Beruflich Dokumente
Kultur Dokumente
Medical Writings: "Let Me See If I Have This Right - . - ": Words That Help Build Empathy
Hochgeladen von
Anonymous fPQaCe8Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Medical Writings: "Let Me See If I Have This Right - . - ": Words That Help Build Empathy
Hochgeladen von
Anonymous fPQaCe8Copyright:
Verfügbare Formate
WORDS THAT MATTER
Medical Writings
“Let Me See If I Have This Right . . . ”: Words That Help Build Empathy
C onsider these two physician–patient dialogues: EMPATHY IN THEORY
Tichener coined the term “empathy” in 1909 from
two Greek roots, em and pathos (feeling into) (15). For
1. Patient: You know, when you discover a lump in
your breast, you kind of feel—well, kind of— (her speech some 50 years thereafter, empathy was discussed in the
tapers off; she looks down; tears form in her eyes). psychological and psychoanalytic literature as a type of
Dr. A: When did you actually discover the lump? vicarious emotional response (16 –23). For example,
Patient: (absently) I don’t know. It’s been a while. Katz (24) wrote “when we experience empathy, [it is] as
if we were experiencing someone else’s feelings as our
2. Patient: (same as above) own. We see, we feel, we respond, and we understand as
Dr. B: That sounds frightening. if we were, in fact, the other person.” Lief and Fox (25)
Patient: Well, yeah, sort of. diluted this strong sense of identification when they
Dr. B: Sort of frightening? used the word to designate the vector for detached con-
Patient: Yeah . . . and I guess I’m feeling like my life cern. They wrote that empathy involves “an emotional
is over. understanding of the patient,” while maintaining suffi-
Dr. B: I see. Worried and sad too. cient separation “so that expert medical skills can be
Patient: That’s it, Doctor. rationally applied to the patient’s problem” (25). In
practice, “emotional understanding” has to be tested by
checking back with the patient, and its accuracy is en-
Dr. A’s patient may well go home feeling unheard hanced through iteration.
and misunderstood. Dr. B’s patient, while equally dis- The concept of empathy has three important impli-
tressed about the possibility of having breast cancer, may cations. First, empathy has a cognitive focus. The clini-
leave the office believing that her doctor understands her. cian “enters into” the perspective and experience of the
One of the most widespread and persistent com- other person by using verbal and nonverbal cues, but she
plaints of patients today is that their physicians don’t neither loses her own perspective nor collapses clinical
listen. For their part, physicians complain that they no distance. Second, empathy also has an affective or emo-
longer have sufficient time to spend with patients, and tional focus. The clinician’s ability to put herself in the
they often blame economic pressures imposed by man- patient’s place— or walk a mile in his moccasins—re-
aged care (1, 2). Nonetheless, they acknowledge that quires the experience of surrogate or “resonant” feelings
personal encounters with patients constitute the most (26). Finally, the definition requires that clinical empa-
satisfying aspect of their professional lives. They recog- thy have an action component. One cannot know with-
nize that empathy, the ability to “connect” with pa- out feedback. The practitioner communicates under-
tients—in a deep sense, to listen, to pay attention—lies standing by checking back with the patient, using, for
at the heart of medical practice (1, 3, 4). example, statements such as “Let me see if I have this
In clinical medicine, empathy is the ability to under- right” or “I want to be sure I understand what you
stand the patient’s situation, perspective, and feelings mean.” This gives the patient opportunities to correct or
and to communicate that understanding to the patient. modulate the physician’s formulation. At the same time
The effective use of empathy promotes diagnostic accu- it expresses the physician’s desire to listen deeply,
racy, therapeutic adherence, and patient satisfaction, thereby reinforcing a bond or connection between clini-
while remaining time-efficient (5–11). Empathy also en- cian and patient.
hances physician satisfaction (12). As with any other Empathy is sometimes confused with sympathy, or
tool, clinical empathy requires systematic practice to emotional identification with the patient’s plight. Sym-
achieve mastery (13, 14). Certain well-timed words and pathetic responses include a physician’s feeling sad and
sentences facilitate empathy during the clinical encoun- becoming teary eyed when his patient starts crying, or a
ter. These “words that work” are the subject of this paper. physician’s experiencing righteous anger when her pa-
© 2001 American College of Physicians–American Society of Internal Medicine 221
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Medical Writings Words That Help Build Empathy
tient recounts an injustice. Sympathy also applies to that the physician remain silent and focus her attention
feelings of loss that people experience in response to on the patient’s story (47, 48).
another’s loss. When present, sympathy often contrib-
utes to the physician–patient relationship, yet physicians Framing or Sign Posting
may not always exhibit sympathy because some patients Clinicians often initiate an empathic response when
are disagreeable, culpable, or unlikable. Empathy, by they “pick up” a suggestion or indication that the pa-
contrast, does not depend on having congruent feelings tient is experiencing concern, conflict, or emotion. Be-
and thus may be more versatile. A physician can be em- cause accurate understanding is not commonly at-
pathic even when he or she cannot be sympathetic (27, 28). tempted in ordinary conversation, patients may be
Numerous investigators have demonstrated the im- unaccustomed to empathic responses. Clinicians may
portance of empathy in the medical encounter. Empa- need to disclose their intent, providing a frame or sign-
thy allows the patient to feel understood, respected, and post for the patient (35). Lengthy warning may be inef-
validated. This promotes patient satisfaction, enhances ficient and exhausting, so we usually abbreviate it in
the quantity and quality of clinical data, improves ad- these ways:
herence, and generates a more therapeutic physician– Let’s see if I have this right.
patient relationship (5–11, 29 –31). To achieve these Sounds like what you’re telling me is . . .
goals, medical educators conceptualized empathy as a set Or simply Sounds like. . .
of teachable and learnable skills and developed a new
focus on communication skills in the medical curricu- Reflecting the Content
lum (13, 14, 32–36). More recently, some educators An empathic response accurately identifies the fac-
have explored the roles of narrative and literature in tual content of the patient’s statement, as well as the
teaching clinical empathy (37–39), and others have em- nature and intensity of the patient’s feelings, concerns, or
phasized the importance of reflection and self-awareness quandaries. A reflection of content (symptoms or ideas)
in maintaining one’s empathic skills (40 – 44). might sound like the following:
So you were fine until this morning when you woke up
EMPATHY IN PRACTICE with pain in your belly, and it’s been growing more severe
Clinical empathy can be visualized as a positive ever since.
feedback loop, or a neurologic track with afferent and Sounds like you think that you have appendicitis and
efferent components (45, 46). The afferent arm includes that you might need to go into the hospital.
verbal and nonverbal cues that lead to the practitioner’s The physician may also mirror the patient’s interests
initial appraisal or understanding of the patient’s mes- and values:
sage. The efferent arm includes the practitioner’s re- So, if I’m hearing you right, what you really enjoy is
sponses— queries such as “Tell me more” or statements going out at night with your friends and having a few drinks.
such as “I can imagine how difficult it is.” Such re-
sponses elicit additional information. While it is impos- Identifying and Calibrating the Emotion
sible for the clinician to understand exactly how the Clinical empathy often entails responding to the pa-
patient feels, in clinical empathy successive cycles may tients’ expressed (or suggested) feelings. This means
lead to a clearer, more accurate “fix” on the patient’s identifying the emotion and calibrating its intensity.
perspective and feelings. Thus, empathic communica- Sometimes emotional content is evident, but the nature
tion includes the following components. of the emotion is unclear. In such cases the patient will
often reveal the feeling, if given an opportunity.
Active Listening Tell me how you’re feeling about this.
This requires nonverbal and paralanguage skills, I have the sense that you feel strongly, but I’m not sure
such as appropriate position and posture; good eye con- I understand exactly what the feeling is. Can you tell me?
tact; mirroring of facial expression; and facilitative re- The following are examples of empathic responses
sponses, such as nodding and minimal expressions (for to patient statements that express sadness, fear, anger,
example, “Hmmm . . .” and “Uh-huh”). It also demands distrust, and ambivalence.
222 7 August 2001 Annals of Internal Medicine Volume 135 • Number 3 www.annals.org
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Words That Help Build Empathy Medical Writings
Sadness: That must have been a pretty painful experi- Then, when corrected, the physician incorporates
ence for you, you sound like it was very sad. the new data into a second (or third) cycle of listening,
Fear: Sounds like you were really frightened when you reflecting, and responding. The process continues until
discovered that lump. the patient confirms the clinician’s understanding: “You
Anger: That situation really got to you, didn’t it? I can got it, Doc,” or “That’s it, Doc.”
imagine how angry I’d feel if that happened to me.
Distrust: It seems you’re not sure whether you should
trust me further after I didn’t get that test result back to you WHEN AND WHERE
last week. Empathy belongs with every patient and through-
Ambivalence: It seems to me that you’re caught in a out every encounter (49, 50). However, much of the
bind about whether to stop smoking or not. time empathy is invisible (one does it unconsciously)
Feelings vary markedly in intensity; often, clinicians because the patient’s needs are relatively transparent and
tend to sanitize or dilute them. Consider this example: the physician’s responses automatic. Clinicians often ini-
Patient: Most days the pain is so terrible that I just tiate an empathic response when they “pick up” an in-
want to stay in bed. I just stare at the ceiling . . . what’s dication that the patient is experiencing concern, con-
the point of it all? flict, or emotion. What are these indications? In some
Doctor: So you’re frustrated about the pain? cases the patient presents a frank expression of suffering
In this case, the physician identified an emotion or emotion; in others, a more subtle affective comment
(frustration) but failed to capture the patient’s profound is casually “dropped” to test the water’s temperature.
sense of helplessness. Weak affective words such as More commonly, the physician might realize that her
“bother,” “annoy,” “upset,” “uneasy,” and “apprehen- patient’s strong feelings are embedded in quasi-factual
sive” are sometimes appropriate. At other times, red- statements or inquiries. Alternatively, the observant cli-
blooded adjectives such as “infuriated,” “enraged,” “tor- nician might notice discordant messages between verbal
mented,” “overwhelmed,” and “terrified” are more in expressions and aspects of nonverbal communication,
order. This patient feels so depressed and helpless that such as eye contact, movements, and autonomic re-
he asks, “What’s the point of it all?” By hearing only sponses. Suchman and coworkers (37) referred to these
annoyance or frustration in the statement, the physician moments as potential empathic opportunities. They
missed a diagnostic cue and perhaps a useful path of found that physicians frequently rejected these opportu-
inquiry and has distanced herself from the patient. An nities by changing the topic. In their study of experi-
alternative answer could be, It sounds to me like you’re enced practitioners, Branch and Malik (51) noted that
completely overwhelmed . . . you must feel helpless. most physicians bypassed such opportunities for getting
Finally, patients are often unaware of, or out of to the heart of their patients’ problems.
touch with, their feelings. Sensitive inquiry by the phy-
sician may provide opportunities for them to acknowl-
edge this situation and “tune into” their feelings (“Well, DON’T JUST DO SOMETHING, STAND THERE
yes, I hadn’t thought of it that way, but now that you Having established an empathic connection, physi-
mention it, I am angry.”) Alternatively, such patients cians are often anxious about what to do next. Some
may continue to reject, deny, or disguise their emotional launch into immediate efforts to reassure. It is effective
responses (“Angry? No way. I’m just stating the facts.”). to delay that effort, allowing a pause of several seconds.
This is often true in situations involving somatization or A good rule might be “don’t just do something, stand
compensation, where social and cultural factors militate there.” During the pause, the patient is experiencing
against emotional disclosure. being understood, which in itself has therapeutic value.
At the same time, the physician can be considering more
Requesting and Accepting Correction deeply just what this patient has been going through.
Respectful acceptance of the patient’s correction is a Sometimes the introspection leads to further powerful
powerful way of communicating the desire to understand. communication. One of us recently reported visiting
Did I miss anything? Anything I left out? with a “difficult patient”:
www.annals.org 7 August 2001 Annals of Internal Medicine Volume 135 • Number 3 223
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Medical Writings Words That Help Build Empathy
I kept reminding myself that I needed to be empathic care arrangements are unavailable in their new commu-
with this patient despite the fact that I was not having nities (52). Is it possible to express empathy for patients
much sympathy for her. I have to admit the task was whose background and life experience are totally differ-
taxing and difficult. What seemed to work with my ent from your own?
patient was honesty. I told her, “You know, I want to
There is a popular belief that one has to experience
understand and to help you, but sometimes I feel like
something oneself in order to understand “what it’s like”
you are driving me crazy. I don’t want to feel that way,
but I do.” Then I went on to say, “Sometimes, when
for another person. Indeed, it would be wrong to min-
doctors feel their patients are driving them crazy it is imize the difficulties of cross-cultural, interracial, or
because the patients experience their own lives as crazy even transgender understanding. However, if clinical
and chaotic.” She looked at me with disbelief and empathy is understood as a feedback loop, one can see
started crying and then told me that she felt she was how successive cycles may lead to improved understand-
losing control and how difficult it was to live with this ing. If nothing else, the clinician’s honest attempt to
pain. She said, “I feel that I am driving myself crazy as understand should facilitate trust. Empathy involves
well as all the people that are around me.” drawing on our own range of feelings and experiences
and then taking an imaginative leap—“Aha! Her feeling
Physicians hear so many difficult and distressing is like. . . . ” This leap may involve metaphor, where one
stories, it is no wonder that they often rush to reassure uses a striking shared characteristic to describe an un-
their patients: It can’t be as bad as that. Everything will be known concept or feeling in terms of something known.
all right. Don’t worry, most of the time it’s a false positive. For example, a physician might say to a patient who
In a profession that values decisiveness and action, it is seems angry and disappointed, You must feel like you
difficult not to do something to defuse patient distress rushed to the platform, only to find that your train had
when it occurs. Reassurance springs to the lips. Such already left.
statements are usually made in good faith and some- In essence, the imaginative leap is a hypothesis. The
times are probabilistically true: that is, it is likely that practitioner may not be able to guess her patient’s feel-
everything will be all right. Nonetheless, such reassur- ings or values on the first try, but clinical empathy as we
ance often fails if the physician does not also communi- have described it is a hypothesis-testing feedback loop
cate an awareness of the patient’s deepest fears or concerns. that allows the physician to move closer to understand-
ing. Here are some examples of empathic statements a
clinician might make in a cross-cultural encounter:
CULTURE AND EMPATHY
Seems like it would be difficult for you not to feel
In our diverse society, physicians encounter patients 100% understood.
from different ethnic and cultural groups, some of I imagine it’s stressful to find that treatments in the
whom have a poor command of the language spoken by United States are different than in your country.
the practitioner. These patients may experience added It has to be very difficult to take pills instead of the
distress because traditional support systems or health herbs that you are accustomed to.
It must be terrifying to have your child so sick, and
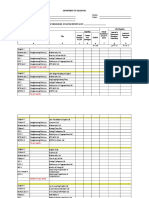
Table 1. Guidelines for Clinical Empathy in the then have to bring him in to see a doctor you’re not accus-
Cross-Cultural Setting tomed to.
Even when a patient speaks the practitioner’s lan-
Understand your own cultural values and biases
Develop a familiarity with the cultural values, health beliefs, and illness guage relatively well, language may still be a barrier to
behaviors of ethnic, cultural, and religious groups served in your practice discussing complex medical topics or to talking about
Ask how the patient prefers to be addressed
Determine the patient’s level of fluency in English and arrange for a personal feelings, beliefs, and values. Often it is unclear
translator, if needed whether language itself is the barrier or, alternatively,
Assure the patient of confidentiality; rumors, jealousy, privacy, and
reputation are crucial issues in close-knit traditional communities cultural practices that prohibit airing certain topics or
Use a speech rate, tone, and style that promote understanding and show revealing certain information. Table 1 presents several
respect for the patient
Check back frequently to determine patient understanding and acceptance guidelines to assist in empathic understanding across
ethnic and cultural barriers. The next step is to ascertain
224 7 August 2001 Annals of Internal Medicine Volume 135 • Number 3 www.annals.org
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Words That Help Build Empathy Medical Writings
Table 2. Words That Work: Statements That Facilitate John L. Coulehan, MD
Empathy State University of New York at Stony Brook
Stony Brook, NY 11794-8036
Queries
“Would you (or could you) tell me a little more about that?”
“What has this been like for you?” Frederic W. Platt, MD
“Is there anything else?” University of Colorado Health Sciences Center
“Are you OK with that?”
“Hmmmm” Denver, CO 80222
Clarifications
“Let me see if I have this right.” Barry Egener, MD
“I want to make sure I really understand what you’re telling me. I am
hearing that . . .”
American Academy on Physician and Patient
“I don’t want us to go further until I’m sure I’ve gotten it right.” Portland, OR 97210
“When I’m done, if I’ve gone astray, I’d appreciate it if you would correct
me. OK?”
Responses
Richard Frankel, PhD
“That sounds very difficult.” Highland Hospital
“Sounds like . . .”
Rochester, NY 14620
“That’s great! I bet you’re feeling pretty good about that.”
“I can imagine that this might feel . . .”
“Anyone in your situation would feel that way . . .” Chen-Tan Lin, MD
“I can see that you are . . .” University of Colorado Health Sciences Center
Denver, CO 80222
Beth Lown, MD
Mount Auburn Hospital
the patient’s beliefs about the nature of the illness and Cambridge, MA 02238
what needs to be done about it (53) and to learn more
William H. Salazar, MD
about the patient’s life experience (54), while maintain-
Medical College of Georgia
ing a sensitive and respectful demeanor.
Augusta, GA 30902
Requests for Single Reprints: John L. Coulehan, MD, Department of
SUMMARY: FROM GOOD LINES TO GOOD Preventive Medicine, HSC L3-086, State University of New York at
ENCOUNTERS Stony Brook, Stony Brook, NY 11794-8036; e-mail, jcoulehan@uhmc
.sunysb.edu.
Table 2 presents words, phrases, and sentences that
are useful in practicing clinical empathy. Empathy Current Author Addresses: Dr. Coulehan: Department of Preventive
might also be visualized as a fastener or lock that enables Medicine, HSC L3-086, State University of New York at Stony Brook,
the physician and patient to “click” together. On the Stony Brook, NY 11794-8036.
physician’s side, the critical step occurs when he or she Drs. Platt and Lin: University of Colorado Health Sciences Center, 4200
East Ninth Avenue, Denver, CO 80222.
says something like
Dr. Egener: American Academy on Physician and Patient, Legacy Clinic
Let me see if I’ve gotten this right. Northwest, 1130 NW 22nd Avenue, Suite 220, Portland, OR 97210.
Sounds like. . . . Dr. Frankel: Highland Hospital, 1000 South Avenue, Rochester, NY
I want to make sure that I understood what you’re 14620.
telling me. Dr. Lown: Mount Auburn Hospital, 300 Mt. Auburn Street, Cam-
I can imagine that this might feel. . . . bridge, MA 02238.
Dr. Salazar: Medical College of Georgia, 1120 15th Street, HS2010,
On the patient’s side, the crucial step occurs when Augusta, GA 30902.
he or she says:
“You got it, Doc.” Ann Intern Med. 2001;135:221-227.
“Exactly.”
“That’s how I feel.” References
If you don’t get such a confirmation, you aren’t 1. Konrad TR, Williams ES, Linzer M, McMurray J, Pathman DE, Gerrity M,
done. et al. Measuring physician job satisfaction in a changing workplace and a chal-
www.annals.org 7 August 2001 Annals of Internal Medicine Volume 135 • Number 3 225
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Medical Writings Words That Help Build Empathy
lenging environment. SGIM Career Satisfaction Study Group. Society of General 24. Katz RL. Empathy: Its Nature and Uses. New York: Free Press; 1963:26.
Internal Medicine. Med Care. 1999;37:1174-82. [PMID: 10549620] 25. Lief HI, Fox RC. Training for “detached concern” in medical students. In:
2. Donelan K, Blendon RJ, Lundberg GD, Calkins DR, Newhouse JP, Leape Lief HI, ed. The Psychological Basis of Medical Practice. New York: Harper &
LL, et al. The new medical marketplace: physicians’ views. Health Aff (Mill- Row; 1963:12-35.
wood). 1997;16:139-48. [PMID: 9314685] 26. Halpern J. Empathy: Using resonance emotions in the service of curiosity. In:
3. Bates AS, Harris LE, Tierney WM, Wolinsky FD. Dimensions and correlates Spiro H, McCrea Curnen MG, Peschel E, St James D, eds. Empathy and the
of physician work satisfaction in a midwestern city. Med Care. 1998;36:610-7. Practice of Medicine. New Haven, CT: Yale Univ Pr; 1993:160-73.
[PMID: 9544600] 27. Wispe L. The distinction between sympathy and empathy: to call forth a
4. McMurray JE, Williams E, Schwartz MD, Douglas J, Van Kirk J, Konrad concept, a word is needed. Journal of Personality and Social Psychology. 1986;
TR, et al. Physician job satisfaction: developing a model using qualitative data. 50:314-21.
SGIM Career Satisfaction Study Group. J Gen Intern Med. 1997;12:711-4. 28. Wilmer HA. The doctor-patient relationship and the issues of pity, sympathy
[PMID: 9383141] and empathy. Br J Med Psychol. 1968;41:243-8. [PMID: 5728595]
5. Beckman HB, Frankel RM. The effect of physician behavior on the collection 29. Bertakis KD, Roter D, Putnam SM. The relationship of physician medical
of data. Ann Intern Med. 1984;101:692-6. [PMID: 6486600] interview style to patient satisfaction. J Fam Pract. 1991;32:175-81. [PMID:
6. Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient’s 1990046]
agenda: have we improved? JAMA. 1999;281:283-7. [PMID: 9918487] 30. Roter D, Lipkin M Jr, Korsgaard A. Sex differences in patients’ and physi-
7. Roter DL, Stewart M, Putnam SM, Lipkin M Jr, Stiles W, Inui TS. Com- cians’ communication during primary care medical visits. Med Care. 1991;29:
munication patterns of primary care physicians. JAMA. 1997;277:350-6. 1083-93. [PMID: 1943269]
[PMID: 9002500] 31. Levinson W, Roter D. Physicians’ psychosocial beliefs correlate with their
8. White J, Levinson W, Roter D. “Oh, by the way . . .”: the closing moments of patient communication skills. J Gen Intern Med. 1995;10:375-9. [PMID:
the medical visit. J Gen Intern Med. 1994;9:24-8. [PMID: 8133347] 7472685]
9. Nightingale SD, Yarnold PR, Greenberg MS. Sympathy, empathy, and phy- 32. Spiro H. What is empathy and can it be taught? Ann Intern Med. 1992;116:
sician resource utilization. J Gen Intern Med. 1991;6:420-3. [PMID: 1744756] 843-6. [PMID: 1482433]
10. Levinson W, Stiles WB, Inui TS, Engle R. Physician frustration in commu- 33. Brock CD, Salinsky JV. Empathy: an essential skill for understanding the
nicating with patients. Med Care. 1993;31:285-95. [PMID: 8464246] physician-patient relationship in clinical practice. Fam Med. 1993;25:245-8.
11. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and phy- [PMID: 8319851]
sician responses in primary care and surgical settings. JAMA. 2000;284:1021-7. 34. Platt FW, Keller VF. Empathic communication: a teachable and learnable
[PMID: 10944650] skill. J Gen Intern Med. 1994;9:222-6. [PMID: 8014729]
12. Suchman AL, Roter D, Green M, Lipkin M Jr. Physician satisfaction with 35. Platt FW, Platt CM. Empathy: a miracle or nothing at all? Journal of Clinical
primary care office visits. Collaborative Study Group of the American Academy Outcomes Management. 1998;5:30-3.
on Physician and Patient. Med Care. 1993;31:1083-92. [PMID: 8246638] 36. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic
13. Cohen-Cole SA. The Medical Interview: The Three-Function Approach. communication in the medical interview. JAMA. 1997;277:678-82. [PMID:
Mosby: St. Louis; 1991. 9039890]
14. Coulehan JL, Block MR. The Medical Interview. Mastering Skills for Clin- 37. Charon R. The narrative road to empathy. In: Spiro H, McCrea Curnen
ical Practice. 4th ed. Philadelphia: FA Davis; 2001. MG, Peschel E, St James D, eds. Empathy and the Practice of Medicine. New
15. More ES. “Empathy” enters the profession of medicine. In: More ES, Mil- Haven, CT: Yale Univ Pr; 1993:147-59.
ligan MA, eds. The Empathic Practitioner. Empathy, Gender, and Medicine. 38. Carson RA. Beyond respect to recognition and due regard. In: Toombs SK,
New Brunswick, NJ: Rutgers Univ Pr; 1994:19-39. Barnard D, Carson RA. Chronic Illness from Experience to Policy. Bloomington,
16. Basch MF. Empathic understanding: a review of the concept and some IN: Indiana Univ Pr; 1995:105-28.
theoretical considerations. J Am Psychoanal Assoc. 1983;31:101-26. [PMID: 39. Hunter KM, Charon R, Coulehan JL. The study of literature in medical
6681414] education. Acad Med. 1995;70:787-94. [PMID: 7669155]
17. Wispe L. History of the concept of empathy. In: Eisenberg N, Strayer J, eds. 40. Novack DH, Suchman AL, Clark W, Epstein RM, Najberg E, Kaplan C.
Empathy and Its Development. Cambridge, UK: Cambridge Univ Pr; 1987:17-37. Calibrating the physician. Personal awareness and effective patient care. Working
18. Book HE. Empathy: misconceptions and misuses in psychotherapy. Am J Group on Promoting Physician Personal Awareness, American Academy on Phy-
Psychiatry. 1988;145:420-4. [PMID: 3348445] sician and Patient. JAMA. 1997;278:502-9. [PMID: 9256226]
19. Buie DH. Empathy: its nature and limitations. J Am Psychoanal Assoc. 41. Coulehan JL. Tenderness and steadiness: emotions in medical practice. Lit
1981;29:281-307. [PMID: 7264177] Med. 1995;14:222-36. [PMID: 8558910]
20. Wilmer HA. The doctor-patient relationship and the issues of pity, sympathy 42. Connelly J. Being in the present moment: developing the capacity for mind-
and empathy. Br J Med Psychol. 1968;41:243-8. [PMID: 5728595] fulness in medicine. Acad Med. 1999;74:420-4. [PMID: 10219225]
21. Strayer J. Affective and cognitive perspectives on empathy. In: Eisenberg N, 43. Epstein RM. Mindful practice. JAMA. 1999;282:833-9. [PMID: 10478689]
Strayer J, eds. Empathy and Its Development. Cambridge, UK: Cambridge Univ 44. Miller SZ, Schmidt HJ. The habit of humanism: a framework for making
Pr; 1987:218-44. humanistic care a reflexive clinical skill. Acad Med. 1999;74:800-3. [PMID:
22. Brothers LA, Finch DM. Physiological evidence for an excitatory pathway 10429589]
from entorhinal cortex to amygdala in the rat. Brain Res. 1985;359:10-20. 45. Barrett-Lennard GT. The phases and focus of empathy. Br J Med Psychol.
[PMID: 4075137] 1993;66(Pt 1):3-14. [PMID: 8485075]
23. Grattan LM, Eslinger PJ. Empirical study of empathy [Letter]. Am J Psy- 46. Gallop R, Lancee WJ, Garfinkel PE. The empathic process and its media-
chiatry. 1989;146:1521-2. [PMID: 2619825] tors. A heuristic model. J Nerv Ment Dis. 1990;178:649-54. [PMID: 2230750]
226 7 August 2001 Annals of Internal Medicine Volume 135 • Number 3 www.annals.org
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Words That Help Build Empathy Medical Writings
47. Hall JA, Roter DL, Rand CS. Communication of affect between patient and 51. Branch WT, Malik TK. Using “windows of opportunities” in brief inter-
physician. J Health Soc Behav. 1981;22:18-30. [PMID: 7240703] views to understand patients’ concerns. JAMA. 1993;269:1667-8. [PMID:
48. Larsen KM, Smith CK. Assessment of nonverbal communication in the 8455300]
patient-physician interview. J Fam Pract. 1981;12:481-8. [PMID: 7462949] 52. Pinderhughes EB. Teaching empathy: ethnicity, race and power at the cross-
49. Suchman AL, Matthews DA. What makes the patient-doctor relationship cultural treatment interface. American Journal of Social Psychology. 1984;4:5-12.
therapeutic? Exploring the connexional dimension of medical care. Ann Intern 53. Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons
Med. 1988;108:125-30. [PMID: 3276262] from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251-8.
50. Suchman AL. Control and Relation: Two Foundational Values and Their [PMID: 626456]
Consequences. In: Suchman AL, Botelho RJ, Hinton-Walker P, eds. Partnerships 54. Platt FW, Gaspar DL, Coulehan JL, Fox L, Adler AJ, Weston WW, et al.
in Healthcare: Transforming Relational Process. Rochester, NY: Univ of Roch- “Tell me about yourself”: the patient-centered interview. Ann Intern Med. 2001;
ester Pr; 1998. 134:1079-85.
Personae
In an effort to bring people to the pages and cover of Annals, the editors
invite readers to submit photographs of people for publication. We are
looking for photographs that catch people in the context of their lives and
that capture personality. Annals will publish photographs in black and white,
and black-and-white submissions are preferred. We will also accept color
submissions, but the decision to publish a photograph will be made after the
image is converted to black and white. Slides or prints are acceptable. Print
sizes should be standard (3ⴖ ⴛ 5ⴖ, 4ⴖ ⴛ 6ⴖ, 5ⴖ ⴛ 7ⴖ, 8ⴖ ⴛ 10ⴖ). Photographers
should send two copies of each photograph. We cannot return photographs,
regardless of publication. We must receive written permission to publish the
photograph from the subject (or subjects) of the photograph or the subject’s
guardian if he or she is a child. A cover letter assuring no prior publication of
the photograph and providing permission from the photographer for Annals
to publish the image must accompany all submissions. The letter must also
contain the photographer’s name, academic degrees, institutional affiliation,
mailing address, and telephone and fax numbers.
Selected Personae submissions will also appear on the cover of Annals. We
look forward to receiving your photographs.
Christine Laine, MD, MPH
Senior Deputy Editor
www.annals.org 7 August 2001 Annals of Internal Medicine Volume 135 • Number 3 227
Downloaded From: http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19988/ by a University of California San Diego User on 01/09/2017
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- PDFDokument234 SeitenPDFAnonymous Ax12P2sr100% (11)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- MetaphysicsDokument148 SeitenMetaphysicsMonizaBorges100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- 3 Days of DarknessDokument2 Seiten3 Days of DarknessIrisGuiang100% (3)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Types of Tests Used in Special EducationDokument5 SeitenTypes of Tests Used in Special EducationCbrc CebuNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Attachment and BPD PDFDokument19 SeitenAttachment and BPD PDFAnonymous fPQaCe8100% (1)
- Avoidant Restrictive Food Intake Disorder: An Illustrative Case ExampleDokument4 SeitenAvoidant Restrictive Food Intake Disorder: An Illustrative Case ExampleAnonymous fPQaCe8100% (1)
- Conflict Resolution in Community Setting (Part-II)Dokument20 SeitenConflict Resolution in Community Setting (Part-II)S.Rengasamy100% (3)
- Guidelines Switching Antidepressants - A3 PDFDokument1 SeiteGuidelines Switching Antidepressants - A3 PDFP̷s̷ʏ̷ᴄ̷ʜ̷ᴏ̷ᴛ̷ɪ̷ᴄ̷ R̷ᴀ̷ɪ̷ɴ̷ʙ̷ᴏ̷ᴡ̷ᴢ̷50% (2)
- Essay Writing FCE Part 1 - Sample Task # 5 - Technological DevelopmentsDokument3 SeitenEssay Writing FCE Part 1 - Sample Task # 5 - Technological DevelopmentsMaria Victoria Ferrer Quiroga100% (1)
- 1881 Lecture by William George LemonDokument12 Seiten1881 Lecture by William George LemonTim LemonNoch keine Bewertungen
- Paul Avis - God and The Creative Imagination - Metaphor, Symbol and Myth in Religion and Theology-Routledge (1999) PDFDokument196 SeitenPaul Avis - God and The Creative Imagination - Metaphor, Symbol and Myth in Religion and Theology-Routledge (1999) PDFCydLosekann100% (2)
- Validity & RealibilityDokument13 SeitenValidity & RealibilityaidilubaidillahNoch keine Bewertungen
- Clinical Implications of Adolescent IntrospectionDokument8 SeitenClinical Implications of Adolescent IntrospectionJoshua RyanNoch keine Bewertungen
- PPT5 - Segmentation Targeting & PositioningDokument105 SeitenPPT5 - Segmentation Targeting & PositioningSrikar ReddyNoch keine Bewertungen
- Lesson Plan - Contemporary Arts From The PhilippinesDokument4 SeitenLesson Plan - Contemporary Arts From The PhilippinesEljay Flores96% (25)
- Panic Disorder Self Help Manual September 20071Dokument40 SeitenPanic Disorder Self Help Manual September 20071Anonymous fPQaCe8Noch keine Bewertungen
- Ebook PanicmanualDokument92 SeitenEbook PanicmanualMagda MoldovanNoch keine Bewertungen
- Medical Writings: "Let Me See If I Have This Right - . - ": Words That Help Build EmpathyDokument7 SeitenMedical Writings: "Let Me See If I Have This Right - . - ": Words That Help Build EmpathyAnonymous fPQaCe8Noch keine Bewertungen
- EatingII FinnSk Rderud PDFDokument10 SeitenEatingII FinnSk Rderud PDFAnonymous fPQaCe8Noch keine Bewertungen
- 20.12 Wernicke Lancet PDFDokument14 Seiten20.12 Wernicke Lancet PDFAnonymous fPQaCe8Noch keine Bewertungen
- Psychotherapeutic Treatment For Anorexia Nervosa: A Systematic Review and Network Meta-AnalysisDokument14 SeitenPsychotherapeutic Treatment For Anorexia Nervosa: A Systematic Review and Network Meta-AnalysisAnonymous fPQaCe8Noch keine Bewertungen
- Incidence of Mild Cognitive Impairment and Alzheimer Disease in Southern Brazil PDFDokument8 SeitenIncidence of Mild Cognitive Impairment and Alzheimer Disease in Southern Brazil PDFAnonymous fPQaCe8Noch keine Bewertungen
- WFBP Guidelines PDFDokument66 SeitenWFBP Guidelines PDFAnonymous fPQaCe8Noch keine Bewertungen
- A Prospective Investigation of The Development of Borderline Personality Symptoms PDFDokument24 SeitenA Prospective Investigation of The Development of Borderline Personality Symptoms PDFAnonymous fPQaCe8Noch keine Bewertungen
- Political and Social Determinants of Life Expectancy in Less Developed CountriesDokument8 SeitenPolitical and Social Determinants of Life Expectancy in Less Developed CountriesAnonymous fPQaCe8Noch keine Bewertungen
- Eating Ones Words III PDFDokument17 SeitenEating Ones Words III PDFAnonymous fPQaCe8Noch keine Bewertungen
- A Development, Mentalization Approach To The Understandind and Treatment of BPD PDFDokument27 SeitenA Development, Mentalization Approach To The Understandind and Treatment of BPD PDFAnonymous fPQaCe80% (1)
- Eating Ones Words III PDFDokument17 SeitenEating Ones Words III PDFAnonymous fPQaCe8Noch keine Bewertungen
- Eating Ones Words I PDFDokument12 SeitenEating Ones Words I PDFAnonymous fPQaCe8Noch keine Bewertungen
- MBT Training Theory PDFDokument52 SeitenMBT Training Theory PDFAnonymous fPQaCe8Noch keine Bewertungen
- HBCJ Npev Vedw T60B PDFDokument20 SeitenHBCJ Npev Vedw T60B PDFAnonymous fPQaCe8Noch keine Bewertungen
- Metacognition, Affect Regulation and Symptom Expression - A Transdiagnostic Perspective PDFDokument7 SeitenMetacognition, Affect Regulation and Symptom Expression - A Transdiagnostic Perspective PDFAnonymous fPQaCe8Noch keine Bewertungen
- 8-Year Follow-Up of Patients Treated For Borderline Personality Disorder - Mentalization-Based Treatment Versus Treatment As Usual PDFDokument8 Seiten8-Year Follow-Up of Patients Treated For Borderline Personality Disorder - Mentalization-Based Treatment Versus Treatment As Usual PDFAnonymous fPQaCe8Noch keine Bewertungen
- Clay Sculpting of Mother and Child Figures Encourages Mentalization PDFDokument9 SeitenClay Sculpting of Mother and Child Figures Encourages Mentalization PDFAnonymous fPQaCe8Noch keine Bewertungen
- Canmat 2013Dokument44 SeitenCanmat 2013Lucas GmrNoch keine Bewertungen
- The Problem With Problem Behaviors - A Systematic Review of The Association Between Individual Patient Behavioral and Psychological Symptoms and Caregiver Depression and Burden Within The Dementia PDFDokument17 SeitenThe Problem With Problem Behaviors - A Systematic Review of The Association Between Individual Patient Behavioral and Psychological Symptoms and Caregiver Depression and Burden Within The Dementia PDFAnonymous fPQaCe8Noch keine Bewertungen
- Bridging The Transmission GapDokument12 SeitenBridging The Transmission GapEsteli189Noch keine Bewertungen
- Litio PDFDokument7 SeitenLitio PDFAnonymous fPQaCe8Noch keine Bewertungen
- CINP - Antidepressant MedicationsDokument207 SeitenCINP - Antidepressant MedicationsAnonymous fPQaCe8Noch keine Bewertungen
- BJP 2011 Young 336 7 PDFDokument3 SeitenBJP 2011 Young 336 7 PDFAnonymous fPQaCe8Noch keine Bewertungen
- Fahmy 2015Dokument7 SeitenFahmy 2015Yasser Alghrafy100% (1)
- CS 213 M: Introduction: Abhiram RanadeDokument24 SeitenCS 213 M: Introduction: Abhiram RanadeTovaNoch keine Bewertungen
- History YGLMDokument28 SeitenHistory YGLMJorge PsicoalternaNoch keine Bewertungen
- Work Motivation & Job Design (Lec. 6, Chap. 7) - UPDATED2Dokument14 SeitenWork Motivation & Job Design (Lec. 6, Chap. 7) - UPDATED2AnnasNoch keine Bewertungen
- Grade 1 Syllabus 2019-2020Dokument15 SeitenGrade 1 Syllabus 2019-2020SiiJuliusKhoNoch keine Bewertungen
- LR Situation Form (1) 11Dokument13 SeitenLR Situation Form (1) 11Honey Cannie Rose EbalNoch keine Bewertungen
- Local Networks: Prepared By: Propogo, Kenneth M. Burce, Mary Jane PDokument20 SeitenLocal Networks: Prepared By: Propogo, Kenneth M. Burce, Mary Jane PPatricia Nicole Doctolero CaasiNoch keine Bewertungen
- Fiuture and Future in The PastDokument11 SeitenFiuture and Future in The PastElena PorceanuNoch keine Bewertungen
- Elliot Self HandicappingDokument28 SeitenElliot Self HandicappingNatalia NikolovaNoch keine Bewertungen
- Edmund Dulac, W B Yeats and The MagiDokument23 SeitenEdmund Dulac, W B Yeats and The MagiRaphael888Noch keine Bewertungen
- RESUME, Sharad PaudyalDokument2 SeitenRESUME, Sharad PaudyalSharad PaudyalNoch keine Bewertungen
- Lesson Plan The Mountain That Loved A BIRD by Sheena E. BernalDokument6 SeitenLesson Plan The Mountain That Loved A BIRD by Sheena E. BernalSheEna Brnl100% (1)
- Succession Under Muslim Law 2Dokument12 SeitenSuccession Under Muslim Law 2Z_JahangeerNoch keine Bewertungen
- International Journal of Project Management: Miia Martinsuo, Martina HuemannDokument3 SeitenInternational Journal of Project Management: Miia Martinsuo, Martina HuemannIrfan AwanNoch keine Bewertungen
- 26 BhargaviDokument13 Seiten26 BhargaviSrishti SrivastavaNoch keine Bewertungen
- Connotative Vs Denotative Lesson Plan PDFDokument5 SeitenConnotative Vs Denotative Lesson Plan PDFangiela goc-ongNoch keine Bewertungen
- Art and Aesthetics: Name Matrix NoDokument3 SeitenArt and Aesthetics: Name Matrix NoIvan NgNoch keine Bewertungen
- Fear and Foresight PRTDokument4 SeitenFear and Foresight PRTCarrieNoch keine Bewertungen
- Linking Employee Satisfaction With ProductivityDokument6 SeitenLinking Employee Satisfaction With Productivityani ni musNoch keine Bewertungen