Beruflich Dokumente
Kultur Dokumente
The Factors Affecting Morbidity and Mortality in Spontaneous Intracerebral Hematomas
Hochgeladen von
Riya CassendraCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
The Factors Affecting Morbidity and Mortality in Spontaneous Intracerebral Hematomas
Hochgeladen von
Riya CassendraCopyright:
Verfügbare Formate
Biomedical Research 2018; 29 (11): 2265-2269 ISSN 0970-938X
www.biomedres.info
The factors affecting morbidity and mortality in spontaneous intracerebral
hematomas.
Ömer Aykanat1*, Metin Ocak2
1Department of Neurosurgery, Medical Faculty, Ahi Evran University, Kırsehir, Turkey
2Department of Emergency, Medical Faculty, Ahi Evran University, Kırsehir, Turkey
Abstract
Objective: In this study, 33 patients with a diagnosis of spontaneous intracerebral hematomas were
investigated retrospectively and factors affecting morbidity and mortality were determined.
Materials and methods: In this study, 33 patients with a diagnosis of SIH in intensive care unit (ICU) of
Ahi Evran University Medical Faculty Hospital were retrospectively reviewed between the dates of
01.09.2016 and 30.11.2017. The factors affecting morbidity and mortality in these patients were studied
in detail by reviewing the patients’ age, gender, admission condition, GCS score, personal background,
hematoma location, hematoma volume, presence/absence of intraventricular hemorrhage, type of
therapy and discharge condition.
Results: The study included 18 female (54.5%) and 15 male patients (45.5%) whose ages were in the
range of 43-91. Seen in 21 patients (63.6%), blackout was the leading cause for the admission. As a result
of the neurological examination on admission, of all the patients, GCS scores of 11 patients (33.3%) were
in the range of 3-7; it was between 8-13 in 17 patients (51.5%) and between 14-15 in 5 patients (15.1%).
When their personal bacgrounds were reviewed, hypertension in 19 patients (57.6%) was seen as the
most common etiological factor. We observed lobar region was the most frequent site for the
spontaneous intracerebral hematomas. 3 patients (9.1%) were applied surgical operation, 4 patients
(12.1%) were applied External Ventricular Drainage and 26 patients (78.8%) were followed up with
medical treatment. The follow-up length of the patients varied in the range of 3-72 days. While 13
patients (39.4%) were discharged with a full-recovery and 5 patients with morbidity (15.%), the other 15
patient (45.5%) died.
Conclusion: As a conclusion, it could be said that while hematoma volume, hematoma location and
presence/absence of intraventricular hemorrhages have significant effect on morbidity and mortality in
SIHs, the most significant factor is the patients’ GCS on admission. In our study, age had no significant
effect on mortality and morbidity.
Keywords: Intracerebral hematoma, Spontaneous, Morbidity, Mortality.
Accepted on April 16, 2018
Introduction and comorbid diseases [5]. While the golden standard is brain
Computed Tomography (CT) for diagnosis, in some cases
Spontaneous intracerebral hematomas (SIHs), which are Magnetic Resonance Imaging (MRI) can also be used. Surgical
intraparenchymal hemorrages result from various nontraumatic or medical therapy can be chosen for treatment depending on
causes, were first defined by Charles Baplesy in 1932 [1]. the age of patient, GCS score, location and volume of
Being one of the leading causes of cerebrovascular diseases hematoma.
and having about 15/10.000 rate of incidence, SIHs has a 50%
monthly mortality rate [2]. Etiology of SIHs comprise of such In this study, 33 patients with a diagnosis of SIH in intensive
vascular pathologies as anti-coagulant usage, amyloid care unit (ICU) of Ahi Evran University Medical Faculty
angiopathy, anteriovenous malformation and use of alcohol. Hospital were retrospectively examined and the factors
However, the most common etiological factor is hypertension affecting morbidity and mortality in the patients were studied
(HT) [3,4]. The condition of the patients during emergency with literature between the dates of 01/09/2016 and
ward admission varies depending on the volume and location 30/11/2017.
of hematoma and the age of patient. However, the disease
prognosis, vary by Glasgow Coma Scale (GCS) during hospital
admission, presence/absence of intraventricular hemorrhage
Biomed Res 2018 Volume 29 Issue 11 2265
Aykanat/Ocak
Materials and Methods
In this study, 33 patients with a diagnosis of SIH in intensive
care unit (ICU) of Ahi Evran University Medical Faculty
Hospital were retrospectively reviewed between the dates of
01/09/2016 and 30/11/2017. The factors affecting morbidity
and mortality in these patients were studied in detail by
reviewing the patients’ age, gender, admission condition, GCS
score, personal background, hematoma location, hematoma
volume, presence/absence of intraventricular hemorrhage, type
of therapy (surgical or medical) and discharge condition. In our
study, we reviewed spontaneous supratentorial hematomas but
we excluded infratentorial and traumatic ones and the ones
caused by tumor and vascular malformation.
The ethical approval was obtained from the ethics committee
of Medical Faculty in Ahi Evran University on 13/02/2018
with 2018-03/36 code number.
Results
The study included 18 female (54.5%) and 15 male patients
(45.5%) whose ages were in the range of 43-91 and the mean
age was 70. Seen in 21 patients (63.6%), blackout was the
leading cause for the admission, followed by hemiparesis in
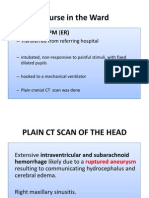
right/left part of body seen in 9 patients (27.3%) and headache Figure 1. The size of hematomas, calculated by measuring x-y-z axes
seen in 7 patients (21.2%) respectively. As a result of the on CT image.
neurological examination on admission, of all the patients,
GCS scores of 11 patients (33.3%) were in the range of 3-7; it The age range of the patients discharged with full-recovery was
was between 8-13 in 17 patients (51.5%) and between 14-15 in 48-91 and the average age was 69. Their GCSs on admission
5 patients (15.1%). When their personal bacgrounds were were in the range of 12-15. While 9 out of these 13 patients
reviewed, hypertension (HT) in 19 patients (57.6%) was seen had lobar hematomas and 1 patient had basal ganglia
as the most common etiological factor, followed by hematoma, the others had thalamic hematomas. The hematoma
anticoagulant use (36.4%) and 5 patients (15.1%) had no any volumes were between 1 ml-30 ml and the average value was
case history. All the patients were diagnosed with brain CT. We 10.2 ml. We observed presence of intraventricular hemorrhage
observed lobar hematoma in 16 patients (48.5%); thalamic only in 1 out of 4 patients who had thalamic and basal ganglia
hematoma in 14 patients (42.4%) and basal ganglia hematoma hematomas. Age range of the patients disharged with
in 3 patients (9.1%). Moreover, we observed the presence of morbidity was 43-77 and the average age was 66.6. Their GCS
intravenricular hemorrhage in 10 out of 17 patients having range was 7-12 on admission. While 1 out of 5 patients had
thalamic and basal ganglia hematomas. The size of hematomas lobar hematoma, the other 4 ones had thalamic hematomas.
were calculated by measuring x-y-z axes on CT images (Figure The hematoma volumes were between 7.5 ml-75 ml and the
1). The volume of hematomas were seen to be in the range of 1 average value was 28.8 ml. We observed presence of
ml-105 ml and the average volume was 19.6 ml. 3 patients intraventricular hemorrhage only in 2 out of 4 patients who had
(9.1%) were applied surgical operation (hematoma evacuation thalamic hematomas. Age range of the patients having died
by craniotomy); 4 patients (12.1%) were applied External was 53-91 and the average age was 69.6. Their GCS range was
Ventricular Drainage (EVD) and 26 patients (78.8%) were 3-11 on admission. While 4 out of 15 patients had lobar
followed up with medical treatment. The follow-up length of hematoma, 9 patients had thalamic hematomas, the other 2
the patients varied in the range of 3-72 days. While 13 patients ones had basal ganglia hematomas. The hematoma volumes
(39.4%) were discharged with a full-recovery and 5 patients were between 2 ml-105 ml and the average value was 25.8 ml.
with morbidity (15.1%), the other 15 patients (45.5%) died We observed presence of intraventricular hemorrhage only in 7
(Table 1). out of 11 patients who had thalamic and basal ganglia
hematomas.
Table 1. Distribution of the patients’ age, gender, complaints, GCS, case history and discharce condition and the distribution of localization and
volume of hematomas and presence/absence of intraventricular hemorrhage.
Age Gender Complaint GCS on Case History Localization Volume Presence/Absence of Outcome
Admission (ml) Intraventricular
hemorrhage
2266 Biomed Res 2018 Volume 29 Issue 11
The factors affecting morbidity and mortality in spontaneous intracerebral hematomas
74 F blackout 4 HT Left thalamic 22.5 + Exitus
91 F blackout 13 HT, Aspirin Left parietal 7.5 - Full recovery
85 F blackout, Right 9 HT, Coraspin Left parietooccipital 18 - Exitus
hemiparesis
84 M blackout 12 HT Right thalamic 6 + Full recovery
78 F blackout, Right 4 DM Left thalamic 33 + Exitus
hemiparesis
56 F blackout 3 Coraspin Right thalamic 15 + Exitus
71 F blackout 4 HT Left parietal 12 - Exitus
68 F blackout, Headache 13 CAD, AF, Coraspin Left frontal 15 - Full recovery
77 F Headache , Left 12 CVA, ARF, Coraspin Right temporal 24 - Morbid
hemiparesis
75 M blackout 7 HT, CVA, Coraspin Left temporoparietal 75 - Morbid
60 M blackout 5 HT, Aspirin Left thalamic 2 + Exitus
53 M Headache 14 No case history Left parietal 30 - Full recovery
79 F blackout 5 CVA, Aspirin Left thalamic 50 + Exitus
75 M blackout 9 No case history Right thalamic 7.5 + Morbid
74 F blackout 5 HT Left thalamic 20 + Exitus
49 F Facial Paresthesia 15 HT Left parietal 13.5 - Full recovery
77 M blackout, Left hemiparesis 12 HT Right thalamic 6 - Full recovery
76 M Left hemiparesis 13 No case history Right parietal 13.5 - Full recovery
43 F Right hemiparesis 10 HT Left thalamic 24 - Morbid
48 M Headache, Left 13 No case history Right basal ganglia 2 - Full recovery
hemiparesis
59 F Gait and speech disorder 12 HT Left parietal 18 - Full recovery
81 M Left hemiparesis 12 Dementia, Aspirin Right temporal 8 - Full recovery
55 F blackout 9 No case history Left basal ganglia 15 - Exitus
91 F blackout 11 HT, Aspirin Left frontal 3 - Exitus
56 M Drowsiness 14 No case history Left frontal 6 - Full recovery
66 M Diplopia, Drowsiness 14 HT Right thalamic 7 - Full recovery
61 M blackout, Left hemiparesis 11 HT Right thalamic 18 - Exitus
55 M blackout 6 CVA, Aspirin, Alcohol Left thalamic 45 + Exitus
79 F blackout 6 HT Right parietal 105 - Exitus
80 F blackout 8 HT, Aspirin Left basal ganglia 4 - Exitus
90 M Headache, Drowsiness 14 HT Right parietal 1 - Full recovery
63 M blackout, Right 11 HT, DM Left thalamic 13.5 + Morbid
hemiparesis
77 F blackout 5 HT Right temporal 24.5 - Exitus
GCS: Glasgow Coma Score; HT: Hypertension; DM: Diabetes Mellitus; CAD: Coronary Artery Disease; AF: Atrial Fibrilation; CVA: Cerebrovascular Accident; ARF: Acute
Renal Failure
Biomed Res 2018 Volume 29 Issue 11 2267
Aykanat/Ocak
Discussion and Conclusion were more effective on morbidity and mortality while in others
presence/absence of intraventricular hemorrhage or location
Spontaneous Intracerebral Hematomas (SIHs), which are (thalamic and basal ganglia hematomas) of hematomas had
defined as intraparenchymal hemorrhage without trauma, has more effect on them. The primary aim of medical treatment is
an average incidence rate of 15/100000 but the rate has been to bring intracranial and cerebral perfusion pressures back to
indicated to vary in the range of 12-51.8/100000 [5-10]. About normal or at least near-normal values, to stabilize the vital
one fifth of SIHs are supratentorial. Some studies have signs of patients and to assure epileptic attack prophylaxis.
indicated that SIHs occur more frequently in 5th and 6th Whereas, the primary aim of surgical treatment is to evacuate
decades of lifespan and are seen more in males and gender has hematoma and to eliminate its pressure on surrounding
no significant effect on mortality [4-6,11]. As opposed to parenchyma tissue and as a result to decrease intracranial
literature, in our case serial, 72.7% of the patients had ages in pressure and reduce secondary cerebral damage. Ultimate aim
and above 7th decade and 80% of the 15 patients who died of the both treatment types is to minimize morbidity and
were females. The most significant risk factor is HT in mortality. In our case study, 3 patients were applied hematoma
literature, followed by old age, use of anticoagulant, DM evacuation via craniotomy; 4 patients were applied EVD and
(diabetes mellitus), alcohol, obesity, vascular malformations the others were followed up with medical treatment. The type
and amiloid angiopathy [12-14]. In our study, HT and use of of treatment was determined by the volume of hematoma,
anticoagulant took the first and second place as etiological presence/absence of midline shift, neurologic state of the
factors with their rate of 57.6% and 36.4% respectively, which patient, regression in the presence of intraventricular
is compatible with literature. The fact that there was no risk hemorrhage and development hydrocephalus.
factor for 15.1% of the patients is quite interesting but it should
be kept in mind that a sudden HT attack might have occurred Many earlier studies have suggested that many SIHs have poor
in these patients. prognosis and the average mortality rate is in the range of
34-50% in SIHs regardless of the type of the treatment
There are variations in localization of SIHs. While some [15,19,21]. In our case serial, the average mortality rate was
studies point out basal ganglia and thalamic region, others refer 45.5%, which was compatible with literature. While one of the
to lobar region as the most common location for SIHs [15-18]. 3 patients who had surgical treatment died, one of them was
The variation might be caused by the geographical conditions discharged with morbidity and one was discharged with full
of the region where the study is conducted; feeding habits of recovery. While all of 4 patients who were applied EVD died,
the patients and racial differences. One common point in all only 10 out of 26 patients followed up with medical treatment
studies conducted up to now is that they indicate basal ganglia died. In our case serial, the patients having >30 ml hematoma
and thalamic regions as the most common location for HT- volume in thalamic and basal ganglia hematomas were
induced SIHs. However, in our study, lobar region was the observed to have higher morbidity and mortality rate. All the
most common location with a rate of 48.5%, which was patients, regardless of outcome (full-recovery, morbidity,
followed by thalamic and ganglia regions with degressive rates mortality), had both deep (basal ganglia and thalamic) and
respectively. As opposed to literature, we observed thalamic superficial (lobar) hematomas in terms of localization; >30 ml
hematomas in 50% of the patients who had no anticoagulant and <30 ml hematomas in terms of volume; present and absent
use but HT trouble in their case histories and lobar hematoma of intraventricular hemorrhages. Age had no significant effect
in the other half. Furthermore, 66.6% of six patients who had on morbidity, mortality or full-recovery. However, the patients
both anticoagulant use and HT in their case histories were discharged with full recovery were observed to have ≥ 12 GCS
observed to have lobar hematomas and the remaining ones to on admission while morbid or mortal patients had ≤ 11 GCS.
have thalamic and basal ganglia hematomas. Since brain CT
has high diagnostic value in acute hemorrhages and is easily As a conclusion, it could be said that while hematoma volume,
accessible, it is the gold standard method for diagnosis of SIH hematoma location and presence/absence of intraventricular
which itself is a kind of acute hemorrhage as well. However, in hemorrhages have significant effect on morbidity and mortality
tumor and vascular malformation-induced hemorrhages, MRI in SIHs, the most significant factor is the patients’ GCS on
could be used to explain the underlying causes. Since we admission. In our study, age had no significant effect on
excluded tumor and vascular malformation-induced mortality and morbidity.
hemorrhages from our study, we used only brain CT for
diagnosis in all patients in the study. References
The type of treatment in SIHs could be surgical (evacuation of 1. Ozer F, Elmacı İ, Aysal F, Ataklı D, Arpacı B.
hematoma via craniotomy or external ventricular drainage spontaneous intracerebral hematoma: Analysis of 177
(EVD) or medical. The type of treatment varies depending on cases. J Dusunen Adam 1991; 4: 64-70.
the age, GCS on admission, volume of hematoma, presence/ 2. Ariesen MJ, Claus SP, Rinkel GJE, Algra A: Risk Faktors
absence of intraventricular hemorrhage and location of for ıntracerebral hemorrhage in the general population.
hematoma. Several studies have stated that the volume of Stroke 2003; 34: 2060.
hematoma, presence/absence of intraventricular hemorrhage 3. Ovül I, Tucbay E, Mutluer S. Spontaneous
and location of hematoma are fairly significant forpatients’ intraparenchymal hematomas. Cerebrovascular Diseases.
prognosis [15,18-21]. In some studies, >30 ml hematomas Izmir, EÜTF Publishing House 1985; 209-221.
2268 Biomed Res 2018 Volume 29 Issue 11
The factors affecting morbidity and mortality in spontaneous intracerebral hematomas
4. Qureshi AI, Giles WH, Croft JB. Racial differences in the haemorrhage in a referral hospital in the central-western
incidence of intracerebral hemorrhage: Effects of blood region of Mexico. Rev Neurol 2005; 40: 656-660.
pressure and education. Neurology 1999; 52: 1617-1621. 14. Skidmore CT, Andrefsky J. Spontaneous intracerebral
5. Anderson CS, Chakera TMH, Stewart-Wynne EG, hemorrhage: epidemiology, pathophysiology, and medical
Jamrozik KD. Spectrum of primary intracerebral management. Neurosurg Clin N Am 2002; 13: 281-288.
haemorrhage in Perth, Western Australia, 1989-1990: 15. Cole FM, Yates PO. Intracerebral microaneurysms and
incidence and outcome. J Neurol Neurosurg Psychiatry small cerebrovascular lesions. Brain 1967; 90: 759-768.
1994; 57: 936-940. 16. Thomas BD: Spontaneous intracerebral hemorrhage.
6. Van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Neurosurgery 1985; 1510-1517.
Algra A, Klijn CJ. Incidence, case fatality, and functional 17. Kase CS. Intracerebral hemorrage: Non-hypertensive
outcome of intracerebral haemorrhage over time, causes. Stroke 1986; 17: 590-594.
according to age, sex, and ethnic origin: A systematic 18. Eroglu A, Atabey C, Topuz KA, Colak A, Demircan N.
review and meta-analysis. Lancet Neurol 2010; 9: Evaluation of 104 cases with spontaneous intracerebral
167-176. hematoma. J Turk Norosirurji 2012; 22: 167-170.
7. Broderick JP, Brott T, Tomsick T, Huster G, Miller R. The 19. Kase CS, Mohr JP. General features of intracerebral
risk of subarachnoid and intracerebral hemorrhages in hemorrhage. Stroke 1986; 497-521.
blacks as compared with whites. N Engl J Med 1992; 326:
20. Tuhrim S, Horowitz DR, Sacher M, Godbold JH.
733-736.
Validation and comparison of models predicting survival
8. Broderick JP, Brott T, Tomsick T, Miller R, Huster G. followingintracerebral hemorrhage. Crit Care Med 1995;
Intracerebral hemorrhage more than twice as common as 23: 950-954.
subarachnoid hemorrhage. J Neurosurg 1993; 78:
21. Davis SM, Broderick J, Hennerici M, Brun NC, Diringer
188-191.
MN, Mayer SA, Begtrup K, Steiner T. Hematoma growth
9. Giroud M, Gras P, Chadan N, Beuriat P, Milan C, Arveux is a determinant of mortality and poor outcome after
P, Dumas R. Cerebral haemorrhage in a French intracerebral hemorrhage. Neurology 2006; 66:
prospective population study. J Neurol Neurosurg 1175-1181.
Psychiatry 1991; 54: 595-598.
10. Qureshi AI, Giles WH, Croft JB. Racial differences in the *Correspondence to
incidence of intracerebral hemorrhage: effects of blood
pressure and education. Neurology 1999; 52: 1617-1621. Ömer Aykanat
11. Little KM, Alexander MJ. Medical versus surgical therapy Department of Neurosurgery
for spontaneous intracranial hemorrhage Neurosurg Clin
N Am 2002; 13: 339-347. Medical Faculty
12. Raymond TFC, Liang-Yu Z. Use of original, modified or Ahi Evran University
new intracerebral hemorrhage score to predict mortality
and morbidity after intracerebral hemorrhage. Stroke Turkey
2003; 34: 1717.
13. Ruiz-Sandoval JL, Ortega-Alvarez L, García-Navarro V,
Romero-Vargas S, González-Cornejo S. Intracerebral
Biomed Res 2018 Volume 29 Issue 11 2269
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Practical MedicineDokument630 SeitenPractical MedicineYong Lim80% (5)
- Immunosuppressants - AMBOSS PDFDokument7 SeitenImmunosuppressants - AMBOSS PDFOpio IsaacNoch keine Bewertungen
- Gynecology: 3.09 - AmenorrheaDokument13 SeitenGynecology: 3.09 - AmenorrheaAnna Mae MarantanNoch keine Bewertungen
- Psychiatry HistoryDokument53 SeitenPsychiatry HistoryMarco Góis100% (5)
- Unani-Dr. Adnan MastanDokument37 SeitenUnani-Dr. Adnan Mastandradnan mastan100% (1)
- Nail PsoriasisDokument13 SeitenNail PsoriasisAira KellyNoch keine Bewertungen
- Physical Assessment - IntegumentDokument102 SeitenPhysical Assessment - IntegumentDeeeeeNoch keine Bewertungen
- Benign Prostatic Hyperplasia Concept MapDokument1 SeiteBenign Prostatic Hyperplasia Concept MapSarah RonquilloNoch keine Bewertungen
- Role of 50 Millesimal Potencies in Primary Dysmenorrhoea Updated PDFDokument106 SeitenRole of 50 Millesimal Potencies in Primary Dysmenorrhoea Updated PDFKamal Patidar50% (2)
- United Republic of Tanzania: Ministry of Health, Community Development, Gender, Elderly and ChildrenDokument50 SeitenUnited Republic of Tanzania: Ministry of Health, Community Development, Gender, Elderly and ChildrenHAMIS MASOUDNoch keine Bewertungen
- Klasifikasi VitiligoDokument49 SeitenKlasifikasi VitiligoVika LeiwaNoch keine Bewertungen
- Effects of Highquality Nursing On Puerpera With Pregnancy HypertensionDokument4 SeitenEffects of Highquality Nursing On Puerpera With Pregnancy HypertensionRiya CassendraNoch keine Bewertungen
- A Case of Virilization and Bilateral Krukenberg Tumours in Late PregnancyDokument4 SeitenA Case of Virilization and Bilateral Krukenberg Tumours in Late PregnancyRiya CassendraNoch keine Bewertungen
- Preclinical Developmental Toxicity Testing and Advanced Invitro Stem Cell BasedsystemsDokument3 SeitenPreclinical Developmental Toxicity Testing and Advanced Invitro Stem Cell BasedsystemsRiya CassendraNoch keine Bewertungen
- Primary Cutaneous Adenoid Cystic Carcinoma A Case Report and Dermoscopic FndingsDokument3 SeitenPrimary Cutaneous Adenoid Cystic Carcinoma A Case Report and Dermoscopic FndingsRiya CassendraNoch keine Bewertungen
- Clinical Effect of Atorvastatintrimetazidine Combined Treatment of Coronary Heart DiseaseDokument4 SeitenClinical Effect of Atorvastatintrimetazidine Combined Treatment of Coronary Heart DiseaseRiya CassendraNoch keine Bewertungen
- The Effects of Resistance Elastic Bands Exercises On Salivary Iga and Salivary Cortisol Levels in Elderly WomenDokument6 SeitenThe Effects of Resistance Elastic Bands Exercises On Salivary Iga and Salivary Cortisol Levels in Elderly WomenRiya CassendraNoch keine Bewertungen
- A Brief Insight Into The Role of Image Fusion in OncologyDokument2 SeitenA Brief Insight Into The Role of Image Fusion in OncologyRiya CassendraNoch keine Bewertungen
- High Dietary Diversity Is Associated With Child Obesity in Iranian School Children An Evaluation of Dietary Diversity ScoreDokument6 SeitenHigh Dietary Diversity Is Associated With Child Obesity in Iranian School Children An Evaluation of Dietary Diversity ScoreRiya CassendraNoch keine Bewertungen
- The Evaluation and Effect of Mental Health of Students Based On Ideological and Political Education InterventionDokument6 SeitenThe Evaluation and Effect of Mental Health of Students Based On Ideological and Political Education InterventionRiya CassendraNoch keine Bewertungen
- Causes Clinical and Imaging Characteristics of Moyamoya Disease in ChildrenDokument6 SeitenCauses Clinical and Imaging Characteristics of Moyamoya Disease in ChildrenRiya CassendraNoch keine Bewertungen
- Severe Septic Complications in A Diabetic Foot Decade After Multiple Injections of A Modeling AgentDokument5 SeitenSevere Septic Complications in A Diabetic Foot Decade After Multiple Injections of A Modeling AgentRiya CassendraNoch keine Bewertungen
- The Efficacy of Tdcs in The Treatment of Migraine A ReviewDokument8 SeitenThe Efficacy of Tdcs in The Treatment of Migraine A ReviewRiya CassendraNoch keine Bewertungen
- The Effects of Zhikang Capsule On The Growth and Apoptosis of Breast Cancer Mcf7Dokument4 SeitenThe Effects of Zhikang Capsule On The Growth and Apoptosis of Breast Cancer Mcf7Riya CassendraNoch keine Bewertungen
- Potential Role of A Recentlydiscovered Biologic HDFX in Prevention Andtreatment of Deadly Communicable Diseases Brought To WesternDokument5 SeitenPotential Role of A Recentlydiscovered Biologic HDFX in Prevention Andtreatment of Deadly Communicable Diseases Brought To WesternRiya CassendraNoch keine Bewertungen
- Longterm Complications of Modified Soave Radical Correction in The Treatment of Hirschsprungs Disease and Its Influences On Life QDokument4 SeitenLongterm Complications of Modified Soave Radical Correction in The Treatment of Hirschsprungs Disease and Its Influences On Life QRiya CassendraNoch keine Bewertungen
- Application of Tar Signature For Breast Mass AnalysisDokument5 SeitenApplication of Tar Signature For Breast Mass AnalysisRiya CassendraNoch keine Bewertungen
- Initial Serum Level of Il10 As An Outcome Predictor in Children With Sepsis PDFDokument5 SeitenInitial Serum Level of Il10 As An Outcome Predictor in Children With Sepsis PDFRiya CassendraNoch keine Bewertungen
- A Case of Inverted Follicular Keratosis With Onset Since ChildhoodDokument2 SeitenA Case of Inverted Follicular Keratosis With Onset Since ChildhoodRiya CassendraNoch keine Bewertungen
- Initial Serum Level of TNF As An Outcome Predictor in Pediatric Patient With SepsisDokument6 SeitenInitial Serum Level of TNF As An Outcome Predictor in Pediatric Patient With SepsisRiya CassendraNoch keine Bewertungen
- Salicylic Acid Mediated Salt Tolerance at Different Growth Stages of Oryza Sativa L and Its Effect On Salicylic Acid BioDokument18 SeitenSalicylic Acid Mediated Salt Tolerance at Different Growth Stages of Oryza Sativa L and Its Effect On Salicylic Acid BioRiya CassendraNoch keine Bewertungen
- Psychological Trauma of Primary Hypertension and The Best Treating ChoiceDokument6 SeitenPsychological Trauma of Primary Hypertension and The Best Treating ChoiceRiya CassendraNoch keine Bewertungen
- Factors Contributing To Nonadherence To Insulin Therapy Among Type 1 and Type2 Diabetes Mellitus Patients in Asser Region Saudi ArDokument6 SeitenFactors Contributing To Nonadherence To Insulin Therapy Among Type 1 and Type2 Diabetes Mellitus Patients in Asser Region Saudi ArRiya CassendraNoch keine Bewertungen
- The Threat of Carbapenemresistant Hypervirulent Klebsiella Pneumoniae CRHVKPDokument4 SeitenThe Threat of Carbapenemresistant Hypervirulent Klebsiella Pneumoniae CRHVKPRiya CassendraNoch keine Bewertungen
- A Noble Approach To Compute The Magnetic Flux Density Magnetic Forcedistribution and Its Application On Magnetic LevitationDokument8 SeitenA Noble Approach To Compute The Magnetic Flux Density Magnetic Forcedistribution and Its Application On Magnetic LevitationRiya CassendraNoch keine Bewertungen
- Uptake of As CD Cu Fe MN PB and ZN in Pasture Grasses On Three Metalcontaminated Soils From MontanaDokument7 SeitenUptake of As CD Cu Fe MN PB and ZN in Pasture Grasses On Three Metalcontaminated Soils From MontanaRiya CassendraNoch keine Bewertungen
- Pulmonary Hypertension in Pulmonary Agenesisa Report of Five Pediatric Cases and Review of Previous CasesDokument5 SeitenPulmonary Hypertension in Pulmonary Agenesisa Report of Five Pediatric Cases and Review of Previous CasesRiya CassendraNoch keine Bewertungen
- An Analysis of The Impact of Reference Groups On Collectivist Families Mealsocial Interaction Behaviour in Sierra LeoneDokument12 SeitenAn Analysis of The Impact of Reference Groups On Collectivist Families Mealsocial Interaction Behaviour in Sierra LeoneRiya CassendraNoch keine Bewertungen
- Retrospective Study of Cholangiocarcinomas Diagnosed in The Hospital of Fuenlabrada in The Period 20062016Dokument3 SeitenRetrospective Study of Cholangiocarcinomas Diagnosed in The Hospital of Fuenlabrada in The Period 20062016Riya CassendraNoch keine Bewertungen
- Depression and Determinant Factors Among Elderly in IndiaDokument2 SeitenDepression and Determinant Factors Among Elderly in IndiaRiya CassendraNoch keine Bewertungen
- A Clinical Vignette On Raoultella Planticola BacteremiaDokument5 SeitenA Clinical Vignette On Raoultella Planticola BacteremiaJamie FleetNoch keine Bewertungen
- Early Diagnosis of NeoplasisDokument25 SeitenEarly Diagnosis of NeoplasisDanielaNoch keine Bewertungen
- Medical Israeli Syllabus For Internal Medicine For Exam LicenseDokument4 SeitenMedical Israeli Syllabus For Internal Medicine For Exam Licensemohammadeid0% (2)
- A Case of Brain Death During PregnancyDokument52 SeitenA Case of Brain Death During PregnancyMa Pilar Peñaflor AñonuevoNoch keine Bewertungen
- EMBRYOLOGY 2nd Year Topical Past Papers 2005-22Dokument7 SeitenEMBRYOLOGY 2nd Year Topical Past Papers 2005-22HussnainNoch keine Bewertungen
- Hema Lec Week 16 Leukocyte Disorders Part 2Dokument4 SeitenHema Lec Week 16 Leukocyte Disorders Part 2Max RuideraNoch keine Bewertungen
- Medical Surgical Nursing QuestionsDokument7 SeitenMedical Surgical Nursing Questionseloisa mae gementizaNoch keine Bewertungen
- The Medical Management of Abnormal Uterine Bleeding in Reproductive-Aged WomenDokument14 SeitenThe Medical Management of Abnormal Uterine Bleeding in Reproductive-Aged Womendiegoesteban1234Noch keine Bewertungen
- SAMY MSK ArthritisDokument125 SeitenSAMY MSK ArthritisZintan HospitalNoch keine Bewertungen
- Goactive Brochure PDFDokument2 SeitenGoactive Brochure PDFsumitNoch keine Bewertungen
- PATHOPHYSIOLOGYDokument5 SeitenPATHOPHYSIOLOGYJoyce Ann CumlatNoch keine Bewertungen
- Aphasia and DysphasiaDokument8 SeitenAphasia and Dysphasiamoizghani37Noch keine Bewertungen
- Damps, Pamps, and Lamps in Immunity and Sterile InflammationDokument26 SeitenDamps, Pamps, and Lamps in Immunity and Sterile InflammationCony G100% (1)
- PhilHealth CF4Dokument2 SeitenPhilHealth CF4B MNoch keine Bewertungen
- Common Symptoms of Gastrointestinal and Abdominal DiseaseDokument34 SeitenCommon Symptoms of Gastrointestinal and Abdominal DiseaseMalueth AnguiNoch keine Bewertungen
- 1 Coagulation Disorderin PregnancyDokument21 Seiten1 Coagulation Disorderin PregnancyIntan Nursiani AgnurNoch keine Bewertungen
- (IM A) (Com Dse) Typhoid Fever (Strawberry)Dokument4 Seiten(IM A) (Com Dse) Typhoid Fever (Strawberry)NoreenNoch keine Bewertungen
- Ledderhose Disease: Pathophysiology Diagnosis and ManagementDokument3 SeitenLedderhose Disease: Pathophysiology Diagnosis and ManagementLeandro PolancoNoch keine Bewertungen
- Nej M CPC 2004992Dokument11 SeitenNej M CPC 2004992Deina IdlcNoch keine Bewertungen