Beruflich Dokumente
Kultur Dokumente
Patho Supplement Handout For Sept 2018 UPDATED May 2018 PDF
Hochgeladen von
emely p. tangoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Patho Supplement Handout For Sept 2018 UPDATED May 2018 PDF
Hochgeladen von
emely p. tangoCopyright:
Verfügbare Formate
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
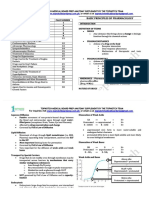
pPLEASE READ BEFORE PROCEEDING Features Necrosis Apoptosis
Cell size Enlarged (swelling) Reduced (shrinkage)
In response to the trend of the Pathology board examinations, Nucleus Pyknosis → Karyorrhexis Fragmentation into
wherein the examinations test the student's ability to diagnose different → Karyolysis nucleosome-sized
diseases through case-based questions, the "Patho Supertable" has now fragments
been redesigned and renamed into "Patho Supplement Handout" that Plasma Disrupted Intact; altered structure,
focuses on how to diagnose certain diseases, based on clinical clues and membrane especially orientation of
morphologic findings; the said change is most evident in the systemic lipids
pathology part. Because the handout has changed its focus and its utility, Cellular Enzymatic digestion; may Intact; maybe released in
it cannot be used as an alternative to the main handout. You can consider contents leak out of cell apoptotic bodies
this as a study outline or guide--that if a concept or a disease appears Adjacent Frequent No
here, then you should study that disease in detail; because the exam inflammation
might ask for concepts related to that disease. The supplement handout Physiologic or Invariably pathologic Often physiologic; may be
provides an avenue for you to apply the concepts in the main handout, by pathologic role pathologic
diagnosing cases.
FORMS OF NECROSIS
To the one who uses this, I hope that you will become a great
Component cells are dead but the basic tissue Coagulative
physician, and become an agent of positive change in this world. You are
architecture is PRESERVED ("acidophilic necrosis
always in my prayers. Good luck! :)
tombstone"); often seen in ischemic injury to most
solid organs (heart, spleen, kidney) EXCEPT the
Kevin A. Elomina, MD
brain
Pathology Resident, Mentor, and Instructor
Facebook: Kevin Elomina Digestion of dead cells, resulting in transformation of Liquefactive
Instagram: @keielomina the tissue into a viscous liquid mass; often seen in necrosis
infections (pus) and in hypoxic death of cells within
PATHO SUPPLEMENT HANDOUT the CNS
The term reserved for ischemic coagulative necrosis Gangrenous
PART I: GENERAL PATHOLOGY of the limbs (dry); may have superimposed bacterial necrosis
1. CELLULAR RESPONSES TO STRESS infection with liquefactive necrosis (wet)
QUESTION ANSWER Cheese-like gross appearance of necrotic areas; often Caseous
CELLULAR ADAPTATION seen in tuberculous infections; tissue architecture is necrosis
Increase in SIZE of cells resulting in increased size of Hypertrophy NOT PRESERVED
organ; cellular adaptation of non-dividing cells e.g. Focal areas of fat destruction, typically seen in acute Enzymatic fat
myocardial fibers pancreatitis; foci of necrosis contain shadowy necrosis
Increase in NUMBER of cells Hyperplasia outlines of necrotic fat cells with basophilic calcium
REDUCTION in cell SIZE and NUMBER resulting in Atrophy deposits (saponification), surrounded by an
decreased size of organ inflammatory reaction
A REVERSIBLE change wherein one differentiated Metaplasia Seen in immune reactions involving blood vessels; Fibrinoid
cell type is replaced by another cell type deposits of immune complexes, together with fibrin necrosis
PRACTICE CASES that have leaked out of vessels, result in a bright pink
and amorphous appearance
55/M, with long-standing history of hypertension, Myocardial
eventually expired from myocardial infarction. infarction; Left
Autopsy: increased thickness of the left ventricular ventricular TYPES OF APOPTOSIS (INIATOR PATHWAYS)
wall with large areas of fibrotic scars. What is the hypertrophy; Inactivation of anti-apoptotic BCL2 protein that Intrinsic
diagnosis, and what cellular adaptation is seen in this Pathologic leads to activation of BAX/BAK channel, allowing (mitochondrial)
case? hypertrophy cytochrome c to leak out of the mitochondria, pathway
47 G0, with granulosa cell tumor, presented with Complex activating apoptosis
menorrhagia. UTZ showed thickened endometrium. atypical Activation of "death receptors" by appropriate Extrinsic (Death
Patient underwent diagnostic curettage. Biopsy hyperplasia; ligands that leads to activation of apoptosis receptor)
showed back-to-back endometrial glands with Pathologic pathway
nuclear atypia. What is the diagnosis (for the hyperplasia
endometrium), and what cellular adaptation is seen TYPES OF CALCIFICATIONS
in this case? Calcium deposition occurring in dead tissues, in the Dystrophic
35/M, with history of poliomyelitis, presented with Denervation absence of calcium metabolic derangements; calcification
disproportionately thinner right lower extremity. atrophy; examples: Psammoma bodies in cancers with
Muscle biopsy showed decrease in size of skeletal Pathologic papillary architecture, and meningioma
myocytes. What is the cellular adaptation seen in this atrophy Calcium deposition in normal tissues occurring in Metastatic
case? the setting of hypercalcemia; example: Calcinosis calcification
39/F, with long-standing history of heartburn and Barrett
water brash. Endoscopy showed multiple pinkish- esophagus; 2. INFLAMMATION AND REPAIR
tan areas at the GEJ. Biopsy showed fragments with Intestinal QUESTION ANSWER
simple columnar epithelium with goblet cells. What metaplasia
GENERAL CONCEPTS
is the diagnosis, and what specific cellular adaptation
Response of vascularized tissues to infections and Inflammation
is seen in this case?
damaged tissues that brings cells and molecules of
host defense from the circulation to the sites where
FORMS OF REVERSIBLE CELL INJURY they are needed, in order to eliminate the offending
The first manifestation of almost all forms of Cellular agent
injury to cells; change is due to influx of ions (and swelling
The initial response to infections and tissue damage Acute
consequently, water) due to failure of energy- inflammation
dependent ion pumps (Na+-K+-ATPase)
Inflammatory response of prolonged duration in which Chronic
Appearance of lipid vacuoles in the cytoplasm; often Steatosis inflammation, tissue injury, and attempts at repair inflammation
seen in cells participating in fat metabolism (liver,
coexist, in varying combinations
heart)
Restoration of tissue architecture and function after Tissue repair
and injury
TYPES OF CELL DEATH
Type of cell death that results from a pathologic cell Necrosis GENERAL TYPES OF INFLAMMATION
injury Feature Acute Chronic
Type of cell death that is energy-dependent, tightly Apoptosis Onset Fast: minutes or hours Slow; days
regulated, and associated with normal cellular
Cellular infiltrate Mainly neutrophils Monocytes/macropha
functions; often physiologic; "programmed cell
ges and lymphocytes
death"
Tissue injury, Usually mild and self- Often severe and
fibrosis limited progressive
Local and systemic Prominent Less
signs
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 1 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
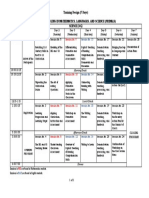
ACUTE INFLAMMATION CHRONIC INFLAMMATION
Components of acute inflammation 1. Dilation of small vessels Main cells involved in chronic inflammation 1. Macrophages
2. Increased microvascular 2. Lymphocytes
permeability Collections of activated macrophages; some of Granuloma
3. Emigration of leukocytes and which form multinucleated giant cells, often with
their activation T lymphocytes, and sometimes associated with
Initial vascular response to injury Vasoconstriction central necrosis
Most notable mediator that Histamine Two kinds of cells seen in granulomas 1. Epithelioid cells
produces vasodilation; stored in 2. Giant cells
mast cells, platelets, and basophils Precursor cell of epithelioid cells and giant cells Macrophages
Most common mechanism of Endothelial cell contraction
increased microvascular REPAIR
permeability in acute inflammation Type of tissue whose cells can readily Labile tissues
Morphologic hallmarks of acute 1. Vasodilation regenerate as long as the pool of stem cells is
inflammation 2. Accumulation of leukocytes preserved; examples: Bone Marrow and
and fluid in the extravascular Vaginal Epithelium
tissue Type of tissue whose cells are quiescent and Stable tissues
Outcomes of acute inflammation 1. Resolution have only minimal replicative activity in their
2. Pus formation (abscess) normal state; capable of proliferating in
3. Healing by fibrosis response to injury or loss of tissue mass;
4. Progression to chronic examples: Smooth muscles, Endothelium, and
inflammation Liver Parenchyma
RECRUITMENT OF LEUKOCYTES Type of tissue whose cells are considered to Permanent tissues
Steps in leukocyte recruitment A. Margination be terminally differentiated and are non-
B. Rolling proliferative in postnatal life; examples:
C. Adhesion Neurons and Cardiac muscle
D. Transmigration Type of repair that happens in labile and Regeneration
E. Chemotaxis stable tissues; influenced by growth factors
The process of leukocyte accumulation at the Margination Type of repair that happens in chronic, severe Connective tissue
periphery of blood vessels inflammation, and in permanent tissues deposition
Transient binding and detachment of Rolling Steps in healing by connective tissue A. Angiogenesis
leukocytes to the endothelium, mediated by deposition B. Formation of
selectins granulation tissue
Firm adhesion of leukocytes to the endothelium, Adhesion C. Remodeling of the
mediated by integrins scar
The process of migration of the leukocytes Transmigration or Most notable growth factor in angiogenesis VEGF
through the endothelium, mediated by PECAM- Diapedesis Most important cytokine for synthesis and TGF-β
1/CD31 deposition of connective tissue
Process of leukocyte migration toward sites of Chemotaxis Hallmark of repair Granulation tissue
infection or injury along a chemical gradient, Components of granulation tissue 1. Proliferation of
mediated by exogenous or endogenous fibroblasts
substances 2. Loose connective
MEDIATORS OF INFLAMMATION tissue
Type of inflammatory mediators that are Cell-derived 3. Angiogenesis
normally sequestered in intracellular granules, mediators 4. Inflammatory cells
and can be rapidly secreted by granule
exocytosis, or are synthesized de novo in
response to a stimulus; examples: Histamine,
3. HEMODYNAMIC DISORDERS
Serotonin, Cytokines, and Arachidonic acid QUESTION ANSWER
derivatives (Prostaglandins and Leukotrienes) GENERAL CONCEPTS
Type of inflammatory mediators that are Plasma-derived Accumulation of fluid in tissues or body cavities Edema (tissues)
produced mainly in the liver, and are present in mediators and effusion
the circulation as inactive precursors that must (body cavities)
be activated by proteolytic cleavage to acquire Increased blood volume within tissues Hyperemia and
their biologic properties; examples: Complement, congestion
Coagulation, and Kinin systems Pathologic counterpart of hemostasis Thrombosis
Vasoactive amine found in platelets and Serotonin A detached intravascular solid, liquid, or gaseous Embolus
neuroendocrine cells; causes vasoconstriction mass that is carried by the blood from its point of
origin to a distant site, where it often causes tissue
ARACHIDONIC ACID METABOLITES dysfunction or infarction
Action Eicosanoids Area of ischemic necrosis caused by occlusion of Infarct
Vasodilation PGI2 (Prostacyclin), PGE1, PGE2, PGD2 either the arterial supply or the venous drainage
Vasoconstriction TXA2, LTC4, D4, E4 State in which diminished cardiac output or reduced Shock
Increased vascular LTC4, D4, E4 effective circulating blood volume impairs tissue
permeability perfusion and leads to cellular hypoxia
Chemotaxis, LTB4, Hydroxyeicosatetraenoic acid (HETE)
leukocyte adhesion EDEMA AND EFFUSION
Four main mechanisms 1. Increased hydrostatic pressure
COMPLEMENT SYSTEM of edema formation 2. Decreased oncotic pressure
Most abundant complement C3 3. Increased vascular permeability
4. Lymphatic obstruction
Complement that acts as an opsonin C3b
General morphologic 1. Clearing and separation of ECM
Anaphylatoxins C3a, C4a, C5a
appearance of edema 2. Subtle cell swelling
Membrane attack complex C5b, C6-C9
PRACTICE CASES
Common complement deficiencies
58/M, with history of MI, presented with Congestive heart
Deficiency of the following complement- C1 inhibitor deficiency
paroxysmal nocturnal dyspnea and failure; Increased
related protein causes hereditary
orthopnea. CXR showed bilateral pleural hydrostatic
angioedema
effusion. What is the diagnosis, the mechanism pressure;
Deficiency of the following complement C3
of edema in this case, and the kind of effusion? Transudate
protein increases susceptibility to infections
32/M, with history of remittent fever and Parapneumonic
involving pyogenic bacteria
productive cough, developed dyspnea. CXR effusion; CAP MR;
Deficiency of the following complement C1q, C2 and C4 showed right pleural effusion with left Increased vascular
proteins increases susceptibility to immune parenchymal infiltrates. What is the permeability;
complex-mediated disease
mechanism of edema in this case, and what is Exudate
Deficiency of the following complement C5-C9 the kind of effusion?
proteins increases susceptibility to Neisseria
infections
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 2 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
57/M, chronic alcoholic, presented with Decreased oncotic Dissolution Rapid shrinkage and total disappearance of recent
increase in abdominal girth. Chemistry pressure thrombi
showed low serum albumin and elevated ALT Organization and Thrombi becomes incorporated in the vessel wall
and AST. Abdominal UTZ showed moderate recanalization with formation of new capillary channels that
ascites. What is the mechanism of edema in this restore blood flow
case?
34/F, known case of breast cancer stage 2 Lymphatic EMBOLISM
(T2N0M0), s/p MRM, left, developed left arm obstruction Most common and most dreaded sequela of deep Pulmonary
swelling. What is the mechanism of edema in venous thrombosis embolism
this case? Embolus occluding the bifurcation of the pulmonary Saddle
trunk; associated with sudden death due to acute right- embolus
TYPES OF EFFUSIONS sided heart failure
Parameter Transudate Exudate PRACTICE CASES
Pathophysiology Abnormalities in Increased vascular 65/F, known case of DVT, came from a 17-hour Pulmonary
Starling forces permeability flight, developed respiratory distress with right embolism
Vascular permeability Normal Increased ventricular wall dysfunction on 2D-Echo. What
Plasma protein leak Absent Present is the diagnosis?
Protein content of Low High 45/F, known case of thyrotoxic heart disease Systemic
fluid and chronic atrial fibrillation, developed thromboembolism
Specific gravity < 1.012 > 1.012 sudden left-sided weakness and loss of (from mural
Fibrin Absent Present sensation. What is the type of embolism thrombus)
Inflammatory cells Absent Present observed in the patient?
38/M, known case of Non-Hodgkin lymphoma, Paradoxical
HYPEREMIA AND CONGESTION developed sudden right-sided weakness. Patient embolism (Cardiac
It is an active process resulting from augmented blood Hyperemia has had a recent admission for a month, and has pathology is PFO)
flow due to arteriolar dilation or increased oxygen a history of a cardiac pathology that the
demand; affected tissue is redder than normal, because cardiologist deemed benign. What is the
of engorgement with oxygenated blood phenomenon observed in the patient?
It is a passive process resulting from impaired venous Congestion 32/M, involved in a motorcycle accident, and Fat embolism
return out of a tissue; tissue has a blue-red color due to sustained a mid-shaft right femoral fracture,
accumulation of deoxygenated blood in the affected without any blunt or penetrating head and chest
tissue trauma. Patient developed progressive
PRACTICE CASES respiratory distress, and died. Autopsy showed
24/M, with a large left atrial myxoma that obstructed Acute fat globules in pulmonary vasculature. What is
flow of blood into the left atrium, subsequently died. pulmonary the diagnosis?
Autopsy of the lung showed engorged alveolar congestion 25 G1P1(1001) developed respiratory distress, Amniotic fluid
capillaries, alveolar septal edema, and focal intra- seizures, and refractory bleeding post-partum, embolism
alveolar hemorrhage. What is the diagnosis? and died. Autopsy showed fetal skin and lanugo
34/F, died from acute right-sided heart failure Acute in pulmonary vasculature. What is the
secondary to saddle embolus. Autopsy of the liver hepatic diagnosis?
showed distended central vein and sinusoids, congestion 30/M, diver, developed respiratory distress and Air embolism
centrilobular ischemic necrosis, and periportal fatty joint pain after rapid ascent. Work-up showed (Decompression
change. What is the diagnosis? gas bubbles in pulmonary vasculature and sickness)
55/M, died of complications from congestive heart Chronic joints. What is the diagnosis?
failure. Autopsy of the lung showed thickened and passive
fibrotic alveolar septa, and hemosiderin-laden congestion, INFARCT
macrophages. What is the diagnosis? lung Infarcts that tend to occur in loose tissues and in Red
60/M, died of complications from heart failure. On Chronic those with dual circulations, previously congested (hemorrhagic)
autopsy, liver is heavier than normal and has a nutmeg- passive tissues, or when flow is reestablished after an infarct
like appearance. Sections show centrilobular congestion, infarction (i.e. after angioplasty of obstructed
hemorrhage, hemosiderin-laden macrophages, and liver artery); examples: Pulmonary and Bowel infarcts
hepatocyte loss of variable degrees. What is the Infarcts that tend to occur in solid organs with end- White
diagnosis? arterial circulations; examples: Myocardial and (anemic)
Splenic infarcts infarct
THROMBOSIS
Components of Virchow triad Endothelial injury, SHOCK
(abnormalities that lead to thrombus Stasis, 55/M, known case of massive MI, developed Cardiogenic shock
formation) Hypercoagulability ventricular fibrillation, and died. What kind of
It is a major contributor to the development Turbulence or shock did the patient suffer from?
of arterial thrombi endothelial injury 65/M, with ruptured abdominal aortic Hypovolemic
It is a major contributor to the development Stasis aneurysm, died. What kind of shock did the shock
of venous thrombi patient suffer from?
Any alteration of the coagulation pathway Hypercoagulability 23/M, college student and dormer, developed Meningococcemia;
that predisposes to thrombosis; can be cough and colds for 2 days, followed by Septic shock
primary (e.g. Factor V Leiden, Protein C and S remittent high-grade fever, with dusky
deficiency) or secondary (e.g. Cancer, atrial ecchymoses on the lower extremities. At ER,
fibrillation, and prolonged immobilization) patient was stuporous with BP = 50 palpatory.
Laminations composed of pale platelet and Lines of Zahn What is the diagnosis, and the kind of shock did
fibrin deposits alternating with darker red the patient suffer from?
cell-rich layers; signify formation of 25/F, suffered from a bee sting, developed Anaphylactic
thrombus in flowing blood; present in generalized wheals, periorbital edema, and shock
antemortem thrombosis respiratory distress. At ER, BP = 70/50. What
Most common site of arterial thrombosis Coronary > cerebral > kind of shock did the patient suffer from?
femoral 28/F, suffered from a blunt trauma of the back Neurogenic shock
Most common site of venous thrombosis Superficial or deep after a vehicular accident, was hypotensive for
veins of the leg several days, and was started on vasopressors
Note: Thrombi in superficial for management. What kind of shock did the
leg veins rarely embolize, patient suffer from?
while thrombi in deep leg
veins are the most common
sources of venous emboli
FATES OF THROMBUS
Fate Definition
Propagation Thrombi accumulate additional platelets and fibrin
Embolization Thrombi dislodge and travel to other sites in the
vasculature
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 3 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
4. GENETIC DISORDERS 21; involves CGG expansion in FMR1 gene in X- syndrome
chromosome; most distinctive feature is macro-
QUESTION ANSWER
orchidism
MENDELIAN DISORDERS
Autosomal dominant neurodegenerative Huntington
One dominant allele is enough to produce Autosomal
disorder; CAG expansion on HTT gene on Ch4; disease
phenotype (heterozygous); diseases with mutations in dominant
relentlessly progressive and uniformly fatal
key structural proteins/receptors are usually
inherited in this manner; examples: Huntington
DISORDERS OF GENOMIC IMPRINTING
disease, Neurofibromatosis, Myotonic dystrophy,
Tuberous sclerosis complex, ADPKD, Familial polyposis Deletion in paternally derived Chromosome 15; Prader-Willi
coli, Hereditary spherocytosis, von Willebrand disease, clinical features include: mental retardation, syndrome
Marfan syndrome, Ehler-Danlos Syndrome (some types), hypotonia, profound hyperphagia, obesity,
Osteogenesis imperfecta, Achondroplasia, Familial small hands and feet, and hypogonadism
hypercholesterolemia, Acute intermittent porphyria Deletion in maternally derived Chromosome 15; Angelman
Two recessive alleles produce phenotype; enzyme Autosomal clinical features include: mental retardation, syndrome
deficiencies are usually inherited in this manner: recessive ataxic gait, seizure, and inappropriate laughter
examples: Cystic fibrosis, Phenylketonuria, “happy puppet”
Galactosemia, Homocystinuria, Lysosomal storage
diseases, α-1-antitrypsin deficiency, Wilson disease, 5. DISEASES OF THE IMMUNE SYSTEM
Hemochromatosis, Glycogen storage diseases, Sickle cell QUESTION ANSWER
anemia, Thalassemias, Congenital adrenal hyperplasia, GELL AND COOMBS CLASSIFICATION OF HYPERSENSITIVITY
Ehler-Danlos Syndrome (some types), Alkaptonuria, Caused by activation of TH2 CD4+ helper T cells by Type I
Neurogenic muscular atrophies, Freidrich ataxia, Spinal environmental antigens, leading to the production of (Immediate,
muscular atrophy IgE antibodies, which become attached to mast cells; IgE-
In this pattern of inheritance, males are usually X-linked examples: Anaphylaxis, Bronchial asthma, Allergic mediated)
affected due to hemizygosity of the allele, but females recessive rhinitis, sinusitis (Hay fever), Food allergies
may express phenotype due to random activation of disorders Vascular dilation, edema, smooth muscle
one X chromosome; examples: Duchenne Muscular contraction, mucus production, tissue injury, and
Dystrophy, Hemophilia A and B, Chronic granulomatous inflammation are characteristic of this type of
disease, G6PD deficiency, Agammaglobulinemia, hypersensitivity
Wiskott-Aldrich syndrome, Diabetes insipidus, Lesch- Caused by antibodies that bind to fixed tissue and cell Type II
Nyhan syndrome, Fragile X syndrome antigens and promote phagocytosis and destruction of (Antibody-
In this pattern of inheritance, females in general are X-linked the coated cells or trigger pathologic inflammation in mediated)
more affected than males (in any scenario), because dominant tissues; examples: Autoimmune hemolytic anemia,
one allele in a female is enough to manifest the trait; disorders Immune thrombocytopenic purpura, Pemphigus
examples: Alport syndrome and Vitamin D-resistant vulgaris, ANCA-vasculitis, Goodpasture syndrome, Acute
rickets rheumatic fever, Myasthenia gravis, Graves disease,
Insulin-resistant diabetes, Pernicious anemia
CHROMOSOMAL DISORDERS Phagocytosis and lysis of cells, inflammation, and
DISORDERS OF AUTOSOMES functional derangements without evidence of cell or
Most common of the chromosomal disorders; Trisomy 21 (Down tissue injury (in some diseases) are characteristic of
leading cause of MR; most common cause: syndrome) this type of hypersensitivity
nondisjunction of Ch21 during meiosis; Caused by antibodies binding to antigens to form Type III
diagnostic clinical features: flat facial profile, complexes that circulate and may deposit in vascular (Immune-
oblique palpebral fissures, and epicanthal folds beds and stimulate inflammation secondary to complex
Prominent occiput, mental retardation, Trisomy 18 complement activation; examples: SLE, PSAGN, mediated)
micrognathia, low-set ears, short neck, (Edward Polyarteritis nodosa, Reactive arthritis, Serum sickness,
overlapping fingers, cardiac defects, renal syndrome) Arthus reaction
malformations, limited hip abduction, and Inflammation and necrotizing vasculitis (fibrinoid
rocker-bottom feet are features of this syndrome necrosis) are characteristic of this type of
Microcephaly and mental retardation, Trisomy 13 (Patau hypersensitivity
microphathalmia, cleft lip and palate, syndrome) Cell-mediated immune responses in which T Type IV (T-
polydactyly, cardiac defects, umbilical hernias, lymphocytes cause tissue injury, either by producing cell-
renal defects, and rocker-bottom feet are features cytokines that induce inflammation and activate mediated/del
of this syndrome macrophages, or by directly killing cells; examples: ayed)
Note: Italicized features would help differentiate it from Rheumatoid arthritis, Multiple sclerosis, Type I Diabetes
Edward syndrome
Mellitus, Inflammatory bowel disease, Psoriasis, Contact
Syndrome consisting of cardiac anomalies, DiGeorge sensitivity
abnormal facies, thymic hypoplasia, cleft palate, syndrome
Perivascular cellular infiltrates, edema, granuloma
hypocalcemia, due to deletion in the long arm of
formation, and cell destruction are characteristic of
Chromosome 22 (part of Ch22q11.2 deletion
this type of hypersensitivity
syndrome, together with velocardiofacial
syndrome)
AUTOIMMUNE DISEASES
DISORDERS OF SEX CHROMOSOMES
32/F, with difficulty in breathing, Systemic lupus
Condition characterized by ≥ 2 X chromosomes Klinefelter
bilateral elbow joint pains, and rash erythematosus (SLE)
and ≥ 1 Y chromosomes; most common syndrome
after sun exposure. CBC showed low
karyotype is 47XXY; important cause of reduced
hemoglobin and reticulocytosis. ANA
spermatogenesis and male infertility; clinical
titer is positive. What is the diagnosis?
features include: eunuchoid body habitus,
Note: Table 6-9 in Robbins and Cotran Pathologic Basis of Disease, 9th ed.
testicular atrophy, micropenis, absence of
p. 218; or Page 11 in Main handout is an important table, as it allows you
secondary sex characteristics, etc.
to diagnose SLE clinically. Make sure you know this by heart.
Complete or partial monosomy of X chromosome; Turner syndrome
Mechanisms of organ damage in SLE Type III (most); Type II
female hypogonadism in phenotypic females;
(opsonization and
Most common abnormality is lack of entire X
phagocytosis, hematologic
chromosome (45XO); single most important
manifestations)
cause of primary amenorrhea; clinical features
include: ovarian streaks, absence of secondary Most common autoantibody in SLE ANA
sex characteristics, short stature, cystic hygromas Most specific autoantibodies for SLE anti-Sm (Smith), anti-dsDNA
of head neck, preductal CoA, etc. (anti-dsDNA correlates with
Type of hermaphrodism characterized by True disease activity)
presence of both ovarian and testicular tissue hermaphrodism Histopathologic findings in SLE with LM: Liquefactive
Type of hermaphrodism characterized by Pseudohermaphro skin involvement degeneration of basal layer,
disagreement between phenotypic and dism edema at DEJ, mononuclear
gonadal sex; examples: MRKH syndrome and infiltrates around blood
androgenital syndromes vessels and skin appendages
IF: Deposition of Ig and
complement at DEJ
TRINUCLEOTIDE REPEAT DISORDERS
Most common cause of MR following Trisomy Fragile X-
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 4 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
Type of LE that associated with Drug-induced lupus Based on the case above, the patient's Chronic GVHD
Hydralazine, INH, Procainamide, and symptoms resolved, but after a few
D-Penicillamine intake; rarely years, he developed cutaneous
involves kidneys and brain; rarely sclerosis, jaundice, and dysphagia.
associated with anti-dsDNA; associated Barium swallow showed esophageal
with anti-histone antibodies strictures. What is the diagnosis?
CLASSES OF LUPUS NEPHRITIDES IMMUNODEFICIENCY SYNDROMES: PRACTICE CASES
Class LM IF PRIMARY IMMUNODEFICIENCIES
Minimal Normal ICs in mesangium 6m/M, with morbilliform rash, recurrent Severe combined
mesangial oral thrush, diaper rash, and failure to immunodeficiency
(Class I) thrive. PE: no cervical lymphoadenopathy. (SCID)
Mesangial Mesangial cell Granular mesangial Ig CXR showed absence of thymic shadow.
proliferative proliferation; often with and complement without What is the diagnosis?
(Class II) mesangial matrix involvement of 7m/M, with unremarkable first 6 months of X-linked
accumulation glomerular capillaries life, developed recurrent pneumonia, and agammaglobulinemia
Focal Swelling and Subendothelial IC steatorrheic diarrhea. Sputum culture (Bruton disease)
(Class III) hypercellularity; capillary deposits revealed H. influenzae, and fecalysis revelaed
necrosis and hyaline Giardia lamblia trophozoites. PE: no
thrombi; <50% of cervical lymphadenopathy. Serum Igs are
glomeruli low. What is the diagnosis?
Diffuse Type III with ≥50% of 4m/M, with cyanosis since birth, associated DiGeorge syndrome
(Class IV) glomeruli; with coarse facial features and cleft palate,
Wire-loop appearance of presented with recurrent viral infections.
capillaries PE: +3 reflexes. CXR showed a boot-shaped
Membranous Diffuse capillary Subepithelial IC deposits heart with absence of thymic shadow. FISH
(Class V) thickening is positive for deletion in Ch22q11.2 locus.
Advance Sclerosis of >90% - What is the diagnosis?
sclerosing glomeruli 8m/M, with history of eczematous Wiskott-Aldrich
(Class VI) dermatitis and recurrent infections. CBC syndrome (X-linked
revealed low platelet. What is the most likely recessive)
34/F, with dry eyes and dry mouth. Lip Sjogren syndrome (late) diagnosis?
biopsy showed acinar atrophy, fibrosis, (Please also study the early 16/F, with a history of viral URTI 3 weeks Isolated IgA deficiency
and hyalinization of the minor salivary histologic findings in Sjogren prior, developed recurrent UTI and AGE. (acquired)
glands. What is the diagnosis? syndrome) Serum IgA is low. What is the diagnosis? Note: There are also
familial forms of IgA
Most common and most important Anti-Ro (SS-A) and anti-La
deficiency
autoantibody detected in Sjogren (SS-B)
syndrome
SECONDARY IMMUNODEFICIENCIES
45/F, with chronic GERD, history of Systemic sclerosis
Most common secondary Acquired immune
progressive dyspnea, and chronic
kidney disease, with note of thickening immunodeficiency; caused by HIV infection; deficiency syndrome
of the skin. What is the diagnosis? hallmark is profound immune deficiency (AIDS)
that leads to opportunistic infections,
Most common autoantibody associated Anti-DNA topoisomerase I
secondary neoplasms, and neurologic
with diffuse cutaneous systemic sclerosis (anti-Scl 70)
manifestations; the virus targets CD4+ T cells
Common autoantibody associated with Anti-centromere
Most common fungal infection in patients Candidiasis
limited scleroderma (limited cutaneous antibodies
with AIDS
systemic sclerosis)
Most common type of lymphoma associated B-cell lymphomas
with HIV infection
TRANSPLANTATION IMMUNOLOGY
AIDS-defining sarcoma caused by Human Kaposi sarcoma
RENAL TRANSPLANT REJECTION
herpesvirus 8 (HHV-8), clinically typified by
48/M, s/p kidney transplant, suddenly Hyperacute rejection appearance of purple patches, plaques or
developed bloody urine few hours nodules on the skin
after the procedure. Nephrectomy
revealed a cyanotic, mottled, and
flaccid kidney with necrotic cortex. 6. NEOPLASIA
Biopsy showed thrombotic occlusion of Note: Specific cancers will be discussed in their respective systems.
the capillaries and fibrinoid necrosis QUESTION ANSWER
of arterial walls. What is the diagnosis? NOMENCLATURE
45/F, with signs of renal failure 2 Acute cellular (T-cell An abnormal mass of tissue with excessive and Neoplasm
months after her renal transplant. mediated) rejection, uncoordinated growth compared to that of normal
Biopsy showed extensive interstitial tubulointerstitial type tissues; its growth persists after cessation of the
mononuclear infiltrate with edema and (tubulitis) stimuli that evoked the growth; literally means "new
mild interstitial hemorrhage. growth"
Immunohistochemical stains for CD3, Localized neoplasms; usually end with –oma, EXCEPT Benign
CD4 and CD8 are positive. What is the lymphoma, seminoma, dysgerminoma, hepatoma, neoplasms
diagnosis? and melanoma (these are malignant neoplasms)
30/M, developed oliguria and Acute antibody-mediated Neoplasms that invade and destroy adjacent tissues Malignant
subsequent renal failure 3 weeks after rejection neoplasms
an uneventful kidney transplant. Biopsy Malignant neoplasms of EPITHELIAL origin; usually Carcinomas
showed inflammation of glomeruli spread by LYMPHATIC route; example: colorectal
and peritubular capillaries with focal adenocarcinoma
thrombosis of small vessels. What is Malignant neoplasms of MESENCHYMAL origin; Sarcomas
the diagnosis? usually spread by HEMATOGENOUS route; example:
24/F, diagnosed with renal failure, Chronic rejection uterine leiomyosarcoma
underwent renal transplant. Four years Benign, but disorganized appearance of tissue Hamartoma
later, increasing level of creatinine indigenous to a particular organ; example: Peutz-
was noted. Biopsy showed interstitial Jegher polyp
fibrosis and tubular atrophy. What is Cytologically and architecturally normal tissue in an Choristoma
the diagnosis? ectopic location; example: Ectopic gastric tissue in (basically,
HEMATOPOIETIC STEM CELL TRANSPLANTATION Meckel diverticulum Ectopia)
66/M, known case of multiple Acute graft vs. host disease
myeloma, underwent HSC (GVHD) CHARACTERISTICS OF BENIGN AND MALIGNANT NEOPLASMS
transplantation, presented with bloody Extent to which neoplastic cells resemble their Differentiation
diarrhea and generalized normal forebears morphologically and functionally
morbilliform rash few weeks after the Considered a hallmark of malignancy, which Anaplasia
procedure. What is the diagnosis? literally means "to form backward"; term used to
describe cells with little or no differentiation
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 5 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
Disorderly but non-neoplastic proliferation of cells; Dysplasia Term used to describe the degree of Tumor stage
described as a loss in uniformity of individual cells localization/spread of the tumor; usual criteria:
and of their architectural orientation location and size of the primary tumor, nodal status,
Fibrous tissue formation in response to neoplasm Desmoplasia and presence of distant metastases; has more
Dysplastic changes that involve the entire thickness Carcinoma in prognostic value than tumor grade; example: AJCC
of the epithelium, without violation of the basement situ cancer staging system (TNM)
membrane Condition secondary to release of products of dying Tumor lysis
Development of secondary implants discontinuous Metastasis cancer cells during chemotherapy; characterized by syndrome
with the primary tumor, in remote tissues; more hyperkalemia, hyperphosphatemia, hyperuricemia,
than any other attribute, this identifies a neoplasm and hypocalcemia
as malignant
Next to metastasis, this is the most reliable feature Local 7. INFECTIOUS DISEASES
that distinguishes malignant from benign tumors invasiveness
QUESTION ANSWER
GENERAL PATTERN OF RESPONSE TO INFECTIONS
CANCER EPIDEMIOLOGY
Usual pattern of inflammation observed in Suppurative
Top 3 common cancers in CHILDREN ALL > CNS tumors > infections with extracellular Gram-positive
Burkitt lymphoma cocci, and Gram-negative rods (pyogenic
Top 3 common cancers in MALES Prostate > Lung > organisms)
Colorectal Usual pattern of inflammation observed in Mononuclear
Top 3 common cancers in FEMALES Breast > Lung > chronic, acute viral, and parasitic infections, and
Colorectal infections involving intracellular bacteria
Top 3 common cancer mortalities in MALES Lung > Prostate > Usual pattern of inflammation observed in Granulomatous
Colorectal tuberculosis, fungal infections, and schistosome
Top 3 common cancer mortalities in Lung > Breast > eggs; response to infectious agents that are not
FEMALES Colorectal easily eliminated
Usual response to viral infections that involves Cytopathic/
MOLECULAR BIOLOGY OF CANCER cytopathic changes in cells (inclusion bodies and Cytoproliferative
Hallmarks of cancer • Self-sufficiency in growth multinucleated giant cells) or proliferation of
signals host cells
• Insensitivity to growth- Usual response to clostridial infections, Tissue necrosis
inhibitory signals Entamoeba histolytica, HBV in liver, and
• Altered cellular Herpesviruses in brain
metabolism Usually a sequela of chronic inflammation, seen Chronic
• Evasion of apoptosis in chronic HBV infection (cirrhosis), and inflammation
• Limitless replicative Schistosoma (pipestem fibrosis) and scarring
potential (immortality)
• Sustained angiogenesis VIRAL DISEASES
• Ability to invade and 10/F, incomplete EPI, presented with cough, Measles
metastasize
colds, and conjunctivitis for 3 days with
• Ability to evade the host
associated cervical lymphadenopathy, followed
immune response
by eruption of rash from the head down,
Normal cellular genes whose products Proto-oncogenes accompanied by high-grade fever. Lymph node
promote cell proliferation; examples: biopsy revealed multinucleated giant cells with
RAS (most commonly mutated proto- eosinophilic nuclear and cytoplasmic inclusions
oncogene in human cancers) and ABL (in (Warthin-Finkeldey cells). What is the
CML) diagnosis?
Mutant or overexpressed versions of Oncogenes 30/M, sexually active, with painful perioral Herpes labialis
proto-oncogenes that function blisters. Biopsy of the blister revealed cells with
autonomously without a requirement pink to purple intranuclear inclusion bodies
for normal growth-promoting signals (Cowdry Type A inclusion bodies). What is the
Genes whose products apply brakes to Tumor suppressor genes diagnosis?
the cell proliferation; abnormalities in 23/F, with history of cough and colds for 3 days, Varicella
such genes lead to carcinogenesis followed by appearance of exquisitely pruritic
“Governor of the cell cycle”; a tumor Rb vesicles resembling "dewdrops on a rose
suppressor gene that exerts petal". Biopsy showed intraepithelial vesicles.
antiproliferative effects by controlling What is the diagnosis?
G1-S checkpoint in the cell cycle; 25/M, sexually active, developed fever and Cytomegalovirus
mutated in Retinoblastoma; key element lymphadenopathy. CBC showed lymphocytosis (CMV) infection
in HPV tumorigenesis with a significant fraction of atypical
"Guardian of the genome"; a tumor p53 lymphocytes. Lymph node biopsy revealed
suppressor gene that regulates cell cycle large, atypical cells with "Owl's eye" nuclei.
progression, DNA repair, cellular Monospot test is negative. What is the
senescence, and apoptosis; the most diagnosis?
frequently mutated tumor-suppressor 28/F, sexually active, developed fever and Epstein-Barr
gene in human cancers; mutated in Li- lymphadenopathy. CBC showed lymphocytosis virus (EBV)
Fraumeni syndrome with a significant fraction of atypical
lymphocytes. Lymph node biopsy revealed
CLINICAL ASPECTS OF NEOPLASIA paracortical hyperplasia, seen in a lot of viral
Progressive loss of body fat and lean body mass, Cancer infections. Monospot test is positive. What is
accompanied by profound weakness, anorexia, and cachexia the diagnosis?
anemia in cancer patients; main cytokine implicated
is TNF BACTERIAL DISEASES
Signs and symptoms not referable to the anatomic Paraneoplastic Main difference between staphylococcal and More extensive
distribution of the tumor; usually due to ectopic syndromes streptococcal infections tissue
hormone production by tumor cells examples: ectopic destruction in
ACTH production (Cushing syndrome) in Small cell staphylococci
lung cancer; Hypercalcemia in squamous cell 10/F, incomplete EPI, developed low-grade Diphtheria,
carcinoma (due to PTHrp expression) fever and sore throat for 2 days, followed by Corynebacterium
Term used to describe the degree of differentiation Tumor grade inspiratory stridor and cyanosis. Patient was diphtheriae
based on histologic appearance of the tumor; intubated, and suppuration with grayish
examples: Gleason scoring in Prostatic pseudomembrane was noted on laryngoscopy.
adenocarcinoma and FIGO grading for endometrioid What is the diagnosis, and the causative
endometrial carcinomas organism?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 6 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
LBB, delivered term via emergency CS for non- Granulomatosis 37/M, without any coronary risk factors, Chagas disease
reassuring fetal status. PE: multiple pustular infantiseptica, with remote history of travel to several (Trypanosoma
lesions. Patient eventually expired. CSF analysis Listeria countries in South America, presented with cruzi)
showed intracellular, Gram-positive bacilli; monocytogenes syncope, and eventual death. Autopsy
Autopsy showed multiple granulomas in major showed an enlarged colon and esophagus.
organs. What is the diagnosis, and the causative Sections of the heart show C-shaped, curved,
organism? trypanosomes infiltrating the
25/M, sexually active, complaining of purulent Neisseria myocardium. What is the diagnosis and the
penile discharge. GS/CS showed Gram- gonorrheae etiologic agent?
negative intracellular diplococci, and growth Metazoans are better studied in Microbiology.
of glucose (+) and maltose (-) colonies on
modified Thayer-Martin agar. What is the 8. ENVIRONMENTAL AND NUTRITIONAL
most likely etiologic agent?
Based on the case above, if no organisms are Chlamydia PATHOLOGY
seen on Gram-stain, what would be the most trachomatis Note: The chapter concerns many topics, but are discussed across
likely etiologic agent? different subjects, and for the interest of time, recurring concepts, as well
8/F, with cystic fibrosis and recurrent Pseudomonas as low-yield topics, are omitted. Please refer to the main handout for a
pneumonia. Lung biopsy showed fleur-de-lis aeruginosa more detailed discussion.
pattern of necrotizing pneumonia and ENVIRONMENTAL PATHOLOGY
perivascular infiltration of organisms QUESTION ANSWER
producing a "blue haze". What is the most likely AIR POLLUTION
etiology of pneumonia in this patient? 34/M, history of sleeping in the car with windows CO
34/M, with a history of a painless nodule on Syphilitic closed, presented with decrease in sensorium, and poisoning
the penis that spontaneously resolved, and gumma, Tertiary cherry red discoloration of the skin and mucosal
flat, velvety, broad-based lesions in the syphilis membranes. What is the most likely diagnosis?
perineum, now with an ulcerated nodule on
the nose. Biopsy showed central coagulation
necrosis, rimmed by palisading macrophages, HEAVY METAL POISONING
and fibroblasts, plasma cell-rich infiltrate, 6/M, with pica, presented with poorly localized Lead
and few organisms. RPR and TPPA are abdominal pain, poor school performance, and poisoning
positive. What is the diagnosis, and what is the decreased play activity. CBC and PBS showed
stage of the disease? microcytic hypochromic anemia, with basophilic
stippling. X-ray showed opacities occupying the
epiphyseal plates. What is the diagnosis?
FUNGAL DISEASES
YEASTS
NUTRITIONAL DISORDERS
28/M, HIV-positive, with a whitish plaque on the Oropharyngeal
PROTEIN-ENERGY MALNUTRITION
buccal mucosa that can be scraped off, showed candidiasis
Parameter Marasmus Kwashiorkor
mucosal erythema. Examination of the plaque (Thrush)
showed pseudohyphal structures. What is the Definition Weight <60% of normal Protein > caloric
diagnosis? deprivation
Based on the case above, if the patient presented Cryptococcus Protein • Somatic: Emaciated • Somatic: relatively
with neurologic manifestations and eventually neoformans component extremities (atrophy) spared
died, and brain autopsy revealed soap bubble affectation • Visceral: minimally • Visceral:
lesions, what is the etiologic agent? depleted (normal hypoalbuminemia →
albumin) generalized edema
MOLDS
Subcutaneous Affected Relatively spared
34/F, with a history of cavitary tuberculosis and Aspergillus
fat
breast cancer treated with alkylating agents,
presented with hemoptysis and dyspnea. The Growth failure Present
patient eventually expired. Autopsy showed a Anemia Yes (mainly due to decreased precursors)
mass occupying the cavity on the lung. Sections Immune and Present (thymic and lymphoid atrophy more marked
show septate hyphal elements, branching at vitamin in kwashiorkor)
acute angles (40°). What is the etiologic agent? deficiencies
34/M, known case of Non-Hodgkin lymphoma Mucor Other findings Head relatively larger • Liver: steatosis
treated with alkylating agents, presented with a than body • Small bowel: atrophy,
necrotic lesion on the nose. Biopsy showed non- loss of microvilli
septate hyphal elements, branching at right • Brain: cerebral
angles. What is the etiologic agent? atrophy, ↓ neurons,
impaired
PARASITIC DISEASES myelinization
PROTOZOA
55/M, with history of travel to Angola, Plasmodium sp., VITAMIN DISORDERS (DEFICIENCIES)
Note: Other vitamin disorders are discussed in Biochemistry
returned home with fever occurring every Malaria
34/M, known case of Crohn disease, presented with Vitamin A
72 hours. Giemsa-stained smears show
chronic steatorrhea and weight loss, was involved in a
numerous ring forms in erythrocytes.
vehicular accident that happened at night. He reported
Methylene blue-stained smear show
that he experienced difficulty in seeing things at night.
hemozoin pigment. What is etiologic agent
What is the most likely vitamin deficient in this patient?
and the diagnosis?
26/F, complaining of gum bleeding with minor trauma. Vitamin C
Based on the case above, if the patient Babesia sp.,
CBC and bleeding parameters are unremarkable. What
presents with fever, and Giemsa-stained Babesiosis
is the most likely vitamin deficient in this patient?
smears show numerous forms resembling a
Maltese cross, and Methylene blue-stained 7/M, with difficulty in ambulating. X-ray showed Vitamin D
smears are negative for hemozoin pigment, bowing of legs and lumbar lordosis. What is the most
what is the etiologic agent and the diagnosis? likely vitamin deficient in this patient?
35/M, with history of travel to Sudan, Leishmania sp.,
presented with anemia and Visceral 9. DISEASES OF INFANCY AND CHILDHOOD
hepatosplenomegaly. Biopsy showed leishmaniasis QUESTION ANSWER
macrophages filled with organisms. What COMPLICATIONS OF PREMATURITY
is the etiologic agent, and the diagnosis? LBB, born preterm at 27 weeks AOG via VSD, Respiratory
38/F, with history of travel to Africa, African sleeping was observed to be tachypneic a few minutes distress syndrome
presented with increased sleeping time, and sickness, after birth, with associated grunting, alar of the newborn
frequent tendencies of fall. PBS showed meningoencephalitic flaring, and intercostal retractions. CXR (Hyaline membrane
flagellated organisms with undulating stage, Trypanosoma showed ground-glass appearance of lung disease)
membrane. CSF showed the same brucei fields with air bronchograms. The patient
organisms. What is the diagnosis, the stage, eventually expired 2 days after, despite
and the etiologic agent? appropriate treatment measures. Autopsy
showed eosinophilic membranes lining the
alveolar walls. What is the diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 7 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
Based on the case above, if the patient had lived Retinopathy of ATHEROSCLEROSIS
because of aggressive management, including prematurity 67/M, known hypertensive and diabetic, Chronic stable
excessive oxygen administration, and (ROP)/Retrolental presented with exertional retrosternal chest angina pectoris,
funduscopy showed retinal fibroplasia heaviness lasting for 5 minutes, relieved by Atherosclerotic
neovascularization, what is the diagnosis? rest and sublingual nitroglycerin. Angiography stenosis
Based on the first case, if the patient had lived, Bronchopulmonary revealed 75% stenosis of the LAD. What is the
and was admitted at the NICU for 7 weeks dysplasia (BPD) diagnosis, and the pathologic consequence of
maintained on >21% FiO2, but was assessed to (Moderate) atherosclerosis that led to the disease in this
require the same FiO2 at discharge, but then case?
several days after, he eventually expired, and Based on the case above, the patient instead Inferior wall
autopsy showed decrease in alveolar presented with retrosternal chest heaviness STEMI, Acute
septation, what is the diagnosis? lasting for 30 minutes at rest, not relieved by plaque change
LBG, born preterm at 29 weeks AOG via VSD, Necrotizing sublingual nitroglycerin. ECG showed ST- (Hemorrhage)
was observed to have hematochezia and enterocolitis (NEC) elevation in leads II, III, and aVf. He had several
abdominal distention. Babygram showed (Severe) episodes of refractory hypotension and
pneumoperitoneum. The patient eventually eventually expired. Autopsy of the coronary
expired after a few days. Autopsy showed vessels showed a large, intraplaque
transmural coagulative necrosis, ulceration, hemorrhage that occluded the whole vessel
and submucosal gas bubbles in the colon. lumen. What is the diagnosis, and the pathologic
What is the diagnosis? consequence of atherosclerosis that led to the
disease in this case?
FEATL HYDROPS
IMMUNE HYDROPS ANEURYSMS AND DISSECTION
Parameter Rh incompatibility ABO incompatibility 34/F, known case of autosomal dominant Subarachnoid
Setup • Mother: Rh(-) • Mother: O polycystic kidney disease, presented with severe hemorrhage
• Fetus: Rh(+) • Fetus: A or B headache and eventual collapse. She was secondary to
• Subsequent pregnancy admitted comatose, and eventually died. ruptured
Signficant: >1cc Rh(+) Antemortem plain cranial CT showed intracranial
fetal RBCs enhancement of the sulci. Autopsy showed berry aneurysm
multiple saccular dilatations along the vessels of
the Circle of Willis, with a ruptured one on the
Severity More severe Less severe ACA-ACoA junction. What is the diagnosis?
Protection RhIg in 28 weeks and No known protection 55/M, known hypertensive, with previous CXR Ruptured
within 72 hours prior to and plain abdominal films only showing abdominal aortic
delivery atheromatous aorta, presented with a pulsating aneurysm
Consequence 1. Hemolysis → Anemia → Cardiac failure (increased abdominal mass. An inexperienced doctor
hydrostatic pressure) and liver failure (decreased vigorously palpated the abdomen, and the
protein synthesis → decreased colloid oncotic patient complained of pain, and became
pressure) → Edema hypotensive, and eventually died. Autospy
2. Hemolysis → Jaundice and Kernicterus revealed a fusiform dilation of the abdominal
aorta with a point of rupture. What is the
CYSTIC FIBROSIS diagnosis?
7/F, with salty sweat, and history of Cystic fibrosis 34/M, 6'5" with long fingers, presented with Ruptured
recurrent pulmonary infections, presented (CF)/Mucoviscidosis; chronic nonproductive cough. PE: BP: 120/10. thoracic aortic
with dyspnea, and cyanosis, and was Bronchiectasis The patient suddenly went overtly hypotensive aneurysm;
intubated. ETA CS showed Pseudomonas with muffled heart sounds and neck vein Marfan syndrome
aeruginosa. The patient eventually expired. distention. The patient eventually expired.
Autopsy showed no diagnostic abnormality Autopsy showed 200 cc of blood in the
on the skin, but sections from the lung show pericardial cavity, with a fusiform dilation of the
dilation of the airways with intense acute aortic root with a point of rupture. What is the
and chronic inflammation, and granulation diagnosis?
tissue formation. What is the underlying Based on the case above, if the patient presented Aortic dissection
cause of death, and what is the diagnosis for with sudden onset of exquisite chest pain,
the pulmonary findings? tearing in character, radiating to the back, with
sudden cardiovascular collapse, and eventual
TUMORS death, and autopsy showed a secondary lumen in
6/M, with an enlarging abdominal mass that Neuroblastoma the thoracic aorta with point of tear noted
crosses the midline, and generalized, dusky proximal to the formation of the secondary
macules, resembling the surface of a blueberry lumen, what is the diagnosis?
muffin. The patient eventually expired. Autopsy
showed a mass in the adrenal gland. Sections VASCULITIDES
show sheets of small, round, blue cells, with 65/F, known case of polymyalgia rheumatica, Giant cell
occasional formation of Homer-Wright rosettes. presented with severe headache and diplopia arteritis (Large
What is the diagnosis? associated with fever and fatigue. PE: arteries)
5/F, with hematuria, and a large abdominal mass, Wilms tumor tenderness over the course of the superficial
mainly located on the right, but appears to cross temporal artery was painful to palpation. Biopsy
the midline. Biopsy of the mass showed a mixture showed intimal thickening of the artery,
of glandular structures, sheets of spindle cells, granulomatous inflammation of the internal
and small, round, blue cells. What is the diagnosis? elastic lamina with infiltrate of T cells and
macrophages. What is the diagnosis?
PART II: SYSTEMIC PATHOLOGY 38/F, with fatigue, weight loss and fever, and
reduced blood pressure, weak pulses in the
Takayasu
arteritis (Large
10. BLOOD VESSELS carotids and upper extremities, ocular arteries)
QUESTION ANSWER disturbances, and neurologic deficits.
HYPERTENSION Morphological findings same as above. What is the
54/F, known hypertensive with rising BUN and Hyaline diagnosis?
creatinine. Impression was hypertensive arteriolosclerosis Note: Both vasculitides affect large arteries and exhibit granulomatous type of
nephrosclerosis. Renal biopsy showed inflammation. In fact, they have the same histologic appearance. It depends on the
clinical data to differentiate both diseases.
homogenous, pink, hyaline material on the
walls of arterioles, with narrowing of the 56/M, known case of chronic active hepatitis B, Polyarteritis
lumen. What is the vascular pathology seen? presented with rapidly accelerating nodosa
hypertension, abdominal pain, bloody stool, and
55/M, presented with sudden onset of oliguria Hyperplastic
myalgia, and eventually expired. Biopsy showed
and a BP of 220/110 mmHg. The patient artieriolosclerosis
segmental transmural necrotizing
eventually died. Autopsy of the kidney showed
inflammation with extensive fibrinoid necrosis
"onion-skin", concentric, laminated thickening
and temporal heterogeneity of lesions. What is
of the walls of arterioles with luminal
the diagnosis?
narrowing, and necrotizing arteriolitis. What is
the vascular pathology seen?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 8 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
4/F presented with fever and maculopapular Kawasaki disease CONGENITAL HEART DISEASES
rash on her trunk and extremities. This is 30/M, with occasional episodes of chest ASD
associated with conjunctival erythema, and heaviness, dyspnea, and syncope. Cardiac
cervical lymph node enlargement. Biopsy examination: (+) systolic murmur at the 2nd
showed segmental transmural necrotizing LICS. CXR: increased pulmonary vascular
inflammation with less fibrinoid necrosis. What markings with RVH. What is the diagnosis?
is the diagnosis? 5/M, apparently asymptomatic, with an VSD
Note: Both vasculitides that affect medium-sized arteries have the same histologic incidental finding of a holosystolic murmur best
appearance; only Kawasaki disease has less fibrinoid necrosis. It depends on the heard at the left lower sternal border,
clinical data to differentiate both diseases.
radiating to the right lower sternal border.
45/M, presented with hemoptysis and hematuria. Microscopic CXR: increased pulmonary vascular markings,
Serology: p-ANCA/MPO-ANCA (+). Biopsy showed polyangiitis BVH, and normal aortic knob size. What is the
a vasculitis pattern similar to PAN, but lesions diagnosis?
are of the same stage, and with fragmented 16/M, apparently asymptomatic, with an PDA
PMNs in post-capillary venules
incidental finding of a heart murmur
(leukocytoclasia). What is the diagnosis?
(continuous, "machinery like") best heard at
34/F, known case of bronchial asthma. CBC: 62% Churg-Strauss the 2nd LICS. CXR: increased pulmonary
eosinophils, without blasts; Serology: p- syndrome vascular markings, LVH/BVH, and enlarged
ANCA/MPO-ANCA (+). Biopsy showed aortic knob. What is the diagnosis?
granulomatous inflammation involving the 4/M, cyanotic with failure to thrive. CXR: Tetralogy of Fallot
respiratory tract and necrotizing vasculitis.
decreased pulmonary vascular markings and (TOF)
What is the diagnosis?
RVH, with a characteristic boot-shaped heart.
54/M, with hemoptysis and hematuria with Granulomatosis What is the diagnosis?
increasing BUN and creatinine. Serology: c-ANCA with angiitis 3d/M, cyanotic, with history of maternal GDM. Transposition of
(PR3-ANCA) (+). Biopsy showed necrotizing (Wegener CXR: Increased pulmonary vascular markings the Great Arteries
granulomas of the respiratory tract, necrotizing granulomatosis)
and RVH, with a characteristic egg on the side (TGA)
vasculitis, and crescentic glomerulonephritis
appearance. What is the diagnosis?
with negative findings on immunofluorescence.
What is the diagnosis?
COARCTATION OF THE AORTA
30/M, smoker, with intermittent claudication Thromboangiitis
Feature Infantile Adult
with the right leg. Biopsy showed segmental obliterans
Obstruction Tubular hypoplasia of Coarctation opposite the
thrombosing acute and chronic vasculitis with (Buerger
aortic arch proximal to ligamentum arteriosum
microabscesses. What is the diagnosis? disease)
the PDA distal to the arch vessels
Associations Turner syndrome -
TUMORS AND TUMOR-LIKE CONDITIONS
Clinical findings Lower extremity • Upper extremity
45/M, chronic alcoholic, known case of liver Spider
cyanosis hypertension
cirrhosis, presented with multiple, radial, telangiectasia
• Rib notching on CXR:
pulsatile arrays of dilated submucosal arteries
increased blood flow to
that blanch with pressure. What is the diagnosis?
intercostal vessels
4/M, with seizures, mental retardation, and Sturge-Weber
Chamber RVH (or biventricular) LVH
hemiplegia. PE: port-wine stain on the left; CT- syndrome
hypertrophy
scan: extraaxial hyperdense lesion on the left
parietal convexity. Biopsy showed dilated venous
vessels. What is the most likely diagnosis? ISCHEMIC HEART DISEASE
4/F, with a pinkish exophytic lesion on the lip Capillary 48/M, known hypertensive, presented with Chronic stable
since birth. Biopsy showed small, endothelial- hemangiomas exertional retrosternal chest heaviness <2 minutes angina
lined spaces, filled with red blood cells. What is in duration that improves with rest. Exercise ECG pectoris
the diagnosis? shows non-specific ST wave changes. Cardiac
markers are negative. What is the diagnosis?
Based on the third case, if the patient reports that Pyogenic
the lesion only appeared 3 months prior, after granuloma Based on the case above, if he presented with chest Unstable
history of trauma, and biopsy showed additional heaviness at rest lasting for 15 minutes, without angina
granulating acute and chronic inflammation, improvement with ISDN sublingual tablets, and
what is the diagnosis? ECG showed ST wave depression in contiguous
leads, but cardiac biomarkers are negative, what is
43/F, with a liver mass. Biopsy showed dilated Cavernous
the diagnosis?
vascular spaces filled with blood. What is the hemangioma
diagnosis? Based on the second case, if the chest pain lasts for NSTEMI
30 minutes, and cardiac biomarkers are positive,
15/F, with short stature and amenorrhea, Cavernous
what is the specific diagnosis?
presented with a mass on the neck, measuring 10 lymphagngioma;
cm in widest dimension. Biopsy showed dilated Turner syndrome Based on the third case, if the patient died 2 hours Waviness of
endothelial lined space without red blood cells. after the onset of chest pain, what would be the fibers at
What is the diagnosis, and what syndrome is expected morphologic finding on autopsy? border of
observed in this case? infarct
29/M, known case of HIV, developed purple Kaposi sarcoma Based on the third case, if the patient died after 2 Coagulation
plaques on bilateral lower extremities. Biopsy days, what would be the expected morphologic necrosis with
showed dermal accumulations of jagged finding on autopsy? neutrophilic
vascular channels lined and surrounded by infiltration
plump spindle cells. What is the diagnosis? Note: Please study this part well in the main handout, because ischemic
46/M, exposed to vinyl chloride, presented with a Hepatic heart disease is one of the most common diseases that you will encounter
liver mass. Biopsy showed sheets of spindle cells angiosarcoma as a physician, and therefore the examiners will never fail to include this
with occasional vessel formation. in the board examination, across all subjects.
Immunohistochemistry: CD31, vWF (+). What is
the diagnosis?
11. HEART
QUESTION ANSWER
HEART FAILURE
67/M, presented with easy fatigability, Left-sided heart
paroxysmal nocturnal dyspnea, and 3-pillow failure
orthopnea. Known case of hypertension, poorly
controlled, for 20 years. What is the type of
heart failure seen in this case?
45/M, known case of COPD, presented with Right-sided heart
decreased sensorium, increased liver span, and failure
lower extremity edema. What is the type of heart
failure seen in this case?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 9 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
HYPERTENSIVE HEART DISEASE PERICARDIAL DISEASES
Parameter Left-sided HHD Right-sided HHD 55/M, with a thoracic aortic aneurysm, near the Pericardial
Incidence More common Less common aortic root, presented with sudden prostration, tamponade
Cause • Systemic hypertension • Pulmonary hypotension, with neck vein distention, and secondary to
hypertension (if distant heart sounds on cardiac auscultation. ruptured
secondary to pulmonary The patient eventually expired. Autopsy showed a thoracic
disease: cor pulmonale) ruptured thoracic aneurysm, and a blood-filled aneurysm
• Most common cause: pericardial cavity. What is the diagnosis?
LSHD
Findings • Concentric LVH usually • Acute cor pulmonale: RV PERICARDITIDES
accompanied by dilation Feature Acute pericarditis Chronic pericarditis
interstitial fibrosis • Chronic cor pulmonale: Forms • Fibrinous/serofibrinous • Usually, consequence of
(impaired filling) → LA RV hypertrophy, (most common); purulent pericarditis
enlargement dilation and possible common causes: AMI • Adhesive
• History/evidence of RSHF (Dressler syndrome), mediastinopericarditis:
hypertension in other uremia, radiation, RF, parietal pericardium
organs SLE, trauma adheres with mediastinal
• Earliest change: • Purulent: infections structures
increased transverse • Hemorrhagic: most • Constrictive pericarditis:
diameter of myocytes common cause: heart enclosed in a dense
→→ variable neoplasms fibrocalcific scar
cell/nuclear • Caseous: most common
enlargement with cause: TB
interstitial fibrosis Clinical • Chest pain, relieved • Adhesive
findings when leaning forward mediastinopericarditis:
VALVULAR HEART DISEASES • Pericardial friction rub Systolic retraction of the
12/F, presented with dyspnea and knee pain (with Acute rheumatic (most striking clinical rib cage and diaphragm,
an antecedent history of ankle pain that fever; Type II finding) pulsus paradoxus
spontaneously improved). History revealed • Constrictive pericarditis:
previous sore throat 4 weeks prior to the onset of diastolic dysfunction
symptoms. ASO titer is high. PE: systolic murmur
at apex. Patient eventually expired. Autopsy of the 12. WHITE BLOOD CELLS,
heart shows Aschoff bodies in the epicardium,
myocardium and endocardium layers. What is the LYMPH NODES, SPLEEN, AND THYMUS
diagnosis, and the type of hypersensitivity that this Note: The chapter focuses on the COMMON white cell disorders. For the
disease exhibits? diseases of the spleen and the thymus, please refer to the main handout.
Based on the case above, suppose that the patient Rheumatic QUESTION ANSWER
lived, and was lost to follow up, and came back after heart disease NON-NEOPLASTIC WHITE CELL DISORDERS
12 years, now with dyspnea. PE: diastolic murmur Decreased number of circulating Leukopenia
at apex. Patient eventually expired. Autopsy of the leukocytes; most commonly involves
heart shows a fish-mouth deformity of the mitral neutrophils (neutropenia); deficiency of
valve. What is the diagnosis? lymphocytes (lymphopenia) is less common,
Based on the second case, suppose that the patient Subacute and is commonly seen in advanced HIV and
survived, but presented with high-grade fever as Infective other diseases
well. Blood CS turned positive for viridans endocarditis Clinically significant neutropenia Agranulocytosis
streptococci. Despite appropriate management, she (<500/mm3); high susceptibility to
died. Autopsy of the heart shows large, irregular infections (Candida and Aspergillus);
masses on the valve cusps that may extend into most common cause is drug toxicity
chordae. What is the specific diagnosis? An increase in the number of white cells Reactive leukocytosis,
in the blood in a variety of inflammatory Leukemoid reaction (high
CARDIOMYOPATHIES states caused by microbial and non- leukocyte alkaline phosphatase
microbial stimuli that may mimic (LAP): a product of normal WBCs;
14/M, with a history of viral URTI, then Dilated used to differentiate it from
leukemia
developed progressive dyspnea, and died. cardiomyopathy leukemias i.e. CML (low LAP))
Autopsy showed enlarged, heavy, flabby secondary to diffuse Enlargement of a lymph node as Reactive lymphadenitis
heart with dilated chambers. Sections interstitial myocarditis immune response to foreign antigens;
from the myocardium show lymphocytic histology usually nonspecific; depends
infiltration. What is the complete diagnosis on duration of disease and type of
25/M, was playing basketball, when he Hypertrophic offending agent
suddenly collapsed, and died. Autopsy cardiomyopathy REACTIVE LYMPHADENITIS: PRACTICE CASES
showed hypertrophic myocardium, 7/F, with obstructive sleep apnea secondary to chronic Follicular
particularly the interventricular septum. hypertrophic tonsils, Grade 3; underwent bilateral hyperplasia
Sections show myofiber disarray, and tonsillectomy and adenoidectomy. Biopsy of the
interstitial fibrosis. What is the diagnosis? adenoids shows increase in the number of germinal
centers (secondary follicles) per unit area. What is the
CARDIAC TUMORS diagnosis for the adenoids?
Parameter Myxoma Rhabdomyoma 27/F, developed fever and lymphadenopathy. Paracortical
Epidemiologic Most common primary Most common Serology: heretophil antibodies (+). Diagnosis was hyperplasia
notes cardiac tumor in adults primary cardiac infectious mononucleosis. Lymph node biopsy shows
tumor in children expansion of the paracortical zones imparting a
Location Atria; LA > RA Ventricles mottled appearance (because of the heterogeneous
Associations • McCune-Albright Tuberous sclerosis population of T-cells, immunoblasts, histiocytes, and
syndrome complex plasmacytoid dendritic cells). What is the diagnosis?
• Carney complex 59/F, known case of breast cancer, underwent sentinel Sinusoidal
Clinical Ball-valve obstruction, Obstruction lymph node biopsy. Lymph node biopsy shows no hyperplasia
presentation embolization, evidence of metastases, but with distention of /Sinus
constitutional symptoms lymphatic sinusoids by histiocytes. What is the histiocytosis
Gross Usually solitary, sessile or Usually multiple, diagnosis?
pedunculated masses gray-white masses
mottled with hemorrhage NEOPLASTIC WHITE CELL DISORDERS
Histology Stellate/globular myxoma Thin strands of Neoplastic proliferation of white cells wherein the Leukemia
cells embedded within cytoplasm that stretch neoplastic white cells populate the peripheral blood and
acid mucopolysaccharide from the nucleus to bone marrow, which leads to peripheral blood
matrix with vessel or the surface membrane cytopenias. Clinical manifestations depend on the cell
gland like projections “spider cells” line/s affected.
Neoplastic proliferation of white cells that presents as Lymphoma
discrete tissue masses
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 10 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
LEUKEMIAS 45/F, apparently asymptomatic. Chronic
Parameter Acute leukemia Chronic leukemia CBC: 300,000/mm3 with neutrophilia, left shift myelogenous
Age Usually younger Usually older (myelocytes and metamyelocytes), and 2% blast leukemia
Morphological Usually more Usually more mature- count (CML)
appearance of cells primitive looking LAP score: Low
Clinical course and Usually aggressive; Usually indolent; FISH studies: (+) BCR-ABL1 t(9;22).
presentation severe symptoms subtle symptoms What is the diagnosis?
Amenability to Usually amenable Usually resistant
treatment LYMPHOMAS
Parameter HL NHL
ACUTE LEUKEMIAS Lymph node Single, axial group of Multiple, peripheral
4/F presents with pallor, recurrent URTI, and Acute involvement nodes (cervical, nodes
epistaxis. lymphoblastic mediastinal, para-
PE: increased liver span and obliterated Traube leukemia (ALL) aortic)
space (precursor B- Spread Contiguous Non-contiguous
CBC: 35% Blast count with lymphocytic cell ALL) Mesenteric nodes and Rare Common
background Waldeyer ring
BM trephine: Hypercellular marrow with diffuse involvement
infiltration of blast cells Extranodal Rare Common
Flow cytometry: 89% Bone marrow blasts presentation
Myeloid markers: MPO, CD117, CD33 (-)
Lymphoid markers: Tdt (+) HODGKIN LYMPHOMA
B-cell lineage marker: CD79a, CD19 (+) 23/F, Filipino, with long-standing solitary left lateral Mixed
T-cell lineage markers: CD3, CD7 (-) neck mass, with fever and night sweats. PPD is cellularity
What is the diagnosis? positive. HL
12/M presents with mediastinal mass. Precursor T- LN biopsy: mixed infiltrate of inflammatory cells with
CT: Multiple mass in the abdomen and mediastinum cell ALL large cells with multiple nuclei, each of which has a
CBC: 40% Blast count with lymphocytic nucleolus ("Owl-eye" nuclei); fibrous nodules are not
background observed
BM trephine: Hypercellular marrow with diffuse IHC: Large cells are positive for CD15 and CD30. What
infiltration of blast cells. is the diagnosis?
Flow cytometry: 78% BM Blasts Based on the case above, if at least one fibrous nodule Nodular
Myeloid markers: MPO, CD117, CD33 (-) is observed, with scattered RS cells, and no observable sclerosis HL
Lymphoid markers: Tdt (+) necrosis, what would be the histologic diagnosis? (Grade I)
B-cell lineage marker: CD79a, CD19 (-) Based on the first case, if histology showed scant Lymphocyte
T-cell lineage markers: CD3, CD7 (+) lymphocytic infiltrate with predominance of large, -depleted HL
What is the diagnosis? pleomorphic cells; some of which look like RS cells,
40/M, presents with bleeding. Acute and IHC: CD30, PAX5 (+), ALK, CD45(-), what is the
CBC: thrombocytopenia, 15% Blast count, with promyelocytic histologic diagnosis?
40% nucleolated WBCs with Auer rods obscuring leukemia
the supposed perinuclear clearing (Golgi zone) of a (WHO Class I) SUBTYPES OF HL
promyelocyte Note: in cases of Association Immuno-
Coags: Elevated PT/PTT t(15;17) AML, Subtype Morphological pearls
with EBV phenotype
FISH: (+) t(15;17) PML-RARA 20% blast count
requirement is not Nodular Reactive T-cells with (-) CD15(+)
What is the diagnosis? needed for sclerosis (NS) fibrous bands forming CD30(+)
diagnosis nodules
36/M, known case of Hodgkin lymphoma Stage Acute myeloid Mixed Mixed leukocytic 70% CD15(+)
IIIB, underwent chemotherapy with alkylating leukemia cellularity (MC) infiltrate without CD30(+)
agents, developed recurrent epistaxis. (AML) fibrous nodules
PE: increased liver span and obliterated Traube (Therapy- Lymphocyte Rich reactive T-cell 40% CD15(+)
space related AML) rich (LR) infiltrate CD30(+)
CBC: Anemia, thrombocytopenia, Leukocytosis (WHO Class II) Lymphocyte Rare reactive Most (+) CD15(+)
(200,000/mm3) with 40% Blast count depleted lymphocytes CD30(+)
BM trephine: Hypercellular marrow with diffuse (LD)
infiltration of blast cells Lymphocyte Reactive B cells; (-) CD15(-)
Flow cytometry: 92% BM Blasts predominant lymphohistiocytic CD30(-)
Myeloid markers: MPO, CD117, CD33 (+) (LP) “popcorn” RS cells CD20(+)
Lymphoid markers: Tdt (-)
B-cell lineage marker: CD79a, CD19 (-) NON-HODGKIN LYMPHOMA
T-cell lineage markers: CD3, CD7 (-) 60/M, with multiple lymphadenopathy. Small
What is the diagnosis? CBC: 5,000/mm3 with 80% lymphocytes (4,000/mm3) lymphocytic
PBS: lymphocytosis with smudge cells lymphoma
DIFFERENCE BETWEEN AML and ALL LN biopsy: Diffuse but vaguely nodular infiltration of (SLL)
Parameter AML ALL small lymphocytes with proliferation centers
Age of onset Adults Children (pseudofollicular pattern)
Presentation Bone marrow failure IHC: CD3(-), CD20, CD5, CD23(+)
CNS spread Rare Common What is the diagnosis?
Prognosis Generally difficult to treat Generally responsive to 70/F, with multiple cervical lymphadenopathy. Follicular
chemotherapy CBC: WBC 20,000, with 80% lymphocytes lymphoma
(15,000/mm3).
CHRONIC LEUKEMIAS LN biopsy: Nodular pattern (Follicular) of
68/M, with multiple lymphadenopathy. Chronic infiltration of small lymphocytes with follicle
CBC: 300,000/mm3 with 95% lymphocytes lymphocytic formation in perinodal fat
(285,000/mm3) leukemia BM trephine: Hypercellular marrow with
PBS: Lymphocytosis with smudge cells. (CLL) paratrabecular lymphoid aggregates
BM trephine: Hypercellular marrow with nodular IHC: CD3, CD5(-), CD20, CD10, BCL2 (+)
lymphoid aggregates. What is the diagnosis?
LN biopsy: Diffuse but vaguely nodular infiltration of 47/M, with an enlarging mass on the ankle and Diffuse Large
small lymphocytes with proliferation centers profound weight loss. B-cell
(pseudofollicular pattern) Incision biopsy: sheets of large, pleomorphic cells lymphoma
IHC: CD3(-), CD20, CD5, CD23(+) Initial diagnosis: Malignant round cell neoplasm (DLBCL),
What is the diagnosis? IHC: CK, vimentin (-), CD45, CD10, BCL6, MUM1(+), high-grade,
Ki-67=80% non-germinal
What is the diagnosis? center type
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 11 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
12/M, with a rapidly enlarging mandibular mass. Burkitt 1m/M, No newborn screening done, with pyuria Glucose-6-
Incision biopsy: sheets of medium-sized lymphocytes lymphoma treated with Co-trimoxazole. Days later, presented phosphate
with several macrophages resembling a "starry sky" with jaundice. PBS: mostly schistocytes (Bite cells). dehydrogenase
pattern. What is the diagnosis? deficiency
IHC: Ki67=100%, MYC(+) (G6PD
FISH: (+) t(8:14) cMYC deficiency)
What is the diagnosis? 6/M, African, presented with relapsing Sickle cell
45/F, with history of Sjogren syndrome, developed a Marginal excrucitating pain on the leg and recurrent anemia (with
right parotid mass. zone pneumonia; Sputum culture revealed: Streptococcus autosplenecto
Incision biopsy: sheets of small lymphocytes lymphoma pneumoniae; PBS: Sickle-shaped erythrocytes. my as
IHC: CD3, CD5, CD10 (-), CD20 (+) What is the diagnosis? complication)
What is the most likely diagnosis? 25/F, chronically anemic, otherwise unremarkable; Thalassemia
67/M, with generalized brown-tan scaly, plaques, Mycosis PBS: microcytic, hypochromic erythrocytes with (β-thalassemia
and was managed as a case of psoriasis for several fungoides several target cells; Gap PCR showed deletion in 1 minor)
months with no relief. (Cutaneous T- β-globin gene. What is the diagnosis?
Skin biopsy: Collections of cells with cerebriform cell
nuclei (Sezary cells) in the epidermis (Pautrier lymphoma) THALASSEMIA SYNDROMES
microabscesses) # Affected
IHC: CD4 (+) Clinical syndrome Clinical manifestations
gene
What is the diagnosis? β-thalassemia
Based on the third case under Hodgkin lymphoma Anaplastic β-thalassemia major 2 Severe; blood transfusion
(diagnosis is lymphocyte-depleted HL), if IHC: CD30, large cell required
ALK (+), CD45(-), PAX5(-), what is the histologic lymphoma, β-thalassemia Variable Severe; regular transfusions
diagnosis? ALK-positive intermedia not required
β-thalassemia minor 1 Asymptomatic with mild or
PLASMA CELL NEOPLASMS absent anemia; (+) red cell
78/M, with enlarging mass on the mandible. Initial Multiple abnormalities
impression was ameloblastoma. myeloma α-thalassemia
Biopsy: Sheets of plasmacytoid cells Silent carrier 1 Asymptomatic; no red cell
IHC: CD138 and Kappa chain (+), Lambda chain (-) abnormality
BM trephine: Hypercellular marrow with α-thalassemia trait 2 Asymptomatic; like β-
plasmacytoid cells thalassemia minor
Flow cytometry: Similar results as IHC HbH disease 3 Severe; like β-thalassemia
CBC: Low hemoglobin intermedia
Chemistry: Elevated serum Ca and creatinine Hydrops fetalis 4 Lethal in utero without
What is the most likely diagnosis? transfusions
MYELODYSPLASTIC SYNDROME 39/M, with cola-colored urine upon first Paroxysmal
60/M, with long-standing anemia and Myelodysplastic morning voiding; Urinalysis: 0-1 RBC/HPF. Flow nocturnal
thrombocytopenia. syndrome cytometry: (-) CD55 and CD59 in almost 100% hemoglobinuria
BM trephine: Hypercellular marrow of red cells. What is the diagnosis?
BM smear: Ringed sideroblasts >20% of 17/F, with history of productive cough with Cold agglutinin
erythroids, hypogranular PMNs, Pseudo-Pelger whitish sputum for 5 days that spontaneously immunohemolytic
Huet cells, and dwarf, hypolobated, and Pawn ball resolved, developed anemia 5 days after; CBC: anemia
megakaryocytes. (Dysplastic forms make up more Increased MCV; PBS: agglutinated erythrocytes
than 10% of each respective population) with schistocytes. Coombs test is positive. What
What is the most likely diagnosis? is the diagnosis?
68/F, known case of CLL, presents with chronic Warm agglutinin
CHRONIC MYELOPROLIFERATIVE DISORDERS anemia. PBS: agglutinated erythrocytes with immunohemolytic
(Technically, CML belongs to this group, but for the sake of easier presentation of
schistocytes. Coombs test is positive. What is the anemia
concepts, it was discussed under Leukemias)
diagnosis?
Common features of chronic • Increased proliferative
myeloproliferative disorders 34/M, documented case of thrombotic Microangiopathic
drive in bone marrow
thrombocytopenic purpura (TTP), presents hemolytic anemia
• Extramedullary
with anemia. PBS: several schistocytes. What is
hematopoiesis
the most likely diagnosis?
• Spent phase
• Variable
HEMOLYTIC ANEMIAS: SUMMARY
transformation to AML
Disease Type of hemolysis Site of hemolysis
Increase in all cell lines, but erythroid Polycythemia vera (PV)
Hereditary Intrinsic Extravascular
lines are more increased; associated
spherocytosis (HS)
with JAK2 mutations in most cases; 2%
G6PD deficiency Intrinsic BOTH
chance of transformation to AML
Sickle cell anemia Intrinsic Extravascular
Increase in megakaryocytic lines; Essential thrombocytosis
(SCA)
associated with JAK2 mutations in 50% of (ET)
cases; transformation to AML is Thalassemia Intrinsic Extravascular
uncommon Paroxysmal nocturnal Intrinsic Intravascular
Extensive deposition of collagen in Primary myelofibrosis hemoglobinuria
marrow by non-neoplastic fibroblasts; (PM) (PNH)
associated with JAK2 mutations in 50- Immunohemolytic Extrinsic BOTH (depending on
60% of cases; 5-20% chance of anemias type)*
transformation to AML Microangiopathic Extrinsic Intravascular
hemolytic anemia
Macroangiopathic Extrinsic Intravascular
13. RED BLOOD CELL AND BLEEDING hemolytic anemia
DISORDERS * - Major types of immunohemolytic anemias usually exhibit
RED CELL DISORDERS EXTRAVASCULAR hemolysis (see main handout)
Note: The chapter focuses on the COMMON anemias (excluding anemia of
acute blood loss). For polycythemia, please refer to the main handout. HYPOPROLIFERATIVE ANEMIAS
QUESTION ANSWER 35/M, strict vegan for 2 years, developed loss of Megaloblastic
HEMOLYTIC ANEMIAS proprioception and anemia. PBS: macro-ovalocytes anemia
Common features: and hypersegmented PMNs. BM trephine biopsy: (Vitamin B12
1. Shortened red cell life span (<120 days) Hypercellular marrow. What is the diagnosis, and deficiency)
2. ↑ EPO levels → ↑ Erythropoiesis (compensatory) what is the vitamin deficient in the following case?
3. Accumulation of hemoglobin degradation products 6/F, with chronic malaise and pallor. CBC: Iron deficiency
3/M, CBC: increased MCHC; PBS: mostly spherical Hereditary microcytic, hypochromic erythrocytes; low serum anemia
cells without central pallor; Osmotic fragility spherocytosis Fe, high TIBC, low ferritin. What is the diagnosis?
testing (+). What is the diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 12 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
35/F with breast carcinoma; CBC: normocytic Anemia of LBB born term with a hilot, developed Vitamin K deficiency
erythrocytes with moderate hypochromia; low chronic hematochezia. CBC: normal platelet count
serum Fe, low TIBC, high ferritin. What is the disease and BT; prolonged PT and PTT. What is the
diagnosis? diagnosis?
12/F, with bacterial URTI and complete course of Aplastic 34 G1P1 postpartum with excessive bleeding. Disseminated
Chloramphenicol for treatment, developed anemia anemia CBC: low platelet; prolonged bleeding intravascular
and epistaxis; PE: no organomegaly; CBC: parameters. Patient eventually expired, and coagulation (DIC)
pancytopenia; BM trephine: Hypocellular marrow. was found to have suffered from amniotic
What is the diagnosis? fluid embolism on autopsy. What is the most
35/F with a mediastinal mass and anemia. Biopsy Pure red cell likely bleeding disorder did the patient suffer
of the mass showed thymoma; CBC: normal WBC aplasia (PRCA) from?
and platelet counts; BM trephine: hypo- to
normocellular marrow with marked decreased BLEEDING DISORDERS: SUMMARY
only in erythroid precursors. What is the diagnosis? Disease PC BT PT PTT
46/F with pallor and epistaxis. PE: Myelophthisic Ehler-Danlos syndrome N N N N
hepatosplenomegaly; CBC: WBC=400,000 with anemia Immune thrombocytopenic ↓ ↑ N N
40% Blasts; PBS: several dacrocytes; BM trephine: purpura
Hypercellular marrow with 35% Blasts. What is the Thrombotic ↓ ↑ N N
most appropriate diagnosis for the anemia? thrombocytopenic purpura
Bernard-Soulier disease ↓ ↑ N N
BLEEDING DISORDERS Glanzmann thrombasthenia N ↑ N N
Note: The chapter focuses on the common bleeding disorders. For Von Willebrand disease N ↑ N ↑
transfusion reactions, please refer to the main handout. Hemophilia N N N ↑
Bleeding Bleeding Vitamin K deficiency N N ↑ ↑
Bleeding Clinical
function disorder DIC ↓ ↑ ↑ ↑
parameters manifestations
determined category
Platelet count Platelet Disorders of Superficial (skin
(PC) number platelet and mucosal)
14. LUNG AND PLEURA
number bleeding, OBSTRUCTIVE AND RESTRICTIVE LUNG DISEASES
Bleeding time Platelet Defects of petechiae Parameter Obstructive Restrictive
(BT) function platelet Fundamental ↑ Airway resistance Reduced expansion of
function Pathology due to obstruction the lung parenchyma
Prothrombin Coagulation: Disorders of Deep-seated with ↓ TLC
time (PT) extrinsic coagulation bleeding, Examples Bronchial asthma, Pulmonary fibrosing
pathway Hemarthroses Emphysema*, Chronic diseases, and chest
Activated partial Coagulation: bronchitis*, wall disorders
thromboplastin intrinsic Bronchiectasis
time (aPTT) pathway Lung volumes ↑ ↓
FEV1 ↓↓ ↓
DISORDERS OF PLATELET NUMBER FVC ↓ ↓↓
(Common laboratory abnormality: THROMBOCYTOPENIA AND FEV1/FVC ratio ↓ (<0.7) Normal to ↑
PROLONGED BLEEDING TIME)
26/F, with SLE. Presents with epistaxis and mild Chronic ITP QUESTION ANSWER
splenomegaly. PBS: large platelets; BM trephine OBSTRUCTIVE LUNG DISEASES
biopsy: Increased megakaryocytes with 70/M, smoker, presented with dyspnea. PE: Emphysema,
dysplasia <10% of population (allowable). What barrel-chested, in tripod position, and centriacinar type
is the diagnosis? moderate distress. Patient eventually expired, (Pink puffers)
11/M, post-viral URTI, presented with epistaxis. Acute ITP despite appropriate management. Autopsy
PBS: large platelets; BM trephine biopsy: showed destruction of air spaces distal to
Increased megakaryocytes with dysplasia <10% terminal bronchioles, leading to their
of population (allowable) enlargement, without obvious fibrosis; the
54/M, known case of MI, maintained on Heparin-induced process mainly involves respiratory
heparin, presented with claudication with his thrombocytopenia bronchioles, with sparing of the alveoli. What is
left leg. Angiography: thrombotic occlusion of (HIT) the diagnosis?
the posterior tibial artery. What is the 35/M, non-smoker, with family history of Emphysema,
diagnosis? multiple deaths either due to liver cancer or a panacinar type
34/M, with fever, pallor, epistaxis, and seizures. Thrombotic pulmonary disease, presented with respiratory
CBC: anemia and thrombocytopenia; PBS: thrombocytopenic distress, and eventually died. Autopsy showed
numerous schistocytes; Elevated serum purpura (TTP) destruction of air spaces distal to terminal
creatinine. What is the diagnosis? bronchioles, leading to their enlargement,
26/M, with history of beef consumption from a Hemolytic Uremic without obvious fibrosis; the process involves
grill offering "unlimited beef", developed pallor Syndrome (HUS) the respiratory bronchioles and the alveoli.
and epistaxis with dysentery. CBC: anemia and What is the diagnosis?
thrombocytopenia; PBS: numerous 50/M, smoker, with history cough with sputum Chronic bronchitis
schistocytes; Elevated serum creatinine. What production for at least 3 months for at least 2 (Blue bloaters)
is the diagnosis? consecutive years, presented with dyspnea, and
DISORDERS OF PLATELET FUNCTION eventually expired. Autopsy showed
(Common laboratory abnormality: PROLONGED BLEEDING TIME) enlargement of mucous-secreting glands and
23/M, with epistaxis; CBC: decreased platelet Bernard-Soulier chronic inflammation with bronchiolar wall
count; normal PT/PTT. What is the diagnosis? syndrome fibrosis. What is the diagnosis?
24/F, with gum bleeding on minor trauma; Glanzmann 15/M, with a history of viral URTI, presented Bronchial asthma
CBC: normal platelet count; normal PT/PTT. thrombasthenia with dyspnea. PE: wheezes all over. Salbutamol (Status
What is the diagnosis? nebulization offered partial relief, however, asthmaticus)
DISORDERS OF COAGULATION after a few hours, patient arrested and expired.
(Common laboratory abnormality: PROLONGED COAGULATION Autopsy showed bronchoconstriction and
PARAMETERS, depending on the pathway involved obstruction of small airways by thick tenacious
mucus plugs. What is the diagnosis?
34/M, with easy bruising. CBC: normal Von Willebrand
platelet count; prolonged BT and PTT; disease (vWD) 13/F, known case of cystic fibrosis, with a Bronchiectasis
normal PT. What is the diagnosis? chronic history of cough with copious amount
of foul-smelling sputum, presented with
12/M, with hemarthrosis of the right knee. Hemophilia
dyspnea and eventually expired. Autopsy showed
CBC: normal platelet count, BT and PT; (Hemophilia A –
grossly dilated airways, with intense acute and
prolonged PTT. What is the diagnosis, and Factor VIII
chronic inflammatory exudation within the
what factors are missing for the major types of deficiency;
walls of the bronchi and bronchioles, fibrosis of
the disease? Hemophilia B
the bronchial and bronchiolar walls, and
(Christmas disease) –
peribronchiolar fibrosis. What is the diagnosis?
Factor IX deficiency
For restrictive lung diseases, please refer to the main handout.
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 13 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
BASIC PATTERNS OF PULMONARY INFECTIONS LUNG CARCINOMAS
Broncho- Note: Remember that most lung tumors are carcinomas (95%), so a lung mass can
Parameter Lobar pneumonia be considered to be malignant unless proven otherwise. Clinically, patients usually
pneumonia
have a history of chronic smoking, and usually present with chronic cough with
Consolidation Patchy Lobar or large portion of lobe
profound weight loss.
Gross Consolidated • Congestion: red, heavy, boggy
45/M, smoker. Mass location: central (left Squamous cell
areas of acute • Red hepatization: red, firm,
primary bronchus). CT guided biopsy (core): carcinoma
suppurative airless
Sheets of anaplastic cells with eosinophilic
inflammation • Gray hepatization: grayish-
cytoplasm with intercellular bridges and
brown
dyskeratotic cells. Immunohistochemistry: p63,
• Resolution: resorption of
p40 (+). What is the diagnosis?
exudates; or organization
39/F non-smoker. Mass location: peripheral. CT Adenocarcinoma
(fibrosis)
guided biopsy (core): Anaplastic cells forming
Histology Neutrophil- • Congestion: vascular
glandular structures; some of which contain
rich exudate engorgement with intra-alveolar
mucin. Immunohistochemistry: TTF-1, napsin A
that fills the fluid, few PMNs, and numerous
(+). What is the diagnosis?
airways bacteria
60/M, smoker. Mass location: central. CT-guided Small cell (Oat
• Red hepatization: PMNs, RBCs,
biopsy: sheets of small, round, blue cells with cell) carcinoma
and fibrin
crushing artifact on a markedly necrotic
• Gray hepatization: RBCs
background. Immunohistochemistry: CD57,
disintegrate, fibrinosuppurative
Chromogranin (+). What is the diagnosis?
exudate
56/M, smoker. Mass location: central. CT-guided Large cell
• Resolution: exudates resorbed
biopsy: sheets of large, anaplastic cells. carcinoma
or ingested by macrophages; or
Immunohistochemistry: p63, p40, TTF-1, napsin (Undifferentiated)
fibrosis
A (-). What is the diagnosis?
OTHER PNEUMONIA SYNDROMES
DISEASES OF THE PLEURA
18/M, in a dormitory, exposed to Atypical pneumonia
60/F, staying at an old ancestral house, Malignant
roommates that have productive cough (probably Mycoplasma in
presented with sudden dyspnea. CXR mesothelioma,
with whitish sputum without fever, origin)
revealed massive left pleural effusion. epithelioid type
presented with the same symptoms. CXR:
CTT was inserted draining 8L of (Note: Malignant
interstitial infiltrates. What is the mesothelioma is commonly
serosanguinous fluid. CXR: ill-defined
diagnosis? associated with asbestos, but
mass occupying the left lobe. CT-guided
34/M, from an intense alcohol drinking Lung abscess the most common cancer
biopsy core: Anaplastic cells forming
session, developed productive cough with asbestos causes is still lung
glandular structures. cancer)
copious, yellowish, foul-smelling sputum
Immunohistochemistry: TTF-1, napsin A (-
and high-grade fever. CXR showed a
), Calretinin, CK5,6 (+). What is the
cavity with air-fluid level on the right
diagnosis?
lower lung field. What is the diagnosis?
TUBERCULOSIS 15. HEAD AND NECK
35/M, presented with productive cough for Tuberculosis, QUESTION ANSWER
2 weeks duration with no relief of pulmonary; ORAL CAVITY
symptoms after a 1-week course of Co- Tuberculous 46/M, smoker, with a white plaque on the Leukoplakia
Amoxiclav, with associated cervical lymphadenitis lateral aspect of the tongue that cannot
lymphadenopathy. CXR: apical opacities; be scraped off. Punch biopsy showed
Sputum AFB: 3+; Lymph node biopsy acanthosis, hyperkeratosis, and atypical
showed caseating granulomas with squamous cells, and an intact basement
Langhans type giant cells. What is the membrane. What is the diagnosis?
diagnosis? Based on the case above, the patient was Squamous cell
Formation of granulomas in a patient with Cell-mediated lost to follow-up, and after 5 years, carcinoma
tuberculosis signifies an intact immunity (Granuloma presented with an ulcerating necrotic
is a T-cell response) mass on the site where the plaque used
Based on the case above, if the patient is Macrophages filled to be. Biopsy showed nests of anaplastic
positive for HIV, and has a profoundly with acid fast bacilli cells with eosinophilic cytoplasm and
depressed CD4 count, what would be the several keratin pearls. What is the
expected morphologic finding? diagnosis?
What is the cytokine secreted by TH1 cells IFN-γ 39/F, with an enlarging mandibular Ameloblastoma
that leads to formation of granulomas? mass. Panoramic X-ray: Soap bubble
lesions with well-defined borders.
TUBERCULOSIS: CLINICAL FORMS Hemimandibulectomy was performed.
Form Lesions Sequelae Biopsy of the mass showed nests with an
Primary • Ghon focus • Healing by fibrosis outer layer of columnar cells with
(consolidation): (generally happens in reverse polarity of nuclei, and an inner
subpleural, (lower part immunocompetent layer, resembling stellate reticulum.
of upper lobe or upper individuals, and with What is the diagnosis?
part of lower lobe) anti-TB therapy)
• Ghon complex: GF + UPPER AIRWAYS
pulmonary hilar node 35/M, smoker, with chronic nasal Nasopharyngeal
involvement congestion and cervical carcinoma
Secondary • Simmon focus • Healing by fibrosis lymphadenopathy. Endoscopy: friable, (Undifferentiated,
(consolidation): apical • Localized caseating cream-white mass obstructing the Lymphoepithelial
destructive lesions nasopharynx. Punch biopsy of the mass, carcinoma)
• Progressive secondary and lymph node biopsy were performed,
Progressive • Erosion into bronchi or • Miliary pulmonary TB and showed sheets and nests of highly
pulmonary vessels anaplastic cells with dense lymphocytic
• Spread into adjacent infiltrate in the stroma. What is the
parenchyma diagnosis?
• Pleural involvement: 4/M, with a history of hoarseness and Laryngeal papilloma
effusions, empyema, stridor. Neonatal history: born via VSD to (Juvenile respiratory
obliterative fibrous a mother with condyloma acuminata via papillomatosis)
pleuritis a hilot in the province. Laryngoscopy:
Miliary • Scattered small • Disseminated multiple, fleshy, papillary excrescences
pulmonary foci of consolidation TB (Miliary pattern in on the larynx. What is the diagnosis?
throughout lung other organs)
parenchyma
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 14 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
70/M, smoker, presented with persistent Laryngeal squamous cell STOMACH
hoarseness. Laryngoscopy: pale-tan carcinoma GASTRITIDES
exophytic mass on the on the larynx with Common presentation: Epigastric pain
friable excrescences. Biopsy shows nests Endoscopy: predominantly antral erythema H. pylori
of anaplastic cells with eosinophilic Serology: anti H. pylori antibodies (+) gastritis
cytoplasm and several keratin pearls. Biopsy: Mononuclear infiltrate in lamina propria
What is the diagnosis? with intestinal metaplasia
What is the diagnosis?
EARS Endoscopy: erythema pronounced at the corpus Autoimmune
35/F with a chronic history of aural Chronic suppurative Serology: anti IF and proton pump antibodies (+) gastritis
fullness and yellowish aural discharge, otitis media with Biopsy: Chief cell loss with mononuclear infiltrate
presented with unilateral hearing loss. cholesteatoma concentrated on the glands
Otoscopy revealed an "earwax-like" mass What is the diagnosis?
in the middle ear space. Mastoidectomy PEPTIC ULCER DISEASE
was done: Biopsy showed stratified Common presentation: Epigastric pain with/without hematemesis
cytologically benign squamous cells and Common morphology: NIGS: N: necrosis, I: acute inflammation, G:
keratinous material. What is the granulation tissue, S: fibrous scar (from superficial to deep)
diagnosis? 34/F, with pain felt shortly after meals, without Gastric ulcer
nocturnal awakening from pain. Gastric pH:
NECK increased
5/M, with a left lateral neck mass along Branchial cleft cyst Endoscopy: Ulcer located at the corpus
the SCM. Excision biopsy was done, and 34/M, with pain felt hours after meals, with nocturnal Duodenal
showed a unilocular cystic space lined by awakening from pain. Gastric pH: decreased ulcer
stratified squamous epithelium with Endoscopy: Ulcer located at the antrum
lymphoid aggregates on the cyst wall. NEOPLASMS
What is the diagnosis? 45/M, with progressive early satiety and Gastric carcinoma,
6/F, with an anterior neck mass at the Thyroglossal duct cyst profound weight loss. Endoscopy revealed an intestinal type
midline that moves with deglutition. ulcerated lesion with heaped-up borders.
Sistrunk procedure was performed, and Biopsy showed structures resembling intestinal
biopsy showed a unilocular cystic space glands, lined by dysplastic epithelial cells
lined by respiratory epithelium with few invading the stroma. What is the diagnosis?
islands of thyroid follicles on the cyst Based on the case above, if biopsy revealed Gastric
wall. What is the diagnosis? poorly cohesive cells with signet ring cells, adenocarcinoma,
what is the diagnosis? diffuse type
SALIVARY GLAND TUMORS Based on the case above, if endoscopy revealed a Gastric MALT
32/F, with a parotid mass. Excision biopsy Pleomorphic adenoma large, exophytic, cream-white, ovoid, fleshy lymphoma
was done, and showed nests of benign mass, and biopsy revealed sheets of uniform,
looking epithelial cells, occasionally small lymphocytes, what is the diagnosis?
forming duct-like structures, embedded Based on the case above, if the patient presented Gastric carcinoid
in a myxoid stroma. What is the with diarrhea, flushing, and episodic dyspnea,
diagnosis? and endoscopy revealed a small, exophytic,
36/F, with a parotid mass. Excision biopsy Mucoepidermoid fleshy, ovoid, fleshy mass, and biopsy showed
was done, and showed sheets of carcinoma sheets and nests of uniform cells with scant
anaplastic squamous and mucus- cytoplasm and stippled nuclei, and
secreting cells. What is the diagnosis? immunohistochemistry: Chromgranin and
37/M, smoker, with a submandibular Warthin tumor Synaptophysin (+), what is the diagnosis?
mass. Excision biopsy was done, and (Papillary cystadenoma Based on the case above, if endoscopy revealed a Gastrointestinal
showed, double-layer of oncocytic lymphomatosum) large, fleshy, ovoid mass, and biopsy showed stromal tumor
epithelial cells with a dense lymphocytic spindle cells, and immunohistochemistry: (GIST)
infiltrate in the stroma. What is the CD117(+), what is the diagnosis?
diagnosis?
30/F, with a mass on the inner side of the Adenoid cystic SMALL AND LARGE INTESTINES
upper lip. Excision biopsy was done, and carcinoma INFLAMMATORY BOWEL DISEASE
showed gland-like structures; some Feature Crohn disease Ulcerative colitis
showing cribriform pattern; lined by Macroscopic
small cells with scant cytoplasm and Bowel region Ileum + colon Colon only
hyperchromatic compact nuclei. What is Distribution Ski lesions Diffuse
the diagnosis?
Stricture Yes Rare
Wall appearance Thick Thin
16. GASTROINTESTINAL TRACT Microscopic
ESOPHAGUS Inflammation Transmural Limited to mucosa
NON-NEOPLASTIC LESIONS Pseudopolyps Moderate Marked
23/M, with burning epigastric pain, heartburn and Reflux Ulcers Deep, knife-like Superficial, broad-
water brash. Endoscopy revealed mucosal breaks and esophagitis based
erythema. Biopsy show eosinophils in mucosa with Lymphoid reaction Marked Moderate
basal zone hyperplasia exceeding 20% of total
Fibrosis Marked Mild to none
epithelial thickness. What is the diagnosis?
Based on the case above, patient was lost to follow up, Barrett Serositis Marked Mild to none
and came back after 5 years, without clinical esophagus Granulomas Yes (~35%) No
improvement. Endoscopy revealed pinkish/reddish Fistulous/sinuses Yes No
areas. Biopsy show intestinal metaplasia. What is the Clinical
diagnosis? Perianal fistula Yes (in colonic No
47/M, chronic alcoholic, diagnosed with cirrhosis, Esophageal disease)
presents with hemoptysis and underwent shock, and varices Fat/vitamin Yes No
eventually expired. Autopsy of the esophagus showed malabsorption
dilated submucosal vessels. What is the diagnosis? Malignant potential With colonic Yes
ESOPHAGEAL CARCINOMA involvement
Common presentation: Progressive dysphagia and/or odynophagia with Recurrence after Common No
constitutional symptoms e.g. weight loss surgery
34/M, smoker, with a history of suicide attempt Squamous cell Toxic megacolon No Yes
through caustic ingestion. Biopsy showed nests of carcinoma
atypical squamous cells invading the stroma.
What is the diagnosis?
34/M, smoker, with chronic untreated GERD. Adenocarcinoma
Biopsy showed glands lined by dysplastic
epithelial cells, invading the stroma. What is the
diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 15 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
NEOPLASMS METABOLIC LIVER DISEASE
56/M, with pallor and weakness. CBC and PBS: Colonic 45/M, known hypertensive and diabetic, non- NAFLD
microcytic hypochromic anemia; low serum Fe, adenocarcinoma alcoholic. Liver biopsy showed lipid droplets in
high TIBC. Colonoscopy was done, showing a bulky, hepatocytes. What is the diagnosis?
fleshy, exophytic mass in the ascending colon. Based on the case above, if liver biopsy showed NASH
Biopsy revealed irregular glands lined by predominantly mononuclear infiltrates,
dysplastic epithelial cells, invading the stroma. periportal fibrosis, and less Mallory-Denk
What is the diagnosis? bodies, what is the diagnosis?
27/M, known diabetic, with skin Hereditary
FAMILIAL TUMOR SYNDROMES hyperpigmentation, and liver cirrhosis. Liver Hemochromatosis
Parameter Familial adenomatous Hereditary nonpolyposis biopsy with Prussian blue revealed hemosiderin
polyposis (FAP) colon cancer (HNPCC) deposition in hepatocytes. What is the
(Lynch syndrome) diagnosis?
Syndrome Multiple colorectal Familial clustering of 34/M, came in the neurology clinic for Wilson disease
adenomas as teenagers colorectum, endometrium, dysarthria. On assessment of pupillary light (Hepatolenticular
stomach, ovary, ureters, reflex, (+) Kayser-Fleisher rings. Chemistry: low degeneration)
brain, small bowel, serum ceruloplasmin and high urinary Cu.
hepatobiliary tract, What is the diagnosis?
pancreas, and skin 21/F, presenting with exertional dyspnea and α-1-antitrypsin
Mutations APC (Ch5) MSH2, MLH1 jaundice, with family history of lung disease. deficiency
Diagnosis 100 polyps Amsterdam criteria Liver biopsy showed PAS (+) hyaline globules.
Clinical Colonic adenocarcinoma What is the diagnosis?
significance develops in 100% of
untreated patients often CHOLESTATIC LIVER DISEASE
before 30 and nearly 44/F, known case of gallstones, presented with Ascending
always by age 50 fever, jaundice and RUQ pain. Patient was cholangitis
Associations Gardner syndrome: started on IV antibiotics and underwent ERCP
Osteomas, thyroid and with sphincterotomy, What is the diagnosis?
desmoid tumors, skin cysts 1w/M, with jaundice and bilirubinuria. TB and Extrahepatic
Turcot syndrome: DB were elevated. If liver biopsy showed biliary atresia
Medulloblastoma, inflammation and fibrosing stricture of the
Glioblastoma hepatic bile ducts, what is the diagnosis?
APPENDIX GALLBLADDER
28/M, with initial periumbilical pain shifting to the Acute NON-NEOPLASTIC CONDITIONS
RLQ, with associated fever, anorexia, and vomiting. suppurative 45/F, obese, presented with colicky Chronic calculous
Appendectomy was performed. Biopsy showed PMNs in appendicitis epigastric pain after eating. cholecystitis
muscularis layer. What is the diagnosis? Cholecystectomy was performed. Grossly, (Xanthogranulomatous
28/F, clinically diagnosed with acute appendicitis, Carcinoid, the gallbladder is filled with stones and cholecystitis)
underwent appendectomy. Sections of the appendix appendix the mucosal surface is ridden with
showed congestion, but an incidental finding of sheets multiple yellow pinpoint excrescences.
and nests of uniform cells with scant cytoplasm and Biopsy showed mononuclear infiltrates in
stippled nuclei. Immunohistochemistry: the mucosa with lipid-laden macrophages
Chromogranin and Synaptophysin (+). What is the (cholesterolosis), and prominent
diagnosis? Rokitansky-Aschoff sinuses. What is the
diagnosis?
17. LIVER AND GALLBLADDER
LIVER TUMORS
45/F, managed as a case of chronic Gallbladder
QUESTION ANSWER
calculous cholecystitis is undergoing adenocarcinoma
VIRAL HEPATITIDES
laparoscopic cholecystectomy, but
25/M, with history of eating street foods, Acute Hepatitis A
gallbladder was found to be large, needing
presented with right upper quadrant pain and infection
conversion to open cholecystectomy. Biopsy
jaundice. ALT and AST were elevated; Serology:
showed irregular glands lined by
anti HAV (+); Liver biopsy showed scant portal
dysplastic epithelial cells, invading the
mononuclear infiltrate, predominantly plasma
stroma. What is the diagnosis?
cells, and hepatocyte necrosis and apoptosis.
50/F, presenting with signs of obstructive Cholangiocarcinoma
What is the diagnosis?
jaundice, with dyspnea. CXR: multiple
43/M, with positive HBsAg 7 months prior, still Chronic active
cannon-ball lesions; Abdominal UTZ:
has (+) HBsAg, (-) anti HBs, and (+) HBeAg. ALT Hepatitis B
multiple hepatic nodules. Patient
and AST were elevated; Liver biopsy showed infection
eventually expired. Biopsy of the bile duct
dense portal mononuclear infiltrate, and
showed glands lined by dysplastic
ground-glass hepatocytes. What is the
epithelial cells that invade the stroma.
diagnosis?
What is the diagnosis?
43/M, with anti-HCV (+) for 8 months, Chronic Hepatitis
underwent HCV RNA testing, which turned out C infection
to be positive. ALT and AST were elevated; Liver
biopsy showed dense portal mononuclear
infiltrate, lymphoid follicles, bile duct injury,
and steatosis. What is the diagnosis?
ALCOHOLIC LIVER DISEASE
56/M, chronic alcoholic, prefers hard drinks, and Hepatocellular
is usually out for drinking sessions at least 4x a steatosis
week. Liver biopsy showed lipid droplets in
hepatocytes. What is the diagnosis?
Based on the case above, if liver biopsy showed Alcoholic
hepatocyte swelling (ballooning) and necrosis, steatohepatitis
Mallory-Denk bodies, and neutrophilic
infiltration, what is the diagnosis?
Based on the case above, if liver biopsy showed Alcoholic
perisinusoidal chicken-wire fence pattern of Steatofibrosis
fibrosis, what is the diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 16 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
AUTOIMMUNE CHOLANGIOPATHIES 18. PANCREAS
Primary sclerosing
Features Primary biliary cirrhosis QUESTION ANSWER
cholangitis
PANCREATITIDES
Age Median age 50 years (30-70) Median age 30
55/M, alcoholic, with history of gallstones, but Acute
Gender 90% Female 70% Male
refused to be operated on, presented with severe pancreatitis
Clinical Progressive Unpredictable but
epigastric pain, boring in character, radiating to (Biliary
course progressive
the back, with associated jaundice, acholic pancreatitis)
Associated Sjogren syndrome (70%) IBD (70%) stools, and tea-colored urine. Despite appropriate
conditions Scleroderma (5%) Pancreatitis (≤25%) management, he expired. Autopsy of the pancreas
Thyroid disease (20%) Idiopathic fibrosing shows microvascular leak and edema, enzymatic
diseases fat necrosis, acute inflammation, destruction of
(retroperitoneal pancreatic parenchyma, and destruction of
fibrosis blood vessels, and interstitial hemorrhage. What
Serology 95% AMA(+) 0-5% AMA(+) (low is the diagnosis?
50% ANA(+) titer) 59/M, alcoholic, complaining of recurrent Chronic
40% ANCA(+) 6% ANA(+) epigastric pain with food intake, with pancreatitis
65% ANCA(+) consequent anorexia and weight loss, coupled
Radiology Normal Strictures and beading with chronic steatorrhea. He was admitted for
of large bile ducts; pneumonia for several days, and eventually
pruning of smaller expired. Autopsy of the pancreas shows fibrosis,
ducts atrophy, dropout of acini, variable dilation of
Inflammation Often granulomatous Sclerosing pancreatic ducts, and chronic inflammation.
Bile ducts Small to medium-sized, All sizes, Intrahepatic What is the diagnosis?
involved Intrahepatic and Extrahepatic NEOPLASMS
Histologic • Active destruction of • Large duct: 68/M, smoker, presents with jaundice, acholic Pancreatic
pearls interlobular bile ducts by Neutrophilic stools, tea-colored urine, with associated cough. adenocarcinoma
lymphoplasmacytic infiltration on a Chemistry: Elevated TB and DB; Serology: (+) CA with metastases
infiltration with or without background of 19-9. Imaging showed a mass on the pancreatic to the liver and
granulomas (Florid duct chronic head, with multiple nodules on the liver and the lungs
lesion) inflammation lungs. Biopsy showed glands lined by dysplastic
• (+) Mallory-Denk bodies • Small duct: onion- epithelial cells accompanied by intensely
• Ductular reaction skin fibrosis desmoplastic stroma. What is the diagnosis?
• Micronodular cirrhosis
with hepatomegaly (vs.
other forms of cirrhosis) 19. KIDNEY
Diagnosis Liver biopsy Radiologic imaging of QUESTION ANSWER
biliary tree (beading of GLOMERULAR DISEASES
contrast medium) Nephritic syndrome: 1. Hematuria (with dysmorphic RBCs and red cell
Others - Increased risk of casts indicating glomerular pathology); 2. Oliguria and azotemia;
cholangiocarcinoma and 3. Hypertension
15/M, with history of sore throat 4 weeks prior to onset of PSAGN
STRUCTURAL ABNORMALITIES IN THE BILIARY TREE symptoms, with an increased ASO titer, and decreased C3.
20/M, with jaundice, RUQ pain, and an Choledochal cyst LM: diffuse hypercellularity (almost, if not all glomeruli)
abdominal mass. Exploratory laparotomy EM: subepithelial humps on GBM
was performed, which showed cystic IF: granular deposits of IgG and complement within the
dilatation of the common bile duct. What capillary walls mesangium
is the diagnosis? Rapidly progressing glomerulonephritis: syndrome of progressive
loss of renal function, characterized by nephritic syndrome often with
TUMORS severe oliguria; histologic hallmark is presence of “crescents”, thus
43/F, asymptomatic, underwent Cavernous hemangioma crescentic GN
abdominal UTZ, with an incidental finding 25/M, smoker, with history of hemoptysis and oliguria RPGN
of a well-demarcated, hyperechoic EM: ruptures in the GBM Type I
nodule that she wants to be removed. IF: linear IgG and C3 deposits along the GBM
Biopsy showed large, dilated blood-filled 15/M, with a history of PSAGN RPGN
spaces lined by endothelial cells. What is EM: “lumpy bumpy” appearance of GBM (due to deposits) Type II
the diagnosis? IF: granular deposition of Ig and complement in GBM
40/F, asymptomatic with an incidental Focal nodular 30/M, known case of microscopic polyangiitis RPGN
finding of a liver nodule with a central hyperplasia EM: no detectable deposits Type III
scar on CT. Angiography: hypervascular IF: negative for Ig and complement
lesion, with normal to increased uptake
in liver scan. Biopsy showed nodules with 19/F with ESRD. Grossly, kidneys are symmetrically Chronic
large arteries not accompanied by veins contracted, surfaces are red-brown and diffusely granular; GN
or bile ducts. What is the diagnosis? histologically, glomeruli are obliterated with marked
Based on the case above, if CT findings did Hepatic adenoma interstitial fibrosis. What is the diagnosis?
not show any central scar, and
angiography showed a hypovascular Nephrotic syndrome: 1. Massive proteinuria (≥3.5g/dL; 2.
lesion with no uptake on liver scan, and Hypoalbuminemia (<3g/dL); 3. Generalized edema; 4. Hyperlipidemia
biopsy showed sheets of normal-looking and lipiduria
hepatocytes without portal tracts, what 7/M, with puffy eyelids and scrotal edema Minimal change
is the diagnosis? LM: none disease/Lipoid
47/M, known case of chronic hepatitis B Hepatocellular EM: uniform and diffuse effacement of foot nephrosis
with cirrhosis, presented with dyspnea carcinoma processes of the podocytes
and jaundice. CXR: multiple cannon ball 29/M, MSM, HIV (+) with a history of heroin abuse. Focal segmental
lesions; elevated serum AFP. CT scan LM: increased mesangial matrix, obliterated glomerulosclero
showed a lesion in the liver with early capillary lumina, and deposition effacement of foot sis (FSGS)
arterial enchancement and early processes of hyaline masses (hyalinosis) and lipid
washout of contrast. Biopsy showed droplets.
sheets of anaplastic hepatocytes; some of EM: Effacement of foot processes
which form pseudoglandular structures. IF: nonspecific trapping of immunoglobulins,
What is the diagnosis? usually IgM, and complement in the areas of
hyalinosis
25/F with Lung carcinoma. Membranous
LM: diffuse thickening of the capillary wall nephropathy
EM: subepithelial deposits along the GBM (spike and
dome appearance); effacement of foot processes
IF: granular deposits of immunoglobulins and
complement along the GBM
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 17 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
29/F with SLE. MPGN Type I NEPHROLITHIASES
LM: Thickened split GBM (Tram track appearance) Common presentation: Painful hematuria
EM: subendothelial electron-dense deposits
IF: Irregular granular C3 deposits, with IgG and TYPES OF NEPHROLITHS
early complement components (C1q and C4) Stone Urine Radiologic Associated
32/F with a complement defect i.e. persistent Dense deposit pH appearance conditions
activation. disease Calcium oxalate Acidic Opaque Various
LM: Thickened split GBM (Tram track appearance) Magnesium Basic Opaque Proteus infections
EM: lamina densa and glomerular capillary wall ammonium Large stones
transformed into irregular, ribbon-like, extremely phosphate/ occupying renal
electron-dense structure Triple calyces: Staghorn
IF: Irregular chunky and segmental linear foci of C3 phosphate/ calculi
deposits in GBM and mesangium, without IgG and Struvite
early complement components (C1q and C4) Uric acid Acidic Lucent Hyperuricemia/Hy
peruricosuria
ISOLATED GLOMERULAR ABNORMALITIES Cystine Acidic Opaque, but difficult Cystinuria
26/F, with history of viral URTI, developed IgA to visualize than Ca
hematuria nephropathy stones
LM: mesangial widening and segmental (Berger disease)
inflammation TUMORS
EM: mesangial electron-dense deposits 62/M, smoker, with hematuria, left flank pain Renal cell
IF: mesangial deposition of IgA, often with C3 and and a palpable left flank mass. CT-scan showed carcinoma (RCC)
properdin and smaller amounts of IgG or IgM a renal mass suspicious of malignancy, and
8/M, with palpable purpura in both lower Henoch- nephrectomy was done. What is the most likely
extremities, abdominal pain, and hematuria Schonlein diagnosis?
Morphologic findings same as above. purpura Biopsy shows rounded or polygonal cells with Clear cell RCC
11/M, with anterior lenticonus, sensorineural Alport abundant clear or granular cytoplasm. What is
hearing loss, and hematuria with proteinuria syndrome the diagnosis?
LM: glomerulosclerosis, vascular sclerosis, tubular Biopsy shows cuboidal or low columnar cells Papillary RCC
atrophy, and interstitial fibrosis arranged in papillary formation with
EM: thin GBM (early); irregular foci of GBM Psammoma bodies. What is the diagnosis?
thickening or attenuation (late); “basket-weave” Biopsy shows pale eosinophilic cells, often with Chromophobe RCC
appearance a perinuclear halo, arranged in solid sheets with a
concentration of the largest cells around blood
TUBULES AND INTERSTITIUM vessels. What is the diagnosis?
25/M, victim of hazing, with multiple ecchymoses Acute tubular
on both thighs, presents with cola-colored urine necrosis (Toxic
and increased BUN and creatinine. ATN) 20. LOWER URINARY TRACT AND MALE
LM: Extensive necrosis of tubules primarily Note: Ischemic ATN GENITAL TRACT
involving the proximal tubules has a different
distribution of
QUESTION ANSWER
necrosis LOWER URINARY TRACT
26/F, with fever, chills and left flank pain. Acute URINARY BLADDER
Urinalysis: WBC: 50-60/HPF with several WBC pyelonephritis 49/M, smoker, with painless hematuria, Muscle-invasive
casts. without any palpable flank or abdominal urothelial carcinoma
LM: Patchy, interstitial suppurative inflammation, mass. Cystoscopy showed multiple (from high-grade
intratubular aggregates of neutrophils, neutrophilic hemorrhagic papillary excrescences. urothelial carcinoma);
tubulitis and tubular necrosis Biopsy was done, which showed a papillary Poor prognosis
35/F, with history of recurrent acute Chronic architecture lined by highly atypical cells compared to
pyelonephritis, presents with increased BUN and pyelonephritis with high mitotic index, invading the superficial invasive
creatinine. muscularis propria. What is the diagnosis, and non-invasive
LM: Thyroidization and tubular atrophy; vascular and what is the prognosis?
sclerosis in scarred areas 49/M, with painless hematuria, and history Squamous cell
25/F, with increased BUN and creatinine, and a Drug-induced of multiple urinalysis results with a finding carcinoma,
history of Methicillin intake. interstitial of parasitic ova with prominent terminal Schistosoma
LM: interstitial inflammation, with abundant nephritis spine. Cystoscopy showed ulcerations with haematobium
eosinophils with several eosinophils and edema heaped-up borders with friable
excrescences. Biospy showed sheets of
VASCULAR DISEASES anaplastic cells with eosinophilic
56/M, known diabetic, with increasing BUN and Nephrosclerosis cytoplasm and prominent intercellular
creatinine. Impression was diabetic nephropathy. bridges. What is the diagnosis, and the
Blood vessels show hyaline arteriolosclerosis. parasitic infection that led its development?
What is the diagnosis?
50/M, known diabetic, with treatment resistant Renal artery TESTIS
hypertension that started 2 months ago. Renal stenosis NON-NEOPLASTIC CONDITIONS
vein sampling: right: normal renin, left: elevated 12/M, with an incidental finding of an Cryptorchidism
renin. What is the most likely diagnosis? absent left testicle, and a left inguinal mass.
Diagnosis was indirect inguinal hernia, left
CYSTIC DISEASES OF THE KIDNEY and the herniated testicle was removed.
Parameter Autosomal dominant Autosomal recessive Biopsy of the testis showed arrest in germ
(Adult) (Childhood) cell development, hyalinization and
Mutation • PKD1 (polycystin-1, PKHD1 (fibrocystin, Ch6; thickening of BM, increase in interstitial
Ch16; distal nephron) fetal kidney, liver and stroma, and prominent Leydig cells. What is
(85%; more severe) pancreas) the diagnosis?
• PKD2 (polycystin-2, 15/M, biker, complained of pain on the right Hemorrhagic
Ch4; all segments of testicle 12 hours prior to consult. Doppler infarction secondary
tubules) (15%; less ultrasound showed absent blood flow on to testicular torsion
severe) the left testicle. The patient was operated
Renal failure Yes immediately, but the testis was grossly
hemorrhagic intraoperatively, and was
Associated • Liver cysts Periportal fibrosis (if
consequently removed. Biopsy of the testis
anomalies • Intracranial berry patients survive infancy)
showed hemorrhagic infarction. What is the
aneurysms
diagnosis?
• Mitral valve prolapse
Most common Coronary or hypertensive Renal failure (in infancy)
cause of death heart disease (40%)
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 18 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TESTICULAR NEOPLASMS Based on the case above, if the atypical squamous High-grade
Common presentation: testicular mass; always take note of the age of the cells occupy the lower full-thickness of the squamous
patient when attempting to diagnose a testicular neoplasm. epithelium, What is the diagnosis? intraepithelial
Note: the most common cause of painless testicular enlargement is a lesion (HSIL),
testicular tumor; so a testicular mass is considered neoplastic, unless Carcinoma in situ
proven otherwise 32 G4P4 (4004), presented with foul-smelling Cervical
35/M, biopsy showed sheets of large, Seminoma (Classic) discharge per vagina, and vaginal bleeding. IE: ~ squamous cell
uniform cells with clear cytoplasm and 4 cm mass on the cervix at the 9 o'clock position, carcinoma
round nuclei with conspicuous nucleoli, Note: Female Bilateral parametria were unremarkable.
and intervening fibrous septae infiltrated counterpart is Speculum examination revealed pale-tan,
with lymphocytes; Immunohistochemistry: Dysgerminoma exophytic mass with friable excrescences. Punch
CD117 (c-kit) and PLAP (+). What is the biopsy was done showing sheets of anaplastic
diagnosis squamous cells. What is the diagnosis?
30/M, biopsy showed large, anaplastic cells Embryonal carcinoma
with indistinct borders, tumor giant cells, BODY OF THE UTERUS
and frequent mitosis. ENDOMETRIOSIS AND ADENOMYOSIS
Immunohistochemistry: CD117, PLAP (-), 43 G0 complaining of intense dysmenorrhea and Endometriosis
CD30 (+). What is the diagnosis? dyspareunia. Ultrasound revealed a cystic mass (Pelvic
3/M, biopsy showed glomeruloid structures Yolk sac on the right ovary. Right oophorocystectomy was endometriosis,
(Schiller-Duval) bodies and PAS-positive tumor/Endodermal perfomed. Incidental finding of multiple severe;
hyaline globules. Immunohistochemistry: sinus tumor/Infantile peritoneal implants was noted, and samples were endomteriotic
AFP (+). What is the diagnosis? embryonal carcinoma taken for biopsy. Grossly, the mass consists of a cyst, right ovary)
40/M, with multiple cannon-ball lesions on Choriocarcinoma unilocular cystic space containing chocolate
CXR, without a palpable testicular mass, brown material. Sections show endometrial
and an elevated serum HCG. VATS was done lining of the cyst wall. Biopsy of the implants
to get a biopsy of the nodules, which showed showed endometrial glands and stroma
sheets of anaplastic cytotrophoblasts and surrounded by a fibrotic stroma with chronic
synctiotrophoblasts without villus inflammation. What is the diagnosis?
formation. What is the diagnosis? 44 G3P3 (3003) complaining of chronic Adenomyosis
5/M, biopsy showed haphazardly arranged Teratoma (Benign) dysmenorrhea and menorrhagia. Corpus size is
neural tissue, cartilage, adipose tissue, compatible with that of 16 weeks AOG. TAHBSO
bone, and epithelial elements. What is the was performed and showing thickened
diagnosis, and what is the expected biological myometria with blood lakes. Biopsy revealed
behavior of the tumor? endometrial stroma with glands in the
Based on the case above, if the same tumor Malignant myometrium found ~ 5mm from the decidua
was observed in a 16-year old, what would basalis layer. What is the diagnosis?
be the expected biologic behavior of the ENDOMETRIAL DISORDERS
tumor? Common presentation: abnormal uterine bleeding
65/M, with rapidly enlarging testicular Testicular lymphoma 44 G2P2 (2002). UTZ: polypoid mass on the Endometrial
mass. Biopsy of the testis showed sheets of (Diffuse Large B-cell endometrial canal. UTZ-guided endometrial polyp
large, anaplastic cells. lymphoma) biopsy was done. Biopsy showed proliferative
Immunohistochemistry: CK and vimentin (-), phase endometrial glands in a fibrous stroma.
LCA/CD45, CD79a (+). What is the diagnosis? What is the diagnosis?
47 G0. Diagnostic curettage was performed Endometrial
PROSTATE yielding curettings with an aggregate diameter of hyperplasia
78/M, with nocturia. KUB-Prostate UTZ: Nodular prostatic 7.0 cm. Biopsy show back-to-back glands; some (Complex
enlarged prostate with estimated weight of hyperplasia of the cells lining the glands exhibit nuclear hyperplasia with
60 grams. Free PSA is elevated. TURP was rounding (normal is cigar-shaped). What is the atypia)
performed. Biopsy showed epithelial and diagnosis?
stromal hyperplasia with fibrous septae 45 G0. Diagnostic curettage was performed Endometrioid
forming multiple nodules. What is the yielding curettings with an aggregate diameter of carcinoma (Type
diagnosis? 5.0 cm. Biopsy showed haphazardly-arranged, I)
80/M, with nocturia. KUB-Prostate UTZ: Prostatic irregular, discrete and confluent glands lined by
enlarged prostate with estimated weight of adenocarcinoma cells with minimal atypia; some showing
60 grams. Complexed PSA is elevated. TURP (Gleason 3+4), WHO cribriform pattern. Areas of squamous
was performed. Biopsy showed small, group grade 2 differentiation are also noted. What is the
predominantly discrete and confluent diagnosis?
glandular structures, with several areas 65 G0, with palpable hypogastric mass. Serous carcinoma
showeding cribriform pattern invading the Diagnostic curettage was performed yielding (Type II)
fibromuscular stroma. What is the curettings with an aggregate diameter of 12.0 cm.
diagnosis? Biopsy showed papillary fronds lined by highly
anaplastic cells with high mitotic rate, some of
which exhibit detachment and hobnail pattern.
21. FEMALE GENITAL TRACT Areas of necrosis are also noted. What is the
Note: The chapter focuses on highly recurring concepts on the female
diagnosis?
genital tract. Please refer to the main handout for a more detailed
MYOMETRIAL TUMORS
discussion.
45 G4P4 (4004), apparently asymptomatic, came Leiomyoma
QUESTION ANSWER
in for a routine gynecologic check-up. UTZ:
CERVIX
multiple myoma uteri. TAHBSO was performed.
32 G0, complaining of post-coital bleeding with Endocervical Grossly, multple, cream-white, well-
minimal dyspareunia. Speculum exam revealed a polyp circumscribed, non-encapsulated, firm masses
fleshy polypoid mass on the cervix. Polypectomy are noted within the myometrium. Sections show
was done, showing a polypoid tissue with benign-looking smooth muscle cells arranged in
endocervical lining and an edematous stroma whorling pattern. What is the diagnosis?
with mild chronic inflammation. What is the
45 G5P5 (5005), with abdominal enlargement Leiomyosarcoma
diagnosis?
and profound weight loss. UTZ: Solitary
45 G5P5 (5005), came for a routine gynecologic Low-grade myometrial mass suspicious of malignancy.
checkup. Pap smear revealed atypical squamous squamous TAHBSO was performed. The mass was noted to be
cells of undetermined significance (ASCUS). intraepithelial grossly necrotic and hemorrhagic. Sections show
Repeat Pap smear revealed atypical squamous lesion (LSIL) sheets of highly atypical cells with necrosis and
cells. Raising suspicion, colposcopy was high mitotic index. IHC: Smooth muscle actin (+).
performed and punch biopsy was done on the What is the diagnosis?
suspicious area. Biopsy showed atypical
squamous cells occupying the lower 1/3 of the
OVARIES
epithelial thickness. What is the diagnosis?
OVARIAN TUMORS
Common presentation: Ovarian mass, with abdominal fullness and
pain (if large); pain is more pronounced if torsion occurs
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 19 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
Surface epithelial (Mullerian) tumors 27/F with bloody nipple discharge. Biopsy Intraductal
Note: Remember that there are benign, borderline, and malignant showed papillary fronds within a duct. papilloma
classifications of these tumors, depending on the cytologic atypia, Immunohistochemistry: p63, CK 5,6 (+). What is
architectural complexity, and stromal invasion. The details of which the diagnosis?
are beyond the scope of being a general practitioner. 35/F. Biopsy showed central nidus of entrapped Complex
Histologically characterized by tubal-like Serous tumors glands within a hyalinized stroma, with sclerosing
epithelial lining fibrocystic changes and epithelial hyperplasia lesion/Radial
Histologically characterized by either intestinal or Mucinous tumor on adjacent areas. What is the diagnosis? scar
endocervical epithelial lining (mucin- PROLIFERATIVE BREAST DISEASES WITH ATYPIA AND CARCINOMA
containing) IN SITU
Histologically characterized by glandular Endometrioid 46/F. Biopsy showed nests of monomorphic cells, Atypical ductal
structures resembling endometrial glands tumors and ducts filled with the same cells, showing hyperplasia
Germ cell tumors cribriform pattern. The changes do not involve the (ADH)
Note: Other germ cell tumors are discussed in Male genital tract whole duct. What is the diagnosis?
Cystic, lined by skin-like structures (dermoid Mature cystic Based on the case above, if the change involves the Ductal
cyst); usually occur in reproductive age women; teratoma whole duct, what would be the diagnosis? carcinoma in
histologically, derivatives from more than one situ (DCIS)
germ layer can be seen; generally benign Based on the second case, if there are dilated ducts Comedo DCIS
Solid masses that usually occur in younger Immature lined by cells with high-grade nuclear atypia and
women and children; histologically composed of teratoma central necrosis, what would be the specific
neuroepithelium; generally malignant diagnosis?
Sex-cord stromal tumors Based on the first case, if biopsy revealed Atypical lobular
Note: Aside from the presence of ovarian mass, depending on the monomorphic cells proliferating within the lobule hyperplasia
capability of the tumor to produce hormones, additional clinical of the acini, but the change is evident in only 10% (ALH)
manifestations referable to sex hormone excess may help you clinch of the acini in a lobule, what would be the
the diagnosis diagnosis?
May clinically present as precocious puberty (in Granulosa cell Based on the fourth case, if the change involves all Lobular
premenarcheal) or abnormal uterine bleeding (in tumor of the acini in a lobule, what is the diagnosis? carcinoma in
menstruating and postmenopausal), due to its situ (LCIS)
estrogen secretion; histologically characterized by CARCINOMAS
sheets of cuboidal granulosa cells; some of the 45/F, with a rash on the nipple area. PE: (+) firm Paget disease of
cells recapitulate ovarian follicle as Call-Exner mass, on the upper outer quadrant of the breast. the nipple
bodies Biopsy of the rash showed large cells with mild
May clinically present with virilization, due to its Sertoli-Leydig nuclear atypia in the epidermis.
androgen secretion; histologically, the tumor cell tumor Immunohistochemistry: Epithelial membrane
recapitulates Tubules formed by Sertoli cells, or antigen (EMA) (+). What is the diagnosis?
Leydig cells interspersed in stroma Based on the case above, mastectomy was Invasive
Usually associated with hydrothorax and ascites Thecoma- performed. Grossly, there is a cream-tan, firm mass (ductal)
(Meig syndrome); histologically composed of fibroma with irregular borders. Sections show cells with carcinoma (No
sheets of fibrous cells or (lipid-laden) plump moderate pleomorphism, forming tubule-like special type)
thecal cells, or in combination structures (>80%) with occasional solid nests Well-
and sheets. Mitosis is 1-3/10 HPF. What is the differentiated
DISEASES OF PREGNANCY diagnosis and what is the histologic grade? (Elston score: 4
31 G1P0 12 weeks AOG, with passage of grape- Complete = 1+2+1)
like vesicles per vagina and bleeding. Corpus hydatidiform Based on the second case, if biopsy showed cords of Invasive lobular
size is 16 weeks AOG. UTZ: snowstorm mole medium-sized cells showing an Indian filing carcinoma
appearance. Suction curettage was done. Biopsy pattern, and cords of cells encircling a duct
revealed DIFFUSE villus edema and trophoblastic (targetoid pattern), and IHC for E-cadherin turned
proliferation with several atypical trophoblasts. out to be negative, what is the diagnosis?
What is the diagnosis? Based on the second case, if biopsy showed nests of Pure mucinous
31 G1P0 12 weeks AOG, with passage of meaty Incomplete atypical cells, floating in pools of mucin, carcinoma
material per vagina and bleeding. Diagnosis was (Partial) comprising 95% of the tumor, what is the
incomplete abortion, and completion curettage hydatidiform diagnosis?
was performed. Biopsy revealed FOCAL villus mole 65/F, with breast pain, and a firm mass at the Inflammatory
edema and trophoblastic proliferation with few upper outer quadrant. PE: erythematous, (+) carcinoma
atypical trophoblasts. What is the diagnosis? orange peel appearance of skin, tender breast.
31 G1P0 (0010) with a history of complete Gestational Biopsy showed solid sheets and nests of cells with
hydatidiform mole with a persistently elevated choriocarcinoma high-grade nuclear atypia, and numerous mitotic
HCG after post-curettage surveillance, presented figures. What is the diagnosis?
with hemoptysis. CXR: cannon-ball lesions. 60/F, with a firm mass on the upper outer Medullary
Biopsy of the lesions showed sheets of atypical quadrant. Biopsy showed syncytium-like solid carcinoma
cytotrophoblasts and syncytiotrophoblasts sheets of large cells with pleomorphic nuclei and
WITHOUT villus formation. What is the prominent nucleoli, with high mitotic index, dense
diagnosis? lymphoplasmacytic infiltrate, and pushing
borders. Immunohistochemistry: ER, and HER-2 (-).
what is the diagnosis?
22. BREAST
In practice, the common complaint of patients with breast disease, which
MOLECULAR SUBTYPES OF BREAST CANCER
warrants histologic evaluation, is the presence of a mass. Other lesions
Luminal HER-2
may have clinical findings that are suggestive of a particular lesion. Feature Basal
A B enriched
QUESTION ANSWER
Phenotype ER(+), HER2(-) HER2(+) ER(-),
NON-PROLIFERATIVE BREAST CHANGES
ER, PR (+/-) HER2(-)
32/F. Biopsy showed fibrosis, increase in the Fibrocystic
Frequency 40-55% ~10% ~20% ~15%
number of acini per lobule, and cystic dilatation change
of the acini; some which show apocrine Proliferation Low High N/A
metaplasia. What is the diagnosis? index
(Ki-67)
PROLIFERATIVE BREAST DISEASES WITHOUT ATYPIA
Treatment Hormonal therapies HER-2 In study
34/F. Biopsy showed fibrocystic changes and Epithelial
(Tamoxifen) targeted
areas showing ducts lined by more than 2 layers hyperplasia
therapy
of cells with slit-like lumina at the periphery,
(Trastuzumab)
and an intact myoepithelial layer. What is the
diagnosis?
STROMAL TUMORS
37/F. Biopsy showed cords and sheets of cells Sclerosing
within a sclerotic stroma, with dilated ducts at adenosis 25/F, with 2.0 cm mass. Biopsy showed Fibroadenoma
the periphery. Immunohistochemistry: p63, CK5,6 proliferation of intralobular stroma that
(+). What is the diagnosis? surrounds and compresses the ducts. What is the
diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 20 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
50/F, with 6.0 cm mass. Biopsy showed intense Phyllodes tumor 67/M, with a history of multinodular goiter, Anaplastic
proliferation of intralobular stroma with leaf-like presented with sudden, massive enlargement of (undifferentiated)
processes lined by ductal epithelium; there is the thyroid gland with profound weight loss. carcinoma
stromal hypercellularity, cellular atypia, and Total thyroidectomy was done. Biopsy showed
increaed mitotic index. What is the diagnosis? sheets of highly anaplastic cells.
Immunohistochemistry: CK (+), thyroglobulin (-
DISEASES OF THE MALE BREAST ). What is the diagnosis?
24/M, with bilateral areolar swelling. Excision Gynecomastia 25/M, with strong history of MEN2A in the Medullary
was performed, and biopsy showed increase in family, underwent total thyroidectomy. Cut carcinoma
connective tissue and epithelial hyperplasia of sections show bilateral thyroid masses. Biopsy
the ducts, without lobule formation. What is the showed sheets of polygonal cells with amyloid
diagnosis? deposition. What is the diagnosis?
ENDOCRINE PANCREAS
23. ENDOCRINE SYSTEM DIABETES MELLITUS
PITUITARY GLAND
15/M, with polyuria, polydipsia, and polyphagia, Type 1 DM
QUESTION ANSWER
forgot his insulin for a week, presented with weakness
34/F, with galactorrhea and amenorrhea. Pituitary adenoma and increased sleeping time at the ER, and eventually
Imaging showed a pituitary mass, (Prolactin cell expired. Autopsy of the pancreas showed lymphocytic
measuring 2.0 cm. Transsphenoidal adenoma) infiltration of the islets (insulitis). What is the
resection was done. Biopsy showed sheets diagnosis?
of benign-looking pituicytes with sparse
44/F, with polyuria, polydipsia, and polyphagia, Type 2 DM
reticulin network. What is the diagnosis?
presented with a gangrenous foot and high-grade
Based on the case above, if metastases Pituitary carcinoma fever. Patient eventually died of septic shock. Autopsy of
were found in other sites, what would be the pancreas showed amyloid deposition. What is the
the diagnosis? diagnosis?
15/M, with a cranial mass. Biopsy showed Craniopharyngioma Based on the case above, if the patient lived longer, but Diabetic
a lesion that looks like an ameloblastoma. (Adamantinomatous) presented with rising BUN and creatinine, and then nephropathy
What is the most likely diagnosis? eventually died of uremia, and autopsy of the kidney
showed hyaline arteriolosclerosis and nodular
THYROID GLAND glomerulosclerosis (Kimmelsteil-Wilson lesion), what
HYPOTHYROIDISM is the diagnosis?
6/M, with mental retardation, short stature, Cretinism Based on the second case, if the patient lived, but Diabetic
coarse facial features, protruding tongue, presented with progressive deterioration of visual retinopathy
umbilical hernia, and history of maternal acuity, and retinal workup showed neovascularization
hypothyroidism. What is the diagnosis? and cotton-wool exudates, what is the diagnosis?
34/F, with profound weight gain, deepening of Myxedema
voice, and nonpitting edema. Skin biopsy PANCREATIC NEUROENDOCRINE TUMORS
showed accumulation of matrix substances, Parameter Insulinoma Gastrinoma
such as glycosaminoglycans and hyaluronic Clinical Hyperinsulinism Hypergastrinemia
acid. What is the diagnosis? syndrome Whipple Triad Zollinger-Ellison
THYROIDITIDES 1. Hypoglycemia (<50 syndrome
35/F, with thyroid enlargement. Total Hashimoto mg/dL) 1. Pancreatic islet
thyroidectomy was done. Biopsy showed thyroiditis 2. Neuroglycopenic cell tumor
lymphoid follicles scattered throughout the symptoms 2. Hypersecretion of
parenchyma with Hurthle cell change. What is 3. Relief upon parenteral gastric acid
the most likely diagnosis? glucose administration 3. Severe peptic
35/F, with a history of viral URTI, complained of De Quervain ulceration (may
anterior neck pain and sudden thyroid thyroiditis occur in jejunum)
enlargement. Total thyroidectomy was done. Location Pancreas Gastrinoma triangle
Biopsy showed granulomatous inflammation. Biologic Usually benign Usually malignant
What is the diagnosis? behavior
GRAVES DISEASE Gross and May recapitulate normal pancreatic islets; even
36/F, with proptosis, pretibial myxedema, and Graves Disease histology malignant tumors can be encapsulated; amyloid
modest thyroid enlargement. TSH is low and deposition (in insulinomas)
FT4 is high. Total thyroidectomy was done.
Biopsy showed diffuse hyperplasia with ADRENAL GLANDS
pseudopapillary structures and moth-eaten ADRENAL CORTEX
colloid. What is the diagnosis?
34/M, obese with moon facies, purple Cushing syndrome
GOITERS abdominal striae, and dorsocervical secondary to cortisol-
45/F, with an anterior neck mass. Total Colloid goiter fullness (buffalo hump). 24-hour urine secreting adrenal
thyroidectomy was done. Cut sections show a cortisol is increased. Plasma ACTH is adenoma
single nodule. Biopsy showed follicles distended decreased. Imaging showed a right adrenal
by abundant amount of colloid. What is the mass. Biopsy showed cells resembling
diagnosis? normal zona fasciculata. What is the
Based on the case above, if cut sections show Multinodular diagnosis?
multiple nodules, and biopsy showed multiple goiter Based on the case above, if plasma ACTH is Cushing disease
nodules distended by colloid, as well as nodules increased, and imaging showed bilateral (Cushing syndrome
forming pseudopapillary structures, what is the adrenal hyperplasia, and cranial MRI secondary to ACTH-
diagnosis? showed a pituitary mass, what is the secreting pituitary
Based on the case above, if the patient presented Plummer diagnosis? adenoma)
with hyperthyroidism, and the histologic syndrome 45/F, presented with weakness and Conn syndrome
diagnosis is still multinodular goiter, what is the treatment-resistant hypertension. Plasma (Primary
clinical diagnosis? aldosterone is elevated. Plasma renin is hyperaldosteronism
TUMORS decreased. Imaging showed a left adrenal secondary to
38/F, with an anterior neck mass. Total Papillary mass. Biopsy showed cells resembling aldosterone-secreting
thyroidectomy was done. Biopsy showed carcinoma normal zona fasciculata with adrenal adenoma)
papillary fronds lined with atypical thyrocytes spironolactone bodies. What is the
with Orphan Annie nuclei and Psammoma diagnosis?
bodies. What is the diagnosis? 6/F, with ambiguous genitalia, presented Congenital adrenal
Based on the case above, if grossly there is only Follicular with fever, cough and colds, with hyperplasia, salt-
one nodule observed, and biopsy showed sheets adenoma hypotension and hypoglycemia. Cortisol wasting type
of benign-looking thyrocytes without capsular and aldosterone levels are decreased.
or vascular invasion, what is the diagnosis? Plasma renin is increased. Serum sodium is
Based on the second case, if capsular and Follicular low, and potassium is high. Imaging showed
vascular invasion were observed, what would carcinoma bilateral adrenal hyperplasia. What is the
be diagnostic? diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 21 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
34/F, with skin hyperpigmentation, Addison disease 45/F, known case of Non-Hodgkin lymphoma, Erytherma
hypotension, hypoglycemia, hyponatremia secondary to developed multiple target lesions. Biopsy showed multiforme
and hyperkalemia. Imaging showed autoimmune superficial perivascular, lymphocytic infiltrate,
irregularly shrunken adrenal glands. adrenalitis dermal edema, and lymphocytes at DEJ associated
Biopsy showed lymphocytic infiltrates. What with necrotic keratinocytes. What is the diagnosis?
is the diagnosis?
CHRONIC INFLAMMATORY DERMATOSIS
ADRENAL MEDULLA 36/F, with salmon pink scaly plaques on the legs with Psoriasis
30/M, with paroxysms of severe hypertension Pheochromocytoma punctate bleeding on removal of the plaque (Auspitz
and elevated plasma metanephrines. Imaging sign). Biopsy of the plaque showed acanthosis with
showed an adrenal mass, and after appropriate elongation of rete ridges, resembling test tubes in a
preoperative evaluation, adrenalectomy was rack, with neutrophils in the parakeratotic stratum
performed with resolution of the hypertension. corneum (Munro microabscesses). What is the
Biopsy showed nests of cells surrounded by diagnosis?
sustentacular cells (zellballen); the nuclei of
the cells exhibit a salt and pepper chromatin BLISTERING DISORDERS
pattern. What is the diagnosis? 48/M, with multiple skin bullae. PE: (+) Nikolsky Pemphigus
sign. Serology: IgG against desmoglein (+). Biopsy vulgaris
MULTIPLE ENDOCRINE NEOPLASIA SYNDROMES showed acanthloysis, and suprabasilar blister with
MEN2A lace-like pattern of immunofluorescence. What is the
MEN1
Parameter Sipple MEN2B diagnosis?
Wermer syndrome
syndrome Based on the case above, if PE: (-) Nikolsky sign. Bullous
Mutation MEN1 RET (2A and 2B have Serology: IgG against BPAG (+); and biopsy showed pemphigoid
distinct mutations) basal layer vacuolization, and subepidermal blister
Syndrome • Pituitary: Prolactinomas Common: with linear pattern of immunofluorescence, what is
(MC) Pheochromocytoma, the diagnosis?
• Parathyroid: Primary MTC** (MEN2B-associated 38/F, known case of celiac disease, with multiple skin Dermatitis
hyperparathyroidism are more aggressive than bullae. Biopsy showed PMNs at tips of dermal herpetiformis
(MC; either adenoma or MEN2A-associated) papillae, and subepidermal blister with granular
hyperplasia) • MEN2A: Parathyroid pattern of immunofluorescnece. What is the
• Pancreas: PP (MC), hyperplasia diagnosis?
Insulinoma or • MEN2B: Neuromas,
gastrinoma* (MC types ganglioneuromas, INFECTIOUS DERMATOSES
that produce Marfanoid habitus 8/F, with multiple honey-colored crusts. Biopsy Impetigo
hypersecretory states) showed accumulation of PMNs beneath the stratum contagiosa
Genetic Importance not well- Important due to MTC corneum. What is the diagnosis?
screening established (mortality prevented by 32/M, with a grayish-tan papule on the neck. Biopsy Verruca
early thyroidectomy) showed papillomatous epithelial hyperplasia, with vulgaris
koilocytic change. What is the diagnosis?
24. SKIN
Note: Please familiarize yourselves with the dermatologic and 25. BONES, JOINTS, AND SOFT TISSUES
dermatopathologic lexicon before proceeding. Note: The chapter only includes bones and joints. For soft tissues, please
QUESTION ANSWER refer to the main handout.
DISORDERS OF PIGMENTATION AND MELANOCYTES BONES
34/F, with a pigmented lesion on the nasolabial fold. Melanocytic QUESTION ANSWER
Biopsy showed nests of uniform, cytologically benign nevus ACQUIRED DISEASES
cells, with extracellular pigment, that are entirely in (Pigmented 60/F, with shortening of stature and lower Osteoporosis,
the dermis, with neurotization underneath. What is intradermal back pain. Lumbar X-ray showed compression decreased bone
the specific diagnosis? nevus) fracture of the L1 vertebra. Lumbar spine mass
45/F, with a variegated pigmented lesion on the arm Melanoma BMD T-score <-2.5 SD. What is the diagnosis,
with irregular borders, measuring 5.0 cm in widest and what is the fundamental abnormality?
dimension. Wide excision was done, and biopsy showed 56/M, with chronic lower back pain and pain Paget disease of
nests of highly anaplastic cells with abundant on the left lower extremity. Lumbar MRI bone (Osteitis
extracellular pigment deposition. What is the showed a lesion on L2 vertebra with deformans)
diagnosis? compression of the left nerve root. Biopsy
showed mosaic pattern of lamellar bone with
BENIGN AND PREMALIGNANT EPITHELIAL LESIONS cement lines “jigsaw puzzle”. What is the
70/M, with a pigmented plaque on the face. Lens Seborrheic diagnosis?
examination showed multiple ostia on the lesion's keratosis OSTEOMYELITIS
surface. Biopsy was done, showing multiple horn cysts. 32/M, with a history of neglected cellulitis on Pyogenic
What is the diagnosis? the ankle area, now presented with loss of osteomyelitis
50/M, with an exophytic, gray-tan mass on the face. Actinic range of motion of the ankle joint, associated
Biopsy showed basal layer atypia with intercellular keratosis with high-grade fever. Debridement was
bridges, blue-gray elastic fibers (solar elastosis), and performed, and samples were taken for biopsy,
dermal chronic inflammation. What is the diagnosis? which showed bone necrosis with brisk
neutrophilic infiltrate and reactive bone
MALIGNANT EPITHELIAL TUMORS formation. What is the diagnosis?
46/M, with an ulcerated lesion on the cheek. Biopsy Squamous 34/F, known case of pulmonary TB and did Pott disease
showed nests of atypical squamous cells invading a cell not complete her 6 months treatment,
desmoplastic stroma, with occasional keratin pearl carcinoma presented with severe back pain on the
formation. What is the diagnosis? lumbar area, with difficulty in maintaining an
34/F, with a pearly, telangiectatic papule on the face. Basal cell erect posture. MRI showed destruction of L2
Biopsy showed nests of basaloid cells with peripheral carcinoma and L3 with abscess formation. Biopsy showed
palisading and stromal retraction, invading the chronic granulomatous inflammation with
dermis. What is the diagnosis? caseation necrosis and Langhans type giant
cells. What is the diagnosis?
ACUTE INFLAMMATORY DERMATOSES TUMORS
26/M, known case of bronchial asthma, and allergic Urticaria 25/M, asymptomatic, with an incidental Osteoid osteoma
rhinitis, presented with multiple wheals. Biopsy finding of a mass on the knee, measuring 1.5
showed superficial dermal edema, and sparse cm. Biopsy showed interlacing bony
superficial perivenular mononuclear infiltrate. What trabeculae with osteoblastic rimming. What is
is the diagnosis? the diagnosis?
29/M, with a history of penicillin intake, developed Acute Based on the case above, if the patient Osteoblastoma
erythematous patches with vesicles. Biopsy showed eczematous presented with pain, and the lesion measures
thickening of the epidermis and the horny cell layer, dermatitis 3.0 cm, with the same histologic findings, what
with epidermal intercellular edema. What is the (drug- is the diagnosis?
diagnosis? related)
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 22 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
Based on the case above, if osteoblastic Fibrous dysplasia 55/M, with polyphagia, polyuria, and Diabetic neuropathy,
rimming is absent, what would be the most polydipsia, with FBS = 130 mg/dL, presented Axonal neuropathy
likely diagnosis? with numbness on both fingers and toes,
25/M, gymnast, presented with limping, on the Osteosarcoma resembling a "glove and stocking pattern" of
right, with pain referred on the knee. X-ray sensory deficit. What is the diagnosis, and the
showed a lesion on the distal femur, (+) pattern of neuropathy observed in this case?
Codman triangle and sunburst appearance.
Biopsy showed lace-like pattern of bone DISORDERS OF NEUROMUSCULAR JUNCTION
deposition by anaplastic tumor cells. What is 32/F, with mediastinal mass; biopsy revealed Myasthenia gravis;
the diagnosis? thymoma, presented with ptosis and Autoantibodies to
34/F, with a mass on the left index finger. Chondroma dysarthria late in the afternoon, with ACH receptor
Biopsy showed sheets of cytologically benign improvement after rest. Edrophonium test
chondrocytes. What is the diagnosis? was positive. What is the diagnosis, and the
27/M, with an incidental finding of a knee Osteochondroma autoantibodies present?
mass. Biopsy showed a bone with an 45/M, heavy smoker, with small cell lung Lambert-Eaton
underlying marrow cavity, covered a carcinoma, presented with ptosis and myasthenic
cartilage cap. What is the diagnosis? difficulty in moving his hips and thighs. syndrome (LEMS);
67/M, with a right scapular mass. Biopsy Chondrosarcoma Associated symptoms include dry mouth and Autoantibodies to
showed sheets of anaplastic cartilage-forming impotence. PE: 0 reflexes on patellar and presynaptic Ca
cells with high mitotic rate. What is the ankle. What is the diagnosis, and the channel
diagnosis? autoantibodies present?
12/M, with a mass on the humerus, with Ewing sarcoma
associated intermittent low-grade fever. ACQUIRED DISORDERS OF SKELETAL MUSCLE
Biopsy showed sheets of small, round, blue 13/F, presented with difficulty in shoulder Dermatomyositis
cells? Immunohistochemistry: vimentin, CD99 abduction, followed by weakness of the
(+). What is the diagnosis? forearm and hand muscles. PE: periorbital lilac
35/F, with a left knee mass. Biopsy showed Giant cell tumor of discoloration (Heliotrope rash) and dusky red
mononuclear cells with abundance of bone patches over knuckles (Gottron papules).
multinucleated giant cells. What is the (Osteoclastoma) Muscle biopsy: Perifascicular atrophy with
diagnosis? perimysial and perivascular mononuclear
infiltrates. What is the diagnosis?
JOINTS 48/M, presented with difficulty in shoulder Polymyositis
DEGENERATIVE BONE DISEASE abduction, followed by weakness of the
62/M, with pain on the right knee that Osteoarthritis forearm and hand muscles; otherwise
worsens with activity. PE: (+) nodules on DIP unremarkable. Muscle biopsy: Random, patchy
(Heberden) and PIP (Bouchard nodes). areas of atrophy with endomysial
Osseous ankylosis is not seen on imaging. mononuclear infiltrates. What is the diagnosis?
What is the most likely diagnosis?
34/F, with morning stiffness and pain on both Rheumatoid MUSCULAR DYSTROPHIES
hands that improve with activity. Patient is arthritis (RA) 5/M, complained of being called "lampa" by his Duchenne Muscular
positive for HLA-DRB1; Serology: RF and anti- playmates. History revealed frequent episodes Dystrophy (DMD)
CCP (+). Imaging showed pannus with osseous of fall. Patient uses his hands to get up (Gower (early)
ankylosis. What is the most likely diagnosis? sign). Muscle biopsy: segmental myofiber Note: Histologic findings
50/M with chronic back pain and stiffness Ankylosing degeneration and regeneration with for late DMD is different
that improve with activity. X-ray of the spine spondylitis preserved fascicular architecture. IHC:
showed a bamboo-stick appearance. Patient is Dystrophin (-)
positive for HLA-B27. What is the diagnosis? Difference in dystrophin immunohistochemistry DMD: Dystrophin(-)
between DMD and BMD BMD: Dystrophin(+)
CRYSTAL-INDUCED ARTHROPATHIES but reduced
Parameter Gout Pseudogout
Types and • Most common: • Sporadic (idiopathic), PERIPHERAL NERVE SHEATH TUMORS
characteristics primary, most hereditary and 23/M, with an arm mass. Biopsy showed Schwannoma/
common: unknown secondary alternating hypercellular (Antoni A) and Neurilemmoma
gene defects • AD: germline hypocellular (Antoni B) areas, composed of benign-
• Hyperuricemia (>6.8 mutations in looking spindle cells with palisading nuclei, and
mg/dL): from pyrophosphate nucleus-less areas (Verocay bodies). IHC: S-100 (+).
increased production transport channel What is the diagnosis?
or impaired excretion 23/M, with an arm mass. Biopsy showed benign- Neurofibroma
Clinical • Usually • Monoarticular or looking spindle cells with collagen bundles
monoarticular, acute polyarticular, from resembling "shredded carrot" appearance. IHC:
(most common: 1st acute to chronic (most CD34 (+). What is the diagnosis?
MTPJ) common: knee)
Crystals Monosodium urate, Calcium pyrophosphate, NEUROFIBROMATOSES
needle-shaped, rhomboid-shaped, Parameter NF Type 1 NF Type 2
negatively birefringent positively birefringent Inheritance AD; NF1 (Ch17) AD; NF2 (Ch22)
Inflammation Intense (neutrophilic) If present, usually milder and gene
than gout
Treatment NSAIDs and colchicine No known treatment Incidence More common Less common
(acute), uric acid Components • Neurofibromas • Bilateral eight nerve
lowering agents • MPNSTs schwannomas
• Optic nerve gliomas • Multiple
• Other glial tumors and meningiomas
26. PERIPHERAL NERVOUS SYSTEM AND hamartomatous lesions • Ependymomas
SKELETAL MUSCLE • Pheochromocytomas (commonly
• Pigmented iris nodules intraspinal)
QUESTION ANSWER
(Lisch nodules)
DISORDERS OF PERIPHERAL NERVES
• Cutaneous hyperpigmented
43/M, with history of fever and non- Guillain-Barre
macules (Café au lait spots)
productive cough a week prior, presented syndrome,
with bilateral weakness involving first the Symmetric ascending
lower extremities until the lower trunk. CSF demyelinating
analysis: mild lymphocytic pleocytosis and polyradiculoneuropa
moderately elevated protein. Biopsy of thy
muscle revealed mononuclear, perivenular
and perineurial infiltrate, with segmental
demyelination of nerve. What is the diagnosis,
and the pattern of neuropathy observed in this
case?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 23 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
28. CENTRAL NERVOUS SYSTEM ACQUIRED METABOLIC AND TOXIC DISTURBANCES
Note: Congenital anomalies are omitted because of low-yield; for 32/F, known case of pernicious anemia, presented Subacute
completion, you may refer to the parent handout. Also, some common with ataxia and numbness of the lower extremities combined
CNS anomalies are discussed in anatomy (under embryology). CNS that led to spastic paralysis and paraplegia, and degeneration
infections are covered in Microbiology, and lumbar tap findings for eventual demise from pneumonia. What is the most
meningitides are covered in IM and Pediatrics. likely diagnosis?
QUESTION ANSWER
WERNICE-KORSAKOFF SYNDROME
EDEMSHOWED
Wernicke
showed Showedlioblastoma Parameter Korsakoff syndrome
encephalopathy
Based on the case above, the patient eventually Tonsillar
Syndrome Psychotic symptoms or Short-term memory
arrested and expired. Autopsy showed herniation
ophthalmoplegia disturbances and
cerebellar tonsils passing through the
Memory device: ataxia, confabulation
foramen magnum, compressing the
confusion, Memory device:
brainstem. What is the type of herniation seen
ophthalmoplegia (ACO) confabulation,
in this case?
hallucinations, amnesia
2m/M with presented with enlargement of the Non-
(CHA)
head and sunsetting of eyes. Imaging showed communicating
Duration Acute Chronic
aqueductal stenosis and dilation of the lateral hydrocephalus
ventricles. What is the specific diagnosis? Reversibility Yes No
with
thiamine
TRAUMATIC VASCULAR DISEASES
Morphology Hemorrhage and necrosis Cystic space with
Parameter Epidural hematoma Subdural hematoma
of the mamillary bodies hemosiderin-laden
Age/Onset Middle age Extremes of age
and the walls of the third macrophages in
Clinical Rapidly evolving Slowly evolving
and fourth ventricles dorsomedial nucleus of
picture neurologic symptoms neurologic symptoms;
the thalamus
with lucid intervals often delayed onset
Blood source Arterial: most common: Venous: bridging veins
TUMORS
middle meningeal artery
65/M, with a cranial mass. Biopsy showed Glioblastoma
(from pterion fracture)
pseudopalisading to tumor cells around areas (WHO IV/IV)
Plain CT-scan Lentiform density Crescent-shaped density
of necrosis with accompanying microvascular
appearance
proliferation proliferation. What is the
diagnosis?
CEREBROVASCULAR DISEASES
Based on the case above (65/M), if thorough Anaplastic
45/M, known hypertensive, presented with left Focal cerebral examination of the sections did not show any astrocytoma (WHO
upper extremity weakness and loss of sensation. ischemia necrosis or microvascular proliferation, what III/IV)
Motor strength grading is 2/5 at left upper would be the more appropriate diagnosis?
extremity, and sensation is about 40%. Plain
Based on the case above (65/M), if biopsy Oligodendroglioma
cranial CT-scan showed a hypodense area on the
showed sheets of round cells with cytoplasmic (WHO II/IV)
region of the right MCA. What is the diagnosis?
halos, resembling a fried-egg appearance,
Based on the case above, if the patient had an Hypertensive what is the diagnosis?
antecedent history of a high BP (200/100 mmHg), intracerebral
Based on the case above, if the mass is located on Intraspinal
and presented with decrease in sensorium, and plain hemorrhage
the spinal cord, and biopsy showed Ependymoma
cranial CT-scan showed a hyperdense lesion with
perivascular pseudorosettes, what is the (WHO II/IV)
perilesional edema on the region of the right MCA,
diagnosis? Note: location of
what is the diagnosis? ependymomas is
41/F, after a heated argument with a store clerk, Subarachnoid different depending on
presented with an intense headache and syncope. hemorrhage the age
Patient went into comatose for several days and 12/M, with cerebellar mass. Biopsy showed Pilocytic
died. Antemortem CT showed hyperdense material bipolar cells with thin, hair-like processes and astrocytoma (WHO
filling the sulci. What is the diagnosis? Rosenthal fibers. What is the diagnosis? I/IV)
15/F, collapsed after an exam week. CT-scan showed Arteriovenous Based on the case above (12/M), if biopsy Medulloblastoma
an irregular hyperdense lesion. CT angiography malformation showed sheets of small, round, blue cells with (WHO IV/IV)
showed a bag of worms appearance. Removal of the Homer-Wright rosettes, what is the diagnosis?
lesion was done. Biopsy showed large vessels with 35/F, presented with progressive headache, Meningothelial
intervening brain tissue. What is the diagnosis? and an intracranial extra-axial mass. Biopsy meningioma (WHO
showed syncytial nests of bland-looking cells I/IV)
DEMYELINATING DISORDERS and several Psammoma bodies. What is the
32/F, with history of diplopia for 2 weeks, 2 years Multiple diagnosis?
prior, now presented with bilateral facial sclerosis
weakness for 3 weeks. Lumbar tap was done 28. EYE
showing moderate pleocytosis, mildly elevated
QUESTION ANSWER
protein, and increased oligoclonal IgG. What is the
ORBIT
most likely diagnosis?
Forward displacement of the eye; has two Proptosis
forms: axial and positional
NEURODEGENERATIVE DISEASES
Most common primary tumor of the orbit Vascular tumors
72/M with progressive dementia and Alzheimer
(Infancy and early
dysautonomia, eventually succumbed to disease (AD)
childhood: capillary
pneumonia. Brain autopsy showed cortical atrophy
hemangioma,
with neuritic plaques, and neurofibrillary tangles.
lymphangioma;
What is the diagnosis?
adults: cavernous
43/F, with tremor, rigidity, and bradykinesia, Parkinson hemangioma)
which became progressive, precluding her to disease (PD)
ambulate properly. She eventually expired due to
EYELID
pneumonia. Brain autopsy showed pallor of
Most common malignancy of the eyelid Basal cell carcinoma
substantia nigra and multiple, intracytoplasmic,
eosinophilic, round to elongated inclusions that
often have a dense core surrounded by a pale halo CONJUNCTIVA
(Lewy bodies). What is the diagnosis? Etiologic agent of conjunctivitis that leads to Chlamydia
45/M, with increased incidence of fall and tendency Amytropic significant conjunctival scarring trachomatis
to drop things, without any sensory deficit. He fell lateral Most common site of conjunctival neoplasms Limbus
from the stairs and died to traumatic brain injury. sclerosis (ALS) Histology of common conjunctival Squamous cell
Autopsy showed thinned-out anterior horn malignancies carcinomas,
neurons, cranial nerve motor nuclei, and Melanomas
corticospinal tract degeneration. What is the
diagnosis?
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 24 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT by KEVIN ELOMINA, MD
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
ANTERIOR SEGMENT Loss of vision secondary to demyelination of Optic neuritis
Inflammation within the vitreous humor Endophthalmitis the optic nerve; most important cause is
Inflammation involving the retina, uvea, Panophthalmitis multiple sclerosis
sclera, and orbit Most common primary optic nerve tumors Pilocytic astrocytomas
Opacification of the lens Cataract and meningiomas
Submucosal fibrovascular connective tissue Pinguecula ---END OF PATHOLOGY---
that does not invade the cornea Edited by: Kevin A. Elomina, MD
Submucosal fibrovascular connective tissue Pterygium
that invades the cornea; associated with These verses are included in my guiding verses in life, and during the
visual problems (astigmatism) boards. These speak of the power of persistence, and the providence of
Diseases characterized by distinctive changes Glaucoma God to His children.
in visual field and optic nerve cup; most are
associated with increased intraocular Luke 11:5-13 New King James Version (NKJV)
pressure
A Friend Comes at Midnight
TYPES OF GLAUCOMA And He said to them, “Which of you shall have a friend, and go to him at
midnight and say to him, ‘Friend, lend me three loaves; for a friend of
Normal
Parameter Open-angle Angle-closure mine has come to me on his journey, and I have nothing to set before
pressure
him’; and he will answer from within and say, ‘Do not trouble me; the
Trabecular Yes No Yes
door is now shut, and my children are with me in bed; I cannot rise and
meshwork
give to you’? I say to you, though he will not rise and give to him because
access
he is his friend, yet because of his persistence he will rise and give him as
Pathogenesis Increased Peripheral Characteristic
many as he needs.
resistance to zone of the iris optic nerve
aqueous outflow adheres to the and visual field
Keep Asking, Seeking, Knocking
in open angle of trabecular changes
“So I say to you, ask, and it will be given to you; seek, and you will find;
the anterior meshwork without
knock, and it will be opened to you. For everyone who asks receives, and
segment (hyperopics, increased IOP
he who seeks finds, and to him who knocks it will be opened. If a son asks
shallow
for bread[a] from any father among you, will he give him a stone? Or if he
anterior
asks for a fish, will he give him a serpent instead of a fish? Or if he asks for
chambers)
an egg, will he offer him a scorpion? If you then, being evil, know how to
Increased IOP Yes Yes No give good gifts to your children, how much more will your heavenly
Acute/Chronic Chronic Acute Chronic Father give the Holy Spirit to those who ask Him!"
UVEA
Inflammation of the tissues that comprise the Uveitis
uvea (iris, ciliary body and choroid)
Most common intraocular malignancy Metastases to uvea
Most common primary intraocular Melanoma
malignancy in adults
RETINA AND VITREOUS
TYPES OF RETINAL DETACHMENT
Parameter Rhegmatogenous Non-rhegmatogenous
Full-thickness Yes No
retinal defect
Pathogenesis Unclean vitreous Any condition that
detachment tears the damages the RPE and
retina; liquefied permits fluid to leak
vitreous accumulates from the choroidal
between RPE and circulation under the
neurosensory retina retina
Photoreceptor Present in chronic; absent in acute
atrophy
Clinical Ophthalmologic emergency
signficance
RETINAL OCCLUSION SYNDROMES
Central retinal artery Central retinal vein
Parameter
occlusion occlusion
Ischemia • Occurs in ischemia • May occur with or
without ischemia
Histologic • Fragments of • Retinal hemorrhages,
findings atherosclerotic plaque dilated tortuous
lodged in retinal circulation retinal veins, cotton-
(Hollenhorst plaques) wool spots, macular
• Cherry-red spot in macula edema, and optic disc
(fovea and foveola) with edema
retinal pallor
Clinical Ophthalmologic emergency -
signficance
Most common type of retinal lymphoma DLBCL
4/M, came for a routine check-up. On pupillary Retinoblastoma
examination, (+) leukocoria, prompting referral to
an ophthalmologist. The patient underwent
operation and an intraocular mass was removed.
Biopsy: small, round, blue cells, with some of cells
encircling a lumen (Flexner-Wintersteiner
rosettes and fleurettes). What is the diagnosis
OPTIC NERVE
Swelling of the optic nerve head; can be Optic nerve edema
unilateral or bilateral (papilledema); usually
caused by nerve compression (unilateral) and
increased ICP (bilateral)
TOPNOTCH MEDICAL BOARD PREP PATHO SUPPLEMENT HANDOUT Page 25 of 25
For inquiries visit www.topnotchboardprep.com.ph or https://www.facebook.com/topnotchmedicalboardprep/
Das könnte Ihnen auch gefallen
- 9a Pathology PDFDokument47 Seiten9a Pathology PDFDianne GalangNoch keine Bewertungen
- SurgeryDokument40 SeitenSurgerychristine_8995Noch keine Bewertungen
- Pathology Supplement Handout Nov 2018Dokument25 SeitenPathology Supplement Handout Nov 2018Zak Kaz100% (2)
- Hi-Yield Notes in PCMDokument19 SeitenHi-Yield Notes in PCMJohn Christopher Luces100% (1)
- Topnotch Pathology Supplemental PICTURES Powerpoint Based On Handouts September 2019Dokument53 SeitenTopnotch Pathology Supplemental PICTURES Powerpoint Based On Handouts September 2019croixNoch keine Bewertungen
- Hi-Yield Notes in Legal MedDokument16 SeitenHi-Yield Notes in Legal MedJohn Christopher Luces100% (1)
- 4 Physiology Supplement Handout Based On Ganong For TOPNOTCH 21 by Jaffar PinedaDokument46 Seiten4 Physiology Supplement Handout Based On Ganong For TOPNOTCH 21 by Jaffar PinedaAthena Borja100% (3)
- 8 - Topnotch - Surgery - SuperExam - PDF - Filename - UTF-8''8 - Topnotch Surgery SuperExam PDFDokument94 Seiten8 - Topnotch - Surgery - SuperExam - PDF - Filename - UTF-8''8 - Topnotch Surgery SuperExam PDFArjun Kataria67% (3)
- 12 - Topnotch Preventive Medicine SuperExamDokument86 Seiten12 - Topnotch Preventive Medicine SuperExamPatricia Anne Reyes50% (2)
- Pathology PRC FinaleditDokument11 SeitenPathology PRC FinaleditVince Cabahug100% (1)
- Topnotch Bridge Ob GyneDokument10 SeitenTopnotch Bridge Ob GyneAngela Saldajeno100% (1)
- Topnotch Surgery Supplement HandoutDokument85 SeitenTopnotch Surgery Supplement HandoutSarah Michelle NiduaNoch keine Bewertungen
- Topnotch Microbiology Supertable UPDATED Jan 2016 by DR - Cocoy Calderon PDFDokument75 SeitenTopnotch Microbiology Supertable UPDATED Jan 2016 by DR - Cocoy Calderon PDFDre Valdez100% (1)
- Topnotch Surgery Reviewer PDFDokument81 SeitenTopnotch Surgery Reviewer PDFMarie Frances Lalican-Ringel100% (16)
- Harrisons Reviewer Most Common 1Dokument59 SeitenHarrisons Reviewer Most Common 1Dre Valdez67% (3)
- Tips Sa Boards TextsDokument3 SeitenTips Sa Boards Textshallegail100% (1)
- Topnotch Ent Supplement Handout Updated April 2016pdf PDFDokument15 SeitenTopnotch Ent Supplement Handout Updated April 2016pdf PDFKenneth NuñezNoch keine Bewertungen
- Topnotch Microbiology Supertable - by DR - Cocoy Calderon, Jaffar Pineda, Troy SoberanoDokument3 SeitenTopnotch Microbiology Supertable - by DR - Cocoy Calderon, Jaffar Pineda, Troy SoberanoJohn Christopher Luces100% (1)
- TOPNOTCH Anatomy Pearls September 2018 PDFDokument24 SeitenTOPNOTCH Anatomy Pearls September 2018 PDFApril Aram100% (1)
- Suggested PLE ReviewersDokument1 SeiteSuggested PLE ReviewersBobet Reña80% (5)
- TOPNOTCH Microbiology-Supertable-by-Dr - Cocoy-Calderon-Jaffar-Pineda-Troy-Soberano-UPDATED-NOVEMBER-2017 PDFDokument34 SeitenTOPNOTCH Microbiology-Supertable-by-Dr - Cocoy-Calderon-Jaffar-Pineda-Troy-Soberano-UPDATED-NOVEMBER-2017 PDFWaiwit KritayakiranaNoch keine Bewertungen
- Hi-Yield Notes in Im & PediaDokument20 SeitenHi-Yield Notes in Im & PediaJohn Christopher LucesNoch keine Bewertungen
- 11 Topnotch Pediatrics SuperExam PDFDokument97 Seiten11 Topnotch Pediatrics SuperExam PDFDre Valdez100% (4)
- PRC ObDokument20 SeitenPRC ObLian BaylosisNoch keine Bewertungen
- 1 Topnotch Biochemistry SuperExam PDFDokument92 Seiten1 Topnotch Biochemistry SuperExam PDFDre ValdezNoch keine Bewertungen
- Topnotch Physiology Summary Tables March 2020 PDFDokument23 SeitenTopnotch Physiology Summary Tables March 2020 PDFRob Lagman100% (1)
- September 2019 Boards TipsDokument3 SeitenSeptember 2019 Boards TipspaoloobiasNoch keine Bewertungen
- Topnotch Surgery Supplement Handout UPDATED April 2016 PDFDokument83 SeitenTopnotch Surgery Supplement Handout UPDATED April 2016 PDFDre ValdezNoch keine Bewertungen
- Topnotch Mnemonics - September 2016Dokument6 SeitenTopnotch Mnemonics - September 2016JB ReyesNoch keine Bewertungen
- Topnotch Medical Juris For MoonlightersDokument78 SeitenTopnotch Medical Juris For Moonlightersmefav7778520Noch keine Bewertungen
- Hi-Yield Notes in SurgeryDokument18 SeitenHi-Yield Notes in SurgeryJohn Christopher Luces50% (2)
- Ple Sept 2019Dokument210 SeitenPle Sept 2019Zak Kaz86% (7)
- TTDokument101 SeitenTTralphNoch keine Bewertungen
- Pathology PLE SamplexDokument5 SeitenPathology PLE SamplexAileen Castillo100% (2)
- Review TipsDokument5 SeitenReview TipsyanafkNoch keine Bewertungen
- Suggested Review MaterialsDokument1 SeiteSuggested Review MaterialsJoher MendezNoch keine Bewertungen
- TOPNOTCH Pathology Pearls September 2018 PDFDokument18 SeitenTOPNOTCH Pathology Pearls September 2018 PDFNica Lopez FernandezNoch keine Bewertungen
- Topnotch Supplement Pharmacology Handout PDFDokument57 SeitenTopnotch Supplement Pharmacology Handout PDFBryan Garma80% (5)
- 06 - Topnotch Pathology SuperExam - NOHIGHLIGHTSDokument99 Seiten06 - Topnotch Pathology SuperExam - NOHIGHLIGHTSFrancine Lucas100% (1)
- 9 Topnotch Internal Medicine Superexampdf PDFDokument95 Seiten9 Topnotch Internal Medicine Superexampdf PDFSheryl Layne Lao-Sebrio100% (1)
- TOPNOTCH Pediatrics Main HO September 2018 PDFDokument84 SeitenTOPNOTCH Pediatrics Main HO September 2018 PDFhellokathyyyyyyNoch keine Bewertungen
- PRC QuestionsDokument45 SeitenPRC QuestionsJohn Christopher Luces100% (2)
- September 2021 PleDokument20 SeitenSeptember 2021 PleGian PagadduNoch keine Bewertungen
- TOPNOTCH Anatomy and Histology Main HO September 2018Dokument117 SeitenTOPNOTCH Anatomy and Histology Main HO September 2018Divine Rose Lepon Legaspi100% (1)
- Ana PLEDokument20 SeitenAna PLEGLeen Rose Onguda AguiLarNoch keine Bewertungen
- Topnotch Surgery Reviewer PDFDokument81 SeitenTopnotch Surgery Reviewer PDFkat0% (1)
- Reviewers From PGIDokument5 SeitenReviewers From PGIdickson100% (2)
- PLE Microbiology Cheat SheetDokument2 SeitenPLE Microbiology Cheat SheetModesto Gallardo100% (1)
- PLE Recall March 2016Dokument13 SeitenPLE Recall March 2016Lian BaylosisNoch keine Bewertungen
- Topnotch Surgery Superexam CompressedDokument34 SeitenTopnotch Surgery Superexam CompressedPia Palacios100% (1)
- Qdoc - Tips Topnotch Supplement Pharmacology HandoutDokument57 SeitenQdoc - Tips Topnotch Supplement Pharmacology HandoutShehana MusahariNoch keine Bewertungen
- Tips For The Physicians Licensure Examination1Dokument7 SeitenTips For The Physicians Licensure Examination1Bobet Reña100% (2)
- 1 Topnotch Biochemistry SuperExam1 PDFDokument92 Seiten1 Topnotch Biochemistry SuperExam1 PDFSheinna BarcelonaNoch keine Bewertungen
- PATHOLOGY MAIN HANDOUT - ExtractDokument15 SeitenPATHOLOGY MAIN HANDOUT - ExtractAshley Chloé UyNoch keine Bewertungen
- Surgery PleDokument16 SeitenSurgery Plejose carlo araojo100% (1)
- PLE 2019 Physiology Answer KeyDokument4 SeitenPLE 2019 Physiology Answer KeydicksonNoch keine Bewertungen
- Physician Licensure Exam March 2019 Recall: MicrobiologyDokument4 SeitenPhysician Licensure Exam March 2019 Recall: MicrobiologyNica Lopez FernandezNoch keine Bewertungen
- TOPNOTCH Patho Supplement Handout For Sept 2018 UPDATED May 2018Dokument25 SeitenTOPNOTCH Patho Supplement Handout For Sept 2018 UPDATED May 2018Waiwit KritayakiranaNoch keine Bewertungen
- Apoptosis LectureDokument103 SeitenApoptosis LectureGajanan SaykhedkarNoch keine Bewertungen
- HY PathologyDokument24 SeitenHY Pathologyyahomed519Noch keine Bewertungen
- 3.1 Understanding Formative AssessmentDokument5 Seiten3.1 Understanding Formative Assessmentemely p. tangoNoch keine Bewertungen
- 3.2 Differentiating Formative and Summative AssessmentsDokument6 Seiten3.2 Differentiating Formative and Summative Assessmentsemely p. tangoNoch keine Bewertungen
- 3.3 Applying Different Formative Assessment TasksDokument8 Seiten3.3 Applying Different Formative Assessment Tasksemely p. tangoNoch keine Bewertungen
- Training Design - PRIMALS 4-6 (Math)Dokument1 SeiteTraining Design - PRIMALS 4-6 (Math)emely p. tangoNoch keine Bewertungen
- Training Design - PRIMALS 4-6 (Science)Dokument1 SeiteTraining Design - PRIMALS 4-6 (Science)emely p. tangoNoch keine Bewertungen
- 11 - SurgpathDokument22 Seiten11 - Surgpathemely p. tangoNoch keine Bewertungen
- Patho Supplement Handout For Sept 2018 UPDATED May 2018Dokument27 SeitenPatho Supplement Handout For Sept 2018 UPDATED May 2018emely p. tangoNoch keine Bewertungen
- Informant: Grandmother (70 %) Reliability General DataDokument8 SeitenInformant: Grandmother (70 %) Reliability General Dataemely p. tangoNoch keine Bewertungen
- Deficiency of Iron: First Semester A.Y. 2015-2016Dokument8 SeitenDeficiency of Iron: First Semester A.Y. 2015-2016emely p. tangoNoch keine Bewertungen
- ChorioamnionitisDokument1 SeiteChorioamnionitisemely p. tangoNoch keine Bewertungen
- Final PathophysiologyDokument3 SeitenFinal Pathophysiologyemely p. tangoNoch keine Bewertungen
- (See Next Diagram) : Autonomic Nervous System Rashelle Lopez-Salvatierra, MD Somatic DivisionDokument7 Seiten(See Next Diagram) : Autonomic Nervous System Rashelle Lopez-Salvatierra, MD Somatic Divisionemely p. tango100% (4)
- P58450a Sa Ial Biology Wbi05 01 Oct19 6th ProofDokument8 SeitenP58450a Sa Ial Biology Wbi05 01 Oct19 6th ProofImran MushtaqNoch keine Bewertungen
- Advances in - Veterinary Dermatology PDFDokument248 SeitenAdvances in - Veterinary Dermatology PDFMohammad Javed AsharNoch keine Bewertungen
- Chorea 9Dokument35 SeitenChorea 9Cristina GhizdavetNoch keine Bewertungen
- Self Help (Non-Fiction)Dokument7 SeitenSelf Help (Non-Fiction)jtwendtNoch keine Bewertungen
- Medical Genetics: JORDE B. L. Et AlDokument30 SeitenMedical Genetics: JORDE B. L. Et AlChris xNoch keine Bewertungen
- Enzyme TherapyDokument34 SeitenEnzyme TherapyMohamed AbdelmoneimNoch keine Bewertungen
- Reviewer in Science 10Dokument2 SeitenReviewer in Science 10fan girlNoch keine Bewertungen
- Achondroplasia Stacy, NikkyDokument14 SeitenAchondroplasia Stacy, NikkyStacy PhuongNoch keine Bewertungen
- Alzheimer Disease Including Focal Presentations PDFDokument14 SeitenAlzheimer Disease Including Focal Presentations PDFpiedrahitasaNoch keine Bewertungen
- Chapter 7 - MutationDokument7 SeitenChapter 7 - MutationblaNoch keine Bewertungen
- Please See Chapter 8: The Nursing Role in Genetic Assessment and Counseling Page 155.Dokument8 SeitenPlease See Chapter 8: The Nursing Role in Genetic Assessment and Counseling Page 155.Stephanie RodriguezNoch keine Bewertungen
- Ethical Issues in Assisted Reproductive Technologies ART 2Dokument49 SeitenEthical Issues in Assisted Reproductive Technologies ART 2Pavan chowdaryNoch keine Bewertungen
- Test Bank For Maternity Nursing 8th Edition, LowdermilkDokument26 SeitenTest Bank For Maternity Nursing 8th Edition, LowdermilkILL101100% (2)
- Instant Download Child Development An Active Learning Approach Third Edition PDF Version PDF ScribdDokument41 SeitenInstant Download Child Development An Active Learning Approach Third Edition PDF Version PDF Scribdstanley.rodriquez278100% (36)
- Topic 10: Activity 1-Genetic DisordersDokument4 SeitenTopic 10: Activity 1-Genetic DisordersMonalisa TrayaNoch keine Bewertungen
- 05 Paediatrics 25092019Dokument9 Seiten05 Paediatrics 25092019Disha100% (1)
- Health Care Ethics 248 305Dokument68 SeitenHealth Care Ethics 248 305elle bello100% (2)
- 2023-05-12T08 - 05 - 49.1880033Z - Esb - Medical - Profile 2Dokument8 Seiten2023-05-12T08 - 05 - 49.1880033Z - Esb - Medical - Profile 2claudiais231966Noch keine Bewertungen
- Assignment 2 - Gene TherapyDokument9 SeitenAssignment 2 - Gene Therapyflat furNoch keine Bewertungen
- Clinical Methods in MedicineDokument555 SeitenClinical Methods in Medicineserry_ann100% (8)
- Pediatric Spots PDFDokument318 SeitenPediatric Spots PDFMoha JundaNoch keine Bewertungen
- Dyskeratosis Congenita and Other Telomere Biology Disorders - UpToDateDokument44 SeitenDyskeratosis Congenita and Other Telomere Biology Disorders - UpToDateMae Matira AbeladorNoch keine Bewertungen
- Chapter 03: Genetic and Genomics: The Basics of Child Health Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDokument3 SeitenChapter 03: Genetic and Genomics: The Basics of Child Health Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNoch keine Bewertungen
- Genetic Disorders: Recessive Disorders (Homozygous) Description Cases Per Birth Sickle Cell Disease (SCD)Dokument18 SeitenGenetic Disorders: Recessive Disorders (Homozygous) Description Cases Per Birth Sickle Cell Disease (SCD)tango0385100% (1)
- ChoreaDokument17 SeitenChoreaNamarig IzzaldinNoch keine Bewertungen
- ASRM - Diagnostic Evaluation of The Infertile FemaleDokument11 SeitenASRM - Diagnostic Evaluation of The Infertile FemaleMina zhouNoch keine Bewertungen
- DNA Mutations and Genetic DiseasesDokument3 SeitenDNA Mutations and Genetic DiseasesPramudith Liyanage0% (1)
- DEI Outreach & Inclusion Part Two Bacchetta CLIN2-13259Dokument2 SeitenDEI Outreach & Inclusion Part Two Bacchetta CLIN2-13259California Stem Cell ReportNoch keine Bewertungen
- Gene Hunting: J. PongraczDokument15 SeitenGene Hunting: J. PongracztahirnaeemkhanNoch keine Bewertungen
- Test Bank For Medical Genetics 4th Edition Lynn B JordeDokument8 SeitenTest Bank For Medical Genetics 4th Edition Lynn B JorderoytuyenbauNoch keine Bewertungen