Beruflich Dokumente
Kultur Dokumente
Severe Hypertension in Children at A Central Referral Hospital in Kwazulu-Natal Province, South Africa
Hochgeladen von
yutefupOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Severe Hypertension in Children at A Central Referral Hospital in Kwazulu-Natal Province, South Africa
Hochgeladen von
yutefupCopyright:
Verfügbare Formate
This open-access article is distributed under
ARTICLE Creative Commons licence CC-BY-NC 4.0.
Severe hypertension in children at a central referral
hospital in KwaZulu-Natal Province, South Africa
D Murigo-Shumba, MB ChB, DCH, Dip HIV Man (SA);
R Bhimma, MB ChB, DCH, FCP (Paeds), MMed (Paed), MD, Cert Nephrology (Paed);
E Naicker, MB ChB, DCH, FCP (Paed), Cert Nephrology (Paed)
Department of Maternal and Child Health, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal,
Durban, South Africa
Corresponding author: D Murigo-Shumba (davidzomurigo@gmail.com)
Background. Hypertension (HPT) is often underdiagnosed in children, although significant morbidity and mortality arises from
hypertensive target organ damage and hypertensive crises.
Objectives. To determine the prevalence, complications and causes of severe HPT in children ≤12 years old at a central hospital.
Methods. Hospital records of children ≤12 years old with severe HPT (stage 2 and higher) from 2005 to 2014 were reviewed. Demographics,
nutritional status, causes, HIV status, presence of target organ damage and treatment were analysed.
Results. Of 821 children admitted to the paediatric nephrology unit, 152 (18.5%) children had severe HPT, with a mean age of 6.3 years; 86
(57%) were boys. A total of 28 (19%) were HIV-positive, and 19 (68%) were treatment naive. Kidney disease accounted for 82% of cases,
46 (30%) having steroid-resistant nephrotic syndrome, 22 (14%) HIV-associated nephropathy, 19 (13%) glomerulonephritis, 21 (14%)
congenital urinary tract abnormalities and 17 (11%) other renal causes. Renovascular causes accounted for 12 (8%) cases. Of these 12, 7 (58%)
had left ventricular hypertrophy (LVH), compared with 10/125 (8%) who had other forms of kidney disease (p<0.023). Hypertensive crises
occurred in 28 (18%) patients, and were significantly more common in children with HPT secondary to renovascular causes than renal
causes (p=0.001).
Conclusion. Renal diseases were the most common cause of severe HPT in children. Hypertensive crises, retinopathy and LVH are
common in renovascular HPT.
S Afr J Child Health 2019;13(1):44-48. DOI:10.7196/SAJCH.2019.v13i1.1564
Hypertension (HPT) is a major non-communicable disease affecting Hypertensive target organ damage is an indication for starting
more than one billion people worldwide, with a rising prevalence. antihypertensive medication.[15] Left ventricular hypertrophy (LVH) is
A study that estimated worldwide blood pressure (BP) trends the most common form of target organ damage seen in children.[15] It
from 1975 to 2015 showed an increase in adults with high BP, is a risk factor for future cardiac disease, and treatment results in its
from 594 million in 1975 to 1.13 billion in 2015, with the highest regression and reduction in cardiac risk.[16]
prevalence noted in low-income countries.[1] The morbidity and While in adults severe HPT can be defined as systolic BP ≥160 mmHg,
mortality associated with HPT is increasing, as revealed in a study or diastolic BP ≥100 mmHg, in children it has not been clearly
that showed a rise in disability-adjusted life years between 1990 and defined. In one review on severe HPT in children and adolescents,
2015.[2] There is evidence from many studies of BP tracking from severe HPT was defined as stage 2 HPT with severe symptoms,[17]
childhood to adulthood.[3,4] It is therefore important to detect and while in another study, it was defined as BP above stage 2 HPT with
treat HPT early so as to reduce the risk of complications. associated symptoms.[18] Severe HPT can be divided into hypertensive
HPT in children is underdiagnosed as there is often no measurement emergency and hypertensive urgency. Hypertensive emergency is
of BP in children presenting to healthcare facilities,[3] and at times severe HPT with target organ damage and life-threatening symptoms
incorrect measuring techniques are used. The prevalence of HPT such as seizures and encephalopathy, while hypertensive urgency has
may therefore be an underestimate, as some cases may have been less serious symptoms such as vomiting and headache, with no target
missed. In a systemic review and meta-analysis of 25 African studies organ damage. The management of these two forms of hypertensive
that recruited patients from 1997 to 2013, the pooled prevalence crisis differ as there is a more urgent need to reduce the BP in
of HPT was found to be 5.5% and that of pre-HPT 12.7% among hypertensive emergency.[15,17]
children and adolescents.[5] A local study in school-age children The present study aimed to determine the prevalence of severe
in the Phoenix area in Durban, South Africa (SA), revealed a HPT, secondary causes, presence of target organ damage and the
prevalence of 2.1% for pre-HPT and 2.6% for HPT.[6] Another school incidence and treatment of hypertensive crises among patients
survey by the National Kidney Foundation of SA (NKFSA) over a admitted to the paediatric nephrology unit at Inkosi Albert Luthuli
9 - 10-year period showed hypertension in 12% of female and 16% Central Hospital (IALCH), Durban, SA.
of male adolescents.[7] Other SA studies reported HPT prevalence
ranging from 1 to 24.4% in children.[3,8-11] Methods
In younger children, secondary HPT is more common than primary, This 10-year retrospective chart review was done at IALCH, which
with renal and renovascular causes making up the largest proportion. serves as a quaternary referral hospital for KwaZulu-Natal and its
The prevalence of primary HPT has, however, been increasing in older neighbouring provinces. Computerised hospital records of patients
children owing to sedentary lifestyles that result in obesity.[12-14] admitted to the paediatric nephrology unit at IALCH from 2005 to
Hypertensive children should be assessed for target organ damage, 2014 were reviewed. Inclusion criteria were all children ≤12 years
which can affect the heart, retina, kidneys and nervous system.[12] with severe HPT. Severe HPT was defined as stage 2 HPT as defined
44 SAJCH APRIL 2019 Vol. 13 No. 1
ARTICLE
by the ‘Fourth report on the diagnosis, evaluation and treatment of are shown in Table 2. Twenty-eight (19%) children were HIV-
high blood pressure in children and adolescents’,[15] which classifies positive; of these, 19 (68%) were not on antiretroviral treatment on
BP as follows: normal if <90th percentile, pre-HPT if ≥90th to <95th presentation (Table 2).
percentile or >120/80 mmHg in adolescents; stage 1 HPT if ≥95th to Table 3 shows the causes of severe HPT in the study group. Renal
99th percentile plus 5 mmHg, stage 2 HPT if >99th percentile plus 5 causes accounted for 82% of cases, the most common cause being
mmHg. BP was measured using automatic non-invasive BP devices nephrotic syndrome. Renovascular causes accounted for 12 (8%)
with an appropriately sized cuff. Blood pressure was measured three cases, Takayasu arteritis 8 (5%) and renal artery stenosis 4 (3%).
times to confirm stage 2 HPT. However, for patients who had signs Systemic causes were noted in 3 (2%) children. All patients with
and symptoms of hypertensive crisis, one reading in the stage 2 HPT severe HPT secondary to steroid-resistant nephrotic syndrome
category was adequate to classify the patient as stage 2. A Pediatric received prednisolone in an attempt to induce remission. However,
BP Calculator (PedsBP, Shuojing Song, USA) and/or age- and sex- severe HPT was only diagnosed when patients were on low-dose
specific BP tables with height percentiles that utilised data from the steroids (≤0.5 mg/kg/day) or weaned off steroids, to remove steroids
above report were used to classify HPT. Patients excluded from the as a possible causal agent for severe HPT.
study were those >12 years old, children with HPT less than stage 2 Sixty-three (42%) children were assessed for LVH, of whom 21
and those managed under other specialist units. (33%) were found to have this. Ten (48%) children with LVH had
Data collected included demographic data, nutritional status, renal causes, while 7 (33%) had renovascular causes. However, LVH
causes of HPT, HIV status, presence of target organ damage and affected patients with renovascular causes more often than patients
hypertensive crisis and its treatment. Nutritional status was assessed with renal causes, as 58% (7/12) with renovascular causes had LVH,
using World Health Organization Child Growth Standards.[19-21] compared with 8% (10/125) who had other forms of kidney disease
Children were classified using BMI or weight-for-length/height: (p<0.023). Although this difference was statistically significant, the
wasted if <–2; normal if –2 to +2; overweight if >+2 to +3; and obese
if >+3. Table 1. Patients with severe HPT (stage 2 or higher), by age
Target organ damage assessed for included LVH as determined group (N=152)
by echocardiography undertaken by a paediatric cardiologist, Age n (%)
nephropathy based on presence or absence of proteinuria on ≤28 days 2 (1)
urine dipstick analysis, retinopathy and cerebrovascular accidents. 29 days - 2 years 24 (16)
Hypertensive crisis information included the number of crises, and
>2 years 126 (83)
the symptoms and treatment of each. Information was captured in
Excel (Microsoft, USA) and analysed by a professional statistician HPT = hypertension.
from the School of Public Health, Biostatistics Department,
University of KwaZulu-Natal.
Permission to conduct the study was obtained from the Biomedical Table 2. Demographics and nutritional and HIV status of
Research Ethics Committee of the University of KwaZulu-Natal (ref. children with severe HPT (N=152)
no. BE507/15). Characteristic n (%)
Sex
Results Male 86 (57)
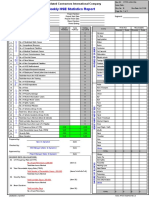
One hundred and fifty-two (18.5%) of 821 children admitted over
Female 66 (43)
the 10-year period had severe HPT, as shown in Fig. 1. Table 1
shows the number of patients in each age group. The mean age of Race
presentation was 6.3 years (range 10 days - 12 years). A total of 86 Black African 138 (91)
(57%) were male and 66 (43%) female. Race and nutritional status Indian 7 (5)
White 2 (1)
Not recorded 5 (3)
Total admissions Nutritional status
n=821 Normal 90 (59)
Overweight 7 (5)
Obese 7 (5)
Wasted 13 (9)
Not recorded 35 (23)
Height
Stage 2 HPT and Below stage 2 HPT
Normal 86 (57)
≤12 yrs old or >12 yrs old
n=152 n=669 Stunted 26 (17)
Tall 5 (3)
Not recorded 35 (23)
HIV status
Negative 104 (68)
Positive
No HPT or
Below stage 2 HPT Untreated 19 (12)
>12 yrs old
n=93 Treated 9 (6)
n=576
Unknown 20 (13)
Fig. 1. Admissions to paediatric nephrology unit at Inkosi Albert Luthuli Central HPT = hypertension.
Hospital, 2005 - 2014. (HPT = hypertension.)
45 SAJCH APRIL 2019 Vol. 13 No. 1
ARTICLE
proportion of patients not assessed for LVH among those with renal renovascular causes accounted for 8% of the cases of severe HPT,
causes was high, as only 33% of patients with renal causes were which is similar to the Polish study above in which renovascular
assessed for LVH. causes accounted for 10% of the cases.[26]
Seventy-seven (51%) children had nephropathy. Of these, 70 (91%) While CVA and hypertensive nephropathy were assessed in the
had severe HPT secondary to renal aetiology, 4 (5%) renovascular present study in almost all patients with severe HPT, LVH was
aetiology and in 3 (4%), the aetiology was unknown. Four (3%) had only assessed in 42% of patients, and even fewer were assessed for
hypertensive retinopathy. Cerebrovascular accident (CVA) was noted hypertensive retinopathy (17%), as shown in Fig. 3. This was a result
in 4 (3%) patients. Retinopathy and CVA were noted more frequently of limited resources, and staffing constraints.
in those with renovascular causes (75%) as opposed to renal causes
(25%), but this was not statistically significant (p>0.3). Table 3. Causes of severe HPT (stage 2 or higher) in children
Hypertensive crises occurred in 28 (18%) patients. Of these, 22 by age (N=152)
(79%) had 1 hypertensive crisis, 4 (14%) had 2 and 2 (7%) had 3 Age (years),
crises. The most common symptoms noted were encephalopathy Cause n (%) mean (SD)
and seizures, which occurred in 25 (89%) and 24 (86%) children, SRNS 46 (30) 5.6 (2.8)
respectively (Fig. 2). The most commonly used drugs for the crises HIVAN 22 (14) 7.5 (2.4)
were nifedipine and labetalol, which were used as the sole agent in
CAKUT 21 (14) 4.8 (3.9)
11 (40%) and 4 (14%) children, respectively. Four (14%) children had
Glomerulonephritis 19 (13) 7.1 (2.7)
a combination of both drugs used sequentially. Less frequently used
drugs included sodium nitroprusside, furosemide and amlodipine. Renovascular* 12 (8) 7.8 (3.5)
Seventeen (61%) children with hypertensive crises were treated with Other renal† 17 (11) 5.4 (3.5)
1 drug only, while 5 (18%) were treated with 2 drugs. Hypertensive Systemic disease‡ 3 (2) 8.3 (3.8)
crisis was significantly more common among the children with Primary 12 (8) 6.7 (4.2)
renovascular causes than in those with renal causes (OR 7.5; 95% CI Total 152 (100) 6.3 (3.3)
2.2 - 26.2; p=0.001) of HPT.
HPT = hypertension; SD = standard deviation; SRNS = steroid-resistant nephrotic
Discussion syndrome; HIVAN = HIV-associated nephropathy; CAKUT = congenital
abnormalities of the kidney and the urinary tract.
There was an 18.5% prevalence of severe HPT (stage 2) among †
*Takayasu arteritis, renal artery stenosis (RAS), acute kidney injury of unknown
children admitted to the paediatric nephrology unit at IALCH over cause, chronic kidney disease of unknown cause, haemolytic uraemic syndrome,
‡
the 10-year study period. While most previous studies determined tubulo-interstitial nephritis, Henoch-Schönlein purpura, systemic lupus
the prevalence of HPT in children, there is a limited number of erythematosus, Wegener’s granulomatosis.
studies that assessed specifically for severe HPT in children. In
keeping with reports from other studies of HPT in children, males
in the present study were more commonly affected by severe HPT
than females, at 57% and 43%, respectively, a ratio of almost 3:2. Encephalopathy
In another study on HPT prevalence, cardiac complications and
antihypertensive medication use in children, 61% of patients were
Seizures
Symptom/sign
male and 39% female.[22]
Antiretroviral treatment for HIV-positive patients reduces the
incidence of HIV-associated nephropathy (HIVAN). In this study, 14% Headache
of the patients with severe HPT had HIVAN, making it the second
most common cause of severe HPT after nephrotic syndrome. Free Vomiting
antiretroviral treatment has been offered in the public sector in SA
since April 2004, but despite this favourable development, 19 (68%) Visual disturbance
HIV-positive children were not on treatment.
The majority of the children had severe HPT due to secondary 0 5 10 15 20 25 30
causes, and 12 (8%) children had HPT of unknown aetiology despite
extensive investigations. In older children and adolescents, primary Fig. 2. Symptoms and signs that occurred in hypertensive crises (multiple
HPT is more common than secondary, which is more often seen symptoms per patient).
in younger children.[12,23] In a study by Gupta-Malhotra et al.[24] on
essential (primary) v. secondary HPT that included children from
160
birth to 19 years, essential HPT occurred at a significantly older age
than secondary HPT, with median ages at diagnosis of 12 years (range 140
3 - 17 years) and 9 years (range 0.08 - 19 years), respectively.The lower 120
prevalence of primary HPT in the current study may be due to the 100 Not assessed
exclusion of children older than 12 years, and of those with less severe
Patients, n
80 Assessed
forms of HPT, since primary HPT presents in less severe forms.
The majority of HPT patients in the current study (125; 82%) had a 60 Pathology present
renal aetiology. This is in keeping with the results of other studies. A 40
study in Romania looking at aetiology and BP patterns in secondary
20
HPT in children showed that renal parenchymal disease accounted
for 83.2% of secondary HPT, which is similar to the present study’s 0
results.[25] Two other studies that have demonstrated renal causes as LVH Nephropathy Retinopathy CVA
the most common causes of secondary HPT are a Polish[26] and a
Thai[27] study in which 68% and 62.7%, respectively, of their cases of Fig. 3. Target organ damage: assessment and results. ( LVH = left ventricular
HPT were due to renal parenchymal disease. In the present study, hypertrophy; CVA = cerebrovascular accident).
46 SAJCH APRIL 2019 Vol. 13 No. 1
ARTICLE
It is recommended by the ‘Fourth report on the diagnosis, evaluation Conclusion
and treatment of high blood pressure in children and adolescents’ Our findings of severe HPT in children aged ≤12 years showed that
that all children and adolescents with established HPT be assessed it occurred more commonly in males. The most common cause
by echocardiogram for LVH.[15] Regression of LVH has been noted was glomerular disease, with the majority of the patients having
with antihypertensive treatment. A study by Kupferman et al.[28] steroid-resistant nephrotic syndrome. Renovascular HPT is the
showed that there may be a decline in LVH with BP reduction in more severe form, as a higher proportion of these patients had target
children with chronic kidney disease. In the present study, only 42% organ damage and hypertensive crises. A high proportion of children
of patients were assessed for LVH, owing to limited resources and with HIV infection who were not on antiretroviral treatment were
staffing constraints. Of these, 33% were noted to have LVH. In a US diagnosed with severe HPT.
study by Hanevold et al.,[29] the prevalence of LVH was 41.1%.[29] The Based on our current findings, we strongly recommended HIV
proportion of patients with LVH in the present study was lower than testing in all children, with early commencement of treatment in
this, possibly because fewer patients were assessed for LVH. those who test HIV-positive, to reduce the prevalence of HIVAN,
Proteinuria as a marker of hypertensive nephropathy was difficult which is a significant cause of severe HPT. Long-term studies should
to assess in this study, as the majority of patients had nephrotic be done in our population to monitor the progression of LVH and
syndrome, meaning that the presence of proteinuria was more retinopathy in children on antihypertensive treatment. Children
likely due to the primary disease than it was a complication of HPT. presenting with encephalopathy or seizures should have their BP
Hypertensive retinopathy is well documented in adults; however, checked as these were the most common presentations in children
there are limited studies available on children. In a study by with hypertensive crisis.
Williams et al.[30] that assessed hypertensive retinopathy in severely
hypertensive children, 18% of the children who had eye assessments
had hypertensive retinopathy. The same study showed that in Acknowledgements. We would like to thank the medical manager of the
patients with renovascular disease, there was a higher prevalence IALCH for permission to publish this data, the staff involved in the care
of hypertensive retinopathy, although this was not statistically of these children and those at the hospitals that referred these children
significant.[30] In our study, 4 (15%) patients had hypertensive to our centre.
retinopathy, comparable to the results of the study by Williams et al.,[30] Author contributions. DM-S: data capture, analysis and writing of the
with 3 (75%) having HPT secondary to renovascular causes.
manuscript. RBh: conceptualisation of the project, data analysis and
HPT is a known risk factor for CVA in adults, and improved BP
control reduces this risk. In children, HPT may be an important factor review of the manuscript. EN: patient care, data capture and review of
in the development of stroke.[31] In our study, 4 (3%) patients had the manuscript.
CVAs, with 3 (75%) of these having HPT secondary to renovascular Funding. None.
causes. Conflict of Interest. None.
Hypertensive crisis occurred in 28 (18%) children. The most
common presentations in the present study were encephalopathy and
seizures, which occurred in 89% and 85% of the cases, respectively. 1. NCD Risk Factor Collaboration. Worldwide trends in blood pressure from
1975 to 2015: A pooled analysis of 1479 population-based measurement
Unlike these results, a study in Taiwan showed headache (54.5%) and studies with 19.1 million participants. Lancet 2017;389(10064):37-55. https://
dizziness (45.5%) as the two most common presenting symptoms.[32] doi.org/10.1016/S0140-6736(16)31919-5
In the present study, the proportion of patients with hypertensive crisis 2. Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and
systolic blood pressure of at least 110 to 115 mmHg, 1990 - 2015. JAMA
was significantly higher among children with renovascular causes of 2017;317(2):165-182. https://doi.org/10.1001/jama.2016.19043
HPT than intrinsic renal causes (58% v. 16%, p<0.001). 3. Kagura J, Adair LS, Musa MG, Pettifor JM, Norris SA. Blood pressure tracking
Intravenous antihypertensive therapy is recommended for in urban black South African children: Birth to twenty cohort. BMC Pediatr
2015;15(1):78. https://doi.org/10.1186/s12887-015-0402-z
hypertensive emergencies for a controlled reduction in BP,[15] 4. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A
aiming to reduce it by 25% in the first 8 hours, then gradually over systematic review and meta-regression analysis. Circulation 2008;117(25):3171-
24 - 48 hours. Hypertensive urgencies can be treated with oral or 3180. https://doi.org/10.1161/circulationaha.107.730366
5. Noubiap JJ, Essouma M, Bigna JJ, Jingi AM, Aminde LN, Nansseu JR.
intravenous antihypertensives.[15] The recommended intravenous Prevalence of elevated blood pressure in children and adolescents in Africa: A
drugs include esmolol, hydralazine, labetalol, nicardipine and systematic review and meta-analysis. Lancet Pub Health 2017;2(8):e375-e386.
sodium nitroprusside.[15] In the present study, almost 90% of https://doi.org/10.1016/s2468-2667(17)30123-8
patients with hypertensive crisis had hypertensive emergencies, 6. Bhimma R, Pillay M, Naidoo D, Vanden Burg MF, Smuts P, Onia R. Hypertension
prevalence and risk factors in children and adolescents of school-going age in
yet only 36% were treated with intravenous antihypertensives. The the Phoenix Area, Durban, South Africa. Pediatr Nephrol 2014;29:2434.
most commonly used antihypertensive was oral nifedipine. The 7. Meyers AM. Promotion of kidney care in countries with limited resources:
reason for the limited use of intravenous antihypertensives is that How does the National Kidney Foundation of South Africa fare? Clin Nephrol
2016;86(Suppl 1):S69-S73. https://doi.org/10.5414/cnp86s111
the majority of patients were treated in a general ward, owing to 8. Monyeki KD, Kemper HCG, Makgae PJ. The association of fat patterning
limited space in the intensive care unit. In the general ward, close with blood pressure in rural South African children: The Ellisras Longitudinal
intensive BP monitoring is not possible, owing to limited staff and Growth and Health Study. Int J Epidemiol 2006;35(1):114-120. https://doi.
org/10.1093/ije/dyi219
equipment, hence the use of oral nifedipine, which is also more 9. Nkeh-Chungag BN, Sekokotla AM, Sewani-Rusike C, Namugowa A, Iputo JE.
readily available and is more easily administered in a general care Prevalence of hypertension and pre-hypertension in 13-17 year old adolescents
setting. living in Mthatha – South Africa: A cross-sectional study. Cent Eur J Public
Health 2015;23(1):59-64. https://doi.org/10.21101/cejph.a3922
The strengths of the current study are that it was carried out over 10. Moselakgomo VK, Toriola AL, Shaw BS, Goon DT, Akinyemi O. [Body mass
a long period of time and a significantly large number of patients index, overweight, and blood pressure among adolescent schoolchildren in
were included in the study. A limitation of the study is that it was Limpopo province, South Africa.] Rev Paul Pediatr 2012;30(4):562-569. https://
conducted at a single centre and not all parameters, such as LVH doi.org/10.1590/S0103-05822012000400015
11. Schutte AE, Van Rooyen JM, Huisman HW, Kruger HS, Malan NT, de Ridder
and retinopathy, were assessed in every patient (Fig. 3). This limits JH . Dietary risk markers that contribute to the aetiology of hypertension in
the conclusions that can be drawn from some of the data obtained. black South African children: The THUSA BANA study. J Hum Hypertens
Another limitation of the study is that, being retrospective, the actual 2013:17(1):29-35. https://doi.org/10.1038/sj.jhh.1001508
12. Spagnolo A, Giussani M, Ambruzzi AM, et al. Focus on prevention, diagnosis
technique of BP measurement in the children may not have been and treatment of hypertension in children and adolescents. Ital J Pediatr
standardised over the period. 2013;39(1):20. https://doi.org/10.1186/1824-7288-39-20
47 SAJCH APRIL 2019 Vol. 13 No. 1
ARTICLE
13. Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity 24. Gupta-Malhotra M, Banker A, Shete S, et al. Essential hypertension v. secondary
and the prevalence of hypertension in school-aged children. Pediatrics hypertension among children. Am J Hypertens 2015;28(1):73-80. https://doi.
2004;113(3):475-482. https://doi.org/10.1542/peds.113.3.475 org/10.1093/ajh/hpu083
14. Malatesta-Muncher R, Mitsnefes MM. Management of blood pressure in 25. Gavrilovici C, Boiculese LV, Brumariu O, Dimitriu AG. Etiology and blood
children. Curr Opin Nephrol Hypertens 2012;21(3):318-322. https://doi. pressure patterns in secondary hypertension in children. Rev Med Chir Soc
org/10.1097/MNH.0b013e328351c415 Med Nat Iasi 2007;111(1):70-81.
15. National High Blood Pressure Education Program Working Group on High 26. Wyszyńska T, Cichocka E, Wieteska-Klimczak A, Jobs K, Januszewicz P. A
Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, single paediatric center experience with 1025 children with hypertension.
evaluation, and treatment of high blood pressure in children and adolescents. Acta Paediatr 1992;81(3):244-246. https://doi.org/10.1111/j.1651-2227.1992.
National Institute of Health publication 05:5267. Bethesda: National Heart, tb12213.x
Lung, and Blood Institute, 2005. 27. Sumboonnanonda A, Chongcharoensuk C, Supavekin S, Pattaragarn A.
16. Devereux RB, Dahlöf B, Gerdts E, et al. Regression of hypertensive left Persistent hypertension in Thai children: Etiologies and outcome. J Med Assoc
ventricular hypertrophy by losartan compared with atenolol: The Losartan Thai 2006;89(Suppl 2):S28-S32.
Intervention for Endpoint Reduction in Hypertension (LIFE) trial. Circulation 28. Kupferman JC, Friedman LA, Cox C, et al. BP control and left ventricular
2004;110(11):1456-1462. https://doi.org/10.1161/01.cir.0000141573.44737.5a hypertrophy regression in children with CKD. J Am Soc Nephrol
17. Flynn JT, Tullus, K. Severe hypertension in children and adolescents: Patho 2014;25(1):167-174. https://doi.org/10.1681/asn.2012121197
physiology and treatment. Pediatr Nephrol 2009;24(6):1101-1112. https://doi. 29. Hanevold C, Waller J, Daniels S, Portman R, Sorof J. The effects of obesity,
org/10.1007/s00467-008-1000-1 gender, and ethnic group on left ventricular hypertophy and geometry in
18. Flynn JT, Bradford MC, Harvey EM. Intravenous hydralazine in hospitalised hypertensive children: A collaborative study of the International Pediatric
children and adolescents with hypertension. J Pediatr 2015;168:88-92. https:// Hypertension Association. Pediatrics 2004;113(2):328-333.
doi.org/10.1016/j.jpeds.2015.07.070 30. Williams KM, Shan AN, Morrison D, Sinha MD. Hypertensive retinopathy in
19. World Health Organization. The WHO Child Growth Standards. http://www. severely hypertensive children: Demographic, clinical and ophthalmoscopic
who.int/childgrowth/standards (accessed 18 January 2018). findings from a 30-year British cohort. J Pediatr Ophthalmol Strabismus
20. World Health Organization. Growth reference 5-19 years. http://www.who.int/ 2013;50(4):222-228. https://doi.org/10.3928/01913913-20130319-01
growthref/en (accessed 18 January 2018). 31. Kupferman JC, Zafeiriou DI, Lande MB, Kirkham FJ, Pavlakis SG. Stroke and
21. World Health Organization. Training Course on Child Growth Assessment. HPT in children and adolescents. J Child Neurol 2017;32(4):408-417. https://
WHO Child Growth Standards. Interpreting Growth Indicators. http://www. doi.org/10.1177/0883073816685240
who.int/nutrition/publications/childgrowthstandards_trainingcourse/en/ 32. Yang W, Zhao L, Chen C, Wu Y, Chang Y, Wu H. First-attack paediatric
(accessed 18 January 2018). hypertensive crisis presenting to the pediatric emergency department. BMC
22. Dobson CP, Eide M, Nylund CM. Hypertension prevalence, cardiac Pediatr 2012;12(1):200. https://doi.org/10.1186/1471-2431-12-200
complications, and antihypertensive medication use in children. J Pediatr
2015;167(1):92-97. https://doi.org/10.1016/j.jpeds.2015.04.016
23. Chandar J, Zilleruelo G. Hypertensive crisis in children. Pediatr Nephrol
2012;27(5):741-751. https://doi.org/10.1007/s00467-011-1964-0 Accepted 18 June 2018.
48 SAJCH APRIL 2019 Vol. 13 No. 1
Das könnte Ihnen auch gefallen
- Hypertension in Children and Adolescents: New PerspectivesVon EverandHypertension in Children and Adolescents: New PerspectivesEmpar LurbeNoch keine Bewertungen
- Home Current Issue Past Issues About APPA Editorial Board Author InstructionsDokument2 SeitenHome Current Issue Past Issues About APPA Editorial Board Author Instructionsselvi destariaNoch keine Bewertungen
- Evaluation and Management of Elevated Blood Pressures in Hospitalized ChildrenDokument11 SeitenEvaluation and Management of Elevated Blood Pressures in Hospitalized ChildrenKhaoulapediatreNoch keine Bewertungen
- Blood Pressure Management in Children On DialysisDokument12 SeitenBlood Pressure Management in Children On DialysisinaNoch keine Bewertungen
- Hypertension and Hemodialysis: Pathophysiology and Outcomes in Adult and Pediatric PopulationsDokument12 SeitenHypertension and Hemodialysis: Pathophysiology and Outcomes in Adult and Pediatric PopulationsinaNoch keine Bewertungen
- Clinical Profile and Outcome in Children of Dengue Hemorrhagic Fever in North IndiaDokument7 SeitenClinical Profile and Outcome in Children of Dengue Hemorrhagic Fever in North IndiaAna Rosida SafwanNoch keine Bewertungen
- Updates On Pediatric Hypertension and New GuidelinesDokument11 SeitenUpdates On Pediatric Hypertension and New GuidelinesLuis Herrero SierraNoch keine Bewertungen
- Paediatrica Indonesiana: Sherly Yuniarchan, Risky Vitria Prasetyo, Ninik Asmaningsih Soemyarso, Mohammad Sjaifullah NoerDokument6 SeitenPaediatrica Indonesiana: Sherly Yuniarchan, Risky Vitria Prasetyo, Ninik Asmaningsih Soemyarso, Mohammad Sjaifullah NoerKimberly MilaranNoch keine Bewertungen
- Hypertension ThesisDokument31 SeitenHypertension ThesisNavin AdhikariNoch keine Bewertungen
- Review: Orit Pinhas-Hamiel, Philip ZeitlerDokument9 SeitenReview: Orit Pinhas-Hamiel, Philip ZeitlerNadhifaNoch keine Bewertungen
- Hypertension in Adolescents and Young Adults Referred To A Tertiary Hypertension Clinic in Cape Town, South AfricaDokument5 SeitenHypertension in Adolescents and Young Adults Referred To A Tertiary Hypertension Clinic in Cape Town, South AfricahanifahNoch keine Bewertungen
- NewbornDokument11 SeitenNewbornahmed KhattabNoch keine Bewertungen
- Left Ventricular Diastolic Dysfunction Among Youth With Obesity and History of Elevated Blood PressureDokument8 SeitenLeft Ventricular Diastolic Dysfunction Among Youth With Obesity and History of Elevated Blood PressureVedith KumarNoch keine Bewertungen
- HT PD Anak IsiDokument23 SeitenHT PD Anak IsiMade WirabhawaNoch keine Bewertungen
- Advances in PediatricsDokument15 SeitenAdvances in PediatricsMaria Carolina FallaNoch keine Bewertungen
- Heart Rate Characteristics and Clinical Signs in Neonatal SepsisDokument6 SeitenHeart Rate Characteristics and Clinical Signs in Neonatal SepsisDamal An NasherNoch keine Bewertungen
- Gruber2015 Article IncreasedRiskOfSevereDiabeticKDokument7 SeitenGruber2015 Article IncreasedRiskOfSevereDiabeticKnoah87Noch keine Bewertungen
- Prevalence and Major Risk Factors of Diabetic Retinopathy: A Cross-Sectional Study in EcuadorDokument5 SeitenPrevalence and Major Risk Factors of Diabetic Retinopathy: A Cross-Sectional Study in EcuadorJorge Andres Talledo DelgadoNoch keine Bewertungen
- Hypertension Management in Transition From CKD A ERDS 2016Dokument7 SeitenHypertension Management in Transition From CKD A ERDS 2016hemer hadyn calderon alvitesNoch keine Bewertungen
- Severe Hypertension in Children and Adolescents: Pathophysiology and TreatmentDokument13 SeitenSevere Hypertension in Children and Adolescents: Pathophysiology and Treatmentagustinaw1981Noch keine Bewertungen
- Emergency Department Management of Pediatric Patients With Cyanotic Heart Disease and FeverDokument8 SeitenEmergency Department Management of Pediatric Patients With Cyanotic Heart Disease and FeverRizky Ferrian FerdiansyahNoch keine Bewertungen
- Obesity, Metabolic Syndrom and Primary HypertensionDokument13 SeitenObesity, Metabolic Syndrom and Primary HypertensionHasriani rijalNoch keine Bewertungen
- Essential Hypertension in Ten & Half Years Old Boy: A Case ReportDokument3 SeitenEssential Hypertension in Ten & Half Years Old Boy: A Case ReportYunika ArumNoch keine Bewertungen
- Heartasia 2016 010847Dokument7 SeitenHeartasia 2016 010847Neneng HumairohNoch keine Bewertungen
- Pediatric Hypertension: Why The Rise in Childhood Hypertension?Dokument9 SeitenPediatric Hypertension: Why The Rise in Childhood Hypertension?Peace ManNoch keine Bewertungen
- Drchirag Hypertension NoteDokument61 SeitenDrchirag Hypertension NoteChirag PatelNoch keine Bewertungen
- Clinical Characteristics of Hyperglycemic Crises in Patients Without A History of DiabetesDokument6 SeitenClinical Characteristics of Hyperglycemic Crises in Patients Without A History of DiabetesDewanggaWahyuPrajaNoch keine Bewertungen
- Epidemiology - Diabetes and Kidney Disease PDFDokument12 SeitenEpidemiology - Diabetes and Kidney Disease PDFSharyna EmyraNoch keine Bewertungen
- Out 2Dokument9 SeitenOut 2Ririn OktavianiNoch keine Bewertungen
- Hypertension Knowledge, Attitude, and Practice in Adult Hypertensive Patients at A Tertiary Care Hospital in Sri LankaDokument11 SeitenHypertension Knowledge, Attitude, and Practice in Adult Hypertensive Patients at A Tertiary Care Hospital in Sri LankaBrian TaylorNoch keine Bewertungen
- Hypertensive CrisisDokument11 SeitenHypertensive CrisisRachmat Wihandana AgasiNoch keine Bewertungen
- Quality of Life of Children With Type 1 Diabetes: A Systematic ReviewDokument12 SeitenQuality of Life of Children With Type 1 Diabetes: A Systematic ReviewNila Sari ChandraNoch keine Bewertungen
- Cherfan 2018Dokument13 SeitenCherfan 2018Maya ElrifaiNoch keine Bewertungen
- Increased Risk of Hyperlipidemia in BPDDokument5 SeitenIncreased Risk of Hyperlipidemia in BPDRebecca SilaenNoch keine Bewertungen
- Hypertension in Infancy: Diagnosis, Management and Outcome: ReviewDokument16 SeitenHypertension in Infancy: Diagnosis, Management and Outcome: ReviewJulio César Valdivieso AguirreNoch keine Bewertungen
- A Study of 50 Cases of Hepatorenal: Syndrome and Its OutcomeDokument16 SeitenA Study of 50 Cases of Hepatorenal: Syndrome and Its OutcomeRishabh GuptaNoch keine Bewertungen
- HiertensiDokument2 SeitenHiertensiCindy AmeLiyana Part IINoch keine Bewertungen
- Vasudevan 2022 Oi 221113 1666636847.63456Dokument13 SeitenVasudevan 2022 Oi 221113 1666636847.63456Sabrina NMNoch keine Bewertungen
- Effect of Congenital Heart Disease On Child Growth: Dr. Deia K Khalaf, Dr. Yusra K Al-Rawi and Dr. Laith A Abdul HadiDokument7 SeitenEffect of Congenital Heart Disease On Child Growth: Dr. Deia K Khalaf, Dr. Yusra K Al-Rawi and Dr. Laith A Abdul HadimuhammadrikiNoch keine Bewertungen
- The Prevalence of ArterialDokument8 SeitenThe Prevalence of ArterialInternational Medical PublisherNoch keine Bewertungen
- BPJ Vol 11 No 2 P 821-825Dokument5 SeitenBPJ Vol 11 No 2 P 821-825hendriNoch keine Bewertungen
- Risk Factors For Hypertension and Its Complications Case Control StudyDokument4 SeitenRisk Factors For Hypertension and Its Complications Case Control StudyutarinuNoch keine Bewertungen
- 14 PDFDokument3 Seiten14 PDFAnonymous bx7YQvNoch keine Bewertungen
- Blood Pressure Measurement in Children andDokument7 SeitenBlood Pressure Measurement in Children andHartanto SantosoNoch keine Bewertungen
- 63 - Original ArticleDokument5 Seiten63 - Original ArticlechairulNoch keine Bewertungen
- Predictors of Intradialytic Hypertension in Chronic End Stage Renal Dialysis Patients in A Tertiary Government Hospital in Davao CDokument13 SeitenPredictors of Intradialytic Hypertension in Chronic End Stage Renal Dialysis Patients in A Tertiary Government Hospital in Davao CSari ChaerunisahNoch keine Bewertungen
- Evaluation of Hypertension in Children and AdolescentsDokument31 SeitenEvaluation of Hypertension in Children and AdolescentsSérgio100% (1)
- Tgs Jurnal 1Dokument7 SeitenTgs Jurnal 1suciNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument24 SeitenNIH Public Access: Author ManuscriptireneaureliaNoch keine Bewertungen
- ALERGYDokument6 SeitenALERGYReZa FriscaNoch keine Bewertungen
- Manejo Hta Unidad Cuidados Criticos PediátricoDokument9 SeitenManejo Hta Unidad Cuidados Criticos PediátricoCatalina Cruz NunjaNoch keine Bewertungen
- 2022 Article 1378Dokument10 Seiten2022 Article 1378Sari RakhmawatiNoch keine Bewertungen
- Hypertension 2015 Falkner 926 31Dokument7 SeitenHypertension 2015 Falkner 926 31Carlos Abuhadba MirandaNoch keine Bewertungen
- Undiagnosed Diabetes and Hypertension in Patients at A Private Dental Clinic in Saudi ArabiaDokument5 SeitenUndiagnosed Diabetes and Hypertension in Patients at A Private Dental Clinic in Saudi ArabiaDentalLearningNoch keine Bewertungen
- Hypertensive Emergencies and Urgencies In.800Dokument1 SeiteHypertensive Emergencies and Urgencies In.800Laura J LlanoNoch keine Bewertungen
- Evaluation of Therapeutic Adherence Among Moroccan Hypertensive Patients About 1482 CasesDokument9 SeitenEvaluation of Therapeutic Adherence Among Moroccan Hypertensive Patients About 1482 CasesAthenaeum Scientific PublishersNoch keine Bewertungen
- 2024 PN DG of HTN DingDokument7 Seiten2024 PN DG of HTN DingАлександра ЛазићNoch keine Bewertungen
- Ref 32 Impact Hiperglikemia Pada ALLDokument5 SeitenRef 32 Impact Hiperglikemia Pada ALLmuarifNoch keine Bewertungen
- Evaluation of Medical Care For Diabetic and Hypertensive Patients in Primary Care in Mexico: Observational Retrospective StudyDokument7 SeitenEvaluation of Medical Care For Diabetic and Hypertensive Patients in Primary Care in Mexico: Observational Retrospective StudyMirna Liliana Carmona GarciaNoch keine Bewertungen
- Association of Severe Stunting in Indigenous Yanomami Children With Maternal Short Stature: Clues About The Intergerational TransmissionDokument10 SeitenAssociation of Severe Stunting in Indigenous Yanomami Children With Maternal Short Stature: Clues About The Intergerational TransmissionyutefupNoch keine Bewertungen
- Public Prosecutor's Office and Social Control in The National Unified Health System: A Systematic ReviewDokument10 SeitenPublic Prosecutor's Office and Social Control in The National Unified Health System: A Systematic ReviewyutefupNoch keine Bewertungen
- Studies Assessing Food Consumption by The Scores Method: A Systematic ReviewDokument16 SeitenStudies Assessing Food Consumption by The Scores Method: A Systematic ReviewyutefupNoch keine Bewertungen
- Factors Associated With A Shorter Duration of Breastfeeding: Key Words Breastfeeding, Epidemiology, ChildDokument10 SeitenFactors Associated With A Shorter Duration of Breastfeeding: Key Words Breastfeeding, Epidemiology, ChildyutefupNoch keine Bewertungen
- Challenges Facing HIV Treatment As Prevention in Brazil: An Analysis Drawing On Literature On TestingDokument16 SeitenChallenges Facing HIV Treatment As Prevention in Brazil: An Analysis Drawing On Literature On TestingyutefupNoch keine Bewertungen
- Temporomandibular Joint Dysfunction Syndrome and Police Work Stress: An Integrative ReviewDokument14 SeitenTemporomandibular Joint Dysfunction Syndrome and Police Work Stress: An Integrative ReviewyutefupNoch keine Bewertungen
- Health Technology Assessment in Brazil - An International PerspectiveDokument14 SeitenHealth Technology Assessment in Brazil - An International PerspectiveyutefupNoch keine Bewertungen
- The Implementation of Senior Health Care in The Family Health Strategy: The View of Professionals and ManagersDokument10 SeitenThe Implementation of Senior Health Care in The Family Health Strategy: The View of Professionals and ManagersyutefupNoch keine Bewertungen
- Ways of Seeing and Doing: Health, Disease and Care in Marketers' Family UnitsDokument10 SeitenWays of Seeing and Doing: Health, Disease and Care in Marketers' Family UnitsyutefupNoch keine Bewertungen
- Physiotherapy For New Actors: Disputes and Innovations in Care For Chronically Ill ChildrenDokument10 SeitenPhysiotherapy For New Actors: Disputes and Innovations in Care For Chronically Ill ChildrenyutefupNoch keine Bewertungen
- Engaging People With Chronic Kidney Disease in Their Own Care An Integrative ReviewDokument10 SeitenEngaging People With Chronic Kidney Disease in Their Own Care An Integrative ReviewyutefupNoch keine Bewertungen
- Coping With Problems That Impact On The Health of A Socially Vulnerable Community From The Residents' PerspectiveDokument10 SeitenCoping With Problems That Impact On The Health of A Socially Vulnerable Community From The Residents' PerspectiveyutefupNoch keine Bewertungen
- En - 1413 8123 CSC 24 05 1699Dokument10 SeitenEn - 1413 8123 CSC 24 05 1699yutefupNoch keine Bewertungen
- En - 1413 8123 CSC 24 05 1585Dokument12 SeitenEn - 1413 8123 CSC 24 05 1585yutefupNoch keine Bewertungen
- Inequality, Difference, Articulation: Sergio CostaDokument14 SeitenInequality, Difference, Articulation: Sergio CostayutefupNoch keine Bewertungen
- Effects of PH, Temperature and Agitation On The Decolourisation of Dyes by Laccase-Containing Enzyme Preparation From Pleurotus Sajor-CajuDokument21 SeitenEffects of PH, Temperature and Agitation On The Decolourisation of Dyes by Laccase-Containing Enzyme Preparation From Pleurotus Sajor-CajuyutefupNoch keine Bewertungen
- THE RACIAL STATE OF THE UNION: Understanding Race and Racial Inequality in The United States of AmericaDokument16 SeitenTHE RACIAL STATE OF THE UNION: Understanding Race and Racial Inequality in The United States of AmericayutefupNoch keine Bewertungen
- Microalgae: Cultivation Aspects and Bioactive Compounds: Review - Biological and Applied SciencesDokument13 SeitenMicroalgae: Cultivation Aspects and Bioactive Compounds: Review - Biological and Applied SciencesyutefupNoch keine Bewertungen
- Development and Psychometric Properties of TQWL-42 To Measure The Quality of Work LifeDokument9 SeitenDevelopment and Psychometric Properties of TQWL-42 To Measure The Quality of Work LifeyutefupNoch keine Bewertungen
- Pseudomonas Aeruginosa: Virulence Factors: and Antibiotic Resistance GenesDokument15 SeitenPseudomonas Aeruginosa: Virulence Factors: and Antibiotic Resistance GenesyutefupNoch keine Bewertungen
- Gut: Key Element On Immune System Regulation: Review - Human and Animal HealthDokument14 SeitenGut: Key Element On Immune System Regulation: Review - Human and Animal HealthyutefupNoch keine Bewertungen
- 1516 8913 Babt 62 E19180470Dokument14 Seiten1516 8913 Babt 62 E19180470yutefupNoch keine Bewertungen
- Use of Inert Gases For The Preservation of Nuclear Blood CellsDokument7 SeitenUse of Inert Gases For The Preservation of Nuclear Blood CellsyutefupNoch keine Bewertungen
- Walker-256 Tumor: Experimental Model, Implantation Sites and Number of Cells For Ascitic and Solid Tumor DevelopmentDokument13 SeitenWalker-256 Tumor: Experimental Model, Implantation Sites and Number of Cells For Ascitic and Solid Tumor DevelopmentyutefupNoch keine Bewertungen
- Population Changes of Eubacteria, Sulfate-Reducing Bacteria and Methanogenic Archaea in An Anaerobic Reactor Processing Ethanol Distillery VinasseDokument13 SeitenPopulation Changes of Eubacteria, Sulfate-Reducing Bacteria and Methanogenic Archaea in An Anaerobic Reactor Processing Ethanol Distillery VinasseyutefupNoch keine Bewertungen
- 1516 8913 Babt 62 E19180259Dokument10 Seiten1516 8913 Babt 62 E19180259yutefupNoch keine Bewertungen
- In Silico Characterization of Meloidogyne Genus: Nematode Cellulose Binding ProteinsDokument13 SeitenIn Silico Characterization of Meloidogyne Genus: Nematode Cellulose Binding ProteinsyutefupNoch keine Bewertungen
- Microscale Direct Transesterification of Microbial Biomass With Ethanol For Screening of Microorganisms by Its Fatty Acid ContentDokument11 SeitenMicroscale Direct Transesterification of Microbial Biomass With Ethanol For Screening of Microorganisms by Its Fatty Acid ContentyutefupNoch keine Bewertungen
- 1516 8913 Babt 62 E19180198Dokument12 Seiten1516 8913 Babt 62 E19180198yutefupNoch keine Bewertungen
- Area Triangulation Method For Automatic Detection of Venous Emptying ManeuversDokument11 SeitenArea Triangulation Method For Automatic Detection of Venous Emptying ManeuversyutefupNoch keine Bewertungen
- Patients' Perceptions of Barriers To Self-Managing Bipolar DisorderDokument10 SeitenPatients' Perceptions of Barriers To Self-Managing Bipolar DisorderMilton MurilloNoch keine Bewertungen
- Retro VirDokument3 SeitenRetro VirJericho MangalinNoch keine Bewertungen
- ECGC PO Descriptive BookDokument74 SeitenECGC PO Descriptive BookAmar Pandey100% (2)
- De So 3Dokument6 SeitenDe So 3To Minh PhuongNoch keine Bewertungen
- CALGB Schema FinalDokument1 SeiteCALGB Schema FinalMohamed MahmoudNoch keine Bewertungen
- Left Thigh Pain: I. Chief Complaint/ Other ComplaintsDokument9 SeitenLeft Thigh Pain: I. Chief Complaint/ Other ComplaintsDominic BristolNoch keine Bewertungen
- Circulatory System QuestionsDokument4 SeitenCirculatory System QuestionsJohn Vincent Gonzales50% (2)
- Phytochemical Analysis, Antimicrobial and Antioxidant Activities of Euphorbia Juss.) : An Unexplored Medicinal Herb Reported From CameroonDokument15 SeitenPhytochemical Analysis, Antimicrobial and Antioxidant Activities of Euphorbia Juss.) : An Unexplored Medicinal Herb Reported From CameroonClara JamirNoch keine Bewertungen
- Alpha Thalassemia PDFDokument21 SeitenAlpha Thalassemia PDFAnonymous Yo0mStNoch keine Bewertungen
- Belgian MalinoisDokument9 SeitenBelgian MalinoislordnrNoch keine Bewertungen
- Regulation of Iron MetabolismDokument21 SeitenRegulation of Iron MetabolismElita Maritan SNoch keine Bewertungen
- Application For Life and Health Insurance ToDokument5 SeitenApplication For Life and Health Insurance Toimi_swimNoch keine Bewertungen
- Foot and Ankle Injuries Kylee Phillips - 0Dokument74 SeitenFoot and Ankle Injuries Kylee Phillips - 0rizwan.mughal1997Noch keine Bewertungen
- Spontaneous Pneumothorax - Management Feb15Dokument12 SeitenSpontaneous Pneumothorax - Management Feb15samuelNoch keine Bewertungen
- Curs 1 Introducere EndodontieDokument24 SeitenCurs 1 Introducere EndodontieVlahul VladNoch keine Bewertungen
- Wild and Ancient Fruit - Is It Really Small, Bitter, and Low in Sugar - Raw Food SOSDokument73 SeitenWild and Ancient Fruit - Is It Really Small, Bitter, and Low in Sugar - Raw Food SOSVictor ResendizNoch keine Bewertungen
- Gingival Inflammation in Mouth Breathing PatientsDokument5 SeitenGingival Inflammation in Mouth Breathing PatientsCamiLunaNoch keine Bewertungen
- Community Theatre and AIDS Studies in International Performance PDFDokument194 SeitenCommunity Theatre and AIDS Studies in International Performance PDFgabriella feliciaNoch keine Bewertungen
- Keep Fit For Life: Meeting The Nutritional Needs of Older PersonsDokument83 SeitenKeep Fit For Life: Meeting The Nutritional Needs of Older Personsapi-342482642Noch keine Bewertungen
- 536 BPG Assessment Foot Ulcer 1Dokument115 Seiten536 BPG Assessment Foot Ulcer 1FebricaPutriArthaNoch keine Bewertungen
- Microbial SafariDokument5 SeitenMicrobial SafariClauu VargasNoch keine Bewertungen
- Bilirubin Metabolism Jaundice PPP 9Dokument27 SeitenBilirubin Metabolism Jaundice PPP 9Regina Marsha Xaveria100% (1)
- Certificate of Analysis, Quality and Conformity: Certified: ISO 9001:2008, ISO 13485-2003 and WHO GMPDokument3 SeitenCertificate of Analysis, Quality and Conformity: Certified: ISO 9001:2008, ISO 13485-2003 and WHO GMPMitha AriantiNoch keine Bewertungen
- Hse Statistics Report Pp701 Hse f04 Rev.bDokument1 SeiteHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Bird Nets PDFDokument4 SeitenBird Nets PDFPaul LawlessNoch keine Bewertungen
- Magic of The Minimum Dose PDFDokument221 SeitenMagic of The Minimum Dose PDFminunat100% (1)
- General Profile: - Pa - 6mos Old - Female - Filipino - Roman Catholic - Alang-Alang Mandaue CityDokument18 SeitenGeneral Profile: - Pa - 6mos Old - Female - Filipino - Roman Catholic - Alang-Alang Mandaue CityRj FornollesNoch keine Bewertungen
- Syphilis: Jessica Lyons Period D STD Project 4/22/13Dokument3 SeitenSyphilis: Jessica Lyons Period D STD Project 4/22/13jesssielynnn33Noch keine Bewertungen
- Child Protection Training ManualDokument229 SeitenChild Protection Training Manualbabuin1Noch keine Bewertungen
- Full Download Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhy PDF Full ChapterDokument36 SeitenFull Download Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhy PDF Full Chapteradrianblackiadxetkrqm100% (15)