Beruflich Dokumente
Kultur Dokumente
Whitaker Test PDF
Hochgeladen von
Kahn GenghisOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Whitaker Test PDF
Hochgeladen von
Kahn GenghisCopyright:
Verfügbare Formate
UROLOGY IN HISTORY
The Whitaker Test
Richard B. Johnston, Christopher Porter
Purpose: The Whitaker test was conceived and developed by Roger H. Whitaker (May 25,
Virginia Mason Medical Center,
1939) while he was a resident at Cambridge University in the late 1960s and early 1970s.
Seattle, WA, USA.
The test combines a urodynamic study with antegrade pyelography to measure the pressure
differential between the renal pelvis and the bladder. The test can differentiate between pa-
tients with residual or recurrent obstruction and those with dilatation secondary to permanent
changes in the musculature.
Materials and Methods: We present the history of the Whitaker test and its place in modern
practice.
Results: It is useful in evaluating patients with questionable ureteropelvic or ureterovesical
junction obstruction and primary defects in the ureteral musculature. It can also be used to
determine when percutaneous nephrostomy tubes can be safely discontinued in postoperative
patients.
Conclusion: The merit of the Whitaker test in comparison to other less invasive tests, specifi-
cally diuretic renography, is the subject of much debate. However, such debate erroneously
Corresponding Author: presupposes that the tests are directly comparable, which they are not. The correct use for the
Richard Johnston, MD
Whitaker test is to assesses potential upper tract obstruction in equivocal cases and should
Department of Urology, Virginia
Mason Medical Center, 1100 Ninth
only be utilized when equivocal results are obtained by other less invasive tests, obstruction
Ave C7-URO, Seattle, Washington is suspected in a poorly functioning kidney, a negative renogram with colic, intermittent
98101, USA.
obstruction, and percutaneous access already exists and the cause of dilatation needs inves-
Tel: +1 206 625 7459
Fax: +1 206 223 7650 tigating.
E-mail: richard.b.johnston@gmail.
com
Received May 2013 Keywords: diagnostic techniques; urological; standards; dilatation; pathologic; diagnosis;
Accepted December 2013
pressure; ureteral obstruction; physiopathology.
UROLOGY JOURNAL Vol. 11 | No. 03 | May - June 2014 | 1727
INTRODUCTION Sustained complete obstruction of the ureter leads to com-
D
ilatation and obstruction of the urinary tract are not plete loss of function and, as such, is easily diagnosed and
synonymous and it is not possible to estimate the must be treated by relieving the obstruction. In contrast,
pressure in the renal pelvis by cross-sectional imag- transient or partial obstruction offers a far more difficult
ing. Even when an obstructing lesion, such as a ureteric cal- clinical situation. While nephron loss will eventually occur,
culus, is identified, the presence or absence of dilatation does it is obviously preferable to identify and treat the obstruction
not predict the extent to which ureter is obstructed. The cor- prior to this irreversible confirmation. However, differenti-
rect diagnosis and treatment plan can often be determined by ating between transient or partial obstruction and dilatation
intravenous urography (IVU), ascending urogram, computed is not possible with only a single pressure measurement in
tomography (CT) scan with contrast and nuclear medicine iso- the renal pelvis or without knowledge regarding flow. There-
tope studies, such as diuretic renograms, when correlated with fore, Whitaker developed a test to measure the pressure dif-
the symptom of pain as a surrogate for obstruction. ferential between the renal pelvis and the bladder at a steady
However, important additional information is occasionally re- flow based on several physical principles.
quired in the event that these noninvasive tests yield equivocal First, Bernoulli's principle states that under conditions of
results. For instance, dilatation may result in a poorly emptying steady flow, the sum of all forms of mechanical energy in
but not actually obstructed system, leading to the stagnation of a fluid along a streamline is the same at all points in that
urine flow and an increased risk of developing a urinary infec- streamline. Therefore, the velocity of a fluid is proportional
tion. Also, when dilatation is not resolved post-surgical repair, to its dynamic pressure.
the question arises of whether the system is still obstructed. Ad-
ditionally, a subgroup of patients with normal renograms con-
sistently present with intermittent loin pain. In these situations,
a Whitaker test can help differentiate cases of renal pathology P = pressure; V= velocity; = density of water
from drug seeking or psychological pathology.
The increased use of cross-sectional imaging and early ‘B’ However, application of this principle to the ureter is com-
mode ultrasound in the 1950s and 1960s resulted in consider- plicated as the diameter of the pipeline is not constant. Due
able advances in the understanding of abnormal ureters, es- to the Venturi effect, this causes differential speeds and pres-
pecially in the pediatric population.(1) However, the measure- sures in the system (Figure 2). Moreover, the ureter is not
ment of renal pelvis pressure received little attention and there a rigid tube and, as such, both intra-abdominal and intra-
was no well-described way to distinguish between congenital vesical pressure affect the upper tract. In fact, adjustment
or postoperative causes of obstruction and unobstructed dil- of the subject’s position can result in a variation of 10-38
atation. This all changed in 1972 when Roger H. Whitaker mm Hg in the renal pelvis.(4) Finally, the kidney continues
(Figure 1), a young resident from Cambridge University who to produce urine, resulting in a contribution to the flow from
had spent a year in the research lab at Johns Hopkins (1968- the nephrons that cannot be calculated. Whitaker overcame
9), published the results of his studies and described his now these issues by standardizing his methodology (Figure 3).
eponymous test – the Whitaker Test. First, he pioneered the use of a single cannula, which he at-
While the concept of a dynamic perfusion-pressure flow tached to a perfusion pump that maintained a fast flow rate
(PPF) study was not new, with several animal model experi- of 10 mL per minute. The choice of 10 mL per minute was
ments and clinical trials already published,(1-3) all previous based in part on it being close to the physiologic maximum
studies had used, at the least, a two cannula technique and that a normal kidney can produce, meaning that the test is
did not describe an exact methodology based on sound physi- theoretically performed in a physiologic range. Also, by
ologic principles. standardizing the flow rate the results could be compared
among patients. Finally, the positioning of the patient was
MATERIALS AND METHODS crucial for obtaining reproducible and interpretable results.
The Whitaker Test Early experiments were carried out on pigs at the Brady
1728 | Urology In History
The Whitaker Test | Johnston et al
Figure 2. The pressure at "1" is higher than at "2" and the fluid
speed at "1" is lower than at "2" because the cross-sectional area at
"1" is greater than at "2".
into groups 1-4. Only 4% of the cases remained equivocal.
RESULTS
Reception and Usefulness of the Test
While Whitaker’s initial report generated significant inter-
Figure 1. Roger H. Whitaker, Cambridge University Staff photo. est, the exact place in the urologic armory for the Whitaker
test has been widely debated over the last 40 years. Without
question, prior to its inception there was a considerable gap
Urological Institute at John Hopkins. Whitaker subsequent- in our understanding of upper tract dilatation and its rela-
ly performed 170 studies on 112 patients with a history of tionship to transient or partial obstruction. Although it is not
equivocal obstruction based on previous conventional radio- a physiological test, it is based on physiological principles.
logic studies.(5) On the basis of these studies, he recognized The standard infusion rate of 10 mL/min is an arbitrary num-
five diagnostic patterns: ber; however, the value was determined by Whitaker after
1. Unobstructed system: at a flow rate of 10 mL/min, ab- extensive experimental and clinical observations.(6) Initially
solute pressure (pressure within the renal pelvis once the criticized as being too high, studies on healthy volunteers
pressure produced by perfusion of the nephrostomy tube or have shown that a kidney can produce 10 mL/min.(7) In fact,
needle is subtracted) of less than 25 cmH2O and relative more recently the rate has been criticized as being too low,
pressure (pressure drop across the site of suspected obstruc- with rates of up to 20 mL/min being necessary to unmask
tion obtained by subtracting bladder pressure from absolute transient, so-called high output, obstruction.(8) The clinical
pressure) of less than 15 cmH2O. importance of these findings is limited, as these high rates,
2. Obstruction between the renal pelvis and bladder: relative while possible, would seldom be seen. The exception would
pressure greater than 22 cmH2O and normal bladder pressure. be in the case of Dietl’s crisis, often seen in young men who
3. Hypertonic bladder: absolute pressure greater than 25 drink large volumes of beer, when forced diuresis causes ex-
cmH2O with a partially filled bladder and relative pressure treme pain due to an undiagnosed underlying ureteropelvic
less than 15 cmH2O. junction obstruction.
4. Hypertonic bladder and separate upper tract obstruction: The Whitaker test is less accurate in massively dilated
both the absolute and relative pressures are elevated. systems. Once the capacity of the renal pelvis exceeds 70
5. Equivocal or partially obstructed: relative pressure be- mL, its concordance with diuretic renography drops from
tween 15 and 22 cmH2O. nearly 90% to less than 50%.(9) In addition, some studies
Using his test, Whitaker was able to classify 96% of patients have found an inconsistent relationship between obstruc-
UROLOGY JOURNAL Vol. 11 | No. 03 | May - June 2014 | 1729
This type of pressure flow perfusion study must be kept in
perspective. It is not a panacea for all obstructions and
should not be used as a short cut to a quick diagnosis. That
we have done only 170 such studies in 8 years for the many
thousands of patients who have passed through our unit sug-
gests that we have been selective and, indeed, many of our
cases have been referred from other hospitals just for the
study. However, the individual patient with such a difficult
diagnostic problem should not be denied the advantage of a
study since it may well be the only present means of obtain-
ing the correct decision in terms of management’
We are indebted to Whitaker for his contribution to urology
that has led to a greater understanding of dilated upper tract
pathology. His test has helped many patients receive appro-
Figure 3. Whitaker test setup. Absolute pressure differences across priate therapy that otherwise would have managed based on
the ureter are obtained by subtracting bladder pressure from renal equivocal results.
pelvis pressure, which also cancels the effect of intra-abdominal
pressure.
REFERENCES
tion of the ureter and increased pressure in the renal pelvis.
1. Backlund L, Reuterskiold AG. The abnormal ureter in children.
While the relationship should be consistent in an inelastic Scand J Urol Nephrol. 1969;3:219-28.
system, elastic recoil, which contributes to the pressure, can 2. Johnston JH. The pathogenesis of hydronephrosis in children. Br J
vary among patients with the same degree of obstruction. Urol. 1969;41:724-34.
Some kidneys with almost completely obstructed ureters 3. Kill F. The function of the ureter and renal pelvis. Oslo University
(10) Press; 1957. p. 185.
can maintain normal pressures.
4. Ellis JH, Campo RP, Marx MV, et al. Positional variation in the Whi-
However, proponents of the test point out that low-pressure
taker test. Radiology. 1995;197:253-5.
obstruction does not cause nephron damage. In fact, it is
5. Whitaker RH. Methods of assessing obstruction in dilated ureters.
believed that a pressure above 22 cm H2O is required to Br J Urol. 1973;45:15-22.
cause damage,(11) and, as such, any clinically relevant ob- 6. Whitaker RH. The Whitaker test. Urol Clin North Am. 1979;6:529-39.
struction, i.e. requiring treatment to prevent renal damage,
7. O’Reilly PH. Diuresis renography. Recent advances and recom-
can be identified by the Whitaker test. The Whitaker test mended protocols. Br J Urol. 1992;69:113-20.
is a dynamic test and interpretation of the numbers alone 8. Lupton EW, Holden D, George NJ, Barnard RJ, Rickards D. Pressure
overlooks the purpose of the investigation in the first place, changes in the dilated upper urinary tract on perfusion at varying
flow rates. Br J Urol. 1985;57:622-4.
which is to make a diagnostic decision in the face of other
9. Djurhuus JC, Sørensen SS, Jørgensen TM, Taagehøj-Jensen F. Predic-
equivocal tests. tive value of pressure flow studies for the functional outcome of
reconstructive surgery for hydronephrosis. Br J Urol. 1985;57:6-9.
CONCLUSION 10. Koff SA. The diagnosis of obstruction in experimental hydrouretero-
Obstruction can only be defined in dynamic terms and the nephrosis. Invest Urol. 1981;19:85-8
Whitaker test gives the most dynamic results. Therefore, it 11. George NR, O’Reilly PH, Barnard RJ, Blacklock NJ. High pressure
is not surprising that after 40 years it is still the go-to test chronic retention. BMJ 1983; 286:1780-3
in situations where other imaging and investigations have
proved to be equivocal. The Whitaker test should not be the
first choice of test, nor was ever designed to be used as such.
(9)
To quote Whitaker:
1730 | Urology In History
Das könnte Ihnen auch gefallen
- Patty Brennan Homeopathic GuideDokument54 SeitenPatty Brennan Homeopathic Guidepawajee0% (1)
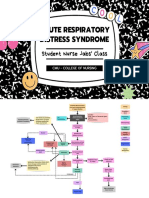
- ARDS Concept Map - BunayogDokument2 SeitenARDS Concept Map - BunayogJacela Annsyle BunayogNoch keine Bewertungen
- A Prospective Study Analyzing The Association Between High-Grade Ureteral Access Sheath Injuries and The Formation of Ureteral StricturesDokument4 SeitenA Prospective Study Analyzing The Association Between High-Grade Ureteral Access Sheath Injuries and The Formation of Ureteral StricturesVinícius Dall'AquaNoch keine Bewertungen
- Report PDFDokument2 SeitenReport PDFAnonymous 6x3CyeNoch keine Bewertungen
- Tanasiychuk2019 Article TheIdealPositionOfThePeritoneaDokument6 SeitenTanasiychuk2019 Article TheIdealPositionOfThePeritoneaGabriela CruzNoch keine Bewertungen
- Role of Transabdominal Ultrasound in Evaluating Patients With Acute Urinary Retention (Aur) Due To Benign Prostatic Hyperplasia (BPH)Dokument3 SeitenRole of Transabdominal Ultrasound in Evaluating Patients With Acute Urinary Retention (Aur) Due To Benign Prostatic Hyperplasia (BPH)Yuni AngrianiNoch keine Bewertungen
- Clinical Study of Bowel ObstructionDokument6 SeitenClinical Study of Bowel ObstructionhorzhanNoch keine Bewertungen
- Measure BUN Creat Urine LeakageDokument4 SeitenMeasure BUN Creat Urine Leakagerendi wibowoNoch keine Bewertungen
- Liang 2008Dokument6 SeitenLiang 2008Novi RobiyantiNoch keine Bewertungen
- Correlation Between Penile Cuff Test and Pressure-Flow Study in Patients Candidates For Trans-Urethral Resection of ProstateDokument6 SeitenCorrelation Between Penile Cuff Test and Pressure-Flow Study in Patients Candidates For Trans-Urethral Resection of ProstatemelianyNoch keine Bewertungen
- Positioning The Instillation of Contrast Cystography: Does It Provide Any Clinical Benefit?Dokument17 SeitenPositioning The Instillation of Contrast Cystography: Does It Provide Any Clinical Benefit?Indah GitaswariNoch keine Bewertungen
- DereviDokument6 SeitenDereviDerevie Hendryan MoulinaNoch keine Bewertungen
- Bani 2006Dokument3 SeitenBani 2006Nael NajeebNoch keine Bewertungen
- Cavallini 2010Dokument8 SeitenCavallini 2010Israel BlancoNoch keine Bewertungen
- Visual Internal Urethrotomy For Adult Male UrethraDokument6 SeitenVisual Internal Urethrotomy For Adult Male UrethraGd SuarantaNoch keine Bewertungen
- RectopexyDokument7 SeitenRectopexyInzamam Ul HaqNoch keine Bewertungen
- ENDUROLOGYDokument3 SeitenENDUROLOGYAlexandra EosNoch keine Bewertungen
- Bladder Wall Thickness On Ultrasonographic CystourethrographyDokument6 SeitenBladder Wall Thickness On Ultrasonographic CystourethrographyNi Wayan Ana PsNoch keine Bewertungen
- Jurnal Retensi UrinDokument4 SeitenJurnal Retensi UrinMuzammil Bin YusufNoch keine Bewertungen
- A Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionDokument6 SeitenA Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionSantosh BabuNoch keine Bewertungen
- Pemeriksaan IVPDokument41 SeitenPemeriksaan IVPChandra Noor SatriyoNoch keine Bewertungen
- Editorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystDokument4 SeitenEditorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystLogical MonsterNoch keine Bewertungen
- PIIS2405456922002619Dokument7 SeitenPIIS2405456922002619Oriol Colet GuitertNoch keine Bewertungen
- Pi Is 0022534715050119Dokument2 SeitenPi Is 0022534715050119xtm69846Noch keine Bewertungen
- CApsule EndodvopyDokument26 SeitenCApsule EndodvopybhaskarlxmNoch keine Bewertungen
- From Functional Imaging in Nephro-Urology (Alain Prigent Etc.) (Z-Library)Dokument10 SeitenFrom Functional Imaging in Nephro-Urology (Alain Prigent Etc.) (Z-Library)Francisco BotelhoNoch keine Bewertungen
- Vur KoreanDokument7 SeitenVur KoreanIoannis ValioulisNoch keine Bewertungen
- 978 1 4613 1851 4 1Dokument276 Seiten978 1 4613 1851 4 1fwefNoch keine Bewertungen
- Role of Open Surgical Drainage or Aspiration in Management of Amoebic Liver AbscessDokument9 SeitenRole of Open Surgical Drainage or Aspiration in Management of Amoebic Liver AbscessIJAR JOURNALNoch keine Bewertungen
- 1 s2.0 S2667008923000253 MainDokument4 Seiten1 s2.0 S2667008923000253 Mainal malikNoch keine Bewertungen
- Risk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryDokument31 SeitenRisk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryWielda VeramitaNoch keine Bewertungen
- 0616 SCuDokument18 Seiten0616 SCuYolanda Dwi OktaviyaniNoch keine Bewertungen
- 002 Revisi HUGI 2020 PPT Rendra SaputraDokument30 Seiten002 Revisi HUGI 2020 PPT Rendra SaputraMunifah YusriyahNoch keine Bewertungen
- Acute Intestinal ObstructionDokument9 SeitenAcute Intestinal ObstructionRoxana ElenaNoch keine Bewertungen
- NeurogenicbladdermanagementwithcompleteurethraldistructionDokument11 SeitenNeurogenicbladdermanagementwithcompleteurethraldistructionPutri Rizky AmaliaNoch keine Bewertungen
- Catheter-Induced Urethritis: A Comparison Between Latex and Silicone Catheters in A Prospective Clinical TrialDokument4 SeitenCatheter-Induced Urethritis: A Comparison Between Latex and Silicone Catheters in A Prospective Clinical TrialpicassowaffleNoch keine Bewertungen
- Review Article: Matthias OelkeDokument6 SeitenReview Article: Matthias OelkeTatiana TanyaNoch keine Bewertungen
- Incontinence Elderly: Algorithmic Method For Assessing Urinary in WomenDokument3 SeitenIncontinence Elderly: Algorithmic Method For Assessing Urinary in WomenUlfia KhoirinnissaNoch keine Bewertungen
- Orthotopicurinarydiversionintheelderly PDFDokument7 SeitenOrthotopicurinarydiversionintheelderly PDFAlessio Di SetteNoch keine Bewertungen
- ACR Appropriateness Criteria Acute Onset FlankDokument7 SeitenACR Appropriateness Criteria Acute Onset FlankcubirojasNoch keine Bewertungen
- Batchala 2021Dokument6 SeitenBatchala 2021qrscentralNoch keine Bewertungen
- Magnetic Marker Monitoring Allows To Characterize Effects of Exogenous Factors On Esophageal Transit of Solid Drug FormsDokument3 SeitenMagnetic Marker Monitoring Allows To Characterize Effects of Exogenous Factors On Esophageal Transit of Solid Drug FormsSaravanan MathiNoch keine Bewertungen
- 1 s2.0 S1477513122005782 MainDokument8 Seiten1 s2.0 S1477513122005782 MainReza EffendiNoch keine Bewertungen
- Nuclear Medicine GuideDokument3 SeitenNuclear Medicine GuidejeffsunilNoch keine Bewertungen
- Rectal Prolapse: Rare Presentation and Complication: Case ReportDokument3 SeitenRectal Prolapse: Rare Presentation and Complication: Case Reportadi tiarmanNoch keine Bewertungen
- Homepage: - : IntroductionDokument7 SeitenHomepage: - : IntroductionIJAR JOURNALNoch keine Bewertungen
- Urodynamics: Role in Incontinence and Prolapse: A Urology PerspectiveDokument8 SeitenUrodynamics: Role in Incontinence and Prolapse: A Urology PerspectiveMaría PradoNoch keine Bewertungen
- Postoperative Catheter Management After Pelvic Reconstructive Surgery: A Survey of Practice StrategiesDokument5 SeitenPostoperative Catheter Management After Pelvic Reconstructive Surgery: A Survey of Practice StrategiesWardah Fauziah El SofwanNoch keine Bewertungen
- Pressure Flow Urodynamic Studies: The Gold Standard For Diagnosing Bladder Outlet ObstructionDokument8 SeitenPressure Flow Urodynamic Studies: The Gold Standard For Diagnosing Bladder Outlet ObstructionmarcelloNoch keine Bewertungen
- Laparoscopic Repair of Vesicovaginal FistulaDokument4 SeitenLaparoscopic Repair of Vesicovaginal FistulaGloria AteNoch keine Bewertungen
- Effects of Transurethral Resection of Prostate On Flow Rate and Voided Volume On Patients With Benign Prostatic HyperplasiaDokument4 SeitenEffects of Transurethral Resection of Prostate On Flow Rate and Voided Volume On Patients With Benign Prostatic HyperplasiaKamran AfzalNoch keine Bewertungen
- Cats With Circumcaval UretersDokument8 SeitenCats With Circumcaval UretersDaniel CapuchoNoch keine Bewertungen
- Vaginal Electrostimulation Therapy in The Symptoms of Women Withoveractive BladderDokument4 SeitenVaginal Electrostimulation Therapy in The Symptoms of Women Withoveractive BladderIJAR JOURNALNoch keine Bewertungen
- Rajiv Gandhi University of Health Sciences Karnataka, BangaloreDokument15 SeitenRajiv Gandhi University of Health Sciences Karnataka, BangaloreJayanth GNoch keine Bewertungen
- Types Sites and Causes of Mechanical Intestinal ObDokument5 SeitenTypes Sites and Causes of Mechanical Intestinal ObPutra FebdianNoch keine Bewertungen
- Posttraumatic Hematuria With Pseudorenal Failure: A Diagnostic Lead For Diagnosing Intraperitoneal Bladder Rupture.Dokument4 SeitenPosttraumatic Hematuria With Pseudorenal Failure: A Diagnostic Lead For Diagnosing Intraperitoneal Bladder Rupture.Ketan VagholkarNoch keine Bewertungen
- Schwarz-Prabhakar2020 Article WhatToDoWhenPerioperativePointDokument8 SeitenSchwarz-Prabhakar2020 Article WhatToDoWhenPerioperativePointkamounthNoch keine Bewertungen
- Clinical Study and Management of Gastric Perforation: Original ResearchDokument4 SeitenClinical Study and Management of Gastric Perforation: Original Researchpeekaboo oooNoch keine Bewertungen
- Clinical Study and Management of Gastric Perforation: Original ResearchDokument4 SeitenClinical Study and Management of Gastric Perforation: Original ResearchEvi NainggolanNoch keine Bewertungen
- Bmri2016 4975851Dokument5 SeitenBmri2016 4975851Mallesh ArjaNoch keine Bewertungen
- Urology Case Reports: S. Palthe, G.A. Dijkstra, M.G. SteffensDokument3 SeitenUrology Case Reports: S. Palthe, G.A. Dijkstra, M.G. SteffensFloro Dave ArnucoNoch keine Bewertungen
- Do We Need Anorectal Physiology Work Up in The Daily Colorectal Praxis?Dokument6 SeitenDo We Need Anorectal Physiology Work Up in The Daily Colorectal Praxis?soudrackNoch keine Bewertungen
- Interpretation of Urodynamic Studies: A Case Study-Based GuideVon EverandInterpretation of Urodynamic Studies: A Case Study-Based GuideNoch keine Bewertungen
- 25490874Dokument563 Seiten25490874Titoun LettounNoch keine Bewertungen
- Multi Organ Dysfunction SyndromeDokument40 SeitenMulti Organ Dysfunction SyndromeDr. Jayesh PatidarNoch keine Bewertungen
- OncologyDokument3 SeitenOncologyMichtropolisNoch keine Bewertungen
- Uterine HyperstimulationDokument2 SeitenUterine HyperstimulationYwagar YwagarNoch keine Bewertungen
- Nguyen 2021Dokument8 SeitenNguyen 2021Yaseen MohamnadNoch keine Bewertungen
- m3 Act3 Emotional DisabilitiesDokument7 Seitenm3 Act3 Emotional Disabilitiesapi-516574894Noch keine Bewertungen
- Pathophysiology of RHDDokument4 SeitenPathophysiology of RHDshmily_0810Noch keine Bewertungen
- NCP 1activity Intolerance N C P BY BHERU LALDokument1 SeiteNCP 1activity Intolerance N C P BY BHERU LALBheru LalNoch keine Bewertungen
- Assessment Diagnosis Rationale Plan Interventions Rationale EvaluationDokument14 SeitenAssessment Diagnosis Rationale Plan Interventions Rationale EvaluationDuran JustineNoch keine Bewertungen
- Blood PressureDokument25 SeitenBlood PressureSilvia FrtNoch keine Bewertungen
- ParasomniaDokument27 SeitenParasomniaVoltic AceroNoch keine Bewertungen
- Caring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyDokument34 SeitenCaring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyRubinaNoch keine Bewertungen
- Egypt Biosimilar Guidline Biologicals RegistrationDokument54 SeitenEgypt Biosimilar Guidline Biologicals Registrationshivani hiremathNoch keine Bewertungen
- Urdaneta City University Graduate School UrdanetaDokument13 SeitenUrdaneta City University Graduate School UrdanetaMa Theresa PunoNoch keine Bewertungen
- Cholelithiasis Case 1Dokument21 SeitenCholelithiasis Case 1Arvin F. LansangNoch keine Bewertungen
- Epidemiological TriadDokument33 SeitenEpidemiological TriadRAPURU BHARGAVINoch keine Bewertungen
- BronchiectasisDokument30 SeitenBronchiectasisMark Gizle PapagayoNoch keine Bewertungen
- Case Presentation On Parkinson'S Disease: Presented By: T.Avinash Vith Pharm D Y13PHD0721Dokument21 SeitenCase Presentation On Parkinson'S Disease: Presented By: T.Avinash Vith Pharm D Y13PHD0721AVINASH TALAPALA100% (1)
- Key To Eye Diagnosis by Tashfeen NasiraDokument8 SeitenKey To Eye Diagnosis by Tashfeen Nasiralakshay sharmaNoch keine Bewertungen
- The Ultimate Guide To Strength TrainingDokument3 SeitenThe Ultimate Guide To Strength Training23gomez0% (1)
- Dr. Gyan P. SinghDokument4 SeitenDr. Gyan P. SinghMohammed AL-TuhamiNoch keine Bewertungen
- Seminar On Shock: IndexDokument37 SeitenSeminar On Shock: IndexGayathri R100% (1)
- Iridology and HypoglycemiaDokument15 SeitenIridology and Hypoglycemiasohail_mashwnaiNoch keine Bewertungen
- Thrombocytopenia Brief DiscussionDokument11 SeitenThrombocytopenia Brief Discussionriel100% (3)
- NCPDokument2 SeitenNCPNiño LuceroNoch keine Bewertungen
- Final Souvenir GipsDokument143 SeitenFinal Souvenir GipsSagar SagarNoch keine Bewertungen
- Charting SystemsDokument4 SeitenCharting SystemsLydia D. GalinganNoch keine Bewertungen