Beruflich Dokumente
Kultur Dokumente
What Is Negative About Negative Appendicectomy Rates? An Experience From A District General Hospital
Hochgeladen von
Wahyu Hendra PrabowoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
What Is Negative About Negative Appendicectomy Rates? An Experience From A District General Hospital
Hochgeladen von
Wahyu Hendra PrabowoCopyright:
Verfügbare Formate
International Surgery Journal
Narayanan A et al. Int Surg J. 2015 May;2(2):161-164
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: 10.5455/2349-2902.isj20150507
Research Article
What is negative about negative appendicectomy rates?
An experience from a district general hospital
Aravindan Narayanan1*, Shalini Sundararaman2, Lakshminarayanan Varadhan3,
Ranbir Rajput4, Vivek Gupta1, Nick Reay-Jones1
1
Department of Surgery, Lister Hospital, East and North Hertfordshire NHS Trust, Stevenage, UK
2
Department of Psychiatry, Hertfordshire Partnership University NHS Foundation Trust, Hertfordshire, UK
3
Consultant Physician, Royal Stoke University Hospital, University Hospitals of North Midlands NHS trust, Stoke on
Trent, UK
4
GP Partner and Clinical Tutor for Leicester Medical School, Maples Family Practice, Hinckley, Leicestershire LE10
1DS, UK
Received: 15 February 2015
Accepted: 22 March 2015
*Correspondence:
Dr. Aravindan Narayanan,
E-mail: aravindan.narayanan@nhs.net
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Negative appendicectomy rate is an important outcome measure following appendicectomy and there is
a huge disparity on the quoted rates amongst various institutions globally. Our aim is to explore the outcomes
following appendicectomy especially in relation to the histologically normal appendix and establish the clinical
implications.
Methods: Data was collected from the OPCS database from 2010-2012 of all emergency appendicectomies (open and
laparoscopic) and retrospective review of all consecutive negative appendicectomies were carried out in that period
with particular emphasis on per-operative findings, pathology reports and the clinical outcome.
Results: 550 open and 118 laparoscopic appendicectomy operations were performed in the study period with age
ranging from 4 to 92 years. There were 319 male and 349 female patients in the study group. The length of stay varied
from 2 days to 10 days with an average of 3.0 days. Of the patients who had negative histology for appendicitis, 66
had alternate findings at pathology. There was no 30- day readmission recorded for these patients from the negative
appendicectomy group and their post-operative pain score was significantly lower (P <0.001).
Conclusions: Although the negative appendicectomy rates are declining globally with the use of imaging modalities,
arguments for removing a macroscopically normal appendix still exists. With varied pathology noted in a
macroscopically normal appendix it is reasonable to remove it especially with resultant better clinical outcome and
perhaps probe the need for achieving lower negative appendicectomy rates.
Keywords: Acute appendicitis, Laparoscopy, Negative appendicectomy, Alternative pathology, Clinical outcome
INTRODUCTION marker traditionally and ultrasound scan and CT imaging
modalities have contributed in keeping the NAR at a
Acute appendicitis is a common reason for emergency minimum with the rates ranging from 12 to 18%. 2 Despite
admission regardless of the age group. Open the decreasing rates of NAR globally, the morbidity
appendicectomy is an important training procedure for associated with these procedures has been on the rise
junior surgeons and on average more than 50000 including prolonged length of stay, wound-related
procedures are performed annually in the UK. 1 Negative complications and death.3 Our aim was to analyse the
Appendicectomy Rates (NAR) have served as a quality outcomes following appendicectomy of all patients who
International Surgery Journal | April-June 2015 | Vol 2 | Issue 2 Page 161
Narayanan A et al. Int Surg J. 2015 May;2(2):161-164
had macroscopically normal appendix and establish the performed as per our departmental policy.
clinical implications from a district general hospital. Histopathological analysis of these 172 patients
confirmed no evidence of acute appendicitis (negative
METHODS appendicectomy) in 150 patients (106 in open
appendicectomy and 44 in laparoscopic group) whilst the
Data was collected from the OPCS database of all remaining had microscopic evidence of appendicitis.
emergency appendicectomy operations carried out at our (12.7%) 66 of the negative appendicectomy group (44%)
hospital. The local clinical effectiveness unit approved had alternate findings as per histopathology in the
our study. A two year period was defined for the study appendix (Table 1).
(2010 to 2012) and those with a clinical diagnosis of
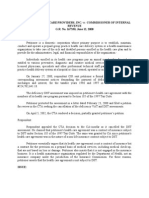
acute appendicitis (image-aided or pure clinical Table 1: Histological analysis of negative
diagnosis) were included in the study. Incidental appendicectomy cases: (macroscopically normal
appendicectomy as part of right-hemicolectomy or any appendix; histologically no evidence of appendicitis).
other procedure were excluded from the study. Clinical
suspicion for acute appendicitis varied in such scenarios Open Laparoscopic
in comparison to the study group which had a strong appendicectomy appendicectomy
clinical diagnosis of acute appendicitis based on group (n=106) group (n=44)
consultant or senior trainee review (ST6 or above) Faecoliths 11 6
including re-assessment. The main outcomes were Fibrous obliteration 16 5
negative appendicectomy rates, 30 day re-admission rates Parasites 6 2
and clinical outcome following negative appendicectomy. Non-specific
For the study, a negative appendicectomy was classed as 4 1
congestion
one where the appendix looks macroscopically normal at Lymphoid
operation and confirmed by histology with no evidence of 3 1
hyperplasia
transmural inflammation suggestive of acute appendicitis.
Crohn’s disease
An audit proforma was used to collect relevant 1 1
involving appendix
demographic data as well as ASA status, pre-op imaging,
Carcinoid 1 2
consultant presence, operating surgeon’s comment about
the appendix and the length of stay. Histopathology Serositis 1
reports were collected on all the patients and analysis of Peritonitis from
the negative appendicectomy reports were carried out in other pathology
conjunction with clinical outcomes. All complications (sigmoid 5
and/or further interventions were recorded including 30- diverticulitis & tubo-
day readmissions or re-attendance at A&E from the ovarian abscess.)
BIMS (blueberry inpatient management systems).
The NAR from our study was 19.27% in the open and
Mean with one standard deviation was computed for the 37.2% in the laparoscopic appendicectomy group. The
relevant data and statistics calculated using student t test NAR was slightly higher in the female population
and fishers exact analysis. A P value of <0.05 was compared to male patients both in the laparoscopic and
considered significant. open appendicectomy groups.
RESULTS The length of stay varied from 2 days to 10 days with an
average of 3.8 days. Pain score analysis revealed a
668 consecutive appendicectomy operations (550 open significant decrease in pain score for the negative
and 118 laparoscopic) were included in the study period appendicectomy group compared to their pre-operative
between Jan 2010 to May 2012. The age ranged from 4 score. None of the patients in the negative
years to 87 years with an average age of 27 ±16.1. appendicectomy group needed re-admission.
There were 309 male and 241 female patients in the open 16 patients in the negative histology group developed a
appendicectomy group and 11 male and 107 female wound infection which settled with conservative
patients in the laparoscopic appendicectomy group. management. 17.8% of patients in open and 27.5% of
American society of anaesthesiologists grading ranged patients in the laparoscopic group who had
from 1 to 3. Consultant presence was noted in 38 of the macroscopically normal appendix were subsequently
118 laparoscopic and 16 of the 550 open appendicectomy found to have histological evidence of appendicitis.
operations of which 12 patients were under 6 years of
age. DISCUSSION
A macroscopically normal looking appendix was noted at This study proposes a persuasive case for probing the
121 open and 51 laparoscopic appendicectomy operations description of negative appendicectomy and the focus to
(25.7% in total) but nevertheless had an appendicectomy achieve lower negative appendicectomy rates. With the
International Surgery Journal | April-June 2015 | Vol 2 | Issue 2 Page 162
Narayanan A et al. Int Surg J. 2015 May;2(2):161-164
varied findings observed on histology reports of a lower NAR.5 Is this due to variations in clinical
macroscopically normal looking appendix, it is judgement especially as a result of the shift pattern of on-
reasonable to remove the normal-looking appendix. From call involving multiple handovers? - It is debatable.
our study, we note that intra-operative assessment of the
appendix may not be reliable in laparoscopic as well as in Limitation
open operations. A significant proportion of patients with
a normal-looking appendix macroscopically will show A limitation of this study was that for the majority of
histological evidence of appendicitis.4 patients in the negative appendicectomy group, pre-
operative imaging was either not undertaken, or it was
Subgroup analysis of patient demographics revealed a not useful in influencing the clinical decision when
comparable age between those with a normal appendix utilised. Few other studies have also shown no reduction
(range 5-92 years with an average of 27 ± 16.1) and in negative appendicectomy with use of CT.8 More
histological evidence of acute appendicitis (Range of 4 - recently a multicentre study from the National Surgical
89 with an average of 28 ± 16.2; P = 0.425). Research Collaborative suggested increased use of CT
imaging to reduce negative appendicectomy rates.
Postoperative pain score based on the Verbal Numerical However about 9% of patients in their study had normal
Rating Scale (VNRS) as well as the faces pain scale appendicectomy despite CT imaging.8 Equally, others
compared favourably with negative appendicectomy have reported reduced negative appendicectomy with use
group. The pain score 24 hrs post op in those with normal of CT scan and/or ultrasonography.10,11
appendix was 4.0±1.0 (2-7) whereas in those with
histological evidence of appendicitis was 6.3 ± 1.3 (3-9); These studies and several others have focussed on
this was statistically significant - P <0.000. negative appendicectomy rates as an important outcome
and various measures to keep this at a minimum. In our
Following appendicectomy the length of stay was study we find it difficult to justify the term negative
significantly reduced in those with normal appendix 2.5 ± appendicectomy as an outcome measure where a number
0.7; range 2-6 days. The average length of stay in those of various, nevertheless significant pathological findings,
with appendicitis was 3.1 ± 1.1 (2-10); P <0.0001. were observed in the macroscopically normal-looking
Amongst the laparoscopic group, female patients had less appendix. This perhaps has greater significance when
postoperative pain score when compared to open corroborated with the improved patient outcome with
appendicectomy regardless of the pathology of the minimal morbidity as observed in our study and hence
appendix and the length of stay was also significantly less the focus should not necessarily be for striving to achieve
2.6 ± 0.7 days (P <0.0001). lower negative appendicectomy rates. A large scale
analysis of all the negative appendicectomy patients from
U. G¨uller et al. and Flum et al. in their papers have multiple centres may shed more light and establish better
reported significant reduction in morbidity and mortality standards of care.
as well cost savings achieved with a reduction in negative
appendicectomy rates.3,5 From our study, there was no Key message
mortality involved in the whole group (n=668) and 16 of
the 150 patients had wound-related infection which Higher negative appendicectomy rates does not
settled with antibiotics. 4 patients (2.8%) in the negative equate to poor performance or adverse clinical
appendicectomy group and 38 (7.2%) of those with outcome.
appendicitis on histology had readmission (P = 0.08); Laparoscopic approach favoured in female
whilst none from the negative appendicectomy had population and better tolerated.
operative intervention, 9 patients from the appendicitis Reduced length of stay with minimal morbidity in
group had percutaneous drainage of a collection under the negative appendicectomy group.
radiology guidance. Flum et al. in their study, quoted a
significantly lower negative appendicectomy rate of Funding: No funding sources
15.5% which was based on North American data and Conflict of interest: None declared
involved open appendicectomy. From our study, the The abstract of this paper was presented as a poster at
negative appendicectomy rate was higher in the the Association of Surgeons of Great Britain and Ireland
laparoscopic group at 37.2% (n=118) whilst 19.27% International Surgical Congress, 2014.
(n=550) had no evidence of appendicitis from the open Ethical approval: Not required
appendicectomy group. There are several studies which
report a similar high NAR.6 Proportion of females with REFERENCES
normal appendix was much higher than those with
pathological appendix and this was statistically 1. Hospital Episode Statistics. Admitted patient care–
significant (P <0.001). Similar findings were reported by England, 2011-2012. Total procedures and
A. Bhangu et al. from their UK based multicentre study interventions, 2013. Available at:
of appendicectomy.7 A high index of suspicion and http://www.hscic.gov.uk/catalogue/PUB08288/hosp
accurate clinical diagnosis does not always equate to a
International Surgery Journal | April-June 2015 | Vol 2 | Issue 2 Page 163
Narayanan A et al. Int Surg J. 2015 May;2(2):161-164
-episstat-admi-tot-ops-11-12-tab.xls. Accessed 2 7. Bhangu A; National Surgical Research
January 2013. Collaborative. Multicentre observational study of
2. Flum DR, Morris A, Koepsell T, Dellinger EP. Has performance variation in provision and outcome of
misdiagnosis of appendicitis decreased over time? A emergency appendicectomy. Br J Surg.
population-based analysis. JAMA. 2001;286:1748- 2013;100:1240-52.
53. 8. Myers E, Kavanagh DO, Ghous H, Evoy D,
3. Flum DR, Koepsell T. The clinical and economic McDermott EW. The impact of evolving
correlates of misdiagnosed appendicitis: nationwide management strategies on negative appendicectomy
analysis. Arch Surg. 2002;137:799-804. rate. Colorectal Dis. 2010;12:817-21.
4. Roberts JK, Behravesh M, Dmitrewski J. 9. Frei SP, Bond WF, Bazuro RK, Richardson DM,
Macroscopic findings at appendicectomy are Sierzega GM, Reed JF. Appendicitis outcomes with
unreliable: implications for laparoscopy and increasing computed tomographic scanning. Am J
malignant conditions of the appendix. Int J Surg Emerg Med. 2008;26:39-44.
Pathol. 2008;16:386-90. 10. McGory ML, Zingmond DS, Nanayakkara D,
5. Guller U, Rosella L, McCall J, Brügger LE, Maggard MA, Ko CY. Negative appendectomy rate:
Candinas D. Negative appendicectomy and influence of CT scans. Am Surg. 2005;71:803-8.
perforation rates in patients undergoing laparoscopic 11. Jones K, Pen˜a AA, Dunn EL, Nadalo L, Mangram
surgery for suspected appendicitis. Br J Surg. AJ. Are negative appendectomies still acceptable?
2011;98:589-95. Am J Surg. 2004;188:748-54.
6. Andersson R, Hugander A, Thulin A, Nystr¨om PO,
Olaison G. Indications for operation in suspected DOI: 10.5455/2349-2902.isj20150507
appendicitis and incidence of perforation. BMJ. Cite this article as: Narayanan A, Sundararaman S,
1994;308:107-10. Varadhan L, Rajput R, Gupta V, Reay-Jones N. What
is negative about negative appendicectomy rates? An
experience from a district general hospital. Int Surg J
2015;2:161-4.
International Surgery Journal | April-June 2015 | Vol 2 | Issue 2 Page 164
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- NSG 324 Literature Review Final DraftDokument6 SeitenNSG 324 Literature Review Final Draftapi-521018364Noch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Tax Banggawan2019 Ch.15-ADokument12 SeitenTax Banggawan2019 Ch.15-ANoreen LeddaNoch keine Bewertungen
- A Complete Healthcare System: MaccabiDokument30 SeitenA Complete Healthcare System: MaccabiEnglishAccessibilityNoch keine Bewertungen
- PASIEN DIGESTIF OHO - 2 Januari 2019 (R1, R2B, R3, R4B)Dokument2 SeitenPASIEN DIGESTIF OHO - 2 Januari 2019 (R1, R2B, R3, R4B)Wahyu Hendra PrabowoNoch keine Bewertungen
- WIDJI Tuesday, 07-05-2019Dokument2 SeitenWIDJI Tuesday, 07-05-2019Wahyu Hendra PrabowoNoch keine Bewertungen
- Tuesday, 7 May 2019: Ren/Bro/Sel/Put/Tom/Whs/Raf/Rdp/Rhs/Yda/ Snu/VleDokument27 SeitenTuesday, 7 May 2019: Ren/Bro/Sel/Put/Tom/Whs/Raf/Rdp/Rhs/Yda/ Snu/VleWahyu Hendra PrabowoNoch keine Bewertungen
- Tuesday, 7 May 2019: Ren/Bro/Sel/Put/Tom/Whs/Raf/Rdp/Rhs/Yda/ Snu/VleDokument26 SeitenTuesday, 7 May 2019: Ren/Bro/Sel/Put/Tom/Whs/Raf/Rdp/Rhs/Yda/ Snu/VleWahyu Hendra PrabowoNoch keine Bewertungen
- Duty Picture Tuesday, 07-05-2019Dokument68 SeitenDuty Picture Tuesday, 07-05-2019Wahyu Hendra PrabowoNoch keine Bewertungen
- 3Dokument232 Seiten3Dipeshwari ThakreNoch keine Bewertungen
- Contoh Surat Lamaran EnglishDokument4 SeitenContoh Surat Lamaran EnglishPurwanti Nurindah SariNoch keine Bewertungen
- Phil. Health Care v. CirDokument2 SeitenPhil. Health Care v. CirPixie Dust100% (2)
- FINAL PostOperative Care Guideline Kidney Transplant RecipientDokument75 SeitenFINAL PostOperative Care Guideline Kidney Transplant RecipientJorge AlvarezNoch keine Bewertungen
- 4+Roadmap+to+NABH+ +finalDokument18 Seiten4+Roadmap+to+NABH+ +finalSameer BugdeNoch keine Bewertungen
- WasdabDokument13 SeitenWasdabfakhri84Noch keine Bewertungen
- Communication Aid To Capacity Evaluation CACEDokument95 SeitenCommunication Aid To Capacity Evaluation CACEStef StenfordNoch keine Bewertungen
- Knowledge, Attitude and Practices (KAP) Studies Conducted Amongst Medical Students of IndiaDokument6 SeitenKnowledge, Attitude and Practices (KAP) Studies Conducted Amongst Medical Students of IndiaAnonymous x8fY69CrnNoch keine Bewertungen
- Journal Homepage: - : IntroductionDokument10 SeitenJournal Homepage: - : IntroductionIJAR JOURNALNoch keine Bewertungen
- MG II S3-The Hospital-Medical VocabularyDokument4 SeitenMG II S3-The Hospital-Medical VocabularyIuliana RaduNoch keine Bewertungen
- The Catholic University of Korea, Seoul St. Mary's Hospital: Contact PointDokument1 SeiteThe Catholic University of Korea, Seoul St. Mary's Hospital: Contact PointAhmed AlhadiNoch keine Bewertungen
- Week 4 - Chapter 4Dokument19 SeitenWeek 4 - Chapter 4Elmer Gatchalian100% (1)
- Bahan Inc TranslateDokument8 SeitenBahan Inc TranslateDedi Irawandi Angela NursisNoch keine Bewertungen
- Alexander FlemingDokument10 SeitenAlexander FlemingA. DuqueNoch keine Bewertungen
- ARMM List of L1 and L2 HospitalsDokument1 SeiteARMM List of L1 and L2 HospitalsMarc Eric RedondoNoch keine Bewertungen
- 06 Disaster WardsDokument15 Seiten06 Disaster WardserwinNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care PlandeliejoyceNoch keine Bewertungen
- Pars by AR - MELBIN BIJU & AR - ASLAMA ASHRAFDokument18 SeitenPars by AR - MELBIN BIJU & AR - ASLAMA ASHRAFARUN GEORGENoch keine Bewertungen
- Estimationpart 1Dokument42 SeitenEstimationpart 1kajale_shrikant2325Noch keine Bewertungen
- Kardex SystemDokument43 SeitenKardex SystemBlanche MillizcentNoch keine Bewertungen
- Title of The ThesisDokument12 SeitenTitle of The ThesisVi RusNoch keine Bewertungen
- Communication Gaps in Nursing PDFDokument6 SeitenCommunication Gaps in Nursing PDFAnonymous vUl83IptiSNoch keine Bewertungen
- Class Diag ExDokument7 SeitenClass Diag ExdamannaughtyNoch keine Bewertungen
- Scrub Typhus: The Re-Emerging Threat - Thesis SynopsisDokument17 SeitenScrub Typhus: The Re-Emerging Threat - Thesis SynopsisRajesh PadhiNoch keine Bewertungen
- Ofocn PowerpointDokument15 SeitenOfocn Powerpointapi-238242808Noch keine Bewertungen
- The Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients With Chest PainDokument10 SeitenThe Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients With Chest PainGrace Angelica Organo TolitoNoch keine Bewertungen
- Redford's ResponseDokument5 SeitenRedford's ResponsepkGlobalNoch keine Bewertungen