Beruflich Dokumente
Kultur Dokumente
Adhesive Capsulitis
Hochgeladen von
GumDropCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Adhesive Capsulitis
Hochgeladen von
GumDropCopyright:
Verfügbare Formate
Review article
Treatment of adhesive capsulitis: a review
Giovanni Maria D’Orsi1, diological appearance. In 1945 Neviaser defined this condi-
Alessio Giai Via2, tion “Adhesive capsulitis” in order to underline the inflam-
Antonio Frizziero3, matory pathogenesis and fibrosis4. Later histologic studies
Francesco Oliva2 confirmed the presence of fibroblasts and chronic inflamma-
tory cells which seep in joint capsule of the shoulder.5 The
1
Department of Rehabilitation and Functional Recovery, current consensus definition of the American Shoulder and
San Giovanni Bosco Hospital, Via F.M. Brignati 255, Naples, Elbow Surgeons is: “condition of uncertain etiology charac-
Italy - Department of Physical Medicine and Rehabilitation, terized by significant restriction of both active and passive
Second University of Naples, P.zza Miraglia 2, Naples, Italy shoulder motion that occurs in the absence of a known in-
2
Department of Orthopaedics and Traumatology, University trinsic shoulder disorder”6,7.
of Rome “Tor Vergata” School of Medicine, Viale Oxford 81, AC occurs in 2% to 5% of the population8. It is more frequent
Rome, Italy in women aged between 40 and 60 years9 and in about 20-
3
Department of Orthopaedic Rehabilitation, University of 30% of cases this condition is bilateral7. Many pathologi-
Padova, Via Giustiniani 2, Padova, Italy cal disorders can be associated with AC as diabetes mel-
litus10,11, thyroid dysfunctions12,13, Dupuytren contracture14,
cardiorespiratory and autoimmune diseases15. Predisposing
Corresponding author: conditions have been investigated as prolonged shoulder
Alessio Giai Via immobility secondary to trauma or surgery, cardiovascular
Department of Orthopaedics and Traumatology, University disease and Parkinson’s disease3,6. There are also evidenc-
of Rome “Tor Vergata” School of Medicine, es that protease inhibitors used for antiretroviral therapy
Viale Oxford 81, Rome, Italy have been associated with the development of AC7.
Tel: +39 339 6298768 AC has been classified as primary and secondary. Primary
e-mail: alessiogiaivia@virgilio.it AC is characterized by global capsular inflammation and fi-
brosis which occurs without any known precipitating cause.
Secondary AC instead includes many conditions causing
shoulder stiffness, such as calcific tendinopathy (CT), rota-
Summary tor cuff tears (RCT), glenohumeral or acromion-clavicular
arthritis and previous shoulder trauma or surgery16,17. It is
Adhesive capsulitis is a condition “difficult to define, very important to identify these disorders because the treat-
difficult to treat and difficult to explain from the point ment will be addressed to sorted out the primary cause be-
of view of pathology”. This Codman’s assertion is still fore treating stiffness.
actual because of a variable nomenclature, an incon- Even the natural history of AC is still debated in the litera-
sistent reporting of disease staging and many types ture. Primary AC is usually a self-limited pathology which
of treatment. There is no consensus on how the best resolves spontaneously by two to four years18, but some
way best to manage patients with this condition, so we Authors described functional limitations, persistent pain and
want to provide an evidence-based overview regarding weakness at long time follow-up19,20.
the effectiveness of conservative and surgical interven- Neviaser et al.21 and Hannafin et al.22 identified 4 stages of
tions to treat adhesive capsulitis. this condition, which have been correlated with clinical ex-
amination and histological features (Tab.1). The first stage
Key words: adhesive capsulitis, frozen shoulder, review, is the painful phase, which is characterized by a gradual
conservative treatment. onset of symptoms. Symptoms persists for less than 3
months and consist of an aching pain referred to the del-
toid insertion and inability to sleep on the affected side. Pa-
Introduction tients may report a mild limitation of ROM which invariably
resolves with the administration of local anesthetic. The ar-
Primary adhesive capsulitis (AC) is a shoulder condition throscopic view, confirmed by biopsies, shows an hypertro-
characterized by a gradual and painful loss of both active phic, vascularized synovitis without adhesions or capsular
and passive range-of-motion (ROM) in all planes of gleno- contracture. The second stage is also called the “freezing
humeral joint, especially external rotation1, resulting from stage”23. Symptoms continues since 3 to 9 months and are
progressive fibrosis and contracture of the glenohumeral characterized by nocturnal pain moreover when the patients
joint capsule. Duplay2 in 1872 was the first author who de- lying on the affected side, furthermore a significant loss of
scribed this condition as “periarthritis”. In 1934 Codman3 both active and passive ROM is referred. Arthroscopic view
used the term “Frozen shoulder” to define a gradually de- shows a thickened ipervascular synovitis. Histology shows
veloping condition, characterized by pain near the deltoid perivascular and subsynovial scar formation with deposition
insertion, inability to sleep on the affected side, painful and of disorganized collagen fibrils and a hypercellular appear-
restricted elevation and external rotation and a normal ra- ance, but no inflammatory infiltrates have been found. In
70 Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78
Treatment of adhesive capsulitis: a review
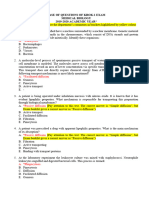
Table 1. Clinical and histological stages of AC.
STAGE SYMPTOMS
LENGTH OF
SYMPTOMS
HISTOLOGICAL
FEATURES
pear to provide significant short-term benefits in pain relief,
Aching pain and
ROM and function but the effect may not be maintained be-
Painful phase moderate limitation of Less than 3 months
Synovitis and capsular
hypertophy
yond six weeks.
ROM
Ipervascular synovitis.
Freezing stage
Severe pain and
reduction of ROM
3 to 9 months Disorganized Collagen Intra-articular steroid injections
Stiffness is
deposition
Dense and
Intra-articular corticosteroid injection are widely used for
Frozen stage predominant. Pain may 9 to 14 months hypercellular AC. Intra-articular corticosteroid injection has showed to
be present. collagenous tissue
Minimal pain and a Not investigated.
provide faster improvement compared to oral route32. All
Thawing stage gradual improvement 15 and 24 months patients were submitted to active exercise and passive joint
of ROM
mobilization treatment. Unluckily the small number of pa-
Table 1. Clinical and histological stages of AC. tients and the short follow up is the limitation. Lorbach et
al.33 compared intra-articular injections of glucocorticoids
stage number 3, the “frozen stage”23, symptoms persists with oral corticosteroids in a well conduced prospective
since 9 to 14 months. The shoulder stiffness is predominant RCT. All patient started, four weeks after the first cortico-
and pain may still be present at the end of motion or at night. steroid administration, an exercise program supervised by
Arthroscopic examinations demonstrates patchy synovial a physiotherapist twice a week and home exercise twice a
thickening and loss of axillary recess; biopsy shows dense, day within a pain-free ROM. They concluded that the use of
hypercellular collagenous tissue. The last stage is the corticosteroids in the treatment of AC led to fast pain relief
“thawing stage”23. It is characterized by minimal pain and a and improved ROM, and that intra-articular injections of glu-
gradual improvement of ROM due to capsular remodeling. cocorticoids showed superior short-term results compared
This stage occurs between 15 and 24 months. Arthroscopic to oral corticosteroids. Three high quality RCTs34-36 com-
and histological correlation has not been investigated. pared steroid injections with placebo, supervised physio-
The diagnosis of AC is usually clinical. X-ray of the shoulder therapy and intra-articular sodium hyaluronate injection. All
reveals no pathological changes, but they are important to trials showed significant benefit of intra-articular injections
exclude other causes of shoulder pain such as CT, gleno- on pain and shoulder disability at short term follow-up. No
humeral or acromion-clavicular osteoarthritis. Sometimes differences were found beyond 3 months between treat-
osteopenia of disuse can be observed. Magnetic resonance ments. The combination of steroid injection with physiother-
imaging (MRI) and MR arthrography may show thickening of apy appeared more effective than physiotherapy or steroid
the coraco-humeral ligament and joint capsule in the rotator injections alone in the recovery of ROM.
interval, loss of axillary recess, obliteration of subcoracoid
fat (subcoracoid triangle sign) which are characteristic find- Sodium hyaluronate intra-articular injection
ings in AC24. Despite their value these imaging techniques Sodium hyaluronate injection into the glenohumeral joint
are not initially indicated to diagnose AC, but they can be appear to be an increasing therapeutic option. Its effective-
used to rule out other intra-articular pathology. ness has been investigated in three RCTs34,37,38. A system-
atic review
21 of Literature39 published in 2011, showed that
intra-articular sodium hyaluronate injection significantly
Treatment improves pain and ROM at short-term follow-up, and a
statistically significant improvement of Constant-Murley
There is no consensus regarding the best treatment for AC. Scores (CMS) was also found. Isolated intra-articular hy-
Many different conservative treatments and invasive proce- aluronate injection has significantly better outcomes than
dures have been described (Tab. 2 and 3). The recognition control, while it showed equivalent outcomes compared to
of the clinical stage of disease must to be addressed in the intra-articular corticosteroid injection, but with fewer side ef-
way to decide the kind of treatment required. fects. Rovetta et al.37 compared patient treated with intra-
articular injections of sodium hyaluronate plus steroid and
Nonsteroidal anti-inflammatory drugs (NSAIDs) exercise to patients treated with intra-articular corticosteroid
Despite their widespread use, there is no evidence in litera- injections alone and exercises. They found better results in
ture to support the effectiveness of NSAIDs for the treat- treatment group than control. Moreover intra-articular hyal-
ment of AC. A systematic review of the literature showed uronate injection seems to have chondroprotection property
significant improvement of symptoms in patients treated and improve the quality of the synovial fluid40.
with NSAIDs compared with placebo25. But the scientific Mobilization and physiotherapy
quality of the studies analyzed provides questionable clini- The first prospective RCT was performed by Bulgen et al.41
cal evidence. The use of NSAIDs at earlier inflammatory in 1984. Forty-two patients were divide into four groups, and
stages of the disease may provide short-term pain relief26,27. the Authors assessed the effect of mobilization (11 patients),
mobilization and ice- pack (12 patients), intra-articular cor-
Oral steroid treatment ticosteroid injection (11 patients) and no treatment (8 pa-
Four randomized controlled trials (RCT) have been identi- tients). They found just a few differences between patients
fied in literature28-31. The last was performed by Buchbinder treated with physiotherapy and no treated controls. More
et al.31 in 2004. The authors compared a short course of recently Griggs et al.42 concluded that patients with phase-
prednisolone to placebo concluding that oral steroids ap- II idiopathic AC can be treated successfully with shoulder-
Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78 71
A. Giai Via et al.
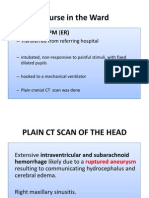
TableTab.2: Studies
2. Studies of conservative
of conservative treatment fortreatment
AC. for AC.
Level of Number of
Authors Year Study Management Follow-up Results
evidence shoulders
Buchbinder
31 2004 RCT II Prednisolone vs. placebo 50 12 weeks Good
et al.
Widiastuti- Intraarticular steroid injection and
samekto et 2004 RCT II physiotherapy vs. oral steroid and 26 2 weeks Excellent
32 physiotherapy
al.
Sodium hyaluronate injection vs.
34
Calis et al. 2006 RCT I intraarticular steroid injection and 95 3 months Poor
physical therapy
Intraarticular corticosteroid injection
Carrete et and physiotherapy vs intraarticular
35 2003 RCT II 93 12 moths Good
al. corticosteroid injection alone,
physiotherapy alone and placebo
Intraarticular corticosteroid injection
and physiotherapy
36
Ryans et al. 2005 RCT II intraarticular corticosteroid injection 78 16 weeks Excellent
alone, placebo injection and
physiotherapy, placebo
Lorbach et Oral corticosteroids vs. intraarticular
33 2010 RCT II 40 12 moths Excellent
al. corticosteroid injection
Intraarticular sodium hyaluronate and
Rovetta et
37 1998 RCT II corticosteroid injection vs corticosteroid 30 6 months Good
al. injection
Takagishi et Intraarticular sodium hyaluronate vs
38 1996 RCT II 20 5 weeks Good
al. corticosteroid injection
Bulgen et Intraarticular corticosteroid injection,
41 1984 RCT II 42 8 months Poor
al. mobilization, ice therapy, placebo
Prospective
42
Griggs et al. 2000 not III Supervised stretching-exercise program 77 22 months Good
randomized
Tanaka et joint mobilization and home self-
47 2010 RCT II 120 24 months Excellent
al. exercise
Prospective
Dicrkes et Intensive physiotherapy vs. gentle
43 2004 not III 77 24 months Poor
al. physiotherapy
randomized
Vermeulen High-grade mobilization techniques vs
44 2006 RCT II 100 12 months Good
et al. gentle mobilization techniques
Johonson et Anterior vs posterior glide mobilization Not
45 2007 RCT I 20 Excellent
al. technique reported
49 low-power laser therapy (LLLT) vs
Stergioulas 2008 RCT II 63 16 weeks Good
placebo
Deep heating plus stretching vs
50
Leung et al. 2008 RCT II superficial heating plus stretching or 30 4 weeks Excellent
stretching exercises alone
51 Supivacaine suprascapular nerve block
Dahan et al. 2000 RCT II 34 1 month Poor
vs placebo
52 Suprascapular nerve block vs intra-
Jones et al. 1999 RCT I 30 12 weeks Good
articular corticosteroids
Buchbinder Arthrographic distension with saline and
55 2004 RCT I 48 3 months Good
et al. corticosteoird vs placebo
TENS and infra-red radiation alone vs
56
Khan et al. 2005 RCT I physical therapies and intra-articular 40 8 weeks Good
corticosteroids
72 Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78
22
Treatment of adhesive capsulitis: a review
Jacobs et Distension only vs, steroid only or
1991 RCT II 47 3 months Poor
Table 2.
al.Studies of conservative treatment for AC.
57
steroid with distension
Arthrographic distension and
Corbeil et
Jacobs 58 et 1992 RCT II corticosteoird
Distension onlyvsvs,
nondistensive
steroid only or 45 3 months Poor
al.57 1991 RCT II arthrography and corticosteoird
47 3 months Poor
al. steroid with distension
59 Arthrographic distension
vs steroidand
Gam et al.
Corbeil et 1998 RCT II Distension and steroid alone 22 12 weeks Good
58 1992 RCT II corticosteoird vs nondistensive 45 3 months Poor
al. arthrography and corticosteoird
Kiwimaki
60 2007 RCT II MUA vs exercise program 125 12 months Poor
et et
Gam al. al.59 1998 RCT II Distension and steroid vs steroid alone 22 12 weeks Good
Quaraishi
Kiwimaki61 2007 RCT I MUA vs hydrodilatation 36 6 months Poor
et al.60 2007 RCT II MUA vs exercise program 125 12 months Poor
et al.
63
Farrel et al.
Quaraishi 2005 Case series III MUA 26 15 years Excellent
61 2007 RCT I MUA vs hydrodilatation 36 6 months Poor
et al.
63
Farrel et al. 2005 Case series III MUA 26 15 years Excellent
Table 3. Studies of operative treatment for AC.
Tab.3: Studies of operative treatment for AC.
Level of Number of
Authors Year Study Management Follow-up Results
evidence shoulders
Tab.3: Studies of operative treatment for AC.
Baums et Retrospective
68 2007 V Arthroscopic release 30 2 years Good
al. study
Level of Number of
Authors Year Study
Retrospective Management Follow-up Results
69
evidence Arthroscopic release in idiopathic shoulders
Cinar et al. 2010 comparative III 28 5 years Good
Baums et Retrospective AC vs diabetic AC
68 2007 study V Arthroscopic release 30 2 years Good
al. study
Retrospective
Ogilvie-Harris Retrospective
71 69 1995 comparative III Arthroscopicrelease
Arthroscopic releaseinvsidiopathic
MUA 40 5 years Excellent
et al.
Cinar et al. 2010 comparative III 28 5 years Good
study AC vs diabetic AC
study
Retrospective
Retrospective Anterior and inferior arthroscopic
Ogilvie-Harris
72 comparative No
Snow et71al. 2009
1995 comparative IIIIII capsular release
Arthroscopic vs posterior
release vs MUA 4840 5 months
5 years Excellent
et al. study difference
study release
Retrospective
73 Retrospective Anterior and inferior arthroscopic
Ozaki et al.72 1989 comparative IV Open release 17 7 years GoodNo
Snow et al. 2009 study III capsular release vs posterior 48 5 months
study difference
release
stretching exercises Retrospective with both treatment strategies and only a minority of out-
1989program. Furthermore stretching exer-
73
Ozaki et al. IV Open release 17 7 years Good
cises should be continued forstudythree months, after that more come measures reached statistical significance. Johnson et
aggressive physiotherapy or invasive management should al. compared anterior versus posterior glide mobilization.
45
be considered. They concluded that a posteriorly directed joint mobilization
The frequency and the technique with which the mobiliza- technique was more effective than an anteriorly directed
tion should be performed is still debated. In a level III study, mobilization technique for improving external rotation after
Diercks et al.43 compared intensive physical therapy pro- three treatment sessions. A retrospective cohort study46 of
gram, including active and passive exercises with stretching more than 2.000 patients affected by AC found that both
beyond the pain threshold to exercises within the pain limits. manual shoulder mobilization techniques and self-exercise
They found that exercises within the pain limits was supe- like stretching and home programs are effective for the
rior than intensive physical therapy and passive stretching treatment of AC. Self-exercises twice47 daily appeared in-
with regard to functional outcome and speed of recovery. In stead superior than shoulder mobilization by a physiothera-
fact 89% of patients treated with exercises within the pain pist twice a week.
limits reached a Constant score of 80 or higher compared The efficacy of physiotherapy interventions for shoulder
to 63% of patients treated with intensive physical therapy. pain and dysfunction have been evaluated by a Cochrane
In contrast, Vermeulen44 found that high-grade mobilization Review48. Unfortunately many pathologies of the shoulder
technique was more effective than low-grade mobilization such as rotator cuff tears, calcific tendinopathy, AC, ante-
technique (within the pain limits) in increasing mobility and rior gleno-humeral instability have been considered. Laser
functional ability. However all patients improved significantly therapy was demonstrated to be more effective than pla-
Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78 73
23
A. Giai Via et al.
cebo for AC48. It was confirmed more recently by Stergiou- distension and injection regard pain and ROM. Only one
las49. Low-level laser treatment seemed to be more effective study59 reported significant improvement in range of motion
than placebo respect to pain but not respect to ROM. So the and lowered analgesic use in the arthrographic distension
Author concluded than lower-level laser therapy did not af- group, but no difference in pain or function between groups.
fect the underlying capsular pathology and adhesion. Leung
et al.50 conducted a RCT which demonstrate that addition Mobilization under anesthesia (MUA)
of deep heating to stretching exercises produces a greater MUA is commonly used when conservative treatments have
improvement in pain relief, and leads to improved perfor- failed, but its effectiveness for the treatment of AC is contro-
mance in daily living activities and in range of motion, more versial. Kivimäki60 examined the effect of MUA in patients
than superficial heating. However there is no evidence that with adhesive capsulitis in a blinded randomized trial with
physiotherapy alone is of benefit for AC48. Ultrasound, mas- a 1-year follow-up. In this study MUA was compared to a
sage, iontophoresis, and phonophoresis not only seems to home exercise program. They found no differences be-
be no effective for the treatment of AC, but they seems to tween these two treatment options in terms of shoulder pain
reduced the likelihood of a favorable outcome. So their use or working ability. Small differences in the range of motion
have been discouraged by some Authors46. were detected favoring the manipulation group at 3 months
follow up, but this was not sustained at 6 months and 12
Suprascapular nerve block months. Quraishi et al.61 assessed the outcome of MUA and
The suprascapular nerve provides nerve supply to muscles hydrodilation in 36 patients with adhesive capsulitis. The
of the shoulder girdle, and to the shoulder joint. Local an- VAS and the Constant score of control group were signifi-
aesthetic blocks of suprascapular nerve are used to treat cantly better than those of MUA group at 6-month follow-up.
painful shoulder conditions such as adhesive capsulitis. On the other side, Dodenhoff et al.62 showed that manipu-
A double-blinded randomised controlled trial51 compared lation under anesthesia can provide early improvement of
three suprascapular blocks with bupivacaine at weekly in- shoulder function and that it is generally a safe procedure.
tervals with placebo. Suprascapular nerve block gave sig- They prospectively assessed 39 shoulders in 37 patients
nificantly more pain relief than placebo at 1 month follow-up. who were diagnosed with primary adhesive capsulitis. Far-
No improvement in ROM was noted. This study present also rell et al.63 reported excellent results in 70% of patients treat-
several limitations, as the high dropout rate and the short- ed with MUA at 15 years follow up, but the limitations of this
term follow-up. Therapeutic effects of suprascapular nerve study were the small sample and the high percentage of
blocks were compared to intra-articular corticosteroid injec- patients lost at follow-up.
tions by Jones et al.52 They found a statistical significant There is no consensus also about the safety of MUA be-
improvement in both groups, but case group showed better cause many iatrogenic lesions have been reported. Hemar-
results regarding pain relieve and ROM at 3 months follow- throsis, capsular tears, glenioid labral detachments, SLAP
up. The authors concluded that suprascapular nerve block lesions, glenohumeral ligament ruptures, rotator cuff’s ten-
could be used in primary care with good results. The stan- don tears, humeral neck fracture and glenoid fracture have
dard suprascapular nerve block technique using needle tip all been reported64,65. Actually there is no evidence that MUA
guided by superficial bony landmarks was compared with is better than daily mobilization exercises66. Moreover, MUA
suprascapular blocks administered under the guidance of should not be used in case of history of fracture or disloca-
electromyography53. After one hour, the electromyography tions, moderate bone loss, and in patients with adhesive
technique produced significantly more pain relief and better capsulitis associated with insulin-dependent diabetes67.
range of motion than the standard technique. Ultrasound- Poor outcomes and frequent recurrences have been report-
guided placement of a perineural catheter to provide contin- ed in patient with diabetes after MUA61.
uous suprascapular nerve block have also been proposed
in a case report54. The continuous nerve block catheter al- Arthroscopy
lowed pain relieve and to start a mobilization program. Many studies confirmed the effectiveness of arthroscopy in
Arthrographic distension treatment of recalcitrant adhesive capsulitis. Baums et al.68
Arthrographic distension is a procedure based on the injec- in a prospective study showed a great improvement in pain,
tion of a saline solution or corticosteroids into the shoulder ROM and shoulder function in patients with resistant ad-
joint to break up the adhesions that might limiting the move- hesive capsulitis treated with arthroscopic release. Cinar et
ment of the shoulder and causing disability. Buchbinder et al.69 compared results of arthroscopic capsular release in
al.55 compared arthrographic distension with steroid and sa- patients with primary AC to patients with AC and insulin-de-
line versus placebo. Case group had significantly greater pendent diabetes. They confirmed the effectiveness of pro-
improvement at three weeks follow up compared to partici- cedure in both groups but the diabetic patients had poorer
pants in the placebo group regarding ROM, pain and dis- results in terms of ROM and Constant Score. Elhassan et
ability. Another RCT compared arthrographic distension with al.70 showed that patients with idiopathic and post-traumatic
steroid and saline associated with physical therapy to physi- shoulder stiffness have better outcomes than patients with
cal therapy alone56. Distension followed by physiotherapy postsurgical stiffness. In a level III study Ogilvie-Harris et
was more effective than physiotherapy alone to reduce pain al.71 compared arthroscopic release with MUA. They stated
and improve ROM at 8 weeks. Three RCT compared disten- that arthroscopic release has supplanted MUA as treatment
sion with corticosteroid injections. Two of these, conducted of choice for resistant adhesive capsulitis because it en-
by Jacobs57 and Corbeil,58 reported no difference between sures more significant and rapid improvements in motion
74 Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78
Treatment of adhesive capsulitis: a review
and pain with lower risk of complications. treated non-surgically first. In the first stage of the disease
It is unclear the extent in which capsule should be released provocative activities should be avoided. For pain control
and which structures should be involved in release. Many NSAIDs, opioids or steroid/hyaluronate intra-articular injec-
authors release only the rotator cuff interval and the con- tions have been used. In case of loss of motion, a stretching
tracted coracohumeral ligament with excellent results. The program, pendulum motions, active-assisted and passive
aim of recent study72 was to assess the overall effective- mobilizations have been used to restore joint mobility. Fi-
ness of arthroscopic capsular release and to determine if nally muscle strengthening exercises were performed.
the combination of anterior and posterior capsular release
had more benefit than only anterior release. The authors
showed that a more extensive release is not related with a Discussion
greater improvement in ROM. However further studies are
necessary. The goal of this study was to provide an overview concern-
ing evidence for the effectiveness of interventions to treat
Open release AC. Unfortunately there is no consensus about the manage-
Many studies have confirmed the effectiveness of the open ment of this pathology and it probably depends on the lack
release in treatment of resistant AC. Ozaki et al.73 performed of high level study.
open release in 17 patients who had recalcitrant chronic AC. NSAIDs are widely prescribed for the treatment of AC, even
They found that the main cause of restricted glenohumeral if there is a lack of evidence to support their effectiveness.
movement was the contracture of coracohumeral ligament They can be used during early inflammatory stage to pro-
and rotator interval. Release of contracted structures re- vide short-term pain relief, but more research is needed to
lieved pain and restored motion of the shoulder in all pa- assess their role. Oral steroids appear to provide significant
tients. short-term benefits but their effect may not be maintained
beyond six weeks. Furthermore treatment with oral steroids
Rehabilitation protocols for a long period involves long-term systemic side effects.
Many treatment options for AC have been reported but A valid alternative is represented by intra-articular steroid
there is no consensus on the best management. Although injections. They seem to provide better results than oral ste-
these methods appear effective they have not been tested roid treatment33 with lower risk of side effects. Intra-articular
with class I studies. injections may be more efficacious in the early stages of
Neviaser and Hannafin proposed a stage based treatment disease when the inflammatory processes are predominant
protocol in their review74. In the first stage the goal of therapy and there is not a significant capsular contracture. However
is the control of inflammation and the relief of pain. This can this finding has yet to be proven with higher level studies.
be obtain with an intrarticular steroid injection mixed with There is evidence for the effectiveness of intra-articular
lidocaine, cryotherapy, TENS. Education, activity modifica- steroid injections for pain in the short term and moderate
tion and gentle range of motion exercises are prescribed. evidence in the medium term. There is no evidence for its
In stage 2 it is important to minimize capsular adhesions effectiveness on ROM, and no differences were found also
and restrictions of motion with passive joint glide, home ex- between steroid injections and manipulation78. A small num-
ercises and active exercises in the plane of the scapula. In ber of RCTs of sodium hyaluronate intra-articular injection
stages 3 and 4 the aim is to treat the marked loss of mo- are published in literature. It seems to provide a significant
tion and abnormal scapulohumeral mechanism. Aggressive improvement in pain severity and a significant benefit on
stretching is the cornerstone of the therapy in this phase. function and disability79. Unfortunately there is insufficient
As the ROM is restored, the strengthening of the rotator evidence to make conclusion about the effectiveness of
cuff muscles begins. Patients who have failed nonoperative sodium hyaluronate injection for the treatment of AC and
treatment were submitted to arthroscopy capsulotomy. The further studies are needed. Mobilization and physiotherapy
posterior capsule is included in the release. At the end of are often prescribed to prevent capsular contracture and im-
procedure they perform a manipulation to assure adequate prove shoulder range of motion. Gentle stretching and home
release. Also Favejee75 think that treatment should be based exercise program within the pain threshold seem to provide
on the stage of the pathology and they proposed a similar better results than more intensive mobilization programs,
therapeutic algorithm. Kelley et al.76 consider extremely im- even if there insufficient evidence to make conclusions
portant to verify the patient’s irritability before deciding on about the most effective physiotherapy79. Regarding physi-
treatment. Patients with high irritability should be treated cal therapy, there is a good evidence for the effectiveness of
with short-duration, relatively pain free stretching and low laser therapy and deep heating especially if applied as ad-
grade joint mobilization to avoid exacerbation of pain and in- juvant to other treatment modalities like mobilization tech-
flammation. The use of intra-articular steroid injection helps niques or exercise programs9. Suprascapular nerve block
to turn off the inflammatory process. As the level of irrita- seems to be useful to reduce pain in the short and mid-term
bility is reduced, more intense stretching and mobilizations follow-up compared with acupuncture, placebo or steroid in-
near the end range can be performed. Patients who have jections78. Hydrodilatation of shoulder joint has been recom-
recalcitrant symptoms and disabling pain may respond to mend by some Authors for patients with adhesive capsulitis
manipulation under anesthesia or arthroscopic release. In resistant to conservative treatment61. It seems to provide
2005 Iannotti et al.77 proposed an algorithm to diagnose and better results and lower risk compered to MUA. However
treat adhesive capsulitis. They proposed that AC should be few RCTs are published in Literature and they involved few
Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78 75
A. Giai Via et al.
patients. MUA has also been proposed for refractory pain trough the relaxation of the surrounding musculature50. As
and stiffness. The results of manipulation have mostly been the ROM increase, a program of strengthening exercises of
reported to be excellent also in the long term, but compara- the scapular muscles and rotator cuff muscles is indicated.
tive studies have shown equivocal benefit when compared In stage 4 the aim of the treatment is restoring the normal
with hydrodilation or home exercises therapy. Than the high function of the shoulder. In addition to strengthening exer-
risk of side effect that discourage its use64,65. cises, proprioceptive exercises are prescribed in order to
Surgical options for treatment of AC have been proposed. correct the compensatory movements and restore a proper
The most popular treatment of resistant AC is arthroscopic dynamic shoulder joint. More aggressive approach can be
release. It has been considered useful also to confirm the proposed for patients refractory after 6 months of conser-
diagnosis, to exclude other significant pathologies, to classi- vative treatment. Arthroscopic release alone or in combina-
fy the stage of the disease. The advantage of this technique tion with manipulative treatment appears to provide better
is its ability to perform precise, selective capsular releases results.
in a very controlled manner.
Open release is the last chance for the most resistant forms
of adhesive capsulitis for patients who failed arthroscopy Conclusions
and closed manipulation. These cases are fortunately rare.
Unfortunately, open release is associated with open proce- There are few evidences to draw firm conclusion about the
dures complications such as prolonged recovery, post-sur- best management of patients with AC and its treatment re-
gical stiffness, increased post-operative pain that can inhibit mains controversial. Treatment should be should be based
early mobilization. on the stage of the disease and on patients characteristics.
We think that treatment of AC should be based on the stage The first approach should be conservative while surgical
of the disease, on patient characteristics and that an indi- option should be considered for patients refractory to con-
vidual rehabilitation program should be proposed. We also servative treatment. Although there are several treatment
think that is very important explain to patients that “normal” options, it would seem that the best treatment has yet to be
is not the expected outcome and the restoration of pre-inju- discovered and further studies are needed.
ry shoulder function is not the goal of treatment. In the first
phase is important to reduce pain and preserve shoulder
functionality is mandatory. NSAIDs or intra-articular steroid References
injections are indicated, paying attention to not exceed 4
weeks of treatment. We prefer to use intra-articular sodium 1. Calis M, Demir H, Ulker S, Kirnap M, Duygulu F, Calis HT.
hyaluronate injection to improve pain and ROM. Better re- Is intraarticular sodium hyaluronate injection an alternative
sults have been proved with the addiction of stretching and treatment in patients with adhesive capsulitis? Rheumatol
exercises program within the pain threshold. For this pur- Int 2006; 26:536-40.
2. Duplay S. De la péri-arthrite scapulo-humérale et des rai-
pose hydrotherapy represents a valid treatment alternative.
deurs de l’epaule qui en sont la consequence. Arch Gen
It offers the possibility, by reducing the force of gravity, to Méd 1872; 20:513-542.
perform a more natural and less stressful movement on the 3. Codman EA. The Shoulder: Rupture of the Supraspinatus
joints. Water also helps in relaxing muscles in order to facili- Tendon and Other Lesions in or About the Subacromial
tate movements. Laser therapy has been used with statisti- Bursa. Boston, MA: T Todd Company; 1934.
cally significant reduction of pain and disability compared 4. Neviaser JS. Adhesive capsulitis of the shoulder. J Bone
to placebo78. In the freezing stage is extremely important to Joint Surg Am 1945; 27:211-222.
prevent and reduce the formation of adhesions. This can be 5. Hand GC, Athanasou NA, Matthews T, Carr AJ. The pa-
thology of frozen shoulder. J Bone Joint Surg Br 2007; 89:
obtained through an exercise program that includes passive
928-932.
mobilization, active exercises carried out in mild scapular 6. Matsen FA, Fu FH, Hawkins RJ. The shoulder: a balance
plane, daily home exercises and self made mobilization. We of mobility and stability. Rosemont, IL: American Academy
use cane or pulleys to improve internal and external rota- of Orthopaedic Surgeons; 1993.
tion. The length and intensity of exercise should be based 7. Zuckerman J, Rokito S. Definition and classification of fro-
on the threshold of pain of the patient. In stage 3, the fro- zen shoulder: a consensus approach. J Shoulder Elbow
zen stage, a significant shoulder stiffness is predominant Surg 2011; 20:322-335.
and the aim of therapy is the treatment of the marked loss 8. Edwald A. Adhesive capsulitis: a review. Am Fam Physi-
cian 2011; 83:417-422.
of ROM. It is extremely important to correct the compen-
9. Wong PLK, Tan HCA. A review on frozen shoulder. Singa-
satory movements and restore a proper dynamic shoulder pore Med J 2010; 51:694-697.
joint. The mainstay of treatment in this phase is represented 10. Massoud SN, Pearse EO, Levy O, Copeland SA. Operative
by physiotherapy. The control of pain is important to in- management of the frozen shoulder in patients with diabe-
crease the intensity, duration and frequency of exercises. tes. J Shoulder Elbow Surg 2002; 11:609-613.
Prolonged low-load stretching and end range mobilization 11. Ogilvie-Harris DJ, Myerthall S. The diabetic frozen shoul-
can be prescribed. To improve shoulder external rotation der: arthroscopic release. Arthroscopy 1997;13:1-8.
posteriorly directed joint mobilization technique is more ef- 12. Wohlgethan JR. Frozen shoulder in hyperthyroidism. Ar-
thritis Rheum 1987; 30:936-939.
fective than an anteriorly directed mobilization technique45.
13. Bowman CA, Jeffcoate WJ, Pattrick M, Doherty M. Bilateral
The addition of deep heating to stretching exercises and adhesive capsulitis, oligoarthritis and proximal myopathy
mobilizations can produce a greater improvement in ROM as presentation of hypothyroidism. Br J Rheumatol 1988;
76 Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78
Treatment of adhesive capsulitis: a review
27:62-64. a placebo-controlled trial. Arthritis Rheum 2003; 48: 829-
14. Smith SP, Devaraj VS, Bunker TD. The association be- 838.
tween frozen shoulder and Dupuytren’s disease. J Shoul- 36. Ryans I, Montgomery A, Galway R, W. G. Kernohan WG,
der Elbow Surg 2001; 10:149-151. McKane R. A randomized controlled trial of intraarticular
15. Bulgen DY, Binder A, Hazleman BL, Park JR. Immunologi- triamcinolone and/or physiotherapy in shoulder capsulitis.
cal studies in frozen shoulder. J Rheumatol 1982; 9: 893- Rheumatology(Oxford) 2005; 44: 529-535.
898. 37. Rovetta G, Monteforte P. Intraarticular injection of sodium
16. Pearsall AW, Speer KP. Frozen shoulder syndrome: diag- hyaluronate plus steroid versus steroid in adhesive capsu-
nostic and treatment strategies in the primary care setting. litis of the shoulder. Int J Tissue React 1998; 20:125-130.
Med Sci Sports Exerc 1998; 30:33-39. 38. Takagishi K, Saito A, Segawa K, Takahira N, Itomitu S.
17. Noel E, Thomas T, Schaeverbeke T, Thomas P, Bonjean M, Evaluation of intra-articular injection in patients with so-
Revel M. Frozen shoulder. Joint Bone Spine 2000; 67:393- called Gojyukata: comparison hyaluronate and steroid. Jpn
400. J Med Pharm Sci 1996; 35: 377-381.
18. Neviaser AS, Hannafin JA. Adhesive capsulitis: A review 39. Harris JD, Griesser MJ, Copelan A, Jones GL Treatment of
of current treatment. Am J Sports Med 2010; 38:2346-56. adhesive capsulitis with intra-articular hyaluronate: A sys-
19. Hand C, Clipsham K, Rees JL, et al. Long-term outcome tematic review. Int J Shoulder Surg 2011; 5:31-37.
of frozen shoulder. J Shoulder Elbow Surg 2008; 17: 231- 40. Iwata H. Pharmacologic and clinical aspects of intraarticu-
236. lar injection of hyaluronate. Clin Orthop Relat Res 1993;
20. Bunker T. Time for a new name for frozen shoulder: con- 289: 285-291.
tracture of the shoulder. Shoulder & Elbow 2009; 1:4-9. 41. Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S.
21. Neviaser RJ, Neviaser TJ. The frozen shoulder: diagnosis Frozen shoulder: prospective clinical study with an evalu-
and management. Clin Orthop Relat Res 1987;223:59-64. ation of three treatment regimens. Ann Rheum Dis 1984;
22. Hannafin JA, Dicarlo EF, Wickiewicz TL, et al. Adhesive 43: 353-360.
capsulitis: capsular fibroplasia of the glenohumeral joint. J 42. Griggs SM, Ahn A, Green A. Idiopathic Adhesive Capsulitis:
Shoulder Elbow Surg 1994; 3: 435-440. A Prospective Functional Outcome Study of Nonoperative
23. Reeves B. The natural history of the frozen shoulder syn- Treatment. J Bone Joint Surg Am 2000; 82:1398-1407.
drome. Scand J Rheumatol 1975; 4:193-196. 43. Diercks RL, Stevens M. Gentle thawing of the frozen
24. Mengiardi B, Pfirrmann CW, Gerber C, Hodler J, Zanetti shoulder: a prospective study of supervised neglect ver-
M. Frozen shoulder: MR arthrographic findings. Radiology sus intensive physical therapy in seventy-seven patients
2004; 233: 486-492. with frozen shoulder syndrome followed up for two years. J
25. Van der Windt DA, van der Heijden GJ, Scholten RJ, Koes Shoulder Elbow Surg 2004; 13: 499-502.
BW, Bouter LM. The efficacy of non-steroidal anti-inflam- 44. Vermeulen HM, Rozing PM, Obermann WR, le Cessie S,
matory drugs (NSAIDS) for shoulder complaints. A system- Vliet Vlieland TP. Comparison of high-grade and low-grade
atic review. J Clin Epidemiol 1995;48:691-704. mobilization techniques in the management of adhesive
26. Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA. Cur- capsulitis of the shoulder: randomized controlled trial. Phys
rent review of adhesive capsulitis. J Shoulder Elbow Surg Ther 2006; 86: 355-368.
2011; 20: 502-514. 45. Johnson AJ, Godges JJ, Zimmerman GJ, Ounanian LL.
27. Neviaser AS, Hannafin JA. Adhesive capsulitis: a review of The effect of anterior versus posterior glide joint mobiliza-
current treatment. Am J Sports Med. 2010; 38:2346-2356. tion on external rotation range of motion in patients with
28. Blockey A, Wright J. Oral cortisone therapy in periarthritis shoulder adhesive capsulitis. J Orthop Sports Phys Ther
of the shoulder. Br Med J 1954; 1:1455-1467. 2007; 37: 88-99.
29. Kessel L, Bayley I, Young A. The upper limb: the frozen 46. Jewell DV, Riddle DL, Thacker LR. Interventions associ-
shoulder. Br J Hosp Med 1981; 25:334-339. ated with an increased or decreased likelihood of pain
30. Binder A, Hazleman BL, Parr G, Roberts S. A controlled reduction and improved function in patients with adhesive
study of oral prednisolone in frozen shoulder. Br J Rheu- capsulitis: a retrospective cohort study. Phys Ther 2009;
matol 1986; 25: 288-292. 89: 419-429.
31. Buchbinder R, Hoving JL, Green S, Hall S, Forbes A, Nash 47. Tanaka K, Saura R, Takahashi N, Hiura Y, Hashimoto R.
P. Short course prednisolone for adhesive capsulitis (fro- Joint mobilization versus self-exercises for limited gle-
zen shoulder or stiff painful shoulder): a randomised, dou- nohumeral joint mobility: randomized controlled study
ble blind, placebo controlled trial. Ann Rheum Dis 2004; of management of rehabilitation. Clin Rheumatol 2010;
63:1460-1469. 29:1439-1444.
32. Widiastuti-Samekto M, Sianturi GP. Frozen shoulder syn- 48. Green S, Buchbinder R, Hetrick S. Physiotherapy inter-
drome: comparison of oral route corticosteroid and intra- ventions for shoulder pain. Cochrane Database Syst Rev
articular corticosteroid injection. Med J Malaysia 2004; 59: 2003: CD004258.
312-316. 49. Stergioulas A. Low-power laser treatment in patients with
33. Lorbach O, Anagnostakos K, Scherf C, seil R, Kohn D, frozen shoulder: preliminary results. Photomed Laser Surg
Pape D. Nonoperative management of adhesive capsuli- 2008; 26:99-105.
tis of the shoulder: oral cortisone application versus intra- 50. Leung MS, Cheing GL. Effects of deep and superficial
articular cortisone injections. J Shoulder Elbow Surg 2010; heating in the management of frozen shoulder. J Rehabil
19:172-179. Med 2008; 40:145-150.
34. Calis M, Demir H, Ulker S, Kirnap M, Duygulu F, Calis HT. 51. Dahan TH, Fortin L, Pelletier M, et al. Double blind random-
Is intraarticular sodium hyaluronate injection an alternative ized clinical trial examining the efficacy of bupivacaine su-
treatment in patients with adhesive capsulitis? Rheumatol prascapular nerve blocks in frozen shoulder. J Rheumatol
Int 2006; 26: 536-540. 2000; 27: 1464-1469.
35. Carette S, Moffet H, Tardif J, et al. Intraarticular corticoste- 52. Jones DS, Chattopadhyay C. Suprascapular nerve block
roids, supervised physiotherapy, or a combination of the for the treatment of frozen shoulder in primary care: a ran-
two in the treatment of adhesive capsulitis of the shoulder: domized trial. Br J Gen Pract 1999; 49:39-41.
Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78 77
A. Giai Via et al.
53. Karatas GK, Meray J. Suprascapular nerve block for pain report. J Shoulder Elbow Surg 2011; 20:23-26.
relief in adhesive capsulitis: comparison of 2 different tech- 66. Kivimaki J, Pohjolainen T, Malmivaara A, et al. Manipula-
niques. Arch Phys Med Rehabil 2002; 83: 593-597. tion under anesthesia with home exercises versus home
54. Børglum J, Bartholdy A, Hautopp H, Krogsgaard MR, Jen- exercises alone in the treatment of frozen shoulder: a ran-
sen K. Ultrasound-guided continuous suprascapular nerve domized, controlled trial with 125 patients. J Shoulder El-
block for adhesive capsulitis: one case and a short topical bow Surg 2007; 16: 722-726.
review. Acta Anaesthesiol Scand 2011; 55:242-247. 67. Janda DH, Hawkins RJ. Shoulder manipulation in patients
55. Buchbinder R, Green S, Forbes A, et al. Arthrographic joint with adhesive capsulitis and diabetes mellitus: a clinical
distension with saline and steroid improves function and note. J Shoulder Elbow Surg 1993; 2:36-38.
reduces pain in patients with painful stiff shoulder: results 68. Baums MH, Spahn G, Nozaki M, Steckel H, Schultz W,
of a randomised, double blind, placebo controlled trial. Ann Klinger HM. Functional outcome and general health status
Rheum Dis 2004; 63: 302-309. in patients after arthroscopic release in adhesive capsulitis.
56. Khan AA, Mowla A, Shakoor MA, Rahman MR. Arthro- Knee Surg Sports Traumatol Arthrosc 2007; 15:638-644.
graphic distension of the shoulder joint in the management 69.Cinar M, Akpinar S, Derincek A, Circi E, Uysal M. Compari-
of frozen shoulder. Mymensingh Med J 2005; 14:67-70. son of arthroscopic capsular release in diabetic and idio-
57. Jacobs LG, Barton MA, Wallace WA, Ferrousis J, Dunn pathic frozen shoulder patients. Arch Orthop Trauma Surg
NA, Bossingham DH. Intra-articular distension and ste- 2010; 130: 401-406.
roids in the management of capsulitis of the shoulder. BMJ 70. Elhassan B, Ozbaydar M, Massimini D, Higgins L, Warner
1991; 302: 1498-1501. JJ. Arthroscopic capsular release for refractory shoulder
58. Corbeil V, Dussault RG, Leduc BE, Fleury J. Adhesive cap- stiffness: a critical analysis of effectiveness in specific eti-
sulitis of the shoulder: a comparative study of arthrography ologies. J Shoulder Elbow Surg 2010; 19:580-587.
with intra-articular corticotherapy and with or without cap- 71. Ogilvie-Harris DJ, Biggs DJ, Fitsialos DP, MacKay M. The
sular distension. Can Assoc Radiol J 1992; 43:127-130. resistant frozen shoulder: manipulation versus arthroscop-
59. Gam AN, Schydlowsky P, Rossel I, Remvig L, Jensen EM. ic release. Clin Orthop Relat Res 1995; 319:238-248.
Treatment of “frozen shoulder” with distension and glucor- 72. Snow M, Boutros I, Funk L. Posterior arthroscopic capsular
ticoid compared with glucorticoid alone. A randomized con- release in frozen shoulder. Arthroscopy 2009; 25:19-23.
trolled trial. Scand J Rheumatol 1998; 27:425-430. 73. Ozaki J, Nakagawa Y, Sakurai G, Tamai S. Recalcitrant
60. Kivimäki J, Pohjolainen T, Malmivaara A, et al. Manipula- chronic adhesive capsulitis of the shoulder: role of contrac-
tion under anesthesia with home exercises versus home ture of the coracohumeral ligament and rotator interval in
exercises alone in the treatment of frozen shoulder: a ran- pathogenesis and treatment. J Bone Joint Surg Am 1989;
domized, controlled trial with 125 patients. J Shoulder El- 71:1511-1515.
bow Surg 2007; 16: 722-726. 74. Neviaser AS, Hannafin JA. Adhesive capsulitis: a review of
61. Quraishi NA, Johnston P, Bayer J, Crowe M, Chakrabarti current treatment. Am J Sports Med 2010; 38:2346-2356.
AJ. Thawing the frozen shoulder: a randomised trial com- 75. Favejee MM, Huisstede BM, Koes BW. Frozen shoulder:
paring manipulation under anaesthesia with hydrodilata- the effectiveness of conservative and surgical interven-
tion. J Bone Joint Surg Br 2007; 89:1197-1200. tions-systematic review. Br J Sports Med 2011; 45:49-56.
62. Dodenhoff RM, Levy O, Wilson A, Copeland SA. Manipula- 76. Kelley MJ, McClure PW, Leggin BG. Frozen shoulder: evi-
tion under anesthesia for primary frozen shoulder: effect dence and a proposed model guiding rehabilitation. J Or-
on early recovery and return to activity. J Shoulder Elbow thop Sports Phys Ther 2009; 39:135-148.
Surg 2000; 9: 23-26. 77. Iannotti JP, Kwon YW. Management of persistent shoulder
63. Farrell CM, Sperling JW, Cofield RH. Manipulation for fro- pain: a treatment algorithm. Am J Orthop (Belle Mead NJ)
zen shoulder: long-term results. J Shoulder Elbow Surg 2005; 34:16-23.
2005;14:480-484. 78. Tashjian RZ. The effectiveness of nonoperative treatment
64. Loew M, Heichel TO, Lehner B. Intraarticular lesions in for frozen shoulder: a systematic review. Clin J Sport Med
primary frozen shoulder after manipulation under general 2012; 22:168-179.
anesthesia. J Shoulder Elbow Surg 2005; 14:16-21. 79. Manud E, Craig D, Suekarran S et al. Management of fro-
65. Magnussen RA, Taylor DC. Glenoid fracture during ma- zen shoulder: a systematic review and cost-effectiveness
nipulation under anesthesia for adhesive capsulitis: a case analysis. Health Technology Assessment 2012; 16:1-243.
78 Muscles, Ligaments and Tendons Journal 2012; 2 (2): 70-78
Copyright of Muscles, Ligaments & Tendons Journal (MLTJ) is the property of CIC Edizioni Internazionali
s.r.l. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright
holder's express written permission. However, users may print, download, or email articles for individual use.
Das könnte Ihnen auch gefallen
- Amit Murli Patel. Physical Therapy Management of Tuberculous Arthritis of The Elbow SRJI Vol - 2, Issue - 1, Year - 2013Dokument10 SeitenAmit Murli Patel. Physical Therapy Management of Tuberculous Arthritis of The Elbow SRJI Vol - 2, Issue - 1, Year - 2013Dr. Krishna N. SharmaNoch keine Bewertungen
- Redler 2019Dokument11 SeitenRedler 2019Shiba MiyukiNoch keine Bewertungen
- Capsulitis Adhesiva PDFDokument14 SeitenCapsulitis Adhesiva PDFErika LópezNoch keine Bewertungen
- 1108 ShoulderDokument5 Seiten1108 ShoulderMilton RezzaNoch keine Bewertungen
- Mar 2008Dokument9 SeitenMar 2008debyanditaNoch keine Bewertungen
- Tendinopatía BarçaDokument26 SeitenTendinopatía BarçaPAcoNoch keine Bewertungen
- Merolla 2015Dokument8 SeitenMerolla 2015Sandro RolimNoch keine Bewertungen
- Chapter 9 - Soft Tissue Damage and HealingDokument28 SeitenChapter 9 - Soft Tissue Damage and HealingdafortminorNoch keine Bewertungen
- Tendinopathy GuidelinesDokument26 SeitenTendinopathy GuidelinesArdis CaniNoch keine Bewertungen
- Pathophysiology of Frozen Shoulder: Text Book Reading (TBR)Dokument10 SeitenPathophysiology of Frozen Shoulder: Text Book Reading (TBR)Mega Mulya Dwi FitriyaniNoch keine Bewertungen
- Post Lumbar Puncture Vertebral Collapse: Discitis andDokument3 SeitenPost Lumbar Puncture Vertebral Collapse: Discitis andRohit GowdaNoch keine Bewertungen
- 2015 Article 367 PDFDokument8 Seiten2015 Article 367 PDFJesse CusterNoch keine Bewertungen
- Acute Limb IschemicDokument3 SeitenAcute Limb IschemicmarisahanaNoch keine Bewertungen
- Diagnosis and Management of Adhesive CapsulitisDokument10 SeitenDiagnosis and Management of Adhesive CapsulitisCarlos Martín De RosasNoch keine Bewertungen
- Tendinopathy Continuum 2008 (Cook & Purdam)Dokument8 SeitenTendinopathy Continuum 2008 (Cook & Purdam)nsboyadzhievNoch keine Bewertungen
- ArthritisDokument10 SeitenArthritisAhana CherianNoch keine Bewertungen
- Jurnal Frozen PDFDokument27 SeitenJurnal Frozen PDFFahmi MiNoch keine Bewertungen
- Lateral Epicondylitis: Instructional Review: Shoulder and ElbowDokument7 SeitenLateral Epicondylitis: Instructional Review: Shoulder and ElbowzoreNoch keine Bewertungen
- A Review On Frozen Shoulder: Singapore Medical Journal September 2010Dokument5 SeitenA Review On Frozen Shoulder: Singapore Medical Journal September 2010Anonymous ckZmIgoNoch keine Bewertungen
- Frozen Shoulder 20 FebruaryDokument29 SeitenFrozen Shoulder 20 Februaryangga nugrahaNoch keine Bewertungen
- Conservative Management of Selected Shoulder ProblemsDokument8 SeitenConservative Management of Selected Shoulder ProblemsDr Franklin Shoenholtz100% (3)
- Atypical Acute Compartment Syndrome: C Ó 2017 T J B J S, IDokument4 SeitenAtypical Acute Compartment Syndrome: C Ó 2017 T J B J S, IGhea Jovita SinagaNoch keine Bewertungen
- RJZ 269Dokument3 SeitenRJZ 269Saffa AzharaaniNoch keine Bewertungen
- 10 17826-Cutf 203634-206098Dokument4 Seiten10 17826-Cutf 203634-206098alaawagdybv2Noch keine Bewertungen
- General Principles of Fractures: Department of Orthopaedic Surgery Liu Xueyong (刘学勇)Dokument82 SeitenGeneral Principles of Fractures: Department of Orthopaedic Surgery Liu Xueyong (刘学勇)Banna Kiran KumarNoch keine Bewertungen
- Sindroma KompartemenDokument8 SeitenSindroma KompartemennurulNoch keine Bewertungen
- What Is Inflammation''? Are We Ready To Move Beyond Celsus?Dokument2 SeitenWhat Is Inflammation''? Are We Ready To Move Beyond Celsus?Lisle CamposNoch keine Bewertungen
- Comparison of Mulligan Technique Versus Muscle Energy Technique in Patients (Ingles)Dokument5 SeitenComparison of Mulligan Technique Versus Muscle Energy Technique in Patients (Ingles)mauricio castroNoch keine Bewertungen
- Treatment of Adhesive Capsulitis of The Shoulder-1Dokument12 SeitenTreatment of Adhesive Capsulitis of The Shoulder-1JONATHAN IVANNoch keine Bewertungen
- Tuberculosis of The Patella, Report CaseDokument4 SeitenTuberculosis of The Patella, Report CaseAnonymous AzXah9n0YNoch keine Bewertungen
- Vascular Abnormalities of SSCDokument9 SeitenVascular Abnormalities of SSCCristina ElenaNoch keine Bewertungen
- SMF Orthopaedi Dan Traumatologi RSU DR Saiful Anwar Malang: Thomas Erwin C J HuwaeDokument58 SeitenSMF Orthopaedi Dan Traumatologi RSU DR Saiful Anwar Malang: Thomas Erwin C J Huwaeyulia manaweanNoch keine Bewertungen
- PRM2020 6965381Dokument9 SeitenPRM2020 6965381zoreNoch keine Bewertungen
- Revisión Bibliográfica Síndrome Compartimental y de Aplastamiento. Actuación PrehospitalariaDokument8 SeitenRevisión Bibliográfica Síndrome Compartimental y de Aplastamiento. Actuación Prehospitalarialyneth lacourtNoch keine Bewertungen
- Overuse Tendinosis, Not Tendinitis: Part 1: A New Paradigm For A Difficult Clinical ProblemDokument10 SeitenOveruse Tendinosis, Not Tendinitis: Part 1: A New Paradigm For A Difficult Clinical ProblemTony100% (4)
- Rotator Cuff Lesions: A Case ReportDokument8 SeitenRotator Cuff Lesions: A Case ReportUbaidillah Romadlon AlfairuziNoch keine Bewertungen
- Supra Spin at UsDokument3 SeitenSupra Spin at UsmarindadaNoch keine Bewertungen
- Pressure Ulcers and Decubitus Patients: Iliadis Christos, Mihalache Anca, Dimitriadou AlexandraDokument3 SeitenPressure Ulcers and Decubitus Patients: Iliadis Christos, Mihalache Anca, Dimitriadou AlexandraerpublicationNoch keine Bewertungen
- Litrev Trauma MuskuloskeletalDokument26 SeitenLitrev Trauma Muskuloskeletaldedyalkarni08Noch keine Bewertungen
- In Practice 2012 Moores 22 6Dokument6 SeitenIn Practice 2012 Moores 22 6ransinghNoch keine Bewertungen
- EpicondilteDokument7 SeitenEpicondilteRicardo fariaNoch keine Bewertungen
- Treatment of Rotator Cuff TendinopathyDokument11 SeitenTreatment of Rotator Cuff TendinopathyYoh ChenNoch keine Bewertungen
- 10.1007@s40141 016 0112 yDokument6 Seiten10.1007@s40141 016 0112 yNicolas ParejaNoch keine Bewertungen
- Adhesive CapsulitisDokument11 SeitenAdhesive Capsulitismetal_moggleNoch keine Bewertungen
- Lisis de Adherencias Epidurales (Parte 1) - Fisiopatología y ClínicaDokument8 SeitenLisis de Adherencias Epidurales (Parte 1) - Fisiopatología y ClínicaVasquez RvhNoch keine Bewertungen
- Anterior Cruciate Ligament Mucoid Degeneration: A Review of The Literature and Management GuidelinesDokument8 SeitenAnterior Cruciate Ligament Mucoid Degeneration: A Review of The Literature and Management Guidelineschandan noelNoch keine Bewertungen
- Tendinopathy vs. TendinitisDokument4 SeitenTendinopathy vs. TendinitismatnpeteNoch keine Bewertungen
- IndianJClinAnaesth 9 3 374 378Dokument5 SeitenIndianJClinAnaesth 9 3 374 378bhaskaracharya dontabhaktuniNoch keine Bewertungen
- 3 Essay OrthoDokument11 Seiten3 Essay Orthogamal attamNoch keine Bewertungen
- Adhesive Capsulitis of The ShoulderDokument7 SeitenAdhesive Capsulitis of The ShoulderKemal TaufikNoch keine Bewertungen
- Treatment Strategy For Frozen ShoulderDokument9 SeitenTreatment Strategy For Frozen ShoulderDiah Rindayani HasbiNoch keine Bewertungen
- JB6 4 121 727Dokument3 SeitenJB6 4 121 727Rhizka djitmauNoch keine Bewertungen
- Minimally Invasive Approach For Extraforaminal Synovial Cyst L5-S1Dokument7 SeitenMinimally Invasive Approach For Extraforaminal Synovial Cyst L5-S1Tatiana RoaNoch keine Bewertungen
- Frozen Shoulder (Buku Komplit Etiologi DLL)Dokument7 SeitenFrozen Shoulder (Buku Komplit Etiologi DLL)Ricky Diah Ayu AnggrainiNoch keine Bewertungen
- AO Principles of Fracture Management - 3rd Ed. - Thieme - 2017Dokument7 SeitenAO Principles of Fracture Management - 3rd Ed. - Thieme - 2017Roberto GuanipaNoch keine Bewertungen
- Calcific Tendinitis of The Shoulder: Grear Hurt, MD, Champ L. Baker, JR, MDDokument9 SeitenCalcific Tendinitis of The Shoulder: Grear Hurt, MD, Champ L. Baker, JR, MDLuis Sebastian Arango OspinaNoch keine Bewertungen
- Capsulitis AdhesivaDokument6 SeitenCapsulitis AdhesivaPEDRONoch keine Bewertungen
- Orthopaedics EmergenciesDokument63 SeitenOrthopaedics EmergencieszzooooeeeeeeNoch keine Bewertungen
- International Journal of Surgery Case ReportsDokument4 SeitenInternational Journal of Surgery Case Reportsanasofia.vargas22Noch keine Bewertungen
- 5 Effects of Cold Stimulation On Cardiac Activation PDFDokument26 Seiten5 Effects of Cold Stimulation On Cardiac Activation PDFGumDropNoch keine Bewertungen
- Current Concepts Concussion 2012 ScorzaDokument10 SeitenCurrent Concepts Concussion 2012 ScorzaGumDrop100% (1)
- 5 Effects of Cold Stimulation On Cardiac Activation PDFDokument26 Seiten5 Effects of Cold Stimulation On Cardiac Activation PDFGumDropNoch keine Bewertungen
- Effect of Breakfast On Weight LossDokument12 SeitenEffect of Breakfast On Weight LossGumDropNoch keine Bewertungen
- Biomechanical Considerations in The Competitive Swimmer Heinlien 2011Dokument7 SeitenBiomechanical Considerations in The Competitive Swimmer Heinlien 2011GumDropNoch keine Bewertungen
- Models of Supervision in EducationDokument11 SeitenModels of Supervision in EducationGumDropNoch keine Bewertungen
- ACL Injury Prevention, More Effective With A Different Way of Motor Learning?Dokument7 SeitenACL Injury Prevention, More Effective With A Different Way of Motor Learning?GumDropNoch keine Bewertungen
- Safety Patient Handling in Nursing PDFDokument40 SeitenSafety Patient Handling in Nursing PDFGumDrop100% (1)
- SI Provocative TestsDokument7 SeitenSI Provocative TestsGumDrop100% (1)
- Manual For OSHA Mandatories 2017Dokument67 SeitenManual For OSHA Mandatories 2017GumDropNoch keine Bewertungen
- Ability of Clinical Tests To Diagnose Stress FX - SR and Meta Analysis Sep2012-RR-Schneiders PDFDokument12 SeitenAbility of Clinical Tests To Diagnose Stress FX - SR and Meta Analysis Sep2012-RR-Schneiders PDFGumDropNoch keine Bewertungen
- Neck Control in CPDokument11 SeitenNeck Control in CPGumDropNoch keine Bewertungen
- PARM LBP CPG 2nd Edition 2017 PDFDokument293 SeitenPARM LBP CPG 2nd Edition 2017 PDFGumDropNoch keine Bewertungen
- CPG - Whiplash Associated DisordersDokument74 SeitenCPG - Whiplash Associated DisordersGumDropNoch keine Bewertungen
- Clinical Practice Guideline Hip Oa CPG 2015 - PARMDokument55 SeitenClinical Practice Guideline Hip Oa CPG 2015 - PARMGumDropNoch keine Bewertungen
- Acupuncture Vs US in Impingement Syndrome RCT July 2005 PDFDokument13 SeitenAcupuncture Vs US in Impingement Syndrome RCT July 2005 PDFGumDropNoch keine Bewertungen
- PARM Stroke Rehabilitation CPG 2011 1 PDFDokument278 SeitenPARM Stroke Rehabilitation CPG 2011 1 PDFGumDropNoch keine Bewertungen
- Comparison of US Therapy of Various Duration in TX of SA ImpingementDokument4 SeitenComparison of US Therapy of Various Duration in TX of SA ImpingementGumDropNoch keine Bewertungen
- Neural Retraining Project Highlights: Completion of First Phase Informs Creation of Clinical Trials ProtocolDokument2 SeitenNeural Retraining Project Highlights: Completion of First Phase Informs Creation of Clinical Trials ProtocolDeepak RanaNoch keine Bewertungen
- Imp PhysiologyDokument16 SeitenImp PhysiologysipransinghNoch keine Bewertungen
- DIPHTHERIADokument12 SeitenDIPHTHERIANununNoch keine Bewertungen
- Shin LuluDokument2 SeitenShin LuluEka HimawanNoch keine Bewertungen
- The Amyloid Beta Peptide A Chemist S Perspective. Role in Alzheimer's and FibrillizationDokument46 SeitenThe Amyloid Beta Peptide A Chemist S Perspective. Role in Alzheimer's and FibrillizationAdrianENoch keine Bewertungen
- Calcium Gluconate Dosage PlusDokument8 SeitenCalcium Gluconate Dosage PlusJaved ArifNoch keine Bewertungen
- Polycythemia Vera: Kimberly Truong Wendy YangDokument22 SeitenPolycythemia Vera: Kimberly Truong Wendy YangAdeena RayNoch keine Bewertungen
- Anterior Triangle of NeckDokument13 SeitenAnterior Triangle of NeckÑäd ÉèmNoch keine Bewertungen
- (IM A) (Com Dse) Typhoid Fever (Strawberry)Dokument4 Seiten(IM A) (Com Dse) Typhoid Fever (Strawberry)NoreenNoch keine Bewertungen
- ENT Trans Disorders of The External EarDokument4 SeitenENT Trans Disorders of The External EarJared Ezrach Cacal SanidadNoch keine Bewertungen
- Hema 1 ErythropoiesisDokument20 SeitenHema 1 Erythropoiesismarie judimor gomezNoch keine Bewertungen
- Sno EditedDokument2.972 SeitenSno EditedDavid Paul HensonNoch keine Bewertungen
- Drug StudyDokument8 SeitenDrug StudyRuel LoriaNoch keine Bewertungen
- Hypothyroidism in Context: Where We've Been and Where We're GoingDokument12 SeitenHypothyroidism in Context: Where We've Been and Where We're Going1130017003 AIMMATUL CHANIFAHNoch keine Bewertungen
- Popis Bolesti, Kod Kojih Liječenje Zapperom Daje Pozitivni RezultatDokument7 SeitenPopis Bolesti, Kod Kojih Liječenje Zapperom Daje Pozitivni RezultatMićo RadenovićNoch keine Bewertungen
- Surgery I #3 - Fluid and ElectrolytesDokument9 SeitenSurgery I #3 - Fluid and ElectrolytesCarl Earvin L. Favorito100% (1)
- Medical Surgical Nursing QuestionsDokument7 SeitenMedical Surgical Nursing Questionseloisa mae gementizaNoch keine Bewertungen
- Amblyopia Hunter PDFDokument12 SeitenAmblyopia Hunter PDFWaqar AhmadNoch keine Bewertungen
- Herrera Et Al-2018-Journal of Clinical PeriodontologyDokument17 SeitenHerrera Et Al-2018-Journal of Clinical PeriodontologydanielaNoch keine Bewertungen
- VancomycinDokument1 SeiteVancomycinJUSTINE ALLYSA MAY CASTILLONoch keine Bewertungen
- Script AbdomenDokument19 SeitenScript AbdomenRespicio Christian Aejay G.Noch keine Bewertungen
- MEDBIO KROK-1 English 2019-2020Dokument65 SeitenMEDBIO KROK-1 English 2019-2020Катерина КабишNoch keine Bewertungen
- August 03 2017 Recalls Mls (Ascpi)Dokument6 SeitenAugust 03 2017 Recalls Mls (Ascpi)Joanna Carel Lopez100% (3)
- 2 Newborn AssesmentDokument23 Seiten2 Newborn Assesment.Noch keine Bewertungen
- Gynecology: 3.09 - AmenorrheaDokument13 SeitenGynecology: 3.09 - AmenorrheaAnna Mae MarantanNoch keine Bewertungen
- Taj Pharma's FDA-Approved Generic Version, Cisplatin InjectionDokument1 SeiteTaj Pharma's FDA-Approved Generic Version, Cisplatin InjectionTAJ PHARMA — A Health Care ProviderNoch keine Bewertungen
- Lymph Nodes Normal Anatomy Major ZonesDokument5 SeitenLymph Nodes Normal Anatomy Major ZoneschristianNoch keine Bewertungen
- O.M Final ExamDokument4 SeitenO.M Final ExamAwilNoch keine Bewertungen
- Abdominal SonographyDokument6 SeitenAbdominal SonographyRio FutabaNoch keine Bewertungen
- A Case of Brain Death During PregnancyDokument52 SeitenA Case of Brain Death During PregnancyMa Pilar Peñaflor AñonuevoNoch keine Bewertungen