Beruflich Dokumente
Kultur Dokumente
Laboratory Handbook PDF
Hochgeladen von
Reymi ThenOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Laboratory Handbook PDF
Hochgeladen von
Reymi ThenCopyright:
Verfügbare Formate
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
LABORATORY
HANDBOOK
APRIL 2019 EDITION
Reference: CAEC Registration I.D. No. 1043
Written by: Laboratory Handbook Group
Peer reviewer: Prof J R Bonham
Approved: February 2019
Review Due: March 2020 (do not use this edition after this date)
Purpose
This handbook gives pre-analytical information and guidance to laboratory
service users when requesting tests and includes:
Details of services provided
Laboratory contact details and opening hours
Details of phlebotomy services
Instructions for completing sample and request form information
Arrangements for transporting samples to the laboratories
Point of care testing
Test table of analyses provided including details of specific sample
requirements
Intended Audience
All users of laboratory services at Sheffield Childrens NHS Foundation Trust
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 1 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 2 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Contents
GENERAL INFORMATION 5
INTRODUCTION 5
INTENDED AUDIENCE 5
REFERENCES 5
DIVISION CONTACT DETAILS 8
PHLEBOTOMY SERVICES 8
SPECIMEN COLLECTION BY CLINICAL STAFF 10
PHLEBOTOMY AND PATIENT IDENTIFICATION 10
THE COMPLETION OF REQUEST FORMS 12
PROTECTION OF PERSONAL DATA AND INFORMATION 14
LABELLING OF PATHOLOGICAL SAMPLES 14
PACKAGING SAMPLES 16
SAMPLE TRANSPORTATION 17
REPORTS 19
UNCERTAINTY OF MEASUREMENT 21
POINT OF CARE TESTING 21
RELATED LABORATORY SERVICES IN SHEFFIELD 27
CLINICAL CHEMISTRY 31
LOCATION OF DEPARTMENT 31
CONTACT DETAILS 31
LABORATORY OPENING TIMES 32
SERVICES PROVIDED 32
SPECIALISED BIOCHEMICAL SERVICES 33
URGENT REQUESTS 37
REQUESTING ADDITIONAL INVESTIGATIONS 39
LIMITATIONS OF RESULTS 40
CONSENT 40
REFERENCE RANGES 40
DEPARTMENT OF PAEDIATRIC HAEMATOLOGY AND BLOOD BANK 61
LOCATION OF DEPARTMENT 61
CONTACT DETAILS 61
ENQUIRIES 62
LABORATORY OPENING TIMES 62
SERVICES PROVIDED 62
URGENT REQUESTS 66
REQUESTING ADDITIONAL INVESTIGATIONS 68
LIMITATIONS OF RESULTS 68
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 3 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
REFERENCE RANGES 69
HISTOPATHOLOGY DEPARTMENT 70
LOCATION OF DEPARTMENT 70
CONTACT DETAILS 70
LABORATORY OPENING TIMES 70
OTHER INVESTIGATIONS 72
URGENT REQUESTS 75
LIMITATIONS OF RESULTS 76
TURNAROUND TIMES 76
SHEFFIELD DIAGNOSTIC GENETICS SERVICE 78
LOCATION OF THE DEPARTMENT 78
CONTACT DETAILS 78
ENQUIRIES AND RESULTS 78
LABORATORY OPENING TIMES 79
SERVICES PROVIDED 79
URGENT REQUESTS 82
REQUESTING ADDITIONAL INVESTIGATIONS 83
LIMITATION OF RESULTS 83
CONSENT 84
ARRANGEMENTS FOR MICROBIOLOGY, VIROLOGY AND IMMUNOLOGY
87
MICROBIOLOGY 87
ANTIBIOTIC ASSAYS 89
VIROLOGY SERVICES 91
IMMUNOLOGY SERVICES 93
CSF SAMPLES 94
SPECIMEN CONTAINERS 97
A-Z LABORATORY TEST/CONDITIONS LIST 100
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 4 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
GENERAL INFORMATION
INTRODUCTION
The Diagnostic Pathology Laboratories form part of the Division of Pharmacy,
Diagnostics and Genetics at Sheffield Children’s NHS Foundation Trust. There
are four laboratory specialities (listed below) and a mortuary service.
Clinical Chemistry
Haematology and Blood Bank
Histopathology and Mortuary
Sheffield Diagnostic Genetics Service
This handbook has been prepared following consultation with users of laboratory
services to give pre-analytical information and guidance to laboratory service
users when requesting tests. Any comments or suggestions for improvement
should be directed to the Laboratory Quality Manager.
INTENDED AUDIENCE
This handbook is for the use of all users of laboratory services at Sheffield
Childrens Hospital. This edition of the handbook should not be used after the
stated review date.
Before requesting tests, regard should also be given to Asher’s Criteria (BMJ
1954, ii-460)
1. Why am I ordering this test?
2. What am I going to look for in the result?
3. If I find it, will it affect my diagnosis?
4. How will this affect my management of the case?
5. Will this ultimately benefit the patient?
GENERAL INFORMATION
REFERENCES
In addition to the information provided in this handbook the Trust provides
Clinical and Medical guidelines for use within SC(NHS)FT. These are available
on the Trust intranet
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 5 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
http://nww.sch.nhs.uk/Health%20Services%20Management%20-
%20SCH/cec/index.asp
http://nww.sch.nhs.uk/Health%20Services%20Management%20-
%20SCH/pages/guidelines.htm
QUALITY
Quality Commitment
Provided that the guidelines as detailed in this handbook are followed all service
users, including referring laboratories, can expect a commitment to continued
quality from the Diagnostic Pathology Laboratories for all work and services that
are provided on their behalf. The Diagnostic Pathology Laboratories will also
proactively engage with service users and institutions that refer tests and will
notify them of any significant issues or changes (including issues with EQA
performance and turnaround times) that can affect results or interpretations that
are given to them or that may impact on patient management and care.
External Quality Assessment and Laboratory Accreditation
We have an established quality management system and all our laboratories
participate in regular audit and external quality assessment schemes such as
the United Kingdom Accreditation Service (UKAS) for ISO15189, Medicines and
Healthcare products Regulatory Agency (MHRA), the Human Tissue Authority
(HTA) and the Joint Accreditation Committee-ISCT (Europe) & EBMT (JACIE).
ISO 15189:2012 which is an international standard which specifies the
requirements for quality and competence for medical laboratories. The
ISO15189 standard has replaced the Clinical Pathology Accreditation (CPA)
standards, which our laboratories were accredited to since their introduction in
1996. The accreditation process involves annual visits by the United Kingdom
Accreditation Service (UKAS) to ensure compliance against the standard.
Accreditation provides assurance to users of the Laboratory Medicine service
that we are providing the best quality service.
A full list of all accredited tests provided by our laboratories are detailed in their
Schedule of Accreditation. Each Schedule of Accreditation can be viewed by
entering the UKAS Reference Number in the search field at the link below:
https://www.ukas.com/search-accredited-organisations
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 6 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Laboratory UKAS Reference
Clinical Chemistry 10139
Haematology 8091
Histopathology 8093
Sheffield Diagnostics Genetics Service 8652
Some tests provided by our laboratories are not included within the Schedule of
Accreditation. These tests are managed within the Laboratory Quality
Management System. If further information is required please contact the
laboratory via the contact details in their section of this handbook.
Further information can be found on the UKAS website
http://www.ukas.com
Quality Assurance
All our laboratories participate in national external quality assurance schemes to
monitor the accuracy and precision of its analyses. Internal quality control is
used to check the validity of results on a day-to-day basis.
Quality Indicators
The laboratories have established a selection of key quality indicators to monitor
and evaluate performance throughout critical aspects of pre-examination,
examination and post-examination processes. Primarily we monitor these
quality indicators to evaluate the laboratory’s contribution to patient care. This
monitoring process is planned, which includes establishing the objectives,
methodology, interpretation, limits, action plan and duration of measurement. To
ensure their continued appropriateness, we review the quality indicators at least
annually as part of our Laboratory Annual Management Review pro cess.
Quality Concerns and Complaints
If you have any issues about the quality of service you receive please contact
GENERAL INFORMATION
the Laboratory Quality Manager, the appropriate Laboratory Manager, the
Associate Director or a Clinical Director. Contact names and numbers are given
in the Contact Details sections of this handbook.
Alternatively health professional service users who wish to make any comments
or suggestions may use the feedback form on the Trust website
https://www.sheffieldchildrens.nhs.uk/laboratory-medicine/
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 7 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
DIVISION CONTACT DETAILS
Sheffield Children’s Hospital
Hospital switchboard 0114 271 7000
Diagnostic Pathology Laboratories
Clinical Directors Prof Ann Dalton Ext 17004
Prof Jim Bonham Ext 53831
Associate Director Sara Elliott Ext 53615
Laboratory Quality Manager Karen Bennett Ext 17240
Magdalena Ext 53885
Laboratory Deputy Quality Manager
Burgess
Catherine Ext 53884
Laboratory Quality Assistant
Bounekhla
Paul Sharman- Ext 53064
Division IT Manager
Armitage
PHLEBOTOMY SERVICES
A phlebotomy service is provided for capaillary blood sample collection on the
wards.
1. Collection of capillary blood samples on wards
Samples are collected by laboratory staff according to the following schedule.
VENUE DEPT RESPONSIBLE COLLECTION TIME
(Monday to Friday)
Children’s Wards Clinical Chemistry & 09.30
Haematology
Children’s Wards (NSU, Clinical Chemistry 13:30
HDU & ICU only)
N.B. On Saturdays, Sundays and bank holidays a collection at 09:30 is
made at the Children’s Hospital for urgent Clinical Chemistry and
Haematology requests. Laboratory staff are unable to carry out capillary
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 8 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
collections at any other time, and venous samples will therefore be
required if request forms are not left out for this round before 9 am.
It is important that request forms are written up before these rounds commence
or phlebotomy requests may be missed.
The weekday 09:30 round is carried out by a team of 4 staff. The other rounds
(including the weekend rounds) are carried out by a maximum of 2 staff, and
therefore requests should be limited to emergencies and new admissions
only.
Outside these times the laboratories can only respond to urgent requests
depending on staff availability.
It is the requester’s responsibility to consider the impact and safety of the patient
on the volume of blood withdrawn by phlebotomy. Please be aware that the
amount of blood collected is always matched to the tests or profiles requested.
It therefore may not be possible to add on extra tests by subsequently phoning
the laboratory. Microbiology samples e.g. gentamycins etc will be collected by
capillary only if they coincide with the scheduled ward rounds. All Microbiology
requests are now analysed at the NGH.
2. Thumb Prick Sample Collection for Blood group and Save Serum/Cross
Match
Blood Bank testing of capillary samples is carried out provided the following are
observed. Exceptions may be discussed with the Consultant Haematologist.
1. Patient must be aged eight years old or under.
2. The patient’s expected potential requirement for blood must be one unit
or under.
3. The patient must have a fully completed and signed blood bank request
form.
4. Collection of blood for other tests at the same time is limited to a FBC.
Deferring tests for later occasions may be considered after discussion
GENERAL INFORMATION
with parents and ourselves.
5. Should serological problems be encountered a venous blood sample will
be needed urgently.
6. Performing a group and save while the patient is an out patient is to be
encouraged. It will forewarn of problems before admission.
7. 1ml EDTA sample should be obtained
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 9 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
SPECIMEN COLLECTION BY CLINICAL STAFF
Clinical staff are responsible for collecting blood samples themselves in the
following instances.
1. If laboratory staff are not available
2. If venous or arterial blood samples are required
3. If samples are required from patients who are distressed, who carry
serious risk of infection or who refuse a capillary sample
4. Any circumstances where procedures other than straightforward
capillary blood collection might be involved
5. If checking a high or low potassium result (Venous or arterial blood
required)
Blood Sampling from Lines and Catheters
Samples collected from lines are often contaminated with the stagnant or
infused fluid in the line. The results of tests may be so extreme as to be
obviously in error. Contamination of a lesser degree is more likely and may be
impossible to spot.
Skin Biopsies
Requests for skin biopsy cultured fibroblasts from SCH patients must be
accompanied by a consent form. Guidelines for sample collection and consent
forms are available on request (contact Dr Simon Olpin or Joanne Croft on 0114
271 7267 (answer phone) simon.olpin@sch.nhs.uk.) For further information and
details of arrangements for skin biopsy requests from external hospitals please
refer to the Skin Biopsies section on page 31 of this handbook.
PHLEBOTOMY AND PATIENT IDENTIFICATION
When taking blood or any other pathological samples the instructions provided in
sections 3.1, 4.2 and 4.4 of the Trust’s Patient Identification Policy must be
observed.
Laboratory personnel who take capillary blood samples from in-patients follow
the procedure given below. It is equally applicable to other staff groups who take
pathological samples.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 10 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen containers should not be labelled in advance of receiving the
specimen.
At the bedside, obtain the patient’s name and date of birth by asking the
patient/parent carer to state it (do not merely get confirmation of a name
you state). Check this information is compatible with the patient
identification band on wrist or ankle.
If the patient is unable to tell you their name, refer to the identification
band and, if possible verify the information by asking the parents/carer
or another member of the clinical staff who knows the patient.
If the patient is unable to tell you and they do not have an identification
band, ask the patient’s parent/carer if present or another member of the
(clinical staff who knows the patient to identify the patient by name, and
date of birth). An identification band should then be generated and
secured to the patient as soon as possible. Collection cannot go
ahead if the band is absent, and phlebotomists are not obliged to wait
until this is completed.
Check that the details on the identification band match the details given
with those provided on the request form.
The patient must not be bled in the absence of a request form or an
alternate agreed test request arrangement.
Proceed with the collection if all is correct. Note: For patients who
cannot wear identification bands on wrist or ankle it is acceptable to
have the band pinned to their clothing. Collection cannot go ahead if
the band is absent.
Once the specimen is received into the container, the patients
identification band must be re-checked before completing the details on
the container to ensure the correct details are matched to this specimen.
The absence of an identification band, or the presence of conflicting
details on the band and request form, are considered as breaches of
Trust policy. Incidents of this nature should be referred to the Ward
Manager and the patient must not be bled.
The sample must be labelled at the bedside. This is Trust policy and is
audited.
GENERAL INFORMATION
Sample and request form information must relate to the person from whom the
sample was taken. Samples labelled with ‘mother of’, ‘father of’ or ‘baby of’ etc
will not be accepted. The only exceptions to this are solid tissue samples for
pre-natal cytogenetic analysis, and fetuses up to 18 weeks gestation that are for
post mortem examination.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 11 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
THE COMPLETION OF REQUEST FORMS
All request forms must contain a minimum of the following essential
information:
1. Full name (initials will be classed as missing information)
2. DoB (age only will be classed as missing information)
3. At least one of the following
Hospital number
A/E or Major Incident Number
NHS number.
Clinical Genetics Family ID
4. Name of the requesting consultant (initials or full name) or location
(ward/department) to which results are to be sent.
5. Test required.
6. Blood Bank request forms must also include details of any special
requirements the patient may have i.e. irradiated (see back of request
form), or details of any underlying conditions that mean the patient could
need special products (see back of request form), and state if the patient
is pregnant. Details of any recent transfusions (including those
performed elsewhere) are also required.
The following information is also highly desirable
7. Name of the person collecting/obtaining the sample.
8. Date & time sample(s) taken (where relevant)
9. Sample type
10. Clinical details (full and appropriate clinical details including
circumstances that may increase the risk of infection e.g. relevant travel
history must be included)
11. Patient’s address including postcode
12. Patient’s sex
13. Clinician’s bleep number
Clinical details and the patient’s age are particularly important in paediatric
requesting so that laboratory staff may:
1. Understand the reason for the request
2. Interpret the results
3. Consider the need for further investigations
4. Advise and assist the clinical staff concerning the results obtained.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 12 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Additional information may be appropriate for specialised metabolic.
toxicological or blood bank requests.
It is the responsibility of the requestor to ensure that a completed laboratory
request form accompanies every sample for which an analysis is required. The
only exemptions to this rule are:
1. When more than one tube is required to provide sufficient sample for the
test.
2. Routine Newborn screening where a completed Guthrie card is sufficient
Please use the correct request form specified as follows:
Green Clinical Chemistry SCH requests for Clinical Chemistry
request form
Pink Haematology request SCH requests for Haematology (NOT for
form Blood Bank – see below)
White Blood Bank request Essential for requests for group, group and
form save serum, group and cross-match, DCT
Yellow Histopathology SCH requests for Histopathology (except
request form Gastrointestinal Biopsies - see below)
White A4 Gastrointestinal SCH requests for Gastrointestinal Biopsies
Biopsies request form (Histopathology) only
Blue Microbiology, SCH requests for Microbiology, Immunology
Immunology, Virology and Virology
request form
GENERAL INFORMATION
Sheffield Diagnostics Requests for Sheffield Diagnostics Genetics
Genetics Service request Service tests (request form is available from
form the Trust website
https://www.sheffieldchildrens.nhs.uk/sdgs/)
If exceptional circumstances dictate that a test request is made verbally or by
letter, then this request must be followed by a completed request form within 7
days.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 13 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
High Risk Samples
Medical staff must also indicate on the request form if the sample to be sent to
the laboratory might carry a risk of Category 3 infection (using the yellow Cat 3
labels on both the request form and sample). An indication should also be made
on the form if the patient has a communicable disease such as rubella, for the
protection of any laboratory staff who might attend the patient.
Please alert the histopathology laboratory prior to sending any high risk samples
to them if possible. Such samples must be placed in 10% formalin and
transported to the laboratory by hand. The request form for these samples must
also identify the biohazard within the clinical details. Samples for other
reference labs related to the same case, should be sent directly to the
appropriate laboratory.
PROTECTION OF PERSONAL DATA AND INFORMATION
Personal data and information on request forms is required in order for the
laboratories to operate and may be stored on laboratory computer files. The
intent of the laboratories is to ensure that any personal data and information is
treated lawfully and in accordance with the NHS requirements concerning
confidentiality and information security standards. To this end we fully endorse
and adhere to the Trust Data Protection Policy, the requirements of which are
primarily based upon the Data Protection Act 1998 which is the key piece of
legislation covering security and confidentiality of personal information.
LABELLING OF PATHOLOGICAL SAMPLES
When collecting and labelling samples, the criteria for patient identification
(outlined earlier) must be followed. Sample and request form information
must also be compatible. Samples will only be accepted for analysis if
minimum criteria are met. This responsibility lies with the person collecting
the sample. Failure to meet these requirements may result in the sample being
rejected.
Minimum Criteria
As defined by laboratory policy all pathological samples sent to the laboratory
must contain a minimum of the following information:
1. Surname /family name
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 14 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
2. Forename (or Baby, Twin One/Two, Triplet One/Two/Three etc, if
forenames have not been given. Initials will be classed as missing
information)
3. At least one of the following
Date of birth (age only will be classed as missing information)
Hospital registration number
A/E or Major Incident Number
NHS number
The Clinical Genetics Family ID number must also be present on samples
sent from Clinical Genetics
And ideally for samples being tested for patient monitoring purposes the
following should also be included.
Date sample taken
Sample type
The ‘ward’ space on bottle labels may be used to write the hospital/A/E/NHS
number , ward is not required.
All samples for Blood Bank must contain a minimum of the following
information:
1. Surname /family name
2. Forename (or Baby, Twin One/Two, Triplet One/Two/Three, etc, if
forenames have not been given. Initials will be classed as missing
information)
3. Date of birth (age only will be classed as missing information)
4. Any of the following
Hospital registration number
A/E or Major Incident number
NHS number
And ideally blood transfusion samples should be signed/initialled by the primary
GENERAL INFORMATION
sample taker.
N.B. When cross matching for infants up to 6 months of age the laboratory
prefers to use maternal plasma in addition to the baby sample. Maternal
samples must be labelled with the mother’s surname, forename and DoB. Such
samples must not be labelled with the child’s hospital number.
Ideally all samples should be labelled by hand. The use of addressograph
labels for labelling blood samples is not encouraged (especially for small
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 15 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
sample bottles), and blood samples for Blood Bank shall not be accepted if they
are labelled as such. However it is acceptable to use addressograph labels for
the larger urine and faeces samples. If addressograph labels are used, it is the
responsibility of the sending service user to ensure that the contents of the
sample container match the patient ID.
In the event of an unconscious child being admitted via A&E, laboratory staff
will accept a sample clearly labelled with: A unique identifier i.e. A&E
number/Major Incident Number, Child’s sex and approximate age.
Laboratory staff are instructed not to amend details on either the sample or the
request form. If you require further details of the sample acceptance policy
please contact the laboratory.
PACKAGING SAMPLES
In signing a request form the person making the request assumes responsibility
under Section 7 of the Health and Safety at Work Act and must adhere to the
following guidelines regarding the labelling and packaging of samples to
minimise the danger of infection.
Every sample must be enclosed in a suitable, leak proof, primary
container.
The sample must be contained in a transparent leak proof plastic
transport bag.
Containers for large specimens, such as some Histopathology or 24-
hour urine specimens, may be enclosed in individual clear plastic sacks,
sealed to contain any leakage.
The request form must be separated from the specimen. Please place
the specimen inside the plastic transport bag attached to the request
form. For larger containers the request from should be securely taped
to the outside of the transport sack containing the specimen.
The request form should not be attached to the sample container or be
used as a sample label.
For Category 3 risk patients the requester must include full and
appropriate clinical details and danger of infection labels on both
request form and sample.
Any labels and stickers used must be self-adhesive.
Pins, staples, and heat sealed bags should not be used.
Plastic transport bags must not be re-used.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 16 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
If any samples are to be transported by postal, courier or taxi service directly
from the clinical area to locations outside the Trust, they must be packed and
labelled according to the regulations for the transport of dangerous goods.
Please contact the laboratory for details of this requirement. Specimens for
transport by post should always be labelled as ‘First Class – Royal Mail only’.
SAMPLE TRANSPORTATION
On-site specimen transport
Primary sample transportation to SCH laboratories is the Pneumatic Tube
System (PTS) and Stations are located in A&E, HDU, PICU, Ward 6, CF Unit,
OPD, Ward 3, Ward 7, Theatres, Oncology/HaemOPD, Theatre Assessment
unit, Ward 3, Ward 4, and Ward 5, Clinical Chemistry, Histopathology,
Haematology and SDGS. Samples can be sent directly to all Pathology
Laboratories from any of these stations. Copies of operating and breakdown
instructions for the pneumatic tube system (PTS) can be found in each of these
areas. Please ensure that the transport pods are properly closed, and do not
attempt to send samples via the pneumatic tube system (PTS) unless they are in
a pod.
N.B Urgent frozen sections from theatre and specimens for histopathology
that have a high risk of infection must not be sent via the pneumatic tube
system (PTS).
For transport of routine samples not suitable for the pneumatic tube system
(PTS) there are also scheduled sample collection rounds of ward and clinic
areas carried out by the Medical Laboratory Assistant (MLA) at the following
times 09:00, (11:30 if the pneumatic tube system (PTS) is not working),
13:30 and 15:45 Monday - Friday. These rounds take about 15 minutes. All
samples for collection must be properly packaged and left at the agreed point on
each ward or clinic area. If there is visible leakage of the specimen prior to
transport, this must be reported to the nurse in charge and it be requested that
GENERAL INFORMATION
the specimen is placed in an additional sealed transport bag.
Specimens fixed in formaldehyde should have the lid securely closed and
contain sufficient formaldehyde to keep the sample moist during transit but to
keep the risk of spillage to a minimum. They should have a formaldehyde
hazard label attached to the outside of the container and be placed into a
secondary leak proof bag. If there is leakage of formalin, the formalin spillage
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 17 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
procedure must be followed; in these cases please contact the Histopathology
Laboratory on 01142717264 for advice.
Specimens can also be taken to the relevant laboratory during working hours
and handed to a member of the laboratory staff. If an incident occurs during
transit, it should be immediately reported to the laboratory and if necessary ask
for assistance. Please note that urgent and fresh Histopathology samples
must be taken by hand to the department and handed directly to a member
of staff.
Some samples will need special requirements for transport e.g. should be
transported on ice, please refer to the test table of analyses at the back of this
handbook for specific requirements.
Samples suspected of biohazard category 4 organisms e.g. Ebola virus, viral
hemorrhagic fever etc, must not be sent via the pneumatic tube system (PTS).
Do not send the specimen to the laboratories.
N.B. Health and safety regulations for on-site transport stipulate that when
carrying specimens, staff must use secure specimen transport carriers.
For occasions when the MLA is not utilised, it is the responsibility of the
person carrying samples to the laboratory to ensure that samples are
carried in the green sealable sample transport bag. Under no
circumstances should anyone transport specimen containers in their
hands or pockets.
Transport of urgent samples
The pneumatic tube system (PTS) is the preferred mode of transport for urgent
samples and for transporting samples out-of-hours, with the exception of
Histopathology samples – see previous page. Urgent specimens must be
arranged with the laboratory before dispatch. Do not merely write ‘Urgent’ on
the request form and send.
Sample transport arrangements during pneumatic tube system (PTS)
failure
In the event of pneumatic tube system (PTS) failurea member of the laboratory
team will collect samples from the wards at the following tmes 09:00, 11:30,
13:30 and 15:45. Outside of these times it is the responsibility of the person
taking the sample to ensure it reaches the appropriate laboratory.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 18 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Transport of samples to STH
A regular CampusLink taxi shuttle collects samples at 09:40, 11:10, 13:10,
14:40, 16:00, and 17:10 Mon-Fri from clinical chemistry for dispatch to the NGH
and RHH laboratories; urgent samples in-between these times may also go via
urgent-taxi. Outside routine working hours, scheduled couriers call into A&E
reception at 17:30, 19:30 and 21:30 on week nights and at 08:30, 11:30, 14:30,
17:30, 19:30 and 21:30 at weekends and bank holidays.
Please note that during routine hours (09:00 -17:00 weekdays) Immunology and
tests referred to STH must be sent via the SCH Clinical Chemistry department.
Also please ensure that when requests for CSF protein, glucose and lactate are
required alongside requests for M, C & S, the CSF sample must not be sent to
Microbiology. The CSF sample is tested at SCH, and the sample for M, C & S is
tested at STH.
REPORTS
Clinical Chemistry, Haematology, Blood Bank, Histopathology, STH
Microbiology and STH Immunology Reports
From April 2012 no printed reports will be sent out from Clinical Chemistry,
Haematology, Blood Bank, Histopathology, Microbiology or Immunology, with
the exception of post mortem reports, reports to external purchasers, dynamic
function tests reports and reports for samples referred to external laboratories.
Printed post mortem reports are sent to the appropriate requesting
consultant/coroner, printed reports for other exceptions are delivered by hand to
the wards and departments at approximately 09.15 and 15.45.
Urgent reports will be telephoned if requested. The laboratory also has limits
outside of which the results are telephoned automatically. Authorised Clinical
Chemistry, Haematology, Blood Bank, Histopathology, Microbiology and
GENERAL INFORMATION
Immunology results are electronically accessible via ward/office computers
through the hospital network or directly from the PC desktop ‘ICE’ icon.
Passwords can be obtained by contacting the ICE Administrator (Ext 53268)
Using ICE desktop reporting.
ICE is available on at least one PC terminal on each ward and should be used to
access results prior to contacting the laboratory. The snowflake desktop icon is
labelled “ICE desktop reporting.”
Upon clicking the ICE Desktop reporting icon a login screen is presented
– click login
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 19 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Enter username and password (not case sensitive) and click login.
Select a ward/location from the list that represents where you are.
The system takes you straight to patient enquiry where a hospital
number or name or DOB can be entered. Click on patient reports
button in left panel. This query will always present all results available
for that patient.
If you wish to view multiple patient reports by ward then click the View
ward report icon within the left hand panel.
This will display only the 20 most recent reports for the default location.
The display defaults to patient reports at the same location as your PC
e.g. M3 or ICU however patient’s results at another location can be
viewed from any workstation by selecting an alternative from the top left
hand pull down list.
To view earlier reports click earlier reports. The default number of days
of previous results in the Ward view is 7 days. This can be changed by
the user or just keep clicking “earlier reports” to go back in time.
Cumulative report displays with graphical views are available and can
be printed.
An online manual is available by clicking manuals in the left hand pane.
The colour of each report indicates the pathology specialty.
When leaving your workstation unattended please log off using log off
button in the lower left hand panel.
The Laboratory handbook can be accessed by entering Resources.
Reports can be filtered by lab speciality and requesting clinician.
Filing of results is audited monthly to ensure reports are viewed and
acted upon as appropriate.
Users are encouraged to notify the laboratory of patient duplicates or
demographic inaccuracies. The quality of report demographics is dependant
upon the quality of data we receive. Consistent use of the hospital number
enables cumulative reports to be created and viewed.
Genetics reports
Genetics reports are sent by first class post, fax or email (by special
arrangement). Urgent rapid prenatal results are faxed directly to the referring
centres. HODS reports are transferred automatically from starlims to the HODs
website. Results are available by phone and urgent results can be telephoned or
faxed if requested.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 20 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
UNCERTAINTY OF MEASUREMENT
In clinical laboratory testing there are potential “uncertainties” that can affect test
results (for example; poor specimen collection or transport, patient related
factors such as biological variation and the presence of drugs, or other
interfering factors).
In addition, the analytical process itself is subject to some degree of inherent
variability and this is often referred to as the “reproducibility” or “imprecision” of
the method. Laboratories regularly monitor this by the use of internal quality
control samples within each batch of analysis and by comparing the results of
external quality assurance schemes designed to ensure that results are
comparable with others laboratories using similar methods.
Despite these control measures it must be recognised that variation can occur
and modestly differing sequential results may not always have clinical relevance.
The relevance of a particular result or a change in value must be considered in
light of both the reproducibility of the method and the biological variation within
the patient. If in doubt concerning the significance of a result or a change in
sequential results, a member of the laboratory or relevant clinical staff should be
contacted and they can help guide interpretation.
Providing relevant clinical details at the time that the request is made can also
clarify the significance of a particular result or a change in results.
Measurement uncertainty data for specific tests can be provided to service users
upon request.
POINT OF CARE TESTING
All POCT equipment is to be used by trained users only. The blood gas
GENERAL INFORMATION
analysers situated on NSU, ICU and A&E procedure room are connected to
Clinical Chemistry by computer link and are for the use of trained and
certificated operators e.g. Anaesthetists/Doctors/Nurses/laboratory staff only.
Training is arranged at induction: see contact details at the end of this section.
Trust policy is that unique barcodes following training are issued to certified staff
and must not be shared with others. Use of the analysers without certification or
training, or the use of another operator’s barcode are disciplinary offences;
constituting both clinical risk , and risk to this vital patient service.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 21 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Haemoglobin fractions, Electrolytes (Sodium, Potassium, Chloride,
Ionised Calcium) and Metabolites (Glucose and Lactate) are available
on each analyser.
Capillary, venous, and arterial samples for blood gas analysis should be
transported using a cardboard tray along with a completed request form
or patient addressograph label which acts as the source of patient
identification to key into the analyser. Samples must be mixed thoroughly
by rotation immediately after collection and prior to analysis to minimise
clots and the sample separating. Avoid air bubbles.
Blood glucose testing is undertaken on the wards using Accu-chek
Inform II dry chemistry hand held meters. An operator Identification
number is required to use this meter and is issued on successful
completion of training and competency assessment. All patients being
monitored for blood glucose should send a paired sample to the
laboratory for analysis daily.
POCT glucose results less than or equal to 3.1 mmol/L must have a
corroborative sample sent to the Clinical Chemistry laboratory in case of
hypoglycaemia.
Urine Specific Gravity testing using the Atago refractometer is available
on Ward 6. Staff must be trained and certificated before they use these
meters.
Urine dipstick testing is performed by trained operators using the
Clinitek Status plus analysers. A barcode is required to use this analyser
and is issued upon successful completion of training and competency
assessment.
Abbott Freestyle Optium H ketone meters are available on ITU/HDU,
Ward 3, Ward 4, A&E/AAU and Ward 5. Staff must be trained and
certified before using these instruments.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 22 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Sample
Test Collection Type Tube Notes / Comments
Type Volume
Any air present must be
expelled immediately after
collection. Mix the sample
as soon as possible after
collection to distribute the
heparin throughout the
Siemens
® 800 µl sample. Mix the
RAPIDLyte
(minimum anticoagulant thoroughly by
Arterial/Venous balanced
fill rolling the syringe between
heparin
volume) your palms at least 20
Blood Gas syringe (3ml)
times & gently inverting it
®
Siemens RAPIDPoint Whole several times. Take care to
500 Blood Gas Analyser blood avoid warming the sample.
Never analyse a clotted
(A&E, ICU & NSU)
sample on the blood gas
analyser.
Fill the tube completely &
cap it with capillary closing
Balanced caps. Mix the sample as
heparinised soon as possible after
Capillary 100 µl
capillary collection to distribute the
(100 µl) heparin throughout the
sample & again just prior to
analysis as a minimum.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 23 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Sample
Test Collection Type Tube Notes / Comments
Type Volume
All inpatients being
Venous, arterial,
A fresh whole monitored by this glucose
neonatal, &
blood drop test strip method must
Glucose capillary whole
taken directly have a ‘paired’ fluoride
Whole blood from the
®
Accu-Chek Inform II from the 0.6 µl sample sent to the Clinical
blood finger. For
Glucose Meter finger is the Chemistry laboratory for a
neonatal patients
sample type glucose test daily.
the outer heel
of choice.
area may be used.
Always calibrate the meter
with each new box of test
strips. Use ONLY the
calibrator supplied with the
β-Ketone test strips.
(Beta-hydroxybutyrate) Test results may be
Fresh
Whole erroneously low if the
Abbott FreeStyle Capillary capillary 1.5 µl
blood patient is severely
Optium H finger-prick.
dehydrated, or severely
Ketone Meter hypotensive, in shock or in
a hyperglycaemic-
hyperosmolar state.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 24 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Sample
Test Collection Type Tube Notes / Comments
Type Volume
HbA1c Whole Capillary Fresh 1.0 µl Conditions such as
(Haemoglobin A1c) blood capillary haemolytic anaemia,
® finger-prick. polycythaemia,
Siemens DCA Vantage
homozygous HbS and
HbA1c Analyser
HbC, can result in
(Diabetic clinics). decreased life span of the
red blood cells which
causes HbA1c results to be
lower than expected.
Urine Collect urine as Z10 0.2 ml
Urine Specific Gravity
per ward policy.
Atago UG-1 Digital
Urine S.G
Refractometer
(Ward 6)
Urine A first voided mid- Z10 10 ml
Urinalysis
stream morning
Siemens Clinitek urine is best for
Status+ routine analysis.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 25 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Reporting Point of Care Test results
Test results must be transcribed onto patient charts and/or nursing notes as
follows:-
1. Transcribe PCCU blood gas reports onto ward charts/patient notes.
2. Sign off all transcribed results as checked.
3. Always include the date and time of test.
4. Always identify the operator.
5. Identify all results from POCT equipment as 'POCT' results in the patient
notes, to distinguish results from those obtained by the Clinical
Chemistry main laboratory analysers.
6. Attach adhesive urine dipstick reports to patient notes.
7. Highlight all abnormal results generated by POCT equipment according
to local ward procedures.
8. Document all actions taken in response to POCT results in the patient
notes e.g. notification to medical staff.
The Clinical Chemistry Duty Biochemist (bleep 095) is available for advice
and/or interpretation of results.
The Point of Care Testing Committee, chaired by Mrs Camilla Scott, oversees all
ward based testing and any concerns, queries or proposed developments
should be directed to this group. Please note that due to accreditation process
changes POCT services are not currently accredited.
POCT Co-ordinator Ext 17305 Bleep 053
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 26 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
RELATED LABORATORY SERVICES IN SHEFFIELD
Telephone
Ext
Laboratory Medicine Directorate Dr B Perunovic 61424
Sheffield Teaching Hospitals (Clinical Director)
Mrs L Hayes (PA) 12296
14309
Telephone 0114 2434343 Mrs E Colgan 69439
(Directorate Manager)
Mr R Fleming (Quality 15319
Manager/Risk Lead)
Ms S Cassidy 69471
(Directorate Business
Manager)
Mrs J Galloway 14257
(Laboratory IT Manager)
Ms J Cooper (PA) 14717
Department of Clinical Chemistry Results line & enquiries 14716
Northern General Hospital Dr G Gillett (Consultant) 14316
Telephone 0114 2434343 Dr H Delaney 14248
(Consultant)
Dr P Masters 52686
(Consultant)
Mr K Green 15707
(Lead Lab Manager
Clinical
Chemistry/Immunology)
Mr D Tazzyman 66454
(Acting Lab Manager
Automation)
Main Sample Reception 14260
GENERAL INFORMATION
Automated Routine 14928
Manual Immunoassay 14244
Trace Metals 14242
PID Area 14438
Toxicology 67240
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 27 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Department of Clinical Chemistry Results line & enquiries 12348
Royal Hallamshire Hospital Mrs P Wilson 61347/123
Telephone 0114 2711900 (Acting Lab Manager) 48
Mr I 61347
Jabbar(Specialist/Techni
cal Lead)
Sample Reception 12812
Main lab 13298
Endocrinology 13136
Department of Haematology Mr R Wardle 12621
Royal Hallamshire Hospital (Lead Lab Manager)
Telephone 0114 2711900 Results line & enquiries 12284
Automation Laboratory 12594
Blood Bank 12333
Cell Markers 12801
Haemolysis 12859
Reception 12998
Coagulation 12955
Department of Haematology Results line & enquiries 14304
Northern General Hospital Dr J Van Veen 14394
Telephone 0114 2434343 (Consultant)
Mr A Weir 14945
(Lab Manager)
Main Sample Reception 14260
Haematology 14723
Coagulation 14943
Blood Bank 14246
Microscope Room 14305
Department of Histology Dr B Perunovic 61424
Royal Hallamshire Hospital (Consultant)
Ms J Jones (PA) 11930/694
39
(Satellite Lab only at NGH) Mr D Whittaker 12663
Telephone 0114 2711900 (Lead Lab Manager)
Ms S Hibberd 13727
(Lab Manager)
Mrs R Leff 68424
(Deputy Lab Manager)
Enquiries 61380
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 28 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Results line 12728
Main Lab 12240
Department of Immunology Results line 15552
Enquiries 69196
Northern General Hospital Dr W Egner 15349
Telephone 0114 2434343 (Consultant)
Dr R Sargur 15704
(Consultant)
Dr D Arnold 15700
(Consultant)
Mr K Green 15707
(Lead Lab Manager
Clinical
Chemistry/Immunology)
Mr J Aldis 15719
(Acting Lab Manager
Main Sample Reception 14260
Electrophoresis 15724
Laboratory
Immunochemistry 15720
Laboratory
Immunofluoresence 69767
Laboratory
PID Area 14438
Pre-natal Screening 15725
Laboratory
Department of Microbiology Results line & enquiries 14777
Northern General Hospital Dr S Thompson 17579
Telephone 0114 2434343 (Consultant) (SCH)
14777
GENERAL INFORMATION
(NGH)
Dr E McLellan 68482
(Consultant) (RHH)
Dr D Partridge 14538
(Consultant) (NGH)
12773
(RHH)
Mr D Whittaker 14528
(Lead Lab Manager)
Main Sample Reception 14260
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 29 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Automated Serology 14928
Chlamydia Laboratory 14256
CL3 Bacteriology 15538
Laboratory
CL3 Virology Laboratory 14539
Enteric Laboratory 14535
Environmental 14534
Laboratory
Main 53245
BacteriologyLaboratory
(B/C Area)
Main 69217
BacteriologyLaboratory
(GUM Area)
Manual Serology (Bench) 52506
Manual Serology 14531
(Samples)
PCR Laboratory 3 66289
PCR Laboratory 4 52749
PCR Laboratory 4 Lobby 52720
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 30 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
CLINICAL CHEMISTRY
LOCATION OF DEPARTMENT
B Floor, Orange Wing
Pathology Block
Sheffield Children’s NHS Foundation Trust
Western Bank
Sheffield S10 2TH
CONTACT DETAILS
Mrs Camilla Scott, Clinical Scientist and Head
of Department Ext 17404
Mrs Camilla Scott’s Secretary – Lynne Ext 17318
Wolstenholme
Mr P Craddock-Jones Laboratory Manager Ext 17444
Bleep 009
Mr Craddock-Jones’s PA – Alison Lenthall Ext 17340
ENQUIRIES
Laboratory Office Ext 17340
Laboratory Office Fax 0114 270 6121
Answering machine and FAX 0114 271 7263
Duty Clinical Scientist Bleep 095
On-call Clinical Scientist Bleep 07659 512616
Acute Section
Routine results/Emergency requests Ext 17305/17306/17427
Matthew Jordinson (Chief Biomedical Ext 17134
Scientist)
CLINICAL CHEMISTRY
Fraser Cocker (Senior Biomedical Scientist) Ext 17134
Sharon Colyer (Principal Clinical Scientist) Ext 17307
Georgina Howson (POCT Co-ordinator) Ext 17134
Metabolic Section
Result enquiries Ext 17445
Claire Hart (Principal Clinical Scientist) Ext 17307
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 31 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Louisa Smith (Chief Biomedical Scientist) Ext 17405
Helen Chapman (Chief Biomedical Scientist) Ext 17405
Stephen Mc Sweeney (Senior Biomedical Ext 17445
Scientist)
Tissue Culture Section
Dr Simon Olpin (& answer phone) Ext 17267
Joanne Croft (Clinical Scientist) Ext 17267/60972
Prenatal diagnosis enquiries Ext 17267
Newborn Screening Section
Newborn screening results (09.00 to 12.30) Ext 17257
Answering machine and fax Ext 17263
Dr Lynette Shakespeare (Screening Lead Ext 17302
Scientist)
Catherine Dibden (Clinical Scientist) Ext 17346
Ullas C-Joseph (Chief Biomedical Scientist) Ext 17500
Sheila Ellin (Senior Biomedical Scientist) Ext 17346
Jade Barber (Senior Biomedical Scientist) Ext 17346
Mrs G Race (Specialist Nurse) Ext 17415
Mrs A M Casbolt (Specialist Nurse) Ext 17415
LABORATORY OPENING TIMES
Normal laboratory opening times Monday to Friday
9.00am- 5.00pm
Receipt of samples which require special handling (e.g. Monday to Friday
growth hormone, insulin, dynamic function tests with 9.00am- 4.00pm
multiple samples or research samples)
For the analysis of urgent samples outside the above times, contact the
Biomedical Scientist on call for Clinical Chemistry via the Hospital
Switchboard.
SERVICES PROVIDED
A 24 hour service is provided for the Children’s Hospital, Ryegate Children’s
Centre, and Becton Centre (CAMHS). Support is also provided for the
management of ward-based blood gas analysis and glucose monitoring.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 32 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specialist paediatric advice is available to help in the interpretation and selection
of tests on a 24 hour basis. Where appropriate (predominantly for immunology,
toxicology and some endocrinology) samples are referred to other local
hospitals.
The newborn screening section of the laboratory covers all babies born in
Derbyshire, Leicestershire, Lincolnshire, Northamptonshire, Nottinghamshire,
Rutland, South Humberside and South Yorkshire.
A Regional service is also provided for the investigation of children with a
suspected metabolic disorder. This service is available to the Sheffield
Children’s NHS Trust without cross charging and to other users on a cost per
test basis . Many of the more complex investigations are free for patients in the
Trent Region and South Humberside as they are covered by contracts for
Newborn metabolic screening.
SPECIALISED BIOCHEMICAL SERVICES
Drug Analyses
Plasma concentrations of the following drugs are measured in this laboratory for
the purpose of therapeutic drug monitoring or in cases of suspected overdose:
Alcohol, Caffeine, Cyclosporin, Iron, Methotrexate, Paracetamol, Salicylate and
Tacrolimus.
Samples for the measurement of other drugs will be referred.
Specimen requirements are given in the laboratory test A-Z listing at the back of
this handbook. In some instances it may be possible to measure drug levels in
other fluids such as urine by arrangement with the laboratory. A toxicology
service is provided at the Northern General Hospital (ext 12046). For further
information on referral services contact the Duty Biochemist (Bleep 095).
CLINICAL CHEMISTRY
Therapeutic drug monitoring
Caffeine analyses are performed routinely. Other drug analyses are performed
as required. The laboratory must be contacted for urgent results. For a valid
interpretation of the results, the following information must accompany each
request:
Type of preparation
daily dose
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 33 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
time of last dose
time blood sample taken
other drugs being taken
Suspected overdose
For a valid interpretation of paracetamol levels, blood samples must not be
taken within 4h of ingestion. After suspected overdose of theophylline, caffeine,
iron, methotrexate or alcohol analyses may be available out of hours after
contacting the on-call Clinical Scientist.
After suspected overdose of other drugs collect up to 10 mL whole blood in
lithium heparin and as much urine as possible in a plain container. The
collection of tissues or other fluids may be appropriate. Contact the Duty
Biochemist (Bleep 095). Samples collected after suspected overdose must give
the type of preparation taken and the estimated time of ingestion.
Post Mortem Samples
Dried blood spot and bile samples taken at post mortem will be returned to the
requesting laboratory, along with the report, for disposal or storage according to
the consent obtained.
Forensic Analyses
If police involvement is likely, special precautions are required for sample
collection. For advice on this and other toxicology matters contact the
Toxicology Laboratory at NGH via switchboard.
Sweat tests
The test is performed by laboratory staff. Please contact the laboratory (ext
17305) to arrange an appointment date for the test to be carried out and
immediately forward a request form. Fully completed request forms must be
sent to the laboratory; whilst they do not accompany the patient/carers they are
the means by which the laboratory ascertains consent has been given. Up to two
sweat tests can be carried out per day, therefore, it is advisable to book well in
advance. Tests are booked for 2.00pm only and usually take place in the
Research and Medical Treatment Lounge (outpatients) or occasionally on the
wards (inpatients) or Cystic Fibrosis Unit. Urgent medical day care sweat tests
will usually only be performed if certain criteria are fulfilled (bleep Duty
Biochemist 095). Advice sheets, directions and map are sent to parents prior to
the test and a further information sheet will also be provided on arrival. Analysis
takes place each Wednesday.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 34 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Investigation of Inborn Errors of Metabolism
A service is provided for the detection, diagnosis and monitoring of patients with
inborn errors of metabolism. Analyses performed are included in the laboratory
test A-Z listing at the back of this handbook. It is important that requests for the
investigation of inborn errors of metabolism are accompanied by adequate
clinical information including drugs being taken at the time of sampling. If the
relevant clinical information is detailed, the laboratory should be contacted by
letter or telephone. See User’s Handbook for Metabolic Investigations for further
details (available from the laboratory).
Skin Biopsies
Further investigation of some disorders requires the use of cultured fibroblasts.
The following are routinely available:-
Screen for disorders of long-or medium-chain fatty acid
oxidation This screen will detect defects of carnitine transport
and deficiency of carnitine-palmitoyltransferase types 1 and 2,
carnitine acylcarnitine translocase deficiency, very-long- or
medium-chain acyl-CoA dehydrogenases, long-chain 3-
hydroxyacyl-CoA dehydrogenase and other disorders of the
trifunctional enzyme complex and mild to severe multiple acyl-
CoA dehydrogenation defects (ethylmalonic-adipic aciduria and
glutaric aciduria type 2).
Carnitine-acylcarnitine translocase
Glutaryl-CoA dehydrogenase (for glutaric aciduria type 1)
Palmitoyl carnitine transferase Type I and II
Propionyl-CoA carboxylase (for propionic acidaemia)
Pyruvate carboxylase
3-Methylcrotonyl-CoA carboxylase
Fumarate hydratase
14 14
Release of CO2 or C-incorporation from various substrates
for the detection of methylmalonic aciduria, isovaleric acidaemia
and other disorders
CLINICAL CHEMISTRY
Very long-chain fatty acids
Very long chain acyl-CoA dehydrogenase
Citrulline incorporation into fibroblasts for detection of defects of
argininosuccinate synthase and argininosuccinate lyase.
Acylcarnitine profiles on cultured fibroblasts incubated with
palmitate and L-carnitine.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 35 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Enquire for disorders not listed. In general the laboratory will advise on the need
for tissue based assays and make the necessary preliminary arrangements.
Consent for skin biopsy collection is the responsibility of the requester. For skin
biopsies taken in SCH within normal working hours (Mon-Fri; 9.00-17.00), a
consent form and pot of sterile culture media is obtainable from the Metabolic
Laboratory Ext. 17445. Please ensure the Trust’s Patient Identification Policy is
followed prior to sample collection (see page 10), and that a fully completed
request form with full clinical details and test request is included. Samples are
transported at room temperature to Clinical Chemistry Department to arrive
ideally no later than 4.30pm, Skin biopsies sent from outside of the Trust must
be sent in sterile media or saline as appropriate.
For skin biopsies sent from external hospitals within the Trent Inherited
Metabolic Disease Group a request form with full clinical details and test request
is required. Sample transport at room temperature, normal first class post to
Clinical Chemistry Department to arrive ideally no later than 4.30pm Mon – Fri.
Please contact laboratory if sample to arrive on the weekend (0114 271 7445 or
271 7267).
For skin biopsies sent from external hospitals outside the Trent Inherited
Metabolic Disease Group, please contact the Tissue Culture laboratory prior to
sample collection to discuss sample collection details and turnaround times. A
request form with full clinical details and test request is required.
Please note turnaround times (TAT) are flexible when applied to cultured cell
assays. As different patient cell lines grow at different rates. In general for most
assays starting from a skin biopsy the TAT is 8-12 weeks.
Muscle Biopsy/CSF Neurotransmitters
Please contact the laboratory on ext 17445 when arranging muscle biopsies and
CSF neurotransmitters. The laboratory requires at least 24 hrs advance notice
of these procedures, in order to commit staff. Appropriate collection medium etc
will be provided by the laboratory staff as well as liquid N 2 in which to freeze the
samples. All collections except those taking place in theatres will be attended by
a metabolic member of staff.
Newborn Screening
Dried blood spot samples are collected on newborn babies at day 5 (5-8 days)
by midwives to screen for phenylketonuria, congenital hypothyroidism, cystic
fibrosis, sickle cell disease, medium chain acyl CoA dehydrogenase (MCAD)
deficiency, maple syrup urine disease (MSUD), homocystinuria, iso valeric
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 36 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
acidaemia (IVA) and glutaric aciduria type 1 (GA1). Results are sent out to the
appropriate Child Health Record Department for entry into the Child Health
Information System and checking against birth lists. Positive cases are referred
for further investigation and treatment to designated paediatricians or
haematologists. Individual negative results are NOT normally sent out to
hospital doctors or Family Practitioners.
This service is largely separate from the routine analytical services offered in the
hospital and in general it is NOT appropriate to enquire directly of the Newborn
Screening Laboratory for a test result. If an abnormal result has been found
then, as soon as it has been confirmed the patient’s Family Practitioner will have
been informed. If you have clinical suspicion of ANY of the disorders screened
for, it is better to initiate further investigations since these are screening assays
only. Please bleep the Duty Biochemist on 095 if advice is required on further
investigations. The newborn screening test for congenital hypothyroidism will
not detect secondary hypothyroidism. Immunoreactive trypsin is not always
abnormal in cystic fibrosis patients with meconium ileus.
URGENT REQUESTS
Requests for urgent analyses out of normal working hours should only be
made if the results must be known before the next full working day and are
likely to have a direct affect on patient management (see Asher’s criteria
pg 5).
During normal working hours
Urgent requests must be arranged with the laboratory by telephone so that if
there is any delay in receipt, steps can be taken to locate the sample. Urgent
samples which arrive in the laboratory without prior arrangement may be
delayed.
Outside normal working hours
The following analyses are available by contacting the Biomedical Scientist on
CLINICAL CHEMISTRY
call through the hospital switchboard.
Blood: urea, Gentamycin, Tobramycin creatinine & electrolytes
(sodium, potassium, chloride, bicarbonate), calcium (with
albumin), magnesium, osmolality, glucose, LFT,
amylase, uric acid, salicylate, paracetamol, iron, alcohol,
lactate, ammonia, CRP, methotrexate (if previously
arranged) and Ferritin (if previously arranged)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 37 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Urine: sodium, potassium, osmolality.
CSF: glucose and protein.
Any samples arriving in the laboratory without contacting the on-call
Biomedical Scientist will be treated as non-urgent and stored for analysis
the following morning.
Where possible please contact the Biomedical Scientist on call after the sample
has been taken unless specific collection information is required. Please keep
calls after 10 pm to a minimum. Calls between 07:30 am and 9:00 am will be
routed via a Principal or Consultant Clinical Scientist.
Other tests may be performed out of hours after discussion with the Biomedical
Scientist on-call who may refer you to the Consultant Clinical Scientist.
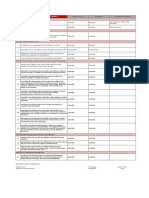
TELEPHONING LIMITS
The results of the following tests will be telephoned to the requesting clinician if
they are above or above the following action limits.
TEST BELOW ABOVE
Alcohol (ETOH) 80
Ammonia (AMON) 50 (neonate 100)
200 (inform DB if new
case)
Amylase (AMYL) 450
Bicarbonate (ECO2) 10 35
Bilirubin – conj. (Bc) 30 (if first result)
Bilirubin – unconj.(Bu) 300
B12 150 (send to RHH)
Blood Gases Where applicable (out patients)
Calcium (Ca) 2.00 (1.75 neonate) 3.10
Creatine Kinase (CK) 500 [>5000 inform DB]
Cortisol (am only unless 150
hypoglycaemic or
stressed)
Cyclosporin 400
Lactate (LAC) 5.0
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 38 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
TEST BELOW ABOVE
Ferritin 3,000
FK506 / Tacrolimus 2.0 12.0
Gentamicin 2.0
Blood Glucose (GLU) 2.7 11.0
CSF Glucose (CSF) Glu 2.8 &/or Ratio 4.4
0.6
Folate 2.0
Iron (Fe) 30.0
Lactate (LAC) 5.0
Magnesium (MG) 0.30
Methotrexate All results
Paracetamol (ACET) 200
Phosphate (PHOS) 0.30
Potassium (K) 3.0 6.0 (7.0 if neonate)
CSF Protein (CSF) Age dependant – any out of range (*)
Salicylate (SALI) 400
Sodium (Na) 120 150
Tobramycin 2.0
Urate (URIC) 750 (<10y)
1000 (>10y)
Urea (UREA) 20.0
REQUESTING ADDITIONAL INVESTIGATIONS
CLINICAL CHEMISTRY
Please be aware that laboratory staff will obtain volumes of blood on capillary
phlebotomy ward rounds appropriate to the tests requested when the
phlebotomist first saw the form. Therefore there is no guarantee that there will
be enough spare for investigations requested later. However laboratory staff will
endeavour if at all possible to maximise the use of that sample.
Furthermore, samples with a high haematocrit/PCV often have much less
available plasma available for analysis following centrifugation; consequently for
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 39 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
the same tests required as another patient with normal haematocrit/PCV either
more blood is required or else fewer tests can be performed.
LIMITATIONS OF RESULTS
(Also see section on Uncertainty of Measurement in the General Information)
Results may be affected by poor storage conditions, delays in sample
transportation, incorrect use of sample preservatives, inappropriate collection
site (e.g. drip arm), or collection time (e.g. therapeutic drugs) and analytical
interferences. Consecutive sample results may be affected by biological and
analytical variation. If advice is required on any of the above issues, please
contact the laboratory. If any report contradicts clinical findings then please
discuss the case with the Duty Biochemist.
CONSENT
It is the responsibility of the referring clinician to obtain consent for testing. A
completed consent form should accompany all tissue culture samples.
REFERENCE RANGES
Reference ranges are provided for guidance in clinical decision making, rather
than for prescriptive use.
They are conventionally set to give the range of values which would be found in
approximately 95% of a statistically ‘Normal’ population. They are derived from
results obtained by this Department and from other sources. Reference ranges
for blood refer to serum or plasma samples unless stated otherwise.
Changes during growth and development create age-related reference ranges
for most analytes. Detailed ranges are kept in the Department and information
upon them may be obtained from one of the Biochemists.
For the day to day interpretation of results age-related reference ranges have
been condensed to cover generally recognised stages of development. These
are generally added to the report automatically by the laboratory computer when
the result is generated.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 40 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Newborn: First 7 days of life for term baby.
Neonate: First month of life for a term baby. Ranges may not apply to
pre-term or small-for-dates babies.
Infant: Normally from the second month to one year, neonates are
included in these ranges if not separately quoted.
Child: Normally one year to adolescence, neonates and infants are
included in these ranges if not separately quoted.
Adult: From the end of adolescence (>16 yr)
CLINICAL CHEMISTRY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 41 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
CLINICAL CHEMISTRY REFERENCE RANGES
Test Age Reference Range
Acid base (blood gas)
Hydrogen (H+) (nmol/L) Newborn 32-47
Neonate/Infant 35-48
Child/Adult 35-45
pH Newborn 7.33-7.49
Neonate/Infant 7.32-7.45
Child/Adult 7.35-7.45
pC02 (kPa) Neonate 3-6-5.4
Infant 3.5-5.5
Child 4.4-6.1
pO2 (Kpa) Neonate 6.7-12.0
Child 11.0-13.5
Adult 10.5-13.5
Imprecision 1.7
Calculated actual bicarbonate (mmol/L) Child 17-27
Adult 24-27
Calculated base excess (mmol/L) Newborn -10 to –2
Infant -7 to –1
Child -4 to +2
Adult -2 to +3
Acid Glycoprotein (orosomucoid) (g/L Child (>5y)/Adult 0.4-1.0 female
0.6-1.2 male
ACTH, 9am (ng/L) Child/Adult <46
Acute phase reactants Neonate 0.9-2.2
Alpha-1-antitrypsin (g/L) Infant 0.8-2.0
Child 1.1-2.3
Adult 1.1-2.1
Alpha-1-antichymotrypsin (g/L) Adult 0.3-0.6
Alanine aminotransferase (ALT, SGPT) Neonate Up to 38
(U/L) Child 5-44
Adult 3-46
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 42 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Albumin (g/L) Neonate 24-40
Infant 25-49
Child 35-48
Adult 35-50
Alkaline Phosphatase (U/L) Neonate 73-391
Infant 59-425
1y-14y 76-308
14y-16y 49-242
Adult 30-130
Alpha fetoprotein (kU/L) Newborn 50,000-150,000
2 weeks 7,000-20,000
4 weeks 1,500-2,500
6 weeks 200-400
8 weeks 50-100
10 weeks 6-12
3 month - Adult 3-8
Ammonia (µmol/L) Neonate Up to 100
Infant/Child/Adul Up to 50
t
Amylase
Plasma U/L 30-100
Urine amylase/creatinine ratio u/mmol
creatinine Child/Adult <38
Angiotensin Converting Enzyme (ACE) 6m-19y 29-112
(U/L)
CLINICAL CHEMISTRY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 43 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Androstenedione (nmol/l) 1-7 days ≤ 10.8 nmol/L
1-4 Weeks ≤ 9.2 nmol/L
1-12 months ≤ 3.1 nmol/L
1-10 years ≤ 2.3 nmol/L
10-17 years ≤ 6.9 nmol/L
Male 17 yrs + ≤ 7.8 nmol/L
Female 17 yrs + ≤ 7.8 nmol/L
Follicular ≤ 6.0 nmol/L
Luteal ≤ 10.3 nmol/L
Post-
menopausal ≤ 6.5 nmol/L
Synacthen test
0mins ≤ 7.6 nmol/L
30 mins ≤ 11.7 nmol/L
Aspartate aminotransferase (AST, Neonate 18-92
SGOT) (U/L) Infant/Child 13-61
Adult 5-61
Bicarbonate (total carbon dioxide) Neonate 14-30
(mmol/L) Infant 16-30
Child 19-28
Adult 22-29
Bile Salts
Glycodihydroxycholanoate
Plasma (µmol/L) 0-6
Urine (µmol/mmol creatinine) 0.02-0.47
Glycotrihydroxycholanoate
Plasma (µmol/L) 0-2
Urine (µmol/mmol creatinine) 0.04-1.39
Taurodihydroxycholanoate
Plasma (µmol/L) 0-2
Urine (µmol/mmol creatinine) 0.01-0.08
Taurotrihydroxycholanoate
Plasma (µmol/L) 0-2
Urine (µmol/mmol creatinine) 0.01-0.08
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 44 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Bilirubin, conjugated (µmol/L) Neonate Up to 10
th
Child/Adult Up to 2 (97.5
centile)
Bilirubin, total paediatric (µmol/L) Neonate Variable
dependent on
child. Action limits
for
phototherapy/exch
ange transfusion
vary from days of
birth and are
lower for
premature babies
– See nomogram
in trust guidance
(Ref 1790v1)
Child/Adult Up to 21
Biotinidase (U/L) Child/Adult 2.5-10.5
C-peptide (fasting adults, pmol/L) Adult 298-2350
Caffeine (mg/ml) 10-35mg/L
Calcium ionised (mmol/L) Child/Adult 1.13 – 1.32
(adjusted to pH
7.4)
Calcium total
Plasma (mmol/L) Neonate 2.14-2.74
Infant 2.13-2.72
Child 2.10-2.56
Adult 2.14-2.51
Urine (mmol/24h) Adult 2.5-7.5
Carbamazepine (Tegretol) (mg/L) Child/Adult 4-12
Carnitine (mol/L)
Total 23-60
CLINICAL CHEMISTRY
Free 15-53
Chloride (mmol/L) Neonate 97-114
Infant 98-113
Child 98-111
Adult 95-108
Cholestanol (µmol/L) All 3-16
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 45 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Cholesterol (mmol/L) Neonate 1.5-4.0
Infant 1.2-4.7
Child 2.8-6.0
16y-19y 2.8-5.7
Adult (desirable) <5.2
Cholinesterase (IU/L) >5300
Complement
Profile (g/L)
C3 0.75-1.65
C4 0.14 -0.54
Components (g/L)
C1 esterase inhibitor 0.15-0.35
C3 nephritic factor Negative
Copper (µmol/L) 0-6 months 5.9-16.3
6 months to 1y 3.8-23.8
Female 1y-13y 11.0-27.0
Female 13y-49y 11.0-38.9
Adult (male) 11.0-27.2
Adult (female) 14.2-35
Urine mol/24h Child/Adult <0.9
Cortisol (nmol/L) 09.00 hrs 0-1m 50-300
(Plasma/serum samples now analysed 1m-1y 70-480
at SCH Clinical Chemistry) 1y -14y 80-580
9.00am – 12 noon Adult 198-720*
midnight Adult <100
*N.B Early morning cortisol of ≤
150nmol/L should prompt discussion
with Endocrinologist.
Urinary free nmol/24h Adult 10-147
Creatinine kinase (creatine 0-90d 28-470
phosphokinase (CK, CPK) (U/L) 90d-1y 24-240
1y-10y 24-175
11y-14y 30-170
15y-18y 27-145
Adult 30-170
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 46 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Creatinine (µmol/L) Newborn 31-107
Neonate 24-76
Infant 13-34
1y-2y 13-34
2y-4y 21-39
5y-11y 29-53
12y-14y 40-69
15y+ Male 54-90
15y+ Female 43-71
Urine Creatinine mmol/kg body Child 0.045-0.34
weight/24h
Creatinine clearance (ml/min/1.73 sq.m) Neonate 40-65
Child 95-150
Adult Over 100mL/min
Cyclosporine (Ciclosporin) (g/L) Child/Adult 100-400
(trough levels)
7-Dehydrocholesterol (µmol/L)
For the diagnosis of Smith Lemli Opitz
Syndrome) >5
Normal (µmol/L) <2
8-Dehydrocholesterol (µmol/L) <3
CLINICAL CHEMISTRY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 47 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
DHEAS (µmol/L) Male 1-7 days 2.5-10.2
Male 8-15 days 1.0-6.1
Male 1-6 <2.0
months
Male 6-12 <0.7
months <0.8
Male 1-4 y <0.5
Male 4-7 y <2.6
Male 7-11 y <4.1
Male 11 y <9.3
Male 12-15 y 1.3-9.7
Male 15-17 y 2.8-9.3
Male 17 y 2.8-11.9
Male 18-19 y 7.6-17.3
Male 20-29 y 3.2-14.0
Male 30-39 y 2.6-14.0
Male 40-49 y 1.9-8.4
Male 50-59 y 1.1-7.8
Male 60-69 y 0.8-4.8
Male >70 y 2.0-10
Female 1-7
days 1.2-6.7
Female 8-15
days <2.0
Female 1-6
months <0.7
Female 6-12 <2.1
months <1.0
Female 1-4 y <1.8
Female 4-7 y <4.3
Female 7-9 y <2.7
Female 9-11 y 0.8-4.8
Female 11 y 0.9-9.6
Female 12-14 y 2.6-10.9
Female 14-17 y 1.8-10.3
Female 17-20 y 1.2-7.3
Female 20-29 y 0.9-6.5
Female 30-39 y 0.7-5.4
Female 40-49 y
Female 50-59 y
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 48 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
DHEAS (µmol/L) continued Female 60-69 y 0.4-4.0
Female >70 y 0.4-2.4
Diazepam (with Nordiazepam) (µg/L) Child/Adult <2500
Digoxin (µg/L) Ideally 6-8h post dose Child/Adult Therapeutic target
range 0.5-2.0
µg/L. In patients
being treated for
heart failure a
target range of
0.5-1.0 µg/L is
recommended
(Hallworth and
Watson
“Therapeutic Drug
Monitoring”, ACB
Venture
Publications 2008
page 98).
Dimethylglycine (µmol/mmol creatinine) 0-16
Dopamine (nmol/mmol creat.) 0-1y <1950
1y-3y <1450
3y-5y <950
5y-8y <850
8y-11y <750
>12y <650
Ferritin (µg/l) 11-89
CLINICAL CHEMISTRY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 49 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Follicle stimulating hormone (FSH) 0-1 Month <22.0
(IU/L) Male 1 month -
6y <2.8
Male 6y-11y <3.8
Male 11y-14y <4.6
Male 14y + 1.5-12
Female 1 month
– 14y 0-11
CLINICAL CHEMISTRY
Follicular phase 3.5-13
Mid cycle 4.7-22
Luteal phase 1.7-7.7
Female 60y +
(post
menopausal) 26-135
Free T3 (pmol/L) 0 – 1 year 3.4 – 7.6
1 – 5 years 4.3 – 7.2
6 – 10 years 4.4 – 6.8
11 – 14 years 3.4 – 6.5
15 – 18 years 2.9 – 6.8
Free T4 (pmol/L) 0 – 1 year 11.0 – 23.6
1 – 5 years 11.0 – 20.8
Free T4 (pmol/L) continued 6 – 10 years 10.9 – 19.0
11 – 14 years 10.0 – 16.9
15 – 18 years 10.2 – 17.3
Galactose-1-Phosphate (µmol/GM-Hb) Child/Adult Up to 30
Galactosaemia on galactose free diet >0.6
Gamma-glutamyl transferase (U/L) Newborn 24-227
Neonate 11-149
1-m-3m <123
4m-6m <53
7m-12m 8-20
Child 10-27
Adult 9-31
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 50 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Glucose plasma fasting (mmol/L) Neonate 2.5-5.5
Child 3.0-6.5
Urine (mmol/L) Neonate Up to 1.1
Child Up to 0.3
Diabetic in
control Up to 150
mmol/24 h
CSF (mmol/L) Child 2.8-4.4
CSF/plasma glucose ratio (mmol/mmol) >0.6
Glycated haemoglobin (HbA1c) Child/Adult 20.0-48.0
(mmol/mol Hb)
Glycosaminoglycans 0-1m 22.1-40.8
(mucopolysaccharides MPS) (Screen) 1m-3m 9.2-38.8
Mg/mmol creatinine 3m-6m 11.9-34.5
6m-12m 4.2-30.5
1y-2y 6.8-21.7
2y-3y 9.7-19.5
3y-5y 6.2-15.4
5y-7y 6.2-12.1
7y-9y 4.1-10.8
9y-11y 4.5-10.8
11y-13y 2.8-10.4
13y-15y 2.0-7.6
over 15y 1.7-4.4
Growth hormone (g/L) 0-7d 1-23
5-15d 1-15
15d-11y <4.7
11y-18y <11
18y+ <4.3
Hexanoylglycine Normal 0.1-1.1
(µmol/mmol creatinine)
High Density Lipoprotein (HDL) – Child 0.8-2.1
CLINICAL CHEMISTRY
Cholesterol (mmol/L) Adult 1.0-1.7
Homocysteine Total (µmol/l) Adult male 0-18
Adult female 0-16
Homovanillic acid (HVA) (mol/mmol Infant 4-25
creatinine) 1y-5y 2-15
>5 2-13
Human chorionic gondatrophin (hCG) Males, Non- <2
(IU/L) preg. women
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 51 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
17-alpha-Hydroxyprogesterone (nmol/L) 1-14d ≤ 9.2 nmol/L
2-13w ≤ 8.7 nmol/L
Range may be higher in ill and 3m-1y ≤ 5.7 nmol/L
premature neonates 1y-3y ≤ 2.9 nmol/L
3y-11y ≤ 2.9 nmol/L
11y-15y ≤ 4.5 nmol/L
>15 years
Male ≤ 6.0 nmol/L
Female
Follicular ≤ 4.4 nmol/L
Luteal ≤ 14.3 nmol/L
Post-
menopausal ≤ 2.9 nmol/L
Synacthen test
0 mins ≤ 6.2 nmol/L
30mins ≤ 12.6 nmol/L
IGF-1 (g/L) 0-2y 28-156
2-4y 40-189
4-6y 50-223
6-7y 62-248
7-8y 78-281
Female 8-9y 99-376
Female 9-10y 114-369
Female 10-11y 134-426
Female 11-12y 160-581
Female 12-13y 201-707
Female 13-14y 256-716
Female 14-15y 284-713
Female 15-16y 279-700
Female 16-17y 270-660
Female 17-18y 246-533
Female 18-19y 233-499
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 52 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
IGF-1 (g/L) continued Male 8-9y 90-284
Male 9-10y 102-304
Male 10-11y 117-305
Male 11-12y 129-339
Male 12-13y 141-419
Male 13-14y 179-540
Male 14-15y 229-691
Male 15-16y 269-697
Male 16-17y 267-673
Male 17-18y 243-527
Male 18-19y 235-512
19-20y 220-471
20-30y 115-340
30-40y 109-324
40-50y 103-310
50-60y 97-292
60-70y 91-282
70-80y 47-207
>80y 40-184
Immunoglobulins
IgG (g/L) Neonate 3.9-17.0
Infant 2.1-10.9
Child 3.1-16.1
Adult 6.0-16.0
IgA (g/L) Neonate 0.01-0.15
Infant 0.05-0.7
Child 0.3-2.8
Adult 0.8-4.0
IgM (g/L) Neonate 0.05-0.4
Infant 0.15-2.1
Child 0.5-2.2
Adult 0.5-2.0
IgE (kU/L) Neonate Up to 5
Infant Up to 11
CLINICAL CHEMISTRY
Child Up to 63
Adult Up to 120
Insulin (from 24/1/11) (pmol/L) Fasting adult 17.8-173
Iron (mol/L) 0-2y 3.6-25.0mol/L
>2y 3.6-26.0mol/L
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 53 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Lactate fasting (mmol/L) Neonate Up to 3.0
Child 0.9-1.8
Adult 0.6-2.4
Lactate dehyrogenase (LDH) (U/L) Neonate Up to 1300
Child 400-900
Adult 340-670
Lipase (U/L) <60
Lithium (mmol/L) 0.4 – 1.0
(risk of toxicity if
>1.5)
Luteinising hormone (LH) (IU/L) Male 0-1y <3.2
Male 1y-11y <1.4
Male 11y-14y <7.8
Male 14y-17y 1.3-9.8
Male 17y+ 1.7-8.6
Female 0-6y <0.5
Female 6y-11y <3.1
Female 11-14y <11.9
Follicular phase 2.4-13
Mid cycle 14-96
Luteinising hormone (LH) (IU/L) Luteal phase 1.0-11
continued Female 60y +
(post
menopausal) 7.7-59
Magnesium Neonate 0.6-1.04
Plasma (mmol/L) Infant/Child 0.64-1.09
Adult 0.7-1.0
Urine (mmol/kg body weight/24h) Child Up to 0.18
(mmol/24h) Adult 2.4-6.5
Manganese (nmol/L) <1y 120-325
Child/Adult 73-210
Risk of toxicity >364
Methylmalonate (µmol/mmol creatinine) Child 1.0-8.0
Adult 0.2-2.4
Microalbumin (mg/mmol creatinine) <2
Myoglobin (g/L)
Serum 28-84
Urine <10
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 54 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Noradrenaline (nmol/24h) 0-1y <430
1y-3y <200
3y-5y <190
5y-8y <180
8y-11y <170
>11y <130
17β-Oestradiol (pmol/L) Dependant on
referall laboratory
used.
Orotic acid (mol/mmol creatinine) Infant/Child/Adul <3.5
t
Osmolality
Plasma (mmol/kg) Child/Adult 275-295
Urine (mmol/kg) Neonate/Child 100-800
After water deprivation administration over 800
Maximum dilution Adult 40-100
Maximum concentration Adult 600-1400
Oxalate (mmol/24h) Child 0.14-0.42
Adult Female 0.04-0.34
Adult Male 0.08-0.49
Paracetamol (mg/L)
Therapeutic range 1-2 h after last dose Child/Adult Up to 30
Overdose; sample taken not less than
4h after overdose: >100
4 hour levels (treatment indicated
– See BNF)
Refer to Nomogram in BNF
Parathyroid hormone (PTH) (ng/L) 2y 6.4 - 88.6
9y 16.2 - 63.0
17y 21.9 - 87.6
19y 16.0 - 60.4
pH Urine Neonate Over 5.0
Child 5.3-7.2
CLINICAL CHEMISTRY
Within 3 hrs of an ammonium chloride
load <5.3
Phenobarbitone (Phenobarbital) (mg/L)
Trough level after at least 14d of Child/Adult 10-40
constant therapy
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 55 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Phenylalanine fasting (mol/L) Newborn 40-110
<6m 32-128
6m-2y 40-140
2y-10y 20-130
10y-17y 30-115
Adult 40-100
Phenytoin (mg/L)
See Trust guidelines for Therapeutic Child/Adult 5-20
Drug Monitoring (1523)
Phosphate fasting (mmol/L) Neonate 1.0-2.7
Plasma Infant 1.1-2.4
Child 0.8-1.9
Adult 0.8-1.5
Urine (mmol/kg/body weight/24h) Child 0.33-1.28
(mmol/24h) Adult 15-50
Phosphoethanolamine (mol/mmol Cr) Child/Adult <10
Heterozygote 3-8 x normal
Homozygote 10-50 x normal
Phytanate (mol/L) Normal 0.2-19.3
Plasmalogens in red blood cells(ratio)
C16 Palmitate 0.060-0.160
C18 Stearate 0.150-0.400
Potassium Neonate 3.5-6.5
Plasma (mmol/L) Infant 3.5-5.7
Child 3.5-5.4
Adult 3.5-5.3
Potassium continued
Urine (mmol/kg body weight) Neonate Up to 2.3
Child Up to 2.0
(25-125 mmol/L)
Adult 25-100 mmol/24h
Pristanic acid (mol/L) Normal 0-1.88
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 56 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Progesterone (nmol/L) Male 0.7-4.3
Female 14-60y No range
Prolactin (mU/L) 0-1y No range
Male 1y + 86-324
Female 1y + 102-496
Protein total
Plasma (g/L) Neonate 33-72
Infant 48-78
Child 60-83
>17yr 60-80
Urine (mg/24h) Neonate Up to 10
Child Up to 50
Adult Up to 100
Urine protein/creatinine ratio (mg/mmol
creatinine) <20
CSF (g/L) Newborn 0.3-1.4
Neonate 0.3-1.2
1m-2m 0.2-0.9
2m-6m 0.1-0.7
>6m 0.1-0.4
Salicylate (mg/L) Therapeutic level
Therapeutic range Child <200
Overdose 4h after ingestion Refer to toxbase
for guidelines on
toxicity
Selenium (mol/L) <2y 0.22-1.22
2y-4y 0.33-1.44
4y-16y 0.52-1.52
CLINICAL CHEMISTRY
>16y 0.61-1.24/g-Hb
Glutathione peroxidase (/g-Hb)
Sex hormone binding globulin (SHBG) Child No range
(nmol/L) prepubertal 14.5-48.4
Male 17y + 26.1-110
Female 17-50y
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 57 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Sodium
Plasma mmol/L) Neonate 131-143
Infant 133-142
Child 133-144
Adult 133-146
Urine (mmol/kg body weight/24h) Neonate Up to 4.4
Child Up to 3.7(40-200
mmol/24h)
Adult 100-200
mmol/24h
s-Sulphocysteine (µmol/mmol <10
creatinine)
Testosterone (nmol/L) Male 0-1 month 2.6-14
Male 1m-6m <6.1
Male 6m-6y <1.12
Male 6-13y <2.37
Male 13-18y 0.98-38.5
Male 18y + 9.9-27.8
Female 0-1
month 0.7-2.2
Female 1m-10y <0.4
Testosterone (nmol/L) continued Female 10-12y <0.9
Female 12y + 0.22-2.9
Theophylline (mg/L) >1 month/Adult 10-20
Can be lower in
neonates
Thyroid stimulating hormone (TSH, 0 – 2 weeks 0.70 – 7.40
thyrotrophin) (mU/L) 2 weeks – 12
months 0.80 – 5.40
1 – 10 years 0.70 – 4.50
11 – 14 years 0.50 – 3.60
15 – 18 years 0.40 – 3.40
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 58 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Transferrin (g/L) Child/Adult 2.0-3.2
Triglyceride fasting (mmol/L) Neonate <1.8
Infant 0.3-1.7
Child 0.4-2.1
Adult <2.5
Trimethylamine (and Oxide) (mol/mmol Interpretation
cr.) given on report
Urea (mmol/L) Neonate 0.5-5.7
Infant 0.3-4.7
Child 1.6-6.0
Adult 2.5-7.8
Uric acid
Plasma (mol/L) Neonate 120-470
Child <10y 160-390
Child >10y 160-500
Adult (male) 200-430
Adult (female) 140-360
Urine (mmol/mmol creatinine) Neonate 0.3-1.7
Infant 0.3-1.3
Child 0.3-0.8
Adult 0.3-0.5
(1.5-4.5
mmol/24h)
Valproate (mg/L) Child/Adult 50-100
>150 may be toxic CLINICAL CHEMISTRY
Very long chain fatty acids (peroxisomal
disorders)
C22 (mol/L) 15-112
C24 (mol/L) 14-80
C26 (mol/L) 0.33-1.50
C24/C22 0.44-0.97
C26/C22 0.005-0.030
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 59 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Test Age Reference Range
Vitamins
A (mol/L) Neonate/Infant 0.50-1.50
1-6y 0.70-1.50
7y-11y 0.91-1.71
12y-18y 0.91-2.51
>19y 0.84-3.60
C (ascorbic acid mol/L) 26.1 – 84.6
E (mol/L) 4.6-14.0
Neonate 9.0-28.0
Child <16y 11.6-35.5
>16y-adult
Vitamin E/Lipid ratio (mol/L) 3-5
1y-6y 2-5
7y-12y 2-4
13y-19y >1.6
Adults
Vanilyl mandelic acid (VMA) Infant 2-12
(mol/mmol creatinine) 1y-5y 2-9
>5y 1-7
Zinc (mol/L) Infant/Child/Adul 7.2-20.4
t
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 60 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
DEPARTMENT OF PAEDIATRIC HAEMATOLOGY
AND BLOOD BANK
LOCATION OF DEPARTMENT
A Floor, Orange Wing
Pathology Block
Sheffield Children’s NHS Foundation Trust
Western Bank
Sheffield S10 2TH
CONTACT DETAILS
Departmental Fax 0114 276 2289
Tel Ext Bleep
Dr E Astwood Consultant Haematologist and 67951 136
Head of department
Secretary 17477
Dr J Payne Consultant Haematologist 17349 168
Secretary 17477
Dr K Patrick Consultant Haematologist 53662 249
Secretary 17477
Specialist Registrar 811 HAEMATOLOGY AND BLOOD BANK
Mr Philip Craddock- Laboratory Manager 17260
Jones
Mrs Paula Simpkin Haematology Service Lead 17230
Miss Michelle Scott Blood Bank Service Lead 17230
Mrs Amanda Baxter Specialist Practitioner of Blood 17107
Transfusion
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 61 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Haematology Data Manager 60865
Mr Shaun Emmitt Nurse Consultant 17329 123
Administrative Assistant 60865
Enquiries/Results Haematology Main Laboratory 17221
Blood Bank 17478
ENQUIRIES
During routine hours technical or clinical enquiries may be made by visit or by
telephone. Out of hours contact is via hospital switchboard.
LABORATORY OPENING TIMES
Normal laboratory opening times Monday to Friday
9.00am- 5.30pm
Receipt of routine samples Monday to Friday
9.00am- 5.00pm
Receipt of samples for crossmatching Monday to Friday
next day 9.00am-2.30pm
SERVICES PROVIDED
A 24-hour service is provided for the Children’s Hospital and the Ryegate
Children’s Centre. A laboratory service is also provided for local GPs.
Specialist paediatric advice is available to help in the management of patients
with haematological problems and in the interpretation of results and selection of
tests from consultant/SpR staff on a 24-hour basis.
The following is extra information not suitable for inclusion in the test table.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 62 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Therapeutic materials available from Blood Bank.
Patients with special transfusion needs can be catered for. Please indicate on
the form. It is crucial that clinical details are given to allow appropriate materials
to be selected e.g. CMV seronegative and gamma irradiated following e.g. IUT,
HSCT or fludarabine therapy etc.
For urgent, emergency, major incidents and complicated cases it is imperative
good communication is maintained with blood bank. During Major Incidents
Blood Bank requests must include a unique major incident number, the
patient gender and approx age.
Red cells request - Require Blood Bank request form. User to complete
usage/tracing label and return to Blood Bank lab.
Platelets, Fresh frozen plasma (FFP) and Cryoprecipitate. Requires phone call
to Blood Bank and a subsequent Blood Bank request form. For elective cases
also requires phone call to consultant haematologist to confirm need and dose.
A group and save sample will be required if blood group is unknown. User to
complete usage/tracing label on blood pack and return to Blood Bank lab.
Human albumin solution (HAS) stored in Blood Bank Laboratory (4.5%/5%
250ml, 20% 50ml). Only need to phone Blood Bank Laboratory if massive
amounts are required or continuous therapy anticipated. Porter to collect from
the Blood Bank Laboratory. User to complete usage/tracing label on package
and return to Blood Bank Laboratory.
Clotting factor concentrates – a variety is stocked. Requires phone call to blood
bank lab following approval from a consultant haematologist.
HLA/HPA selected platelets can be supplied. Requires phone call to consultant
HAEMATOLOGY AND BLOOD BANK
haematologist and blood bank lab and subsequent blood bank request form.
May require a sample.
Sample Requirements for Blood Bank
1ml EDTA (pink top) blood sample required for patients aged 6 months – 8
years.
2.5ml EDTA (pink top) blood sample required for patients aged 8 years or
over unless unable to obtain a venous sample for clinical reason.
For patients aged < 6 months please see below.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 63 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Baby group and crossmatch samples for Blood Bank
Complete the dedicated blood bank request form including the maternal details
section.
For infants under 6 months of age we require 0.5ml EDTA (pink top) of baby
blood sample (fully labelled with registration number) and 2.5ml EDTA (pink top)
of maternal sample fully labelled with maternal name and DOB. Subsequent
blood issues do not require further samples until 6 months of age. It is crucial we
are informed of historical intra-uterine transfusions.
When a crossmatch is requested, service users are responsible for notifying the
laboratory when blood transfusion has been received at another hospital after a
Blood Bank sample has been taken.
Transfusion Reaction Investigation.
Inform a consultant haematologist. Require 5ml plain clotted sample (glass vial
white top not sera gel) and 5ml EDTA (pink top), the remainder of all units given.
D-Dimers in the diagnosis of venous thrombo-embolism.
D Dimer testing in the SC(NHS)FT Haematology laboratory is set up to detect
cases of disseminated intravascular coagulation (DIC). The method used is not
validated by SCH for the exclusion of deep vein thrombosis (DVT) or pulmonary
embolism (PE) in children. The test must not be used for this purpose.
In general blood samples should not be sent to the Royal Hallamshire Hospital
for more sensitive testing, as the protocols used there have only been validated
in adult patients. For individual adolescent children with suspected VTE d-dimer
measurement at STH may be useful as part of the investigative algorithm but
should always be discussed with a consultant haematologist prior to sending
samples.
If a DVT is suspected it should be investigated with Doppler ultrasound scan,
after discussion with the Radiologist. If in doubt, please contact the on-call
Haematology Consultant or SpR to discuss.
Note there is detailed guidance available in the Ward 6 Haematology/Oncology
guidelines which can be found in a folder on Ward 6 above the nurses station -
see Section 12- Anti-Coagulation - 1333 Acute Venous Thrombosis (Ward
6/12/1333).
The guideline can also be located in the SC(NHS)FT Guidelines on the intranet.
Guidelines, minutes, policies, committees/approved clinical guidelines and
protocols/ Haematology+Oncology/Ward M3/Anti-Coagulation/ 1333 Acute
Venous Thrombosis (Section 11.9 reviewed by Jeanette Payne, March 2012).
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 64 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Capillary sampling for coagulation tests.
Bearing in mind the need to have a free flowing and thoroughly anticoagulated
sample for coagulation tests we normally require venous or arterial samples.
However if venous access is unavailable the following circumstances/notes
apply: -
0.5ml dedicated sample tube obtained from haematology on a named
patient basis.
During routine ward rounds
Prothrombin time (PT) for paracetamol overdose. 1 other test e.g. FBC
may be obtained – if this is exceeded the whole request will be left for
medical staff.
INR for monitoring of oral anticoagulants in infants and small children. 1
other test may be obtained – if this is exceeded the whole request will
be left for medical staff.
Anti-Xa for monitoring of low molecular weight heparin.
Capillary samples are unsuitable for APTT and will give erroneous
results.
Specialist Coagulation assays/studies.
The fill level in coagulation vials is crucial. Please discuss your request with the
lab prior to sampling to determine exact requirements for volume and vial type.
Approval with a consultant haematologist is required for factor assays, platelet
function and thrombophilia tests. SCH performs assays for FII, FV, FVII, FVIII,
FIX, FX, FXI, FXII, FVIII inhibitor, FIX inhibitor, lupus anticoagulant, platelet
function (PFA100), Von Willebrands ( vWf, Rcof) and anti-Xa assay (for
monitoring Low Molecular Weight heparin and unfractionated heparin) and APTT
ratio (for monitoring unfractionated heparin), and D-Dimers (for DIC). HAEMATOLOGY AND BLOOD BANK
Other available tests which require approval by an SCH consultant
haematologist and which we refer onto Royal Hallamshire hospital include FXIII
assay, tests for thrombophilia (ATIII, protein C, protein S, FV Leiden, anti-
phospholipid antibodies), Dimers (VTE) and more specialised tests of platelet
function.
Bone Marrow investigations.
Discuss requests with a consultant haematologist.
The following is available on fluid bone marrow: morphology; cytochemistry for
classification of acute leukaemia; Perl’s stain for ferritin/haemosiderin (iron
status); immunophenotyping by flow cytometry for classification of acute
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 65 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
leukaemia; CD34 cell enumeration; (and karyotype and molecular genetic
analysis by Sheffield Diagnostic Genetics Service)
Lymphocyte subsets.
Includes determination of total (CD3), helper/inducer (CD4), and
suppressor/cytotoxic (CD8) T cells, B cells and NK cells. Requires approval from
Immunology Consultant before requesting.
URGENT REQUESTS
Urgent samples that arrive in the laboratory without prior notification run the risk
of being delayed.
For the analysis of urgent samples outside normal hours, contact the Biomedical
Scientist on call for Haematology/Blood Bank via the Hospital Switchboard.
Please note that the service is run from home with staff travelling to the
laboratory to analyse urgent tests as appropriate.
Requests for urgent analyses out of normal working hours should only be
made if the results must be known before the next full working day and are
likely to directly affect patient management (see Asher’s criteria in the
Intended Audience section).
Outside normal working hours
The following analyses are available by contacting the Biomedical Scientist on
call through the hospital switchboard. NOTE: Out of hours samples taken for
FBC, film examination, ESR sickle test and slide test for infectious
mononucleosis, and for which results are not required until the next
working day, can be stored at 2-8°C and sent to the Haematology
Department for the following morning or sent to the laboratory but indicate
“not urgent” on the form. Any samples arriving in the laboratory without
contacting the on-call Biomedical Scientist will be treated as non-urgent
and stored for analysis the following morning.
Full blood count (Hb, Hct, Red cell count and indices, platelet count,
total and differential white cell count).
Examination of blood film for malarial or other blood-borne
parasites/malaria rapydtest
Sickle solubility (HbS) screening test.
Slide test for infectious mononucleosis.
Reticulocyte count.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 66 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Screening test for red cell G6PD deficiency.
Coagulation screen-prothrombin time, activated partial thromboplastin
time, fibrinogen level, and D-dimers if disseminated intravascular
coagulation is suspected.
Tests for monitoring anticoagulant control can be performed if clinically
urgent.
Blood group (ABO and RhD type).
Crossmatch.
Direct antiglobulin (Coombs) test.
Blood component/product issue.
The following guidelines on Haematological test choice are provided for
specific clinical situations:
Children with Petechial Rash and Fever (? Septicaemia)
Full blood count only is required; coagulation screen is not, if it is being
done merely to exclude the diagnosis of meningitis.
Neonates with prolonged jaundice
Prothrombin time is indicated in this situation (in practice a coagulation
screen comprising PT, APTT and Fibrinogen will be performed).
FBC in children with probable bacterial infection to whom antibiotic therapy has
been given
Urgent FBC cannot be justified if treatment has already been given. The
sample can be obtained but sent for analysis on the next routine working
day.
ESR as an urgent request
HAEMATOLOGY AND BLOOD BANK
An ESR will only be performed as an urgent test in cases of suspected
septic arthritis where the presentation is not clear-cut. It is not
warranted when the diagnosis is obvious, or when the child can be
monitored until the morning. The test is only performed when the
request is made after consulting the on-call consultant orthopaedic
surgeon.
Blood counts on febrile neutropenic oncology patients
These may not be necessary, depending upon the time and level of the
last neutrophil count. The requesting clinician should be asked to check
the last count on ICE before the on-call Biomedical Scientist agrees to
the request.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 67 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Issue of blood components and products (fresh frozen plasma, cryoprecipitate,
platelets, factor concentrates) - after discussion between the requesting medical
officer and the on-call Biomedical Scientist.
Other tests may be performed out of hours only after reference to the Clinical
Haematologist on call, who can be contacted via the hospital switchboard.
REQUESTING ADDITIONAL INVESTIGATIONS
The ability to extend original requests is dependent on having sufficient
remaining sample, its storage arrangements and technical/quality constraints.
Typically: -
Glandular fever screens up to 24h
Sickle screen up to 48hours.
Blood films up to 24h
Coagulation tests up to 8 hours
Group and save samples are retained for approx 6 months.
In general contact the laboratory by telephone to determine the practicalities and
then provide an additional request form to confirm the additional anaysis.
LIMITATIONS OF RESULTS
(Also see section on Uncertainty of Measurement in the General Information)
The effect of storage on analyses is dependant upon the choice of analysis and
storage conditions. No sample should be stored (even temporarily) at greater
than room temp unless specifically requested to do so. Avoid using shelves
above radiators or workstations with lamps beneath. It is best practice to forward
all samples to the lab upon collection. If delay is unavoidable or analysis not
immediately required see later note re non-urgent FBC on call, then storage
within a suitable fridge is preferable. Please ensure date and time sample
collected is noted on all request forms - thus allowing the lab to judge whether
to process the individual analysis".
Significant interference can occur in coagulation testing due to heparin; on Hb
due to severe lipaemia and on Hb phenotype/fraction quantitation due to
transfusion. Difficult sampling causing sample activation/clotting interferes with
coagulation tests and platelet count and possibly other FBC parameters.
Samples diluted at source with e.g. infusion liquid or line flush will influence
results for all analyses and may go un-noticed.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 68 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Variability of results due to analytical imprecision is dependent upon the test,
method and result value. Blood bank investigations will be influenced by
previous transfusions/infusions. Users may contact the laboratory to discuss
particular concerns.
REFERENCE RANGES
Reference ranges are provided on ICE and the printed laboratory report for
guidance in the interpretation of results. Age related reference ranges are
provided as appropriate but they do not take into account normal racial variation
or differences between venous and capillary sample type. Please seek advice
from the laboratory if necessary.
HAEMATOLOGY AND BLOOD BANK
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 69 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
HISTOPATHOLOGY DEPARTMENT
LOCATION OF DEPARTMENT
Laboratory and Office - C Floor
Mortuary – A Floor
Pathology Block
Sheffield Children’s NHS Foundation Trust
Western Bank
Sheffield S10 2TH
CONTACT DETAILS
The Consultant Head of Department, Prof M Cohen 17486
Lab Manager, T Taylor 17373
Senior Biomedical Staff, J Ager, P Arnold 17264
Mortuary Manager, T Donn 53460
PM consent advice 67809/53317
Mortuary enquiries 17246
Reports/Results 17254
Technical laboratory advice 17264
Urgent requests 17264
On call pathologist (24 hours) Through
switchboard
On call mortuary staff Through
switchboard
Bereavement coordinator, S McGovern 53317
LABORATORY OPENING TIMES
Normal laboratory opening times Monday to Friday
8.00am – 5.15pm
Mortuary 8.00am to 4.15pm
Please call ext 17264 to inform the Laboratory if fresh samples (i.e. not in
formalin) are to be sent after 4.30pm.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 70 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
SERVICES PROVIDED
The Histopathology Department provides a specialised paediatric and neonatal
biopsy service to the Surgical and Medical Directorates at the Sheffield
Children’s Hospital NHS Foundation Trust and provides a perinatal service to
the regional Trusts. The Department also supports the provision of services for
Oncology, Metabolic Disorders and Neuromuscular Disorders to North Trent,
operating within the Children’s Hospital Trust. Local expertise is available for
special investigations in enzyme histochemistry and immunochemistry. This
laboratory is accredited under the UKAS ISO 15189 accreditation scheme and
holds a HTA licence.
Note: Please be aware the following tests carried out by the Histopathology
laboratory are not currently accredited by UKAS:
Engel's Gomori
Oil Red O
NADH-TR
Succinate Dehydrogenase
Cytochrome Oxidase
Myoadenylate Deaminase
Phosphofructokinase (PFK)
Acid Phosphatase
Acetylcholinesterase (AChE)
Sirius Red
PHOX2B
Regular clinico-pathological conferences are held in the Department with the
Oncology, Clinical Genetics, Surgical and Gastroenterology teams and the
Department contributes to the monthly perinatal audit meetings at the Jessop
Wing (STH).
A perinatal and paediatric post mortem service is provided to the Children’s
Hospital and Health Authorities throughout South Yorkshire and North
HISTOPATHOLOGY
Derbyshire, together with coronial post mortem service for wider regions.
Mortuary staff will provide advice on death procedures to bereaved relatives
following a death (SCH only).
The Department participates in the death Review Panels from South Yorkshire
and Derbyshire.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 71 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Consultation
We welcome telephone calls to discuss the appropriate handling of specimens
and interpretation of the histological findings (Tel ext 17264).
Requests for Post Mortems
Clinical staff are welcome to attend post mortem examinations related hospital
deaths. Mortuary APTs inform of the starting time on request. (Tel ext 17246)
Requests for post mortem examination should be directed to the Consultant
Head of Department. (Tel ext 17486)
In certain circumstances, the death must be reported to the Coroner. The Junior
Doctors’ handbook gives some guidance on this issue but you may wish to
discuss this with the pathologist before contacting the Coroner’s Officer.
Requests for post mortem examination on all other deaths must be
accompanied by a completed consent form and detailed request form. Consent
forms must accompany all fetuses including those < 24 weeks gestation. You
will be notified of the starting time of the post mortem and you are entirely at
liberty to attend. Preliminary post mortem findings can be made available within
48 hours, if requested, and a microscopic report with full conclusion within 6
weeks.
The mortuary staff are available between 8am and 4.15pm (ext 17246), for
advice regarding consent for post mortems and can supply the consent forms
and booklets to parents explaining post mortems. Doctors who obtain consent
are strongly advised to read these before talking with parents.
OTHER INVESTIGATIONS
Routine Histology (i.e. samples received in buffered formalin)
Fixed tissue samples (samples in buffered formalin) can be sent to the
laboratory by the air tube delivery system or by hand to the Histopathology
Specimen Reception. Samples may be placed in a plastic universal or larger
container in tissue fixative (buffered formalin), which is available from Theatres.
The laboratory does not supply containers with fixative. However, the laboratory
can provide fixative for the larger specimens that need to be placed in a
specimen bucket, please phone the laboratory to arrange. Samples should only
be placed in fixative for routine histology. If in any doubt, please telephone the
laboratory for advice (ext 17264).
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 72 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
The container should be large enough to accommodate fixative at least 10 x the
volume of tissue to ensure adequate fixation. Avoid squeezing tissue specimens
into small containers as this will cause distortion and result in difficulty with
diagnostic interpretation.
NB Please be aware of the hazards associated with buffered formalin
(available from the laboratory).
Unfixed Samples and Special Investigations
The following specimens must not be placed in fixative and if small must be
kept moist by placing on gauze or cotton wool moistened with saline. They must
be immediately transported by hand to the Laboratory and handed directly to a
member of the Histopathology staff. Unfixed samples for histopathology
must not be sent via the pneumatic tube system (PTS). Please be aware
that if the pneumatic tube system (PTS) fails during transit of a precious sample
(i.e. a sample which cannot be repeated), the material may be unsuitable for
histology once retrieved.
a) Rectal biopsies for the investigation of Hirschsprung’s disease.
The rectal biopsy card should be placed onto a piece of cotton wool moistened
with saline in a universal container to prevent drying. The sample must not be
immersed in saline, nor should it be placed on dry cotton wool. The request
form must clearly state if the report is for :
Pull through (immediate report) or
Urgent acetylcholinesterase (urgency dependent on clinical need). This
technical procedure takes approximately 4 hours, if a result is required
on the same day the sample should be received by the laboratory before
1.30pm.
Next day acetylcholinesterase
Please include your bleep or extension number on which to receive the
telephoned report or discussion of the case.
b) Liver biopsies
Place samples in a small amount of saline in a universal container and hand to a
HISTOPATHOLOGY
member of Histopathology in person. A portion can be sent away for copper
measurement if requested.
c) Needle or trucut tumour samples
Place samples in Hams F10 culture medium (obtained from Histopathology ext
17264) in a universal container and hand to a member of Histopathology in
person.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 73 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
d) Large tumour samples and lymph nodes
Place samples in a dry specimen container of sufficient size to prevent tissue
distortion or damage and deliver to a member of Histopathology in person. Flow
cytometry may be undertaken by the laboratory on suitable samples.
e) Renal biopsies
Please contact a consultant histopathologist to discuss details of the case.
f) Needle biopsies of muscle
These are collected by a Biomedical Scientist who will attend the procedure and
advise on the adequacy of sampling if requested by the clinician. The
specimens are placed on filter paper moistened with saline in a disposable Petri
dish to ensure that drying does not occur.
It is important that the Laboratory be given advanced warning of renal and
needle biopsies of muscle in order that arrangements can be made for
appropriate technical advice and assistance.
g) Open muscle biopsies are usually taken in Theatre. The sample should
be placed in a Petri dish with moistened filter paper as above. It must be
dispatched to Histopathology without delay by the Theatre porter. , Please
handle with care and dispatch to the lab as urgently as tissue is required
for urgent frozen section diagnosis. Biomedical Scientists do not attend
open muscle biopsies in theatre.
As far as possible muscle biopsies should be taken from the vastus lateralis
muscle for the purpose of standardisation to permit fibre type proportions to be
assessed accurately. Fibre type proportions vary considerably between muscle
groups. The sample must not be taken near the myotendonous insertion, and
under no circumstances should the specimen be squeezed with forceps. Please
contact histopathology if further advice is required. Muscle biopsies for clinical
chemistry must be frozen in theatre; please contact Clinical Chemistry with
regards to this.
h) Neuropathology samples
These samples are not dealt with by histopathology at SCH but must be sent
directly to the Histopathology department at the Royal Hallamshire Hospital (see
section Transport of samples to STH page 16). These samples include:
CSF specimens
Nerve biopsies
Surgical brain tissue
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 74 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
If these samples are fresh (i.e. not in buffered formalin) they must be delivered
by hand direct from the clinical location and without delay to the Histopathology
department at the Royal Hallamshire Hospital. However if tumour banking is
required, please send sample for freezing and storage to Histopathology SCH
(Sample for diagnosis to go directly to RHH).
i) Bone marrow trephines
Place directly in buffered formalin in a universal container and transport to
histopathology laboratory.
j) EM samples
Tissue samples – place directly into PG fix (available from
histopathology lab) and send to SCH histopathology laboratory.
Blood for Battens – 2mls of whole blood in an EDTA (pink container) or
Citrate tube (purple container) and send to histopathology laboratory
without delay.
Please be aware of the hazards associated with PG fix (available from the
laboratory).
k) Cytology samples
All samples for cytology should be placed in a sterile container e.g universal
(can be obtained from Histopathology lab if required) and handed to a member
of histopathology in person before 4.30 pm.
BAL, Please state if fat laden macrophages and / or differential counts
are required. Tel ext 17264 for further information.
CSF. These must be sent directly to the Histopathology department at
the Royal Hallamshire Hospital.
l) Out-of-hours
When specimen is taken out of hours the Consultant Histopathologist may be
contacted via the switchboard (0).
URGENT REQUESTS
HISTOPATHOLOGY
Action required for handling samples which are indicated as urgent is decided by
the histopathologist and clinician on a case by case basis. Clinicians should
therefore discuss requests for "Urgent" samples with the Histopathologist as
soon as possible to agree a course of action to be taken and time scale for
report.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 75 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
During normal working hours
Examination of frozen sections must be pre-arranged with aH, preferably giving
at least 24h notice. Please give a contact phone number to which the urgent
report will be given. Rectal biopsies for acetyl cholinesterase histochemistry
may be reported within 4 hours of receipt when the department is specifically
instructed and they are received before 1.30pm, otherwise the procedure will be
carried out the following day. The Laboratory must be informed if an urgent
result is required. (ext 17246)
Outside normal working hours
Frozen sections for intra-operative diagnosis or suction rectal biopsies requiring
acetyl cholinesterase staining during evenings or weekends can be arranged if
necessary through the on-call consultant via the hospital switchboard. Every
effort will be made to respond to short notice/urgent requests as quickly as
possible. A pathologist will telephone all urgent reports to the requesting
clinician, followed by written confirmation.
LIMITATIONS OF RESULTS
(Also see section on Uncertainty of Measurement in the General Information)
The opinion described in a Histopathology report must be interpreted within the
clinical findings and a judgement made. If any Histopathology report contradicts
clinical findings, please discuss the case with the Consultant Histopathologist .
TURNAROUND TIMES
The department recognises and aspires to the Royal College of Pathologists
recommendations regarding turnaround times where applicable for surgical
samples. The department is actively striving to improve the turnaround times for
non-surgical sample requests but please note that in certain circumstances the
turnaround time may be longer, and on these occasions the service user is at
liberty to request an urgent report.
Routine samples not requiring special stains or immunocytochemistry or
EM – 5 working days.
Routine samples requiring special stains or immuno – 10 working days.
Muscle biopsies for enzyme histochemistry – 10 working days.
Sample for EM – up to 8 weeks depending upon the service provider
turnaround time.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 76 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Inter-operative frozen sections – as soon as possible but between 15 and
30 minutes.
Rectal biopsies for acetylcholinesterase – urgent samples within 4 hours of
receipt if received before 1.30pm, otherwise they will be carried out the
following day.
Post mortem reports – 6 weeks.
Placenta Investigation Reports- 28 days
HISTOPATHOLOGY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 77 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
SHEFFIELD DIAGNOSTIC GENETICS SERVICE
LOCATION OF THE DEPARTMENT
C Floor, Blue Wing
Sheffield Children’s NHS Foundation Trust
Western Bank
SHEFFIELD S10 2TH
CONTACT DETAILS
Departmental Director Ann Dalton 53743
Business Development Manager Denise Harris 53641
Head of Laboratory James Steer 17009
Deputy Head of Laboratory Service Andrew Marland 17021
Head of Oncology Kath Smith 17011
Deputy Head of Oncology Rebecca Pollitt 17012
Lead Scientist – Oncology Khalid Tobal 17047
Head of Constitutional Kath Smith 17019
Deputies of Constitutional Richard Kirk 53641
Lead Scientists – Constitutional Duncan Baker 17041
Nick Beauchamp 58038
Miranda Durkie 58038
Mandy Nesbitt 60584
General enquiries 0114 271 7014
Fax Machine 0114 275 0629
Email address SDGS@sch.nhs.uk
Website link http://wwwsheffieldchildrens.nhs.uk/SDGS.htm
Samples coming via the STH/SCFT pneumatic tube system (PTS) – address 51
ENQUIRIES AND RESULTS
Contact can be made by telephone, email, fax or letter during normal working
hours. For further information, clinical advice and interpretation contact the
relevant Head of Section or the Director as detailed above.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 78 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
To contact a member of staff by email use the following formula:
forename.surname@sch.nhs.uk
LABORATORY OPENING TIMES
Normal laboratory opening times:
Monday to Friday 9am – 5.30pm
Saturday 10am – 11.30am
The laboratory does not offer an out of hours service. However, it may be
possible to organise analysis of urgent samples outside of these times by prior
agreement.
SERVICES PROVIDED
We aim to outline the service offered by each group for the guidance of medical,
nursing and laboratory staff. The laboratory should be contacted for advice
should there be any doubt concerning any of the procedures; some of the tests
require discussion with the laboratory before the sample is sent. The most up to
date version of the Sheffield Diagnostics and Genetics Service is available on
the website (https://www.sheffieldchildrens.nhs.uk/sdgs/).
SHEFFIELD DIAGNOSTIC GENETICS SERVICE
The genetic services are currently organised into two main groups: Oncology
and Constitutional.
Oncology
Cytogenetic, FISH and molecular tests are offered as part of the diagnosis and
management of acute leukaemia, chronic myeloproliferative disorders and
myelodysplastic syndromes and for a number of specific solid tumours (including
sarcomas) and lymphomas. We offer molecular testing by sanger sequencing or
next generation sequencing panel testing for specific somatic mutations used to
define treatment sensitivity.
Please note that at present the service does not cover routine analysis in Non-
Hodgkin’s lymphoma (other than those described in the table) or Hodgkin’s
disease. Other cases of particular diagnostic value or research interest will be
accepted where possible, preferably by prior arrangement.
Cytogenetic analysis can be performed on bone marrow, blood or fresh tumour
biopsy. We require between 0.25 and 1.0ml of bone marrow aspirate (preferably
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 79 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
not the final exudate) in 5ml of transport medium containing heparin and
antibiotics. This medium is supplied on request from the department and should
be stored at +4ºC and kept in sterile containers e.g. universals. In addition, one
drop of marrow should be placed in transport medium with colcemid as the
marrow is taken. The medium is provided ready for use on request from SDGS,
and these instant cultures should arrive at the laboratory within one hour for
immediate processing.
If blood samples are sent for cytogenetics we require 5-10ml of blood in a lithium
heparin tube. Please do not put blood into transport medium. Provided a suitable
marrow sample has been sent there is no need for an accompanying blood.
Cytogenetic analysis on blood is only possible if there are sufficient immature
cells present, as in CML and some acute leukaemias.
FISH testing will be performed alone or as an adjunct to cytogenetic analysis for
detection or clarification of abnormalities or to exclude/confirm cryptic gene
fusions where appropriate. FISH can be carried out on bone marrow, blood,
solid tissue biopsy and on certain archive material including paraffin embedded
tissue sections (PETS). We carry a large number of FISH probes including those
required for the accurate diagnosis of the diseases described above and probes
for some lymphomas and sarcomas which are listed in the test tables by
disease. This list of probes is regularly updated and many other probes may be
obtained if considered of value in patient management.
Samples for Multiple Myeloma FISH testing require 2-5ml of Bone Marrow in
EDTA, to be received before 4pm on a Thursday to allow plasma cell enrichment
by CD138 separation. Outside of these hours or if a sample cannot be sent in
EDTA, FISH testing will be attempted on the whole marrow sample.
For molecular analysis 2-5ml of blood or bone marrow in K-EDTA (pink or purple
tops) is required. Smaller samples can be processed but may not be sufficient
for the test required and are more likely to fail. If in doubt please contact the
laboratory.
Samples should arrive no later than the day after they are taken. Solid tumour
samples should preferably arrive on the day they are taken and no later than the
following day. Please do not rely on first class post at weekends or bank
holidays.
Molecular testing and FISH are also available for a number of disorders from
paraffin embedded tumour tissue samples.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 80 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
For the accumulation of accurate information on the relationship between
genetic findings and clinical conditions, it is important to have accurate referral
information.
Constitutional
Please see testing information for a full list of tests. This includes genetic
analysis (cytogenetics, FISH, microarrays (arrayCGH) and molecular testing for
dosage and/or sequencing or by next generation sequencing panels of patients
with learning disabilities, neurodegenerative conditions, connective tissue
disorders, infertility, disorder of sexual development, inborn errors of metabolism
and haemochromatosis, haemostasis and haemoglobinopathies and also
includes fetal testing for the detection of aneuploidy or chromosomal
rearrangements in pregnancies that are at a high risk of producing a
chromosomally abnormal child.
Karyotype analysis is carried out from in vitro culture of blood samples and FISH
is offered as an adjunct to classical chromosome analysis when appropriate.
For fetal testing of amniotic fluid, chorionic villus or fetal blood samples. Rapid
aneuploidy screening by QF-PCR or FISH is offered and abnormalities
detectable include trisomy 21, 18 and 13, sex chromosome aneuploidies and
triploidy (this rapid service is also offered for newborn babies to detect these
abnormalities). This may be is backed up with conventional karyotype analysis
or microarray (array CGH)
FISH for specific syndromes is not carried out on prenatal cytogenetics samples
SHEFFIELD DIAGNOSTIC GENETICS SERVICE
unless indicated by a family history or to clarify a result from the chromosomal
analysis. An exception is the use of the TBX1 probe for the 22q11.2 region. All
referrals with heart defects are screened by FISH using this probe as some
cases may be associated with deletion in this region.
Microarray (arrayCGH) testing is available for patients with developmental delay
and/or multiple congenital abnormalities, autistic spectrum disorder, or seizures.
This is carried out as a higher resolution alternative to karyotyping. Please note
that Fragile X syndrome testing will not be initiated prior to array testing but is
available after a normal array result has been issued for patients with a specific
clinical query or appropriate maternal family history.
2-3ml venous blood in lithium heparin is required for a blood karyotype. 4ml
venous blood in lithium heparin is required for chromosome breakage / fragility
testing. 2-3ml venous blood in lithium heparin and 2-3ml of blood in K-EDTA is
required for microarray (arrayCGH) testing. Skin biopsy samples from patients
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 81 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
should be around 1-2mm in diameter, and 1mm in depth, taken from an alcohol
swabbed area. The depth is important as dermal tissue needs to be sampled.
The sample should be transported in bottles of sterile tissue culture medium
(available by request from the laboratory). Sterile saline can be used if no
medium is available. If delay in transport is unavoidable, samples should be
stored at +4oC. Samples must not be placed in Formalin.
In cases of fetal loss, IUD, stillbirth or therapeutic termination due to fetal
3
abnormality, we require a small biopsy of fetal placenta (approx 1cm
membrane, cord and placenta taken from, at or near the cord origin). We are
unable to accept a fetus. Specimens should be placed into sterile tissue culture
medium as above. In addition to placental biopsy, when possible, 1-3 ml sample
of fetal cord blood in lithium heparin can be successful. (NB Cardiac blood is
rarely successful).
Blood samples in K-EDTA (pink or purple tops) are received routinely for
molecular genetic analysis. Volume should be 2-5ml: smaller samples can be
processed but may not be sufficient for the test required and are more likely to
fail. DNA can be extracted from a variety of other tissues but if in doubt about
the sample size or suitability please contact the laboratory before taking the
sample.
Certain other diseases, also listed in the back of this booklet, are covered by our
consortium partners, to whom samples are forwarded by the laboratory. Tests
referred to our consortium partner or to other laboratories can be delayed in
reporting due to transfer time and factors beyond the control of this laboratory.
Please contact us if the sample is urgent.
Molecular prenatal diagnosis should be arranged well in advance if possible to
allow time to acquire any relevant test results or samples. Clinical genetics
service involvement is essential for all prenatal diagnosis referrals. Reliable
prenatal diagnoses require that the initial diagnosis has been clearly established
and it is important to appreciate the need for rigorous investigation even when
the index case presents in a terminal phase with little hope of useful intervention.
URGENT REQUESTS
Turnaround times listed in the test tables are generalised and we will always
endeavour to process urgent samples as quickly as possible. Current turnaround
times are detailed on the SDGS website. Urgent samples should be clearly
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 82 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
identified and telephone contact numbers listed in order to report results. In the
case of clinical need do not hesitate to contact the laboratory to request an
urgent result so that appropriate arrangements can be made.
REQUESTING ADDITIONAL INVESTIGATIONS
If further tests are required on samples already sent, this may be possible as
cytogenetics samples are stored for a period of between one month and one
year before disposal. DNA / RNA samples are stored, as appropriate, on the
majority of samples received in the laboratory for the purposes of validation,
controls and family studies. If further testing is required contacting the laboratory
directly is the most straight forward way to do this.
LIMITATION OF RESULTS
(Also see section on Uncertainty of Measurement in the General Information)
Cytogenetic results
Cytogenetic results from blood samples will be based on the analysis of a
minimum of 3 banded cells. The presence of mosaicism for any chromosome
abnormality is not routinely investigated by the level of analysis performed
unless dictated by the clinical referral reason or suggested by an observation
during routine analysis. The standard count for detection of a clone present at
greater than 10% level is 30 cells. This is reported in the karyotype comments if
SHEFFIELD DIAGNOSTIC GENETICS SERVICE
carried out.
Microarray (arrayCGH) testing will not detect balanced rearrangements or ploidy
changes and is limited in detecting mosaicism. The resolution of arrayCGH
analysis will be stated on the report.
Prenatal reports are based on the analysis of a minimum of three banded cells,
and therefore are unlikely to detect mosaicism. It should be noted that the
majority of samples sent for prenatal chromosome analysis are taken with a view
to screening for common numerical chromosomal abnormalities, particularly
Down syndrome. For technical reasons, the quality of structural analysis on such
samples is often conducted at a lower level than that which is required to reliably
detect small and unexpected chromosomal deletions and other rearrangements.
Although many structural chromosomal abnormalities will be detected, those that
fall below the limits of resolution of the analysis will be missed.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 83 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
For oncology samples a normal cytogenetic result is based on the complete
analysis of a minimum of 10 G-banded cells usually with the examination of at
least a further 10 cells. The number of cells analysed in abnormal cases or
previously abnormal cases may be increased or decreased according to the
reason for referral. A normal in situ hybridisation result is based on the exclusion
of a given abnormality in a minimum of 100 interphase cells. An indication will be
given if minimum standards are not reached.
For all cytogenetics analyses the ability to detect subtle, unexpected
chromosome rearrangements is governed by the resolution of banding achieved
This is intrinsically highly variable. If the quality of the preparation or extent of
the analysis performed is not considered adequate for the reason for referral this
will be indicated on the report.
DNA Sequencing
Sensitivity of DNA sequencing is over 95%. Since all mutations are checked in
two separate amplicons, if possible by two independent methods, sensitivity is
>99%. Rare cases of single nucleotide polymorphisms under the primer binding
sites may lead to non-amplification of one allele. The specificity is 100% where
the mutation or type of mutation has been previously reported. Where the
change is novel, it may be necessary to carry out family studies and it still may
not be possible to reach a conclusion regarding pathogenicity.
Low Level Mutations
In some circumstances it may prove difficult to detect mutations present at a low
level, e.g. in cases of mosaicism or mitochondrial heteroplasmy or where there
is a mixed cell population due to malignancy. Sensitivity of detection may be
tissue-specific and in some cases alternative sample types may be required.
Non-paternity
An error in the diagnosis of disease status may occur if the true biological
relationships of the family members being tested are not as stated. For example,
non-paternity means that the stated father of an individual is not the true
biological father. Any erroneous diagnosis in a family member can lead to an
incorrect diagnosis for other related individuals who are being tested.
CONSENT
Samples received in the Genetics laboratory are accepted under the assumption
that the patient has consented to genetic testing and to laboratory disposal of
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 84 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
any remaining sample. This is clearly identified by the information for the
referring clinician on the laboratory referral form. When the patient has not
consented for disposal by the laboratory, all remaining sample will be returned to
the referring hospital for appropriate disposal. To keep return of sample to a
minimum, large amounts of tissue should not be sent.
DNA (either pure or a crude preparation) is retained from the majority of samples
received in the Laboratory for the purposes of validation, controls and family
studies. It is important that the patients are aware of this. A consent form
covering this and other issues is available. If there are any problems with the
storage of samples, please contact the laboratory. The guidelines for consent
have recently been revised by the Royal College of Pathologists (September
2011). The changes recommended will be implemented in line with pathology
services nationally.
Predictive testing in late onset disorders such as Huntington disease or
Hereditary Cancer is only available through the Genetic Counselling Service, as
is diagnostic testing for dominant disorders where the family implications can be
complex, and the issues of consent require detailed discussion and
documentation. Predictive testing for adult onset disorders in children lies
outside our professional guidelines; in the event of a sample being referred, the
referring clinician will be contacted.
Carrier testing in children is generally to be avoided until the child is considered
Gillick competent. Where it is necessary to exclude the child being affected, the
report will not report the genotype but simply “unaffected” if the child is a carrier
or normal. The results will be recorded in the lab and be available to the child
once they are able to consent.
SHEFFIELD DIAGNOSTIC GENETICS SERVICE
All prenatal testing involving assessment of maternal cell contamination using
the Powerplex 16 kit assumes that the appropriate consent has been obtained
for the analysis of all chromosomes. If this is not the case the laboratory must
be contacted, prior to the prenatal sample being taken, to discuss the matter
further.
All Other Genetic Disorders
For those diseases not available in Sheffield, testing may be available through
the UK Genetic Testing Network; access to the Network at present is through
the laboratory. Many of the tests sent elsewhere attract a charge. There is a
ring-fenced budget for this under the control of the Sendaways group and
overseen by the Commissioners. This group meets regularly and all clinicians
are welcome to present a request, either in person, by proxy, by letter or by
submission of the appropriate form (available from Denise Harris). For further
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 85 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
information please contact the Head of the Laboratory Ann Dalton, who is also
Chair of the Sendaways Group. Tests referred to our consortium partner or to
other laboratories can be delayed in reporting due to transfer time and factors
beyond the control of this laboratory. Please contact us if the sample is urgent.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 86 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
ARRANGEMENTS FOR MICROBIOLOGY, VIROLOGY
AND IMMUNOLOGY
There are no Microbiology, Virology or Immunology laboratories on site and
these services are provided by Sheffield Teaching Hospitals Trust. Their
handbook can be accessed at SCH and is available at:
http://nww.sth.nhs.uk/NHS/LaboratoryMedicine/Default.asp?page=1.
All Microbiology/Virology services are now provided from the NGH site only.
MICROBIOLOGY
Clinical Microbiology Advice
There is a Consultant Microbiologist based full time at Sheffield Children’s
Hospital (Room E70, Top Floor Orange Wing) who can provide clinical advice.
Office extension 17579, Bleep 255.
Laboratory Queries
For laboratory queries please contact the laboratory at the NGH ext 14777
between the hours of 08:00 –20:00 weekdays, or 08:30 – 16:00 on weekends
and bank holidays.
NB: Please remember that microbiology specimens can take a considerable
length of time to process and should if possible be delivered well BEFORE the
end of a normal working day, ideally before 16.00 hrs
On Call Service
Weekdays 20:00 - 08:00 hrs
Weekends 16:00 - 08:00 hrs
Bank Holidays 16:00 – 08:00 hrs
Outside normal working hours a single Biomedical Scientist is available to
process emergency and urgent specimens. Contact must be made with the
person on call before sending any urgent specimens for analysis. There is no
guarantee that any non urgent work will be processed outside normal working
hours. NGH switchboard has a copy of the current out of hours rota.
MICROBIOLOGY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 87 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Sample Transport to Microbiology (NGH Laboratory Medicine Building)
Weekdays 09.00 – 17.00 hrs
Where from Time
09.40, 11.10, 13.10, 14.40,
Routine
16.00, 17.10
Weekdays SCH Clinical
Taxi arranged via SCH
(09.00-17.00) Chemistry
Urgent Clinical Chemistry if outside
routine pickup times
Notes for urgent samples
Prior to sending, SCH Clinical Chemistry should be alerted that an urgent
sample is being sent so that the urgency of the request can be discussed
and it can be established whether the sample may be sent by a scheduled
taxi or whether an urgent taxi needs to be booked. The sample should
then be sent by pneumatic tube system (PTS) (clearly labelled as urgent)
or by hand to SCH Clinical Chemistry reception (see Sample
Transportation section).
The Microbiology department at NGH must be informed by requestors that
the sample is being sent so they can ensure it is dealt with promptly on
arrival.
For any enquiries please contact the Microbiology laboratory ext 14777.
Out of hours service (including weekday evenings, Saturday, Sunday and
Bank Holiday)
**Clinical Chemistry are NOT responsible for out of hours transportation
arrangements**
Where from Time
08.30, 11.30,
Sat./Sun./Bank
14.30, 17.30,
A&E holidays
Routine 20.30, 22.30
Reception
17.15, 18.30,
Out of hours Week nights
20.30, 22.30
Urgent transport booked via
A&E
Urgent switchboard (if no routine
Reception
transport within 30 minutes)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 88 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Notes for urgent samples
Urgent samples should be clearly identified as urgent on the request form.
Contact the on-call Microbiology Biomedical Scientist (via the NGH
switchboard) at the same time as sending urgent samples.
Results
Authorised Microbiology results are electronically accessible via ward/office
computers through the hospital network or directly from the PC desktop ‘ICE’
icon. Passwords can be obtained by contacting the IT helpdesk. Please refer to
page 18 for instructions on how to access results.
Microbiology specimens over ‘long’ weekends
Please ensure that on long bank holiday weekends that sample fridges/boxes on
wards/units are regularly inspected, and samples transported as above, to avoid
sample deterioration leading to potentially misleading results. Any concerns or
comments should be communicated to Duncan Whittaker, Microbiology
Departmental Manager, Laboratory Medicine Building, NGH.
MICROBIOLOGY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 89 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
ANTIBIOTIC ASSAYS
The following assays are performed by Clinical Chemistry at SCH
Gentamicin and Tobramycin -.
In most clinical situations these agents are given once daily (every 36 hours in
neonates < 7days as per BNF-c). Oncology/Haematology (gentamicin) and
Cystic Fibrosis (tobramycin) use approved protocols. The gentamicin dosing
guidance can be applied to any group of patients but the tobramycin guidance
applies to CF patients only.
If the gentamicin dose is once daily, please refer to the Trust guidelines on
therapeutic monitoring. If three times daily dosage of gentamicin is used then
pre and one hour post levels must be taken. Therapeutic range pre: <2
microgram/mL. One hour post: 5-10 microgram/mL
Optimum sample size: Venous blood. 1ml-clotted blood in a plain tube
Capillary blood. 1ml-clotted blood in microtubes
Note: Venous blood is required for CF patient levels.
Samples should be sent to SCH Clinical Chemistry for processing. Where
possible out of hours testing should be avoided. The department runs a
traditional on-call service whereby the Biomedical Scientist on-call does not
have to stay at the hospital. As such notification must be made to the person
working on-call if a sample requires analysis. The person on-call may ask
questions about the urgency of the bloods in order to plan their workload
Vancomycin
st th th
Pre-dose level 24 hours after 1 dose (i.e. pre 4 dose if TDS dosing, pre 5
dose if QDS dosing). Sample size and destination as per gentamicin. Pre-dose
level should be 10-15 mg/L, unless otherwise specified by Consultant
Microbiologist or Pharmacist.
During normal lab hours send samples to Clinical Chemistry at SCH for dispatch
to NGH Microbiology. “On-call” contact the on-call STH Clinical Chemistry via
NGH switchboard and send sample direct to NGH (see page 81)
Other antibiotic levels
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 90 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Please contact Microbiologist.
See following protocols for further information.
Guidelines for the use of antibiotics that require assays are available:
- Guidelines for once daily gentamicin in infants and children (CG893)
Available from the clinical guidelines section of the SCH intranet pages.
A search for ‘gentamicin’ will identify the document.
- Intravenous guideline for cystic fibrosis
Available within the Medical Handbook (Section 16.2B)
- Antibiotic doses
Available within the Medical Handbook (Section 15.2)
MICROBIOLOGY
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 91 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
VIROLOGY SERVICES
The Virology Department is based within Microbiology at the Northern General
Hospital.
Department Staff and General Information
Dr Mohammed Raza (Consultant Virologist) Ext 14526, NGH
Dr Alison Cope (Consultant Virologist) Ext 14526, NGH
Dr Cariad Evans (Consultant Virologist) Ext 14526, NGH
Leeanne Tovey (Virology Department Manager) Ext 14056, NGH
Miss Geraldine Ball (Serology Manager) Ext 14531/14056, NGH
Virology SpR Office Ext 66477, NGH
Laboratory Hours
Weekdays 9am - 5.20 pm Saturdays 9am - 12.30 pm
Emergency Requests via Virology SpR Ext 66477, NGH or NGH Bleep 537
General Enquiries/ Results Enquiries Ext 14777, NGH
On-Call Service
Consultant Virologist (via NGH switchboard) provides an advice-only on call
service.
Please consult annually updated bronchiolitis flow chart for details of RSV
testing service. Rapid tests for RSV are carried out by the SCH Haematology
Department with results published to ICE. Tests are carried out in batches
throughout the day, the times of which are published at the start of each RSV
season.
Urgent out of hours virology requests other than rapid RSV must be
phoned to the on call Consultant Virologist (See above)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 92 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
IMMUNOLOGY SERVICES
The Immunology Department is based at the Northern General Hospital.
Transport to the NGH Immunology department is by STH-arranged van
collections organised by the NGH Transport Manager (Ext 14701) and
Campuslink. The van visits various laboratories and GP surgeries and calls for
samples to the NGH at approximately 10:30 am and 2:30 pm, Monday to Friday.
Outside of these times Monday to Friday, samples can also be transported by
the CampusLink taxi sample shuttle at 09:40, 11:10, 13:10, 14:40, 15:40 and
16:00.
Also see section 6.2 of the Paediatric Medicine pages in the Guidelines for
SC(NHS)FT Medical Staff Combined Book for immunology investigations’
http://nww.sch.nhs.uk/Health%20Services%20Management%20-
%20SCH/documents/GUIDELINES_HANDBOOK/2007/index.htm
Department Staff and General Information
Dr William Egner (Consultant) Ext 115349, NGH
Dr Egner’s secretary Ext 15705
Kevin Green (Lead Laboratory Manager) Ext 15707, NGH
Mr Green’s secretary Ext 15706
Immunology enquiries Ext 15552/69196
Laboratory Hours
Weekdays 9.00am - 5.00 pm
Results, from April 2012 no printed reports will be sent out. Authorised
IMMUNOLOGY
Immunology results are electronically accessible via ward/office computers
through the hospital network or directly from the PC desktop ‘ICE’ icon.
Passwords can be obtained by contacting the ICE Administrator (Ext 53268).
Please refer to page 18 for instructions on how to access results.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 93 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
CSF SAMPLES
Volume of CSF required for specific tests (paediatric samples)
1 BEFORE you take the CSF -
∙ Decide which test you require
∙ Calculate the volume of CSF this will need.
∙ Work out the number of drops that this will be.
Regardless of the size of needle used, 1ml of CSF is equivalent to 20 drops.
Remember that all volumes given are the minimum required, so extra drops are
always useful.
2 For MICROBIOLOGY investigations - See table for volumes required.
∙If the CSF is bloodstained, take the volume you require into three
screw-topped universal containers (these have a conical bottom).
Number them 1,2,3.
∙If the CSF is clear, take the volume into a single universal container.
DO NOT use the flat bottomed sputum pots for collecting CSF as they
cannot be centrifuged and fluid will be lost transferring to a universal
container.
3 For CLINICAL CHEMISTRY INVESTIGATIONS -
∙Glucose and/or Lactate: take 4-5 drops into a paediatric fluoride-
heparin tube.
∙Protein: take 4-5 drops into a paediatric 1ml plain tube/universal 25mL.
Blood stained samples will elevate results!
∙Serine and glycine 8-10 drops into paed 1mL plain tube.
*Please label these tubes by hand
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 94 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
4 Put the tests that you require in ORDER OF PRIORITY on the request
form, so that we can allocate CSF accordingly. This is VERY important
for very small volumes.
5 Transport specimens to the laboratory without delay: Protein, glucose
and lactate to the Clinical Chemistry at SCH, all other bottles via the
pneumatic tube system (PTS) to Microbiology at RHH. Please ensure
that porters and nurses etc are instructed to not send the sample for
protein/glucose to the NGH along with the sample for C&S
6 If the specimen is to be examined out of normal working hours,
ALWAYS inform the relevant biomedical scientists on duty.
CSF SAMPLES
SAMPLES
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 95 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
All volumes given are the minimum required
INVESTIGATION Volume of Number of Additional blood
CSF Drops sample required
Microbiology
Culture (bacterial/fungal)
Cell count
0.5ml
Gram film 10 NO
minimum
Indian ink film
(if indicated)
Z-N film Mycobacterial 0.5ml
10 NO
culture minimum
Cryptococcal antigen 0.5 ml 10 YES
0.25 ml
PCR 5 YES
minimum
Virology 0.5 ml 10 YES
Syphilis
Borrelia 0.25ml for 5 for each
YES
Leptosspira each test test
Toxoplasma
Clinical Chemistry
Glucose 0.25 ml 4-5 YES
Protein 0.25 ml 4-5 NO
Lactate 0.25 ml 4-5 NO
Serine Glycine 0.25 ml 4-5 YES
NB The plain 1 ml bottles issued by the laboratory for sending CSF samples for
protein estimation must only be used for this purpose. These bottles are non-
sterile and are not suitable for M, C & S requests. They should also not be used
for blood samples as this results in insufficient sample being collected - please
use the 1ml or 5ml labelled bottles supplied to the ward.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 96 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
SPECIMEN CONTAINERS
Please refer to the A-Z Laboratory test listing table for details of the type of specimen required for each test.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 97 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
PINK
Paediatric
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 98 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 99 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
A-Z LABORATORY TEST/CONDITIONS LIST
The table on the following pages gives an alphabetical list of analyses provided by either the laboratories at SCH or related laboratories giving
details of specific sample requirements and where they are analysed. For tests carried out by ISO 15189 accredited laboratories at SCH, the tests
listed are included in the accreditation schedule unless otherwise stated. For all tests analysed at SCH, the table also shows the expected
turnaround time (TAT) in routine situations. Turnaround times for histology samples can be found in the Histopathology section. Further
information on analyses referred to STH can be found in the STH Laboratory Medicine Handbook @
http://nww.sth.nhs.uk/NHS/LaboratoryMedicine/Default.asp?page=1.
Lab to send to codes
CC Clinical Chemistry HP Histopathology
CCM Clinical Chemistry Metabolic Laboratory POCT Point of care test (for CC in exceptional circumstances)
H Haematology and Blood Bank SDGS Sheffield Diagnostic Genetics Service
Referral lab codes
BCH Birmingham Children’s Hospital NAT National Hospital Neurology and Neurosurgery
BCITYH Birmingham City Hospital NEURO University College London, Institute of Neurology
BMU Biolab Medical Unit, London NGH Northern General Hospital
BUH Birmingham University Hospital NHSBT NHS Blood and Transplant
BRI Bristol Royal Infirmary NRVI Newcastle Royal Victoria Infirmary
CCFE Chalfont Centre For Epilepsy PRU Protein Reference Unit, Sheffield
CHILD University College London, Institute of Child Health RBH Royal Brompton Hospital
CHURCH Churchill Hospital, Oxford RDGH Rotherham District General Hospital
GEOR St George’s Hospital, London RHH Royal Hallamshire Hospital
GRI Glasgow Royal Infirmary SAS centre Supra – Regional Assay Centre
GUY Guy’s and St Thomas’ Hospital, London SGH Southampton General Hospital
JAMES St James’s University Hospital, Leeds SOUTH Southmead Hospital, Bristol
KING King’s College Hospital, London SRH Salford Royal Hospital
LLAN Llandough Hospital, Cardiff TROP Centre for Tropical Medicine and Global Health, Oxford
LRI Leicester Royal Infirmary UHSM University Hospital of South Manchester
LSTM Liverpool School of Tropical Medicine WILL Willink BGU, Central Manchester University Hospitals
MCH Manchester Children’s Hospital
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 100 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Acid-base (blood gas) Blood Arterial Siemens 0.8mL ≤10min Do not use non- CC -
Venous Rapidlyte heparinised (POCT)
balanced Plastipaks! Mix
heparin thoroughly by
syringe (3ml) rotation.
Acid-base (blood gas) Blood Capillary Heparinised 0.10mL ≤10min CC -
capillary See pH, pCO2, (POCT)
pO2, base excess
and bicarbonate.
Acid Lipase /Esterase - - - - - Refer to White cell - -
enzyme
Acid Glycoprotein (Orosomucoid) Blood Venous S. Gel 2ml - - CC NGH
ACTH (Adrenocorticotrophic hormone) Blood Venous EDTA 5ml - Bleep duty CC RHH
(1ml = biochemist prior to
min) collection 095.
Needs to be
received by lab
within 4hrs of
collection.
Acute Lymphoblastic Leukaemia (ALL)/BCR- Blood/Bone - EDTA 0.5-5ml 2-4 Must be sent to the SDGS -
ABL marrow weeks laboratory
immediately
Acute Lymphoblastic Leukaemia (ALL) (+/- Bone marrow - Universal with 0.25-1ml 10 days - SDGS -
FISH) /leukaemic 5-10ml of /5-10ml
blood transport
medium /Li
Hep tube
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 101 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Acute Myeloid Leukaemia (AML) (+/- FISH) Bone marrow - Universal with 0.25-1ml 10 days - SDGS -
/leukaemic 5-10ml of /5-10ml
blood transport
medium /Li
Hep tube
Acute Myeloid Leukaemia /AML/ AML- Blood/Bone - EDTA 0.5-5ml 2-4 Must be sent to the SDGS -
M2/AML-17 marrow weeks laboratory
immediately
Acute Myeloid Leukaemia /AML/ Flt3/NPM1 Blood/Bone - EDTA 0.5-5ml 7 days - SDGS -
mutation screen marrow
Acute phase reactants Blood Venous S. Gel 2ml - - CC NGH
Acute Promyeloic Leukaemia (APL)/AML Blood/Bone - EDTA 0.5-5ml 2-4 Must be sent to the SDGS -
M3/AML-17 marrow weeks laboratory
immediately
ADAMTS13 deficiency (thrombotic Blood Venous EDTA 0.5-5ml 8 weeks - SDGS -
thrombocytopenic purpura)
Adrenoleukodystrophy (ALD) (X-linked) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Acyl carnitine profile Bile - Guthrie card Two 4-6 PM samples CCM -
spots weeks
Acyl carnitine profile Blood Venous Li Hep 0.5ml 5-14 (PM samples TAT CCM -
plasma days 4-6 weeks)
Serum
Acyl carnitine profile Blood Spots Venous Guthrie card Two 5-14 (PM samples TAT CCM -
(Li Hep - spots days 4-6 weeks)
whole blood)
Acyl carnitine profile CSF - Plain tube 0.1ml 4-6 PM samples CCM -
weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 102 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Adenosine Deaminase (ADA) PNP Blood Venous EDTA 2.5ml - - H GUY
Adrenal cortical antibodies Blood Venous S. Gel 2ml - - CC NGH
Adrenaline / Noradrenaline Blood Venous Li Hep 2ml 2-4 Send on ice CC RBH
plasma weeks immediately
Adrenalin Urine 24 hrs Bottle 10ml - - CC NGH
contains 10-
30 mls
H2SO4
Adrenoleucodystrophy (ALD) gene mutation Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Alanine aminotransferase ALT, SGPT Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Albumin Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Alcohol (Ethanol) Blood Venous Fluoride Hep - 4h Contact lab to CC -
arrange analysis
Aldosterone Blood Venous Li Hep 2ml - Send to lab within CC SAS centre
plasma 2h of collection
Alkaline phosphatase (ALP) Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Alkaline phosphatase (ALP) isoenzymes Blood Venous S. Gel 0.5ml 4h Only send if total CC RHH
/capillary ALP elevated
ALK Breakapart (2p23) Paraffin - - - 1-2 Contact lab prior to SDGS -
embedded weeks referral
tissue biopsy
Alpha-1-antichymotrypsin - - - - - See acute phase CC -
reactants
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 103 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Alpha-1-antitrypsin - - - - - See acute phase CC -
reactants
Alpha fetoprotein (AFP) Blood Venous S. Gel 0.5ml - - CC NGH
Alpha Subunit Blood Venous S Gel 0.5ml - - CC BUH
Alpha-thalassaemia Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Alport Syndrome sequencing panel Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Aluminium Blood Venous Acid washed 2ml - Contact lab prior to CC NGH
plain tube collection. Do not
separate.
Alveolar rhabdomyosarcoma PETS 2x4u - - - 14 days - SDGS -
sections on
slides
Amino Acids Blood Venous or Li Hep 1ml 2 weeks - CCM -
capillary plasma
(serum /
fluoride OK)
Amino Acids Blood Spots Venous or Guthrie card Two 1 week Known patient CCM -
capillary (Li Hep - spots monitoring only
whole blood)
Amino Acids CSF - Plain tube 0.2ml 1 week Paired plasma CCM -
(fluoride OK) required
Amino Acids Hair - Plain - 2 Contact lab prior to CCM -
universal / months collection
specimen bag
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 104 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Amino Acids Urine Random / Plain 10ml 5 - 14 Do not use Z10 CCM -
24 hrs universal days containers for
Clinical Chemistry
samples
Aminophyline (Theophylline) Blood Venous / Li Hep 0.5ml - - CC RHH
capillary plasma
5 Aminosalicylic Acid Blood Venous S Gel 2 ml - - CC NGH
Amiodarone + Desethylamiodarone Blood Venous S Gel or Li 1 -2 ml - - CC LRI
Hep plasma
Ammonia Blood Venous / Li Hep 0.5ml <1hr Send on ice. No CC -
Arterial serum
Amylase Blood Venous / Li Hep 0.5ml 4h - CC -
capillary plasma
AMylotrophic Lateral Sclerosis and Dementia Blood Venous EDTA 0.5-5ml 16 - SDGS -
Next Generation Sequencing Panel weeks
Anaplastic large cell lymphoma ALK positive PETS 2x4m - - - 14 days - SDGS -
sections on
slides
Androgen Insensitivity Syndrome (Testicular Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Feminisation) weeks
Androgen metabolites Urine 24hr Plain bottle - - 24hr collection CC KING
preferred but will
accept 20ml spot
samples, absolute
min volume 2 ml.
Aneuploidy FISH test Amniotic Fluid - Sterile 2-5ml 2-3 - SDGS -
Sample Universal days
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 105 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
ANF (Anti Nuclear Factor) Blood Venous S. Gel 2ml - - CC NGH
Angiotensin converting enzyme (ACE) Blood Venous S. Gel 2ml - - CC RHH
Anti-phospholipid antibodies Blood - - - - See Auto immune CC NGH
antibodies
Anti-phospholipid antibodies Blood Venous Citrate or - - See coagulation H RHH
plain studies. This test is
for Haematology
patients only unless
previously
approved by the
Haematology
Consultants.
Anticonvulsants Blood - - - - See individual CC -
drugs
Anti -DNA antibodies Blood Venous S. Gel 2ml - - CC NGH
Anti Diuretic Hormone (ADH) Blood Venous Li Hep 2ml - Separate freeze CC SAS centre
plasma within 30 mins
Anti-Gliadin antibodies Blood Venous Plain tube 2ml - - CC NGH
serum
Antimicrosomal antibodies Blood Venous S. Gel 2ml - - CC NGH
Anti-mullerian hormone Blood Venous Plain tube 2ml - - CC RHH
Anti-neutrophil abs (not ANCA) Blood Venous S. Gel 1ml - By arrangement H NHSBT
with NHSBT Bristol Bristol
only
Anti nuclear factor(ANF) Blood Venous S Gel 2ml - - CC NGH
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 106 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Antithrombin Deficiency Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Anti-thrombin III Blood Venous Citrate 2.5ml Discuss See coagulation H RHH
studies
Anti-Xa (for low molecular weight heparin and Blood Venous Citrate 1.0ml Discuss D/W Haematology H -
unfractionated heparin control) (preferable). SpR or Consultant
Capillary if require
sample information on
acceptable when to take the
(for LMWH) sample. see Coag
if venous studies
access
difficult but
capillary
sample
bottle needs
to be
obtained
from the
Haem lab.
Apolipoprotein E (APOE) Blood Venous EDTA 0.5-5ml 6 weeks - SDGS -
APTT Ratio (for unfractionated heparin Blood Venous Citrate 1.0ml 2h Contact Haem H -
control) Consultant. See
Coag studies.
Array CGH (see CGH) - - - - - - - -
Arsenic Blood Venous EDTA 5ml - Exclude fish from CC SAS centre,
diet 5d prior to test Guildford
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 107 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Arsenic Urine Early Plain - - Exclude fish from CC SAS centre,
morning universal diet 5d prior to test Guildford
Ascorbic Acid in leucocytes Blood Venous EDTA 5ml - Bleep duty CC RHH
biochemist prior to
collection 095
ASOT (Anti-Streptolycin O Titre) Blood Venous S.Gel 2ml - - CC NGH
Aspartate amino transferase (AST) Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Ataxia Next generation sequencing panel SDGS -
(see hereditary ataxia and migraine panel)
Autoimmune Antibodies Blood Venous S. Gel 2-3ml - - CC NGH
B12 - vitamin - - - - See Haematinic CC -
assay
Barbiturates (overdose) Phenobarbitone Blood /random Venous Li Hep 2ml - - CC NGH
urine plasma/ plain
universal
Barbiturates (Theraputic) Blood Venous Li Hep 1ml - Trough after 14d of CC RHH
/capillary constant therapy
Batten’s Disease (Electron Microscopy) Blood Venous EDTA 2mls 6 weeks If enzyme assay HP RHH
required contact
duty Biochemist on
bleep 095 prior to
collection to obtain
sample
requirements
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 108 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Base Excess (calculated) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Base Excess (calculated) Blood Capillary Heparinised 0.10mL ≤10min Add capillary POCT -
capillary closing caps. Mix (CC)
thoroughly by
rotation.
Bernard-Soulier syndrome (GP1BA, GB1BB, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
GP9) weeks
Beta HCG (? pregnant) Blood Venous S. Gel 1ml - Min 200 µl serum CC RHH
/capillary
Beta HCG (? Tumour marker) Blood Venous / S. Gel or 1ml - Send with AFP and CC NGH
capillary / plain placental ALP
arterial
Beta-thalassaemia Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Actual Bicarbonate (calculated) – blood gas Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 109 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Actual Bicarbonate (calculated) – blood gas Blood Capillary Heparinised 0.10mL ≤10min Add capillary POCT -
analyser capillary closing caps. Mix (CC)
thoroughly by
rotation.
Bicarbonate (total carbon dioxide) Blood Venous Li Hep 0.5ml 4h (Plasma) CC -
/capillary
Bile Salts / Acids Blood Venous Li Hep 1ml 4 weeks Not for cholestasis CCM -
plasma in pregnancy
Bile Salts/Acids Urine Random Plain 5ml 4 weeks Not for cholestasis CCM -
universal in pregnancy
Bilirubin (conjugated including total Blood Venous Li Hep 0.5ml 4h - CC -
paediatric) /capillary plasma
Biotin - - - - - Bleep duty CC BMU
biochemist 095
Biopterins - - - - - Bleep duty CC BCH
biochemist 095
Biotinidase Blood Venous Li Hep 1ml 5-14 - CCM -
plasma days
Bladder cancer PETS 2x4m - - - 14 days - SDGS -
sections on
slides
Blood count - - - - - See FBC H -
Blood gases - - - - ≤10 See Acid -base POCT -
mins (CC)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 110 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Blood group & crossmatch Blood Venous EDTA 2.5ml Depend Telephone the H Difficult
ent on laboratory where cases
clinical request is urgent. referred to
need. Must use blood NHSBT,
Routine bank form. Sample Sheffield
request must be fully
s are 2 labelled. See
days for detailed section
a group ‘Requirements for
and Blood Bank’ and
save ‘Baby group and
crossmatch
samples for Blood
Bank Sample’
which describe
infant requests and
special needs
Blooms syndrome Blood Venous Li Hep 2-3ml 28 days Please inform the SDGS -
laboratory prior to
sample dispatch
Bone Biopsy for bone diseases Bone biopsy - - - See Send direct to Histo Histo RHH
Histo RHH RHH
section
Bone markers (Bone Specific Alkaline Blood Venous S. Gel/ plain 2ml - Allow to clot. CC NGH
Phosphatase) Random urine universal blood Separate within 4
10ml hrs of collection
urine
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 111 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Bone marrow biopsy Formalin fixed - See - See Use formalin safety HP -
Histopath Histo specimen bag
section for section
further details
Bone marrow investigations Bone marrow Discuss Discuss Discuss Discuss Contact cons H -
Haem. See detailed
section
Bone profile Blood Venous / Li Hep 0.5ml 4h Calcium, albumin, CC -
capillary plasma phosphate, alkaline
phosphatase
BRAF (V-raf murine sarcoma viral oncogenes PETS 8x10m - - - 1-2 - SDGS -
homolog B1) p.Val600Glu mutation sections in weeks
universal
Brain Biopsy Brain biopsy - - - See Send direct to Histo - RHH
Histo RHH. If fresh must
section be delivered by
hand.
Breast Cancer - HER2 FISH PETS 2x4m - - - 14 days - SDGS -
sections on
slides
Bromide Blood Venous/ Lith hep/ S 1 ml - - CC NGH
capillary Gel
Bruck Syndrome (PLOD2) Blood Venous EDTA 0.5 -5ml 2-8 - SDGS -
weeks
Burkitt lymphoma PETS 2x4m - - - 14 days - SDGS -
sections on
slides
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 112 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
C peptide Blood - - - - See Insulin CC RHH
C- reactive protein CRP Blood Venous / Li Hep 0.5ml 4h - CC -
capillary plasma
C1 esterase inhibitor Blood Venous S. Gel 2ml - - CC NGH
C3 conversion Blood Venous EDTA 2ml - - CC NGH
C3 nephrotic factor Blood Venous / S. Gel 2ml - - CC NGH
capillary
C4 Blood Venous / S. Gel 2ml - - CC NGH
capillary
Caeruloplasmin Blood Venous S. Gel 2ml - Min 200µl serum CC NGH
Caffeine Blood Venous / Li Hep 0.5ml 7 days Assayed weekly on CC -
capillary plasma Tuesday
CA125 Blood Venous S Gel 2ml - - CC NGH
Calcitonin Blood Venous EDTA or 3-5ml -
Bleep duty CC NGH or
serum biochemist prior to SAS centre
collection 095
Calcium (ionised) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Calcium (ionised) Blood Capillary Heparinised 0.10mL ≤10min Mix thoroughly by POCT -
capillary rotation. (CC)
Calcium (total) Blood Venous / Li Hep 0.5ml 4h - CC -
capillary plasma
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 113 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Calculi (stones) Stones - - - - - CC LRI
CALR Exon 9 mutation screen (?PMF and Blood/Bone Venous EDTA 0.5-5ml 2 weeks - SDGS -
?ET) Marrow
Carbamezapine (Tegretol) Blood Venous / Li Hep 0.5 ml - - CC RHH
capillary plasma
Carbon dioxide (total) Blood - - - - See bicarbonate CC -
Carbon monoxide Blood Venous / Heparinised - - - POCT -
capillary syringe/capill (CC)
ary
Carboxyhaemoglobin (COHb; reported as Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
%Hb) – blood gas analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Carboxyhaemoglobin (COHb; reported as Blood Capillary Heparinised 0.10mL ≤10min Mix thoroughly by POCT -
%Hb) – blood gas analyser capillary rotation. (CC)
Cardiolipin Blood Venous S. Gel 2 ml - - CC NGH
Cardiolipin (For Barth Syndrome) Blood Venous EDTA 1-3ml - Send Mon-Thur CC BRI
only
Carotene Bllood Venous Li Hep /S Gel 5ml - Protect from light CC RDGH
Carnitine See Acylcarnitine CCM -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 114 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Carnitine Urine Random / Plain 10ml 5-14 Do not use Z10 CCM -
24 hrs universal days containers for
Clinical Chemistry
Samples
Carnitine Acylcarnitine Translocase (CACT) Blood or Venous EDTA 0.5-5ml 2-8 - SDGS -
Deficiency Fibroblasts weeks
Carnitine Palmitoyl Transferase Type2 Blood or Venous EDTA 0.5-5ml 2-8 - SDGS -
(CPT2) Deficiency Fibroblasts weeks
Carnitine Palmitoyl Transferase Type2 Fibroblasts - - - 6-8 - CCM -
weeks
Carotenoids - - - - - See Vitamin A CC -
Cartilage-associated protein (CRTAP) – Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
autosomal recessive OI weeks
Catecholamine metabolites Urine - - - - See VMA & VHA CCM -
Catecholamines - - - - - See adrenaline & CC NGH
nor-adrenaline
CEA (carcinoembryonic antigen ) Blood Venous S Gel 2 ml - - CC NGH
CBCL/CTCL / Skin lymphoma/ mycosis Paraffin - - 5 micron 2-8 - SDGS -
fungoides (IgH or T cell gene embedded unmount weeks
rearrangements) tissue biopsy ed
sections
CD34+ cell count Blood Venous EDTA 2.5ml Discuss Contact consultant H -
haematologist prior
to collection
Cerebral AD Arteriopathy with Subcortical Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Infarcts & Leukoencephalopathy - CADASIL weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 115 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
CGH/microarray Blood Sample Venous EDTA/Li Hep 2-3ml 6-12 - SDGS -
months
Chimerism/pre or post bone marrow/stem cell Blood/Bone - EDTA 0.5-5ml 10 days - SDGS -
transplant (BMT/SCT)/donor for marrow
BMT/SCT/matched unrelated donor (MUD) –
Sex matched (Powerplex)
Chimerism/pre or post bone marrow/stem cell Blood/Bone - EDTA 0.5-5ml 10 days - SDGS -
transplant (BMT/SCT)/donor for marrow
BMT/SCT/matched unrelated donor (MUD) –
Sex mis- matched (FISH)
Chitotriosidase Blood Venous EDTA 2-5ml - - CC WILL
Chloride Blood Venous / Li Hep 0.5ml 4h - CC -
capillary plasma
Chloride (blood gas analyser) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous / Rapidlyte syr. syr. heparinised (CC)
Capillary balanced containers. Mix
heparin 0.10mL ≤10min thoroughly by
syringe (3ml) cap. cap. rotation.
or capillary
closing caps.
Chloride Sweat - - - - See sweat test CC -
Cholestanol Blood Venous Li Hep or 1ml 4 weeks - CCM -
serum
Cholesterol Blood Venous / Li Hep or 0.5ml 4h Fasting sample CC -
capillary serum
Cholinesterase Blood Venous EDTA 2-5ml - - CC SOUTH
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 116 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Chromogranin A Blood Venous S. Gel 2-3ml - Part of standard gut CC NGH
hormone profile
Chromosome – Adult (with or without FISH) Blood Venous / Li Hep 2-3ml 28 days - SDGS -
capillary
Chromosome –Child (with or without FISH) Blood Venous / Li Hep 1-2ml 28 days - SDGS -
capillary
Chromosome –Neonate Blood Venous / Li Hep 0.5 – 10 days * smaller samples SDGS -
capillary 1ml* can be attempted
but may reduce the
likelihood of a
successful result
Chromosome (with or without FISH) Amniotic Fluid - Sterile 10-20ml 14 days - SDGS -
PRENATAL sample universal
Chromosome (with or without FISH) CVS - Sterile 3-4 14 days CV direct usually SDGS -
PRENATAL universal in fronds next working day.
transport
medium
Chromosome (with or without FISH) Fetal blood - Li Hep 0.5-1ml 10 days - SDGS -
PRENATAL cordocentesis
Chromosome (with or without FISH) Cord blood - Li Hep 1-3ml 10 days - SDGS -
POSTNATAL
Chromosome (with or without FISH) Placental - Sterile tissue <1cm 28 days - SDGS -
FETAL LOSS biopsy at cord culture cubed
insertion sire, medium pots
fetal
membrane,
villi, cord
biopsy.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 117 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Chromosome (with or without FISH) Skin biopsy - Sterile tissue 1-2mm 2-3 - SDGS -
culture cubed weeks
medium pots
Chromosome (with or without FISH) Solid Tumour - Universal with <1cm 2-3 - SDGS -
Biopsy 5-10ml of cubed weeks
transport
medium
Chronic Lymphoproliferative Leukaemia Bone marrow - Universal with - 28 days - SDGS -
(CLL) - FISH 5-10ml of
transport
medium
Chronic Myeloid Disease (CML) karyotyping Bone marrow - Universal with 0.25-1ml 28 days Urgent samples SDGS -
& BCR ABL1 FISH /leukaemia 5-10ml of BM or have a TAT of 14
blood transport 1ml days. See SDGS
medium /Li BM/VB section
Hep tube
Chronic Myeloid Leukaemia (CML)/leukemic Blood/Bone - EDTA 0.5-5ml 14 days Must be sent to the SDGS -
BCR-ABL1 quantification marrow laboratory
immediately
Cleido Cranial Dysplasia Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Clonazepam Blood Venous Fluoride 1ml - - CC RHH
Coagulation factor assay/other studies Blood Venous. Citrate Contact Discuss Fill level is crucial. H Some to
lab See detailed RHH
section for
description of tests
available
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 118 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Coagulation screen Blood Venous. NB Citrate 1.0ml 2h Fill level is crucial. H -
not See Haematology
capillary Specialist
Coagulation
assays/studies.
Section for
description of tests,
anticoagulation
therapy control and
D-Dimers in ?DVT
Coeliac screen - - - - - See anti-glyadin CC -
antibodies
Cold Agglutinins Blood Venous EDTA & plain 1ml 1 day Samples must be H -
tube EDTA transported to the
plus laboratory while
>2ml still warm
plain
tube
Collagen 6 related myopath panel Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Collagen screen Blood Venous S. Gel 2ml - - CC NGH
Colorectal Cancer (HNPCC/FAP) Extended Venous EDTA 0.5-5ml 12
- - SDGS -
Gene Panel weeks
Complement C3, C4 only Blood Venous EDTA/ S. Gel 2-3ml - State on form CC NGH
whether plasma or
serum. If left for
longer than 1 night -
freeze
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 119 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Complement CH50, APCH50 functional Blood Venous S. Gel 2-3ml - Send within 2hrs of CC NGH
activity of either pathway collection.
Congenital Bilateral Absence of Vas Deferens Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(CBAVD) weeks
Congenital thrombotic thrombocytopenic Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
purpura (ADAMTS13 deficiency) weeks
Copper Blood Venous / Li Hep 0.75ml - 2ml venous sample CC NGH
capillary plasma required for zinc,
caeruloplasmin
Copper Liver biopsy Fresh - - - - See Histopathology HP -
section
Cortisol Blood Venous Li Hep, 0.5 ml 4-24 h - CC -
/capillary min
Creatinine Blood Venous / Li Hep, S.Gel 0.5ml 4h - CC -
capillary plasma
Creatine kinase CK (or Creatine Blood Venous / Li Hep 0.5ml 4h - CC -
phosphokinase CPK) capillary plasma
Cri-du-chat syndrome Blood Venous Li Hep 2-3ml 28 days - SDGS -
Crigler-Najjar Syndrome types I and II Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Cryoglobulins Blood Venous EDTA and 2ml of - Contact CC Lab. CC NGH
S.Gel each Keep at 37C
Crossmatch Blood - - - - See Blood group & H -
crossmatch
CRTAP (autosomal recessive OI) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 120 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
CSF Amino Acids CSF - Plain 0.5ml 1week Require paired
plasma, contact lab
if NKH suspected
CSF cytology CSF - Plain - See Send direct to Histo - RHH
Universal Histo RHH
section
CSF cell count CSF - Plain x 3 15 drops 5h Haemic cell count. H -
x3 Ensure 3 vials are
labelled 1,2 & 3
CSF glucose CSF - Fluoride 0.5ml 4h - CC -
CSF protein CSF - Plain 0.5ml 4h - CC -
Cutis Laxa sequencing panel Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Cyanide Blood Venous Fluoride 1ml - - CC NGH
Whole blood
Cyclosporine (Ciclosporin) Blood Venous / EDTA 0.5ml 2-24h Analysed Tue and CC -
capillary Fri, urgent requests
only at other times.
Must be received
before 15.00 for
analysis that day
CYP2C19 Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
CYP3A4 Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 121 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Cystic fibrosis Blood or Venous EDTA 0.5-5ml 1-8 - SDGS -
Guthrie spots weeks
Cystine Urine Random / Plain 10ml 5-14 - CCM -
24 hrs universal days
Cystine in leucocytes Blood - Li Hep 3ml - Please contact Duty CC JAMES
Biochemist
D-Dimers (DIC) Blood Venous Citrate 1ml Depend Fill level is critical H -
ent on
Clinical
Urgency
D-Dimers (VTE) Blood Venous Citrate 1ml Depend Discuss with clinical H RHH
ent on Haematology team
Clinical prior to request
Urgency
7-Dehydrocholesterol Blood Venous Li Hep 1ml 4 weeks - CCM -
plasma
7-Dehydrocholesterol (Prenatal test for Smith Amniotic fluid 10mls 5 days -
Lemli Optiz Syndrome)
8-Dehydrocholesterol Blood Venous Li Hep 1ml 4 weeks - CCM -
plasma
Delta F508 - - - - - See Cystic Fibrosis SDGS -
Dentatorubral pallidoluysian atrophy (DRPLA) Blood Venous EDTA 0.5-5ml 2-6 - SDGS -
weeks
Dermatofibrosarcoma protuberans PETS 2x4m - - - 14 days - SDGS -
sections on
slides
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 122 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
DHEAS Blood Venous/ Serum/ 200µl - - CC RHH
capillary plasma
DHR Blood Venous EDTA whole 0.5ml - Plus 0.5ml EDTA CC NGH
blood Control patient
DHT ( Di hydrotestosterone ) Blood Venous Li Hep/S.Gel 500µl - - CC SAS centre
Diamond Blackfan Anaemia (RPS19) Blood - EDTA 0.5-5ml 2-8 - SDGS -
weeks
Diamond Blackfan Anaemia (dosage testing Blood - EDTA 0.5-5ml 8 - SDGS -
by MPLA) weeks
Diazepam (with nordiazepam) Blood Venous Li Hep/S. Gel 2ml CC RHH
- -
Dibucaine number - - - - - See CC -
pseudocholin’ase
Differential WBC - - - - - See FBC H -
Digoxin Blood Venous / S. Gel 1 ml - Ideally 6-8hrs post CC RHH
capillary dose
Dimethylglycine Urine Random Plain 2ml 4-6 Do not use Z10 CCM -
universal weeks containers for
Clinical Chemistry
Samples
Direct anti-globulin test (DAT, DCT) Blood Venous EDTA 0.5ml 24hours Use blood bank H -
/capillary form.
Dopamine - - - - - See Adrenalin CC RHH
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 123 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Dopa-responsive dystonia (Segawa Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
syndrome), dominant weeks
Dopa-responsive dystonia, recessive Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Tyrosine hydroxylase deficient weeks
Down syndrome – PRENATAL (with or Amniotic fluid - Sterile 10-20ml 10-14 *Rapid FISH test SDGS -
without FISH) universal days* usually reported the
next working day
Down syndrome – POSTNATAL - - - - - See chromosome - -
Dystonia 1 or Idiopathic Torsion Dystonia, Blood Venous EDTA 0.5-5ml 2-6 - SDGS -
dominant weeks
Dystonia and parkinsonism Next Generation Blood Venous EDTA 0.5-5ml 16 - SDGS -
Sequencing Panel weeks
Dystrophia myotonica (DM) Blood Venous EDTA 0.5-5ml 2 weeks - SDGS -
EBV or CMV PCR Blood Venous EDTA 2ml - - CC NGH
EGFR (exons 18-21) PETS 8x10μ - - - 7 days EGFR testing from SGDS -
sections in required, please
universal or contact laboratory
tumour block
Ehlers-Danlos Classical (COL5A1 and Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
COL5A2) weeks
Ehlers Danlos Next Generation Sequencing Blood Venous EDTA 0.5-5ml 12 - SDGS -
Panels (Vascular, Classic and Kyphoscoliotic) weeks
Ehlers-Danlos Syndrome Classical Skin - - - 2-8 - SDGS -
(COL5A1)- Null allele biopsy/cultured weeks
fibroblasts
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 124 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Ehlers-Danlos Syndrome-hypermobile Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(TNXB) weeks
Ehlers-Danlos Syndrome-KMH (FKBP14) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Ehlers-Danlos Syndrome-Kyphoscoliotic Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(PLOD1) weeks
Ehlers-Danlos Syndrome- Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
musculocontractural (CHST14) weeks
Ehlers-Danlos Syndrome – vascular Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(COL3A1) weeks
Ehlers-Danlos Syndrome arthrochalasic Blood Venous EDTA 0.5-5mn 2-8 - SDGS -
(COL1A1 and COL1A2) weeks
Electrolytes Blood Venous/ Li Hep 0.5ml 4h See potassium, CC -
capillary plasma sodium , chloride,
bicarbonate
Electron Microscopy Various Biopsy Tube Small 8 wks Fixative should be HP RHH
containing biopsy stored at 4ºC and
gluteraldehyd applied within 5
e fixative mins. Deliver
(available promptly to Lab.
from Histo)
Endomysial Antibodies Blood Venous/ S Gel 2ml - - CC NGH
capillary
Enzymes - - - - - See individual CC -
enzymes
Episodic ataxia type 1 Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 125 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Episodic ataxia Next generation sequencing Blood Venous EDTA 0.5-5ml 8 weeks - SDGS -
panel
Epoxy Carbemazepine Blood Venous / S Gel 2ml - - CC NGH
Capillary
ESR Blood Venous/ EDTA 0.5ml 24h Can be performed H -
capillary along with FBC
Ethosuximide Blood Venous/ Li Hep 1ml - Store 4°C CC NGH
capillary
Ethylmalonic acid Urine Random Plain 5 ml 4-6 Do not use Z10 CCM
universal weeks containers for
Clinical Chemistry
Samples
Extended lymphocyte markers Blood Venous/ EDTA 1.0ml - By special H RHH, NGH
capillary arrangement RHH, or NRVI
Immunology NGH
or Immunology
Newcastle
dependant on
clinical situation.
Ewings sarcoma and rearrangement of PETS 2x4m - - - 14 days - SDGS -
EWSR1 associated with clear cell sarcoma, sections on
extraskeletal myxoid chondrosarcoma and slides
desmoplastic small round cell tumour
Factor V deficiency (F5) Blood Venous EDTA 0.5-5ml 8 weeks - SDGS -
Factor XI Deficiency (Haemophilia C) Blood Venous EDTA 0.5-5ml 2-8 SDGS -
molecular test weeks
Factor XIII Deficiency molecular test Blood Venous EDTA 0.5-5ml 2-8 SDGS -
weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 126 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Faecal alpha 1 antitripsin Faeces Random Faecal pot 10g - Freeze immediately CC PRU
faeces
Faecal calprotectin Faeces Formed Faecal pot - - - CC RDGH
faeces
Faecal elastase Faeces Formed Faecal pot - - Not suitable for CC RHH
faeces patients < 2 wks old
Faecal fat Faeces - - - - Fat globule - NGH
microscopy
recommended.
Contact Clin Chem
duty biochemist
bleep 095
Faecal Occult Blood Faeces - Faeces pot - - - CC BCH
Familial Adenomatous Polypsis Coli (FAP) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(APC sequencing and MLPA) weeks
Familial Adenomatous Polypsis Coli (FAP) & Blood Venous EDTA 0.5-5ml 2-8 - SGDS -
MUTYH Gene Panel (APC & MUTYH weeks
sequencing and MLPA)
Familial hemiplegic migraine next generation Blood Venous EDTA 0.5-5ml 8 weeks - SDGS -
sequencing panel.
Familial hypercholesterolaemia (LDLR Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
sequencing and MLPA ApoB p.(Arg3527Gln) weeks
mutation analysis; PCSK9 p.(Asp374Tyr)
mutation analysis)
Familial motor neurone disease / amyotrophic Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
lateral sclerosis with or without frontotemporal weeks
dementia (ALS/FTD) C9orf72 gene
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 127 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Familial motor neurone disease / amyotrophic Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
lateral sclerosis (ALS) SOD1 gene weeks
Familial motor neurone disease / amyotrophic Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
lateral sclerosis (ALS) TARDBP gene weeks
Familial Porencephaly (COL4A1 & COL4A2) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Familial Porencephaly (COL4A1 & COL4A2) Blood Venous EDTA 0.5-5ml 12 - SDGS -
by Next generation Sequencing weeks
Familial Thoracic Aortic Aneurysms Next Blood Venous EDTA 0.5-5ml 12 - SDGS -
Generation Sequencing Panel weeks
Fanconi anaemia Blood Venous Li Hep 2-3ml 28 days Please inform the SDGS -
laboratory prior to
sample dispatch
Fanconi Anaemia (FANCA, FANCC, FANCG) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
FBC (full blood count) Blood Venous / EDTA 1ml 24 1ml suff for film, H -
capillary hours ESR, GF test and
retics also. See
detailed section for
tests included
Ferritin Blood Venous / Li Hep 0.5ml 2-72 hrs - CC
arterial
Fibrinogen - - - - - See Coagulation H -
screen
Fibrinogen disorders (FGA, FGB, FGG) Blood Venous EDTA 0.5-5ml 8 weeks - SDGS -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 128 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
Film for blood cell morphology Blood Venous / EDTA - 24 Performed only if H -
capillary hours FBC findings or
clinical details
indicates
appropriate
FISH Constitutional Tests – see table below Blood Venous Li Hep 2-3ml Depend - SDGS -
for list of tests ent on
urgency
CONSTITUTIONAL FISH TEST
Gene Comments
In Chromosome Order 1-22,X,Y
1p36.33 microdeletion syndrome (inc.
CEB108/T7 and D1Z2 Terminal and interstitial deletions detected
hypertrichotic osteochondrodysplasia)
2q37.3 Brachydactyly-mental retardation
microdeletion syndrome (inc. Albright
D2S447
hereditary osteodystrophy (AHO)-like
metacarpal/metatarsal shortening)
4p16.3 Wolf-Hirschhorn microdeletion syndrome WHSC1
5p15.3 Isolated Cat Cry microdeletion syndrome
FLJ25076 (ICS) and
(ICS) and 5p15.2 Cri Du Chat microdeletion
CTNND2 (CDC) respectively
syndrome (CDC)
5q35 Sotos microdeletion syndrome NSD1
7q11.23 Williams microdeletion syndrome ELN
7q11.23 microduplication syndrome (inc. speech
ELN
delay, ADHD)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 129 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
CONSTITUTIONAL FISH TEST
Gene Comments
In Chromosome Order 1-22,X,Y
8q12.1-12.2 CHARGE microdeletion syndrome
(inc.ocular coloboma, heart defects of any type,
CHD7
atresia of the choaneae, retardation, genital and
ear anomolies)
8q23.3-8q24.1 Langer-Giedion microdeletion
TRPS1 and EXT1
syndrome (inc. trichorhinophalangeal syndrome
respectively
type 1 and multiple cartilaginous exostoses)
9q34.3 Kleefstra microdeletion syndrome (inc.
craniofacial features, hypotonia, obesity, D9S325
microcephaly and speech delay)
15q11.2 Prader-Willi microdeletion/
SNRPN For 1st line test see molecular genetic referral
microduplication syndrome
15q11.2 Angelman microdeletion syndrome D15S10/UBE3A For 1st line test see molecular genetic referral
16p13.3 Rubenstein-Taybi microdeletion
syndrome (inc. short stature, talon cusps, patellar CREBBP
dislocation, broad thumbs and big toes)
17p13.3 Miller-Dieker microdeletion syndrome LIS1 (PAFAH1B1)
17p11.2 Smith-Magenis microdeletion syndrome RAI1
17p11.2 Potocki-Lupski microduplication
syndrome (inc. neonatal hypotonia, sleep apnea,
RAI1
hyperactivity, structural cardiovascular
abnormalities)
17q11.2 NF1 (Von Recklinghausen) microdeletion
NF1 (RP1-4C23) Home grown
syndrome
17q21.31 microdeletion syndrome (inc. neonatal
hypotonia, developmental delay and speech MAPT
delay)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 130 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
CONSTITUTIONAL FISH TEST
Gene Comments
In Chromosome Order 1-22,X,Y
22q11.2 DiGeorge/VCFS microdeletion or
TBX1
microduplication syndrome
22q13.3 Phelan-McDermid microdeletion
N85A3 is the control sequence for TBX1
syndrome (inc. neonatal hypotonia, absent or N85A3
delayed speech)
Xp22.3 or Yp11.32 Leri-Weill Dyschondrosteosis
inc. short stature and madelung deformity
(heterozygous microdeletion syndrome) or Langer Located in the PAR1 pseudoautosomal regions
SHOX
Mesomelic Dysplasia inc. severe short stature of both X and Y chromosomes
and skeletal abnormalities (homozygous
microdeletion syndrome)
Xp22.3 Kallmann microdeletion syndrome (inc.
KAL1
hypogonadotrophic hypogonadism and anosmia)
Xp22.3 Steroid Sulphatase Deficiency
STS
microdeletion syndrome inc. X-Linked Ichthyosis
Critical for the determination of phenotypic
Xq13.2 X inactivation centre deletion XIST
severity of abnormal X chromosomes
Yp11 Swyer microdeletion syndrome (XY female)
and detection of unbalanced t(X;Y) leading to XX SRY Sex determining region
with male phenotype
XCEN/YCEN/18CEN/13q14/21q22.13-q22.2 Sex DXZ1/DYZ3/D18Z1/RB1/D21
chromosome aneuploidy, Edward, Patau and S342, Common aneuploidy detection
Down syndrome D21S341,D21S259
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 131 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to
Test Tube Volume TAT Notes/Comments Referred to
type type send to
FISH Oncology Tests – see table below for Blood/Bone - Universal with - Depend - SDGS -
list of tests marrow or 5 – 10mls of ent on
paraffin transport urgency
embedded medium/Li
tissue Hep tube
ONCOLOGY FISH TEST
Gene Comments
A – Z by gene name
AFF1 (MLLT2)/MLL dual fusion 4q21-22/11q23
ALK Breakapart 2p23 All variants (contact lab before referral)
ALK/EML4 Dual Fusion inv(2)(p21p23)
BCL2 Breakapart 18q21 All variants
BCL6 Breakapart 3q26.2 All variants
Tricolour –Complex deletion rearrangement
BCR/ABL1/ASS Dual Fusion t(9;22)(q34;q11)
pattern monitoring possible
BLADDER PANEL- Single locus probes 3, 7 and 17 aneuploidy detection and 9 short
3CEN/7CEN/9p21/17CEN
D3Z1/D7Z1/p16/D17Z1 arm deletion detection
CBFB Breakapart 16q22 All variants
inv(16)(p13q22) and
CBFB/MYH11 Dual Fusion
t(16;16)(p13;q22)
CCND1 Breakapart 11q13 All variants
CCND1/D11Z1 Single locus probes 11q13/11CEN CCND1 amplification detection
CDKN2C(p18)/CKS1B amplification in MM
1p32.3/1q21 CDKN2C deletion / CKS1B
single locus probes
CERVICAL PANEL Single locus probes
Detection of hTERC and/or MYC gain
hTERC/MYC/D7Z1 3q26.2/8q24/7CEN
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 132 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
ONCOLOGY FISH TEST
Gene Comments
A – Z by gene name
CHD5/1qter single locus probes 1p36 Short arm deletion detection
CLL PANEL Single locus probes
11q22.3/17p13.1 Deletion detection
MIX 1 - ATM/TP53
Aneusomy 12 and aneusomy 13 or
12CEN/13q14.3/13q34 heter/homozygous long arm deletion detection
MIX 2 – D12Z3/D13S319/13q34
D1Z2 Single locus probe 1p36 Short arm deletion detection
D8Z2 Single locus probe 8CEN Aneusomy 8 detection
D12Z3 Single locus probe 12CEN Aneusomy 12 detection
D7S522/D7Z1 Single locus probes 7q31/7CEN Monosomy or long arm deletion detection
D13S25 Single locus probe 13q14 Monosomy or long arm deletion detection
D13S319 Single locus probe 13q14 Monosomy or long arm deletion detection
D20S108 Single locus probe 20q12 Monosomy or long arm deletion detection
DDIT3 Breakapart 12q13 All variants formerly CHOP
DEK/NUP214 Dual Fusion t(6;9)(p22;q34)
Dermatofibrosarcoma protruberans panel
Detection of t(17;22)(q22;q13) and amplification
chromosomes COL1A1 and PDGFB – 17q22 and 22q13
in supernumerary ring
breakapart probes
DXZ1/DYZ3 Single locus probes XCEN/YCEN Sex mismatched monitoring
EGR1/D5S23,D5S721 5q31/5p15.2 Monosomy or long arm deletion detection
EML4 Breakapart 2p21 All variants
ETV6 Breakapart 12p13 All variants
ETV6/RUNX1 Dual Fusion t(12;21)(p13;q22) Formerly TEL/AML1
Tricolour
EVI1 (D3S1243/hTERC/RH123089) Breakapart 3q26.2
All variants
EWSR1 Breakapart 22q12 All variants
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 133 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
ONCOLOGY FISH TEST
Gene Comments
A – Z by gene name
EWSR1/FLI1 Dual Fusion t(11;22)(q24;q12)
FGFR1/D8Z2 Breakapart and single locus probe 8p11/8CEN All variants and FGFR1 amplification
All variants Formerly FKHR
FOXO1 Breakapart 13q14
See also PAX3
FUS Breakapart 16p11 All variants
GLIOMA PANEL Single locus probes
Mix 1 –
1p36/1q25
EGFL3,TP73/ANGPTL1,ABL2 Loss of 1p relative to 1q and loss of 19q
Mix 2 - ZNF44,ZK1,MAN2B1/GLTSCR1+2,CRX relative to 19p
19p13/19q13
HER2/D17Z1 Single locus probes 17q11.2-q12 HER2 amplification detection
17q11.2-q12/ HER2 amplification detection and TOP2A
HER2/TOP2A/D17Z1 Single locus probes
17q21-22/17CEN deletion
IGH Breakapart 14q32 All variants
IGH/BCL2 Dual Fusion t(14;18)(q32;q21)
IGH/CCND1,MYEOV Dual Fusion t(11;14)(q13;q32)
IGH/FGFR3 Dual Fusion t(4;14)(p16;q32)
IGH/MAF Dual Fusion t(14;16)(q32;q23)
IGH/MAFB Dual Fusion T(14;20)(q32.33;q11.1-q13.1) MM
IGH/MYC/D8Z2 Dual Fusion t(8;14)(q24;q32) Aneusomy 8 also detected
IGK Breakapart 2p12 All variants
IGL Breakapart 22q11 All variants
MALT Breakapart 18q21 All variants
MDM2/D12Z1 Single locus probes 12q14.3-q15/12CEN MDM2 amplification detection
MELANOMA PANEL Single locus probes
D6Z1/RREB1/MYB/CCND1 6CEN/6p25/6q23/11q13
MLL Breakapart 11q23 All variants
MYB Single locus probe 6q23 Long arm deletion detection
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 134 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
ONCOLOGY FISH TEST
Gene Comments
A – Z by gene name
MYC Breakapart 8q24 All variants
MYC/D8Z2 Single locus probes 8q24/8CEN Detection of gain of 8q24 relative to 8CEN
N-MYC/D2Z1 Single locus probes 2p24/2CEN N-MYC amplification detection
NUP98 breakapart 11p15 AML, ALL, CML-bc
p16(D9S1749-D9S1752)/CEP9 Single locus
9p21/9CEN Short arm deletion detection
probes
All variants
PAX3 Breakapart 2q35
See also FOXO1
PBX1/TCF3 dual fusion probe t(1;19)(q23;p13.3) ALL
4q12 FIP1L1/CHIC2/PDGFRA Tricolour
PDGFRA /LNX/ SCFD2 Breakapart
rearrangement All variants
PDGFRB Breakapart 5q32 All variants
PIK3CA Single locus probe 3q26.32 PIK3CA amplification detection
PML/RARA Dual Fusion t(15;17)(q22;q21)
PROSTATE PANEL
Mix 1 – Tricolour, all variants
Mix 1 – TMPRSS2/ERG Breakapart 21q22
Mix 2 - Long arm deletion detection
Mix 2 - PTEN/CEP10 Single locus probes 10q23/10CEN
PTEN/CEP10 Single locus probes 10q23/10CEN Long arm deletion detection
RARA Breakapart 17q21 All variants
RB1 13q14 Monosomy or long arm deletion detection
ROS1 Breakapart 6q22 All variants
RUNX1/RUNX1T1 Dual Fusion t(8;21)(q22;q22) Formerly AML1/ETO
SEC63/D6Z1 6q21/6CEN Long arm deletion detection
SS18 Breakapart 18q11.2 All variants Formerly SYT
TCF3 Breakapart 19p13.3 All variants, formerly E2A
TCR a/d Breakapart 14q11.2 All variants
TP53/D17Z1 Single locus probes 17p13.1/17CEN Short arm deletion detection
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 135 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
ONCOLOGY FISH TEST
Gene Comments
A – Z by gene name
TP53/MPO Single locus probes 17p13.1/17q22 i(17q) detection
Uveal Melanoma Single Locus Probes 3 centromere and 8
Aneuploidy detection
D3Z1/D8Z2 centromere
ZNF217 20q13.2 ZNF217 amplification detection
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Fish Odour Syndrome Urine - - - - See Trimethylamine CCM -
& Dimethyglycine
Fish Odour Syndrome (Molecular Genetic - - - - - See - -
testing) Trimethylaminuria
Fk506 (tacrolimus ) Blood Venous / EDTA whole 0.5ml 1 day - CC -
capillary blood
Fluoride number Blood - - - - See CC -
pseudocholin’ase
Folate - - - - - See Haematinic CC -
assay
Follicle stimulating Hormone FSH Blood Venous Li Hep / S. 2ml - - CC RHH
Gel
Follicular lymphoma / DLBCL PETS 2x4m - - - 14 - SDGS -
sections on days
slides
Fragile X syndrome Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Free fatty acids Blood - - - - See Intermediary CCM -
metabolites
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 136 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Free T3, T4 Blood Venous Li Hep 1ml 1-3 - CC -
days
Friedreich Ataxia Blood Venous EDTA 0.5-5ml 2-6 - SDGS -
weeks
Fructose-1,6-bisphosphatase deficiency Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Fumarate hydratase Amniotic Fluid - Plain 5ml ASAP Please contact the CCM -
universal metabolic lab prior to
collection
Fumarate hydratase Fibroblasts - Culture 1-2 mm 2 Refer to Skin CCM -
medium months Biopsies
Fumarate Hydratase Deficiency (FH Blood or Venous EDTA 0.5-5ml 2-8 - SDGS -
sequencing and MPLA) Fibroblasts weeks
Galactitol Urine Random Plain 5ml 5-14 Please contact the CCM -
universal days duty biochemist
Galactokinase Blood Venous Lith Hep 1 ml - Send on ICE CC SOUTH
Whole blood
Galactosaemia screen Blood Venous or Li Hep whole 0.5ml 2 days Not EDTA CCM -
capillary blood
Galactosaemia screen Blood Spots Venous or Guthrie card Two 1 week - CCM -
capillary (Li Hep - spots
whole blood)
Galactose-1-phosphate Blood Venous Li Hep whole 5ml Send Please contact the CCM -
blood away duty biochemist
Galactose-1-phosphate uridyl transferase Blood - - - - See Galactosaemia CCM -
screen
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 137 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Gamma glutamyl transferase GGT Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Gastrin - - - - - Bleep duty CC SAS
biochemist prior to centre
collection 095
GATA2 Blood/Bone Venous EDTA 0.5-5ml 8 - SDGS -
Marrow weeks
Gentamicin Blood Venous / S. Gel / plain 1ml - - CC -
capillary
Gilbert syndrome Blood Venous EDTA 0.5-5ml 6-8 - SDGS -
weeks
Glandular fever screen - - - - - See I.M screen H -
Glanzmann Thrombasthaemia Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Glioma PETS 2x2m - - - 14 - SDGS -
and 2x4m days
sections on
slides
Gliadin antibodies Blood Venous/ S Gel 2 ml - - CC NGH
capilary
Globulin - - - - - See Immunoglobulins CC NGH
Glucagon Blood Venous EDTA 1ml - Send on ice CC SAS
immediately centre
Glucose Blood Venous / Fluoride/Li 0.5ml 4h Li Hep acceptable CC -
capillary Hep only if <60 mins old
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 138 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Glucose (blood gas analyser) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous / Rapidlyte syr. syr. heparinised (CC)
Capillary balanced containers. Keep
heparin 0.10mL ≤10min well mixed right up
syringe (3ml) cap. cap. until analysis. Mix
/capillary thoroughly by
withclosing rotation.
caps.
Glucose CSF - Fluoride hep 0.1ml 4h - CC -
Glucose Urine 24 hr Plain bottle 4h 10 ml aliquot CC -
Glucose-6-phosphate dehydrogenase Blood Venous / EDTA 1.0ml Discus Screen performed at H -
(G6PD) capillary s SCH. Assay
performed if screen is
abnormal and is
referred to Haem
RHH
Glucose Transporter 1 (GLUT1) deficiency Blood Venous EDTA 0.5-5ml 2-8 SDGS -
syndrome (SLC2A1 sequencing and MLPA) weeks
Glutaric acid Amniotic Fluid - Plain 10ml 2 Contact lab prior to CCM -
universal weeks amniocentesis
Glutaric AciduriaType 1 (GA1) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Glutaric Aciduria Type 1 Fibroblasts - - - 6-8 - CCM -
weeks
Glutathione peroxidase - - - - - See selenium CC GRI
Glycated haemaglobin - - - - - See HbA1c - -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 139 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Glyceric Acid chirality (D or L) Urine Random Plain 5ml 4-6 - CCM -
universal weeks
Glycine Blood Venous Li Hep 0.5ml 1 week - CCM -
plasma
Glycine CSF - Plain tube 0.2ml 1 week Must be paired with a CCM -
plasma sample
Glycogen Storage Disease Next Generation Blood Venous EDTA 0.5-5ml 8 - SDGS -
Sequencing Panels: Liver, Muscle, Heart, weeks
Generalised Panel
Glycogen Storage Disease Type 0 (GYS2 – Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
liver, GYS1-muscle) weeks
Glycogen Storage Disease Type 1a (von Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Gierke disease) (G6PC) weeks
Glycogen Storage Disease Type 1 non-a Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(SLC37A4) weeks
Glycogen Storage Disease Type II (Pompe Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
disease) (GAA) weeks
Glycogen Storage Disease Type III (AGL) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Glycogen Storage Disease Type IV Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(Andersen disease) (GBE1) weeks
Glycogen Storage Disease Type V (McArdle Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
disease) (PYGM) weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 140 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Glycogen Storage Disease Type VI (Hers Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Disease)(PYGL) weeks
Glycogen Storage Disease Type VII (Tarui Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
disease)(PFKM) weeks
Glycogen Storage Disease Type IX (X- Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
linked) (PHKA2-liver, PHKA1-muscle) weeks
Glycogen Storage Disease Type IX Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(autosomal) (PHKB, PHKG2) weeks
Glycogen Storage Disease Type X Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(PGAM2) weeks
Glycogen Storage Disorder Enzymes Blood Venous Li Hep whole 5ml - Please contact the CCM -
blood duty biochemist prior
to collection
Glycosaminoglycans Urine Random / Plain 10ml 4-6 Do not use Z10 CCM -
24 hrs universal weeks containers for Clinical
Chemistry Urine
samples.
Gonadotrophins - - - - - See FSH and LH CC -
Group Blood - - - - See Blood group & H -
crossmatch
Group and save Blood - - - - See Blood group & H -
crossmatch
Growth hormone Blood Venous Li Hep 2ml - - CC RHH
plasma
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 141 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Growth hormone antibodies Blood Venous S. Gel / Li 5ml - - CC NGH
Hep
Gut hormone profile Blood Venous EDTA 10ml 3 Transport on ice CC SAS
weeks centre
Haemochromatosis Blood Venous EDTA 0.5-5ml 4 - SDGS -
weeks
Haemoglobin Blood - - - - See FBC H -
Haematinic Assay Blood Venous / S. Gel 1ml 5 days - CC -
capillary
Haemoglobin (total, tHb; g/L) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
- blood gas analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Haemoglobin (total, tHb; g/L) Blood Capillary Heparinised 0.10mL ≤10min Add capillary closing POCT -
- blood gas analyser capillary caps. Mix thoroughly (CC)
by rotation.
Haemoglobin studies Blood Venous / EDTA 2ml 10 Hb HPLC and HbA2 H -
capillary days fraction identification
, F, S quantitation
Haemolysis tests Blood Venous EDTA Discuss 10 Discuss with H -
days consultant
haematologist to
determine choice of
tests.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 142 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Haemophilia A/Factor VIII deficiency Blood Venous EDTA 0.5-5ml2-8 SDGS -
molecular test weeks
Haemophilia A/Factor VIII deficiency - Next Blood venous EDTA 0.5-5ml 8 - SDGS -
Generation Sequencing Panel weeks
Haemophilia B/Factor IX deficiency Blood Venous EDTA 0.5-5ml 2-8 SDGS -
molecular test weeks
Haemophilia C/ Factor XI Deficiency Blood Venous EDTA 0.5-5ml 2-8 SDGS -
molecular test weeks
Haemosiderin Bone marrow Bone Discuss with Discuss 3 days Discuss with H -
marrow lab consultant
aspirate haematologist.
Haemosiderin Urine Urine Plain 10ml 3 days Discuss with H -
consultant
haematologist
Haptoglobin Blood Venous Plain / S. Gel 2ml 10 Discuss with H RHH
days consultant
haematologist
HbA1C Blood Venous / EDTA 0.5ml 4h - CC -
capillary
HDL cholesterol Blood Venous S. Gel 1ml 4h - CC -
Helicobacter pylori faecal antigen test Faeces
Heparin control Blood Venous Citrate 1.0ml Discus See also anti- H -
s Xa/APTT ration.
Contact Haem
Consultant.
Hepatitis B PCR Blood Venous S. Gel/EDTA 2ml - Label as “high risk” CC NGH
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 143 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Hepatitis C PCR Blood Venous S. Gel/EDTA 2 x 2ml - Label as “high risk” CC NGH
Hepatitis B or C serology Blood Venous S. Gel 2ml - Ask for Hep B s Ag, CC NGH
CoreAb and SAb.
Label as “high risk”
Her2 Paraffin - - - 1-2 Contact lab prior to SDGS -
embedded weeks referral
tissue biopsy
Hereditary Ataxia and Migraine Next Blood Venous EDTA 0.5-5ml 16 - SDGS -
Generation Sequencing Panel weeks
Hereditary Breast and Ovarian Cancer Blood Venous EDTA 0.5-5ml 8 Performed by Next SDGS -
(BRCA1 & BRCA2) weeks Generation
full Sequencing & MLPA
screen
2
weeks
predicti
ve
Hereditary Breast and Ovarian Cancer Blood Venous EDTA 0.5-5ml 12 - SDGS -
Extended Gene Panel weeks
Hereditary Leiomyomatosis with renal cell Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
carcinoma (HLRCC/MCUL) (FH sequencing weeks
and MLPA)
Hereditary Non Polyposis Colorectal Cancer Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(HNPCC) weeks
Hereditary Non Polyposis Colorectal Cancer Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(HNPCC) Gene Panel (including MLPA) weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 144 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Hereditary Non Polyposis Colorectal Cancer Blood and Venous EDTA 0.5-5ml 8 - SDGS -
(HNPCC) Tumour Microsatellite Instability PETS 8X10um weeks
Analysis (MSI) sections in
universal
Hereditary Spastic Paraparesis (dominant, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
pure) SPAST gene weeks
Hereditary Spastic Paraparesis (dominant, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
pure) ATL1 gene weeks
Hereditary Spastic Paraparesis (dominant, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
pure) REEP1 gene weeks
Hereditary Spastic Paraparesis (HSP) Next Blood Venous EDTA 0.5-5ml 16 - SDGS -
Generation Sequencing Panel weeks
Hereditary spherocytosis – See Haemolysis
- - - - - - - -
tests
Hexanoylglycine Amniotic Fluid - Plain 5ml ASAP Prenatal diagnosis of CCM -
universal MCADD. Metabolic
lab MUST be
contacted
Hexanoylglycine Urine Random Plain 2ml 4weeks Do not use Z10 CCM -
universal containers for Clinical
Chemistry Urine
samples.
5 HIAA Urine 24 hr 10ml 10% 10ml - 5 hydroyxindole CC NGH
H2SO4 acetic acid
High density lipoprotein (HDL) - - - - - See HDL cholesterol CC -
High Sensitivity Troponin T Blood Venous S. Gel 0.5ml - - CC RHH
/capillary
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 145 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Histamine - - - - - Contact Immunology CC NGH
ext 15552
Histopathology acetylcholinesterase Unfixed rectal Keep Moist See Histo - See By prior HP -
Rectal biopsy biopsy See Histo section for Histo arrangement, must
section for further details section include phone
further number for report,
details must indicate
urgency, for same
day result the sample
must be received
before 1.30pm
Histopathology fixed samples Formalin fixed - See Histo - See Use formalin safety HP -
section for Histo specimen bag
further details section
Histopathology inter-operative frozen Unfixed Keep Moist See Histo - See By prior HP -
section See Histo section for Histo arrangement, must
section for further details section include phone
further number for report
details
Histopathology liver biopsy Unfixed Keep Moist See Histo - See Indicate if dry copper HP -
if small section for Histo estimation is required
sample. further details section
See Histo
section for
further
details
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 146 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Histopathology Lymph node or tumour Unfixed Keep Moist See Histo - See By prior arrangement HP -
if small section for Histo
sample. further details section
See Histo
section for
further
details
Histopathology needle muscle biopsy Unfixed Keep See Histo - See By prior arrangement HP -
Moist. See section for Histo
Histo further details section
section for
further
details
Histopathology needle or trucut ? tumour Unfixed needle In Hams See - See By prior arrangement HP -
biopsy F10, from Histopath Histo
Histopath section for section
lab further details
Histopathology open muscle biopsy Unfixed Keep See - See By prior arrangement HP -
Moist. See Histopath Histo
Histo section for section
section for further details
further
details
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 147 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
HIV DNA Blood Venous EDTA 2ml - Test used to monitor CC NGH
infants born to
infected mothers.
Plasma must be
separated within 6
hrs.
Label as “high risk”
HIV Viral load (RNA) Blood Venous EDTA 2ml - Test used to monitor CC NGH
infected patients.
Plasma must be
separated within 6
hrs.
Label as “high risk”
HLA / tissue typing Blood Venous EDTA 2.5ml. If 10 Dedicated form H NHSBT
leuco- days required - obtain from
penic blood bank lab
then 5ml
HLA antibody/platelet antibody Blood Venous EDTA + plain 5ml 10 Dedicated form H NHSBT
EDTA + days required - obtain from
2ml plain blood bank lab.
Discuss with
consultant
haematologist
HMMA Urine - - - - See VMA CCM -
Homocysteine Blood Venous Li Hep or 2ml 2 Must be separated CCM -
fasting EDTA weeks within 30 mins
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 148 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Homocysteine (free) Urine Random / Plain 5ml 7 - 10 Please note Plasma CCM -
24 hrs universal days is preferred sample
for total
homocysteine
Homovanillic acid Urine - - - - See HVA CCM -
Human chorionic gonadotrophin Blood Venous S. Gel/ Li 3 ml - S. Gel preferred CC RHH
Hep
Huntington disease Blood Venous EDTA 0.5-5ml 2 - SDGS -
weeks
HVA Urine Random / 24 hr 10ml 1 week - CCM -
24 hrs collected into
10 ml HCL
Hydrogen ion concentration (H+) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
– blood gas analyser, see also pH Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation
Hydrogen ion concentration (H+) Blood Capillary Heparinised 0.10mL ≤10min Add capillary closing POCT -
– blood gas analyser, see also pH capillary caps. Mix thoroughly (CC)
by rotation.
3-Hydroxy Butyrate Blood - - - - See Intermediary CCM -
metabolites
2-Hydroxy Glutaric Acid Chirality (D or L) Urine Random Plain 5ml 4 - CCM -
universal weeks
17 α Hydroxyprogesterone Blood Venous Li Hep 1ml - - CC RHH
plasma/S Gel
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 149 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
1,25 Hydroxyvitamin D Blood Venous S. Gel 3ml 3 Protect from light CC -
weeks
25 Hydroxyvitamin D Blood Venous S. Gel serum 3ml 3 Protect from light CC -
weeks
Hypochromic red cells Blood Venous / EDTA Within 1 day - H -
capillary FBC
Hypophosphatasia (ALPL) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
IgG subclasses Blood Venous S. Gel 2ml - Responses to CC NGH
vaccinations are a
more useful initial
test of immune
fraction than IgG
subclasses.
IGF-1 Blood Venous S. Gel 1ml - - CC RHH
IGF-BP3 Blood Venous S. Gel 1ml - - CC SAS
centre,
Guildford
Immunoglobulins (IgG, IgA, IgM, IgE) Blood Venous S. Gel 1ml - - CC NGH
Infectious mononucleosis (I.M.) screen Blood Venous / EDTA 0.5ml 1 day Can perform along H -
capillary with FBC with 1ml
total
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 150 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
INR Blood Venous / Citrate 1ml 1day See coagulation H -
capillary screen. Restrictions
apply If capillary.
Dedicated tube for
capillary collection
obtained from
Haematology
Inhibin Blood Venous/ S Gel 1ml - - CC NGH
capillary
Insulin Blood Venous Li Hep 5ml - Additional 2ml CC RHH
plasma fluoride for
intermediate
metabolites
Insulin antibodies Blood Venous S. Gel 2ml - - CC NGH
Interferon CSF - Sterile - - Freeze within 2hrs of CC France
universal collection.
Please contact the
Duty Biochemist
Intermediary Metabolites Blood Venous or Fluoride 2ml 1-5 Includes Glucose, CCM -
capillary plasma days Lactate, 3-Hydroxy
Butyrate and Free
fatty acids
Intracellular Magnesium Blood Venous Lith hep 2ml - - CC RHH
Whole blood 0.5ml
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 151 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Iodine Urine Random Universal - - - CC SGH
Iron Blood Venous/ Li Hep 0.5ml 4h Suspected overdose CC -
capillary plasma measure at 4h
Islet cell antibodies Blood Venous S. Gel 2ml - - CC NGH
Isoelectric focusing of Transferrin Blood Venous/ S Gel 1ml - - CC NEURO
capillary
Isohaemagglutinins (anti A, anti B, IgM) Blood Venous S. Gel or 1ml 24h Ask for quantitative H -
EDTA titres. Needs blood
bank form filled
appropriately
JAK2 (V617F mutation) Blood/Bone Venous EDTA 0.5-5ml 2 - SDGS -
marrow weeks
JAK2 Exon 12 mutation screen Blood/Bone Venous EDTA 0.5-5ml 2 - SDGS -
(polycythaemia rubra vera/PRV) marrow weeks
Kallmann syndrome Blood Venous Li Hep 2-3ml 28 - SDGS -
days
Karyotype
- - - - - See Chromosome SDGS -
KIT-D816V Blood/Bone Venous EDTA 0.5-5ml 2 - SDGS -
marrow weeks
KRAS ( v-Ki-ras2 Kirsten rat sarcoma viral Paraffin Biopsy - - 1-2 - SDGS -
oncogene homolog) for CRC and NSCLC embedded weeks
and other tissue biopsy
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 152 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Lactate Blood Venous or Fluoride 0.5ml 4h Fasting if not part of CC -
capillary plasma Hypoglycaemia
screen
Lactate (blood gas analyser) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous / Rapidlyte syr. syr. heparinised (CC)
Capillary balanced containers. Keep
heparin 0.10mL ≤10min well mixed right up
syringe (3ml) cap. cap. until analysis. Mix
or capillary thoroughly by
with closing rotation.
caps.
Lactate CSF - Fluoride tube 0.2ml 4 days - CCM -
Lactate dehydrogenase LDH Blood Venous / Li Hep 0.5ml 4h - CC -
capillary plasma
Lactose tolerance test Blood - - - - Bleep duty CC -
biochemist 095
Lamotrigine Blood Venous/ Lith Hep/ 1ml CC NGH
capillary S Gel - -
Latex fixation test Blood Venous S Gel 3 ml CC NGH
- -
Laxative screen Urine Random Plain 10ml - - CC NGH
universal
Lead Blood Venous Li Hep / 1ml - - CC NGH
EDTA whole
blood
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 153 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Leber Hereditary Optic Neuropathy (LHON) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Leucine Proline-Enriched Proteoglycan Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(LEPRE1) (autosomal recessive OI) weeks
Leucocyte enzyme - - - - - See white cell CC -
enzyme
Leukaemia cytochemistry - - - - - See bone marrow H -
Levetiracetam (Keppra) Blood Venous/ Li Hep/ 1ml - - CC CCFE
capillary S Gel
Li Fraumeni (TP53 gene sequencing and Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
MLPA) weeks
Lipase Blood Venous/ Lith Hep/ S 0.5ml 1-2 - CC
Capillary Gel weeks
Lipids Blood Venous / Li Hep / S. 0.5ml 4h See cholesterol, HDL CC -
capillary Gel and triglyceride
Lipoprotein (a) Lp (a) Blood Venous / Li Hep 1m - - CC GEOR
capillary
Lithium Blood Venous S Gel 3ml - - CC RHH
Liver function tests LFT Blood Venous / Li Hep 0.5ml 4h See bilirubin, ALP, CC -
capillary ALT, GGT, total
protein albumin
LLMI BAL Bronchial Sterile >2mls 5 days Macrophage lipid HP -
aspirate universal content analysis
Long Chain 3- Hydroxyacyl-CoA - Blood or Venous EDTA 0.5-5ml 2 Common mutation SDGS -
Dehydrogenase Deficiency (LCHAD) Guthrie spots weeks only
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 154 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Long Chain Fatty Acids Blood - - - - See Very Long Chain CCM -
Fatty Acids
Lupus inhibitor / anticoagulant Blood Venous Citrate 1ml 1 Week See coagulation H -
studies
Luteinising hormone LH Blood Venous Li Hep 2ml - - CC RHH
plasma / S.
Gel
Lymphocyte subsets Blood Venous EDTA 1ml 5 days. Not for first line H -
investigation.
Requires approval
from Immunology
consultant before
requesting assay.
Lysosomal Enzymes Blood Venous EDTA whole 5ml - Please contact the CCM MCH
blood duty biochemist
Macroglobulins Blood Venous S Gel 4ml - - CC NGH
Magnesium Blood Venous / Li Hep 0.5ml 4h Avoid haemolysis CC -
capillary plasma
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 155 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Malarial parasites (blood film/ Malaria Blood Venous / EDTA 1ml Discus Can perform along H LSTM
Rapyd Test (MRT)) capillary s with FBC.
Three negative
diagnostic samples
over a period of 24-
48 hours are
necessary to exclude
malaria. These
repeat tests should
include blood films
and MRT. It is
recommended these
further samples are
taken 24 hours and
48 hours post initial
presentation. Please
include details of
recent travel history
on the request form.
Please note that the
MRT method is not
validated for the
detection of P
knowlesi.
Malt lymphoma PETS 2x2m - - - 14 - SDGS -
and 2x4m days
sections on
slides
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 156 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Manganese Blood Capillary EDTA 0.5ml - Bleep duty CC SAS
only biochemist prior to centre,
collection 095 Guildford
Mannan binding protein Blood Venous S. Gel 1ml - - CC NGH
Mantle cell lymphoma PETS 2x2m - - - 14 - SDGS -
and 2x4m days
sections on
slides
Medium Chain Acyl CoA-dehydrogenase Blood or Venous EDTA 0.5-5ml 2-8 - SDGS -
Deficiency Guthrie spots weeks
Meningococcal PCR Blood Venous EDTA 0.5ml - Take as early as CC NGH
possible after
presentation
Mercury Blood Venous/ EDTA 1ml - Early morning Urine CC SAS
Urine Capillary 10ml min centre
Metanephrine (Metadrenaline) Blood Venous EDTA 3ml 3-4 Send on ice CC SRH
weeks immediately.
Methaemoglobin (MetHb; reported as %Hb) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
– blood gas analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Methaemoglobin (MetHb; reported as %Hb) Blood Capillary Heparinised 0.10mL ≤10min Add capillary closing POCT -
– blood gas analyser capillary caps. Mix thoroughly (CC)
by rotation.
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 157 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Methotrexate Blood Venous/ Li Hep 0.75ml <12hrs Send first sample CC -
capillary plasma 48hr post dose
Methylmalonic Acid Amniotic Fluid - Plain 5ml Discus Prenatal diagnosis of CCM -
universal s Methylmalonic
Acidaemia.
Metabolic lab MUST
be contacted
Methylmalonic Acid Urine Random Plain 5ml 2 Do not use Z10 CCM -
universal weeks containers for Clinical
Chemistry Urine
samples.
Microarray Skin Biopsy Sterile Culture 1-2mm 28 - SDGS -
tissue medium pots cubed days
Microarray Fetal Loss Placental - Sterile tissue <1cm 28 - SDGS -
biopsy at cord culture cubed days
insertion site, medium pot
fetal
membrane,
villi, cord
biopsy & skin
biopsy
Microsatellite Instability Analysis (MSI) Blood and Venous EDTA 0.5-5ml 8 - SDGS -
Paraffin weeks
embedded
tissue biopsy
Microarray (see CGH) - - - - - - - -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 158 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Mitochondrial Disorder, Leber Hereditary Blood Venous EDTA 0.5-5ml 2-8 Please contact lab to SDGS -
Optic Neuropathy, MELAS, MERRF, NARP. weeks discuss sample type
Mitochondrial DNA Blood - - - - See SDGS section CC -
Monospot - - - - - See I.M screen H -
MPL Exon 10 mutation screen (?PMF and Blood/Bone Venous EDTA 0.5-5ml 2-8 - SDGS -
?ET) Marrow weeks
MTHFR (Methylene Tetra Hydra Folate Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Reductase deficiency) weeks
Mucopolysaccharides Urine Random Plain 5ml 4 Do not use Z10 CCM -
universal weeks containers for Clinical
Chemistry Urine
samples.
Multiple Endocrine Neoplasia Type 1 Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(MEN1 gene sequencing & MLPA) weeks
Multiple Endocrine Neoplasia Type 2 Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(MEN2) and Hirschsprung disease (RET weeks
gene)
Muscle Biopsy - - - - - Metabolic lab MUST CCM -
be contacted to
arrange ext 17445
Muscle Biopsy for Histopathology Fresh - See - See Histopath lab MUST HP -
Histopath Histo be contacted to
section for section arrange
further details
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 159 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Muscle enzymes Blood Venous or Li Hep 0.5ml 4h See CK, LDH, AST CC -
capillary plasma
MutYH-associated polyposis (MAP) Blood Venous EDTA 0.5-5ml 2-4 - SDGS -
(MUTYH gene) UK common mutation weeks
screen/carrier testing
Mycophenolate Blood Venous/ Li hep 0.5ml - Separate quickly CC RBH
capillary EDTA
Myelin basic Protein CSF - - 0.2ml - Freeze immediately CC CHURC
H
Myelodysplastic syndromes (MDS) Bone marrow - Universal 0.25-1ml 28 - SDGS -
with 5-10ml days
of transport
medium
Myeloperoxidase (cytochemical qualitative) Blood Venous/ca EDTA 0.5ml Discus Can perform along H -
pillary s with FBC depending
upon clinical setting
Myeloproliferative disease (MPD) Bone marrow - Universal 0.25-1ml 28 - SDGS -
with 5-10ml days
of transport
medium
Myeloproliferative disorder/essential Blood / Bone - EDTA 0.5-5ml 2 - SDGS -
thrombocythaemia(ET)/polycythaemia marrow weeks
rurbra vera (PRV)/ myelofibrosis (MF) -
JAK2
MYH9-related disorders (GATA2, SBDS, Blood Venous EDTA 0.5-5ml 8 - SDGS -
RUNX1) weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 160 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
MutYH Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Myoadenylate Deaminase deficiency Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(AMPD1) weeks
Myoglobin Blood Venous S. Gel 2ml - - CC NGH
Myoglobin Urine Random Plain 10ml - Preferred CC NGH
universal
N acetylaminoglucoaminidase Urine Fresh Universal 2ml - Store frozen CC CHILD
Random
Neonatal Alloimmune Thrombocytopenia Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(NAIT) weeks
Neuroblastoma PETS 2x2m - - - 14 - SDGS -
and 2x4m days
sections on
slides
Neuroblastoma Biopsy & resection Fresh - See Histo - See - HP -
section for Histo
further details section
Neurone Specific Enolase Blood Venous S. Gel 2-3ml - - CC NGH
Neurotransmitters CSF - Special - - Metabolic lab MUST CCM -
requirements be contacted to
arrange
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 161 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Neutrophil adhesion molecules Blood Venous EDTA 1ml - By arrangement with H NRVI
Imm lab Newcastle
only
Noradrenaline Blood Venous Li Hep 2ml 2-4 Send on ice CC RBH
plasma weeks immediately
Noradrenaline Urine 24 hr Bottle +10ml 20ml - - CC NGH
H2SO4
Normetanephrine (Nor-adrenaline) Blood Venous EDTA 1ml 3-4 Send on ice CC SRH
weeks immediately.
Oestradiol Blood Venous Li Hep 2ml CC RHH
plasma - -
Oestrogen Urine 24hr Plain bottle / 10 ml CC MCH/JA
few drops of - - MES
chloroform
Oligosaccharides Urine - Random 10ml - - CC WILL
Oligoclonal bands CSF - 0.5ml CC NGH
Blood S Gel 5ml - -
Organic Acids Urine Random / Plain 10ml 2 Not Boric Acid. Do CCM -
24 hrs universal weeks not use Z10
containers for Clinical
Chemistry Urine
samples.
Orosomucoid - - - - - See Acid CC NGH
Glycoprotein
Orotic Acid Urine Random / Plain 10ml 2 - CCM -
24 hrs universal weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 162 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Osmolality Blood Venous/ Li Hep 0.5ml 4h - CC -
capillary plasma
Osmolality Urine Random Plain 1ml 4h - CC -
urine universal
Osteocalcin Blood Venous EDTA 5ml - Bleep duty CC RHH
biochemist prior to
collection 095
Osteogenesis Imperfecta Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Osteogenesis Imperfecta – autosomal Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
dominant Next generation Sequencing weeks
Panel
Osteogenesis Imperfecta – autosomal Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
recessive (CRTAP, LEPRE1, PPIB) weeks
Osteogenesis Imperfecta – autosomal Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
recessive Next generation Sequencing weeks
Panel
Osteogenesis Imperfecta Type V (IFITM5) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Osteoporosis and osteoporosis Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
pseudoglioma syndrome (LRP5) weeks
Oxalate Urine Random Bottle+10ml 25ml - CARE -store at room CC BCH
urine HCL temp
Oxcarbazepine and 10 hydroxycarbazepine Blood Venous Li hep/ 0.2ml - - CC CCFE
S Gel min
5-Oxoproline Amniotic Fluid - - - - See Pyroglutamic CCM -
acid
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 163 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Oxygen saturation (sO2 ; reported as %) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
– blood gas analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Oxygen saturation (sO2 ; reported as %) Blood Capillary Heparinised 0.10mL ≤10min Add capillary closing POCT -
– blood gas analyser capillary caps. Mix thoroughly (CC)
by rotation.
Oxyhaemoglobin (O2Hb ; reported as %Hb) Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
– blood gas analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
Oxyhaemoglobin (O2Hb ; reported as %Hb) Blood Capillary Heparinised 0.10mL ≤10min Add capillary closing POCT -
– blood gas analyser capillary caps. Mix thoroughly (CC)
by rotation.
Pancreatic polypeptide Blood Venous EDTA 1ml - ON ICE CC SAS
SEP WITHIN centre
15MINS
Paracetamol Blood Venous / Li Hep 0.5ml 4h Overdose; sample CC -
capillary plasma taken not less than
4h post OD.
If IV overdose is
suspected contact
the duty biochemist
(bleep 095)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 164 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Paraquat Blood Venous Li Hep 10ml - Contact Clin Chem CC NGH
plasma RHH before
collection
Parathyroid hormone PTH Blood Venous EDTA 1ml - Paired 0.5ml Li hep CC -
sample for bone
profile. Analysed
Tue and Thurs,
urgent requests only
at other times.
Parkinsonism next generation sequencing - - - - - - SDGS -
panel (Please see Dystonia and
Parkinsonism next generation sequencing
panel)
pCO2 / pO2 / pH Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Blood gas analyser Venous Rapidlyte heparinised (CC)
balanced Plastipaks.
heparin Don’t let sediment.
syringe (3ml) Mix thoroughly by
rotation.
pCO2 / pO2 / pH Blood Capillary Heparinised 0.10mL ≤10min Add capillary closing POCT -
Blood gas analyser capillary caps. Mix thoroughly (CC)
by rotation.
Peroxisomal Biogenesis Disorders (PEX1, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
PEX6, PEX10, PEX12, PEX26) weeks
pH Blood - - - - See pCO2 POCT -
(CC)
pH Urine Random Plain 10ml 1 day - CC -
universal
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 165 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
PHA response (or other mitogen responses - - - - - Contact G Wild ext CC NGH
e.g. candida, tetanus, PPD) 15394
Phenobarbitone (Phenobarbital) Blood Venous / Li Hep 0.5ml - - CC RHH
capillary plasma
Phenylalanine Blood Venous or Li Hep 0.5ml 1 week - CCM -
capillary plasma
(serum OK)
Phenylalanine Blood Spots Venous or Guthrie Card Two 1 week - CCM -
capillary (Li Hep - spots
whole blood)
Phenytoin Blood Venous / Li Hep 0.5 ml - - CC RHH
capillary plasma
Phosphate Blood Venous / Li Hep 0.5ml 4h Avoid haemolysis CC -
capillary plasma
Phosphate Urine 24hr / Plain bottle/ 10ml 4h - CC -
random universal
Phosphate excretion indices Blood+urine - - - - PEI,TRP,TmP/GFR CC -
Phosphoethanolamine Urine Random Plain 10ml 2 - CCM -
universal weeks
Phosphoglycerate Mutase (muscle, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
deficiency of) weeks
Phytanate Blood - - - - See Very Long Chain CCM -
Fatty Acids
Phytosterols Blood Venous Li Hep 1ml 4 - CCM -
plasma weeks
(serum OK)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 166 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
PIK3CA (Phosphatidylinositol 3 – kinase, PETS 8x10μ - - - 1-2 - SDGS -
catalytic, alpha polypeptide) sections in weeks
universal
Pipecolic Acid Blood Venous Li Hep 1ml 4 - CCM -
plasma weeks
Pipecolic Acid CSF - Plain tube 0.5ml 4 - CCM -
weeks
Pipecolic Acid Urine Random Plain 5ml 4 - CCM -
universal weeks
PLAP Placental ALP Blood - - - - - CC NGH
CSF
Plasmalogens Blood Venous EDTA 2ml 4 Washed packed red CCM -
weeks cells
Platelet antibody - - - - - See HLA H -
Platelet count - - - - - See FBC H -
Platelet function - - - - - See coagulation H -
studies. Discuss with
consultant
haematologist
Platelet specific typing Blood Venous EDTA 2.5ml. If 14 Dedicated form H NHSBT
thromb- days required - obtain from
ocyto- blood bank lab.
penic - Discuss with
5ml consultant
haematologist
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 167 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
PNP See Adenosine
Deaminase (ADA)
pO2 Blood - - - - See pCO2 POCT -
(CC)
Polycystic Kidney Disease (autosomal Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
dominant) PKD1 & PKD2 Full-gene weeks
sequencing and MLPA
Polycystic Liver Disease (autosomal Blood Venous EDTA 1-5ml 2-8 - SDGS -
dominant) PRKCSH & SEC63 gene weeks
sequencing
Porphobilinogen screen Urine 24hr/ Plain - - Protect from light CC RHH
random bottle/univers
al
Porphyrin screen Urine Random Plain 10ml - Protect from light CC RHH
universal Contact Duty
Biochemist. EDTA
blood and faeces
samples may also be
appropriate
depending on the
symptoms
Potassium Blood Venous / Li Hep 0.5ml 4h Avoid haemolysis. CC -
capillary plasma Use venous blood to
check result
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 168 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Potassium – blood gas analyser Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous / Rapidlyte syr. syr. heparinised (CC)
Capillary balanced containers. Mix
heparin 0.10mL ≤10min thoroughly by
syringe (3ml) cap. cap. rotation.
or capillary
with closing
caps.
Potassium Urine 24hr / Plain bottle/ 10ml 4h - CC -
random universal
PPIB (autosomal recessive OI) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Prednisolone Blood Venous S Gel 1 ml - Contact lab before CC RBH
sending sample
2-3 hrs POST dose
Pregnanetriol Urine 24hr Plain bottle 10ml - Serum/plasma CC RHH
hydroxyprogest’one
preferred for
management of 21
hydroxylase
deficiency
Pristanate Blood - - - - See Very Long chain CCM -
Fatty Acids
Prolactin Blood Venous Li Hep 2ml - - CC RHH
plasma
Protein CSF - Plain tube 0.5ml 4h - CC -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 169 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Protein Urine 24hr/ Plain bottle / 2ml 4h - CC -
random universal
Protein , Total Blood Venous/ Li Hep 0.5ml 4h - CC -
capillary plasma
Protein /creatinine ratio Urine 24hr/ Plain bottle / 2ml 4h - CC -
random universal
Protein C and S - - - - - See coagulation H -
studies. Discuss with
consultant
haematologist
Protein C Deficiency Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Protein S Deficiency Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Protein selectivity Blood Venous S. Gel 4ml - - CC NGH
Protein selectivity Urine 4hr urine Plain - - CC NGH
universal
Prothrombin (3' non 20210G>A prothrombin Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
variants) weeks
Protoporphyrin (erythrocyte) - - - - - See ZPP H -
Pseudoxanthoma Elasticum Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Pseudocholinesterase (scholine sensitivity) - - - - - See Cholinesterase - -
Purines and Pyrimidines Urine Random / Plain 10ml Send Please contact the CCM GUY
24 hrs universal away duty biochemist
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 170 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Pyroglutamic acid Amniotic Fluid - Plain 10ml 2 Contact the lab prior CCM -
universal weeks to amniocentesis
Pyruvate Blood Venous - - Contact the lab for CC NRVI
special tubes ext
17445
Pyruvate CSF - - - Contact the lab for CC NRVI
special tubes ext
17445
Pyruvate carboxylase Fibroblasts - Culture 1-2mm 2 Refer to Skin CCM -
medium months Biopsies
Quantiferon (Gamma interferon for TB) Blood Venous/ Li Hep 3 ml total - Contact CC NGH
capillary plasma Microbiologist (SCH)
for special tubes ext
17579/53158
Quinine Blood Venous S Gel 5ml - - CC NGH
Quantitative BCR-ABL (MRD) Blood/Bone - EDTA 0.5-5ml 2 Must be sent to the SDGS -
marrow weeks laboratory
immediately
RAST (radio allergo-sorbent test for specific Blood Venous S. Gel 5ml - - CC NGH
IgE)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 171 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Rectal biopsy for acetylcholinesterase Unfixed rectal Moist See Histo - See By prior HP -
biopsy section for Histo arrangement, must
further details section include phone
number for report,
must indicate
urgency, for same
day result the sample
must be received
before 1.30pm
Reducing Substances Faeces Random Plain - 4 days Fresh sample CCM -
universal
Reducing Substances Urine Random Plain 5ml 4 days Fresh sample CCM -
universal
Renin, and Aldosterone Blood Venous Li Hep 2ml - Bleep duty CC SAS
biochemist 095 prior centre,
to collection Leeds
Reticulin antibodies Blood Venous S Gel 4ml - - CC NGH
Reticulocyte count (retics) Blood Venous / - 0.5ml 1 day Can perform along H -
capillary with FBC
Retinoblastoma Blood Venous Li Hep 2-3ml 28 - SDGS -
days
Retinol, retinoids - - - - - See vitamin A CC RDGH
Rheumatoid factor Blood Venous S. Gel 2ml - - CC NGH
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 172 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
RSV (BinaxNOW card) Nasal NPA Plain 1ml 15-20 Store at room Lab staff -
Pharyngeal Universal mins temperature for up to will collect
Aspirate (NPA) 4 hours in designated samples at
transport box or fir up dedicated
to 24 hours at 2-8°C times
RSV (Rapid Test/PCR) Nasal NPA Plain 1ml 1 week Store at room Lab staff NGH
Pharyngeal universal temperature for up to will collect
Aspirate (NPA 4 hours in designated samples at
transport box or fir up dedicated
to 24 hours at 2-8°C times
RUNX1 Blood/Bone Venous EDTA 0.5-5ml 8 - SDGS -
Marrow weeks
Salicylate Blood Venous / Li Hep 0.75ml 4h 2hrs post dose CC -
capillary plasma therapeutic range
SBDS Blood/Bone Venous EDTA 0.5-5ml 8 - SDGS -
Marrow weeks
Selenium Blood Venous Li Hep 3ml - CC NGH
plasma or
serum (no
gel)
Serotonin Blood Venous EDTA +5mg 2ml - Frozen within 10 CC NAT
Ascorbic acid mins
Serotonin Tumour Marker Blood Venous EDTA +5mg 1ml - Frozen within 10 CC JAMES
Ascorbic acid mins
Serotype Specific Pneumococcus Serology Blood Venous S. Gel 1ml - By arrangement with CC NGH
Immunology lab only
Sex Hormone Binding Globule Blood Venous Li Hep 2ml - - CC RHH
plasma
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 173 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
SGOT (Aspartate aminotransferase) Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
SGPT (Alanine aminotransferase) Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Sickle cell disease Blood Venous EDTA 0.5-5ml 2 - SDGS -
weeks
Sickle cell disease (newborn screening – Dried blood Capillary - - 2 Referrals via SDGS -
transfused babies) spot weeks Newborn screening
only
Sickle Hb screen Blood Venous EDTA 1ml 1 day Can perform along H -
/capillary with FBC 1 ml total
and confirmed by
HPLC
Silver Urine - Random Few ml CC SAS
Blood urine or - - centre,
whole blood Guildford
Sirolimus Blood Venous/ EDTA 0.2ml CC UHSM
- -
capillary Whole blood
Sitosterols Blood - - - - See phytosterols CCM -
Skin Biopsy – tissue culture Skin - - - - Refer to Skin CCM -
Biopsies under
Clinical Chemistry
Skin – Immunology Fresh - - - - See Histo section for Send direct -
further details. to Imm
Contact Immunology NGH
NGH – ext 15552.
Sodium Blood Venous/ Li Hep 0.5ml 4h Also blood gas CC -
capillary plasma analyser
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 174 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Sodium – blood gas analyser Blood Arterial / Siemens 0.8mL ≤10min Do not use non- POCT -
Venous / Rapidlyte syr. syr. heparinised (CC)
Capillary balanced containers. Mix
heparin 0.10mL ≤10min thoroughly by
syringe (3ml) cap. cap. rotation.
or capillary
with closing
caps,
Sodium Urine 24hr Plain bottle/ 10ml 4h - CC -
random universal
Sorbitol Urine - - - - See Galactitol CCM -
Specific gravity Urine Random Plain 1ml 4h Request osmolality CC -
universal
Spinal Muscular Atrophy, 5q linked Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Spinobulbar Muscular Atrophy (Kennedy Blood Venous EDTA 0.5-5ml 2-6 - SDGS -
disease X linked) weeks
Spinocerebellar Ataxia types 1-3, 6, 7, 12 Blood Venous EDTA 0.5-5ml 2-6 - SDGS -
and 17 weeks
Steroid profile 24 hr Urine 24hr - - - Bleep duty CC -
biochemist 095
Sterols Blood Venous Li Hep 1ml 3 - CCM -
plasma weeks
Stones - - - - - See calculi CC -
Stickler syndrome sequencing panel Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 175 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Sugar Chromatography Urine Random Plain 10ml Send Please contact the CCM -
universal away duty biochemist
Sulphocysteine (this replaces the urine Urine Random Plain 5ml 3 For the diagnosis of CCM -
sulphite test) universal weeks sulphite oxidase or
molybdenum cofactor
deficiency. If strongly
suspected contact
the lab for urgent
analysis.
Sweat test (chloride) Sweat - - - - Arrange with lab CC -
SYNGAP-1 – associated intellectual Blood - EDTA 2-8 - SDGS -
diasability weeks
Synovial sarcoma PETS 2x4m - - - 14 - SDGS -
sections on days
slides
Tacrolimus (FK506) - - - - - See FK506 CC -
Testosterone Blood Venous Li Hep 2ml - - CC RHH
plasma
Thalium Blood Venous EDTA 10ml - - CC SAS
centre
Thalium Urine Random Sterile 30ml - - CC SAS
universal centre
Theophylline Blood Venous / Li Hep 0.5ml - - CC RHH
capillary plasma
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 176 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Thiopentone Blood Venous/ EDTA 1ml - Duty biochemist must CC LLAN
capillary be contacted prior to
sample collection
Thiopurine methyltransferase TPMT Blood Venous EDTA whole 2-5ml CC BCITYH
blood - -
TPMT metabolites (6-TGN + 6-MMPN) Blood Venous EDTA whole 2-5ml CC BCITYH
blood - -
Thrombophilia tests - - - - - See coagulation H RHH
studies. Discuss with
consultant
haematologist
Thyroid antibodies Blood Venous S. Gel 2ml CC NGH
- -
Thyroid binding globulin TBG Blood Venous S. Gel 2ml CC NGH
- -
Thyroid function tests TFT Blood Venous Li Hep 2ml 1-3 Includes TSH and CC -
plasma days fT4
Thyroid stimulating hormone TSH Blood Venous Li Hep 1ml 1-3 - CC -
plasma days
Thyroid stimulating hormone TSH Dried blood Dried blood Guthrie card - 1-5 Not offered as a CC
spot spot days separate test except
for TSH monitoring
and for needle-
phobic patients by
arrangement.
Tiagabine Blood Venous S Gel 2ml CC CCFE
- -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 177 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Tissue transglutamainse Blood Venous S. Gel 2ml CC NGH
- -
Tissue type - - - - - See HLA typing H -
Tobramycin Blood Venous/ S. Gel 1ml - - CC -
capillary
Topiramate Blood Venous / Li hep/ 1ml - - CC CCFE
Capillary S Gel
Total thyroxine T4 Blood Venous Li Hep 1ml - - CC RHH
plasma
Toxicology screen Blood Venous Li Hep 5ml - - CC NGH
plasma
Toxicology screen Urine Random Plain 10ml - - CC NGH
universal
TPMT Pyrosequencing Blood or Venous EDTA 0.5-5ml 4 - SDGS -
Buccal swabs weeks
TNF alpha Blood Venous/ S Gel 1ml - - CC PRU
capillary
Trace elements - - - - - See Cu, Zn, Se, Fe CC RHH
Transcobalamin II assay Blood Venous Plain 5ml Discus Discuss with H Discuss
universal s consultant
haematologist
Transferrin Blood Venous S. Gel 2ml - - CC NGH
Transferrin IEF Blood Venous S. Gel 2ml - - CC NAT
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 178 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Transfusion reaction - - - - - See detailed section. H -
Discuss with
consultant
haematologist
Transketolase Blood Venous EDTA 5ml - By arrangement only. CC RDGH
Store and send
frozen
Triglycerides Blood Venous / Li Hep 0.5ml 4h - CC -
capillary plasma
Trimethylamine Urine Random / 24 hr 10ml 6-8 - CCM -
24 hrs collected into weeks
10 ml 6M
HCL. pH<2
Trimethylaminuria /Fish Odour Syndrome Blood Venous EDTA 0.05-5ml 2-8 - SDGS -
(FMO3) weeks
Triodothyronine T3 - - - - - See free T3 CC -
Troponin (High Sensitivity Troponin T) Blood Venous S. Gel 0.5ml - - CC RHH
/capillary
Tryptase Blood Venous EDTA / S. 2ml - For allergy disorders CC NGH
Gel +mast cell
syndromes
Tumour markers - - - - - See Alpha feto CC NGH
protein + BHCG
Tyrosine hydroxylase deficient dopa- Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
responsive dystonia (Segawa) weeks
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 179 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
U/E Blood Venous Li Hep 0.5ml 4h See Na, K, Cl, CC -
/capillary plasma Bicarb, Urea,
Creatinine
UKALL2003/UKALLR3 MRD TRIALS Bone marrow - ACD 2.5-10ml Depen Peripheral blood in SDGS -
dant on ACD is acceptable at
time diagnosis if the WCC
point is > 20x10^9/l.
Research trials.
Uniparental disomy chromosome 7 / Russell Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Silver Syndrome weeks
Urea Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Urea Urine 24hr Plain bottle/ 10ml 4h - CC -
/random universal
Urea Cycle Disorders (OTC, CPS1, NAGS, Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
ASL, ASS, ARG) weeks
Uric acid Blood Venous Li Hep 0.5ml 4h - CC -
/capillary plasma
Uric acid Urine 24hr Plain bottle/ 10ml 4h - CC -
/random universal
Urinary electrolytes - - - - - See sodium, CC -
potassium
Urinary free cortisol Urine 24 hr plain Aliquot 10ml - - CC SAS
bottle centre,
Leeds
Urine Amylase/creatinine Urine Random Plain 1ml 4h Ratio CC -
urine universal µmmol/creatinine
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 180 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Urine Calcium/creatinine Urine Random Plain 1ml 4h Ratio CC -
urine universal µmmol/creatinine. On
second urine passed
during day
Urine copper Urine 24 hr plain Aliquot 10 ml - - CC NGH
bottle
Urine copper Wilson's disease Urine 24hr basal - - - - CC NGH
Urine copper Wilson's disease Urine 2nd 24hr - - - 2 12hrly doses of CC NGH
penicillamine given
Urine creatinine Urine 24 hr plain Aliquot 10ml 4h For creatinine CC -
bottle clearence Blood +
Complete Urine
collection. Include
child's weight &
height
Vaccination responses (Bacterial, Hib, Blood Venous S. Gel 2-4ml - - CC NGH
Pneumococcus, Tetanus,Men C)
Valproate (Valproic acid) Blood Venous Li Hep 1ml - - CC RHH
/capillary
Vancomycin Blood Venous S. Gel 1ml - - CC NGH
/capillary
Vanilyl Mandelic Acid (VMA) Urine - - - - See VMA CCM -
Very Long Chain Fatty Acids Blood Venous Li Hep 1ml 4 - CCM -
plasma weeks
(serum /
fluoride OK)
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 181 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
Very Long Chain Fatty Acids Fibroblasts - Culture - 2 Refer to skin biopsies CCM -
medium months
Very-long-chain-acyl-CoA dehydrogenase Blood or Venous EDTA 0.5-5ml 2-8 - SDGS -
(VLCAD) deficiency fibroblasts weeks
Viral serology (e.g. Polio, Measles, Mumps, Blood Venous S. Gel 3-5ml - Discuss with lab CC NGH
Rubella, Varicella)
Vitamin A Blood Venous Li Hep 3ml - Protect from light at CC RDGH
all times
Vitamin A and E Blood venous Li Hep 3ml - Protect from light at CC RDGH
all times
Vitamin B1 thiamine Blood Venous EDTA 5ml - Request CC RDGH
transketolase
Vitamin B12 - - - - - See Haematinic CC -
assay
Vitamin C Blood Contact lab prior to CC RDGH
- - - - collection
Vitamin D Blood Venous/Ca S. Gel/Li Hep 3ml - Protect from light at CC SAS
pillary all times centre
VKORC1 gene (Warfarin resistance) Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
VMA Urine 24hr Bottle+10ml - 5-14 A random urine CC -
HCL days sample may be
accepted if urgent but
discuss with Duty
Biochemist prior to
sending -
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 182 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
von Willebrand Disease type 1- 3r molecular Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
test weeks
von Willebrand Disease platelet type Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
(GP1BA gene) molecular test weeks
Warfarin resistance (VKORC1 gene) and Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
combined vitamin K clotting factor weeks
deficiency type 2
WBC white cell count - - - - - See FBC H -
White cell cystine Blood Venous Li Hep whole 3ml Send Please contact the CCM JAMES
blood away duty biochemist
White cell enzymes Blood Venous EDTA whole 5ml Send By arrangement with CCM -
blood away the duty biochemist
(bleep 095).
Accepted Monday-
Wednesday before
12:00. Add relevant
clinical details to
form.
Wilms Tumour, Frasier syndrome, Denys Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
Drash syndrome, (Wilms Tumour weeks
Suppressor) WT1 Gene sequencing and
MPLA
Wilson disease Blood Venous EDTA 0.5-5ml 2-8 - SDGS -
weeks
Zinc Blood Venous Li Hep 1ml - 2ml if copper CC NGH
plasma required
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 183 of 184
CAEC Registration Identifier: 1043 Sheffield Children’s (NHS) Foundation Trust
Laboratory Handbook
Specimen Collection Lab to Referred
Test Tube Volume TAT Notes/Comments
type type send to to
ZPP (Zinc protoporphyrin) Blood Venous EDTA 0.5ml 7 days Can perform along H -
/capillary with FBC if 1ml total
QPulse Document Reference: 999-0018 Approved by: Prof J R Bonham
Author: Laboratory Handbook Group Date of Issue: April 2019 Review date: March 2020
© SC(NHS)FT 2017. Page 184 of 184
Das könnte Ihnen auch gefallen
- 68th AACC Annual Scientific Meeting Abstract eBookVon Everand68th AACC Annual Scientific Meeting Abstract eBookNoch keine Bewertungen
- Standard Operator Clinical ChemistryDokument15 SeitenStandard Operator Clinical ChemistryLady Dia100% (2)
- Senior Medical Laboratory Technician: Passbooks Study GuideVon EverandSenior Medical Laboratory Technician: Passbooks Study GuideNoch keine Bewertungen
- Laboratory Turnaround TimeDokument17 SeitenLaboratory Turnaround TimeNicole HoNoch keine Bewertungen
- Laboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceVon EverandLaboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceBewertung: 5 von 5 Sternen5/5 (3)
- Mls Imls Reading ListDokument3 SeitenMls Imls Reading ListPeng KwanNoch keine Bewertungen
- Toxicology of Heavy MetalsDokument53 SeitenToxicology of Heavy Metalsfarkad rawiNoch keine Bewertungen
- Clinical Lab TechnqDokument67 SeitenClinical Lab TechnqRatnamala SarmaNoch keine Bewertungen
- Medical Lab Scientist Exam GuideDokument11 SeitenMedical Lab Scientist Exam GuideswasahmedNoch keine Bewertungen
- IFCC TF Ethics in Lab MedicineDokument16 SeitenIFCC TF Ethics in Lab MedicineDr.Deepanshu SinghalNoch keine Bewertungen
- Preanalytical ErrorsDokument99 SeitenPreanalytical ErrorsSulakshmi KurlekarNoch keine Bewertungen
- POCT and PT by Group6bsmt3bDokument15 SeitenPOCT and PT by Group6bsmt3bRuzzelle Mae ParasNoch keine Bewertungen
- Specific Criteria For Accreditation of Medical LaboratoriesDokument19 SeitenSpecific Criteria For Accreditation of Medical LaboratoriesAhmad Naeem Sajed MicrobiologistNoch keine Bewertungen
- Diploma in Medical Lab Technician Course SyllabusDokument29 SeitenDiploma in Medical Lab Technician Course SyllabusMohanbabu DivotsNoch keine Bewertungen
- 03 - SOP Clinical PathologyDokument88 Seiten03 - SOP Clinical PathologyKailash PrajapatNoch keine Bewertungen
- How To Be A Lab Director 2017Dokument200 SeitenHow To Be A Lab Director 2017pieterinpretoria391Noch keine Bewertungen
- Rapid RPR Test Detects Syphilis AntibodiesDokument27 SeitenRapid RPR Test Detects Syphilis AntibodiesRajkishor YadavNoch keine Bewertungen
- Code of Ethics Guidance DocumentDokument30 SeitenCode of Ethics Guidance DocumentASHVINBHAI VACHHANI100% (1)
- 1 Eqa SopDokument2 Seiten1 Eqa SopRajeev PareekNoch keine Bewertungen
- Assay Guidance ManualDokument1.397 SeitenAssay Guidance ManualJoost Van Bree67% (3)
- Error in Laboratory TestDokument8 SeitenError in Laboratory TestBirupakshya RoutNoch keine Bewertungen
- Quality Assurance in The Blood Transfusion LabDokument25 SeitenQuality Assurance in The Blood Transfusion LabMichelle AnsahNoch keine Bewertungen
- Step-by-Step Medical Lab AccreditationDokument30 SeitenStep-by-Step Medical Lab Accreditationvasudeva yasas0% (1)
- Guidelines for Safe POCT ManagementDokument33 SeitenGuidelines for Safe POCT Managementdrella118100% (1)
- B Blab 7 Panel Spring 2012Dokument16 SeitenB Blab 7 Panel Spring 2012pzaballero7063Noch keine Bewertungen
- Clinical ChemistryDokument333 SeitenClinical ChemistryshooberNoch keine Bewertungen
- Lecture Method ValidationDokument46 SeitenLecture Method Validationsarah575Noch keine Bewertungen
- Clinical Chemistry - Theory, Analysis, CorrelationDokument344 SeitenClinical Chemistry - Theory, Analysis, Correlationaristides.quinteroNoch keine Bewertungen
- CC1 - Topic 1Dokument11 SeitenCC1 - Topic 1Marie MontemarNoch keine Bewertungen
- Tropical Haematology and Blood Transfusion PDFDokument77 SeitenTropical Haematology and Blood Transfusion PDFZiauddin AzimiNoch keine Bewertungen
- Diagnostics BrochureDokument20 SeitenDiagnostics BrochureVladimir AtanasiuNoch keine Bewertungen
- Leadership and Management TheoriesDokument7 SeitenLeadership and Management TheoriesVenesse Jaznen Zambrona Nabiong100% (1)
- MLS exam guide outlines content areasDokument15 SeitenMLS exam guide outlines content areasEy ZaNoch keine Bewertungen
- Point of Care Testing Policy Guideline: Edition 1: 2016Dokument40 SeitenPoint of Care Testing Policy Guideline: Edition 1: 2016Paul100% (1)
- Ascp International Procedures BookDokument29 SeitenAscp International Procedures BookNHNoch keine Bewertungen
- Exercise 8 Direct Antiglobulin Test (DAT) : ObjectivesDokument9 SeitenExercise 8 Direct Antiglobulin Test (DAT) : ObjectivesTrang HuynhNoch keine Bewertungen
- Quality Lectures - Pre-Analytic Variables - Dr. Tamer SolimanDokument323 SeitenQuality Lectures - Pre-Analytic Variables - Dr. Tamer Solimanola bakryNoch keine Bewertungen
- CLIA ChecklistDokument10 SeitenCLIA ChecklistMichael HallNoch keine Bewertungen
- Duties and Responsibilities of LabDokument5 SeitenDuties and Responsibilities of LabKate Camat Faminialagao100% (1)
- Examination Content Guideline CDokument5 SeitenExamination Content Guideline CNHNoch keine Bewertungen
- Blood Bak Process MapDokument1 SeiteBlood Bak Process MapspanwzNoch keine Bewertungen
- ABO Blood GroupDokument42 SeitenABO Blood Groupjong188Noch keine Bewertungen
- Blood Banking Chapter 1Dokument9 SeitenBlood Banking Chapter 1throwawyNoch keine Bewertungen
- CLIA Waived Codes ListDokument41 SeitenCLIA Waived Codes ListKarunanidhi PalaniveluNoch keine Bewertungen
- Sop 2Dokument51 SeitenSop 2ALCAZAR, RENZ JAZTINE R.100% (1)
- 638 DXH 520 Hematology Analyzer Brochure BR 66953 en GLB A4Dokument12 Seiten638 DXH 520 Hematology Analyzer Brochure BR 66953 en GLB A4Madness InvokerNoch keine Bewertungen
- Chemical Pathology Job Description December 2011Dokument9 SeitenChemical Pathology Job Description December 2011Chengyuan ZhangNoch keine Bewertungen
- Manual For Procurement of Diagnostics-001-June2013Dokument34 SeitenManual For Procurement of Diagnostics-001-June2013Jose MirandaNoch keine Bewertungen
- IQCPDokument1 SeiteIQCPPrabhu Selvaraj100% (1)
- Blood Bank SOP 2015Dokument52 SeitenBlood Bank SOP 2015ddophlaak labdeptNoch keine Bewertungen
- Medical Laboratory Technician Career JournalDokument2 SeitenMedical Laboratory Technician Career Journalapi-406104878100% (1)
- Clinical Research ClassDokument110 SeitenClinical Research ClassEreshNoch keine Bewertungen
- Recognising Anomalous ABO Blood Group ReactionsDokument16 SeitenRecognising Anomalous ABO Blood Group ReactionsFahim100% (1)
- Common Medical Laboratory Errors PDFDokument2 SeitenCommon Medical Laboratory Errors PDFRosalyn100% (1)
- Laboratory ScopesDokument67 SeitenLaboratory ScopesNash Si100% (1)
- 04 - Haematology SOPDokument120 Seiten04 - Haematology SOPKailash PrajapatNoch keine Bewertungen
- HANDBOOK For Good Clinical Lab PDFDokument265 SeitenHANDBOOK For Good Clinical Lab PDFLife LearningNoch keine Bewertungen
- Ascp Boc Study Guide 5e ContentsDokument12 SeitenAscp Boc Study Guide 5e ContentsCleo SalvadorNoch keine Bewertungen
- What Medical Lab Scientists DoDokument2 SeitenWhat Medical Lab Scientists DoChester KyleNoch keine Bewertungen
- Guidelines For Safe Work Practices in Human and Animal Clinical Diagnostic LaboratoriesDokument352 SeitenGuidelines For Safe Work Practices in Human and Animal Clinical Diagnostic LaboratoriesAndreasNoch keine Bewertungen
- Educacion Basada en VideosDokument9 SeitenEducacion Basada en VideosReymi ThenNoch keine Bewertungen
- PCB Schematic File OpenScope MZ 2016Dokument12 SeitenPCB Schematic File OpenScope MZ 2016Reymi ThenNoch keine Bewertungen
- FLL 2016 2017 Competition Table Building InstructionDokument4 SeitenFLL 2016 2017 Competition Table Building InstructionReymi ThenNoch keine Bewertungen
- LabVIEW-Arduino Data Acquisition and TelemetryDokument38 SeitenLabVIEW-Arduino Data Acquisition and TelemetryReymi ThenNoch keine Bewertungen
- Robert G. Bartle - Introducción Al Análisis Matemático-LIMUSA (1980) PDFDokument507 SeitenRobert G. Bartle - Introducción Al Análisis Matemático-LIMUSA (1980) PDFReymi Then71% (7)
- A6a7a6ca20 at CommendsDokument191 SeitenA6a7a6ca20 at CommendsHuy DannyNoch keine Bewertungen
- Internet, Intranet and Extranet: Network Access Point (NAP)Dokument9 SeitenInternet, Intranet and Extranet: Network Access Point (NAP)Kenneth CasuelaNoch keine Bewertungen
- Ride-Sharing Apps and Privacy in Pakistan: A Study of Uber and Careem PracticesDokument45 SeitenRide-Sharing Apps and Privacy in Pakistan: A Study of Uber and Careem Practiceskandy khan khanNoch keine Bewertungen
- CiC BrochureDokument2 SeitenCiC BrochuretimarliNoch keine Bewertungen
- Complaint FormDokument4 SeitenComplaint FormLuke FarrugiaNoch keine Bewertungen
- Data Privacy ActDokument43 SeitenData Privacy ActJoy Manaog90% (21)
- User Reissue MasterAccount Form NewDokument4 SeitenUser Reissue MasterAccount Form NewVintonius Raffaele PRIMUSNoch keine Bewertungen
- State Bank of India, Sydney Branch: Terms and ConditionsDokument6 SeitenState Bank of India, Sydney Branch: Terms and ConditionsSujib BarmanNoch keine Bewertungen
- D-1 SupplierDataProtectionRequirements v.2Dokument1 SeiteD-1 SupplierDataProtectionRequirements v.2Maria Princess AlturaNoch keine Bewertungen
- OetDokument15 SeitenOetAchwani Santosh0% (1)
- 2018-022 - Final Response (Sent 06 Oct 2017)Dokument85 Seiten2018-022 - Final Response (Sent 06 Oct 2017)Bob MackinNoch keine Bewertungen
- PDFDokument7 SeitenPDFAnna BacakovaNoch keine Bewertungen
- Information Security Policy v5Dokument35 SeitenInformation Security Policy v5Thanesh YogaNoch keine Bewertungen
- Assayfit Pro Curve Fitting Full ManualDokument89 SeitenAssayfit Pro Curve Fitting Full ManualAnonymous p16X39fPyNoch keine Bewertungen
- Brian Barrientos DocuDokument87 SeitenBrian Barrientos Docuroveline tolica50% (2)
- Grants for Professional Writers: Creative WritingDokument16 SeitenGrants for Professional Writers: Creative WritingRuy CastroNoch keine Bewertungen
- Nova Scotia Nominee Program NSNP 100 - Application Form For The Principal ApplicantDokument22 SeitenNova Scotia Nominee Program NSNP 100 - Application Form For The Principal ApplicantPrasanta GhoruiNoch keine Bewertungen
- AIPDM ArticleDokument8 SeitenAIPDM Articleacademic workNoch keine Bewertungen
- Gartner - GDPR Clarity-19 Frequently Asked Questions AnsweredDokument6 SeitenGartner - GDPR Clarity-19 Frequently Asked Questions AnsweredDennis O'DonohueNoch keine Bewertungen
- Application Form - Apprenticeship-2 PDFDokument5 SeitenApplication Form - Apprenticeship-2 PDFJanus LinNoch keine Bewertungen
- GDPR Applicant Privacy PolicyDokument5 SeitenGDPR Applicant Privacy PolicyRomina RusNoch keine Bewertungen
- Template Consent FormDokument5 SeitenTemplate Consent FormAlexandru ComanNoch keine Bewertungen
- Personal data notice from Puncak Athenaeum ManagementDokument1 SeitePersonal data notice from Puncak Athenaeum Managementعصام السامرائيNoch keine Bewertungen
- Scoot Conditions of Carriage FinalDokument28 SeitenScoot Conditions of Carriage FinalRenuga I. KuppusamyNoch keine Bewertungen
- Accenture CoBE Brochure EnglishDokument56 SeitenAccenture CoBE Brochure EnglishMmdNoch keine Bewertungen
- UPS OAR Alumni Update Form UPAA Application Option OAR and UPAA Privacy NoticesDokument10 SeitenUPS OAR Alumni Update Form UPAA Application Option OAR and UPAA Privacy NoticesMelani NaperiNoch keine Bewertungen
- Things You Need To Know About Telstra Services c048Dokument12 SeitenThings You Need To Know About Telstra Services c048Tayntayn MugolNoch keine Bewertungen
- InvestHedge Forum BrochureDokument9 SeitenInvestHedge Forum BrochureHedgeFund Intelligence100% (1)
- Ap 2012 French Language Free Response Questions PDFDokument11 SeitenAp 2012 French Language Free Response Questions PDFWANG EmilieNoch keine Bewertungen
- Introduction To European Data Protection OutlineDokument91 SeitenIntroduction To European Data Protection OutlinewhitergNoch keine Bewertungen
- 494-500 Lisgar MPAC 2008 Assessment 532kDokument8 Seiten494-500 Lisgar MPAC 2008 Assessment 532kjawaid6970Noch keine Bewertungen