Beruflich Dokumente
Kultur Dokumente
Pi Is 0301562914010837
Hochgeladen von
Namita Bose0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
6 Ansichten1 SeiteDocuments
Originaltitel
Pi is 0301562914010837
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenDocuments
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
6 Ansichten1 SeitePi Is 0301562914010837
Hochgeladen von
Namita BoseDocuments
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
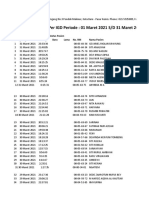
S60 Ultrasound in Medicine and Biology Volume 41, Number 4S, 2015
average abnormal ovarian volume was 22.2 cc (range 9.6-
No Sludge Sludge 40cc, median-17cc). Average abnormal to normal ratio was
Pregnancy Outcomes: (n513) (n533) P-value 11.3 (range: 2.8-50, median-3.7). The 17 postmenarchal cases
Gestational age at 37 5/7 37 2/7 0.643a ranged from 12-19 yrs. All the postmenarchal uteri were pear
delivery (wks)1 (23 1/7, 40 2/7) (22 3/7, 40 3/7) shaped (fundus wider than cervix). Uterine length mean was
Delivery at , 24 wks2 1/33 (3%) 1/33 (7.7%) 0.490b 7.6 cm (range: 5.3-9.7cm). Average normal postmenarchal
Delivery at , 25 wks2 1/13 (7.7%) 1/31 (3.2%) 0.508b ovarian volume was 6.5 cc (range: 3-17.6cc). Average abnormal
Delivery at , 28 wks2 2/13 (15.3%) 1/33 (3.2%) 0.204b ovarian volume was 44.4 cc (range: 17.8-88cc), median is 3.9.
Delivery at , 32 wks2 3/13 (23.1%) 5/33 (15.1%) 0.648b Average abnormal to normal ratio was 6.8 (range: 3.3-25.2, me-
Delivery at , 34 wks2 3/13 (23.1%) 8/33 (24.2%) 1.000b dian 6.4).
Deliver at , 37 wks2 5/13 (38.5%) 14/33 (42.4%) 0.749b Conclusions: Premenarchal uterine shapes were
Baby Weight (g)3 2813 (1003) 2802 (752) 0.977c tubular. Postmenarchal uterine shapes were pear shaped. The
median abnormal premenarchal ovarian volume was 17cc while
1
median(min,max); 2proportion (%) 3mean(sd); aWilcoxon-test;bFisher- the postmenarchal abnormal ovarian volume was 34cc. The me-
test;ct-test; dian abnormal ovarian volume to normal ratio was 3.7 for pre-
menarchal and 6.4 for postmenarchal cases. Uterine shape and
length can help determine prepubertal or postpubertal status
in the baseline number of previous preterm did not significantly and affect expected abnormal volumes helping aid torsion diag-
affect the results. nosis.
Conclusions: Despite associated differences in Cx
funneling and shorter Cx, the presence of IAS did not affect 2090707 The Effect of Bedside Ultrasound (US) Assistance
pregnancy outcome in terms of gestational age at birth. These on The Proportion Of Successful Infant Lumbar
results suggest that the presence of IAS does not contraindicate Punctures in a Pediatric Emergency Department:
the use of cerclage in asymptomatic pts who are candidates for A Randomized Controlled Trial
cerclage.
Jeffrey Thomas Neal,1 Aaron Chen1 1Pediatrics,
Children’s Hospital of Philadelphia, Philadelphia,
PA, United States
Pediatric Ultrasound Objectives: The reported rate of unsuccessful/trau-
matic lumbar puncture (LP) in children is as high as 50-60%.
Moderator: Annamaria Deganello, MD
Bedside US allows visualization of anatomic landmarks and
has been shown to reduce LP failure rates in adults. Increasing
2072981 Can Uterine Shape and Size Predict Expected
the proportion of successful LPs in the ED could significantly
Volumes In Ovarian Torsion: A Pilot Study
reduce the rate of unnecessary hospitalizations, procedures,
Anand Majmudar,1,2 Harris L. Cohen1,2 and antibiotic use. Data on the effect of bedside US on the suc-
1
Radiology, Lebonheur Children’s Hospital, cess rate of infant LP, however, is limited. Our OBJECTIVES: is
Memphis, TN, United States; 2Radiology, University to determine if bedside US-assisted site marking increases the
of Tennessee Health Science Center, Memphis, TN, proportion of successful infant LPs by clinicians in our pediatric
United States ED.
Methods: This was a prospective, randomized
Objectives: To observe, if there is a difference be- controlled study of infants aged 0 to 6 months presenting to
tween pediatric premenarchal and postmenarchal ovarian our ED and requiring an LP; subjects with a known spinal
measurements in torsion. To note, if uterine size analysis cord abnormality (such as tethered cord) were excluded. Sub-
can be used to help assess expected range of volumes of jects randomized to traditional LP (TLP) had LP as per routine
abnormal ovaries. standard of care; subjects randomized to ultrasound-assisted LP
Methods: We retrospectively evaluated the presurgi- (USLP) received a bedside US of the spine during which the
cal ultrasound exams of pathologically proven ovarian torsion conus was identified and the intervertebral space (L2/3, L3/4,
cases in a children’s hospital between Jan 2008 and July 2014. or L4/5) with the most cerebrospinal fluid (CSF) was marked,
The volumes of abnormal and normal ovaries were determined with the LP performed at the marked location. Subjects were
by the prolate ellipse formula of width x length x depth x 0.523. considered to have a successful LP if CSF fluid was obtained
Only the patients in whom two ovaries were seen in three di- and CSF red blood cells (RBC) were ,1000 per mm3. Fisher’s
mensions were included. Uterus shapes and lengths were evalu- exact test was used to analyze the proportions of success rates, at
ated to see whether they could help to determine premenarchal a significance level of 0.05.
or postmenarchal state and whether that information affected Results: 37 infants were included in this preliminary
the range of abnormal volumes or the ratio of abnormal ovarian analysis: 19 TLP, 18 USLP; mean age: 30.2 days TLP, 22.6 days
volume to normal ovarian volume. USLP; provider level of training on first attempt: TLP (78.9%
Results: 6 premenarchal and 17 postmenarchal cases trainee, 21.1% fellow/attending), USLP (94.4% trainee, 5.6%
of ovarian torsion were noted. The 6 premenarchal cases ranged fellow/attending). Results of success: first attempt (TLP
from 4-11yrs of age. All premenarchal uteri were tubular in 36.8%, USLP 55.6%, p-value 5 0.33), within three attempts
shape (fundal width equal to cervical width). The premenarchal (TLP 47.4%, USLP 72.2%, p-value 5 0.184).
mean uterine length was 4.0 cm (range: 2.9-5.6cm). Average Conclusions: Although not statistically significant, it
normal ovarian volume was 5.2 cc (range: 0.8-12.7cc). The appears there is a trend for improved success with USLP over
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Virginia HendersonDokument16 SeitenVirginia HendersonDANELA DURANNoch keine Bewertungen
- Trauma Evaluation and Management: Early Care of The Injured PatientDokument130 SeitenTrauma Evaluation and Management: Early Care of The Injured PatienttesfahuntekleNoch keine Bewertungen
- Michelle Martin Resume 2021 Final 1pageDokument1 SeiteMichelle Martin Resume 2021 Final 1pageapi-540444992Noch keine Bewertungen
- Translate This Into Communicative English!: 1 Assignment, Nursing English, 2 SemesterDokument2 SeitenTranslate This Into Communicative English!: 1 Assignment, Nursing English, 2 SemesterYunita TriscaNoch keine Bewertungen
- Early Childhood CariesDokument4 SeitenEarly Childhood CariesAstia Dwiputri LestariNoch keine Bewertungen
- Antibiotic Susceptibility of Bacterial Isolates FRDokument8 SeitenAntibiotic Susceptibility of Bacterial Isolates FRkaren leeNoch keine Bewertungen
- Infusion Set and Blood Transfusion SetDokument56 SeitenInfusion Set and Blood Transfusion Setsaahil_goje1400Noch keine Bewertungen
- P.E 3A Learning Activity Sheet WEEK 5 6Dokument7 SeitenP.E 3A Learning Activity Sheet WEEK 5 6Ris CorreaNoch keine Bewertungen
- Triase IGD Maret 2021Dokument33 SeitenTriase IGD Maret 2021IRAYANANoch keine Bewertungen
- MaretDokument132 SeitenMarettipanoesaNoch keine Bewertungen
- Retaining WallDokument10 SeitenRetaining Wallsandip patilNoch keine Bewertungen
- NCP: Diabetes Mellitus Prepregnancy/GestationalDokument11 SeitenNCP: Diabetes Mellitus Prepregnancy/GestationalJavie85% (13)
- Infertility A Review On Causes Treatment and ManagementDokument19 SeitenInfertility A Review On Causes Treatment and Managementreza tryasNoch keine Bewertungen
- Lenin PostmortemDokument6 SeitenLenin Postmortemapi-196020598Noch keine Bewertungen
- Career Research EssayDokument6 SeitenCareer Research Essayapi-399119600Noch keine Bewertungen
- Hyphema Uveitis AnteriorDokument3 SeitenHyphema Uveitis AnteriorMadelaineNoch keine Bewertungen
- 157 - Clinical Trials Adverse Events ChaDokument6 Seiten157 - Clinical Trials Adverse Events ChaWoo Rin ParkNoch keine Bewertungen
- Sample Letter of Medical NecessityDokument4 SeitenSample Letter of Medical NecessityGregory RussellNoch keine Bewertungen
- CDR 24 S 8 eDokument66 SeitenCDR 24 S 8 eHerminio Fuentes VelezNoch keine Bewertungen
- Neuropsychiatry and Behavioral NeurologyDokument302 SeitenNeuropsychiatry and Behavioral NeurologyTomas Holguin70% (10)
- Sindh Institute of Urology and Transplantation (Siut), Karachi BY Muhammad Asim Halim (Irs)Dokument4 SeitenSindh Institute of Urology and Transplantation (Siut), Karachi BY Muhammad Asim Halim (Irs)asimhalimNoch keine Bewertungen
- AlopeciaDokument2 SeitenAlopeciaAldrich ArquizaNoch keine Bewertungen
- Shock ExamDokument3 SeitenShock ExamMilagros Fuertes Yosores100% (1)
- Delirium: Annals of Internal MedicineDokument16 SeitenDelirium: Annals of Internal Medicinemariell3193Noch keine Bewertungen
- Resume VeronicaDokument3 SeitenResume Veronicajomar_saquingNoch keine Bewertungen
- Hazard Identification and Prevention: (Ndlon-Osha)Dokument12 SeitenHazard Identification and Prevention: (Ndlon-Osha)Eugine BalomagaNoch keine Bewertungen
- Esthetic Impact of Premolar Extraction and Nonextraction Treatments On Korean Borderline PatientsDokument8 SeitenEsthetic Impact of Premolar Extraction and Nonextraction Treatments On Korean Borderline Patientsblogger bloggerNoch keine Bewertungen
- Tata Kelola DM Di FKTPDokument29 SeitenTata Kelola DM Di FKTPRSTN BoalemoNoch keine Bewertungen
- Special Requirements of Electronic Medical Record Systems in Obstetrics and GynecologyDokument4 SeitenSpecial Requirements of Electronic Medical Record Systems in Obstetrics and GynecologysayansambitNoch keine Bewertungen
- Master DiagnosisDokument708 SeitenMaster DiagnosisardinardinNoch keine Bewertungen