Beruflich Dokumente
Kultur Dokumente
JAMA Oncology, 2019-Prophylactic Cranial Irradiation Vs Observation in Patients With Locally Advanced Non
Hochgeladen von
Palak GuptaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
JAMA Oncology, 2019-Prophylactic Cranial Irradiation Vs Observation in Patients With Locally Advanced Non
Hochgeladen von
Palak GuptaCopyright:
Verfügbare Formate
Research
JAMA Oncology | Original Investigation
Prophylactic Cranial Irradiation vs Observation in Patients
With Locally Advanced Non–Small Cell Lung Cancer
A Long-term Update of the NRG Oncology/RTOG 0214 Phase 3
Randomized Clinical Trial
Alexander Sun, MD; Chen Hu, PhD; Stuart J. Wong, MD; Elizabeth Gore, MD; Gregory Videtic, MD;
Swati Dutta, MD; Mohan Suntharalingam, MD; Yuhchyau Chen, MD, PhD; Laurie E. Gaspar, MD; Hak Choy, MD
Supplemental content
IMPORTANCE Brain metastasis (BM) rates are high in locally advanced non–small cell lung
cancer (LA-NSCLC), approaching rates seen in small cell lung cancer, where prophylactic
cranial irradiation (PCI) is standard of care. Although PCI decreases the incidence of BM in
LA-NSCLC, a survival advantage has not yet been shown.
OBJECTIVE To determine if PCI improves survival in LA-NSCLC.
DESIGN, SETTING, AND PARTICIPANTS Radiation Therapy Oncology Group (RTOG) 0214 was a
randomized phase 3 clinical trial in stage III NSCLC stratified by stage (IIIA vs IIIB), histologic
characteristics (nonsquamous vs squamous) and therapy (no surgery vs surgery). The study
took place at 291 institutions in the United States, Canada, and internationally. Of 356
patients with stage III NSCLC entered onto this study, 16 were ineligible; therefore, 340
patients were randomized.
INTERVENTION FOR CLINICAL TRIALS Observation vs PCI.
MAIN OUTCOMES AND MEASURES The primary outcome was overall survival (OS). The
secondary end points were disease-free survival (DFS) and incidence of BM.
RESULTS Of the 340 total participants, mean (SD) age was 61 years; 213 of the participants
were men and 127 were women. The median follow-up time was 2.1 years for all patients, and
9.2 years for living patients. The OS for PCI was not significantly better than observation
(hazard ratio [HR], 0.82; 95% CI, 0.63-1.06; P = .12; 5- and 10-year rates, 24.7% and 17.6% vs
26.0% and 13.3%, respectively), while the DFS (HR, 0.76; 95% CI, 0.59-0.97; P = .03; 5- and Author Affiliations: Princess
Margaret Cancer Centre, Toronto,
10-year rates, 19.0% and 12.6% vs 16.1% and 7.5% for PCI vs observation) and BM (HR, 0.43;
Ontario, Canada (Sun); NRG
95% CI, 0.24-0.77; P = .003; 5- and 10-year rates, 16.7% vs 28.3% for PCI vs observation) Oncology Statistics and Data
were significantly different. Patients in the PCI arm were 57% less likely to develop BM than Management Center, Philadelphia,
those in the observation arm. Younger patients (<60 years) and patients with nonsquamous Pennsylvania (Hu); Johns Hopkins
University School of Medicine,
disease developed more BM. On multivariable analysis, PCI was associated with decreased Baltimore, Maryland (Hu); Medical
BM and improved DFS, but not improved OS. Multivariable analysis within the nonsurgical College of Wisconsin, Milwaukee
arm suggests that PCI effectively prolongs OS, DFS, and BM. (Wong, Gore); Cleveland Clinic
Foundation, Cleveland, Ohio
(Videtic); Michigan Cancer Research
CONCLUSIONS AND RELEVANCE In patients with stage III LA-NSCLC without progression of Consortium CCOP, Ann Arbor (Dutta);
disease after therapy, PCI decreased the 5- and 10-year rate of BM and improved 5- and University of Maryland Medical
10-year DFS, but did not improve OS. Although this study did not meet its primary end point, System, Baltimore (Suntharalingam);
University of Rochester, Rochester,
the long-term results reveal many important findings that will benefit future trials. Identifying New York (Chen); University of
the appropriate patient population and a safe intervention is critical. Colorado, Denver (Gaspar);
University of Texas Southwestern
Medical Center, Dallas (Choy).
TRIAL REGISTRATION ClinicalTrials.gov identifier: NCT00048997
Corresponding Author: Alexander
Sun, MD, Department of Radiation
Oncology, Princess Margaret Cancer
Centre–University Health Network,
University of Toronto, 610 University
JAMA Oncol. doi:10.1001/jamaoncol.2018.7220 Ave, Toronto, Ontario, Canada M5G
Published online March 14, 2019. 2M9 (alex.sun@rmp.uhn.on.ca).
(Reprinted) E1
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Research Original Investigation Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer
Figure 1. Participant Enrollment Flow Diagram
Key Points
356 Randomized Question Does prophylactic cranial irradiation (PCI) improve
survival in patients with locally advanced non–small cell lung
cancer (LA-NSCLC) compared with observation alone?
176 Allocated to intervention 180 Allocated to observation
158 Received allocated Findings In this prospective randomized phase 3 clinical trial
intervention including 340 evaluable patients with LA-NSCLC, PCI decreased
the 5- and 10-year rate of brain metastases and improved 5- and
10-year disease-free survival, but did not improve overall survival
8 Lost to follow-up 4 Lost to follow-up compared with observation alone.
8 Patients withdrew consent to 4 Patients withdrew consent
follow-up to follow-up Meaning Although this study did not meet its primary end point
of overall survival, the long-term results reveal many important PCI
163 Analyzed 177 Analyzed
findings, which will benefit future trials.
13 Excluded from analysis 3 Excluded from analysis
6 Withdrew consent 2 Registered >16 weeks patient recruitment and all patients signed approved in-
5 Registered >16 weeks from completion of
from completion of definitive therapy formed consents prior to trial enrollment. The trial protocol
definitive therapy 1 Withdrew consent is available in Supplement 1.
1 Bone metastasis at time
of registration
1 Patient had colon cancer, Treatment and Follow-up
not NSCLC
Patients were stratified by stage (IIIA or B), histologic charac-
teristics (nonsquamous or squamous), and therapy (surgery
NSCLC indicates non–small cell lung cancer.
or no surgery) and then randomized to PCI or observation. Pa-
tients randomized to PCI were treated with 2 Gy/fraction, five
C
ombined-modality therapy, including chemotherapy, days per week, to 30 Gy. Acute PCI toxic events were evalu-
irradiation, and/or surgery, has resulted in improved sur- ated using the Common Terminology Criteria (CTC) version 2.0
vival of locally advanced non–small cell lung cancer (LA- grading criteria. Late PCI toxic events were evaluated using the
NSCLC). This lengthened survival is associated with in- RTOG/European Organisation for Research and Treatment of
creased incidence of brain metastases (BM),1-12 which can have Cancer (EORTC) Late Toxicity Criteria. Patients were fol-
a devastating impact on survival and quality of life (QOL). Rates lowed up 6 months from start of PCI, every 6 months for 2 years
of BM reported in NSCLC studies are as high as 55%,13-20 ap- and then yearly. Brain imaging with MRI or CT was per-
proaching rates seen in small cell lung cancer (SCLC), where formed at 6 and 12 months and then annually thereafter.
prophylactic cranial irradiation (PCI) is standard of care. Al-
though PCI decreases the incidence of BM in LA-NSCLC,21-23 Study Design and End Points
a survival advantage has not yet been shown. The primary end point of this study was OS, and secondary end
The NRG Oncology/Radiation Therapy Oncology Group points included DFS and BM. Overall survival failure events
(RTOG) led a study of PCI in LA-NSCLC after definitive pri- were defined as death due to any cause. Disease-free survival
mary therapy. The primary end point of the study was overall failure events were defined as the earliest event of death due
survival (OS), with secondary end points including disease- to any cause, local progression, regional metastasis, distant me-
free survival (DFS) and development of BM. This is an up- tastasis, or second primary. Brain metastases failure events
dated long-term analysis of the previously reported prelimi- were defined as any evidence of BM. Time to event was mea-
nary results.24 sured from date of randomization to date of failure or date of
most recent follow-up if no failure occurred.
Statistical Methods
Methods
The rates of OS and DFS were estimated using Kaplan-Meier
Patient Population method,25 and BMs were estimated using cumulative inci-
Patients with stage IIIA/B NSCLC without disease progres- dence function.26 The comparisons between PCI and obser-
sion after completing definitive locoregional therapy with ir- vation were based on log-rank tests27,28 stratified by Ameri-
radiation and/or surgery with or without chemotherapy were can Joint Committee on Cancer (AJCC) stage (IIIA vs IIIB); prior
randomized to PCI or observation (Figure 1). Patients were re- surgery (no vs yes); histologic characteristics (nonsquamous
staged and enrolled within 16 weeks of completing definitive vs squamous) and Zubrod performance status (0 vs >0). Cox
therapy. Patients were restaged with a computed tomogra- proportional hazards models29 were used to evaluate the im-
phy (CT) scan of the chest/abdomen and magnetic resonance pact of treatment on OS and DFS after adjusting for all these
imaging (MRI) of the brain within six weeks of study entry. factors and age (<60 vs ≥60 years). Cause-specific hazard ap-
Brain CT with contrast was allowed if MRI was contraindi- proach was used to analyze BM in presence of death without
cated. Patients could have no evidence of progressive intra- BM as a competing event. 30 Subgroup analysis was per-
thoracic disease, BM, or extracranial metastases. All institu- formed based on prespecified stratification factors at random-
tions obtained institutional review board approval prior to ization when the heterogeneity of treatment effects was sup-
E2 JAMA Oncology Published online March 14, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer Original Investigation Research
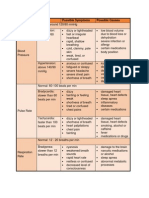
Table 1. Outcome Estimates for Entire Study
PCI (n = 163) Observation (n = 177)
Event Estimate % (95% Event Estimate % (95%
Outcome by Time No. at Risk CI) No. at Risk CI) PCI vs Observation, HR (95% CI)a P Valueb
Overall survival 0.82 (0.63-1.06) .12
2y 90 56.3 (48.3-63.6) 91 53.0 (45.3-60.1)
5y 39 24.7 (18.3-31.6) 42 26.0 (19.6-32.8)
10 y 15 17.6 (12.1-23.9) 11 13.3 (8.4-19.4)
MST (95% CI) 2.4 y (2.0-2.9) 2.1 y (1.7-2.7)
No. of events 131 146
Disease-free survival 0.76 (0.59-0.97) .03
2y 58 36.1 (28.7-43.5) 55 31.5 (24.7-38.4)
5y 30 19.0 (13.3-25.4) 26 16.1 (11.0-22.0)
10 y 10 12.6 (8.0-18.3) 7 7.5 (4.0-12.5)
MST (95% CI) 1.3 y (1.0-1.6) 1.0 (0.9-1.1)
No. of events 141 159
Brain metastasis 0.43 (0.24-0.77) .003
2y 86 10.9 (6.7-17.6) 81 24.3 (18.1-32.0)
5y 39 16.7 (10.6-25.9) 37 28.3 (21.2-37.2)
10 y 15 16.7 (10.6-25.9) 11 28.3 (21.2-37.2)
MST (95% CI) Not reached Not reached
No. of events 20 40
Abbreviations: AJCC, American Joint Committee on Cancer; HR, hazard ratio; squamous) and Zubrod performance status (0 vs >0).
MST, median survival time; PCI, prophylactic cranial irradiation. b
From stratified log-rank test, stratified by AJCC stage (IIIA vs IIIB); prior surgery
a
From stratified Cox proportional hazard model, stratified by AJCC stage (IIIA vs (no vs yes); histologic characteristics (nonsquamous vs squamous) and Zubrod
IIIB); prior surgery (no vs yes); histologic characteristics (nonsquamous vs performance status (0 vs >0).
ported by tests for interaction (eg, prior surgery) or of interest to detect the targeted difference in OS. Patients died primar-
(eg, histology).31 All statistical comparisons were considered ily due to their lung cancer. The survival estimates and HR in-
statistically significant at a 2-sided P < .05, and no multiple dicated that there appeared to be no improvement in survival
comparison adjustments were made. All statistical analyses with the use of PCI. Five-year and 10-year OS rates were 24.7%
were run with SAS, 9.4 (SAS Institute Inc) software. and 17.6% for PCI and 26.0% and 13.3% for observation, re-
spectively (Table 1 and Figure 2). Estimated median survival
(MS) duration was 2.4 years (95% CI, 2.0-2.9) and 2.1 years (95%
CI, 1.7-2.7) for PCI and observation, respectively. The HR for
Results PCI vs observation was 0.82 (95% CI, 0.63-1.06; P = .12).
This study opened on September 19, 2002, and closed owing
to poor accrual on August 30, 2007. This report includes all data DFS and BM
reported as of December 15, 2016. All data analysis took place There were 300 DFS events at the time of analysis. Five-year
from December 1, 2017 to January 15, 2018. A total of 527 deaths and 10-year DFS rates were 19.0% and 12.6% for PCI and 16.1%
and a projected accrual of 1058 participants were targeted to and 7.5% for observation, respectively (P = .03) (Table 1 and
detect a 20% risk reduction (hazard ratio [HR], 0.8, observa- Figure 2). The HR for PCI vs observation was 0.76 (95% CI, 0.59-
tion arm as reference) in death with 80% power and a 1-sided 0.97). There were 60 BM events and the 5-year and 10-year BM
significance level of P = .025. The total accrual at study clo- rates were 16.7% in the PCI arm and 28.3% in the observation
sure was 356 patients. Among 356 patients entered, 9 pa- arm (P = .004) (Table 1 and Figure 2). The corresponding HR
tients (7 PCI, 2 observation) were ineligible and 7 patients (6 was 0.43 (95% CI, 0.24-0.77). These results continued to be
PCI, 1 observation) withdrew consent. Therefore 340 pa- statistically significant.
tients were eligible for this study. The median follow-up time
was 2.1 years (range, 0.1-12.6 years) for all patients, and 9.2 years Prognostic Variables
for 63 patients still alive. The pretreatment characteristics were Multivariable Cox proportional hazards models were per-
evenly distributed between the 2 arms except Zubrod perfor- formed (Table 2). Surgery, Zubrod performance status, and age
mance status . The majority of patients received a platinum were associated with OS. Surgery was associated with DFS. A
doublet chemotherapy regimen. multivariable model of BM was also performed, but owing to
the limited number of events, the results should be inter-
Primary End Point preted with caution. Use of PCI remained strongly associated
At the time of this analysis, 277 deaths had occurred in 340 with decreased risk of developing BM; histological character-
evaluable patients, which provided approximately 45% power istics and age also appeared to be important factors. Younger
jamaoncology.com (Reprinted) JAMA Oncology Published online March 14, 2019 E3
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Research Original Investigation Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer
in the PCI arm and 30 (23%) patients in the observation arm
Figure 2. PCI vs Observation in Patients with Locally Advanced Non–
Small Cell Lung Cancer
experienced treatment failure in the brain as the first site of
failure, of which, ten (9%) and 28 (21%) were isolated events,
A Overall survival respectively. Among patients whose treatments failed, 75 (66%)
100 in the PCI arm and 68 (52%) in the observation arm first ex-
perienced local or regional failure; 62 (54%) in the PCI arm and
75 80 (61%) in the observation arm first experienced distant fail-
Overall Survival, %
ure; 23 (20%) in the PCI arm and 17 (13%) in the observation
50 arm first experienced local/regional and distant failure; and 9
(8%) PCI and 16 (12%) observation patients developed a sec-
ond primary tumor prior to experiencing any other failure
25 PCI
(eFigure 1 in Supplement 2).
Observation
0
0 1 2 3 4 5 6 7 8 9 10 11 Subgroup Analysis
Time Since Randomization, y There were 225 patients (66%) who did not have surgery.
PCI 163 122 90 64 47 39 35 34 30 22 15 Table 3 details the OS between the PCI and observation arms
Observation 177 134 91 65 51 42 35 33 24 17 11
in this subgroup. As evidenced by the data in Table 3, there were
significant differences in OS between the 2 arms, with an MS
B Disease-free survival
of 2.3 years for PCI and 1.9 years for observation, respec-
100
tively. The rates of DFS were significantly different between
the 2 arms. For BM, the rates for PCI were significantly lower
Disease-Free Survival, %
75
than those for observation. Multivariable analysis of OS
(eTable 1 in Supplement 2) revealed PCI patients had lower risks
50 of death (HR, 0.73; 95% CI, 0.54-0.98; P = .04). Zubrod per-
formance status (>0) was found to be significantly associated
PCI
25 with increased risk of death. A lower risk of DFS events was
Observation associated with PCI (HR, 0.70; 95% CI, 0.52-0.93; P = .01). For
0 BM, PCI patients were less likely to develop BM than those in
0 1 2 3 4 5 6 7 8 9 10 11
observation (HR, 0.34; 95% CI, 0.17-0.68; P = .002). In addi-
Time Since Randomization, y
tion, younger (<60 years) patients and patients with nonsqua-
PCI 163 91 58 46 36 30 27 25 23 16 10
Observation 177 92 55 35 29 26 23 22 15 9 7 mous cancers had higher rates of BM.
For subgroup analysis of the 115 patients treated with sur-
C Brain metastasis gery, there was no difference between the 2 arms for OS, MS,
100 DFS, or BM. Multivariable analysis (eTable2 in Supplement 2)
revealed that older age (≥60 years) and stage IIIB cancer were
75 associated with increased risks of death. In addition, patients
with stage IIIB cancer had higher risk of DFS events, and pa-
tients with nonsquamous cancer had higher risk of BM.
50
There was no difference between PCI and observation
Observation among the 225 patients with nonsquamous histologic charac-
25
PCI teristics with respect to OS (eTable3 in Supplement 2). Simi-
lar to the main analysis, there was a significant benefit for DFS
0 (HR, 0.72; 95% CI, 0.53-0.98; P = .04) and BM (HR, 0.43; 95%
0 1 2 3 4 5 6 7 8 9 10 11
Time Since Randomization, y CI, 0.25-0.78; P = .01) with the use of PCI. There were 115 pa-
PCI 163 115 86 62 47 39 35 34 30 22 15
tients with squamous histologic characteristics. There was no
Observation 177 117 81 58 46 37 31 31 23 17 11 difference in OS and DFS between the 2 arms. There was an
insufficient number of events within the BM end point for sub-
PCI indicates prophylactic cranial irradiation.
group analysis in this population.
patients (<60 years) and patients with nonsquamous cancer PCI-Related Toxic Events
were more likely to develop BM. Grade 3 acute PCI toxic events occurred in 6 (4%) of the cases
in the PCI arm, which included fatigue, hematologic, ataxia,
Patterns of First Failure depression, and headache. There was 1 (1%) grade 4 acute PCI
A total of 114 and 132 patients in the PCI and observation arms, toxic event reported (depression). Five (3%) patients in the PCI
respectively, experienced some sort of treatment failure. Fail- arm reported grade 3 late PCI toxic events. The only addi-
ing locally was defined as failure at the primary site; region- tional grade 3 late PCI toxic event, not reported initially, was
ally was defined as the regional lymph nodes, and distantly was soft-tissue necrosis. Neurocognitive function findings were pre-
any site beyond local or regional. Of these, 11 (10%) patients
E4 JAMA Oncology Published online March 14, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer Original Investigation Research
Table 2. Cox Proportional Hazard Multivariable Analysis Results for Entire Study
Overall Survival Disease-Free Survival Brain Metastasis
Covariate Comparison HR (95% CI) P Value HR (95% CI) P Value HR (95% CI) P Value
Treatment arm PCI 0.84 (0.66-1.07) .16 0.78 .04 0.44 (0.25-0.77 .01
(0.62-0.99)
Observation (RL) 1 [Reference]
Age ≥60 years 1.39 (1.08-1.79) .01 1.14 (0.90 .29 0.57 (0.34-0.97) .04
1.45
<60 years 1 [Reference]
Zubrod >0 1.34 (1.05-1.72) .02 1.18 .17 1.00 (0.59-1.70) .99
(0.93-1.49)
0 1 [Reference]
Prior surgery Yes 0.82 (0.62-1.07) .14 0.79 .07 0.65 (0.36-1.19) .16
(0.61-1.02)
No 1 [Reference]
AJCC stage IIIB 1.17 (0.91-1.50) .22 1.23 .10 0.88 (0.51-1.54) .65
(0.96-1.56)
IIIA 1 [Reference]
Histologic Squamous 1.08 (0.84-1.39) .56 1.01 .91 0.20 (0.08-0.46) .01
characteristics (0.80-1.29)
Nonsquamous 1 [Reference]
Abbreviations: AJCC, American Joint Committee on Cancer; HR, hazard ratio; MST, median survival time; PCI, prophylactic cranial irradiation.
viously published,32,33 however, with longer follow-up, there On multivariable analysis, observation, nonsquamous can-
was insufficient data for further analysis. cer, and age (<60 years) were associated with higher risk of BM,
while performance status, surgery, and stage were not. There
was no difference in BM rates between patients with stage IIIA
and IIIB disease. However, data regarding volume of disease
Discussion and extent of nodal involvement were not available. Ceresoli
The NRG Oncology/RTOG 0214 randomized clinical trial was et al5 reported borderline significance of bulky mediastinal dis-
developed to address the apparent increasing incidence of BM ease (nodes >2 cm) and the incidence of BM. Robnett et al17
in patients who are living longer with improved control of lo- reported 2-year actuarial incidence of BM of 36% with stage
coregional disease with advanced radiation and surgery tech- IIIB disease and 29% with stage II/IIIA disease. Wang et al34
niques and who are experiencing fewer extracranial distant me- conducted a more extensive analysis of impact of nodal dis-
tastases with multidrug chemotherapy. Studies have shown ease on BM in 223 patients treated surgically with stage IIIA/B
t h at t h o s e w it h a d e n o c a r c i n o m a o r n o n s q u a m o u s disease. Brain metastases were greater in patients with more
disease16,18,34,35 were at higher risk of BM. Higher BM rates are lymph nodes and nodal regions involved.
also associated with greater extent of disease.5,17,36,37 Addi- In multivariable analysis of the patients studied by Cer-
tionally, studies with trimodality therapy including surgery re- esoli et al,5 age younger than 60 years was associated with an
ported the highest rates of BM.2,3,5-7,9,10,12 The NRG Oncology/ increased risk of BM (31% vs 9%, P = .03). Carolan et al14 showed
RTOG 0214 trial was therefore stratified by histologic that 25.6% of patients younger than 60 years experienced first
characteristics (squamous or nonsquamous), stage (IIIA or IIIB), failure in the brain compared with 11.4% of patients 60 years
and therapy for primary disease (surgery or no surgery) to mini- or older. In a review of 4 SWOG studies, patients younger than
mize potential bias in estimating overall treatment effect due 50 years of age were at increased risk for developing BM with
to any heterogeneous treatment effects within these sub- a hazard ratio of 1.8 (P = .046).13 Review of the Metropolitan
groups. Although this study was closed prematurely owing to Detroit Cancer Surveillance System showed the highest inci-
poor accrual, it still represents the largest randomized clini- dence of BM in patients with lung cancer occurred in patients
cal trial to evaluate PCI in LA-NSCLC to our knowledge. With between the ages of 40 and 49 years.40 Other series have not
one-third of the planned sample size, the current long-term shown an increased risk of BM with young age.1,17
report was only able to provide approximately 45% power to The reliability of subset analyses in this trial are limited by
detect the hypothesized effect size in OS. Not surprisingly, this the low numbers, although the results are informative and may
long-term analysis failed to show a statistically significant im- guide future trials. The rates of OS and DFS were evaluated in
provement in OS, although the observed magnitude (HR, 0.82) subsets of patients with nonsquamous cancer, with surgery,
was numerically similar to the hypothesized (HR, 0.8). In ad- and without surgery for primary disease. Patients with nons-
dition, with more events than the initial report, this study quamous disease had more BMs than those with squamous dis-
shows that PCI improves DFS and decreases the risk of BM by ease. The use of PCI significantly decreased the risk of BM (HR,
57%. A number of randomized and nonrandomized studies 0.43; 95% CI, 0.24-0.78; P = .01) and a DFS event (HR, 0.72;
have consistently shown that PCI is associated with de- 95% CI, 0.53-0.98; P = .04). Perhaps there was no difference
creased risk of BM in patients with LA-NSCLC.2,7,9,10,12,21-23,38,39 between PCI and observation among the 225 patients with non-
jamaoncology.com (Reprinted) JAMA Oncology Published online March 14, 2019 E5
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Research Original Investigation Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer
Table 3. Outcome Estimates, by Prior Surgery Status
Event Estimate % (95% Event Estimate % (95%
Outcome by Time No. at Risk CI) No. at Risk CI) PCI vs Observation HR (95% CI)a P Valueb
No Prior Surgery
PCI (n = 106) Observation (n = 119)
Overall survival 0.70 (0.52-0.96) .03
2y 60 58.3 (48.2-67.1) 54 47.7 (38.3-56.4)
5y 23 22.8 (15.2-31.3) 21 19.5 (12.7-27.3)
10 y 9 16.6 (10.1-24.5) 5 8.9 (4.2-15.7)
MST (95% CI) 2.3 y (2.0-3.0) 1.9 (1.4-2.2)
No. of events 85 102
Disease-free survival 0.69 (0.51-0.93) .01
2y 38 36.6 (27.5-45.8) 28 24.0 (16.7-32.0)
5y 18 17.8 (11.1-25.8) 12 10.7 (5.9-17.1)
10 y 6 11.7 (6.4-18.9) 3 4.9 (1.8-10.2)
MST (95% CI) 1.1 y (0.8-1.6) 1.0 (0.6-1.0)
No. of events 92 110
Brain metastasis 0.36 (0.18-0.72) .01
2y 57 9.5 (5.0-17.5) 47 27.0 (19.2-37.2)
5y 23 13.0 (7.3-22.8) 19 31.0 (22.1-42.3)
10 y 9 13.0 (7.3-22.8) 5 31.0 (22.1-42.3)
MST (95% CI) Not reached Not reached
No. of events 11 29
Prior Surgery
PCI (n = 57) Observation (n = 58)
Overall survival 1.15 (0.72-1.84) .56
2y 30 52.6 (39.0-64.6) 37 63.8 (50.1-74.7)
5y 16 28.1 (17.2-40.0) 21 38.9 (26.3-51.2)
10 y 6 19.3 (10.3-30.4) 6 22.1 (11.9-34.4)
MST (95% CI) 2.5 y (1.4-3.4) 3.1 y (2.2-5.3)
No. of events 46 44
Disease-free survival 0.95 (0.60-1.51) .84
2y 20 35.1 (23.1-47.4) 27 46.6 (33.4-58.7)
5y 12 21.1 (11.6-32.4) 14 27.0 (16.2-38.9)
10 y 4 14.0 (6.6-24.3) 4 12.9 (5.1-24.4)
MST (95% CI) 1.5 y (1.0-1.6) 1.6 y (1.0-2.6)
No. of events 49 49
Brain metastasis 0.66 (0.24-1.84) .43
2y 29 13.6 (6.3-28.0) 34 19.1 (10.7-32.7)
5y 16 22.6 (11.3-42.0) 18 23.1 (13.1-39.0)
10 y 6 22.6 (11.3-42.0) 6 23.1 (13.1-39.0)
MST (95% CI) Not reached Not reached
No. of events 8 11
Abbreviations: AJCC, American Joint Committee on Cancer; HR, hazard ratio; performance status (0 vs >0).
MST, median survival time; PCI, prophylactic cranial irradiation. b
From stratified log-rank test, stratified by AJCC stage (IIIA vs IIIB); histologic
a
From stratified Cox proportional hazard model, stratified by AJCC stage (IIIA vs characteristics (nonsquamous vs squamous) and Zubrod performance status
IIIB); histologic characteristics (nonsquamous vs squamous) and Zubrod (0 vs >0).
squamous cancer with respect to OS; as in a subgroup of pa- subset analyses showed that patients with surgery had a rela-
tients, targeted therapies can be effective as salvage treat- tively low rate of BM, and the risk did not appear to be influ-
ment, including for BM, especially new-generation targeted enced by PCI. A possible explanation is that patients in the NRG
agents.41-46 Oncology/RTOG 0214 trial who were undergoing surgery had
Although it was expected that patients with surgery for more favorable disease than in reported trimodality trials. The
treatment of primary disease would have a higher rate of BM proportion of patients with subclinical or gross N2 disease is
and would therefore be more likely to benefit from PCI, this not known, although it is likely that patients treated surgi-
was not shown in this trial. Contrary to what was anticipated, cally had lower-volume disease, including bulk of nodal dis-
E6 JAMA Oncology Published online March 14, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer Original Investigation Research
ease and number of nodal stations, relative to the nonsurgi- It is the risk-benefit ratio that helps to determine the ad-
cal patients in this trial. visability of a particular treatment. The risks of PCI are mainly
Subset analysis of patients treated nonsurgically showed related to the effects on neurocognitive function, which we and
higher incidence of BM in the observation arm at 5 and 10 years others have previously reported.2,7,32,33,47-50 Effective strate-
(31%) than in the observation arm of the surgery group (23%). gies to decrease these risks include the use of the neuropro-
This may be owing to higher risk of BM in the nonsurgical group tectant memantine51 and PCI with hippocampal avoidance.52-55
owing to disease burden. Median OS (2.3 years vs 1.9 years, Both of these strategies have shown promising results when
P = .03) and DFS (1.1 years vs 1.0 years; P = .01) were better with treating known BM with whole brain radiotherapy. Prospec-
PCI in nonsurgical patients. On multivariable analysis, PCI and tive randomized phase 2/3 studies will be addressing these
favorable performance status were associated with improved same strategies in SCLC, where PCI is part of standard of
OS, and PCI was associated with improved DFS in the nonsur- care56-59 and may be appropriate for select patients with LA-
gical subset. The therapeutic effect of PCI, if any, appears to NSCLC and high risk of BM.
be mainly driven by patients treated without surgery. Multi- The challenge in the future is to exploit the therapeutic ra-
variable analysis within this patient population suggests that tio of benefits vs risks. Patients most likely to benefit from PCI
PCI effectively prolongs OS (HR, 0.73; P = .04) and DFS (HR, are those at highest risk of developing BM. These patients
0.70; P = .01), and decreases BM (HR, 0.34; P = .002). The origi- would include those treated without surgery or with poor risk
nal study design assumed the MS time for operable and inop- features such as nonsquamous cancer, young age, and high-
erable patients as 38 and 17 months, respectively, and hypoth- volume disease. To minimize the risk, promising strategies in-
esized detection of a 20% relative risk reduction among both clude hippocampal avoidance radiotherapy techniques and/or
operable and inoperable patients (HR, 0.8, observation arm as neuroprotectants (memantine). Furthermore, as the stan-
reference level). Had all patients in this study been treated with- dard treatment of unresectable stage III disease is in the pro-
out surgery, the corresponding subgroup analysis suggests that c e s s o f c h a nge w it h t h e a dd it i o n o f c o n s o l i d at i o n
PCI would have effectively reduced the relative risk of death immunotherapy,60,61 this has to be taken into account for fu-
by 30% (HR, 0.70). We had hypothesized that the incidence ture trials.
rates of BM would improve from 23.4% to 15.0% by using PCI.
This long-term analysis supports this hypothesis in both the Limitations
overall population (28.3% to 16.7%, HR, 0.43) and in patients The main limitation of this study was the lack of patient ac-
treated without surgery (31.0% to 13.0%, HR, 0.36). crual, which likely contributed to the lack of OS benefit for the
Of the patients who experienced failure, 10% in the PCI arm entire cohort. If the planned sample size had been accrued, then
and 23% in the observation arm experienced failure in the brain there may have been enough statistical power to detect the hy-
as the first site of failure, of which 9% and 21% were isolated pothesized effect size in OS, as the observed magnitude (HR,
events, respectively. With the advent of stereotactic radiosur- 0.82) was numerically similar to the hypothesized (HR, 0.8).
gery for BM, it is likely that many of these patients were treated This study, the largest randomized phase 3 clinical trial to evalu-
with stereotactic radiosurgery, thereby potentially confound- ate PCI in LA-NSCLC to our knowledge, is currently part of an
ing the OS results, more so in the observation arm. Further- international collaborative effort, which is performing an in-
more, the decrease in BM, especially as the first site of fail- dividual patient data meta-analysis of similar randomized stud-
ure, likely contributed to the improvement in DFS seen in the ies. It is hoped that this meta-analysis will have the power to
PCI arm. Since BMs have such a profound impact on QOL, it is detect an OS advantage for PCI, as was the case for the estab-
likely that this benefit in DFS would translate into improved lishment of PCI in SCLC.56
QOL. Unfortunately, we do not have enough long-term data
on QOL to confirm this potentially important finding.
The main difference between the preliminary analysis and
this long-term update is the improvement in DFS. With lon-
Conclusions
ger follow-up, DFS of PCI patients became statistically signifi- In conclusion, this final analysis did not show an overall sur-
cantly better than observation (HR, 0.76, 95% CI, 0.59-0.97; vival benefit, although PCI improved DFS and decreased the
P = .03; 5- and 10-year rates 19.0% and 12.6% vs 16.1% and 7.5% risk of BM in patients with LA-NSCLC. It is very unlikely that
for PCI vs observation). Although OS was also improved with a single definitive study with and without PCI for NSCLC will
longer follow-up, it was not significant.(HR, 0.82; 95% CI, 0.63- ever be completed, although establishing an accepted means
1.06; P = .12; 5- and 10-year rates, 24.7% and 17.6% vs 26.0% of prevention of BM remains important. Currently, the most
and 13.3%, for PCI vs observation) The lack of patients ac- effective therapy to prevent BMs is PCI. Identifying the ap-
crued likely contributed to the lack of OS benefit. Unfortu- propriate patient population and a safe intervention is criti-
nately, it is unlikely with even longer follow-up that OS will cal.
show a difference in this study because of the limited num-
bers of patients still alive.
ARTICLE INFORMATION Published Online: March 14, 2019. Author Contributions: Dr Sun had full access to all
Accepted for Publication: November 30, 2018. doi:10.1001/jamaoncol.2018.7220 of the data in the study and takes responsibility for
jamaoncology.com (Reprinted) JAMA Oncology Published online March 14, 2019 E7
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Research Original Investigation Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer
the integrity of the data and the accuracy of the carcinoma. Cancer. 2001;92(1):160-164. doi:10. 18. Cox JD, Scott CB, Byhardt RW, et al. Addition of
data analysis.. 1002/1097-0142(20010701)92:1<160::AID- chemotherapy to radiation therapy alters failure
Study concept and design: Sun, Hu, Gore, Choy. CNCR1304>3.0.CO;2-X patterns by cell type within non-small cell
Acquisition, analysis, or interpretation of data: Sun, 7. Stuschke M, Eberhardt W, Pöttgen C, et al. carcinoma of lung (NSCCL): analysis of radiation
Hu, Wong, Gore, Videtic, Dutta, Suntha, Chen, Prophylactic cranial irradiation in locally advanced therapy oncology group (RTOG) trials. Int J Radiat
Gaspar. non-small-cell lung cancer after multimodality Oncol Biol Phys. 1999;43(3):505-509. doi:10.1016/
Drafting of the manuscript: Sun, Hu, Gore. treatment: long-term follow-up and investigations S0360-3016(98)00429-5
Critical revision of the manuscript for important of late neuropsychologic effects. J Clin Oncol. 1999; 19. Komaki R, Scott CB, Sause WT, et al; Radiation
intellectual content: All authors. 17(9):2700-2709. doi:10.1200/JCO.1999.17.9.2700 Therapy Oncology Group. Eastern Cooperative
Statistical analysis: Sun, Hu. Oncology Group. Induction cisplatin/vinblastine
Obtained funding: Choy. 8. Choi NC, Carey RW, Daly W, et al. Potential
impact on survival of improved tumor downstaging and irradiation vs. irradiation in unresectable
Administrative, technical, or material support: Sun, squamous cell lung cancer: failure patterns by cell
Wong, Gore, Choy. and resection rate by preoperative twice-daily
radiation and concurrent chemotherapy in stage type in RTOG 88-08/ECOG 4588. Int J Radiat Oncol
Study supervision: Sun, Hu, Gore, Choy. Biol Phys. 1997;39(3):537-544. doi:10.1016/S0360-
IIIA non-small-cell lung cancer. J Clin Oncol. 1997;15
Conflict of Interest Disclosures: Dr Choy reports (2):712-722. doi:10.1200/JCO.1997.15.2.712 3016(97)00365-9
stock/ownership interest in Texas Radiotherapy 20. Arriagada R, Le Chevalier T, Quoix E, et al.
Innovation and Optimization, consulting/advisory 9. Albain KS, Rusch VW, Crowley JJ, et al.
Concurrent cisplatin/etoposide plus chest ASTRO (American Society for Therapeutic
role with Vertex Pharmaceutical and Boehringer Radiology and Oncology) plenary: Effect of
Ingelheim, and research funding from Celgene. No radiotherapy followed by surgery for stages IIIA
(N2) and IIIB non-small-cell lung cancer: mature chemotherapy on locally advanced non-small cell
other disclosures are reported. lung carcinoma: a randomized study of 353
results of Southwest Oncology Group phase II study
Funding/Support: This project was supported by 8805. J Clin Oncol. 1995;13(8):1880-1892. doi:10. patients. GETCB (Groupe d’Etude et Traitement des
RTOG grant U10 CA21661, CCOP grant U10 1200/JCO.1995.13.8.1880 Cancers Bronchiques), FNCLCC (Féderation
CA37422, and Stat grant U10 CA32115 from the Nationale des Centres de Lutte contre le Cancer)
National Cancer Institute (NCI). This manuscript’s 10. Strauss GM, Herndon JE, Sherman DD, et al. and the CEBI trialists. Int J Radiat Oncol Biol Phys.
contents are solely the responsibility of the authors Neoadjuvant chemotherapy and radiotherapy 1991;20(6):1183-1190. doi:10.1016/0360-3016(91)
and do not necessarily represent the official views followed by surgery in stage IIIA non-small-cell 90226-T
of the National Cancer Institute. carcinoma of the lung: report of a Cancer and
Leukemia Group B phase II study. J Clin Oncol. 1992; 21. Cox JD, Stanley K, Petrovich Z, Paig C, Yesner R.
Role of the Funder/Sponsor: The funders had no 10(8):1237-1244. doi:10.1200/JCO.1992.10.8.1237 Cranial irradiation in cancer of the lung of all cell
role in the design and conduct of the study; types. JAMA. 1981;245(5):469-472. doi:10.1001/
collection, management, analysis, and 11. Weiden PL, Piantadosi S. Preoperative jama.1981.03310300023013
interpretation of the data; preparation, review, or chemotherapy (cisplatin and fluorouracil) and
radiation therapy in stage III non-small-cell lung 22. Umsawasdi T, Valdivieso M, Chen TT, et al. Role
approval of the manuscript; and decision to submit of elective brain irradiation during combined
the manuscript for publication. cancer: a phase II study of the Lung Cancer Study
Group. J Natl Cancer Inst. 1991;83(4):266-273. doi: chemoradiotherapy for limited disease non-small
Data Sharing Statement: See Supplement 3. 10.1093/jnci/83.4.266 cell lung cancer. J Neurooncol. 1984;2(3):253-259.
doi:10.1007/BF00253278
REFERENCES 12. Skarin A, Jochelson M, Sheldon T, et al.
Neoadjuvant chemotherapy in marginally 23. Russell AH, Pajak TE, Selim HM, et al.
1. Chen AM, Jahan TM, Jablons DM, Garcia J, resectable stage III M0 non-small cell lung cancer: Prophylactic cranial irradiation for lung cancer
Larson DA. Risk of cerebral metastases and long-term follow-up in 41 patients. J Surg Oncol. patients at high risk for development of cerebral
neurological death after pathological complete 1989;40(4):266-274. doi:10.1002/jso.2930400413 metastasis: results of a prospective randomized
response to neoadjuvant therapy for locally trial conducted by the Radiation Therapy Oncology
advanced nonsmall-cell lung cancer: clinical 13. Gaspar LE, Chansky K, Albain KS, et al. Time Group. Int J Radiat Oncol Biol Phys. 1991;21(3):637-
implications for the subsequent management of from treatment to subsequent diagnosis of brain 643. doi:10.1016/0360-3016(91)90681-S
the brain. Cancer. 2007;109(8):1668-1675. doi:10. metastases in stage III non-small-cell lung cancer:
a retrospective review by the Southwest Oncology 24. Gore EM, Bae K, Wong SJ, et al. Phase III
1002/cncr.22565 comparison of prophylactic cranial irradiation
Group. J Clin Oncol. 2005;23(13):2955-2961. doi:10.
2. Pöttgen C, Eberhardt W, Grannass A, et al. 1200/JCO.2005.08.026 versus observation in patients with locally
Prophylactic cranial irradiation in operable stage IIIA advanced non-small-cell lung cancer: primary
non small-cell lung cancer treated with neoadjuvant 14. Carolan H, Sun AY, Bezjak A, et al. Does the analysis of radiation therapy oncology group study
chemoradiotherapy: results from a German incidence and outcome of brain metastases in RTOG 0214. J Clin Oncol. 2011;29(3):272-278. doi:
multicenter randomized trial. J Clin Oncol. 2007;25 locally advanced non-small cell lung cancer justify 10.1200/JCO.2010.29.1609
(31):4987-4992. doi:10.1200/JCO.2007.12.5468 prophylactic cranial irradiation or early detection?
Lung Cancer. 2005;49(1):109-115. doi:10.1016/j. 25. Kaplan EL, Meier P. Nonparametric estimation
3. Mamon HJ, Yeap BY, Jänne PA, et al. High risk of lungcan.2004.12.004 from incomplete observations. J Am Stat Assoc.
brain metastases in surgically staged IIIA 1958;35:457-481. doi:10.1080/01621459.1958.
non-small-cell lung cancer patients treated with 15. Albain KS, Crowley JJ, Turrisi AT III, et al. 10501452
surgery, chemotherapy, and radiation. J Clin Oncol. Concurrent cisplatin, etoposide, and chest
radiotherapy in pathologic stage IIIB non-small-cell 26. Kalbfleisch JD, Prentice RL. The Statistical
2005;23(7):1530-1537. doi:10.1200/JCO.2005.04.123 Analysis of Failure Time Data. Hoboken, New Jersey:
lung cancer: a Southwest Oncology Group phase II
4. Keith B, Vincent M, Stitt L, et al. Subsets more study, SWOG 9019. J Clin Oncol. 2002;20(16): John Wiley & Sons; 2011.
likely to benefit from surgery or prophylactic cranial 3454-3460. doi:10.1200/JCO.2002.03.055 27. Mantel N. Evaluation of survival data and two
irradiation after chemoradiation for localized new rank order statistics arising in its consideration.
non-small-cell lung cancer. Am J Clin Oncol. 2002; 16. Andre F, Grunenwald D, Pujol JL, et al. Patterns
of relapse of N2 non–small cell lung carcinoma Cancer Chemother Rep. 1966;50(3):163-170.
25(6):583-587. doi:10.1097/00000421-200212000-
00011 patients treated with preoperative chemotherapy: 28. Kim K, Tsiatis AA. Study duration for clinical
should prophylactic cranial irradiation be trials with survival response and early stopping rule.
5. Ceresoli GL, Reni M, Chiesa G, et al. Brain reconsidered? Cancer. 2001;91:2394-2400. doi:10. Biometrics. 1990;46(1):81-92. doi:10.2307/2531632
metastases in locally advanced nonsmall cell lung 1002/1097-0142(20010615)91:12<2394::AID-
carcinoma after multimodality treatment: risk 29. Cox DR. Regression models and life-tables
CNCR1273>3.0.CO;2-6 (with discussion). J R Stat Soc B. 1972;34:187-200.
factors analysis. Cancer. 2002;95(3):605-612. doi:
10.1002/cncr.10687 17. Robnett TJ, Machtay M, Stevenson JP, Algazy 30. Prentice RL, Kalbfleisch JD, Peterson AV Jr,
KM, Hahn SM. Factors affecting the risk of brain Flournoy N, Farewell VT, Breslow NE. The analysis
6. Law A, Karp DD, Dipetrillo T, Daly BT. Emergence metastases after definitive chemoradiation for
of increased cerebral metastasis after high-dose of failure times in the presence of competing risks.
locally advanced non-small-cell lung carcinoma. Biometrics. 1978;34(4):541-554. doi:10.2307/
preoperative radiotherapy with chemotherapy in J Clin Oncol. 2001;19(5):1344-1349. doi:10.1200/
patients with locally advanced nonsmall cell lung 2530374
JCO.2001.19.5.1344
E8 JAMA Oncology Published online March 14, 2019 (Reprinted) jamaoncology.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non–Small Cell Lung Cancer Original Investigation Research
31. Gail M, Simon R. Testing for qualitative 41. Wu YL, Ahn MJ, Garassino MC, et al. CNS 51. Brown PD, Pugh S, Laack NN, et al; Radiation
interactions between treatment effects and patient efficacy of osimertinib in patients with Therapy Oncology Group (RTOG). Memantine for
subsets. Biometrics. 1985;41(2):361-372. doi:10. T790M-positive advanced non-small-cell lung the prevention of cognitive dysfunction in patients
2307/2530862 cancer: data from a randomized phase III trial receiving whole-brain radiotherapy: a randomized,
32. Sun A, Bae K, Gore EM, et al. Phase III trial of (AURA3). J Clin Oncol. 2018;36(26):2702-2709. double-blind, placebo-controlled trial. Neuro Oncol.
prophylactic cranial irradiation compared with doi:10.1200/JCO.2018.77.9363 2013;15(10):1429-1437. doi:10.1093/neuonc/not114
observation in patients with locally advanced 42. Zhang I, Zaorsky NG, Palmer JD, Mehra R, Lu B. 52. Gutiérrez AN, Westerly DC, Tomé WA, et al.
non-small-cell lung cancer: neurocognitive and Targeting brain metastases in ALK-rearranged Whole brain radiotherapy with hippocampal
quality-of-life analysis. J Clin Oncol. 2011;29(3):279- non-small-cell lung cancer. Lancet Oncol. 2015;16 avoidance and simultaneously integrated brain
286. doi:10.1200/JCO.2010.29.6053 (13):e510-e521. doi:10.1016/S1470-2045(15)00013- metastases boost: a planning study. Int J Radiat
33. Gondi V, Paulus R, Bruner DW, et al. Decline in 3 Oncol Biol Phys. 2007;69(2):589-597. doi:10.1016/j.
tested and self-reported cognitive functioning after 43. Johung KL, Yeh N, Desai NB, et al. Extended ijrobp.2007.05.038
prophylactic cranial irradiation for lung cancer: survival and prognostic factors for patients with 53. Gondi V, Pugh SL, Tome WA, et al. Preservation
pooled secondary analysis of Radiation Therapy ALK-rearranged non-small-cell lung cancer and of memory with conformal avoidance of the
Oncology Group randomized trials 0212 and 0214. brain metastasis. J Clin Oncol. 2016;34(2):123-129. hippocampal neural stem-cell compartment during
Int J Radiat Oncol Biol Phys. 2013;86(4):656-664. doi:10.1200/JCO.2015.62.0138 whole-brain radiotherapy for brain metastases
doi:10.1016/j.ijrobp.2013.02.033 44. Gerber NK, Yamada Y, Rimner A, et al. Erlotinib (RTOG 0933): a phase II multi-institutional trial.
34. Komaki R, Cox JD, Stark R. Frequency of brain versus radiation therapy for brain metastases in J Clin Oncol. 2014;32(34):3810-3816. doi:10.1200/
metastasis in adenocarcinoma and large cell patients with EGFR-mutant lung adenocarcinoma. JCO.2014.57.2909
carcinoma of the lung: correlation with survival. Int Int J Radiat Oncol Biol Phys. 2014;89(2):322-329. 54. Kazda T, Jancalek R, Pospisil P, et al. Why and
J Radiat Oncol Biol Phys. 1983;9(10):1467-1470. doi: doi:10.1016/j.ijrobp.2014.02.022 how to spare the hippocampus during brain
10.1016/0360-3016(83)90319-X 45. Reungwetwattana T, Nakagawa K, Cho BC, radiotherapy: the developing role of hippocampal
35. Perez CA, Pajak TF, Simpson JR, et al. et al. CNS response to osimertinib versus standard avoidance in cranial radiotherapy. Radiat Oncol.
Long-term observations of the patterns of failure in epidermal growth factor receptor tyrosine kinase 2014;9:139. doi:10.1186/1748-717X-9-139
patients with unresectable non-oat cell carcinoma inhibitors in patients with untreated EGFR-mutated 55. Péchoux CL, Sun A, Slotman BJ, De Ruysscher
of the lung treated with definitive radiotherapy. advanced non-small-cell lung cancer. J Clin Oncol. D, Belderbos J, Gore EM. Prophylactic cranial
Cancer. 1987;59:1874-1881. doi:10.1002/1097-0142 2018;JCO2018783118. irradiation for patients with lung cancer. Lancet Oncol.
(19870601)59:11<1874::AID-CNCR2820591106>3. 46. Costa DB, Shaw AT, Ou SH, et al. Clinical 2016;17(7):e277-e293. doi:10.1016/S1470-2045(16)
0.CO;2-Z experience with crizotinib in patients with 30065-1
36. Wang SY, Ye X, Ou W, Lin YB, Zhang BB, Yang H. advanced ALK-rearranged non–small-cell lung 56. Aupérin A, Arriagada R, Pignon JP, et al;
Risk of cerebral metastases for postoperative locally cancer and brain metastases. J Clin Oncol. 2015;33 Prophylactic Cranial Irradiation Overview
advanced non-small-cell lung cancer. Lung Cancer. (17):1881-1888. doi:10.1200/JCO.2014.59.0539 Collaborative Group. Prophylactic cranial irradiation
2009;64(2):238-243. doi:10.1016/j.lungcan.2008. 47. Arriagada R, Le Chevalier T, Borie F, et al. for patients with small-cell lung cancer in complete
08.012 Prophylactic cranial irradiation for patients with remission. N Engl J Med. 1999;341(7):476-484. doi:
37. Komaki R, Scott CB, Byhardt R, et al. Failure small-cell lung cancer in complete remission. J Natl 10.1056/NEJM199908123410703
patterns by prognostic group determined by Cancer Inst. 1995;87(3):183-190. doi:10.1093/jnci/ 57. Meert AP, Paesmans M, Berghmans T, et al.
recursive partitioning analysis (RPA) of 1547 87.3.183 Prophylactic cranial irradiation in small cell lung
patients on four radiation therapy oncology group 48. Gregor A, Cull A, Stephens RJ, et al; United cancer: a systematic review of the literature with
(RTOG) studies in inoperable nonsmall-cell lung Kingdom Coordinating Committee for Cancer meta-analysis. BMC Cancer. 2001;1:5. doi:10.1186/
cancer (NSCLC). Int J Radiat Oncol Biol Phys. 1998; Research (UKCCCR) and the European Organization 1471-2407-1-5
42(2):263-267. doi:10.1016/S0360-3016(98)00213- for Research and Treatment of Cancer (EORTC). 58. Slotman B, Faivre-Finn C, Kramer G, et al;
2 Prophylactic cranial irradiation is indicated EORTC Radiation Oncology Group and Lung Cancer
38. Li N, Zeng ZF, Wang SY, et al. Randomized following complete response to induction therapy Group. Prophylactic cranial irradiation in extensive
phase III trial of prophylactic cranial irradiation in small cell lung cancer: results of a multicentre small-cell lung cancer. N Engl J Med. 2007;357(7):
versus observation in patients with fully resected randomised trial. Eur J Cancer. 1997;33(11):1752-1758. 664-672. doi:10.1056/NEJMoa071780
stage IIIA-N2 nonsmall-cell lung cancer and high risk doi:10.1016/S0959-8049(97)00135-4 59. Schild SE, Foster NR, Meyers JP, et al; North
of cerebral metastases after adjuvant 49. Wolfson AH, Bae K, Komaki R, et al. Primary Central Cancer Treatment Group. Prophylactic
chemotherapy. Ann Oncol. 2015;26(3):504-509. analysis of a phase II randomized trial Radiation cranial irradiation in small-cell lung cancer: findings
doi:10.1093/annonc/mdu567 Therapy Oncology Group (RTOG) 0212: impact of from a North Central Cancer Treatment Group
39. De Ruysscher D, Dingemans AC, Praag J, et al. different total doses and schedules of prophylactic Pooled Analysis. Ann Oncol. 2012;23(11):2919-2924.
Prophylactic cranial irradiation versus observation cranial irradiation on chronic neurotoxicity and doi:10.1093/annonc/mds123
in radically treated stage III non-small-cell lung quality of life for patients with limited-disease 60. Antonia SJ, Villegas A, Daniel D, et al; PACIFIC
cancer: a randomized phase III NVALT-11/DLCRG-02 small-cell lung cancer. Int J Radiat Oncol Biol Phys. Investigators. Durvalumab after chemoradio-
Study. J Clin Oncol. 2018;36(23):2366-2377. doi:10. 2011;81(1):77-84. doi:10.1016/j.ijrobp.2010.05.013 therapy in stage III non–small-cell lung cancer.
1200/JCO.2017.77.5817 50. Le Péchoux C, Laplanche A, Faivre-Finn C, et al; N Engl J Med. 2017;377(20):1919-1929. doi:10.1056/
40. Barnholtz-Sloan JS, Sloan AE, Davis FG, Prophylactic Cranial Irradiation (PCI) Collaborative NEJMoa1709937
Vigneau FD, Lai P, Sawaya RE. Incidence Group. Clinical neurological outcome and quality of 61. Antonia SJ, Villegas A, Daniel D, et al; PACIFIC
proportions of brain metastases in patients life among patients with limited small-cell cancer Investigators. Overall survival with durvalumab
diagnosed (1973 to 2001) in the Metropolitan treated with two different doses of prophylactic after chemoradiotherapy in stage III NSCLC. N Engl J
Detroit Cancer Surveillance System. J Clin Oncol. cranial irradiation in the intergroup phase III trial Med. 2018;379(24):2342-2350. doi:10.1056/
2004;22(14):2865-2872. doi:10.1200/JCO.2004.12. (PCI99-01, EORTC 22003-08004, RTOG 0212 and NEJMoa1809697
149 IFCT 99-01). Ann Oncol. 2011;22(5):1154-1163. doi:
10.1093/annonc/mdq576
jamaoncology.com (Reprinted) JAMA Oncology Published online March 14, 2019 E9
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a East Carolina University User on 03/14/2019
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Arthritis and SaturnDokument4 SeitenArthritis and SaturnJatinder SandhuNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- 2 Year Physical Therapy NotesDokument129 Seiten2 Year Physical Therapy Notesthwiseman94% (17)
- Acute Respiratory FailureDokument17 SeitenAcute Respiratory FailurejulianajosNoch keine Bewertungen
- Ayurvedic treatment of hearing lossDokument9 SeitenAyurvedic treatment of hearing lossshweta kotwal100% (1)
- 02 - LEC DOH Programs For Communicable - Non-Communicable DiseasesDokument21 Seiten02 - LEC DOH Programs For Communicable - Non-Communicable DiseasesJAN CAMILLE LENONNoch keine Bewertungen
- Evaluation of Sleep Disturbances in Children With Epilepsy A Questionnaire BasedDokument4 SeitenEvaluation of Sleep Disturbances in Children With Epilepsy A Questionnaire BasednoiNoch keine Bewertungen
- La Consolacion College Manila School of Nursing Course SyllabusDokument4 SeitenLa Consolacion College Manila School of Nursing Course SyllabusJayson Magdael SalvadorNoch keine Bewertungen
- Transfusion-Associated Circulatory Overload (TACO)Dokument2 SeitenTransfusion-Associated Circulatory Overload (TACO)belongs2diah3058100% (1)
- (MS II Lec) Endocrine System2Dokument8 Seiten(MS II Lec) Endocrine System2IlawNoch keine Bewertungen
- Ovarian Cancer Antigen (Ca-125) : Enzyme Immunoassay Test Kit Catalog Number: 10103Dokument2 SeitenOvarian Cancer Antigen (Ca-125) : Enzyme Immunoassay Test Kit Catalog Number: 10103yousrazeidan1979Noch keine Bewertungen
- AIHADokument4 SeitenAIHAKristine Mae AbrasaldoNoch keine Bewertungen
- NizoralDokument4 SeitenNizoralianecunar100% (2)
- Procedure 28-: Assessing The Nose and Sinuses: Physical AssessmentDokument2 SeitenProcedure 28-: Assessing The Nose and Sinuses: Physical Assessmentlee jenoNoch keine Bewertungen
- Neema Rawat Microteaching (Spina Bifida)Dokument67 SeitenNeema Rawat Microteaching (Spina Bifida)Dimple GoyalNoch keine Bewertungen
- Sample Questions 2Dokument6 SeitenSample Questions 2Filipino Nurses CentralNoch keine Bewertungen
- Maxillary Sinus Health DiseaseDokument36 SeitenMaxillary Sinus Health Diseasesaba mahrNoch keine Bewertungen
- Pathology Course Audit-3Dokument26 SeitenPathology Course Audit-3Joana Marie PalatanNoch keine Bewertungen
- Multiple Sclerosis - CompiledDokument7 SeitenMultiple Sclerosis - CompiledAdib Aiman A RashidNoch keine Bewertungen
- Breath Stacking A Guide For PatientsDokument2 SeitenBreath Stacking A Guide For PatientsaagarwalmdNoch keine Bewertungen
- Paracetamol OverdoseDokument1 SeiteParacetamol OverdoseMilanisti22Noch keine Bewertungen
- RENAAL Overview: Brenner BM, Et Al. N Engl J Med. 2001 345 (12) :861-869Dokument7 SeitenRENAAL Overview: Brenner BM, Et Al. N Engl J Med. 2001 345 (12) :861-869ekadtorNoch keine Bewertungen
- All by Gyn Obst Depart PDFDokument27 SeitenAll by Gyn Obst Depart PDFRaouf Ra'fat Soliman100% (2)
- Animal Bite: Pablo R. Quedado, MDDokument36 SeitenAnimal Bite: Pablo R. Quedado, MDPrincess Noreen SavellanoNoch keine Bewertungen
- Chromosomal Disorder GuideDokument21 SeitenChromosomal Disorder GuideRemiel MarticioNoch keine Bewertungen
- Icd XDokument30 SeitenIcd Xrsud butengNoch keine Bewertungen
- Soal Uas B.ingDokument6 SeitenSoal Uas B.ingNopriani InuarNoch keine Bewertungen
- Vital Signs Assessment TableDokument2 SeitenVital Signs Assessment Tableapi-250869701Noch keine Bewertungen
- Terminolohiyang Pampandemya Na Nasa Wikang Ingles at Implikasyon Nito Sa Pag UnawaDokument13 SeitenTerminolohiyang Pampandemya Na Nasa Wikang Ingles at Implikasyon Nito Sa Pag UnawaTan KarlNoch keine Bewertungen
- Case 3 - JJ - Oral PracticalDokument3 SeitenCase 3 - JJ - Oral PracticalCindy MurphyNoch keine Bewertungen
- Small Intestinal Bacterial Overgrowth: A Primary Care ReviewDokument6 SeitenSmall Intestinal Bacterial Overgrowth: A Primary Care ReviewjilujNoch keine Bewertungen