Beruflich Dokumente
Kultur Dokumente
Medicine Card 2
Hochgeladen von
Theodore LiwonganCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Medicine Card 2
Hochgeladen von
Theodore LiwonganCopyright:
Verfügbare Formate
Symposium: The Rhinitis–Asthma Connection: One Linked Airway
The upper and lower airways: The epidemiological and
pathophysiological connection
Raymond G. Slavin, M.D., M.S.
ABSTRACT
The upper and lower airways do not exist as anatomically and functionally distinct areas. There are important relationships
between both the nose and the paranasal sinuses and asthma. Both allergic rhinitis and rhinosinusitis may impact bronchial
asthma. The patient with rhinitis should be observed carefully for the development of asthma, and those with asthma should be
considered to have either rhinitis or rhinosinusitis.
(Allergy Asthma Proc 29:553–556, 2008; doi: 10.2500/aap.2008.29.3169)
Key words: Allergic rhinitis, airway hyperreactivity, asthma, connection, epidemiology, inflammation, lower
airway, pathophysiology, rhinosinusitis, upper airway
Lesions in the nose and the sinuses are so common in
asthma as to be almost a clinical characteristic, and they
may be of diagnostic importance.
Frances Rackeman, M.D., 1931
M ore than three-quarters of a century ago, a Bos-
ton allergist in private practice made the afore-
mentioned statement. Dr. Rackeman astutely observed
may be associated with several comorbidities includ-
ing allergic conjunctivitis, rhinosinusitis, and asthma.
that rather than assuming that the upper and lower
Association of Allergic Rhinitis and Asthma
airways are anatomically and physiologically distinct,
there are important relationships between the two. There are a number of studies showing a significant
Specifically, diseases of the upper airway can impact association between allergic rhinitis and asthma (Table
unfavorably on the lower airway and worsen asthma. 1). In terms of coexistence, up to 80% of asthmatic
I would like to discuss two upper airway diseases, patients have been diagnosed with rhinitis.2 Asthma
viz., allergic rhinitis and rhinosinusitis, and their rela- has been diagnosed in up to 58% of patients with
tionships to asthma. I will deal largely with the epide- rhinitis.3 Rhinitis occurs simultaneously with or pre-
miological and pathophysiological connections. cedes asthma in up to 64% of patients.4 There is also
evidence that patients with asthma who deny symp-
toms of rhinitis have inflammatory changes in their
ALLERGIC RHINITIS nasal mucosa. Therefore, one may argue that in most
Allergic rhinitis is an extremely common disease, patients with asthma, the entire respiratory tract is
affecting ⬎40 million Americans. It has proven to be involved. This has prompted the introduction of the
quite costly, both directly in terms of dollars spent and term chronic allergic airways syndrome.5 At the lower
indirectly in terms of life-style impact.1 Allergic rhinitis end of the spectrum are patients with upper airway
diseases alone, whereas the high end consists of pa-
tients with both rhinitis and asthma. Nonallergic rhi-
nitis has also been found to be associated with asthma.6
From the Division of Immunobiology, Section of Allergy and Clinical Immunobiology,
Department of Internal Medicine, Saint Louis University School of Medicine, St. Patients with perennial rhinitis had almost four times
Louis, Missouri the incidence of asthma as patients with no rhinitis.
Presented at the meeting of the Eastern Allergy Society, Naples, Florida, May 4, 2008
There are no financial disclosures
Another example of comorbidity of rhinitis and
Raymond G. Slavin, M.D., M.S., Saint Louis University School of Medicine, 1402 asthma occurs in patients sensitive to aspirin and non-
South Grand Boulevard, St. Louis, MO 63106 steroidal anti-inflammatory drugs.7 In the workplace,
E-mail address: slavinrg@slu.edu
Copyright © 2008, OceanSide Publications, Inc., U.S.A.
symptoms of rhinitis are commonly associated with
occupational asthma. One study showed 92% of sub-
Allergy and Asthma Proceedings 553
Table 1 Interrelationships between allergic rhinitis Table 2 Similarities between the upper and lower
and asthma airways
Allergic rhinitis and asthma frequently coexist Anatomic
Allergic rhinitis is a risk factor for developing asthma Continuous basement membrane, pseudostratified
Rhinitis makes asthma worse columnar epithelium, mucosal transport, mucous
Nasal dysfunction may cause changes in lower glands, goblet cells, and innervation
airway function via both direct and indirect Circadian rhythm
mechanisms Triggers
Nonspecific (cold air and cigarette smoke)
Allergens (seasonal and nonseasonal)
jects with occupational asthma experienced rhinitis Patterns of inflammation
symptoms.8 Given all of these examples, it can be Hyperresponsiveness
stated that both allergic and nonallergic rhinitis are Acute late-phase response
strongly associated with asthma.
Rhinitis as a Risk Factor for Asthma Table 3 Changes in the nose that affect the lower
One of the most convincing studies indicating that airway
having allergic rhinitis predisposes to asthma was per-
formed at Brown University.9 More than 1800 incom- Filter function failure of nose: Increased allergen/
ing freshmen were evaluated for allergy. None of them irritant burden on lower airway
had asthma. Some of the group had allergic rhinitis Heat and humidification failure of nose: Exercise-
and were skin test positive, but the rest were negative induced asthma
by history and skin testing. The 23-year follow-up Increased lower airway responsiveness: Specific and
questionnaire revealed that the group who had allergic nonspecific
rhinitis as freshman had developed asthma three times Viral upper respiratory infection
more commonly than those with no history of allergic Nasal bronchial reflex
rhinitis. Of the group who developed asthma, 86% also
had allergic rhinitis. Among the participants with both
asthma and seasonal allergic rhinitis, 44.8% experi- mold) and perennial (house-dust mites and animals).
enced the development of seasonal allergic rhinitis The cellular mediators of inflammation for both in-
first, 34.5% experienced the development of asthma clude mast cells, eosinophils, basophils, and Th2 lym-
first, and 20.7% experienced the development of both phocytes. The number of eosinophils in the nose has
diseases at the same time. been shown to correlate with eosinophilic infiltration
in the bronchi. Finally, both the nose and the lung
Impact of Allergic Rhinitis on Asthma Severity show airway hyperresponsiveness as well as an acute
There appears to be evidence of increased symptom and late-phase response. In patients with pure rhinitis
severity, involving the entire respiratory tract, in pa- and no evidence of asthma, inhalation of methacholine,
tients with both rhinitis and asthma. In patients with a parasympathomimetic agent, results in an increase in
more severe rhinitis, a number of asthma parameters lower airway responsiveness that approaches that seen
are worsened including weekly attacks, nightly awak- in asthma.
ening, related work loss, and asthma severity as deter-
mined by the National Asthma Education Prevention Changes in the Nose That Affect the Lower Airway
Program designation.10 In addition to the horizontal relationship between
rhinitis and asthma (i.e., the impressive coexistence of
Anatomic and Physiological Similarities of Rhinitis rhinitis and asthma) there is also a vertical relationship,
and Asthma by which changes in the nose affect the lower airway
There are many similarities between the upper and (Table 3). One example is the important role the nose
lower airways including a continuous basement mem- plays in filtering, warming, and humidifying inspired
brane, pseudostratified columnar epithelium, mucosal air. If the nose is bypassed, more irritants, allergens,
transport, tubuloalveolar seromucous glands, goblet and colder drier air reach the lung, resulting in a wors-
cells, parasympathetic and sympathetic innervation, ening of asthma. In one study on exercise-induced
and circadian rhythm response (Table 2).11 Triggers for asthma, subjects with spontaneous breathing (i.e.,
upper and lower airway responsiveness are the same, breathing through the nose and mouth) showed a
including nonspecific irritants (e.g., cold air and ciga- slight decrease in forced expiratory volume in 1 second
rette smoke) and allergens, both seasonal (pollens and (FEV1) compared with subjects breathing exclusively
554 November–December 2008, Vol. 29, No. 6
through their nose. Mouth breathers showed a much Rhinosinusitis and Asthma
greater decline in FEV1 with exercise.12 It has been suggested that the term sinusitis be re-
Nasal provocation has also been shown to alter lower placed by rhinosinusitis, a more descriptive and accu-
airway function. Stimulation of the nose by histamine rate word for the following reasons. Rhinitis typically
or allergen resulted in a fall in FEV1 in patients with precedes sinusitis, sinusitis without rhinitis is rare, the
pure allergic rhinitis and no evidence of asthma either mucosa of the nose and sinuses is contiguous, and
clinically and/or by pulmonary function testing.13 In symptoms of nasal obstruction and nasal discharge are
another study, nasal challenge with allergen resulted in prominent in sinusitis.
an influx of eosinophils in nasal epithelium and lamina The frequent association of paranasal sinus disease
propria as well as in bronchial epithelium and lamina and bronchial asthma has been noted for many years.21
propria. In addition, there was an up-regulation of A number of clinical studies in the 1920s and 1930s
adhesion molecules ICAM-1, VCAM-1, and E-selectin. emphasized the importance of rhinosinusitis as a trig-
The local expression of these adhesion molecules in the ger for asthma. However, the relationship then seemed
bronchial epithelium correlated with the number of to fall into disrepute and little was written about the
mucosal eosinophils.14 The reverse also occurs with relationship for the next several decades. One prevail-
allergen bronchial challenge resulting in an increase in ing thought was that sinus changes simply reflected an
nasal mucosal eosinophils.15 Another example of the epiphenomenon, viz., a disease of the entire respiratory
upper and lower airway relationships is the effect of membrane. Therefore, management of rhinosinusitis
viral upper respiratory infections (URI) on asthma. per se would be expected to have little effect on the
Clearly, these infections are the most frequent cause of course of lower respiratory tract disease. In the last 20
emergency room visits and hospitalizations for years, the relationship of rhinosinusitis and asthma has
asthma. During a viral URI, the lower airway is more been revived.
responsive to both histamine and allergen inhalation.16 There is no question that a high incidence of radio-
Nasal inoculation with strain 16 rhinovirus in allergic graphic evidence of rhinosinusitis is present in patients
asthmatic patients resulted in an increase in circulating with asthma. A study from France22 indicated that
neutrophils 48 hours later, which correlated with an patients with mild-to-moderate asthma had an 87%
increase in nasal concentration of IL-8 and G-CSF. An incidence of abnormal sinus CTs while patients with
increase in bronchial neutrophils was seen 96 hours severe steroid-dependent asthma showed 100% abnor-
later.17 A clinical correlate may be that a short course mal sinus CT. In Finland23 there was an 87% abnormal
on montelukast, a leukotriene antagonist, has been CT sinus incidence in adults with asthma exacerba-
shown to improve asthma systems and health care tions. A later study in the Netherlands showed much
utilization in children experiencing a viral URI.18 the same thing; severe adult asthmatic patients had an
Evidence for a nasal-bronchial reflex has been seen in incidence of 87% abnormal sinus CT.24
studies on patients with unilateral trigeminal neuralgia
who underwent nerve resection. Briefly, nasal expo-
sure to silica on both sides of the nose showed a Mechanisms Relating Rhinosinusitis and Asthma
significant increase in lower airway resistance after Although a number of possibilities have been sug-
silica exposure on the intact side with no change seen gested, the precise mechanisms linking rhinosinusitis
on the resected side.19 to asthma are not known. One theory proposes that the
airway hyperresponsiveness seen in rhinosinusitis
Mechanisms Underlying Rhinitis and Asthma might depend on pharyngobronchial reflexes triggered
Connections by seeding of the inflammatory process into the phar-
A number of theories have been proposed to account ynx through postnasal drainage of mediators and in-
for the relationship between the nose and the lung. I fected material from affected sinuses. The theory is
have already alluded to the term chronic allergic air- based on the finding that intrabronchial and particu-
ways syndrome, sometimes referred to as the “one larly extrabronchial reactivity were strongly associated
airway– one disease” hypothesis. Denburg et al. found with the degree of pharyngitis as determined by his-
that after nasal allergen challenge, there was an in- tory, physical examination, and nasal lavage. In a later
crease in circulating mature basophils and eosinophils study, the authors showed actual damage of pharyn-
and an increase in progenitors of eosinophils and ba- geal mucosa in patients with chronic rhinosinusitis
sophiles. An increase in CD35⫹ cells was also seen, marked by epithelial thinning and a striking increase in
which is indicative of punitive progenitor cells of all pharyngeal nerve fiber density.25 This would favor an
linkages. Their conclusion was “that allergic inflamma- increase in excessive irritants to submucosal nerve end-
tion involves a systemic process in which the bone ings inducing the release of sensory neuropeptides via
marrow actively contributes to maintain and sustain axon reflexes with activation of a neural arch, resulting
disease and symptoms.”20 in reflex airway constriction.
Allergy and Asthma Proceedings 555
Another possibility is the same as proposed for the 10. Huse DM, Hartz SC, Russell MW, et al. Allergic rhinitis may
relationship between rhinitis and asthma, viz., the one- worsen asthma symptoms in children: The international asthma
outcomes registry. Am J Respir Crit Care Med 153:A860, 1996.
airway hypothesis. In a study of 22 patients with re-
11. Slavin RG. Interrelationships between the upper and lower
fractory chronic rhinosinusitis, there was a striking airways, Chap, 9. In Asthma, Slavin RG, and Reisman RE (Eds).
similarity of features with those of bronchial asthma Philadelphia: American College of Physicians, 131–140, 2002.
including eosinophilic inflammation, epithelial shed- 12. Shturman-Ellstein R, Zeballos RJ, Buckley JM, et al. The bene-
ding, and basement membrane thickening.26 Finally, a ficial effects of nasal breathing on exercise-induced brochocon-
striction. Am Rev Respir Dis 118:65–72, 1978.
systemic process could be involved with the inflamma-
13. Togias AG, Naclerio RM, Proud D, et al. Studies on the allergic
tory mucosa of rhinosinusitis releasing cytokines, and nonallergic nasal inflammation. J Allergy Clin Immunol
which stimulate the bone marrow to release inflamma- 81:782–790, 1988.
tory cells, which then migrate to the lung. 14. Braunstahl GJ, Overbeek SE, Klein JA, et al. Nasal allergen
provocation induces adhesion molecule expression and tissue
eosinophilia in upper and lower airways. J Allergy Clin Immu-
nol 107:469 – 479, 2001.
CONCLUSION 15. Braunstahl GJ, Kleinjen A, Overbeck SE, and Prins JB. Segmen-
Although the precise mechanisms have not been elu- tal bronchial provocation induces nasal inflammation in allergic
cidated, there appear to be important links between the rhinitis patients. Am J Respir Crit Care Med 161:2051–2057,
upper and lower airways. Physicians must be accus- 2000.
16. Lemanske RE Jr, Dick EC, Swenson LA, et al. Rhinovirus upper
tomed to examining both parts of the respiratory tract. respiratory infection increases airway hyperreactivity and late
Patients with rhinitis should be observed carefully for asthmatic responses. J Clin Invest 83:1–10, 1998.
the development or coexistence of asthma and those 17. Jarjour NN, Gern JE, Kelly EAB, et al. The effect of an experi-
with asthma should be considered to have rhinitis or mental rhinovirus 16 infection on bronchial lavage neutrophils.
rhinosinusitis. J Allergy Clin Immunol 105:1169 –1177, 2000.
18. Robertson CF, Price D, Henry R, et al. Short- course monte-
lukast for intermittent asthma in children. Am J Respir Crit Care
Med 175:323–329, 2007.
REFERENCES 19. Kaufman J, Chen J, and Wright GW. The effect of trigeminal
1. Nathan RS. The burden of allergic rhinitis. Allergy Asthma Proc resection on reflex bronchoconstruction after nasal and naso-
28:3–9, 2007. pharyngeal irritation in man. Am Rev Respir Dis 101:768 –773,
2. Simons FE. Allergic rhinobronchitis: The asthma–allergic rhini- 1970.
tis link. J Allergy Clin Immunol 104:534 –540, 1999. 20. Denburg JS, Sehmi R, Saito H, et al. Systemic aspects of allergic
3. Kapsali E, Horowitz F, Diemer F, and Togias A. Rhinitis is disease: Bone marrow responses. J Allergy Clin Immunol
ubiquitous in allergic asthmatics. J Allergy Clin Immunol 106(suppl):S292–S296, 2000.
99(suppl):S138, 1997. 21. Gottlbieb MJ. Relation of intranasal disease in the production of
4. Pedersen PA, and Weeke ER. Asthma and allergic rhinitis in the bronchial asthma. J Am Med Assoc 85:105–107, 1925.
same patients. Allergy 38:25–29, 1983. 22. Brescioani M, Paradis L, Roches AD, et al. Rhinosinusitis in
5. Togias AG. Systemic immunologic and inflammatory aspects of severe asthma. J Allergy Clin Immunol 107:73– 80, 2000.
allergic rhinitis. J Allergy Clin Immunol 106:S247–S250, 2000. 23. Rossi OV, Pirila T, Laitenen H, and Huhte E. Sinus aspirates and
6. Leynaert B, Neukvich F, Demoly P, and Bousquet J. Epidemio- radiographic abnormalities in severe attacks of asthma. Int Arch
logic evidence for asthma and rhinitis comorbidity. J Allergy Allergy Immunol 103:209 –213, 1994.
Clin Immunol 106:S201–S205, 2000. 24. ten Brincke A, Grootendorst DC, Schmidt JT, et al. Chronic
7. Stevenson DD. Drug-induced asthma, Chap. 13 In Asthma, sinusitis in severe asthma is related to sputum eosinophilia. J
Slavin RG, and Reisman RE (Eds). Philadelphia: American Col- Allergy Clin Immunol 109:621– 626, 2002.
lege of Physicians, 101–207, 2002. 25. Rolla G, Cologrand P, Scappaticci E, et al. Damage of the
8. Malo JL, Lemiere C, Desjardin A, et al. Prevalence and intensity pharyngeal mucosa and hyperresponsiveness of the airway in
of rhinoconjunctivitis in subjects with occupational asthma. Eur sinusitis. J Allergy Clin Immunol 100:52–57, 1997.
Respir J 710:1513–1515, 1997. 26. Ponikau JV, Sherris DA, Kephart GM, et al. Features of airway
9. Greisner WA III, Settipane RJ, and Settipane GA. Co-existence remodeling and eosinophile inflammation in chronic rhinosi-
of asthma and allergic rhinitis: A 23-year follow-up study of nusitis: Is the histopathology similar to asthma? J Allergy Clin
college students. Allergy Asthma Proc 19:185–188, 1998. Immunol 112:877– 882, 2003. e
556 November–December 2008, Vol. 29, No. 6
Das könnte Ihnen auch gefallen
- Main Idea 2Dokument3 SeitenMain Idea 2api-234576762100% (3)
- Rapid Assessment SheetDokument5 SeitenRapid Assessment SheetElise HowardNoch keine Bewertungen
- Anatomical TermsDokument8 SeitenAnatomical TermsDAGUMAN, FIONA DEI L.Noch keine Bewertungen
- Zoo Animal Flash Cards1 PDFDokument2 SeitenZoo Animal Flash Cards1 PDFsaraNoch keine Bewertungen
- Relationship Between Asthma and Rhinitis: Epidemiologic, Pathophysiologic, and Therapeutic AspectsDokument7 SeitenRelationship Between Asthma and Rhinitis: Epidemiologic, Pathophysiologic, and Therapeutic AspectsStanley SuhermanNoch keine Bewertungen
- Adakah Korelasi Antara Asthma Bronciale Dengan RhinosinusitisDokument3 SeitenAdakah Korelasi Antara Asthma Bronciale Dengan RhinosinusitisAkhta YudistiraNoch keine Bewertungen
- Chronic Dry Cough in Allergic Respiratory Diseases: Diagnostic and Management ApproachDokument6 SeitenChronic Dry Cough in Allergic Respiratory Diseases: Diagnostic and Management ApproachAaron HongreiNoch keine Bewertungen
- The United Allergic Airway: Connections Between Allergic Rhinitis, Asthma, and Chronic SinusitisDokument4 SeitenThe United Allergic Airway: Connections Between Allergic Rhinitis, Asthma, and Chronic SinusitisMuhammad NizarNoch keine Bewertungen
- Connection Between Allergic Rhinitis, Asma and SinusitisDokument4 SeitenConnection Between Allergic Rhinitis, Asma and Sinusitisأحمد نور الهدايةNoch keine Bewertungen
- Recent Developments in United Airways DiseaseDokument7 SeitenRecent Developments in United Airways DiseaseStanislaus Stanley SuhermanNoch keine Bewertungen
- Bronchial Asthma GuideDokument59 SeitenBronchial Asthma GuideJb TlntinoNoch keine Bewertungen
- Definisi AsmaDokument12 SeitenDefinisi AsmaDayu Punik ApsariNoch keine Bewertungen
- The Common Cold Current Therapy and Natural HistoDokument6 SeitenThe Common Cold Current Therapy and Natural HistoNur Wahdania PutriNoch keine Bewertungen
- Bab I Pendahuluan Latar Belakang: Universitas Sumatera UtaraDokument4 SeitenBab I Pendahuluan Latar Belakang: Universitas Sumatera UtarakobexNoch keine Bewertungen
- Allergic Rhinitis and Bronchial Asthma: Parthiv MehtaDokument4 SeitenAllergic Rhinitis and Bronchial Asthma: Parthiv MehtaAnisa Dinda NurlianaNoch keine Bewertungen
- OkanoDokument8 SeitenOkanostanleyNoch keine Bewertungen
- Chapter 9. Bronchial Asthma: Khaled O Hadeli MD, FCCPDokument19 SeitenChapter 9. Bronchial Asthma: Khaled O Hadeli MD, FCCPgireeshsachinNoch keine Bewertungen
- Lectures PPS Sinusitis - PpsDokument32 SeitenLectures PPS Sinusitis - PpsAlfonso Molina RamirezNoch keine Bewertungen
- Otorhinolaryngology: Allergic Laryngitis: Chronic Laryngitis and Allergic SensitizationDokument4 SeitenOtorhinolaryngology: Allergic Laryngitis: Chronic Laryngitis and Allergic SensitizationSyafira AlimNoch keine Bewertungen
- Allergy and Sinus Disease: Mja Practice Essentials - AllergyDokument1 SeiteAllergy and Sinus Disease: Mja Practice Essentials - AllergyGilang IrwansyahNoch keine Bewertungen
- Number 1Dokument3 SeitenNumber 1Michael HostiadiNoch keine Bewertungen
- Classification of AsthmaDokument4 SeitenClassification of AsthmaAlejandro LugoNoch keine Bewertungen
- United Airway DiseaseDokument41 SeitenUnited Airway DiseaseOlivia LieNoch keine Bewertungen
- Asthma: Allergy Asthma and Clinical Immunology November 2011Dokument10 SeitenAsthma: Allergy Asthma and Clinical Immunology November 2011Sarmad AlwardiNoch keine Bewertungen
- Rhinosinusitis PDFDokument14 SeitenRhinosinusitis PDFSekarrini VidyatamiNoch keine Bewertungen
- 909 FullDokument7 Seiten909 FullAndi Kumalasari MappaNoch keine Bewertungen
- Pa Tho Physiology of AsthmaDokument18 SeitenPa Tho Physiology of AsthmaNeil-Vince ConejosNoch keine Bewertungen
- AsthmaDokument118 SeitenAsthmaDaroo D.TNoch keine Bewertungen
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDokument15 SeitenWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsFitria SyafrinaNoch keine Bewertungen
- Allergic RhinitisDokument226 SeitenAllergic RhinitisGustavo Graco100% (1)
- 4 PDFDokument9 Seiten4 PDFAdan MorenoNoch keine Bewertungen
- Patogenesis de La RinitisDokument39 SeitenPatogenesis de La Rinitiskriss krammNoch keine Bewertungen
- Allergic Rhinitis and Its Impact On AsthmaDokument188 SeitenAllergic Rhinitis and Its Impact On AsthmaSergioNoch keine Bewertungen
- Asthma and COPD in Alpha 1 Antitrypsin Deficiency Evidence For The Dutch HypothesisDokument10 SeitenAsthma and COPD in Alpha 1 Antitrypsin Deficiency Evidence For The Dutch HypothesisMohammed SaleetNoch keine Bewertungen
- An Understanding of The Genetic Basis of Asthma: Review ArticleDokument13 SeitenAn Understanding of The Genetic Basis of Asthma: Review ArticlerastiooNoch keine Bewertungen
- Aeroallergens, Air Pollutants, and Chronic Rhinitis and RhinosinusitisDokument7 SeitenAeroallergens, Air Pollutants, and Chronic Rhinitis and RhinosinusitisRidho RifhansyahNoch keine Bewertungen
- Chronic Cough Guide: Causes, Symptoms and TreatmentsDokument7 SeitenChronic Cough Guide: Causes, Symptoms and TreatmentsChandra LathifNoch keine Bewertungen
- Allergic Rhinitis: Review Open AccessDokument8 SeitenAllergic Rhinitis: Review Open AccessJuanNoch keine Bewertungen
- Asthma: (Assignment 2)Dokument8 SeitenAsthma: (Assignment 2)nuraNoch keine Bewertungen
- Zhu 18 05Dokument8 SeitenZhu 18 05ABNoch keine Bewertungen
- Mechanisms of Asthma: William W. Busse, MD, and Lanny J. Rosenwasser, MDDokument6 SeitenMechanisms of Asthma: William W. Busse, MD, and Lanny J. Rosenwasser, MDaulia kamal ansari panggabeanNoch keine Bewertungen
- ASTHMADokument17 SeitenASTHMAvinda astri permatasariNoch keine Bewertungen
- 10 1016@j Aller 2012 08 004Dokument8 Seiten10 1016@j Aller 2012 08 004Muhammad FakhrizalNoch keine Bewertungen
- Asthma Lecture: Chronic Airway Inflammation, Triggers, and TreatmentDokument23 SeitenAsthma Lecture: Chronic Airway Inflammation, Triggers, and TreatmentShannon RamsumairNoch keine Bewertungen
- 1 s2.0 S1526054219300818 MainDokument10 Seiten1 s2.0 S1526054219300818 MainAna LarrabeitiNoch keine Bewertungen
- Sam CD Asthma ReciveredDokument36 SeitenSam CD Asthma ReciveredDr. Muha. Hasan Mahbub-Ur-RahmanNoch keine Bewertungen
- Asthma 2Dokument8 SeitenAsthma 2Evangelist Stephen NziokaNoch keine Bewertungen
- Allergic Rhinitis History and Presentation PDFDokument6 SeitenAllergic Rhinitis History and Presentation PDFJimena LopezNoch keine Bewertungen
- Management of Allergic Rhinitis: P. Van Cauwenberge, H. Van HoeckeDokument20 SeitenManagement of Allergic Rhinitis: P. Van Cauwenberge, H. Van HoeckePeter SalimNoch keine Bewertungen
- HHS Public Access: Asthma in The Primary Care SettingDokument20 SeitenHHS Public Access: Asthma in The Primary Care SettingKarina UtariNoch keine Bewertungen
- Asthma: A Guide to the Heterogeneous DiseaseDokument18 SeitenAsthma: A Guide to the Heterogeneous DiseaseSam HuntNoch keine Bewertungen
- The Pathophysiology - Diagnosis and Treatment of Allergic RhinitisDokument16 SeitenThe Pathophysiology - Diagnosis and Treatment of Allergic RhinitisAnonymous XFDJfsGviNoch keine Bewertungen
- Jurnal CDCDokument9 SeitenJurnal CDCPutri WafiroNoch keine Bewertungen
- All 73 50Dokument14 SeitenAll 73 50Adinda NadiaNoch keine Bewertungen
- Acute Severe AsthmaDokument5 SeitenAcute Severe AsthmaRizsa Aulia DanestyNoch keine Bewertungen
- Asthma in elderly patientsDokument6 SeitenAsthma in elderly patientsbrakim23Noch keine Bewertungen
- Asma Exacerbacioes EpidemiologiaDokument7 SeitenAsma Exacerbacioes Epidemiologiahebert ramosNoch keine Bewertungen
- 5485 Jurnal Edit - Fix.2pptxDokument36 Seiten5485 Jurnal Edit - Fix.2pptxAdita AyuNoch keine Bewertungen
- 4 - AsthmaDokument14 Seiten4 - AsthmaAmmar AlnajjarNoch keine Bewertungen
- Bronchial Asthma GuideDokument72 SeitenBronchial Asthma GuidePrincewill SeiyefaNoch keine Bewertungen
- Asthma Treatment Breakthrough: Mepolizumab Relieves Severe CasesDokument8 SeitenAsthma Treatment Breakthrough: Mepolizumab Relieves Severe CasesCandha NurcahyaNoch keine Bewertungen
- Dafpus Baru 1Dokument3 SeitenDafpus Baru 1stanleyNoch keine Bewertungen
- Rhinitis Alergi 1Dokument7 SeitenRhinitis Alergi 1Dian PrastiwiNoch keine Bewertungen
- The Toxicant Induction of Irritant Asthma, Rhinitis, and Related ConditionsVon EverandThe Toxicant Induction of Irritant Asthma, Rhinitis, and Related ConditionsNoch keine Bewertungen
- WJG 19 9003 PDFDokument10 SeitenWJG 19 9003 PDFTheodore LiwonganNoch keine Bewertungen
- 1 PB PDFDokument11 Seiten1 PB PDFTheodore LiwonganNoch keine Bewertungen
- ADokument7 SeitenATheodore LiwonganNoch keine Bewertungen
- Statin Use and The Risk of Dementia in Patients With Stroke: A Nationwide Population-Based Cohort StudyDokument7 SeitenStatin Use and The Risk of Dementia in Patients With Stroke: A Nationwide Population-Based Cohort StudyTheodore LiwonganNoch keine Bewertungen
- Venkat Esh 2008Dokument10 SeitenVenkat Esh 2008Theodore LiwonganNoch keine Bewertungen
- Pathophysiology of Empty Nose Syndrome: Contemporary ReviewDokument5 SeitenPathophysiology of Empty Nose Syndrome: Contemporary ReviewTheodore LiwonganNoch keine Bewertungen
- Chronic PancreatitisDokument23 SeitenChronic PancreatitisAlvin YeeNoch keine Bewertungen
- JNC 8 Guideline Algorithm for Treating HypertensionDokument2 SeitenJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- Venkat Esh 2008Dokument10 SeitenVenkat Esh 2008Theodore LiwonganNoch keine Bewertungen
- 81 89 PDFDokument9 Seiten81 89 PDFSuril VithalaniNoch keine Bewertungen
- AC0100NAUV10NrHU0r0 Nl AdocsooNf crrsoNcvto l0 svlrv u010cDokument3 SeitenAC0100NAUV10NrHU0r0 Nl AdocsooNf crrsoNcvto l0 svlrv u010cTheodore LiwonganNoch keine Bewertungen
- Cellulitis 01Dokument3 SeitenCellulitis 01Farid Fauzi A ManwanNoch keine Bewertungen
- Medicine Card 2Dokument1 SeiteMedicine Card 2ladki6Noch keine Bewertungen
- Learn Dengue Clinical Case ManagementDokument1 SeiteLearn Dengue Clinical Case ManagementArdhiNoch keine Bewertungen
- Human Anatomy Essay Test QuestionsDokument2 SeitenHuman Anatomy Essay Test QuestionsvelangniNoch keine Bewertungen
- History Taking Note CardDokument3 SeitenHistory Taking Note Cardrmelendez001100% (1)
- Dissection Rules and ProceduresDokument1 SeiteDissection Rules and ProceduresTheodore LiwonganNoch keine Bewertungen
- Predicting bacterial conjunctivitisDokument5 SeitenPredicting bacterial conjunctivitisTheodore LiwonganNoch keine Bewertungen
- OSSIFIED LIGAMENTDokument3 SeitenOSSIFIED LIGAMENTTheodore LiwonganNoch keine Bewertungen
- Osteology 1Dokument1 SeiteOsteology 1Theodore LiwonganNoch keine Bewertungen
- Print Endocrine System Exam FlashcardsDokument10 SeitenPrint Endocrine System Exam FlashcardsTheodore LiwonganNoch keine Bewertungen
- Book1 PDFDokument2 SeitenBook1 PDFTheodore LiwonganNoch keine Bewertungen
- Personal DevelopmentDokument2 SeitenPersonal DevelopmentTheodore LiwonganNoch keine Bewertungen
- Print Endocrine System Exam FlashcardsDokument10 SeitenPrint Endocrine System Exam FlashcardsTheodore LiwonganNoch keine Bewertungen
- Setting and Reaching Academic GoalsDokument2 SeitenSetting and Reaching Academic GoalsTheodore LiwonganNoch keine Bewertungen
- Bls Skill SheetsDokument141 SeitenBls Skill SheetsTheodore Liwongan100% (1)
- Document 1Dokument2 SeitenDocument 1Theodore LiwonganNoch keine Bewertungen
- First Aid SummaryDokument4 SeitenFirst Aid SummaryTheodore LiwonganNoch keine Bewertungen
- National Emergency Medical ServicesDokument129 SeitenNational Emergency Medical ServicesTheodore Liwongan100% (1)
- 2013 Skin and Wound Infections - StudentDokument35 Seiten2013 Skin and Wound Infections - Studentmicroperadeniya0% (1)
- Eng GR WorksheetDokument36 SeitenEng GR WorksheetrupNoch keine Bewertungen
- The Five-Minute Daily Energy RoutineDokument4 SeitenThe Five-Minute Daily Energy RoutineSatinder Bhalla100% (1)
- Active and Passive Voice Exercise: 1. I Did Not Beat HerDokument2 SeitenActive and Passive Voice Exercise: 1. I Did Not Beat HerAlex Halliwell67% (3)
- Chapter II - Bodies of Fire - The Accupuncture MeridiansDokument41 SeitenChapter II - Bodies of Fire - The Accupuncture MeridiansScott Canter100% (1)
- Comparative Anatomy Classification ChartDokument2 SeitenComparative Anatomy Classification Chartapi-613673827Noch keine Bewertungen
- Rood S ApproachDokument33 SeitenRood S Approachmedway physio teamNoch keine Bewertungen
- Fables Grade 2Dokument4 SeitenFables Grade 2angeliNoch keine Bewertungen
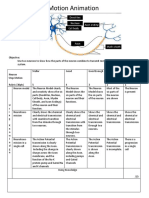
- Neurons Stop Motion AnimationDokument2 SeitenNeurons Stop Motion Animationapi-495006167Noch keine Bewertungen
- Eucoelomates Lab ReportDokument13 SeitenEucoelomates Lab Reportsatvindar singhNoch keine Bewertungen
- Lab6 Fossilization PDFDokument9 SeitenLab6 Fossilization PDFjimmypsNoch keine Bewertungen
- Task 6 and 7 ANIMALSDokument2 SeitenTask 6 and 7 ANIMALSRonny AlexanderNoch keine Bewertungen
- How To Clicker Train Your Cat PDFDokument5 SeitenHow To Clicker Train Your Cat PDFNesly100% (1)
- Art336 Pre Lab 9Dokument4 SeitenArt336 Pre Lab 9rian afriansyahNoch keine Bewertungen
- Soal Bahasa Inggris Kelas 11 IpaDokument6 SeitenSoal Bahasa Inggris Kelas 11 IpaDavid SyaifudinNoch keine Bewertungen
- NEET UG Biology Evolution PDFDokument22 SeitenNEET UG Biology Evolution PDFamsaeangovanNoch keine Bewertungen
- Story-Telling Competition Title: The Milkmaid and Her PailDokument6 SeitenStory-Telling Competition Title: The Milkmaid and Her PailCoffee&LoveNoch keine Bewertungen
- How Evolution Occurs Beyond Natural SelectionDokument6 SeitenHow Evolution Occurs Beyond Natural Selectionbrenden chapmanNoch keine Bewertungen
- Demidov - A Shooting Trip To Kamchatka 1904Dokument360 SeitenDemidov - A Shooting Trip To Kamchatka 1904Tibor Bánfalvi100% (1)
- Kriteria Diagnosis ObgynDokument6 SeitenKriteria Diagnosis ObgynJustisiani Fatiria, M.D.Noch keine Bewertungen
- Cure - Family Health MatterzDokument14 SeitenCure - Family Health MatterzGeorge AniborNoch keine Bewertungen
- Mosaic - TRD1 - U2 - EP CorregidoDokument6 SeitenMosaic - TRD1 - U2 - EP CorregidoSonia Daniela Ayuso FrutosNoch keine Bewertungen
- The Teachings of DiogenesDokument14 SeitenThe Teachings of Diogenesryanash777100% (1)
- The Cat Burglar's RetirementDokument3 SeitenThe Cat Burglar's RetirementrachaelNoch keine Bewertungen
- 2nd QRTR Anet ReteachDokument13 Seiten2nd QRTR Anet Reteachapi-310709379Noch keine Bewertungen
- GCC Customs Tariff 2017 for Live Animals & Animal ProductsDokument435 SeitenGCC Customs Tariff 2017 for Live Animals & Animal ProductsColin LoboNoch keine Bewertungen