Beruflich Dokumente
Kultur Dokumente
1619 Full PDF
Hochgeladen von
Jefta AlfatraOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
1619 Full PDF
Hochgeladen von
Jefta AlfatraCopyright:
Verfügbare Formate
ACR
APPROPRIATENESS
CRITERIA Head Trauma
Patricia C. Davis, for
the Expert Panel on
Neurologic Imaging
C raniocerebral injuries are a common cause of hospital ad-
mission following trauma, and are associated with signif-
icant long-term morbidity and mortality. CT remains essen-
verse relationship between declining clinical or neurologic sta-
tus as described by the GCS9 and the incidence and severity of
CT abnormalities related to head injury.10-12
tial for detecting lesions that require immediate neurosurgical Clinical selection criteria for CT scanning of patients with
intervention as well as those that require in-hospital observa- minor or mild injury (ie, GCS score ⬎12) who harbor signif-
tion and medical management.1 For patients with minor head icant intracranial pathology and/or require acute surgical in-
injury (Glasgow Coma Scale [GSG] score of 13–15), the New tervention have been problematic. Rapid CT scanning is
Orleans Criteria2 and the Canadian CT Head Rule3 are clinical readily available in most hospitals that treat head injured pa-
guidelines with high sensitivity for detecting injuries that re- tients; thus CT has value as a screening tool to triage minor or
quire neurosurgical intervention and offer a potential reduc- mild head-injured patients who require hospital admission or
tion in unnecessary CT scans.4-6 surgery from those who can be safely discharged without hos-
Other imaging modalities such as MR imaging depict non- pital admission.13-15 Although this approach offers reduced
surgical pathology not visible on CT. Cervical spine imaging is inpatient services and reduced cost, the result is greater CT use
indicated for patients with head injury who have signs, symp- in the emergency setting.11,13-15 In the minor head injury set-
toms, or a mechanism of injury that might result in spinal ting with a GCS score of 15, the New Orleans Criteria2 found
injury, and in those who are neurologically impaired (see the 100% sensitivity for CT identification of an acute trauma le-
ACR Appropriateness Criteria for Spine Trauma). sion by using risk factors of headache, vomiting, drug or alco-
hol intoxication, older than age 60, short-term memory defi-
ACR CRITERIA
Skull Radiography cit, physical findings of supraclavicular trauma, and/or
Masters et al7 developed and tested a management strategy seizure. Stiell et al3 reported 100% sensitivity for detecting
that shifted the focus of neuroimaging of head trauma away neurosurgical and/or clinically important brain injury in sub-
from skull radiography and toward CT scanning. Skull radi- jects with a GCS score of 13–15 based on high-risk factors of
ography is useful for imaging of calvarial fractures, penetrat- failure to reach a GCS score of 15 within 2 hours, suspected
ing injuries, and radiopaque foreign bodies. open skull fracture, 2 or more vomiting episodes, sign of basal
skull fracture, or age ⱖ65.
CT Clinical criteria for scanning of children with head injury have
CT advantages for evaluation of the head-injured patient in- been less reliable than those for adults, particularly for children
clude its sensitivity for demonstrating mass effect, ventricular younger than age 2.16,17 For this reason, more liberal use of CT
size and configuration, bone injuries, and acute hemorrhage. scanning has been suggested for pediatric patients. This must be
CT offers widespread availability, rapidity of scanning, and balanced with the higher risk of radiation exposure in childhood
compatibility with medical devices. Its limitations include in- via judicious patient selection for scanning as well as manage-
sensitivity in detecting small and nonhemorrhagic lesions ment of radiation dose.8,18,19 Noncontrast head CT plays an es-
such as contusion, particularly adjacent to bony surfaces. Like- sential role in the evaluation of children with suspected physical
wise, diffuse axonal injuries (DAIs) that result in small brain injury from child abuse (see the ACR Appropriateness Criteria
lesions go undetected on CT. CT is relatively insensitive for for Suspected Physical Abuse—Child).
detecting increased intracranial pressure or cerebral edema Early and repeated CT scanning may be required for dete-
and for early demonstration of hypoxic-ischemic encephalop- rioration, especially in the first 72 hours after head injury, to
athy (HIE) that may accompany head injury. Potential risks of detect delayed hematoma, hypoxic-ischemic lesions, or cere-
exposure to ionizing radiation warrant judicious patient selec- bral edema.20 CT has a role in subacute or chronic head injury
tion for CT scanning as well as radiation dose management.8 for depicting atrophy, focal encephalomalacia, hydrocepha-
There is a consensus that patients identified as moderate- lus, and chronic subdural hematoma.
risk or high-risk for intracranial injury should undergo early
noncontrast CT for evidence of intracerebral hematoma, mid- Cerebral Angiography, CTA, MRA
line shift, or increased intracranial pressure. There is an in- Cerebral angiography has a role in diagnosis and management
of traumatic vascular injuries such as pseudoaneurysm, dis-
This article is a summary of the complete version of this topic, which is available on the
ACR Website at www.acr.org/ac. Practitioners are encouraged to refer to the complete
section, or uncontrolled hemorrhage. Vascular injuries typi-
version. cally occur with penetrating trauma, basal skull fracture, or
Reprinted with permission of the American College of Radiology. trauma to the neck.21-23
Please address correspondence to Patricia C. Davis, MD, Department of Quality & Safety, CT angiography (CTA) and MR angiography (MRA) have a
American College of Radiology, 1891 Preston White Dr, Reston, VA 20191-4397. role as less invasive screening tools for detection of traumatic
AJNR Am J Neuroradiol 28:1619 –21 兩 Sep 2007 兩 www.ajnr.org 1619
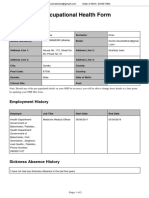
Clinical condition— head trauma
CT, MRI, CT, head, MRI, brain, CTA, MRA,
head, brain, X-ray and/or without without head head
without without CT, cervical and with and with and and Angiography, X-ray,
contrast contrast spine† contrast contrast neck neck cerebral skull
Minor or mild acute closed head injury 7a 4 5 3 2 3b 3b 1 1
(GCS ⱖ13), without risk factors or
neurologic deficit
Minor or mild acute closed head injury, 9 6c 6 2 3 5cd 5cd 1 1
focal neurologic deficit and/or risk
factors
Moderate or severe acute closed head 9 6 8 2 2 5 5 1 2
injury
Mild or moderate acute closed head 9 7e 7 2 4f 4d 4d 1 5
injury, child ⬍2 years old
Subacute or chronic closed head injury 6 8 2h 2 3 4i 4i 1 2
with cognitive and/or neurologic
deficit(s)g
Closed head injury; rule out carotid or 8 8e 5 6j 6 8 8k 6c 2
vertebral artery dissection‡
Penetrating injury, stable, neurologically 9 5l 8m 4j 4l 7 6l 5d 8n
intact
Skull fracture 9 6l 6 4 4lo 7d 4l 1 5i
a b c
Note:—Appropriateness criteria scale from 1 to 9; 1 indicates least appropriate; 9, most appropriate; , known to be low yield; , rarely indicated with mild trauma; , for problem solving;
d
, if vascular injury suspected; e , include diffusion-weighted images; f , potentially useful in suspected non-accidental trauma; g , PET or SPECT for brain ⫽ 4 – used for selected cases;
h
, assuming there are no spinal neurologic deficits; i , for selected cases; j consider perfusion; k , add T1 images; l , if MRI is safe; m , if neck or C-spine is site of injury; n , if calvarium
is site of injury; o , useful if infection is suspected. †, see the ACR Appropriateness Criteria on Spine Trauma; ‡, see the ACR Appropriateness Criteria on Cerebrovascular Disease.
vascular lesions. MRA and fat-suppressed T1-weighted MR22 or DAI.29-31 DAI results in characteristic lesions in increasing or-
CTA may reveal carotid or vertebral dissection, although angiog- der of injury severity in the: 1) cerebral white matter and gray-
raphy remains the gold standard for dissection depiction. white matter junction, 2) corpus callosum, particularly the
splenium, and 3) dorsal upper brain stem and cerebellum.29,32
MR Imaging Superior depiction of nonsurgical lesions with MR imaging
MR imaging is hindered by its limited availability in the acute may affect medical management and predict the degree of
trauma setting, long imaging times, sensitivity to patient motion, neurologic recovery.29,33 Diffusion-weighted MR imaging and
incompatibility with various medical devices, and relative insen- apparent diffusion coefficient (ADC) mapping depict cyto-
sitivity to subarachnoid hemorrhage. Other factors include the toxic injury almost immediately. In acute brain trauma, focal
need for MR imaging-specific monitoring equipment and venti- contusion and DAI may show restricted diffusion and evolve
lators, and the risk of scanning patients with certain indwelling over time to atrophy / encephalomalacia.34,35 Perfusion imag-
devices (eg, cardiac pacemaker, cerebral aneurysm clip) or for- ing with CT or MR imaging may prove helpful for disorders of
eign bodies. In part, these limitations can be overcome by situat- vascular autoregulation or ischemia.36
ing MR imaging scanners close to emergency care areas with ap-
propriate design and equipment for managing acutely injured Other Imaging Modalities
patients.24,25 Open bore geometry, faster imaging sequences, and
A few reports suggest a role for functional imaging techniques
improved patient monitoring equipment allow a greater role for
(SPECT, PET, xenon-enhanced CT, functional MR imaging)
MR imaging in closed head injuries.
to assess cognitive and neuropsychologic disturbances as well
MR imaging is sensitive for detecting and characterizing
as recovery following head trauma.37-40
subacute and chronic brain injuries. MR abnormalities in sub-
acute head injury have been used to predict the recovery out-
come of posttraumatic vegetative state.26 While CT is sensitive Review Information
for detecting of injuries requiring a change in treatment,27 MR This guideline was originally developed in 1996. The last re-
imaging also is used for acute head-injured patients with non- view and update was completed in 2006.
surgical, medically stable pathology. Hemosiderin-sensitive
T2-weighted gradient echo sequences reveal small subacute or Appendix
chronic hemorrhages. Diffusion sequences improve detection Expert Panel on Neurologic Imaging: Patricia C. Davis, MD,
of acute infarction associated with head injury. Fluid-attenu- Principal Author, Northwest Radiology Consultants, Atlanta, Ga;
ated inversion recovery (FLAIR) images are more sensitive David J. Seidenwurm, MD, Panel Chair; James A. Brunberg, MD;
than conventional MR imaging sequences for depicting of Robert Louis De La Paz, MD; Pr. Didier Dormont; David B.
subarachnoid hemorrhage and for lesions bordered by CSF.28 Hackney, MD; John E. Jordan, MD; John P. Karis, MD; Suresh
The soft tissue detail offered by MR imaging is superior to Kumar Mukherji, MD; Patrick A Turski, MD; Franz J. Wippold
that of CT for depicting nonhemorrhagic primary lesions such II, MD; Robert D Zimmerman, MD; Michael W. McDermott,
as contusions, for secondary effects of trauma such as edema MD, American Association of Neurologic Surgeons; Michael A.
and hypoxic-ischemic encephalopathy, and for imaging of Sloan, MD, MS, American Academy of Neurology.
1620 Davis 兩 AJNR 28 兩 Sep 2007 兩 www.ajnr.org
References 21. Gaskill-Shipley MF, Tomsick TA. Angiography in the evaluation of head and
1. Saul TG, and Joint Section on Neurotrauma and Critical Care of the American neck trauma. Neuroimaging Clin N Am 1996;6:607–24
Association of Neurological Surgeons and Congress of Neurological Surgeons. 22. Ozdoba C, Sturzenegger M, Schroth G. Internal carotid artery dissection: MR im-
Management of Head Injury April 1998 aging features and clinical-radiologic correlation. Radiology 1996;199:191–98
2. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography 23. Showalter W, Esekogwu V, Newton KI, et al. Vertebral artery dissection. Acad
in patients with minor head injury. N Engl J Med 2000;343:100 – 05 Emerg Med 1997;4:991–95
3. Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for 24. Gentry LR, Godersky JC, Thompson B, et al. Prospective comparative study of
patients with minor head injury. Lancet 2001;357:1391–96 intermediate-field MR and CT in the evaluation of closed head trauma. AJR
4. Haydel MJ. Clinical decision instruments for CT scanning in minor head in- 1988;150:673– 82
jury. JAMA 2005;294:1551–53 25. Mittl RL, Grossman RI, Hiehle JF, et al. Prevalence of MR evidence of diffuse
5. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian axonal injury in patients with mild head injury and normal head CT findings.
CT Head Rule and the New Orleans Criteria for CT scanning in patients with AJNR Am J Neuroradiol 1994;15:1583– 89
minor head injury. JAMA 2005;294:1519 –25 26. Kampfl A, Schmutzhard E, Franz G, et al. Prediction of recovery from post-
6. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head traumatic vegetative state with cerebral magnetic-resonance imaging. Lancet
Rule and the New Orleans Criteria in patients with minor head injury. JAMA 1998;351:1763– 67
2005;294:1511–18 27. Fiser SM, Johnson SB, Fortune JB. Resource utilization in traumatic brain
7. Masters SJ, McClean PM, Arcarese JS, et al. Skull x-ray examinations after head injury: the role of magnetic resonance imaging. Am Surg 1998;64:1088 –93
trauma. Recommendations by a multidisciplinary panel and validation study. 28. Ashikaga R, Araki Y, Ishida O. MRI of head injury using FLAIR. Neuroradiology
N Engl J Med 1987;316:84 –91 1997;39:239 – 42
8. National Cancer Institute USNIoH. Radiation risks and pediatric computed 29. Gentry LR. Imaging of closed head injury. Radiology 1994;191:1–17
tomography (CT): a guide for health care providers.; 2002 30. Gentry LR, Godersky JC, Thompson B. MR imaging of head trauma: review of
9. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A the distribution and radiopathologic features of traumatic lesions. AJR
practical scale. Lancet 1974;2:81– 84 1988;150:663–72
10. Kido DK, Cox C, Hamill RW, et al. Traumatic brain injuries: predictive use- 31. Gentry LR, Thompson B, Godersky JC. Trauma to the corpus callosum: MR
fulness of CT. Radiology 1992;182:777– 81 features. AJNR Am J Neuroradiol 1988;9:1129 –38
11. Reinus WR, Zwemer FL, Jr., Fornoff JR. Prospective optimization of patient 32. Arfanakis K, Haughton VM, Carew JD, et al. Diffusion tensor MR imaging in
selection for emergency cranial computed tomography: univariate and mul- diffuse axonal injury. AJNR Am J Neuroradiol 2002;23:794 – 802
tivariate analyses. Invest Radiol 1996;31:101– 08 33. Doezema D, King JN, Tandberg D, et al. Magnetic resonance imaging in minor
12. Shackford SR, Wald SL, Ross SE, et al. The clinical utility of computed tomo- head injury. Ann Emerg Med 1991;20:1281– 85
graphic scanning and neurologic examination in the management of patients 34. Rugg-Gunn FJ, Symms MR, Barker GJ, et al. Diffusion imaging shows abnor-
with minor head injuries. J Trauma 1992;33:385–94 malities after blunt head trauma when conventional magnetic resonance im-
13. Livingston DH, Loder PA, Hunt CD. Minimal head injury: is admission nec- aging is normal. J Neurol Neurosurg Psychiatry 2001;70:530 –33
essary? Am Surg 1991;57:14 –17 35. Smith DH, Meaney DF, Lenkinski RE, et al. New magnetic resonance imaging
14. Nagy KK, Joseph KT, Krosner SM, et al. The utility of head computed tomog- techniques for the evaluation of traumatic brain injury. J Neurotrauma
raphy after minimal head injury. J Trauma 1999;46:268 –70 1995;12:573–77
15. Stein SC, O’Malley KF, Ross SE. Is routine computed tomography scanning too 36. Wintermark M, Chiolero R, van Melle G, et al. Relationship between brain
expensive for mild head injury? Ann Emerg Med 1991;20:1286 – 89 perfusion computed tomography variables and cerebral perfusion pressure in
16. Dietrich AM, Bowman MJ, Ginn-Pease ME, et al. Pediatric head injuries: can severe head trauma patients. Crit Care Med 2004;32:1579 – 87
clinical factors reliably predict an abnormality on computed tomography? 37. Ichise M, Chung DG, Wang P, et al. Technetium-99m-HMPAO SPECT, CT
Ann Emerg Med 1993;22:1535– 40 and MRI in the evaluation of patients with chronic traumatic brain injury:
17. Homer CJ, Kleinman L. Technical report: minor head injury in children. Pe- a correlation with neuropsychological performance. J Nucl Med
diatrics 1999;104:e78 1994;35:217–26
18. The ALARA (as low as reasonably achievable) concept in pediatric CT in- 38. Jacobs A, Put E, Ingels M, et al. Prospective evaluation of technetium-99m-
telligent dose reduction. Multidisciplinary conference organized by the HMPAO SPECT in mild and moderate traumatic brain injury. J Nucl Med
Society of Pediatric Radiology. August 18 –19, 2001. Pediatr Radiol 1994;35:942– 47
2002;32:217–313 39. Jantzen KJ, Anderson B, Steinberg FL, et al. A prospective functional MR im-
19. Paterson A, Frush DP, Donnelly LF. Helical CT of the body: are settings ad- aging study of mild traumatic brain injury in college football players. AJNR
justed for pediatric patients? AJR 2001;176:297–301 Am J Neuroradiol 2004;25:738 – 45
20. Stein SC, Spettell C, Young G, et al. Delayed and progressive brain injury in 40. Kinuya K, Kakuda K, Nobata K, et al. Role of brain perfusion single-photon
closed-head trauma: radiological demonstration. Neurosurgery 1993;32:25– emission tomography in traumatic head injury. Nucl Med Commun 2004;25:
30; discussion 30 –31 333–37
AJNR Am J Neuroradiol 28:1619 –21 兩 Sep 2007 兩 www.ajnr.org 1621
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Myofascial Pain Dysfunction Syndrome - A RevisitDokument9 SeitenMyofascial Pain Dysfunction Syndrome - A RevisitRhea RejiNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Body Parts Governed by PlanetsDokument2 SeitenBody Parts Governed by PlanetsBratva Ankit Mishra100% (1)
- SCE Practicaldiabetes - ElzohryDokument107 SeitenSCE Practicaldiabetes - ElzohryAE67% (3)
- SP42 Thoracentesis (Adult)Dokument7 SeitenSP42 Thoracentesis (Adult)Adam HuzaibyNoch keine Bewertungen
- Girl InterruptedDokument7 SeitenGirl Interruptedapi-365678992Noch keine Bewertungen
- Lipo LaserDokument13 SeitenLipo LaserLuis A Gil Pantoja100% (1)
- Festival Dance Lesson - Module 2 - P.E. 3rd Quarter PPT 2 of 2Dokument29 SeitenFestival Dance Lesson - Module 2 - P.E. 3rd Quarter PPT 2 of 2Maria Fe VibarNoch keine Bewertungen
- Che 225 Control of Communicable DiseasesDokument19 SeitenChe 225 Control of Communicable DiseasesAbdullahi Bashir SalisuNoch keine Bewertungen
- Wound CareDokument77 SeitenWound CareNestor Balboa100% (1)
- Medical Biotechnology Multiple Choice Question (GuruKpo)Dokument13 SeitenMedical Biotechnology Multiple Choice Question (GuruKpo)GuruKPO91% (11)
- Guia NICE 2011 AutismoDokument51 SeitenGuia NICE 2011 Autismomecho9002Noch keine Bewertungen
- Lesson Plan On Spina BifidaDokument24 SeitenLesson Plan On Spina BifidaPriyaNoch keine Bewertungen
- TM Joint PDFDokument16 SeitenTM Joint PDFdhruvNoch keine Bewertungen
- Occupational Health Form: General DetailsDokument2 SeitenOccupational Health Form: General DetailsKhushal khanNoch keine Bewertungen
- Acute Parenchymal Liver DiseaseDokument29 SeitenAcute Parenchymal Liver Diseasejeevan ghimireNoch keine Bewertungen
- PMLS Lesson 5Dokument7 SeitenPMLS Lesson 5Althea EspirituNoch keine Bewertungen
- Carotid Sinus Massage - MuraliDokument31 SeitenCarotid Sinus Massage - MuraliAhsan MohammedNoch keine Bewertungen
- Parasitology: - IntroductionDokument62 SeitenParasitology: - IntroductionHana AliNoch keine Bewertungen
- Medical Symptoms QuestionnaireDokument29 SeitenMedical Symptoms QuestionnaireOlesiaNoch keine Bewertungen
- OS Pharmacy L III - IVDokument125 SeitenOS Pharmacy L III - IVashagrie67% (3)
- Brain AbscessDokument13 SeitenBrain AbscessRian AprizaNoch keine Bewertungen
- Family Laboratory For Medical Analysis: Test & SpecimenDokument1 SeiteFamily Laboratory For Medical Analysis: Test & SpecimenMohamad BadranNoch keine Bewertungen
- Itpc PT ProcessDokument2 SeitenItpc PT ProcessKyle MañiboNoch keine Bewertungen
- Aneurysm: Symptoms of An AneurysmDokument3 SeitenAneurysm: Symptoms of An AneurysmArun MuralidharanNoch keine Bewertungen
- University of Zimbabwe Dissertation TopicsDokument4 SeitenUniversity of Zimbabwe Dissertation TopicsCustomWritingPaperServiceCanada100% (1)
- Hydatidiform MoleDokument2 SeitenHydatidiform MoleIrfan HardiNoch keine Bewertungen
- Using Pediatric Pain Scales Neonatal Infant Pain Scale (NIPSDokument2 SeitenUsing Pediatric Pain Scales Neonatal Infant Pain Scale (NIPSSevina Eka ChannelNoch keine Bewertungen
- KSPCB BIOMEDICAL POSTER 1aDokument1 SeiteKSPCB BIOMEDICAL POSTER 1armulmadgiNoch keine Bewertungen
- Research Article: Oral Care of Hospitalised Older Patients in The Acute Medical SettingDokument5 SeitenResearch Article: Oral Care of Hospitalised Older Patients in The Acute Medical SettingMohammed Falih HassanNoch keine Bewertungen
- Internal Medicine: Dr. Nindyasari Diajeng Larasati Tim UKMPPD FKU MalahayatiDokument209 SeitenInternal Medicine: Dr. Nindyasari Diajeng Larasati Tim UKMPPD FKU MalahayatiSilvi Qiro'atul AiniNoch keine Bewertungen