Beruflich Dokumente
Kultur Dokumente
2017 11 17 PRM Raducha PDF
Hochgeladen von
Kamran AfzalOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
2017 11 17 PRM Raducha PDF
Hochgeladen von
Kamran AfzalCopyright:
Verfügbare Formate
P ED IATRIC REHA B ILITATION MED IC IN E (PR M)
A Review of Brachial Plexus Birth Palsy: Injury and Rehabilitation
JEREMY E. RADUCHA, MD; BRIAN COHEN, MD; TRAVIS BLOOD, MD; JULIA KATARINCIC, MD
A BST RA C T A NATOMY
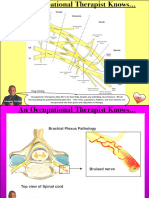
Brachial plexus injuries during the birthing process can The brachial plexus is derived from the fifth cervical (C5) to
leave infants with upper extremity deficits corresponding the first thoracic (T1) nerve roots. It undergoes a complex
to the location of the lesion within the complex plexus pattern of branching and convergence before terminating as
anatomy. Manifestations can range from mild injuries with peripheral nerves that provide motor and sensory innervation
complete resolution to severe and permanent disability. to the upper extremity. (Figure 1, Table 1) The plexus can be
Overall, patients have a high rate of spontaneous recovery divided into supraclavicular (roots and trunks) and sub-cla-
(66–92%).1,2 Initially, all lesions are managed with passive vicular (cords and terminal branches) for prognostic pur-
range motion and observation. Prevention and/or correc- poses, with supraclavicular injuries having worse outcomes.9
tion of contractures with occupational
therapy and serial splinting/casting along Figure 1. Brachial Plexus Anatomy
with encouraging normal development
are the main goals of non-operative treat-
ment. Surgical intervention may be war-
ranted, depending on functional recovery.
K E YWORD S: Brachial plexus, Erb’s palsy,
Klumpke’s palsy, serial splinting
INTRO D U C T I O N
Brachial plexus birth palsy (BPBP) involves
injury to any nerve of the brachial plexus
during birth. It occurs in 0.42 to 4.6 cases
per 1,000 births, which translates to approxi-
mately 5 to 50 cases per year in Rhode Island,
with varying degrees of severity.1–3 The most
common presentation is Erb’s Palsy (50-
60%), followed by the more severe upper
plexus and pan-plexus variants.1,4 Klumpke’s
lower plexus palsy is rare, and occurs in 0.6%
of all patients.5 Maternal risk factors include gestational dia- Pathophysiology
betes, multi-parity and having a previous child with a brachial The majority of BPBPs are traction injuries, as with shoul-
plexus injury. Maternal factors can cause fetal macrosomia der dystocia when traction on the infant’s neck leads to an
and/or shoulder dystocia, increasing the risk of forceps or increased neck shoulder angle.1 Very rarely, compression
suction-assisted deliveries and traction nerve injury.6 Since injuries from fractured clavicles, hematomas, and pseudo-
the majority of fetuses present in the left occiput anterior aneurysm can occur.7 Lesions can be divided into symptom-
position, with the right shoulder under the maternal pel- atic categories using multiple systems. The simplest approach
vis, the right upper extremity is most commonly involved.7 is to classify lesions as pre-ganglionic or post-ganglionic,
However, only about half of patients have these risk fac- distal to the dorsal root ganglion. Pre-ganglionic lesions,
tors, demonstrating our lack of true understanding of the with the nerve injured proximally, e.g., root avulsions, are
etiology.8 This article will review the pathology, diagnosis, more difficult to heal/repair and have worse outcomes than
treatment, rehabilitation and outcomes of BPBP. post-ganglionic lesions. It is only possible to determine this
W W W. R I M E D . O R G | ARCHIVES | N O V E M B E R W E B PA G E NOVEMBER 2017 RHODE ISL AND M EDICAL JOURNAL 17
P ED IATRIC REHA B ILITATION MED IC IN E (PR M)
Table 1. Brachial Plexus Functions
Branching Location Nerve Root Innvervation Muscle action
Roots Dorsal Scapular n. C5 M: Rhomboid mm. and Levator Scapulae m. Rhom: scapular retraction, Levator=scapular elevation
Long Thoracic n. C5,C6 & C7 M: Serratus anterior m. Scapular protraction
First intercostal n. T1 M: intercostal m. n/a
Trunks Suprascapular n. C5, C6 M: Supraspinatus m, Infraspinatus m. S: Supra= Arm abduction. Infra= Arm external rotation
Shoulder joint capsule
Nerve to Subclavius C5, C6 M: Subclavius m. n/a
Divisions none
Cords
Posterior Upper Subscapular n C5-T1 Motor : Upper subscapularis m. Arm internal rotation
Lower Subscapular n C5-T1 Motor : Lower Subscapularis m., Teres LS= Arm internal rotation
Major m.
Thoracodorsal n. C5-T1 Motor : Latissimus dorsi m. Arm adduction
Lateral Lateral Pectoral n. C5-C7 Motor : Pectoralis Major m. Arm Adduction
Medial Medial Pectoral n. C8-T1 Motor : Pectoralis Major m., Pectoralis Arm Addution
Minor m.
Medial Brachial cutaneous n. C8-T1 Sensory : medial arm n/a
Medial Antebrachial cutaneous n. C8-T1 Sensory: medial forearm n/a
Terminal Nerves Radial n. C5-T1 Motor : Triceps mm, brachioradialis m., Elbow extension, Wrist extension, Finger Extension, Thumb
ECRL, ECRB, ECU, EDC, EIP, EDM, EPL, EPB, extension, thumb abduction, Forearm supination;
APL, Supinator m., Finger extensors Brachioradialis=elbow flexion
Sensory : posterior brachial cutaneous,
inferior lateral brachial cutaneous,
posterior antebrachial cutaneous,
superficial radial (post. radial hand)
Axillary n. C5-T1 Motor: Deltoid m., Teres Minor m., Delt= Arm abduction, Teres= Arm external rotation
Sensory: Lateral proximal arm
Musculocutaneous n. C5-C7 Motor : Biceps brachii m., Brachialis m, Elbow Flexion, Forearm supination S: lateral forearm
corocobrachialis m.
Sensory: Lateral cutaneous n. of the
forearm
Median n. C5-T1 Motor : FCR, Palmaris longus m., FDS, radial Wrist flexion, Forearm pronation, thumb
1/2 FDP, Pronator teres m. FPL, Pronator flexion/abduction/opposition, finger PIP flexion, IF/MF MCP
quadratus m., FPB (superficial head), and DIP flexion
Opponens pollicis, APB, 1st-2nd lumbricals
Sensory : Radial 3 1/2 fingers, palmar
cutaneous branch
Ulnar n. C8-T1 Motor : FCU, ulnar 1/2 FDP, Flexor DM, Wrist flexion, Thumb adduction/flexion, SF
Abductor DM, Opponens DM, Adductor flexion/abduction/opposition, finger adduction/abduction, 4th
pollicis, FPB (deep head), Palmaris brevis and 5th finger DIP/MCP flexion
m. Dorsal interossei mm. Palmar interossei
mm., 3rd-4th Lumbricals
Sensory : Dorsal ulnar cutaneous n., Palmar
ulnar cutaneous n.
classification after advanced imaging. The Sunderland clas- Table 2. Sunderland Classification
sification (Table 2) categorizes nerve injuries based on the Type of Nerve Injury Prognosis
nerve structures damaged, ranging in severity from neuro-
praxia to neurotmesis.10 As expected, patients with less severe Neuropraxia Stretch injury with intact Spontaneous recovery
nerve continuity likely
damage, e.g., neuropraxia, have a better chance at recovery.
The most common way to describe BPBPs is based on Axonotmesis Axonal injury with intact Variable recovery
the nerve roots involved, which can be detected by phys- nerve sheath
ical examination. Upper trunk (Erb-Duchenne) palsies
Neurotmesis Complete nerve rupture; Poor prognosis for
involve only the disruption of input from the C5 and C6 neither axon nor sheath spontaneous recovery
nerve roots. Upper plexus palsies involve roots C5, C6 and intact
C7, with the addition of more distal deficits. Lower plexus
Sunderland SS. The anatomy and physiology of nerve injury. Muscle Nerve.
(Klumpke’s) palsies involve the C8 and T1 nerve roots and 1990;13(9):771-784. doi:10.1002/mus.880130903
can also affect the sympathetic chain with pre-ganglionic
injuries. The most severe is the all-encompassing pan-plexus
injury involving nerve roots C5-T1, with disruption to all
functions of the upper extremity.
W W W. R I M E D . O R G | ARCHIVES | N O V E M B E R W E B PA G E NOVEMBER 2017 RHODE ISL AND M EDICAL JOURNAL 18
P ED IATRIC REHA B ILITATION MED IC IN E (PR M)
DIAGN O S I S two-week period of immobilization to promote healing and
Maternal history, physical examination and diagnostic imag- decrease pain,9 but others find little evidence that immobi-
ing can provide a wealth of information to make the proper lization has any benefit.1 Contractures can begin as early
diagnosis and injury classification. The patient’s mother as 2-3 weeks after birth, with the glenohumeral joint most
should be interviewed for the BPBP risk factors mentioned commonly affected. Without early treatment, the contrac-
previously. Abnormal primitive reflexes, e.g., Moro reflex tures can progress rapidly and cause posterior subluxation/
and tonic neck reflex, are often the first clues in the new- dislocation of the humeral head.1,9,12
born examination. It is also important to palpate the infant’s After an initial observation period, children can be cate-
clavicle and humerus, as fractures can affect upper extremity gorized as having either partial or total paralysis. Patients
movements and be confused with brachial plexus palsy. A with total paralysis should be referred to a tertiary center for
septic shoulder and isolated radial nerve palsy should also be early surgical evaluation, as they have a very low likelihood
in the differential diagnosis, but they are less common and of spontaneous recovery. Patients with partial paralysis have
are associated with different physical and laboratory findings. a higher chance of recovery, and there is complete recovery
Depending where the lesion is located, the patient’s by 3 months of age with as many as 92% of these patients.9,13
affected extremity will present in different positions. With Other evidence suggests complete recovery rates may not
Erb’s palsy (C5-6), the arm is adducted and internally rotated be as high as originally thought, with as many as 20–30%
at the shoulder and extended at the elbow, due to weakness of patients having a long-term defecit.1,2 Patients who do
in the deltoid, supero-posterior rotator cuff and biceps. A not have complete recovery by 1 month of age should be
patient with upper plexus palsy (C5-7) has the above pos- evaluated by a pediatric therapist for continued monitoring
ture as well as wrist and fingers flexion due to radial nerve and rehabilitation. Many physicians use the lack of antigrav-
involvement and wrist/finger extensor weakness. Pan-plexus ity biceps function return by 3 months as an indication for
injuries (C5-T1) typically present with a flaccid extremity. nerve surgery since it is a poor prognostic indicator for com-
Pre-ganglionic injuries, which carry a worse prognosis,, plete spontaneous recovery;1,4 however, this does not pre-
may lead to head tilting to the opposite side (denervation clude good functional recovery. Recovery of wrist extension
of paraspinal musculature), medial winging of the scapula, is also a positive prognostic sign. Other physicians advocate
diaphragm dysfunction, and Horner’s syndrome. continued rehabilitation until at least 6 months of age before
As children age, their disabilities become more apparent. considering surgery. Some evidence has shown that children
Scoring systems such as the Toronto Test Score, Active who recovered antigravity biceps function between the 3rd
Movement Scale, and Modified Mallet system have been and 6th months of life always had an incomplete recovery
developed to grade and track upper extremity function.11 compared to those who regained function prior to 3 months.9
The Modified Mallet score is the most commonly used If children undergo surgery, it is typically performed
when evaluating older children (≥3 years old). It uses five between 3 and 8 months of age; earlier surgery (at 3 months)
categories to assess shoulder function, with a 0–5 grading is indicated in children with pan-plexus palsies and Horner’s
for each category. Higher scores correlate to higher function, syndrome. The main goals of surgery, in order of importance,
but the examination requires patient participation and is are to restore elbow flexion, shoulder abduction, shoulder
heavily weighted toward shoulder external rotation. external rotation, wrist extension and hand function.7 The
Imaging can help clarify the diagnosis and classifica- options for early surgical intervention include direct nerve
tion. Initially, radiographs of the upper extremity should be repair with resection and grafting, or nerve transfers from
obtained to rule out fractures, which could be confused with surrounding motor nerves. In spite of surgery, many patients
or occur concomitantly with brachial plexus palsy. MRI and still suffer some degree of long-term sequalae.2 In patients
CT myelography can be used to detect root avulsions. Elec- who develop contracture or have persistent weakness, later
tromyography has been suggested if there is no nerve recov- surgery can be beneficial. Lysis of contractures, osteotomies
ery by 6 months of age, in order to detect a pre-ganglionic and local tendon transfers can help return functional motion
injury, which is potentially amenable to operative interven- and correct deformities.12,14
tion. Other evidence shows, however, that electromyography Children who recover meaningful biceps function by 6
can be discordant from clinical bicep function at 3 months of months of age are typically treated non-operatively with
age and the test may not be a reliable indicator for surgery.1 rehabilitation and monitoring. There is little high grade
research discussing non-operative management techniques
and protocols for brachial plexus birth palsies. All non-oper-
T REAT M E N T A ND O UT COM E S ative treatment involves a multidisciplinary team approach,
Treatment for a suspected brachial plexus palsy should with occupational therapy and splinting to prevent or correct
begin immediately with frequent, passive range of motion of contractures. The goals of treatment prior to muscle func-
the affected upper extremity. Parents should be instructed to tion recovery are to prevent contracture, strengthen recov-
range both arms at every diaper change to make it a daily rou- ering muscles, stimulate sensory nerves, and encourage the
tine and encourage compliance. Some authors recommend a achievement of normal developmental milestones. As the
W W W. R I M E D . O R G | ARCHIVES | N O V E M B E R W E B PA G E NOVEMBER 2017 RHODE ISL AND M EDICAL JOURNAL 19
P ED IATRIC REHA B ILITATION MED IC IN E (PR M)
child grows, passive range of motion should be transitioned References
to participation in age-appropriate activities for rehabilita- 1. Malessy MJA, Pondaag W. Obstetric Brachial Plexus Inju-
ries. Neurosurg Clin N Am. 2009;20(1):1-14. doi:10.1016/j.
tion with regular follow-up to assess functional scores, arm nec.2008.07.024.
growth and joint integrity. Elbow flexion contractures are 2. Hoeksma AF, Wolf H, Oei SL. Obstetrical brachial plexus inju-
a fairly common occurrence, even with triceps sparing pal- ries: incidence, natural course and shoulder contracture. Clin
Rehabil. 2000;14(5):523-526. doi:10.1191/0269215500cr341oa.
sies. For children who develop contractures, stretching and
3. Evans-Jones G, Kay SPJ, Weindling AM, et al. Congenital bra-
serial night splinting can be used for contractures less than chial palsy: incidence, causes, and outcome in the United
20 degrees. Treating deformities in this range will prevent Kingdom and Republic of Ireland. Arch Dis Child Fetal Neo-
natal Ed. 2003;88(3):F185-9. http://www.ncbi.nlm.nih.gov/
progression and help cosmetic appearance, as the elbow’s pubmed/12719390. Accessed May 15, 2017.
functional range of motion is between 30–130 degrees.15 4. Kozin SH. Brachial Plexus Microsurgical Indications. J Pediatr
Serial casting and splinting of elbow flexion contractures Orthop. 2010;30:S49-S52. doi:10.1097/BPO.0b013e3181cd9ed2.
can yield good results, but this approach can be compli- 5. al-Qattan MM, Clarke HM, Curtis CG. Klumpke’s birth palsy.
Does it really exist? J Hand Surg Br. 1995;20(1):19-23. http://
cated by radial head dislocation, bony ingrowth at the joint, www.ncbi.nlm.nih.gov/pubmed/7759926. Accessed May 15,
and loss of elbow flexion while gaining extension. Much of 2017.
the research is focused on elbow flexion contractures but 6. Gilbert WM, Nesbitt TS, Danielsen B. Associated factors in 1611
cases of brachial plexus injury. Obstet Gynecol. 1999;93(4):536-
contractures preventing forearm supination and shoulder 540. http://www.ncbi.nlm.nih.gov/pubmed/10214829. Accessed
external rotation are also commonly present. A pilot study May 15, 2017.
has shown improvement in Toronto and Active Movement 7. Shenaq SM, Bullocks JM, Dhillon G, Lee RT, Laurent JP. Man-
agement of infant brachial plexus injuries. Clin Plast Surg.
Scales of supination and shoulder external rotation with a 2005;32(1):79-98. doi:10.1016/j.cps.2004.09.001.
Supination-External rotation orthosis worn 22 hours per day 8. Hale HB, Bae DS, Waters PM. Current concepts in the man-
with reprieves for therapy twice per day.16 Botulinum toxin agement of brachial plexus birth palsy. J Hand Surg Am.
2010;35(2):322-331. doi:10.1016/j.jhsa.2009.11.026.
injections with serial casting have also shown promise in 9. Abid A. Brachial plexus birth palsy: Management during the
patients who failed serial casting alone.17 The toxin relaxes first year of life. Orthop Traumatol Surg Res. 2016;102(1 Sup-
the antagonist muscle at the contracted joint, particularly in pl):S125-32. doi:10.1016/j.otsr.2015.05.008.
10. Sunderland SS. The anatomy and physiology of nerve injury.
cases of co-contraction, a common long-term complication. Muscle Nerve. 1990;13(9):771-784. doi:10.1002/mus.880130903.
Despite the lack of consensus regarding surgical indica- 11. Duff S, DeMatteo C. Clinical Assessment of the Infant and
tions and rehabilitation protocols, patients do have good Child Following Perinatal Brachial Plexus Injury. J Hand Ther.
2015;28(2):126-134. doi:10.1016/j.jht.2015.01.001.
long-term outcomes. Most studies show the majority of
12. Abid A, Accadbled F, Louis D, et al. Arthroscopic release for
patients are independent in activities of daily living, even shoulder internal rotation contracture secondary to brachi-
with persistent functional deficits.1,2,7,8,13,19 In a subjective al plexus birth palsy: clinical and magnetic resonance imag-
ing results on glenohumeral dysplasia. J Pediatr Orthop B.
study of adolescents, all patients reported a ‘really good’ 2012;21(4):305-309. doi:10.1097/BPB.0b013e328353688e.
quality of life, but they were also all dissatisfied with their 13. Laurent JP, Lee R, Shenaq S, Parke JT, Solis IS, Kowalik L. Neu-
current condition and hoped for continued improvement.20 rosurgical correction of upper brachial plexus birth injuries. J
Neurosurg. 1993;79(2):197-203. doi:10.3171/jns.1993.79.2.0197.
14. Abzug JM, Kozin SH. Evaluation and Management of Brachial
Plexus Birth Palsy. Orthop Clin North Am. 2014;45(2):225-232.
CON C L U S I O N doi:10.1016/j.ocl.2013.12.004.
Brachial plexus birth palsies can be stressful and challeng- 15. Ho ES, Roy T, Stephens D, Clarke HM. Serial casting and splint-
ing of elbow contractures in children with obstetric brachial
ing for parents and children. Despite a better understanding plexus palsy. J Hand Surg Am. 2010;35(1):84-91. doi:10.1016/j.
of the pathology and treatment options, injury incidence jhsa.2009.09.014.
has remained unchanged.1–3 In general, upper plexus palsies 16. Durlacher KM, Bellows D, Verchere C. Sup-ER orthosis: an in-
novative treatment for infants with birth related brachial plexus
recover better than lower plexus and pan-plexus palsies; injury. J Hand Ther. 2014;27(4):335-39; quiz 340. doi:10.1016/j.
neuropraxia does better than neurotmesis; and post-gan- jht.2014.06.001.
glionic lesions recover better than pre-ganglionic lesions. 17. Basciani M, Intiso D. Botulinum toxin type-A and plaster cast
treatment in children with upper brachial plexus palsy. Pediatr
Care should continue to focus on early identification and Rehabil. 2006;9(2):165-170. doi:10.1080/13693780500402229.
therapy to minimize complications. Early referral to tertiary 18. Kerr C, McDowell B, Cosgrove A, Walsh D, Bradbury I, Mc-
centers is crucial, as a multi-disciplinary approach can help Donough S. Electrical stimulation in cerebral palsy: a random-
ized controlled trial. Dev Med Child Neurol. 2006;48(11):870-
promote recovery and prevent complication. Fortunately 876. doi:10.1017/S0012162206001915.
there is a high rate of spontaneous recovery, but for patients 19. DiTaranto P, Campagna L, Price AE, Grossman JAI. Outcome
who don’t recover spontaneously there are non-surgical and following nonoperative treatment of brachial plexus birth inju-
ries. J Child Neurol. 2004;19(2):87-90. doi:10.1177/0883073804
surgical options to improve functional outcomes and pre- 0190020101.
vent devastating contractures. With an ever-expanding body 20. Squitieri L, Larson BP, Chang KWC, Yang LJS, Chung KC. Un-
of research geared towards improving care and knowledge derstanding quality of life and patient expectations among ado-
lescents with neonatal brachial plexus palsy: a qualitative and
of the injury, the future should show improved long-term quantitative pilot study. J Hand Surg Am. 2013;38(12):2387-
outcomes for these patients. 2397.e2. http://www.ncbi.nlm.nih.gov/pubmed/24416766. Ac-
cessed May 8, 2017.
W W W. R I M E D . O R G | ARCHIVES | N O V E M B E R W E B PA G E NOVEMBER 2017 RHODE ISL AND M EDICAL JOURNAL 20
P ED IATRIC REHA B ILITATION MED IC IN E (PR M)
Authors Correspondence
Jeremy E. Raducha, MD; Department of Orthopaedic Surgery, Jeremy E. Raducha, MD
Warren Alpert Medical School of Brown University, Department of Orthopaedic Surgery
Providence, RI. Rhode Island Hospital
Brian Cohen, MD; Department of Orthopaedic Surgery, Warren 593 Eddy Street
Alpert Medical School of Brown University, Providence, RI. Providence, RI 02903
Travis Blood, MD; Department of Orthopaedic Surgery, Warren 401-444-4030
Alpert Medical School of Brown University, Providence, RI. Fax 401-444-6182
Julia Katarincic, MD; Department of Orthopaedic Surgery, Warren Jeremy.raducha@gmail.com
Alpert Medical School of Brown University, Providence, RI.
W W W. R I M E D . O R G | ARCHIVES | N O V E M B E R W E B PA G E NOVEMBER 2017 RHODE ISL AND M EDICAL JOURNAL 21
Das könnte Ihnen auch gefallen
- Brachial Plexus Master Study GuideDokument155 SeitenBrachial Plexus Master Study GuideabusultandiaaNoch keine Bewertungen
- 2017 11 17 PRM RaduchaDokument6 Seiten2017 11 17 PRM RaduchaRock RockkNoch keine Bewertungen
- Brachial Plexus Palsy: RiasfDokument42 SeitenBrachial Plexus Palsy: RiasfRiaFernandesNoch keine Bewertungen
- The Way of Thinking in Brachial Plexus InjuryDokument48 SeitenThe Way of Thinking in Brachial Plexus InjuryYoonHeeNyNoch keine Bewertungen
- Anatomy All NotesDokument77 SeitenAnatomy All NotesBat ManNoch keine Bewertungen
- Brachial PlexusDokument61 SeitenBrachial PlexusGutu Garemewu BiruNoch keine Bewertungen
- Muscle Innervation Spinal Segment Action Additional Notes: Pectoralis Major MDokument10 SeitenMuscle Innervation Spinal Segment Action Additional Notes: Pectoralis Major MpoNoch keine Bewertungen
- Extremities Table of NervesDokument3 SeitenExtremities Table of NervesFG ArciagaNoch keine Bewertungen
- Brachial Plexus ExaminationDokument7 SeitenBrachial Plexus ExaminationMalvinder Singh DhillonNoch keine Bewertungen
- 01 Muscle Tables Upper LimbDokument7 Seiten01 Muscle Tables Upper LimbhawkreadNoch keine Bewertungen
- UE Muscles OINADokument3 SeitenUE Muscles OINAUshuaia Chely FilomenoNoch keine Bewertungen
- The Upper ExtremityDokument9 SeitenThe Upper ExtremityHiruzaminNoch keine Bewertungen
- Peripheral Nerves of UL by GarimaDokument69 SeitenPeripheral Nerves of UL by GarimaGarima Gupta100% (1)
- Methodic Materials MovementDokument20 SeitenMethodic Materials MovementKapil PancholiNoch keine Bewertungen
- Nasa Khan MRCS A Notes 2018 PDFDokument834 SeitenNasa Khan MRCS A Notes 2018 PDFWaqas Haleem100% (5)
- Singh's OsceDokument466 SeitenSingh's OsceShuaib AhmedNoch keine Bewertungen
- Muscle Upper LimbsDokument65 SeitenMuscle Upper LimbsTom WuNoch keine Bewertungen
- Guia de Pontos Motores PDFDokument18 SeitenGuia de Pontos Motores PDFDaniel Gonçalves SantosNoch keine Bewertungen
- UPPER EX - UNODokument16 SeitenUPPER EX - UNOrsbagtasNoch keine Bewertungen
- MSKDokument7 SeitenMSKKY KimberlyNoch keine Bewertungen
- 7-Pectoral Region and AxillaDokument11 Seiten7-Pectoral Region and AxillaKainat LatifNoch keine Bewertungen
- Muscles of The Upper Limb 2Dokument63 SeitenMuscles of The Upper Limb 2kiiroiiNoch keine Bewertungen
- Nerves and Innervated MusclesDokument108 SeitenNerves and Innervated Musclesphantasma669Noch keine Bewertungen
- Pages From (Susan O'Sullivan, Raymond Siegelman) National PhyDokument1 SeitePages From (Susan O'Sullivan, Raymond Siegelman) National Phydrng48Noch keine Bewertungen
- Anatomy Review of Extreme TiesDokument65 SeitenAnatomy Review of Extreme Tiesskihard0404749Noch keine Bewertungen
- Tendon Transfers For Radial Nerve PalsyDokument62 SeitenTendon Transfers For Radial Nerve Palsyavinashrao39Noch keine Bewertungen
- Muscles of Upper LimbDokument21 SeitenMuscles of Upper Limbمحمد علىNoch keine Bewertungen
- Muscles of Shoulder and ArmDokument3 SeitenMuscles of Shoulder and ArmAhadNoch keine Bewertungen
- Anatomy - CH 6 & 7Dokument7 SeitenAnatomy - CH 6 & 7cpNoch keine Bewertungen
- Anatomy Concept Book AtfDokument246 SeitenAnatomy Concept Book AtfRishi ShekharNoch keine Bewertungen
- Anatomy Tables SarahDokument4 SeitenAnatomy Tables Sarahanasadel1234.1Noch keine Bewertungen
- Muscle Origin/Insertion/Action/Innervation Chart Muscles of Upper Extremity Muscle Name Origin Insertion Action InnervationDokument11 SeitenMuscle Origin/Insertion/Action/Innervation Chart Muscles of Upper Extremity Muscle Name Origin Insertion Action InnervationNurul Afiqah Fattin AmatNoch keine Bewertungen
- Muscle Origin Insertion Nerve Action Comment ShoulderDokument10 SeitenMuscle Origin Insertion Nerve Action Comment ShoulderAdam IrsyaddyraNoch keine Bewertungen
- Arms v2Dokument28 SeitenArms v2Richard DahildahilNoch keine Bewertungen
- Lapsus Fraktur Neck FemurDokument32 SeitenLapsus Fraktur Neck FemurZóélkårnåín PhåntómhívéNoch keine Bewertungen
- Lecture 9 - The Wrist and Hand Regions - Jones - Full Slides PDFDokument77 SeitenLecture 9 - The Wrist and Hand Regions - Jones - Full Slides PDFAustin KellyNoch keine Bewertungen
- Ulnar Nerve Examination For Ulnar Nerve PalsyDokument14 SeitenUlnar Nerve Examination For Ulnar Nerve Palsyalimran MahmudNoch keine Bewertungen
- Muscle Origin Insertion Innervation Actions: ShoulderDokument5 SeitenMuscle Origin Insertion Innervation Actions: ShoulderSíofra MurphyNoch keine Bewertungen
- 01 Motor SystemDokument51 Seiten01 Motor SystemAhmed Adel SaadNoch keine Bewertungen
- Motor System:: BackgroundDokument12 SeitenMotor System:: BackgroundAda SandeepNoch keine Bewertungen
- Spinal Cord InjuriesDokument109 SeitenSpinal Cord InjuriesGurinder GillNoch keine Bewertungen
- Nerve Supply To The Upper Limb: Laura Jayne Watson November 13, 2015Dokument15 SeitenNerve Supply To The Upper Limb: Laura Jayne Watson November 13, 2015Hacker 75Noch keine Bewertungen
- Old BrachialDokument27 SeitenOld BrachialAyesha MajidNoch keine Bewertungen
- Radial Nerve Palsy: - Aetiology, Clinical FeaturesDokument9 SeitenRadial Nerve Palsy: - Aetiology, Clinical FeaturesRoshandiep GillNoch keine Bewertungen
- Muscle Origin Insertion Innervation Actions: ShoulderDokument26 SeitenMuscle Origin Insertion Innervation Actions: ShoulderAnan SanNoch keine Bewertungen
- UL AnatomyDokument34 SeitenUL AnatomyMejNoch keine Bewertungen
- Final Bony Thorax by DanDokument7 SeitenFinal Bony Thorax by DanDanica Dela Peña BritaniaNoch keine Bewertungen
- Muscles AnatomyDokument14 SeitenMuscles AnatomyJiya JithinNoch keine Bewertungen
- Ana211 Brachial PlexusDokument8 SeitenAna211 Brachial PlexusKalu ComforterNoch keine Bewertungen
- Brachial Plexus Anatomy: Abdulaziz R. Alanzi Medical Student, Al-Imam University Riyadh, Saudi ArabiaDokument23 SeitenBrachial Plexus Anatomy: Abdulaziz R. Alanzi Medical Student, Al-Imam University Riyadh, Saudi ArabiaArybaa MeerNoch keine Bewertungen
- 1D-19 GRSANA Reviewer 1.04 - Muscles of The Shoulder RegionDokument16 Seiten1D-19 GRSANA Reviewer 1.04 - Muscles of The Shoulder RegionShaira Aquino VerzosaNoch keine Bewertungen
- Subclavius Pectoralis Minor: Axial Skeleton To Shoulder Girdles (Ventral Side)Dokument6 SeitenSubclavius Pectoralis Minor: Axial Skeleton To Shoulder Girdles (Ventral Side)馮素琴Noch keine Bewertungen
- Upper Extermity: A. SkeletalDokument24 SeitenUpper Extermity: A. SkeletalDinda BiolawatikaNoch keine Bewertungen
- Case Report Case Report On The Clinical Results of A Combined Cellular Therapy For Chronic Spinal Cord Injured PatientsDokument5 SeitenCase Report Case Report On The Clinical Results of A Combined Cellular Therapy For Chronic Spinal Cord Injured PatientsGustavo MovigliaNoch keine Bewertungen
- Nerve SupplyDokument5 SeitenNerve SupplyRerin Tampubolon100% (1)
- NeuroanatomyDokument8 SeitenNeuroanatomyNinjaNoch keine Bewertungen
- AnatomyDokument9 SeitenAnatomyfarahjurdi8Noch keine Bewertungen
- CLAVICULADokument9 SeitenCLAVICULANylla Shin Hyenna LieNoch keine Bewertungen
- Wrist Drop Claw Hand Median Nerve Palsy: Dr. Srivatsa.NDokument46 SeitenWrist Drop Claw Hand Median Nerve Palsy: Dr. Srivatsa.NMurali KarthikkNoch keine Bewertungen
- Erbs Palsy PDFDokument4 SeitenErbs Palsy PDFKamran AfzalNoch keine Bewertungen
- Does Gender Influence Learning Style Preferences of First-Year Medical Students?Dokument7 SeitenDoes Gender Influence Learning Style Preferences of First-Year Medical Students?Kamran AfzalNoch keine Bewertungen
- Brachial Plexus Injury PDFDokument2 SeitenBrachial Plexus Injury PDFKamran AfzalNoch keine Bewertungen
- Elearning: A Review of Internet-Based Continuing Medical EducationDokument11 SeitenElearning: A Review of Internet-Based Continuing Medical EducationKamran AfzalNoch keine Bewertungen
- Dr. Kamran Afzal Su IiDokument39 SeitenDr. Kamran Afzal Su IiKamran AfzalNoch keine Bewertungen
- Welcome To The Diabetic Foot Module!Dokument67 SeitenWelcome To The Diabetic Foot Module!Kamran AfzalNoch keine Bewertungen
- Diabetic Foot UlcersDokument60 SeitenDiabetic Foot UlcersKamran AfzalNoch keine Bewertungen
- Effects of Transurethral Resection of Prostate On Flow Rate and Voided Volume On Patients With Benign Prostatic HyperplasiaDokument4 SeitenEffects of Transurethral Resection of Prostate On Flow Rate and Voided Volume On Patients With Benign Prostatic HyperplasiaKamran AfzalNoch keine Bewertungen
- Stoevelaar, Herman JohanDokument232 SeitenStoevelaar, Herman JohanKamran AfzalNoch keine Bewertungen
- Effects of Transurethral Resection of Prostate (Turp) On Uroflowmetry Parameters On Patients Having Benign Prostatic HyperplasiaDokument6 SeitenEffects of Transurethral Resection of Prostate (Turp) On Uroflowmetry Parameters On Patients Having Benign Prostatic HyperplasiaKamran AfzalNoch keine Bewertungen
- Significance of Operative Parameters On Outcomes After Transurethral Resection of The ProstateDokument6 SeitenSignificance of Operative Parameters On Outcomes After Transurethral Resection of The ProstateKamran AfzalNoch keine Bewertungen
- Mri Brain and Orbits: Name Age/Gender Ref. by MRN Report Date C-5-86311 Reg. DateDokument2 SeitenMri Brain and Orbits: Name Age/Gender Ref. by MRN Report Date C-5-86311 Reg. DateArslan MunawarNoch keine Bewertungen
- Kuliah Medula SpinalisDokument85 SeitenKuliah Medula SpinalisMuhamad Thohar ArifinNoch keine Bewertungen
- Difficult Airway AlgorithmDokument48 SeitenDifficult Airway AlgorithmshikhaNoch keine Bewertungen
- Simple Strength For Difficult Times: An 8-Week Progressive PlanDokument3 SeitenSimple Strength For Difficult Times: An 8-Week Progressive PlanmarkNoch keine Bewertungen
- Inner SmileDokument1 SeiteInner SmileIon ConstantinNoch keine Bewertungen
- Body (مفردات جسم الإنسان)Dokument6 SeitenBody (مفردات جسم الإنسان)Armylova OfficialNoch keine Bewertungen
- Skeleton Axial and AppendicularDokument33 SeitenSkeleton Axial and AppendicularAnnisa Safira100% (1)
- 100 Interesting Facts About The Human BodyDokument10 Seiten100 Interesting Facts About The Human BodyhpradeepNoch keine Bewertungen
- Basic Science Anaesthesia Update 2008Dokument200 SeitenBasic Science Anaesthesia Update 2008Ruben Kovač100% (1)
- Ped 026 Sas Lesson 2Dokument20 SeitenPed 026 Sas Lesson 2Glenn PlecisNoch keine Bewertungen
- Thyroid Disorders: Dr. Lubna DwerijDokument52 SeitenThyroid Disorders: Dr. Lubna DwerijNoor MajaliNoch keine Bewertungen
- Syndesmosis GoodDokument35 SeitenSyndesmosis GoodRoger WatersNoch keine Bewertungen
- Introduction To NeuroanatomyDokument21 SeitenIntroduction To Neuroanatomybelete abyuNoch keine Bewertungen
- BIO2A03-Muscle Lecture Notes 1Dokument22 SeitenBIO2A03-Muscle Lecture Notes 1JeevikaGoyalNoch keine Bewertungen
- NCM101 Health Assessment ExaminationDokument11 SeitenNCM101 Health Assessment ExaminationJonah R. Merano100% (1)
- Chapter 1 The Human OrganismDokument12 SeitenChapter 1 The Human OrganismJenny AnneNoch keine Bewertungen
- Herniated Nucleus PulposusDokument29 SeitenHerniated Nucleus PulposusRussel JanoloNoch keine Bewertungen
- Taylor 2018Dokument16 SeitenTaylor 2018Zahra Alpi SyafilaNoch keine Bewertungen
- Case Presentation and Literature Review of Adrenal MassesDokument50 SeitenCase Presentation and Literature Review of Adrenal MassesAnas Mk HindawiNoch keine Bewertungen
- Obstructive UropathyDokument3 SeitenObstructive UropathyGerardLum100% (1)
- Chang2013 Morphometric Analysis of The Cranial Base in AsiansDokument8 SeitenChang2013 Morphometric Analysis of The Cranial Base in Asianssolodont1Noch keine Bewertungen
- Myobraces Say No To Traditional BracesDokument4 SeitenMyobraces Say No To Traditional Bracesrishabh guptaNoch keine Bewertungen
- Nexgen Legacy Lps Flex Knee BrochureDokument8 SeitenNexgen Legacy Lps Flex Knee BrochureKamelBelkhirNoch keine Bewertungen
- 18 18 1 SMDokument5 Seiten18 18 1 SMNadira NurinNoch keine Bewertungen
- MMT Elbow Extension by Sir DR UsamaDokument17 SeitenMMT Elbow Extension by Sir DR UsamaUsama SohailNoch keine Bewertungen
- Knee - Acl - Accelerated Rehabilitation Following Acl-Ptg ReconstructionDokument7 SeitenKnee - Acl - Accelerated Rehabilitation Following Acl-Ptg ReconstructionAdmirNoch keine Bewertungen
- Distasis RectiDokument6 SeitenDistasis Rectigkarthispt100% (2)
- Physical Assessment of Preeclamptic PatientDokument3 SeitenPhysical Assessment of Preeclamptic PatientAndreiNoch keine Bewertungen
- BIMC Update PresentationDokument25 SeitenBIMC Update PresentationWahyuNoch keine Bewertungen
- Final Internalmed2Dokument1.788 SeitenFinal Internalmed2Sharayu DhobleNoch keine Bewertungen