Beruflich Dokumente
Kultur Dokumente
AMENORRHEA
Hochgeladen von
Christian PasicolanOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
AMENORRHEA
Hochgeladen von
Christian PasicolanCopyright:
Verfügbare Formate
AMENORRHEA
Criseline D. Tolentino, MD, DPOGS, FPSSTD
MENSTRUAL CYCLE (REVIEW)
GYNECOLOGY - AMENORRHEA Page 1
o Gonadotropin control of the ovarian and endometrial cycles.
o The ovarian-endometrial cycle has been structured as a 28-day cycle.
o The follicular phase (days 1-14) is characterized by rising levels of estrogen, thickening of the
endometrium, and selection of the dominant “ovulatory” follicle.
o During the luteal phase (days 14-21), the corpus luteum (CL) produces estrogen which prepare the
endometrium for implantation.
o If implantation occurs, the developing blastocysts will begin to produce hCG and rescue the CL, thus
maintaining progesterone production.
HYPOTHALAMUS-PITUTARY-OVARIAN AXIS
GYNECOLOGY - AMENORRHEA Page 2
NORMAL FEMALE PUBERTAL DEVELOPMENT
PRIMARY AMENORRHEA
Absence of menses (IN WOMEN) by 16 years of age in the presence of normal secondary sexual
characteristics.
Absence of menses (IN WOMEN) by 14 years of age when there is no visible secondary sexual
characteristics.
SECONDARY AMENORRHEA
Absence of menstruation for three normal menstrual cycles of six months after menarche.
GYNECOLOGY - AMENORRHEA Page 3
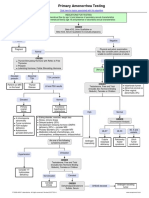
EVALUATION OF PRIMARY AMENORRHEA
History and PE completed For a patient with primary amenorrhea
Secondary sexual characteristic present
No Yes
Measure FSH and LH levels perform UTZ of uterus
FSH and LH <5 IU/L FSH >20 IU/L uterus absent/abnormal uterus present/Normal
LH >40 IU/L
Hypognadotropic hypergonadotropic karyotype analysis outflow obstruction
Hypogonadism hypogonadism
karyotype analysis
46XY 46XX No Yes
46XY 46XX evaluate for imperforate hymen
Secondary or transverse
Amenorrhea vaginal septum
Androgen mullerian
Insensitivity agenesis
syndrome
premature turner’s
ovarian syndrome
failure
HYPERGONADOTROPIC HYPOGONADISM (GONADAL FAILURE)
Elevated levels of FSH and LH that result from decreased negative feedback mechanism.
1. Gonadal Dysgenesis
Turner’s Syndrome (45X)
o Is the most common abnormality causing gnadal failure and primary amenorrhea
2. Partial deletions of X Chr
3. Mosaicism (45X, 46XY)
4. Pure Gonadal Dysgenesis (46XX, 46XY)
5. 17 £ hydroxylase with 46XX
HYPOGONADOTROPIC HYPOGONADISM
When the hypothalamus fails to secrete adequate amounts of GnRH
When the pituitary disorder associated with inadequate production or release of pituitary gonadotropins
is present.
1. Physiology delay
o Most common manifestation
o Delayed reactivation of the GnRH pulse generation
2. Kallman’s Syndrome
o 2nd most common
o Insufficient pulsatile secretion of GnRH
3. Central Nervous System Tumor
o Most common is craniopharyngioma
GYNECOLOGY - AMENORRHEA Page 4
TREATMENT
Cyclic estrogen and progesterone therapy
0.625 mg/day of Estradiol
Progestin (MPA 5-10mg)
Should be added for the first 12 days of the month
If 17 £ hydroxylase deficiency is confirmed, corticosteroid replacement is instituted as well as estrogen
and progestin
MAYER ROKITANSKY-KUSTER-HAUSSER SYNDROME
o 2nd most frequent cause of primary amenorrhea
o Absence of the uterus (cervix) and/ or vagina
ANDROGEN INSENSITIVITY
o Phenotypically female, genotypically male (XY)
o Defect in the androgen receptor gene located in the X Chr
o Anti mullerian hormone is present
o Testes, rather tha ovaries, arepresent in the abdomen
GUIDELINES OR PROGESTERONE AND ESTROGEN/ PROGESTOGEN CHALLENGE TEST
Drug Dosing Duration
Progestogen Challenge Test
MPA (Provera) 10 mg PO, OD 7-10 days
Norethindrone (Aygestin) 5 mg PO, OD 7-10 days
progesterone 200 parenteral, OD Single dose
Progesterone micronized 400 mg PO, OD 7-10 days
Progesterone micronized gel (4-8%) Intravaginally every other day Six applications
Estrogen / Progesterone Challege test
Estrogen / Progesterone (Prevnarin) 1.25 mg PO, OD 21 days
or
Estrdiol (Estrace) 2 mg PO, OD 21 days
followed by
Progestational agent As noted above
GYNECOLOGY - AMENORRHEA Page 5
EVALUATION OF SECONDARY AMENORRHEA
Patient presenting with secondary amenorrhea, negative pregnancy test
Check TSH and Prolactin levels
Both normal normal prolactinlevels normal TSH
Abnormal TSHlevels abnormal Prolactin levels
Progestogen thyroid disease PRL ≤100 ng/ml PRL >100 ng/ml
Challenge test 100 mcg/L
Withdrawal bleed no withdrawal bleed consider other causes MRI to evaluate
prolactinoma
Normogonadotropic estrogen/progestogen
Hypogonadism challenge test negative MRI
Withdrawal bleed no withdrawal bleed consider other
causes
Check FSH and LH outflow obstruction
FSH >20 IU/L FSH and LH <5 IU/L
LH >40 IU/L
Hypergonadotropic perform MRI to evaluate
Hypogonadism for pituitary tumor
Normal MRI, hypogonadotropic
Hypogonadism
GYNECOLOGY - AMENORRHEA Page 6
Das könnte Ihnen auch gefallen
- Ok Ok Notes PediaDokument14 SeitenOk Ok Notes PediaChristian PasicolanNoch keine Bewertungen
- Problem Set: The Endocrine SystemDokument6 SeitenProblem Set: The Endocrine SystemMyshaM0990% (3)
- Dr. Shehla Jamal Assistant Professor: OBG S M S & RDokument69 SeitenDr. Shehla Jamal Assistant Professor: OBG S M S & RAppy LoveNoch keine Bewertungen
- 3 AmenorrrheaDokument29 Seiten3 AmenorrrheaKilp MosesNoch keine Bewertungen
- AmenorrheaDokument55 SeitenAmenorrheaAla AbushehabNoch keine Bewertungen
- AmenorrheaDokument26 SeitenAmenorrheaThatStudentNoch keine Bewertungen
- 2 AmenorrheaDokument41 Seiten2 AmenorrheaKilp MosesNoch keine Bewertungen
- Primary Amenorrhoea 2Dokument42 SeitenPrimary Amenorrhoea 2sivaNoch keine Bewertungen
- Clinical Guidelines ForDokument54 SeitenClinical Guidelines ForHenry SudharsonoNoch keine Bewertungen
- AmenorrheaDokument41 SeitenAmenorrheaBonitavanyNoch keine Bewertungen
- Perdarahan Uterus DisfungsionalDokument22 SeitenPerdarahan Uterus DisfungsionalAggiFitiyaningsihNoch keine Bewertungen
- Amen or RheaDokument41 SeitenAmen or Rheakhadzx100% (2)
- AmenorrheaDokument41 SeitenAmenorrheadoraNoch keine Bewertungen
- An Overview in InfertilityDokument50 SeitenAn Overview in InfertilityNi Wayan Yunita SariNoch keine Bewertungen
- Infertility in Male and FemaleDokument27 SeitenInfertility in Male and FemaleDanai JanuaritaNoch keine Bewertungen
- Biochemical Investigation of Infertile Couple-My PresentationDokument91 SeitenBiochemical Investigation of Infertile Couple-My PresentationOlukoyejo OluwaboriNoch keine Bewertungen
- 2.1.6.2 Amenorea Dan DismenoreaDokument21 Seiten2.1.6.2 Amenorea Dan DismenoreaRahmatia SyukrinaNoch keine Bewertungen
- Menstrual Disorders and PCOS Webinar EMBRYO FKUI 2022Dokument49 SeitenMenstrual Disorders and PCOS Webinar EMBRYO FKUI 2022angelinputri100% (1)
- InfertilityDokument18 SeitenInfertilityphuyalaryan666Noch keine Bewertungen
- Chapter 27. Amenorrhea: Berek & Novak's Gynecology 14 Edition (P 1035 1068) R3 Jung Mi ByunDokument95 SeitenChapter 27. Amenorrhea: Berek & Novak's Gynecology 14 Edition (P 1035 1068) R3 Jung Mi Byunhossam626Noch keine Bewertungen
- Amenorrhea: Oleh Dr. H M A Ashari SpogDokument29 SeitenAmenorrhea: Oleh Dr. H M A Ashari SpogsiTengilNoch keine Bewertungen
- AmenorrhoeaDokument38 SeitenAmenorrhoeaheydydNoch keine Bewertungen
- 4.primary - Secondary AmenorrheaDokument5 Seiten4.primary - Secondary AmenorrheaAhmed Al GhaithiNoch keine Bewertungen
- Physiology of Female ReproductionDokument3 SeitenPhysiology of Female ReproductionAntoine JeriNoch keine Bewertungen
- Amenorrhea: Oleh Dr. H M A Ashari Spog (K)Dokument29 SeitenAmenorrhea: Oleh Dr. H M A Ashari Spog (K)Devi SuryandariNoch keine Bewertungen
- Amenorrhea ImprovedDokument3 SeitenAmenorrhea ImprovedCriselda Charisse ReganionNoch keine Bewertungen
- Amen or RheaDokument34 SeitenAmen or RheaAsma Naseer CheemaNoch keine Bewertungen
- 4.4 (Amenorrhea) University of AlexanderDokument28 Seiten4.4 (Amenorrhea) University of AlexanderAnonymous XSXlZJvyWNoch keine Bewertungen
- Seminar: Guide: Co-Guide: Pramoted byDokument35 SeitenSeminar: Guide: Co-Guide: Pramoted byDhara MeenaNoch keine Bewertungen
- Shigref MushtaqDokument28 SeitenShigref Mushtaqeisha aliNoch keine Bewertungen
- Primary Amenorrhea Testing AlgorithmDokument1 SeitePrimary Amenorrhea Testing AlgorithmGabriella AguirreNoch keine Bewertungen
- Primary Amenorrhea Testing AlgorithmDokument1 SeitePrimary Amenorrhea Testing AlgorithmfarmasiNoch keine Bewertungen
- Amenorrhea PDFDokument5 SeitenAmenorrhea PDFKenneth Robin CarbonellNoch keine Bewertungen
- Gynecology - Secondary AmenorrheaDokument2 SeitenGynecology - Secondary AmenorrheaAnsley MadalaNoch keine Bewertungen
- OB 2nd SGDDokument4 SeitenOB 2nd SGDJxyp MundoNoch keine Bewertungen
- Precociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Dokument31 SeitenPrecociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Priya RaviNoch keine Bewertungen
- Ambiguous GenitaliaDokument16 SeitenAmbiguous Genitaliamohdmaghyreh100% (1)
- Primary Amenorrhea: Rabika Almina RabiaDokument30 SeitenPrimary Amenorrhea: Rabika Almina RabiaAlmina RehmanNoch keine Bewertungen
- First Aid For The OBS&GYN Clerkship CH 17 (Amenorrhea)Dokument9 SeitenFirst Aid For The OBS&GYN Clerkship CH 17 (Amenorrhea)黃芳昌Noch keine Bewertungen
- Amenorrhea - Algorithm & DifferentialsDokument9 SeitenAmenorrhea - Algorithm & DifferentialsItharshan IndreswaranNoch keine Bewertungen
- Infertility 001Dokument257 SeitenInfertility 001Habtamu Nigussie100% (1)
- Laboratory and Radiographic Tests For Ambiguous GenitaliaDokument8 SeitenLaboratory and Radiographic Tests For Ambiguous GenitaliaMaria Lucia RossiNoch keine Bewertungen
- Simplifikasi Amenore: Hanom Husni SyamDokument30 SeitenSimplifikasi Amenore: Hanom Husni Syamamarendra WardhanaNoch keine Bewertungen
- Infertility: Villanueva, Ian Joseph Virata, Marc Jenaro Yabuki, Ukari Yambot, Kathleen KayDokument13 SeitenInfertility: Villanueva, Ian Joseph Virata, Marc Jenaro Yabuki, Ukari Yambot, Kathleen KayBea SamonteNoch keine Bewertungen
- Obstetrics & Gynecology NotesDokument7 SeitenObstetrics & Gynecology NotesMary Ella WoodNoch keine Bewertungen
- AmenorrheaDokument41 SeitenAmenorrheaarfahregarNoch keine Bewertungen
- Laboratory Tests For EndocrinologyDokument6 SeitenLaboratory Tests For EndocrinologyAnastasia100% (1)
- Amenorrhea & Heavy Menstrual BleedingDokument22 SeitenAmenorrhea & Heavy Menstrual BleedingJanesel Plariza PanerioNoch keine Bewertungen
- Secondary Amenorrhea: DR Hanaa AlaniDokument44 SeitenSecondary Amenorrhea: DR Hanaa AlaniAakashNoch keine Bewertungen
- AmenorrheaDokument41 SeitenAmenorrheaDewi Felayati Gusni100% (2)
- Amenorrhea: DR - Muhammad Rusda, SP - OG (K)Dokument41 SeitenAmenorrhea: DR - Muhammad Rusda, SP - OG (K)sridhaniNoch keine Bewertungen
- AmenorrheaDokument13 SeitenAmenorrheaJanesel Plariza PanerioNoch keine Bewertungen
- IVF Infertility Treatment IndiaDokument26 SeitenIVF Infertility Treatment India24x7emarketing100% (1)
- Amenorrhea WorkupDokument10 SeitenAmenorrhea WorkupHaoKeat HoeNoch keine Bewertungen
- Homoeopathic Management of InfertilityDokument92 SeitenHomoeopathic Management of InfertilityDrSaji86% (7)
- Hyper Pro Lac Tine MiaDokument47 SeitenHyper Pro Lac Tine Miakharbosham100% (3)
- Amenorrhoea Primary & SecondaryDokument24 SeitenAmenorrhoea Primary & SecondaryAnushaAgrawalNoch keine Bewertungen
- Assesment of Amen or RheaDokument49 SeitenAssesment of Amen or Rheakhadzx100% (2)
- Laboratory Investigation of Amenorrhea:: DefinitionsDokument8 SeitenLaboratory Investigation of Amenorrhea:: DefinitionsAmelia SetiawatiNoch keine Bewertungen
- Obstetrics & Gynecology: Original Review & Revision HyderabadDokument739 SeitenObstetrics & Gynecology: Original Review & Revision Hyderabad24k.avinashNoch keine Bewertungen
- AMENORRHOEADokument16 SeitenAMENORRHOEAdrravindermehetreyNoch keine Bewertungen
- 2019 PPMP and App-Non Cse FormDokument8 Seiten2019 PPMP and App-Non Cse FormChristian PasicolanNoch keine Bewertungen
- Physics of RadiologyDokument9 SeitenPhysics of RadiologyChristian PasicolanNoch keine Bewertungen
- Lec 4 Platelet and CoagulationDokument17 SeitenLec 4 Platelet and CoagulationChristian PasicolanNoch keine Bewertungen
- Narag, MarkDokument64 SeitenNarag, MarkChristian PasicolanNoch keine Bewertungen
- ENDOMETRIOSISDokument5 SeitenENDOMETRIOSISChristian PasicolanNoch keine Bewertungen
- Pediatrics Tckler-3 PDFDokument100 SeitenPediatrics Tckler-3 PDFChristian PasicolanNoch keine Bewertungen
- Cagayan Valley Medical Center Carig Sur, Tuguegarao City CagayanDokument8 SeitenCagayan Valley Medical Center Carig Sur, Tuguegarao City CagayanChristian PasicolanNoch keine Bewertungen
- Pedia OncoDokument8 SeitenPedia OncoChristian PasicolanNoch keine Bewertungen
- Pedia Tickler Cont 20190210175903 PDFDokument80 SeitenPedia Tickler Cont 20190210175903 PDFChristian PasicolanNoch keine Bewertungen
- LeukemiaDokument33 SeitenLeukemiaChristian PasicolanNoch keine Bewertungen
- Cagayan State University - College of Information TechnologyDokument26 SeitenCagayan State University - College of Information TechnologyChristian Pasicolan50% (2)
- WRUV7926Dokument3 SeitenWRUV7926rajashekarcse533Noch keine Bewertungen
- Sonography of Normal and Abnormal Thyroid and Parathyroid Glands PDFDokument15 SeitenSonography of Normal and Abnormal Thyroid and Parathyroid Glands PDFJheyson Javier Barrios PereiraNoch keine Bewertungen
- Science 3 DLP 7 - Parts of The Skin and Their FunctionsDokument12 SeitenScience 3 DLP 7 - Parts of The Skin and Their FunctionsEmily DaymielNoch keine Bewertungen
- Biology NEET-11 EM: Chemical Control & Co-OrdinationDokument1 SeiteBiology NEET-11 EM: Chemical Control & Co-Ordinationnileshsaini2006Noch keine Bewertungen
- 123 Sur HypoparathyroidismDokument3 Seiten123 Sur HypoparathyroidismHurryNoch keine Bewertungen
- LEC 01 - Principles of EndocrinologyDokument44 SeitenLEC 01 - Principles of EndocrinologyIoana Cozma100% (1)
- Laporan PhyxioEx METEND - Rohid AlfazonDokument27 SeitenLaporan PhyxioEx METEND - Rohid AlfazonZayne GamingNoch keine Bewertungen
- Adrenal Gland 111Dokument28 SeitenAdrenal Gland 111Renz OrtegaNoch keine Bewertungen
- Anatomy and Physiology OvaryDokument6 SeitenAnatomy and Physiology OvaryFretchell Aripal MontesNoch keine Bewertungen
- CH 3 Form 5Dokument30 SeitenCH 3 Form 5Noor Amira RamliNoch keine Bewertungen
- Tyroid Drug - ppt3Dokument15 SeitenTyroid Drug - ppt3nurliah armandNoch keine Bewertungen
- Sinadinos Christa - Herbal Support For HypothyroidismDokument11 SeitenSinadinos Christa - Herbal Support For HypothyroidismDiah Siti FatimahNoch keine Bewertungen
- Diagnosis of HypothyroidismDokument10 SeitenDiagnosis of HypothyroidismHanzla IrfanNoch keine Bewertungen
- Thyroid Tietz Textbook 2012 PDFDokument21 SeitenThyroid Tietz Textbook 2012 PDFIvana BajunovicNoch keine Bewertungen
- Tulajabahvani StotrDokument2 SeitenTulajabahvani StotrHema DhaneNoch keine Bewertungen
- Puberty Below: Role of HormonesDokument3 SeitenPuberty Below: Role of HormonesCyril CauilanNoch keine Bewertungen
- Lesson Plan 2020-2021Dokument7 SeitenLesson Plan 2020-2021MELIE BAGARESNoch keine Bewertungen
- Diagestive, Urinary and Reproductive SystemDokument39 SeitenDiagestive, Urinary and Reproductive SystemCarolina Calle HerreraNoch keine Bewertungen
- Shashikant PDFDokument4 SeitenShashikant PDFAacharya Shashikant VashishthNoch keine Bewertungen
- Diagnosis and Treatment of Primary AldosteronismDokument17 SeitenDiagnosis and Treatment of Primary AldosteronismcastillojessNoch keine Bewertungen
- Sidney H. Ingbar (Editor), Sidney C. Werner (Editor) by Lippincott Williams & Wilkins PublishersDokument10 SeitenSidney H. Ingbar (Editor), Sidney C. Werner (Editor) by Lippincott Williams & Wilkins Publishersbyrock66Noch keine Bewertungen
- EndocrinologyDokument57 SeitenEndocrinologyeleonora rosaNoch keine Bewertungen
- Hypophysis CerebriDokument21 SeitenHypophysis CerebriAli Akand AsifNoch keine Bewertungen
- Disorders of The Endocrine SystemDokument84 SeitenDisorders of The Endocrine Systemcy lifeNoch keine Bewertungen
- Anatomy and PhysiologyDokument10 SeitenAnatomy and PhysiologyBurni GuevaraNoch keine Bewertungen
- Endocrine System Function and AssessmentDokument3 SeitenEndocrine System Function and Assessmentbomoore79Noch keine Bewertungen
- Ip Lot 40380Dokument1 SeiteIp Lot 40380MaherNoch keine Bewertungen
- CC Chatterjee's Human Physiology 12th Volume 2Dokument7 SeitenCC Chatterjee's Human Physiology 12th Volume 2food onNoch keine Bewertungen
- Hypopituitarism - ThomasDokument40 SeitenHypopituitarism - ThomasguidanceNoch keine Bewertungen