Beruflich Dokumente
Kultur Dokumente
Structured Reporting of Multiphasic CT For Hepatocellular Carcinoma: Effect On Staging and Suitability For Transplant
Hochgeladen von
Renz Marion AlemaniaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Structured Reporting of Multiphasic CT For Hepatocellular Carcinoma: Effect On Staging and Suitability For Transplant
Hochgeladen von
Renz Marion AlemaniaCopyright:
Verfügbare Formate
Gastrointestinal Imaging • Original Research
Poullos et al.
Multiphasic CT Reporting for HCC
Gastrointestinal Imaging
Original Research
Structured Reporting of
Multiphasic CT for Hepatocellular
Carcinoma: Effect on Staging and
Suitability for Transplant
Peter D. Poullos1 OBJECTIVE. The purpose of this study is to evaluate whether use of a standardized radi-
Joseph J. Tseng1 ology report template would improve the ability of liver transplant surgeons to diagnose stage
Marc L. Melcher 2 T2 hepatocellular carcinoma (HCC) and determine patient suitability to undergo orthotopic
Waldo Concepcion2 liver transplant (OLT).
Andreas M. Loening 3 MATERIALS AND METHODS. In this retrospective study, a standardized template
was devised, and its use was mandated for reporting of liver CT findings for patients with
Jarrett Rosenberg 4
cirrhosis and HCC. Two surgeons analyzed 200 reports (100 before and 100 after template
Jüergen K. Willmann1
American Journal of Roentgenology 2018.210:766-774.
implementation) for descriptions of cirrhosis, portal hypertension, lesion enhancement char-
Poullos PD, Tseng JJ, Melcher ML, et al. acteristics, tumor thrombus, portal and superior mesenteric vein patency, and Organ Procure-
ment Transplantation Network (OPTN) class. Ability to determine Milan criteria and surgeon
satisfaction were also assessed. Data obtained before and after template implementation were
statistically analyzed using the Cochran-Mantel-Haenszel test.
RESULTS. Template implementation increased the percentage of reports documenting
the presence or absence of portal hypertension (74% to 88% for surgeon 1 and 86% to 87%
for surgeon 2; p = 0.042); lesion number (76% to 88% for surgeon 2 [no change for surgeon
1]; p = 0.038), size (95% to 96% for surgeon 1 and 82% to 93% for surgeon 2; p = 0.03), and
enhancement (93% to 94% for surgeon 1 and 80% to 91% for surgeon 2; p = 0.049); presence
of tumor thrombus (10% to 57% for surgeon 1 and 31% to 63% for surgeon 2; p < 0.001); and
OPTN class (8% to 82% for surgeon 1 and 2% to 81% for surgeon 2; p < 0.001). The surgeons
Keywords: hepatocellular carcinoma, liver transplant,
Organ Procurement and Transplantation Network,
were significantly more able to determine the presence of T2 disease and qualification for ex-
standard reporting, template ception points after implementation of the template (increasing from 80% to 94%; p = 0.025).
Satisfaction with reports also improved (p < 0.0001).
doi.org/10.2214/AJR.17.18725 CONCLUSION. The reporting template improved determination of patient suitability to
undergo transplant according to the Milan criteria.
Received July 5, 2017; accepted after revision
August 22, 2017.
epatocellular carcinoma (HCC) Patients with cirrhosis who do not have
Based on a presentation at the Radiological Society of
North American 2015 annual meeting, Chicago, IL.
1
Department of Radiology, Division of Body Imaging,
H is a major cause of death among
patients with end-stage liver dis-
ease (ESLD). For patients with
HCC are prioritized by calculating the model
for end-stage liver disease (MELD) score on
the basis of bilirubin, creatinine, and interna-
Stanford University, 300 Pasteur Dr, Stanford, CA HCC and ESLD, potentially curative options tional normalized ratio (INR) values. MELD
94305-5621. Address correspondence to J. J. Tseng include surgical resection, ablation, and or- alone, however, does not reflect the progno-
(jtseng3@stanford.edu).
thotopic liver transplant (OLT). For trans- sis for HCC in patients [2] in whom tumor
2
Department of Surgery, Division of Multi Organ plant candidates who are ineligible for cura- progression, vascular invasion, and metastat-
Transplantation, Stanford University, Stanford, CA. tive resection, OLT is a desirable method for ic disease can preclude transplant. To rec-
simultaneously removing the HCC and re- tify this disadvantage, the United Network
placing the failing cirrhotic liver. OLT, how- for Organ Sharing, which organizes the Or-
3
Department of Radiology, Division of Body MRI,
Stanford University, CA.
ever, requires that the patient be placed on a gan Procurement and Transplantation Net-
4
Department of Radiology, Stanford University, waiting list. In 2016, a total of 14,750 pa- work (OPTN) in the United States, has cre-
Stanford, CA. tients were listed as waiting for transplant, ated an exception categorization that allows
but only 7841 transplants were performed; patients with HCC to obtain a higher MELD
AJR 2018; 210:766–774
1206 patients died while waiting, and an ad- score that more appropriately reflects their
0361–803X/18/2104–766 ditional 1404 patients were removed from medical urgency for liver transplant. Candi-
the list because they were too sick to under- dates meeting these criteria receive an ini-
© American Roentgen Ray Society go transplant [1]. tial MELD score equivalent of 22, and fur-
766 AJR:210, April 2018
Multiphasic CT Reporting for HCC
ther points are awarded based on laboratory The purpose of the present study is to template listed as a “body CT abdomen liver tri-
values [3]. evaluate whether the use of a standardized phasic” (Appendix 4) was also created for reports
To obtain points, HCC lesions must meet radiology report template would improve the assessing patients without stage T2 HCC (with
specific OPTN imaging-based criteria [4]. Le- ability of liver transplant surgeons to diag- this less detailed template hereafter referred to as
sions are designated OPTN class 1 (definite- nose stage T2 HCC and suitability for OLT. the “non-OPTN template”). Before template im-
ly benign) through class 5 (definitely HCC), plementation, radiologists used their own personal
depending on their size and arterial enhance- Materials and Methods style of dictation to create reports.
ment as well as the presence of washout, cap- Template Design
sule, threshold growth, or a combination of An institutional review board waiver was Report Collection
these features. Candidates must have at least granted for this study, and informed consent was Eighteen months after the start date, reports of
one OPTN class 5 lesion and stage T2 disease, waived because of the retrospective methods used. patients with HCC were collected for analysis, with
as defined by the Milan criteria (Appendix 1), The study was HIPAA compliant. an arbitrary goal of collecting 100 reports dictated
to qualify for exception points. To apply, the Two abdominal radiologists created the tem- before template implementation and 100 reports dic-
transplant team must complete standard Unit- plate for patients with stage T2 HCC (Appendix tated after template implementation. The lead author
ed Network for Organ Sharing documentation 3) to include all imaging details needed to apply requested that the radiology information technol-
that includes comprehensive imaging details for exception points. This template was derived in ogy team search the radiology information system
(Appendix 2). Surgeons rely on radiology re- part from templates freely available through the for multiphasic (late arterial, portal venous, and de-
ports that, unfortunately, often omit the de- Radiological Society of North America Informat- layed) liver CT reports containing the terms “cir-
tails required for these forms. Significant time ics Reporting website [11], and additional modifi- rhosis” and either “hepatocellular carcinoma” or
is spent reevaluating imaging studies because cations were made to mimic the required OPTN “HCC.” The search results were returned in a chron-
of information missing from the reports, es- documentation completed by the transplant team. ologically sorted order with the use of spreadsheet
sentially requiring a second radiologist to re- After creation of this template, the chief of clinical software (Excel, version 15.0, Microsoft) with an ac-
American Journal of Roentgenology 2018.210:766-774.
interpret the case (for example, at liver trans- transplantation reviewed and approved its use. Of companying word-processed document (Microsoft
plant tumor boards). importance, the surgeons surveyed in the present Word 2013, Microsoft) containing the reports.
Structured reporting has been endorsed study were unaware of our research intentions and Inclusion criteria (Table 1) were designed to fa-
by the American College of Radiology and their future role as report analysts. cilitate collection of a variety of reports for pa-
other professional societies as a method of tients who were close to meeting the Milan criteria,
communicating the most pertinent and use- Template Implementation for whom accurate staging would be particular-
ful information with the use of standardized On January 13, 2014 (the start date), an e-mail ly important. Exclusion criteria were designed to
language and formatting [5, 6]. Template cre- was sent to all radiology faculty and trainees, minimize reports including likely benign lesions
ation should be a multidisciplinary effort, designating our template mandatory for use in or early HCC. Although hyperenhancing lesions
and studies have shown that both referring reports regarding patients with stage T2 HCC. smaller than 1 cm and hypoenhancing lesions may
physicians and radiologists favor structured OPTN educational references were also included. probably represent HCC (according to the Liv-
over conventional nonstructured reports [7– The template was made available in a real-time er Imaging Reporting and Data System or OPTN
9]. Although widely adopted, the clinical radiology reporting platform (Power Scribe 360, class 4), these patients do not qualify for exception
impact of such templates has not been well Nuance) under the listing “body CT abdomen liver points and therefore were excluded. Likewise, we
studied in the literature. However, findings OPTN HCC.” This template will hereafter be re- excluded patients with advanced HCC, who also
from early studies are promising [10]. ferred to as the “OPTN template.” A less detailed do not qualify for exception points.
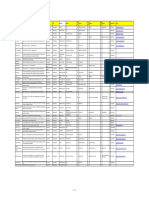
TABLE 1: Inclusion and Exclusion Criteria for Chart Review
Inclusion Criteria Exclusion Criteria
The report states that a lesion is “consistent with HCC” or equivalent language Report specifies that the patient does not have cirrhosis (making hepatectomy
an option)
Multiphasic CT of adequate quality (judged to be adequate unless stated Lesions that are “likely benign,” “unlikely to represent HCC,” or have an
otherwise) equivalent status
The report either states that the patient has cirrhosis or makes no mention of Lesions that are less than 1 cm or larger than 10 cm in maximum diameter
cirrhosis
Lesions that are reported as “too numerous to count, ”innumerable” or as
having an equivalent status
Infiltrative (non–mass-forming) HCC
Hypoenhancing HCC
Prior hepatectomy or liver transplant for HCC
Organ Procurement Transplantation Network class 3
Technically limited examination (unenhanced or single phase)
Nonabdominal study (CT chest or interventional procedure)
Note—HCC = hepatocellular carcinoma.
AJR:210, April 2018 767
Poullos et al.
tree, as well as information about portal hyperten-
Report review of triphasic Report review of triphasic sion (splenomegaly, ascites, varices, and related el-
liver CT done for HCC liver CT done for HCC
evaluation prior to evaluation after ements). Report syntax was not altered in any way.
January 13, 2014 January 13, 2014
Survey Creation
397 Reports excluded while 282 Reports excluded while A survey was created to analyze each report (Ta-
reaching goal of 100 reports reaching goal of 100 reports ble 3). The first eight questions (regarding funda-
meeting inclusion criteria meeting inclusion criteria
mental information) were questions with yes or no
responses that assessed the adequacy of informa-
100 Reports meeting 100 Reports meeting
tion crucial and fundamental to all reports of pa-
inclusion criteria inclusion criteria
tients with ESLD and HCC. Questions nine and 10
(regarding OPTN designation) assessed the inclu-
200 Reports truncated, sion and correctness of OPTN grading. Questions
sanitized, and randomized 11 and 12 (regarding making the diagnosis) were
for review by surgeons more subjective and included an option for uncer-
tainty. Question 13 assessed overall satisfaction.
Fig. 1—Report selection flowchart. HCC = hepatocellular carcinoma.
Report Analysis
Reports were reviewed and collected chrono- abdominal CT reports was lesions that were un- The 200 reports were randomized using a free
logically, working both backward and forward likely to represent HCC (n = 123), followed by le- online randomizer (Research Randomizer, ver-
from the start date. The lead author provided to sions with indeterminate HCC status (n = 17) and sion 4.0, Social Psychology Network) and were
another author both OPTN literature and verbal presence of too many lesions (n = 17). collated into a single 200-page PDF document,
American Journal of Roentgenology 2018.210:766-774.
instruction regarding inclusion and exclusion cri- with each page containing only one unique re-
teria. The two authors then collected 20 reports to- Report Sanitization and Truncation port. Each surgeon, blinded to study goal and de-
gether, practicing selection using the inclusion and Reports were sanitized to remove all protect- sign, received a copy of this document, along with
exclusion criteria. The author who had received ed health information, clinical information, and a link to the electronic survey. Study survey data
instruction then collected 20 additional reports on dates. They were further truncated by deleting in- were collected and managed using research elec-
his own, which the lead author then reviewed for formation related to IV contrast medium and ra- tronic data capture tools (REDCap, version 6.9.3,
accuracy. Once trained satisfactorily, the author diation dose, as well as statements related to the Stanford University).
trained by the lead author collected the remaining thorax, pancreas, adrenals, kidneys and ureters,
160 reports, which were then reviewed once more bowel, lymph nodes, abdominal wall, and bones. Response Tabulation
by the lead author to determine adherence to the All that remained (when included) was text de- Questions 1–9 elicited yes or no responses,
inclusion and exclusion criteria. scribing liver morphologic findings, hepatic vas- whereas questions 10–12 offered a third response
To find 100 pretemplate reports meeting inclu- culature, liver lesions, gallbladder, and biliary option (unsure) because they inquired about the
sion criteria, we reviewed 497 reports dating up to
TABLE 2: Reasons for Report Exclusion Among Abdominal CT Studies
27 months before the start date. To find 100 post-
template reports, we reviewed 382 reports dating up Reason for Report Exclusion Before Template After Template
to 20 months after the start date. A total of 397 pre-
Not likely HCC 169 123
template and 182 posttemplate reports were exclud-
ed (Fig. 1). Detailed reasons for exclusion are listed Nonabdominal CT 95 88
in Table 2. If a single patient had multiple unique Prior hepatic surgery 26 2
reports, those were not excluded. All posttemplate Prior OLT 23 7
reports meeting inclusion criteria were included, re-
Too many lesions 19 17
gardless of whether the OPTN template was used.
It was decided a priori to do an intention-to-treat Metastatic disease 14 7
analysis, avoiding overoptimistic estimates of tem- Indeterminate lesion 13 17
plate effectiveness resulting from inclusion bias. Maximum lesion diameter < 1 cm 11 4
Ninety-five pretemplate and 88 posttemplate
Technically limited 9 4
reports were eliminated because they were not
for abdominal CT. These included interventional Maximum lesion diameter > 10 cm 7 1
radiology procedures and CT scans of the chest Infiltrative HCC 5 0
that were inadvertently captured in our radiology Tumor thrombus 4 5
information system search results. In the pretem-
OPTN class 3 2 7
plate group, the two most common reasons for ex-
clusion of abdominal CT reports were lesions that Hypoenhancing HCC 0 0
were unlikely to represent HCC (n = 169) and pre- Total 397 282
vious hepatic surgery (n = 26). In the posttemplate Note—HCC = hepatocellular carcinoma, OLT = orthotopic liver transplant, OPTN = Organ Procurement
group, the most common reason for exclusion of Transplantation Network.
768 AJR:210, April 2018
Multiphasic CT Reporting for HCC
TABLE 3: Questions Appearing on the Survey Submitted to Surgeon Readers
1. Does the report adequately convey presence or absence of cirrhosis? [yes or no]
2. Does the report adequately convey the presence or absence of portal hypertension? [yes or no]
3. Does the report adequately state the number of lesion(s)? [yes or no]
4. Does the report adequately state the size of the lesion(s)? [yes or no]
5. Does the report clearly state the enhancement characteristics (both arterial and portal venous and/or delayed phases) of the lesion(s)? [yes or no]
6. Does the report adequately communicate the presence or absence of tumor thrombus? [yes or no]
7. Does the report adequately communicate portal vein patency? [yes or no]
8. Does the report adequately communicate SMV patency? [yes or no]
9. Does the report mention OPTN class? [yes or no]
10. Is the OPTN class correct? [yes, no, or unsure]
11. Assuming the imaging description is correct, does the patient have hepatocellular carcinoma? [Yes, no, or not enough information to judge]
12. Based purely on this report, in the absence of contraindications to transplant, can you determine whether or not this patient falls within the Milan criteria
and qualifies for MELD priority score? [yes, he qualifies; no, he does not qualify; or unsure and need more imaging details]
13. How satisfied are you with the information contained in this report? [1, not at all satisfied; 2, dissatisfied; 3, neutral; 4, satisfied; 5, very satisfied]
Note—Information appearing in brackets in each question indicates possible responses. SMV = superior mesenteric vein, OPTN = Organ Procurement Transplantation
Network, MELD = Model for End Stage Liver Disease.
ability to draw conclusions on the basis of report obtained after that date. Of the 100 re-
American Journal of Roentgenology 2018.210:766-774.
Overall Survey Results
information. Both “yes” and “no” were considered ports obtained after template implementa- The total number of positive respons-
positive responses, whereas “unsure” was consid- tion, 47% complied with the OPTN template es and the interobserver agreement (kappa)
ered a failure of reporting. Thus, for questions 10– format, and 53% did not. Intention-to-treat between two surgeons for pretemplate and
12, yes and no responses were grouped together analysis was performed, and all 100 re- posttemplate reports are presented in Ta-
and compared with unsure responses. For ques- ports obtained after template implementa- ble 5. Question 9, regarding the mentioning
tion 10, the surgeon reading the report made the tion were compared with all 100 reports ob- of OPTN criteria, had the greatest level of
determination of whether the OPTN designation tained before implementation. agreement, with a kappa value of 0.84 (95%
was correct. CI, 0.755–0.900).
Patient Characteristics Of the 13 total questions on the survey, re-
Statistical Analysis The 100 pretemplate reports referred to 88 sponses for ten improved significantly after
The data from the survey results were export- individual patients; three patients each had template implementation. These ten ques-
ed from the research electronic data capture tool three reports, six patients had two, and 79 pa- tions were questions 2, 3, 4, 5, 6, 9, 10, 11, 12
into spreadsheet software. An author who was not tients had one. Sixty-four reports were for men and 13. Questions 2, 3, 4, 5 and 11 showed
involved in either the study design or data collec- and 36 were for women. The age range of the marginally significant improvements (p =
tion analyzed the data using statistical software patients was 39–80 years, with a mean and 0.025–0.049). Questions 6, 10, 12, and 13
(Stata, version 14, StataCorp). Differences in re- median age of 60 years. The 100 posttemplate showed highly significant improvements
sponses to questions before and after implemen- reports referred to 78 patients; six patients had (p < 0.0001–0.001).
tation of the template were tested using Cochran- three unique reports, 10 patients had two, and
Mantel-Haenszel tests stratified by surgeon, with 62 patients had one. Sixty-nine reports were Inclusion of Fundamental Information:
a null hypothesis of no difference between preim- for men and 31 were for women. The patient Questions 1–8
plementation and postimplementation responses. age range was 49–73 years, with a mean age of With regard to these eight questions, ade-
The effect of report attributes on postimplementa- 62 years and a median age of 64 years. Patient quacy improved for five, and three showed no
tion satisfaction was assessed by multivariable lo- characteristics are summarized in Table 4. change after template implementation.
gistic regression with the surgeon considered a co-
variate. A significance level of p < 0.05 was used.
TABLE 4: Patient Characteristics in 100 Reports Obtained Before Versus
Subgroup analysis was also performed using
100 Reports After Template Implementation
similar statistical methods to compare the post-
template reports that used the OPTN template (n = Characteristic Before Template After Template
47) with posttemplate reports that deviated from No. of unique patients 88 78
the OPTN template (n = 53).
Age range (y) 39–80 49–73
Results Mean age (y) 60 62
Template Compliance Median age (y) 60 64
One hundred reports meeting our inclu- No. of men 64 69
sion criteria were obtained before the tem-
No. of women 36 31
plate implementation date, and 100 were
AJR:210, April 2018 769
Poullos et al.
TABLE 5: Total Number of Positive Responses and Interobserver Agreement (Kappa Value) Between Two Surgeons
for Reports Obtained Before and After Template Implementation
Positive Responses (%) Kappa Value
Before Template After Template
Before After Overall
Question Number and and Topic Surgeon 1 Surgeon 2 Surgeon 1 Surgeon 2 p Template Template Overall 95% CI
Question 1: cirrhosis 97 93 95 92 0.52 0.37 0.59 0.5 0.216–0.762
Question 2: portal hypertension 74 86 88 87 0.042 0.27 0.41 0.32 0.159–0.489
Question 3: no. of lesions 98 76 98 88 0.038 0.04 −0.04 0.01 −0.046 to 0.122
Question 4: size of lesions 95 82 96 93 0.03 0.10 0.14 0.12 0.045–0.313
Question 5: enhancement 93 80 94 91 0.049 −0.12 0.07 −0.05 −0.113 to 0.074
Question 6: tumor thrombus 10 31 57 63 < 0.001 0.22 0.46 0.46 0.327–0.567
Question 7: PV patency 80 68 72 65 0.22 0.49 0.52 0.51 0.379–0.631
Question 8: SMV patency 37 37 34 37 0.76 0.70 0.72 0.71 0.597–0.805
Question 9: OPTN mentioned 8 2 82 81 < 0.001 0 0.63 0.84 0.755–0.900
Question 10: OPTN correct (% of question 9) 50 0 100 96 < 0.001 — — — —
Question 11: HCC 80 80 95 93 0.025 0.31 0.14 0.27 0.131–0.415
Question 12: Milan criteria 78 80 89 96 < 0.0001 0.25 0.40 0.34 0.249–0.444
American Journal of Roentgenology 2018.210:766-774.
Question 13: satisfaction 3 30 50 80 < 0.0001 0.01 0.28 0.36 0.047–0.182
Note—PV = portal vein, SMV = superior mesenteric vein, OPTN = Organ Procurement and Transplantation Network, HCC = hepatocellular carcinoma, — = not applicable.
The five items that improved were pres- implementation (p < 0.001). Subgroup analy- Transplantability
ence or absence of portal hypertension, sis reveals that four of 47 OPTN template re- Before implementation of the template,
number of lesion(s), size of the lesion(s), en- ports (8.5%) did not mention OPTN. None of 20% (surgeon 1) or 22% (surgeon 2) of the
hancement characteristics, and the presence these four patients, however, had T2 disease, reports studied were perceived as not con-
or absence of tumor thrombus. Of these five so not using the OPTN template was a cor- taining enough information for the surgeons
items, the most statistically significant im- rect decision. One patient had a 6.6-cm le- to decide whether the patient met the Milan
provement was the mention of tumor throm- sion, another patient had six tumors, a third criteria. This value decreased to 4% (surgeon
bus, which increased from 10% (surgeon 1) patient had a lesion with questionable wash- 1) or 11% (surgeon 2) after template imple-
or 31% (surgeon 2) before template imple- out, and the last patient had a lesion that was mentation (p < 0.0001) (Fig. 3).
mentation to 57% (surgeon 1) or 63% (sur- actually OPTN class 4, although that was
geon 2) after template implementation (p < not explicitly stated. In contrast, 12 of the 53 Satisfaction
0.001). Subgroup analysis after template im- non–OPTN-template reports (22.6%) did not Before template implementation, surgeon
plementation showed that 91% (surgeon 1) or mention OPTN. Of those 12 reports, seven 1 was satisfied or very satisfied with 3% of
89% (surgeon 2) of the 47 OPTN template (58%) were for patients with T2 disease, and the reports. However, this value increased to
reports reported the presence or absence of therefore should have mentioned OPTN. 50% for reports created after template im-
tumor thrombus, compared with 74% (sur- Surgeon 1 stated that of the 8% of pre- plementation (p < 0.0001). Before template
geon 1) or 68% (surgeon 2) of the 53 non- template reports that mentioned OPTN, implementation, surgeon 2 was satisfied or
OPTN template reports (for surgeon 1, p = 50% were correctly classified. Of the 82% of very satisfied with 30% of the reports. This
0.035; for surgeon 2, p = 0.015). One patient posttemplate reports that mentioned OPTN, value increased to 80% for reports created
in the pretemplate group and one patient in 100% were correctly classified. Surgeon 2 after template implementation (p < 0.0001)
the posttemplate group had a tumor throm- stated that of the 2% of the pretemplate re- (Fig. 4). When multivariate analysis was per-
bus. The three items for which no improve- ports that mentioned OPTN, 100% were cor- formed, the items that were correlated with
ment was seen were presence or absence of rectly classified. Also, of the 81% of post- report satisfaction were portal hypertension,
cirrhosis, portal vein patency, and superior template reports that mentioned OPTN, 96% tumor thrombus, portal vein patency, and
mesenteric vein patency. were correctly classified. OPTN class (p < 0.001 for all).
Organ Procurement Transplantation Network Making the Diagnosis Discussion
Designation: Questions 9 and 10 Before template implementation, 80% of Determining whether patients with HCC
The surgeons responded that the percent- reports (for both surgeons 1 and 2) were per- are eligible for MELD exception points is
age of reports that mentioned the OPTN were ceived to adequately convey the presence or challenging because of the various clinical
8% (surgeon 1) or 2% (surgeon 2) before tem- absence of HCC. After template implementa- and imaging data that must be reported. By
plate implementation, compared with 82% tion, this finding improved to 95% (surgeon utilizing structured reporting, we significant-
(surgeon 1) or 81% (surgeon 2) after template 1) or 93% (surgeon 2) (p = 0.025) (Fig. 2). ly improved communication of relevant in-
770 AJR:210, April 2018
Multiphasic CT Reporting for HCC
100 100
80 80
Percentage of Responses
Percentage of Responses
60 60
40 40
20 20
0 0
Before After Before After Before After Before After
Template Template Template Template Template Template Template Template
Surgeon 1 Surgeon 2 Surgeon 1 Surgeon 2
No Unsure Yes No Unsure Yes
American Journal of Roentgenology 2018.210:766-774.
Fig. 2—Bar graph of reader response to survey question 11 (“Assuming imaging Fig. 3—Bar graph of reader response to survey question 12 (“Based purely on this
description is correct, does patient have hepatocellular carcinoma?”). report, in absence of contraindications to transplant, can you determine whether
or not this patient falls within Milan criteria and qualifies for MELD priority
score?”). MELD = model for end-stage liver disease.
formation as well as surgeon satisfaction. pressions were compared with arthroscopic MRI examinations. By utilizing a 12-item
Specifically, we improved the ability of sur- findings, and the overall accuracy increased structured reporting template for brain MRI
geons to diagnose HCC and assess suitability from 53% to 76% when readers used the examinations of patients with known or sus-
for MELD exception points. structured template as opposed to traditional pected multiple sclerosis, the authors were
Our results are concordant with those of reports. Dickerson et al. [13] also compared able to show that reports obtained after tem-
other studies that have shown that structured the differences in report thoroughness and plate implementation yielded a significant in-
reports provide superior description and satisfaction between reports obtained before crease in multiple sclerosis–relevant findings
evaluation of the clinical question and im- and after template implementation that de- and positive ratings by neurologists. Reports
prove the confidence of referring physicians scribed multiple sclerosis findings on brain obtained after template implementation men-
[7–9, 12]. Brook et al. [12] compared struc-
tured versus traditional reports of multipha-
sic CT for the ability to assess for resectabil- 100
ity of pancreatic carcinoma. They found that
structured reports provided more complete
reporting of 12 key features (7.3 of 12 fea- 80
Percentage of Responses
tures for nonstructured reports vs 10.6 of 12
features for structured reports (p < 0.01), and
they increased the sufficiency of information 60
needed for surgical planning [12].
The results of our study compare favor-
ably with those of other studies in the medi- 40
cal literature. There was an 80% (surgeon 1)
or 50% (surgeon 2) perceived improvement
20
in the completeness of information needed
to determine whether patients met the Milan
criteria in our study.
0
Ellerman et al. [10] did a similar analysis Fig. 4—Bar graph of
Before After Before After
by comparing the ability of structured and reader response to
Template Template Template Template
Surgeon 1 Surgeon 2
traditional MRI reports to predict osteochon- survey question 13
dritis dissecans lesion stability. International (“How satisfied are
Very Unsatisfied Neutral Satisfied
you with information
Cartilage Repair Society criteria were used contained in this Unsatisfied Very Satisfied
in the structured template. Radiologic im- report?”).
AJR:210, April 2018 771
tioned 11.1 findings, whereas those obtained at liver transplant tumor board and to improve Network: national data. Health Resources and
Poullos et al.
before implementation mentioned 5.8 find- communication and surgeon satisfaction. Services Administration website. optn.transplant.
ings (p < 0.001). The posttemplate reports The present study has several limitations. hrsa.gov/data/view-data-reports/national-data.
also were more likely to receive positive rat- First, there may have been an inherent bias Published 2017. Accessed April 9, 2017
ings, compared with the pretemplate reports of the surgeons to prefer reports containing 2. Bernardi M, Stefano G, Maurizio B. The MELD
(56% vs 28%; p = 0.01) [13]. Other authors OPTN terminology, especially because they score in patients awaiting liver transplant: strengths
have also shown that structured reports are had been lobbying for us to report it. We were and weaknesses. J Hepatol 2011; 54:1297–1306
preferred, clearer, and result in greater inter- also concerned that the readers might guess the 3. Health Resources and Services Administration
reader agreement [7, 8, 14]. goal of the study, thereby further biasing the (HRSA). OPTN: policies. HRSA website. Policy
Implementing a standardized reporting results. However, we took measures to conceal 3.6 organ distribution: allocation of livers. optn.
template can be labor intensive and can take this goal: the readers had no input into study transplant.hrsa.gov/governance/policies/. hrsa.gov/
time to gain traction. Although we had held design, we did not discuss the reason for the policiesAndBylaws/policies.asp. Published 2012.
division meetings and circulated e-mails survey (which was administered nearly 2 years Accessed April 9, 2017
about the clinical importance of lesion cate- after we implemented the OPTN template), 4. Wald C, Russo MW, Heimbach JK, Hussain
gorization with either the Liver Imaging Re- and all the reports were randomized and made HK, Pomfret EA, Bruix, J. New OPTN/UNOS pol-
porting and Data System or OPTN since Jan- to look similar. icy for liver transplant allocation: standardization of
uary of 2013, routine voluntary reporting by A potential source of bias is the inclusion liver imaging, diagnosis, classification, and report-
radiologists was sporadic. In January 2014, of multiple reports from the same subjects be- ing of hepatocellular carcinoma. Radiology 2013
when the OPTN template was made man- cause similar disease burden and alliterative 266:376–382
datory, the number of reports classifying le- reporting may have influenced subsequent re- 5. Kahn CE Jr, Langlotz CP, Burnside ES, et al. To-
sions with the use of these criteria substan- ports. Furthermore, the retrospective structure ward best practices in radiology reporting.
tially improved; nonetheless, only 47% of of the study is a weakness. A prospective ran- Radiology 2009; 252:852–856
reports complied with template use within domized trial of reporting may have provided 6. Dunnick NR, Langlotz CP. The radiology report
the 20 months after introduction. more valid results; however, with 10 body im- of the future: a summary of the 2007 Intersociety
Correctness of classification also im- aging fellows and 20 faculty members (includ-
American Journal of Roentgenology 2018.210:766-774.
Conference. J Am Coll Radiol 2008; 5:626–629
proved. The template contained a built-in ing some from other divisions) interpreting 7. Schwartz LH, Panicek DM, Berk AR, Li Y,
decision support tool; essentially, an OPTN a large number of studies at multiple clinical Hricak H. Improving communication of diagnos-
cheat sheet was included below the impres- sites, randomization would have been imprac- tic radiology findings through structured report-
sion section of the report, along with instruc- tical. Also, the fact that only 47% of the post- ing. Radiology 2011; 260:174–181
tions indicating to delete the cheat sheet be- template reports actually followed the OPTN 8. Naik SS, Hanbidge A, Wilson SR. Radiology reports:
fore report approval. This likely improved template could be viewed as a weakness. How- examining radiologist and clinician preferences re-
efficiency and accuracy because dictating ever, the inclusion of non-OPTN template garding style and content. AJR 2001; 176:591–598
trainees no longer had to spend time search- studies in our analysis actually strengthens the 9. Grieve FM, Plumb AA, Khan SH. Radiology re-
ing online for OPTN classification materials, results because improvement was still shown. porting: a general practitioner’s perspective. Br J
which may or may not be reliable. Undoubt- Of course, it is impossible to know which com- Radiol 2010; 83:17–22
edly, simultaneous education of trainees and ponent of the improvement was the result of 10. Ellermann JM, Donald B, Rohr S, et al. Magnetic
faculty also had an effect. education and which was the result of the tem- resonance imaging of osteochondritis dissecans:
One obvious reason for improved confi- plate, but likely both are important. It would validation study for the ICRS classification sys-
dence in the diagnosis of HCC might be that be reasonable to expect that future studies that tem. Acad Radiol 2016; 23:724–729
the OPTN template is much more detailed only included the OPTN template would show 11. RSNA Informatics Reporting website. Radiological
than the non-OPTN template. A detailed re- even more significant improvements. society of North America (RSNA). radreport.org/
port not only communicates more informa- In conclusion, the results of the present index.php. Accessed January 30, 2018
tion, but it also likely conveys more radiologist study suggest that the implementation of a 12. Brook OR, Brook A, Vollmer CM, Kent TS, S anchez
confidence and competence. In addition to its standardized reporting template was valu- N, Pedrosa I. Structured reporting of multiphasic CT
detail, it is arranged more logically in a format able in improving communication between for pancreatic cancer: potential effect on staging and
(United Network for Organ Sharing paper- radiologists and transplant surgeons. By surgical planning. R adiology 2015; 274:464–472
work) that is recognizable and makes sense. prompting the radiologist to comment on 13. Dickerson E, Davenport MS, Syed F, et al. Effect of
Perhaps no other outcome of our study is specific details, the template was able to im- template reporting of brain MRIs for multiple sclero-
more important than the ability to determine prove the quality and completeness of tripha- sis on report thoroughness and neurologist-rated
whether a patient meets the Milan criteria and sic liver CT reports, as well as the satisfac- quality: results of a prospective quality improvement
thus qualifies for the MELD priority score. Al- tion of surgeons. With implementation of a project. J Am Coll Radiol 2017; 14:371.e1–379.e1
though the template improved the ability of the standardized reporting template, institutions 14. Ghoshhajra BB, Lee AM, Ferencik M, et al. Inter-
surgeon to determine this, a larger study with may be able to increase the accuracy of ra- preting the interpretations: the use of structured
longer follow-up would be needed to determine diologic diagnosis and staging of HCC and reporting improves referring clinicians’ compre-
whether there was a difference in applications be well equipped to determine whether pa- hension of coronary CT angiography reports. J Am
for exception points between the two groups. tients qualify for MELD exception points. Coll Radiol 2013; 10:432–438
Even if that were not the case, less lofty goals 15. Mazzaferro V, Regalia E, Doci R, et al. Liver
are also worthwhile, such as decreasing trans- References transplantation for the treatment of small hepato-
plant coordinator documentation time to make 1. Health Resources and Services Administration cellular carcinomas in patients with cirrhosis.
it easier for radiologists to prepare or present (HRSA). Organ Procurement and Transplantation New Engl J Med 1996; 334:693–700
(Appendixes start on next page)
772 AJR:210, April 2018
Multiphasic CT Reporting for HCC
APPENDIX 1: Milan Criteria for Liver Transplant for Patients With Hepatocellular Carcinoma
The Milan criteria for patient suitability to undergo liver transplant for hepatocellular carcinoma include the following [15]:
• Single tumor less or equal to 5 cm
• Presence of two to three tumors, none of which exceed 3 cm
• No indication of vascular invasion, extrahepatic manifestations, or both
APPENDIX 2: Standardized Paperwork Required for Placement of Patients on Transplant Waiting List
Figures 5–7 are templates provided by United Network of Organ Sharing (UNOS) for centers to use when recording hepatocellular carci-
noma imaging findings. Documentation of these findings is required by UNOS when applying for model for end-stage liver disease (MELD)
exception points for patients with end-stage liver disease and hepatocellular carcinoma who require placement on a transplant waiting list.
They are not to be submitted with the report, and centers may choose to develop their own documentation methods.
American Journal of Roentgenology 2018.210:766-774.
Fig. 5—Optional reporting template for MRI. OPTN = Organ Procurement Fig. 6—Optional reporting template for CT. OPTN = Organ Procurement
Transplantation Network, SI = signal intensity. © 2018 UNOS. Used with permission. Transplantation Network, SI = signal intensity. © 2018 UNOS. Used with permission.
Fig. 7—Optional summary report template. OPTN = Organ Procurement
Transplantation Network, HCC = hepatocellular carcinoma, MELD = model for end-
stage liver disease. © 2018 UNOS. Used with permission.
AJR:210, April 2018 773
Poullos et al.
APPENDIX 3: Standard Reporting Template for APPENDIX 4: Template for Patients Without Stage T2
Hepatocellular Carcinoma (HCC) Hepatocellular Carcinoma (HCC)
Assessment
LIVER:
LIVER: Morphology:
Cirrhosis: Focal lesions:
Portal hypertension: Hepatic vasculature:
Liver lesions: REMAINING ABDOMEN:
Largest lesion size: Biliary tree:
Lesion location: Gallbladder:
Late arterial hyperenhancement: Spleen:
Portal venous phase washout: Pancreas:
Portal venous phase pseudocapsule enhancement: Adrenal glands:
Delayed phase washout: Kidneys and ureters:
Delayed pseudocapsule enhancement: Gastrointestinal tract:
Tumor thrombus: Peritoneal cavity:
Largest axial dimension: (This does not include the pseudocapsule in Vasculature:
measurement)
Lymph nodes:
Largest CC dimension:
American Journal of Roentgenology 2018.210:766-774.
Abdominal wall:
Contrast phase used for measurement:
Musculoskeletal:
Size on prior study:
IMPRESSION:
Prior study date:
1. Number of HCC lesions:
Infiltrative hepatocellular carcinoma:
2. Largest lesion size:
Portal vein:
3. Findings meet OPTN criteria class:
Superior mesenteric vein:
4. Cirrhotic changes:
Splenic vein:
5. Portal hypertension:
Hepatic venous system:
Note—OPTN = Organ Procurement Transplantation Network.
Hepatic arterial system:
REMAINING ABDOMEN:
Biliary tree:
Gallbladder:
Spleen:
Pancreas:
Adrenal glands:
Kidneys and ureters:
Gastrointestinal tract:
Peritoneal cavity:
Vasculature:
Lymph nodes:
Abdominal wall:
Musculoskeletal:
IMPRESSION:
1. Number of HCC lesions
2. Largest lesion size:
3. Findings meet OPTN criteria class:
4. Cirrhotic changes:
5. Portal hypertension:
Note—CC = craniocaudal, OPTN = Organ Procurement Transplantation Network.
774 AJR:210, April 2018
Das könnte Ihnen auch gefallen
- CT ScanDokument6 SeitenCT ScanqweqweqwNoch keine Bewertungen
- Optimal Image Guided Radiation Therapy Strategy FoDokument6 SeitenOptimal Image Guided Radiation Therapy Strategy FoMariamilllNoch keine Bewertungen
- PDF PHDokument10 SeitenPDF PHWennyNoch keine Bewertungen
- Effect of Visceral Adipose Tissue On The AccuracyDokument8 SeitenEffect of Visceral Adipose Tissue On The AccuracyMaria GoretiNoch keine Bewertungen
- Preoperative Computed Tomography Angiography in Autologous Breast Reconstruction-Incidence and Impact of IncidentalomasDokument6 SeitenPreoperative Computed Tomography Angiography in Autologous Breast Reconstruction-Incidence and Impact of IncidentalomasNora Vianey Alcantara VelascoNoch keine Bewertungen
- J HPB 2016 02 489Dokument2 SeitenJ HPB 2016 02 489hud6427Noch keine Bewertungen
- Jurnal Abdel GawadDokument9 SeitenJurnal Abdel GawadSeptiana meta handayaniNoch keine Bewertungen
- Pancreatic Duct TextureDokument9 SeitenPancreatic Duct TextureAdarsh GhoshNoch keine Bewertungen
- Accuracy of 18FFDG PETCT in Detection and Restaging of Recurrent Ovarian CancerDokument7 SeitenAccuracy of 18FFDG PETCT in Detection and Restaging of Recurrent Ovarian CancerHana SalemNoch keine Bewertungen
- Role of CT Scan in Diagnosis of Acute AppendicitisDokument6 SeitenRole of CT Scan in Diagnosis of Acute AppendicitisIndahNoch keine Bewertungen
- Intensity-Modulated or Conformal Radiotherapy Improves The Quality of Life of Patients With Nasopharyngeal CarcinomaDokument10 SeitenIntensity-Modulated or Conformal Radiotherapy Improves The Quality of Life of Patients With Nasopharyngeal CarcinomaAde Febrian RamadhanNoch keine Bewertungen
- MainDokument8 SeitenMainNurulrezki AtikaNoch keine Bewertungen
- Expert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancerDokument10 SeitenExpert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancermarrajoanaNoch keine Bewertungen
- Characterization of Adrenal Metastatic Cancer Using FDG PET CTDokument8 SeitenCharacterization of Adrenal Metastatic Cancer Using FDG PET CTEngky ChristianNoch keine Bewertungen
- 10 1002@jmri 27182 PDFDokument10 Seiten10 1002@jmri 27182 PDFMădălina MoldovanuNoch keine Bewertungen
- Simultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDokument8 SeitenSimultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDr Shiv ChopraNoch keine Bewertungen
- 1 s2.0 S245210942100097X MainDokument7 Seiten1 s2.0 S245210942100097X MainhidayatullahhaqyaarNoch keine Bewertungen
- PIIS0003497509010868Dokument6 SeitenPIIS0003497509010868Karthik SgNoch keine Bewertungen
- Highres Mri Surgery Early RectalccDokument10 SeitenHighres Mri Surgery Early RectalccCsiszár MártonNoch keine Bewertungen
- P. Wang Et Al.2019Dokument6 SeitenP. Wang Et Al.2019Mai M. AlshalNoch keine Bewertungen
- Zheng Et Al., 2012Dokument6 SeitenZheng Et Al., 2012soledadsaezNoch keine Bewertungen
- Clinical Impact of FDG PET-CT On Management Decisions For Patients With Primary Biliary TumoursDokument10 SeitenClinical Impact of FDG PET-CT On Management Decisions For Patients With Primary Biliary TumourslkitkatgirlNoch keine Bewertungen
- 1 s2.0 S0302283815001578 MainDokument7 Seiten1 s2.0 S0302283815001578 MainyuenkeithNoch keine Bewertungen
- A Prospective Evaluation of Serum Carcinoembryonic Antigen (CEA) Levels in The Management of Colorectal CarcinomaDokument2 SeitenA Prospective Evaluation of Serum Carcinoembryonic Antigen (CEA) Levels in The Management of Colorectal CarcinomaVitjki PramadiNoch keine Bewertungen
- Prognostic Nomogram Predicting Survival of PatientDokument8 SeitenPrognostic Nomogram Predicting Survival of PatienteugeniaNoch keine Bewertungen
- Contemporary Approach To The Diagnosis of Malignant Pleural EffusionDokument8 SeitenContemporary Approach To The Diagnosis of Malignant Pleural EffusionranityaindraNoch keine Bewertungen
- Oncologic Outcomes of Robotic Thyroidectomy: 5-Year Experience With Propensity Score MatchingDokument8 SeitenOncologic Outcomes of Robotic Thyroidectomy: 5-Year Experience With Propensity Score MatchingmawarmelatiNoch keine Bewertungen
- Accuracy of Abbreviated Protocol ofDokument5 SeitenAccuracy of Abbreviated Protocol ofBella YulandaNoch keine Bewertungen
- Management of Neck Mets in HNNDokument9 SeitenManagement of Neck Mets in HNNMuhammad Azeem KhanNoch keine Bewertungen
- Erectile Function After Partial Penectomy For Penile CancerDokument8 SeitenErectile Function After Partial Penectomy For Penile CancerTai rascunhos TaiNoch keine Bewertungen
- 1 s2.0 S1525157821002154 MainDokument13 Seiten1 s2.0 S1525157821002154 MainKanaka K KNoch keine Bewertungen
- Evaluation of FDG PET in Skeletal MetastasesDokument10 SeitenEvaluation of FDG PET in Skeletal MetastaseslkitkatgirlNoch keine Bewertungen
- Improved Outcome by Adding Concurrent Chemotherapy ToDokument9 SeitenImproved Outcome by Adding Concurrent Chemotherapy ToRaul Matute MartinNoch keine Bewertungen
- At TomograpyhDokument9 SeitenAt TomograpyhCarmen BaezNoch keine Bewertungen
- Urological Oncology: A Comparison Between Clinical and Pathologic Staging in Patients With Bladder CancerDokument5 SeitenUrological Oncology: A Comparison Between Clinical and Pathologic Staging in Patients With Bladder CancerAmin MasromNoch keine Bewertungen
- Clinicalinvestigation Non-VascularinterventionsDokument7 SeitenClinicalinvestigation Non-VascularinterventionsSandu AlexandraNoch keine Bewertungen
- Elevated Preoperative Neutrophil To Lymphocyte Ratio Predicts Survival Following Hepatic Resection For Colorectal Liver MetastasesDokument6 SeitenElevated Preoperative Neutrophil To Lymphocyte Ratio Predicts Survival Following Hepatic Resection For Colorectal Liver MetastasesDumitru RadulescuNoch keine Bewertungen
- TouijerDokument7 SeitenTouijerVinko GrubišićNoch keine Bewertungen
- TSWJ2012 731089Dokument9 SeitenTSWJ2012 731089samamansorNoch keine Bewertungen
- Ijss Oct Oa25 PDFDokument5 SeitenIjss Oct Oa25 PDFGonçalo Cunha-CoutinhoNoch keine Bewertungen
- Anticanres 14037Dokument5 SeitenAnticanres 14037Shafa ShaviraNoch keine Bewertungen
- Cross Trial - Preoperative Chemoradiotherapy For Esophageal or Junctional Cancer - Nejm 2012Dokument12 SeitenCross Trial - Preoperative Chemoradiotherapy For Esophageal or Junctional Cancer - Nejm 2012api-308365861Noch keine Bewertungen
- CamamaDokument6 SeitenCamamahbio reparacion y soporteNoch keine Bewertungen
- Tugas Jurnal PK SolDokument6 SeitenTugas Jurnal PK SolSantia LeemNoch keine Bewertungen
- Srep 30353Dokument7 SeitenSrep 30353ErtyWitalayaL.ToruanNoch keine Bewertungen
- Different Styles of IGRTDokument10 SeitenDifferent Styles of IGRTPeter CaldwellNoch keine Bewertungen
- 2010 Article 22Dokument16 Seiten2010 Article 22Andreas KrishnaputraNoch keine Bewertungen
- 10 1111@codi 15424Dokument22 Seiten10 1111@codi 15424yongky sugandaNoch keine Bewertungen
- Radiotherapy and Oncology: Brachytherapy of Cervical CancerDokument8 SeitenRadiotherapy and Oncology: Brachytherapy of Cervical CancerodivarNoch keine Bewertungen
- 33Dokument11 Seiten33Joana KellenNoch keine Bewertungen
- Head and Neck Surgery: Pressure Ulcer Prevention Strategies in Prolonged SurgeryDokument2 SeitenHead and Neck Surgery: Pressure Ulcer Prevention Strategies in Prolonged SurgeryBenny KurniawanNoch keine Bewertungen
- JurnalDokument4 SeitenJurnalBIntangsinagaNoch keine Bewertungen
- Abstract 2015 in Surgery PDFDokument281 SeitenAbstract 2015 in Surgery PDFDrAmmar MagdyNoch keine Bewertungen
- Prostate Cancer Detection Rate in Indonesian MenDokument7 SeitenProstate Cancer Detection Rate in Indonesian MenYusuf RachmanNoch keine Bewertungen
- Abstracts From The Global Embolization Sympo 2021 Journal of Vascular and inDokument21 SeitenAbstracts From The Global Embolization Sympo 2021 Journal of Vascular and infreedy freedyNoch keine Bewertungen
- Abdominoperineal Resection For Squamous Cell Anal Carcinoma: Survival and Risk Factors For RecurrenceDokument8 SeitenAbdominoperineal Resection For Squamous Cell Anal Carcinoma: Survival and Risk Factors For RecurrenceWitrisyah PutriNoch keine Bewertungen
- Analysis of The Risk Factors of Untransplantable Recurrence After Primary Curative Resection For Patients With Hepatocellular CarcinomaDokument8 SeitenAnalysis of The Risk Factors of Untransplantable Recurrence After Primary Curative Resection For Patients With Hepatocellular CarcinomaJoão Gabriel Ferreira ArgondizziNoch keine Bewertungen
- Austin Journal of Nuclear Medicine and RadiotherapyDokument5 SeitenAustin Journal of Nuclear Medicine and RadiotherapyAustin Publishing GroupNoch keine Bewertungen
- Tumor Liquid BiopsiesVon EverandTumor Liquid BiopsiesFlorence SchaffnerNoch keine Bewertungen
- Biliopancreatic Endoscopy: Practical ApplicationVon EverandBiliopancreatic Endoscopy: Practical ApplicationKwok-Hung LaiNoch keine Bewertungen
- Ent OpdDokument5 SeitenEnt OpdRenz Marion AlemaniaNoch keine Bewertungen
- Positron Emission Tomography in The Diagnostic Work-Up of Screening-Detected Lung NodulesDokument10 SeitenPositron Emission Tomography in The Diagnostic Work-Up of Screening-Detected Lung NodulesRenz Marion AlemaniaNoch keine Bewertungen
- Functional Recovery After Rehabilitation For Cerebellar StrokeDokument5 SeitenFunctional Recovery After Rehabilitation For Cerebellar StrokeRenz Marion AlemaniaNoch keine Bewertungen
- Aleluya Verse 12, 13, 14Dokument1 SeiteAleluya Verse 12, 13, 14Renz Marion AlemaniaNoch keine Bewertungen
- How Great Thou ArtDokument8 SeitenHow Great Thou ArtRenz Marion AlemaniaNoch keine Bewertungen
- Stay With Me Lord Ferdzmb SATB LAOmmxviii PDFDokument2 SeitenStay With Me Lord Ferdzmb SATB LAOmmxviii PDFRenz Marion AlemaniaNoch keine Bewertungen
- Mary Did You Know PDFDokument7 SeitenMary Did You Know PDFRenz Marion AlemaniaNoch keine Bewertungen
- On Bended Knee Boyz II Men PDFDokument9 SeitenOn Bended Knee Boyz II Men PDFRenz Marion AlemaniaNoch keine Bewertungen
- European Journal of Pharmaceutical and Medical ResearchDokument17 SeitenEuropean Journal of Pharmaceutical and Medical ResearchRenz Marion AlemaniaNoch keine Bewertungen
- Guía Clínica HTA 2011Dokument310 SeitenGuía Clínica HTA 2011marcelagarciavNoch keine Bewertungen
- Nervous System Brain Retina - QDokument70 SeitenNervous System Brain Retina - QVarshLokNoch keine Bewertungen
- Coliform Analysis in Wastewater 2012Dokument24 SeitenColiform Analysis in Wastewater 2012engrbvgNoch keine Bewertungen
- Vishal Sachan: Current Address: Permanent AddressDokument4 SeitenVishal Sachan: Current Address: Permanent Addressvishal sachanNoch keine Bewertungen
- Cognitive Behavioral Guided Self Help For The Treatment Od Recurrent Binge EatingDokument19 SeitenCognitive Behavioral Guided Self Help For The Treatment Od Recurrent Binge EatingIsmael RodriguezNoch keine Bewertungen
- LCB ResponseDokument13 SeitenLCB ResponseLas Vegas Review-JournalNoch keine Bewertungen
- Students Choose Life Stand On The RH BillDokument1 SeiteStudents Choose Life Stand On The RH BillCBCP for LifeNoch keine Bewertungen
- Sample Written Program For Respiratory ProtectionDokument45 SeitenSample Written Program For Respiratory ProtectionSergio MacedoNoch keine Bewertungen
- Katrina D. Varon Bs-Nursing 2Dokument13 SeitenKatrina D. Varon Bs-Nursing 2Marc FresNoch keine Bewertungen
- Patient AssesmentDokument18 SeitenPatient AssesmentMarian Ioan-LucianNoch keine Bewertungen
- Daftar Pustaka-1Dokument4 SeitenDaftar Pustaka-1Ismi OktaNoch keine Bewertungen
- DSWD Guidelines For Residential FacilitiesDokument12 SeitenDSWD Guidelines For Residential FacilitiesCharlene Ordoñez Dela CruzNoch keine Bewertungen
- Kansas Foodborne Illness ManualDokument186 SeitenKansas Foodborne Illness ManualLeo M. Pedro Jr.Noch keine Bewertungen
- PR Ke-2Dokument2 SeitenPR Ke-2Maulia IsnainiNoch keine Bewertungen
- AOS Injury Classification Systems Poster THORACOLUMBARDokument1 SeiteAOS Injury Classification Systems Poster THORACOLUMBARWilliams Maita GallardoNoch keine Bewertungen
- Menstrual DisordersDokument45 SeitenMenstrual DisordersMegat Mohd Azman Adzmi100% (1)
- Sieff D.F. 2017 Trauma Worlds and The Wisdom of Marion Woodman AuthorsDokument18 SeitenSieff D.F. 2017 Trauma Worlds and The Wisdom of Marion Woodman AuthorsMelissa Viana100% (1)
- PMJJBYDokument1 SeitePMJJBYArun PaiNoch keine Bewertungen
- Drugs For Cough: DR - Vijay BhushanamDokument14 SeitenDrugs For Cough: DR - Vijay Bhushanamheka_amrongNoch keine Bewertungen
- Oplan Kalusugan Sa DepEd SY 2019Dokument4 SeitenOplan Kalusugan Sa DepEd SY 2019Klaribelle Villaceran100% (1)
- John Kerr BDokument3 SeitenJohn Kerr BRex Loren de LeonNoch keine Bewertungen
- Discharge Planning: MedicationDokument3 SeitenDischarge Planning: MedicationLeasNoch keine Bewertungen
- Research Sa Chem Trabaho'a Na!Dokument14 SeitenResearch Sa Chem Trabaho'a Na!NoellhaJeanetteGabeLiwagonNoch keine Bewertungen
- Name Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailDokument8 SeitenName Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailshrutiNoch keine Bewertungen
- Chapter 4 Marketing Department: Company 1-Apollo Hospitals Enterprises LTD (Apollo)Dokument20 SeitenChapter 4 Marketing Department: Company 1-Apollo Hospitals Enterprises LTD (Apollo)TYB92BINDRA GURSHEEN KAUR R.Noch keine Bewertungen
- Ovarian CancerDokument71 SeitenOvarian CancerAyuni SallehNoch keine Bewertungen
- Second M.B.B.S Degree Examination, 2011 207. Forensic MedicineDokument3 SeitenSecond M.B.B.S Degree Examination, 2011 207. Forensic MedicineBalaKrishnaNoch keine Bewertungen
- Investigations in Rheumatology: What's New?Dokument10 SeitenInvestigations in Rheumatology: What's New?i can always make u smile :DNoch keine Bewertungen
- Pain Management: Dr. Prabowo Wicaksono Span Bagian/Smf Anestesi FK Unissula/Rsisa 2007Dokument27 SeitenPain Management: Dr. Prabowo Wicaksono Span Bagian/Smf Anestesi FK Unissula/Rsisa 2007Fendy PrasetyoNoch keine Bewertungen
- Water and Electrolyte Balance Case StudyDokument3 SeitenWater and Electrolyte Balance Case Studyzamadula100% (3)