the females, as in the male, the infantile pituitary gland and
ovaries are capable of full function if appropriately stimulated. However, as is also true in the male,
and for reasons not understood, the hypothalamus does not secrete significant quantities of GnRH
during childhood.
1. The events of puberty in the female (such as enlargement of the vagina, uterus and
B uterine tubes; deposition of fat in the breasts and hips) are largely a result of increased
production of estrogens by the ovaries.
2. Estrogen is effective at very low concentrations and generates a slowly developing
long-term response in target tissues by binding to an intracellular receptor.
3. Menopause results from exhaustion of the ovarian reserve and is characterized by low
ovarian hormone and elevated gonadotropin levels.
4. The follicle is the functional unit of the ovary. Follicles contain epithelial cells (granulosa
and cumulus) and outer stromal cells(thecal). All these cells surround the primary oocyte
that remains arrested in the first meiotic prophase until just before ovulation.
5. Follicles develop from the smallest (primordial) to a large antral follicle over a period of
months. The latter part of the follicular development requires gonadotropins.
Saad Alqahtani, Twitter @saaddes
reproductive system
The first half of the monthly menstrual cycle is referred to as the luteal
phase.
The second half of the monthly menstrual cycle is referred to as the follicular
phase.
SAADDES
• both statements are true
• both statements are false
• the first statement is t rue, the second is false
• the first statement is fa lse, the second is true
272
copyright Cl 20 13-2014 Dental Decks
BIOCHEMISTRY/PHYSIOLOGY
Saad Alqahtani, Twitter @saaddes
• both statements are false
The menstrual cycle refers to an approximately 28-day cycle d riven by the following ovarian
events:
• Development of one large antral follicle to a preovulatory follicle (the follicular phase}
• Ovulation
• The formation and death of a corpu s luteum of menstruation (the luteal phase}
The first half of the mont hly menstrual cycle is referred to as the follicular phase of the ovary.
This phase corresponds to the menstrual and proliferative phases of the uteri ne endometri um.
The second half of the monthly menstrual cycle is referred to as the luteal phase of the ovary.
This phase is dominated by hormonal secretions of the corpus luteum.
During the mid to late follicular phase (days 6 to 14 of the menstrual cycle}, the ovary pro-
SAADDES
d uces estradiol, which induces all cells of the endometrium to proliferate (called the prolifera-
t ive phase of the uterus}. After ovula tion, the ovary enters the luteal phase (days 16 to 28} and
produces progesterone. Progesterone stimulates secretion from the uterine g lands (called the
secretory phase of the uteru s}.
In the absence of an implanting embryo, t he corpus luteum dies, progesterone production
ceases and t he uterine endometrium is sloughed. This is called the menstrual, or period, of the
uterus and corresponds to days 1 to 5 of the follicular phase of the ovary.
*** Decreasing estrogen and progesterone levels sti mulate the hypothalamus to produce
GnRH and the cycle begins again.
The cervix is the lower portion of the uterus. Cervica l mucus is hormonally regulated so t hat
at midcycle in response to estrogen, cervical mucus promotes entry of sperm into t he uterus
from the vagina. During t he lutea l phase in response to progesterone, cervical mucus be-
comes thick and poses a barrier to entry of sperm and microbes into the uterus.
Fertilization is a complex series of events t hat occur in the oviduct and lead to penetration of
t he oocyte by sperm .
Saad Alqahtani, Twitter @saaddes
Ovarian Cycle
.. t
Prim.,ry $t(()nd,sory Vtsiw Mr CO'l)u$ luttum RttrtSSiO<n Cwpu'
foll ~'k r(l(l;d.- r<:~llict..~ room ~lbit.-.ns
SAADDES
Ovulation chart showing ovar ian cycle and uterine cycle
272-1
Saad Alqahtani, Twitter @saaddes
Das könnte Ihnen auch gefallen
- (DD13 14) Bio PhysioDokument587 Seiten(DD13 14) Bio PhysiominiarNoch keine Bewertungen
- DISACCHARIDES Lecture For 1st Year MBBS Delivered by Dr. Waseem On 01 March 2010Dokument29 SeitenDISACCHARIDES Lecture For 1st Year MBBS Delivered by Dr. Waseem On 01 March 2010IMDCBiochemNoch keine Bewertungen
- DD17 Biochemistry and PhysiologyDokument576 SeitenDD17 Biochemistry and PhysiologyFujiNoch keine Bewertungen
- Carbohydrates Part 2Dokument35 SeitenCarbohydrates Part 2glenn johnstonNoch keine Bewertungen
- Lecture 17 - Glycosides Intro, ClassificationDokument6 SeitenLecture 17 - Glycosides Intro, Classificationahsanonweb1983Noch keine Bewertungen
- CarbohydratesDokument48 SeitenCarbohydratesTrescia Mae EstilloreNoch keine Bewertungen
- Glycosides SAE ADDokument47 SeitenGlycosides SAE ADAsif SaleemNoch keine Bewertungen
- 03 CarbohydrateDokument45 Seiten03 CarbohydrateManojitNoch keine Bewertungen
- Biochemistry Midterm Carbohydrates: ClassificationsDokument21 SeitenBiochemistry Midterm Carbohydrates: ClassificationsArah Lyn ApiagNoch keine Bewertungen
- Carbohydrate Bhavishya 1Dokument21 SeitenCarbohydrate Bhavishya 1Bhavishya ParmarNoch keine Bewertungen
- DR Youssra Al-HilalyDokument54 SeitenDR Youssra Al-HilalyAymen AbdulrahmanNoch keine Bewertungen
- 2 Carbohydrates-Part 2 2022Dokument45 Seiten2 Carbohydrates-Part 2 2022MarieFranz ChuaNoch keine Bewertungen
- 1 A (11) CarbohydratesDokument12 Seiten1 A (11) Carbohydratesenakshi perusingheNoch keine Bewertungen
- Absorbation and Digestion of CarbohydratesDokument49 SeitenAbsorbation and Digestion of CarbohydratesBehailu TsegayeNoch keine Bewertungen
- 4.digestion of CarbohydratesDokument45 Seiten4.digestion of CarbohydratesEkber IsmayilovNoch keine Bewertungen
- Carbohydrate Part IDokument32 SeitenCarbohydrate Part IHamza QaziNoch keine Bewertungen
- Carbohydrates: DR Nazakat Hussain Assistant ProfessorDokument55 SeitenCarbohydrates: DR Nazakat Hussain Assistant ProfessorMuhammad JamalNoch keine Bewertungen
- CarbohydratesDokument112 SeitenCarbohydratesmaryam ijazNoch keine Bewertungen
- Biographic of YogiDokument22 SeitenBiographic of YogiKaveen VijayNoch keine Bewertungen
- Carbohydrates: Presented byDokument28 SeitenCarbohydrates: Presented byHans Christian MacasaNoch keine Bewertungen
- Glycosaminoglycan: Mukesh Dhital Asst - Prof.Clinical BiochemistryDokument14 SeitenGlycosaminoglycan: Mukesh Dhital Asst - Prof.Clinical BiochemistrymukeshNoch keine Bewertungen
- Carbohydrates 27.8.20 FN 202Dokument39 SeitenCarbohydrates 27.8.20 FN 202Mahmudur RahmanNoch keine Bewertungen
- Carbohydrates - DisaccharidesDokument3 SeitenCarbohydrates - DisaccharidesCamille Ann Faigao FamisanNoch keine Bewertungen
- Module 6 - CarbohydratesDokument76 SeitenModule 6 - CarbohydratesPauline Grace CadusaleNoch keine Bewertungen
- Di and PolysaccharideDokument17 SeitenDi and PolysaccharideafrNoch keine Bewertungen
- L4 CarbohydratesDokument21 SeitenL4 Carbohydrateshaiqalfariq07Noch keine Bewertungen
- Biochemistry - CarbohydratesDokument40 SeitenBiochemistry - CarbohydratesBalakrishnan RengeshNoch keine Bewertungen
- Biochemistry I (SGS 236)Dokument33 SeitenBiochemistry I (SGS 236)Mustafa SaßerNoch keine Bewertungen
- GlycolysisDokument51 SeitenGlycolysisKazar ProbusNoch keine Bewertungen
- Metabolism of Carbohydrates - 2Dokument67 SeitenMetabolism of Carbohydrates - 2gostrider0093sNoch keine Bewertungen
- OutputDokument12 SeitenOutputMarielle VentulaNoch keine Bewertungen
- Called Saccharides Most Abundant Molecules On Earth Essential Component of All Living OrganismsDokument32 SeitenCalled Saccharides Most Abundant Molecules On Earth Essential Component of All Living OrganismsShyla ManguiatNoch keine Bewertungen
- Glycosides 1Dokument11 SeitenGlycosides 1thetmaroothetmaroo42Noch keine Bewertungen
- CarbohydratesDokument64 SeitenCarbohydratesErwin CredoNoch keine Bewertungen
- Biologically Importants of Carbohydrates Students Lecture NotesDokument10 SeitenBiologically Importants of Carbohydrates Students Lecture NotesKRISTINE CHAD NAVALES CANTALEJONoch keine Bewertungen
- Lecture 6-Carbohydrates Spring 24Dokument25 SeitenLecture 6-Carbohydrates Spring 24ziadwageh74Noch keine Bewertungen
- I Dun Like Study (Print Ver) - Levi FINALDokument12 SeitenI Dun Like Study (Print Ver) - Levi FINALlevisha suppiahNoch keine Bewertungen
- Chapter 4: Chemical Composition of Cell: CarbohydratesDokument16 SeitenChapter 4: Chemical Composition of Cell: CarbohydratesHema LataNoch keine Bewertungen
- CarbohydratesDokument35 SeitenCarbohydratesRaincel Mae WarnacNoch keine Bewertungen
- 9 ชีวพลังงานและเมแทบอลิซึมของคาร์โบไฮเดรตDokument41 Seiten9 ชีวพลังงานและเมแทบอลิซึมของคาร์โบไฮเดรต22vk6svnb4Noch keine Bewertungen
- Carbohydrate PPT in PDFDokument23 SeitenCarbohydrate PPT in PDFsadaf zaidiNoch keine Bewertungen
- 2 - CarbohydratesDokument25 Seiten2 - CarbohydratesEDISON DE LOS SANTOSNoch keine Bewertungen
- Carbohydrates: Chapter 7 (Part II)Dokument19 SeitenCarbohydrates: Chapter 7 (Part II)Omer KareemNoch keine Bewertungen
- Digestion of CarbohydratesDokument30 SeitenDigestion of CarbohydratesRona May EsperanzateNoch keine Bewertungen
- CarbohydratesDokument10 SeitenCarbohydratesAtul KumarNoch keine Bewertungen
- CarbohydratesDokument22 SeitenCarbohydratesgifty NambeyeNoch keine Bewertungen
- Carbohydrates ReviewerDokument6 SeitenCarbohydrates ReviewerNino D. AtilanoNoch keine Bewertungen
- Complex Carbohydrates - GlycoproteinsDokument28 SeitenComplex Carbohydrates - GlycoproteinsJessica SannohNoch keine Bewertungen
- Carbohydrates: Biological MoleculesDokument50 SeitenCarbohydrates: Biological MoleculesRalph FranciscoNoch keine Bewertungen
- Aakash Modules 06Dokument125 SeitenAakash Modules 06tenn84269Noch keine Bewertungen
- Karbohidrat: Dyke Gita Wirasisya, S.Farm., M.SC., Apt Program Studi Farmasi, Fakultas Kedokteran, Universitas MataramDokument37 SeitenKarbohidrat: Dyke Gita Wirasisya, S.Farm., M.SC., Apt Program Studi Farmasi, Fakultas Kedokteran, Universitas Matarambrahmani ptrNoch keine Bewertungen
- Carbohydrates 131204014552 Phpapp02 PDFDokument27 SeitenCarbohydrates 131204014552 Phpapp02 PDFTweenie Dalumpines100% (4)
- CH 7Dokument29 SeitenCH 7Àhmâd ÂqéłNoch keine Bewertungen
- Carbohydrates Lecture 1Dokument52 SeitenCarbohydrates Lecture 1hafsaharshadNoch keine Bewertungen
- CARBOHYDRATEDokument14 SeitenCARBOHYDRATEAbhay PatelNoch keine Bewertungen
- Plasma Glycoproteins, Proteoglycans and MucinDokument73 SeitenPlasma Glycoproteins, Proteoglycans and MucinJacob MasikaNoch keine Bewertungen
- Carbohydrates Part 2Dokument48 SeitenCarbohydrates Part 2biotecnika_testNoch keine Bewertungen
- Fast Facts: Long-Chain Fatty Acid Oxidation Disorders: Understand, identify and supportVon EverandFast Facts: Long-Chain Fatty Acid Oxidation Disorders: Understand, identify and supportNoch keine Bewertungen
- PediatricDokument190 SeitenPediatricسامي التريكيNoch keine Bewertungen
- Ortho13 14Dokument64 SeitenOrtho13 14priyasargunan100% (4)
- Ortho13 14Dokument64 SeitenOrtho13 14priyasargunan100% (4)
- Ortho13 14Dokument64 SeitenOrtho13 14priyasargunan100% (4)
- P436 Lect 10p5Dokument15 SeitenP436 Lect 10p5Zhenhua HuangNoch keine Bewertungen
- Mobil Dte 20Dokument3 SeitenMobil Dte 20alexander900616Noch keine Bewertungen
- Complete Physical Chemistry McqsDokument13 SeitenComplete Physical Chemistry Mcqszafarchem_iqbalNoch keine Bewertungen
- Indian School Muscat: Senior Section Department of ChemistryDokument1 SeiteIndian School Muscat: Senior Section Department of ChemistryRitaNoch keine Bewertungen
- E3877 Optics FormulasDokument6 SeitenE3877 Optics FormulasKaran DoshiNoch keine Bewertungen
- 1989 - Rapid Extraction of Bacterial Genomic DNA With Guanidium ThiocyanateDokument6 Seiten1989 - Rapid Extraction of Bacterial Genomic DNA With Guanidium ThiocyanateramarquezoNoch keine Bewertungen
- Determination of Bendamustine Hydrochloride in Pure and Dosage Forms by Ion-Associative Complex FormationDokument6 SeitenDetermination of Bendamustine Hydrochloride in Pure and Dosage Forms by Ion-Associative Complex FormationHeidi HughesNoch keine Bewertungen
- Why Use Nitrogen To Purge MoistureDokument2 SeitenWhy Use Nitrogen To Purge MoistureketasriNoch keine Bewertungen
- Chemistry and Standardization of Bakuchi Oil An Ayurwedic Medicial Oil Used Trasditionally in Thee Treatment of Vitiligo PDFDokument155 SeitenChemistry and Standardization of Bakuchi Oil An Ayurwedic Medicial Oil Used Trasditionally in Thee Treatment of Vitiligo PDFTopala SorinNoch keine Bewertungen
- Nitrofuran Metabolit by Lcmsms (Just MSMS Method)Dokument4 SeitenNitrofuran Metabolit by Lcmsms (Just MSMS Method)Ageng Wahyu PatrianitaNoch keine Bewertungen
- Toluene Methylation To Para-XyleneDokument164 SeitenToluene Methylation To Para-XyleneAhmed AliNoch keine Bewertungen
- Induction HeatingDokument29 SeitenInduction HeatingwchavezbNoch keine Bewertungen
- Pub - Essentials of Nuclear Medicine Imaging 5th Edition PDFDokument584 SeitenPub - Essentials of Nuclear Medicine Imaging 5th Edition PDFNick Lariccia100% (1)
- Law of Errors: Errors in Measurement SystemDokument6 SeitenLaw of Errors: Errors in Measurement Systemrodrigo100% (1)
- 1.8 3 PVDF Hmwpe CableDokument1 Seite1.8 3 PVDF Hmwpe CableRobert LiraNoch keine Bewertungen
- Compressible Fluid FlowDokument41 SeitenCompressible Fluid FlowSushil Thakkar100% (1)
- M 3031 (2013-06)Dokument16 SeitenM 3031 (2013-06)Hatada FelipeNoch keine Bewertungen
- Separation Techniques WorksheetDokument2 SeitenSeparation Techniques WorksheetyuniNoch keine Bewertungen
- DPP 15-17 PDFDokument5 SeitenDPP 15-17 PDFAnkur GoyalNoch keine Bewertungen
- Background 1Dokument8 SeitenBackground 1KuIzzuNoch keine Bewertungen
- Bilberry PosterDokument1 SeiteBilberry PosterIrma Puspita DewiNoch keine Bewertungen
- Characteristics of Ionic CompoundsDokument4 SeitenCharacteristics of Ionic Compoundsjerm655Noch keine Bewertungen
- Sudhir Memorial Institute Chemistry Quantity of CaesinDokument16 SeitenSudhir Memorial Institute Chemistry Quantity of CaesinKi NgNoch keine Bewertungen
- Diagram PsychrometricDokument4 SeitenDiagram PsychrometricJanry EfriyantoNoch keine Bewertungen
- 06 05 16 Heko Bucket ElevatorDokument36 Seiten06 05 16 Heko Bucket ElevatorLeoncio Alexander Maza InfantesNoch keine Bewertungen
- Polymers Unit IIIDokument33 SeitenPolymers Unit IIIdinnu14Noch keine Bewertungen
- Molecular Laboratory Design QAQC Considerations PDFDokument46 SeitenMolecular Laboratory Design QAQC Considerations PDFSIDNoch keine Bewertungen
- Production of Liquid Fuel From Plastic Waste Using Integrated Pyrolysis Method With Refinery Distillation Bubble Cap Plate Column-1Dokument9 SeitenProduction of Liquid Fuel From Plastic Waste Using Integrated Pyrolysis Method With Refinery Distillation Bubble Cap Plate Column-1Bambang Sardi SardiNoch keine Bewertungen
- Kinetics of Oxidation of Ammonia in Solutions Containing Ozone With or Without Hydrogen PeroxideDokument6 SeitenKinetics of Oxidation of Ammonia in Solutions Containing Ozone With or Without Hydrogen PeroxideBrent WoottonNoch keine Bewertungen
- Homogeneous and Structured PCD-WC-Co Materials For DrillingDokument9 SeitenHomogeneous and Structured PCD-WC-Co Materials For Drillingdan_cunningham_15Noch keine Bewertungen