Beruflich Dokumente
Kultur Dokumente
Gardiner 2019
Hochgeladen von
Desmiyati AdoeCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Gardiner 2019
Hochgeladen von
Desmiyati AdoeCopyright:
Verfügbare Formate
ARTICLE IN PRESS
THE JOURNAL OF PEDIATRICS • www.jpeds.com ORIGINAL
ARTICLES
Randomized Clinical Trial Comparing Breath-Enhanced to Conventional
Nebulizers in the Treatment of Children with Acute Asthma
Mike A. Gardiner, MD1, and Matthew H. Wilkinson, MD, MPH2
Objective To compare the efficacy of a breath-enhanced and a conventional jet nebulizer in the treatment of chil-
dren with moderate to severe acute asthma.
Study design We enrolled subjects between 6 and 18 years of age presenting to the emergency department
(ED) with acute asthma and an initial forced expiratory volume in 1 second (FEV1) <70% of predicted. We ex-
cluded patients with chronic disease, who required immediate resuscitation, or failed spirometry. Subjects were ran-
domized to breath-enhanced or conventional jet delivery of a 5-mg albuterol treatment. Our primary outcome was
change in FEV1, and secondary outcomes included change in clinical asthma scores, ED length of stay, disposi-
tion, and side effects. Student t test and multivariable linear regression were used to evaluate the primary outcome.
Results In total, 497 patients were assessed for eligibility with 118 enrolled and 107 subjects available for analy-
sis of the primary outcome. Improvement in FEV1 was significantly greater with conventional jet nebulizer (mean
DFEV1 +13.8% vs +9.1%, P = .04). This difference remained significant after adjustment for baseline differences.
Subgroup analysis of 57 subjects with spirometry meeting American Thoracic Society/European Respiratory Society
guidelines yielded similar results (mean DFEV1 +14.5% vs +8.5%, P=.03). There were no significant differences in
clinical asthma scores, ED length of stay, disposition, or side effects.
Conclusions Albuterol delivered via conventional jet nebulizer resulted in significantly greater improvement in
FEV1 than albuterol delivered by breath-enhanced nebulizer, without significant differences in clinical measures.
Conventional jet nebulizers may deliver albuterol to children with acute asthma more effectively than breath-
enhanced nebulizers. (J Pediatr 2018;■■:■■-■■).
Trial registration ClinicalTrials.gov: NCT02566902.
sthma exacerbations are among the most frequent reasons for children to visit the emergency department (ED).1 Current
A standard of care treatment of acute asthma includes administration of an inhaled short acting b2-agonist, systemic glu-
cocorticoids, and correction of hypoxemia.2 Although it has long been accepted that the use of inhaled short acting
b2-agonist is efficacious, there have been efforts to develop more effective and efficient means of delivering aerosolized medications.
Breath-enhanced nebulizers are one of several new technology nebulizers designed to more effectively deliver aerosolized medi-
cation. Breath-enhanced nebulizers continuously nebulize medication into a holding chamber, using a system of 1-way valves
to direct exhaled air away from the holding chamber. This design minimizes medication loss upon exhalation and allows de-
livery of a bolus dose of nebulized aerosol.3-5 Although breath-enhanced nebulizer studies on in vitro lung models and healthy
adult subjects have demonstrated improved lung deposition of aerosol,3-8 study in children with acute asthma is lacking. To
our knowledge, only 1 prior study has evaluated breath-enhanced nebulizers in
pediatric patients with acute asthma.9 This study demonstrated that a breath-
enhanced treatment algorithm was noninferior to a conventional jet algorithm,
however, was limited by small sample size and did not evaluate spirometry data.
From the 1Department of Pediatrics, University of
We performed a prospective blinded-observer randomized clinical trial to test California, San Diego, Rady Children’s Hospital—San
the hypothesis that the use of a breath-enhanced nebulizer for albuterol delivery Diego, La Jolla, CA; and 2Department of Pediatrics,
University of Texas at Austin, Dell Children’s Medical
leads to a greater improvement in forced expiratory volume in 1 second (FEV1) Center of Central Texas, Austin, TX
than use of a conventional jet nebulizer in children presenting to a pediatric ED Funded by a 2014 Scientific, Education and Research
Foundation of University of Texas—Southwestern-Austin
with a moderate to severe acute asthma exacerbation. Prior to implementation Research/Fellow Grant (SERF-RG). All funds used
for study supplies and equipment. University of
into practice, this study of breath-enhanced nebulizers was necessary to evaluate Texas—Southwestern did not participate in study design,
collection, analysis or interpretation of data, writing of this
manuscript, or decision to submit for publication. M.W.
served as a consultant for and received grant funding
from Salter Labs. The authors declare no conflicts of
interest.
ATS American Thoracic Society Portions of this study were presented at the Pediatric
Academic Societies annual meeting, May 5-8, 2018,
ED Emergency department Toronto, Ontario, and as a poster at the University of
ERS European Respiratory Society California, San Diego/Rady Children’s Hospital Pediatric
FEV1 Forced expiratory volume in 1 second Research Symposium, May 10, 2018, San Diego,
California.
MDI Metered-dose inhaler
PAS Pediatric Asthma Score 0022-3476/$ - see front matter. © 2018 Elsevier Inc. All rights
PASS Pediatric Asthma Severity Score reserved.
https://doi.org10.1016/j.jpeds.2018.08.083
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■ • ■■ 2018
whether they provide improved bronchodilation compared with breath-enhanced nebulizer led to greater lung deposition, that
less expensive conventional jet nebulizers. larger or repeated doses of albuterol delivered by breath-
enhanced nebulizers may result in unacceptable side effects.
Methods Patients randomized to the breath-enhanced group re-
ceived therapy with a NebuTech HDN, Breath-Enhanced High-
This study was performed as a blinded-observer randomized Density Jet Nebulizer (Salter Labs, Arvin, California) via
clinical trial at a large urban pediatric ED with an annual mouthpiece. Patients randomized to the conventional jet arm
volume of approximately 80 000 visits. The study was ap- received therapy with a Hudson RCI Micro Mist nebulizer
proved by the hospital’s Institutional Review Board and reg- (Teleflex Medical, Research Triangle Park, New Jersey) via
istered on www.clinicaltrials.gov (NCT02566902). We enrolled mouthpiece. Both study arms received 5-mg nebulized albuterol
a convenience sample of children with physician-diagnosed diluted to 3.5 mL with 0.9% normal saline. Nebulizers were
asthma, age 6 and 18 years with English or Spanish speaking attached to wall oxygen at a flow rate of 8 liters per minute
guardian(s), presenting to the pediatric ED with symptoms of and treatment was continued until solution was completely
acute asthma, objective signs of acute asthma (pediatric asthma nebulized. Steroid administration and other therapies were used
score >0), and an FEV1 less than 70% predicted on initial spi- per ED protocol at treating physician discretion and were not
rometry (moderate to severe asthma exacerbation).2,10,11 Po- included as a part of study protocol.
tential subjects were excluded if they were unable to perform Computerized 1:1 randomization was completed prior to
initial spirometry, had chronic diseases other than asthma, re- the start of the study. Blinding of the enrolling personnel was
quired immediate resuscitation at the discretion of the treat- accomplished by creating identical opaque study boxes for each
ing physician, received albuterol in the ED prior to enrollment, subject, labeled only with the subject identification, prior to
or if there were not 2 available study personnel at the time of the start of the study. These boxes contained the subject’s pre-
ED arrival. assigned nebulizer (breath-enhanced or conventional jet) and
Written informed consent and Health Insurance Portabil- were only opened by the study personnel administering study
ity and Accountability Act authorization were obtained from medication. Boxes were created and sealed by a participant not
each subject’s parent or guardian, and written assent was ob- otherwise involved with the study and maintained in a locked
tained from all subjects aged seven years or older. This study office and until the time of randomization so as to not reveal
received funding from a small institutional grant, which was group allocation until the time of enrollment. Study boxes were
used for purchase of study supplies. identical in appearance and had similar weight regardless of
Potential subjects were identified and enrolled at the time nebulizer type contained. Adequacy of blinding was assessed
of ED triage, prior to administration of albuterol in the ED. after study completion by asking the blinded study person-
Enrolling study personnel remained blinded to group alloca- nel to predict which nebulizer was used and comparing this
tion throughout the study (blinded-observer) and were re- prediction with the assigned study arm by c2 analysis.
sponsible for data collection. At the time of enrollment baseline Study personnel consisted of pediatric emergency medi-
spirometry measurement, initial vital signs, and clinical asthma cine fellows and attending physicians, with 1 research nurse
severity were recorded. Clinical asthma severity was assessed who was trained on study enrollment. All study personnel un-
using 2 previously validated clinical asthma scores, the Pedi- derwent a training session detailing consent and enrollment
atric Asthma Score (PAS) and Pediatric Asthma Severity Score for this study. As a part of this training, proper spirometry tech-
(PASS) (Appendix 1; available at www.jpeds.com).12,13 Study nique and methods for encouraging spirometry effort were re-
subjects were randomized to receive treatment with either the viewed, with all personnel required to demonstrate the ability
experimental (breath-enhanced) or control (conventional jet) to perform beside spirometry and medication administra-
nebulizer. A parallel study design with 1:1 group allocation was tion prior to being cleared for participation.
used. A second unblinded member of the study team re- Spirometry was performed in the ED with a handheld spi-
vealed group allocation by opening a pre-assigned study box rometer (ndd EasyOne Plus, ndd Medical Technologies, Inc,
containing either the control or experimental nebulizer and Andover, Massachusetts). This spirometer has been previ-
administered a 5-mg nebulized albuterol treatment to the ously validated compared with formal spirometry in adult
subject via the provided nebulizer. Ten minutes following subjects.14 In keeping with the most recent American Tho-
completion of the study treatment, the blinded enrolling study racic Society/European Respiratory Society (ATS/ERS) guide-
personnel completed a post-treatment assessment of the subject lines, participants performed a minimum of 3 and maximum
including spirometry, vital signs, clinical asthma severity, and of 8 forced expiratory maneuvers to obtain 1-3 adequate
treatment side effects. Subjects who required further treat- samples.15 FEV1 calculation was performed by the spirometer
ment were released to standard of care treatment at the dis- based on National Health and Nutrition Examination Survey
cretion of the treating emergency physician, with further III study data.10 The highest recorded FEV1 was used for analy-
treatments delivered by conventional jet nebulizer. This single- sis. Adequacy of spirometry maneuvers was assessed by the spi-
treatment study design was chosen to allow for equal treat- rometer which provided letter grades A-F based on acceptability
ments to all subjects regardless of whether they only required of maneuvers (Appendix 2; available at www.jpeds.com). For
a single ED treatment, or several treatments and hospital the purposes of this study, grades A-D were deemed
admission. In addition, there was concern that if the adequate for enrollment. This acceptability range was chosen
2 Gardiner and Wilkinson
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
■■ 2018 ORIGINAL ARTICLES
to include all subjects able to perform at least 1 acceptable ma-
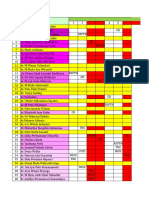
Table I. Baseline characteristics at study enrollment
neuver. Subjects with pre and post-treatment spirometry of
grades A or B met stricter ATS/ERS guidelines for acceptable Conventional
Variables jet Breath-enhanced
spirometry and were evaluated by subgroup analysis. Spirom-
etry attempts were deemed subjectively unacceptable by study Number analyzed, total no (1° outcome) 58 (55) 57 (52)
Age, y, mean (SD) 9.8 (2.6) 10.1 (3.0)
personnel if the subject demonstrated immediate cough, glottis Sex, male, no (%) 37 (63.8) 27 (47.4)
closure, significant leak, mouthpiece obstruction, or early ter- Baseline severity, no (%)
mination of exhalation. Mild intermittent 20 (34.5) 27 (47.4)
Mild persistent 11 (19.0) 12 (21.0)
The primary outcome measure was improvement in FEV1 Moderate persistent 20 (34.5) 14 (24.6)
as measured by absolute improvement in percent of pre- Severe persistent 7 (12.0) 4 (7.0)
dicted. Measurement of FEV1 has been used throughout prior Ethnicity, no (%)
Hispanic 30 (51.7) 33 (57.9)
asthma literature as a reliable measure of airway obstruction African American 25 (43.1) 21 (36.8)
and effectiveness of treatment in patients with acute asthma.16-19 Caucasian 3 (5.2) 3 (5.3)
FEV1 measurement has been recommended by the National Weight, kg, mean (SD) 39.5 (16.4) 41.1 (16.5)
BMI, mean (SD) 19.7 (5.7) 19.7 (5.0)
Heart, Lung, and Blood Institute as a means of assessing the Duration of symptoms, d, median (IQR) 2 (1-3) 2 (2-3)
degree of airway obstruction, and response to therapy in acute Albuterol last 24 h, doses, median (IQR) 2 (0-4) 4 (2-6)
asthma.2 Secondary outcomes included change in asthma se- Nebulized, doses 0 (0-1) 1 (0-3)
MDI, doses 1 (0-2.75) 2 (2-4)
verity scores (PAS and PASS), ED length of stay, admission rate, Pre-arrival steroids, no (%) 8 (13.8) 2 (3.5)
and side effects. ED steroids prior to study treatment, 37 (63.8) 38 (66.7)
By evaluating data from previously performed studies,16-18,20 no (%)
Initial RR, breaths/min, mean (SD) 28.1 (9.4) 28.9 (7.6)
a sample size calculation was performed with a 2-sided a of Initial O2, % saturation, mean (SD) 96.0 (2.1) 95.7 (2.6)
0.05, b of 0.20. With the assumptions that control group would Initial PAS score, median (IQR) 4 (3-5) 4 (2-5)
experience an absolute improvement in FEV1 of 10% pre- Initial PASS score, median (IQR) 2 (2-3) 2 (1-3)
Initial FEV1, % predicted, mean (SD) 39.4 (13.4) 42.0 (14.8)
dicted, with a standard deviation of 10% predicted, it was cal-
culated that 128 subjects with adequate spirometry would be BMI, body mass index; O2, oxygen saturation; RR, respiratory rate.
needed to detect an improvement differential of 5% of pre-
dicted between treatment arms.
Treatment groups were analyzed on an intention-to-treat Three subjects were erroneously enrolled and randomized
basis. The primary outcome of change in FEV1 was analyzed who did not meet the predefined inclusion and exclusion cri-
using a 2-tailed Student t test. A multivariable linear regres- teria (Figure). In the breath-enhanced group, 1 subject had an
sion model was used to assess for the potential confounding initial FEV1 >70% of predicted, and in the conventional jet
effect of differences in baseline demographic and illness char- group 1 subject had an initial FEV1 >70% of predicted, and
acteristics on the primary outcome. Our regression model was another had been previously enrolled in this study. As these
created using purposeful variable selection with an entry cri- subjects objectively did not meet our enrollment criteria, they
terion of P < .2 and P < .05 required for final model reten- were excluded from the intention-to-treat analysis.21
tion. Changes in clinical asthma scores were evaluated by Mann- Results for primary and secondary outcomes are detailed
Whitney U test, admission rate and medication side effects by in Table II. Analysis of changes in FEV1 demonstrated that sub-
c2 or Fisher exact tests, and ED length of stay by 2-tailed Student jects treated with the control conventional jet nebulizer had
t test. All statistical analyses were performed using STATA 15 a statistically significantly greater improvement in FEV1 than
(StataCorp LLC, College Station, Texas). those treated with the breath-enhanced nebulizer (mean DFEV1
+13.8% vs +9.1% of predicted, P = .04). This difference between
Results groups remained statistically significant after multivariable linear
regression (P = .02). All variables in Table I were evaluated for
Subjects were enrolled over a 20-month period from October entry into the model and only initial respiratory rate (P = .01),
2015 to May 2017 at which time the principal investigator asthma severity prior to acute exacerbation (P = .05), and steroid
changed institutions and study was stopped. In total, 497 po- administration prior to ED arrival (P = .001) showed statis-
tential subjects were screened for eligibility. Of those screened, tical significance and were retained in the final model. Sub-
118 subjects met inclusion criteria and were randomized. Of group analysis of the 57 subjects who met ATS/ERS spirometry
these subjects, 107 were analyzed for the primary outcome and guidelines showed a similar difference between groups (mean
115 subjects analyzed for secondary outcomes (Figure; avail- DFEV1 +14.5% vs +8.5% of predicted, P = .03). There were no
able at www.jpeds.com). The baseline demographics and char- significant differences between groups in secondary out-
acteristics of the acute asthma episode are detailed in Table I. comes including changes in PAS (P = .29), PASS (P = .97), ED
Subjects in the breath-enhanced arm were less commonly male, length of stay (P = .99), or admission rate (P = .96). Ob-
had lower baseline asthma severity, received more albuterol in served side effects were nausea, vomiting, headache, dizzi-
the 24 hours prior to arrival to the ED, and had a lower pro- ness, palpitations, tremor/shakiness, and weakness. These side
portion of subjects who had received oral steroids prior to ED effects were all transient and were not statistically different
arrival. The 2 groups were otherwise similar. between groups. Assessment of blinding revealed no significant
Randomized Clinical Trial Comparing Breath-Enhanced to Conventional Nebulizers in the Treatment of 3
Children with Acute Asthma
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
We identify several potential limitations of our study. The
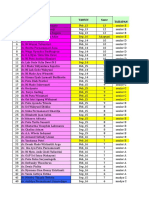
Table II. Results for primary and secondary outcomes
failure to demonstrate changes in secondary outcomes including
Conventional jet Breath-enhanced clinical asthma scores, ED length of stay, and admission rates
Outcomes n = 58* n = 57† P value is likely related to the study design involving a single 5-mg
D FEV1, % predicted, 13.8 (10.5-17.2) 9.1 (6.1-12.1) .04 albuterol treatment. This design gave us a clean comparison
mean (95% CI) of the effect of a single albuterol treatment on spirometry mea-
D FEV1 (ATS/ERS‡), % 14.5 (10.2-18.7) 8.5 (5.5-11.4) .03 surements, though may limit the applicability of these results
predicted, mean
(95% CI) to clinical practice where multiple treatments and larger doses
D PAS score, median −1 (−2 to −1) −2 (−2 to −1) .29 are typically utilized. Likewise, this study was not powered to
(IQR) address these secondary outcomes, and a larger sample size may
D PASS score, −1 (−1 to 0) −1 (−1 to 0) .97
median (IQR) be needed to evaluate these outcomes. Although we antici-
ED length of stay, 246.3 (220.4-272.3) 246.2 (220.4-272.0) .99 pate that the greater bronchodilation demonstrated by the con-
min, mean ventional jet nebulizer group in this study would translate to
(95% CI)
Admission rate, % 19.0 (10.6-31.5) 19.3 (10.8-32.0) .96 improved or noninferior clinical outcomes in a larger study
(95% CI) using multiple treatments, this cannot be determined from our
Side effects, % 8.6 (3.5-19.5) 8.8 (3.6-19.9) 1.00 data.
(95% CI)
Although we effectively blinded the study personnel re-
*n = 55 for primary outcome, n = 31 for D FEV1 (ATS/ERS). sponsible for subject enrollment and assessment, a potential
†n = 52 for primary outcome, n = 26 for D FEV1 (ATS/ERS).
‡Spirometry meeting ATS/ERS Guidelines.16 source of bias is the lack of blinding of parents, subjects, and
study personnel delivering nebulized albuterol. We do not
suspect that the majority of parents or subjects knew the dif-
association between predicted and actual group allocation ference between nebulizers and, if present, we would expect
(P = .54). this potential bias to favor the newer technology breath-
enhanced nebulizer.
Discussion In our study protocol, we administered albuterol without
the addition of ipratropium bromide, it is unclear how the
In this blinded-observer, randomized clinical trial, we dem- results of this study would be altered with the inclusion of
onstrated that in children aged between 6 and 18 years with ipratropium bromide. Likewise, the post-treatment assess-
moderate to severe acute asthma, albuterol delivered with a con- ment was performed 10 minutes following treatment comple-
ventional jet nebulizer resulted in greater improvement in FEV1 tion. This time was chosen to minimize study-related delays
than an equal treatment delivered by a breath-enhanced nebu- for children requiring further treatment, though may have given
lizer. There were no observed differences in secondary out- inadequate time for complete bronchodilation. It is uncer-
comes between groups including changes in clinical asthma tain how a longer observation period would impact our results.
severity scores. These results may indicate that in this patient Although we attempted to account for spirometry effort
population, a breath-enhanced nebulizer may not deliver through utilization of subjective assessment by study person-
albuterol as effectively as a conventional jet nebulizer. Strengths nel and the spirometer’s grading of curves, the encourage-
of this study include the larger sample size than prior studies, ment and determination of spirometry effort in children proved
the equal treatment of the 2 groups, and successful blinding difficult throughout the study. This was especially true of
of assessors. younger children. It is possible that variable spirometry effort
The findings in this study are contrary to what has been dem- may have impacted our results.
onstrated in breath-enhanced studies using lung models and The clinical asthma pathway at our institution does not
healthy adult controls.3-8 One potential explanation may be the include metered-dose inhaler (MDI) albuterol in the ED, and
mouthpiece design of the breath-enhanced nebulizer as it relates all albuterol treatments are delivered by nebulizer. As such, con-
to the breathing pattern of children with acute asthma. The ventional jet nebulizer was chosen as the control group for this
breath-enhanced mouthpiece separates the subject from the study. We appreciate that MDIs have been demonstrated as
aerosol holding chamber, leaving a small volume of exhaled noninferior to jet nebulizers,16,17,20,22-24 and that there are EDs
air that does not contain aerosol (dead-space). This dead- that use MDI albuterol regularly. It is unclear from these results
space volume is the first air inhaled by the subject with each how breath-enhanced nebulizers compare with MDIs and
breath. Although this dead-space volume is small in compari- further study would be needed to address this.
son with a healthy adult’s inspiratory volume, it may be more Finally, this was a single-center trial performed at an urban
important in children with acute asthma. Pediatric patients with tertiary care children’s hospital with a large proportion of His-
moderate to severe bronchoconstriction typically demon- panic subjects. The results of this study may not be general-
strate a rapid and shallow breathing pattern. It is possible that izable to other clinical settings or different patient populations.
children in this setting gain benefit from the cloud of aero- In conclusion, the results of this study indicate that breath-
solized albuterol that is continuously created by the conven- enhanced nebulizers may be less effective at delivering aerosol
tional jet nebulizer and that the dead-space of the breath- to pediatric patients with moderate to severe acute asthma com-
enhanced nebulizer is more impactful in this patient population. pared with conventional jet nebulizers. Although this study was
4 Gardiner and Wilkinson
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
■■ 2018 ORIGINAL ARTICLES
not designed to include a formal cost analysis, the less expen- 10. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values
sive conventional jet nebulizers provided greater improvement from a sample of the general U.S. population. Am J Respir Crit Care Med
1999;159:179-87.
in FEV1 with no difference in clinical outcomes. Given our find- 11. Sabato K, Ward P, Hawk W, Gildengorin V, Asselin JM. Randomized con-
ings and currently available data, we cannot recommend the trolled trial of a breath-actuated nebulizer in pediatric asthma patients
use of breath-enhanced nebulizers as a replacement for con- in the emergency department. Respir Care 2011;56:761-70.
ventional jet nebulizers. ■ 12. Qureshi F, Pestian J, Davis P, Zaritsky A. Effect of nebulized ipratropium
on the hospitalization rates of children with asthma. N Engl J Med
1998;339:1030-5.
Submitted for publication Jun 8, 2018; last revision received Aug 3, 2018;
13. Gorelick MH, Stevens MW, Schultz TR, Scribano PV. Performance of a
accepted Aug 31, 2018
novel clinical score, the Pediatric Asthma Severity Score (PASS), in the
Reprint requests: Mike A. Gardiner, MD, Department of Pediatrics, University evaluation of acute asthma. Acad Emerg Med 2004;11:10-8.
of California, San Diego, Rady Children’s Hospital—San Diego, La Jolla, CA.
14. Barr RG, Stemple KJ, Mesia-Vela S, Basner RC, Derk SJ, Henneberger PK,
E-mail: magardiner@ucsd.edu
et al. Reproducibility and validity of a handheld spirometer. Respir Care
2008;53:433-41.
Data Statement 15. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al.
Standardisation of spirometry. Eur Respir J 2005;26:319-38.
16. Colacone A, Afilalo M, Wolkove N, Kreisman H. A comparison of albuterol
Data will be made available on request. administered by metered dose inhaler (and holding chamber) or wet nebu-
lizer in acute asthma. Chest 1993;104:835-41.
17. Schuh S, Johnson DW, Stephens D, Callahan S, Winders P, Canny GJ. Com-
References parison of albuterol delivered by a metered dose inhaler with spacer versus
1. American Lung Association, Epidemiology and Statistics Unit. Trends in a nebulizer in children with mild acute asthma. J Pediatr 1999;135:22-
asthma morbidity and mortality [Internet]. http://www.lung.org/ 7.
finding-cures/our-research/trend-reports/asthma-trend-report.pdf. 18. Lin Y-Z, Huang F-Y. Comparison of breath-actuated and conventional
2012. Accessed May 15, 2018. constant-flow jet nebulizers in treating acute asthmatic children. Acta
2. National Asthma Education and Prevention Program. Expert Panel Report Paediatr Taiwan 2004;45:73-6.
3 (EPR-3): guidelines for the diagnosis and management of asthma- 19. Wilkinson M, Bulloch B, Garcia-Filion P, Keahey L. Efficacy of racemic
summary report 2007. J Allergy Clin Immunol 2007;120:S94-138. albuterol versus levalbuterol used as a continuous nebulization for the
3. Hess DR. Aerosol delivery devices in the treatment of asthma. Respir Care treatment of acute asthma exacerbations: a randomized, double-blind,
2008;53:699-723. discussion723–5. clinical trial. J Asthma 2011;48:188-93.
4. Rubin BK, Fink JB. The delivery of inhaled medication to the young child. 20. Idris AH, McDermott MF, Raucci JC, Morrabel A, McGorray S, Hendeles
Pediatr Clin North Am 2003;50:717-31. L. Emergency department treatment of severe asthma. Metered-dose inhaler
5. Ho SL, Kwong WT, O’Drowsky L, Coates AL. Evaluation of four breath- plus holding chamber is equivalent in effectiveness to nebulizer. Chest
enhanced nebulizers for home use. J Aerosol Med 2001;14:467-75. 1993;10:665-72. American College of Chest Physicians.
6. Newnham DM, Lipworth BJ. Nebuliser performance, pharmacokinet- 21. Yelland LN, Sullivan TR, Voysey M, Lee KJ, Cook JA, Forbes AB. Apply-
ics, airways and systemic effects of salbutamol given via a novel nebuliser ing the intention-to-treat principle in practice: guidance on handling
delivery system (“Ventstream”). Thorax 1994;49:762-70. randomisation errors. Clin Trials 2015;12:418-23.
7. Newman SP, Pitcairn GR, Hooper G, Knoch M. Efficient drug delivery 22. Cates CJ, Crilly JA, Rowe BH. Holding chambers (spacers) versus nebulisers
to the lungs from a continuously operated open-vent nebulizer and low for beta-agonist treatment of acute asthma. Cochrane Database Syst Rev
pressure compressor system. Eur Respir J 1997;7:1177-81. 2006;(9):CD000052.
8. Devadason SG, Everard ML, Linto JM, Le Souëf PN. Comparison of drug 23. Newman KB, Milne S, Hamilton C, Hall K. A comparison of albuterol
delivery from conventional versus “Venturi” nebulizers. Eur Respir J administered by metered-dose inhaler and spacer with albuterol by nebu-
1997;10:2479-83. lizer in adults presenting to an urban emergency department with acute
9. Wilkinson M, King B, Iyer S, Higginbotham E, Wallace A, Hovinga C, et al. asthma. Chest 2002;121:1036-41.
Comparison of a rapid albuterol pathway with a standard pathway for 24. Tien I, Dorfman D, Kastner B, Bauchner H. Metered-dose inhaler: the
the treatment of children with a moderate to severe asthma exacerba- emergency department orphan. Arch Pediatr Adolesc Med 2001;155:1335-
tion in the emergency department. J Asthma 2018;55:244-51. 9.
Randomized Clinical Trial Comparing Breath-Enhanced to Conventional Nebulizers in the Treatment of 5
Children with Acute Asthma
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
Appendix 1
Clinical asthma scores
PAS
categories Definition 0 1 2
RR Respiratory rate (30 s rate × 2)
6-12 y ≤26 27-30 ≥31
>12 y ≤23 24-27 ≥28
O2 Oxygen requirement (on RA × 2 min) >95% RA 90%-95% RA <90% RA
Appearance Auscultation Clear breath sounds to end Expiratory wheezes Inspiratory and expiratory wheeze
expiratory wheeze only or diminished breath sounds
Work of breathing Nasal flaring ≤1 accessory muscle 2 accessory muscles ≥3 accessory muscles
Suprasternal, intercostal, or subcostal
muscle use
Dyspnea Speaks full sentences Speaks partial sentences Speaks short phrases, single
words, grunting
PASS
clinical findings Definition 0 1 2
Wheezing High-pitched expiratory sound heard by auscultation None or mild Moderate Severe wheezing or absent wheezing
because of poor air exchange
Work of breathing Observed use of accessory muscles or retractions None or mild Moderate Severe
Prolongation of expiration Ratio of duration of expiration to inspiration Normal or mildly Moderately Severely prolonged
prolonged prolonged
O2, oxygen saturation; RA, room air; RR, respiratory rate.
Appendix 2
Spirometry grading criteria*
A A: At least 3 acceptable tests AND the difference between the best 2 FEV1 and FVC values is equal to or less than 100 mL (80 mL if FVC <1.0L)
B At least 3 acceptable tests AND the difference between the best 2 FEV1 and FVC values is equal to or less than 150 mL (100 mL if FVC <1.0L)
C At least 2 acceptable tests AND the difference between the best 2 FEV1 and FVC values is equal to or less than 200 mL (150 mL if FVC <1.0L)
D At least 2 acceptable trials but the results are not reproducible OR only 1 acceptable trial
F No acceptable test available
FVC, forced vital capacity.
*Reproduced from ndd EasyOne Plus Operator's Manual, ndd Medical Technologies, Inc, Andover, Massachusetts.
5.e1 Gardiner and Wilkinson
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
■■ 2018 ORIGINAL ARTICLES
Excluded (n = 324)
Not meeting inclusion criteria (n = 275)
Enrollment o 116 PAS score zero
Assessed for eligibility (n = 497) o 61 Immediate resuscitation required
o 41 Treatment prior to enrollment
o 35 Two study personnel unavailable
o 12 Chronic disease
o 7 Language barrier
o 3 Allergy to albuterol
Attempted initial spirometry (n = 173) Declined to participate (n = 26)
Excluded (n = 55) Other reasons (n = 23)
o 8 Alternative diagnosis likely
Not meeting inclusion criteria (n = 55)
o 6 Developmental delay
o 32 FEV1 > 70% predicted
o 6 Parent/guardian unavailable
o 23 Failed initial spirometry Randomized (n = 118)
o 3 Previously enrolled
Allocation
Conventional jet nebulizer (n = 60) Breath-enhanced nebulizer (n = 58)
Excluded (n = 2) Excluded (n = 1)
Not meeting inclusion criteria (n = 2) Not meeting inclusion criteria (n = 1)
o 1 FEV1 > 70% predicted o 1 FEV1 > 70% predicted
o 1 Previously enrolled
Analysis
Analyzed for secondary outcomes (n = 58) Analyzed for secondary outcomes (n = 57)
Excluded from primary analysis (n = 3) Excluded from primary analysis (n = 5)
o 3 Failed post spirometry o 5 Failed post spirometry
Analyzed for primary outcome (n = 55) Analyzed for primary outcome (n = 52)
Figure. CONSORT flow diagram.
Randomized Clinical Trial Comparing Breath-Enhanced to Conventional Nebulizers in the Treatment of 5.e2
Children with Acute Asthma
FLA 5.5.0 DTD ■ YMPD10270_proof ■ November 2, 2018
Das könnte Ihnen auch gefallen
- Sridhar 2016Dokument6 SeitenSridhar 2016Desmiyati AdoeNoch keine Bewertungen
- Neonatal Hyperbilirubinemia PolicyDokument8 SeitenNeonatal Hyperbilirubinemia PolicyDesmiyati AdoeNoch keine Bewertungen
- Lembar Observasi Pasien Infeksi TropisDokument3 SeitenLembar Observasi Pasien Infeksi TropisDesmiyati AdoeNoch keine Bewertungen
- Jaga April 2019 KoreksiDokument12 SeitenJaga April 2019 KoreksiDessyadoeNoch keine Bewertungen
- Hipoglicemia Neonatal InglésDokument6 SeitenHipoglicemia Neonatal InglésOsiithaa CañaszNoch keine Bewertungen
- Original Contributions: A Randomized Trial Comparing Metered Dose Inhalers and Breath Actuated NebulizersDokument8 SeitenOriginal Contributions: A Randomized Trial Comparing Metered Dose Inhalers and Breath Actuated NebulizersDesmiyati AdoeNoch keine Bewertungen
- Gardiner 2019Dokument7 SeitenGardiner 2019Desmiyati AdoeNoch keine Bewertungen
- Gautam 2011Dokument10 SeitenGautam 2011Desmiyati AdoeNoch keine Bewertungen
- Assessment of Clinical Outcome of Children With Sepsis Outside The Intensive Care UnitDokument9 SeitenAssessment of Clinical Outcome of Children With Sepsis Outside The Intensive Care UnitDesmiyati AdoeNoch keine Bewertungen
- HFO NeonatusDokument10 SeitenHFO NeonatusDesmiyati AdoeNoch keine Bewertungen
- Bottino 2018Dokument7 SeitenBottino 2018Desmiyati AdoeNoch keine Bewertungen
- Can Tey 2018Dokument6 SeitenCan Tey 2018Desmiyati AdoeNoch keine Bewertungen
- Gardiner 2019Dokument7 SeitenGardiner 2019Desmiyati AdoeNoch keine Bewertungen
- Feb-19 Feb-19 Feb-19 Feb-19 Feb-19 Feb-19 Feb-19 Feb-19Dokument5 SeitenFeb-19 Feb-19 Feb-19 Feb-19 Feb-19 Feb-19 Feb-19 Feb-19Desmiyati AdoeNoch keine Bewertungen
- Jurnal Peri PDFDokument19 SeitenJurnal Peri PDFTanty YuliantiNoch keine Bewertungen
- No Nama Tahun SMTR TahapanDokument15 SeitenNo Nama Tahun SMTR TahapanDesmiyati AdoeNoch keine Bewertungen
- MPI IndeksDokument5 SeitenMPI IndeksDesmiyati AdoeNoch keine Bewertungen
- Neonatal Hyperbilirubinemia PolicyDokument8 SeitenNeonatal Hyperbilirubinemia PolicyDesmiyati AdoeNoch keine Bewertungen
- Shankaran 2019Dokument11 SeitenShankaran 2019Desmiyati AdoeNoch keine Bewertungen
- Jadwal Rotasi Residen IKA FK UNUD/RSUP Sanglah Bulan Februari 2018Dokument13 SeitenJadwal Rotasi Residen IKA FK UNUD/RSUP Sanglah Bulan Februari 2018Desmiyati AdoeNoch keine Bewertungen
- Jurnal NeonatusDokument41 SeitenJurnal NeonatusDesmiyati AdoeNoch keine Bewertungen
- Malakian 2018Dokument14 SeitenMalakian 2018Desmiyati AdoeNoch keine Bewertungen
- Revised Guidelines On AES - JEDokument30 SeitenRevised Guidelines On AES - JEegalivanNoch keine Bewertungen
- Full TextDokument16 SeitenFull TextDesmiyati AdoeNoch keine Bewertungen
- JADWAL ROTASI RESIDEN IKA FK UNUD NOVEMBER 2018Dokument5 SeitenJADWAL ROTASI RESIDEN IKA FK UNUD NOVEMBER 2018Desmiyati AdoeNoch keine Bewertungen
- Glasgow Coma Scale For Infants Children PDFDokument1 SeiteGlasgow Coma Scale For Infants Children PDFDesmiyati AdoeNoch keine Bewertungen
- Cerebral EdemaDokument6 SeitenCerebral EdemaantonopoulosalNoch keine Bewertungen
- 5 6057344157398073400Dokument69 Seiten5 6057344157398073400Desmiyati AdoeNoch keine Bewertungen
- NO Program Program Book Scientific Program FileDokument2 SeitenNO Program Program Book Scientific Program FileDesmiyati AdoeNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- School Threat AssessmentDokument12 SeitenSchool Threat AssessmentChelsea ElizabethNoch keine Bewertungen
- Phenol Hazards and PrecautionsDokument3 SeitenPhenol Hazards and PrecautionsMarnel Roy MayorNoch keine Bewertungen
- Turn Around Time of Lab: Consultant Hospital ManagementDokument22 SeitenTurn Around Time of Lab: Consultant Hospital ManagementAshok KhandelwalNoch keine Bewertungen
- Nursing Audit ScheduleDokument2 SeitenNursing Audit ScheduleArvinjohn Gacutan0% (1)
- Dementia Rating ScaleDokument2 SeitenDementia Rating ScaleIqbal BaryarNoch keine Bewertungen
- Safety Signs and SymbolsDokument5 SeitenSafety Signs and Symbolsjon pantz100% (1)
- Functional Electrical StimulationDokument11 SeitenFunctional Electrical StimulationMohd Khairul Ikhwan AhmadNoch keine Bewertungen
- Mechanical Syllabus PDFDokument225 SeitenMechanical Syllabus PDFshashiNoch keine Bewertungen
- LESSON 1 and LESSON 2Dokument5 SeitenLESSON 1 and LESSON 21234567werNoch keine Bewertungen
- Immunization WHODokument17 SeitenImmunization WHOMuhammad Hardhantyo PuspowardoyoNoch keine Bewertungen
- Diabetes and Hearing Loss (Pamela Parker MD)Dokument2 SeitenDiabetes and Hearing Loss (Pamela Parker MD)Sartika Rizky HapsariNoch keine Bewertungen
- 2) Water Quality and Health in Egypt - Dr. AmalDokument50 Seiten2) Water Quality and Health in Egypt - Dr. AmalAlirio Alonso CNoch keine Bewertungen
- Sulphonamides: A Pharmaceutical ReviewDokument3 SeitenSulphonamides: A Pharmaceutical ReviewinventionjournalsNoch keine Bewertungen
- Nurse Licensure Examination Review Center for Allied Professions (RCAPDokument15 SeitenNurse Licensure Examination Review Center for Allied Professions (RCAPnikko0427Noch keine Bewertungen
- Declaration of Erin EllisDokument4 SeitenDeclaration of Erin EllisElizabeth Nolan BrownNoch keine Bewertungen
- LC (Lethal Concentration) : Uji Toksisitas KuantitatifDokument31 SeitenLC (Lethal Concentration) : Uji Toksisitas Kuantitatifbagi_fileNoch keine Bewertungen
- 03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumDokument16 Seiten03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumFloba Ika SianturiNoch keine Bewertungen
- Mumps Guide: Causes, Symptoms, Treatment & PreventionDokument14 SeitenMumps Guide: Causes, Symptoms, Treatment & PreventionChristian JonathanNoch keine Bewertungen
- HAV IgG/IgM Test InstructionsDokument2 SeitenHAV IgG/IgM Test InstructionsRuben DuranNoch keine Bewertungen
- PE 11 Cardio Endurance Workout ReflectionsDokument2 SeitenPE 11 Cardio Endurance Workout ReflectionsFranky MendozaNoch keine Bewertungen
- MHFL Functional FoodsDokument24 SeitenMHFL Functional FoodsZekel HealthcareNoch keine Bewertungen
- Audits, Gap Assessments, CAPA - 0Dokument230 SeitenAudits, Gap Assessments, CAPA - 0mgvtertv100% (3)
- Pediatric Nutrition and Nutritional Disorders: PediatricsDokument4 SeitenPediatric Nutrition and Nutritional Disorders: Pediatricsapi-3829364Noch keine Bewertungen
- ASHRAE Std 62.1 Ventilation StandardDokument38 SeitenASHRAE Std 62.1 Ventilation Standardcoolth2Noch keine Bewertungen
- Atls 1Dokument5 SeitenAtls 1Mega MalyndaNoch keine Bewertungen
- Basic Principles of Cross-Examination: Claire F. RushDokument14 SeitenBasic Principles of Cross-Examination: Claire F. RushSellappan RathinamNoch keine Bewertungen
- What Is Drug ReflectionDokument8 SeitenWhat Is Drug ReflectionCeilo TrondilloNoch keine Bewertungen
- MadRiverUnion01 13 21editionDokument8 SeitenMadRiverUnion01 13 21editionMad River UnionNoch keine Bewertungen
- Retyped: CHAP THORNDokument13 SeitenRetyped: CHAP THORNប៉ាក់ ចាន់រ៉ា - Pak ChanraNoch keine Bewertungen
- REAL in Nursing Journal (RNJ) : Penatalaksanaan Pasien Rheumatoid Arthritis Berbasis Evidence Based Nursing: Studi KasusDokument7 SeitenREAL in Nursing Journal (RNJ) : Penatalaksanaan Pasien Rheumatoid Arthritis Berbasis Evidence Based Nursing: Studi Kasustia suhadaNoch keine Bewertungen