Beruflich Dokumente
Kultur Dokumente
Causes Clinical and Imaging Characteristics of Moyamoya Disease in Children
Hochgeladen von
Riya CassendraCopyright
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Causes Clinical and Imaging Characteristics of Moyamoya Disease in Children
Hochgeladen von
Riya CassendraCopyright:
Biomedical Research 2018; 29 (6): 1154-1159 ISSN 0970-938X
www.biomedres.info
Causes, clinical and imaging characteristics of moyamoya disease in children.
Cai-Xia Wang1, Qing-Yi Wang2, Yi-Ming Zhao1, Mei Zhou1, Xiu-Xia Chen1, Rui-Yun Zhang1
1Department of Pediatrics, Qingdao Municipal Hospital, Qingdao, PR China
2Department of Pain, Qingdao Municipal Hospital, Qingdao, PR China
Abstract
Introduction: Moyamoya disease is a progressive, chronic occlusive vascular disease of the circle of
Willis arteries leading to the development of collateral circulation to compensate the occlusion.
Purpose: This study aims to investigate the potential causes and clinical and imaging characteristics of
Moyamoya Disease (MMD) in children.
Methods: A retrospective analysis was performed on the clinical data of 14 MMD children, in which the
potential causes were analysed, and the clinical and imaging characteristics were observed.
Results: The average patient age was 6.15 y (range 21 months-13 y), and the female/male ratio was
1.3:1.0. There were 332 cases of ischemia and 196 hemorrhages. Eight cases had inducing factors
including five cases of upper respiratory tract infection. Twelve cases exhibited limb weakness or
hemiplegia. Among these patients, eight cases developed these manifestations as initial symptoms.
Furthermore, seven cases presented language barriers, two cases had twitch, and two cases had
headaches with unclear vision. All 14 patients underwent cranial Magnetic Resonance Imaging (MRI)
and the results revealed that twelve cases had cerebral infarction, and two cases had cerebral
hemorrhage. Five of 14 patients experienced stenosis or occlusion at the siphon part of the bilateral
internal carotid arteries, seven patients had bilateral anterior cerebral artery stenosis or occlusion, 8
were bilateral middle cerebral artery stenosis or occlusion, and 2 were bilateral posterior cerebral
artery stenosis or occlusion. All patients smoke-like vessels in the basal ganglia region.
Conclusion: High-risk age of child MMD ranged between 4-10 y old, which mostly manifested as
transient cerebral ischemic insults; and inducing factors were mostly upper respiratory tract infections.
Keywords: Moyamoya disease, Children, Motivations, Clinical characteristic, Magnetic resonance angiography.
Accepted on December 18, 2017
Introduction
the occluded or stenotic regions corresponding to the
Moyamoya syndrome is a disease in which certain arteries in lenticulostriate and thalamoperforate arteries. This makes the
the brain are constricted. Blood flow is blocked by the blood leak out of the arteries, causing pressure to the brain and
constriction, and also by blood clots (thrombosis) [1]. The subsequent headaches. The Ministry of Health and Welfare of
moyamoya syndrome is a cerebrovascular condition that Japan has defined 4 types of moyamoya disease (MMD):
predisposes affected patients to stroke in association with ischemic, hemorrhagic, epileptic, and "other." The ischemic
progressive stenosis of the intracranial internal carotid arteries type has been shown to predominate in childhood, while the
and their proximal branches. First described in 1957 as hemorrhagic type is more often observed in the adult
“hypoplasia of the bilateral internal carotid arteries,” [2]. The population.
characteristic appearance of the associated network of
abnormally dilated collateral vessels on angiography was later Moyamoya Disease (MMD), by the appearance of smoke on
likened to “something hazy, like a puff of cigarette smoke,” relevant angiographs resultant from the tangle of tiny vessels in
[3], which, in Japanese, is moyamoya. response to stenosis. This makes the blood leak out of the
arteries, causing pressure to the brain and subsequent
Moyamoya Disease (MMD), is a chronic, occlusive headaches. Though the research of moyamoya disease has
cerebrovascular disease involving bilateral stenosis or made great strides in the past 60 years, the etiology and
occlusion of the terminal portion of the Internal Carotid pathogenesis are largely unknown. The pathogenesis of
Arteries (ICAs) and/or the proximal portions of the anterior moyamoya disease is unknown, although the gene Ring Finger
cerebral arteries and Middle Cerebral Arteries (MCAs). Protein 213 (RNF213) has been implicated [4]. In Japan, the
Moyamoya disease is also characterized by irregular incidence of Moyamoya Disease (MMD) is 1/1000,000 [5].
perforating vascular networks, called moyamoya vessels, near There are two onset peaks in age: under 10 y old and within
Biomed Res 2018 Volume 29 Issue 6 1154
Wang/Wang/Zhao/Zhou/Chen/Zhang
30-40 y old; and the ratio of male to female patients is protein and blood coagulation function, Antistreptolysin O
approximately 1:1.7. (ASO), complement C3, antinuclear antibodies and anti-
neutrophils; while eight children received serum Epstein-Barr
The diagnosis of moyamoya is suggested by CT, MRI, or
Virus (EBV), herpes simplex virus, and rubella virus antibody
angiogram results. Contrast-enhanced T1-weighted images are
tests. Moreover, six children received mycoplasma antibody
better than FLAIR images for depicting the leptomeningeal ivy
tests.
sign in moyamoya disease. MRI and MRA should be
performed for the diagnosis and follow-up of moyamoya
disease. Diffusion-weighted imaging can also be used for
Diagnostic criteria
following the clinical course of children with moyamoya The radiological diagnosis criteria proposed in 1997 by the
disease, in whom new focal deficits are highly suspicious of Moyamoya Disease Research Committee of the Japanese
new infarcts. Ministry of Health and Welfare was used as a reference [7]: (1)
The natural history of this disorder is not well known. The long stenosis or occlusion exist in the end of the internal carotid
term outlook for patients with treated moyamoya seems to be artery, or in the initial segments of the middle and anterior
good. cerebral arteries; (2) the arteries of the skull base are filled, and
the surroundings of the blockings exhibit abnormal blood
Recent investigations have established that both moyamoya vessel nets; (3) bilateral involvement. When the above three
disease and Arteriovenous Fistulas (AVFs) of the lining of the conditions are met and systemic disease is excluded, MMD
brain, the dura, are associated with dural angiogenesis. These diagnosis can be established. In MMD children, smoke-like
factors may represent a mechanism for ischemia contributing vessels sometimes primarily appear on one side, and the
to the formation of dural AVFs [6]. contralateral artery develops lesions with the increase of age.
With the development of Magnetic Resonance Imaging (MRI) Therefore, unilateral lesions are also considered in children for
diagnostic techniques, reports in China on MMD have MMD.
gradually increased in recent years. In our hospital, 14
hospitalized children were confirmed with this disease from Results
July 2003 to June 2008. Details are reported as follows.
Clinical characteristics
Materials and Methods We identified 14 patients who met the criteria for study
inclusion. The age of these children ranged between 21 months
Case data and 13 y old, with an average age of 6.15 y old. Among them,
A total of 14 hospitalized children diagnosed with MMD by the age of 11 children ranged between 21 months and 10 y old
clinical information combined with imaging tests from July (78.5%). Furthermore, among these 14 children, eight children
2000 to June 2008 were included into this study. The age of were female and six children were male, with a female-to-male
these children ranged between 21 months and 13 y old, with an ratio of 1.3:1. The course of the disease ranged from 1.5 h to
average age of 6.15 y old. Among them, the age of 11 children four years. Inducing factors: Eight children had inducing
ranged between 21 months and 10 y old (78.5%). Furthermore, factors including five cases of upper respiratory tract infections
among these 14 children, eight children were female and six (four cases had fever and one case had cough). Among these
children were male, with a female-to-male ratio of 1.3:1. The children, three children with fever developed limb weakness or
course of the disease ranged from 1.5 h to four years. Seven paralysis within three days, and one child with fever developed
children went to see a doctor after the first onset, five children limb weakness four days after the fever. Furthermore, two
went to see a doctor after the second onset, and two children children fell and developed paralysis on the same day, while
went to see a doctor after the third onset. Five children were one case was induced by intense crying.
diagnosed with viral encephalitis at the first diagnosis, one Initial symptoms: Eight children exhibited limb weakness or
child was diagnosed with mycoplasma encephalitis, and three hemiplegia, two children exhibited twitch, and two children
children were diagnosed with acute hemiplegia syndrome. developed unclear vision. Furthermore, one child had
conscious disturbance after headaches and vomiting, and one
Methods child had hearing loss.
Clinical data of 14 children were retrospectively summarized. Clinical manifestations: Twelve children exhibited limb
Adjuvant examinations: Six children underwent cranial weakness or hemiplegia, among which 10 cases had repetitive
Computed Tomography (CT) examinations, and all 14 patients limb weakness or hemiplegia, three cases had alternate
underwent cranial MRI and Magnetic Resonance Angiography episodes, and seven cases exhibited unilateral involvement.
(MRA). Furthermore, three children underwent Digital Furthermore, five cases developed persistent hemiplegia from
Subtraction Angiography (DSA), Eight Children Underwent onset, while five cases first exhibited repetitive episodes and
Electroencephalography (EEG) examinations, and six children gradually progressed to persistent hemiplegia. In addition,
received cerebrospinal fluid tests. In addition, all 14 children seven cases exhibited distortion of commissure, facial paralysis
were tested for tuberculin, blood sedimentation, C-reactive and unclear articulation, two cases exhibited twitch, two cases
1155 Biomed Res 2018 Volume 29 Issue 6
Causes, clinical and imaging characteristics of moyamoya disease in children
involuntary movement of extremities with numbness, and two twitch exhibited focus-derived abnormal discharges. In the
cases had headaches with unclear vision. Among these 14 remaining six patients, five patients exhibited abnormal slow-
patients, five patients had a history of infection before onset, wave band enhancement. Furthermore, six patients received
and one patient had head trauma five years before the onset of cerebrospinal fluid examinations, in which two children had a
MMD. Furthermore, one case was combined with cutis slightly increased cell count (0.016 × 109 and 0.012 × 109,
marmorata telangiectatica congenita, one case had respectively). In 14 cases, white blood cell count increased in
hyperthyroidism, and one case had chicken pox viral five cases; which were 18.7, 16.2, 12.1, 11.8 and 10.3 × 109,
encephalitis six month before onset. Moreover, two cases had a respectively (normal cell count is 3.6-9.2 × 109). Blood
family history of cerebrovascular disease, and the mother of sedimentation was conducted in 14 cases, and was found to
one child with cutis marmorata telangiectatica congenita also increase to 25 mm/h in one case (normal: <15 mm/h for male
had the same disease. and <20 mm/h female). Six cases underwent mycoplasma
pneumoniae antibody detection, in which three cases had
Adjuvant examination abnormal results (results for the two cases were both 1:40, and
the result for the other case was 1:80). Eight cases received
Neural imageologic tests: Six children received cranial CT rubella virus antibody detection, in which three cases were
examinations, and all children were found to have cerebral found as positive (one case was found positive for
ischemic changes. All 14 children received cranial MRI and cerebrospinal fluid mycoplasma pneumoniae antibody). In
MRA examinations. MRI manifestations: Twelve cases had addition, EBV and herpes simplex virus antibody tests revealed
cerebral infarction, and two cases had cerebral hemorrhage. negative results in three cases. In all 14 children, tuberculin,
Cerebral infarction manifested as infarcts or softened lesions. blood sedimentation, C-reactive protein and blood coagulation
Eight cases had encephalatrophy and seven cases had function, ASO, complement C3, antinuclear antibodies and
ventriculomegaly. Lesions were characterized by long T1 and anti-neutrophils tests revealed no abnormal results.
T2 signals. Nine cases exhibited bilateral MMD in MRA
images, and five cases had unilateral MMD. Furthermore, five
Treatment and prognosis
cases had stenosis or occlusion in the siphon part of bilateral
internal carotid arteries, seven cases had stenosis or occlusion Among the 14 children with proven diagnosis, one child died
in the bilateral anterior cerebral arteries, eight cases had of serious cranial high pressure and respiratory failure caused
stenosis or occlusion in the bilateral middle cerebral arteries, by cerebral infarction; and the remaining children received
and two cases had stenosis or occlusion in the bilateral anterior internal medicine conservative treatment. Nutrition for brain
cerebral arteries. In addition, five cases had an unclear display cells, intracraninal pressure lowering by mannitol and
of the anterior communicating artery, and four cases had an furosemide or a small dose of hormone, as well as anti-
unclear display of the posterior communicating artery. inflammation, expansion of blood vessels and calcium channel
Moreover, 14 cases had smoke-like vessels in the basal ganglia antagonist treatments, were performed. In addition,
region. Three children underwent DSA examinations, and rehabilitation, functional exercise, psychological therapy and
these results were consistent with those of MRA. Both MRI special education were provided according to the conditions of
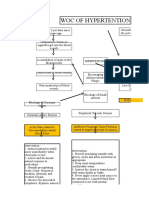
and MRA cranial examination results of one child are shown in the children. Among these children, three cases received
Figure 1. vasodilatation within 24 hours after onset of the disease.
Follow-ups
Among the 14 patients, the one who was 12 y old boy, had
stenosis of bilateral internal carotid arteries, experienced 3-
times extensive cerebral infarction, died 6 months later after
onset, and the others survived. The 13 survived patients
continuously take small dose aspirin and dipyridamole orally.
Among the rest 13 patients, 4 patients suffered hemiplegia, 2
walked unsteadily and the others suffered no hemiplegia.
Figure 1. Examining results of one case in MRI, MRA. A: Among 4 hemiplegic patients, one is 21-months girl, one is 4 y
examination result of MRA suggested that inner segment of bilateral old boy, one is 6 y old boy and one is 11 y old boy; 3 patients
internal carotid artery became thin, A1 segment of bilateral anterior with bilateral internal carotid artery stenosis and one patient
cerebral artery and proximal segment of cerebral middle artery with bilateral middle cerebral artery stenosis; 2 patients with
blocked and massive compensatory enlargement veins like smoke
the left lower limb paralysis and 2 patients with the right lower
were also observed. B and C: examining results of MRI T2W1 and
DW1 showed multiple long T2 and high signal in the bilateral
limb paralysis; the 6 y old boy with light dysgnosia by Gesell
ventricle and bilateral parietal and under the cortex of right occipital and the other three normal. Among the 2 patients who walked
lobe. unsteadily, one is 5 y old boy and the other one is 8 y old boy,
and they have normal intelligence and can walk by stick and
Other adjuvant examinations: Eight children received wheelchair. Among 7 patients who have no hemiplegia, only
electroencephalography examinations and two cases with
Biomed Res 2018 Volume 29 Issue 6 1156
Wang/Wang/Zhao/Zhou/Chen/Zhang
one had mild mental retardation and 4 patients with bilateral moyamoya disease. However, the mechanisms leading from
internal carotid artery stenosis were given the medical support. RNF213 mutations to MMD clinical features are still unknown
[18]. (2) Inflammation and immune responses. A variety of
Discussion acquired factors such as EBV infection, cerebral trauma,
tuberculous meningitis, and multiple Takayasu arteritis and
The prevalence of the disease among the Nanjing in China was radiation injury can cause chronic inflammation of the central
3.92/100,000, as reported by Miao et al. in 2010, showing a nervous system; and result in MMD [19]. Besides, the study
rising trend [8]. Moyamoya disease cases typically present [20] also shows thyroid storm may trigger cerebral ischemia in
acutely with various cerebrovascular events including Moyamoya disease and lead to rapid progression of
intracranial hemorrhage, TIAs, brain infarction, and sometimes cerebrovascular occlusive disease. Greco et al. [21] reported
epileptic seizures. The Ministry of Health and Welfare of Japan cases of mycoplasma pneumoniae infection followed by
has defined 4 types of MMD with the following presentation MMD. In the present study, six children underwent
percentages: ischemic 63.4%, hemorrhagic 21.6%, epileptic mycoplasma pneumoniae antibody detection, and three cases
7.6%, and “other”7.5% [9]. As reported before, the ischemic revealed positive results. Among these three cases, one case
type of MMD predominates in childhood, making up 69% of was positive for cerebrospinal fluid mycoplasma pneumoniae
cases in patients under 10 years old, which is consistent with antibody; suggesting that mycoplasma pneumoniae infection
our results [10]. However, the epidemiological features of might be correlated with MMD. Furthermore, in this study, one
MMD determined by this study differed from those in previous child developed chicken pox viral encephalitis six months
reports. In the previous literature, women have a higher before the occurrence of MMD. This case should be given
incidence than men, with the female/male predominance attention, as the study of Makoto et al. [22] also reported one
ranging from 1.8:1 to 4.25:1. In the present study, the ratio of case of MMD caused by chicken pox virus infection.
girls to boys was 1.3:1, which is much lower than the ratio Secondary MMD is also known as moyamoya syndrome.
reported compared with the other Asian and Western countries. Some literatures have reported that MMD co-existed with
This might reveal that MMD has been associated with the age- systemic lupus erythematosus, AIDS, Behcet's disease,
specific ratio patterns [11-14]. multiple Takayasu arteritis, hyperthyroidism and cutis
In our study, all 14 children received cranial MRI and MRA marmorata telangiectatica congenita. In this study, one child
examinations, in which 12 cases were found to have cerebral and the mother both developed cutis marmorata telangiectatica
ischemia changes, and two cases were found to have cerebral congenita. In MMD, cell proliferation and vascular dysfunction
hemorrhage. MRA revealed stenosis or occlusion in internal are associated with T cell immune dysfunction. In the above
carotid artery, as well as in the anterior, middle and posterior cases, immune complex injury following infections or
cerebral arteries; and abnormalities in the anterior and middle autoimmune injury has been considered. That is, the
cerebral arteries were the most common. Furthermore, smoke- intravascular elastic layer is curved and broken, and the medial
like vessels mostly occurred in the basal ganglia region. Three smooth muscle proliferates towards the intima at the break site.
children received DSA examination, and the results were These would result in luminal stenosis or occlusion, and
consistent with those obtained by MRA. In this study, MRI chronic ischemia in brain tissues at the artery distal end; and
combined with MRA examination can not only display subsequently, compensatory hyperplasia of small blood vessels
vascular lesions, but also show cerebral infarction, and capillaries. Hemorrhagic MMD has two major imaging
cerebromalacia, cerebral hemorrhage and cerebral atrophy; features: the dilatation and abnormal branching of anterior
which is secondary to vascular lesions. Furthermore, it is choroidal artery or posterior communicating artery, and
convenient, noninvasive, does not need a contrast agent, and is multiple microbleeds, which may predict subsequent
conducive to long-term follow-ups. Some literatures have hemorrhage [23].
revealed that MRA examination has certain limitations such as It has been reported in the previous literature that this disease
low spatial resolution, exaggeration of the extent of the mostly occurred when crying, eating hot food, blowing
vascular occlusion, and poor display of intracranial collateral balloons and other excessive breathing activities; and
circulation. Therefore, in MMD patients who require surgery, symptoms continuously re-appear. Moyamoya Disease (MMD)
DSA still needs to be performed in order clearly examine these is a chronic, occlusive cerebrovascular disease characterized by
specific sites. progressive stenosis at the terminal portion of the internal
The cause of MMD remains unclear. At present, the following carotid artery and an abnormal vascular network at the base of
views have been reported. (1) Genetic factors. The the brain [24]. Since both sides of the brain are affected, the
epidemiological characteristics of MMD prompt the onset of clinical syndromes initially manifest as vascular Parkinsonism
the disease, as a kind of polygenic hereditary disease. Studies [25], meanwhile hemiplegia, intelligence decline, seizures and
have found that [15-17] chromosomes 3p24, 2-p26, 6q, 17q25 headaches are observed usually. Therefore, to improve the
and 8q23 were related to familial MMD. Characteristics of quality of life of MMD patients not only the protection from
genetic moyamoya syndromes are presented, with a focus on the neurological insult but also the maintenance or
recently reported mutations in BRCC3/MTCP1 and GUCY1A3 improvement of cognitive function is inevitable [26]; which
genes and Liu et al. provided evidence suggesting, for the first alternatively appear in the left and right side. In this study, the
time, the involvement of RNF213 in genetic susceptibility to average age of onset was 6.15 y old, which belong to the
1157 Biomed Res 2018 Volume 29 Issue 6
Causes, clinical and imaging characteristics of moyamoya disease in children
school-age onset. Eight children were female and six children intracranial collateral circulation. Therefore, in MMD patients
were male. Before the disease, crying and fatigue were the who require surgery, DSA still needs to be performed in order
incentives. It is noteworthy to mention that, in this study, five clearly examine these specific sites.
children developed upper respiratory tract infections before the
In this study, we performed conservative treatment for patients
onset of MMD; reminding us to determine whether infection is
with ischemia rather than surgical treatment. Conservative
the cause of the disease and which one is worth to be further
treatment is mainly symptomatic treatment. For patients with
discussed.
ischemia, capacity expansion, blood vessel expansion and
MMD can affect both children and adults, but MMD in intracraninal pressure lowering treatment should be given as
pediatric patients exhibits distinct clinical features, and the soon as possible (within a week, preferably within 24 h). If
treatment prognoses are different from adult patients. Children there are any infection factors, anti-infection treatment should
are the group at highest risk for MMD. In children, the disease be actively given. In recent years, surgical treatment has
mainly manifests as ischemia, while bleeding is the primary presented a good effect. Especially, the effectiveness of
symptom in adults [27].The onset age of the disease is mostly surgical revascularization for preventing ischemic stroke had
under 10 y old, and the average age is approximately 4.5 y old. been generally accepted by many studies [29]. It also has been
Japanese girls are more prone to this disease. In adults, cerebral reported that patients with hemorrhagic MMD had a much
hemorrhage is the main symptom; while cerebral ischemia is higher rate of rebleeding and poorer prognosis than those with
the initial symptom, which occurs in 95% of children. In this the ischemic type. Surgical revascularization procedures can
study, 21 month-old to 10 y old children accounted for 78.5%. improve cerebral perfusion and have a positive impact in
MRI revealed that 12 cases had cerebral ischemia, and two preventing rebleeding in patients with hemorrhagic MMD [30].
cases had cerebral hemorrhage; which is basically consistent However, in our study, the treatment conservatively for the
with that reported in Southeast Asia [28]. In this study, 12 of patient with the ischemic types has been proved effective.
14 patients had the onset with limb weakness or hemiplegia,
In conclusion, high-risk age of child MMD ranged between
which accounted for 85.7%. Among these 12 patients, 10
4-10 y old, which mostly manifested as transient cerebral
patients had repeated episodes, which accounted for 71.4%.
ischemic insults; and inducing factors were mostly upper
Five cases exhibited persistent hemiplegia at the beginning of
respiratory tract infections. We believe that genetic research for
the disease, prompting that hemiplegia is the most common
the susceptibility gene such as RNF213 would be more
clinical manifestation in children with MMD. Other
supportive to lead to the definitive diagnosis of moyamoya
manifestations are unclear vision, sensory disturbance,
disease in the future if the genetic analysis of such
headaches, epileptic seizure, and involuntary movement. These
susceptibility gene becomes generally available in each clinic.
prompt that limb weakness or hemiplegia, sensory disturbance,
and language barrier are the main manifestations of MMD in
children. Especially for patients with repetitive limb weakness References
or hemiplegia, timely cranial imageologic tests should be 1. Scott RM, Smith ER. Moyamoya disease and moyamoya
given. syndrome. N Engl J Med 2009; 360: 1226-1237.
DSA is the gold standard for the diagnosis of MMD, but it is 2. Takeuchi K, Shimizu K. Hypoplasia of the bilateral internal
an invasive test. At present, DSA has not been accepted by carotid arteries. Brain Nerve 1957; 9: 37-43.
most families of these diseased children. The application of 3. Suzuki J, Takaku A. Cerebrovascular moyamoya disease.
MRI and MRA provides a non-invasive diagnostic method for Disease showing abnormal net-like vessels in base of brain.
the vascular pathological examination of MMD. All 14 Arch Neurol 1969; 20: 288-299.
children received cranial MRI and MRA examinations, in 4. Ma J, Liu Y, Ma L, Huang S, Li H, You C. RNF213
which 12 cases were found to have cerebral ischemia changes, polymorphism and Moyamoya disease: A systematic
and two cases were found to have cerebral hemorrhage. MRA review and meta-analysis. Neurol India 2013; 61: 35-39.
revealed stenosis or occlusion in internal carotid artery, as well 5. Fukui M. Current state of study on moyamoya disease in
as in the anterior, middle and posterior cerebral arteries; and Japan. Surg Neurol 1997; 47: 138-143.
abnormalities in the anterior and middle cerebral arteries were 6. Killory BD, Gonzalez LF, Wait SD, Ponce FA,
the most common. Furthermore, smoke-like vessels mostly Albuquerque FC, Spetzler RF. Simultaneous unilateral
occurred in the basal ganglia region. Three children received moyamoya disease and ipsilateral dural arteriovenous
DSA examination, and the results were consistent with those fistula: case report. Neurosurgery 2008; 62: 1375-1376.
obtained by MRA. In this study, MRI combined with MRA
7. Fukui M. Guideline for the diagnosis and treatment of
examination can not only display vascular lesions, but also
spontaneous occlusion of the Circle of Willis (Moyamoya
show cerebral infarction, cerebromalacia, cerebral hemorrhage
Disease) of the Ministry of Health and Welfare, Japan. Clin
and cerebral atrophy; which is secondary to vascular lesions.
Neuro Surg 1997; 99: 238-240.
Furthermore, it is convenient, noninvasive, does not need a
8. Miao W, Zhao PL, Zhang YS, Liu HY, Chang Y, Ma J,
contrast agent, and is conducive to long-term follow-ups. Some
Huang QJ, Lou ZX. Epidemiological and clinical features
literatures have revealed that MRA examination has certain
of Moyamoya disease in Nanjing, China. Clin Neurol
limitations such as low spatial resolution, exaggeration of the
Neurosurg 2010; 112: 199-203.
extent of the vascular occlusion, and poor display of
Biomed Res 2018 Volume 29 Issue 6 1158
Wang/Wang/Zhao/Zhou/Chen/Zhang
9. Fukui M. Current state of study on moyamoya disease in infarctions due to Moyamoya disease. J Pediatr Endocrinol
Japan. Surg Neurol 1997; 47: 138-143. Metabol 2016; 29: 221-225.
10. Cho HJ, Jung YH, Kim YD, Nam HS, Kim DS, Heo JH. 21. Greco F, Castellano Chiodo D, Sorge A, Perrini S, Sorge G.
The different infarct patterns between adulthood-onset and Multiple arterial ischemic stroke in a child with moyamoya
childhood-onset moyamoya disease. J Neurol Neurosurg disease and Mycoplasma pneumoniae infection. Minerva
Psychiatry 2011; 82: 38-40. Pediatr 2006: 58: 63-68.
11. Baba T, Houkin K, Kuroda S. Novel epidemiological 22. Ueno M, Oka A, Koeda T, Okamoto R, Takeshita K.
features of moyamoya disease. J Neurol Neurosurg Unilateral occlusion of the middle cerebral artery after
Psychiatry 2008; 79: 900-904. varicella-zoster virus infection. Brain Develop 2002; 24:
12. Chiu D, Shedden P, Bratina P, Grotta JC. Clinical features 106-108.
of moyamoya disease in the United States. Stroke 1998; 29: 23. Wan M, Duan L. Recent progress in hemorrhagic
1347-1351. moyamoya disease. Br J Neurosurg 2015; 29: 189-191.
13. Hallemeier CL, Rich KM, Grubb RL, Chicoine MR, Moran 24. Kim JS. Moyamoya disease: epidemiology, clinical
CJ, Cross DT, Zipfel GJ, Dacey RG, Derdeyn CP. Clinical features, and diagnosis. J Stroke 2016; 18: 2-11.
features and outcome in North American adults with 25. Leea TH, Sungb SM, Chob HJ. Moyamoya disease initially
moyamoya phenomenon.Stroke 2006; 37: 1490-1496. manifesting as vascular parkinsonism. J Neurol Sci 2015;
14. Kraemer M, Heienbrok W, Berlit P. Moyamoya disease in 357: 412-413.
Europeans. Stroke 2008; 39: 3193-3200. 26. Shim KW, Park EK, Kim JS, Kim DS. Cognitive outcome
15. Inoue TK, Ikezaki K, Sasazuki T, Matsushima T, Fukui M. of pediatric moyamoya disease. J Korean Neurosurg Soc
Linkage analysis of moyamoya disease on chromosome 6. J 2015; 57: 440-444.
Child Neurol 2000; 15: 179-182. 27. Piao J, Wu W, Yang Z, Yu J. Research progress of
16. Guey S, Tournier-Lasserve E, Hervé D, Kossorotoff M. moyamoya disease in children. Int J Med Sci 2015; 12:
Moyamoya disease and syndromes: from genetics to 566-575.
clinical management. Appl Clin Genet 2015; 8: 49-68. 28. Morioka M, Hamada J, Todaka T, Yano S, Kai Y, Ushio Y.
17. Liu W, Morito D, Takashima S, Mineharu Y, Kobayashi H, High-risk age for rebleeding in patients with hemorrhagic
Hitomi T, Hashikata H, Matsuura N, Yamazaki S, Toyoda moyamoya disease: long-term follow-up study.
A, Kikuta K, Takagi Y, Harada KH, Fujiyama A, Herzig R, Neurosurgery 2003; 52: 1049-1054.
Krischek B, Zou L, Kim JE, Kitakaze M, Miyamoto S, 29. Kim T, Oh CW, Bang JS, Kim JE, Cho WS. Moyamoya
Nagata K, Hashimoto N, Koizumi A. Identification of disease: treatment and outcomes. J Stroke 2016; 18: 21-30.
RNF213 as a susceptibility gene for moyamoya disease and 30. Liu XJ, Zhang D, Wang S, Zhao YL, Teo M, Wang R, Cao
its possible role in vascular development. PLoS One 2011; Y, Ye X, Kang S, Zhao JZ. Clinical features and long-term
6: 22542. outcomes of moyamoya disease: a single-center experience
18. Bersano A, Guey S, Bedini G, Nava S, Herve D, Vajkoczy with 528 cases in China. J Neurosurg 2015; 122: 392-399.
P, Tatlisumak T, Sareela M, van der Zwan A, Klijn CJ,
Braun KP, Kronenburg A, Acerbi F, Brown MM, Calviere *Correspondence to
L, Cordonnier C, Henon H, Thines L, Khan N, Czabanka
M, Kraemer M, Simister R, Prontera P, Tournier-Lasserve Rui-Yun Zhang
E, Parati E, EuropeanMoyamoya Disease Initiative. Department of Pediatrics
Research progresses in understanding the pathophysiology
of moyamoya disease. Cerebrovasc Dis 2016; 41: 105-118. Qingdao Municipal Hospital
19. Kirkham FJ, Hogan AM. Risk factors for arterial ischemic PR China
stroke in childhood. CNS Spectr 2004; 9: 451-464.
20. Noh BH, Cho SW, Ahn SY. Simultaneous occurrence of
diabetic ketoacidosis, thyroid storm, and multiple cerebral
1159 Biomed Res 2018 Volume 29 Issue 6
Das könnte Ihnen auch gefallen
- Coronary Vasomotion AbnormalitiesVon EverandCoronary Vasomotion AbnormalitiesHiroaki ShimokawaNoch keine Bewertungen
- Understanding and Treating Moyamoya Disease in ChildrenDokument11 SeitenUnderstanding and Treating Moyamoya Disease in ChildrenFitriyana WinarnoNoch keine Bewertungen
- Moyamoya Disease: Current Concepts and Future Perspectives: ReviewDokument11 SeitenMoyamoya Disease: Current Concepts and Future Perspectives: ReviewThirumanjari KarthikeyanNoch keine Bewertungen
- BMC NeurologyDokument8 SeitenBMC NeurologyTarun MathurNoch keine Bewertungen
- MMD EpidDokument10 SeitenMMD EpidGilbert Sterling OctaviusNoch keine Bewertungen
- Moyamoya Epidemiology, Presentation, and DiagnosisDokument9 SeitenMoyamoya Epidemiology, Presentation, and DiagnosisshiloinNoch keine Bewertungen
- Interdisciplinary Neurosurgery: Advanced Techniques and Case ManagementDokument7 SeitenInterdisciplinary Neurosurgery: Advanced Techniques and Case ManagementMuhammad Fuad MahfudNoch keine Bewertungen
- Moyamoya Disease in ChildrenDokument13 SeitenMoyamoya Disease in ChildrenMiguelIbañezNoch keine Bewertungen
- The First Affiliated Hospital of Zhengzhou University, Nöroloji, Zhengzhou, ÇinDokument12 SeitenThe First Affiliated Hospital of Zhengzhou University, Nöroloji, Zhengzhou, ÇinwithoutlifeNoch keine Bewertungen
- Acute Ischemic Stroke in Pediatric Patients: Illustrative Teaching CaseDokument4 SeitenAcute Ischemic Stroke in Pediatric Patients: Illustrative Teaching CaseErick DjuandaNoch keine Bewertungen
- Epidemiology, Aetiology, and Management of IschaemicDokument12 SeitenEpidemiology, Aetiology, and Management of IschaemicKhairunNisaNoch keine Bewertungen
- 1212 Full PDFDokument9 Seiten1212 Full PDFChris KronzNoch keine Bewertungen
- Predictive Factors of Epilepsy in MMDDokument7 SeitenPredictive Factors of Epilepsy in MMDGilbert Sterling OctaviusNoch keine Bewertungen
- Stroke in Children: Eview RticleDokument11 SeitenStroke in Children: Eview RticleÁgnes GedőNoch keine Bewertungen
- 226-Article Text-717-3-10-20141213Dokument5 Seiten226-Article Text-717-3-10-20141213jasleen.jk92Noch keine Bewertungen
- A Decade of Management of Subdural Haematoma in Children Aged 2 To 24 Months Hospitalized at The Paediatric Neurosurgery Department of La Timone Children's HospitalDokument8 SeitenA Decade of Management of Subdural Haematoma in Children Aged 2 To 24 Months Hospitalized at The Paediatric Neurosurgery Department of La Timone Children's HospitalEditor IJTSRDNoch keine Bewertungen
- 2009 8 Focus09158Dokument5 Seiten2009 8 Focus09158ninostranoNoch keine Bewertungen
- Intacranial Complications of Chronic Suppurative Otitis Media, Ottico-Antral TypeDokument4 SeitenIntacranial Complications of Chronic Suppurative Otitis Media, Ottico-Antral TypeRio OktabyantoroNoch keine Bewertungen
- Aneurismas Cerebrais Na InfânciaDokument5 SeitenAneurismas Cerebrais Na Infânciaarlindodavila2010Noch keine Bewertungen
- Clinical Spectrum and Outcome of Cerebral Venous Sinus Thrombosis in ChildrenDokument4 SeitenClinical Spectrum and Outcome of Cerebral Venous Sinus Thrombosis in ChildrenDra. Carol Angélica Artigas GómezNoch keine Bewertungen
- Tumefactive Demyelinating Lesions: Nine Cases and A Review of The LiteratureDokument9 SeitenTumefactive Demyelinating Lesions: Nine Cases and A Review of The LiteraturePS NeuroNoch keine Bewertungen
- Cardiovascular Risk Factors in Childhood and Carotid Artery Intima-Media Thickness in AdulthoodDokument7 SeitenCardiovascular Risk Factors in Childhood and Carotid Artery Intima-Media Thickness in AdulthoodDharmanna RathodNoch keine Bewertungen
- Pathophysiology and Genetic Factors in Moyamoya DiseaseDokument6 SeitenPathophysiology and Genetic Factors in Moyamoya Diseasethomsoon01Noch keine Bewertungen
- Scientific Report Journal 22 NovDokument6 SeitenScientific Report Journal 22 Novnaresh kotraNoch keine Bewertungen
- ADEM Vs MS: A Diagnostic Dilemma - A Follow-Up Study.: Poster No.: Congress: Type: AuthorsDokument18 SeitenADEM Vs MS: A Diagnostic Dilemma - A Follow-Up Study.: Poster No.: Congress: Type: AuthorsJoeNoch keine Bewertungen
- Research Progress of Moyamoya Disease in ChildrenDokument10 SeitenResearch Progress of Moyamoya Disease in ChildrenClaudia JessicaNoch keine Bewertungen
- CM PediatricsDokument8 SeitenCM PediatricsZdravko HeinrichNoch keine Bewertungen
- Neurochirurgie MoyamoyaDokument8 SeitenNeurochirurgie MoyamoyaAnastasia UrsuNoch keine Bewertungen
- Risk Factors and Mechanisms of Stroke in Young Adults: The FUTURE StudyDokument11 SeitenRisk Factors and Mechanisms of Stroke in Young Adults: The FUTURE StudyRizka FebrianaNoch keine Bewertungen
- Review Article: Ischemic Stroke in Infants and Children: Practical Management in EmergencyDokument8 SeitenReview Article: Ischemic Stroke in Infants and Children: Practical Management in EmergencyEstela MachadoNoch keine Bewertungen
- Acute Necrotizing Encephalopathy of Childhood: Correlation of MR Findings and Clinical OutcomeDokument5 SeitenAcute Necrotizing Encephalopathy of Childhood: Correlation of MR Findings and Clinical OutcomeayubahriNoch keine Bewertungen
- MoyamoyaDokument11 SeitenMoyamoyaSubashssNoch keine Bewertungen
- Idiopathic Intracranial Hypertension: A Retrospective Clinical StudyDokument4 SeitenIdiopathic Intracranial Hypertension: A Retrospective Clinical StudyNouchan NoupNoch keine Bewertungen
- Strokeaha 118 021301Dokument6 SeitenStrokeaha 118 021301Rahma Nur AmeliaNoch keine Bewertungen
- Accepted Manuscript: Pediatric NeurologyDokument11 SeitenAccepted Manuscript: Pediatric Neurologyaria tristayanthiNoch keine Bewertungen
- Jurnal 1Dokument9 SeitenJurnal 1AnnisNoch keine Bewertungen
- A Case Series On Meningioma Based On Who Grading SystemDokument15 SeitenA Case Series On Meningioma Based On Who Grading SystemIJAR JOURNALNoch keine Bewertungen
- Retrospective Analysis of 49 Cases of Brain Abscess and Review of The LiteratureDokument11 SeitenRetrospective Analysis of 49 Cases of Brain Abscess and Review of The LiteraturenisaNoch keine Bewertungen
- Ictus en Joven Ferro2010Dokument12 SeitenIctus en Joven Ferro2010Mez RealNoch keine Bewertungen
- Tratamiento Quirúrgico Efectivo de Las Malformaciones Cavernosas Cerebrales - Un Estudio Multicéntrico de 79 Pacientes PediátricosDokument4 SeitenTratamiento Quirúrgico Efectivo de Las Malformaciones Cavernosas Cerebrales - Un Estudio Multicéntrico de 79 Pacientes PediátricosGonzalo Leonidas Rojas DelgadoNoch keine Bewertungen
- Otogenic Brain Abscess Our ExperienceDokument5 SeitenOtogenic Brain Abscess Our ExperienceNeysaAzaliaEfrimaisaNoch keine Bewertungen
- Intracranial Aneurysms in Childhood: 27-Year Single-Institution ExperienceDokument10 SeitenIntracranial Aneurysms in Childhood: 27-Year Single-Institution Experiencezrated786Noch keine Bewertungen
- Intracranial Aneurysms in Childhood - 27 - Year Sigle Institution ExperienceDokument10 SeitenIntracranial Aneurysms in Childhood - 27 - Year Sigle Institution ExperienceRony EvangelistaNoch keine Bewertungen
- Hsu2019 PDFDokument6 SeitenHsu2019 PDFrachmadyNoch keine Bewertungen
- Risk Factors and Outcome of Overt Stroke in Sickle Cell Patients Admitted in Two Reference Hospitals in Yaounde and DoualaDokument14 SeitenRisk Factors and Outcome of Overt Stroke in Sickle Cell Patients Admitted in Two Reference Hospitals in Yaounde and DoualaSam NickNoch keine Bewertungen
- 58 Iajps58122019 PDFDokument4 Seiten58 Iajps58122019 PDFiajpsNoch keine Bewertungen
- Vermeer 2002Dokument5 SeitenVermeer 2002MarkNoch keine Bewertungen
- Mineralizing Angiopathy With Infantile Basal GanglDokument8 SeitenMineralizing Angiopathy With Infantile Basal GanglakshayajainaNoch keine Bewertungen
- Craniopharyngioma: Analysis of Factors That Affect The OutcomeDokument5 SeitenCraniopharyngioma: Analysis of Factors That Affect The OutcomeRiri KumalaNoch keine Bewertungen
- Ophthalmological Findings in Children With EncephalitisDokument8 SeitenOphthalmological Findings in Children With EncephalitisSabila TasyakurNoch keine Bewertungen
- Risk Factors Association With Severity of White Matter Lesions On Magneticresonance Imaging 2327 5146 1000290Dokument7 SeitenRisk Factors Association With Severity of White Matter Lesions On Magneticresonance Imaging 2327 5146 1000290Ranganathan Rma IyerNoch keine Bewertungen
- 1 s2.0 S1092913420301374 MainDokument5 Seiten1 s2.0 S1092913420301374 MainNisha ChaaNoch keine Bewertungen
- Neurofibromatosis Tipo 1 y Gliomas de Vías Ópticas. Una Serie de 80 PacientesDokument7 SeitenNeurofibromatosis Tipo 1 y Gliomas de Vías Ópticas. Una Serie de 80 PacientesHanderson RamirezNoch keine Bewertungen
- Sphenoid Sinus Diseases - A Review of 1,442 PatientsDokument8 SeitenSphenoid Sinus Diseases - A Review of 1,442 PatientsMario NarváezNoch keine Bewertungen
- Ijoto2017 9650910 PDFDokument7 SeitenIjoto2017 9650910 PDFSeptia P. MayasariNoch keine Bewertungen
- Cvja 24 28 PDFDokument6 SeitenCvja 24 28 PDFvitriaNoch keine Bewertungen
- Duygu 2020Dokument4 SeitenDuygu 2020Aditya HendraNoch keine Bewertungen
- Central Pontine and Extrapontine Myelinolysis. A Systematic ReviewDokument8 SeitenCentral Pontine and Extrapontine Myelinolysis. A Systematic ReviewFernando Vazquez SSNoch keine Bewertungen
- Anti-N-methyl-D-aspartate Receptor (NMDAR) Encephalitis: A Series of Ten Cases From A University Hospital in MalaysiaDokument6 SeitenAnti-N-methyl-D-aspartate Receptor (NMDAR) Encephalitis: A Series of Ten Cases From A University Hospital in MalaysiaAbhishek KayalNoch keine Bewertungen
- 1 s2.0 S0165587617302975 Main PDFDokument4 Seiten1 s2.0 S0165587617302975 Main PDFAchmad YunusNoch keine Bewertungen
- Primary Cutaneous Adenoid Cystic Carcinoma A Case Report and Dermoscopic FndingsDokument3 SeitenPrimary Cutaneous Adenoid Cystic Carcinoma A Case Report and Dermoscopic FndingsRiya CassendraNoch keine Bewertungen
- Effects of Highquality Nursing On Puerpera With Pregnancy HypertensionDokument4 SeitenEffects of Highquality Nursing On Puerpera With Pregnancy HypertensionRiya CassendraNoch keine Bewertungen
- Preclinical Developmental Toxicity Testing and Advanced Invitro Stem Cell BasedsystemsDokument3 SeitenPreclinical Developmental Toxicity Testing and Advanced Invitro Stem Cell BasedsystemsRiya CassendraNoch keine Bewertungen
- The Effects of Resistance Elastic Bands Exercises On Salivary Iga and Salivary Cortisol Levels in Elderly WomenDokument6 SeitenThe Effects of Resistance Elastic Bands Exercises On Salivary Iga and Salivary Cortisol Levels in Elderly WomenRiya CassendraNoch keine Bewertungen
- Clinical Effect of Atorvastatintrimetazidine Combined Treatment of Coronary Heart DiseaseDokument4 SeitenClinical Effect of Atorvastatintrimetazidine Combined Treatment of Coronary Heart DiseaseRiya CassendraNoch keine Bewertungen
- A Brief Insight Into The Role of Image Fusion in OncologyDokument2 SeitenA Brief Insight Into The Role of Image Fusion in OncologyRiya CassendraNoch keine Bewertungen
- A Case of Virilization and Bilateral Krukenberg Tumours in Late PregnancyDokument4 SeitenA Case of Virilization and Bilateral Krukenberg Tumours in Late PregnancyRiya CassendraNoch keine Bewertungen
- A Case of Inverted Follicular Keratosis With Onset Since ChildhoodDokument2 SeitenA Case of Inverted Follicular Keratosis With Onset Since ChildhoodRiya CassendraNoch keine Bewertungen
- The Threat of Carbapenemresistant Hypervirulent Klebsiella Pneumoniae CRHVKPDokument4 SeitenThe Threat of Carbapenemresistant Hypervirulent Klebsiella Pneumoniae CRHVKPRiya CassendraNoch keine Bewertungen
- High Dietary Diversity Is Associated With Child Obesity in Iranian School Children An Evaluation of Dietary Diversity ScoreDokument6 SeitenHigh Dietary Diversity Is Associated With Child Obesity in Iranian School Children An Evaluation of Dietary Diversity ScoreRiya CassendraNoch keine Bewertungen
- The Evaluation and Effect of Mental Health of Students Based On Ideological and Political Education InterventionDokument6 SeitenThe Evaluation and Effect of Mental Health of Students Based On Ideological and Political Education InterventionRiya CassendraNoch keine Bewertungen
- Potential Role of A Recentlydiscovered Biologic HDFX in Prevention Andtreatment of Deadly Communicable Diseases Brought To WesternDokument5 SeitenPotential Role of A Recentlydiscovered Biologic HDFX in Prevention Andtreatment of Deadly Communicable Diseases Brought To WesternRiya CassendraNoch keine Bewertungen
- Severe Septic Complications in A Diabetic Foot Decade After Multiple Injections of A Modeling AgentDokument5 SeitenSevere Septic Complications in A Diabetic Foot Decade After Multiple Injections of A Modeling AgentRiya CassendraNoch keine Bewertungen
- The Efficacy of Tdcs in The Treatment of Migraine A ReviewDokument8 SeitenThe Efficacy of Tdcs in The Treatment of Migraine A ReviewRiya CassendraNoch keine Bewertungen
- The Effects of Zhikang Capsule On The Growth and Apoptosis of Breast Cancer Mcf7Dokument4 SeitenThe Effects of Zhikang Capsule On The Growth and Apoptosis of Breast Cancer Mcf7Riya CassendraNoch keine Bewertungen
- Initial Serum Level of Il10 As An Outcome Predictor in Children With Sepsis PDFDokument5 SeitenInitial Serum Level of Il10 As An Outcome Predictor in Children With Sepsis PDFRiya CassendraNoch keine Bewertungen
- Initial Serum Level of TNF As An Outcome Predictor in Pediatric Patient With SepsisDokument6 SeitenInitial Serum Level of TNF As An Outcome Predictor in Pediatric Patient With SepsisRiya CassendraNoch keine Bewertungen
- Application of Tar Signature For Breast Mass AnalysisDokument5 SeitenApplication of Tar Signature For Breast Mass AnalysisRiya CassendraNoch keine Bewertungen
- Longterm Complications of Modified Soave Radical Correction in The Treatment of Hirschsprungs Disease and Its Influences On Life QDokument4 SeitenLongterm Complications of Modified Soave Radical Correction in The Treatment of Hirschsprungs Disease and Its Influences On Life QRiya CassendraNoch keine Bewertungen
- Psychological Trauma of Primary Hypertension and The Best Treating ChoiceDokument6 SeitenPsychological Trauma of Primary Hypertension and The Best Treating ChoiceRiya CassendraNoch keine Bewertungen
- Factors Contributing To Nonadherence To Insulin Therapy Among Type 1 and Type2 Diabetes Mellitus Patients in Asser Region Saudi ArDokument6 SeitenFactors Contributing To Nonadherence To Insulin Therapy Among Type 1 and Type2 Diabetes Mellitus Patients in Asser Region Saudi ArRiya CassendraNoch keine Bewertungen
- Salicylic Acid Mediated Salt Tolerance at Different Growth Stages of Oryza Sativa L and Its Effect On Salicylic Acid BioDokument18 SeitenSalicylic Acid Mediated Salt Tolerance at Different Growth Stages of Oryza Sativa L and Its Effect On Salicylic Acid BioRiya CassendraNoch keine Bewertungen
- The Factors Affecting Morbidity and Mortality in Spontaneous Intracerebral HematomasDokument5 SeitenThe Factors Affecting Morbidity and Mortality in Spontaneous Intracerebral HematomasRiya CassendraNoch keine Bewertungen
- Uptake of As CD Cu Fe MN PB and ZN in Pasture Grasses On Three Metalcontaminated Soils From MontanaDokument7 SeitenUptake of As CD Cu Fe MN PB and ZN in Pasture Grasses On Three Metalcontaminated Soils From MontanaRiya CassendraNoch keine Bewertungen
- Depression and Determinant Factors Among Elderly in IndiaDokument2 SeitenDepression and Determinant Factors Among Elderly in IndiaRiya CassendraNoch keine Bewertungen
- Pulmonary Hypertension in Pulmonary Agenesisa Report of Five Pediatric Cases and Review of Previous CasesDokument5 SeitenPulmonary Hypertension in Pulmonary Agenesisa Report of Five Pediatric Cases and Review of Previous CasesRiya CassendraNoch keine Bewertungen
- A Noble Approach To Compute The Magnetic Flux Density Magnetic Forcedistribution and Its Application On Magnetic LevitationDokument8 SeitenA Noble Approach To Compute The Magnetic Flux Density Magnetic Forcedistribution and Its Application On Magnetic LevitationRiya CassendraNoch keine Bewertungen
- An Analysis of The Impact of Reference Groups On Collectivist Families Mealsocial Interaction Behaviour in Sierra LeoneDokument12 SeitenAn Analysis of The Impact of Reference Groups On Collectivist Families Mealsocial Interaction Behaviour in Sierra LeoneRiya CassendraNoch keine Bewertungen
- Retrospective Study of Cholangiocarcinomas Diagnosed in The Hospital of Fuenlabrada in The Period 20062016Dokument3 SeitenRetrospective Study of Cholangiocarcinomas Diagnosed in The Hospital of Fuenlabrada in The Period 20062016Riya CassendraNoch keine Bewertungen
- Central Retinal Vein Occlusion Differential DiagnosisDokument12 SeitenCentral Retinal Vein Occlusion Differential Diagnosismina2085Noch keine Bewertungen
- Appendix A: Doppler Ultrasound and Ankle-Brachial Pressure IndexDokument26 SeitenAppendix A: Doppler Ultrasound and Ankle-Brachial Pressure IndexabigailNoch keine Bewertungen
- Exam MCQ Clinanatomy 2022-23Dokument21 SeitenExam MCQ Clinanatomy 2022-23CHoudhary Hassan WarraichNoch keine Bewertungen
- 1 - Cardiac Output FINALDokument9 Seiten1 - Cardiac Output FINALNiruja Sri100% (1)
- CH 3 Hemodynamic Disorders, Thromboembolic Disease,: A. CongestionDokument11 SeitenCH 3 Hemodynamic Disorders, Thromboembolic Disease,: A. Congestion賴宥瑄Noch keine Bewertungen
- HEART Grade 9Dokument3 SeitenHEART Grade 9Hansel MusimaNoch keine Bewertungen
- Unusual Presentation of May-Thurner SyndromeDokument5 SeitenUnusual Presentation of May-Thurner SyndromeJ. Ruben HermannNoch keine Bewertungen
- Circulatory System - BiologyDokument11 SeitenCirculatory System - BiologyAmanda AllenNoch keine Bewertungen
- Raynaud'S Disease AND Buerger'S Disease: By: Joy-Rena S. Ochondra BSN Ii-ADokument29 SeitenRaynaud'S Disease AND Buerger'S Disease: By: Joy-Rena S. Ochondra BSN Ii-Ajoyrena ochondraNoch keine Bewertungen
- Anatomy of The Mediastinum CXRDokument26 SeitenAnatomy of The Mediastinum CXRHassan AliNoch keine Bewertungen
- NSSBIO3E SB1B Ch08 e PDFDokument60 SeitenNSSBIO3E SB1B Ch08 e PDFr6 obiNoch keine Bewertungen
- Chapter 3 f3Dokument101 SeitenChapter 3 f3Ghanapathi RamanathanNoch keine Bewertungen
- Why Do We Measure Coronary Artery Calcium Score?Dokument6 SeitenWhy Do We Measure Coronary Artery Calcium Score?eugeniaNoch keine Bewertungen
- Cap 5 - Monitorización CardiovascularDokument53 SeitenCap 5 - Monitorización CardiovascularMonserrath ReséndizNoch keine Bewertungen
- Lymphoid Tissue Common Notes Part 1Dokument31 SeitenLymphoid Tissue Common Notes Part 1Mace DueñasNoch keine Bewertungen
- CardioDokument6 SeitenCardioGrace GurdielNoch keine Bewertungen
- Cardiovascular Surgery in The Elderly: Salim and LDokument19 SeitenCardiovascular Surgery in The Elderly: Salim and LThanh BinhNoch keine Bewertungen
- Arteries of AbdomenDokument3 SeitenArteries of Abdomenmero1983Noch keine Bewertungen
- RRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRDokument2 SeitenRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRRSaginesh MkNoch keine Bewertungen
- PCI Vs CABG (Final)Dokument44 SeitenPCI Vs CABG (Final)AnindyaSarkar100% (1)
- The Cardiovascular System: Elaine N. MariebDokument151 SeitenThe Cardiovascular System: Elaine N. Mariebwhiskers qtNoch keine Bewertungen
- Chest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsDokument16 SeitenChest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsJose AnaconaNoch keine Bewertungen
- WOC CaseDokument4 SeitenWOC Casedwi adindaNoch keine Bewertungen
- ESC Guidelines On The Diagnosis and Treatment of Peripheral Artery DiseasesDokument56 SeitenESC Guidelines On The Diagnosis and Treatment of Peripheral Artery DiseasesJuan José Ruiz CastilloNoch keine Bewertungen
- Mp1 Biomedicalines Marketing: To: Quality Medical TradingDokument4 SeitenMp1 Biomedicalines Marketing: To: Quality Medical TradingJanna FabiaNoch keine Bewertungen
- Open Access Atlas of Otolaryngology, Head & Neck Operative SurgeryDokument13 SeitenOpen Access Atlas of Otolaryngology, Head & Neck Operative Surgeryhusdfadfg adfsadfsNoch keine Bewertungen
- Correct Answer: 4. Premedicate The Client With An Analgesic Before AmbulatingDokument49 SeitenCorrect Answer: 4. Premedicate The Client With An Analgesic Before AmbulatingPortage ExamsNoch keine Bewertungen
- Oberoi International School Teacher's Name : Shobi Nandkeolyar Class : GR 9 Biology Student's Name : Parashie Sidhwani Date : 15/04/20Dokument44 SeitenOberoi International School Teacher's Name : Shobi Nandkeolyar Class : GR 9 Biology Student's Name : Parashie Sidhwani Date : 15/04/20Parashie SidhwaniNoch keine Bewertungen
- Laporan Sistem SirkulasiDokument10 SeitenLaporan Sistem SirkulasiRosa AmaliaNoch keine Bewertungen
- Acute Chest PainDokument103 SeitenAcute Chest PainYajjat GargNoch keine Bewertungen
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (81)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Noch keine Bewertungen
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Breaking the Habit of Being YourselfVon EverandBreaking the Habit of Being YourselfBewertung: 4.5 von 5 Sternen4.5/5 (1459)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 3.5 von 5 Sternen3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Peaceful Sleep Hypnosis: Meditate & RelaxVon EverandPeaceful Sleep Hypnosis: Meditate & RelaxBewertung: 4.5 von 5 Sternen4.5/5 (142)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipVon EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipBewertung: 4.5 von 5 Sternen4.5/5 (1135)
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissVon EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissBewertung: 4.5 von 5 Sternen4.5/5 (82)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (4)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)