Beruflich Dokumente
Kultur Dokumente
Juvenile Nasopharyngeal Angiofibroma With Intracranial Extension - A Review of 29 Cases
Hochgeladen von
Satya WangsaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Juvenile Nasopharyngeal Angiofibroma With Intracranial Extension - A Review of 29 Cases
Hochgeladen von
Satya WangsaCopyright:
Verfügbare Formate
[Downloaded free from http://www.jnaccjournal.org on Tuesday, February 5, 2019, IP: 182.253.63.
142]
Original Article
Juvenile nasopharyngeal angiofibroma with
intracranial extension – A review of 29 cases
Varun Jain, Surya Kumar Dube, Charu Mahajan1, Hemanshu Prabhakar
Abstract
Background: Complete resection has been the preferred treatment for extracranial juvenile nasopharyngeal
angiofibromas (JNA) but resection of JNA with intracranial extension (ICE) can be quite challenging because of the
associated risk of extensive haemorrhage. The aim of this study was to assess the neurological outcome of patients
undergoing surgery for removal of JNA with ICE and analyse various perioperative anaesthetic factors that could possibly
affect the outcome. Materials and Methods: This retrospective study was conducted including patients with JNA with
ICE requiring combined otolaryngological and neurosurgical approach for tumour removal at our centre from January
2001 to December 2010. Patient’s medical and anaesthesia records were reviewed and data regarding patient demography,
pre‑operative investigations, anaesthetic management, post‑operative investigations and complications, number of days
of intensive care unit (ICU) and hospital stay and Glasgow Outcome Scale (GOS) at the time of discharge from hospital
were collected and reviewed. Results: A total of 29 patients were operated. The median age of presentation was
15 years. Nineteen patients (65.5%) had a good GOS of 5 at discharge, 7 (24.1%) had moderate outcome with GOS of
4 and 3 patients (10.3%) had poor outcome with GOS of ≤3.There was one mortality in our study. Perioperative factors
affecting the GOS at discharge were amount of intra‑operative blood loss, intra‑operative infusion of packed red blood
cells (RBCs) and colloid and post‑operative haemoglobin. Conclusion: The outcome of patients with JNA is affected
by intra‑operative blood loss and transfusion.
Key words: Anaesthesia, blood loss, juvenile nasopharyngeal angiofibroma, outcome
INTRODUCTION As the tumour grows, it extends into the maxillary,
ethmoid and sphenoid sinuses, the nasopharynx, and
Juvenile nasopharyngeal angiofibroma (JNA) is a benign, laterally into the infratemporal fossa. Intracranial
locally invasive, highly vascular tumour that arises invasion into the middle fossa commonly occurs
from the lateral wall or the roof of the nasopharynx through the pterygomaxillary space and the tumour may
especially the sphenopalatine foramen. [1‑4] JNA erode superiorly into the sella and anterior skull base.
accounts for approximately 0.5% of all head and neck Approximately 20% of patient of JNA have evidence
neoplasms.[3] The median age at diagnosis is 15 years of skull base invasion at the time of diagnosis.[3] The
and occurs exclusively in adolescent males.[4] blood supply to the tumour is mainly from external
carotid artery but draws feeder from internal carotid
Access this article online artery as the tumour extends intracranially. The tumour
Quick Response Code: consists of proliferating irregular blood vessels that
Website:
characteristically lack smooth muscle and elastic fibres
www.jnaccjournal.org
making its notorious for sustained bleeding.
DOI: Complete resection has been the preferred treatment
10.4103/2348-0548.124846 for extracranial JNAs,[4] but resection of JNA with
intracranial extension (ICE) can be quite challenging
Department of Neuroanaesthesiology, Neurosciences Center, All India Institute of Medical Sciences, New Delhi, 1Department
of Anaesthesia, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India
Address for correspondence:
Dr. Hemanshu Prabhakar, Department of Neuroanaesthesiology, Neurosciences Center, All India Institute of Medical Sciences, New Delhi ‑ 110 029,
India. E‑mail: prabhakarhemanshu@rediffmail.com
Journal of Neuroanaesthesiology and Critical Care
40 | Vol. 1 • Issue 1 • Jan-Apr 2014 |
[Downloaded free from http://www.jnaccjournal.org on Tuesday, February 5, 2019, IP: 182.253.63.142]
Jain, et al.: Juvenile nasopharyngeal angiofibroma with intracranial extension
both for the anaesthesiologists and the surgeons mainly reviewed. Various parameters were correlated with
because of the associated risk of extensive haemorrhage. GOS. For the purpose of analysis, GOS was divided
The advancement in anaesthesiology and diagnostic into three categories: GOS ≤3 (poor), GOS 4 (moderate)
imaging techniques and pre‑operative angiographic and GOS 5 (good).
embolisation has contributed towards the successful
management of JNA with ICE. The aim of this study Anaesthesia Protocol
was to assess the neurological outcome of patients A standard management protocol was followed for
undergoing surgery for removal of JNA with ICE and all patients. All patients were assessed one day prior
analyse various perioperative anaesthetic factors that to proposed surgery and adequate blood and blood
could possibly affect the outcome. products were arranged. Patients who had intra‑arterial
embolisation for the tumour were taken up for surgery
MATERIALS AND METHODS within 48 h of procedure. Standard monitors including
electrocardiography (ECG), pulse oximetry (SPO2),
After obtaining Institute Ethics Committee approval, non‑invasive BP (NIBP), end tidal carbon dioxide (ETCO2)
this retrospective study was conducted including and nasopharyngeal temperature were used in all patients.
patients with JNA with ICE requiring combined In all patients general anaesthesia (GA) was induced
otolaryngological and neurosurgical approach for with either propofol or thiopentone with fentanyl and
tumour removal at our centre from January 2001 rocuronium and was maintained with oxygen, nitrous
to December 2010. All patients with Radkowski oxide and isoflurane/sevoflurane with intermittent boluses
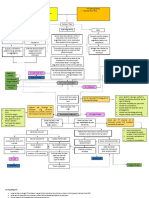
classification [Table 1] Grade III tumour extension of fentanyl and vecuronium. Arterial line and central
referred to the Neurosurgery department were studied. venous cannulation was done in all cases for invasive
Patient’s medical and anaesthesia records were blood pressure (IBP) and central venous pressure (CVP)
reviewed and data regarding patient demography, monitoring. Two wide bore peripheral intravenous
pre‑operative investigations, anaesthetic management, accesses were secured in all the patients. Patients were
post‑operative investigations and complications, placed in reverse tredelenberg position and mechanical
number of days of intensive care unit (ICU) and hospital ventilation was adjusted to ETCO2 of 33 ± 2 mmHg.
stay and Glasgow Outcome Scale (GOS) [Table 2] at Arterial blood gas (ABG) analysis was performed routinely
the time of discharge from hospital were collected and post‑induction (baseline ABG) and frequently thereafter,
correlating with the episodes of heavy blood loss.
Table 1: Radkowski classification of juvenile
angiofibromas Goals for anaesthesiologist were to provide stable
intra‑operative haemodynamics, to keep the mean BP
Stage Details
at lower normal range of 50–70 mmHg. Blood loss
IA Limited to the nose and nasopharyngeal area calculation and fluid replacement was as per the senior
IB Extension into one or more sinuses anaesthesiologist’s assessment. Blood loss was calculated
IIA Minimal extension into pterygopalatine fossa by assessing the collected blood in the surgical field,
IIB Occupation of the pterygopalatine fossa without suction bottles, soaked mops and serial ABGs. Fluid
orbital erosion replacement was judged on the basis of pre‑operative
IIC Infratemporal fossa extension without cheek or haemoglobin, blood loss, urine output, hemodynamic
pterygoid plate involvement stability and ABG analysis. We used ringer lactate and
0.9% normal saline (each litre alternatively) and 6%
IIIA Erosion of the skull base (middle cranial fossa or
pterygoids) hydroxyethyl starch (HES) as intravenous fluid. Cell
saver was available for every case but its usage was at
IIIB Erosion of the skull base with intracranial extension
with or without cavernous sinus involvement
the discretion of the surgeon. Blood transfusion was
started when haemoglobin fell below 8 g/dl and patient
showed signs of hemodynamic instability. Autologous
Table 2: Glasgow outcome scale blood was transfused prior to allogenic blood when
1. Dead available. At the end of surgery all the anaesthetics
2. Vegetative state, unable to interact with environment; were discontinued and patient’s trachea was extubated
unresponsive or patients were shifted with the endotracheal tube
in situ for further management to the neurosurgical
3. Severe disability, able to follow commands/unable to
live independently ICU. Any coagulation, haematological or electrolyte
disturbances in the post‑operative period was managed
4. Moderate disability, able to live independently; unable
to return to work or school
with standard management protocol. In intubated
patients, tracheal extubation was planned in discussion
5. Good recovery, able to return to work or school
with neurosurgical team after confirming hemodynamic
Journal of Neuroanaesthesiology and Critical Care
| Vol. 1 • Issue 1 • Jan-Apr 2014 | 41
[Downloaded free from http://www.jnaccjournal.org on Tuesday, February 5, 2019, IP: 182.253.63.142]
Jain, et al.: Juvenile nasopharyngeal angiofibroma with intracranial extension
stability, satisfactory clinical neurological condition and 7 (24.1%) had moderate outcome with GOS of 4 and
radiological review. 3 patients (10.3%) had poor outcome with GOS of ≤3.
There was one mortality in our study.
Data Collection
Various pre‑operative parameters recorded were Demographic and Pre‑Operative Data
demographic data (age, gender, weight and blood All the patients were males and the median
group), recurrence, number of previous surgeries for age of presentation was 15 years with range of
removal of angiofibroma, history of embolisation and 8-29 years [Table 3]. Median weight of patients was about
baseline investigations (haemoglobin, platelets and 43 kg with range of 22-60 kg. A total of 20 patients (69%)
coagulation profile), intra‑operative data (duration had undergone at least one surgery previously and
of surgery, type of anaesthetic techniques, amount this time presented with a recurrence, whereas the
of blood loss, amount of fluids infused, use of cell remaining 9 patients presented first time for surgery.
saver and autologous blood transfused, anaesthesia No other co‑morbidity was present in any of the patients
and surgical duration, ABG and other investigation and all the patients had full Glasgow Coma Scale score
reports and extubation details), post‑operative at presentation (Eye 4, Verbal 5, Motor 6). Two of the
details (post‑operative haemoglobin, coagulation patients received tablet flutamide pre‑operatively in our
profile, post‑operative blood transfusion, number of study. A total of 19 patients (65.52%) had intra‑arterial
days on ventilator and duration of ICU and hospital embolisation of tumour before surgery. Median baseline
stay). Post‑operative recovery was assessed using GOS haemoglobin, INR and platelet count of patients were
score by the neurosurgical team at discharge. 12.7 g/dl, 1.09 and 233000/mm3, respectively. All the
above demographic data and pre‑operative work‑up of
Statistical Analysis patients was statistically correlating, although there was
Statistical analysis was done using the software SPSS a trend towards the younger age group, showing better
version 15.0 (Illinois, Chicago, USA). The data is GOS at discharge.
presented in median (range) or number (percentage).
The numerical data was categorised and compared Operative Data
using Kruskal–Wallis test. The significant result was GA was induced with either propofol (18 patients)
compared by post‑hoc comparison with probability or thiopentone (11 patients). Median duration of
adjustment. Strength of correlation between blood loss surgery was 6.75 h. Patients with GOS 5 had a shorter
and fluid infused was by Spearman’s rank correlation surgical time of 6.1 h compared with patients with GOS
coefficient. Categorical data (blood group, use of cell 4 (7.5 h) and GOS ≤3 (8.16 h). Median blood loss was
saver, embolisation history, history of previous surgery 2500 ml (600–9400 ml). Increasingly higher blood loss
and type of induction agent used) and GOS were tested was noticed in patients with poorer GOS. Median blood
using Mann–Whitney Wilcoxon test. The P < 0.05 is loss in patients with GOS 5 was 2000 ml, compared with
considered significant. 4000 ml in patients with GOS 4 and 8000 ml in patients
with GOS ≤ 3 (P = 0.023) [Table 4]. Patients who had
RESULTS intra‑arterial embolisation pre‑operatively had lesser
intra‑operative blood loss (median 2100 ml) compared
A total of 29 patients were operated from 2001 to 2010 with those not embolised (median 2900 ml); data was,
at our centre with Grade III Radkowski JNA requiring however, statistically not significant (P = 0.696). Similarly,
combined otolaryngological and neurosurgical approach patients embolised needed 3 units (range 2-9 units)
for dissection and removal of JNA with ICE. A total of packed red blood cells (RBCs) transfusion compared
19 patients (65.5%) had a good GOS of 5 at discharge, with 5.5 units (range 0-11 units) in non‑embolised
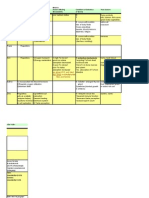
Table 3: Demographic and Pre‑operative baseline characteristics
GOS Total (N=29) ≤3 (N=3) 4 (N=7) 5 (N=19) P value
Age (years) 15 (8-29) 19 (15-22) 18 (14-26) 14 (8-29) 0.11
Weight (kg) 43 (22-60) 40 (30-46) 47 (40-60) 43 (22-60) 0.32
Recurrence 20 1 6 13 0.25
Embolisation 19 (65.5%) 1 (33.3%) 5 (71.4%) 13 (68.4%) 0.46
Haemoglobin (g%) 12.7 (10-16.4) 12.1 (10-16.4) 12.7 (11.1-14.1) 13 (10.2-15.2) 0.98
Baseline INR 1.09 (0.9-1.2) 1.09 (1-1.2) 1.08 (1-1.1) 1.1 (0.9-1.2) 0.64
Baseline Plt (*105/mm3) 2.33 (1.71-3.12) 3.02 (1.98-3.1) 2.1 (1.85-3.12) 2.37 (1.71-3.12) 0.38
[data presented in median (range)], GOS = Glasgow outcome scale, N = Number of patients, INR = International normalised ratio, Plt = Platelets
Journal of Neuroanaesthesiology and Critical Care
42 | Vol. 1 • Issue 1 • Jan-Apr 2014 |
[Downloaded free from http://www.jnaccjournal.org on Tuesday, February 5, 2019, IP: 182.253.63.142]
Jain, et al.: Juvenile nasopharyngeal angiofibroma with intracranial extension
Table 4: Intra‑operative parameters and glasgow outcome scale
GOS Total (N=29) ≤3 (N=3) 4 (N=7) 5 (N=19) P value
Duration of Sx (h) 6.75 (5.0-9.5) 8.16 (5.16-9.5) 7.5 (5.5-8.0) 6.16 (5.0-9.2) 0.47
Blood loss (ml) 2500 (600-9400) 8000 (2500-9400) 4000 (1300-7000) 2000 (600-4800) 0.02
Cell saver 17 (58.6%) 2 (66.7%) 3 (42.9%) 12 (63.2%) 0.62
Autologous 200 (0-3800) 2000 (0-3000) 0 (0-3800) 490 (0-1500) 0.35
RBC (units) 4 (0-11) 6 (5-7) 6 (2-11) 3 (0-7) 0.04
FFP (units) 2 (0-8) 0 (0-8) 4 (0-6) 2 (0-5) 0.13
PRP (units) 0 (0-8) 0 (0-8) 0 (0-7) 2 (0-4) 1.0
Crystalloids (ml) 5500 (3000-10000) 8000 (4000-9000) 7500 (4500-10000) 5000 (3000-9000) 0.05
Colloid (ml) 700 (0-2000) 2000(1000-2000) 500 (0-1500) 500 (0-1000) 0.046
[data presented in numbers (percentage)] GOS = Glasgow outcome scale, N = Number of patients, Sx = Surgery, RBC = Red blood cells, FFP = Fresh frozen
plasma, PRP = Platelet rich plasma
patients, although data was again statistically shock. The median post‑operative haemoglobin was
insignificant (P = 0.2627). Overall, median 4 units of 10.9 g/dl and INR 1.10. Post‑operative haemoglobin
blood, 2 units fresh frozen plasma (FFP), 5.5 L crystalloid correlated with GOS at discharge (P = 0.047) [Table 5]. No
and 700 ml colloid was transfused in all the cases. blood was transfused in ICU to patients who had GOS 5
Generally, no median plasma rich platelets (PRP) were at discharge, but median 1 and 2 units were transfused to
transfused intra‑operatively. Packed RBCs transfusion patients with GOS 4 and GOS ≤3, respectively. However,
was less in GOS 5 patients (3 units) compared with the difference was statistically insignificant. Patients
GOS 4 and GOS ≤3 patient group (median 6 units each). with GOS 4 and GOS 5 were electively ventilated for
Lower crystalloid requirements were noted in GOS 5 approximately 12 h post‑operatively and were tracheally
group (5000 ml) as against 7500 ml in GOS 4 group and extubated next morning. Median ICU stay for these
8000 ml in GOS ≤3 group. Similarly, colloid transfusion patients was 2 days. However, patients with GOS ≤3
was less in GOS 5 and GOS 4 category patients (median were ventilated for 3 days (median, maximum 5 days)
500 ml) compared with about 2000 ml in GOS ≤3 category and had an ICU stay for 7 days. None of the patients
patients. Cell saver was employed in 17 (58.6%) of needed re‑intubation. The median hospital stay was
29 cases. Mean blood loss when cell saver was used was 5 days.
3670 ± 2380 ml compared with 2433.3 ± 1683 ml in patients
where cell saver was not used (P = 0.143). Mean amount An interesting finding in our study was that all three
of packed RBCs transfused in patients where cell saver patients with GOS ≤3 were blood group A‑positive
was used was 4.3 units compared with 4.6 units where but rest of the patients with GOS 4 and GOS 5 had a
cell saver was used (P = 0.322). However, a positive higher incidence of blood group B‑positive. Overall,
correlation between blood loss and amount of autologous there was a higher incidence of JNA with ICE in blood
blood transfused existed (P = <0.0001). Packed RBCs group B‑positive patients (51.7%) [Table 6].
transfusion correlated positively with the amount of
blood loss (P = <0.0001) irrespective of cell saver usage. DISCUSSION
Metabolic acidosis (37.9%), hypocalcaemia (10.3%)
and hyperkalemia (10.3%) were the most commonly Primary findings of our study were that majority of
encountered metabolic and electrolyte abnormality in patients undergoing surgery for JNA with ICE (Radowski
our series. classification grade III) had a good neurological outcome.
Only 10.3% of patients had poor neurological outcome
Post‑Operative Data at discharge with a GOS score of ≤3. Perioperative
At the end of surgery, all patients except one were shifted factors affecting the GOS at discharge were amount
to ICU for elective ventilation. One patient was extubated of intra‑operative blood loss, amount of fluid infused
in the operating room. This was a 28‑year‑old male with intra‑operatively especially packed RBCs and colloid
an early ICE of tumour. Intra‑operative, this patient and post‑operative haemoglobin. Secondary findings
had 600 ml blood loss and had a stable hemodynamic in our analysis showed that intra‑arterial embolisation
course. There was one mortality (GOS 1) of a 15‑year‑old of tumour pre‑operatively reduces the intra‑operative
male weighing 30 kg. The patient had undergone blood loss and amount of blood transfused; although the
surgery twice previously and incurred blood loss of findings were not statistically significant. Intra‑operative
8000 ml (maximum per kg blood loss in this retrospective use of cell saver may be useful in reducing the amount
data) and succumbed to hypovolemic haemorrhagic of allogenic blood transfused.
Journal of Neuroanaesthesiology and Critical Care
| Vol. 1 • Issue 1 • Jan-Apr 2014 | 43
[Downloaded free from http://www.jnaccjournal.org on Tuesday, February 5, 2019, IP: 182.253.63.142]
Jain, et al.: Juvenile nasopharyngeal angiofibroma with intracranial extension
Table 5: Post‑operative parameters and glasgow outcome scale
GOS Total (N=29) ≤3 (N=3) 4 (N=7) 5 (N=19) P value
Post‑op Hb (g%) 10.9 (3.8-3.5) 6.3 (3.8-11.6) 10.1 (6.9-11.3) 11 (9.2-13.5) 0.04
Post‑op INR 1.1 (0-5) 2.9 (0-5) 1.1 (1-2.1) 1.1 (1-2.6) 0.41
Post op BT (units) 0 (0-3) 2 (0-3) 1 (0-3) 0 (0-3) 0.26
Ventilatory days 0.5 (0-5) 3 (0.5-5) 0.5 (0.5-2) 0.5 (0-2) 0.19
ICU stay (days) 2 (1-8) 7 (1-8) 2 (2-4) 2 (1-4) 0.26
Hospital stay (days) 5 (1-10) 5 (1-10) 5 (4-7) 5 (3-7) 0.39
[data presented in median (range)], GOS = Glasgow outcome scale, INR = International normalised ratio, ICU = Intensive care unit
Table 6: Blood group and glasgow outcome scale at least twice previously. This recurrence is higher than
Blood GOS (%) that reported in literature but since this depicted the
group recurrence rate in patients who were referred to the
≤3 (N=3) 4 (N=7) 5 (N=19)
neurosurgical department at our institute, this probably
A‑positive 3 (100) 2 (28.6) 3 (15.8) does not reflect the complete picture. Rather it emphasis
B‑positive 0 4 (57.1) 11 (57.9) the fact JNA can reappear as a higher grade tumour.
AB‑positive 0 1 (14.3) 2 (10.5)
Intra‑operative blood loss has been most troublesome
O‑positive 0 0 2 (10.5)
aspect in management of JNA. Median blood loss in
O‑negative 0 0 1 (5.3) our study was 2500 ml (range 600-9400 ml). Moulin
[data presented in numbers (percentage)], GOS = Glasgow outcome scale, et al.[12] compared intra‑operative blood loss in embolised
N = Number of patients
and non‑embolised patients undergoing surgery for
JNA removal. In their study, the mean blood loss was
The demographical data reviewed from this retrospective
5380 ml in patients without embolisation and 1037 ml
study are comparable to studies done previously.[5,6] In
in those with embolisation. Ezri et al.[13] found the blood
this study, the typical presentation of angiofibroma is
loss in non‑embolised patients undergoing surgery
an adolescent male with an median age of 15 years and
for removal of JNA was 4800 ± 1600 ml. Bales et al.[3]
median weight of 43 kg. Effect of craniofacial surgery
reported lower blood loss in five patients who had a
necessary for removal of intra‑cranially spread JNA on
craniofacial resection and observed a mean blood loss
neurological outcome has not been studied previously
of 1120 ml (range, 700-1750 ml). In our series, excessive
because of the fact that JNA is primarily a head and neck
blood loss was the major perioperative factor, which
tumour and it is assumed that neurological outcome
will be good. We have shown for the first time that such influenced the GOS. Patients with good GOS (5) had
an extensive intracranial surgery can have an effect lower blood loss intra‑operatively compared with
on neurological status of a patient. Although majority patients with poorer GOS (4 and ≤3).
of cases (65.5%) had a good neurological outcome of Various techniques are helpful in reducing the
GOS 5, 24.1% of cases had a decrease in neurological intra‑operative blood loss like use of reverse
outcome with a GOS of 4 and 10.3% of cases had a poor trendelenberg position, hypotensive anaesthesia [13]
GOS of ≤ 3. Mortality has been associated with such and embolisation of the tumour. We employed reverse
an extensive surgery when accompanied with massive
trendelenberg position in all our patients and the aim
haemorrhage.[4,6] Our study also witnessed one mortality
was to keep the mean blood pressure in the range of 55–
associated with JNA surgery. The patient had massive
65 mmHg by titration of inhalation agent. Embolistion
uncontrollable blood loss intra‑operatively, which was
of tumour was done in 65.5% of patients pre‑operatively
maximum observed blood loss in this study (266.7 ml/kg
and all the patients were taken up for surgery within
body weight).
48 h as consistent with other studies.[6,14] There was no
Recurrence has been suggested as a major complication uniform consensus among surgeons at our institute
in greater part of surgical literature,[6‑9] despite the about embolisation of tumour as embolisation though
benign and unifocal origin of JNA. Tumour recurrence reduces blood loss may prevent complete evacuation of
is primarily seen with high grade tumours with ICE, in tumour. Embolistion of tumour was helpful in decreasing
part, due to failure to recognise skull base erosion.[3,10] amount of packed RBCs transfused intra‑operatively (3
Recurrence rate for JNA has been reported from 17% units) versus 5.5 units in non‑embolised tumours. This
to 86%.[9,11] For 20 of 29 (69%) patients in our study, was similar to findings by Mann et al.[3] in their 12‑year
there was a recurrence. For six of these cases, there study. However, pre‑operative embolisation did not
was multiple recurrence and they had been operated seem to influence the GOS directly.
Journal of Neuroanaesthesiology and Critical Care
44 | Vol. 1 • Issue 1 • Jan-Apr 2014 |
[Downloaded free from http://www.jnaccjournal.org on Tuesday, February 5, 2019, IP: 182.253.63.142]
Jain, et al.: Juvenile nasopharyngeal angiofibroma with intracranial extension
Two of our patients received flutamide in the preoperative REFERENCES
period. Flutamide (2‑methyl‑n‑[4‑nitro‑3{trifluoromethyl}
phenyl] propanamide) is an orally active non‑steroidal 1. Martin H, Ehrlich HE, Abels JC. Juvenile nasopharyngeal
angiofibroma. Ann Surg 1948;127:513‑36.
androgen antagonist (NSAA) a non‑steroidal anti‑androgen 2. Herman P, Lot G, Chapot R, Salvan D, Huy PT. Long term
drug administrated orally and is widely used in the follow‑up of juvenile nasopharyngeal angiofibromas: Analysis
treatment of cancer of the prostate.[15,16] There are conflicting of recurrences. Laryngoscope 1999;109:140‑7.
reports regarding the usefulness of its use to reduce the size 3. Bales C, Kotapka M, Loevner LA, Al‑Rawi M, Weinstein G,
Hurst R, et al. Craniofacial resection of advanced juvenile
of JNA in the literature. Gates et al.[17] and Thakar et al.[15]
nasopharyngeal angiofibroma. Arch Otolaryngol Head Neck
reported reduction of JNA size in their studies. However, Surg 2002;128:1071‑8.
in another study by Labra et al.,[16] the authors did not 4. Bremer JW, Neel HB 3rd, DeSanto LW, Jones GC. Angiofibroma:
find any significant reduction in the JNA size. Nausea, Treatment trends in 150 patients during 40 years.
hepatotoxicity and mild breast tenderness are the common Laryngoscope 1986;96:1321‑9.
5. Tewfik TL, Tan AK, al Noury K, Chowdhury K, Tampieri D,
reported side effects of flutamide and regular liver function Raymond J, et al. Juvenile nasopharyngeal angiofibroma.
test has to be done in patients receiving flutamide.[15] The J Otolaryngol 1999;28:145‑51.
probability of hepatic derangement is to be taken into 6. Mann WJ, Jecker P, Amedee RG. Juvenile angiofibromas:
consideration in patients receiving flutamide. Changing surgical concept over the last 20 years. Laryngoscope
2004;114:291‑3.
Besides techniques to reduce blood loss, other useful 7. Gupta AC, Murthy DP. Intracranial juvenile nasopharyngeal
angiofibroma. Aust N Z J Surg 1997;67:477‑82.
method of preserving blood is by use of cell saver. In our
8. Tang IP, Shashinder S, Gopala Krishnan G, Narayanan P.
study, although the amount of blood loss was statistically Juvenile nasopharyngeal angiofibroma in a tertiary centre:
similar whether cell saver is used or not, it was clinically Ten‑year experience. Singapore Med J 2009;50:261‑4.
much less in the group where cell saver was not used. 9. Elsharkawy AA, Kamal EM, Tawfik A, Zaher A, Kasem M.
Considering that packed RBCs were transfused in both Juvenile nasopharyngeal angiofibroma with intracranial
extension: Analysis of 23 Egyptian patients. Int J Pediatr
groups equally, and there was positive correlation of Otorhinolaryngol 2010;74:755‑9.
blood loss and amount of autologous blood transfused 10. Donald PJ, Enepikedes D, Boggan J. Giant juvenile
proves that patients in whom cell saver was employed nasopharyngeal angiobroma: Management by skull‑base
were saved of excessive allogenic blood transfusion. It is surgery. Arch Otolaryngol Head Neck Surg 2004;130:882‑6.
therefore judicious to use cell saver where major blood 11. Deschler DG, Kaplan MJ, Boles R. Treatment of large juvenile
nasopharyngeal angiobroma. Otolaryngol Head Neck Surg
loss is expected. Again use of cell saver did not influence 1992;106:278‑84.
the GOS directly. 12. Moulin G, Chagnaud C, Gras R, Gueguen E, Dessi P,
Gaubert JY, et al. Juvenile nasopharyngeal angiofibroma:
Lastly, factor affecting the GOS was haemoglobin in Comparison of blood loss during removal in embolized group
the post‑operative period; higher haemoglobin value versus nonembolized group. Cardiovasc Intervent Radiol
was associated with better neurological outcome. 1995;18:158‑61.
13. Ezri T, Roth Y, Geva D, Konichezky S, Marshak G, Halperin D.
A cautious approach in the post‑operative period anesthetic management of juvenile nasopharyngeal angiobroma
regarding extubation is warranted in these patients resection. J Cardiothorac Vasc Anesth 2003;17:622‑4.
because of the risk of aspiration due to inadequate 14. Nicolai P, Berlucchi M, Tomenzoli D, Cappiello J, Trimarchi M,
haemostasis, coagulation disorder and airway oedema Maroldi R, et al. Endoscopic surgery for juvenile angiofibroma:
associated with prolonged surgery and tumour handling. When and how. Laryngoscope 2003;113:775‑82.
15. Thakar A, Gupta G, Bhalla AS, Jain V, Sharma SC, Sharma R,
Therefore, all but one patient were shifted intubated in et al. Adjuvant therapy with flutamide for presurgical volume
ICU post‑operatively and extubation was planned after reduction in juvenile nasopharyngeal angiofibroma. Head
confirmation with surgeons about haemostasis. No Neck 2011;33:1747‑53.
re‑intubation was needed in any of the patients. 16. Labra A, Chavolla‑Magaña R, Lopez‑Ugalde A,
Alanis‑Calderon J, Huerta‑Delgado A. Flutamide as a
To summarise, our study on 29 patients of JNA with preoperative treatment in juvenile angiofibroma (JA) with
intracranial invasion: Report of 7 cases. Otolaryngol Head
ICE undergoing tumour resection via combined Neck Surg 2004;130:466‑9.
otolaryngolocial and neurosurgical approach showed 17. Gates GA, Rice DH, Koopmann CF Jr, Schuller DE. Flutamide induced
that outcome of patients was affected by intra‑operative regression of angiofibroma. Laryngoscope 1992;102:641‑4.
blood loss and fluid management, a basic but important
clinical skill for all anaesthesiologists. This study also How to cite this article: Jain V, Dube SK, Mahajan C, Prabhakar H.
highlights the fact that it is important to replace the Juvenile nasopharyngeal angiofibroma with intracranial extension-
A review of 29 cases. J Neuroanaesthesiol Crit Care 2014;1:40-5.
blood timely and adequately in surgeries where major
blood loss occurs. Source of Support: Nil, Conflict of Interest: None declared.
Journal of Neuroanaesthesiology and Critical Care
| Vol. 1 • Issue 1 • Jan-Apr 2014 | 45
Das könnte Ihnen auch gefallen
- Endocrine Surgery: Butterworths International Medical Reviews: SurgeryVon EverandEndocrine Surgery: Butterworths International Medical Reviews: SurgeryI. D. A. JohnstonNoch keine Bewertungen
- Lavado IntraventricularDokument8 SeitenLavado IntraventricularGlessin MurilloNoch keine Bewertungen
- 2012 - Frympas G.Dokument8 Seiten2012 - Frympas G.alejandra gonzalezNoch keine Bewertungen
- 2013 - BoghaniDokument11 Seiten2013 - Boghanialejandra gonzalezNoch keine Bewertungen
- 2022 Perioperative Complications of Transvenous Embolization of Ruptured Intracranial Arteriovenous MalformationsDokument7 Seiten2022 Perioperative Complications of Transvenous Embolization of Ruptured Intracranial Arteriovenous MalformationsstaseaditNoch keine Bewertungen
- Guo 2019Dokument8 SeitenGuo 2019Dr. Gerald ToyoNoch keine Bewertungen
- Predictors and Outcomes of Shunt-Dependent Hydrocephalus in Patients With Aneurysmal Sub-Arachnoid HemorrhageDokument8 SeitenPredictors and Outcomes of Shunt-Dependent Hydrocephalus in Patients With Aneurysmal Sub-Arachnoid HemorrhageNovia AyuNoch keine Bewertungen
- A Case Report On Middle Cerebral Artery Aneurysm.44Dokument5 SeitenA Case Report On Middle Cerebral Artery Aneurysm.44SuNil AdhiKariNoch keine Bewertungen
- 1 s2.0 S0929664617300487 MainDokument8 Seiten1 s2.0 S0929664617300487 MainSuryati HusinNoch keine Bewertungen
- EsofagoDokument6 SeitenEsofagoWillie VanegasNoch keine Bewertungen
- Meroni2017 CompressedDokument8 SeitenMeroni2017 Compresseddayllyn iglesiasNoch keine Bewertungen
- Chirurgia Hemoragiei Din Ganglionii BazaliDokument8 SeitenChirurgia Hemoragiei Din Ganglionii BazaliAndreea DanielaNoch keine Bewertungen
- Rare and Fatal Complications of Tonsillectomy Sudden Pneumothorax and Extensive Subcutaneous EmphysemaDokument8 SeitenRare and Fatal Complications of Tonsillectomy Sudden Pneumothorax and Extensive Subcutaneous EmphysemaJoko NugrohoNoch keine Bewertungen
- AngiofibromaDokument7 SeitenAngiofibromaPandu DiputraNoch keine Bewertungen
- Primary Operative Renal Salvage of Grade-4 Blunt Renal Injury: A Case ReportDokument4 SeitenPrimary Operative Renal Salvage of Grade-4 Blunt Renal Injury: A Case ReportArsyad FadliNoch keine Bewertungen
- Ho Et Al 2022 Management of Descending Necrotizing Mediastinitis A Severe Complication of Deep Neck Infection Based OnDokument8 SeitenHo Et Al 2022 Management of Descending Necrotizing Mediastinitis A Severe Complication of Deep Neck Infection Based OncharlaayasyafefiNoch keine Bewertungen
- Middle Meningeal Artery Embolization For Chronic Subdural Hematoma in Elderly Patients at High Risk of Surgical TreatmentDokument8 SeitenMiddle Meningeal Artery Embolization For Chronic Subdural Hematoma in Elderly Patients at High Risk of Surgical TreatmentJUANNoch keine Bewertungen
- Tto VasoespasmoDokument6 SeitenTto VasoespasmoHernando CastrillónNoch keine Bewertungen
- 2 5373127936972950922Dokument6 Seiten2 5373127936972950922teguh sNoch keine Bewertungen
- Neurogenic Pulmonary Edema Due To Traumatic Brain Injury Evidence of Cardiac DysfunctionDokument10 SeitenNeurogenic Pulmonary Edema Due To Traumatic Brain Injury Evidence of Cardiac DysfunctionydtrgnNoch keine Bewertungen
- Postoperative Meningitis After Spinal Surgery: A Review of 21 Cases From 20,178 PatientsDokument5 SeitenPostoperative Meningitis After Spinal Surgery: A Review of 21 Cases From 20,178 PatientsntnquynhproNoch keine Bewertungen
- Septic PatientsDokument12 SeitenSeptic PatientsBruno NdoumouNoch keine Bewertungen
- Predictors of Cerebrospinal Fluid Leaks in Endoscopic Surgery For Pituitary TumorsDokument6 SeitenPredictors of Cerebrospinal Fluid Leaks in Endoscopic Surgery For Pituitary Tumorsfabian arassiNoch keine Bewertungen
- Jurnal AnastesiDokument7 SeitenJurnal AnastesiStefania MarlinaNoch keine Bewertungen
- Short - and Long-Term Outcomes at A Single InstitutionDokument7 SeitenShort - and Long-Term Outcomes at A Single InstitutionJonathan Frimpong AnsahNoch keine Bewertungen
- Intraoperative Hemoadsorption in High-Risk PatientDokument13 SeitenIntraoperative Hemoadsorption in High-Risk Patientmuhammad24fayazNoch keine Bewertungen
- 2018 - Article Erdocan 8p.pdf - CopieDokument6 Seiten2018 - Article Erdocan 8p.pdf - CopieThomas HussonNoch keine Bewertungen
- Precedex Delirium Spine - AA2023Dokument9 SeitenPrecedex Delirium Spine - AA2023Ahida VelazquezNoch keine Bewertungen
- Perioperative Management of AdrenalectomyDokument13 SeitenPerioperative Management of AdrenalectomyTJ LapuzNoch keine Bewertungen
- Intracerebral and Subarachnoid Hemorrhage in Patients With CancerDokument8 SeitenIntracerebral and Subarachnoid Hemorrhage in Patients With CancerMadeNoch keine Bewertungen
- EJCO - Volume 6 - Issue 2 - Pages 117-123Dokument7 SeitenEJCO - Volume 6 - Issue 2 - Pages 117-123doaa ahmadNoch keine Bewertungen
- Epidermoid Cysts TNEDokument10 SeitenEpidermoid Cysts TNEbello_england_209552Noch keine Bewertungen
- Ich - Inducido Por DrogasDokument14 SeitenIch - Inducido Por DrogasMarceloAndresCastañedaDuarteNoch keine Bewertungen
- Avaliação Ultra-Sonográfica Das Técnicas de Punção Da Veia Jugular Interna em CriançasDokument4 SeitenAvaliação Ultra-Sonográfica Das Técnicas de Punção Da Veia Jugular Interna em CriançasJing CruzNoch keine Bewertungen
- 1 s2.0 S0104001421000385 MainDokument4 Seiten1 s2.0 S0104001421000385 MainSuci dwi CahyaNoch keine Bewertungen
- Role of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyDokument6 SeitenRole of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyIJAR JOURNALNoch keine Bewertungen
- Original Article: ArticleinfoDokument5 SeitenOriginal Article: ArticleinfoBIOMEDSCIDIRECT PUBLICATIONSNoch keine Bewertungen
- Topical Steroids in Rhinosinusitis and Intraoperative Bleeding: More Harm Than Good?Dokument7 SeitenTopical Steroids in Rhinosinusitis and Intraoperative Bleeding: More Harm Than Good?lala poNoch keine Bewertungen
- Juvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyDokument3 SeitenJuvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyGiiszs AlvarezNoch keine Bewertungen
- (10920684 - Neurosurgical Focus) Falcotentorial Meningiomas - Clinical, Neuroimaging, and Surgical Features in Six PatientsDokument7 Seiten(10920684 - Neurosurgical Focus) Falcotentorial Meningiomas - Clinical, Neuroimaging, and Surgical Features in Six PatientsPutri PrameswariNoch keine Bewertungen
- Diagnosis and Treatment of Pericallosal Artery Aneurysms: SciencedirectDokument4 SeitenDiagnosis and Treatment of Pericallosal Artery Aneurysms: SciencedirectRais RyuzakiNoch keine Bewertungen
- Nihms 805170Dokument16 SeitenNihms 805170Santri WelayNoch keine Bewertungen
- HEMOPTISISDokument6 SeitenHEMOPTISISJufrialdy AldyNoch keine Bewertungen
- Juvenile Nasopharyngeal Angiofibroma: Mehmet Fatih Garça, Sevil Ari Yuca, Köksal YucaDokument7 SeitenJuvenile Nasopharyngeal Angiofibroma: Mehmet Fatih Garça, Sevil Ari Yuca, Köksal YucaIkaKusumaWardhaniNoch keine Bewertungen
- Hemagioma SCDokument5 SeitenHemagioma SCCelebre MualabaNoch keine Bewertungen
- Jurnal Bedah SarafDokument10 SeitenJurnal Bedah SarafSarah AmaniNoch keine Bewertungen
- Conclusion: Long-Term Follow-Up ForDokument31 SeitenConclusion: Long-Term Follow-Up ForHima HuNoch keine Bewertungen
- Peripheral Nerve Blocks For Above Knee Amputation in High-Risk PatientsDokument7 SeitenPeripheral Nerve Blocks For Above Knee Amputation in High-Risk PatientstiobuanaNoch keine Bewertungen
- DSADokument7 SeitenDSANantini GopalNoch keine Bewertungen
- Percutaneous Aortic Valve Implantation: The Anesthesiologist PerspectiveDokument11 SeitenPercutaneous Aortic Valve Implantation: The Anesthesiologist Perspectiveserena7205Noch keine Bewertungen
- Pericardiectomy For Tuberculous Effusive-Constrictive PericarditisDokument5 SeitenPericardiectomy For Tuberculous Effusive-Constrictive PericarditisIJAR JOURNALNoch keine Bewertungen
- Bilateral External Carotid Artery Ligation A LifeDokument3 SeitenBilateral External Carotid Artery Ligation A LifeYoshua Eric IrawanNoch keine Bewertungen
- CE (Ra1) F (RK) PF1 (AJ SL RK) PN (P)Dokument4 SeitenCE (Ra1) F (RK) PF1 (AJ SL RK) PN (P)karthik padmanathanNoch keine Bewertungen
- An Atypical Esthesioneuroblastoma of The Sphenoid Sinus A Case ReportDokument4 SeitenAn Atypical Esthesioneuroblastoma of The Sphenoid Sinus A Case ReportInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Application of Intracranial Pressure-Directed Therapy On DCIDokument9 SeitenApplication of Intracranial Pressure-Directed Therapy On DCIRonaldo MofuNoch keine Bewertungen
- Artigo HGF Neorologia Maio 2021Dokument11 SeitenArtigo HGF Neorologia Maio 2021Daniela MarinhoNoch keine Bewertungen
- Juvenile Nasopharyngeal AngiofibromaDokument16 SeitenJuvenile Nasopharyngeal AngiofibromaIren UbroNoch keine Bewertungen
- TTDokument11 SeitenTTRony palwagunaNoch keine Bewertungen
- Trauma EsplenicoDokument9 SeitenTrauma EsplenicoFelipe MayorcaNoch keine Bewertungen
- Extracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac ArrestDokument10 SeitenExtracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac Arrestika nur annisaNoch keine Bewertungen
- Jurnal SatyaDokument5 SeitenJurnal SatyaSatya WangsaNoch keine Bewertungen
- BCS NGT, Aspirasi AsitesDokument10 SeitenBCS NGT, Aspirasi AsitesSatya WangsaNoch keine Bewertungen
- Kasus:: Dka: Keton 5 Meq/L, Blood Glucose 250, PH 7.3, Ketonemia and Ketonuria, Serum Bicarbonate 18 Meq/L or LessDokument3 SeitenKasus:: Dka: Keton 5 Meq/L, Blood Glucose 250, PH 7.3, Ketonemia and Ketonuria, Serum Bicarbonate 18 Meq/L or LessSatya WangsaNoch keine Bewertungen
- 5 - ThrombopoiesisDokument3 Seiten5 - ThrombopoiesisSatya WangsaNoch keine Bewertungen
- Targeted Therapy in CancerDokument51 SeitenTargeted Therapy in CancerSatya WangsaNoch keine Bewertungen
- Wabah TBC Di IndiaDokument7 SeitenWabah TBC Di IndiaSatya WangsaNoch keine Bewertungen
- Wabah TBC Di VietnamDokument8 SeitenWabah TBC Di VietnamSatya WangsaNoch keine Bewertungen
- Biology Notes HSCDokument116 SeitenBiology Notes HSCYuki SuzukiNoch keine Bewertungen
- Micro HSB A - Myeloid Tissue HistologyDokument2 SeitenMicro HSB A - Myeloid Tissue HistologyGaelle Lisette MacatangayNoch keine Bewertungen
- GR 7 Ventures PEDokument232 SeitenGR 7 Ventures PEFaithNoch keine Bewertungen
- Types of Anaemia and How To Remember Them: With Sophie BroughtonDokument28 SeitenTypes of Anaemia and How To Remember Them: With Sophie BroughtonurtikikeNoch keine Bewertungen
- Pleading The Blood Is A Legal Thing!Dokument4 SeitenPleading The Blood Is A Legal Thing!Victor Ramlall100% (1)
- Group 7 Case StudyDokument4 SeitenGroup 7 Case StudyROSE GARETH SEGYEPNoch keine Bewertungen
- MANUAL ElectrophoresisDokument24 SeitenMANUAL ElectrophoresisMohamed Ali50% (2)
- Listening Script FullDokument93 SeitenListening Script FullkbalvinNoch keine Bewertungen
- Biopure Corporation - Pricing of OxyglobinDokument42 SeitenBiopure Corporation - Pricing of OxyglobinKotwal Mohit KotwalNoch keine Bewertungen
- MCQs On Respiration Physiology With KeyDokument7 SeitenMCQs On Respiration Physiology With KeyMudassar Roomi94% (31)
- 52 1023122 0 1Dokument7 Seiten52 1023122 0 1Kula Segara PandiyanNoch keine Bewertungen
- Sir Joseph Barcroft Obituario DHBarron Science1947Dokument2 SeitenSir Joseph Barcroft Obituario DHBarron Science1947Andrés MorenoNoch keine Bewertungen
- Warfarin Mechanism of Action, Indications AtfDokument4 SeitenWarfarin Mechanism of Action, Indications AtfAmir mohammad moori MohammadiNoch keine Bewertungen
- ( ) : Registration No.: Name (In English) : Class: Institution: Date of BirthDokument3 Seiten( ) : Registration No.: Name (In English) : Class: Institution: Date of Birtheverly.Noch keine Bewertungen
- Hematology NotesDokument3 SeitenHematology NotesFarisa Jane BanggoNoch keine Bewertungen
- Test Bank For Clinical Hematology and Fundamentals of Hemostasis 5th Edition HarmeningDokument6 SeitenTest Bank For Clinical Hematology and Fundamentals of Hemostasis 5th Edition HarmeningWilbur Penny100% (29)
- Book 9 PDFDokument33 SeitenBook 9 PDFMayuk KNoch keine Bewertungen
- Hematology Review NotesDokument28 SeitenHematology Review NoteszachNoch keine Bewertungen
- Minerals ChartDokument2 SeitenMinerals Chartautumn15_7Noch keine Bewertungen
- Hematology Lecture 1 - Blood and Its Components - BackupDokument51 SeitenHematology Lecture 1 - Blood and Its Components - BackupHaizickNoch keine Bewertungen
- Clinical Guideline: Sepsis in PregnancyDokument24 SeitenClinical Guideline: Sepsis in PregnancyYerni DaeliNoch keine Bewertungen
- Lecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Dokument58 SeitenLecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Kirt Anonuevo100% (3)
- Pathology - Chapter 14Dokument14 SeitenPathology - Chapter 14Cory GrayNoch keine Bewertungen
- Dr. Norhafiza Saad-24 PagesDokument37 SeitenDr. Norhafiza Saad-24 PagesCallumNoch keine Bewertungen
- DLL - SCIENCE - Q2 - W2Dokument8 SeitenDLL - SCIENCE - Q2 - W2Carole FuentesNoch keine Bewertungen
- Concept MapDokument4 SeitenConcept MapDud AccNoch keine Bewertungen
- Lesson 4 Hydrostatic Pressure Osunero, Kim John S. BSED 2D SCIE 4Dokument4 SeitenLesson 4 Hydrostatic Pressure Osunero, Kim John S. BSED 2D SCIE 4Kim John OsuneroNoch keine Bewertungen
- IB Biology Option D - Human Physiology HL A3 Revision SheetDokument1 SeiteIB Biology Option D - Human Physiology HL A3 Revision SheetMarwan PharaonNoch keine Bewertungen
- Adequacy of Perfusion During Cardiopulmonary BypassDokument64 SeitenAdequacy of Perfusion During Cardiopulmonary BypassBranka Kurtovic50% (2)
- DK-The British Medical Association-Complete Family Health GuideDokument992 SeitenDK-The British Medical Association-Complete Family Health Guidedangnghia211290% (10)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisVon EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisBewertung: 5 von 5 Sternen5/5 (8)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (5)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedBewertung: 4 von 5 Sternen4/5 (61)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (46)