Beruflich Dokumente
Kultur Dokumente
Nature 1
Hochgeladen von
Natàlia PadillaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nature 1
Hochgeladen von
Natàlia PadillaCopyright:
Verfügbare Formate
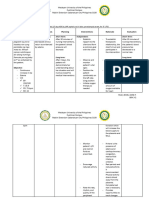
REVIEWS
SGLT2 inhibition — a novel strategy
for diabetes treatment
Edward C. Chao and Robert R. Henry
Abstract | Inhibiting sodium–glucose co-transporters (SGLTs), which have a key role in the
reabsorption of glucose in the kidney, has been proposed as a novel therapeutic strategy
for diabetes. Genetic mutations in the kidney-specific SGLT2 isoform that result in benign
renal glycosuria, as well as preclinical and clinical studies with SGLT2 inhibitors in type 2
diabetes, support the potential of this approach. These investigations indicate that elevating
renal glucose excretion by suppressing SGLT2 can reduce plasma glucose levels, as well as
decrease weight. Although data from ongoing Phase III trials of these agents are needed to
more fully assess safety, results suggest that the beneficial effects of SGLT2 inhibition might
be achieved without exerting significant side effects — an advantage over many current
diabetes medications. This article discusses the role of SGLT2 in glucose homeostasis and the
evidence available so far on the therapeutic potential of blocking these transporters in
the treatment of diabetes.
Sodium-glucose
The aetiology of type 2 diabetes mellitus (T2DM) is intri‑ to the sustained elevated serum glucose levels observed
co-transporters cate and multifaceted, but virtually all patients contend in individuals with diabetes, as they have an increased
(SGLTs). A family of membrane with both relative insulin deficiency and insulin resist‑ capacity for renal glucose reabsorption5. Inhibiting this
proteins that transport glucose, ance to varying degrees. The resulting hyperglycaemia glucose reabsorption, thereby allowing its excretion in
as well as some ions, vitamins
can facilitate β‑cell failure in the pancreas and worsen the urine (glycosuria), is therefore emerging as a potential
and amino acids across the
brush-border membrane of insulin resistance, thus triggering a cycle of impaired new approach to the treatment of diabetes. Glycosuria,
the proximal convoluted metabolism and glucotoxicity 1. Glucotoxicity can con‑ however, has historically been perceived as a sign of met‑
tubules in the kidney and tribute to increased apoptosis of β‑cells, causing dimin‑ abolic decompensation and of adverse clinical sequelae.
epithelial cells in the intestine.
ished β‑cell mass and thus reduced gene transcription, Therefore, utilizing this manifestation as a therapeutic
synthesis and secretion of insulin2. strategy for diabetes represents a paradigm shift.
The use of current agents for T2DM is often limited Sodium–glucose co-transporters (SGLTs) are responsible
by their potential to induce significant adverse effects. for renal glucose reabsorption, with SGLT2 performing
For instance, metformin can cause gastrointestinal effects most of this task and the remainder by SGLT1 (Ref. 6).
such as diarrhoea and nausea, and rarely, lactic acidosis, The development of inhibitors targeted against SGLTs
whereas sulphonylureas or insulin can induce hypogly‑ grew out of experiments with the compound phlorizin,
caemia as well as weight gain3. Thiazolidinedione use which was first isolated in the 1800s and was found to
is also associated with weight gain and oedema3. Newer improve blood glucose levels in laboratory animals. This
Section of Endocrinology, drugs, such as the incretin mimetics, may produce nausea, is in addition to observations in patients who had a rare
Metabolism and Diabetes, vomiting and diarrhoea4. Glycaemic control can be dif‑ genetic abnormality in these transporters, those with a
VA San Diego Healthcare ficult to attain, even with a combination of multiple condition termed familial renal glycosuria6.
System and University of
oral agents, and with insulin added. Thus, the quest to As SGLT2 inhibitors do not target the major patho‑
California, San Diego School
of Medicine, 3350 La Jolla develop therapeutic agents with novel mechanisms of physiological defects in T2DM — namely insulin resist‑
Village Drive, 111 G San action without these side effects continues. ance and impaired insulin secretion — they represent
Diego, California 92161, The kidney has a key role in regulating glucose levels a potentially promising new option in the treatment of
USA. — by mediating the reabsorption of glucose back into the diabetes. This Review will provide an overview of the
Correspondence to E.C.C.
e-mail: edward.chao@va.gov
plasma — following filtration of the blood; this is a crucial function of the kidney in glucose homeostasis, focusing
doi:10.1038/nrd3180 evolutionary adaptation to maintaining glucose homeo‑ on the pivotal role of SGLT2: its unique mechanism, as
Published online 28 May 2010 stasis and to retaining calories. This process contributes well as its development as a novel therapeutic target for
NATuRe RevIewS | Drug Discovery voLuMe 9 | juLy 2010 | 551
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
diabetes. Currently available preclinical and clinical data interplay of numerous regulatory processes (fIG. 2).
Familial renal glycosuria
A genetic disorder of the renal
on SGLT2 inhibitors in the treatment of T2DM will be Glucose uptake by the central nervous and peripheral
tubules characterized by discussed. tissues is matched by glucose production, which is pri‑
persistent isolated glycosuria marily mediated by the liver and to a lesser degree by the
without hyperglycaemia. Glucose transport in the kidney kidney 10. The kidney also serves a unique function in
The disorder results from
mutations in SLC5A2, the gene
Cell membranes, which are composed of lipids, are glucose homeostasis through filtration and reabsorption
encoding sodium–glucose impermeable to glucose, a polar compound. Therefore, of glucose. under normal circumstances, approximately
co-transporter 2. the transport of glucose across the cell membrane 180 g of glucose per day is freely filtered and essentially
requires the assistance of carrier proteins located within completely reabsorbed by the kidney, thus contributing
the cell membrane. once plasma glucose has been filtered to maintaining this balance12 (fIG. 3). The filtered load of
in the kidney by the glomeruli, it is reabsorbed by the glucose is the product of the plasma glucose concentra‑
SGLTs across the apical or luminal membranes of the tion and the glomerular filtration rate. So, as the plasma
epithelial cells of the proximal tubule, coupling the trans‑ concentration of glucose increases, the filtered load of
port of sodium with that of glucose (fIG. 1). glucose increases in a linear manner. when the plasma
SGLT2 and SGLT1 actively transport glucose across glucose concentration is greater than ~200 mg per 100 ml,
the proximal convoluted tubule (PCT) cells of the kidney all of the filtered glucose is reabsorbed, as the reabsorp‑
with varying capacities7 (TABLe 1). SGLT2 is a high‑capacity, tive capacity of the SGLTs is not yet saturated. In other
low‑affinity transporter found mainly in the S1 segment words, the threshold for glucose excretion has not been
of the PCT8. SGLT2 is thought to account for approxi‑ reached (please refer to fIG. 4 for a graphical depiction)12.
mately 90% of reabsorbed glucose and its expression is The reabsorption curve is no longer linear at a plasma
limited to the kidney. By contrast, SGLT1, a low‑capacity, glucose concentration of ~200–250 mg per 100 ml, as, at
high‑affinity transporter, is situated in the more distal this point, the co‑transporters are approaching saturation.
S2/S3 segment of the PCT and reabsorbs the remaining Some of the filtered glucose is therefore not reabsorbed,
percentage of the filtered glucose9,10. SGLT2 catalyses the but is excreted. Filtered glucose is reabsorbed in the
active transport of glucose against a concentration gradi‑ PCT, and healthy people do not exceed the maximum
ent across the apical (luminal) membrane by coupling amount of glucose that can be reabsorbed (the tubular
it with the transport of sodium10,11 (fIG. 1). The inward maximum or Tmax), which, on average, is approximately
sodium gradient across the luminal epithelium is main‑ 375 mg per min12 (fIG. 4). when the filtered glucose load
tained by ATP‑driven active extrusion of sodium across surpasses the Tmax, the glucose excretion rate increases
the anti‑luminal surface into the blood8,9. Intracellular linearly and parallels the curve for filtered load. Both the
glucose diffuses passively out of the cell, down a concen‑ reabsorption and excretion curves, by contrast, exhibit
tration gradient and across the anti‑luminal membrane nonlinear shapes as the glucose Tmax is approached. This
into the intercellular space — which is in equilibrium loss of linearity represents the threshold occurring at a
with the blood — by basolateral (anti‑luminal) glucose lower plasma glucose concentration than the Tmax, and is
transporter type 2 (GLuT2; also known as SLC2A2) termed splay 12. There are two reasons for splay: first, all
and GLuT1 (also known as SLC2A1) facilitative glucose nephrons do not have the same Tmax, and nephrons with
transporters11. a lower Tmax excrete glucose in the urine before those
Plasma glucose concentrations are normally main‑ with a higher Tmax (Ref. 12). Second, as the affinity of the
tained within a narrow range, which is crucial for organs SGLT is low, if a glucose molecule becomes unattached
such as the brain, which uses glucose almost exclusively from its carrier, it will probably be excreted in the urine,
as its energy source. This balance involves the complex even if there are unoccupied binding sites remaining
on the co‑transporters10. Thus, any amount of filtered
glucose exceeding the Tmax is excreted and appears as
Lumen Blood glucose in the urine.
Glucose GLUT2 Glucose Potential of SGLT inhibition in treating diabetes
The high plasma glucose levels that are characteristic
Na+ and Na+ of uncontrolled T2DM exceed the maximum threshold
S1 proximal
glucose at 1:1 SGLT2
tubule of glucose reabsorption, saturating the SGLT receptors,
stoichiometry Glucose and resulting in the increased excretion of glucose in the
urine5. Patients with T2DM also express a significantly
K+
Na+ ATPase
Na+ higher number of SGLT2 and GLuT2 than healthy
individuals, as shown by a preclinical study of cultured
PCT cells taken from human patients9. Renal glucose
Figure 1 | sgLT2 mediates glucose reabsorption in the kidney. Sodium–glucose
uptake is also greatly elevated in these cells taken from
co-transporter 2 (SGLT2) catalyses the active transport of glucose (against a
concentration gradient) across the luminal membrane by coupling it with the downhill
subjects with T2DM9. Patients with T2DM also face the
Nature Reviews | Drug Discovery
transport of Na+. The inward Na+ gradient across the luminal epithelium is maintained effects of the hyperglycaemic state, which further worsen
by active extrusion of Na+ across the basolateral (anti-luminal) surface into the insulin deficiency and insulin resistance. The resultant
intercellular fluid, which is in equilibrium with the blood. Glucose passively diffuses out glucotoxicity can elevate the risk of developing long‑
of the cell down a concentration gradient by basolateral facilitative transporters: term complications, including microvascular disease
glucose transporter type 2 (GLUT2) and GLUT1. (such as neuropathy, nephropathy and retinopathy) as
552 | juLy 2010 | voLuMe 9 www.nature.com/reviews/drugdisc
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
Table 1 | A comparison of selected characteristics of SGLT1 and SGLT2 diabetes had been induced by partial pancreatectomy
— with controls. using euglycaemic hyperinsulinaemic
sgLT1 sgLT2 clamp studies, phlorizin was found to normalize insulin
site Mostly small intestine, some Almost exclusively kidney sensitivity in these diabetic rats, but did not influence
in kidney and heart insulin action in controls16. Administration of phlorizin
renal location Late proximal straight tubule Early proximal convoluted resulted in glycosuria, which normalized both the fasting
(S3 segment) tubule (S1 segment) and fed plasma glucose levels and completely reversed
Affinity for glucose High (Km = 0.4 mM) Low (Km = 2mM) insulin resistance. when phlorizin was discontinued,
capacity for glucose Low High hyperglycaemia and insulin resistance recurred. This
transport study was the first demonstration that hyperglycaemia
alone can lead to the development of insulin resistance
Percent of renal ~10% ~90%
glucose reabsorption via glucotoxicity. Phlorizin was used in multiple subse‑
quent investigations that helped to establish that hyper‑
SGLT, sodium–glucose co-transporter. Data from Ref. 11.
glycaemia contributes to the insulin resistance that
characterizes T2DM17.
well as macrovascular disease (such as cardiovascular, Although studies revealed that phlorizin administered
cerebral and peripheral vascular disease)13. uncontrolled orally to mice blunted the increase in blood glucose lev‑
hyperglycaemia is tightly linked to polyuria and glyco‑ els after ingesting a glucose solution, it was not further
suria, and contributes to both the pathophysiology and developed as a possible anti‑diabetes therapy due to poor
complications of T2DM. Although both unchecked intestinal absorption and resultant low bioavailability, as
hyperglycaemia and the therapeutic blockade of renal well as rapid in vivo β‑glucosidase degradation15. Another
glucose reabsorption share the manifestation of glyco‑ significant disadvantage is that phlorizin also acts on
suria, only SGLT2 inhibition involves lowering of the SGLT1, which is mainly expressed in the gastrointestinal
renal glucose excretion threshold, which functions to tract. SGLT1 gene mutations lead to glucose and galac‑
reduce the level of hyperglycaemia. tose malabsorption, dehydration, and diarrhoea15. A third
Suppressing glucose reabsorption, through blockade of drawback is when phlorizin is hydrolysed in the gut, phlo‑
SGLT, would increase urinary glucose excretion, thereby retin is produced, which inhibits facilitative glucose trans‑
reducing plasma glucose levels and potentially offering porters, such as GLuT1 (Ref. 15). Suppression of intestinal
a novel therapeutic strategy, without the adverse effects GLuT1 impairs intestinal transport of glucose and results
that accompany currently available agents for T2DM. in gastrointestinal side effects, such as diarrhoea. This and
one concern with inhibiting glucose reabsorption and other studies fuelled the search for a phlorizin derivative
inducing glycosuria is a possible deleterious effect on that would minimize these shortcomings.
kidney function, resulting in excessive water loss in the
urine and dehydration. However, in individuals with Early agents. Given that phlorizin lacked specificity for
familial renal glycosuria, an autosomal genetic disorder SGLT2 and was associated with substantial side effects,
that leads to impaired function of SGLT2, renal function efforts were made to develop new compounds to inhibit
remains normal, even when greater than 50 g of glucose SGLT2 with high potency and selectivity. other aims
is lost in the urine each day 14. This suggests that even included optimizing bioavailability through enhanced
long‑term impairment of SGLT function does not cause stability, and improving safety profiles. The first orally
significant adverse renal effects (see the Safety section available phlorizin derivative reported was T‑1095
below for further discussion of this disorder). (fIG. 5a). Preclinical studies on this agent confirmed the
Investigating the inhibition of SGLT could both fur‑ initial evidence that inhibition of renal SGLTs could be a
ther advance our continually evolving understanding of viable target for therapy in diabetes. Although this com‑
diabetes, as well as the clinical application of this knowl‑ pound was more metabolically stable than phlorizin,
edge in patients with this disorder. Given the potential it too was nonselective18. T‑1095 was not developed
of this novel therapeutic strategy, several SGLT inhibi‑ further, so no clinical data are available for this agent.
tors have been discovered and developed in recent years. Subsequently, sergliflozin and remogliflozin (fIG. 5a),
Late‑stage clinical trials are now in progress that could which possessed greater SGLT2 selectivity, were tested
clarify the efficacy and safety of this approach in large and sergliflozin progressed to clinical trials.
numbers of patients. In a placebo‑controlled study of 18 subjects, treatment
with sergliflozin for 14 days produced sustained suppres‑
Development of SGLT2 inhibitors sion of renal glucose reabsorption and a dose‑related
Phlorizin. Phlorizin (fIG. 5a) has played a vital role in glycosuria. A dose‑related reduction in body weight
elucidating the mechanism of renal glucose reabsorp‑ was also observed over the study period, with mean
tion and the role of hyperglycaemia in diabetes. This changes of –0.09 (placebo), –1.55 (500 mg sergliflozin)
agent was first isolated in 1835 by French chemists from and –1.74 kg (1,000 mg sergliflozin) from baseline19.
the root bark of the apple tree, and was subsequently Remogliflozin also induced a dose‑dependent increase
found to be a potent but relatively nonselective inhibi‑ in urinary glucose excretion, and lowered fasting plasma
tor of both SGLT2 and SGLT1 (Ref. 15). Rossetti and his glucose levels as well as glycated haemoglobin (HbA1c)
team compared the effects of phlorizin on blockade of levels in mice and rats 20. For reasons not entirely
renal glucose reabsorption in diabetic rats — in which known, but most probably related at least in part to their
NATuRe RevIewS | Drug Discovery voLuMe 9 | juLy 2010 | 553
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
development can be found using the ClinicalTrials.gov
Glucagon Insulin Insulin identifiers listed in TABLe 2. Structures of some of the
SGLT2 inhibitors under development have been dis‑
Fat
closed and these can be seen in fIG. 5b.
Pancreas
+ – +
Dapagliflozin. Dapagliflozin (developed by Bristol‑Myers
Squibb and AstraZeneca), which is the furthest advanced
Liver compound in development in the SGLT2 inhibitor class, is
currently in Phase III trials as a once‑daily, oral treatment
90 mg per for T2DM (TABLe 2). A C‑aryl glucoside linkage found
Skeletal
100 ml muscle in dapagliflozin confers resistance to degradation in the
gastrointestinal tract by β‑glucosidase enzymes21 (fIG. 5b).
Consequently, dapagliflozin can be administered orally in
Fasting plasma an unmodified form, therefore carrying a more favour‑
Kidney glucose able pharmacokinetic profile than the earlier agents. In
addition, it is approximately 1,200‑times more selective
Figure 2 | Normal glucose homeostasis. This outlines the hormonal interactions for SGLT2 over SGLT1. An in vitro study revealed that
that are important in regulating normal glucose homeostasis. Normal fasting glucose
dapagliflozin exhibited around 30‑times greater potency
homeostasis involves the hormonal regulation of glucose Nature Reviews
utilization | Drug Discovery
and production,
as well as the filtration and reabsorption of glucose by the kidney10. Under basal against SGLT2 in humans than phlorizin, and approxi‑
conditions, glucose uptake by the tissues is matched by glucose production from mately 4‑fold less potency versus phlorizin against human
the liver; this enables fine regulation of glucose at a fixed level. Gluconeogenesis in the SGLT1 (Ref. 22).
liver helps prevent hypoglycaemia. In the rat, dapagliflozin administration resulted in an
acute increase in glycosuria, unaccompanied by hypogly‑
caemia21,22. In Zucker diabetic fatty rats, a doubling of
urine glucose levels was noted with all doses of dapagli‑
pharmacokinetic profiles, and possibly also due to flozin compared with vehicle22. Fasting and postprandial
an unfavourable efficacy and side‑effect profile, these glucose levels decreased, concomitant with the glycosuria.
agents did not undergo further development. Indeed, Similarly, fasting glucose was reduced in streptozocin‑
both sergliflozin and remogliflozin contain o‑glucoside induced diabetic rats following administration of a
linkages that render them susceptible to hydrolysis by single dose of dapagliflozin22. Such declines in fasting
β‑glucosidase enzymes in the gastrointestinal tract. glucose levels were sustained in Zucker diabetic fatty rats
after 15 days of repeated dosing of dapagliflozin. This
Agents currently under development and other preclinical studies suggested a potential novel
Although there are several SGLT2 inhibitors now in strategy of treating hyperglycaemia through a mecha‑
various stages of clinical development (TABLe 2), for many nism that did not directly affect insulin secretion or its
of these agents there is currently little published data actions. These observations of efficacy in animal models
available. Nevertheless, several clinical studies of dapagli‑ led to further clinical investigations in humans.
flozin, which is now in Phase III trials, have been pub‑ Komoroski and colleagues conducted the first clinical
lished and therefore can be discussed. Preliminary trial studies that evaluated the safety, pharmacokinetic and
data for canagliflozin are also accessible and are summa‑ pharmacodynamic parameters of single and multiple
rized below. Limited information for other agents under doses of dapagliflozin in healthy individuals23. In the
single‑ascending dose study, a single dose of 2.5 mg,
5 mg, 10 mg, 20 mg, 50 mg, 100 mg, 250 mg or 500 mg of
SGLT2 dapagliflozin, or placebo was randomly assigned. Subjects
were then enrolled at the next higher dose if results from
Glucose
the first trial indicated that dapagliflozin was safe and well
S1 segment tolerated in at least six subjects. The multiple‑ascending
of proximal dose study was similarly designed, with the administra‑
tubule tion of five sequential doses of 2.5 mg, 10 mg, 20 mg,
50 mg or 100 mg of dapagliflozin, or placebo. Doses
Collecting SGLT1 Distal S2/S3
duct segment
~90% reabsorption of 20–50 mg per day of dapagliflozin produced near‑
of proximal maximal SGLT2 blockade (a glucose excretion of up to
~10% reabsorption
tubule ~3 g per hour and ~60 g per day) for at least 24 hours.
The glycosuria observed was sustained, dose‑dependent,
and did not cause hypoglycaemia in these subjects. Renal
glucose reabsorption was inhibited by approximately
20–30% on day 1 and approximately 16–50% on day 14.
No glucose To define the entire dose–response curve for patients
Figure 3 | renal handling of glucose in a non-diabetic individual. Virtually all the with T2DM, Komoroski and colleagues examined quan‑
glucose filtered is reabsorbed, and none appears in the urine. The locations for tities of dapagliflozin up to 100 mg in a randomized,
sodium–glucose co-transporter 2 (SGLT2) and SGLT1 are shown. Adapted from Ref. 12. double‑blind Phase II clinical trial of 47 individuals24.
Nature Reviews | Drug Discovery
554 | juLy 2010 | voLuMe 9 www.nature.com/reviews/drugdisc
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
Subsequent to this initial 2‑week study, List and
Rate of glucose filtration/reabsorption/
colleagues performed a 12‑week, double‑blind, ran‑
Tmax Tmax domized, parallel‑group, placebo‑controlled Phase II
375
trial in 389 treatment‑naive subjects with T2DM25.
excretion (mg per min)
200 Dapagliflozin given at 2.5 mg, 5 mg, 10 mg, 20 mg or
Reabsorption 50 mg once daily was compared with placebo. extended
release metformin of 750 mg force‑titrated to 1,500 mg
at week 2 was also included as an active comparator.
100 Excretion
Statistically significant reductions from baseline in
HbA1c were observed in all dapagliflozin‑treated
Actual Theoretical subjects, ranging from –0.55% to –0.9%, compared
threshold threshold with –0.18% in the placebo group and –0.73% in the
180 200 300 metformin group. The effect of dapagliflozin on uri‑
Plasma glucose (mg per 100ml) nary glucose excretion was also assessed. In contrast to
Figure 4 | renal glucose handling before and following metformin and placebo‑treated subjects, mean urinary
inhibition of sgLT2. With gradual infusion of glucose, glucose levels rose from between 5.8 g to 10.9 g per
as the plasma glucose concentration increases,
Nature Reviews | Drugthe
Discovery 24 hours at baseline to 51.8 g to 85.0 g per 24 hours
reabsorption progressively increases following the line at week 12 in the dapagliflozin group. These elevations
marked reabsorption curve (in red). At plasma glucose were sustained for the entire duration of the study.
concentrations <200 mg per 100 ml, all the filtered glucose weight was also lowered across all dapagliflozin groups
is reabsorbed and there is no excretion. When glucose (ranging from –2.5% to –3.4%), with minor decreases
reaches a threshold, around 200–250 mg per 100 ml, the in weight detected within the metformin and placebo
maximum capacity of the renal tubule to reabsorb glucose groups. Fasting plasma glucose levels declined dose‑
— or theTmax — is exceeded and once it passes this,
dependently in all dapagliflozin groups, and reductions
glucose begins to be excreted into the urine (blue line,
labelled excretion). The breaking point, however, is not were seen as early as the first week. The lowest dapagli‑
abrupt. Splay (the curved dotted lines between the actual flozin dose of 2.5 mg yielded a near‑maximal effect
and theoretical thresholds) represents glucose excretion on postprandial glucose levels. After 12 weeks, fasting
in the urine before saturation (Tmax) is fully attained, and is plasma glucose was the sole metabolic parameter that
explained by some nephrons releasing glucose at a slightly had a dose‑dependent response to dapagliflozin. SGLT2
lower threshold, others somewhat higher, and the relatively inhibition exerted a relatively greater effect on postpran‑
low affinity of the sodium–glucose co-transporters (SGLTs). dial glucose levels than on fasting plasma glucose levels,
The dotted lines underneath the arrows depict renal which suggests that renal glucose excretion serves as a
glucose handling after SGLT2 inhibition. The SGLT2 mechanism to relieve postprandial hyperglycaemia.
inhibitors lower the Tmax of glucose, which in turn increases
Recently, wilding and colleagues published a study
the excretion of glucose by the kidneys.
investigating the effect of dapagliflozin on HbA1c, fast‑
ing plasma glucose, postprandial glucose and weight in
patients with T2DM, who were experiencing suboptimal
These subjects were between the ages of 55–60 years control on oral agents and high insulin doses26. A total of
with unimpaired renal function, and were either drug‑ 71 individuals with T2DM were randomized in 26 cen‑
naive or on stable doses of metformin. The participants tres in the united States and in Canada. Patients were
were randomized to receive dapagliflozin at 5 mg, 25 mg on stable‑dose insulin‑sensitizing agents — metformin
or 100 mg, or placebo once daily for 14 days. At the end ≥1,000 mg and/or pioglitazone ≥30 mg, or rosiglitazone
of the study, fasting serum glucose levels were signifi‑ 4 mg — for ≥6 weeks and half of their usual insulin
cantly reduced across all dapagliflozin groups in a dose‑ dose (at least 50 units daily) for at least 12 weeks before
dependent manner. Doses of up to 100 mg were well enrolment, with no change in dose for at least 6 weeks.
tolerated by subjects for the 2 weeks of the study. Daily Twenty‑three patients were randomized to placebo, 24 to
urinary glucose excretion increased in a dose‑dependent the dapagliflozin 10 mg group, and 24 received 20 mg of
manner, although the amount of glucose excreted on day dapagliflozin. The primary end point — the change in
14 was slightly lower than on day 1. Subjects receiving HbA1c from baseline at week 12 (last observation car‑
placebo showed no change in the cumulative amount ried forward) — was reported to decrease 0.7% (10 mg)
of glucose excreted in the urine over 24 hours and no and 0.78% (20 mg) in the dapagliflozin groups versus
significant reductions in fasting serum glucose levels. placebo. Indeed, 65.2% of patients in both dapagliflozin
Dapagliflozin also induced a significant decline in glucose groups exhibited a ≥0.5% decline from baseline HbA1c
excursion after an oral‑glucose‑tolerance test, which compared with 15.8% of the placebo cohort. The mean
was measured as area under the plasma concentration– changes in fasting plasma glucose levels from baseline
Glucose excursion time curve (0–4 hours) on day 2 (ranging from –9.6% at week 12 were +17.8 mg per 100 ml (placebo), +2.4 mg
This is usually defined as to –13.7% with P<0.001) and on day 13 (ranging from per 100 ml (10 mg dapagliflozin) and –9.6 mg per 100 ml
the change in glucose –17.6% to –22.6% with P<0.001), as compared with (20 mg dapagliflozin). The mean changes in total body
concentration from before
to after a meal. In research
placebo. Dapagliflozin therefore demonstrated efficacy weight were –1.9 kg (placebo), –4.5 kg (10 mg dapagli‑
settings this is pre- and post- in dose‑ranging studies in healthy subjects as well as in flozin) and ‑4.3 kg (20 mg dapagliflozin). Mean changes
oral-glucose-tolerance tests. those with T2DM. in postprandial glucose at 120 minutes at week 12 (last
NATuRe RevIewS | Drug Discovery voLuMe 9 | juLy 2010 | 555
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
a OH
modification of diet in renal disease‑estimated glomer‑
OH O
ular filtration rates at the end of the study were normal
HO OH compared with baseline.
O Dapagliflozin was also examined as an add‑on
H3C O
OH agent to metformin over 24 weeks in 546 patients with
OH
O O O O T2DM who were not being sufficiently controlled on
O O stable doses of metformin alone at 1,500 mg per day or
H3C OH
HO OH greater 27. In a multicentre, randomized, double‑blind,
O OH
OH placebo‑controlled clinical trial that has been reported
Phlorizin T-1095
in abstract form, subjects were equally divided into four
groups, all on open‑label metformin, to which dapagli‑
O O
O flozin 2.5 mg, 5 mg or 10 mg, or placebo were added. For
O O the primary end point — the change in HbA1c at the
O
end of the study — all groups with dapagliflozin added
O O O
O O HO
HO O on to metformin demonstrated statistically significant
OH reductions from baseline HbA1c, which were greater
HO OH N N
than those observed with metformin treatment alone.
OH
weight also revealed a dose‑dependent decrease, ranging
Sergliflozin Remogliflozin from –2.66% to –3.43%.
b F
Canagliflozin. Canagliflozin (developed by johnson &
HO
johnson) (fIG. 5b; TABLe 2) is also currently undergoing
S O Phase III trials, with results in abstract form anticipated for
HO HO Cl presentation at the 2010 American Diabetes Association
O H Scientific Sessions. In preclinical studies, a single oral
HO HO OH O administration of 3 mg per kg of canagliflozin decreased
H
plasma glucose levels independent of food intake in mice
HO OH Canagliflozin Dapagliflozin
on a high‑fat, hyperglycaemic diet. In normoglycaemic
mice, canagliflozin administration led to a minimal
H
O N NH2 change in plasma glucose levels. Canagliflozin had a
HN
N
longer plasma half‑life and greater oral bioavailability
O
HO compared with its predecessor, T‑1095 (Ref. 28).
O O
O An example of one of the double‑blind, Phase III
HO OH
HO clinical trials currently underway is the CANTATA‑Su
H
HO OH O (canagliflozin treatment and trial analysis‑sulfonylurea)
DSP-3235
trial, which is examining the efficacy and safety of canag‑
liflozin 100 mg or 300 mg once a day for 104 weeks com‑
O Cl
HO O pared with glimepiride 1 mg titrated to a maximum of
H S
O O 6 mg or 8 mg once a day for 104 weeks in patients with
HO
T2DM, who are not optimally controlled on stable‑dose
H
HO OH
HO OH O
metformin monotherapy 29. The primary end point is
OH the change in HbA1c; the secondary end point is the
LX-4211 TS-071 percentage change in body weight. Studies are also being
Figure 5 | Available structures of sgLT inhibitors. a | Early agents. Phlorizin and conducted on canagliflozin as monotherapy (100 mg and
T-1095 are nonselective for the sodium–glucose co-transporters
Nature(SGLTs),
Reviewswhereas
| Drug Discovery 300 mg) compared with placebo in patients with T2DM
sergliflozin and remogliflozin exhibit markedly increased selectivity for SGLT2. who are inadequately controlled with diet and exercise30;
b | Agents currently in development. All agents are selective for SGLT2, except for not controlled with metformin and sulphonylurea31; and
DSP-3235, which targets SGLT1. canagliflozin 100 mg and 300 mg compared with placebo
and an active‑control (sitagliptin 100 mg) in patients
with T2DM not controlled with metformin32.
observation carried forward) were +18.7 mg per 100 BI‑10773 and BI‑44847. BI‑10773 (developed by
ml with placebo and insulin; –34.3 mg per 100 ml for Boehringer Ingelheim) is a selective SGLT2 inhibitor
10 mg dapagliflozin and insulin; and –41.9 mg per that is currently in Phase II trials. Preclinical data have
100 ml for 20 mg dapagliflozin and insulin. The urinary demonstrated greater blockade of SGLT2 compared with
glucose excretion at week 12 for those receiving pla‑ remogliflozin, with an IC50 value of 3.1–0.7 nM compared
cebo was –1.5 g per 24 hours, compared with 83.5 g per with an IC50 value of 12–4 nM. In addition, the increase
24 hours in the 10 mg dapagliflozin group, and 85.2 g in urinary glucose excretion over 24 hours was signifi‑
per 24 hours for those given 20 mg dapagliflozin. Mean cantly higher in Zucker diabetic fatty rats and db/db mice
decreases in standing systolic and diastolic blood pres‑ given BI‑10773 than in those administered with remo‑
sure were detected in both dapagliflozin cohorts. The gliflozin33. Boehringer Ingelheim is also investigating a
556 | juLy 2010 | voLuMe 9 www.nature.com/reviews/drugdisc
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
Table 2 | SGLT2 inhibitors currently in development
Drug company Highest clinicalTrials.gov identifier
(alternative name) development
status
Dapagliflozin Bristol-Myers Squibb/ Phase III NCT01055691; NCT00643851; NCT00528372;
(BMS-512148)21–27 AstraZeneca NCT01095666; NCT01095653; NCT00673231;
NCT00528879; NCT00660907; NCT00680745
Canagliflozin Johnson & Johnson/ Phase III NCT01064414; NCT01081834; NCT01106625;
(TA-7284, Mitsubishi Tanabe NCT01106677; NCT01106690; NCT01106651;
JNJ-28431754)28–32 Pharma NCT01032629; NCT00968812
ASP-1941 Astellas/Kotobuki Phase III NCT01054092; NCT01057628
BI-10773 (Ref. 33) Boehringer Ingelheim Phase II NCT01011868
BI-44847 Boehringer Ingelheim Phase II Not applicable
(under license from
Ajinomoto)
TS-071 Taisho Pharmaceutical Phase II Not applicable
CSG-452 Roche/Chugai Phase II Not applicable
(R-7201, RG-7201) Pharmaceutical
LX-4211 Lexicon Phase II NCT00962065
Pharmaceuticals
DSP-3235 GlaxoSmithKline/ Phase I NCT00976261
(KGA-3235, Dainippon Sumitomo
GSK-1614235, (under license from Kissei
1614235)* Pharmaceuticals)
ISIS-SGLT2Rx Isis Pharmaceuticals Phase I NCT00836225
(ISIS-388626)34,35
Unknown Sirona Biochem (under Discovery Not applicable
license from TFChem)
SGLT, sodium–glucose co-transporter. *Selective for SGLT1; all other agents are selective for SGLT2.
second SGLT2 inhibitor from this series, BI‑44847, which mRNA expression without affecting SGLT1 expression35.
is undergoing Phase II trials, although most of the clinical These findings were observed in studies in dogs over
activity appears to be centred on BI‑10773. 6 weeks; Sprague Dawley rats over 3 months; and Zucker
diabetic fatty rats over 6 months35. ISIS‑388626 selec‑
Other agents. other SGLT2 inhibitors currently tively targeted kidney proximal tubules and there was no
being studied in Phase II trials include TS‑071 accumulation of this agent in cardiac, liver or intesti‑
(Taisho Pharmaceutical), CSG‑452 (Roche/Chugai nal tissues after 6 months of administration in Zucker
Pharmaceutical) and LX‑4211 (Lexicon Pharmaceuticals) diabetic fatty rats35. In these rats, HbA1c significantly
(fIG. 5b; TABLe 2). ASP‑1941 (Astellas/Kotobuki) is now decreased from 10.9 ± 0.3% in controls given saline to
in Phase III clinical studies in japan, and Phase II trials 6.3 ± 0.8% in animals treated with the antisense oli‑
in europe and the united States (TABLe 2). DSP‑3235 gonucleotide. Marked glycosuria and plasma glucose
(GlaxoSmithKline/Dainippon Sumitomo) is an SGLT1 reductions were also noted. Blood urea nitrogen, serum
inhibitor that is currently being evaluated in Phase I trials. creatinine, plasma electrolytes and urine electrolytes did
However, clinical data for these compounds have not yet not change significantly. The results of Phase I studies
been published. are forthcoming.
Antisense oligonucleotide
SGLT2 antisense oligonucleotide inhibitors. ISIS‑388626 Safety of SGLT2 inhibition
inhibitor (also know as ISIS‑SGLT2Rx and is being developed by one of the major safety concerns of many diabetes
When the sequence of a Isis Pharmaceuticals) represents a novel approach to agents is the potential development of hypoglycaemia.
particular gene is known to SGLT2 inhibition — the use of an RNAase H chimeric However, given that SGLT2 inhibitors act independ‑
cause a particular disease,
antisense oligonucleotide inhibitor to block the expres‑ ently of glucose‑dependent insulin secretion by the
a strand of nucleic acid can be
synthesized (DNA, RNA or a sion of the SGLT2 gene in vivo. Normoglycaemic mice pancreatic β‑cells, and that they incompletely inhibit
chemical analogue) that will responded to ISIS‑388626 with a 14‑fold to 130‑fold glucose reabsorption, this type of adverse effect is not
bind to the mRNA produced increase in urine glucose excretion at 1–30 mg per kg expected. Indeed, results from the dapagliflozin clinical
by that gene and inactivate per week, and 7‑fold to 125‑fold elevation at greater than trials so far have reported virtually no instances of major
that gene. Antisense is
complementary to the ‘sense’
3 mg per kg per week34. wancewicz and colleagues dem‑ hypoglycaemic events24–26. Further results are pending
sequence of the target gene’s onstrated that administration of ISIS‑388626 once a week from larger trials of longer duration. Although the risk
mRNA. yielded an approximately 80% reduction of renal SGLT2 of hypoglycaemia is low, it is important to investigate its
NATuRe RevIewS | Drug Discovery voLuMe 9 | juLy 2010 | 557
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
potential development if SGLT2 inhibitors are admin‑ these agents selectively target renal glucose transporters,
istered in combination with other anti‑diabetic agents, without affecting the counter‑regulatory hormones39.
such as metformin or the insulin secretagogues. The energy deficit induced by excretion of calories in
Given the mechanism of action of SGLT2 inhibitors, the urine can lead to weight loss, or at a minimum, result
other safety issues include the development of urinary in a weight‑neutral effect. The prospective aetiology of a
tract infections and fungal genitourinary infections, as slight diuretic‑like effect awaits further determination,
well as deterioration of renal function. Clinical studies and includes glucose inducing an osmotic diuresis, or
so far on dapagliflozin have found that the rates of uri‑ may be secondary to sodium loss. Hypertension could
nary tract infections were comparable in treatment and therefore possibly be concomitantly improved. As the
placebo groups. elevated urine volume of 400–600 ml target tissue is limited to the kidney, the potential for
per day was detected in the studies of dapagliflozin, and off‑target adverse effects is also minimized, and the data
was associated with a dose‑related elevation in haemato‑ from the studies completed so far indicate that this class
crit (range 1.5–2.9%)25, and increased urea. The diuresis of agents has been generally safe and well tolerated.
may be due more to an osmotic effect than to sodium Their novel mechanism of action suggests that
loss. Two recent clinical studies noted an increased inci‑ SGLT2 inhibitors might have the potential to be used
dence in fungal genitourinary infections, most occurring in combination with oral anti‑diabetic agents as well as
in the higher dosage groups25–26. insulin to exert additive or synergistic effects on lower‑
In addition, in all the three larger trials of the cur‑ ing glucose levels in T2DM, although the results of such
rently most advanced SGLT2 inhibitor, dapagliflozin, no investigations are awaited. In addition, the potential for an
deaths have occurred24–26 and no serious adverse events increase in side effects, such as hypoglycaemia, following
related to dapagliflozin were observed in the studies by such combination therapy is unknown.
Komoroski and colleagues23,24 and List and colleagues25. A question that has also not yet been answered is
Although two subjects experienced a serious adverse whether — and to what extent — inhibiting SGLT1
event in the study by wilding and colleagues26, one was activity along with inhibiting SGLT2 would yield addi‑
on placebo, while the other received the higher dose tional clinical improvement. Theoretically, greater
(20 mg) of dapagliflozin. glycaemic control and weight loss could reasonably be
Perhaps the most compelling evidence for the long‑ expected if both were blocked. However, owing to its
term safety of this class of agents that affect glucose presence in the small intestine, blocking SGLT1 could
reabsorption is found from studying individuals with generate less desirable effects that accompany the delayed
familial renal glycosuria — an autosomal genetic disorder absorption of carbohydrates. Mutations of SGLT1 pro‑
resulting from mutations in the gene encoding SGLT2; duce little or no glycosuria; thus, the role of SGLT1 in
its mode of transmission is thought to be co‑dominant the kidney would seem to be much more limited than
with incomplete penetrance36,37. Familial renal glycosu‑ that of SGLT2 (RefS 38,39). Studies on dual inhibition of
ria is characterized by persistent isolated glycosuria of SGLT2 and SGLT1 are ongoing. SGLT1 is also expressed
approximately 10–120 g per day, in the face of normal in large numbers in human cardiac myocytes, but any
fasting serum glucose, normal glucose tolerance tests, the potential effects on the heart are not yet known40. of
absence of any signs of general renal tubular dysfunction note, cardiomyopathy has not been reported in indi‑
or other pathological changes, and normal life expectan‑ viduals with the genetic disorder of glucose and galac‑
cies36,37. Individuals with familial renal glycosuria usually tose malabsorption41. In addition, the potential effect of
report no complaints, and only rarely have hypoglycae‑ SGLT suppression on SGLTs found elsewhere, such as
mia or hypovolaemia. the hypothalamus, is unclear. Indeed, SGLT inhibitors
are lipid‑soluble, and can therefore cross the blood–
Future directions and concluding remarks brain barrier, warranting additional research.
of the SGLTs, inhibition of SGLT2 offers the most Another area of uncertainty involves the contributions
promise as a therapeutic strategy because it is respon‑ of diuresis versus reduction in adiposity to total weight
sible for most of the renal glucose reabsorption and loss. one study postulated that the larger reduction in
since it is expressed exclusively in the kidney. Clinical weight during week 1 of dapagliflozin administration,
trials of many of the SGLT2 inhibitors are in the early coupled with a partial, rapid resurgence in weight after
stages; nevertheless, data from investigations so far are discontinuation of higher doses, might represent the
encouraging. Currently, all published clinical studies effect of diuresis, whereas more sustained weight loss is
of SGLT2 inhibitors have been performed in individu‑ due to decreased adipose tissue25. The safety of this class
als with T2DM, although they may also be beneficial of agents in women of child‑bearing age also is unknown,
in the treatment of T1DM. Acute administration of as is the impact of these inhibitors on bone metabolism.
SGLT2 inhibitors reduces both preprandial and post‑ In summary, increasing urinary glucose excretion
prandial blood glucose, and chronic administration represents a new approach to addressing the challenge of
may decrease glucotoxicity 38. Inhibition of SGLT2 rep‑ hyperglycaemia. SGLT2 inhibitors may have indications
resents a particularly appealing approach to treating both in the prevention and treatment of T2DM, and
diabetes, as, in contrast to many other current diabetes perhaps T1DM, with a possible application in obesity.
therapies, SGLT2 inhibitors do not directly influence Further studies in large numbers of human subjects are
insulin secretion, thereby utilizing a novel mechanism necessary to delineate efficacy, safety and how to most
of action. Thus, there is a low risk of hypoglycaemia, as effectively use these agents in the treatment of diabetes.
558 | juLy 2010 | voLuMe 9 www.nature.com/reviews/drugdisc
© 2010 Macmillan Publishers Limited. All rights reserved
REVIEWS
1. Prentki, M. & Nolan, C. J. Islet cell failure in type 2 21. Meng, W. et al. Discovery of dapagliflozin: a potent, [online], http://clinicaltrials.gov/ct2/show/NCT011066
diabetes. J. Clin. Invest. 116, 1802–1812 (2006). selective renal sodium-dependent glucose 25?term=canagliflozin&rank=3 (2010).
2. Kaiser N. & Leibowitz G. J. Glucotoxicity and beta-cell cotransporter 2 (SGLT2) inhibitor for the treatment 32. Johnson & Johnson Pharmaceutical Research &
failure in type 2 diabetes mellitus. J. Pediatr. Endo. of type 2 diabetes. J. Med. Chem. 51, 1145–1149 Development, L.L.C. The CANTATA-D Trial
Metab. 16, 5–22 (2003). (2008). (Canagliflozin Treatment and Trial Analysis — DPP-4
3. Inzucchi, S. E. Oral antihyperglycemic therapy for The authors detail the initial identification of Inhibitor Comparator Trial). ClinicalTrials.gov
type 2 diabetes. JAMA 287, 360–372 (2002). dapagliflozin, the first agent in a new class of oral Idenitifier: NCT01106677. ClinicalTrials.gov website
4. Buse, J. B. et al. Effects of exenatide (Exendin-4) on selective SGLT2 inhibitors. [online], http://clinicaltrials.gov/ct2/show/NCT011066
glycemic control over 30 weeks in sulfonylurea-treated 22. Han, S. et al. Dapagliflozin, a selective SGLT2 inhibitor, 77?term=canagliflozin&rank=4 (2010).
patients with type 2 diabetes. Diabetes Care 27, improves glucose homeostasis in normal and diabetic 33. Grempler, G. et al. In vitro properties and in vivo effect
2628–2635 (2004). rats. Diabetes 57, 1723–1729 (2008). on urinary glucose excretion of BI 10773, a novel
5. Farber S. J., Berger E. Y. & Earle D. P. Effect of 23. Komoroski, B. et al. Dapagliflozin, a novel SGLT2 selective SGLT2 inhibitor. [Abstract 521-P].
diabetes and insulin of the maximum capacity of the inhibitor, induces dose-dependent glucosuria in American Diabetes Association website [online],
renal tubules to reabsorb glucose. J. Clin. Invest. 30, healthy subjects. Clin. Pharmacol. Ther. 85, 520–526 http://professional.diabetes.org/Abstracts_Display.
125–129 (1951). (2009). aspx?TYP=1&CID=73270 (2009).
6. Jabbour, S. A. & Goldstein, B. J. Sodium glucose The first studies on this agent in humans 34. Bhanot, S. et al. ISIS 388626, an SGLT2 antisense
co-transporter 2 inhibitors: blocking renal tubular are discussed in this paper. It describes drug, causes robust and sustained glucosuria in
reabsorption of glucose to improve glycaemic control single-ascending and multiple-ascending dose multiple species and is safe and well-tolerated.
in patients with diabetes. Int. J. Clin. Pract. 62, studies of dapagliflozin, and found that it produced [Abstract 328-OR]. American Diabetes Association
1279–1284 (2008). dose-dependent glycosuria in healthy volunteers. website [online], http://professional.diabetes.org/
7. Brown, G. K. Glucose transporters: structure, function, 24. Komoroski, B., Vachharajani, N., Feng, Y., Li, L., Abstracts_Display.aspx?TYP=1&CID=74543
and consequences of deficiency. J. Inherited Metab. Kornhauser, D. & Pfister, M. Dapagliflozin, a novel, (2009).
Dis. 23, 237–246 (2000). selective SGLT2 inhibitor, improved glycemic control 35. Wancewicz, E. V. et al. Long term safety and efficacy of
8. Wright, E. M. & Turk, E. The sodium/glucose over 2 weeks in patients with type 2 diabetes mellitus. ISIS 388626, an optimized SGLT2 antisense inhibitor,
cotransport family SLC5. Pflugers Arch. 447, Clin. Pharmacol. Ther. 85, 513–519 (2009). in multiple diabetic and euglycemic species. [Abstract
510–518 (2004). Dapagliflozin was first shown in this clinical 334-OR]. American Diabetes Association website
9. Rahmoune, H. et al. Glucose transporters in human investigation to produce elevations in glycosuria [online], http://professional.diabetes.org/Abstracts_
renal proximal tubular cells isolated from the urine that were dose-dependent in patients with T2DM. Display.aspx?TYP=1&CID=68615 (2008).
of patients with non-insulin-dependent diabetes. It also demonstrated improvements in fasting 36. Calado, J., Soto, K., Clemente, C., Correia, P. & Rueff, J.
Diabetes 54, 3427–3434 (2005). plasma glucose and postprandial glucose (post- Novel compound heterozygous mutations in SLC5A2
This preclinical study is the first demonstration oral-glucose-tolerance test) that were independent are responsible for autosomal recessive renal
in a human model that elevated renal glucose of effects on insulin. glucosuria. Hum. Genet. 114, 314–316 (2004).
transporter expression and function are associated 25. List, J. F., Woo, V., Morales, E., Tang, W. & 37. van den Heuvel, L. P., Assink, K., Willemsen, M. &
with T2DM. Fiedorek, F. T. Sodium–glucose cotransport inhibition Monnens, L. Autosomal recessive renal glucosuria
10. Wright, E. M. Renal Na–glucose cotransporters. with dapagliflozin in type 2 diabetes. Diabetes Care attributable to a mutation in the sodium glucose
Am. J. Renal Physiol. 280, F10–F18 (2001). 32, 650–657 (2009). cotransporter (SGLT2). Hum. Genet. 111, 544–547
11. Lee, Y. J. & Han, H. J. Regulatory mechanisms of Na+/ 26. Wilding, J. P. et al. A study of dapagliflozin in (2002).
glucose cotransporters in renal proximal tubule cells. patients with type 2 diabetes receiving high doses of 38. Bakris, G. L., Fonseca, V. A., Sharma, K. &
Kidney Int. Suppl. 106, S27–S35 (2007). insulin plus insulin sensitizers: applicability of a novel Wright, E. M. Renal sodium–glucose transport:
12. Abdul-Ghani, M. A., DeFronzo, R. A. Inhibition of renal insulin-independent treatment. Diabetes Care 32, role in diabetes and potential clinical implications.
glucose reabsorption: a novel strategy for achieving 1656–1662 (2009). Kidney Int. 75, 1272–1277 (2009).
glucose control in type 2 diabetes mellitus. Endocr. The authors provide evidence that SGLT2 inhibition 39. Wright, E. M. in Metabolic Basis of Inherited Disease
Pract. 14, 782–790 (2008). can reduce weight and blood glucose in patients (eds Scriver, C. R., Beaudet, A. L., Sly, W. S. &
13. Nathan, D. M. Long-term complications of diabetes with T2DM who, despite being on high doses Valle, D.) 4891–4908 (McGraw-Hill, New York, 2001).
mellitus. N. Engl. J. Med. 328, 1676–1685 (1993). of insulin and oral insulin-sensitizer therapy, 40. Zhou, L. et al. Human cardiomyocytes express
14. Santer, R. et al. Molecular analysis of the SGLT2 gene are suboptimally controlled. high levels of Na+/glucose cotransporter1 (SGLT1).
in patients with renal glucosuria. J. Am. Soc. Nephrol. 27. Bailey, C. J., Gross, J. L., Bastone, L., Bastien, A. & J. Cell Biochem. 90, 339–346 (2003).
14, 2873–2882 (2003). List, J. F. Dapagliflozin as an add-on to metformin 41. Wright, E. M. Genetic disorders of membrane
15. Ehrenkranz, J. R., Lewis, N. G., Kahn, C. R. & Roth, J. lowers hyperglycemia in type 2 diabetes patients transport: glucose galactose malabsorption.
Phlorizin: a review. Diabetes Metab. Res. Revs. 21, inadequately controlled with metformin alone. Am. J. Physiol. Gastrointest. Liver Physiol. 275,
31–38 (2005). Diabetologia 52, S76 (2009). 879–892 (1998).
16. Rossetti, L., Smith, D., Shulman, G. I., Papachristou, D. 28. Nomura, S., Sakamaki, S. & Hongu, M. Discovery of
& DeFronzo, R. A. Correction of hyperglycemia with novel C-glucosides with thiophene ring as sodium Acknowledgements
phlorizin normalizes tissues sensitivity to insulin in dependent glucose cotransporter 2 inhibitors for the This project was supported by the Veterans Administration
diabetic rats. J. Clin. Invest. 79, 1510–1515 (1987). treatment of type 2 diabetes mellitus. [Abstract MEDI Medical Center, San Diego and the University of California,
This manuscript presents the first in vivo studies 151]. American Chemical Society website [online], San Diego, USA.
that link hyperglycaemia with the development of http://oasys2.confex.com/acs/238nm/techprogram/
insulin resistance. P1283845.HTM (2009). Competing interests statement
17. Freitas, H. S. et al. Na+–glucose transporter-2 29. Johnson & Johnson Pharmaceutical Research & The authors declare competing financial interests: see web
messenger ribonucleic acid expression in kidney of Development, L.L.C. CANagliflozin Treatment And Trial version for details.
diabetic rats correlates with glycemic levels: Analysis-Sulfonylurea (CANTATA-SU) SGLT2 add-on to
involvement of hepatocyte nuclear factor-1α expression metformin versus glimepiride. ClinicalTrials.gov
and activity. Endocrinology 149, 717–724 (2008). Idenitifier: NCT00968812. ClinicalTrials.gov website DATABASES
18. Oku, A. et al. T-1095, an inhibitor of renal Na+–glucose [online], http://clinicaltrials.gov/ct2/show/NCT009688 OMIM:
cotransporters, may provide a novel approach to 12?term=canagliflozin&rank=5 (2010). http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=OMIM
treating diabetes. Diabetes 48, 1794–1800 (1999). 30. Johnson & Johnson Pharmaceutical Research & Familial renal glycosuria
19. Hussey, E. K. et al. Multiple-dose pharmacokinetics Development, L.L.C. The CANTATA-M (CANagliflozin UniProtKB: http://ca.expasy.org/sprot
and pharmacodynamics of sergliflozin etabonate, Treatment and Trial Analysis — Monotherapy) Trial. GLUT1 | GLUT2 | SGLT1 | SGLT2
a novel inhibitor of glucose reabsorption, in healthy ClinicalTrials.gov Idenitifier: NCT01081834.
FURTHER INFORMATION
overweight and obese subjects: a randomized double- ClinicalTrials.gov website [online], http://clinicaltrials.
ClinicalTrials.gov: http://clinicaltrials.gov
blind study. J. Clin. Pharmacol. 3 Mar 2010 gov/ct2/show/NCT01081834?term=canagliflozin&ra
Division of Endocrinology and Metabolism, UCSD
(doi:10.1177/0091270009352185). nk=2 (2010).
Department of Medicine: http://endocrinology.ucsd.edu
20. Fujimori, Y. et al. Remogliflozin etabonate, in a novel 31. Johnson & Johnson Pharmaceutical Research &
The Center for Metabolic Research, VA San Diego
category of selective low-affinity sodium glucose Development, L.L.C. The CANTATA-MSU Trial
Healthcare System: http://www.vacmr.org
cotransporter (SGLT2) inhibitors, exhibits antidiabetic (Canagliflozin Treatment And Trial Analysis —
efficacy in rodent models. J. Pharmacol. Exp. Ther. Metformin and Sulphonylurea). ClinicalTrials.gov ALL LiNks Are AcTive iN THe oNLiNe PDf
327, 268–276 (2008). Idenitifier: NCT01106625. ClinicalTrials.gov website
NATuRe RevIewS | Drug Discovery voLuMe 9 | juLy 2010 | 559
© 2010 Macmillan Publishers Limited. All rights reserved
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Bacteria Found in UrineDokument7 SeitenBacteria Found in UrineAria DomingoNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Essential Questions in Paediatrics For MRCPCH v2 PDFDokument208 SeitenEssential Questions in Paediatrics For MRCPCH v2 PDFa4aboo100% (11)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- BIO 211 Chapter 18 AssignmentDokument20 SeitenBIO 211 Chapter 18 Assignmentf1l2o3r4e5n6Noch keine Bewertungen
- Body Parts Governed by PlanetsDokument2 SeitenBody Parts Governed by PlanetsBratva Ankit Mishra100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Assessment of Vital Signs&GCSDokument3 SeitenAssessment of Vital Signs&GCSNicole Jackson100% (3)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Preeclampsia Nursing Care PlanDokument5 SeitenPreeclampsia Nursing Care PlanBSN 3-2 RUIZ, Jewel Anne F.Noch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Icp Member Handbook Il PDFDokument36 SeitenIcp Member Handbook Il PDFjohnNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Family Laboratory For Medical Analysis: Test & SpecimenDokument1 SeiteFamily Laboratory For Medical Analysis: Test & SpecimenMohamad BadranNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Daftar Jurnal Kedokteran Internasional GratisDokument3 SeitenDaftar Jurnal Kedokteran Internasional GratisdoktermutiaNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- WES Ablasi SVT AVRT - Travilla Bastian A. PangestutiDokument1 SeiteWES Ablasi SVT AVRT - Travilla Bastian A. PangestutiHervin RamadhaniNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- DctsDokument30 SeitenDctsInuyashayahoo100% (1)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Gujarat Technological University: W.E.F. AY 2017-18Dokument3 SeitenGujarat Technological University: W.E.F. AY 2017-18raj royelNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- ANMDokument13 SeitenANMhiiihhhhhhhhNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Improving VO2 Max Through ExerciseDokument1 SeiteImproving VO2 Max Through ExercisecathyNoch keine Bewertungen
- 2004 NEJM Photosensitivity NEJ 2004Dokument7 Seiten2004 NEJM Photosensitivity NEJ 2004Alma EscobarNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- CBDRP Reporting Form 1Dokument1 SeiteCBDRP Reporting Form 1Romer EnajeNoch keine Bewertungen
- Tolak Angin TranslatedDokument3 SeitenTolak Angin TranslatedWadz MuharNoch keine Bewertungen
- Clinical Features and Diagnosis of Abdominal Aortic Aneurysm - UpToDateDokument53 SeitenClinical Features and Diagnosis of Abdominal Aortic Aneurysm - UpToDateALVARO ARIASNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Classification of Tongue Cancer Resection and Treatment AlgorithmDokument8 SeitenClassification of Tongue Cancer Resection and Treatment AlgorithmRahma WatiNoch keine Bewertungen
- Medical Symptoms QuestionnaireDokument29 SeitenMedical Symptoms QuestionnaireOlesiaNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Complications of Insulin TherapyDokument16 SeitenComplications of Insulin TherapyIngrid NicolasNoch keine Bewertungen
- The Administration of Medications I. Speaking 'Administering Medications'Dokument5 SeitenThe Administration of Medications I. Speaking 'Administering Medications'Meri AndaniNoch keine Bewertungen
- Specific Proteins Calibrator-150721009-BS600Dokument2 SeitenSpecific Proteins Calibrator-150721009-BS600S6b2Noch keine Bewertungen
- HargaDokument68 SeitenHargarsurNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Dr. Ugi Sugiri, SpEm - PPT OBMED PDFDokument56 SeitenDr. Ugi Sugiri, SpEm - PPT OBMED PDFDaniel Aprianto SihotangNoch keine Bewertungen
- 103, Kanakia - B. Zillion Building, Lbs Marg, Kurla (W), Mumbai - 400 070Dokument10 Seiten103, Kanakia - B. Zillion Building, Lbs Marg, Kurla (W), Mumbai - 400 0708460074686Noch keine Bewertungen
- Beth PRC FormDokument11 SeitenBeth PRC FormNev Bryan DapitanNoch keine Bewertungen
- Girl InterruptedDokument7 SeitenGirl Interruptedapi-365678992Noch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- PMLS Lesson 5Dokument7 SeitenPMLS Lesson 5Althea EspirituNoch keine Bewertungen
- EMS Final Exam JulyDokument267 SeitenEMS Final Exam Julyraja bouguerraNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)